- 1Department of Dermatology, Fourth Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin, China
- 2Department of Internal Medicine, Heilongjiang Academy of Traditional Chinese Medicine, Harbin, China
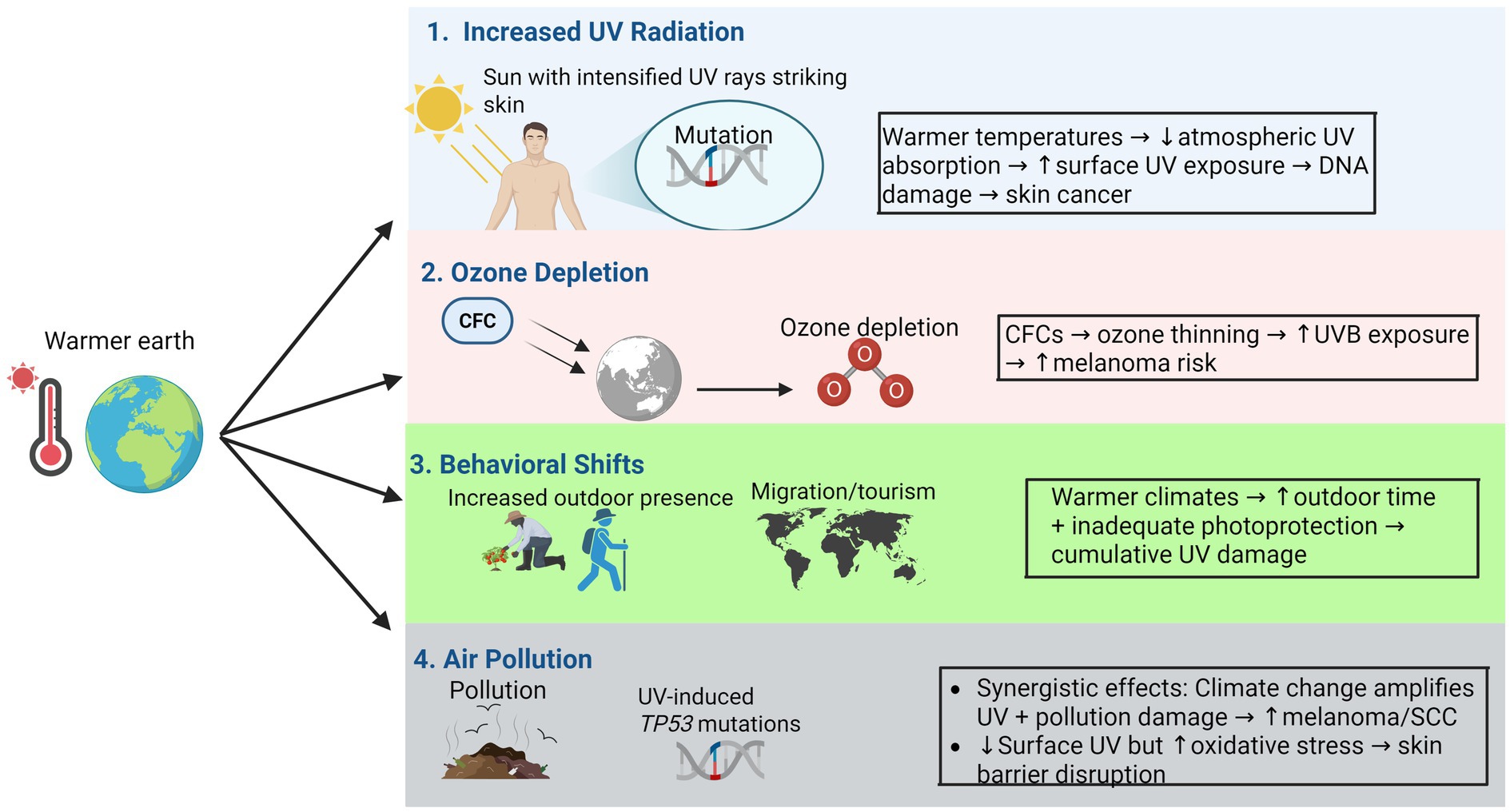
Climate change is increasingly recognized as a major public health challenge with wide-ranging effects on health conditions, including skin cancer. Rising global temperatures and heightened ultraviolet (UV) radiation intensity due to ozone depletion are contributing to a significant increase in skin cancer cases worldwide. This review explores the impact of altered UV radiation levels, behavioral shifts, and environmental factors on vulnerable populations in relation to the connection between climate change and rising skin cancer incidence. This relationship is further complicated by several paradoxes involving human behavior, ozone layer recovery, and socioeconomic factors. The discussion focuses on the mechanisms linking climate change to higher skin cancer rates, particularly the roles of UV radiation exposure, increased temperatures, and ozone layer depletion. These environmental changes disproportionately affect vulnerable groups, such as children, the older adults, and populations in high-risk geographic regions. To mitigate the growing burden of skin cancer associated with climate change, public health strategies including sun safety education, early detection programs, and international climate policies must be prioritized. Predicting skin cancer incidence rates depends on current and past sun protection behaviors and preventive measures. This review underscores the need for a coordinated global response to climate change and its impact on skin cancer, emphasizing prevention, early diagnosis, and effective treatment.
1 Introduction
Global climate change, driven by human activities, profoundly impacts ecosystems and human health, including altering disease patterns (1). Of particular urgency is the documented relationship between climate change and rising incidence rates of preventable cancers, most notably cutaneous melanoma and keratinocyte cancers (basal cell and squamous cell carcinoma (SCC)) (2). Skin cancer, one of the most common malignancies globally, primarily stems from excessive ultraviolet (UV) radiation exposure, which induces DNA damage in epidermal cells, particularly keratinocytes and melanocytes (3). Alarmingly, global temperature elevations correlate strongly with intensified solar UV radiation reaching the Earth’s surface, thereby amplifying skin cancer risks in UV-vulnerable regions such as equatorial zones and high-altitude areas (4).
Epidemiological data reveal a marked increase in skin cancer incidence across regions experiencing pronounced climatic alterations. For example, a longitudinal study in Scandinavia reported a > 4% annual increase in melanoma incidence over the past two decades, correlating with prolonged summer seasons and more frequent heatwaves (5). Warmer climates lead to more outdoor activities and lifestyle changes, which inadvertently increase exposure to higher UV levels (6). Regions like Scandinavia and northern Canada, historically protected by low traditional sun exposure profiles such as shorter summers and lower UV indices, now report rising cases as climate patterns, specifically, polar-amplified warming and shifting jet streams alter these patterns, leading to extended periods of high solar irradiance (7). This mini-review examines the multifaceted relationship between climate change and skin cancer epidemiology, focusing on the mechanisms of UV radiation, ozone depletion, and temperature-induced behavioral changes. Furthermore, it highlights disproportionately affected high-risk groups and synthesizes current evidence to inform targeted prevention strategies and adaptive public health policies.
2 Effects of climate change factors on skin cancer
UV radiation induces direct DNA damage through the formation of cyclobutane pyrimidine dimers (CPDs) and 6–4 photoproducts, which, if not adequately repaired, lead to characteristic UV-signature mutations such as C → T and CC → TT transitions. These mutations drive cutaneous carcinogenesis by disrupting key oncogenes and tumor suppressor genes, resulting primarily in basal cell carcinoma (BCC), SCC, and melanoma (8, 9). While BCC typically exhibits slow growth and local invasiveness, SCC possesses a greater potential for metastasis if left untreated. Melanoma, although less common, is responsible for the majority of skin cancer-related mortality due to its highly aggressive behavior and propensity for early dissemination (10, 11).
2.1 Increased ultraviolet radiation
The relationship between UV exposure and skin cancer is complex, involving various factors such as the intensity and duration of exposure, geographical location, and individual susceptibility. While climate change does not directly generate UV radiation, it exacerbates exposure through indirect mechanisms. Warmer atmospheric conditions reduce UV absorption capacity, particularly in equatorial regions, allowing more solar radiation to reach terrestrial surfaces (12). Concurrently, shifting weather patterns prolong sunny periods, such as extended summer months (March to October in temperate regions) with earlier sunrises and later sunsets, while higher temperatures (consistently exceeding 25 °C) encourage prolonged outdoor activities during peak daylight hours, both significantly extending UV exposure duration (13). A review on UV-induced immunosuppression discusses how UV exposure can down-regulate immune responses, thereby increasing the risk of skin cancer. UV radiation induces localized and systemic immunosuppression by modulating cytokine production and activating regulatory T cells, which diminishes the immune system’s ability to recognize and eliminate UV-damaged cells, thereby increasing skin cancer risk (14). Furthermore, the role of UV radiation in skin carcinogenesis is underscored by its ability to cause genetic mutations and promote the unregulated proliferation of skin cells, as discussed in a comprehensive review on the subject. UV radiation induces signature mutations, such as C → T and CC → TT transitions, primarily in tumor suppressor genes like TP53 in squamous cell carcinoma and PTCH1 in basal cell carcinoma, which disrupt apoptosis and promote uncontrolled cellular proliferation, as detailed in a comprehensive review on UV-induced skin carcinogenesis (15). The Stockholm public health cohort study explored the association between skin cancer and various UVR indicators finding significant associations with skin cancer risk (16). These findings underscore the multifaceted nature of UV radiation’s impact on skin cancer development and highlight the need for effective prevention strategies, including public education and behavioral modifications to reduce UV exposure.
2.2 Stratospheric ozone depletion
The Montreal Protocol, an international treaty signed by 197 countries, has been instrumental in phasing out the production of ozone-depleting substances. This treaty has not only contributed to the gradual recovery of the ozone layer, a projected return of mid-latitude and polar ozone levels to 1980 values by the mid-21st century but also played a role in mitigating climate change, as many of the substances controlled under the protocol (chlorofluorocarbons (CFCs) and hydrochlorofluorocarbons (HCFCs)) are also potent greenhouse gases with a global warming potential thousands of times greater than carbon dioxide. The stratospheric ozone layer, absorbing ~90% of harmful UV radiation, has been critically degraded by CFCs despite the Montreal Protocol’s regulatory success (17–19). Persistent ozone holes over polar regions permit heightened UV penetration, disproportionately affecting sparsely populated Arctic/Antarctic zones and mid-latitude countries. However, the path to ozone recovery is subject to a complex paradox where climate change can alter stratospheric temperatures and wind patterns, potentially delaying the restoration of protective ozone layers in some regions and prolonging elevated UV exposure risks. Australia exemplifies this crisis, where ozone depletion synergizes with geographic factors to yield the world’s highest skin cancer prevalence (20, 21). Notably, delayed ozone layer recovery prolongs UV exposure even in temperate regions, escalating risks for populations unadapted to intense solar radiation (22).
2.3 Global warming and altered ultraviolet radiation patterns
The interactive effects of stratospheric ozone depletion and climate change further complicate the scenario. Climate change can influence the dynamics of ozone depletion, while ozone depletion itself can affect climate patterns. These interlinking effects have implications for air quality, ecosystems, and human health. The Environmental Effects Assessment Panel of the Montreal Protocol has been evaluating these complex interactions, emphasizing the importance of continued monitoring and research to understand the full scope of these environmental changes (4).
Global warming has become an important environmental issue, reshaping the distribution of ultraviolet radiation through disrupted weather systems. Extended summers and intensified heatwaves prolong high-UV exposure windows, while orbital and atmospheric alterations redistribute solar radiation geographically (23, 24). Urban heat islands, intensified by climate change, further elevate risks in cities through dual temperature and UV spikes (25). Moreover, the interaction between increased environmental temperatures and UV radiation may further complicate the risk factors for skin cancer. Elevated temperatures can enhance the effects of UV radiation on the skin, accelerating photoaging and increasing the likelihood of photocarcinogenesis. Studies have shown that higher environmental temperatures can influence the biological effects of UV radiation, potentially leading to more severe skin damage, such as deep tissue inflammation and accelerated photoaging, and a higher incidence of skin cancer (26).
2.4 Shifting population demographics and increased migration
As climate change progresses, it can lead to shifts in population distributions due to factors such as rising sea levels, increased frequency of extreme weather events, and changes in agricultural productivity. These shifts can, in turn, affect the exposure of populations to UV radiation, a major risk factor for skin cancer. Migrants from low-UV regions like northern latitudes to sun-intensive areas often lack protective behaviors like sunscreen use, increasing susceptibility to burns and cumulative damage (27). This adaptation gap, combined with limited awareness, drives abrupt rises in skin cancer incidence among relocated groups, highlighting the need for targeted education in migration corridors.
2.5 Climate change and behavioral shifts
Climate change fundamentally reshapes skin cancer epidemiology. Rising melanoma and non-melanoma skin cancer rates to elevated temperatures, extended summer seasons, and heightened UV radiation exposure (28, 29). Notably, geographic patterns of skin cancer risk are shifting—regions like Scandinavia and parts of Canada, traditionally considered low-risk due to limited sun exposure, now report increasing cases as populations face unfamiliar UV intensity levels. A seminal European study found melanoma spikes correlate strongly with increased solar radiation and unusually high summer temperatures, revealing new vulnerabilities in cooler climate populations (30). These studies highlighted the importance of understanding how climate change can influence human behavior, leading to increased health risks such as skin cancer.
Warmer climates promote outdoor lifestyles, inadvertently increasing UV exposure. Leisure activities such as hiking, cycling, and tourism along with urban recreation surge with rising temperatures, yet sun protection practices lag behind behavioral changes (31, 32). Northern populations, previously sheltered by colder climates, now engage in prolonged outdoor activities without established protective habits, accelerating photoaging and carcinogenesis (33, 34). Tourism exacerbates risks, as high-altitude destinations with thinner atmospheres and reflective snowscapes intensify UV damage, often overlooked by underprepared visitors (35–37).
Furthermore, public health efforts face a significant behavioral paradox (28) where climate change creates more pleasant and inviting weather that encourages extended outdoor activities, inadvertently increasing population-wide UV exposure. This creates a counterintuitive scenario where improved weather conditions, a perceived benefit of climate change, can ultimately lead to adverse health outcomes by undermining sun-protection messages. Effective public health campaigns must therefore navigate this paradox by promoting sun-safe practices within the context of an active outdoor lifestyle, rather than simply advising against outdoor activities.
2.6 The complex role of air pollution in ultraviolet exposure
Climate change paradoxically modulates UV-skin interactions through air pollution. While particulates scatter UV radiation, reducing surface levels, pollutants like black carbon and ozone directly damage skin via oxidative stress and inflammation (38, 39). Chronic exposure impairs collagen synthesis and epidermal integrity, synergizing with UV to elevate urban skin cancer rates (40). Wildfire-driven pollution surges, intensified by climate change, further threaten cities where heat islands concentrate both pollutants and outdoor activities (41). This dual exposure creates a novel risk axis, demanding integrated mitigation strategies (Figure 1).
3 New research findings on the link between climate change and skin cancer
3.1 Innovative sun protection technologies
While climate change amplifies UV exposure risks, parallel technological breakthroughs are redefining photoprotection strategies. The effectiveness of sun protection methods, including the use of sunscreens, protective clothing, and behavioral changes, has been the subject of extensive research.
3.1.1 Next-generation sunscreens
Next-generation sunscreens represent significant advancements over traditional formulations, offering superior, longer-lasting protection characterized by high efficacy, providing SPF 50 + with broad-spectrum (UVA/UVB) coverage, enhanced durability, such as 8-h photostability and water resistance to improve compliance during prolonged outdoor exposure, and improved formulations that incorporate advanced filters (Tinosorb S, Mexoryl XL) and antioxidant complexes (vitamin C, ferulic acid) to counteract oxidative stress and deliver more comprehensive protection against photodamage.
3.1.2 Advanced textiles and wearable sensors
Sun-protective clothing with ultraviolet protection factors (UPF) exceeding 50 offers reliable, chemical-free protection. Wearable UV sensors provide real-time, personalized exposure monitoring, alerting users to potential overexposure risks and empowering informed behavioral modifications (42–44). Sunscreens are a widely used form of sun protection, and their effectiveness in preventing skin cancer has been supported by evidence from randomized controlled trials. For instance, a study conducted in Australia demonstrated that the regular application of broad-spectrum sunscreen could reduce the risk of developing cutaneous SCC and melanoma, although it did not significantly impact the incidence of BCC. This finding underscores the importance of using sunscreen as part of a comprehensive sun protection strategy (45).
3.2 Artificial intelligence and early detection
Artificial intelligence (AI) and machine learning are transforming dermatology through enhanced skin cancer detection capabilities. These technologies enable earlier and more accurate identification of malignant lesions, particularly valuable in regions with limited access to dermatologists (46). AI powered tools allow users to self-monitor suspicious skin changes, providing early warnings of potential malignancies. Developing predictive algorithms that assess skin cancer risk by analyzing genetic predispositions alongside lifestyle and environmental exposure factors is being implemented (32, 47). This approach promises more personalized prevention strategies and targeted screening programs, ensuring high-risk individuals receive timely interventions and education about their specific risk profiles.
3.3 Emerging skin cancer treatment options
Immunotherapy, particularly checkpoint inhibitors, has revolutionized melanoma treatment, improving survival rates for advanced-stage patients (48). Targeted therapies attack specific genetic mutations, offering precision over traditional chemotherapy. Photodynamic therapy (PDT) shows particular promise for treating various skin cancers (49). This approach combines light-activated photosensitizing agents with targeted illumination to selectively destroy malignant cells while sparing healthy tissue. Current research explores expanding PDT applications from superficial tumors to deeper or larger malignancies.
4 Interventions to mitigate climate impact on skin cancer-taking references from case studies
While skin cancer is largely preventable through sun safety measures, climate change may exacerbate UV exposure risks, necessitating enhanced prevention and early detection strategies (50). To address these challenges, targeted interventions are essential, particularly for high-risk populations and regions facing unique environmental and socioeconomic vulnerabilities. Certain populations face elevated vulnerability to climate change-driven skin cancer risks. These include residents of high-UV regions (equatorial zones, high-altitude areas) and socioeconomically disadvantaged groups with limited access to healthcare, education, and protective resources (sunscreen, shade) (51). Prolonged sunlight exposure due to rising temperatures further increases UV risks in these regions (52). Low-income communities often lack healthcare access, delaying skin cancer screenings and worsening outcomes. Age also influences susceptibility: children’s sensitive skin and outdoor activity increase damage risk, while the older adults accumulate lifetime UV damage (53). Migrant populations relocating from low- to high-UV areas face heightened sunburn risk due to unfamiliarity with sun protection.
Australia exemplifies climate change’s impact on skin cancer. Its high baseline UV exposure has intensified due to ozone layer depletion from CFCs (54). With the world’s highest skin cancer incidence (affecting ~50% of Australians), public health strategies like the SunSmart campaign (since 1981) promote sunscreen use, protective clothing, and shade-seeking during peak UV hours (55). Despite reducing melanoma rates in younger cohorts, climate change prolongs UV exposure, challenging prevention efforts. Moreover, northern countries (Sweden, Finland) report increasing skin cancer rates linked to warmer summers and extended UV exposure (56). Previously low-risk due to cooler climates, these regions now face heightened risk from heatwaves and cultural shifts toward sunbathing. Public health campaigns emphasize sunscreen use and screenings, targeting fair-skinned individuals and those with family histories (57). In addition, Urban heat islands (elevated temperatures from infrastructure and scarce greenery) amplify UV exposure in cities like Los Angeles and New York (58). Outdoor workers (construction crews) face reflected UV radiation, while tanning bed use persists despite known risks. Air pollution exacerbates skin damage via free radical formation (59). Mitigation includes sun safety education, free screenings, and urban green spaces (60).
These case studies demonstrate that the impact of climate change on skin cancer is profoundly mediated by a socioeconomic paradox (61). Lower socioeconomic status populations often have less recreational sun exposure but experience higher rates of occupational UV exposure and later-stage skin cancer diagnoses. This disparity stems from barriers such as lack of access to sunscreen, protective clothing, shade, and healthcare, as well as less sun safety education. This paradox was exacerbated during the COVID-19 pandemic, where reduced healthcare access disproportionately affected these groups. As climate change increases UV exposure risks, it will likely widen these existing health inequities, as vulnerable populations have the fewest resources to adapt to environmental changes. These cases highlight the need for region-specific strategies to address unique local challenges and reduce UV radiation and pollutant exposure, mitigating future global skin cancer burdens.
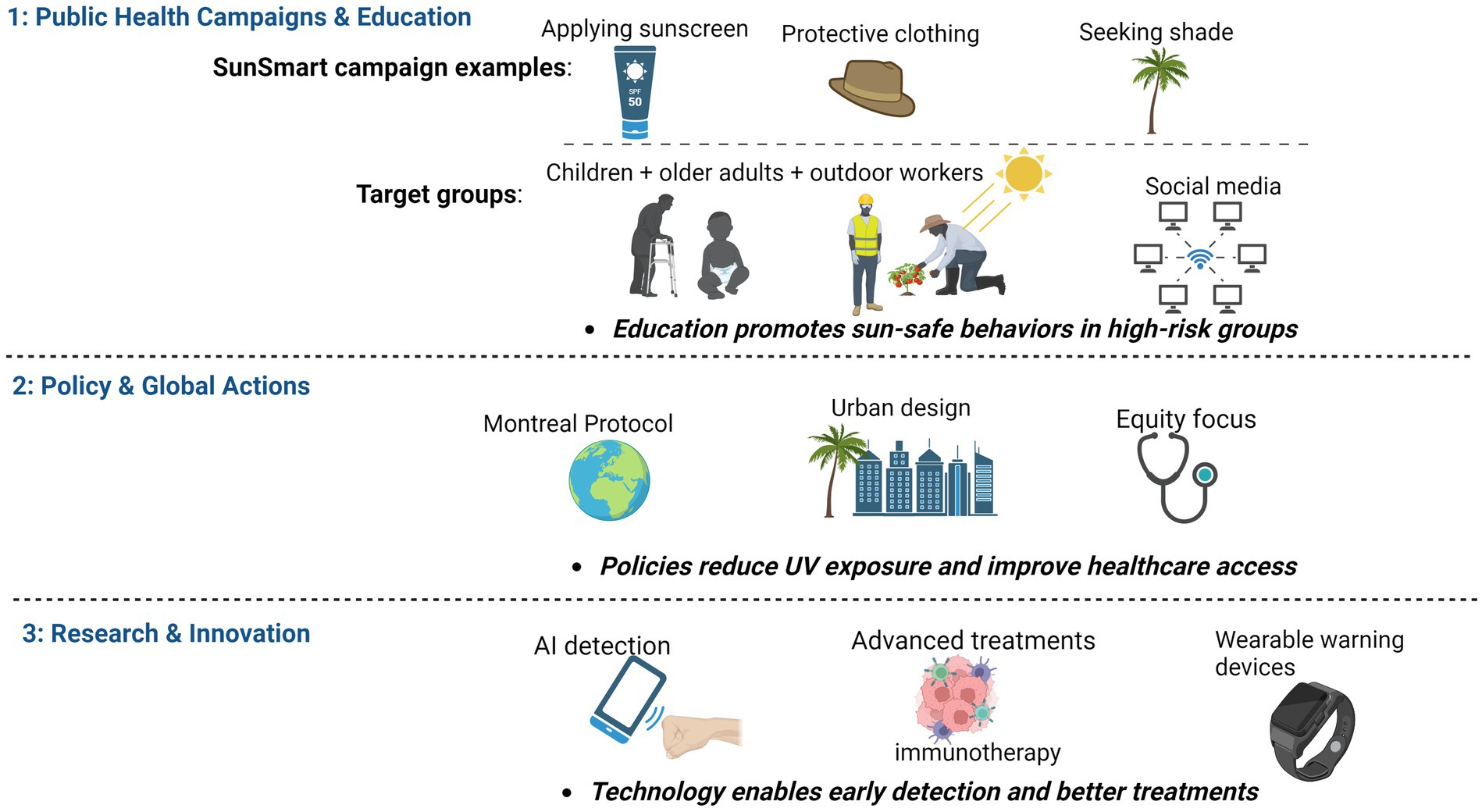
5 Methods of reducing skin cancer incidence resulting from climate change
Public health experts and policymakers must address climate change’s contribution to rising skin cancer incidence. While large-scale environmental changes require systemic action, effective strategies exist to mitigate risk, promote prevention, and improve outcomes. Key approaches include public health campaigns, international policy actions, and research innovations in detection and treatment.
5.1 Public health campaigns and education
Public health campaigns emphasizing UV radiation dangers and sun protection are crucial. Promoting sun-safe behaviors like sunscreen use, protective clothing, and seeking shade during peak sunlight is essential, especially as climate change increases temperatures and sunlight exposure. Global and national health organizations, such as the WHO, should implement tailored campaigns for high-risk groups like children, the older adults, and outdoor workers. Messages should be disseminated through TV, social media, and community programs, addressing risks from tanning beds. Schools, summer camps, and health centers play a vital role in educating families about sun protection. Employers should provide free or subsidized sunscreen and protective gear for outdoor workers and incorporate sun safety into workplace wellness programs (62).
5.2 Policy actions and international cooperation
International cooperation and policy changes are essential to address climate change and reduce UV radiation exposure. Policies targeting carbon emissions, ozone layer protection, and environmental degradation can mitigate skin cancer risks (63). The Montreal Protocol, which reduced ozone-depleting CFCs, remains a key agreement. Continued ozone layer protection and efforts to reduce greenhouse gas emissions are critical (64). Governments should promote renewable energy, improve air quality, and implement urban design strategies like shaded areas and green roofs to reduce sunlight exposure (65, 66). At the national level, policies should target high-risk populations, such as those living in regions with high UV exposure, by improving access to skin cancer prevention tools and early detection services. These policies should target high-risk populations by improving access to prevention tools and early detection services, such as subsidized sunscreen and free screenings. Collaboration with healthcare providers is necessary to ensure culturally appropriate materials for migrant populations.
5.3 Research and innovation in skin cancer detection and treatment
Research and innovation in early detection, treatment, and prevention are vital to reduce the impact of climate change on skin cancer. Advances in diagnostic tools and treatment methods are needed to address rising incidence (67). Technologies like dermoscopy and AI-powered mobile applications improve skin cancer detection, enabling early medical intervention (68). Routine screenings, particularly for vulnerable communities, enhance early diagnosis and treatment outcomes (69). Treatment options, such as immunotherapy and targeted therapies, have advanced significantly, improving outcomes for melanoma patients. Research must prioritize developing more effective treatments and ensuring global access to these technologies. Innovations in preventive technologies, like sun-protective fabrics and wearable UV monitors, can improve sun safety practices (Figure 2).
6 Conclusion
Climate change is intensifying skin cancer risks, requiring a multifaceted response. Rising temperatures and UV levels are increasing skin cancer incidence, even in previously low-risk regions. While advancements in diagnostics, sun protection, and treatments are promising, they are insufficient alone. Comprehensive public health strategies are crucial, including sun safety education, climate action to curb UV exposure, and better access to early detection and care. Factors like ozone depletion, shifting UV patterns, and climate-driven migration further complicate the issue. This review discusses public health campaigns and education as key mitigation strategies. This paradox explains why such campaigns are necessary yet often challenging, they must motivate individuals to act for a collective, statistical good. This review directly addresses this in sections on behavioral shifts and migration, describing how warmer climates promote outdoor lifestyles and how migrants may lack protective behaviors. The paradox lies in the fact that the appealing weather created by climate change counterintuitively increases the risk it necessitates protecting against. Collaboration among public health officials, policymakers, and researchers is essential to protect vulnerable populations and reduce the skin cancer burden. Integrating prevention into global health initiatives is urgent. Through innovation, policy reform, and education, we can mitigate climate change’s health impacts and strive for a future with reduced cancer risks and improved public health outcomes.
Author contributions
LW: Conceptualization, Writing – original draft, Writing – review & editing. YC: Writing – review & editing. JL: Writing – review & editing. XY: Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Youth Talent Cultivation Program of the China Association of Chinese Medicine (202557–011).
Acknowledgments
Figures were Created in https://BioRender.com.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AI, Artificial Intelligence; BCC, Basal Cell Carcinoma; CC>TT, Cytosine-Cytosine to Thymine-Thymine (mutation); CFCs, Chlorofluorocarbons; C > T, Cytosine to Thymine (mutation); CPDs, Cyclobutane Pyrimidine Dimers; HCFCs, Hydrochlorofluorocarbons; PAHs, Polycyclic Aromatic Hydrocarbons; PDT, Photodynamic Therapy; ROS, Reactive Oxygen Species; SCC, Squamous Cell Carcinoma; SPF, Sun Protection Factor; UVR/UV, Ultraviolet Radiation/Ultraviolet; UPF, Ultraviolet Protection Factor; WHO, World Health Organization; 6-4PPs, 6–4 Photoproducts.
References
1. Agache, I, Hernandez, ML, Radbel, JM, Renz, H, and Akdis, CA. An overview of climate changes and its effects on health: from mechanisms to one health. J Allergy Clin Immunol Pract. (2025) 13:253–64. doi: 10.1016/j.jaip.2024.12.025
2. Yu, P, Xu, R, Yang, Z, Ye, T, Liu, Y, Li, S, et al. Cancer and ongoing climate change: who are the Most affected? ACS Environ Au. (2023) 3:5–11. doi: 10.1021/acsenvironau.2c00012
3. Pfeifer, GP. Mechanisms of UV-induced mutations and skin cancer. Genome Instab Dis. (2020) 1:99–113. doi: 10.1007/s42764-020-00009-8
4. Barnes, PW, Robson, TM, Neale, PJ, Williamson, CE, Zepp, RG, Madronich, S, et al. Environmental effects of stratospheric ozone depletion, UV radiation, and interactions with climate change: UNEP environmental effects assessment panel, update 2021. Photochem Photobiol Sci. (2022) 21:275–301. doi: 10.1007/s43630-022-00176-5
5. Wang, M, Gao, X, and Zhang, L. Recent global patterns in skin cancer incidence, mortality, and prevalence. Chin Med J. (2025) 138:185–92. doi: 10.1097/CM9.0000000000003416
6. Umar, SA, and Tasduq, SA. Ozone layer depletion and emerging public health concerns - an update on epidemiological perspective of the ambivalent effects of ultraviolet radiation exposure. Front Oncol. (2022) 12:866733. doi: 10.3389/fonc.2022.866733
7. Roro, AG, Terfa, MT, Solhaug, KA, Tsegaye, A, Olsen, JE, and Torre, S. The impact of UV radiation at high altitudes close to the equator on morphology and productivity of pea (Pisum sativum) in different seasons. South Afr J Bot. (2016) 106:119–28. doi: 10.1016/j.sajb.2016.05.011
8. Umar, SA, and Tasduq, SA. Integrating DNA damage response and autophagy signalling axis in ultraviolet-B induced skin photo-damage: a positive association in protecting cells against genotoxic stress. RSC Adv. (2020) 10:36317–36. doi: 10.1039/D0RA05819J
9. Fania, L, Didona, D, Morese, R, Campana, I, Coco, V, Di Pietro, FR, et al. Basal cell carcinoma: from pathophysiology to novel therapeutic approaches. Biomedicine. (2020) 8:449. doi: 10.3390/biomedicines8110449
10. Tahir, M, Naeem, A, Malik, H, Tanveer, J, Naqvi, RA, and Lee, SW. DSCC_Net: multi-classification deep learning models for diagnosing of skin Cancer using Dermoscopic images. Cancers (Basel). (2023) 15:2179. doi: 10.3390/cancers15072179
11. Zhang, X, Li, H, Liu, C, and Yuan, X. Role of ROS-mediated autophagy in melanoma (review). Mol Med Rep. (2022) 26:303. doi: 10.3892/mmr.2022.12819
12. Bernhard, GH, Neale, RE, and Barnes, PW. Environmental effects of stratospheric ozone depletion, UV radiation and interactions with climate change: UNEP environmental effects assessment panel, update 2019. Photochem Photobiol Sci. (2020) 19:542–84. doi: 10.1039/d0pp90011g
13. Knight, T, Price, S, Bowler, D, Hookway, A, King, S, Konno, K, et al. How effective is ‘greening’ of urban areas in reducing human exposure to ground-level ozone concentrations, UV exposure and the ‘urban heat island effect’? An updated systematic review. Environ Evid. (2021) 10:12. doi: 10.1186/s13750-021-00226-y
14. Hart, PH, and Norval, M. Ultraviolet radiation-induced immunosuppression and its relevance for skin carcinogenesis. Photochem Photobiol Sci. (2018) 17:1872–84. doi: 10.1039/c7pp00312a
15. Mancebo, SE, and Wang, SQ. Skin cancer: role of ultraviolet radiation in carcinogenesis. Rev Environ Health. (2014) 29:265–73. doi: 10.1515/reveh-2014-0041
16. Ivert, LU, Dal, H, Rodvall, Y, and Lindelöf, B. Analysis of the Stockholm public health cohort: exploring how ultraviolet radiation and other factors associate with skin Cancer. J Skin Cancer. (2024) 2024:7142055. doi: 10.1155/2024/7142055
17. Birmpili, T. Montreal protocol at 30: the governance structure, the evolution, and the Kigali amendment. Compt Rendus Geosci. (2018) 350:425–31. doi: 10.1016/j.crte.2018.09.002
18. Gareau, BJ. A critical review of the successful CFC phase-out versus the delayed methyl bromide phase-out in the Montreal protocol. Int Environ Agreements Polit Law Econ. (2010) 10:209–31. doi: 10.1007/s10784-010-9120-z
19. DasSarma, P, and DasSarma, S. Survival of microbes in earth’s stratosphere. Curr Opin Microbiol. (2018) 43:24–30. doi: 10.1016/j.mib.2017.11.002
20. Dexter, BR, King, R, Parisi, AV, Harrison, SL, Konovalov, DA, and Downs, NJ. Keratinocyte skin cancer risks for working school teachers: scenarios and implications of the timing of scheduled duty periods in Queensland, Australia. J Photochem Photobiol B Biol. (2020) 213:112046. doi: 10.1016/j.jphotobiol.2020.112046
21. Petkov, B, Vitale, V, Di Carlo, P, Mazzola, M, Lupi, A, Diémoz, H, et al. The 2020 Arctic ozone depletion and signs of its effect on the ozone column at lower latitudes. Bull Atmos Sci Technol. (2021) 2:8. doi: 10.1007/s42865-021-00040-x
22. Jindal, M, Kaur, M, Nagpal, M, Singh, M, Aggarwal, G, and Dhingra, GA. Skin Cancer management: current scenario and future perspectives. Curr Drug Saf. (2023) 18:143–58. doi: 10.2174/1574886317666220413113959
23. Neale, RE, Barnes, PW, Robson, TM, Neale, PJ, Williamson, CE, Zepp, RG, et al. Environmental effects of stratospheric ozone depletion, UV radiation, and interactions with climate change: UNEP environmental effects assessment panel, update 2020. Photochem Photobiol Sci. (2021) 20:1–67. doi: 10.1007/s43630-020-00001-x
24. Tardif, D, Toumoulin, A, Fluteau, F, Donnadieu, Y, Le Hir, G, Barbolini, N, et al. Orbital variations as a major driver of climate and biome distribution during the greenhouse to icehouse transition. Sci Adv. (2021) 7:eabh2819. doi: 10.1126/sciadv.abh2819
25. Li, Y, Schubert, S, Kropp, JP, and Rybski, D. On the influence of density and morphology on the urban Heat Island intensity. Nat Commun. (2020) 11:2647. doi: 10.1038/s41467-020-16461-9
26. de Vries, E, Arnold, M, Altsitsiadis, E, Trakatelli, M, Hinrichs, B, Stockfleth, E, et al. Potential impact of interventions resulting in reduced exposure to ultraviolet (UV) radiation (UVA and UVB) on skin cancer incidence in four European countries, 2010-2050. Br J Dermatol. (2012) 167:53–62. doi: 10.1111/j.1365-2133.2012.11087.x
27. Dayrit, JF, Sugiharto, A, Coates, SJ, Lucero-Prisno, DE 3rd, Davis, MDD, and Andersen, LK. Climate change, human migration, and skin disease: is there a link? Int J Dermatol. (2022) 61:127–38. doi: 10.1111/ijd.15543
28. Leiter, U, and Garbe, C. Epidemiology of melanoma and nonmelanoma skin cancer--the role of sunlight. Adv Exp Med Biol. (2008) 624:89–103. doi: 10.1007/978-0-387-77574-6_8
29. Dennis, LK. Cumulative sun exposure and melanoma in a population-based case-control study: does sun sensitivity matter? Cancers (Basel). (2022) 14:1008. doi: 10.3390/cancers14041008
30. Alvim- Ferraz, MCM, Sousa, SIV, Martins, FG, and Ferraz, MP. Tropospheric and stratospheric ozone: scientific history and shifts in early perspectives regarding the impact on human health. Atmos. (2024) 15:1504. doi: 10.3390/atmos15121504
31. Laschewski, G, and Matzarakis, A. Weather-related human outdoor behavior with respect to solar ultraviolet radiation exposure in a changing climate. Atmos. (2022) 13:1183. doi: 10.3390/atmos13081183
32. Jones, OT, Matin, RN, van der Schaar, M, Prathivadi Bhayankaram, K, Ranmuthu, CKI, Islam, MS, et al. Artificial intelligence and machine learning algorithms for early detection of skin cancer in community and primary care settings: a systematic review. Lancet Digit Health. (2022) 4:e466–76. doi: 10.1016/S2589-7500(22)00023-1
33. Jay, O, Capon, A, Berry, P, Broderick, C, de Dear, R, Havenith, G, et al. Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet. (2021) 398:709–24. doi: 10.1016/S0140-6736(21)01209-5
34. Adamson, AS, Welch, H, and Welch, HG. Association of UV radiation exposure, diagnostic scrutiny, and melanoma incidence in US counties. JAMA Intern Med. (2022) 182:1181–9. doi: 10.1001/jamainternmed.2022.4342
35. Mikati, T, Taur, Y, Seo, SK, and Shah, MK. International travel patterns and travel risks of patients diagnosed with cancer. J Travel Med. (2013) 20:71–7. doi: 10.1111/jtm.12013
36. Godovykh, M, and Ridderstaat, J. Health outcomes of tourism development: a longitudinal study of the impact of tourism arrivals on residents’ health. J Destin Mark Manag. (2020) 17:100462. doi: 10.1016/j.jdmm.2020.100462
37. Zerefos, C, Fountoulakis, I, Eleftheratos, K, and Kazantzidis, A. Long-term variability of human health-related solar ultraviolet-B radiation doses for the 1980s to the end of the 21st century. Physiol Rev. (2023) 103:1789–826. doi: 10.1152/physrev.00031.2022
38. Kocifaj, M, and Barentine, JC. Air pollution mitigation can reduce the brightness of the night sky in and near cities. Sci Rep. (2021) 11:14622. doi: 10.1038/s41598-021-94241-1
39. Dombrovsky, LA, Solovjov, VP, and Webb, BW. Effect of ground-based environmental conditions on the level of dangerous ultraviolet solar radiation. J Quant Spectrosc Radiat Transf. (2022) 279:108048. doi: 10.1016/j.jqsrt.2021.108048
40. Bocheva, G, Slominski, RM, and Slominski, AT. Environmental air pollutants affecting skin functions with systemic implications. Int J Mol Sci. (2023) 24:10502. doi: 10.3390/ijms241310502
41. Chowdhury, A, Nosoudi, N, Karamched, S, Parasaram, V, and Vyavahare, N. Polyphenol treatments increase elastin and collagen deposition by human dermal fibroblasts; implications to improve skin health. J Dermatol Sci. (2021) 102:94–100. doi: 10.1016/j.jdermsci.2021.03.002
42. Patel, SP, and Chien, AL. Sun protective clothing and sun avoidance: The Most critical components of Photoprotection in patients with melanoma. Dermatologic Surg. (2021) 47:333–7. doi: 10.1097/DSS.0000000000002794
43. Fernau, E, Ilyas, SM, and Ilyas, EN. The impact of routine laundering on ultraviolet protection factor (UPF) values for commercially available sun-protective clothing. Cureus. (2023) 15:e42256. doi: 10.7759/cureus.42256
44. Henning, AJ, Downs, N, and Vanos, JK. Wearable ultraviolet radiation sensors for research and personal use. Int J Biometeorol. (2022) 66:627–40. doi: 10.1007/s00484-021-02216-8
46. Nelson, CA, Pachauri, S, Balk, R, Miller, J, Theunis, R, Ko, JM, et al. Dermatologists’ perspectives on artificial intelligence and augmented intelligence - a cross-sectional survey. JAMA Dermatol. (2021) 157:871–4. doi: 10.1001/jamadermatol.2021.1685
47. Schreidah, CM, Gordon, ER, Adeuyan, O, Chen, C, Lapolla, BA, Kent, JA, et al. Current status of artificial intelligence methods for skin cancer survival analysis: a scoping review. Front Med (Lausanne). (2024) 11:1243659. doi: 10.3389/fmed.2024.1243659
48. Bagchi, S, Yuan, R, and Engleman, EG. Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Annu Rev Pathol. (2021) 16:223–49. doi: 10.1146/annurev-pathol-042020-042741
49. Allegra, A, Pioggia, G, Tonacci, A, Musolino, C, and Gangemi, S. Oxidative stress and photodynamic therapy of skin cancers: mechanisms, challenges and promising developments. Antioxidants (Basel). (2020) 9:448. doi: 10.3390/antiox9050448
50. Garbe, C, Forsea, AM, Amaral, T, Arenberger, P, Autier, P, Berwick, M, et al. Skin cancers are the most frequent cancers in fair-skinned populations, but we can prevent them. Eur J Cancer. (2024) 204:114074. doi: 10.1016/j.ejca.2024.114074
51. Watson, TPG, Tong, M, Bailie, J, Ekanayake, K, and Bailie, RS. Relationship between climate change and skin cancer and implications for prevention and management: a scoping review. Public Health. (2024) 227:243–9. doi: 10.1016/j.puhe.2023.12.003
52. Liu, Z, and Yu, L. Stay or leave? The role of air pollution in urban migration choices. Ecol Econ. (2020) 177:106780. doi: 10.1016/j.ecolecon.2020.106780
53. Raymond-Lezman, JR, and Riskin, S. Attitudes, behaviors, and risks of sun protection to prevent skin cancer amongst children, adolescents, and adults. Cureus. (2023) 15:e34934. doi: 10.7759/cureus.34934
54. Bernhard, GH, Bais, AF, Aucamp, PJ, Klekociuk, AR, Liley, JB, and McKenzie, RL. Stratospheric ozone, UV radiation, and climate interactions. Photochem Photobiol Sci. (2023) 22:937–89. doi: 10.1007/s43630-023-00371-y
55. Uchiyama, R, Spicer, R, and Muthukrishna, M. Cultural evolution of genetic heritability. Behav Brain Sci. (2021) 45:e152. doi: 10.1017/S0140525X21000893
56. Olsen, CM, Pandeya, N, Ragaini, BS, Neale, RE, and Whiteman, DC. International patterns and trends in the incidence of melanoma and cutaneous squamous cell carcinoma, 1989-2020. Br J Dermatol. (2024) 190:492–500. doi: 10.1093/bjd/ljad425
57. Thoonen, K, van Osch, L, Drittij, R, de Vries, H, and Schneider, F. A qualitative exploration of parental perceptions regarding children’s sun exposure, sun protection, and sunburn. Front Public Health. (2021) 9:596253. doi: 10.3389/fpubh.2021.596253
58. Matte, T, Lane, K, Tipaldo, JF, Barnes, J, Knowlton, K, Torem, E, et al. NPCC4: climate change and new York City’s health risk. Ann N Y Acad Sci. (2024) 1539:185–240. doi: 10.1111/nyas.15115
59. Ali, A, Khan, H, Bahadar, R, Riaz, A, and Asad, M. The impact of airborne pollution and exposure to solar ultraviolet radiation on skin: mechanistic and physiological insight. Environ Sci Pollut Res Int. (2020) 27:28730–6. doi: 10.1007/s11356-020-09280-4
60. Conte, S, Aldien, AS, Jette, S, LeBeau, J, Alli, S, Netchiporouk, E, et al. Skin Cancer prevention across the G7, Australia and New Zealand: a review of legislation and guidelines. Curr Oncol. (2023) 30:6019–40. doi: 10.3390/curroncol30070450
61. Grafanaki, K, Georgiou, S, and Stratigos, AJ. Solidarity and voluntarism amid the COVID-19 pandemic: skin Cancer screening for blood donors. Dermatol Pract Concept. (2021) 11:e2021080. doi: 10.5826/dpc.1103a80
62. Gui, H, Jia, JL, and Nord, KM. Strategies to improve access to photoprotection and sun safety for diverse socioeconomic communities. Arch Dermatol Res. (2024) 316:597. doi: 10.1007/s00403-024-03309-1
63. The Lancet, O. Climate change and skin cancer: urgent call for action. Lancet Oncol. (2023) 24:823. doi: 10.1016/S1470-2045(23)00348-0
64. Elavarasan, MR, Pugazhendhi, R, Irfan, M, Mihet-Popa, L, Khan, IA, and Campana, PE. State-of-the-art sustainable approaches for deeper decarbonization in Europe – an endowment to climate neutral vision. Renew Sust Energ Rev. (2022) 159:112204. doi: 10.1016/j.rser.2022.112204
65. Aboagye, PD, and Sharifi, A. Urban climate adaptation and mitigation action plans: a critical review. Renew Sust Energ Rev. (2024) 189:113886. doi: 10.1016/j.rser.2023.113886
66. Barriuso, F, and Urbano, B. Green roofs and walls design intended to mitigate climate change in urban areas across all continents. Sustainability. (2021) 13:2245. doi: 10.3390/su13042245
67. Soglia, S, Perez-Anker, J, Lobos Guede, N, Giavedoni, P, Puig, S, and Malvehy, J. Diagnostics using non-invasive Technologies in Dermatological Oncology. Cancers (Basel). (2022) 14:5886. doi: 10.3390/cancers14235886
68. Yan, AF, Chen, Z, Wang, Y, Campbell, JA, Xue, QL, Williams, MY, et al. Effectiveness of social needs screening and interventions in clinical settings on utilization, cost, and clinical outcomes: a systematic review. Health Equity. (2022) 6:454–75. doi: 10.1089/heq.2022.0010
Keywords: climate change, skin cancer, UV radiation, ozone depletion, sun protection
Citation: Wang L, Chi Y, Li J and Yuan X (2025) The impact of climate change on skin cancer incidence: mechanisms, vulnerabilities, and mitigation strategies. Front. Public Health. 13:1674975. doi: 10.3389/fpubh.2025.1674975
Edited by:
Arthit Phosri, Mahidol University, ThailandReviewed by:
Katerina Grafanaki, General University Hospital of Patras, GreeceCopyright © 2025 Wang, Chi, Li and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Li, bGlqaW5nMjAyNUB5ZWFoLm5ldA==; Xingxing Yuan, eXVhbnhpbmd4aW5nQGhsanVjbS5lZHUuY24=
 Lin Wang1
Lin Wang1 Xingxing Yuan
Xingxing Yuan