- 1Graduate Medical Education, Falls Church, VA, United States
- 2Inova Fairfax Medical Campus, Inova Health System Falls Church, Falls Church, VA, United States
- 3Department of Medicine, Cooper Medical School of Rowan University, Cooper University Healthcare, Camden, NJ, United States
The recent announcement by Health Secretary Robert F. Kennedy Jr. that medical schools must offer nutrition courses or risk losing federal funding from the Department of Health and Human Services represents a watershed moment for American medical education (1). Kennedy's declaration that “there's almost no medical schools that have nutrition courses” and his commitment to withhold funding from institutions that fail to implement comprehensive nutrition programs signals an unprecedented opportunity to address a fundamental gap in physician training. This mandate builds upon the growing recognition of this educational deficit, recently highlighted by the 2022 bipartisan passage of House Resolution 1118 in the United States (U.S.) House of Representatives, which called for meaningful nutrition education for medical trainees (2). This mandate arrives at a critical juncture when diet-related chronic diseases continue to devastate American health, making nutrition education not merely beneficial but essential for the future of medical practice.
The current state of nutrition education in medical training is inadequate to meet the mounting health challenges facing our patients. In the most recent survey, medical students spend an average of only 19 h on required nutrition education over their entire 4-year curriculum failing to meet the even the minimum hours recommended 40 years ago (3). This limited exposure focuses predominantly on biochemistry and vitamin deficiency states -conditions that are not major health problems in the U.S. today. Following medical school, nutrition education during graduate medical education is minimal or, more commonly, entirely absent. The Accreditation Council for Graduate Medical Education's Common Program Requirements lack any requirement for physicians-in-training to learn about nutrition or diet, a glaring omission given the central role of nutrition in disease prevention and management (4).
This educational deficit becomes even more concerning when examined against the backdrop of America's chronic disease epidemic. Diet-related diseases contribute to over 11 million premature deaths annually worldwide, with poor-quality diet identified as the leading cause of death in the United States (5). More than two-thirds of American adults are overweight or obese, and half have diabetes or pre-diabetes, conditions that disproportionately affect vulnerable populations (6, 7). These statistics represent not just individual tragedies but a systemic failure to prioritize prevention through evidence-based nutritional interventions.
The evidence supporting nutrition as a therapeutic intervention is overwhelming and continues to grow. Randomized clinical trials have demonstrated that dietary interventions can both prevent and manage critical diseases, including diabetes and cardiovascular disease. Mediterranean-style diets have been shown to reduce recurrent cardiovascular events by 72%, representing an absolute difference of 2.83 events per year compared with control groups (7). For individuals with elevated fasting blood glucose, combining dietary changes with physical activity reduced the risk of developing diabetes by 58%—nearly double the 31% reduction achieved with metformin alone (8). These outcomes rival or exceed many pharmaceutical interventions, yet physicians receive minimal training in implementing such dietary strategies.
Current clinical care guidelines recognize nutrition as a primary intervention, with the American Heart Association and American College of Cardiology positioning “healthy lifestyle” at the apex of their treatment algorithms for both primary and secondary prevention of atherosclerotic cardiovascular disease (9). The disconnect between guideline recommendations and physician preparedness raises a fundamental question: how can clinicians effectively implement these evidence-based recommendations without adequate training in nutrition?
Five compelling reasons underscore why nutrition education deserves special attention in medical training reform. First, the U.S. Burden of Disease Collaborators have identified poor-quality diet as the leading cause of death in the United States, with the prevalence and cost of diet-related diseases predicted to continue climbing if left unchecked (10, 11). Second, there is renewed interest in shifting healthcare from disease management to health promotion and prevention- areas that physicians will find difficult to advance without a solid foundation in nutrition education and counseling (12). Third, patients are bombarded with confusing and often contradictory nutrition messages from media sources, creating an urgent need for physicians to provide authoritative, evidence-based guidance. Fourth, there is increasing attention on the wellness and self-care of residents and fellows, and nutrition education has the potential to enhance physician wellbeing while making them more effective counselors. Lastly, the economic case for nutrition education is becoming increasingly compelling as primary prevention makes more economic sense than expensive secondary and tertiary care.
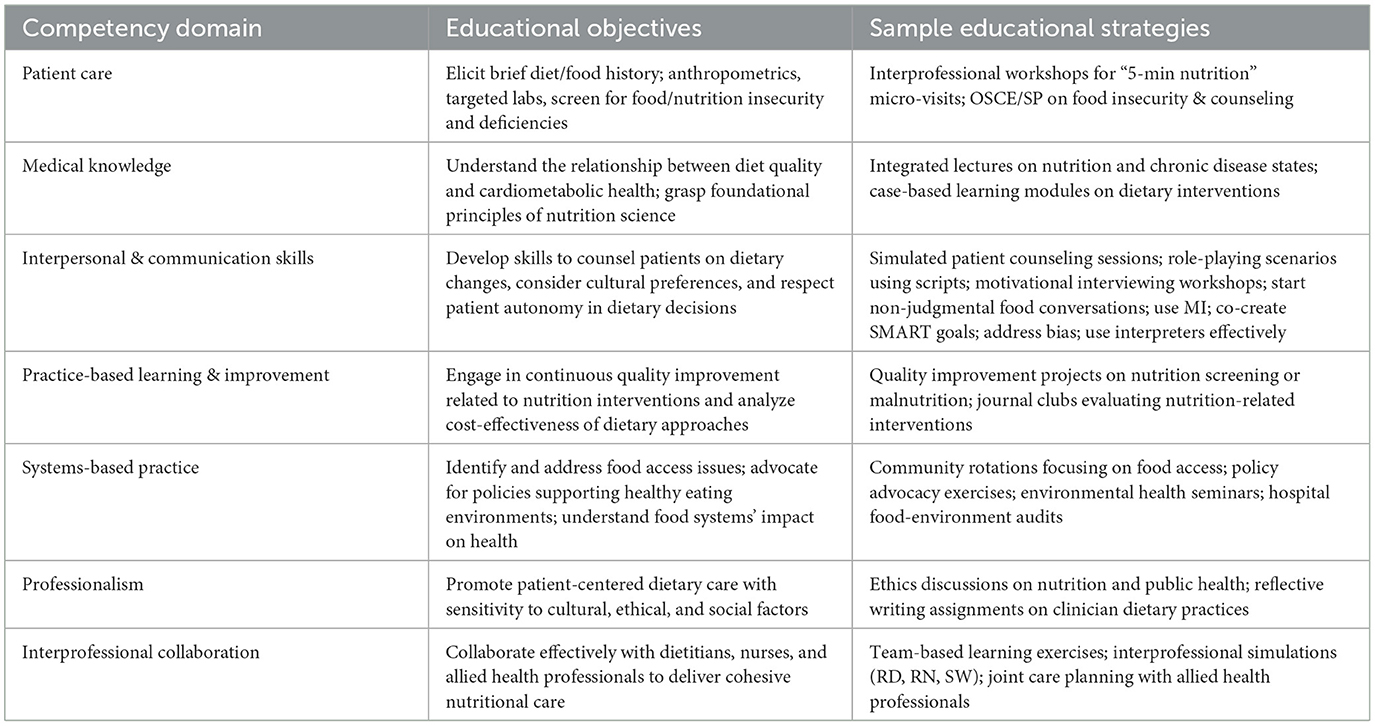
Frameworks should encompass multiple educational strategies across different competency domains. Medical knowledge competencies should include understanding the relationship between diet quality and cardiometabolic health, while interpersonal and communication skills should encompass effective dietary counseling techniques that consider patient goals and social determinants of health. Clinicians who are going into fields such as family medicine, obstetrics, pediatrics, or internal medicine in particular should have targeted, clinically relevant nutrition education in residency training as it may not be feasible to cover detailed clinical information comprehensively within an already dense undergraduate medical curriculum. Interdisciplinary collaboration and communication with nutrition experts can support and enhance clinical decision-making and promote effective patient care. Practice-based learning and improvement competencies should address cost-effectiveness of dietary interventions and quality improvement projects targeting nutritional factors. Systems-based practice competencies should explore food accessibility, environmental determinants of health, and advocacy for policy changes that support healthy dietary patterns (Table 1).
The integration of comprehensive nutrition education into medical training demands that nutrition should not be considered an isolated discipline but rather a vital, practical determinant of health woven throughout existing curricula. Beyond curricular changes, healthcare institutions can demonstrate their commitment to nutrition by aligning their practices with their educational messages. Medical training programs and conferences should serve foods that align with the USDA Dietary Guidelines for Americans and AHA Healthy 8, replacing the highly and ultra-processed foods commonly found at medical gatherings (9).
Some might argue that physicians do not need extensive nutrition education because other healthcare professionals, including dietitians, are better positioned to make dietary recommendations. However, when physicians understand and adopt healthy lifestyle behaviors, they are often more effective at guiding their own patients toward healthy changes (13). Organizations such as the American College of Lifestyle Medicine which certifies healthcare professionals in lifestyle medicine, including nutrition have successfully included nutrition as a core component of medical education, along with specific strategies these institutions have adopted, would enrich the discussion and demonstrate how such efforts are shaping the future of medical training. In addition, healthy behavior change requires a coordinated team effort that can include appropriately trained dietitians, nutritionists, nurses, health coaches, and culinary professionals. The problem is that most physicians currently lack sufficient education to contribute meaningfully to this team. At minimum, physicians need adequate training to initiate nutrition conversations with patients and make effective referrals and address behavior change during patient encounters (14).
Moreover, a more balanced and impactful approach to patient care recognizes the value of interdisciplinary care management. A well-trained healthcare team consisting of nurse practitioners, physician assistants, dietitians, community health workers, and other allied health professionals can drive improvements in chronic disease management, reduce healthcare costs, and enhance outcomes across diverse populations. This collaborative model is especially critical in rural and underserved communities where physician shortages persist. In such settings, empowering the broader care team with shared nutritional knowledge ensures that patients receive consistent, evidence-based dietary guidance. Integrating nutrition competencies across disciplines also enhances team-based care, promoting shared decision-making, continuity, and patient trust.
Secretary Kennedy's directive represents a historic opportunity to transform medical education and improve patient outcomes through evidence-based nutrition training. The medical community must embrace this moment to build comprehensive, integrated nutrition curricula that prepare physicians to address the chronic disease epidemic. By equipping future physicians with the knowledge and skills to promote nutritious dietary patterns, we can achieve better health outcomes for our patients while reducing healthcare costs and advancing the fundamental mission of medicine: to prevent disease and promote health (15). In an era marked by escalating diet-related disease burdens, incremental progress is no longer sufficient. A comprehensive, interdisciplinary approach to nutrition education must now be recognized as an essential component of patient care and public health.
Author contributions
SK: Conceptualization, Writing – review & editing. EC: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. RFK Jr. to Tell Medical Schools to Teach Nutrition or Lose Federal Funding. ABC News (2025). Available online at: https://abcnews.go.com/Politics/rfk-jr-medical-schools-teach-nutrition-lose-federal/story?id=122482788 (Accessed June 16, 2025).
2. H.Res.1118 - 117th Congress (2021-2022): Expressing the Sense of the House of Representatives that the United States Recognizes the Mounting Personal and Financial Burden of Diet-Related Disease in the United States and Calls on Medical Schools, Graduate Medical Education Programs, and Other Health Professional Training Programs to Provide Meaningful Physician and Health Professional Education on Nutrition and Diet. Congress.gov | Library of Congress (2022). Available online at: https://www.congress.gov/bill/117th-congress/house-resolution/1118/committees (Accessed June 16, 2025).
3. Adams KM, Butsch WS, Kohlmeier M. The state of nutrition education at US medical schools. J Biomed Educ. (2015) 1:1–7. doi: 10.1155/2015/357627
4. Common Program Requirements (2023). Available online at: https://www.acgme.org/programs-and-institutions/programs/common-program-requirements/ (Accessed June 16, 2025).
5. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lacent. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
6. Qian F, Liu G, Hu FB, Bhupathiraju SN, Sun Q. association between plant-based dietary patterns and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA Intern Med. (2019) 179:1335–44. doi: 10.1001/jamainternmed.2019.2195
7. GBD 2021 US Obesity Forecasting Collaborators. National-level and state-level prevalence of overweight and obesity among children, adolescents, and adults in the USA, 1990–2021, and forecasts up to 2050. Lancet. (2024) 404:2278–98. doi: 10.1016/S0140-6736(24)01548-4
8. Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean Diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. (2018) 378:e34. doi: 10.1056/NEJMoa1800389
9. Diabetes Prevention Program (DPP) (2015). Available online at: https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp (Accessed June 16, 2025).
10. The US Burden of Disease Collaborators. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. (2018) 319:1444–72. doi: 10.1001/jama.2018.0158
11. Mozaffarian D, Callahan EA, Frist WH. The MAHA commission report and diet-related diseases in youth. JAMA. (2025) 4:487–8. doi: 10.1001/jama.2025.11413
12. Life's Essential 8 - How to Eat Better Fact Sheet from American Heart Association (2022). Available online at: https://www.heart.org/en/healthy-living/healthy-lifestyle/lifes-essential-8/how-to-eat-better-fact-sheet (Accessed June 16, 2025).
13. Aggarwal M, Devries S, Freeman AM, Ostfeld R, Gaggin H, Taub P, et al. The deficit of nutrition education of physicians. Am J Med. (2018) 131:339–45. doi: 10.1016/j.amjmed.2017.11.036
14. Oberg EB, Frank E. Physicians' health practices strongly influence patient health practices. J R Coll Physicians Edinb. (2009) 39:290–1. doi: 10.4997/JRCPE.2009.422
Keywords: plant-based diet, medical education, nutrition education, nutrition education and chronic disease, plant-forward diet
Citation: Kalwaney S and Cerceo E (2025) Nutrition as preventive medicine: a call for integration into medical education. Front. Public Health 13:1653382. doi: 10.3389/fpubh.2025.1653382
Received: 25 June 2025; Accepted: 22 August 2025;
Published: 11 September 2025.
Edited by:
Adelita Gonzales Cantu, The University of Texas Health Science Center at San Antonio, United StatesReviewed by:
Christiane Meireles, UT Health, San Antonio, United StatesRuth Grubesic, Schreiner University, United States
Copyright © 2025 Kalwaney and Cerceo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elizabeth Cerceo, Y2VyY2VvLWVsaXphYmV0aEBjb29wZXJoZWFsdGguZWR1
†ORCID: Elizabeth Cerceo orcid.org/0000-0003-3155-2193
 Shirley Kalwaney
Shirley Kalwaney Elizabeth Cerceo
Elizabeth Cerceo