- 1Department of Nursing, West China Second University Hospital, Sichuan University/ West China School of Nursing, Sichuan University, Chengdu, Sichuan, China
- 2Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), Ministry of Education, Chengdu, Sichuan, China
- 3Department of Obstetrics Nursing, West China Second University Hospital, Sichuan University/ West China School of Nursing, Sichuan University, Chengdu, Sichuan, China
Background: Body image is an individual’s internal representation of physical appearance. Perinatal depression, a psychological condition with severe implications, is influenced by body dissatisfaction. However, no studies have systematically quantified their association.
Objective: To evaluate the correlation between body image and depressive symptoms in the perinatal period through meta-analysis.
Methods: A systematic search was conducted in PubMed, Embase, The Cochrane Library, Medline, CNKI, Wanfang, and VIP databases, and studies assessing body image and perinatal depression were included. Two researchers independently screened, extracted, and assessed study quality. Meta-analysis used Review Manager 5.4, with the correlation coefficient (r) as the effect size, and studies assessing body image and perinatal depression were included.
Results: Twenty-eight studies involving 7,241 women were included. For pregnancy, the summary r for the reverse and forward scoring groups was 0.34 (95% CI: 0.24, 0.44; p < 0.01) and −0.34 (95% CI: −0.37, −0.30; p < 0.01), respectively. The four dimensions of body image (Feeling Fat, Attractiveness, Salience of Weight and Shape, and Strength and Fitness) were 0.34 (95% CI: 0.28, 0.40), −0.36 (95% CI: −0.42, −0.31), 0.31 (95% CI: 0.25, 0.36), and −0.32 (95% CI: −0.37, −0.26), respectively (all p < 0.01). For postpartum, the summary r = 0.35 (95% CI: 0.26, 0.43; p < 0.01) (reverse scoring group), and for the four dimensions: 0.30 (95% CI: 0.23, 0.38), −0.41 (95% CI: −0.46, −0.36), 0.27 (95% CI: 0.20, 0.35), and −0.34 (95% CI: −0.39, −0.28), respectively (all p < 0.01). The results for all subgroups were robust, with no significant publication bias.
Conclusion: Body dissatisfaction is consistently and moderately associated with perinatal depression. Early identification and interventions may help prevent depression and improve maternal–infant health outcomes.
Systematic review registration: PROSPERO, identifier CRD42025639158, https://www.crd.york.ac.uk/PROSPERO/view/CRD42025639158.
1 Introduction
The perinatal period is a unique phase in women’s lives, characterized by multiple transitions in physical, psychological, and social roles. During this period, they not only undergo significant changes but also face psychological challenges associated with identity transformation (1, 2), making it a vulnerable stage for the development of mental health problems (3). Perinatal depression, defined as depression occurring during pregnancy or postpartum, is a particularly pressing mental health concern. Data from the United States Centers for Disease Control and Prevention indicated that pregnancy-related deaths caused by mental health disorders accounted for 22.7% of deaths from 2017 to 2019 in the U. S., making it a major contributor to perinatal mortality (4). Beyond impairing maternal mental health, perinatal depression exerts far-reaching implications on offspring and families. Specifically, pregnancy-related depression may increase the risk of adverse outcomes, such as fetal growth restriction, preterm birth, and low birth weight; elevate the incidence of postpartum depression and spousal depression; and reduce breastfeeding rates (5). Postpartum depression can disrupt the mother-infant bonding (6), which may, in turn, impair the normal development of children’s emotions, cognition, and behaviors (7) and lead to maternal role maladaptation and decreased quality of life (6).
Beyond the impacts, previous studies have identified multiple risk factors for perinatal depression, including a history of depression, inadequate social and economic support, chronic stressful life events, unintended pregnancies (8), and traumatic childbirth experiences (9). In recent years, body image has emerged as an increasingly recognized factor influencing perinatal mental health. Growing evidence links body image to several perinatal outcomes, such as postpartum anxiety, depression, eating disorders, mother-infant bonding, and other problems (10–13). Most of these studies were conducted in Western contexts, with relatively fewer studies from Asian populations.
Body image is defined as an individual’s internal representation of their physical appearance, encompassing three dimensions: cognition, affective, and behavioral intention (14, 15). While societal ideals of female beauty have evolved over time, women consistently face pressure to conform to the mainstream aesthetics of their respective societies. Chronic social comparison of one’s appearance to these societal ideals may lead to cognitive biases, which in turn may result in body image disturbance or body dissatisfaction—negative perceptions and evaluations of one’s physical appearance (14, 15). Existing research has established a moderate-to-strong association between body dissatisfaction and adverse mental health outcomes, including depression, anxiety, and distress (16). Although pregnancy is often perceived as a “protected” phase, growing evidence emphasizes that sociocultural pressures persist, driving women to pursue unrealistic bodily and aesthetic ideals (2, 17).
During pregnancy, rapid physiological changes in women’s bodies may further diverge from societal ideals of body shape, prompting the reassessment of body image (18). Evidence from the United States suggests that over 50% of perinatal women experience body dissatisfaction (19, 20). Unlike the non-pregnant states, the changes during pregnancy are normal physiological adaptations to support fetal development. U.S.-based research investigating behaviors associated with positive body image among postpartum mothers has shown that some women prioritize maternal bodily function over aesthetic concerns, facilitating adaptive re-evaluation of their body image and psychological adjustment (10, 21). In contrast, others struggle to accept these changes, experiencing heightened awareness of altered physical appearance and negative emotions toward their bodies—even perceiving these changes as threats to their self-identity (22). Negative body image during pregnancy has been linked to a range of adverse maternal and child health outcomes, most prominently pregnancy and postpartum depression (17, 23–25). Beyond this, negative body image is also significantly associated with impaired emotion regulation (26). For instance, a French study found that women with body dissatisfaction were four times more likely to develop perinatal depression (27). Similarly, a large longitudinal study from Hong Kong, China, indicated that body dissatisfaction may either precede depression and anxiety (25) or serve as a somatic manifestation of emotional symptoms. Given these associations, assessing body image could serve as an effective tool for early identification of perinatal depression.
Although many studies and narrative reviews have explored and summarized the role of body image in perinatal depression, they did not provide a quantitatively synthesized effect size or examine stage-specific differences. Most of the existing evidence, particularly from countries such as Australia and the United States, is based on individual observational studies, making it difficult to draw consistent conclusions. Therefore, a meta-analytic approach is needed to integrate the fragmented evidence and provide a precise quantitative estimate of this association. Accordingly, the aim of this review is to (1) systematically assess and quantify the association between body image and perinatal depression; (2) explore potential differences in the strength of this association between the pregnancy and postpartum periods through subgroup analysis; and (3) provide evidence to increase healthcare professionals’ attention to body shape and weight-related pressures experienced by perinatal women, thereby supporting the integration of body image assessment into routine perinatal care.
2 Materials and methods
This meta-analysis is registered in the International Prospective Register of Systematic Reviews (PROSPERO) trial registry (CRD42025639158) and was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.1 Search strategy
The following databases were searched to identify relevant research: PubMed, Embase, The Cochrane Library, Medline, China National Knowledge Infrastructure (CNKI), Wanfang Database, and VIP Chinese Journal Database (VIP). Additionally, the reference lists of included studies were checked for a complete literature search. Searches covered the period from the inception of each database to December 2024. The search strategies are presented in Supplementary Data 1.
A combination of subject terms and free-text terms was used for the search:
Subject Terms: Pregnancy, Pregnancy Trimester; Body Image, Body Dissatisfaction; Depression, Postpartum, Puerperal Disorders, Depressive Disorder/Postnatal Depression.
Free-text Terms: pregnant*, gravida*, matern*, gestation, prenatal, antenatal; body satisfaction, body appreciation, body concerns, body image disturbance, body schema*, body representation*; postpartum depression, postnatal depression, depression, postnatal, perinatal depression, puerperium depression, new mother depression, maternal depression, postpartum mood disorders, depression after childbirth, post-birth depression, baby blues.
2.2 Selection criteria
The inclusion and exclusion criteria for this study were as follows:
Inclusion Criteria:
1. Study population: women during pregnancy or the postpartum period;
2. Outcome measurements: assessment of both body image and depressive symptoms during pregnancy or the postpartum period;
3. Statistical analysis: reporting of correlation analysis between the body image and depressive symptoms;
4. Language: studies published in Chinese or English.
Exclusion Criteria:
1. Outcome measurement: Use of self-designed questionnaires without validation.
2. Accessibility: unavailability of the full text.
3. Data availability: failure to report or extract specific correlation coefficients.
2.3 Literature screening
Retrieved records were first de-duplicated using EndNote X9 software. Two independent authors then screened the titles and abstracts to exclude ineligible studies, including animal studies, reviews, systematic reviews, meta-analyses, qualitative studies, and case reports based on titles and abstracts. After reading the full text, studies with irrelevant content or those lacking correlation coefficients were further excluded. Any disagreements were resolved through discussion with the research team.
2.4 Quality assessment
Two independent authors used the Agency for Healthcare Research and Quality (AHRQ) checklist to assess the quality of the included studies. Referring to a previous meta-analysis (28), each item of the AHRQ checklist was scored as 1 point (for “yes” responses) or 0 points (for “no” or “unclear” responses). A total score of 0–3 was categorized as low quality, 4–7 as medium quality, and 8–11 as high quality. The quality assessment process was the same as the literature screening.
2.5 Data extraction
Two independent authors extracted data from each included study: the first author, publication year, country, study design, sample size, maternal age, timing of outcome measurement, measurement tools and scores, and correlation coefficients between body image and depression symptoms.
2.6 Outcome measures
2.6.1 Body image levels
The body image was assessed using two categories of measurement tools: pregnancy-specific tools and universal tools.
Pregnancy-specific tools: The Body Understanding Measure for Pregnancy Scale (BUMPs) (29) and the Body Image in Pregnancy Scale (BIPS) (30).
Universal tools: The Body Attitudes Questionnaire (BAQ) (31), Body Shape Questionnaire (BSQ) (32), Eating Disorder Inventory (EDI) (33), Body Cathexis Scale (BCS) (34), Body Image Concern Inventory (BICI) (35), Body Areas Satisfaction Scale (BASS) (36), and Body Self Questionnaire (BSQ-self) (37). Among these tools, the Body Part Satisfaction Scale (BPSS) (38), Body Image Scale (BIS) (39), and BASS (36) are scored in the forward direction; higher scores indicate greater body satisfaction, while the other tools are scored in the reverse direction; higher scores indicate greater body dissatisfaction.
2.6.2 Depression levels
Depressive symptoms were assessed using the following tools: Edinburgh Postnatal Depression Scale (EPDS) (40), Beck Depression Inventory (BDI) (41), Hospital Anxiety and Depression Scale (HADS) (42), Center for Epidemiologic Studies Depression Scale (CES-D) (22), and the Depression subscale of the Depression, Anxiety, and Stress Scale (DASS) (43).
2.7 Data analysis
Statistical analyses were performed using Review Manager 5.4, with a significance level set at p < 0.05.
Heterogeneity was assessed using Cochran’s Q test and the I2 statistics (44–46). The pooled effect size was estimated based on heterogeneity results: a fixed-effects model was used if p > 0.1 and I2 < 50% (low-to-moderate heterogeneity), whereas a random-effects model was used if p < 0.1 and I2 ≥ 50% (high heterogeneity).
Pearson’s correlation coefficient (r) was used as the effect size to quantify the association between body image and depressive symptoms. For meta-analysis, (1) Spearman’s correlation coefficients from individual studies were first converted to Pearson’s r. (2) All Pearson’s r values were transformed using Fisher’s z-transformation. (3) Inverse transformation of Fisher’s z-scores was performed to estimate the summary correlation coefficient (summary r) (47). The detailed formulas are provided in Supplementary Data 2. When multiple subgroup results were reported in one study, each result was treated as an independent study.
Subgroup analyses were conducted according to the timing of outcome measurement (pregnancy/postpartum) and the scoring direction of body image tools (forward/reverse scoring). Sensitivity analysis was performed using the leave-one-out method to evaluate the robustness of the pooled result. Publication bias was assessed using funnel plots and the trim-and-fill method in R 4.4.2. The detailed R codes are provided in Supplementary Data 3.
3 Results
3.1 Literature search results
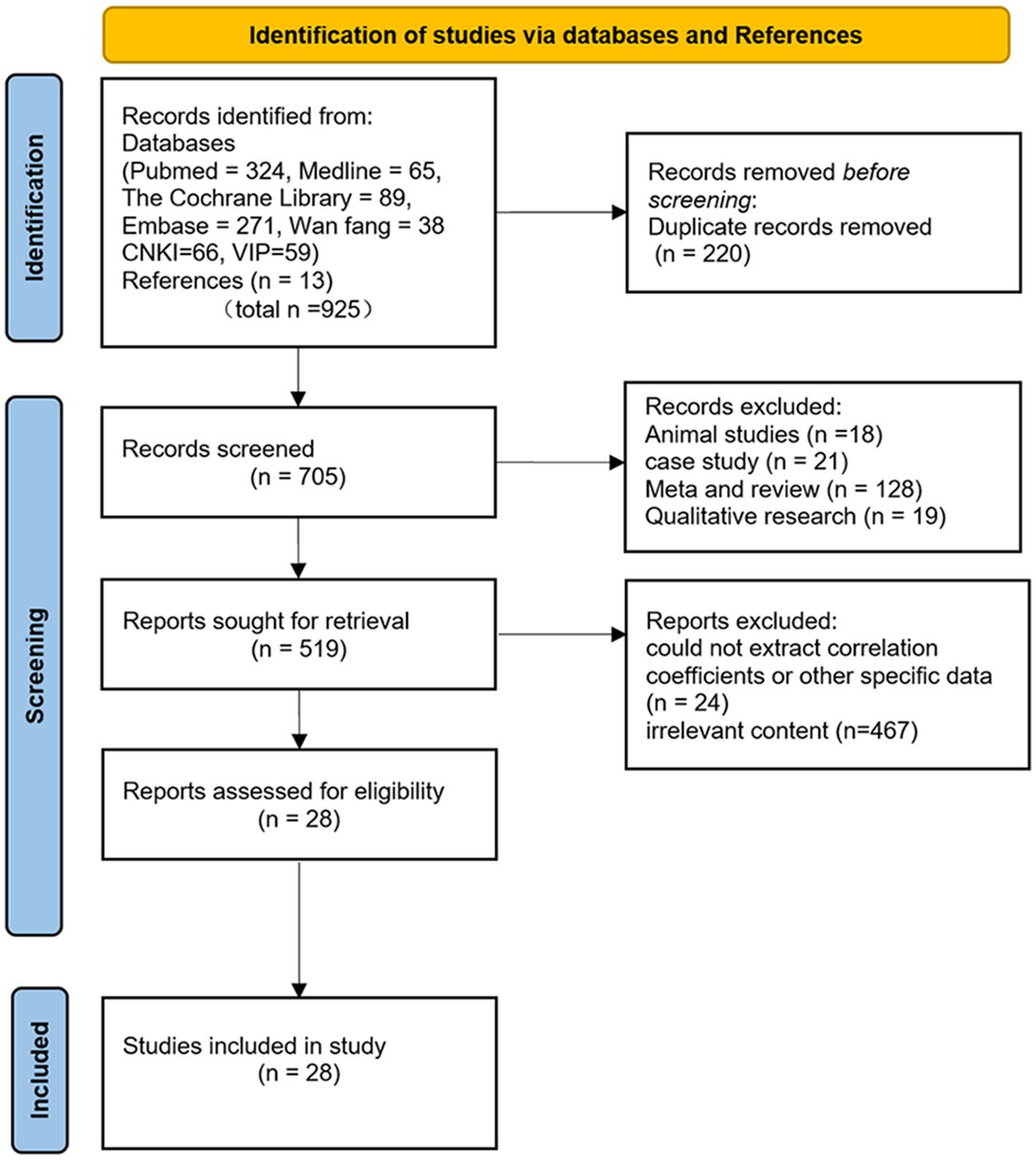
The results of the literature search and screening process are illustrated in Figure 1 (PRISMA flowchart). A total of 925 records were retrieved from the databases. After removing 220 duplicates, 705 records were screened based on titles and abstracts. During this screening stage, 186 records were excluded (including animal studies, narrative reviews, systematic reviews, meta-analyses, case reports, and qualitative studies), leaving 519 records for full-text assessment. After full-text review, 467 records were excluded due to irrelevant content, and 24 records could not extract correlation coefficients or other specific data. Ultimately, 28 articles that met the inclusion and exclusion criteria were included in the meta-analysis (17, 39, 48–73).
3.2 Characteristics of included studies
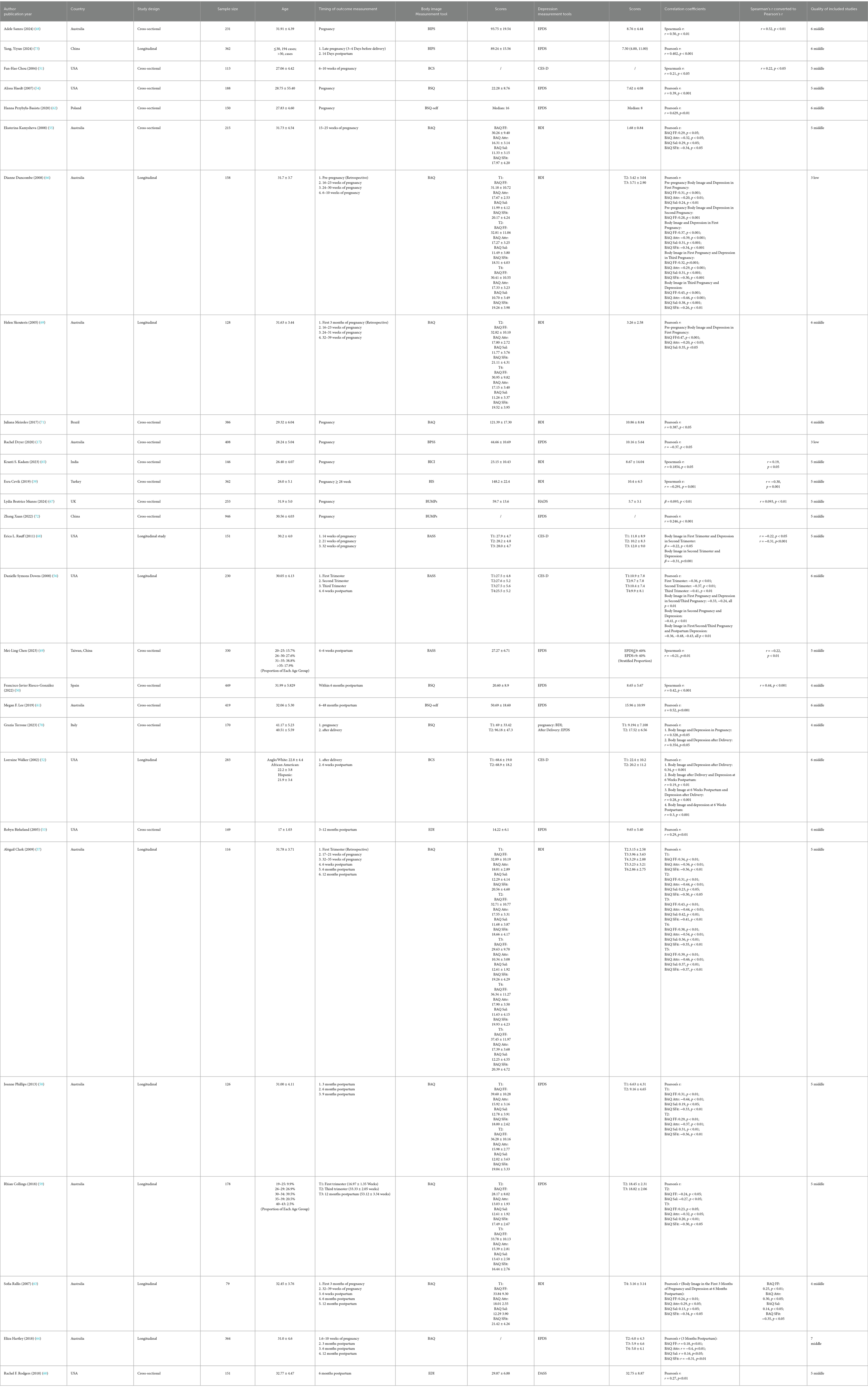
The 28 included studies comprised a total sample of 7,241 women. Seventeen were cross-sectional studies (17, 39, 48–51, 53–55, 60–62, 65, 67, 70–72), and 11 were longitudinal (52, 56–59, 63, 64, 66, 68, 69, 73). Geographically, the majority of studies were conducted in Australia (n = 11) (17, 48, 55, 57–59, 61, 63, 64, 66, 69), followed by the United States (n = 7) (51–54, 56, 60, 68), and 3 from China (49, 72, 73). The studies covered three time periods: pre-pregnancy, pregnancy, and postpartum. Seventeen studies reported the correlation coefficients for body image and depression during pregnancy (17, 39, 48, 51, 54–57, 59, 62, 65–68, 70–72), eleven reported the correlation coefficients for postpartum body image and postpartum depression (49, 50, 52, 53, 57–61, 64, 70), one study reported the correlation coefficients for pre-pregnancy body image and postpartum depression (63), two reported the correlation coefficients for pre-pregnancy body image and pregnancy depression (66, 69), and two reported the correlation coefficients for pregnancy body image and postpartum depression (56, 73). For depression assessment, the Edinburgh Postnatal Depression Scale (EPDS) was the most widely used tool (n = 14) (17, 48–50, 53, 54, 58, 59, 61, 62, 64, 70, 72, 73). For body image measurement, the Body Attitudes Questionnaire (BAQ) was the most frequently used (n = 9) (55, 57–59, 63, 64, 66, 69, 71) (Table 1).
3.3 Quality assessment results
The quality of the 28 included studies was assessed using the 11-item AHRQ checklist. Of the 28 studies, 2 studies were rated as low quality (17, 66), and the remaining 26 were rated as moderate quality (39, 48–64, 67–73). No high-quality studies were identified. None of the studies described measures taken to ensure data quality and/or control for confounding factors, resulting in a score of 0 for these items. Among the 11 longitudinal studies, all except two (52, 58) described the completeness of follow-up data. Three studies did not report participant response rates or data collection completeness (49, 53, 70). Detailed quality assessment scores for each study are presented in Table 1 and Supplementary Table 1.
3.4 Meta-analysis results
Subgroup analyses were conducted based on the timing of outcome measurement and the scoring direction of body image measurement tools. For studies using the BAQ, subgroup analyses were performed for its four dimensions (Feeling Fat, FF; Strength and Fitness, SFit; Salience of Weight and Shape, Sal; Attractiveness, Attr). The overall forest plot for all meta-analyses is shown in Figures 2, 3.
3.4.1 Correlation between body image and depression symptoms during pregnancy
Reverse-Scoring Body Image Scales (BIPS, BCS, BSQ, EDI, BUMPs, BICI): A meta-analysis of 9 studies (48, 51, 54, 62, 65, 67, 70–72) using a random-effects model showed the following results: summary Fisher’s Z = 0.35 (95% CI: 0.24, 0.47; p < 0.01), I2 = 87% (high heterogeneity), summary r = 0.34 (95% CI: 0.24, 0.44). The effect size was statistically significant, indicating a moderate positive correlation between body dissatisfaction and depression during pregnancy.
Forward-Scoring Body Image Scales (BPSS, BIS, BASS): A meta-analysis of 4 studies (17, 39, 56, 68) using a random-effects model showed the following results: summary Fisher’s Z = −0.35 (95% CI: −0.39, −0.31; p < 0.01), I2 = 10% (low heterogeneity), summary r = −0.34 (95% CI: −0.37, −0.30). The effect size was statistically significant, indicating a moderate negative correlation between body satisfaction and depression during pregnancy.
BAQ Subgroup Analysis: After excluding outliers (details in Section 3.5 Sensitivity Analysis), the meta-results of 3 studies (55, 57, 66) were as follows:
FF: summary Fisher’s Z = 0.35 (95% CI: 0.29, 0.42; p < 0.01), I2 = 0%, summary r = 0.34 (95% CI: 0.28, 0.40);
Attr: summary Fisher’s Z = −0.38 (95% CI: −0.45, −0.32; p < 0.01), I2 = 0%, summary r = −0.36 (95% CI: −0.42, −0.31);
Sal: summary Fisher’s Z = 0.32 (95% CI: 0.25, 0.38; p < 0.01), I2 = 0%, summary r = 0.31 (95% CI: 0.25, 0.36);
SFit: summary Fisher’s Z = −0.33 (95% CI: −0.39, −0.27; p < 0.01), I2 = 0%, summary r = −0.32 (95% CI: −0.37, −0.26).
All dimensions showed statistically significant effect sizes with low heterogeneity. Perceptions of fatness and weight/shape were moderately positively correlated with depression, while perceptions of strength, fitness, and attractiveness were moderately negatively correlated with depression.
3.4.2 Correlation between body image and depression symptoms during postpartum
Only one article (49) used a forward-scoring scale; a descriptive analysis was performed directly: this study reported a negative correlation between body satisfaction and postpartum depressive symptoms.
Reverse-Scoring Body Image Scales (BIPS, BCS, BSQ, EDI, BUMPs, BICI): A meta-analysis of 6 studies (50, 52, 53, 60, 61, 70) using a random-effects model showed the following results: summary Fisher’s Z = 0.36 (95% CI: 0.27, 0.46; p < 0.01), I2 = 79% (high heterogeneity), summary r = 0.35 (95% CI: 0.26, 0.43). The effect size was statistically significant, indicating a moderate positive correlation between body dissatisfaction and depression during the postpartum period.
BAQ Subgroup Analysis: The meta-results of 4 studies (57–59, 64) were as follows:
FF: summary Fisher’s Z = 0.31 (95% CI: 0.23, 0.40; p < 0.01), I2 = 46% (moderate heterogeneity), summary r = 0.30 (95% CI: 0.23, 0.38);
Attr: summary Fisher’s Z = −0.44 (95% CI: −0.50, −0.38; p < 0.01), I2 = 2%, summary r = −0.41 (95% CI: −0.46, −0.36);
Sal: summary Fisher’s Z = 0.28 (95% CI: 0.20, 0.37; p < 0.01), I2 = 52% (moderate heterogeneity), summary r = 0.27 (95% CI: 0.20, 0.35);
SFit: summary Fisher’s Z = −0.35 (95% CI: −0.41, −0.29; p < 0.01), I2 = 0%, summary r = −0.34 (95% CI: −0.39, −0.28).
All dimensions showed statistically significant effect sizes, with moderate heterogeneity for FF and Sal dimensions and low heterogeneity for Attr and SFit dimensions. Perceptions of fatness and weight/shape were moderately positively correlated with depression, while perceptions of strength, fitness, and attractiveness were moderately negatively correlated with depression.
3.5 Sensitivity analysis
Sensitivity analysis using the leave-one-out method showed that the overall meta-results were robust, and it was not performed for the “pre-pregnancy body image and depression symptoms in pregnancy” subgroup due to the small number of included studies (n = 2). The rest of the detailed results are presented in Supplementary Tables 2.1, 2.2.
For the FF and Sal dimensions of the BAQ during pregnancy, excluding the study by Rhian Collings (59), significantly reduced heterogeneity (FF: I2 from 90 to 0%; Sal: I2 from 91 to 0%) and altered the effect sizes (FF: from 0.27 [0.10, 0.45] to 0.30 [0.29, 0.42]; Sal: from 0.22 [0.02, 0.41] to 0.32 [0.25, 0.38]). Given the negative effect size in this study, contrary to the rest of the studies, combined with the sensitivity analysis results, the data from this study was classified as an outlier and excluded from the final analysis.
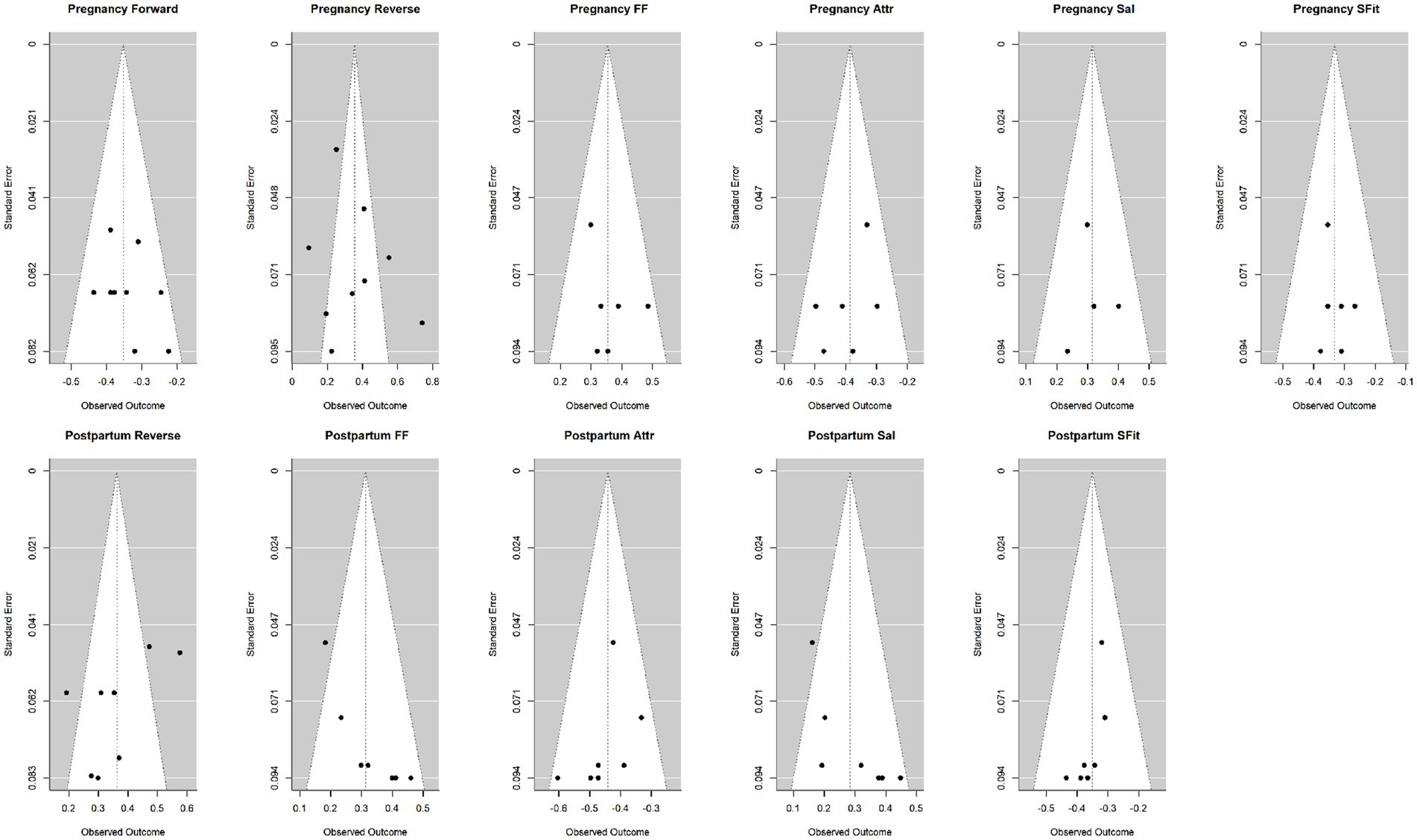
3.6 Publication bias assessment
Funnel plots and the trim-and-fill method were used to assess publication bias. Publication bias analysis was not performed for the “pre-pregnancy body image and depression symptoms during pregnancy” subgroup (n = 2, insufficient for reliable funnel plot interpretation). No significant publication bias was observed for the pregnancy subgroups (0–2 missing studies). There was a slight publication bias in the postpartum subgroups (particularly for the FF dimension), which may limit the interpretation of results. The funnel plots and the results of the trim-and-fill method are provided in Figure 4 and Supplementary Table 3.
4 Discussion
This meta-analysis synthesized 28 studies to quantify the association between body image and perinatal depression, addressing a critical gap in prior quantitative synthesis. The results indicate a significant, moderate association between body image and perinatal depression, which is consistent with multiple previous studies and narrative reviews (17, 23–25, 27, 29, 74). Women who are more satisfied with their body image are less likely to have depression during pregnancy and postpartum, reinforcing body image disturbance as an important risk factor for perinatal depression. This study extends prior work by explicitly testing for stage-specific differences. Although previous studies suggest that postpartum women experience less protective body image compared to pregnancy and are more susceptible to pressures of achieving an ideal postpartum body shape (13), our analysis did not find a significant difference between stages (Table 2). To ensure that our findings reflect the most up-to-date evidence, we conducted a supplementary search in September 2025 for studies published after our original search period (up to December 2024). This additional search did not identify any eligible studies.
Subgroup analyses provided additional insights. Reverse-scored tools (pregnancy and postpartum) showed a significant positive correlation between body dissatisfaction and depression symptoms. Forward-scored tools (during pregnancy) indicated a significant negative correlation between body image satisfaction and depression symptoms. BAQ subgroup analysis further revealed dimension-specific differences in body image: perception of body fat (FF), salience of weight and body shape (Sal) showed positive correlations with depression, while perception of body attractiveness (Attr) and physical strength and fitness (SFit) correlated negatively. The subgroup analyzing pre-pregnancy body image and depression symptoms during pregnancy showed the same results, but with only 2 included studies (no sensitivity/publication bias analyses).
Body image disturbance may contribute to depression via various psychological and social pathways. Psychologically, body dissatisfaction may directly reduce self-esteem and self-worth, creating a vicious cycle where low self-esteem exacerbates negative feelings about appearance and attractiveness (12, 75). Additionally, depressive symptoms such as guilt, worthlessness, and hopelessness, as well as rumination and catastrophic thinking, can further amplify focus on perceived bodily “flaws,” deepening this cycle (76). In terms of social factors, exposure to idealized slimness can negatively affect body image and mood, while positive portrayals of bodily changes offer protection (77–79). Social support, particularly from partners, is also critical—receiving positive feedback on their bodies from partners is an overwhelmingly positive experience for women, and those whose partners are delighted with their body shape tend to show greater body satisfaction (80, 81). Family involvement more broadly may help reduce societal pressures and promote healthier adjustment to bodily changes.
Therefore, body image could be considered as part of prenatal mental health screening, and the assessment may be an effective tool for early identification of perinatal depression (25, 27, 29). However, less than one-third of professionals assess or discuss body image in routine prenatal care (82, 83), and nearly 20% of women report weight-related stigma in healthcare settings (84). As a result, a growing number of studies are calling for increased training for healthcare professionals to provide more specialized support for pregnant women (27, 85, 86), especially since over 80% of women are willing to participate in body image-focused programs (19). Prenatal courses and psychological education that emphasize normal physical changes and highlight the body’s functionality may help pregnant women reduce excessive concerns about appearance and may therefore represent promising strategies to support maternal mental health (87). Although this study provides a theoretical basis for the association between body image and depression during the perinatal period, there are some limitations. First, high heterogeneity in pregnancy (I2 = 87%) and postpartum (I2 = 79%) reverse-scoring subgroups, probably due to differences in the measurement tools, which somewhat limits the explanatory power of the results. Second, the small number of studies in some subgroups (e.g., pre-pregnancy body image) affected the generalizability of the results.
This study is the first meta-analysis to quantify the association between body image and perinatal depression, reinforcing the view that body image disturbance is an important risk factor and providing scientific evidence for clinical practice. Future research should adopt longitudinal designs or risk-based metrics (e.g., odds ratios or risk ratios) to more directly quantify the likelihood of perinatal depression associated with body dissatisfaction, thereby offering a clearer understanding of the magnitude of this risk. In addition, future studies should design and implement interventions to improve body image, which may provide new pathways for supporting maternal mental health.
5 Conclusion
This meta-analysis indicate a significant, moderate association between body image and perinatal depression, highlighting the importance of body image in this period. Early identification and targeted interventions may help reduce the risk of perinatal depression and improve maternal and infant health outcomes. Future research can further explore the mechanisms and develop intervention strategies to support clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
JH: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft. XC: Data curation, Formal analysis, Methodology, Writing – original draft. BL: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We want to thank all the researchers and participants who contributed to this study. Special thanks to our supervisor, Biru Luo, for her invaluable guidance and support throughout the research and manuscript preparation process. We also extend our appreciation to the editors and reviewers for their insightful comments and constructive criticism.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1655639/full#supplementary-material
References
1. Penner, F, and Rutherford, HJV. Emotion regulation during pregnancy: a call to action for increased research, screening, and intervention. Arch Womens Ment Health. (2022) 25:527–31. doi: 10.1007/s00737-022-01204-0
2. Prinds, C, Nikolajsen, H, and Folmann, B. Yummy mummy - the ideal of not looking like a mother. Women Birth. (2020) 33:e266–73. doi: 10.1016/j.wombi.2019.05.009
3. Langan, R, and Goodbred, AJ. Identification and Management of Peripartum Depression. Am Fam Physician. (2016) 93:852–8.
4. Justesen, K, and Jourdaine, D. Peripartum depression: detection and treatment. Am Fam Physician. (2023) 108:267–72.
5. Field, T. Prenatal depression risk factors, developmental effects and interventions: a review. J Pregnancy Child Health. (2017) 4:301. doi: 10.4172/2376-127X.1000301
6. Slomian, J, Honvo, G, Emonts, P, Reginster, JY, and Bruyère, O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Women's Health (Lond Engl). (2019) 15:1745506519844044. doi: 10.1177/1745506519844044
7. Goodman, JH. Perinatal depression and infant mental health. Arch Psychiatr Nurs. (2019) 33:217–24. doi: 10.1016/j.apnu.2019.01.010
8. Nelson, HD, Darney, BG, Ahrens, K, Burgess, A, Jungbauer, RM, Cantor, A, et al. Associations of unintended pregnancy with maternal and infant health outcomes: a systematic review and Meta-analysis. JAMA. (2022) 328:1714–29. doi: 10.1001/jama.2022.19097
9. Bay, F, and Sayiner, FD. Perception of traumatic childbirth of women and its relationship with postpartum depression. Women Health. (2021) 61:479–89. doi: 10.1080/03630242.2021.1927287
10. Gillen, MM, Markey, CH, Rosenbaum, DL, and Dunaev, JL. Breastfeeding, body image, and weight control behavior among postpartum women. Body Image. (2021) 38:201–9. doi: 10.1016/j.bodyim.2021.04.006
11. Dryer, R, Chee, P, and Brunton, R. The role of body dissatisfaction and self-compassion in pregnancy-related anxiety. J Affect Disord. (2022) 313:84–91. doi: 10.1016/j.jad.2022.06.068
12. Linde, K, Lehnig, F, Nagl, M, Stepan, H, and Kersting, A. Course and prediction of body image dissatisfaction during pregnancy: a prospective study. BMC Pregnancy Childbirth. (2022) 22:719. doi: 10.1186/s12884-022-05050-x
13. Singh Solorzano, C, Porciello, G, Violani, C, and Grano, C. Body image dissatisfaction and interoceptive sensibility significantly predict postpartum depressive symptoms. J Affect Disord. (2022) 311:239–46. doi: 10.1016/j.jad.2022.05.109
14. Murnen, S, Cash, T, Smolak, L, Cash, T, and Cash, TF. Body image: A handbook of science, practice, and prevention. (2012) New York, Publisher: Guilford Press.
15. Grogan, S. Body image: Understanding body dissatisfaction in men, women and children. 4th ed (2021). New York, Publisher: Guilford Press.
16. Emmer, C, Bosnjak, M, and Mata, J. The association between weight stigma and mental health: a meta-analysis. Obes Rev. (2020) 21:e12935. doi: 10.1111/obr.12935
17. Dryer, R, Graefin von der Schulenburg, I, and Brunton, R. Body dissatisfaction and fat talk during pregnancy: predictors of distress. J Affect Disord. (2020) 267:289–96. doi: 10.1016/j.jad.2020.02.031
18. Hill, B, Skouteris, H, McCabe, M, and Fuller-Tyszkiewicz, M. Body image and gestational weight gain: a prospective study. J Midwifery Womens Health. (2013) 58:189–94. doi: 10.1111/j.1542-2011.2012.00227.x
19. Vanderkruik, R, Ellison, K, Kanamori, M, Freeman, MP, Cohen, LS, and Stice, E. Body dissatisfaction and disordered eating in the perinatal period: an underrecognized high-risk timeframe and the opportunity to intervene. Arch Womens Ment Health. (2022) 25:739–51. doi: 10.1007/s00737-022-01236-6
20. Rodgers, RF, Campagna, J, Hayes, G, Sharma, A, Runquist, E, Fiuza, A, et al. Experiences of embodiment during pregnancy and the postpartum period: a qualitative study. Body Image. (2024) 48:101645. doi: 10.1016/j.bodyim.2023.101645
21. Raspovic, AM, Prichard, I, Yager, Z, and Hart, LM. Mothers’ experiences of the relationship between body image and exercise, 0–5 years postpartum: a qualitative study. Body Image. (2020) 35:41–52. doi: 10.1016/j.bodyim.2020.08.003
22. Radloff, LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
23. Hartley, E, Hill, B, McPhie, S, and Skouteris, H. The associations between depressive and anxiety symptoms, body image, and weight in the first year postpartum: a rapid systematic review. J Reprod Infant Psychol. (2018) 36:81–101. doi: 10.1080/02646838.2017.1396301
24. Nagl, M, Jepsen, L, Linde, K, and Kersting, A. Measuring body image during pregnancy: psychometric properties and validity of a German translation of the body image in pregnancy scale (BIPS-G). BMC Pregnancy Childbirth. (2019) 19:244. doi: 10.1186/s12884-019-2386-4
25. Chan, CY, Lee, AM, Koh, YW, Lam, SK, Lee, CP, Leung, KY, et al. Associations of body dissatisfaction with anxiety and depression in the pregnancy and postpartum periods: a longitudinal study. J Affect Disord. (2020) 263:582–92. doi: 10.1016/j.jad.2019.11.032
26. Spinoni, M, Singh Solorzano, C, and Grano, C. A prospective study on body image disturbances during pregnancy and postpartum: the role of cognitive reappraisal. Front Psychol. (2023) 14:1200819. doi: 10.3389/fpsyg.2023.1200819
27. Riquin, E, Lamas, C, Nicolas, I, Dugre Lebigre, C, Curt, F, Cohen, H, et al. A key for perinatal depression early diagnosis: the body dissatisfaction. J Affect Disord. (2019) 245:340–7. doi: 10.1016/j.jad.2018.11.032
28. Xie, W, Chen, L, Feng, F, Okoli, CTC, Tang, P, Zeng, L, et al. The prevalence of compassion satisfaction and compassion fatigue among nurses: a systematic review and meta-analysis. Int J Nurs Stud. (2021) 120:103973. doi: 10.1016/j.ijnurstu.2021.103973
29. Kirk, E, and Preston, C. Development and validation of the body understanding measure for pregnancy scale (BUMPS) and its role in antenatal attachment. Psychol Assess. (2019) 31:1092–106. doi: 10.1037/pas0000736
30. Watson, B, Fuller-Tyszkiewicz, M, Broadbent, J, and Skouteris, H. Development and validation of a tailored measure of body image for pregnant women. Psychol Assess. (2017) 29:1363–75. doi: 10.1037/pas0000441
31. Ben-Tovim, DI, and Walker, MK. The development of the Ben-Tovim Walker body attitudes questionnaire (BAQ), a new measure of women’s attitudes towards their own bodies. Psychol Med. (1991) 21:775–84. doi: 10.1017/S0033291700022406
32. Cooper, PJ, Taylor, MJ, Cooper, Z, and Fairbum, CG. The development and validation of the body shape questionnaire. Int J Eat Disord. (1987) 6:485–94. doi: 10.1002/1098-108X(198707)6:4<485::AID-EAT2260060405>3.0.CO;2-O
33. Garner, D. Eating disorder Inventory2: Professional manual. Odessa, FL: Psychological Assessment Resources (1991).
34. Secord, PF, and Jourard, SM. The appraisal of body-cathexis: body-cathexis and the self. J Consult Clin Psychol. (1953) 17:343–7. doi: 10.1037/h0060689
35. Littleton, HL, Axsom, D, and Pury, CL. Development of the body image concern inventory. Behav Res Ther. (2005) 43:229–41. doi: 10.1016/j.brat.2003.12.006
36. Cash, TF, Pruzinsky, T, and Cline, CJ. Body images: development, deviance and change. Ann Plast Surg. (1992) 29:94. doi: 10.1097/00000637-199207000-00023
37. Sakson-Obada, O, and Wycisk, J. The body self and the frequency, intensity and acceptance of menopausal symptoms. Menopause Review. (2015) 14:82–9. doi: 10.5114/pm.2015.52150
38. Slade, PD, Dewey, ME, Newton, T, Brodie, D, and Kiemle, G. Development and preliminary validation of the body satisfaction scale (BSS). Psychol Health. (1990) 4:213–20. doi: 10.1080/08870449008400391
39. Cevik, E, and Yanikkerem, E. The factors affecting self-esteem, depression and body image of pregnant women in a state hospital in Turkey. J Pak Med Assoc. (2019) 70:1159–1164. doi: 10.5455/JPMA.19892
40. Cox, JL, Holden, JM, and Sagovsky, R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
41. Beck, AT, and Beck, RW. Screening depressed patients in family practice. A rapid technic. Postgrad Med. (1972) 52:81–5. doi: 10.1080/00325481.1972.11713319
42. Zigmond, AS, and Snaith, RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
43. Lovibond, PF, and Lovibond, SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
44. Cochran, WG. The combination of estimates from different experiments. Biometrics. (1954) 10:101–29. doi: 10.2307/3001666
45. Higgins, JP, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
46. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
47. Borenstein, M, Hedges, LV, Higgins, JPT, and Rothstein, HR. Effect sizes based on correlations In: M Borenstein, LVH Hedges, JPT Higgins, and HR Rothstein, editors. Introduction to Meta-Analysis (2009). 41–3.
48. Samra, A, and Dryer, R. Problematic social media use and psychological distress in pregnancy: the mediating role of social comparisons and body dissatisfaction. J Affect Disord. (2024) 361:702–11. doi: 10.1016/j.jad.2024.06.057
49. Chen, M-L, and Chang, S-R. The relationship between body dissatisfaction and postpartum depressive symptoms: a cross-sectional study. J Affect Disord. (2023) 324:418–23. doi: 10.1016/j.jad.2022.12.102
50. Riesco-González, FJ, Antúnez-Calvente, I, Vázquez-Lara, JM, Rodríguez-Díaz, L, Palomo-Gómez, R, Gómez-Salgado, J, et al. Body image dissatisfaction as a risk factor for postpartum depression. Medicina (Kaunas). (2022) 58:752. doi: 10.3390/medicina58060752
51. Chou, FH, Lin, LL, Cooney, AT, Walker, LO, and Riggs, MW. Psychosocial factors related to nausea, vomiting, and fatigue in early pregnancy. J Nurs Scholarsh. (2004) 35:119–25. doi: 10.1111/j.1547-5069.2003.00119.x
52. Walker, L, Timmerman, GM, Kim, M, and Sterling, B. Relationships between body image and depressive symptoms during postpartum in ethnically diverse, low income women. Women Health. (2002) 36:101–21. doi: 10.1300/J013v36n03_07
53. Birkeland, R, Thompson, JK, and Phares, V. Adolescent motherhood and postpartum depression. J Clin Child Adolesc Psychol. (2005) 34:292–300. doi: 10.1207/s15374424jccp3402_8
54. Haedt, A, and Keel, P. Maternal attachment, depression, and body dissatisfaction in pregnant women. J Reprod Infant Psychol. (2007) 25:285–95. doi: 10.1080/02646830701691327
55. Kamysheva, E, Skouteris, H, Wertheim, EH, Paxton, SJ, and Milgrom, J. Examination of a multi-factorial model of body-related experiences during pregnancy: the relationships among physical symptoms, sleep quality, depression, self-esteem, and negative body attitudes. Body Image. (2008) 5:152–63. doi: 10.1016/j.bodyim.2007.12.005
56. Downs, DS, DiNallo, JM, and Kirner, TL. Determinants of pregnancy and postpartum depression: prospective influences of depressive symptoms, body image satisfaction, and exercise behavior. Ann Behav Med. (2008) 36:54–63. doi: 10.1007/s12160-008-9044-9
57. Clark, A, Skouteris, H, Wertheim, EH, Paxton, SJ, and Milgrom, J. The relationship between depression and body dissatisfaction across pregnancy and the postpartum: a prospective study. J Health Psychol. (2009) 14:27–35. doi: 10.1177/1359105308097940
58. Phillips, J, King, R, and Skouteris, H. The influence of psychological factors on post-partum weight retention at 9 months. Br J Health Psychol. (2013) 19:751–66. doi: 10.1111/bjhp.12074
59. Collings, R, Hill, B, and Skouteris, H. The influence of psychological factors on postpartum weight retention 12 months post-birth. J Reprod Infant Psychol. (2018) 36:177–91. doi: 10.1080/02646838.2018.1424323
60. Rodgers, RF, O'Flynn, JL, Bourdeau, A, and Zimmerman, E. A biopsychosocial model of body image, disordered eating, and breastfeeding among postpartum women. Appetite. (2018) 126:163–8. doi: 10.1016/j.appet.2018.04.007
61. Lee, MF, Williams, SL, and Burke, KJ. Striving for the thin ideal post-pregnancy: a cross-sectional study of intuitive eating in postpartum women. J Reprod Infant Psychol. (2019) 38:127–38. doi: 10.1080/02646838.2019.1607968
62. Przybyła-Basista, H, Kwiecińska, E, and Ilska, M. Body acceptance by pregnant women and their attitudes toward pregnancy and maternity as predictors of prenatal depression. Int J Environ Res Public Health. (2020) 17:9436. doi: 10.3390/ijerph17249436
63. Rallis, S, Skouteris, H, Wertheim, EH, and Paxton, SJ. Predictors of body image during the first year postpartum: a prospective study. Women Health. (2007) 45:87–104. doi: 10.1300/J013v45n01_06
64. Hartley, E, Hill, B, Bailey, C, Fuller-Tyszkiewicz, M, and Skouteris, H. The associations of weight status and body attitudes with depressive and anxiety symptoms across the first year postpartum. Womens Health Issues. (2018) 28:530–8. doi: 10.1016/j.whi.2018.07.002
65. Kadam, KS, Anvekar, AR, and Unnithan, VB. Depression, sleep quality, and body image disturbances among pregnant women in India: a cross-sectional study. J Yeungnam Med Sci. (2023) 40:394–401. doi: 10.12701/jyms.2023.00087
66. Duncombe, D, Wertheim, EH, Skouteris, H, Paxton, SJ, and Kelly, L. How well do women adapt to changes in their body size and shape across the course of pregnancy? J Health Psychol. (2008) 13:503–15. doi: 10.1177/1359105308088521
67. Munns, LB, and Preston, C. The role of bodily experiences during pregnancy on mother and infant outcomes. J Neuropsychol. (2024) 19:131–51. doi: 10.1111/jnp.12370
68. Rauff, EL, and Downs, DS. Mediating effects of body image satisfaction on exercise behavior, depressive symptoms, and gestational weight gain in pregnancy. Ann Behav Med. (2011) 42:381–90. doi: 10.1007/s12160-011-9300-2
69. Skouteris, H, Carr, R, Wertheim, EH, Paxton, SJ, and Duncombe, D. A prospective study of factors that lead to body dissatisfaction during pregnancy. Body Image. (2005) 2:347–61. doi: 10.1016/j.bodyim.2005.09.002
70. Terrone, G, Bianciardi, E, Fontana, A, Pinci, C, Castellani, G, Sferra, I, et al. Psychological characteristics of women with perinatal depression who require psychiatric support during pregnancy or postpartum: a cross-sectional study. Int J Environ Res Public Health. (2023) 20:5508. doi: 10.3390/ijerph20085508
71. Meireles, JFF, Neves, CM, Carvalho, PHB, and Ferreira, MEC. Body image, eating attitudes, depressive symptoms, self-esteem and anxiety in pregnant women of Juiz de fora, Minas Gerais, Brazil. Cienc Saude Coletiva. (2017) 22:437–45. doi: 10.1590/1413-81232017222.23182015
72. Xuan, Z, Wu, L, Han, J, C, Q, Mao, F, W, J, et al. Reliability and validity test of the Chinese body understanding measure for pregnancy scale. J Shandong University (Health Science). (2022) 60:87–91,109.
73. Yang, Y, Zhou, H, Zhu, Z, Pu, C, Wang, Y, Zhang, Y, et al. The mediating effeet of mother-infant attachment on the relationship between maternal body image during pregnancy and postpartum depression. Chin J Pract Nurs. (2024) 40:58–63.
74. Incollingo Rodriguez, AC, Dunkel Schetter, C, Brewis, A, and Tomiyama, AJ. The psychological burden of baby weight: pregnancy, weight stigma, and maternal health. Soc Sci Med. (1982) 2019:112401. doi: 10.1016/j.socscimed.2019.112401
75. Erkaya, R, Karabulutlu, Ö, and Yeşilçiçek Çalik, K. The effect of maternal obesity on self-esteem and body image. Saudi J Biol Sci. (2018) 25:1079–84. doi: 10.1016/j.sjbs.2018.02.003
76. Hartley, E, Fuller-Tyszkiewicz, M, Skouteris, H, and Hill, B. A qualitative insight into the relationship between postpartum depression and body image. J Reprod Infant Psychol. (2021) 39:288–300. doi: 10.1080/02646838.2019.1710119
77. Nagl, M, Jepsen, L, Linde, K, and Kersting, A. Social media use and postpartum body image dissatisfaction: the role of appearance-related social comparisons and thin-ideal internalization. Midwifery. (2021) 100:103038. doi: 10.1016/j.midw.2021.103038
78. Nippert, KE, Tomiyama, AJ, Smieszek, SM, and Incollingo Rodriguez, AC. The media as a source of weight stigma for pregnant and postpartum women. Obesity (Silver Spring, Md). (2021) 29:226–32. doi: 10.1002/oby.23032
79. Becker, E, Rodgers, RF, and Zimmerman, E. #body goals or #Bopo? Exposure to pregnancy and post-partum related social media images: effects on the body image and mood of women in the peri-pregnancy period. Body Image. (2022) 42:1–10. doi: 10.1016/j.bodyim.2022.04.010
80. Watson, B, Broadbent, J, Skouteris, H, and Fuller-Tyszkiewicz, M. A qualitative exploration of body image experiences of women progressing through pregnancy. Women Birth. (2016) 29:72–9. doi: 10.1016/j.wombi.2015.08.007
81. Tavakoli, M, Hasanpoor-Azghady, SB, and Farahani, LA. Predictors of mothers’ postpartum body dissatisfaction based on demographic and fertility factors. BMC Pregnancy Childbirth. (2021) 21:8. doi: 10.1186/s12884-020-03501-x
82. Leddy, MA, Jones, C, Morgan, MA, and Schulkin, J. Eating disorders and obstetric-gynecologic care. J Womens Health. (2009) 18:1395–401. doi: 10.1089/jwh.2008.1183
83. Yager, Z, Calleja-Agius, J, Jagomagi, T, Khalaf, A, Sjöbeck, J, Karamouzi, P, et al. European health professionals’ knowledge, attitudes and beliefs about perinatal depression and body image concerns. Adv Ment Health. (2023) 21:247–60. doi: 10.1080/18387357.2023.2210703
84. Incollingo Rodriguez, AC, Smieszek, SM, Nippert, KE, and Tomiyama, AJ. Pregnant and postpartum women’s experiences of weight stigma in healthcare. BMC Pregnancy Childbirth. (2020) 20:499. doi: 10.1186/s12884-020-03202-5
85. Incollingo Rodriguez, AC, and Nagpal, TS. The WOMBS framework: a review and new theoretical model for investigating pregnancy-related weight stigma and its intergenerational implications. Obes Rev. (2021) 22:e13322. doi: 10.1111/obr.13322
86. Olander, EK, Hill, B, and Skouteris, H. Healthcare professional training regarding gestational weight gain: recommendations and future directions. Curr Obes Rep. (2021) 10:116–24. doi: 10.1007/s13679-021-00429-x
Keywords: body image, depression, pregnancy, postpartum period, body dissatisfaction
Citation: He J, Chen X and Luo B (2025) The association between body image and depressive symptoms in pregnant and postpartum women: a meta-analysis. Front. Public Health. 13:1655639. doi: 10.3389/fpubh.2025.1655639
Edited by:
Virtudes Pérez-Jover, Miguel Hernández University, SpainReviewed by:
Zali Yager, Victoria University, AustraliaChonnakarn Jatchavala, Prince of Songkla University, Thailand
Copyright © 2025 He, Chen and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Biru Luo, bHVvbXJAc2N1LmVkdS5jbg==
 Jingbo He
Jingbo He Xin Chen2,3
Xin Chen2,3