- 1School of Medicine and Health Management, Tongji Medical College of Huazhong University of Science and Technology, Wuhan, China
- 2Research Center for Rural Health Service, Key Research Institute of Humanities and Social Sciences of Hubei Provincial Department of Education, Wuhan, China
- 3Department of Neurology, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Third Hospital of Shanxi Medical University, Tongji Shanxi Hospital, Taiyuan, China
Background: As chronic diseases become more prevalent in rural China, maintaining health and functional capacity has become a major challenge. In this context, individual proactive health behaviors (PHB) may play a crucial role. However, the mechanisms through which PHB influence somatic functional status (SFS) are still unclear. Particularly, the role of social participation (SP) in this process remains unexplored.
Methods: A cross-sectional survey was conducted among 3,295 chronic disease patients in rural China. Data on PHB and SFS was evaluated using validated Likert scales. Data on SP were collected using a binary-response questionnaire covering seven domains of activity. Descriptive statistics were used to characterize the sample demographics and the distributions of key variables. Hierarchical regression analysis was performed to test the mediation effects.
Results: The mean scores for participants were 24.98 ± 5.89 for PHB, 2.22 ± 1.21 for SP, and 43.33 ± 10.00 for SFS. Significant correlations were found between PHB and SP (r = 0.21, p < 0.001), SP and SFS (r = 0.23, p < 0.001), and PHB and SFS (r = 0.11, p < 0.001). Hierarchical regression and bootstrap analyses confirmed that SP partially mediated the relationship between PHB and SFS, explaining 42.01% of the total effect.
Conclusion: Among rural patients with chronic diseases in China, individual health proactivity primarily enhances somatic function by promoting social participation. Therefore, integrated interventions that encourage both proactive health behaviors and social participation are recommended. These interventions can optimize chronic disease management outcomes in this population.
1 Introduction
The escalating burden of chronic diseases poses a formidable challenge to global health systems (1–3), particularly in rural area where aging populations and limited healthcare resources converge (4–6). As predicted, the prevalence of chronic noncommunicable diseases will increase to 40% by 2030 in China (7, 8). Despite nationwide initiatives like the “Healthy China 2030” strategy and the National Chronic Disease Comprehensive Prevention and Control Demonstration Zone Program (9), rural areas persistently demonstrate higher growth rates in chronic disease prevalence compared to urban counterparts (10–12). This disparity underscores an urgent need to identify modifiable behavioral factors that can optimize functional health outcomes within resource-constrained settings. Additionally, this study specifically focuses on patients with hypertension, diabetes, and stroke. These conditions were selected because they are the most prevalent chronic diseases in rural China and are major contributors to long-term disability and functional decline (13–15), making them a critical priority for public health intervention (16). According to the latest research data, the prevalence of hypertension in China is approximately 29.6% (17), diabetes is 13.7% (18), and stroke is 1.8% (19). Their high prevalence also ensures a sufficiently large and representative sample for our analysis.
Emerging paradigms in health promotion emphasize proactive health behavior (PHB) – a construct that represents an individual’s proactive engagement in managing their health, encompassing anticipatory health monitoring, voluntary participation in preventive care, and collaborative decision-making with healthcare providers (20, 21). PHB moves beyond passive disease management by empowering individuals to systematically acquire self-management skills through information-seeking and resource utilization (22, 23), aligning with the World Health Organization’s framework for patient-centered chronic care (24). While PHB is associated with better disease control (25), their direct impact on preserving somatic functional status (SFS)—the ability to perform daily physical activities—may be limited, especially in complex rural settings (26, 27). This is because the translation of health behaviors into tangible functional benefits often depends on psychological and social mechanisms, such as enhanced self-efficacy and social support (28, 29). Therefore, the pathway from individual agency to functional health is likely mediated by broader social processes (30, 31).
To understand these processes, the social-ecological model provides a robust theoretical framework, positing that health outcomes are shaped by the interplay between individual behaviors and multiple levels of the social environment (32, 33). Within this framework, social participation (SP) is one of the critical social determinant of health, which means active involvement in community and social activities (34), influencing both mental and physical well-being (35, 36). It is important to distinguish the concept of social participation used in this study from social prescribing, a formal healthcare intervention where healthcare professionals refer patients to non-clinical community services via a link worker (37, 38). Our measure of social participation captures the individual’s spontaneous and voluntary engagement in community activities, reflecting their inherent level of social integration (39, 40). According to the social-ecological model, individual-level factors and community-level factors are not isolated; rather, they interact in a reciprocal manner (41, 42). For instance, an individual’s health proactivity may empower them to overcome barriers and engage more confidently in social life (43), and a supportive social environment can facilitate access to health resources and reinforce healthy behaviors (44). Despite the theoretical plausibility of this interaction, several critical knowledge gaps still exists. First, the interaction between individual-level PHB and community-level SP in influencing health has not been fully examined. Second, few studies have explored SP as a potential mediator between PHB and SFS. Given the latent complex relationship between PHB and SFS, exploring only their direct effects would undoubtedly oversimplify the issue. Therefore, it is essential to understand how key factors like SP mediate the relationship between PHB and SFS, offering more actionable insights for clinical practice.
This research aims to clarify the associations among PHB, SP, and SFS, and to quantify the role of SP as a pathway through which health-proactive behaviors contribute to functional preservation. The analysis is framed within the unique sociocultural and healthcare context of rural China. The findings are expected to provide insights for developing integrated public health strategies that utilize social participation to enhance the somatic functional well-being of rural populations.
2 Methods
2.1 Study design
2.1.1 Participants and setting
The study was conducted from July to August 2023 using a stratified random sampling method. In the first stage, six townships in Qianjiang City, Hubei Province were selected as primary sampling units. The selected townships are representative of typical rural areas in central China, characterized by agrarian livelihoods, close-knit social networks, and a significant proportion of the population engaged in farming. In the second stage, individual patients were selected from chronic disease registries maintained by local health centers in each township, using systematic random sampling. The final sample included 3,600 participants, with a target allocation of 240 hypertension patients, 240 diabetes patients, and 120 stroke patients per township. This resulted in a total of 1,440 hypertension patients, 1,440 diabetes patients, and 720 stroke patients. For cases of multimorbidity, the first-reported condition was designated as the primary diagnosis to assign each participant to a single disease category for analysis. The numerical allocation aimed to balance the representation of the three target diseases, with larger sample sizes for hypertension and diabetes due to their higher prevalence in the target population.
2.1.2 Data collection procedures
Data were collected through face-to-face interviews, with trained research staff directly entering the participants’ responses into the questionnaire on mobile devices via the Chinese online survey platform Wenjuanxing (wjx.cn). This approach ensured the survey was accessible to all eligible participants, particularly those who were illiterate or less familiar with digital technology. To ensure data quality and response validity, individuals with incomplete responses or unreasonably short completion times (<400 s, validated through pilot testing) were excluded, resulting in a final analytical sample of 3,295 participants.
2.1.3 Ethical considerations
The study was approved by the Ethical Review Committee of Tongji Medical College, Huazhong University of Science and Technology ([2022] IEC-A251) (China). All participants or their legal guardians/appropriate representatives (in case of illiterate participants) provided informed consent to participate in this study.
2.2 Measurement of proactive health behavior
The proactive health behavior (PHB) scale was adapted from a validated instrument originally developed for Chinese hypertensive patients (45), demonstrating good validity and reliability in populations with chronic diseases. To focus specifically on the core construct of initiative and self-management in chronic disease care, we selected eight core items from the “proactive health responsibility” subdomain of this scale. The selected items were: (1) initiating physical examinations, (2) reporting physical discomfort, (3) participating in health education programs, (4) seeking health guidance, (5) obtaining multidisciplinary care advice, (6) consulting healthcare professionals for health recommendations, (7) clarifying medical doubts proactively, and (8) acquiring disease self-management knowledge. Responses were captured using a 5-point Likert scale (1 = never to 5 = always), with total scores ranging from 8 to 40. The scale showed excellent internal consistency in our sample (Cronbach’s α = 0.810). To further assess its reliability within each disease subgroup, we calculated Cronbach’s alpha separately for patients with hypertension (Cronbach’s α = 0.805), diabetes (Cronbach’s α = 0.806), and stroke (Cronbach’s α = 0.814). These results demonstrated high reliability and internal consistency across all three chronic disease groups, confirming the scale’s applicability for use in this mixed cohort.
2.3 Measurement of somatic functional status
Somatic functional status (SFS) was assessed using the validated Functional Activities Questionnaire (FAQ), a widely recognized and reliable tool for measuring difficulties in activities of daily living (46–49). Respondents rated their capacity to perform essential daily tasks including meal preparation, financial management, and community mobility on a 5-point Likert scale, where 1 = “totally dependent on others” and 5 = “fully independent.” Total scores ranged from 10 to 50. The Chinese adaptation showed the strong internal consistency in our sample (Cronbach’s α = 0.95).
2.4 Measurement of social participation
Social participation, a complex and multidimensional concept reflecting individual engagement in community activities, was measured using a binary response (yes/no) questionnaire consisting of seven dimensions (50). The domains included political participation (civic activities including voting and community decision-making), economic participation (income-generating activities like formal employment or agricultural work), voluntary participation (unpaid community services like environmental clean-up initiatives), family participation (e.g., caregiving and intergenerational support), community participation (e.g., membership in local organizations), digital participation (e.g., online social interaction), and other forms of participation. The total score of the scale was the sum of the dimension scores, ranging from 0 to 7. The scale showed low internal consistency (Cronbach’s α = 0.149). This is expected, as the scale aims to capture the broad scope of engagement across seven diverse domains, rather than a single, unified construct. Thus, it reflects the distinct nature of these activities.
2.5 Measurement of covariates
To control for confounding demographic factors, we selected several covariates based on literature review and included them in the regression model (51, 52). These variables were categorized and incorporated as follows: (1) gender (male, female); (2) age (59 and below, 60–69, and 70 and above); (3) education level (uneducated, primary, middle, high school, and above); (4) occupation type (unemployed, farmers, freelancers, administrators, private owners, and others); (5) household income (less than ¥500 per month, ¥500–1,000 per month, ¥1,000–1,500 per month, ¥1,500–2,000 per month, more than ¥2,000 per month, and not disclosed).
2.6 Analytical strategy
The categorical variables were described using frequency (%), and the differences in frequency were examined using test. Pearson correlation was used to analyze the correlation between main variables. Hierarchical regression analysis (53) was used to examine the mediating effect of SP (M) on the relationship between PHB (X) and SFS (Y). During model construction, the following tests were conducted: (1) examining whether PHB (X) significantly affects SP(M); (2) testing whether PHB(X) significantly influences SFS(Y); and (3) assessing whether SP(M) significantly impacts SFS(Y). If these tests were validated, the next step was to investigate whether the effect of PHB(X) on SFS(Y) weakened upon the inclusion of SP(M), and whether SP(M) still significantly affected SFS(Y). If the results were affirmative, it would indicate the presence of a mediating effect. Subsequently, a bootstrap analysis with 5,000 resamples was used to test the significance of the mediation effect. All analyses were conducted with SPSS 27.0, with a p-value < 0.05 considered as statistically significant.
3 Results
3.1 Participant demographics
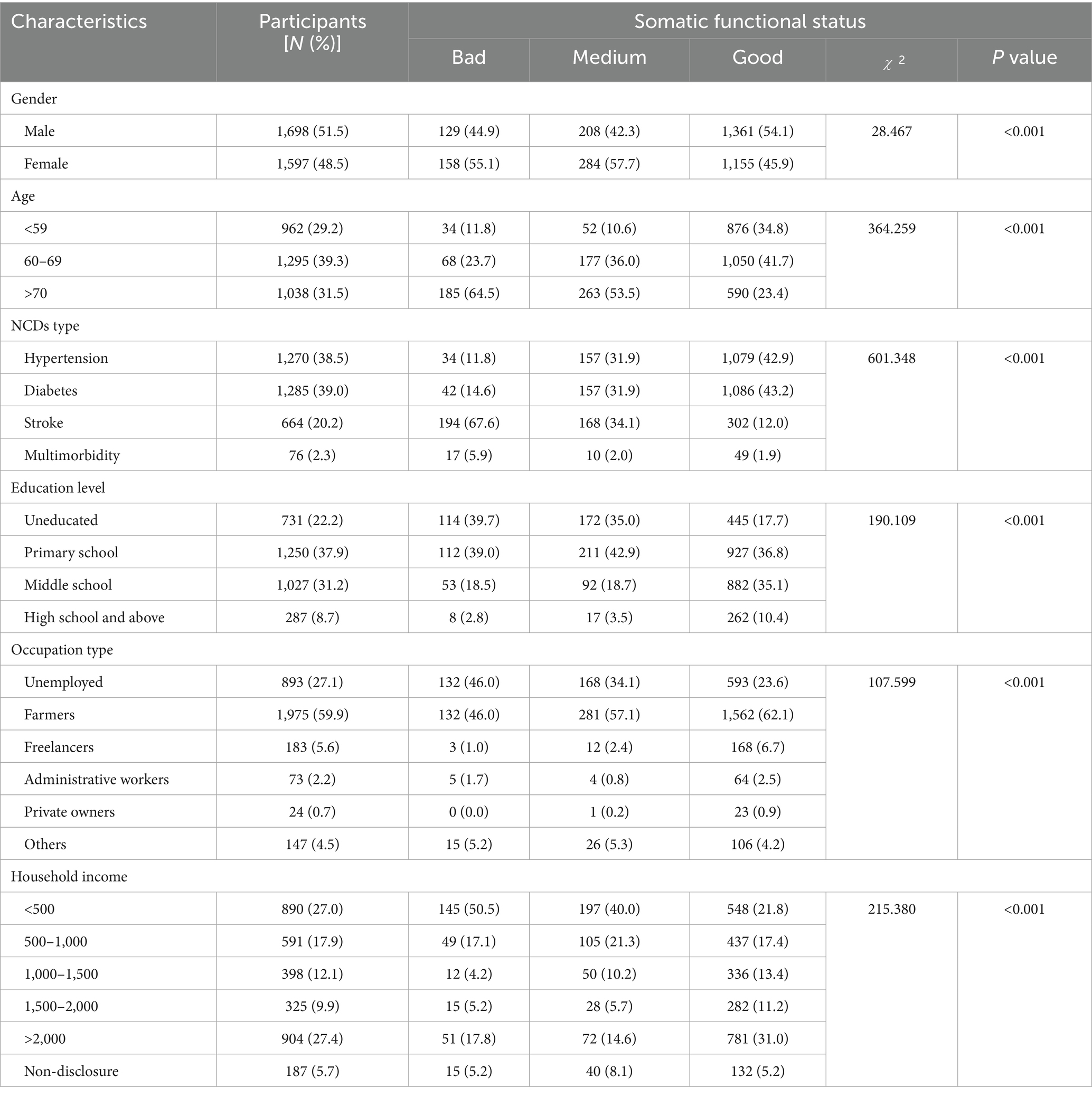
This study included 3,295 patients with chronic diseases. The majority had hypertension (n = 1,270, 38.5%) or diabetes (n = 1,285, 39.0%), followed by stroke (n = 664, 20.2%). A small proportion of participants (n = 76, 2.3%) reported having multimorbidity, defined as the presence of two or more chronic conditions. SFS scores differed significantly across all demographic and socioeconomic groups (all p < 0.001). Detailed demographic characteristics and comparisons of SFS levels across different demographic groups are presented in Table 1.
3.2 Correlation analysis among PHB, SP, and SFS
The mean scores were 24.98 ± 5.89 for proactive health behavior, 2.22 ± 1.21 for social participation, and 43.33 ± 10.00 for somatic functional status. In the correlation analysis, demographic factors such as gender, age, educational level occupation type, and per capita monthly household income were meticulously controlled. The derived findings from Pearson’s correlation analysis conspicuously indicated a statistically significant, positive correlation between the measure of social participation and both the proactive health behavior (r = 0.21, p < 0.001) and the somatic functional status (r = 0.23, p < 0.001). Furthermore, a significant positive association was also observed between the proactive health behavior and the somatic functional status (r = 0.11, p < 0.001), as detailed in Table 2.
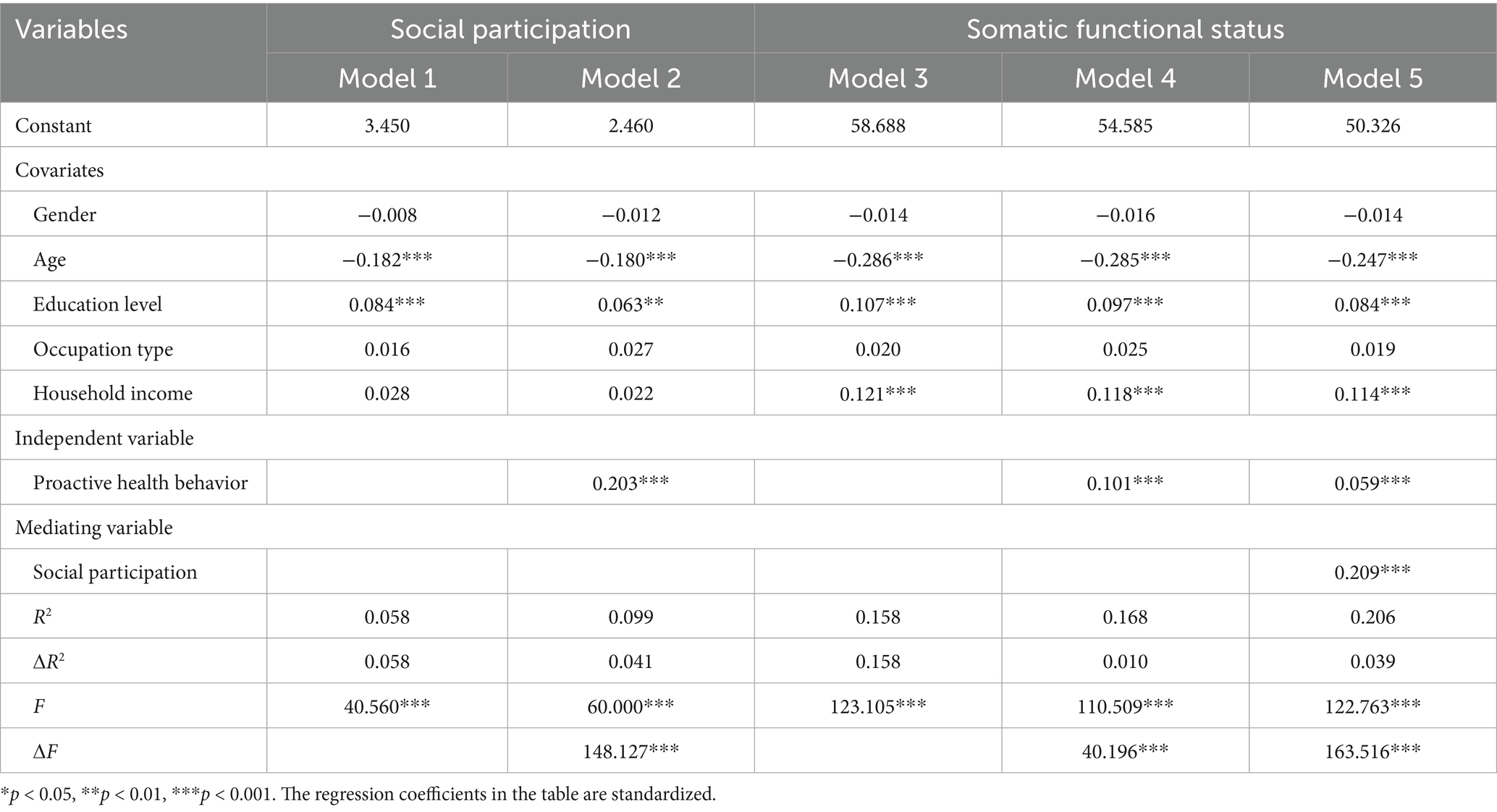
3.3 Mediating role of SP between PHB and SFS
In the analysis presented within Table 3, Model 1 elucidated that, among the plethora of covariates examined, only age (β = −0.182, p < 0.001) and education levels (β = 0.084, p < 0.001) exhibited significant influence on the levels of social participation among rural chronic disease patients. Model 2 established a substantial positive effect of proactive health behavior on social participation (β = 0.203, p < 0.001). Furthermore, upon adjustment for the influence of extraneous variables, Model 4 revealed a noteworthy positive correlation between proactive health behavior and the somatic functional status of the patients (β = 0.101, p < 0.001). Additionally, the exploration extended to the between proactive health behavior, social participation, and the somatic functional status of patients, with findings encapsulated in Model 5. Herein, it was demonstrated that social participation acted as a mediating factor between proactive health behavior and the somatic functional status (β = 0.209, p < 0.001). Among them, the mediation effect (ab) was 0.042, the total effect (c) was 0.101, and 42.01% of the total effect was realized through the mediator of social participation, as illustrated in Figure 1. To confirm the significance of the indirect effect, we conducted a bootstrap analysis. The mediating effect was found to be statistically significant, as the 95% confidence interval did not include zero. This result strongly supports the role of SP as a significant mediator in the relationship between PHB and SFS.
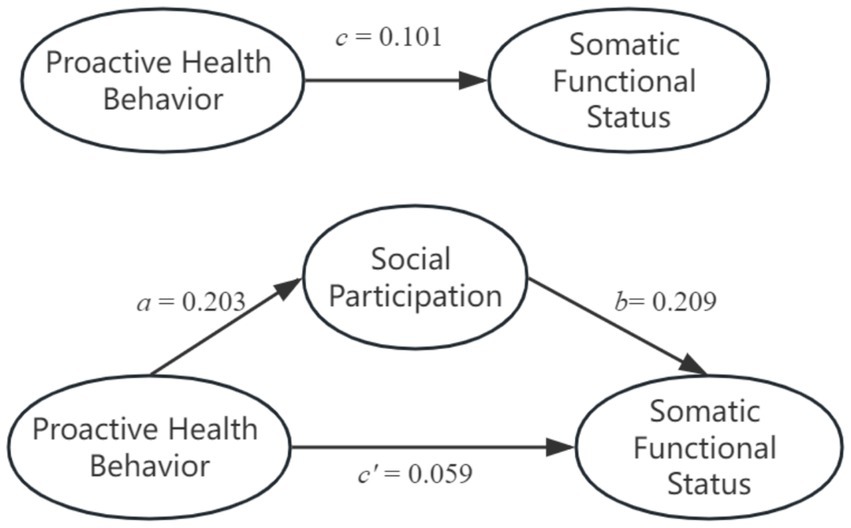
Figure 1. The mediating effect of social participation between proactive health behavior and somatic functional status.
4 Discussion
This study offers new insights into the relationship between individual agency, social context, and physical functional health in the management of chronic diseases in rural areas. The modest direct correlation between PHB and SFS (r = 0.11), coupled with a substantial 42.01% mediation effect of SP, suggests that PHB may not lead to immediate functional improvements. Instead, they promote increased SP, which creates a supportive environment for functional preservation. The functional benefits of individual health initiatives are largely realized through social integration within the community. Moreover, younger age and higher education levels are significantly associated with better somatic functional status, underscoring the influence of sociodemographic factors on functional health outcomes.
The core finding of a significant mediation effect can be explained by the interplay of behavioral mechanisms and the unique socio-cultural context of rural China. Mechanistically, PHB likely enhances patients’ health literacy and self-efficacy (54). This, in turn, empowers them to participate more confidently and purposefully in social activities. The resulting increase in SP fosters a “health-enabling social ecology,” which provides platforms for both formal and informal peer support, health information exchange, and collective monitoring (55). At the same time, SP helps reduce psychological stress and boosts self-efficacy (56, 57), all of which contribute directly to the preservation of physical function. The remarkably high mediation proportion is particularly reflective of the rural Chinese context. Rural area often function as “acquaintance society,” characterized by strong collectivist values and dense social networks (58, 59). In this environment, SP is not merely a leisure activity, it also serves as a fundamental expression of social identity and responsibility. The rich social capital embedded in these areas enables SP to significantly amplify the benefits of PHB, transforming individual health efforts into collective well-being. This explains why a large portion of PHB’s impact on SFS is mediated through social participation.
Our results align with and extend prior research in three aspects. First, prior studies on rural populations have primarily focused on passive disease management strategies (60, 61). In contrast, this study shifts the emphasis to individual-level PHB among patients with chronic conditions. The moderate levels of PHB observed in our study (M = 24.98 ± 5.90) highlight considerable potential for improvement. This suggests that there is significant room for proactive behavioral interventions (62–64). Second, the mediating role of SP (β = 0.209, p < 0.001) corroborates ecological models of health (65), revealing how individual health behaviors interact with community-level social capital. This finding challenges conventional wisdom that rural health outcomes primarily depend on healthcare infrastructure (66, 67), instead highlighting the synergistic potential of combining PHB promotion with community engagement programs. Third, the age gradient in SP (β = −0.182, p < 0.001) underscores the critical need for age-tailored health communication strategies, particularly as China’s rural population rapidly ages (68).
The findings of this study offers meaningful implications for theory and practice. Theoretically, the validated “PHB → SP → SFS” pathway enhances our understanding of how PHB may lead to positive health outcomes, emphasizing the crucial mediating role of SP. Practically, the results indicate that interventions focused solely on promoting PHB may have limited effectiveness. Instead, the impact of such interventions is likely to be more substantial when combined with efforts to foster SP. These findings advocate for a shift from isolated health education to integrated interventions that promote both PHB and SP, with a particular emphasis on counteracting the age-related decline in social participation. To implement this in rural settings, we recommend integrating health initiatives into existing social structures. For example, establishing “Health Corners” within popular gatherings like “(square dancing), “forming “Village Health Promotion Teams” led by trusted community leaders, and implementing a “Health Points” system that rewards both health actions and social participation. These context-specific strategies capitalize on the social capital inherent in rural areas, transforming individual health efforts into collective benefits. This approach offers a practical pathway for policies, such as “Healthy Villages,” to improve chronic disease management.
This study has several limitations. First, the cross-sectional design limits the ability to draw definitive causal conclusions, as reverse causation cannot be ruled out. Additionally, the use of self-reported data for all key variables may introduce social desirability bias. The sample was also drawn from a specific rural region in Hubei Province, which may limit the generalizability of the findings to other regions or cultural contexts. Furthermore, the partial mediation effect suggests that a significant portion of the variance in the PHB-SFS relationship remains unexplained. This implies that other factors, such as biological mechanisms or healthcare system elements, may play a role (69, 70). Future research should address these limitations by adopting longitudinal or intervention designs, incorporating objective biomarkers, and conducting multi-center studies to establish causal relationships and test the robustness of our mediation model across diverse populations.
5 Conclusion
This study provides empirical evidence that SP plays a significant role in mediating the relationship between PHB and SFS among chronic disease patients in rural China. Our results show that the functional benefits of health proactivity are primarily realized through SP, which accounts for 42.01% of the total effect. This highlights the importance of individual agency in health management, which is most effectively translated into preserved physical function when supported by a robust social environment. We recommend that public health strategies, especially within the framework of China’s “Healthy Villages” initiative, should combine the promotion of PHB with efforts to strengthen SP. This approach would leverage the synergistic effects of both factors on functional health. Such integration can be achieved by incorporating health promotion into existing village structures and social activities, utilizing the rich social capital found in rural life.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The datasets are not publicly available to protect participant privacy but can be provided by the corresponding author upon reasonable request. Requests to access these datasets should be directed to c2Z0YW5nMjAxOEBodXN0LmVkdS5jbg==.
Ethics statement
The studies involving humans were approved by Ethical Review Committee of Tongji Medical College, Huazhong University of Science and Technology. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
YH: Writing – original draft, Writing – review & editing, Methodology. HQ: Writing – review & editing, Writing – original draft, Formal analysis. YP: Writing – review & editing, Writing – original draft, Methodology CW: Writing – review & editing, Investigation. HD: Writing – review & editing, Data curation. JS: Writing – review & editing, Investigation. KZ: Writing – review & editing, Supervision. YW: Writing – review & editing, Conceptualization. ST: Funding acquisition, Project administration, Writing – review & editing. MZ: Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by National Key R&D Program in China (2022YFE0133000), National Nature Science Foundation of China (72004073, 72374079), Natural Science Foundation of Hubei Province (JCZRYB202500352), Research and Innovation Team Project for Scientific Breakthroughs at Shanxi Bethune Hospital (2024AOXIANG05).
Acknowledgments
We thank all the volunteer participants for their patience and participation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer YT declared a shared affiliation with one of the authors MZ to the handling editor at time of review.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
2. Lyu, J, Zhang, W, Li, W, Wang, S, and Zhang, J. Epidemic of chronic diseases and the related healthy lifestyle interventions in rural areas of Shandong Province, China. BMC Public Health. (2020) 20:606. doi: 10.1186/s12889-020-08729-y
3. Huang, D, Wang, J, Fang, H, Fu, Y, and Lou, J. Longitudinal association of chronic diseases with depressive symptoms in middle-aged and older adults in China: mediation by functional limitations, social interaction, and life satisfaction. J Glob Health. (2023) 13:4119. doi: 10.7189/jogh.13.04119
4. Peng, W, Zhang, L, Wen, F, Tang, X, Zeng, L, Chen, J, et al. Trends and disparities in non-communicable diseases in the Western Pacific region. Lancet Reg Health West Pac. (2024) 43:100938. doi: 10.1016/j.lanwpc.2023.100938
5. Asante, D, Mclachlan, CS, Pickles, D, and Isaac, V. Understanding unmet care needs of rural older adults with chronic health conditions: A qualitative study. Int J Environ Res Public Health. (2023) 20:3298. doi: 10.3390/ijerph20043298
6. Wang, C, Pu, R, Ghose, B, and Tang, S. Chronic musculoskeletal pain, self-reported health and quality of life among older populations in South Africa and Uganda. Int J Environ Res Public Health. (2018) 15:15. doi: 10.3390/ijerph15122806
7. World Health Organization. (2015). China country assessment report on ageing and health. Available online at: https://www.who.int/publications/i/item/9789241509312 (accessed June 10, 2024).
8. Xue, L, Cai, M, Liu, Q, Ying, X, and Wu, S. Trends and regional variations in chronic diseases and their risk factors in China: an observational study based on National Health Service Surveys. Int J Equity Health. (2023) 22:110–20. doi: 10.1186/s12939-023-01910-w
9. Chen, P, Li, F, and Harmer, P. Healthy China 2030: moving from blueprint to action with a new focus on public health. Lancet Public Health. (2019) 4:e447. doi: 10.1016/S2468-2667(19)30160-4
10. Peng, W, Chen, S, Chen, X, Ma, Y, Wang, T, Sun, X, et al. Trends in major non-communicable diseases and related risk factors in China 2002–2019: an analysis of nationally representative survey data. Lancet Reg Health Western Pacific. (2024) 43:100809. doi: 10.1016/j.lanwpc.2023.100809
11. Chen, X, Giles, J, Yao, Y, Yip, W, Meng, Q, Berkman, L, et al. The path to healthy ageing in China: a Peking University–lancet commission. Lancet. (2022) 400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X
12. Zhou, M, Sun, X, and Huang, L. Chronic disease and medical spending of Chinese elderly in rural region. Int J Qual Health Care. (2021) 33:33. doi: 10.1093/intqhc/mzaa142
13. Zhang, M, Shi, Y, Zhou, B, Huang, Z, Zhao, Z, Li, C, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey. BMJ (Online). (2023) 380:e71952. doi: 10.1136/bmj-2022-071952
14. Feigin, VL, Abdollahi, A, Abreu, LG, Adzigbli, LA, Ahmad, S, Ahmed, A, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet Neurol. (2024) 23:973–1003. doi: 10.1016/S1474-4422(24)00369-7
15. Ding, C, Bao, Y, Bai, B, Liu, X, Shi, B, and Tian, L. An update on the economic burden of type 2 diabetes mellitus in China. Expert Rev Pharmacoecon Outcomes Res. (2022) 22:617–25. doi: 10.1080/14737167.2022.2020106
16. Ding, H, Chen, Y, Yu, M, Zhong, J, Hu, R, Chen, X, et al. The effects of chronic disease management in primary health care: evidence from rural China. J Health Econ. (2021) 80:102539. doi: 10.1016/j.jhealeco.2021.102539
17. Zhang, X, and Wu, J. Temporal trends and relevant factors of hypertension in China: A cross-sectional study based on national surveys from 2002 to 2019. Blood Press. (2025) 34:2468172. doi: 10.1080/08037051.2025.2468172
18. Zhou, Y, Liu, J, Zhao, Z, Zhou, M, and Ng, M. The national and provincial prevalence and non-fatal burdens of diabetes in China from 2005 to 2023 with projections of prevalence to 2050. Mil Med Res. (2025) 12:28. doi: 10.1186/s40779-025-00615-1
19. Ji, C, Ge, X, Zhang, J, and Tong, H. The stroke burden in China and its long-term trends: insights from the global burden of disease (GBD) study 1990-2021. Nutr Metab Cardiovasc Dis. (2025) 35:103848. doi: 10.1016/j.numecd.2025.103848
20. Liu, J, Li, W, Yao, H, and Liu, J. Proactive health: an imperative to achieve the goal of healthy China. China CDC Wkly. (2022) 4:799–801. doi: 10.46234/ccdcw2022.156
21. Jiang, F, and Tang, Y. Promoting mental health and preventing mental disorders: adopting a proactive health approach. Alpha Psychiatry. (2025) 26:39495. doi: 10.31083/AP39495
22. Chaoyi, C, Zhanchun, F, Fang, T, Can, S, Yunlong, S, and Huixin, L. Development of the proactive health behavior scale for patients with chronic diseases and its reliability and validity evaluation. Chin J Behav Med Brain Sci. (2024) 33:362–8. doi: 10.3760/cma.j.cn371468-20230820-00063
23. Xiang, G, Li, X, Z, L, and W, H. Reflection and exploration of digital chronic disease management based on the proactive health index. Shanghai Jiao Tong Da Xue Xue Bao Yi Xue Ban. (2023) 43:137–42. doi: 10.3969/j.issn.1674-8115.2023.02.001
24. World Health Organization Framework on integrated, people-centred health services. In: Report by the Secretariat, World Health Organization (2016).
25. Tang, S, Bishwajit, G, Ji, L, Feng, D, Fang, H, Fu, H, et al. Improving the blood pressure control with the ProActive attitude of hypertensive patients seeking follow-up services: evidence from China. Medicine (Baltimore). (2016) 95:e3233. doi: 10.1097/MD.0000000000003233
26. Zimmer, Z, Wen, M, and Kaneda, T. A multi-level analysis of urban/rural and socioeconomic differences in functional health status transition among older Chinese. Soc Sci Med. (2010) 71:559–67. doi: 10.1016/j.socscimed.2010.03.048
27. Moon, H, Cha, S, and Park, E. Perceived barriers to rural elderly women's health-promoting behaviors: an ecological perspective. Int J Environ Res Public Health. (2020) 17:17. doi: 10.3390/ijerph17176107
28. van Hof, KS, Hoesseini, A, Verdonck-De Leeuw, IM, Jansen, F, Leemans, CR, Takes, RP, et al. Self-efficacy and coping style in relation to psychological distress and quality of life in informal caregivers of patients with head and neck cancer: A longitudinal study. Support Care Cancer. (2023) 31:104. doi: 10.1007/s00520-022-07553-x
29. Yu, J, Jin, Y, Si, H, Bian, Y, Liu, Q, Qiao, X, et al. How does social support interact with intrinsic capacity to affect the trajectory of functional ability among older adults? Findings of a population-based longitudinal study. Maturitas. (2023) 171:33–9. doi: 10.1016/j.maturitas.2023.03.005
30. Petkovic, J, Duench, S, Trawin, J, Dewidar, O, Pardo Pardo, J, Simeon, R, et al. Behavioural interventions delivered through interactive social media for health behaviour change, health outcomes, and health equity in the adult population. Cochrane Database Syst Rev. (2021) 2021:CD012932. doi: 10.1002/14651858.CD012932.pub2
31. Weaver, RR, Lemonde, M, Payman, N, and Goodman, WM. Health capabilities and diabetes self-management: the impact of economic, social, and cultural resources. Soc Sci Med. (2014) 102:58–68. doi: 10.1016/j.socscimed.2013.11.033
32. Bronfenbrenner, U. The ecology of human development: Experiments by nature and design. Cambridge, Massachusetts: Harvard University Press (1979).
33. Richard, L, Gauvin, L, and Raine, K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health. (2011) 32:307–26. doi: 10.1146/annurev-publhealth-031210-101141
34. Levasseur, M, Lussier-Therrien, M, Biron, ML, Raymond, E, Castonguay, J, Naud, D, et al. Scoping study of definitions of social participation: update and co-construction of an interdisciplinary consensual definition. Age Ageing. (2022) 51:51. doi: 10.1093/ageing/afab215
35. Choi, S. The effects of social participation restriction on psychological distress among older adults with chronic illness. J Gerontol Soc Work. (2020) 63:850–63. doi: 10.1080/01634372.2020.1830217
36. Takahashi, R, Okada, T, Ide, K, Tsuji, T, and Kondo, K. Promoting social participation in the primary care field: an ecological study on the potential reduction of multimorbidity prevalence. J Prim Care Community Health. (2024) 15:7053419. doi: 10.1177/21501319241293717
37. Surugiu, R, Iancu, MA, Lăcătus, AM, Dogaru, CA, Stepan, MD, Eremia, IA, et al. Unveiling the presence of social prescribing in Romania in the context of sustainable healthcare—a scoping review. Sustainability. (2023) 15:11652. doi: 10.3390/su151511652
38. Petrazzuoli, F, Vidal-Alaball, J, Kenkre, J, Kloppe, T, Evers, S, Napierala, H, et al. Best practice approaches to social prescribing in European primary care: a Delphi protocol focused on link workers. Adv Clin Exp Med. (2025). doi: 10.17219/acem/208216
39. Tomioka, K, Kurumatani, N, and Saeki, K. The differential effects of type and frequency of social participation on IADL declines of older people. PLoS One. (2018) 13:e207426. doi: 10.1371/journal.pone.0207426
40. Zheng, J, Xu, J, and Liu, D. The effect of activities of daily living on anxiety in older adult people: the mediating role of social participation. Front Public Health. (2024) 12:1450826. doi: 10.3389/fpubh.2024.1450826
41. Rutter, M In: M Ungar, editor. Resilience: Causal pathways and social ecology. New York, NY: Springer New York (2012). 33–42.
42. Lounsbury, DW, and Mitchell, SG. Introduction to special issue on social ecological approaches to community health research and action. Am J Community Psychol. (2009) 44:213–20. doi: 10.1007/s10464-009-9266-4
43. Rm, R, and El, D. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. (2000) 55:68–78. doi: 10.1037//0003-066x.55.1.68
44. Mishra, A, Singh, AK, Parida, SP, Pradhan, SK, and Nair, J. Understanding community participation in rural health care: A participatory learning and action approach. Front Public Health. (2022) 10:860792. doi: 10.3389/fpubh.2022.860792
45. Wei, Y, Zhang, L, and Chen, F. An active health behavior scale for hypertensive patients: development and reliability and validity evaluation. Chin J Public Health. (2023) 39:370–4. doi: 10.11847/zgggws1139802
46. Pfeffer, RI, Kurosaki, TT, Harrah, CH, Chance, JM, and Filos, S. Measurement of functional activities in older adults in the community. J Gerontol. (1982) 37:323–9. doi: 10.1093/geronj/37.3.323
47. Yin, L, Ren, Y, Wang, X, Li, Y, Hou, T, Liu, K, et al. The power of the functional activities questionnaire for screening dementia in rural-dwelling older adults at high-risk of cognitive impairment. Psychogeriatrics. (2020) 20:427–36. doi: 10.1111/psyg.12524
48. Gonzalez, DA, Clark, MJ, Gonzales, MM, and Benge, J. Brief report: an evaluation of item bias on the functional activities questionnaire. Arch Clin Neuropsychol. (2023) 38:276–82. doi: 10.1093/arclin/acac071
49. Gonzalez, DA, Gonzales, MM, Resch, ZJ, Sullivan, AC, and Soble, JR. Comprehensive evaluation of the functional activities questionnaire (FAQ) and its reliability and validity. Assessment. (2022) 29:748–63. doi: 10.1177/1073191121991215
50. Wang, R, Chen, Z, Zhou, Y, Shen, L, Zhang, Z, and Wu, X. Melancholy or mahjong? Diversity, frequency, type, and rural-urban divide of social participation and depression in middle-and old-aged Chinese: a fixed-effects analysis. Soc Sci Med. (2019) 238:112518. doi: 10.1016/j.socscimed.2019.112518
51. Choi, E, Han, K, Chang, J, Lee, YJ, Choi, KW, Han, C, et al. Social participation and depressive symptoms in community-dwelling older adults: emotional social support as a mediator. J Psychiatr Res. (2021) 137:589–96. doi: 10.1016/j.jpsychires.2020.10.043
52. Su, B, Li, D, Xie, J, Wang, Y, Wu, X, Li, J, et al. Chronic disease in China: geographic and socioeconomic determinants among persons aged 60 and older. J Am Med Dir Assoc. (2023) 24:206–212.e5. doi: 10.1016/j.jamda.2022.10.002
53. Baron, RM, and Kenny, DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037//0022-3514.51.6.1173
54. Montgomery, A, Lainidi, O, and Georganta, K. Why talking is not cheap: adverse events and informal communication. Healthcare (Basel). (2024) 12:12. doi: 10.3390/healthcare12060635
55. Lorthios-Guilledroit, A, Richard, L, and Filiatrault, J. Factors associated with the implementation of community-based peer-led health promotion programs: A scoping review. Eval Program Plann. (2018) 68:19–33. doi: 10.1016/j.evalprogplan.2018.01.008
56. Kirby, ED, Williams, VP, Hocking, MC, Lane, JD, and Williams, RB. Psychosocial benefits of three formats of a standardized behavioral stress management program. Psychosom Med. (2006) 68:816–23. doi: 10.1097/01.psy.0000238452.81926.d3
57. Grigaitytė, I, and Söderberg, P. Why does perceived social support protect against somatic symptoms: investigating the roles of emotional self-efficacy and depressive symptoms? Nord Psychol. (2021) 73:226–41. doi: 10.1080/19012276.2021.1902845
58. Jing, T, Zhao, X, Xing, H, Bao, C, and Zhan, L. The influence of strong social ties on the choice of long-term care model for middle-aged and older adults in China. Front Public Health. (2023) 11:1112422. doi: 10.3389/fpubh.2023.1112422
59. Barbalet, J. The analysis of Chinese rural society: Fei Xiaotong revisited. Mod China. (2021) 47:355–82. doi: 10.1177/0097700419894921
60. Worsley-Tonks, KEL, Angwenyi, S, Carlson, C, Cisse, G, Deem, SL, Ferguson, AW, et al. A framework for managing infectious diseases in rural areas in low-and middle-income countries in the face of climate change-East Africa as a case study. PLOS glob. Public Health. (2025) 5:e 3892. doi: 10.1371/journal.pgph.0003892
61. Beaglehole, R, Epping-Jordan, J, Patel, V, Chopra, M, Ebrahim, S, Kidd, M, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: A priority for primary health care. Lancet. (2008) 372:940–9. doi: 10.1016/S0140-6736(08)61404-X
62. Pullyblank, K, Brunner, W, Wyckoff, L, Krupa, N, Scribani, M, and Strogatz, D. Implementation of evidence-based disease self-management programs in a rural region: leveraging and linking community and health care system assets. Health Educ Behav. (2022) 49:894–903. doi: 10.1177/10901981221078516
63. Killaspy, H, Harvey, C, Brasier, C, Brophy, L, Ennals, P, Fletcher, J, et al. Community-based social interventions for people with severe mental illness: A systematic review and narrative synthesis of recent evidence. World Psychiatry. (2022) 21:96–123. doi: 10.1002/wps.20940
64. Bishwajit, G, Tang, S, Yaya, S, He, Z, and Feng, Z. Lifestyle behaviors, subjective health, and quality of life among chinese men living with type 2 diabetes. Am J Mens Health. (2017) 11:357–64. doi: 10.1177/1557988316681128
65. Lu, N, and Wu, B. Perceived neighborhood environment, social capital and life satisfaction among older adults in Shanghai, China. Sci Rep. (2022) 12:6686. doi: 10.1038/s41598-022-10742-7
66. Gizaw, Z, Astale, T, and Kassie, GM. What improves access to primary healthcare services in rural communities? A systematic review. BMC Fam Pract. (2022) 23:313. doi: 10.1186/s12875-022-01919-0
67. Eze, OI, and Chukwuma, IF. Does expanding health insurance in rural Nigeria result in improved health outcomes and poverty reduction? J Glob Health Econ Policy. (2024) 4:e2024007. doi: 10.52872/001c.125491
68. Fang, EF, Scheibye-Knudsen, M, Jahn, HJ, Li, J, Ling, L, Guo, H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24:197–205. doi: 10.1016/j.arr.2015.08.003
69. Acabchuk, RL, Kamath, J, Salamone, JD, and Johnson, BT. Stress and chronic illness: the inflammatory pathway. Soc Sci Med. (2017) 185:166–70. doi: 10.1016/j.socscimed.2017.04.039
70. Palmer, K, Marengoni, A, Forjaz, MJ, Jureviciene, E, Laatikainen, T, Mammarella, F, et al. Multimorbidity care model: recommendations from the consensus meeting of the joint action on chronic diseases and promoting healthy ageing across the life cycle (JA-CHRODIS). Health Policy. (2018) 122:4–11. doi: 10.1016/j.healthpol.2017.09.006
Keywords: proactive health behavior, social participation, somatic function status, rural health, chronic disease management
Citation: Huang Y, Qing H, Pan Y, Wang C, Dong H, Song J, Zhang K, Wei Y, Tang S and Zhang M (2025) The proactive health behavior and somatic functional status in Chinese rural chronic patients: the mediating effects of social participation. Front. Public Health. 13:1668760. doi: 10.3389/fpubh.2025.1668760
Edited by:
Ding Li, Southwestern University of Finance and Economics, ChinaReviewed by:
Yan Tong, Shanxi Medical University, ChinaYongxia Mei, Zhengzhou University, China
Gheorghe Gindrovel Dumitra, University of Medicine and Pharmacy of Craiova, Romania
Chaofan Li, Shandong University, China
Ramkrishna Mondal, All India Institute of Medical Sciences, India
Copyright © 2025 Huang, Qing, Pan, Wang, Dong, Song, Zhang, Wei, Tang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shangfeng Tang, c2Z0YW5nMjAxOEBodXN0LmVkdS5jbg==; Min Zhang, emhhbmdfbWluXzM0NjRAMTI2LmNvbQ==
 Yangzhen Huang1,2
Yangzhen Huang1,2 Jia Song
Jia Song Yilin Wei
Yilin Wei Shangfeng Tang
Shangfeng Tang Min Zhang
Min Zhang