- Physical Education College, Jiangxi Normal University, Nanchang, China
Background: With the increase in the global aging population, the mental health of older adults has become increasingly prominent. This study aims to explore the relationship between the interaction of physical activity and sleep quality in older adults and depression and anxiety.
Methods: A multi-stage stratified random sampling method was employed to survey various communities within Nanchang City, collecting data from 2,497 older adults. The assessment tools included the Physical Activity Rating Scale (PARS-3), Pittsburgh Sleep Quality Index (PSQI), the 9-item Patient Health Questionnaire (PHQ-9), and the 7-item Generalized Anxiety Disorder scale (GAD-7).
Results: Among 2,497 participants, 582 (23.30%) had depressive tendencies; 1,122 (44.90%) had anxiety tendencies. The detection rate of depression and anxiety was higher in females than in males. Logistic regression analysis results showed that low physical activity was positively correlated with depression and anxiety (OR = 9.46; 3.66), while poor sleep quality was positively associated with depression and anxiety (OR = 2.40; 9.96) (P < 0.05). There is an interactive effect between physical activity and sleep quality in relation to anxiety and depressive symptoms in older adults. Specifically, compared to low physical activity combined with poor sleep quality, the combination of high physical activity and good sleep quality is associated with reduced levels of both anxiety and depression (P < 0.05).
Conclusion: This investigation underscores the dynamic interplay among physical activity, sleep quality, depressive symptoms, and anxiety in older adults, forming a critical foundation for designing tailored interventions to enhance mental health outcomes in this population.
1 Introduction
The global trend of aging continues to accelerate. Demographic data reveal that 14.6% of Southeast Asia's population comprises adults aged 65 or older. Concurrently, China ranks among nations experiencing the most rapid population aging globally (1). Within this older adult cohort, depression and anxiety represent highly prevalent mental health challenges (2). Empirical evidence indicates that clinically significant depressive manifestations affect approximately one-fifth to one-third (20%-30%) of older adults in China. Concurrently, anxiety-related symptomatology is observed in roughly one-tenth to one-sixth (10%−15%) of older adults (3). Extensive research has established that late-life depression and anxiety frequently co-occur with somatic comorbidities. These conditions notably contribute to autonomic dysregulation, compromise cognitive functions (particularly memory retention and information processing), and significantly elevate the risk of suicidal ideation or behavior among older adults (3–5). Compared to non-depressed peers, older adults with depression exhibit significantly greater mortality risk. Furthermore, depression directly impairs cardiovascular integrity and disrupts metabolic homeostasis (6, 7). Consequently, proactive clinical prioritization of geriatric psychological wellbeing is imperative.
Physical activity (PA) has been established as an effective emotional regulation strategy, modulating affective states through both physiological (8–10) and psychological (11–13) pathways. According to the tenets of cognitive-behavioral theory (14), human cognition, emotion, and behavior are interconnected. Robust evidence confirms that physical activity ameliorates depressive and anxiety symptoms in geriatric populations. The principal neurobiological mechanism entails the regulation of neuroendocrine activity, prompting the endogenous secretion of compounds such as endorphins that elicit euphoric states (15, 16). Concurrently, physical activity attenuates peripheral inflammatory processes. This anti-inflammatory action attenuates disturbances in neurochemical homeostasis, including impaired neurotransmitter signaling, and suppresses excessive activation of the hypothalamic-pituitary-adrenal (HPA) axis, which serves as a central pathway mediating the neuroendocrine stress response (17–19). Moreover, physical activity directly induces neuromuscular relaxation, alleviating somatic tension and affective distress (20–22). Crucially, nocturnal rest quality exerts profound modulatory effects on emotional states (23, 24). Suboptimal sleep constitutes a significant independent predictor for depressive and anxiety disorders, with epidemiological evidence consistently demonstrating substantially elevated depression prevalence among individuals with sleep disturbances compared to age-matched counterparts (25–27). The International Society for Sleep Research (ISRS) emphasizes that nocturnal restoration processes involve active cerebral maintenance and neural homeostasis (28). Consequently, optimal sleep architecture promotes emotional stability and confers prophylactic effects against affective disorders (29, 30).
Prior research has established that physical activity exerts a significant impact on depression and anxiety, while sleep quality is similarly associated with these mental health conditions. Nevertheless, the interplay or synergistic effects of physical activity and sleep quality on depressive and anxiety symptoms remain underexplored, especially among older adults in China. Consequently, this study aims to examine the interactive effects of physical activity and sleep quality on depression and anxiety among Chinese older adults. Rather than evaluating these factors in isolation, the analysis centers on their interaction within China's distinctive sociocultural and epidemiological milieu. This approach yields novel etiological insights that can inform the development of precision, culturally calibrated interventions aimed at reducing affective morbidity in this rapidly aging population.
2 Materials and methods
2.1 Participants
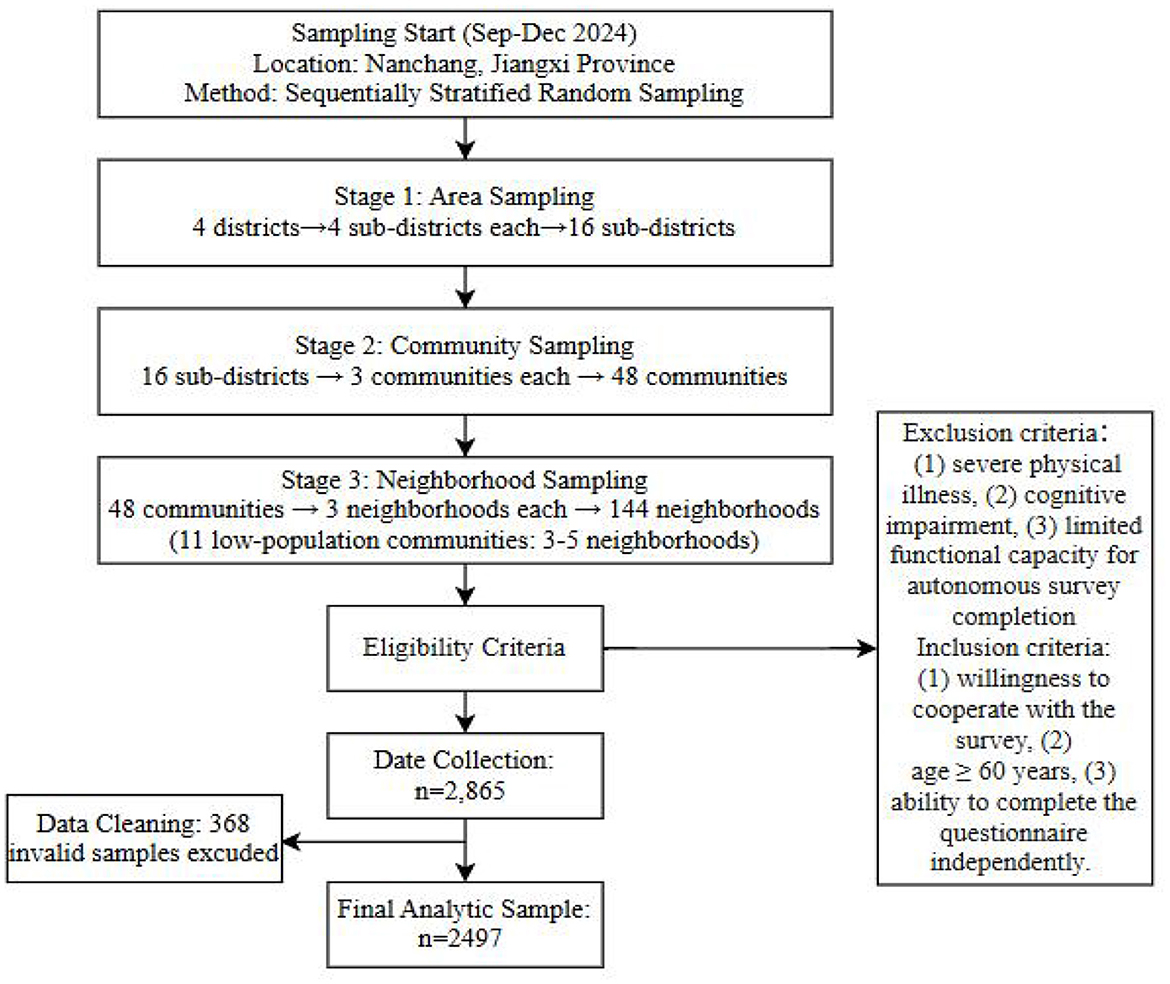
All data are derived from offline surveys conducted in Nanchang City, Jiangxi Province, China, from September to December 2024. Methodologically, we implemented a sequentially stratified random sampling approach across multiple recruitment phases. Four districts were selected for the survey, with four streets sampled from each district, totaling 16 streets. Second, three communities were chosen from each of the 16 sub-districts, and three residential areas were selected from each of the 48 communities, totaling 144 residential areas. Due to the small population in some residential areas, 11 communities selected 3–5 residential areas for the survey. Inclusion criteria: (1) willingness to cooperate with the survey, (2) age ≥ 60 years, (3) ability to complete the questionnaire independently. Exclusion criteria: (1) severe physical illness, (2) cognitive impairment, (3) limited functional capacity for autonomous survey completion. Written informed consent was obtained from all enrolled participants prior to data collection. A total of 2,865 samples were collected, with 368 invalid samples excluded. The final analytic cohort comprised 2,497 eligible participants, representing an 87.43% valid response rate (Figure 1). There were 1,034 males (41.50%) and 1,463 females (58.50%); 1,906 were married (76.30%), 446 were widowed (18.70%), and 145 were divorced or other (5.00%); Educational stratification within the cohort revealed, elementary-level attainment or below predominated (n = 995; 40.50%), followed by junior secondary education (n = 1,125; 45.10%), with high school (n = 228; 9.10%) and tertiary qualifications (n = 129; 5.30%) comprising the remainder. This study was conducted with the approval of the Ethics Committee of Jiangxi Normal University (Approval No. IRB-JXNU-PEC-20240516) and in accordance with the principles of the Declaration of Helsinki.
2.2 Measures
2.2.1 Physical activity rating scale (PARS-3)
This investigation employed Liang's revised Physical Activity Assessment Instrument (31) to quantify PA engagement among older adults. The tool evaluates three dimensions through Likert-type items (e.g., “Rate your typical exercise intensity”), utilizing a 5-point metric (1 = minimal, 5 = extensive). A composite score is derived from exercise intensity, duration, and frequency domains, with elevated scores indicating greater PA involvement. Using established stratification thresholds: scores <19 denote low PA, 20–42 moderate PA, and ≥43 high PA. The instrument demonstrated robust internal consistency (α=0.845).
2.2.2 Pittsburgh sleep quality index (PSQI)
Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (PSQI) (32), a validated instrument developed by Buysse (32). This 19-item tool assesses seven sleep domains through Likert-scaled responses (0–3), incorporating queries such as “Report your typical bedtime during the past month (24-h format)”. Elevated global scores denote superior sleep quality. Psychometric analysis confirmed robust internal consistency (α = 0.892).
2.2.3 Patient health questionnaire-9 items (PHQ-9)
Depressive symptomatology was assessed using the 9-item Patient Health Questionnaire (PHQ-9) (33). This instrument evaluates symptom frequency across nine domains (e.g., “Experiencing self-critical thoughts or perceptions of personal/familial failure”) via a four-tiered frequency metric (0 = never; 3 = nearly daily). A threshold score of ≥5 indicates clinically significant depression, with escalating scores reflecting greater symptom severity. Psychometric validation demonstrated exceptional internal consistency (α= 0.941).
2.2.4 Generalized anxiety disorder-7 (GAD-7)
Anxiety symptoms were evaluated using the Generalized Anxiety Disorder 7-item scale (GAD-7) (34). This instrument measures symptom frequency across seven domains (e.g., “Experiencing persistent nervous tension or irritability”) via a 4-point severity metric (0 = not at all; 3 = nearly every day). Clinical severity stratification delineates: 0–4 = minimal anxiety, 5–9 = mild, 10–13 = moderate, 14-18 = moderately severe, and 19–21 = severe anxiety. Elevated total scores correspond to greater symptom burden. Psychometric analysis confirmed robust internal consistency (α = 0.841).
2.3 Data analysis
Analyses were conducted using SPSS version 26.0 following a sequential analytical protocol. After performing descriptive characterization of demographic variables, sex differences in physical activity (PA), sleep quality, depression, and anxiety among older adults were assessed using chi-square tests. Subsequent analyses entailed adjustment for potential confounders, including gender, age, marital status, educational level, primary income source, number of chronic diseases, and self-rated health status. Separate logistic regression models were fitted to examine the independent associations of PA and sleep with depression and anxiety, respectively. Finally, multiplicative interaction terms between PA and sleep were introduced to evaluate their synergistic effects on depression and anxiety outcomes, with statistical significance defined as P < 0.05.
3 Results
3.1 Testing for common method bias
To address potential common method variance arising from the self-report nature of the measures, Harman's single-factor test was performed in accordance with established methodology (35). An exploratory factor analysis including all items related to physical activity, sleep quality, depression, and anxiety revealed four factors with eigenvalues above 1.0. The most substantial factor explained 23.391% of the total variance (<40%), suggesting that common method bias does not pose a significant threat to the interpretation of the results in this study. Suggesting minimal common method bias concern in this investigation.
3.2 Demographic information on older adults
The study cohort comprised 2,497 older adults (Table 1), with a gender distribution of 1,034 males (41.40%) and 1,463 females (58.60%). Physical activity stratification revealed low levels in 1,827 participants (73.20%), moderate in 422 (16.90%), and high in 248 (9.90%). Suboptimal sleep quality was observed in 1,011 individuals (40.50%), while 1,486 (59.50%) reported good sleep parameters. Clinically significant depressive symptomatology was present in 582 participants (23.30%), while anxiety manifestations affected 1,122 (44.90%) (Table 2). A significant gender disparity was observed in physical activity levels (χ2 = 22.724, P < 0.001). Females demonstrated lower participation in moderate-to-high intensity activities and were overrepresented in low-activity categories compared to males. Females exhibited substantially higher depression prevalence (390/1,463, 26.70% vs. 192/1,034, 18.6% in males; χ2 = 22.175, P < 0.001) and anxiety burden (731/1,463, 50.00% vs. 391/1,034, 37.80% in males; χ2 = 36.153, P < 0.01) (Table 3).
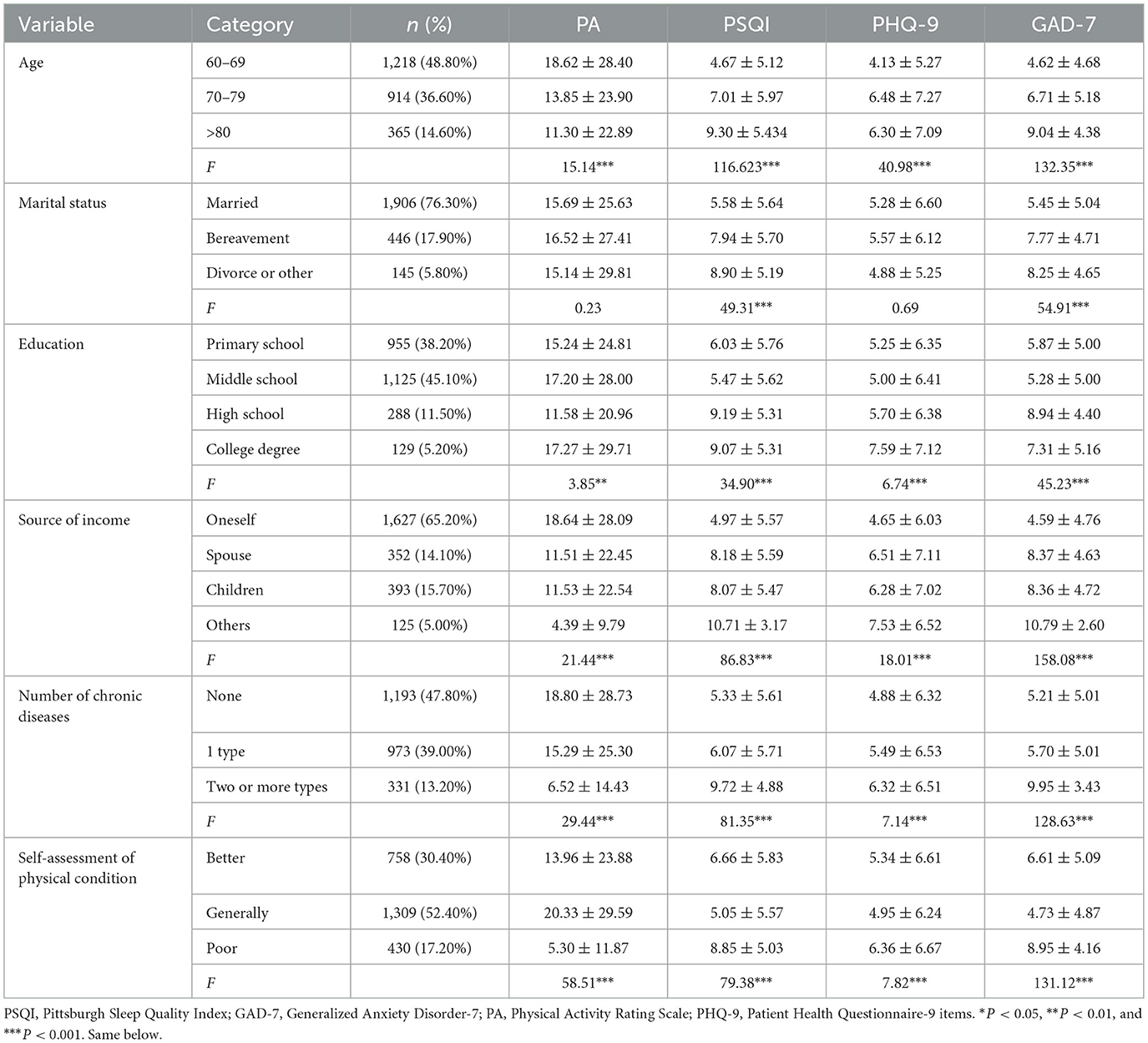
Table 1. Comparative analysis of physical activity and sleep quality relative to depression and anxiety across demographic subgroups in older adults (N = 2,497)
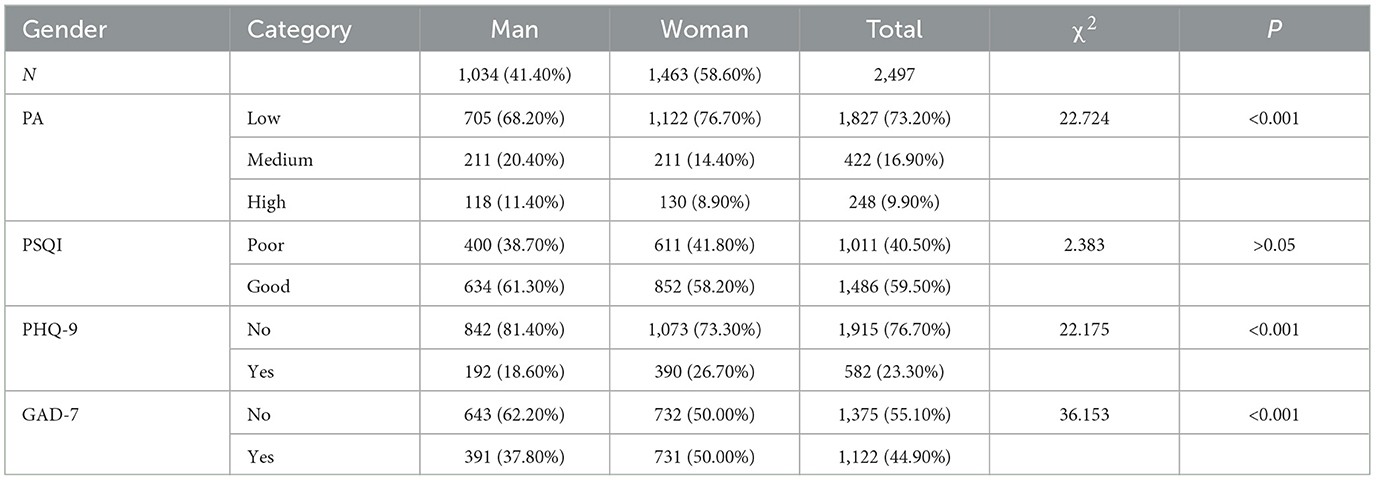
Table 2. Factor-specific characterization of physical activity, sleep quality, depression, and anxiety in sex-stratified geriatric cohorts.
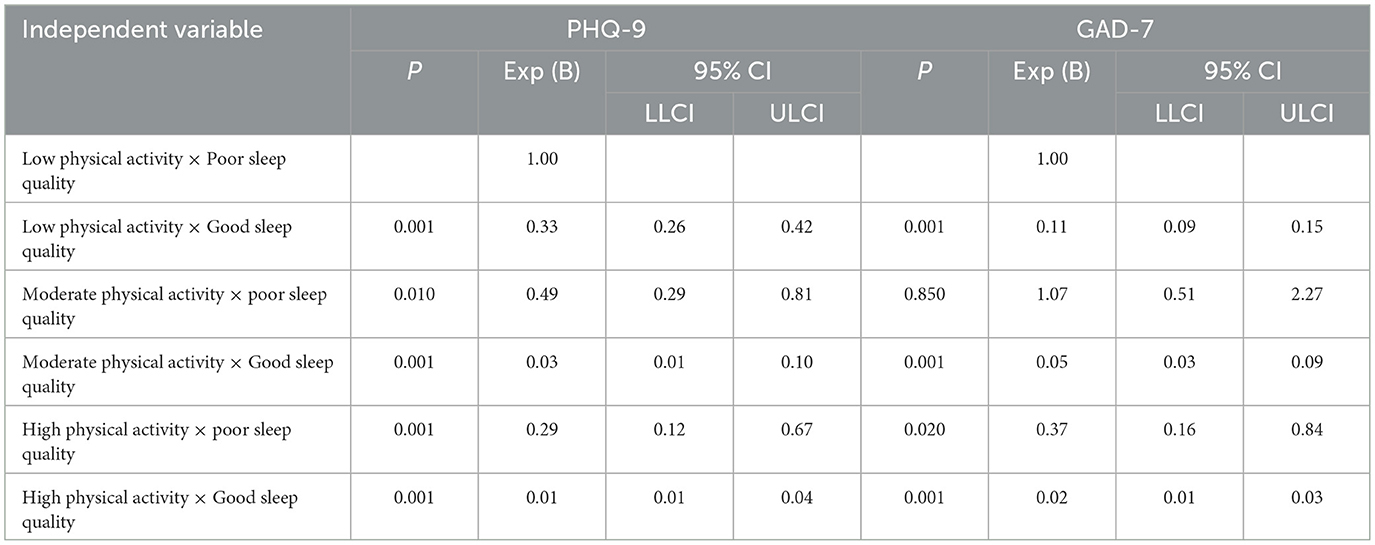
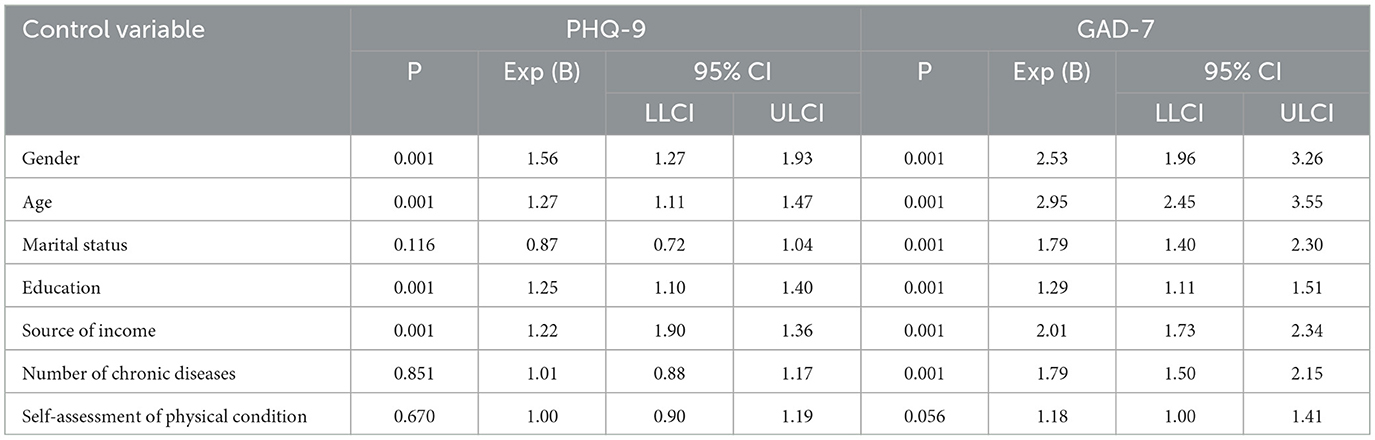
Table 3. Binary logistic regression analysis of the interaction between physical activity, sleep quality, depression, and anxiety.
3.3 The relationship between physical activity, sleep quality, depression, and anxiety in older adults
Following adjustment for core demographic covariates in the older adult population, multivariable logistic regression models were specified with depression/anxiety dichotomization (reference: absence) as outcomes. Primary exposures included physical activity (reference: high PA) and sleep quality (reference: good sleep). The analysis revealed significantly elevated depression risk with low PA (OR = 9.46, 95%CI 2.89–30.97) and anxiety vulnerability (OR = 3.66, 95%CI 2.21–6.06). Moderate PA independently predicted anxiety (OR = 2.85, 95%CI 1.49–5.46). Suboptimal sleep quality demonstrated strong associations with both depression (OR = 2.40, 95%CI 1.40–4.12) and anxiety (OR = 9.96, 95%CI 7.34–13.52), with all associations statistically significant (P < 0.05).
3.4 The interaction between physical activity and sleep quality and its relationship with depression and anxiety
Before examining the interaction effects, we assessed collinearity among the measures of physical activity, sleep quality, depression, and anxiety. Variance inflation factors ranged from 1.128 to 1.614, well below the conservative threshold of 3.0, indicating no multicollinearity and meeting the assumptions for subsequent modeling. Subsequent model fit assessment yielded excellent indices: normed χ2/df = 2.189, RMSEA = 0.022, CFI = 0.990, NFI = 0.982, RFI = 0.980, TLI = 0.989, and GFI = 0.990. All metrics exceeded recognized thresholds for model fit, demonstrating that the model is well specified and has sufficient statistical power to test interaction effects.
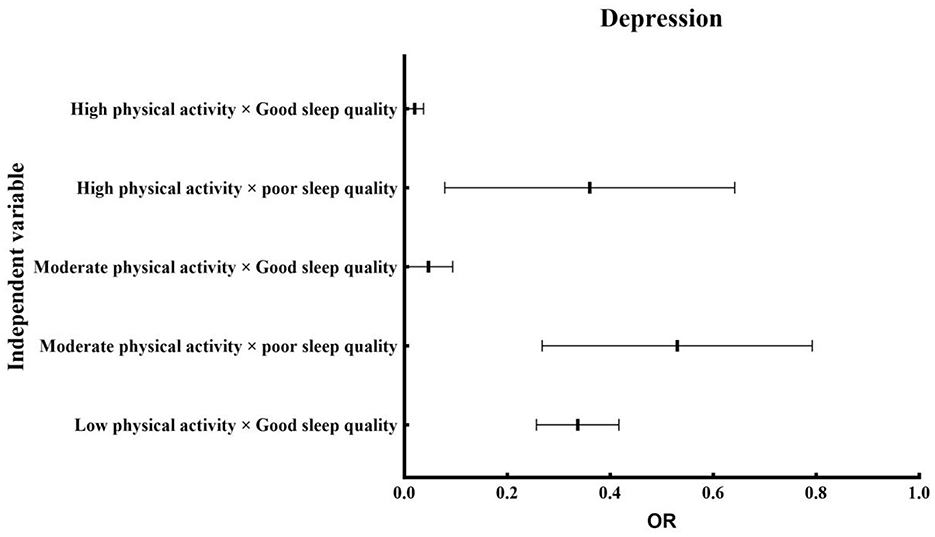
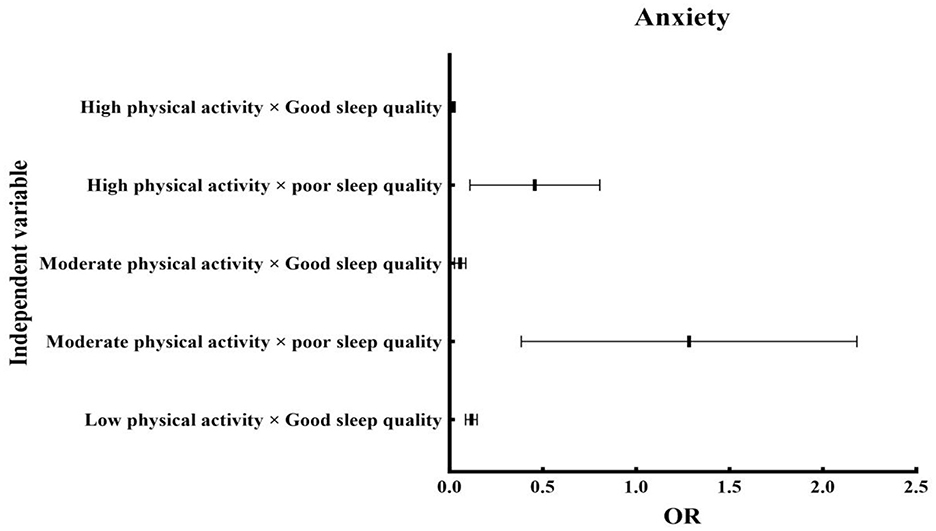
Following adjustment for core demographic covariates (Table 4), binary logistic regression models examined PA-sleep interaction effects (reference: low PA × poor sleep) on depression and anxiety outcomes (Figures 2, 3). Analyses revealed significant effects between physical activity and sleep quality on modulating affective symptomatology (depression, anxiety)in older adults. Relative to the reference group (low PA/poor sleep), Individuals with good sleep quality demonstrated significantly reduced depression/anxiety across all PA levels. Those with poor sleep showed depression reduction regardless of PA status. High PA with poor sleep conferred specific anxiety reduction (P < 0.05). Notably, no significant anxiety and PA interaction was found in the moderate PA and poor sleep subgroup (P > 0.05).
4 Discussion
In this survey of older adults over the age of 60 living in the community, 73.20% (n = 827) exhibited low PA. This rate is slightly lower than the 78.7% reported by Wang et al. (36) but remains markedly higher than the 60.9% documented among older adults in the United States (37). Moreover, Males demonstrated significantly higher PA metrics than females (38–40). Previous research reflects higher activity frequency among older women but greater intensity among men (41). Meta-analytic evidence indicates male preference for vigorous pursuits (golf, bowling, resistance training, team sports) vs. female proclivity for lower-intensity activities (walking, domestic tasks, retail activities, community dance) (42). Positive self-rated health correlated strongly with elevated PA engagement (43, 44). Substantiating the perception-activity feedback loop. Concurrently, 40.50% of participants exhibited clinically significant sleep disturbances, a proportion higher than the 35.9% pooled estimate reported by Lu et al. (45). aligning with multinational prevalence studies (46–48). Older adult females demonstrated 2.3-fold higher sleep disorder prevalence than males, potentially attributable to shortened endogenous circadian periodicity that heightens vulnerability to chronodisruption. In addition, the detection rate of depression and anxiety is higher in older women than in older men. Previous studies have also confirmed this (49–51). Affective disorder prevalence was markedly elevated in females (depression: 26.70% vs. 18.60%; anxiety: 50.00% vs. 37.80%). This disparity may stem from sexually dimorphic neurochemical susceptibility (52–54). Age-related decline in monoaminergic neurotransmission, particularly within serotonergic and dopaminergic systems, disproportionately disrupts affective regulation in females. This effect is mediated through several neurobiological mechanisms, including an accelerated rate of neurotransmitter catabolism, estrogen-mediated alterations in receptor sensitivity, and diminished neurotrophic support within limbic structures (55, 56).
Multivariable regression analyses demonstrated that physical activity (PA) and sleep quality function as protective factors, mitigating depression and anxiety incidence risk among older adults after demographic adjustment. The biopsychosocial framework (57) underscores biological, psychological, and social determinants in ameliorating geriatric affective disturbances. Physiologically, exercise potentiates monoamine neurotransmission (58) and chronically attenuates hypothalamic-pituitary-adrenal (HPA) axis hyperactivity (59, 60). thereby reducing allostatic load and improving affective symptomatology. Psychologically, moderate PA facilitates Stress dysregulation mitigation (61), improves psychological resilience (62, 63), and Self-efficacy fortification (64, 65). it can promote interpersonal communication and increase social interaction (66, 67) and collectively foster affective disorder resilience (68). Comparatively, suboptimal sleep elevates depression risk 2.4-fold and anxiety vulnerability 9.96-fold vs. optimal sleepers, indicating that superior sleep parameters substantially reduce Depression and anxiety risk (69). Empirical observations confirm elevated depression prevalence in sleep-disordered populations vs. general cohorts (27, 70). Establishing sleep quality as a cardinal modulator of affective disorder susceptibility. Crucially, comparative effect magnitude analysis reveals sleep quality demonstrates superior protective effect sizes against depression/anxiety relative to PA, constituting the principal etiological precursor of geriatric affective pathology.
Binary logistic regression revealed significant PA-sleep interaction effects on depression and anxiety in older adults. Relative to the reference group (low PA/poor sleep), Individuals with good sleep quality demonstrated reduced depression/anxiety across all PA levels. Those maintaining PA engagement despite poor sleep showed depression risk mitigation. High PA coupled with poor sleep conferred specific anxiety reduction. These patterns indicate that optimizing either PA or sleep quality provides effective risk mitigation when both factors are suboptimal. Empirical evidence supports the existence of bidirectional neuroregulatory pathways linking physical activity and sleep (71–73), which collectively modulate emotional states in older adults. Mechanistically, PA stimulates monoamine neurotransmission essential for mood regulation (74). Quality sleep maintains neurochemical homeostasis, enhancing daytime neuromodulatory efficiency. Furthermore, regular PA potentiates sleep architecture through shortened sleep latency and extended sleep duration (75, 76). Conversely, restorative sleep (77, 78) enhances exercise capacity via Improved physiological recovery, Increased exercise endurance, and Optimal energy mobilization. In turn, provides better recovery and preparation for physical activity, giving older adults more energy and endurance during exercise. This mutually beneficial relationship helps older adults develop healthy lifestyles, effectively diminishing population-attributable risk for mood and anxiety disorders (79, 80).
4.1 Limitations
This investigation acknowledges several limitations regarding generalizability. First, the geographically circumscribed sampling frame, which was exclusively recruited from an urban cohort in Nanchang, China, may constrain extrapolation to broader geriatric populations. Region-specific socio-ecological covariates such as healthcare accessibility and cultural practices potentially modulate physical activity (PA), sleep architecture, and affective outcomes. Subsequent research should therefore implement stratified random sampling across heterogeneous settings, such as rural, suburban, and multi-center locations, while incorporating socio-ecological covariates like ethnic composition within covariate-adjusted models to enhance ecological validity.
Second, the self-report methodology precludes definitive causal attribution regarding physical activity and sleep quality on affective disorders. Crucially, the temporal precedence remains indeterminate; it is unclear whether PA enhancement drives sleep improvement or, conversely, superior sleep facilitates PA engagement. To address this, subsequent research will implement prospective sequential designs, including randomized controlled trials (RCTs) with protocolized PA and sleep interventions along with multi-wave assessments. These will integrate time-lagged analytics and cross-lagged structural equation modeling to elucidate directional pathways among PA parameters, sleep architecture, and mental health trajectories across temporal domains.
Third, a major limitation concerns the pervasive use of self-reported measures across all constructs, including physical activity, sleep quality, depression, and anxiety. Such exclusive reliance on subjective reports introduces substantial risks of recall bias, social desirability bias, and cognitive interpretation errors. These biases may be especially pronounced among older adults, who may exhibit varying levels of neurocognitive integrity. The absence of objective measures, such as accelerometry-based physical activity monitoring, polysomnographic sleep assessment, or clinician-administered diagnostic interviews, considerably limits the accuracy and robustness of the data. Future studies should incorporate multimodal assessment strategies that combine self-report with objective metrics to strengthen validity and reduce measurement bias.
5 Conclusions
A substantial proportion of older adults exhibited insufficient physical activity (PA) levels. Notably, older women demonstrated poorer sleep quality and more severe depressive and anxiety symptoms compared to their male counterparts. Critically, the interaction between PA and sleep quality exerted significant effects on geriatric depression and anxiety. These findings confirm that both PA engagement and sleep optimization constitute effective non-pharmacological interventions for mitigating affective disorders in aging populations. First, Governments and community centers should implement age-appropriate exercise initiatives (e.g., group walking programs, Tai Chi classes) specifically designed for older adults. Multimodal interventions combining sleep hygiene education (e.g., circadian rhythm management, sleep environment optimization) with mental health workshops should be delivered through community health campaigns. However, it should be acknowledged that the generalizability of these findings may be constrained to urban contexts within China.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Jiangxi Normal University (IRB-JXNU-PEC-20240516). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YY: Formal analysis, Resources, Visualization, Writing – original draft, Writing – review & editing. WH: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. CH: Funding acquisition, Supervision, Validation, Writing – original draft, Writing – review & editing. WZ: Conceptualization, Investigation, Project administration, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Population Prospects. World Population Prospects 2024: Summary of Results: Unedited Version. (2024). Available online at: https://digitallibrary.un.org/record/4053940 (Accessed July 25, 2025).
2. Baiyewu, O., Esan, O., and Elugbadebo, O. (2021). Mental health of older adults. In: Innovations in Global Mental Health. Cham: Springer. p. 1379–1397. doi: 10.1007/978-3-030-57296-9_119
3. He Z-F, Tan W-Y, Ma H, Shuai Y, Shan Z, Zhai J, et al. Prevalence and factors associated with depression and anxiety among older adults: a large-scale cross-sectional study in China. J Affect Disorders. (2024) 346:135–43. doi: 10.1016/j.jad.2023.11.022
4. Zhao W, Zhang Y, Liu X, Yue J, Hou L, Xia X, et al. Comorbid depressive and anxiety symptoms and frailty among older adults: findings from the West China health and aging trend study. J Affect Disord. (2020) 277:970–6. doi: 10.1016/j.jad.2020.08.070
5. Li L, Pan K, Li J, Jiang M, Gao Y, Yang H, et al. The associations of social isolation with depression and anxiety among adults aged 65 years and older in Ningbo, China. Sci Rep. (2024) 14:19072. doi: 10.1038/s41598-024-69936-w
6. Krittanawong C, Maitra NS, Qadeer YK, Wang Z, Fogg S, Storch EA, et al. Association of Depression and Cardiovascular Disease. Am J Med. (2023) 136:881–95. doi: 10.1016/j.amjmed.2023.04.036
7. Huang Y, Chen X, Cai X. The non-linear association between depression scores and all-cause mortality: a cohort study based on NHANES 2005–2018 data. Sci Rep. (2025) 15:15492. doi: 10.1038/s41598-025-00366-y
8. Fan Y, Wang Y, Ji W, Liu K, Wu H. Exercise preconditioning ameliorates cognitive impairment and anxiety-like behavior via regulation of dopamine in ischemia rats. Physiol Behav. (2021) 233:113353. doi: 10.1016/j.physbeh.2021.113353
9. Marques A, Marconcin P, Werneck AO, Ferrari G, Gouveia ÉR, Kliegel M, et al. bidirectional association between physical activity and dopamine across adulthood-a systematic review. Brain Sci. (2021) 11:829. doi: 10.3390/brainsci11070829
10. Gorrell S, Shott ME, Frank GKW. Associations between aerobic exercise and dopamine-related reward-processing: informing a model of human exercise engagement. Biol Psychol. (2022) 171:108350. doi: 10.1016/j.biopsycho.2022.108350
11. Li X, Yu H, Yang N. The mediating role of resilience in the effects of physical exercise on college students' negative emotions during the COVID-19 epidemic. Sci Rep. (2021) 11:24510. doi: 10.1038/s41598-021-04336-y
12. Smith PJ, Merwin RM. The role of exercise in management of mental health disorders: an integrative review. Annu Rev Med. (2021) 72:45–62. doi: 10.1146/annurev-med-060619-022943
13. Qin G-Y, Han S-S, Zhang Y-S, Ye Y-P, Xu C-Y. Effect of physical exercise on negative emotions in Chinese university students: the mediating effect of self-efficacy. Heliyon. (2024) 10:e37194. doi: 10.1016/j.heliyon.2024.e37194
14. Kendall PC. Cognitive-behavioral therapies with youth: guiding theory, current status, and emerging developments. J Consult Clin Psychol. (1993) 61:235–47. doi: 10.1037//0022-006X.61.2.235
15. Dinas PC, Koutedakis Y, Flouris AD. Effects of exercise and physical activity on depression. Ir J Med Sci. (2011) 180:319–25. doi: 10.1007/s11845-010-0633-9
16. Heissel A, Heinen D, Brokmeier LL, Skarabis N, Kangas M, Vancampfort D, et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br J Sports Med. (2023) 57:1049–57. doi: 10.1136/bjsports-2022-106282
17. You T, Arsenis NC, Disanzo BL, LaMonte MJ. Effects of exercise training on chronic inflammation in obesity : current evidence and potential mechanisms. Sports Med. (2013) 43:243–56. doi: 10.1007/s40279-013-0023-3
18. Frodermann V, Rohde D, Courties G, Severe N, Schloss MJ, Amatullah H, et al. Exercise reduces inflammatory cell production and cardiovascular inflammation via instruction of hematopoietic progenitor cells. Nat Med. (2019) 25:1761–71. doi: 10.1038/s41591-019-0633-x
19. Chen H, Lu T, Sui H, Tao B, Chen H, Yan J. Bidirectional relationships between physical exercise and depressive symptoms among Chinese older adults evidence from the China family panel studies. Sci Rep. (2025) 15:15689. doi: 10.1038/s41598-025-00947-x
20. Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. (2011) 11:607–15. doi: 10.1038/nri3041
21. Liu Y, Yan T, Chu JM-T, Chen Y, Dunnett S, Ho Y-S, et al. The beneficial effects of physical exercise in the brain and related pathophysiological mechanisms in neurodegenerative diseases. Lab Invest. (2019) 99:943–57. doi: 10.1038/s41374-019-0232-y
22. Kazeminia M, Salari N, Vaisi-Raygani A, Jalali R, Abdi A, Mohammadi M, et al. The effect of exercise on anxiety in the elderly worldwide: a systematic review and meta-analysis. Health Qual Life Outcomes. (2020) 18:363. doi: 10.1186/s12955-020-01609-4
23. O'Callaghan VS, Couvy-Duchesne B, Strike LT, McMahon KL, Byrne EM, Wright MJ. A meta-analysis of the relationship between subjective sleep and depressive symptoms in adolescence. Sleep Med. (2021) 79:134–44. doi: 10.1016/j.sleep.2021.01.011
24. Zhu Y, Jiang C, Yang Y, Dzierzewski JM, Spruyt K, Zhang B, et al. Depression and anxiety mediate the association between sleep quality and self-rated health in healthcare students. Behav Sci. (2023) 13:82. doi: 10.3390/bs13020082
25. Joo HJ, Kwon KA, Shin J, Park S, Jang S-I. Association between sleep quality and depressive symptoms. J Affect Disord. (2022) 310:258–65. doi: 10.1016/j.jad.2022.05.004
26. Nguyen VV, Zainal NH, Newman MG. Why sleep is key: poor sleep quality is a mechanism for the bidirectional relationship between major depressive disorder and generalized anxiety disorder across 18 years. J Anxiety Disord. (2022) 90:102601. doi: 10.1016/j.janxdis.2022.102601
27. Yin X, Li W, Liang T, Lu B, Yue H, Li S, et al. Effect of electroacupuncture on insomnia in patients with depression: a randomized clinical trial. JAMA Netw Open. (2022) 5:e2220563. doi: 10.1001/jamanetworkopen.2022.20563
28. Zimmerman ME, Benasi G, Hale C, Yeung L-K, Cochran J, Brickman AM, et al. The effects of insufficient sleep and adequate sleep on cognitive function in healthy adults. Sleep Health. (2024) 10:229–36. doi: 10.1016/j.sleh.2023.11.011
29. Talamini LM, Juan E. Sleep as a window to treat affective disorders. Curr Opin Behav Sci. (2020) 33:99–108. doi: 10.1016/j.cobeha.2020.02.002
30. Tomaso CC, Johnson AB, Nelson TD. The effect of sleep deprivation and restriction on mood, emotion, and emotion regulation: three meta-analyses in one. Sleep. (2021) 44. doi: 10.1093/sleep/zsaa289
31. Liang D. Stress levels and their relationship to physical activity among college students. Chinese Mental Health J. (1994) 1994:5–6.
32. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
33. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders patient health questionnaire. JAMA. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
34. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
35. Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
36. Wang L-Y, Chen H-X, Zhu H, Hu Z-Y, Zhou C-F, Hu X-Y. Physical activity as a predictor of activities of daily living in older adults: a longitudinal study in China. Front Public Health. (2024) 12. doi: 10.3389/fpubh.2024.1444119
37. Keadle SK, McKinnon R, Graubard BI, Troiano RP. Prevalence and trends in physical activity among older adults in the United States: a comparison across three national surveys. Prev Med. (2016) 89:37–43. doi: 10.1016/j.ypmed.2016.05.009
38. Li X, Zhang W, Zhang W, Tao K, Ni W, Wang K, et al. Level of physical activity among middle-aged and older Chinese people: evidence from the China health and retirement longitudinal study. BMC Public Health. (2020) 20:1682. doi: 10.1186/s12889-020-09671-9
39. Huang Y, Lu Z. A cross-sectional study of physical activity and chronic diseases among middle-aged and elderly in China. Sci Rep. (2024) 14:30701. doi: 10.1038/s41598-024-78360-z
40. Wang LYT, Lim WS, Tan R-S, Teo LLY, Tan SY, Ooi CH, et al. Frequency, intensity and duration of physical activity is associated with frailty in older adults with cardiac aging. Sci Rep. (2025) 15:15679. doi: 10.1038/s41598-025-00657-4
41. Liao Y-H, Kao T-W, Peng T-C, Chang Y-W. Gender differences in the association between physical activity and health-related quality of life among community-dwelling elders. Aging Clin Exp Res. (2021) 33:901–8. doi: 10.1007/s40520-020-01597-x
42. Stenner BJ, Buckley JD, Mosewich AD. Reasons why older adults play sport: a systematic review. J Sport Health Sci. (2020) 9:530–41. doi: 10.1016/j.jshs.2019.11.003
43. Beyer A-K, Wolff JK, Warner LM, Schüz B, Wurm S. The role of physical activity in the relationship between self-perceptions of ageing and self-rated health in older adults. Psychol Health. (2015) 30:671–85. doi: 10.1080/08870446.2015.1014370
44. Xiao S, Bi Y, Chen W. What factors preventing the older adults in China from living longer: a machine learning study. BMC Geriatr. (2024) 24:625. doi: 10.1186/s12877-024-05214-8
45. Lu L, Wang S-B, Rao W, Zhang Q, Ungvari GS, Ng CH, et al. The prevalence of sleep disturbances and sleep quality in older Chinese adults: a comprehensive meta-analysis. Behav Sleep Med. (2019) 17:683–97. doi: 10.1080/15402002.2018.1469492
46. Jaqua EE, Hanna M, Labib W, Moore C, Matossian V. Common sleep disorders affecting older adults. Perm J. (2023) 27:122–32. doi: 10.7812/TPP/22.114
47. Madan Jha V. The prevalence of sleep loss and sleep disorders in young and old adults. Aging Brain. (2023) 3:100057. doi: 10.1016/j.nbas.2022.100057
48. Dong P, Cheng C, Yin W, Li Z, Shi Y, Gao M, et al. Frailty as a mediator between sleep quality and cognitive impairment among the rural older adults: a cross-sectional study. BMC Geriatr. (2025) 25:7. doi: 10.1186/s12877-024-05657-z
49. Wu NW, Yang F, Xia J, Ma TP, Yu C, Li NX. Analysis of the status of depression and the influencing factors in middle-aged and older adults in China. Sichuan Da Xue Xue Bao Yi Xue Ban. (2021) 52:767–71. doi: 10.12182/20210960507
50. Tang T, Jiang J, Tang X. Prevalence of depressive symptoms among older adults in mainland China: a systematic review and meta-analysis. J Affect Disord. (2021) 293:379–90. doi: 10.1016/j.jad.2021.06.050
51. Cui L, Ding D, Chen J, Wang M, He F, Yu S. Factors affecting the evolution of Chinese elderly depression: a cross-sectional study. BMC Geriatr. (2022) 22:109. doi: 10.1186/s12877-021-02675-z
52. Laird KT, Krause B, Funes C, Lavretsky H. Psychobiological factors of resilience and depression in late life. Transl Psychiatry. (2019) 9:88. doi: 10.1038/s41398-019-0424-7
53. Mariani N, Cattane N, Pariante C, Cattaneo A. Gene expression studies in Depression development and treatment: an overview of the underlying molecular mechanisms and biological processes to identify biomarkers. Transl Psychiatry. (2021) 11:354. doi: 10.1038/s41398-021-01469-6
54. Guo J, Huang X, Dou L, Yan M, Shen T, Tang W, et al. Aging and aging-related diseases: from molecular mechanisms to interventions and treatments. Signal Transduct Target Ther. (2022) 7:391. doi: 10.1038/s41392-022-01251-0
55. Rodríguez JJ, Noristani HN, Verkhratsky A. The serotonergic system in ageing and Alzheimer's disease. Prog Neurobiol. (2012) 99:15–41. doi: 10.1016/j.pneurobio.2012.06.010
56. Hu C, Zhang W, Huang W, Jin C. How grit enhances physical exercise in college students: mediating roles of personal growth initiative and self-efficacy. Front Psychol. (2025) 16. doi: 10.3389/fpsyg.2025.1652984
57. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196:129–36. doi: 10.1126/science.847460
58. Wang M, Nasb M, Wu T, Jia M, So K-F. Exercise-mediated circulating metabolites for brain health. Adv Exerc Health Sci. (2024) 1:221–30. doi: 10.1016/j.aehs.2024.11.001
59. Su C-H, Chuang H-C, Hong C-J. Physical exercise prevents mice from L-Kynurenine-induced depression-like behavior. Asian J Psychiatry. (2020) 48:101894. doi: 10.1016/j.ajp.2019.101894
60. Soong RY, Low CE, Ong V, Sim I, Lee C, Lee F, et al. Exercise interventions for depression, anxiety, and quality of life in older adults with cancer: a systematic review and meta-analysis. JAMA Netw Open. (2025) 8:e2457859. doi: 10.1001/jamanetworkopen.2024.57859
61. Hamer M, Endrighi R, Poole L. Physical activity, stress reduction, and mood: insight into immunological mechanisms. Methods Mol Biol. (2012) 934:89–102. doi: 10.1007/978-1-62703-071-7_5
62. Li N, Wang D, Zhao X, Li Z, Zhang L. The association between physical exercise behavior and psychological resilience of teenagers: an examination of the chain mediating effect. Sci Rep. (2024) 14. doi: 10.1038/s41598-024-60038-1
63. Hu C. Letter to the editor regarding: “leisure-time physical activity patterns and predictors in patients before and after metabolic and bariatric surgery: a cross-sectional study.” Obes Surg. (2025). doi: 10.1007/s11695-025-08248-y. [Epub ahead of print].
64. Tikac G, Unal A, Altug F. Regular exercise improves the levels of self-efficacy, self-esteem and body awareness of young adults. J Sports Med Phys Fit. (2022) 62:7. doi: 10.23736/S0022-4707.21.12143-7
65. Peng B, Chen W, Wang H, Yu T. How does physical exercise influence self-efficacy in adolescents? A study based on the mediating role of psychological resilience. BMC Psychol. (2025) 13. doi: 10.1186/s40359-025-02529-y
66. Goodarzi S, Teymouri Athar MM, Beiky M, Fathi H, Nakhaee Z, Omran SP, et al. Effect of physical activity for reducing anxiety symptoms in older adults: a meta-analysis of randomized controlled trials. BMC Sports Sci Med Rehabil. (2024) 16:153. doi: 10.1186/s13102-024-00947-w
67. Xing Z, Ge C. The relationship between physical exercise and social adjustment in Chinese university students: the sequential mediating effect of peer attachment and self-esteem. Front Psychol. (2025) 16. doi: 10.3389/fpsyg.2025.1525811
68. White RL, Vella S, Biddle S, Sutcliffe J, Guagliano JM, Uddin R, et al. Physical activity and mental health: a systematic review and best-evidence synthesis of mediation and moderation studies. Int J Behav Nutr Phy. (2024) 21:134. doi: 10.1186/s12966-024-01676-6
69. Fu T, Guo R, Wang H, Yu S, Wu Y. The prevalence and risk factors of sleep disturbances in community-dwelling older adults: a systematic review and meta-analysis. Sleep Breath. (2025) 29. doi: 10.1007/s11325-025-03267-6
70. Jiang H-X, Ding C, Liu Y-C, Yu J. Good sleep quality shields older adults from depressive symptoms linked to isolation: Comparing online and in-person social connections. Geriatr Nur. (2025) 62:51–7. doi: 10.1016/j.gerinurse.2025.01.035
71. Kline CE. The bidirectional relationship between exercise and sleep: Implications for exercise adherence and sleep improvement. Am J Lifestyle Med. (2014) 8:375–9. doi: 10.1177/1559827614544437
72. Raudsepp L. One-year longitudinal study found a bidirectional relationship between physical activity and sleep disturbance in teenage Estonian girls. Acta Paediatr. (2018) 107:1433–8. doi: 10.1111/apa.14279
73. Semplonius T, Willoughby T. Long-term links between physical activity and sleep quality. Med Sci Sports Exercise. (2018) 50:2418–24. doi: 10.1249/MSS.0000000000001706
74. Schmitt K, Holsboer-Trachsler E, Eckert A. BDNF in sleep, insomnia, and sleep deprivation. Ann Med. (2016) 48:42–51. doi: 10.3109/07853890.2015.1131327
75. Kline CE, Hillman CH, Bloodgood Sheppard B, Tennant B, Conroy DE, Macko RF, et al. Physical activity and sleep: an updated umbrella review of the 2018 Physical Activity Guidelines Advisory Committee report. Sleep Med Rev. (2021) 58:101489. doi: 10.1016/j.smrv.2021.101489
76. Korkutata A, Korkutata M, Lazarus M. The impact of exercise on sleep and sleep disorders. npj Biol Timing Sleep. (2025) 2:5. doi: 10.1038/s44323-024-00018-w
77. Gao X, Qiao Y, Chen Q, Wang C, Zhang P. Effects of different types of exercise on sleep quality based on Pittsburgh Sleep Quality Index in middle-aged and older adults: a network meta-analysis. J Clin Sleep Med : JCSM : Off Publ Am Acad Sleep Med. (2024) 20. doi: 10.5664/jcsm.11106
78. Li L, Li X, Huang Y, Li H, Li C, Ma Y, et al. An RCT META analysis based on the effect of tai chi exercise therapy on the outcome of elderly patients with moderate-to-severe sleep disorders-a systematic review study. Heliyon. (2024) 10:e24085. doi: 10.1016/j.heliyon.2024.e24085
79. Kang SJ, Leroux A, Guo W, Dey D, Strippoli M-PF, Di J, et al. Integrative modeling of accelerometry-derived sleep, physical activity, and circadian rhythm domains with current or remitted major depression. JAMA Psychiatry. (2024) 81:911–8. doi: 10.1001/jamapsychiatry.2024.1321
Keywords: older adults, physical activity, sleep quality, depression, anxiety
Citation: Yuan Y, Huang W, Hu C and Zhang W (2025) The interaction of physical activity and sleep quality with depression and anxiety in older adults. Front. Public Health 13:1674459. doi: 10.3389/fpubh.2025.1674459
Received: 28 July 2025; Accepted: 07 October 2025;
Published: 23 October 2025.
Edited by:
Alberto Sardella, University of Catania, ItalyReviewed by:
Kannadhasan Suriyan, Study World College of Engineering, IndiaSakchai Srisuk, Nakhon Phanom University, Thailand
Copyright © 2025 Yuan, Huang, Hu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenying Huang, aHVhbmd3ZW55aW5nNjZAMTYzLmNvbQ==; Chang Hu, aHVjaGFuZ0BqeG51LmVkdS5jbg==
 Yuqing Yuan
Yuqing Yuan Wenying Huang*
Wenying Huang* Chang Hu
Chang Hu Wen Zhang
Wen Zhang