- 1Department of Obstetric and Gynaecological Nursing, Institute of Nursing and Midwifery, Faculty of Health Sciences with the Institute of Maritime and Tropical Medicine, Medical University of Gdańsk, Gdańsk, Poland
- 2Laboratory of Functional Diagnostics, Central Scientific and Research Laboratory, University of Physical Culture in Krakow, Kraków, Poland
- 3Department of Physical Activity and Health, Sport Sciences School of Rio Maior (ESDRM), Polytechnic University of Santarém, Rio Maior, Portugal
- 4Sport Physical Activity and Health Research & Innovation Centre (SPRINT), Rio Maior, Portugal
Background: Cesarean section (CS) is a common surgical procedure in obstetrics, and its prevalence has been increasing globally. While the immediate outcomes of CS are well-documented, its long-term effects, particularly on maternal health, remain an area of active research. One of the critical concerns is the impact of a previous CS on gestational body mass gain (GBMG), physical activity (PA) and the likelihood of undergoing another CS in subsequent pregnancies.
Objective: The aim of this study is to evaluate the potential association of a previous CS on GBMG, PA levels and the likelihood of repeat cesarean delivery in a cohort of multiparous women.
Methods: This prospective cohort study, enrolling 109 Caucasian women, was conducted at a tertiary care hospital in northern Poland. Participants were recruited from antenatal outpatient clinics. The participants were divided into two groups: those who underwent previous CS and those who had vaginal delivery. Data collection was conducted in two phases. In the first phase, socio-demographic information was gathered, and participants were asked to complete the Polish version of the Get Active Questionnaire for Pregnancy. In the second phase, biomedical data routinely collected during childbirth were obtained.
Results: Women with a history of CS were found to have a significantly higher likelihood of excessive gestational GBMG and were more likely to undergo another cesarean delivery in subsequent pregnancies. However, no significant differences were observed between groups in terms of insufficient GBMG or PA levels before and during pregnancy.
Conclusions: The results allow to suggest that previous CS is associated with an increased risk of excessive GBMG and repeat cesarean delivery. However, it does not appear to have direct impact on PA levels during pregnancy. These findings emphasize the importance of monitoring GBMG and promoting healthy lifestyle behaviors to improve maternal and outcomes, particularly in women with a history of CS. Future research is needed to explore the long-term effects of CS on maternal health and its influence on subsequent pregnancies.
1 Introduction
Cesarean section (CS) is a surgical procedure involving incisions through the abdominal wall and uterus to deliver a baby (1). Historically, it was performed only in life-threatening situations; however, advancements in surgical techniques and anesthesia have made it a common obstetric practice (2–4). According to the guidelines of the Polish Society of Gynecologists and Obstetricians (5) and the American College of Obstetricians and Gynecologists (3), the main indications for CS include: obstructed labor, abnormal fetal presentation, multiple pregnancy (especially when the first fetus is not in cephalic presentation), placenta previa, placental abruption, a history of uterine surgery (e.g., previous CS or myomectomy), abnormal fetal heart rate patterns (suggesting fetal distress), maternal infections such as active genital herpes and serious maternal medical conditions, i.e., severe preeclampsia or eclampsia. An analysis of data from over nine million births across 28 European countries confirms that CS is a widely used method of childbirth. In 2015, national CS rates ranged from 16.0% to 55.9% and from 16.0% to 52.2% and in 2019 (6).
The indications for performing CS are evolving and now, in many countries, they also include psychosocial factors such as fear of childbirth or even CS on maternal request, but only in the absence of medical indications. Data on the prevalence of CS upon maternal request in developed countries are limited, as many healthcare systems do not record these cases separately (7). Nevertheless, the reasons behind increasingly liberal attitudes toward CS are complex and not always simple to define. The rising number of such procedures is mainly attributed to sociocultural and economic factors as well as the widespread belief that CS is a safe and convenient alternative to vaginal birth. Advances in surgical care have further reinforced this perception, despite the fact that operative delivery still carries significant risks for both mother and child. The growing demand for CS without medical indications continues to generate controversy among clinicians and researchers due to well-documented negative health consequences in both the short- and long-term (8). The main short-term maternal complications include, among others, excessive bleeding, injury to adjacent organs (such as the bladder, intestines or ureters), uterine scar dehiscence and longer postpartum recovery (9). Long-term complications may involve bowel obstruction (ileus), abdominal wall disorders and an increased risk of complications in subsequent pregnancies, such as uterine rupture, placenta accreta spectrum disorders, ectopic pregnancy, intrauterine fetal demise and pre-term birth. In the most severe cases, additional surgical interventions may be required, for instance hysterectomy or revision of the surgical wound (10). In conclusion, although CS remains an essential tool in modern obstetrics, alike any other medical intervention, it should be used only when medically justified.
Previous research on CS has been primarily focused on short-term clinical outcomes, such as perioperative complications, neonatal condition and postpartum recovery. Significantly less attention has been given to the potential long-term impact of CS on women's health behaviors, including PA levels and body mass management—factors that are essential determinants of maternal health. It was hypothesized that women with a history of CS are more likely to undergo repeat cesarean deliveries, have lower levels of PA and are at greater risk of excessive gestational body mass gain (GMBG) or postpartum body mass retention compared to women with a history of vaginal birth. We also assumed that the decline in PA following CS is not merely a temporary phenomenon, but may persist over time and negatively affect maternal health as well as the course of future pregnancies.
2 Material and methods
2.1. Study design
The prospective cohort study was conducted at a tertiary care hospital in northern Poland, with participants recruited from patients attending the antenatal outpatient clinic. Data collection was carried out in two stages. In the first stage, women who met the inclusion criteria were invited to complete a questionnaire consisting of self-reported items presented in the form of a medical interview. Based on the information obtained during the interview, participants were categorized into two groups: those who gave birth via CS and those who had a vaginal delivery. During the second stage, access was obtained to standard biomedical data routinely collected during childbirth. All procedures adhered to the principles of the Declaration of Helsinki (1964) and its subsequent amendments. Ethical approval for the study was granted by the Bioethics Committee of the Medical University of Gdansk (Approval No. NKBBN/406-1/2024).
2.2. Participants
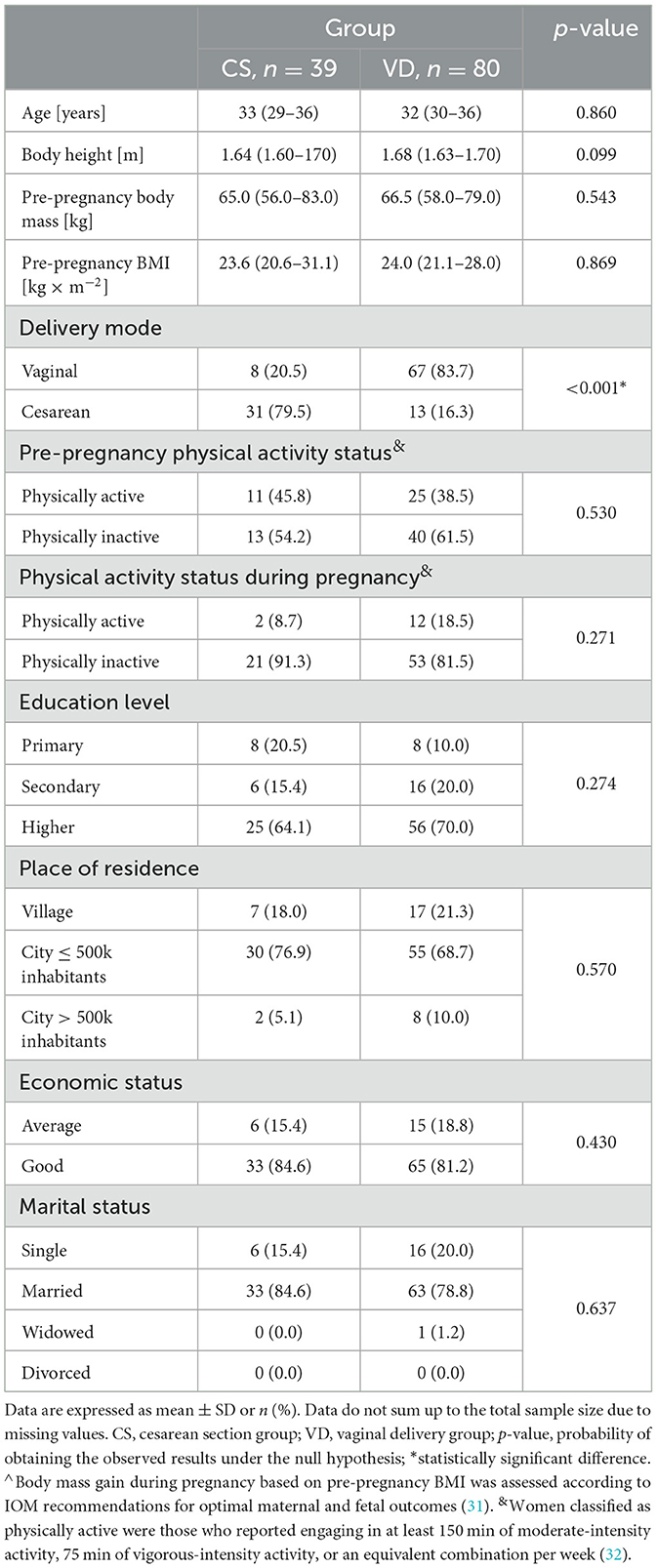
The study comprised 109 Caucasian women who met the following eligibility criteria: entry into the third trimester (after the 28th week of gestation), age of 18 years or older, fluency in Polish, absence of medical contraindications to PA, a history of at least one previous pregnancy (multiparous), no diagnosis of placenta previa and a planned delivery at a hospital associated with the outpatient clinic where recruitment took place. Participants were thoroughly informed about the purpose and protocol of the study, as well as their right to withdraw from the study at any time. The participants provided written informed consent to participate in the research. The women gave their consent not only to take part in the study but also to allow access to anonymized medical data concerning themselves. The basic characteristics of study participants are presented in Table 1.
2.3. Outcomes
Socio-demographic data were obtained during the medical interview. Information on PA levels was collected using the Polish version of the Get Active Questionnaire for Pregnancy (11). The Get Active Questionnaire for Pregnancy (GAQ-P) allows assessment of potential contraindications to physical activity as well as evaluation of the frequency, intensity, duration and type of physical activity undertaken before and during pregnancy, as well as the activity planned until the end of pregnancy. Data regarding GBMG and mode of delivery were extracted from standard medical records routinely collected during childbirth.
2.4. Statistical analysis
All statistical analyses were carried out in Python 3.13.1 using the pandas, NumPy and statsmodels.formula.api libraries. To assess the effect of delivery mode on dependent variables, logistic regression analysis was applied. For ratio-scale variables, group differences were examined using the Student's t-test, Welch's t-test or the Mann–Whitney U test, depending on whether the assumptions of normality (verified via the Shapiro–Wilk test) and homogeneity of variances (assessed using Levene's test) were met. For nominal variables, comparisons between groups were performed using the χ2 test. A p-value below 0.05 was considered statistically significant.
3 Results
3.1. Basic characteristics of participants
The data presented in Table 1 show that women with a history of cesarean section (CS group) and those with a previous vaginal delivery (VD group) did not differ significantly in terms of age, height, pre-pregnancy body mass or body mass index. No statistically significant differences were observed between the groups in terms of physical activity levels (before or during pregnancy), education, place of residence, and economic or marital status. The only variable for which a statistically significant difference was demonstrated regarded the mode of delivery in the current pregnancy—women in the CS group were significantly more likely to deliver via cesarean section again.
3.2. Outcomes
According to the data presented in Table 2, women in the CS group had a statistically significant more than two-fold increased risk of excessive gestational body mass gain compared to those in the VD group. Additionally, the likelihood of undergoing a repeat cesarean delivery was nearly 20 times higher in the CS group, and this association was also statistically significant. In contrast, a history of CS was not significantly associated with an increased risk of insufficient gestational weight gain, nor with engagement in physical activity prior to or during pregnancy.
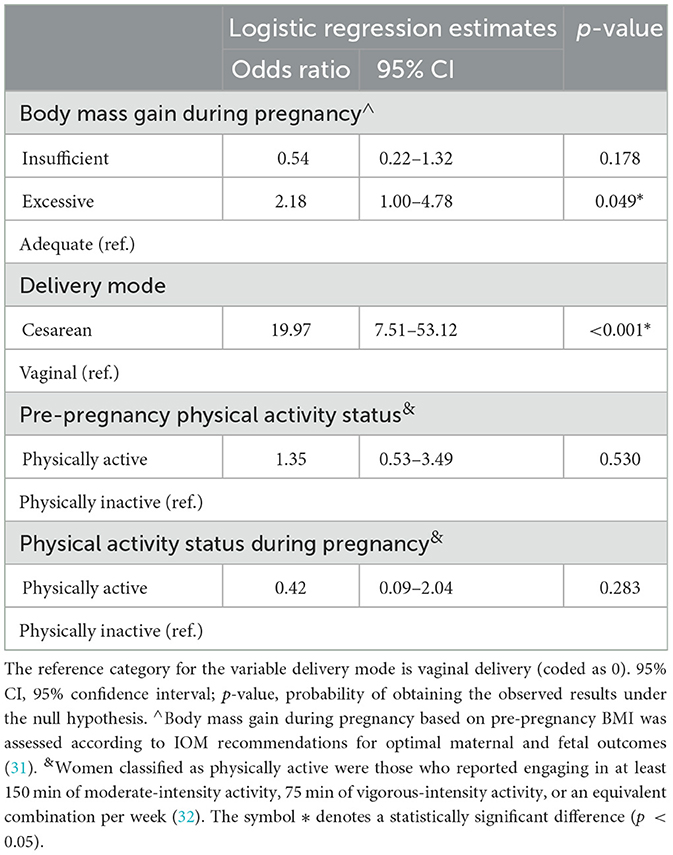
Table 2. Analysis of associations between cesarean section and maternal outcomes in subsequent pregnancy.
4 Discussion
The aim of this study was to evaluate the long-term consequences of a previous CS on the course of subsequent pregnancies and selected lifestyle-related factors, particularly PA and GBMG. To the best of the authors' knowledge, this is one of the first studies focused on the long-term behavioral and health-related consequences of a primary cesarean delivery, going beyond the commonly studied short-term postpartum outcomes. The findings indicate that a prior CS is associated with an increased risk of excessive GBMG and a higher likelihood of undergoing a repeat cesarean delivery. However, no significant associations were found between previous cesarean section and insufficient gestational body mass gain (GBMG) or lower levels of physical activity before or during pregnancy, which is consistent with the findings of other studies in this area (12).
One possible explanation for the observed association between a history of CS and excessive GBMG in subsequent pregnancies is the potential long-term impact of surgical delivery on maternal health behaviors and metabolic adaptation. Cesarean delivery may contribute to more prolonged postpartum recovery, reduced physical functioning as well as persistent changes in abdominal and pelvic musculature which, in turn, could limit the return to regular PA and predispose to gradual body mass retention between pregnancies. The retained postpartum body mass may create a baseline for excessive body mass gain during subsequent pregnancies, especially if combined with common lifestyle factors such as reduced PA or inadequate dietary habits.
Furthermore, CS is often medically linked with maternal conditions such as obesity, gestational diabetes and hypertensive disorders, which are themselves associated with altered metabolic regulation and a higher risk of excessive GBMG (13–15). Thus, the pathway may be partly biological and partially behavioral, involving both the physical limitations resulting from a prior surgical delivery and the broader context of maternal health status. Excessive GBMG carries significant health implications for both the mother and the offspring, including an increased risk of hypertensive disorders, gestational diabetes, macrosomia, postpartum body mass retention and long-term obesity, all of which may further increase the likelihood of surgical delivery in future pregnancies (13, 16). This allows to underline the significance of preconception counseling and body mass management among women with a history of cesarean section in order to minimize the cycle of repeat surgical deliveries and metabolic complications.
Excessive GBMG following a previous CS can have substantial health consequences for the mother, both in the short- and long-term. From an obstetric perspective, excessive body mass gain is associated with an increased risk of pregnancy complications such as gestational diabetes, hypertensive disorders and labor dystocia—all of which are known to elevate the likelihood of another cesarean delivery (13, 17, 18). Moreover, higher GBMG may lead to excessive fetal growth (macrosomia), which not only complicates vaginal delivery but also increases the risk of birth injuries and necessitates operative delivery (9, 19).
Beyond delivery, excessive body mass gain during pregnancy is a strong predictor of postpartum body mass retention, which contributes to long-term maternal overweightness and obesity (20–23). This, in turn, escalates the risk of developing chronic conditions such as type 2 diabetes, cardiovascular disease and metabolic syndrome (13, 20, 21). Additionally, maternal obesity negatively influences fertility and increases the risk of complications in future pregnancies, thus, creating a self-perpetuating cycle of adverse health outcomes (15). These findings allow to highlight the importance of body mass monitoring and individualized nutritional counseling during pregnancy, particularly in women with a history of cesarean section, to reduce the likelihood of excessive body mass gain and its subsequent health burdens.
A prior CS is a well-established risk factor for repeat cesarean delivery in subsequent pregnancies, and this association is both clinical and structural. Current obstetric guidelines acknowledge that previous cesarean delivery is often a direct indication for planned repeat cesarean section, especially in the absence of conditions favorable for a trial of labor after cesarean (TOLAC) (24, 25). Although TOLAC is considered a safe and recommended option in specific circumstances, including a low-transverse uterine scar and no contraindicating obstetric factors, many women do not meet these criteria or are advised against TOLAC due to individual risk profiles.
The decision to perform a repeat cesarean is often influenced by concerns related to uterine rupture, which, while relatively rare, is associated with severe maternal and neonatal morbidity as well as mortality (26, 27). Beyond the delivery itself, undergoing multiple cesarean sections substantially increases the risk of significant complications, including excessive intraoperative bleeding, placenta previa, placenta accreta spectrum disorders and surgical injuries to the bladder or bowel. Moreover, repeated cesarean deliveries are associated with a higher likelihood of postoperative infections, thromboembolic events, longer hospitalization and chronic pelvic pain (16, 27, 28).
In the current study, a significant association was not demonstrated between a history of CS and reduced PA levels before or during a subsequent pregnancy. This finding may suggest that cesarean delivery itself does not substantially influence long-term behavioral patterns related to PA. However, it remains an open question as to what the baseline PA levels were before the previous pregnancy, as it is possible that these were already insufficient. In the present research, this aspect was not assessed and the behavioral dimension of PA was the sole focus in the context of subsequent pregnancies. Moreover, to date, the available literature primarily offers guidelines and expert recommendations on the timing, safety and benefits of returning to PA after CS, as well as suggested types of exercises (29, 30), rather than objective data on the actual activity levels in this population. This gap highlights the novelty of the trial, as there is still a lack of empirical studies in which authors would directly address the PA patterns of women following cesarean delivery.
The findings of this study have significant practical implications, particularly in the context of healthcare management for women who have undergone CS. The results suggest that a history of cesarean delivery is associated with an increased risk of excessive GBMG and a higher likelihood of repeat CS delivery in subsequent pregnancies. Therefore, it is crucial to systematically monitor the metabolic health of women post-cesarean, offering appropriate preventive strategies aimed at controlling body mass gain during pregnancy and promoting PA, which could potentially reduce these adverse outcomes. In terms of decision-making regarding the mode of delivery, the need for a more individualized approach to women who have previously undergone a CS is highlighted in this study, ensuring that each case is evaluated based on the specific risks and benefits for both the mother and child.
4.1 Study limitations and strengths
Despite the valuable insights provided in the current study, several limitations should be acknowledged. Firstly, the observational nature of the research limits the ability to infer causal relationships between previous CS and outcomes such as excessive GBMG or repeat cesarean delivery. Additionally, the study relied on self-reported data for PA, which may introduce recall bias and affect the accuracy of the results. Another limitation is the lack of data on participants' pre-pregnancy activity levels, which could provide a more comprehensive understanding of the factors influencing postpartum PA and future pregnancy outcomes. Furthermore, the sample was limited to a specific geographic area, which may have affected the generalizability of the findings to other populations. Lastly, in the study, the long-term impact was not assessed of cesarean delivery on maternal health beyond the immediate pregnancy period, leaving room for future research to explore the enduring effects on physical well-being and overall quality of life.
The main strength of the study is that it lies in shifting the focus from immediate medical consequences to long-term behavioral outcomes, with particular emphasis on subsequent pregnancies and overall maternal well-being. Accordingly, the aim of this study was to assess the relationship between the history of cesarean section (CS) and subsequent obstetric outcomes, physical activity (PA) patterns and maternal body mass regulation. This comprehensive approach allowed for multidimensional evaluation of the interplay between prior delivery mode, lifestyle factors and health outcomes, offering valuable insights into the long-term consequences of CS on women's health. The study's strength regards its focus on real-world data collected from a well-defined population, the use of standardized measurement tools and consideration of both medical as well as behavioral determinants, which together provide a robust basis for evidence-based recommendations in postnatal care and physical activity counseling.
5 Conclusion
In the present study, it is highlighted that women who have had a CS in a previous pregnancy are at a higher risk of excessive GBMS and may be more likely to have another cesarean in subsequent pregnancies. The importance of carefully considering cesarean delivery due to its potential long-term impact on maternal health is also emphasized. Future studies should be focused on understanding how pre-pregnancy PA levels influence outcomes after cesarean delivery and explore the long-term effects of cesarean births on maternal health. Additionally, further research is needed to develop targeted interventions to promote safe PA and body mass management after CS, improving overall maternal well-being in subsequent pregnancies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Bioethics Committee of the Medical University of Gdansk. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
AS: Investigation, Conceptualization, Validation, Funding acquisition, Data curation, Software, Resources, Writing – review & editing, Project administration, Formal analysis, Supervision, Writing – original draft, Methodology. BZ: Visualization, Formal analysis, Writing – review & editing, Writing – original draft, Supervision. RS-R: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The publication fee were financed under the program Initiative of Excellence -Research University (IDUB) of the Medical University of Gdańsk (MUG).
Rita Santos-Rocha is supported by Polytechnic University of Santarém & SPRINT – Sport Physical Activity and Health Research & Innovation Center [UID/06185/2023], by national funds through FCT – Fundação para a Ciência e Tecnologia – Portuguese Foundation for Science and Technology, within the scope of the project Active Pregnancy [2023.14896.PEX]. PI: Rita Santos-Rocha. doi: 10.54499/2023.14896.PEX. Website: https://sprint-sci.com/en/research-innovation/research-projects-external/active-pregnancy-202314896pex. YouTube Channel: @GravidezAtiva-ActivePregnancy.
This work is an output framed within the scope of the European Universities Alliance ACE2 - Applied Connected Entrepreneurial Engaged European University: https://www.ace2eu.eu/.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung S, Mikes BA, Martingano DJ, Mahdy H. Cesarean Delivery - StatPearls. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK546707/ (Accessed April 14, 2025).
2. Nunes I, Nicholson W, Theron G. FIGO good practice recommendations on surgical techniques to improve safety and reduce complications during cesarean delivery. Int J Gynecol Obstet. (2023) 163:21–33. doi: 10.1002/ijgo.15117
3. Committee ACOG. Cesarean Birth. Available online at: https://www.acog.org/womens-health/faqs/cesarean-b (Accessed April 11, 2025).
4. Visser GHA, Ubom AE, Neji K, Nassar A, Jacobsson B, Nicholson W, et al. Opinion paper: drivers and solutions to the cesarean delivery epidemic with emphasis on the increasing rates in Africa and Southeastern Europe. Int J Gynaecol Obstet Off organ Int Fed Gynaecol Obstet. (2023) 163:5–9. doi: 10.1002/ijgo.15111
5. Wielgos M, Bomba-Opon D, Breborowicz GH, Czajkowski K, Debski R, Leszczynska-Gorzelak B, et al. Recommendations of the Polish Society of gynecologists and obstetricians regarding caesarean sections. Ginekol Pol. (2018) 89:644–57. doi: 10.5603/GP.a2018.0110
6. Amyx M, Philibert M, Farr A, Donati S, Smárason AK, Tica V, et al. Trends in caesarean section rates in Europe from 2015 to 2019 using Robson's ten group classification system: a Euro-Peristat study. BJOG. (2024) 131:444–54. doi: 10.1111/1471-0528.17670
7. Masciullo L, Petruzziello L, Perrone G, Pecorini F, Remiddi C, Galoppi P, et al. Caesarean section on maternal request: an Italian comparative study on patients' characteristics, pregnancy outcomes and guidelines overview. Int J Environ Res Public Health. (2020) 17:4665. doi: 10.3390/ijerph17134665
8. Ayres-de-Campos D, Simon A, Modi N, Tudose M, Saliba E, Wielgos M, et al. European Association of perinatal medicine (EAPM) European Midwives Association (EMA): joint position statement: caesarean delivery rates at a country level should be in the 15–20% range. Eur J Obstet Gynecol Reprod Biol. (2024) 294:76–8. doi: 10.1016/j.ejogrb.2024.01.005
9. Sandall J, Tribe RM, Avery L, Mola G, Visser GHA, Homer CSE, et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. (2018) 392:1349–57. doi: 10.1016/S0140-6736(18)31930-5
10. Rahman M, Khan N, Rahman A, Alam M, Khan A. Long-term effects of caesarean delivery on health and behavioural outcomes of the mother and child in Bangladesh. J Heal Popul Nutr. (2022) 41:45. doi: 10.1186/s41043-022-00326-6
11. Szumilewicz A, Davenport MH, Scholz A, Sikora-Szubert A, Santos-Rocha R, Karowicz-Bilinska A, et al. Translation and cross-cultural adaptation of the get active questionnaire for pregnancy (kwestionariusz “Badz Aktywna w Ciaży”) to support physical activity among pregnant women in Poland. Ginekol Pol. (2024) 95:483–501. doi: 10.5603/gpl.97888
12. Davenport MH, Ruchat S-M, Sobierajski F, Poitras VJ, Gray CE, Yoo C, et al. Impact of prenatal exercise on maternal harms, labour and delivery outcomes: a systematic review and meta-analysis. Br J Sports Med. (2019) 53:99–107. doi: 10.1136/bjsports-2018-099821
13. Grieger JA, Hutchesson MJ, Cooray SD, Bahri KM, Zaman S, Segan L, et al. A review of maternal overweight and obesity and its impact on cardiometabolic outcomes during pregnancy and postpartum. Ther Adv Reprod Heal. (2021) 15:2633494120986544. doi: 10.1177/2633494120986544
14. Huang L, Zhang J, Sun H, Dong H, Li R, Cai C, et al. Association of gestational weight gain with cesarean section: a prospective birth cohort study in Southwest China. BMC Pregnancy Childbirth. (2021) 21:57. doi: 10.1186/s12884-020-03527-1
15. Riemma G, De Franciscis P, Torella M, Narciso G, La Verde M, Morlando M, et al. Reproductive and pregnancy outcomes following embryo transfer in women with previous cesarean section: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. (2021) 100:1949–60. doi: 10.1111/aogs.14239
16. Miseljic N, Ibrahimovic S. Health implications of increased cesarean section rates. Mater Sociomed. (2020) 32:123–6. doi: 10.5455/msm.2020.32.123–6
17. Todd IMF, Magnus MC, Pedersen LH, Burgner D, Miller JE. Caesarean section and risk of infection in offspring: systematic review and meta-analysis of observational studies. BMJ Med. (2024) 3:e000995. doi: 10.1136/bmjmed-2024-000995
18. Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. (2018) 15:1–22. doi: 10.1371/journal.pmed.1002494
19. Słabuszewska-Józwiak A, Szymański JK, Ciebiera M, Sarecka-Hujar B, Jakiel G. Pediatrics consequences of caesarean section—a systematic review and meta-analysis. Int J Environ Res Public Health. (2020) 17:8.31. doi: 10.3390/ijerph17218031
20. Acosta-Manzano P, Acosta FM, Coll-Risco I, Romero-Gallardo L, Flor-Alemany M, Martínez-González LJ, et al. The influence of exercise, lifestyle behavior components, and physical fitness on maternal weight gain, postpartum weight retention, and excessive gestational weight gain. Int J Sport Nutr Exerc Metab. (2022) 32:425–38. doi: 10.1123/ijsnem.2021-0201
21. Kramer CK, Ye C, Hanley AJ, Connelly PW, Sermer M, Zinman B, et al. Postpartum weight retention and the early evolution of cardiovascular risk over the first 5 years after pregnancy. Cardiovasc Diabetol. (2024) 23:101. doi: 10.1186/s12933-024-02184-4
22. Carvalho B, Ferreira LB, Santos TN, Souza RCV, Santos LC. Weight retention 12 months postpartum: association with sociodemographic, gestational and puerperal factors. Rev Bras Saúde Matern Infant. (2023) 23:e20220392. doi: 10.1590/1806-9304202300000392-en
23. Makama M, Skouteris H, Moran LJ, Lim S. Reducing postpartum weight retention: a review of the implementation challenges of postpartum lifestyle interventions. J Clin Med. (2021) 10:1891. doi: 10.3390/jcm10091891
24. Royal College of Obstetricians and Gynaecologists. Birth after Previous Caesarean Birth (Green-top Guideline No. 45) (2015). Available online at: https://www.rcog.org.uk/guidance/browse-all-guidance/green-top-guidelines/birth-after-previous-caesarean-birth-green-top-guideline-no-45/ (Accessed April 12, 2025).
25. Metz TD, Berghella V, Barss V. Choosing the Route of Delivery After Cesarean Birth. Alphen aan den Rijn: UptoDate, Wolters Kluwer (2019)
26. Dabian B, Elmahdy S, Elmazny A, Mohammed B, Elzyat A. Effect of maternal obesity on operative and post-operative complications of elective cesarean section: an observational cross-sectional study. Egypt J Hosp Med. (2024) 96:2385–93. doi: 10.21608/ejhm.2024.363732
27. Berghella V. Cesarean Birth: Postoperative Care, Complications, and Long-Term Sequelae. Alphen aan den Rijn: UptoDate, Wolters Kluwer (2023)
28. Chen H, Tan D. Cesarean section or natural childbirth? Cesarean birth may damage your health. Front Psychol. (2019) 10:1–7. doi: 10.3389/fpsyg.2019.00351
29. Macones GA, Caughey AB, Wood SL, Wrench IJ, Huang J, Norman M, et al. Guidelines for postoperative care in cesarean delivery: enhanced recovery after surgery (ERAS) society recommendations (part 3). Am J Obstet Gynecol. (2019) 221:247–e1. doi: 10.1016/j.ajog.2019.04.012
30. Ahamnonu U, Nixon C, Ramseth E. Supporting the Mother's Recovery After Cesarean Section: A Narrative Literature Review. Seinäjoki: SeAMK (2022).
31. Rasmussen KM Yaktine AL Institute Institute of Medicine (US) National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, DC: National Academies Press (2015). 1–250 p.
Keywords: cesarean section, physical activity, pregnancy, gestational weight gain, women's health
Citation: Szablewska AW, Zając B and Santos-Rocha R (2025) From one birth to the next: how cesarean section affects maternal physical activity and health in later pregnancy—A prospective cohort study. Front. Public Health 13:1657089. doi: 10.3389/fpubh.2025.1657089
Received: 30 June 2025; Accepted: 24 July 2025;
Published: 13 August 2025.
Edited by:
Jian Sun, Guangzhou Sport University, ChinaReviewed by:
Kadeeja Murrell, Arizona State University, United StatesDr. Alka Pawalia, Guru Jambheshwar University of Science and Technology, India
Copyright © 2025 Szablewska, Zając and Santos-Rocha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Weronika Szablewska, YW5uYS5zemFibGV3c2thQGd1bWVkLmVkdS5wbA==
 Anna Weronika Szablewska
Anna Weronika Szablewska Bartosz Zając
Bartosz Zając Rita Santos-Rocha
Rita Santos-Rocha