- 1School of Medicine, Akita University, Akita, Japan
- 2Department of Environmental Health Science and Public Health, Akita University Graduate School of Medicine, Akita, Japan
- 3Department of Nursing, Akita University Graduate School of Health Sciences, Akita, Japan
- 4Faculty of Nursing and Midwifery, Royal College of Surgeons in Ireland, University of Medicine, and Health Sciences, Dublin, Ireland
- 5Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne, United Kingdom
- 6Health Professions Education Centre, Royal College of Surgeons in Ireland, RCSI University of Medicine and Health Sciences, Dublin, Ireland
Introduction: Social prescribing (SP) has not yet been officially introduced in Japan. This qualitative case study aimed to identify the challenges and facilitating factors in the implementation of SP among the socially isolated older population in Akita Prefecture, Japan, based on the perspectives of general practitioners (GP), link workers (LW), and patients.
Method: We conducted a qualitative case study using semi-structured interviews and Braun & Clarke-informed thematic analysis in seven medical districts in Akita, Japan, with GP (n = 7), LW (n = 10), and older patients (n = 4).
Results: Participants (GP and LW) emphasized that SP needed to be tailored to individual needs and that LW played a vital role as social resources in sparsely populated rural communities. The project was publicly funded; participants emphasized that, in the absence of financial support, intrinsic motivation would be important to sustaining implementation. Both groups raised concerns about ensuring LW’s competencies, the accessibility and cost of community resources, and the limited availability of such resources in rural areas. Patients highlighted that the effectiveness of SP varied by personal characteristics, and that transport barriers significantly restricted participation, highlighting the need for local support to mitigate this challenge. Establishing patients’ trust in LW and GP, along with effective communication, was viewed as essential for identifying and addressing patient-level barriers.
Conclusion: In rural, resource-constrained settings such as Akita, successful SP depends on tailoring to individual needs, ensuring LW competence, and addressing transport barriers. These findings suggest that future policies should focus on sustainable funding for LW, integration with existing health and welfare systems, and mobility solutions.
1 Introduction
Social Prescribing (SP) is defined by the World Health Organization as a means of connecting patients to nonclinical community services to improve health and well-being (1). Loneliness and social isolation negatively affect well-being, subjective health, cognitive function, depression, and all-cause mortality, and are increasingly recognized as global public health issues requiring preventive approaches (2–7). SP has therefore gained particular attention in Western countries as a strategy to address these challenges, alongside other social determinants of health (SDH) (8–11).
Japan faces an unprecedented demographic challenge, with 29% of the population aged ≥65 years, projected to reach 38.4% by 2065 (12). In 2021, the Japanese government’s Basic Policies for Economic and Fiscal Management and Reform first identified SP as a preventive measure against isolation and loneliness (13). Between 2021 and 2023, pilot projects were launched in several prefectures, including Akita Prefecture, which has Japan’s highest proportion of older adults and severe winter isolation, as one of the pilot sites.
Despite growing interest, Japan lacks a formal infrastructure or public funding framework for SP, and little is known about how it can be implemented in resource-limited rural prefectures. Therefore, this study examined the perspectives of general practitioners (GP), link workers (LW), and socially isolated older adults in Akita Prefecture to identify key challenges and facilitating factors for implementing SP.
2 Methods
2.1 Study design
This study employed a qualitative case study design, with the case defined as a taskforce-led SP pilot across seven medical districts in Akita Prefecture. While this approach has inherent limitations in that its findings are difficult to directly generalize and may be subject to researcher bias (14), it was chosen for its ability to explore in-depth complex, context-dependent phenomena (14–16). This enabled a comprehensive understanding of the underlying processes and mechanisms that quantitative methods cannot sufficiently capture.
In 2021, a taskforce was formed in Akita Prefecture to conduct a pilot project on SP. The taskforce included the Akita Prefecture Government, the Akita Medical Association, the Department of Environmental Health Science and Public Health at Akita University, the Akita Health Insurance Council, and other relevant organizations. The taskforce first included five GP; after 2022, three additional GP were added to the task force to test its effectiveness in a larger number of subjects. The taskforce members, including GP, recruited 18 LW through their own social networks, including their clinical and relevant workplaces. GP referred LW to patients, and the LW visited patients’ homes and identified patients’ conditions using an assessment sheet.
The assessment sheet (Supplementary material 1) used in this study was newly created by referring to existing scales (Hasegawa Dementia Scale (17), UCLA Loneliness Scale (18)), questions from publicly available websites (19), and original questions developed specifically for the purpose of this study. To ensure its validity and relevance, the sheet was iteratively revised over the three-year project based on feedback from experts, including a professor from the Department of Public Health, GP and LW involved in the study. The assessment sheet developed for the present study included questions about living alone (20), medical or nursing care requirements (21), shut-in (socially isolated) (18, 22), economic hardship (23–25), mental health status (21, 26), environmental hygiene (known as a trigger for dementia) (27–29), someone asking for help (30), and dementia (a reason for social isolation) (17, 31, 32). Based on the assessment sheet, LW referred patients to local social resources.
From 2021 to 2023, GP selected 47 patients. Among the 47 patients, only 22 had access to social resources. The social resources defined in this study include exercise groups, tea parties, knitting groups, volunteer groups, public assistance, and nursing care insurance. Figure 1 shows the social resources in Akita Prefecture, available in 2021, and represented by dots. This map was created within the taskforce, using ArcGIS Pro (Esri, United States) and only publicly available social resource information. The map shows that social resources in Akita Prefecture are concentrated in large cities and are sparse in other areas.
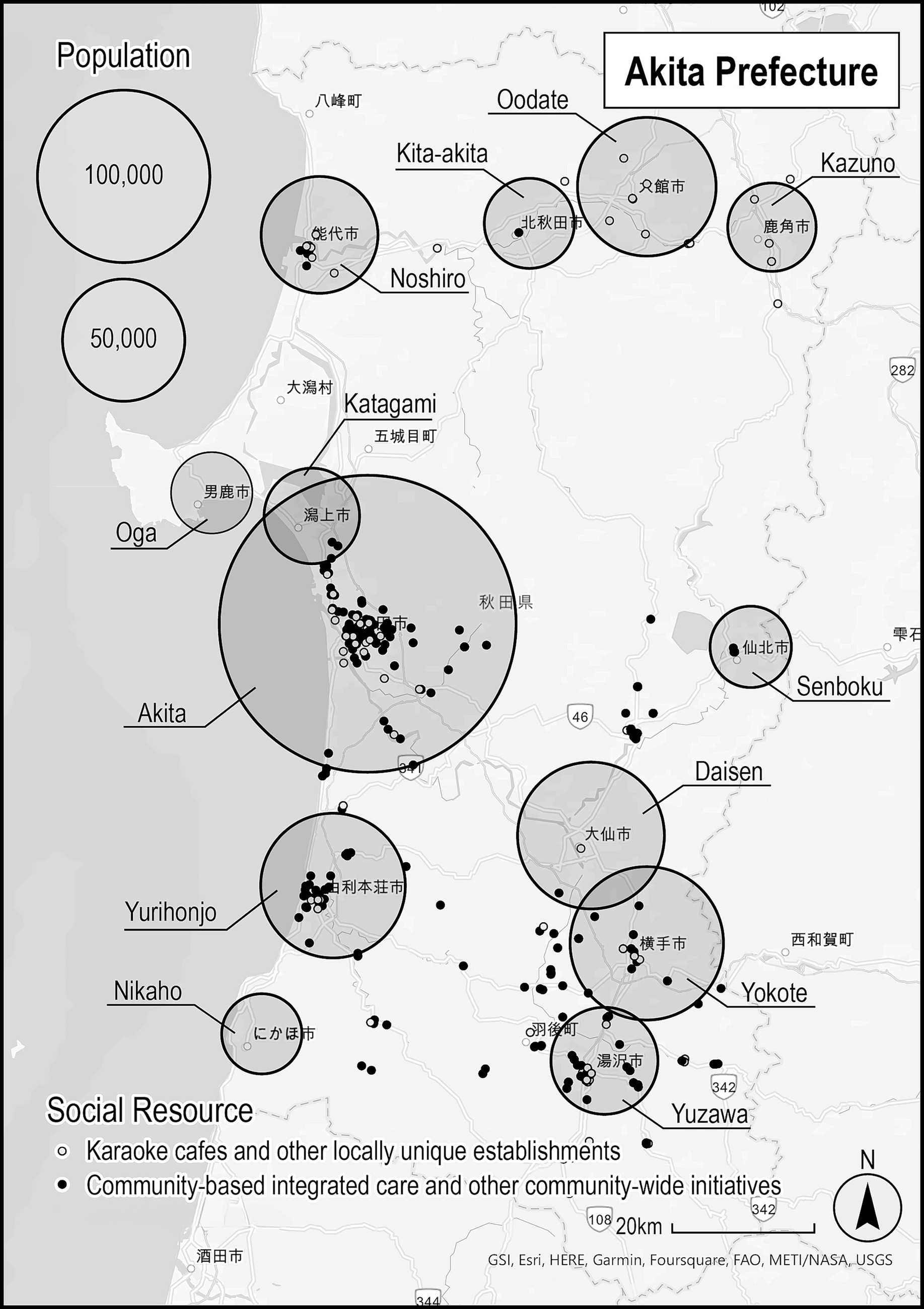
Figure 1. Distribution of social resources and population in Akita. Data sources: Map—ArcGIS Pro (Esri, United States); Social resources map created by the Akita Social Prescribing Taskforce in 2021; Population—Akita Prefecture, Mino Kuni Akita Net (https://www.pref.akita.lg.jp/pages/archive/2078), 2021 data. White dots, Karaoke cafes and other locally unique establishments. Black dots, Community-based integrated care and other community-wide initiatives.
2.2 Study participants and study framework
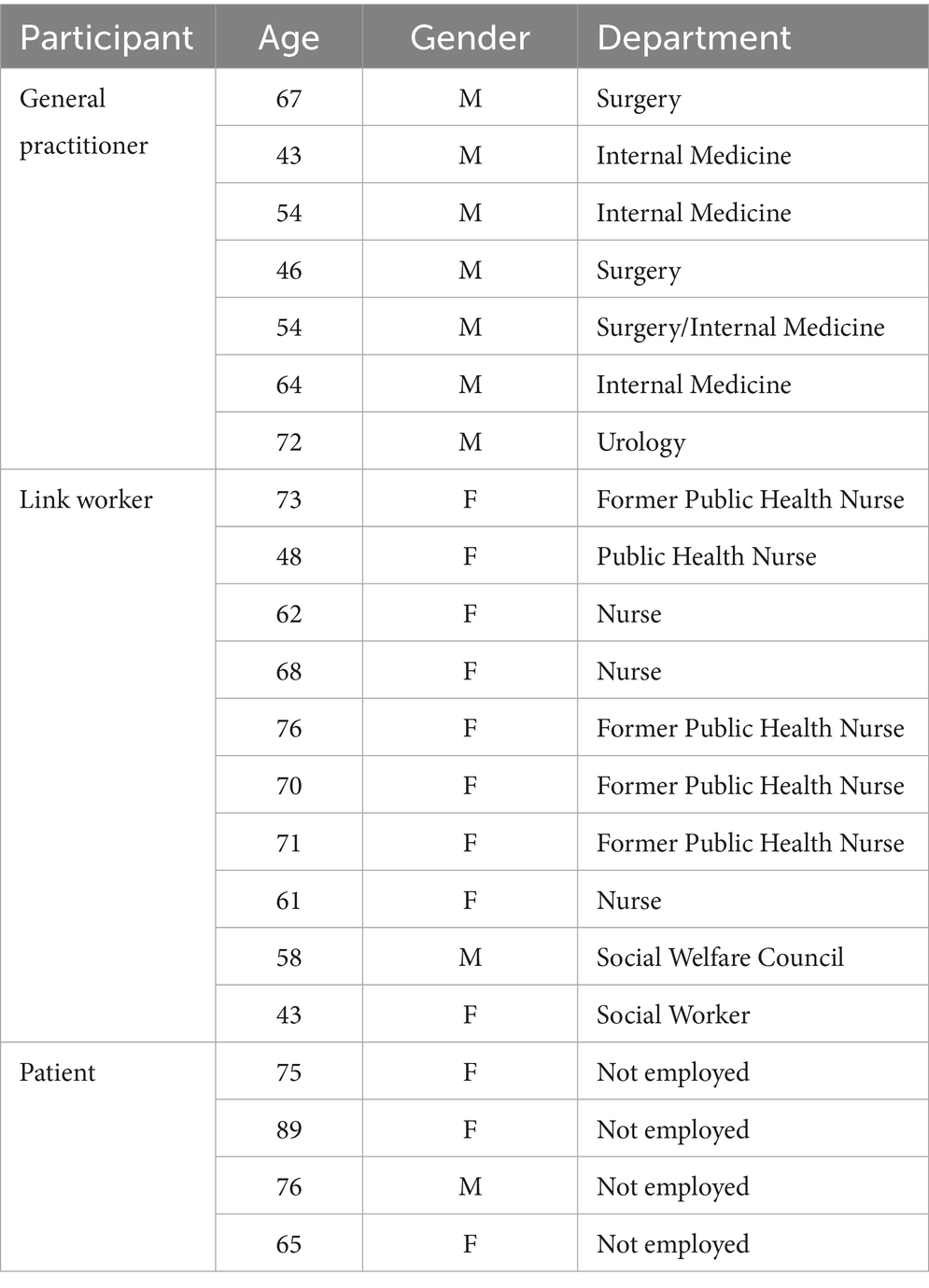
The attributes of the participants are shown in Table 1. Participants were purposively selected to include a diverse range of characteristics and backgrounds. The study included seven GP (all male, mean age: 57.1 ± 10.9 years) and 10 LW (male: 1, female: 9, mean age: 63.0 ± 10.9 years) from seven medical districts of Akita Prefecture. We directly invited GP and LW to participate through existing connections within the task force. Some LW joined the study at the request of their affiliated GP.
We also asked participating GP and LW to assist with the recruitment of patients. Using a research brochure that explained the concept of SP and provided an overview of this study, they recruited individuals who met the following criteria: (1) were cooperative and (2) were facing or at high risk of social isolation (e.g., older caregivers or older adults living alone). Of the 47 patients enrolled in the pilot project, only four were interviewed (male: 1, female: 3, mean age: 76.3 ± 9.8 years), as most were excluded due to cognitive impairment, frailty, or the perceived burden of participation. Seasonal factors, such as heavy snowfall and limited transport in rural Akita, along with COVID-19 restrictions, further limited patients’ availability and researcher visits. Consequently, the patients’ sample was small, and the transferability of findings should be interpreted with caution.
2.3 Data collection
One-on-one semi-structured interviews were conducted between Dec 7, 2021, and Oct 8, 2023. Separate interview guidelines were developed for GP, LW, and patients (Supplementary material 2). The interviews were conducted via online (Zoom Communications, Inc.) for GP and LW; two patient interviews were conducted by telephone and two in person. Prior to the interviews, seven medical students and one faculty member were trained to perform equally by two faculty members through role-playing. A verbatim transcript was created from the audio data recorded by the researchers. Data collection continued until no substantially new codes or themes emerged, with saturation reached after 17 interviews with GP and LW. Four patients’ interviews were included to provide complementary perspectives, although further recruitment was limited by frailty and cognitive impairment among the eligible patient population. Thus, the final sample was considered adequate to capture variation across professional and patients’ experiences.
2.4 Data analysis
A team of seven medical students, one graduate student, and three faculty members conducted a thematic analysis following Braun and Clarke’s six-phase framework (33): familiarization, coding, theme development, review, definition, and reporting. Each interview transcript was assigned to a single team member for initial coding using MAXQDA Analytics Pro 2022 (Release 22.2.0), focusing on the perspectives of GP, LW, and patients regarding the implementation of SP. Any questions or disagreements regarding codes were resolved through team discussion and consensus-building. The first author then organized similar codes into subcategories, categories, and overarching themes. A subsequent team meeting was held to review and refine the categories and themes based on each researcher’s perspective, ensuring that coding and interpretation did not rely on a single viewpoint and enhancing analytical rigor. At this stage, the team confirmed that no additional categories were emerging, supporting the conclusion that data saturation had been reached. Finally, the results were shared with all GP and a subset of LW to verify that the findings accurately reflected participants’ perspectives (data triangulation). GP and LW’s perspectives, which were similar, were presented together, whereas patients’ perspectives were presented separately due to the emergence of distinct categories.
2.5 Trustworthiness
To enhance the rigor of this qualitative case study, we applied Lincoln and Guba’s four criteria of trustworthiness: credibility, dependability, confirmability, and transferability (34). Credibility was supported through investigator triangulation and member checking with all GP and selected LW, ensuring that interpretations accurately reflected participants’ perspectives. Dependability was ensured by discussing and resolving discrepancies among coders within the team, maintaining consistency in analytic procedures. Confirmability was strengthened by systematically documenting and sharing data and analytic procedures, and by storing codes and transcripts in MAXQDA to ensure auditability. Transferability was promoted by including participants with diverse roles, occupations, ages, and sexes, and by providing a detailed description of the rural context in Akita Prefecture.
2.6 Ethical considerations
The study protocol was approved by the Ethics Committee of the Akita Medical GP Association (approval No. 52, October 24, 2023). Informed consent was obtained orally from all GP, LW, and patients prior to participation. The audio data was promised to be deleted after the completion of the study.
3 Results
Demographic characteristics of all participants can be shown in Table 1.
3.1 Perspectives of GP and LW
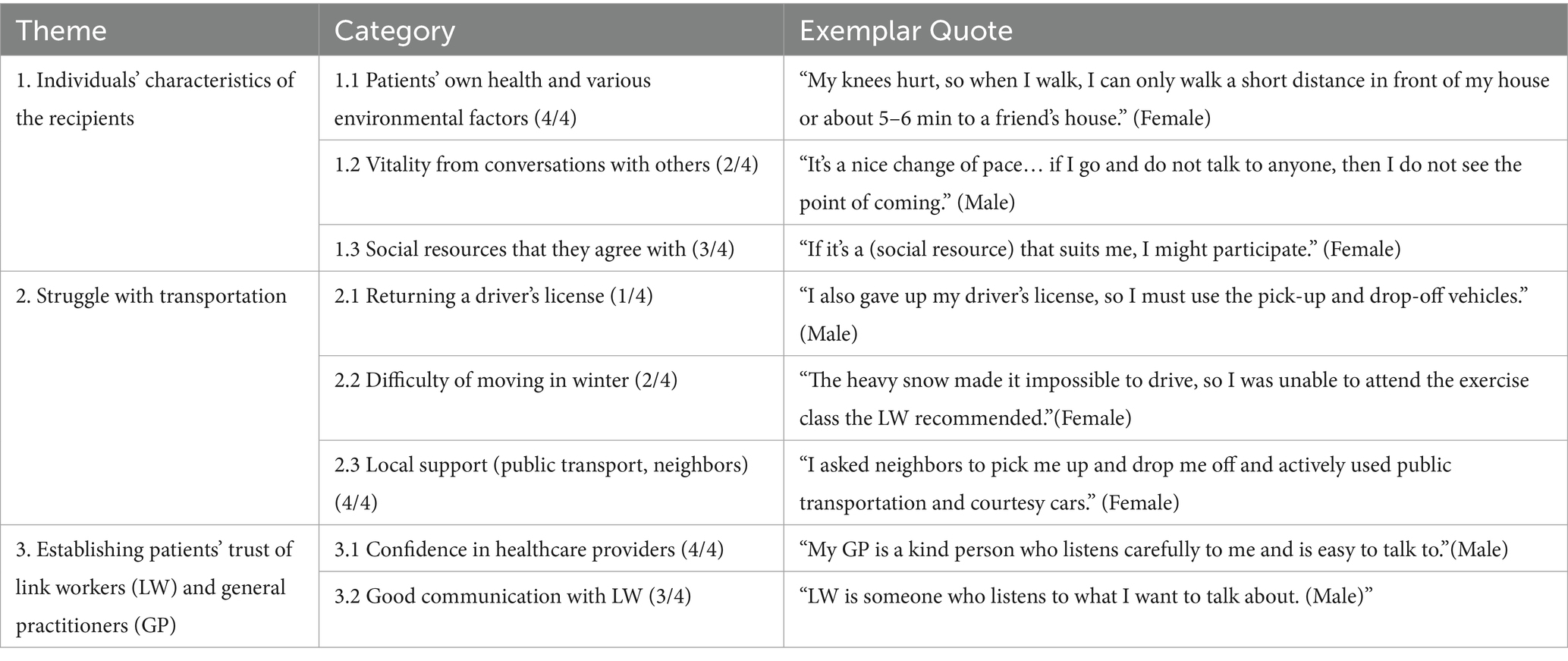
The average interview duration was 39 min and 43 s for GP (n = 7, all male, mean age: 57.1 ± 10.9 years) and 38 min and 53 s for LW (n = 10, male: 1, female: 9, mean age: 63.0 ± 10.9 years). We identified four major themes through thematic analysis. These themes, their categories, frequencies, and representative quotes are summarized in Table 2, while the following sections describe them in detail.
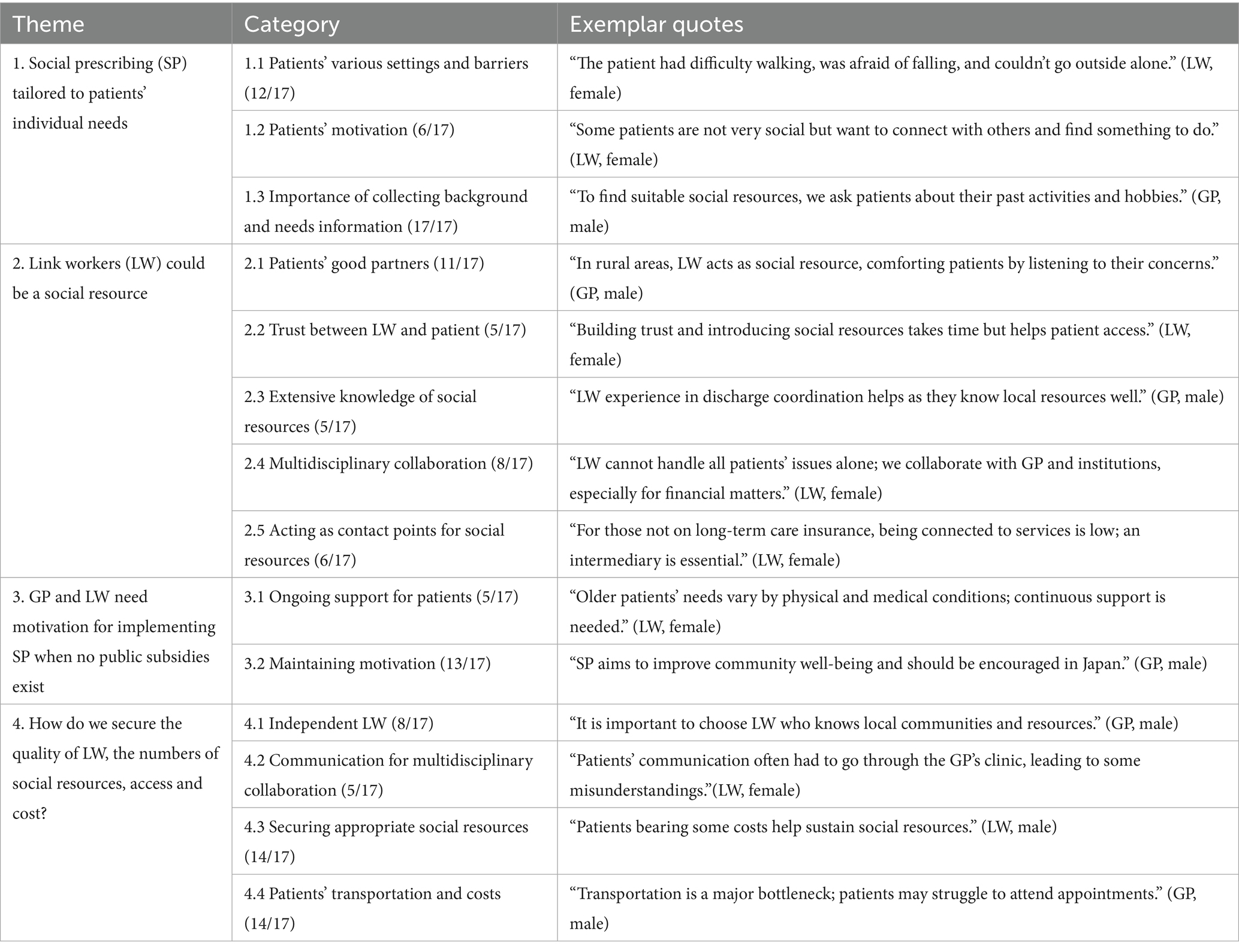
Table 2. General practitioners and link workers’ perspectives: themes, categories, exemplar quotes, and frequency (n/17).
3.1.1 SP tailored to patients’ individual needs
Patients’ diverse backgrounds and health conditions influenced their engagement with SP. Three categories emerged. First, patients experienced different settings and barriers to engaging with SP (i.e., “Patients’ various settings and barriers” to SP, mentioned by 12 out of 17 participants). Second, these differences affected their motivation to participate in SP (i.e., “Patients’ motivation” for SP, mentioned by 6 out of 17 participants). Finally, participants emphasized the importance of collecting detailed information about patients’ backgrounds and needs to ensure appropriate referrals to social resources (i.e., “Importance of collecting background and needs information,” mentioned by 17 out of 17 participants).
3.1.2 LW could be a social resource
LW provided emotional support, built trust, and coordinated with multiple stakeholders to facilitate patient access to social resources. There were five categories. LW was found to play an important role as social resources. The LW becomes the patient’s talking partner (i.e., “Patients’ good partners,” mentioned by 11 out of 17 participants) and encourages the participation of social resources by building a trusting relationship with patients (i.e., “Trust between LW and patient,” mentioned by 5 out of 17 participants). They worked as LW based on their extensive knowledge of social resources obtained from their usual job activities (i.e., “Extensive knowledge of social resources,” mentioned by 5 out of 17 participants), but they also collaborated with practitioners, other medical professionals, government officials, and other multidisciplinary professionals to obtain additional background information on social resources (i.e., “Multidisciplinary collaboration,” mentioned by 8 out of 17 participants). They also served as points of contact for introducing social resources (i.e., “Acting as contact points for social resources,” mentioned by 6 out of 17 participants).
3.1.3 GP and LW need motivation for implementing SP when no public subsidies exist
GP and LW emphasized that ongoing support and commitment are crucial despite time constraints. There were two categories: GP and LW indicated that ongoing patient involvement, support, and time are essential for SP to be successful (i.e., “Ongoing support for patients,” mentioned by 5 out of 17 participants). GP and LW sometimes found it time consuming to refer patients to SP in addition to their regular work. Despite these difficulties, they understood the importance of implementing SP for socially isolated patients (i.e., “Maintaining motivation,” mentioned by 13 out of 17 participants).
3.1.4 How do we secure the quality of LW, the numbers of social resources, access and cost?
Participants identified training, coordination, resource availability, and transportation as key challenges. There were four categories. In addition to clarifying the position of LW, LW candidates need to be trained to take on the role of LW (i.e., “Independent LW,” mentioned by 8 out of 17 participants). LW needed help communicating and coordinating schedules with multiple professions, patients, and key persons (i.e., “Communication for multidisciplinary collaboration,” mentioned by 5 out of 17 participants). In this regard, one GP noted that this profession requires an understanding of confidentiality regarding patients’ privacy. Due to the shortages in social resources in rural depopulated areas like Akita, it is questionable whether available and suitable social resources for patients exist (i.e., “Securing appropriate social resources,” mentioned by 14 out of 17 participants). It is also very important to understand how patients can secure transportation means and costs from their homes to access such resources, as there is no or very limited transportation available to this population (i.e., “Patients’ transportation and costs” to participate in social resources, mentioned by 14 out of 17 participants).
3.2 Perspectives of patients
The average interview duration was 53 min and 4 s for patients (n = 4, male: 1, female: 3, mean age: 76.3 ± 9.8 years). We identified three major themes based on patients’ perspectives. These themes, their categories, frequencies, and representative quotes are summarized in Table 3, while the following sections describe them in detail.
3.2.1 Individuals’ characteristics of the recipients
Patients’ health conditions, living arrangements, and personal preferences influenced their engagement with SP. There were three categories: four patients who participated in SP had their own health issues and various concerns in their daily lives, such as living alone as older adults or living as older couples. (i.e., “Patients own health and various environmental factors,” mentioned by 4 out of 4 participants). Patients stated that they felt invigorated by talking with LW, people they met with social resources, family, and friends (i.e., “Vitality from conversations with others,” mentioned by 2 out of 4 participants). To participate in social resources, patients need to be healthy and in a community that suits them (i.e., “Social resources that they agree with,” mentioned by 3 out of 4 participants).
3.2.2 Struggle with transportation
Limited transportation options, especially for older patients, created barriers to accessing social resources. There were three categories: Many of the patients had given up their driver’s licenses due to illness or advanced age (i.e., “Returning a driver’s license,” mentioned by 1 out of 4 participants), making it difficult for them to get around, especially in the winter when it snows (i.e., “Difficulty of moving in winter,” mentioned by 2 out of 4 participants). However, they used mobile vending services to buy groceries, asked neighbors to pick them up and drop them off, and actively used public transportation and courtesy cars (i.e., “Local support,” mentioned by 4 out of 4 participants).
3.2.3 Establishing patients’ trust of LW and GP
Trust in healthcare providers and good communication with LW facilitated engagement with SP. There were two categories: LW and patients had a good relationship with the four patients we interviewed. Patients had trust in healthcare providers and participated in SP (i.e., “Confidence in healthcare providers,” mentioned by 4 out of 4 participants). They said that even if they were not participating in social resources, they felt more comfortable talking with their LW about daily issues or concerns (i.e., “Good communication with LW,” mentioned by 3 out of 4 participants).
4 Discussion
GP and LW’s perspectives were similar and revealed four themes, while patients’ perspectives yielded three themes. GP and LW reported that SP needs to be individualized for each patient, and patient interviews similarly revealed that differences in patients’ personal characteristics and physical conditions often made accessing social resources challenging. Moreover, GP and LW suggested that LW themselves could function as social resources for patients. All four patients reported that their LW served as a trusted conversational partner who alleviated loneliness. This illustrates an intrinsic motivation to reduce loneliness which appeared to be associated with SP uptake when matched with a reliable human connection. This may further suggest that human relationships and interaction are not merely due to the availability of physical resources but could also be a key driver for engagement. At the same time, patients without private vehicles relied on public transport or local pick-up services, but limited availability of these options constrained access even when motivation to engage was present. Even those with cars were sometimes unable to travel in winter due to heavy snow, indicating that seasonal factors introduced unpredictable barriers that eroded motivation over time. Both GP and LW identified transport challenges as an important factor that may hinder the sustainability of SP. In addition, GP and LW raised concerns about the quality and workload of LW, the adequacy of available social resources relative to patients’ needs, and associated costs. These factors together may highlight a mechanism whereby motivation alone was insufficient to ensure uptake when appropriate, accessible resources were lacking.
This tailored support may be key to SP success, as shown in previous studies (35–39). In addition, although it may depend on recipient characteristics and individual human relationship difficulties, many of the patients perceived the benefits of social interactions, such as conversations with their friends (40) or LW as positive (25). For example, LW was able to become a social resource by presenting themselves as simple listeners to patients’ worries and concerns. Many previous studies have also suggested that trusting relationships between LW and patients may represent central elements in achieving well-being and are the key to successful linkages to suitable services (28, 41, 42). In addition, such active listening provided by LW met patients’ needs in underserved areas, such as Akita, where transportation in winter is impeded due to heavy snowfall.
Nevertheless, as previous studies have shown (41, 43), the availability of social resources, such as local communities and transportation, appears to be an important factor for SP implementation. As a possible solution, LW could collaborate with patients to create social resources concurrently with SP. As suggested by previous evidence (27), SP from a medical perspective often centers on concepts such as person-centeredness, empowerment, and co-production. One such study appeared to show how a few older recipients of SP were empowered by the LW and subsequently built social resources collaboratively within limited regions (27). Furthermore, another study has indicated that the goal of SP can be to increase recipients’ self-confidence and enable them to make their own plans for social independence, such as forming walking groups, community cafés, or cooking groups (42). In our study, there was an example of LW who planned to open a coffee shop. These activities are not only empowering but can also be a means of co-producing plans and social advancement in the current aging population (5) Such activities may be empowering and could also be a means of co-producing plans and social advancement in the current aging population (11). These activities require long-term involvement and support from LWs, as well as their experience in community development (44). Future studies should explore Information and Communication Technology (ICT) applications to social resources in underserved areas where both social and personnel resources are scarce (45). Online services may also be an area for exploration, especially in the winter months when many older adults have difficulty getting around. Emerging evidence suggests that meeting people virtually may have similar positive effects to meeting them in person (46–48). Regarding transportation, the use of automated vehicles in rural areas is considered potentially able to improve the quality of rural public transportation (49). While ICT solutions and autonomous transport hold long-term potential, their feasibility is constrained by high costs (50) and the necessity of infrastructure development (51). Additionally, low digital literacy among the older adults (52) and concerns about data governance and privacy (53) are also challenges. As immediate, low-cost alternatives, interventions such as telephone befriending programs (54), the development of nature-based activity programs with demonstrated mental health benefits (55), and demand-responsive transportation and shared taxis (56) could provide accessible support for socially isolated older adults in rural areas like Akita.
In addition, SP that involves one-on-one support between LW and recipients can be extremely time-consuming (52), and has been criticized for its low cost-effectiveness and the concern that it may only benefit a limited group of people (57–59). While GP and LW recognize the benefits and are motivated to engage in such activities, carrying them out on a voluntary basis in addition to their regular duties places a considerable burden on them (60–63). Therefore, it is important to implement SP as efficiently as possible while utilizing existing systems.
Firstly, the points of contact for SP may warrant consideration. In the United Kingdom, where SP originated, GP-led SP was introduced in the government’s long-term plan in 2019 (64), under which GP is reimbursed on a per capita basis, with GP receiving payment based on the number of patients they manage. This structure facilitates the establishment of long-term patient relationships and emphasizes reducing the frequency of visits and alleviating staff workload, thereby enabling greater focus on preventive care. Consequently, GP-led SP has become prevalent in the UK; however, some challenges exist owing to the new official started (64). In Japan, patients have the autonomy to visit any medical facility of their choice, resulting in GP not overseeing all patients and a lack of continuity of care. In addition to medical insurance, Japan also has a long-term care insurance system that caters to older adults who may not need medical care but need welfare services, specific health checkups, and specific health guidance for people aged 40–74. Like Japan, South Korea’s healthcare system is not GP-managed, although local primary care clinics similarly play a GP-like role in providing first-contact care. During the COVID-19 pandemic, a community-based SP pilot in a rural South Korean community statistically confirmed a reduction in loneliness and depression among older adults, as well as an increase in their sense of social participation and self-esteem (65). This model was not GP-led; rather, it leveraged local community resources. Therefore, it is desirable to establish multiple points of contact to implement SP effectively. In this study, a questionnaire was designed for the early detection of social isolation in social and medical settings.
Secondly, in a nation without LW, the key issue is who fulfills this role (30). For example, similar challenges have been reported in Romania, where the formal roles of LW and the structures for SP are not well-established (66). In the UK, LW is employed by organizations in the voluntary sector and are either commissioned to work for the national health service (NHS) or are hired directly by the NHS (67). In Japan, there are already roles fulfilling health counseling for older adults in the community, such as in large hospitals and long-term care welfare facilities. The problem, however, is not only the lack of these roles and the consistent nature of the work, but also the degree to which patients can be connected to social resources. In urban areas, where social resources are plentiful, existing positions may easily connect patients to social resources. However, in Akita Prefecture, where social resources are scarce, as in this study, LW are required not only to refer patients to social resources but also to provide transportation (68, 69) and create new social resources to support them in getting to social resources. In this regard, it may be possible to divide the functions of LW by strengthening multidisciplinary collaborations. To implement SP, it is a challenge to secure a stable financial foundation. For instance, it is a matter for consideration how to set an appropriate remuneration for LW and related multidisciplinary teams. It is also thought to be necessary to consider patient payments in addition to the framework of the insurance system. Some GP and LW who participated in this study expressed the view that social resources need to be something patients feel are worth paying for.
One of the main strengths of this study is the triangulation of perspectives, incorporating GP, LW, and patients, which allowed for a comprehensive understanding of factors affecting the implementation of SP. In addition, this study provides Japan-specific insights into facilitators and barriers, offering valuable information for promoting SP in underpopulated areas with limited social resources. The study also highlights specific and actionable themes, such as transportation challenges, workforce limitations, and social resource mapping. These findings may inform policy-making and practical implementation efforts aimed at establishing SP in local communities.
This study has several limitations. Firstly, only four patients were interviewed, which limits the transferability of patients’ perspectives. In addition, there is a possibility of selection bias, as participating patients were mainly recruited via their GP, and participating GP and LW were likely more motivated to take part in SP intervention. Future studies should recruit larger and more diverse patients’ samples through multiple channels, independent of GP networks, to reduce this bias. Secondly, responses from GP and LW may have been influenced by social desirability bias and the structure of the interview guides, and future work could incorporate anonymous surveys or mixed methods to mitigate these effects. Thirdly, there is a possibility of selection bias, as participating GP and LW were likely more motivated toward SP, and patients were mainly recruited via their GP, which may have affected who was invited and agreed to participate. Finally, the study was conducted in a single rural prefecture (Akita), and findings may not be directly generalizable to urban or other regional contexts in Japan; comparative studies across multiple settings are warranted.
5 Conclusion
In rural, resource-constrained settings such as Akita, successful SP depends on tailoring to individual needs, ensuring LW competence, and addressing transport barriers. These findings suggest that future policies should focus on sustainable funding for LW, integration with existing health and welfare systems, and mobility solutions.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the ethics committee of the Akita Medical GP Association (approval date: Oct 24, 2023, No. 52). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
NO: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing. ME: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – review & editing. MA: Data curation, Formal analysis, Investigation, Project administration, Writing – review & editing. AI: Data curation, Formal analysis, Project administration, Writing – review & editing. TY: Data curation, Formal analysis, Investigation, Writing – review & editing. SJ: Writing – review & editing. SM: Supervision, Writing – review & editing. ML: Writing – review & editing. CR: Writing – review & editing. JI: Writing – review & editing. KN: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Ministry of Health, Labour and Welfare’s model project under the Subsidy for [Smooth Operation of the Medical Care System for older adults (KOUREISHA IRYOUSEIDO ENKATSU UNEI JIGYOHI):FY 2021-2023]. The funders had no role in the design of the study; the collection, analysis, and interpretation of data; or the writing of the manuscript.
Acknowledgments
We would like to express our sincere gratitude to Kisara Kato, Shizune Tanaka, Tomoka Ando, Kento Wakisaka and Junko Hirayama for their invaluable assistance with data analysis. We are also deeply grateful to the Akita Medical Association for their cooperation in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1659713/full#supplementary-material
References
1. World Health Organization Regional Office for the Western Pacific. A toolkit on how to implement social prescribing. (2022). Available online at: https://www.who.int/publications/i/item/9789290619765. [Accessed May 7, 2025].
2. Yang, K, and Victor, C. Age and loneliness in 25 European nations. Ageing Soc. (2011) 31:1368–88. doi: 10.1017/s0144686x11000642
3. Park, C, Majeed, A, Gill, H, Tamura, J, Ho, RC, and Mansur, RB. The effect of loneliness on distinct health outcomes: a comprehensive review and Meta-analysis. Psychiatry Res. (2020) 294:113514. doi: 10.1016/j.psychres.2020.113514
4. Crespo, DP, Carrasco, PM, Díaz-Mardomingo, C, Villalba-Mora, E, and Montenegro-Peña, M. Social loneliness in older adults with mild cognitive impairment: predictive factors and associated clinical characteristics. J Alzheimer's Dis. (2024) 97:697–714. doi: 10.3233/jad-230901
5. Zhang, Y, Kuang, J, Xin, Z, Fang, J, Song, R, and Yang, Y. Loneliness, social isolation, depression and anxiety among the elderly in Shanghai: findings from a longitudinal study. Arch Gerontol Geriatr. (2023) 110:104980. doi: 10.1016/j.archger.2023.104980
6. Holt-Lunstad, J, Smith, TB, Baker, M, Harris, T, and Stephenson, D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
7. Kino, S, Stickley, A, Arakawa, Y, Saito, M, Saito, T, and Kondo, N. Social isolation, loneliness, and their correlates in older Japanese adults. Psychogeriatrics. (2023) 23:475–86. doi: 10.1111/psyg.12957
8. Morse, DF, Sandhu, S, Mulligan, K, Tierney, S, Polley, M, Chiva Giurca, B, et al. Global developments in social prescribing. BMJ Glob Health. (2022) 7:e008524. doi: 10.1136/bmjgh-2022-008524
9. Cawston, P. Social prescribing in very deprived areas. Br J Gen Pract. (2011) 61:350. doi: 10.3399/bjgp11x572517
10. Hazeldine, E, Gowan, G, Wigglesworth, R, Pollard, J, Asthana, S, and Husk, K. Link worker perspectives of early implementation of social prescribing: a ‘researcher-in-residence’ study. Health Soc Care Community. (2021) 29:1844–51. doi: 10.1111/hsc.13295
11. Rempel, ES, Wilson, EN, Durrant, H, and Barnett, J. Preparing the prescription: a review of the aim and measurement of social referral programmes. BMJ Open. (2017) 7:e017734. doi: 10.1136/bmjopen-2017-017734
12. Statistics Bureau. Ministry of Internal Affairs and Communications, Japan. Japan Statistical Yearbook (2024). Available online at: https://www.stat.go.jp/english/data/nenkan/73nenkan/index.html [Accessed April 17, 2025].
13. Cabinet Office. Government of Japan. Basic Policy on Economic and Fiscal Management and Reform (2021). Available online at: https://www5.cao.go.jp/keizai-shimon/kaigi/cabinet/honebuto/2021/2021_basicpolicies_en.pdf [Accessed April 17, 2025].
14. Crowe, S, Cresswell, K, Robertson, A, Huby, G, Avery, A, and Sheikh, A. The case study approach. BMC Med Res Methodol. (2011) 11:100. doi: 10.1186/1471-2288-11-100
15. Takahashi, ARW, and Araujo, L. Case study research: opening up research opportunities. RAUSP Manag J. (2020) 55:100–11. doi: 10.1108/rausp-05-2019-0109
16. Anthony, S, and Jack, S. Qualitative case study methodology in nursing research: an integrative review. J Adv Nurs. (2009) 65:1171–81. doi: 10.1111/j.1365-2648.2009.04998.x
17. Imai, Y, and Hasegawa, K. The revised Hasegawa’s dementia scale (HDS-R)-evaluation of its usefulness as a screening test for dementia. Hong Kong J Psychiatry. (1994) 4:162–5.
18. Hughes, ME, Waite, LJ, Hawkley, LC, and Cacioppo, JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. (2004) 26:655–72. doi: 10.1177/0164027504268574
19. Murai, K. Theory and practice of primary care (No. 81): Social prescribing – A case example of the medical association’s initiative: Utsunomiya City Medical Association, Tochigi Prefecture [SHAKAI-TEKI SHOHOU: ISHI-KAI NO TORIKUMI JIREI – TOCHIGI-KEN UTSUNOMIYA-SHI ISHI-KAI NO BAAI]. Japan Medical Journal [NIHON IJI SHINPO]. (2020) 50:12–13.
20. Li, C, Jin, S, Cao, X, Han, L, Sun, N, and Allore, H. Catastrophic health expenditure among Chinese adults living alone with cognitive impairment: findings from the CHARLS. BMC Geriatr. (2022) 22:640. doi: 10.1186/s12877-022-03341-8
21. Kvaal, K, Halding, AG, and Kvigne, K. Social provision and loneliness among older people suffering from chronic physical illness. A mixed-methods approach. Scand J Caring Sci. (2014) 28:104–11. doi: 10.1111/scs.12041
22. Hu, X, Fan, D, and Shao, Y. Social withdrawal (hikikomori) conditions in China: a Cross-sectional online survey. Front Psychol. (2022) 13:826945. doi: 10.3389/fpsyg.2022.826945
23. Corwin, TR, Ozieh, MN, Garacci, E, Palatnik, A, and Egede, LE. The relationship between financial hardship and incident diabetic kidney disease in older US adults – a longitudinal study. BMC Nephrol. (2021) 22:167. doi: 10.1186/s12882-021-02373-3
24. Barnett, K, Mercer, SW, Norbury, M, Watt, G, Wyke, S, and Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43. doi: 10.1016/s0140-6736(12)60240-2
25. Payne, RA, Abel, GA, Guthrie, B, and Mercer, SW. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. Can Med Assoc J. (2013) 185:E221–8. doi: 10.1503/cmaj.121349
26. Ohrnberger, J, Fichera, E, and Sutton, M. The relationship between physical and mental health: a mediation analysis. Soc Sci Med. (2017) 195:42–9. doi: 10.1016/j.socscimed.2017.11.008
27. Gao, SS, Chu, CH, and Young, FYF. Oral health and care for elderly people with alzheimer’s disease. Int J Environ Res Public Health. (2020) 17:5713. doi: 10.3390/ijerph17165713
28. Li, R, Li, R, Xie, J, Chen, J, Liu, S, Pan, A, et al. Associations of socioeconomic status and healthy lifestyle with incident early-onset and late-onset dementia: a prospective cohort study. Lancet Heal Longev. (2023) 4:e693–702. doi: 10.1016/s2666-7568(23)00211-8
29. Delwel, S, Binnekade, TT, Perez, RSGM, Hertogh, CMPM, Scherder, EJA, and Lobbezoo, F. Oral hygiene and oral health in older people with dementia: a comprehensive review with focus on oral soft tissues. Clin Oral Investig. (2018) 22:93–108. doi: 10.1007/s00784-017-2264-2
30. Holt-Lunstad, J. Why social relationships are important for physical health: a systems approach to understanding and modifying risk and protection. Annu Rev Psychol. (2018) 69:437–58. doi: 10.1146/annurev-psych-122216-011902
31. Scarpetti, G, Shadowen, H, Williams, GA, Winkelmann, J, Kroneman, M, and Groenewegen, PP. A comparison of social prescribing approaches across twelve high-income countries. Health Policy. (2024) 142:104992. doi: 10.1016/j.healthpol.2024.104992
32. Marshall, J, Papavasiliou, E, Allan, L, Bradbury, K, Fox, C, Hawkes, M, et al. Reimagining dementia care: a complex intervention systematic review on optimising social prescribing (SP) for carers of people living with dementia (PLWD) in the United Kingdom. Health Expect. (2025) 28:e70286. doi: 10.1111/hex.70286
33. Braun, V, and Clarke, V. Toward good practice in thematic analysis: avoiding common problems and be(com)ing a knowing researcher. Int J Transgender Health. (2023) 24:1–6. doi: 10.1080/26895269.2022.2129597
34. Guba, E, and Lincoln, Y. Fourth generation evaluation. Thousand Oaks, CA: Sage Publications (1989). 448 p.
35. Araki, K, Takahashi, Y, Okada, H, and Nakayama, T. Social prescribing from the patient’s perspective: a literature review. J Gen Fam Med. (2022) 23:299–309. doi: 10.1002/jgf2.551
36. Wood, E, Ohlsen, S, Fenton, SJ, Connell, J, and Weich, S. Social prescribing for people with complex needs: a realist evaluation. BMC Fam Pract. (2021) 22:53. doi: 10.1186/s12875-021-01407-x
37. Naito, Y, Ohta, R, and Sano, C. Solving social problems in aging rural japanese communities: the development and sustainability of the osekkai conference as a social prescribing during the covid-19 pandemic. Int J Environ Res Public Health. (2021) 18:11849. doi: 10.3390/ijerph182211849
38. Grayer, J, Cape, J, Orpwood, L, Leibowitz, J, and Buszewicz, M. Facilitating access to voluntary and community services for patients with psychosocial problems: a before-after evaluation. BMC Fam Pract. (2008) 9:27. doi: 10.1186/1471-2296-9-27
39. Dash, S, McNamara, S, de Courten, M, and Calder, R. Social prescribing for suicide prevention: a rapid review. Front Public Health. (2024) 12:1396614. doi: 10.3389/fpubh.2024.1396614
40. Hanlon, P, Gray, CM, Chng, NR, and Mercer, SW. Does self-determination theory help explain the impact of social prescribing? A qualitative analysis of patients’ experiences of the Glasgow ‘deep-end’ community links worker intervention. Chronic Illn. (2021) 17:173–88. doi: 10.1177/1742395319845427
41. Tierney, S, Wong, G, Roberts, N, Boylan, AM, Park, S, and Abrams, R. Supporting social prescribing in primary care by linking people to local assets: a realist review. BMC Med. (2020) 18:65. doi: 10.1186/s12916-020-1510-7
42. Moffatt, S, Steer, M, Lawson, S, Penn, L, and O’Brien, N. Link worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. BMJ Open. (2017) 7:e015203. doi: 10.1136/bmjopen-2016-015203
43. Menhas, R, Yang, L, and Danish Nisar, R. Community-based social healthcare practices in China for healthy aging: a social prescription perspective analysis. Front Public Health. (2023) 11:1252157. doi: 10.3389/fpubh.2023.1252157
44. South, J, Higgins, TJ, Woodall, J, and White, SM. Can social prescribing provide the missing link? Prim Health Care Res Dev. (2008) 9:310–8. doi: 10.1017/s146342360800087x
45. Balki, E, Hayes, N, and Holland, C. Effectiveness of technology interventions in addressing social isolation, connectedness, and loneliness in older adults: systematic umbrella review. JMIR Aging. (2022) 5:e40125. doi: 10.2196/40125
46. Allen, C, Vassilev, I, Kennedy, A, and Rogers, A. Long-term condition self-management support in online communities: a meta-synthesis of qualitative papers. J Med Internet Res. (2016) 18:e56. doi: 10.2196/jmir.5260
47. Hobbs, WR, Burke, M, Christakis, NA, and Fowler, JH. Online social integration is associated with reduced mortality risk. Proc Natl Acad Sci USA. (2016) 113:12980–4. doi: 10.1073/pnas.1605554113
48. Johnston, AC, Worrell, JL, Gangi, PMD, and Wasko, M. Online health communities: an assessment of the influence of participation on patient empowerment outcomes. Inf Technol People. (2013) 26:213–35. doi: 10.1108/itp-02-2013-0040
49. Dianin, A, Gidam, M, and Hauger, G. What can be done with today’s budget and demand? Scenarios of rural public transport automation in Mühlwald (South Tyrol). Public Transp. (2024) 16:295–332. doi: 10.1007/s12469-023-00333-8
50. Jiménez, FN, Brazier, JF, Davoodi, NM, Florence, LC, Thomas, KS, and Gadbois, EA. A technology training program to alleviate social isolation and loneliness among homebound older adults: a community case study. Front Public Health. (2021) 9:750609. doi: 10.3389/fpubh.2021.750609
51. Othman, K. Exploring the implications of autonomous vehicles: a comprehensive review. Innov Infrastruct Solut. (2022) 7:165. doi: 10.1007/s41062-022-00763-6
52. Thangavel, G, Memedi, M, and Hedström, K. Customized information and communication technology for reducing social isolation and loneliness among older adults: scoping review. JMIR Ment Health. (2022) 9:e34221. doi: 10.2196/34221
53. Garcia, A, Balingbing, AM, and Palad, Y. Exploring literature on data governance in the health Care of Older Persons: scoping review. JMIR Aging. (2025) 8:e73625. doi: 10.2196/73625
54. Yeung, DYL, Jiang, D, Warner, LM, Choi, NG, Ho, RTH, Kwok, JYY, et al. The effects of volunteering on loneliness among lonely older adults: the HEAL-HOA dual randomised controlled trial. Lancet Heal Longev. (2025) 6:e65–74. doi: 10.1016/j.lanhl.2024.100664
55. Darcy, PM, Armitt, H, Hurd, A, Paton, LW, White, PCL, and Coventry, PA. Green social prescribing: a before and after evaluation of a novel community-based intervention for adults experiencing mental health problems. Health Soc Care Community. (2025) 2025:2016261. doi: 10.1155/hsc/2016261
56. Roh, CG, and Kim, J. What are more efficient transportation Services in a Rural Area? A case study in Yangsan City, South Korea. Int J Environ Res Public Health. (2022) 19:11263. doi: 10.3390/ijerph191811263
57. Kiely, B, Croke, A, O’Shea, M, Boland, F, O’Shea, E, Connolly, D, et al. Effect of social prescribing link workers on health outcomes and costs for adults in primary care and community settings: a systematic review. BMJ Open. (2022) 12:e062951. doi: 10.1136/bmjopen-2022-062951
58. Islam, MM. Does social prescribing address social determinants of health? Front Public Health. (2025) 13:1531801. doi: 10.3389/fpubh.2025.1531801
59. Spanos, S, Wijekulasuriya, S, Ellis, LA, Saba, M, Schroeder, T, and Officer, C. Integrating non-clinical supports into care: a systematic review of social prescribing referral pathways for mental health, wellbeing, and psychosocial improvement. Int J Integr Care. (2025) 25:21. doi: 10.5334/ijic.9127
61. Wilson, J, and Read, J. What prevents GPs from using outside resources for women experiencing depression? A new Zealand study. Fam Pract. (2001) 18:84–6. doi: 10.1093/fampra/18.1.84
62. Watt, G, Brown, G, Budd, J, Cawston, P, Craig, M, Jamieson, R, et al. General practitioners at the deep end: the experience and views of general practitioners working in the most severely deprived areas of Scotland. Occas Pap R Coll Gen Pract. (2012) 89:i–v.
63. Whitelaw, S, Thirlwall, C, Morrison, A, Osborne, J, Tattum, L, and Walker, S. Developing and implementing a social prescribing initiative in primary care: insights into the possibility of normalisation and sustainability from a UK case study. Prim Health Care Res Dev. (2017) 18:112–21. doi: 10.1017/s1463423616000219
64. National Health Service England. Social prescribing summary guide. (2020). Available online at: https://www.england.nhs.uk/wp-content/uploads/2020/06/social-prescribing-summary-guide-updated-june-20.pdf (Accessed May 7, 2025).
65. Kim, JE, Lee, YL, Chung, MA, Yoon, HJ, Shin, DE, Choi, JH, et al. Effects of social prescribing pilot project for the elderly in rural area of South Korea during COVID-19 pandemic. Health Sci Rep. (2021) 4:e320. doi: 10.1002/hsr2.320
66. Surugiu, R, Iancu, MA, Lăcătus, AM, Dogaru, CA, Stepan, MD, Eremia, IA, et al. Unveiling the presence of social prescribing in Romania in the context of sustainable healthcare—a scoping review. Sustainability. (2023) 15:11652. doi: 10.3390/su151511652
67. Rhodes, J, and Bell, S. “‘It sounded a lot simpler on the job description’”: a qualitative study exploring the role of social prescribing link workers and their training and support needs (2020). Health Soc Care Community. (2021) 29:e338–47. doi: 10.1111/hsc.13358
68. Islam, MM. Social prescribing—an effort to apply a common knowledge: impelling forces and challenges. Front Public Health. (2020) 8:515469. doi: 10.3389/fpubh.2020.515469
Keywords: social prescribing, link workers, older adults, social isolation, general practitioners, qualitative research
Citation: Ota N, Ebihara M, Aoki M, Iwasawa A, Yamazaki T, Jung S, Makabe S, Lynch M, Rothwell C, Illing J and Nomura K (2025) Social prescribing for socially isolated older adults in rural Japan: a qualitative case study. Front. Public Health. 13:1659713. doi: 10.3389/fpubh.2025.1659713
Edited by:
Jill Sonke, University of Florida, United StatesReviewed by:
Roxana Surugiu, University of Medicine and Pharmacy of Craiova, RomaniaIkhwan Yuda Kusuma, University of Szeged, Hungary
Copyright © 2025 Ota, Ebihara, Aoki, Iwasawa, Yamazaki, Jung, Makabe, Lynch, Rothwell, Illing and Nomura. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kyoko Nomura, a25vbXVyYUBtZWQuYWtpdGEtdS5hYy5qcA==
†Present address: Atsushi Iwasawa, Department of Nursing, Faculty of Nursing and Nutrition, Shukutoku University, Chiba, Japan
 Naho Ota
Naho Ota Mayu Ebihara2
Mayu Ebihara2 Atsushi Iwasawa
Atsushi Iwasawa Charlotte Rothwell
Charlotte Rothwell Kyoko Nomura
Kyoko Nomura