- 1School of Art and Design, Guangdong University of Technology, Guangzhou, China
- 2School of Literature and Media, Nanfang College Guangzhou, Guangzhou, China
- 3Institute for Design, Hebei Academy of Fine Arts, Shijiazhuang, China
- 4School of Computer Science and Technology, Taiyuan Normal University, Taiyuan, China
The rapid aging of the population in the Guangdong-Hong Kong-Macao Greater Bay Area (GBA) has increased demand for smart healthcare solutions. Artificial intelligence (AI)-based nursing technologies show promise in alleviating care burdens, yet family caregivers—often the primary decision-makers—exhibit low adoption rates due to trust issues and risk perception. This study investigated factors influencing caregivers’ behavioral intention to adopt AI nursing technologies by developing an extended Unified Theory of Acceptance and Use of Technology (UTAUT) model incorporating trust and perceived risk. A cross-sectional survey was conducted across hospitals and care institutions in the GBA (n = 163) and analyzed using Partial Least Squares Structural Equation Modeling (PLS-SEM). Results indicated that trust, perceived usefulness (performance expectancy), and institutional support (facilitating conditions) were positively associated with intention to adopt. Social influence also had a positive effect but was significantly weakened by perceived risk, while age moderated the effect of perceived difficulty on adoption intention. The findings highlight the importance of improving system transparency, tailoring interface design for older users, and building trust through institutional support, suggesting that policymakers and developers should prioritize inclusive, age-adaptive AI design and ethical governance to enhance caregiver acceptance and AI integration in older population.
1 Introduction
The global community is facing an unprecedented demographic challenge: rapid population aging. According to the Ministry of Civil Affairs and the National Working Commission on Aging of China, by the end of 2023, the number of individuals aged 60 and above in China had reached 296.97 million—21.1% of the total population—with those aged 65 and over accounting for 216.76 million (15.4%). Over the next decade, the country is projected to add more than 20 million older adults individuals annually, and the population of the oldest old (aged 80 and above) is expected to surpass 50 million by 2035 (1). This demographic shift, coupled with a rising burden of chronic disease, places immense strain on healthcare and caregiving systems.
In the economically vibrant and densely populated Guangdong–Hong Kong–Macao Greater Bay Area (GBA), population aging presents similarly urgent challenges. Ensuring access to high-quality and sustainable eldercare services has become a critical regional priority. According to a recent industry report by KPMG, the rapid advancement of artificial intelligence (AI) is reshaping opportunities in healthcare and eldercare. Over the coming decade, AI technologies are expected to drive transformative innovations—from AI-assisted diagnostic systems and personalized treatment plans to autonomous caregiving robots—potentially alleviating workforce shortages and enhancing service delivery (2).
The GBA has emerged as a testbed for AI-driven healthcare innovations. As reported by China Daily, public hospitals in Hong Kong are deploying AI systems to identify high-risk patients and enable early intervention. Locally developed models, such as the ophthalmic diagnostic system VisionFM, now demonstrate accuracy on par with or superior to expert clinicians. In Shenzhen, AI-assisted surgical planning platforms like “CARES Copilot” are being integrated into clinical practice. Collectively, these advancements signal a growing regional commitment to leveraging AI for more efficient, intelligent healthcare systems (3).
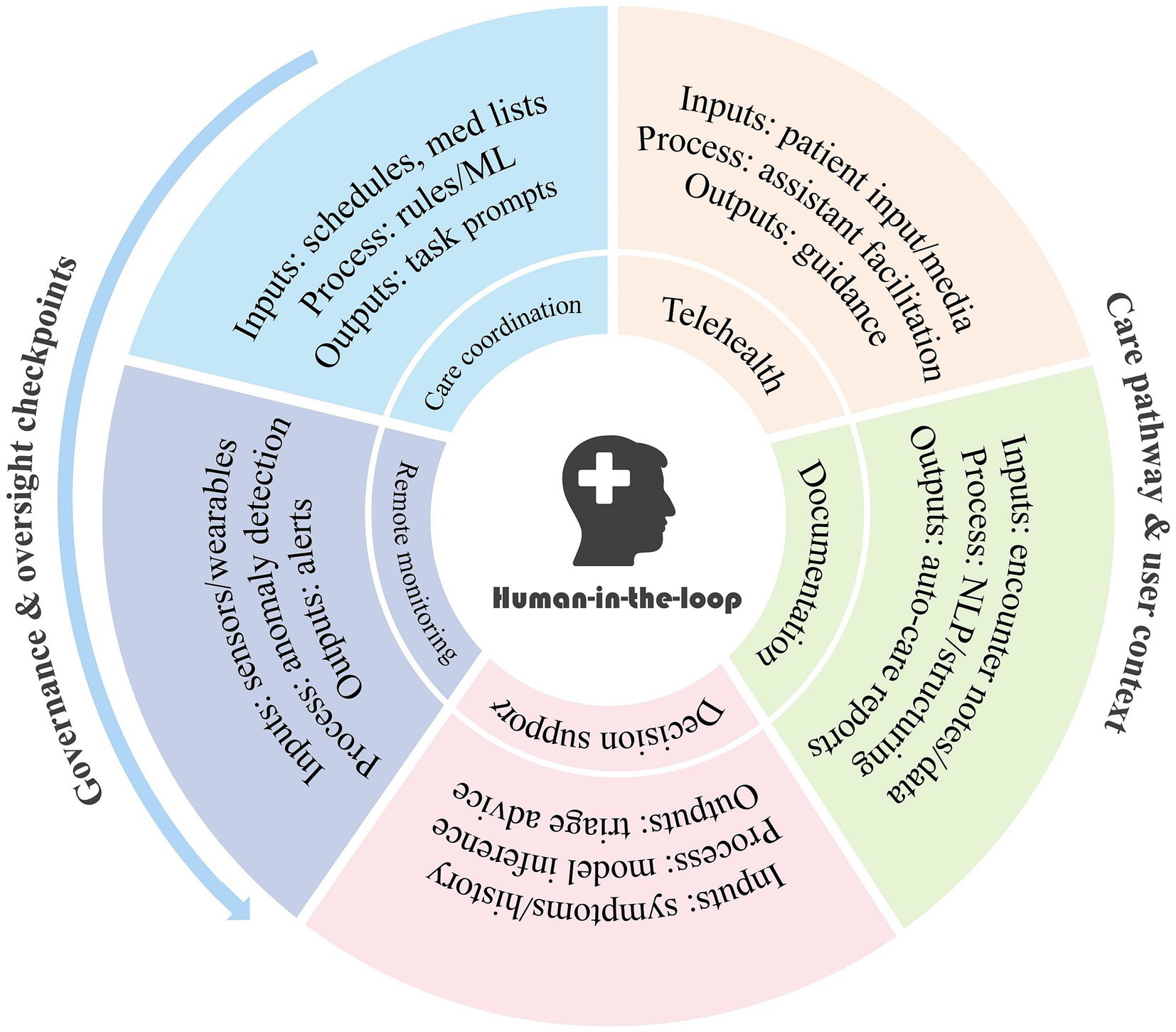
To provide readers with a clearer overview of the diversity of AI-driven healthcare systems in the region, we have summarized the main categories of current applications in Figure 1, including remote monitoring, care coordination, telehealth, documentation, and decision support.
However, the realization of AI’s full potential hinges not only on technical capability, but also on end-user acceptance. In clinical and caregiving contexts—where safety, reliability, and ethics are paramount—trust plays a pivotal role. Despite AI’s promise, widespread skepticism persists among patients and their families. Studies indicate that 65.8% of surveyed adults express low trust in the use of AI in healthcare, and 57.7% doubt the healthcare system’s ability to prevent AI-related harm (4). Even as general health and AI literacy improve, trust deficits remain, suggesting that building acceptance will require deeper engagement and transparency (5).
Mistrust is often exacerbated by negative user experiences with overhyped or underperforming AI caregiving products. Such setbacks have made trust and perceived risk key barriers to adoption. Notably, when it comes to eldercare decisions, family members frequently serve as surrogate decision-makers. Many older adults rely on family due to cognitive limitations or unfamiliarity with digital tools, depending on them to install health apps, interpret electronic health records, or facilitate telehealth consultations (6, 7).
In this context, family caregivers often become de facto gatekeepers for AI adoption. If they harbor doubts or perceive high risk, they may withhold consent for AI-assisted care, regardless of its potential benefits (8). Therefore, understanding the perspectives of patients’ families—their willingness to adopt AI caregiving technologies and the factors shaping their trust—is crucial to unlocking the transformative value of AI in eldercare. As the GBA continues to accelerate AI integration into healthcare systems, addressing the needs, concerns, and behavioral intentions of these key stakeholders is essential for achieving meaningful, user-centered innovation.
2 Research questions
Although earlier research highlighted the persistent resistance to innovation in care services (9, 10), more recent evidence indicates that the COVID-19 pandemic has accelerated the adoption of digital health and also reshaped the dynamics of trust. For instance, Park et al.’s research found that the emotions of family caregivers strongly influence their willingness to adopt medical AI (6); After surveying 2,039 respondents, Nong and at found that although health literacy has improved, respondents’ trust in the use of AI in the healthcare system remains fragile (5). Similarly, a quantitative survey and analysis by Janne Kauttonen and other researchers on trust and acceptance of artificial intelligence applications in the healthcare sector revealed that doubts about AI-assisted healthcare persisted after the pandemic, mainly stemming from emotional and privacy concerns. These findings highlight the necessity of examining the acceptance of AI care in the post-pandemic care environment (11). In the context of sensor-based health monitoring, studies by T.F. Kummer have shown that hospitals in Germany and Australia deploying intelligent surveillance systems frequently encounter user anxiety triggered by a complex interplay of factors. These include uncertainty about the system’s effectiveness, concerns over privacy and security, and emotionally driven intuitive rejection (10). Such findings underscore that, in healthcare settings, technology adoption is shaped not only by rational cost–benefit evaluations but also by psychological and affective dimensions.
Located at the crossroads of Eastern and Western medical traditions and cultural frameworks, the Guangdong–Hong Kong–Macao Greater Bay Area (GBA) presents a distinctive context in which public perceptions of medical AI are shaped by a unique interplay of influences. The bases for trust and the ways users perceive risk in this region are likely to diverge significantly from those observed elsewhere. Nevertheless, existing research on public acceptance of AI-driven healthcare solutions within the GBA remains limited, with even fewer studies concentrating on the perspectives of family caregivers—a stakeholder group of considerable importance.
Conventional frameworks for studying technology acceptance, such as the Technology Acceptance Model (TAM) and the Unified Theory of Acceptance and Use of Technology (UTAUT), are commonly utilized to evaluate factors influencing the adoption of AI in healthcare and eldercare environments (12). Despite their broad application, these models frequently overlook essential psychological components, particularly trust and perceived risk (8). Although the UTAUT’s core elements—performance expectancy, effort expectancy, social influence, and facilitating conditions—offer explanatory power in general information systems research, their ability to predict user intentions diminishes in healthcare contexts, where the stakes of decision-making and potential errors are much higher.
In such settings, trust in AI’s reliability and safety, as well as perceived risks of unintended harm, become pivotal in shaping decisions. Overlooking these factors may obscure the reasons why some family members remain unwilling to authorize the use of AI-based care technologies, even when their potential benefits are clearly demonstrated (4, 8). Therefore, there is a compelling need to extend existing theoretical models by incorporating trust as a central antecedent and perceived risk as a moderating factor in explaining AI adoption behaviors in healthcare.
Based on these insights, this study seeks to answer the following core research question:
What factors influence family members’ willingness to adopt AI caregiving technologies in the Greater Bay Area, and how do trust and perceived risk shape this decision-making process?
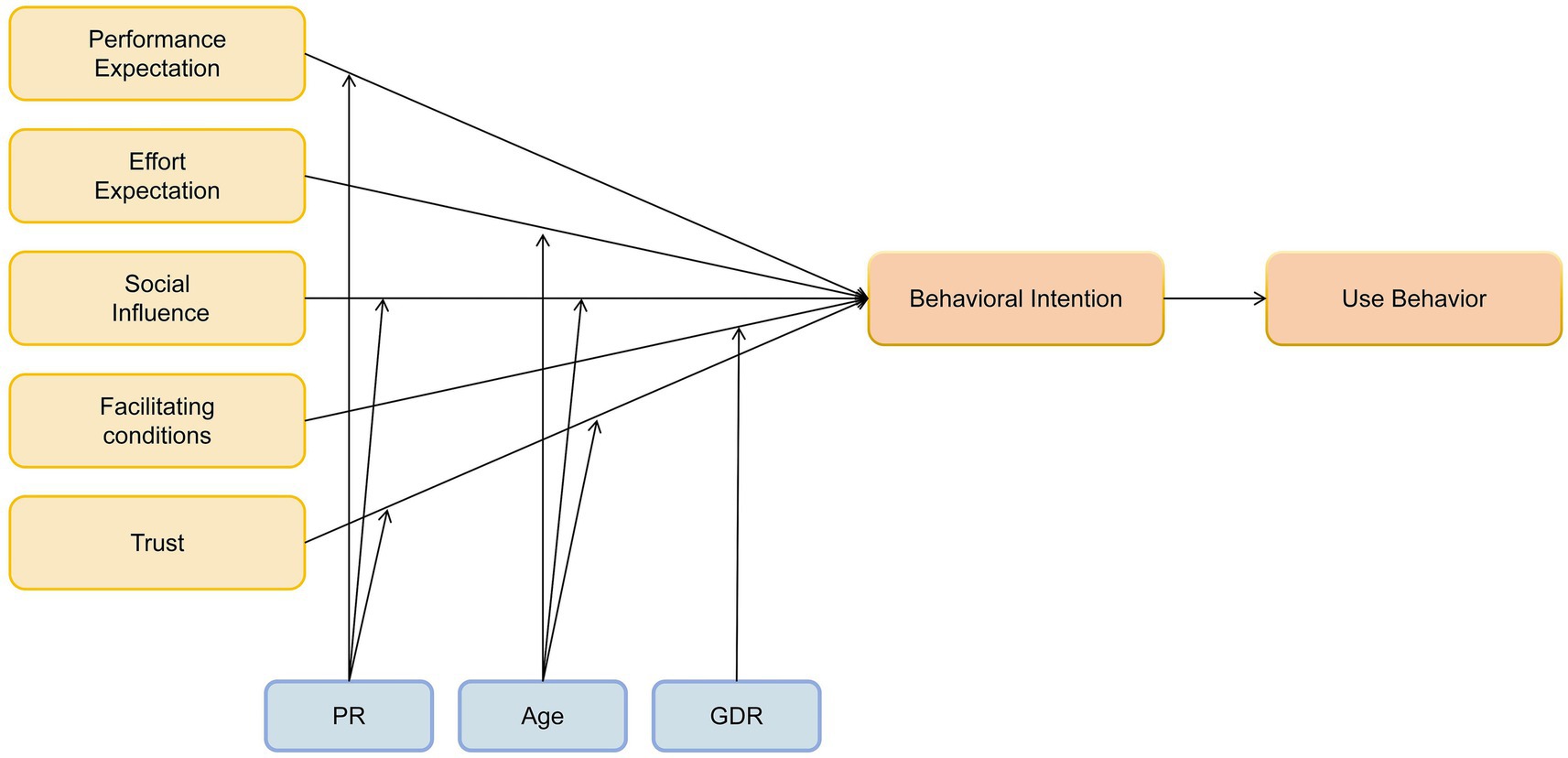
To tackle this research gap, we construct an extended conceptual framework grounded in UTAUT, incorporating trust and perceived risk as pivotal psychological factors. Specifically, the model maintains the core UTAUT predictors—performance expectancy (perceived AI utility), effort expectancy (ease of use), social influence (social encouragement/pressure), and facilitating conditions (supportive resources/infrastructure)—as foundational determinants of behavioral intention. Trust is integrated as an additional direct antecedent, defined as family members’ assurance in the safety and competence of AI-assisted caregiving. Furthermore, we propose that perceived risk—conceptualized as the subjective assessment of potential adverse consequences linked to AI use—exerts a moderating effect on the trust-intention relationship. This synthesized framework seeks to provide a more holistic explanation of the psychological drivers shaping AI adoption choices in eldercare, particularly within the Greater Bay Area’s unique socio-technical environment.
3 Literature review
3.1 The current landscape of AI in nursing
Research on artificial intelligence (AI) in nursing and healthcare has flourished in recent years, characterized by multi-directional and multi-layered advancements. Functionally, AI has been employed across a wide spectrum of applications, including medication management, patient monitoring and engagement, and optimization of nursing administration (13, 14). A comprehensive systematic review identified core applications of AI in healthcare, such as diagnostic assistance, disease management, personalized health interventions, patient self-management, and improvements in hospital operations (15). These functionalities are increasingly being extended to nursing contexts.
In clinical practice, AI-driven decision support systems (DSS) can aid nurses in assessing patient conditions and formulating personalized care plans, thereby enhancing decision accuracy and reducing workload (16). In disease management and rehabilitation, intelligent monitoring devices and algorithms enable real-time tracking of vital signs and symptoms, allowing for timely alerts and interventions by healthcare providers or family caregivers—ultimately improving patient outcomes and self-management (17). AI technologies are also reshaping administrative workflows in nursing by streamlining staff scheduling, predicting bed turnover, and minimizing paperwork, thus improving overall service efficiency (18).
Several case studies highlight tangible progress in both domestic and international contexts. For example, deep learning models have demonstrated high accuracy in diagnosing hepatic diseases, offering a promising AI-assisted approach for future hepatology care (19). In inpatient monitoring, AI-enabled sensors provide continuous 24/7 surveillance and early risk detection, potentially reducing nurses’ burden and improving patient safety. However, some family members perceive such monitoring as intrusive, citing privacy concerns, emotional detachment, and skepticism toward technological reliability (20).
In caregiving and elder services, socially assistive robots and AI-enabled smart speakers have been introduced to provide companionship, medication reminders, and emergency alerts (20). Although pilot implementations show promise in enhancing patient well-being and safety, broader adoption remains constrained by emotional, ethical, and risk-related concerns (21).
Overall, AI in nursing represents a dual function of empowerment and efficiency enhancement—enabling care professionals to perform better and expanding the reach and responsiveness of nursing services. Buchanan et al. (22) argue that AI systems can alleviate administrative burdens, allowing nurses to focus on tasks that demand human empathy and clinical judgment. This human-AI collaboration model is widely regarded as the future of nursing.
Nevertheless, scholars urge caution, noting potential risks such as algorithmic bias, decision opacity, and system failures, which necessitate robust governance mechanisms to ensure the trustworthiness and reliability of AI in clinical practice (6, 23). The key principles identified for successful AI implementation in healthcare are trustworthiness, usability, and accessibility—AI must be perceived as reliable, easy to use, and readily available to patients and their families (24).
In the Guangdong–Hong Kong–Macao Greater Bay Area (GBA), AI nursing research exhibits unique characteristics. The region boasts strong investments in healthcare innovation, with notable projects from institutions such as the Hong Kong Hospital Authority (3). Robert (20) notes that the emergence of AI caregiving technologies is likely to reshape the healthcare workforce in the near future. For instance, Hong Kong hospitals have piloted AI assistants with cartoon avatars to remind patients to take medications, and have actively gathered feedback from patients and families (3). Similarly, smart older adults care programs in Guangdong report that trust from older adults and their families is critical to AI product adoption (25).
These regional experiences underline the interactive relationship between technological innovation and user acceptance. The success of AI in nursing is not solely determined by algorithmic sophistication or hardware capabilities; it also hinges on the system’s ability to address humanistic, ethical, and experiential expectations from users—especially patients and their families.
3.2 The UTAUT model and its applications in healthcare
In information systems, the Unified Theory of Acceptance and Use of Technology (UTAUT), introduced by Venkatesh et al. (26), is a widely utilized framework. It identifies four core determinants of behavioral intention toward technology adoption: Performance Expectancy (usefulness), Effort Expectancy (ease of use), Social Influence (peer/social pressure), and Facilitating Conditions (supportive environment). Empirical evidence demonstrates that these factors collectively predict up to 70% of intention variance, underscoring UTAUT’s status as a parsimonious and comprehensive model (26).
Since its introduction, UTAUT has been applied extensively across diverse sectors, including educational technology (27), healthcare (28), Emotional support (29), e-government (30), financial technologies (31), and mobile internet (32). These applications reaffirm the model’s utility in capturing the essential cognitive and contextual determinants of technology adoption.
Nevertheless, it is acknowledged that healthcare’s unique complexities may restrict the applicability of the standard UTAUT framework. Decisions in health contexts are often emotionally intense, carry high stakes, and encompass multifaceted psychological and ethical dimensions. Key influences such as trust, privacy worries, safety concerns, and moral judgments—not explicitly covered by core UTAUT—may play a decisive role in healthcare technology adoption (4, 8, 33).
As a result, numerous studies have proposed extensions to UTAUT by incorporating Trust and Perceived Risk as additional variables. For instance, Cao et al. (34) integrated trust, risk perception, and health consciousness into an extended UTAUT model to study mobile health app adoption among Japanese youth. Their findings showed that trust significantly boosted usage intentions, while perceived risk had a clear negative effect.
Thus, although UTAUT remains a powerful theoretical lens, it requires contextual adaptation to fully capture the nuances of technology acceptance in healthcare. This is particularly true in domains such as AI-enabled caregiving, where users—especially family members of patients—may base decisions more on emotional security and perceived risk than on functionality or convenience alone (18, 35).
Building upon the UTAUT framework, this study incorporates trust and perceived risk to create a model sensitive to the Greater Bay Area’s unique cultural and institutional context. The resulting hybrid model is designed to reveal patient families’ genuine perspectives and concerns about AI in caregiving, offering richer insights into the sociotechnical dynamics underlying adoption decisions.
4 Research hypotheses
Performance expectancy, as defined by Venkatesh et al. (26), denotes an individual’s perception that adopting a specific technology will enhance their task performance or goal attainment. Empirical evidence consistently links this expectancy to stronger intentions to adopt technologies (36). Conversely, effort expectancy captures the perceived ease of use and low effort required when utilizing a technology (26). This dimension similarly predicts adoption intention (37). To enhance clarity for nursing participants, effort expectancy was assessed using reverse-scored items in this study.
Social influence is conceptualized as an individual’s belief about whether significant others (e.g., society, hospitals, physicians) expect them to use a particular technology (26). Within AI-based nursing, this translates to perceptions of AI acceptance by these key stakeholders. Facilitating conditions represent the perceived availability of resources and support enabling effective technology use (26).
Building on UTAUT’s theoretical foundation, the following hypotheses are advanced:
H0: Family caregivers' wilingness to accept AI-based nursing significantly influences their actual usage behavior.
H1: Performance expectancy has a significant positive effect on behavioral intention to use AI-based nursing.
H2: Reverse-coded effort expectancy has a significant negative effect on behavioral intention to use AI-based nursing.
H3: Social influence has a significant positive effect on behavioral intention to use AI-based nursing.
H4: Facilitating conditions have a significant positive effect on behavioral intention to use AI-based nursing.
Considering the specific context of AI in nursing, this study further proposes that trust in AI shapes nurses’ acceptance willingness (38). Therefore, an additional hypothesis is formulated:
H5: Trust in AI has a significant positive effect on family caregivers’ behavioral intention to use AI-based nursing.
As AI-based nursing is an emerging technology, nurses’ decision-making may involve more complex psychological and organizational factors. For instance, under high perceived risk, nurses may question whether AI can make accurate diagnoses; perceived risk may suppress social normative pressure, rendering social influence less effective; and there may be cognitive dissonance between perceived risk and trust (e.g., concerns about algorithmic transparency). Therefore, perceived risk is introduced as a moderating variable:
H6a: Perceived risk may weaken the positive effect of performance expectancy on behavioral intention.
H6b: Perceived risk may weaken the positive effect of social influence on behavioral intention.
H6c: Perceived risk may weaken the effect of trust in AI on behavioral intention.
Age is also introduced as a moderating variable. Older individuals tend to experience a decline in working memory capacity, making them more cognitively burdened by multi-step AI operations and more susceptible to frustration (39). Furthermore, older users are more emotionally motivated and less susceptible to social approval or authoritative opinions (40). Glikson and Woolley (38) also suggest that a high level of trust can reduce perceived risk in older adults. Based on this, the following hypotheses are proposed:
H7a: Older caregivers are more sensitive to the perceived difficulty of operating AI systems.
H7b: Age weakens the effect of social influence on behavioral intention.
H7c: Increased age strengthens the effect of trust in AI on behavioral intention.
Venkatesh and Morris (26) found that gender moderates the effect of facilitating conditions on technology acceptance, with women being more influenced by the availability of support. Additionally, research in healthcare settings has shown that female nurses tend to have greater needs for team-based resources and collaboration. Therefore, the following hypothesis is proposed (Figure 2):
H8: Sensitivity to facilitating conditions differs significantly between genders.
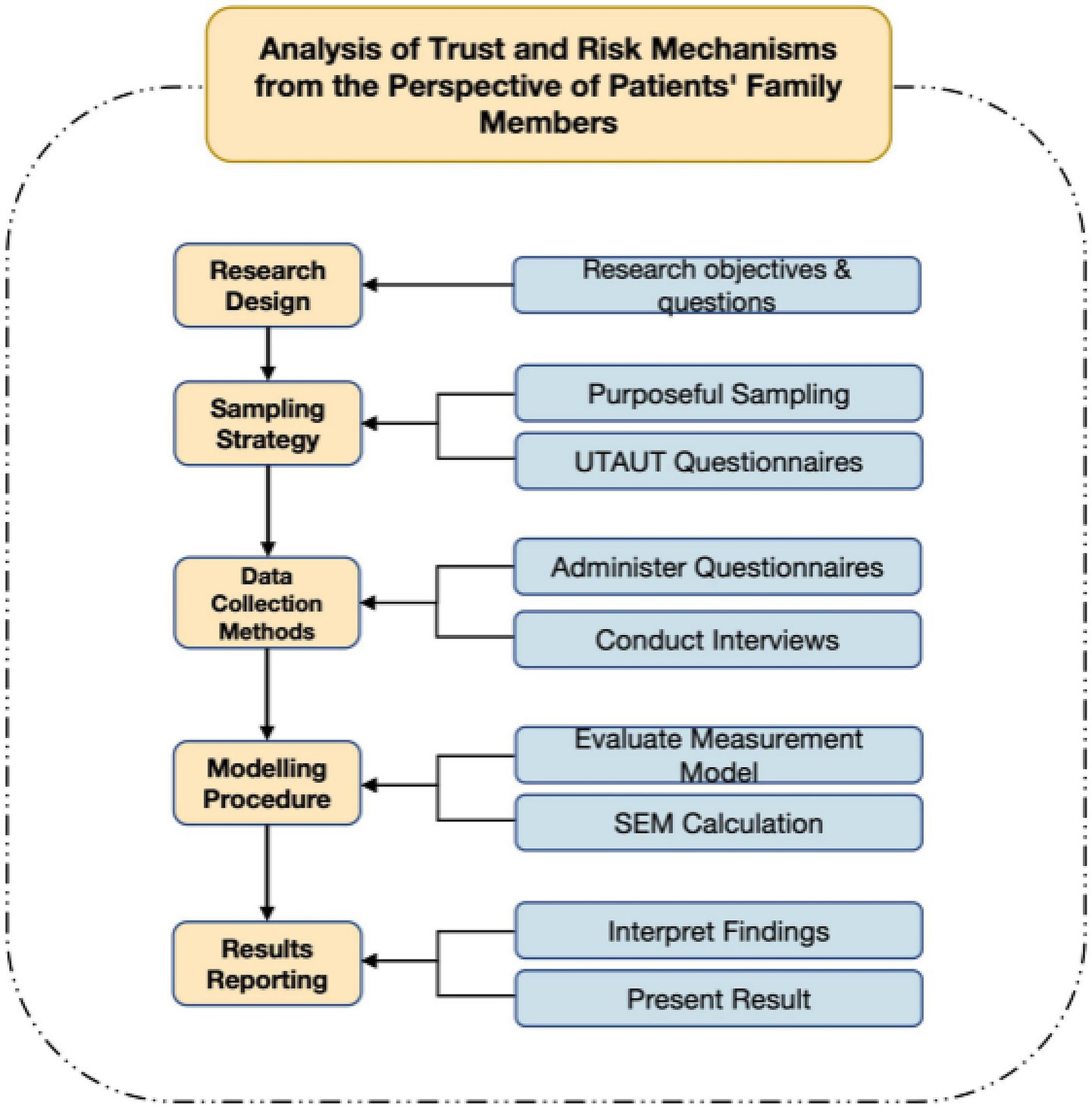
5 Research methodology
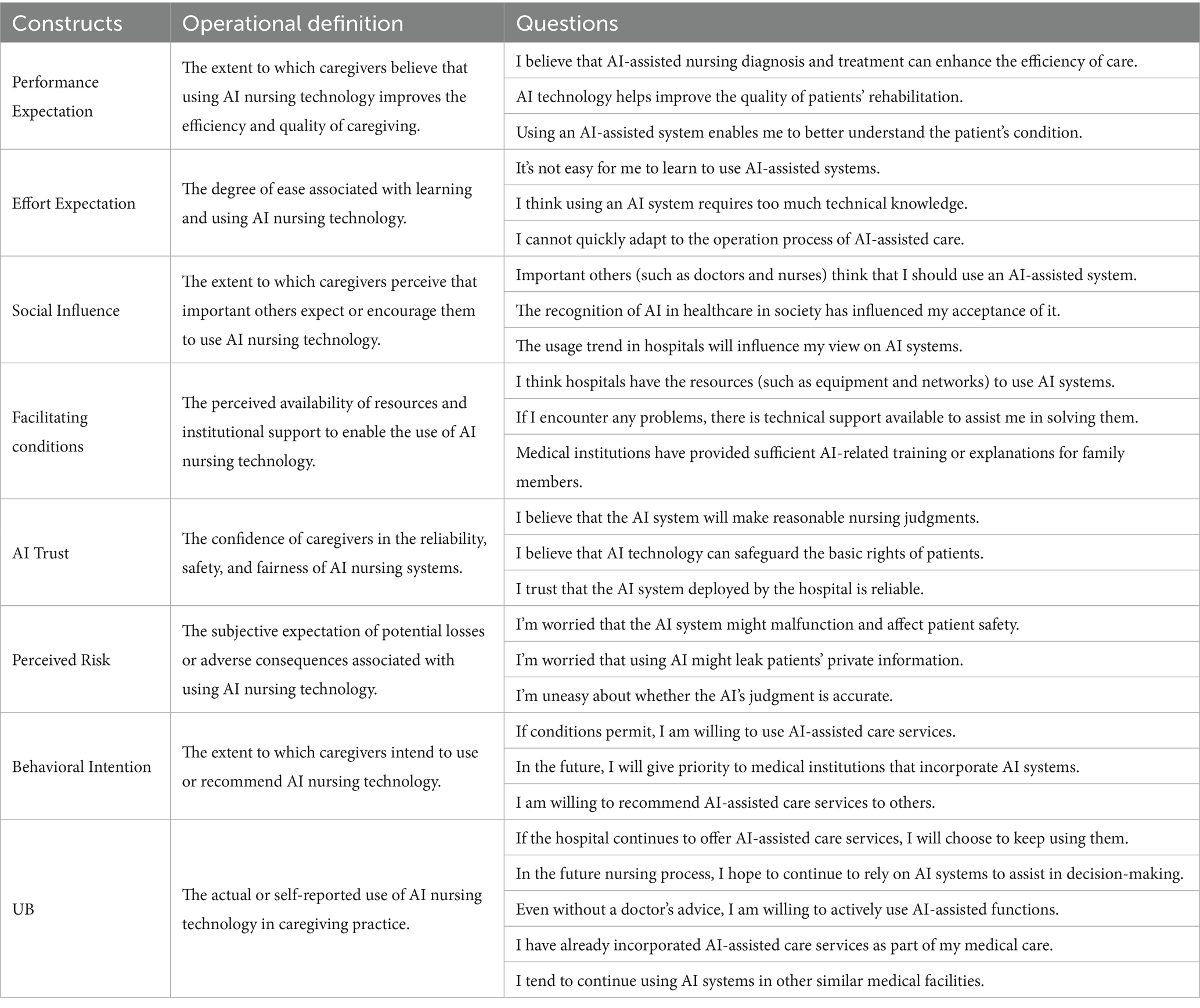
5.1 Measures and operational definitions
All constructs in this study were measured using reflective multi-item scales adapted from established literature to ensure validity and reliability. The items were rated on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). To enhance comprehension among family caregivers—who may be unfamiliar with specific AI technologies—we provided a clear explanation in the survey introduction: “AI nursing technologies refer to intelligent systems or devices that assist in older adults care, such as health monitoring sensors, medication reminders, emergency alert systems, or companion robots.” Detailed operational definitions and measurement items for each construct are provided in the Table 1.
Control variables such as age (continuous) and gender (categorical) were also included.
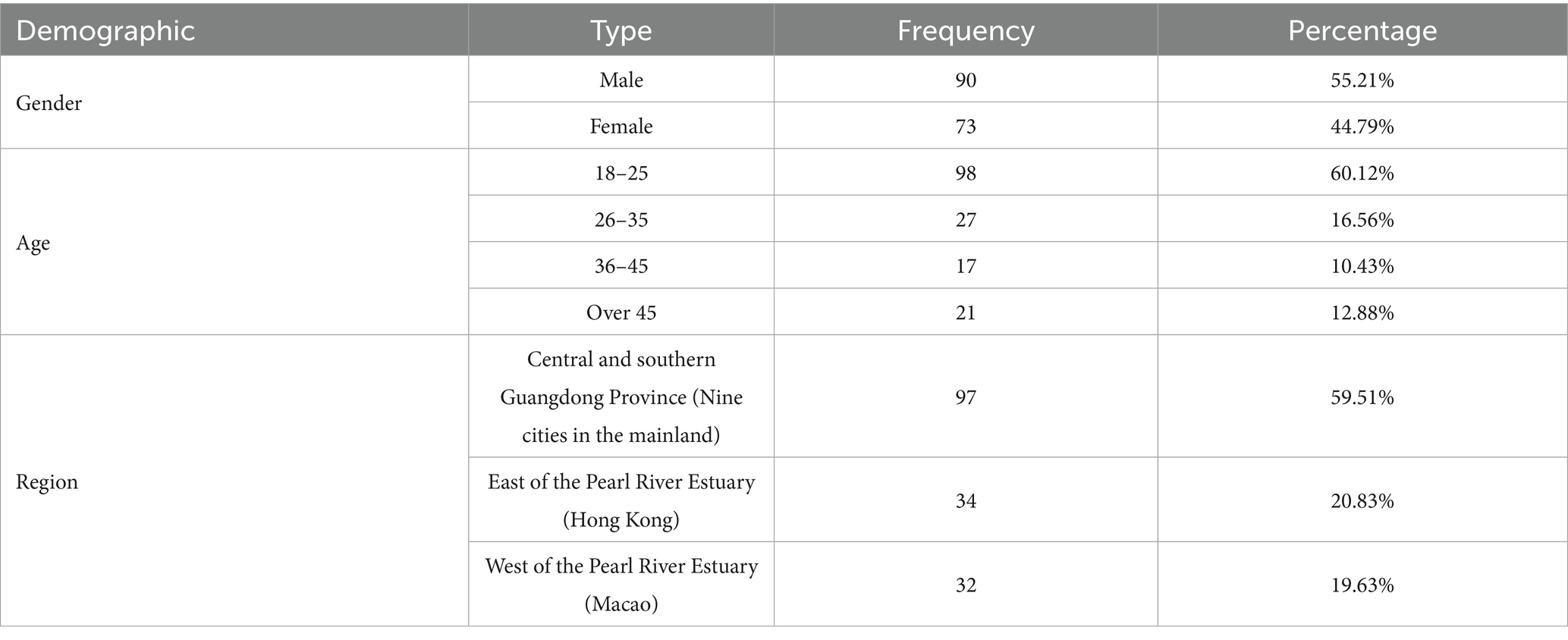
5.2 Sample recovery and analysis
This study targeted family members responsible for medical decision-making or participating in caregiving processes for older adults patients within the Guangdong-Hong Kong-Macao Greater Bay Area, encompassing nine cities in central and southern Guangdong Province, Hong Kong Special Administrative Region, and Macao Special Administrative Region (Figure 3).
Recruitment was conducted through both online and offline channels. For the online sample questionnaires were distributed via academic networks and caregiver community groups on WeChat, X (formerly Twitter), and Facebook, Participants were provided with an introductory statement explaining study objectives, ethical approval, and voluntary participation guidelines before beginning the survey. For the offline sample, paper questionnaires were distributed at partner hospitals and nursing institutions, with trained research assistants present to assist respondents if needed.
A total of 163 valid responses were collected. Among these, 89 respondents (54.6%) were recruited through hospitals, while 74 respondents (45.4%) were recruited through nursing institutions, With respect to recruitment channel, 94 participants (57.7%) were recruited online while 69 participants (42.3%) were recruited offline, This distribution ensured representation of both hospital-based and institution-based caregiving contexts, while leveraging online platforms to reach younger and digitally active caregivers.
Given the methodological requirements for structural equation modeling (SEM), psychological avoidance tendencies among caregiver populations, and the necessity for stable parameter estimates and adequate statistical power, the study aimed for at least 150 valid questionnaires. In May 2024, questionnaires were distributed throughout the Greater Bay Area. After eliminating incomplete or severely flawed responses, 163 valid samples remained for quantitative analysis. To enhance questionnaire design and clarity, the research team conducted brief supplementary interactions after questionnaire completion in select cases, involving short (1–2 min) follow-up questions such as “Which questions did you find difficult?” or “Did any options seem inconsistent with your actual experiences?” These interactions were neither audio-recorded nor thematically analyzed but rather served to verify item clarity and rationality for future questionnaire refinements; they were excluded from formal data analysis (Table 2).
For data analysis, this study utilized Partial Least Squares Structural Equation Modeling (PLS-SEM) via SmartPLS 4 software. PLS-SEM is well-suited for exploratory research involving complex models and is comparatively flexible with respect to sample size and data distribution assumptions. The analysis proceeded in two stages. First, the measurement model was evaluated by examining the reliability and validity of the latent constructs—specifically, Cronbach’s alpha and Average Variance Extracted (AVE)—as well as assessing multicollinearity through Variance Inflation Factors (VIF). Following the guideline by Hair et al. (41), VIF values exceeding 5 suggest problematic multicollinearity; in this study, all indicators showed VIF values well below this threshold, indicating no significant multicollinearity issues. Second, the structural model was assessed in terms of path coefficient significance, explanatory power (R2), and predictive relevance (Stone-Geisser’s Q2). Path coefficients were tested for statistical significance using a bootstrapping procedure with 5,000 resamples (Figure 4).
6 Research results
6.1 Reliability and validity assessment
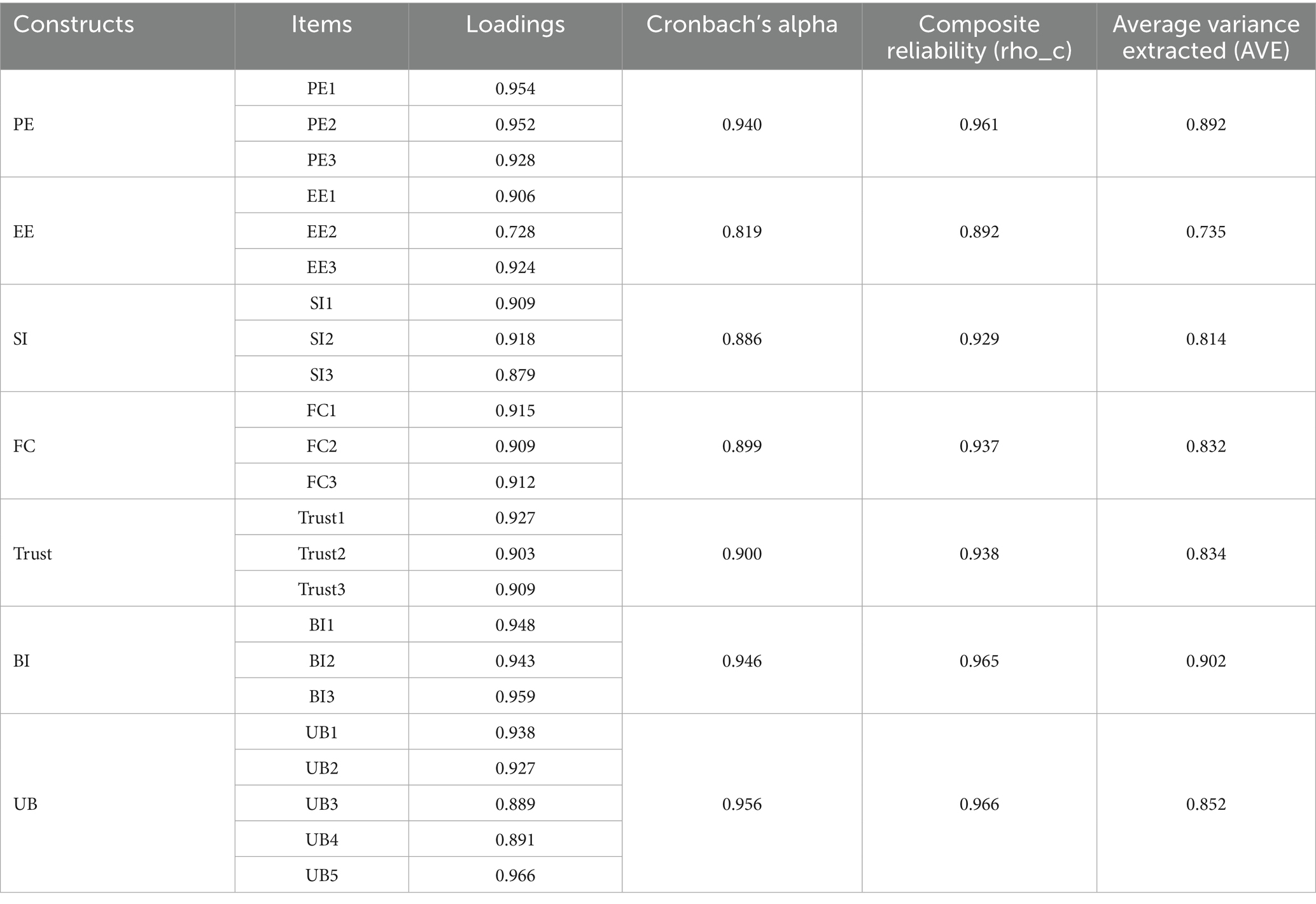
This study used the Partial Least Squares (PLS) algorithm within SmartPLS 27 software to systematically examine constructs in the questionnaire, focusing primarily on key indicators such as Cronbach’s alpha, composite reliability (CR), and factor loadings.
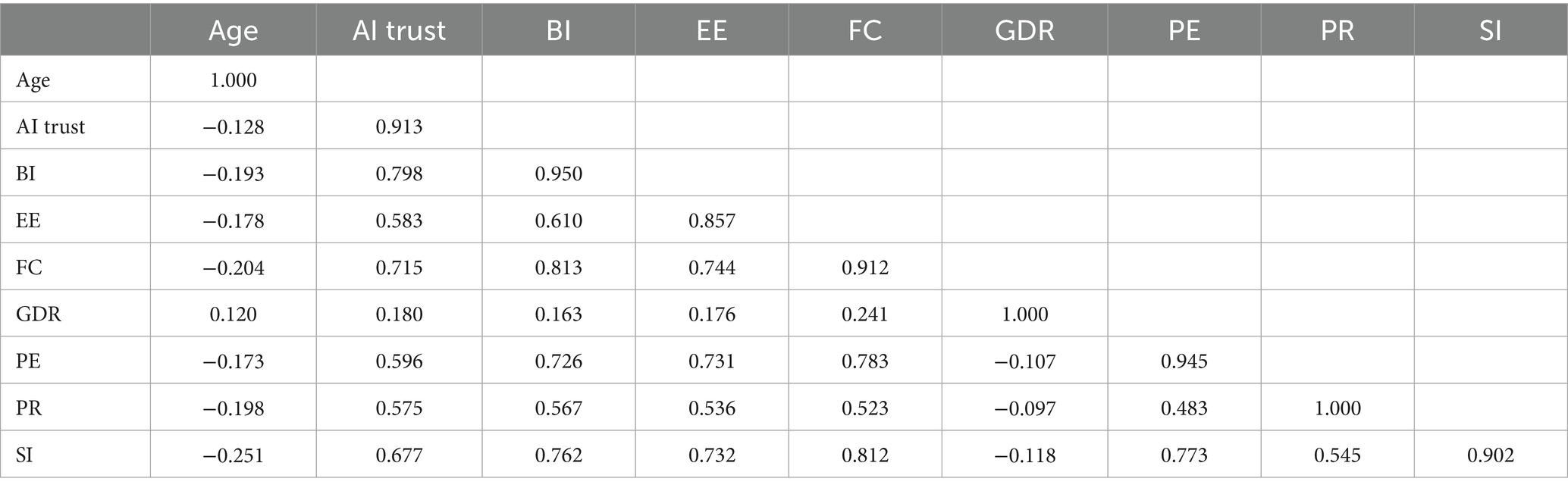
Validity was evaluated through convergent validity and discriminant validity assessments. Convergent validity was assessed using Average Variance Extracted (AVE). As indicated in Table 3, all variables demonstrated AVE values exceeding the threshold of 0.5. Cronbach’s alpha values between 0.6 and 0.7 typically represent acceptable reliability (42). Behavioral Intention had the highest AVE (0.902). Discriminant validity was assessed based on the Fornell-Larcker criterion by comparing the square roots of AVE values with the correlation coefficients between variables (Table 4). All latent variables met discriminant validity requirements, consistent with Hair et al.’s recommendations for systematic PLS modeling (43).
Overall, the measurement model exhibited ideal levels of reliability, convergent validity, and discriminant validity. Empirical data showed that Cronbach’s alpha coefficients for all latent variables exceeded the acceptable threshold of 0.7, confirming excellent internal consistency and reliability (44). AVE values were all above 0.5, confirming convergent validity. Additionally, discriminant validity was confirmed by each construct’s square root of AVE being significantly higher than its correlations with other constructs, satisfying the Fornell-Larcker criterion (41).
6.2 Structural model assessment
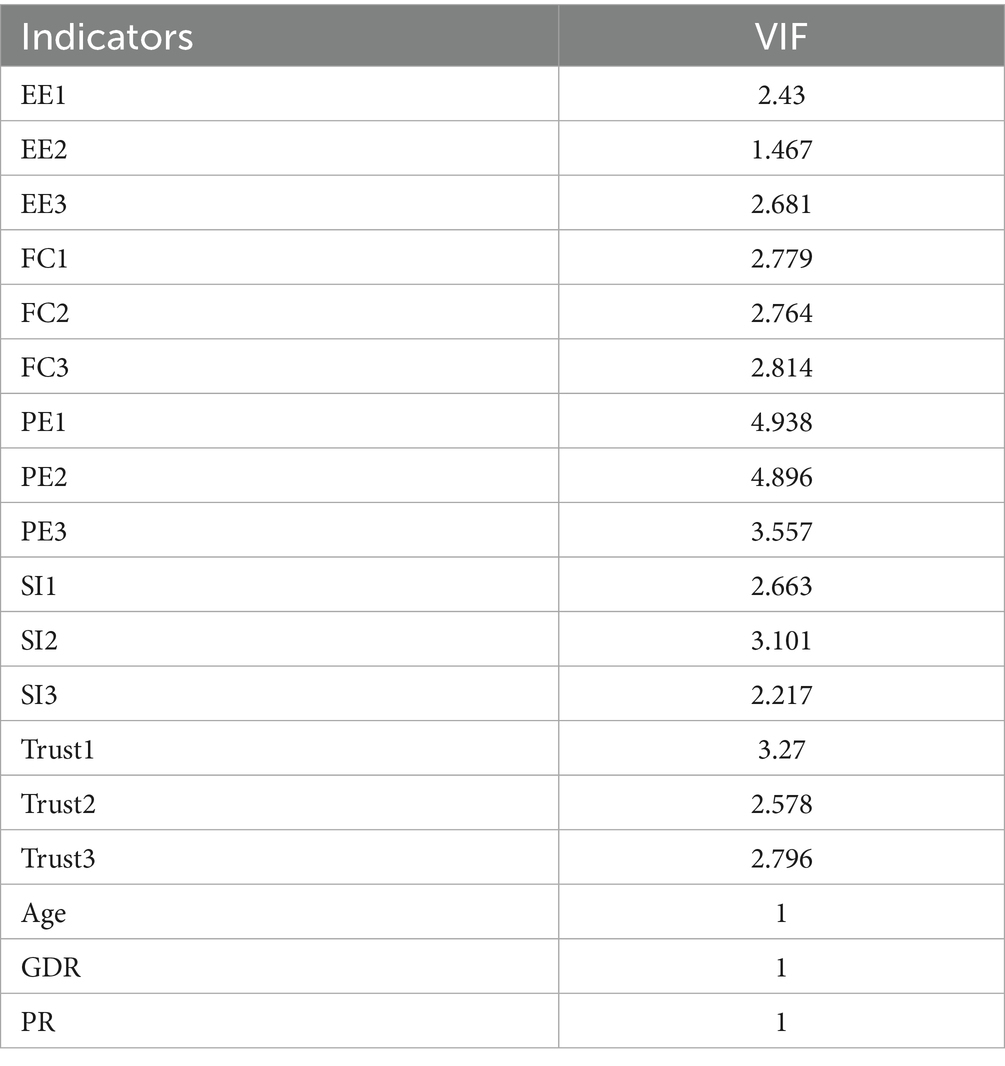
The Variance Inflation Factor (VIF) was employed as the primary diagnostic tool for multicollinearity within PLS modeling. Hair et al. recommended that a VIF value above 5 indicates significant multicollinearity issues (Table 5).
All latent variables in this study had VIF values below 5, confirming the absence of serious multicollinearity and validating the questionnaire’s construct settings. This result further indicates that questionnaire items effectively distinguished among dimensions, thus minimizing biases and distortions from multicollinearity.
6.3 Model explanatory power assessment
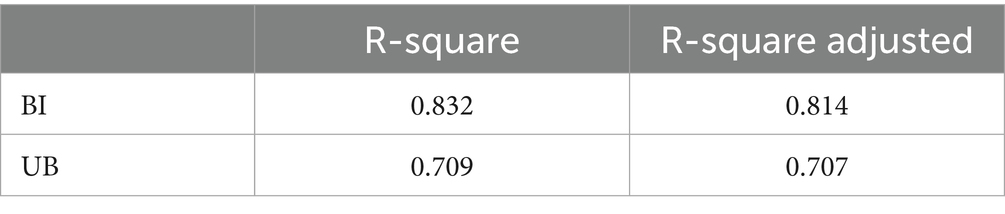
In the Partial Least Squares Structural Equation Modeling (PLS-SEM) framework, researchers estimate path coefficients and factor loadings to maximize explained variance (R2) for endogenous latent variables (Table 6). The PLS method is particularly suitable for small sample sizes and complex models, offering effective predictions among latent constructs. Hair et al. established a standardized assessment framework classifying R2 effect sizes as strong (0.75), moderate (0.50), and weak (0.25).
The results indicated a high explanatory power for behavioral intention (BI), with R2 = 0.832, significantly exceeding the typical UTAUT benchmark of 50–60%. This demonstrates that core predictors, such as performance expectancy and effort expectancy, explained 83% of the variance in behavioral intentions toward AI nursing applications. The adjusted R2 value (0.814), accounting for degrees of freedom, further underscored model robustness. Usage behavior (UB) had an R2 of 0.709 and an adjusted R2 of 0.707, showing that the model maintained strong explanatory power even after accounting for control variables and interaction effects.
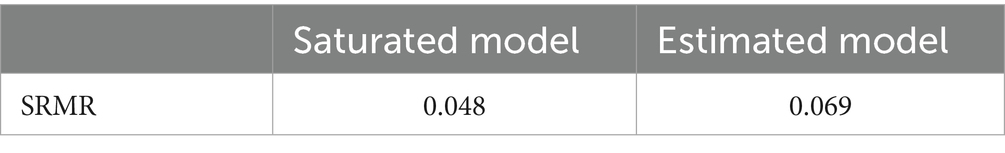
6.4 Model fit assessment
Model fit was evaluated using the Standardized Root Mean Square Residual (SRMR). According to Henseler and Sarstedt (45), an SRMR value should be below 0.14. Analysis revealed that the SRMR value of the saturated model was 0.048, and the SRMR value of the estimated model was 0.069 (Table 7). Both values were significantly below the threshold, indicating acceptable model fit.
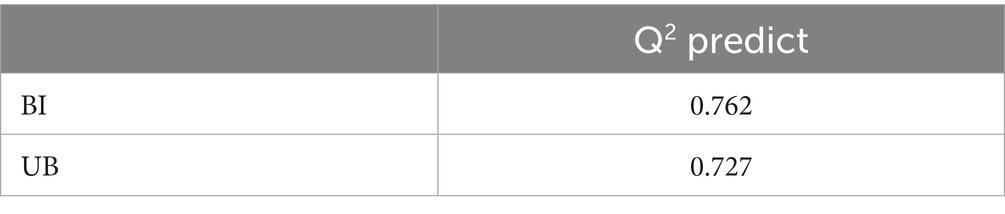
6.5 Predictive relevance assessment
Predictive relevance (Q2) is a critical indicator of predictive validity in PLS models, ranging from −∞ to 1, with higher values indicating stronger predictive capability. Using the PLSpredict algorithm, predictive relevance for behavioral intention (BI) was Q2 = 0.762, and for usage behavior (UB) was Q2 = 0.727 (Table 8). Both values substantially exceeded 0, confirming the model’s strong predictive effectiveness.
6.6 Results analysis and discussion
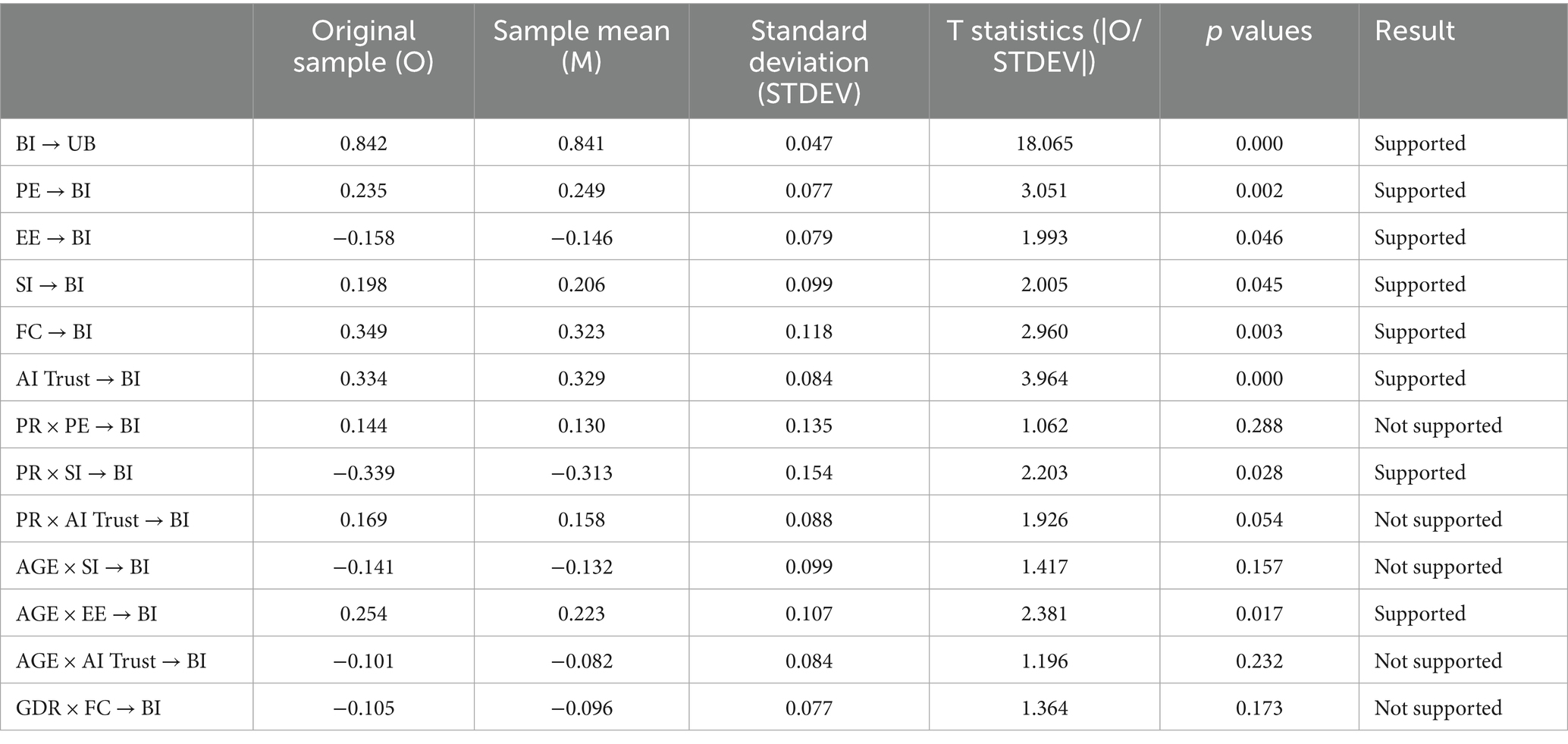
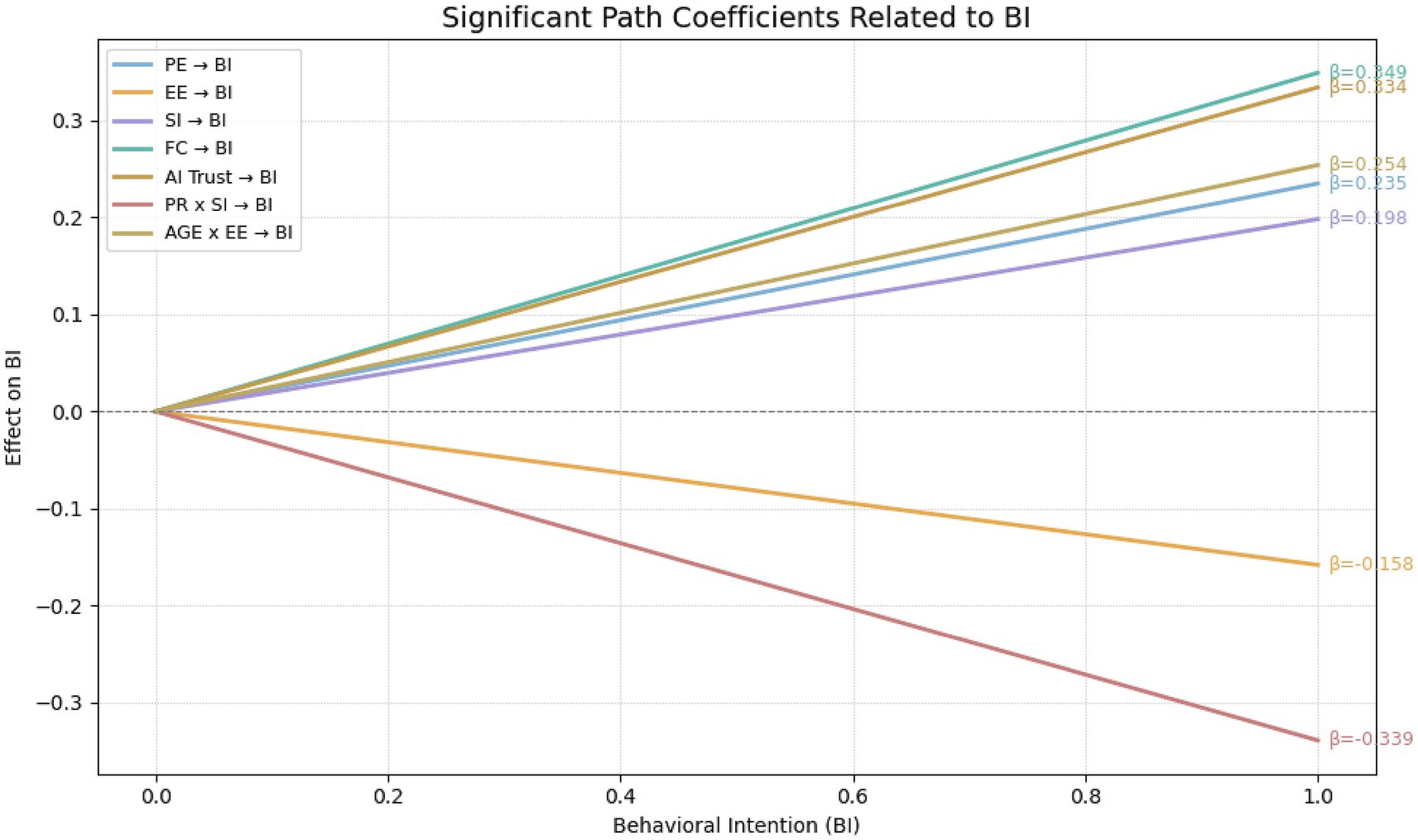
Bootstrapping with 5,000 resamples was utilized to calculate path coefficients and determine their significance. Path significance (T-statistic > 1.96 and p-value ideally < 0.05) determined hypothesis support, while the size of path coefficients indicated effect strength. Furthermore, the magnitude of each path coefficient reflects the relative strength of influence exerted by the independent variables on the corresponding dependent construct. The results of the hypothesis testing are summarized in Table 9. Figure 5 presents a bar chart illustrating the standardized β coefficients for each hypothesized path, with color coding used to differentiate between supported and unsupported hypotheses. Additionally, Figure 6 displays simple slope interaction plots, depicting variations in behavioral intention (BI) across different levels of key independent variables. These visualizations offer an intuitive representation of both the strength and directionality of the observed relationships.
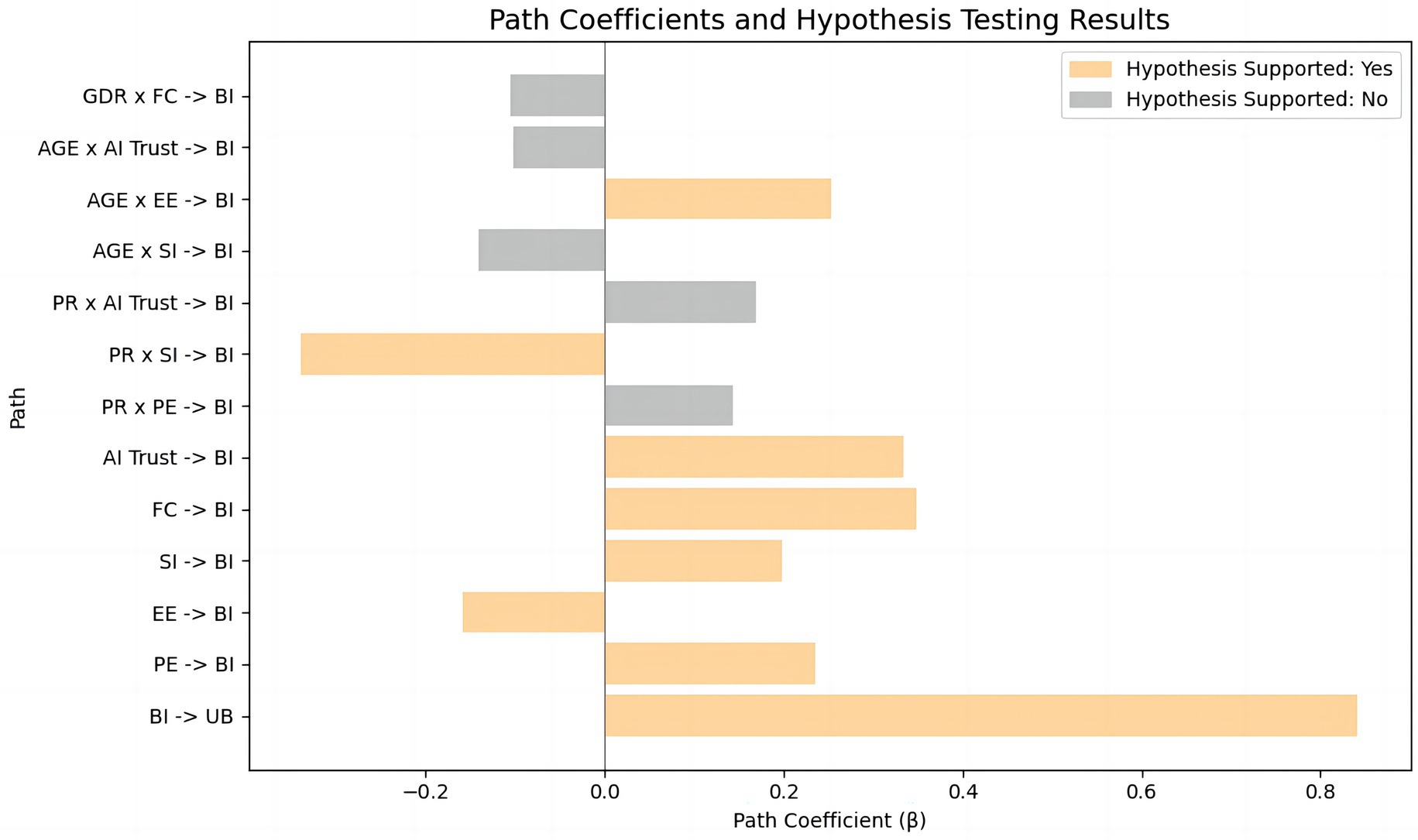 UB" and "PR x SI -> BI", both supported with positive coefficients. Other paths vary in support and coefficient size." id="fig5" loading="lazy">
UB" and "PR x SI -> BI", both supported with positive coefficients. Other paths vary in support and coefficient size." id="fig5" loading="lazy">
Figure 5. Path coefficients and hypothesis testing results.
6.6.1 Supported hypotheses
The path from Behavioral Intention (BI) to Usage Behavior (UB) was highly significant (β = 0.842, t = 18.065, p < 0.001), confirming the strong translation from AI nursing intention to actual usage behavior. Performance Expectancy (PE) significantly enhanced BI (β = 0.235, t = 3.051, p = 0.002), supporting H1. Reverse-coded Effort Expectancy (EE) negatively influenced BI (β = −0.158, t = 1.993, p = 0.046), supporting H2. Social Influence (SI) positively affected BI (β = 0.198, t = 2.005, p = 0.045), supporting H3. Facilitating Conditions (FC) strongly drove BI (β = 0.349, t = 2.960, p = 0.003), supporting H4. AI Trust significantly predicted BI (β = 0.334, t = 3.964, p < 0.001), supporting H5. Age significantly amplified the negative influence of EE on BI (β = 0.254, t = 2.381, p = 0.017), supporting H7a. Perceived Risk (PR) negatively moderated the relationship between SI and BI (β = −0.339, t = 2.203, p = 0.028), supporting H6b.
6.6.2 Unsupported hypotheses
Perceived Risk did not significantly moderate Performance Expectancy (H6a: β = 0.144, t = 1.062, p = 0.288), possibly due to institutional risk management in the Greater Bay Area (e.g., insurance, review mechanisms). The moderation effect of PR on AI Trust (H6c: β = 0.169, t = 1.926, p = 0.054) approached significance, suggesting potential clinical implications, possibly influenced by trust calibration mechanisms (46). Age did not significantly moderate the influence of SI on BI (H7b: β = −0.141, t = 1.417, p = 0.157), possibly due to older nurses prioritizing emotional goals over social evaluations. Similarly, Age did not significantly moderate AI Trust’s effect on BI (H7c: β = −0.101, t = 1.196, p = 0.232), perhaps reflecting heightened cognitive vigilance among older professionals in high-risk healthcare contexts. Gender’s moderating effect on FC (H8: β = −0.105, t = 1.364, p = 0.173) was not significant, likely reflecting diminished gender differences due to professional identity and widespread digital literacy.
7 Research significance and objectives
This study aimed to explore the factors influencing family caregivers’ acceptance of AI nursing technology and the underlying mechanisms, constructing and empirically testing a theoretical model integrating the Unified Theory of Acceptance and Use of Technology (UTAUT) with additional variables of trust and perceived risk. The study focused specifically on the Guangdong-Hong Kong-Macao Greater Bay Area—a region characterized by both international and local features—to provide valuable insights for promoting effective application of AI in nursing services within this region and beyond. The findings identified performance expectancy (β = 0.235, p < 0.01), facilitating conditions (β = 0.349, p < 0.01), and caregiver trust (β = 0.334, p < 0.001) as the three primary factors driving behavioral intention to use AI nursing. These results indicate that caregivers prioritize whether AI effectively reduces caregiving burdens (e.g., automated nursing reports), sufficient technical support from hospitals (e.g., 24-h equipment maintenance), and trust in algorithm reliability. Although social influence significantly enhanced usage intention (β = 0.198, p < 0.05), its effect was notably attenuated by perceived risk (moderation effect β = −0.339, p < 0.05). Furthermore, older caregivers exhibited significantly higher sensitivity to operational complexity (interaction effect of age and effort expectancy β = 0.254, p < 0.05), suggesting a need for simplified interaction designs. However, the moderating effect of age on social influence was not significant (p > 0.05), highlighting the rigorous and autonomous nature of caregivers’ decision-making processes regarding AI nursing.
Although AI systems in the Greater Bay Area span a wide spectrum—from monitoring sensors and scheduling tools to telehealth platforms and clinical decision support—their very heterogeneity contributes to uncertainty among caregivers. Even when certain systems demonstrate strong technical performance in pilot programs, caregivers often generalize concerns about malfunction, privacy, or operational complexity across all AI systems. This explains why our study found persistently low trust (β = 0.334, p < 0.001) despite evidence of effectiveness in similar contexts, and why perceived risk significantly weakened the effect of social influence (β = −0.339, p < 0.05). Building trust therefore requires not only improving algorithmic performance but also enhancing system transparency, caregiver training, and human-in-the-loop oversight mechanisms.
By focusing on caregivers as decision-makers and employing literature review and empirical analysis, this research advances social understanding of caregivers’ decision logic concerning AI nursing acceptance. It facilitates theoretical innovation in AI nursing research, shifting focus from technological efficacy to family acceptance mechanisms, and highlights how risk perception reshapes technology acceptance in safety-sensitive contexts.
Within the unique social-technological and healthcare context of the Guangdong-Hong Kong-Macao Greater Bay Area, this study holds particular research value. On the one hand, the region boasts advanced medical technologies and high digital literacy, potentially leading to overall greater acceptance of AI nursing. Conversely, the differences of institutional among cities (e.g., Hong Kong, Guangzhou, Macao) add valuable complexity to regional AI adoption research. This study aimed to identify regional variations in caregiver trust and risk perception and their effects on technology adoption intentions, thus informing region-specific policy development.
8 Research limitations and future directions
This study has several limitations. First, the sample size was relatively small. Our target population—primary family members actively involved in caregiving and medical decision-making—was inherently difficult to recruit, given substantial psychological and time pressures during patient care; strict adherence to ethical standards and informed consent without inducements further reduced response rates. Second, the sample was concentrated in the Guangdong–Hong Kong–Macao Greater Bay Area and skewed younger (ages 18–25 constituted 60.12%), which limits generalizability to other age groups and regions. Model- and design-related constraints should also be noted. Although the theoretical framework included trust and perceived risk, it did not fully capture deeper ethical constructs such as algorithmic transparency and accountability mechanisms, which may partly explain why certain moderation effects (e.g., H6a, H6c) were not significant. Moreover, the cross-sectional survey design cannot reflect dynamic shifts in technology acceptance—especially adaptations in caregiver trust following real-world AI exposure. Our ethical–legal discussion remains partly conceptual and jurisdiction-specific.
While the EU Artificial Intelligence Act (Regulation (EU) 2024/1689) establishes a risk-based regime, key implementation details and timelines are still evolving; by contrast, China currently regulates AI through sector-specific instruments rather than a single comprehensive act. Likewise, patient co-ownership models (e.g., GPOC) show early feasibility in the literature but have not yet been operationalized or evaluated in our context (47–49). To address these limitations, future work will:
i. Pilot consent and portability pathways consistent with co-ownership principles;
ii. Conduct prospective fairness and harm audits (including subgroup performance and post-deployment monitoring) grounded in Ethics-by-Design and the four biomedical-ethics principles (50, 51);
iii. Align documentation (e.g., data-governance records, model cards, and logging) with emerging high-risk obligations and fundamental-rights protections highlighted by the EU framework.
In parallel, we will expand sample diversity—especially older decision-makers—strengthen cross-region comparisons, integrate ethical and institutional context variables, and adopt longitudinal designs to better illuminate trust-building mechanisms and risk-mitigation pathways in high-risk healthcare scenarios, thereby providing more precise decision-support for the sustainable implementation of smart nursing in aging societies.
Our findings also highlight the lack of formal training programs for caregivers in the use of AI-driven healthcare systems. Despite receiving some technical support, caregivers often struggled with system complexity and malfunction, which negatively affected their trust and willingness to adopt these technologies. Future studies should explore the development of structured, accessible training programs to enhance caregiver competency in using AI healthcare tools, especially for older caregivers who may face additional technological barriers. Moreover, it is essential that technical support be available, comprehensive, and responsive to caregivers’ needs to improve their experience with AI systems.
Finally, our study did not differentiate in detail between the multiple categories of AI-driven healthcare systems (e.g., monitoring, coordination, documentation), which may limit comparability across heterogeneous applications. Future research should stratify system types to better capture context-specific trust dynamics.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This study involving human subjects underwent ethical review and received formal approval from the Institutional Review Board (or Ethics Committee) of Hebei Academy of Fine Arts (protocol code HAFA20250220) on 20 February 2025. The research protocol strictly adhered to the Declaration of Helsinki principles, China’s ethical guidelines for non-clinical research, and institutional governance frameworks. Prior to participation, all individuals provided written informed consent after receiving detailed explanations of study objectives, procedures, and data handling methods.
Author contributions
CY: Formal analysis, Writing – original draft, Visualization, Methodology, Data curation, Project administration, Resources, Validation, Investigation, Software, Supervision, Conceptualization, Writing – review & editing. ZW: Formal analysis, Data curation, Writing – original draft, Software, Investigation, Conceptualization. MW: Project administration, Formal analysis, Conceptualization, Writing – original draft, Methodology, Investigation. RK: Writing – original draft, Investigation, Validation, Resources, Project administration. FY: Writing – original draft, Software, Formal analysis, Conceptualization, Investigation. CC: Data curation, Methodology, Visualization, Project administration, Validation, Supervision, Investigation, Resources, Funding acquisition, Software, Writing – review & editing, Writing – original draft, Formal analysis.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the grant GD22CYS11, with the Article Processing Charge (APC) supported by the General Program of Guangdong Province Philosophy and Social Sciences Planning.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ministry of Civil Affairs and National Working Commission on Aging. (2024). 2023 annual report on the development of national undertakings for the elderly. The State Council of the People's Republic of China. Available online at: http://www.gov.cn/lianbo/bumen/202410/P020241012307602653540.pdf
2. KPMG International. (2024). Realizing the value of AI in MedTech within Asia Pacific. Available online at: https://kpmg.com/cn/zh/home/insights/2025/03/realizing-the-value-of-ai-in-medtech-within-asia-pacific.html
3. Caudevilla, O. (2025). HK at forefront deploying AI in healthcare, innovation. China Daily Hong Kong. Available online at: https://www.chinadailyhk.com/hk/article/601492
4. Lee, AT, Ramasamy, RK, and Subbarao, A. Understanding psychosocial barriers to healthcare technology adoption: a review of TAM technology acceptance model and unified theory of acceptance and use of technology and UTAUT frameworks. Healthcare. (2025) 13:250. doi: 10.3390/healthcare13030250
5. Nong, P, and Platt, J. Patients’ trust in health systems to use artificial intelligence. JAMA Netw Open. (2025) 8:e2460628. doi: 10.1001/jamanetworkopen.2024.60628
6. Park, EH, Werder, K, Cao, L, and Ramesh, B. Why do family members reject AI in health care? Competing effects of emotions. J Manag Inf Syst. (2022) 39:765–92. doi: 10.1080/07421222.2022.2096550
7. Werder, K, Cao, L, Park, EH, and Ramesh, B. Why AI monitoring faces resistance and what healthcare organizations can do about it: an emotion-based perspective. J Med Internet Res. (2025) 27:e51785. doi: 10.2196/51785
8. Kenesei, Z, Kökény, L, Ásványi, K, and Jászberényi, M. The central role of trust and perceived risk in the acceptance of autonomous vehicles in an integrated UTAUT model. Eur Transp Res Rev. (2025) 17:8. doi: 10.1186/s12544-024-00681-x
9. Heidenreich, S, and Kraemer, T. Innovations—doomed to fail? Investigating strategies to overcome passive innovation resistance. J Prod Innov Manag. (2016) 33:277–97. doi: 10.1111/jpim.12273
10. Kummer, TF, Recker, J, and Bick, M. Technology-induced anxiety: manifestations, cultural influences, and its effect on the adoption of sensor-based technology in German and Australian hospitals. Inf Manag. (2017) 54:73–89. doi: 10.1016/j.im.2016.04.002
11. Kauttonen, J, Rousi, R, and Alamaki, A. Trust and acceptance challenges in the adoption of AI applications in health care: quantitative survey analysis. J Med Internet Res. (2025) 27:e65567. doi: 10.2196/65567
12. Alaiad, A, and Zhou, L. The determinants of home healthcare robots adoption: an empirical investigation. Int J Med Inform. (2014) 83:825–40. doi: 10.1016/j.ijmedinf.2014.07.003
13. Gao, Y, Jiang, Y, Peng, Y, Yuan, F, Zhang, X, and Wang, J. Medical image segmentation: a comprehensive review of deep learning-based methods. Tomography. (2025) 11:52. doi: 10.3390/tomography11050052
14. Martinez-Ortigosa, A, Martinez-Granados, A, Gil-Hernández, E, Rodriguez-Arrastia, M, Ropero-Padilla, C, and Roman, P. Applications of artificial intelligence in nursing care: a systematic review. J Nurs Manag. (2023) 2023:1–12. doi: 10.1155/2023/3219127
15. Al Khatib, I, and Ndiaye, M. Examining the role of AI in changing the role of nurses in patient care: systematic review. JMIR Nurs. (2025) 8:e63335. doi: 10.2196/63335
16. Topaz, M, Murga, L, Gaddis, KM, McDonald, MV, Bar-Bachar, O, Goldberg, Y, et al. Mining fall-related information in clinical notes: comparison of rule-based and novel word embedding-based machine learning approaches. J Biomed Inform. (2019) 90:103103. doi: 10.1016/j.jbi.2019.103103
17. Almagharbeh, WT. The impact of AI-based decision support systems on nursing workflows in critical care units. Int Nurs Rev. (2025) 72:e13011. doi: 10.1111/inr.13011
18. Rony, MKK, Kayesh, I, Bala, SD, Akter, F, and Parvin, MR. Artificial intelligence in future nursing care: exploring perspectives of nursing professionals—a descriptive qualitative study. Heliyon. (2024) 10:e25718. doi: 10.1016/j.heliyon.2024.e25718
19. Zhou, LQ, Wang, JY, Yu, SY, Wu, GG, Wei, Q, Deng, YB, et al. Artificial intelligence in medical imaging of the liver. World J Gastroenterol. (2019) 25:672–82. doi: 10.3748/wjg.v25.i6.672
20. Robert, N. How artificial intelligence is changing nursing. Nurs Manag. (2019) 50:30–9. doi: 10.1097/01.NUMA.0000578988.56622.21
21. Loewenstein, GF, Weber, EU, Hsee, CK, and Welch, N. Risk as feelings. Psychol Bull. (2001) 127:267–86. doi: 10.1037/0033-2909.127.2.267
22. Buchanan, C, Howitt, ML, Wilson, R, Booth, RG, Risling, T, and Bamford, M. Predicted influences of artificial intelligence on the domains of nursing: scoping review. JMIR Nurs. (2020) 3:e23939. doi: 10.2196/23939
23. Werder, K, Cao, L, Ramesh, B, and Park, EH. Empower diversity in AI development. Commun ACM. (2024) 67:31–4. doi: 10.1145/3676885
24. Balagurunathan, Y, Mitchell, R, and El Naqa, I. Requirements and reliability of AI in the medical context. Phys Med. (2021) 83:72–8. doi: 10.1016/j.ejmp.2021.02.024
25. China Radio International. (2025). Guangdong advances smart elderly care through technological innovation. Available online at: https://gd.cri.cn/n/20250318/4e7d6bc8-d694-3212-ca17-7b70b8887294.html
26. Venkatesh, V, and Morris, MG. Why don't men ever stop to ask for directions? Gender, social influence, and their role in technology acceptance and usage behavior. MIS Q. (2000) 24:115–39. doi: 10.2307/3250981
27. Kahnbach, L, Hase, A, Kuhl, P, and Lehr, D. Explaining primary school teachers’ intention to use digital learning platforms for students’ individualized practice: comparison of the standard UTAUT and an extended model. Front Educ. (2024) 9:1353020. doi: 10.3389/feduc.2024.1353020
28. Hassan, I, Murad, M, El-Shekeil, I, and Liu, J. Extending the UTAUT2 model with a privacy calculus model to enhance the adoption of a health information application in Malaysia. Informatics. (2022) 9:31. doi: 10.3390/informatics9020031
29. Fu, K, Ye, C, Wang, Z, Liu, Z, Wu, M, and Yuan, Y. Ethical dilemmas and the reconstruction of subjectivity in digital mourning in the age of AI: an empirical study on the acceptance intentions of bereaved family members of cancer patients. Front Digit Health. (2025) 7:1618169. doi: 10.3389/fdgth.2025.1618169
30. Zeebaree, M, Agoyi, M, and Aqel, M. Sustainable adoption of e-government from the UTAUT perspective. Sustainability. (2022) 14:5370. doi: 10.3390/su14095370
31. Rahi, S, Mansour, M, Alghizzawi, M, and Alnaser, F. Integration of UTAUT model in internet banking adoption context. J Res Interact Mark. (2019). doi: 10.1108/jrim-02-2018-0032
32. Al-Saedi, K, Al-Emran, M, Ramayah, T, and Abusham, E. Developing a general extended UTAUT model for M-payment adoption. Technol Soc. (2020) 62:101293. doi: 10.1016/j.techsoc.2020.101293
33. Lai, CY, Cheung, KY, Chan, CS, and Law, KK. Integrating the adapted UTAUT model with moral obligation, trust and perceived risk to predict ChatGPT adoption for assessment support: a survey with students. Comput Educ Artif Intelli. (2024) 6:100246. doi: 10.1016/j.caeai.2024.100246
34. Cao, J, Kurata, K, Lim, Y, Sengoku, S, and Kodama, K. Social acceptance of mobile health among young adults in Japan: an extension of the UTAUT model. Int J Environ Res Public Health. (2022) 19:15156. doi: 10.3390/ijerph192215156
35. Wennberg, J, and Gittelsohn, A. Small area variations in health care delivery: a population-based health information system can guide planning and regulatory decision-making. Science. (1973) 182:1102–8. doi: 10.1126/science.182.4117.1102
36. Kumar, JA, and Bervell, B. Google classroom for mobile learning in higher education: modelling the initial perceptions of students. Educ Inf Technol. (2019) 24:1793–817. doi: 10.1007/s10639-018-09858-z
37. Hu, S, Laxman, K, and Lee, K. Exploring factors affecting academics’ adoption of emerging mobile technologies—an extended UTAUT perspective. Educ Inf Technol. (2020) 25:4615–35. doi: 10.1007/s10639-020-10171-x
38. Glikson, E, and Woolley, AW. Human trust in artificial intelligence: review of empirical research. Acad Manag Ann. (2020) 14:627–60. doi: 10.5465/annals.2018.0057
39. Morris, M, Schindehutte, M, and Allen, J. The entrepreneur's business model: toward a unified perspective. J Bus Res. (2005) 58:726–35. doi: 10.1016/j.jbusres.2003.11.001
40. Carstensen, LL, Mikels, JA, and Mather, M. Aging and the intersection of cognition, motivation, and emotion In: JE Birren and KW Schaie, editors. Handbook of the psychology of aging : Academic Press (2006). 343–62.
41. Hair, JF, Sarstedt, M, Hopkins, L, and Ringle, CM. Partial least squares structural equation modeling: an emerging tool in business research. J Bus Res. (2018) 85:326–37.
42. Ursachi, G, Horodnic, IA, and Zait, A. How reliable are measurement scales? External factors with indirect influence on reliability estimators. Proc Econ Finan. (2015) 20:679–86. doi: 10.1016/S2212-5671(15)00123-9
43. Hair, JF, Sarstedt, M, Pieper, TM, and Ringle, CM. The use of partial least squares structural equation modeling in strategic management research: a review of past practices and recommendations for future applications. Long Range Plan. (2012) 45:320–40. doi: 10.1016/j.lrp.2012.09.008
44. Mator, TA. Understanding Cronbach’s alpha: a guide to internal consistency reliability. J Med Educ. (2019) 84:1234–45.
45. Henseler, J, and Sarstedt, M. Goodness-of-fit indices for partial least squares path modeling. Comput Stat. (2013) 28:565–80. doi: 10.1007/s00180-012-0317-1
46. Zhang, Y., Liao, Q. V., and Bellamy, R. K. (2020). “Effect of confidence and explanation on accuracy and trust calibration in AI-assisted decision making.” in Proceedings of the 2020 conference on fairness, accountability, and transparency. pp. 295–305.
47. Davids, J, ElSharkawy, M, Lidströmer, N, Ashrafian, H, and Herlenius, E. Technical sandbox for a global patient co-owned cloud (GPOC). BMC Digit Health. (2024) 2:74. doi: 10.1186/s44247-024-00128-2
48. Lidströmer, N, Davids, J, ElSharkawy, M, Ashrafian, H, and Herlenius, E. Systematic review and meta-analysis for a global patient co-owned cloud (GPOC). Nat Commun. (2024) 15:2186. doi: 10.1038/s41467-024-46503-5
49. Lidströmer, N, Davids, J, ElSharkawy, M, Ashrafian, H, and Herlenius, E. A summit on a global patient co-owned cloud (GPOC). BMC Digital Health. (2024) 2:75. doi: 10.1186/s44247-024-00112-w
50. Brey, P, and Dainow, B. Ethics by design for artificial intelligence. AI Ethics. (2024) 4:1265–77. doi: 10.1007/s43681-023-00330-4
Keywords: AI nursing technologies, family caregivers, trust, perceived risk, UTAUT
Citation: Ye C, Wang Z, Wu M, Kang R, Yuan F and Chen C (2025) Behavioral drivers of AI nursing acceptance in the Greater Bay Area: a family-caregiver perspective on trust and risk. Front. Public Health. 13:1650804. doi: 10.3389/fpubh.2025.1650804
Edited by:
Deepanjali Vishwakarma, University of Limerick, IrelandReviewed by:
Te-Chuan Chen, National Sun Yat-sen University, TaiwanHyeri Shin, Kyunh Hee University, Republic of Korea
Niklas Lidströmer, Karolinska Institutet (KI), Sweden
Copyright © 2025 Ye, Wang, Wu, Kang, Yuan and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chen Chen, Y2hlbmNoZW5AZ2R1dC5lZHUuY24=
†These authors have contributed equally to this work
 Chenxi Ye
Chenxi Ye Zeyu Wang
Zeyu Wang Miaohui Wu
Miaohui Wu Runhao Kang
Runhao Kang Fujiang Yuan
Fujiang Yuan Chen Chen
Chen Chen