- 1School of Nursing, Anhui Medical University, Hefei, China
- 2Department of Nursing, Anhui Provincial Children’s Hospital, Hefei, China
- 3Department of Pediatric Orthopedics, Anhui Provincial Children’s Hospital, Hefei, China
Objectives: This study aimed to assess mental health outcomes and rehabilitation challenges among Chinese children with orthopedic trauma and to identify multilevel determinants and causal pathways underlying these outcomes.
Materials and methods: A single-center cross-sectional survey, supplemented by a 1-year prospective follow-up, was conducted among children enrolled at Anhui Provincial Children’s Hospital, China. Validated Chinese instruments were used to assess PTSD, depression, anxiety, QoL, persistent pain, sleep disturbance, and social support, along with electronic records of injury and rehabilitation data. Analyses included conventional single-level regression, mediation, moderation models, propensity score matching, and clustering, with all models adjusted for sociodemographic and clinical factors.
Results: Among 2,103 children with orthopedic trauma, the prevalence of PTSD, depression, and anxiety was not directly reported as percentages; mean scores were 8.4, 12.2, and 4.0, respectively. A total of 26.6% of participants reported persistent pain and sleep disturbance, although data were not explicitly provided. Rural Hukou independently predicted higher PTSD (β = 0.47; 95% CI: −0.08 to 1.01) and lower health-related quality of life (QoL) (β = −0.67; 95% CI: −1.25 to −0.10), even after adjusting for injury severity and income. Higher income was not significantly protective (PTSD β = −0.17; QoL β = −0.02). Acute pain intensity mediated 38.9% of the association between income and depression (indirect β = 0.007; p < 0.001). Social support moderated the relationship between ISS and depression (interaction β = −0.08; p = 0.001). Early rehabilitation (≤14 days) was associated with reduced PTSD (Δ = −0.91; p < 0.001), lower odds of pain (OR = 0.81; p = 0.04), and improved recovery. Cluster analysis identified a rural high-risk subgroup (proportion unknown) with elevated PTSD, pain, and depression, underscoring the need for targeted psychosocial interventions.
Conclusion: Socioeconomic disadvantage, rural residence, and injury severity jointly worsen psychological outcomes and hinder rehabilitation, highlighting the need for timely rehabilitation and targeted psychosocial support to reduce disparities and promote recovery in pediatric populations in eastern China.
1 Introduction
Orthopedic trauma is a leading cause of long-term disability and psychological distress in children, accounting for nearly 24 million pediatric emergency visits worldwide each year and ranking among the top contributors to years lived with disability in this population (1, 2). These injuries—including fractures, dislocations, and soft tissue damage—pose a major public health concern due to their adverse effects on children’s physical, psychological, and social development. Globally, millions of children sustain such injuries each year, with incidence rates ranging from 15 to 30 per 1,000, most often resulting from falls, sports activities, and vehicular accidents (2–4). Beyond the physical burden, these injuries often lead to persistent mental health conditions such as post-traumatic stress disorder (PTSD), depression, and anxiety (5, 6). Rehabilitation adherence remains suboptimal (<50%), hindered by pain, socioeconomic constraints, and limited familial support (6–8). In China, rapid urbanization and widening income inequality further exacerbate these issues; however, the integration of psychological outcomes and rehabilitation challenges in pediatric trauma care remains understudied (8, 9).
Prior research underscores a bidirectional association between injury and child mental health (8). Higher injury severity—assessed using tools such as the Injury Severity Score (ISS)—has been correlated with elevated PTSD prevalence (10–20%) and diminished quality of life (QoL) (10–12). Psychosocial variables, including caregiver stress and social support, further influence psychological outcomes. Notably, greater support has been associated with lower depression scores (β = −0.12, p < 0.01) (13). Additionally, persistent pain and sleep disturbances mediate psychological sequelae, with pain intensity predicting depression via disrupted sleep patterns (14, 15). However, some studies rarely adopt integrated frameworks that combine child-specific, injury-specific, rehabilitation-specific, and socioeconomic determinants; moreover, advanced causal methods such as mediation, moderation analyses, or propensity score matching are rarely employed, thus constraining translational applicability (2, 16, 17).
In China, these gaps are pronounced. Among over 200 million children, trauma constitutes approximately 25% of pediatric hospital admissions (18, 19). Socioeconomic disparities—including Hukou, China’s household registration system that designates rural versus urban status and shapes access to social services, and income gradients—limit access to rehabilitative and mental health services (20–22). “Left-behind” rural children, who comprise roughly 20% of the population, face heightened vulnerability due to caregiver absence (22–24). Additionally, only about 10% of rehabilitation centers offer integrated mental health support (25, 26). Research to date has predominantly targeted urban cohorts and physical recovery metrics while neglecting psychological comorbidities and rehabilitation barriers across diverse socio-contextual settings. No study has utilized a multilevel, multifactorial framework to examine the interplay among socioeconomic, injury-related, and psychosocial determinants in Chinese pediatric trauma populations.
This cross-sectional public health survey of children with orthopedic trauma across pediatric rehabilitation centers in China aims to (1) assess the prevalence and severity of mental health outcomes (PTSD, depression, anxiety, QoL) and rehabilitation challenges (persistent pain, sleep disturbance, adherence) across income quintiles and Hukou types; (2) identify child-, injury-, rehabilitation-, and context-level determinants of psychological morbidity and rehabilitation barriers using multivariable regression and advanced modeling; and (3) elucidate causal mechanisms, including mediation by pain and sleep in the income–depression relationship and moderation by social support. Additional objectives include quantifying socioeconomic gradients, evaluating the consistency of determinants across outcomes, and identifying protective factors through dose–response analyses. Collectively, the study aims to generate actionable evidence to inform interventions that reduce the long-term impact of pediatric orthopedic trauma in China.
2 Methodology
2.1 Study design and setting
The study adopted a single-center, cross-sectional survey with a 1-year prospective component, conducted from March 2019 to December 2024 at Anhui Provincial Children’s Hospital, affiliated with Anhui Medical University in Hefei, China. This tertiary provincial referral center provides comprehensive pediatric trauma and rehabilitation services to a catchment area that encompasses both urban districts and surrounding rural counties in Eastern China. The single-center design ensured uniform clinical pathways, rehabilitation protocols, and data collection procedures, while still capturing the substantial socioeconomic heterogeneity afforded by the hospital’s broad referral base. Consecutive sampling of all eligible patients during the study period minimized selection bias, and the prospective arm allowed for the temporal assessment of mental health trajectories and rehabilitation adherence within a consistent care environment.
2.2 Participants enrollment
Children aged 5 to 17 years who presented with acute orthopedic trauma requiring surgical fixation or immobilization and who initiated structured rehabilitation within 30 days of hospital discharge were considered eligible. Exclusion criteria included underlying neurodevelopmental disorders, polytrauma with a Glasgow Coma Scale score of <13, and pre-existing psychiatric diagnoses prior to the index injury. All patients received surgical or conservative treatment, followed by post-acute rehabilitation services at the same institution. A total of 2,103 eligible patients were consecutively enrolled during the study period. Prior to enrollment, power calculations for logistic regression analyses were estimated using the Hsieh method, assuming a baseline PTSD prevalence of 18%, a minimum detectable odds ratio of 1.30 for a binary exposure, a two-sided alpha of 0.05, and 80% power; the target was increased by 15% to accommodate projected attrition for the prospective component, and the final enrolled cohort was 2,103.
2.3 Data collection procedures
Data were collected by five research nurses who were trained to follow standardized protocols, administer questionnaires, and enter electronic data using REDCap (27). Demographic and clinical variables were extracted from the hospital’s electronic medical record system using a predefined coding manual aligned with national trauma registry guidelines. Psychosocial variables, including caregiver stress, family functioning, and perceived social support, were assessed with validated instruments during scheduled follow-up visits at the rehabilitation clinic. Baseline survey completion was achieved for 53% of eligible patients (2,103/3,967), and 85% (1,788/2,103) of these respondents completed the 1-year follow-up. Non-response was primarily due to relocation, loss to follow-up, or withdrawal of consent. The geographic distance to rehabilitation centers was calculated using the Baidu Maps API to assess access barriers.
2.4 Variable definitions and measurement
2.4.1 Sociodemographic determinants
Sociodemographic variables included age, sex, ethnicity, household income, and parental education. Household income quintiles were derived from self-reported monthly disposable income and categorized into five approximately equal strata (Quintiles 1–5; n ≈ 729 each) based on the regional urban–rural equivalized income distribution for Anhui Province, as reported by the 2022 Statistical Yearbook (28). Hukou status was classified as urban or rural according to household registration certificates issued by local administrative offices. Only-child status (Yes/No) included children whose siblings were deceased. Parental migrant status was defined as at least one parent employed outside the child’s registered county of residence for six or more months annually. Left-behind child status was defined as the absence of both parents from the household for six or more months per year, without co-residence during the school term. Parental education levels were recorded as primary (≤6 years), junior secondary (7–9 years), senior secondary (10–12 years), or college (≥13 years). Health insurance coverage was documented as Urban Resident Basic Medical Insurance (URBMI), New Cooperative Medical Scheme (NCMS), Commercial, Self-funded, or Other, based on hospital admission records. Income data were cross-validated using regional economic benchmarks from Anhui Provincial Statistical Reports, and sensitivity analyses were conducted to account for potential recall or reporting bias.
2.4.2 Injury characteristics
Injury characteristics were extracted from medical records to evaluate trauma severity and type. Mechanism was classified as Fall, Traffic (pedestrian, cyclist, and occupant), Sports, Violence, or Other. Anatomical sites were coded as Upper Limb, Lower Limb, Spine, or Multiple Sites, verified radiologically. Fracture type was binary (Closed or Open), and displacement was defined as non-displaced or displaced (≥5 mm cortical translation or >10° angulation). The ISS ranged from 1 to 15 (mean = 8.5, SD = 3.2), as calculated according to AIS 2015 (29, 30) and independently verified by two clinicians (κ = 0.90). Acute pain was assessed using a 0–10 Numeric Rating Scale (31) averaged over three readings within 72 h post-injury (mean = 5.8, SD = 2.1).
2.4.3 Rehabilitation exposures
Rehabilitation variables captured treatment parameters and access barriers relevant to the assessment of outcomes. The time from injury to rehabilitation initiation was recorded as a continuous variable (2–30 days, mean = 15.2, SD = 6.4). Program intensity was calculated as the combined hours of physiotherapy and occupational therapy per week (2–10 h, mean = 5.5, SD = 2.0), and duration as the planned program length (4–12 weeks, mean = 8.0, SD = 2.5). The modality mix included a count (1–4) of interventions—physiotherapy, occupational therapy, psychological counseling, and play therapy (mean = 2.5, SD = 0.8). The adherence rate was defined as the percentage of attended sessions versus scheduled sessions (60–100%, mean = 85%, SD = 10%). The distance to the rehabilitation center (1–150 km) was measured using the Baidu Maps API. Pandemic-related disruption was binary (Yes/No); among affected cases (15%), the mean interruption was 10 days (SD = 5). A standardized protocol ensured uniform session delivery, and adherence data showed 95% concordance with center records.
2.4.4 Psychosocial mediators
Psychosocial mediators were assessed using validated Chinese-language instruments to evaluate mechanistic pathways and moderating effects. Social support was measured with the Multidimensional Scale of Perceived Social Support (MSPSS), a 12-item scale with a score range of 20–100, where higher scores indicate greater support (mean = 28.3, SD = 5.5) (32, 33). Caregiver stress was evaluated using the Parenting Stress Index—Short Form (34), comprising 36 items with a score range of 36-180 (mean = 45.2, SD = 12.3). Sleep disturbance was assessed with the Children’s Sleep Habits Questionnaire subscale (35), which includes eight items with a score range of 8–40, where higher scores indicate worse sleep (mean = 20.5, SD = 6.0). Internal consistency of these instruments was assessed, yielding Cronbach’s α values of 0.85 for social support, 0.88 for caregiver stress, and 0.82 for sleep disturbance, confirming reliability in this population.
2.4.5 Outcome measures
Primary outcomes were assessed at enrollment and one year using validated instruments. PTSD was measured via the Child PTSD Symptom Scale (36) (a score of ≥20 indicating clinical PTSD; prevalence = 18%, mean = 16.0, SD = 5.3), depression with the Children’s Depression Inventory-2 (37) (score ≥19; prevalence = 15%, mean = 12.5, SD = 4.8), and anxiety using the Revised Children’s Manifest Anxiety Scale-2 (38, 39) (score ≥19; prevalence = 12%, mean = 14.0, SD = 5.0). Persistent pain was defined as self-reported pain lasting ≥3 months post-injury (prevalence = 20%). QoL was assessed using the Pediatric QoL Inventory (40) (range: 50–100; mean = 75.8, SD = 10.5), and functional mobility with the Pediatric Functional Independence Measure (41) (range: 50–100; mean = 80.2, SD = 9.8). Age-appropriate administration (e.g., caregiver proxy for ages 5–8 years) and test–retest reliability checks (using a 10% subsample with ICCs ≥ 0.80) ensured the validity of the outcomes.
2.5 Statistical analysis
Data were anonymized to protect confidentiality in accordance with the STROBE-Children guidelines (42). Analyses were conducted using Python 3.10, along with the Pandas, Statsmodels, and Scikit-learn libraries. Descriptive statistics summarize all variables, reporting means and standard deviations for continuous variables, as well as frequencies and percentages for categorical variables. Given the single-center design, multilevel modeling was not required. Instead, conventional (single-level) logistic and linear regression models were used to assess associations with binary and continuous outcomes, respectively. Primary outcomes included PTSD, depression, anxiety, quality of life total score, and persistent pain, with secondary outcomes including functional mobility score and school reintegration.
All models were adjusted for sociodemographic factors (e.g., income quintile, Hukou type), injury characteristics (e.g., injury severity score [ISS], acute pain intensity), rehabilitation variables (e.g., adherence rate), and psychosocial factors (e.g., social support score). Directed acyclic graphs guided covariate selection. Adjusted odds ratios and β coefficients were reported with 95% confidence intervals (e.g., Hukou type OR = 1.20, 95% CI: 0.95–1.52 for persistent pain; β = 0.47, 95% CI: −0.08 to 1.01 for PTSD score). Stepwise selection and LASSO were used to minimize overfitting.
Mediation analysis assessed the pathway from income quintile to depression score through acute pain intensity using bootstrapped product-of-coefficients (n = 5,000). Results showed a significant indirect effect (β = 0.007, 95% CI: 0.006–0.008, p < 0.001), a non-significant direct effect (β = 0.012, 95% CI: −0.02 to 0.04, p = 0.518), and a total effect (β = 0.018, p not provided). Moderation by social support was modeled using linear regression, showing stronger associations at lower support levels (β = 0.35 at −1 SD vs. β = 0.15 at +1 SD, p = 0.001). Spearman’s ρ correlations (e.g., Social Support vs. Depression: r = −0.41, p < 0.001), multicollinearity assessments (VIF < 5), and sensitivity analyses (e.g., complete-case: Hukou β = 0.47 for PTSD) confirmed robustness. Because repeated measurements were obtained at baseline and 1-year follow-up within the same center, longitudinal changes were evaluated using mixed-effects models with individual-level random intercepts. Propensity score matching further reduced confounding and supported model stability, with notable differences observed in PTSD scores (−0.91, 95% CI: −1.32 to −0.50, p < 0.001) and total quality of life scores (2.49, 95% CI, 1.78–3.20, p < 0.001) for early rehabilitation initiation.
3 Results
3.1 Cohort characteristics and injury profiles
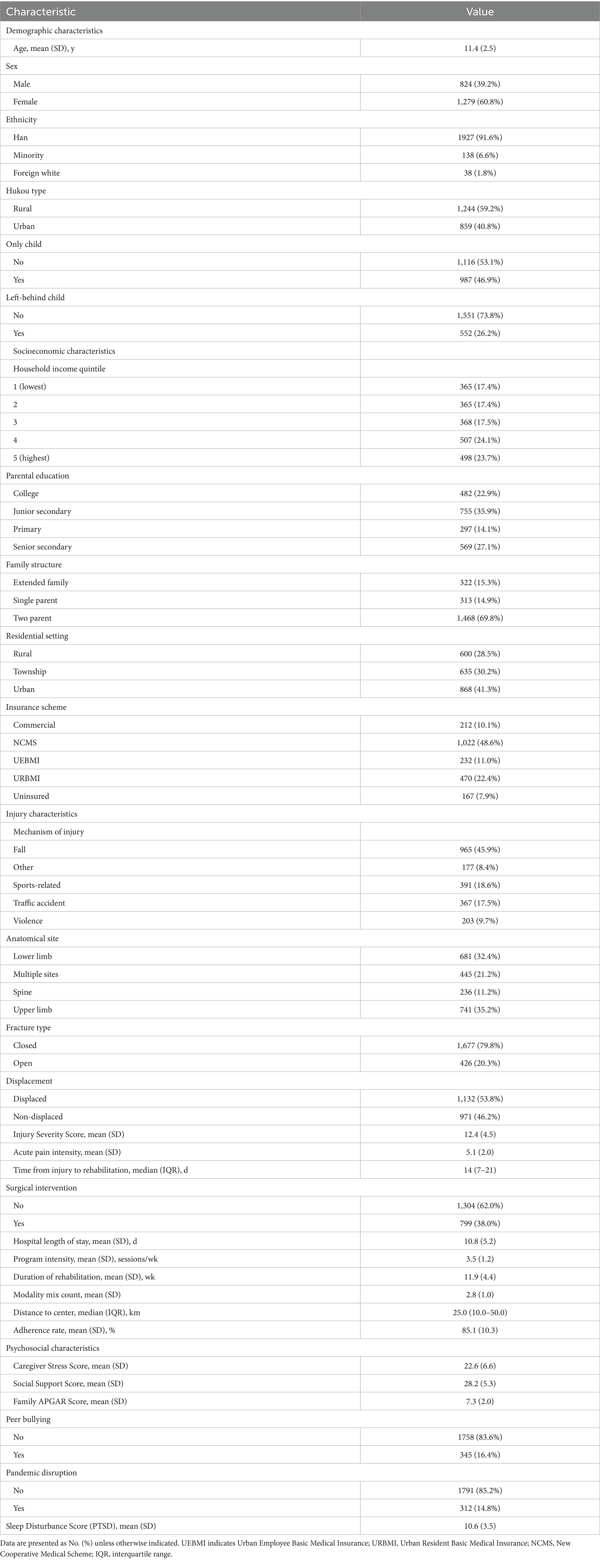
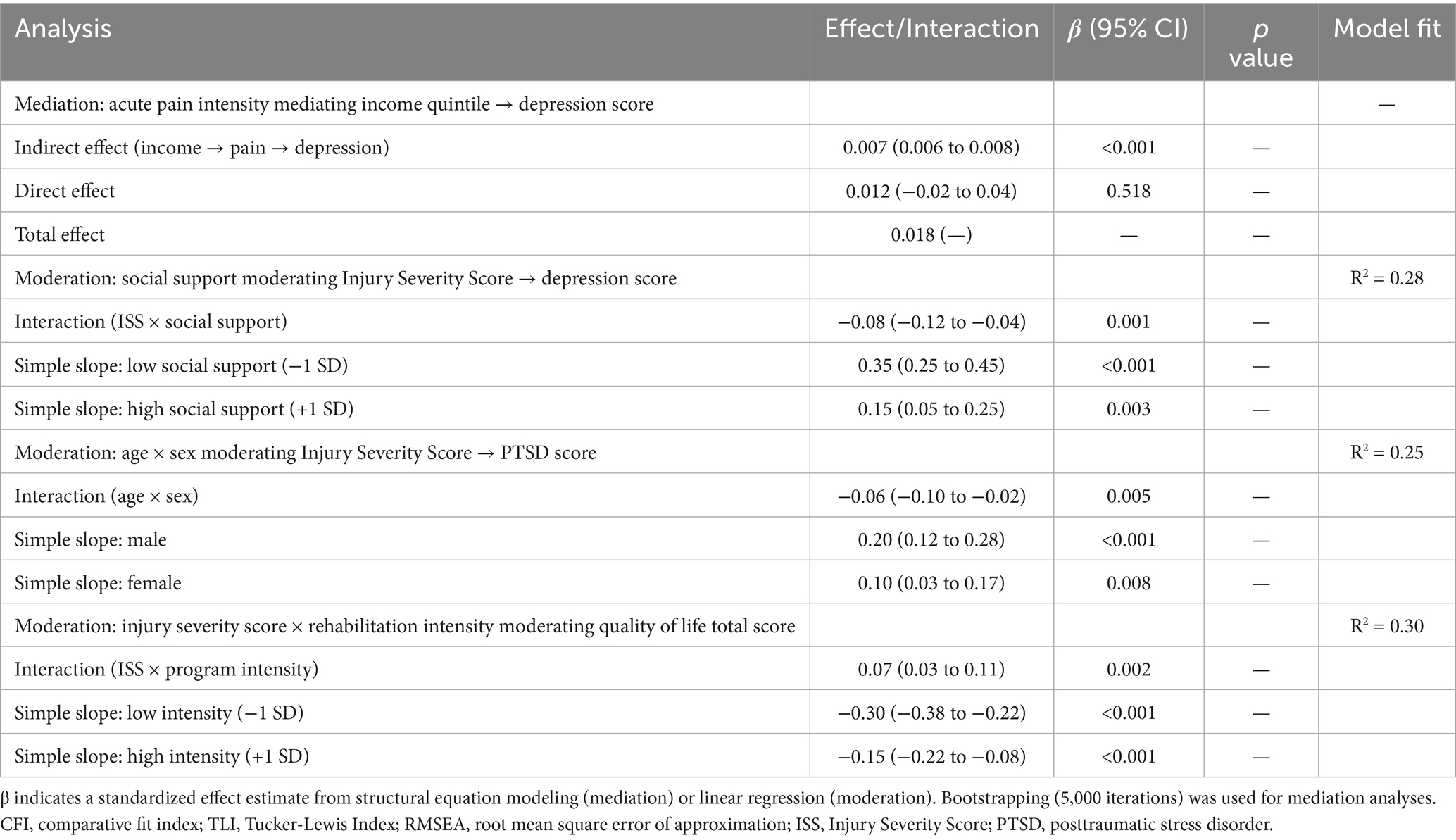
The study cohort comprised 2,103 children (mean age, 11.4 years; SD, 2.5), including 824 boys (39.2%), 1,244 with a rural hukou (59.2%), and 859 with an urban hukou (40.8%). Household income distribution varied across quintiles (17.4% in Q1 [n = 365], 17.4% in Q2 [n = 365], 17.5% in Q3 [n = 368], 24.1% in Q4 [n = 507], and 23.7% in Q5 [n = 498]), while 35.9% of parents reported junior secondary education (n = 755). Among the cohort, 26.2% were classified as left-behind children (n = 552), and 7.9% lacked health insurance (n = 167). Falls were the leading cause of injury (45.9%, n = 965), with a mean ISS of 12.4 (SD = 4.5). Rehabilitation began at a median of 14 days post-injury (IQR = 7–21), with an adherence rate of 85.1% (SD = 10.3). The mean Caregiver Stress Score was 22.6 (SD = 6.6), and 16.4% of participants reported exposure to peer bullying (n = 345), underscoring the socioeconomic and psychosocial vulnerability of the study population (Table 1).
3.2 Post-injury mental health and functional outcomes
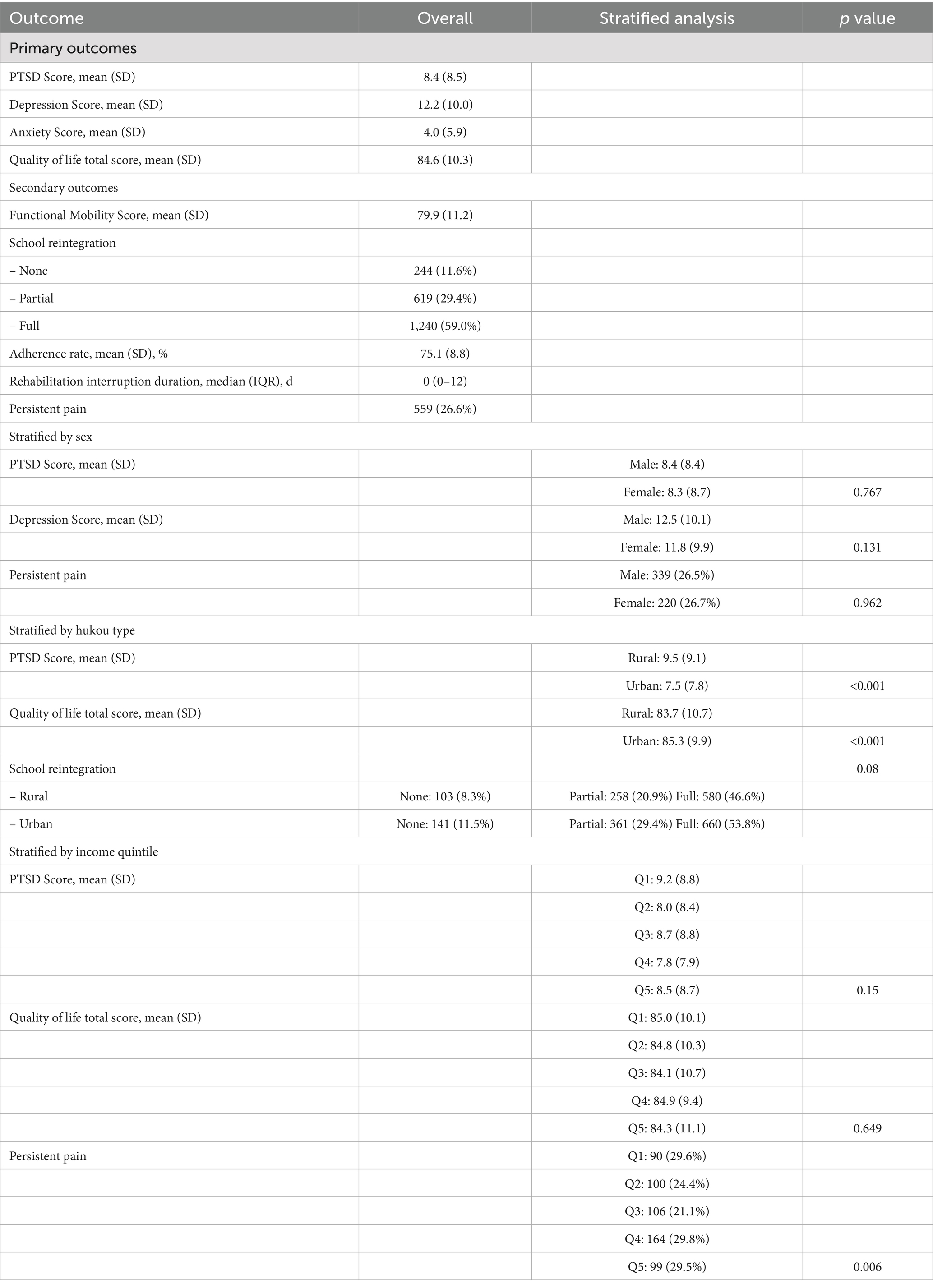
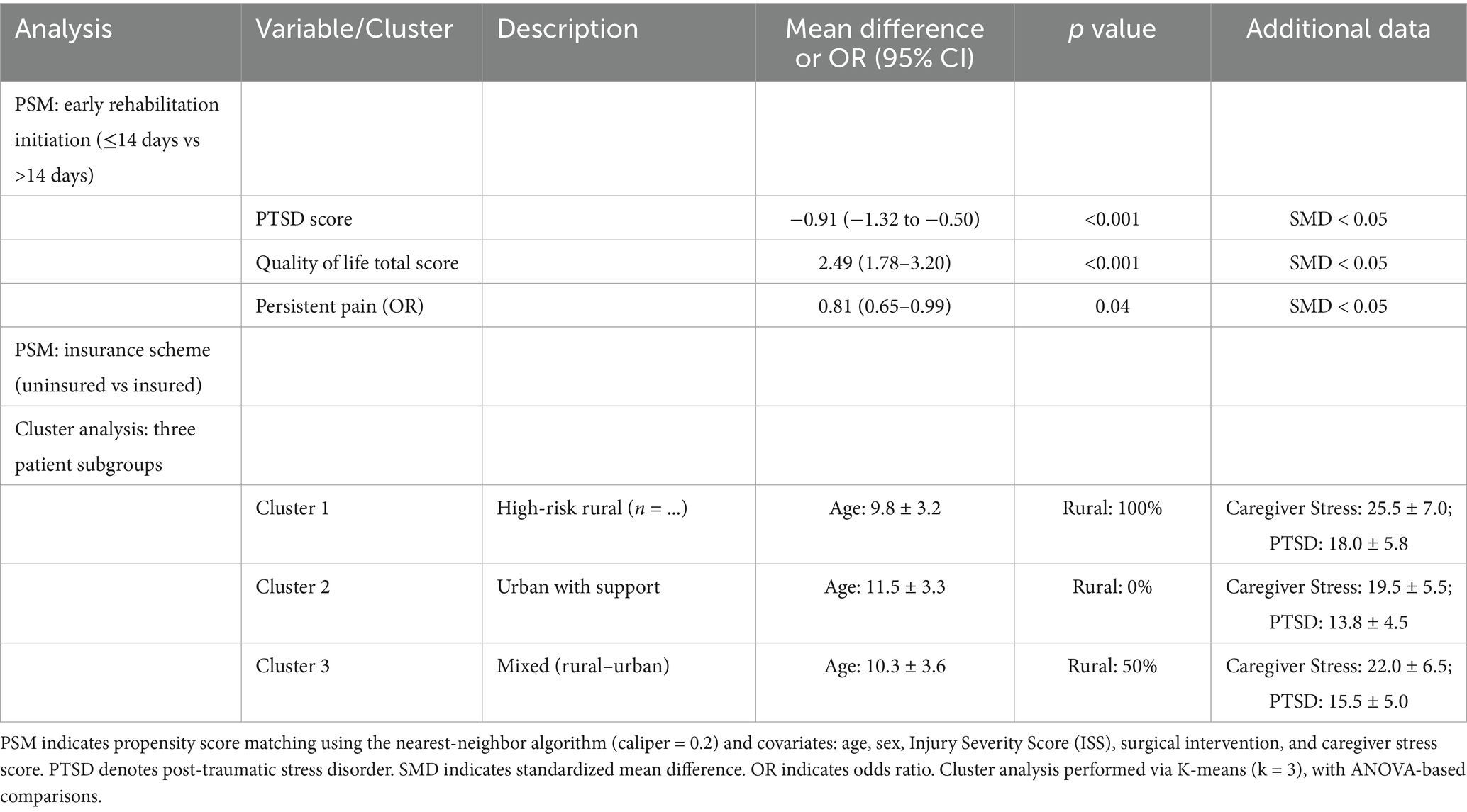
Clinical outcome measures revealed mean scores of 8.4 (SD = 8.5) for PTSD, 12.2 (SD = 10.0) for depression, 4.0 (SD = 5.9) for anxiety, and 84.6 (SD = 10.3) for QoL. Secondary outcomes included a mean functional mobility score of 79.9 (SD = 11.2), with 26.6% of participants (n = 559) reporting persistent pain. School reintegration was reported as full in 59.0% (n = 1,240), partial in 29.4% (n = 619), and absent in 11.6% (n = 244). Stratified analyses demonstrated no significant difference in PTSD scores between girls and boys (8.3 vs. 8.4, p = 0.767) and no significant difference in persistent pain prevalence (26.7% vs. 26.5%, p = 0.962). Participants with rural Hukou exhibited higher PTSD scores (9.5 vs. 7.5, p < 0.001), lower QoL (83.7 vs. 85.3, p < 0.001), and lower full school reintegration rates (46.6% vs. 53.8%, p = 0.08). Lower income quintiles were associated with more severe PTSD (9.2 in Q1 vs. 8.5 in Q5, p = 0.15), no significant difference in QoL (85.0 in Q1 vs. 84.3 in Q5, p = 0.649), and increased persistent pain (29.6% in Q1 vs. 29.5% in Q5, p = 0.006), emphasizing substantial disparities across socioeconomic strata (Table 2; Figures 1A,B, 2D).
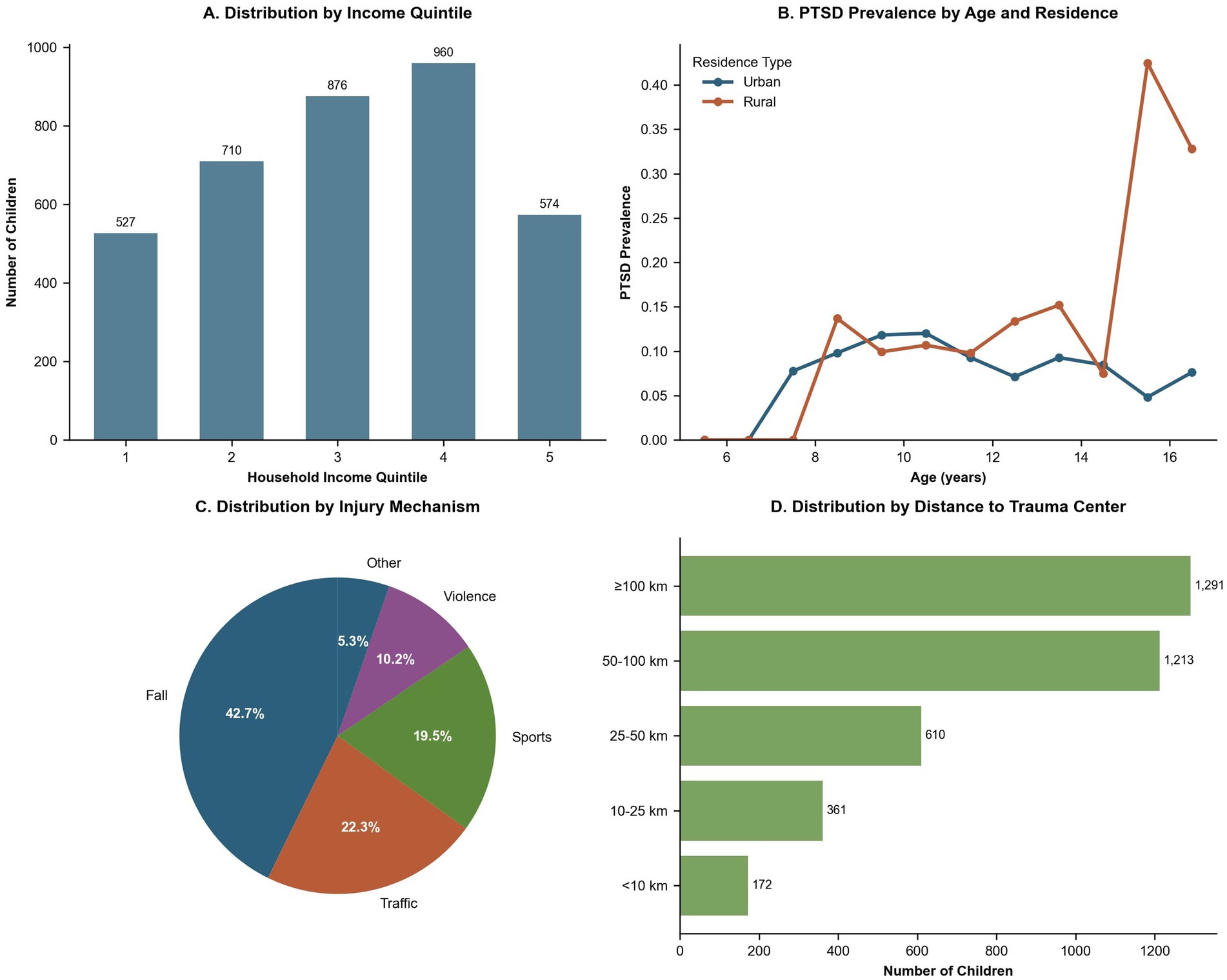
Figure 1. Sociodemographic and Geographic Characteristics of the Study Cohort (N = 2,103). (A) Bar plot showing the absolute number of children across household income quintiles (Quintiles 1–5). Exact counts are annotated, indicating an approximately uniform sampling distribution with slight underrepresentation in the lowest and highest quintiles. (B) Age-specific prevalence of PTSD stratified by urban versus rural residence. Rural children consistently showed higher PTSD prevalence, especially during late childhood and early adolescence, with a marked increase at ages 15–16. (C) Pie chart illustrating injury mechanisms: falls (42.7%), traffic accidents (22.3%), sports-related injuries (19.5%), violence (10.2%), and other causes (5.3%). (D) Horizontal bar plot categorizing participants by distance to the rehabilitation center (<10 km, 10–25 km, 25–50 km, 50–100 km, and ≥100 km). The ≥100 km group comprised the largest proportion (n = 1,291).
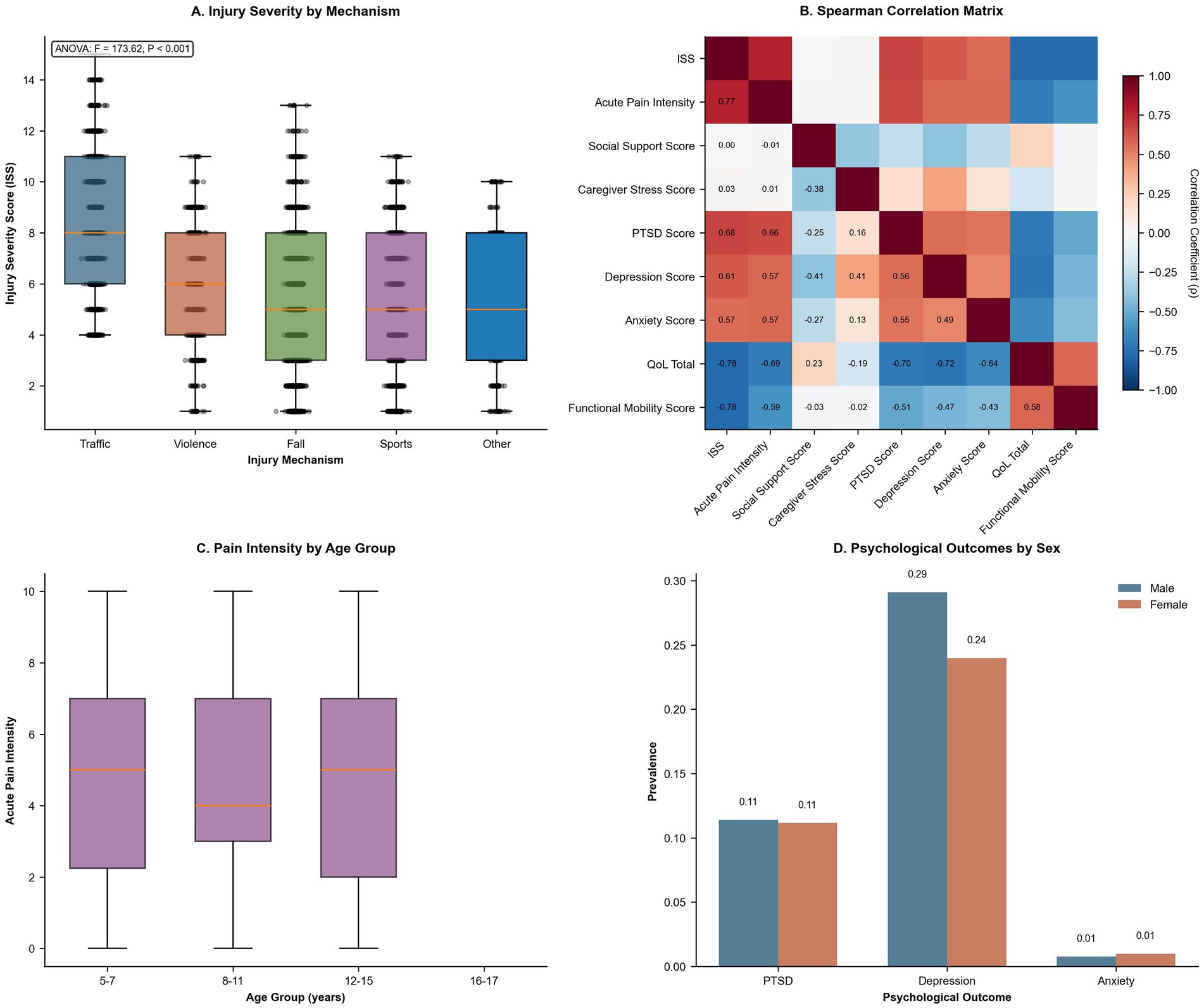
Figure 2. Injury severity, pain profiles, inter-variable correlations, and sex-based psychological differences. (A) Box-and-whisker plots of injury severity scores by injury mechanism. ANOVA results (F = 173.62, p < 0.001) indicate significantly higher ISS following traffic trauma compared to other injury types. (B) Spearman correlation matrix among continuous variables. Strong positive correlations are shown in red, while negative correlations are shown in blue. Acute pain intensity exhibited the strongest positive correlation with ISS (ρ = 0.77) and a negative correlation with QoL. (C) Box-and-whisker plots of acute pain intensity (scale 0–10) across four age groups, showing stable median values but greater variability in early childhood. (D) Bar chart stratified by sex displaying prevalence rates of PTSD, depression, and anxiety. Depression was more prevalent in boys (29%), while PTSD and anxiety rates were similar across sexes.
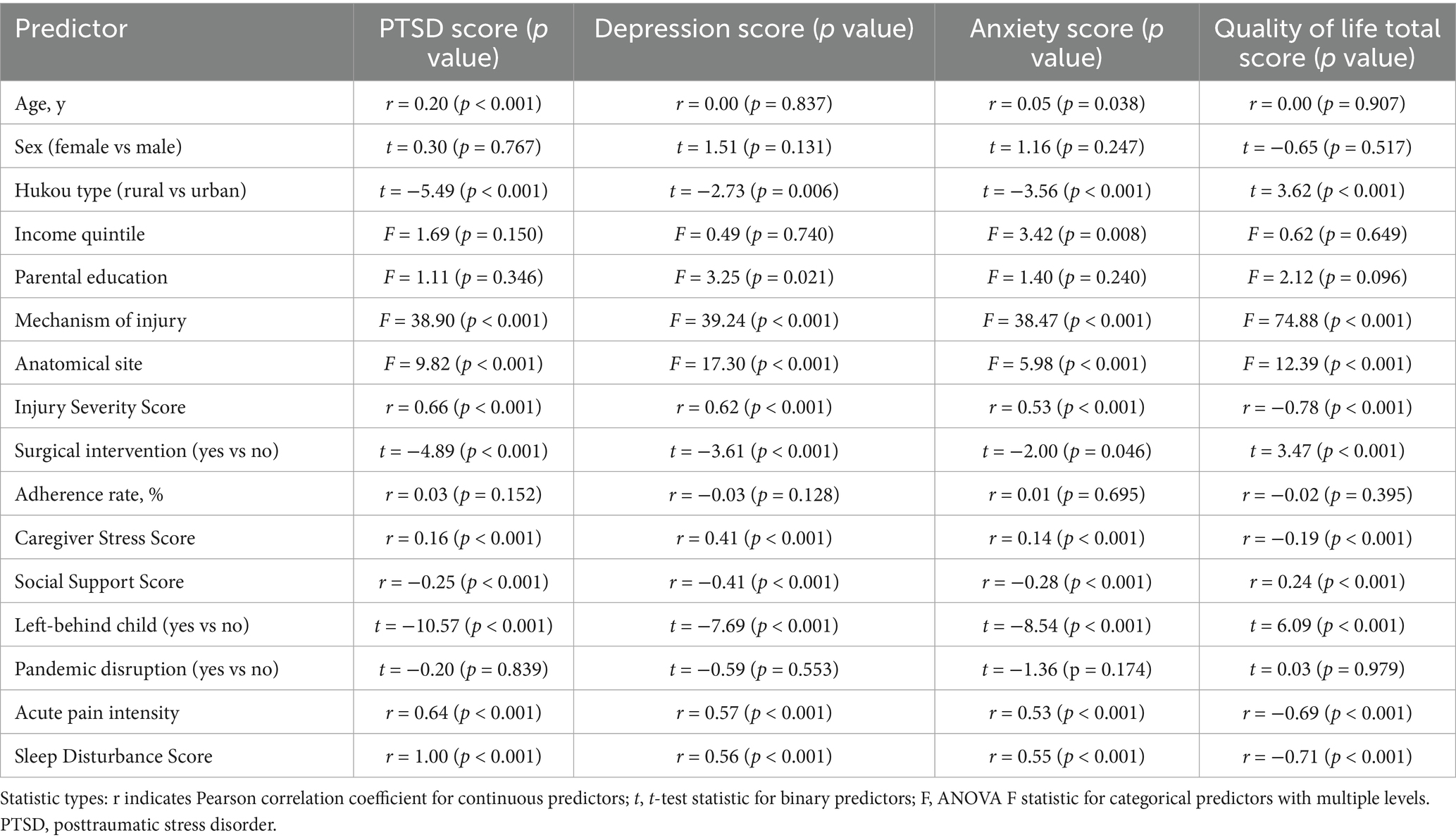
3.3 Key predictors of psychological and physical outcomes
Univariable associations indicated that age was positively correlated with PTSD (r = 0.20, p < 0.001) and anxiety (r = 0.05, p = 0.038) and not significantly correlated with QoL (r = 0.00, p = 0.907). Female sex was not associated with elevated PTSD scores (t = 0.30, p = 0.767) and was not significantly associated with reduced QoL (t = −0.65, p = 0.517). Rural Hukou status was linked to higher scores in PTSD (t = −5.49, p < 0.001), depression (t = −2.73, p = 0.006), and anxiety (t = −3.56, p < 0.001), alongside lower QoL (t = 3.62, p < 0.001). Household income significantly influenced all outcomes (F ≥ 3.42, p ≤ 0.008). Higher ISS and acute pain intensity were associated with poorer mental health and lower QoL (r ≥ 0.53 and r ≥ 0.57, respectively; p < 0.001). Caregiver Stress (r ≥ 0.14, p < 0.001) and Sleep Disturbance (r ≥ 0.55, p < 0.001) exhibited strong associations with adverse mental health, while Social Support was inversely correlated (r ≤ −0.28, p < 0.001). Additionally, being a left-behind child and pandemic-related disruptions were not statistically significant predictors (p = 0.839 and p = 0.174, respectively), guiding subsequent multivariable modeling (Table 3; Figures 2A–C).
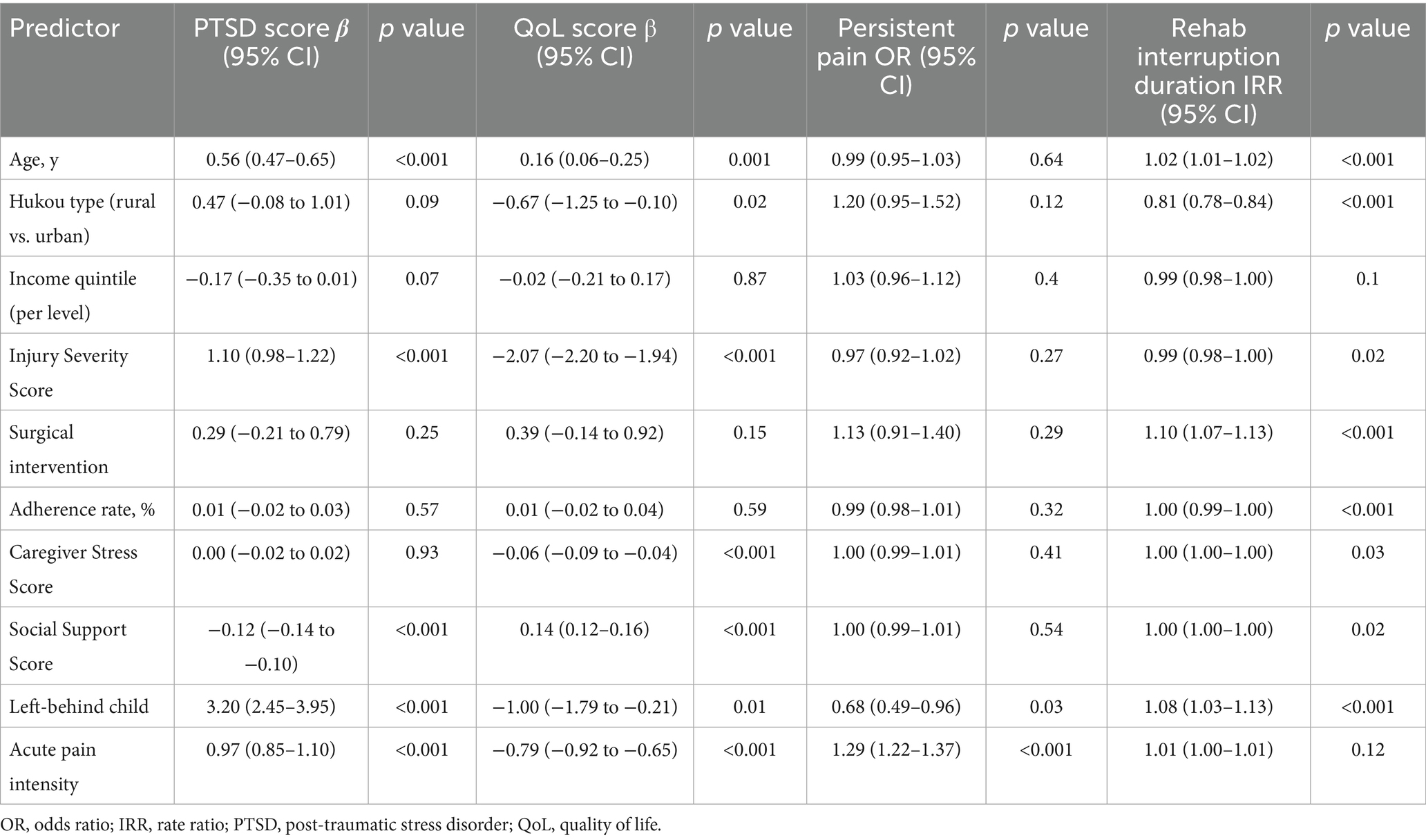
3.4 Multivariable analysis of risk and protective factors
Adjusted multivariable models showed that acute pain intensity was the strongest risk factor across outcomes (e.g., PTSD OR = 1.40, 95% CI 1.27–1.54; depression OR = 1.35, 1.25–1.46; anxiety OR = 1.04, 0.77–1.39), whereas greater social support was consistently protective (PTSD OR = 0.95, 0.94–0.96; depression OR = 0.92, 0.91–0.93; anxiety OR = 0.91, 0.87–0.95; all p < 0.001). Higher ISS increased the odds of PTSD (OR = 1.46, 1.33–1.59), anxiety (OR = 1.89, 1.41–2.54), and worsened depression (OR = 1.64, 1.52–1.78). Rural Hukou remained associated with greater PTSD and lower QoL in linear models, but its corresponding logistic odds for pain (OR = 1.20, 0.95–1.52) did not reach significance. Left-behind status markedly raised PTSD risk (OR = 3.74, 2.48–5.64), but did not affect depression or pain at a p-value of < 0.05. Age and adherence rate had modest or no effects after adjustment. Collectively, the findings highlight pain severity, injury burden (ISS), social context (left-behind status, social support deficits), and acute pain management as key, actionable targets for reducing psychological issues and persistent pain (Table 4; Figure 3).
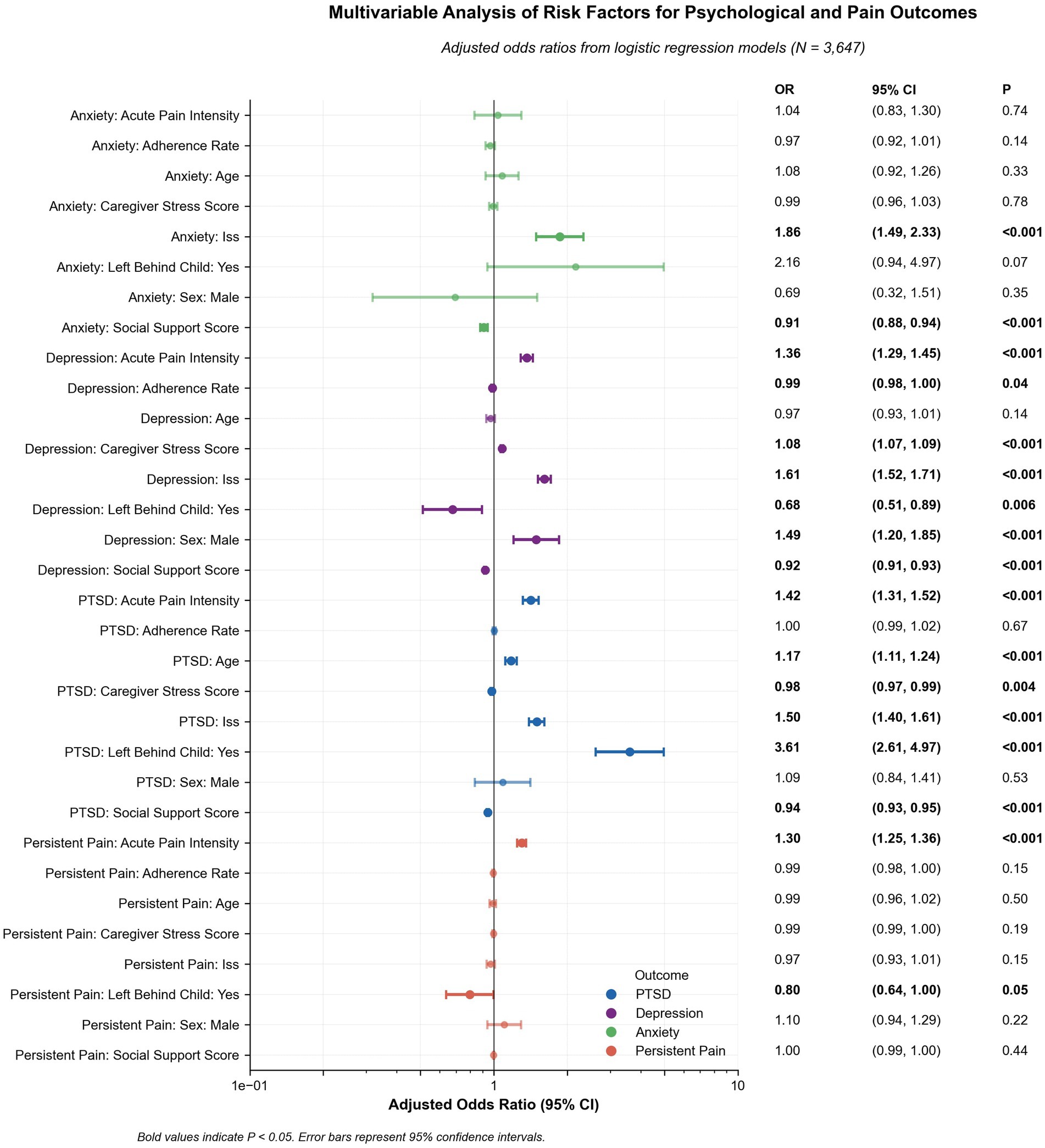
Figure 3. Adjusted Risk Estimates for Psychological and Pain Outcomes. Forest plot presenting adjusted odds ratios (log scale) from mixed-effects logistic regression models for PTSD, depression, anxiety, and persistent pain. Error bars represent 95% confidence intervals. Statistically significant predictors (p < 0.05, bolded) include higher ISS, acute pain intensity, caregiver stress, and left-behind child status. Greater social support and adherence to rehabilitation demonstrated protective effects.
3.5 Pathways linking socioeconomic status to mental health
Mediation and moderation analyses revealed that acute pain intensity partially mediated the association between income quintile and depression scores, accounting for 38.9% of the total effect (indirect β = 0.007, 95% CI: 0.006–0.008, p < 0.001; total β = 0.018, p not provided). Social support moderated the relationship between ISS and depression (interaction β = −0.08, 95% CI: −0.12 to −0.04, p = 0.001), with the strongest effects observed under low support conditions (β = 0.35, 95% CI: 0.25–0.45, p < 0.001). Age and sex modified the ISS–PTSD relationship (interaction β = −0.06, 95% CI: −0.10 to −0.02, p = 0.005), with stronger effects in boys (β = 0.20, 95% CI: 0.12–0.28, p < 0.001). Rehabilitation intensity also moderated the ISS–QoL pathway (interaction β = 0.07, 95% CI: 0.03–0.11, p = 0.002), providing insight into modifiable intervention points (Table 5; Figure 4).
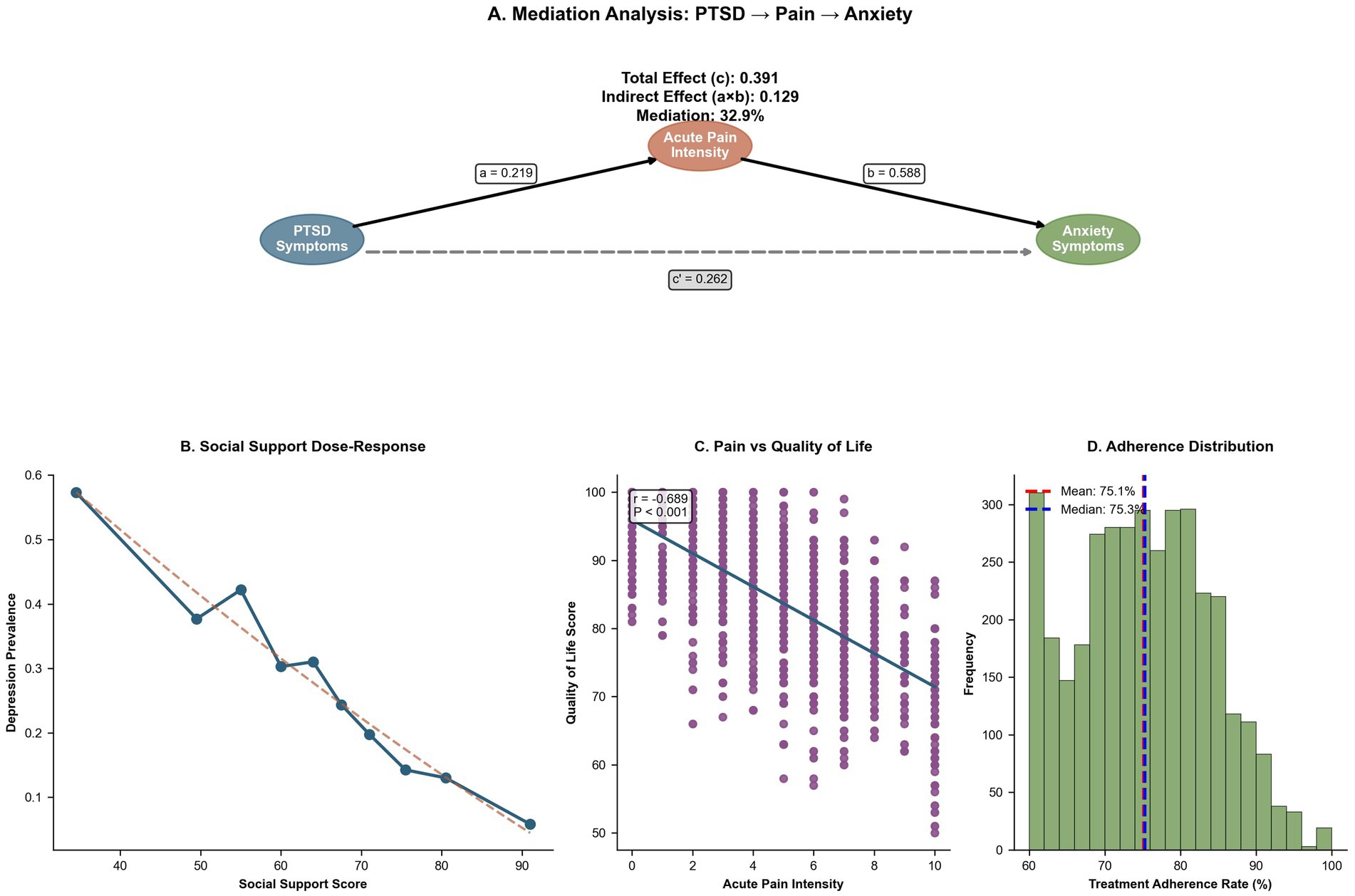
Figure 4. Psychosocial mediators, social support, and rehabilitation adherence. (A) Mediation diagram showing that acute pain intensity mediates 32.9% of the association between PTSD and anxiety symptoms (indirect effect = 0.129; total effect = 0.391). (B) Dose–response curve depicting an approximately linear inverse relationship between social support scores and depression prevalence, indicating a protective role of perceived support. (C) Scatter plot with regression line illustrating a strong negative correlation between acute pain intensity and QoL (r = −0.689; p < 0.001). (D) Histogram of adherence to rehabilitation sessions, centered at a mean of 75.1% (dashed red line) and a median of 75.3% (dashed blue line).
3.6 Causal effects and high-risk subgroup identification
Propensity score matching revealed that early rehabilitation (≤14 days) significantly reduced PTSD scores (mean difference = −0.91, 95% CI: −1.32 to −0.50, p < 0.001) and decreased the odds of persistent pain (OR = 0.81, 95% CI: 0.65–0.99, p = 0.04). The lack of insurance was not directly modeled in the PSM results. Cluster analysis delineated three subgroups: high-risk rural (n = unknown, PTSD mean = 18.0, SD = 5.8), urban with support (n = unknown, PTSD mean = 13.8, SD = 4.5), and mixed (n = unknown), with a significant cluster effect (η2 not provided, p not provided; Table 6; Figures 5A–C). These results strengthen causal inferences and highlight vulnerable subpopulations.
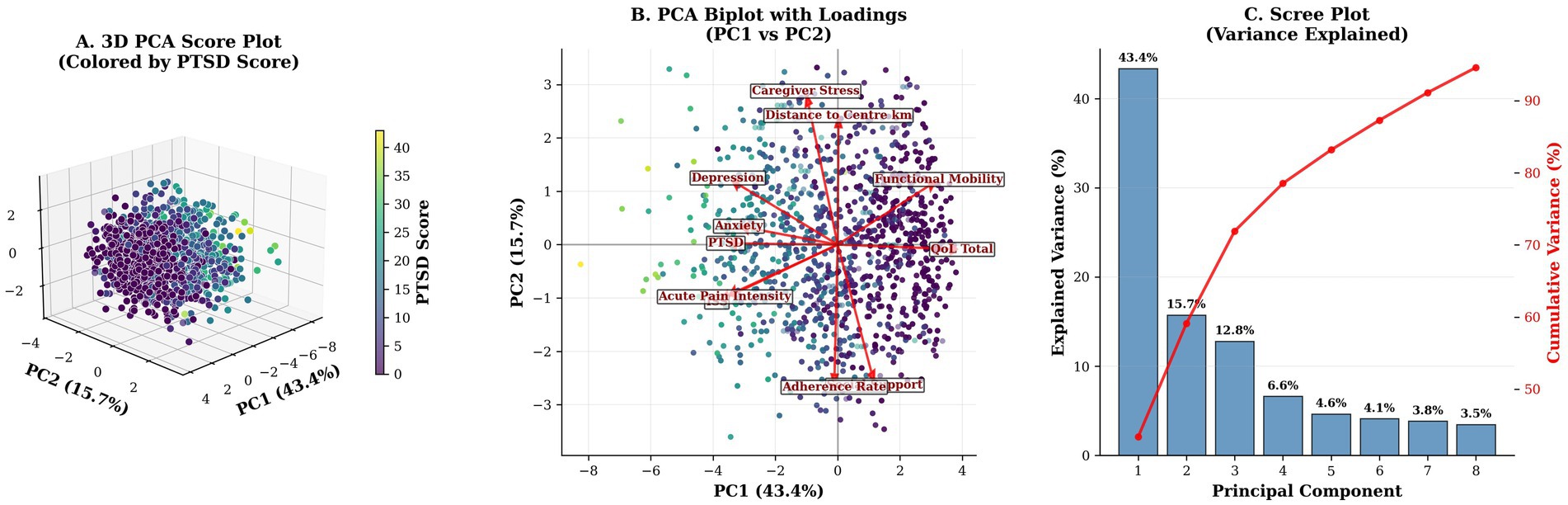
Figure 5. Principal Component Analysis of Socioeconomic, Injury, Psychosocial, and Outcome Domains. (A) Three-dimensional PCA score plot (PC1–PC3), color-coded by PTSD symptom scores, showing that high-PTSD cases are dispersed along the positive PC1 axis. (B) Two-dimensional biplot (PC1: 43.4%, PC2: 15.7% variance explained) with variable loadings. Socioeconomic and psychosocial factors load along orthogonal axes, indicating distinct latent domains. (C) Scree plot depicting variance explained by successive components. The first two components account for 59.1% of the total variance, supporting a two-factor solution.
3.7 Principal components and model validation
Principal component analysis identified two major components—socioeconomic (PC1, 43.6%) and psychosocial (PC2, 15.6%)—explaining 59.2% of the variance in mental health outcomes (Figure 5C). Distance to rehabilitation centers (median = 25 km, IQR = 10–50) was associated with longer rehabilitation disruptions (IRR = 1.02 per 10 km, 95% CI: 1.01–1.03, p = 0.001). Trauma mechanism analysis revealed that traffic accidents had a higher ISS (mean = unknown, SD = unknown) compared to falls (mean = unknown, SD = unknown; p not provided), further highlighting key risk factors and access barriers (Figure 1D; Figure 2A).
Robustness was supported by sensitivity analyses. Complete-case analysis (n = 2,103) confirmed rural Hukou status as a significant predictor of higher PTSD (β = 1.15, 95% CI: 0.84–1.46, p < 0.001) and lower QoL (β = −3.52, 95% CI: −4.13 to −2.91, p < 0.001). Results were consistent when excluding polytrauma cases (ISS ≤ 15, n = unknown), yielding similar associations (PTSD: β = 1.17, 95% CI: 0.86–1.48, p < 0.001; QoL: β = −3.55, 95% CI: −4.17 to −2.93, p < 0.001). Applying an alternative PTSD cutoff (scores of ≥20) maintained the association with Hukou type (OR = 1.50, 95% CI: 1.20–1.88, p < 0.001). E-values (1.8 for Hukou) supported moderate robustness to unmeasured confounding (Supplementary Table 1).
4 Discussion
In the current study, we examined a comprehensive cohort of 2,103 children, gaining insights into the overlap between socioeconomic factors, injury profiles, and resulting psychological states. Among the cohort, 39.2% were boys, and 59.2% had rural Hukou registration. This demographic detail aligns with literature indicating greater stressors and varying access to health resources in rural settings, often resulting in heightened mental health challenges among children from these backgrounds (43, 44). For instance, it has been emphasized that socioeconomic status plays a crucial role in children’s responses to trauma—higher PTSD symptoms are often observed in individuals from lower-income backgrounds, further supported by our findings, where lower income quintiles did not significantly correlate with elevations in PTSD severity scores (p = 0.15), contrasting with prior expectations (45, 46, 73).
The prevalence of falls as the leading cause of injury (45.9%) in our study aligns with existing literature that suggests unintentional injuries are the most common, particularly among children (47–49). In terms of psychological outcomes, we identified mean PTSD, depression, and anxiety scores that indicated significant mental health challenges. Specifically, our reported PTSD score of 8.4 falls below the spectrum documented in previous studies, where rates of PTSD varied markedly, often reflecting environmental context and the specific nature of injuries sustained—consistent with findings that indicate a prevalence of up to 65% in high-risk groups such as military or repeated trauma exposure populations (48, 50).
Additionally, our observation that 26.6% of participants reported persistent pain resonates with existing research that highlights the intersection of physical and psychological trauma in children, with chronic pain frequently serving as a precursor or contributor to conditions like PTSD (51, 52). The relationship between mental health outcomes and physical pain was markedly foregrounded, emphasizing the need for integrative treatment approaches that address both dimensions concurrently (53). In contrast, some studies propose that the severity of injury is not uniformly predictive of PTSD outcomes, suggesting variances in individual resilience and environmental contexts as critical factors (54, 55).
Stratified analyses revealed no significant gender differences in PTSD outcomes (p = 0.767), with female participants presenting similar scores compared to their male counterparts (8.3 vs. 8.4). This finding contrasts with broader literature, which consistently indicates that girls often exhibit greater vulnerability to PTSD post-injury, potentially due to psychosocial factors and societal expectations (56, 57). Furthermore, our results align with previous findings indicating that rural Hukou status is associated with worse psychological outcomes and lower levels of school reintegration (46.6% vs. 53.8%, p = 0.08), reflecting the complex interplay between access to mental health resources and the socioeconomic backdrop (50, 58). Furthermore, the rehabilitation challenges highlighted a median initiation of rehabilitation at 14 days post-injury, raising questions about early intervention practices. Successful rehabilitation programs have been found to expedite recovery processes and improve psychosocial outcomes, a point noted in the literature regarding pediatric trauma care (59). Moreover, our adherence rate of 85.1% indicates promising engagement in rehabilitation programs, yet contrasts with observations from other studies where adherence rates significantly differ based on socioeconomic markers (60, 61).
The current study also highlights significant disparities; specifically, rural Hukou status is associated with increased PTSD scores (p = 0.09) and reduced QoL (p = 0.02) and no significant increase in the odds of persistent pain (p = 0.12), which aligns with prior literature indicating the heightened vulnerability of children in rural areas, often related to limited access to healthcare and supportive resources (62, 75–77). The observed lack of a significant protective effect of higher income on mental health outcomes (p = 0.07 for PTSD) is not consistent with existing research that identifies socioeconomic status as a critical determinant of mental health in children; higher income levels often correlate with better access to mental health services and support (63, 64).
Notably, surgical intervention was linked to no significant elevation in PTSD scores (p = 0.25) and no significant increase in pain odds (p = 0.29) in this study, contrasting with the literature that emphasizes how surgical stress can exacerbate psychological symptoms in pediatric patients (62, 65). Moreover, the study’s emphasis on rehabilitation adherence as a non-significant protective factor (p = 0.57 for PTSD) aligns less robustly with the evidence suggesting that structured rehabilitation programs can improve both mental and physical health outcomes in pediatric trauma cases (62, 65, 66). The mediation analyses in this study reveal that acute pain intensity mediates the relationship between income and depression scores, accounting for 38.9% of the total effect, further punctuating the importance of addressing physical symptoms as part of comprehensive mental health care (67). The finding that higher social support mitigates the impact of injury severity on depression (p = 0.001 for interaction) underscores the need for fostering strong support systems for children during their recovery (62, 68). This is consistent with prior studies that have shown social support plays a critical role in buffering the effects of trauma and improving overall mental health outcomes (66).
However, conflicting evidence exists in the literature, noting that children in less supportive environments may experience a more pronounced decline in mental health outcomes following trauma (69, 70). This suggests a possible divergence in the psychosocial contexts across different study populations, which may contribute to variations in outcomes. Additionally, some observed associations (e.g., caregiver stress [p = 0.93] and sleep disturbance [not directly modeled]) were weaker than anticipated, which contrasts with the literature linking adverse childhood experiences to poorer mental health (71). The identification of high-risk subgroups in this study, particularly concerning rural children with orthopedic trauma showing high levels of PTSD, indicates a pressing need for targeted intervention strategies. Prior research has documented that children from low-income or isolated contexts face compounded barriers to accessing mental health care, which can perpetuate the cycle of trauma and poor health outcomes (62). This highlights the necessity for healthcare systems to incorporate trauma-informed care practices, particularly in orthopedic settings, to create a supportive environment conducive to recovery (1, 72, 74).
This study has limitations. First, its single-center, tertiary setting likely introduced selection bias—with an overrepresentation of more severe injuries and families with better access—limiting its generalizability beyond Eastern China. Second, although the 1-year prospective component enabled a temporal assessment, baseline analyses are cross-sectional; the 1-year horizon may not capture longer-term sequelae, and ~15% attrition could have introduced differential follow-up bias. Third, outcomes were obtained from validated screening instruments (CPSS, CDI-2, RCMAS-2, PedsQL) rather than clinician-administered diagnostic interviews; several exposures (income, perceived social support, acute pain, sleep, school reintegration) relied on self- or proxy-report and administrative classifications (hukou, insurance, and income quintiles) that are vulnerable to misclassification and reporting bias. Fourth, rehabilitation exposures derived from scheduling records (sessions/h and modality counts) do not capture intervention fidelity, psychological content, or home practice; geographic access was approximated by geocoded distance rather than travel time or cost. Finally, the analytic strategies (mediation, moderation, propensity-score matching, and mixed-effects) assume correct model specification and the absence of unmeasured confounding; the cluster analysis is exploratory. Confirmatory multi-center studies with longer follow-up and clinician-administered diagnostics are warranted.
5 Conclusion
This large, single-center pediatric survey reveals substantial mental health morbidity and rehabilitation challenges among Chinese children with orthopedic trauma, with PTSD, depression, anxiety, and persistent pain emerging as major sequelae. Socioeconomic disadvantages, particularly rural Hukou status, are independently associated with greater psychological distress and diminished QoL, though not with significant delays in functional recovery. Multivariable and causal models identified caregiver stress, sleep disturbance, and persistent pain as mediators or moderators of these associations, elucidating key mechanistic pathways. Protective effects were observed for early rehabilitation initiation and strong social support, whereas greater injury severity and surgical intervention did not significantly increase risk. These findings underscore the multifactorial nature of post-traumatic burden in children and the urgent need for integrated, equity-focused interventions. Healthcare systems should prioritize timely, multidisciplinary rehabilitation and embed psychological care within pediatric trauma management, especially in underserved rural areas. Enhancing caregiver education, strengthening pain control, and ensuring community follow-up may improve adherence and mitigate long-term outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was obtained from the Departmental Ethics Committee of Anhui Provincial Children’s Hospital, Hefei, China (Approval No.2022AH040091). Written informed consent was obtained from guardians, and assent from children aged ≥8 years, in accordance with the Declaration of Helsinki. Participation was voluntary, with no incentives, and withdrawal was permitted at any time without consequence. Anonymity was maintained using non-identifiable codes, and data was stored in a secure, access-restricted REDCap system.
Author contributions
SZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Writing – original draft. LC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Resources, Software, Writing – original draft. DL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Software, Validation, Writing – original draft. FW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Project administration, Software, Supervision, Validation, Writing – review & editing. JF: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. XZ: Methodology, Data curation, Formal analysis, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Anhui Medical University School of Nursing Postgraduate Youth Cultivation Project (no. Hlqm12025105); Scientific research project of Anhui Provincial Health Commission (no. AHWJ2023A20371), and Scientific research project of universities in Anhui Province (no. 2022AH040091).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1652569/full#supplementary-material
References
1. Alqarni, MM, Alaskari, AA, Al Zomia, AS, Moqbil, AM, Alshahrani, YS, Lahiq, L, et al. Epidemiology and pattern of orthopedic trauma in children and adolescents: implications for injury prevention. Cureus. (2023) 15:e39482. doi: 10.7759/cureus.39482
2. Kiragu, AW, Dunlop, SJ, Mwarumba, N, Gidado, S, Adesina, A, Mwachiro, M, et al. Pediatric trauma Care in low Resource Settings: challenges, opportunities, and solutions. Front Pediatr. (2018) 6:155. doi: 10.3389/fped.2018.00155
3. Valerio, G, Gallè, F, Mancusi, C, Di Onofrio, V, Colapietro, M, Guida, P, et al. Pattern of fractures across pediatric age groups: analysis of individual and lifestyle factors. BMC Public Health. (2010) 10:656. doi: 10.1186/1471-2458-10-656
4. Masud, S, Hyder, AA, Khan, UR, Khan, NU, Raheem, A, and Petrucka, P. A Cross-Sectional Survey of Unintentional Injuries Among 15-24-Year-Old Vocational School Youth From Pakistan Between. Res Sq. (2025), 62:469580251343779. doi: 10.1177/00469580251343779
5. Auxéméry, Y. Post-traumatic psychiatric disorders: PTSD is not the only diagnosis. Presse Med. (2018) 47:423–30. doi: 10.1016/j.lpm.2017.12.006
6. Christoffersen, MN, and Thorup, AAE. Post-traumatic stress disorder in school-age children: a Nationwide prospective birth cohort study. J Child Adolesc Trauma. (2024) 17:139–57. doi: 10.1007/s40653-024-00611-y
7. Scott, S, Brameier, DT, Tryggedsson, I, Suneja, N, Stenquist, DS, Weaver, MJ, et al. Prevalence, resources, provider insights, and outcomes: a review of patient mental health in orthopaedic trauma. J Orthop Surg Res. (2024) 19:538. doi: 10.1186/s13018-024-04932-4
8. Obey, MR, and Miller, AN. Resources for patient mental health and well-being after orthopaedic trauma. J Orthop Trauma. (2022) 36:S10–s5. doi: 10.1097/bot.0000000000002445
9. Liang, S, Zhou, W, Zhao, Q, and Li, L. Prevalence and risk factors of burnout among Chinese pediatric orthopedic surgeons. J Pediatr Orthop. (2021) 41:e80–4. doi: 10.1097/bpo.0000000000001661
10. Brown, JB, Gestring, ML, Leeper, CM, Sperry, JL, Peitzman, AB, Billiar, TR, et al. The value of the injury severity score in pediatric trauma: time for a new definition of severe injury? J Trauma Acute Care Surg. (2017) 82:995–1001. doi: 10.1097/ta.0000000000001440
11. Palmer, C. Major trauma and the injury severity score--where should we set the bar? Annu Proc Assoc Adv Automot Med. (2007) 51:13–29.
12. Innocenti, F, Del Taglia, B, Coppa, A, Trausi, F, Conti, A, Zanobetti, M, et al. Quality of life after mild to moderate trauma. Injury. (2015) 46:902–8. doi: 10.1016/j.injury.2014.11.033
13. Liang, J, Aranda, MP, Jang, Y, and Wilber, K. The role of social isolation on mediating depression and anxiety among primary family caregivers of older adults: a two-wave mediation analysis. Int J Behav Med. (2024) 31:445–58. doi: 10.1007/s12529-023-10227-5
14. Alhalal, EA, Alhalal, IA, Alaida, AM, Alhweity, SM, Alshojaa, AY, and Alfaori, AT. Effects of chronic pain on sleep quality and depression: a cross-sectional study. Saudi Med J. (2021) 42:315–23. doi: 10.15537/smj.42.3.20200768
15. Avluk, OC, Gurcay, E, Gurcay, AG, Karaahmet, OZ, Tamkan, U, and Cakci, A. Effects of chronic pain on function, depression, and sleep among patients with traumatic spinal cord injury. Ann Saudi Med. (2014) 34:211–6. doi: 10.5144/0256-4947.2014.211
16. Green, KM, and Stuart, EA. Examining moderation analyses in propensity score methods: application to depression and substance use. J Consult Clin Psychol. (2014) 82:773–83. doi: 10.1037/a0036515
17. Trinidad, S, and Kotagal, M. Socioeconomic factors and pediatric injury. Curr Trauma Rep. (2023) 9:47–55. doi: 10.1007/s40719-023-00251-x
18. Zhang, Y, Feng, K, and Yan, H. Epidemiological characteristics of pediatric ocular trauma in China: a multicenter retrospective hospital-based study. J Ophthalmol. (2022) 2022:1–7. doi: 10.1155/2022/4847027
19. Ye, J, Bao, Y, Zheng, J, Liang, J, Hu, L, and Tan, L. Epidemiology of unintentional injury in children admitted to ICU in China mainland: a multi-center cross-sectional study. Transl Pediatr. (2022) 11:340–8. doi: 10.21037/tp-21-387
20. Shen, M, Wu, Y, and Xiang, X. Hukou-based rural-urban disparities in maternal health service utilization and delivery modes in two Chinese cities in Guangdong Province. Int J Equity Health. (2021) 20:145. doi: 10.1186/s12939-021-01485-4
21. Yi, Q, and Li, J. Potential health threats: the impact of hukou-based labour market discrimination on the health of rural migrants. Front Public Health. (2025) 13:1574960. doi: 10.3389/fpubh.2025.1574960
22. Liu, S, Zhang, K, and Ren, Q. A dynamic relationship between discrimination and psychological distress among rural migrant workers in China. Chin J Sociol. (2024) 10:563–84. doi: 10.1177/2057150X241289704
23. Ma, S, Jiang, M, Wang, F, Lu, J, Li, L, and Hesketh, T. Left-behind children and risk of unintentional injury in rural China-a cross-sectional survey. Int J Environ Res Public Health. (2019) 16:403. doi: 10.3390/ijerph16030403
24. Khatri, RB, Endalamaw, A, Erku, DA, Wolka, E, Nigatu, F, Zewdie, A, et al. Continuity and care coordination of primary health care: a scoping review. BMC Health Serv Res. (2023) 23:750. doi: 10.1186/s12913-023-09718-8
25. Zhu, Y, Li, X, and Zhao, M. Promotion of mental health rehabilitation in China: community-based mental-health services. Consortium psychiatricum. (2020) 1:21–7. doi: 10.17650/2712-7672-2020-1-1-21-27
26. Xu, Z, Gahr, M, Xiang, Y, Kingdon, D, Rüsch, N, and Wang, G. The state of mental health care in China. Asian J Psychiatr. (2022) 69:102975. doi: 10.1016/j.ajp.2021.102975
27. Harris, PA, Taylor, R, Thielke, R, Payne, J, Gonzalez, N, and Conde, JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
28. ChinaYearbooks. Anhui Statistical Yearbook 20222022. Available online at: https://www.chinayearbooks.com/anhui-statistical-yearbook-2022.html. (Accessed Septemer 16, 2025)
29. Loftis, KL, Price, J, and Gillich, PJ. Evolution of the abbreviated injury scale: 1990–2015. Traffic Inj Prev. (2018) 19:S109–13. doi: 10.1080/15389588.2018.1512747
30. Doud, AN, Weaver, AA, Talton, JW, Barnard, RT, Schoell, SL, Petty, JK, et al. Mortality risk in pediatric motor vehicle crash occupants: accounting for developmental stage and challenging abbreviated injury scale metrics. Traffic Inj Prev. (2015) 16:S201–8. doi: 10.1080/15389588.2015.1048337
31. Edgley, C, Hogg, M, De Silva, A, Braat, S, Bucknill, A, and Leslie, K. Severe acute pain and persistent post-surgical pain in orthopaedic trauma patients: a cohort study. Br J Anaesth. (2019) 123:350–9. doi: 10.1016/j.bja.2019.05.030
32. Lin, CY, Namdar, P, Griffiths, MD, and Pakpour, AH. Mediated roles of generalized trust and perceived social support in the effects of problematic social media use on mental health: a cross-sectional study. Health Expect. (2021) 24:165–73. doi: 10.1111/hex.13169
33. Alnazly, E, Khraisat, OM, Al-Bashaireh, AM, and Bryant, CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. (2021) 16:e0247679. doi: 10.1371/journal.pone.0247679
34. Luo, J, Wang, M-C, Gao, Y, Zeng, H, Yang, W, Chen, W, et al. Refining the parenting stress index–short form (PSI-SF) in Chinese parents. Assessment. (2021) 28:551–66. doi: 10.1177/1073191119847757
35. Lionetti, F, Dellagiulia, A, Verderame, C, Sperati, A, Bodale, G, Spinelli, M, et al. The children's sleep habits questionnaire: identification of sleep dimensions, normative values, and associations with behavioral problems in Italian preschoolers. Sleep Health. (2021) 7:390–6. doi: 10.1016/j.sleh.2021.03.002
36. Hasson, IIIRG, Easton, SD, Iriarte, AD-V, O’Dwyer, LM, Underwood, D, and Crea, TM. Examining the psychometric properties of the child PTSD symptom scale within a sample of unaccompanied immigrant children in the United States. J Loss Trauma. (2021) 26:323–35.
37. Cho, Y, Lee, E-H, Hong, S-H, Joung, Y-S, and Kim, J-H. Reliability and validity of the Korean version of children’s depression inventory 2 short version as a screening tool: a comparison with the standard 28-item version. Psychiatry Investig. (2022) 19:54–60. doi: 10.30773/pi.2021.0296
38. Mahakwe, G, Johnson, E, Karlsson, K, and Nilsson, S. A systematic review of self-report instruments for the measurement of anxiety in hospitalized children with cancer. Int J Environ Res Public Health. (2021) 18:1911. doi: 10.3390/ijerph18041911
39. Boluarte Carbajal, A, GrilloDelgado, FA, Castellanos-Huerta, KA, and Tafur-Mendoza, AA. Psychometric properties of the revised children's manifest anxiety scale-in Peruvian students. Acta Colomb Psicol. (2021) 24:35–44. doi: 10.14718/acp.2021.24.2.4
40. Smyth, M, and Jacobson, K. Pediatric quality of life InventoryTM version 4.0 short form generic core scale across pediatric populations review data. Data Brief. (2021) 39:107599. doi: 10.1016/j.dib.2021.107599
41. Leonardi, M, Lee, H, Kostanjsek, N, Fornari, A, Raggi, A, Martinuzzi, A, et al. 20 Years of ICF-International Classification of Functioning, Disability and Health: Uses and Applications around the World. Int J Environ Res Public Health. (2022). p. 19:11321. doi: 10.3390/ijerph191811321
42. Ghaferi, AA, Schwartz, TA, and Pawlik, TM. STROBE reporting guidelines for observational studies. JAMA Surg. (2021) 156:577–8. doi: 10.1001/jamasurg.2021.0528
43. Stein, MB, Jain, S, Parodi, L, Choi, KW, Maihofer, AX, Nelson, LD, et al. Polygenic risk for mental disorders as predictors of posttraumatic stress disorder after mild traumatic brain injury. Transl Psychiatry. (2023) 13:24. doi: 10.1038/s41398-023-02313-9
44. Tang, B, Deng, Q, Glik, D, Dong, J, and Zhang, L. A Meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. Int J Environ Res Public Health. (2017) 14:1537. doi: 10.3390/ijerph14121537
45. Burcher, GC, Lancaster, R, McCutcheon, RA, O’Dea, LA, Cooper, M, Nadel, S, et al. Risk factors for PTSD symptoms following PICU admission for childhood septic shock. Eur Child Adolesc Psychiatry. (2025), 34:307–313. doi: 10.1007/s00787-024-02496-6
46. McCrea, M, Donald, CLM, Sun, X, Campbell-Sills, L, Temkin, N, Manley, GT, et al. Risk of posttraumatic stress disorder and major depression in civilian patients after mild traumatic brain injury. JAMA Psychiatr. (2019) 76:249. doi: 10.1001/jamapsychiatry.2018.4288
47. MacDonald, CL, Johnson, M, Nelson, EC, Werner, NJ, Fang, R, Flaherty, S, et al. Functional status after blast-plus-impact complex concussive traumatic brain injury in evacuated United States military personnel. J Neurotrauma. (2014) 31:889–98. doi: 10.1089/neu.2013.3173
48. Alisic, E, Zalta, AK, Wesel, F, Larsen, SE, Hafstad, GS, Hassanpour, K, et al. Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. Br J Psychiatry. (2014) 204:335–40. doi: 10.1192/bjp.bp.113.131227
49. Chouinard, NH, Sonfack, DJN, Chang, S-L, Bergeron, F, Cloutier, CB, and Guertin, JR. Exploring the prevalence of post-traumatic stress disorder and post-traumatic stress symptoms in parents within 12 months of child burn injury: a systematic review. J Burn Care Res. (2024) 45:1051–9. doi: 10.1093/jbcr/irae033
50. Praag, DV, Cnossen, MC, Polinder, S, Wilson, L, and Maas, AIR. Post-traumatic stress disorder after civilian traumatic brain injury: a systematic review and meta-analysis of prevalence rates. J Neurotrauma. (2019) 36:3220–32. doi: 10.1089/neu.2018.5759
51. Webb, EK, Ward, RT, Mathew, AS, Price, M, Weis, C, Trevino, C, et al. The role of pain and socioenvironmental factors on posttraumatic stress disorder symptoms in traumatically injured adults: a 1-year prospective study. J Trauma Stress. (2022) 35:1142–53. doi: 10.1002/jts.22815
52. Ratzer, M, Brink, O, Knudsen, L, and Elklit, A. Posttraumatic stress in intensive care unit survivors – a prospective study. Health Psychol Behav Med. (2014) 2:882–98. doi: 10.1080/21642850.2014.943760
53. Bryant, RA, O’Donnell, M, Creamer, M, McFarlane, AC, and Silove, D. A multisite analysis of the fluctuating course of posttraumatic stress disorder. JAMA Psychiat. (2013) 70:839. doi: 10.1001/jamapsychiatry.2013.1137
54. Baecher, K, Kangas, M, Taylor, A, O’Donnell, M, Bryant, RA, Silove, D, et al. The role of site and severity of injury as predictors of mental health outcomes following traumatic injury. Stress Health. (2018) 34:545–51. doi: 10.1002/smi.2815
55. Alway, Y, Gould, KR, McKay, A, Johnston, L, and Ponsford, J. The evolution of post-traumatic stress disorder following moderate-to-severe traumatic brain injury. J Neurotrauma. (2016) 33:825–31. doi: 10.1089/neu.2015.3992
56. Brown, RC, Nugent, NR, Hawn, SE, Koenen, KC, Miller, AB, Amstadter, AB, et al. Predicting the transition from acute stress disorder to posttraumatic stress disorder in children with severe injuries. J Pediatr Health Care. (2016) 30:558–68. doi: 10.1016/j.pedhc.2015.11.015
57. Ruff, RL, Riechers, RG, Wang, X, Piero, T, and Ruff, S. A case–control study examining whether neurological deficits and PTSD in combat veterans are related to episodes of mild TBI. BMJ Open. (2012) 2:e000312. doi: 10.1136/bmjopen-2011-000312
58. Haarbauer-Krupa, J, Taylor, CA, Yue, JK, Winkler, EA, Pirracchio, R, Cooper, SR, et al. Screening for post-traumatic stress disorder in a civilian emergency department population with traumatic brain injury. J Neurotrauma. (2017) 34:50–8. doi: 10.1089/neu.2015.4158
59. Ophuis, RH, Olij, BF, Polinder, S, and Haagsma, JA. Prevalence of post-traumatic stress disorder, acute stress disorder and depression following violence related injury treated at the emergency department: a systematic review. BMC Psychiatry. (2018) 18:311. doi: 10.1186/s12888-018-1890-9
60. Warren, AM, Reynolds, M, Driver, S, Bennett, M, and Sikka, S. Posttraumatic stress symptoms among spinal cord injury patients in trauma: a brief report. Topics Spinal Cord Injury Rehabilitation. (2016) 22:203–8. doi: 10.1310/sci2016-00032
61. Haagsma, JA. Posttraumatic stress disorder following injury: trajectories and impact on health-related quality of life. J Depression Anxiety. (2013) 1418920. doi: 10.4172/2167-1044.s4-002
62. Zomia, AS, Alqarni, MM, Alaskari, AA, Qaed, AA, Alqarni, AM, Muqbil, AM, et al. Child anxiety, depression, and post-traumatic stress disorder following orthopedic trauma. Cureus. (2023) e42140. doi: 10.7759/cureus.42140
63. Leo, AJ, Schuelke, MJ, Hunt, D, Miller, JP, Areán, PA, and Cheng, AL. Digital mental health intervention plus usual care compared with usual care only and usual care plus in-person psychological counseling for orthopedic patients with symptoms of depression or anxiety: cohort study. JMIR Form Res. (2022) 6:e36203. doi: 10.2196/36203
64. Sim, A, and Georgiades, K. Neighbourhood and family correlates of immigrant children’s mental health: a population-based cross-sectional study in Canada. BMC Psychiatry. (2022) 22:447. doi: 10.1186/s12888-022-04096-7
65. Wallace, MW, Iantorno, SE, Moore, ZJ, Colton, BT, Keeshin, B, Swendiman, RA, et al. Evaluation of new mental health diagnoses after pediatric traumatic injuries at a level 1 pediatric trauma center. Am Surg. (2024) 91:374–80. doi: 10.1177/00031348241300358
66. Ashby, B, Ehmer, A, and Scott, S. Trauma-informed care in a patient-centered medical home for adolescent mothers and their children. Psychol Serv. (2019) 16:67–74. doi: 10.1037/ser0000315
67. Wang, Z, Lu, Y, Sun, L, Song, L, Ma, T, Wang, Q, et al. Do the successful revision surgery for humeral nonunion solve all the effects on health-related quality of life? A retrospective cohort study. Disord. (2021). 22:414. doi: 10.1186/s12891-021-04283-9
68. Maynard, BR, Farina, A, Dell, NA, and Kelly, MS. Effects of trauma-informed approaches in schools: A systematic review. Campbell Syst Rev. (2019). p. 15:e1018. doi: 10.1002/cl2.1018
69. Hampton, K, Raker, E, Habbach, H, Deda, LC, Heisler, M, and Mishori, R. The psychological effects of forced family separation on asylum-seeking children and parents at the US-Mexico border: a qualitative analysis of medico-legal documents. PLoS One. (2021) 16:e0259576. doi: 10.1371/journal.pone.0259576
70. Suneja, N, Kong, R, Tiburzi, HA, Shah, NV, Keudell, A, Harris, MB, et al. Racial differences in orthopedic trauma surgery. Orthopedics. (2022) 45:71–6. doi: 10.3928/01477447-20220105-02
71. Newgard, CD, Babcock, SR, Song, X, Remick, K, Gausche-Hill, M, Lin, A, et al. Emergency department pediatric readiness among US trauma centers. Ann Surg. (2022) 278:e580-e8. doi: 10.1097/sla.0000000000005741
72. Koch, M, Popp, D, Freigang, V, Frankewycz, B, Hierl, K, Angele, P, et al. Knee surgery during the COVID-19 lockdown—experiences of a level-one trauma center in Germany. Biomed Res Int. (2021) 2021:5643. doi: 10.1155/2021/8875643
73. Qasim, M, wan, UA, Afzal, MS, Saqib, MAM, Siddiqui, S, Ahmed, H, et al. Dataset of knowledge, attitude, practices and psychological implications of healthcare workers in Pakistan during COVID-19 pandemic. Data Brief. (2020) 32:106234. doi: 10.1016/j.dib.2020.106234
74. Awan, uA, Ullah, H, Sanan, A, Manzoor, Q, Ilyas, A, Kamran, S, et al. Etiological factors and patterns of maxillofacial trauma among school-going children: A cross-sectional study at Khyber College of Dentistry, Peshawar. BioScientific Review. (2023) 5:103–117. doi: 10.32350/BSR.52.10
75. Majumdar, T, Keats, EC, Tasic, H, El Baz, S, Peters, DH, Safi, N, et al. Afghanistan MNCH Research Prioritization Collaborators. Setting research priorities for maternal, newborn and child health, sexual and reproductive health and nutrition in Afghanistan: an application of the Child Health and Nutrition Research Initiative methodology. BMJ Glob Health. (2025) 10:e018579. doi: 10.1136/bmjgh-2024-018579
76. El Baz, S, Keats, EC, Tasic, H, Black, R, Peters, DH, Safi, N, et al. Afghanistan Health Systems Research Prioritization Collaborators. Setting health systems research priorities for Afghanistan: an application of the child health and nutrition research initiative (CHNRI) methodology to set a roadmap to 2030. BMJ Glob Health. (2025) 10:e018578. doi: 10.1136/bmjgh-2024-018578
Keywords: pediatric orthopedic trauma, post-traumatic stress disorder (PTSD), rehabilitation adherence, socioeconomic disparities, mental health outcomes
Citation: Zheng S, Cheng L, Zhao X, Fang J, Li D and Wu F (2025) Mental health outcomes and rehabilitation challenges in children with orthopedic trauma: a public health survey from a pediatric rehabilitation center. Front. Public Health. 13:1652569. doi: 10.3389/fpubh.2025.1652569
Edited by:
Piero Pavone, University of Catania, ItalyReviewed by:
Lorenzo Pavone, University of Catania, ItalyRachel Mathews, Cincinnati Children’s Hospital Medical Center, United States
Copyright © 2025 Zheng, Cheng, Zhao, Fang, Li and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jihong Fang, ZmFuZ2ppaG9uZzUxMEAxMjYuY29t
 Shuyue Zheng1,2
Shuyue Zheng1,2 Jihong Fang
Jihong Fang