- School of Public Health, Fudan University, Shanghai, China
Purpose: Rehabilitation policies constitute a critical guiding framework for national and regional development. This study aims to use policy tools to analyze the specific content and structural characteristics of China’s rehabilitation-related policies from 2010 to 2023, and provide a new reference perspective for international rehabilitation policy research.
Materials and methods: A three-dimensional analytical framework of “policy tool type–policy theme characteristic–stakeholder” was developed. Data were drawn from nation-level policies on rehabilitation medical services issued by the State Council of the People’s Republic of China and the National Health Commission. Based on established inclusion and exclusion criteria, 41 valid policy documents were selected. NVivo (release 14.23.1) was used for four-level coding, and reliability and validity tests were conducted. Policy texts were first quantified, followed by descriptive analysis.
Results: A total of 298 codes were identified. Among policy tool types, environmental tools accounted for the highest proportion (58.05%), followed by supply-side tools (32.98%), while demand-side tools had the lowest proportion (9.06%). From the stakeholder perspective, provider organizations (42.95%) were the core target, followed by regulatory authorities (19.13%) and rehabilitation service recipients (19.80%). Clinical practitioners and the rehabilitation capital market each accounted for 9.06%, with most of the policies related to passive response-type policies.
Conclusion: China’s current rehabilitation medical service policies have insufficient use of supply-side and demand-side tools, and uneven policy coverage among stakeholders. The structural application of policy tools should be optimized, particularly by strengthening the role of demand-side policy tools.
1 Introduction
Rehabilitation is defined as the multidisciplinary and coordinated application of interventions to reduce physiological, psychological, and social functional impairments in individuals with illnesses, injuries, or disabilities (1). It primarily focuses on improving patients’ functional abilities following successful clinical treatment to support their continued daily living. Empirical evidence shows that rehabilitation is significantly cost-effective (2), enhances quality of life (3, 4), shortens hospital length of stay (5), lowers readmission rates (6, 7), and enhances occupational reintegration efficacy (8).
With the acceleration of global population aging and rapid development of medical technology, the demand for rehabilitation has increased rapidly in many countries and regions (9, 10). In response, developed countries in Europe and America have introduced numerous policies and legislative measures to promote the development of rehabilitation services (11, 12) and meet the growing needs of the population requiring rehabilitation services. As a developing country, China faces more complex challenges in this field. Between 1990 and 2019, the number of individuals requiring rehabilitation services in China increased from 268 million to 460 million, reflecting a 71.6% increase, ranking among the highest globally (13).
Although rehabilitation plays an increasingly important role in addressing health governance challenges (14), international research has primarily focused on rehabilitation practices (15, 16), technologies (17, 18), and outcomes (19, 20). Most rehabilitation policy analyses have examined policy implementation (21) or specific disease categories (22), lacking comprehensive analysis from a holistic perspective and systematic examination of policy structures. Policy tools, defined as the mechanisms through which governments formulate, evaluate, and implement policy alternatives, constitute a central domain in policy science (23) and serve as a critical analytical framework in public policy research (24). The selection and application of policy tools have a significantly influence on a government’s capacity to achieve its policy objectives (25). Each tool provides operational guidance for the implementation and regulation of government policies in a concise, actionable form (26).
In this study, we sought to bridge the current research gap by applying policy tools to examine existing rehabilitation medical service policies in China. We identified specific indicators for each analytical dimension of policy tools and explored the feasibility of cross-analysis between policy tools and stakeholders, thereby providing a new reference perspective for international rehabilitation policy research. It is important to note that the “quantitative analysis” in this study refers specifically to the process of converting non-numerical information such as policy texts into measurable numerical data, rather than the broader methodological distinction between quantitative and qualitative research.
2 Materials and methods
2.1 Information sources
This study systematically retrieved policy documents on rehabilitation services from the State Council Policy Repository. The primary search terms were “rehabilitation,” “rehabilitation medical services,” “rehabilitation medicine,” and “rehabilitation medical system.” The search covered policy documents issued between October 1, 2010, and October 1, 2023, by the State Council, the General Office of the State Council, and ministerial bodies under the State Council, including the National Health Commission, Ministry of Civil Affairs, National Healthcare Security Administration. To ensure thematic relevance and methodological validity, the initially identified policy corpus was subjected to rigorous screening using pre-established eligibility criteria, encompassing both inclusion and exclusion conditions:
2.1.1 Inclusion criteria
a. Documents containing substantive provisions directly related to rehabilitation service delivery mechanisms.
b. Nation-level tools (e.g., notices, decisions, and guidelines) issued through official State Council channels.
2.1.2 Exclusion criteria
a. Documents of low relevance, such as replies or inter-departmental forwarded letters.
b. Documents that only mention keywords without providing substantive content.
c. Duplicate documents.
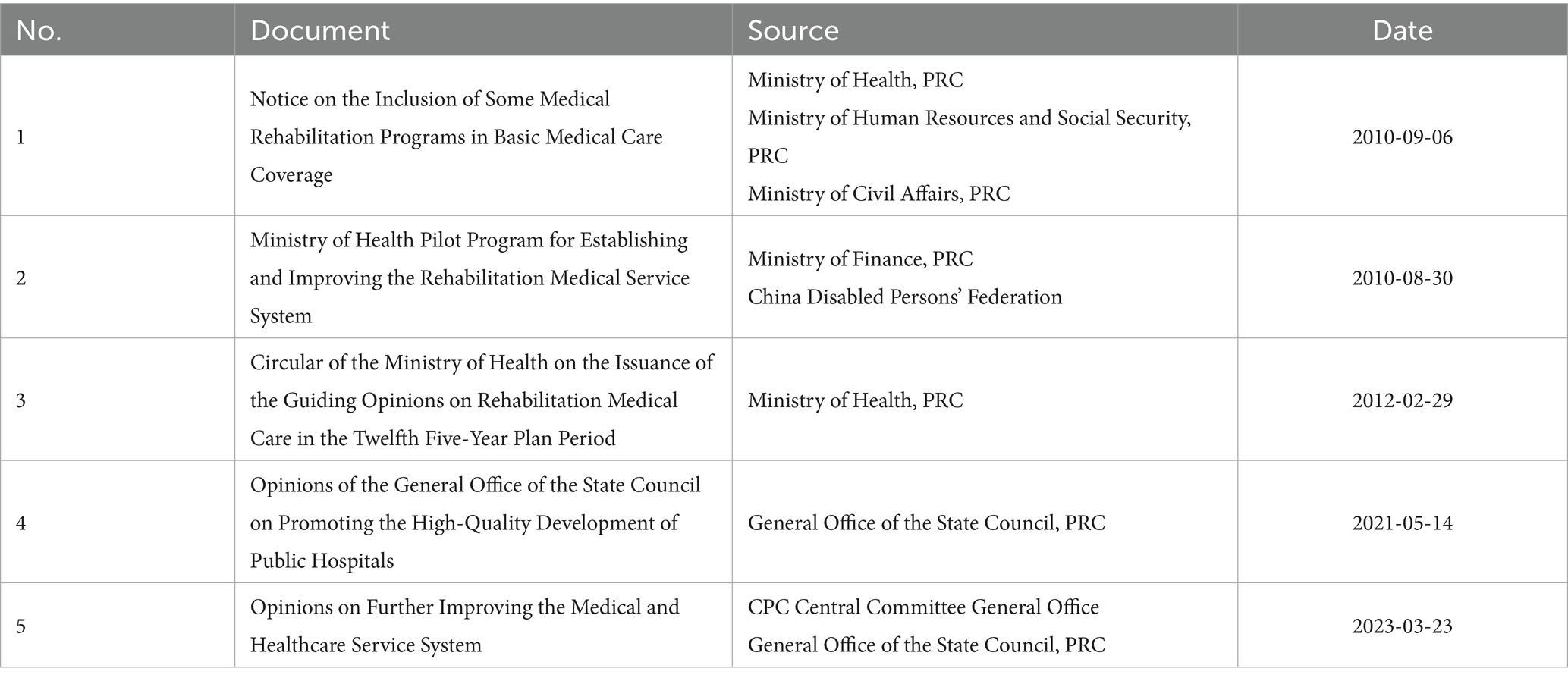
Based on these criteria, a total of 41 policy documents met the eligibility requirements and were included in the Rehabilitation Medical Service Policy Database. Representative examples are provided in Table 1.
2.2 Textual coding
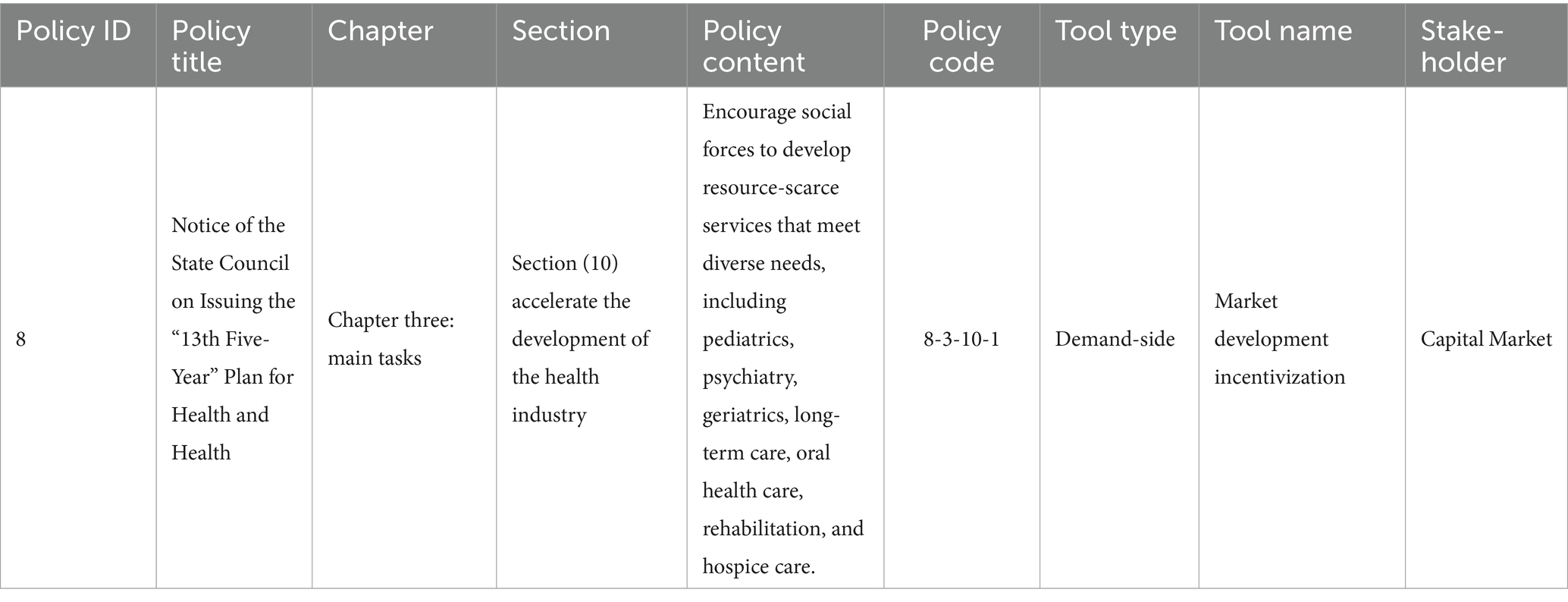
The coding of samples began with manual intensive reading of policy texts, followed by content consolidation and hierarchical coding of the texts using NVivo release 14.23.1 (38) software. The coding adopts a four-level structure: “policy number - chapter number - section number - text content.” Subsequently, frequency statistical analysis and comparative analysis were conducted on the policy samples to summarize the composition of rehabilitation medical service policy tools in mainland China and propose optimization suggestions. As shown in Table 2, documents were numbered in chronological order of issuance, with the example document assigned number 8; its third chapter is numbered 3; the tenth subsection of Chapter 3 is numbered 10; each sentence containing specific descriptions within the subsection is assigned an individual code. In this subsection example, the first sentence is coded as 1, resulting in the final code 8–3–10-1. Only codes related to rehabilitation policies were included in the result analysis, while those not related to rehabilitation policies were excluded.
2.3 Reliability and validity testing
To ensure the reliability of rehabilitation policy coding, two coders independently conducted simultaneous coding. Before coding, both coders engaged in detailed discussions to reach consensus on coding categories, principles, and procedures. After completing their coding independently, the coders compared their results to generate two sets of coding outcomes. These were subsequently evaluated by experts who reviewed the consistency between the two sets, identified discrepancies, and facilitated revisions through group discussions. Ultimately, Group A identified 292 codes related to the research theme, while Group B selected 301 such codes. Among these, 286 codes were rated as consistent between the two groups. Following group discussions, the final set of valid codes was confirmed to be 298. The percentage of agreement for reliability stood at 93.16%, and the percentage of agreement for validity reached 96.46%. These results indicate that the coding outcomes of this study are valid.
2.4 Analytical framework construction
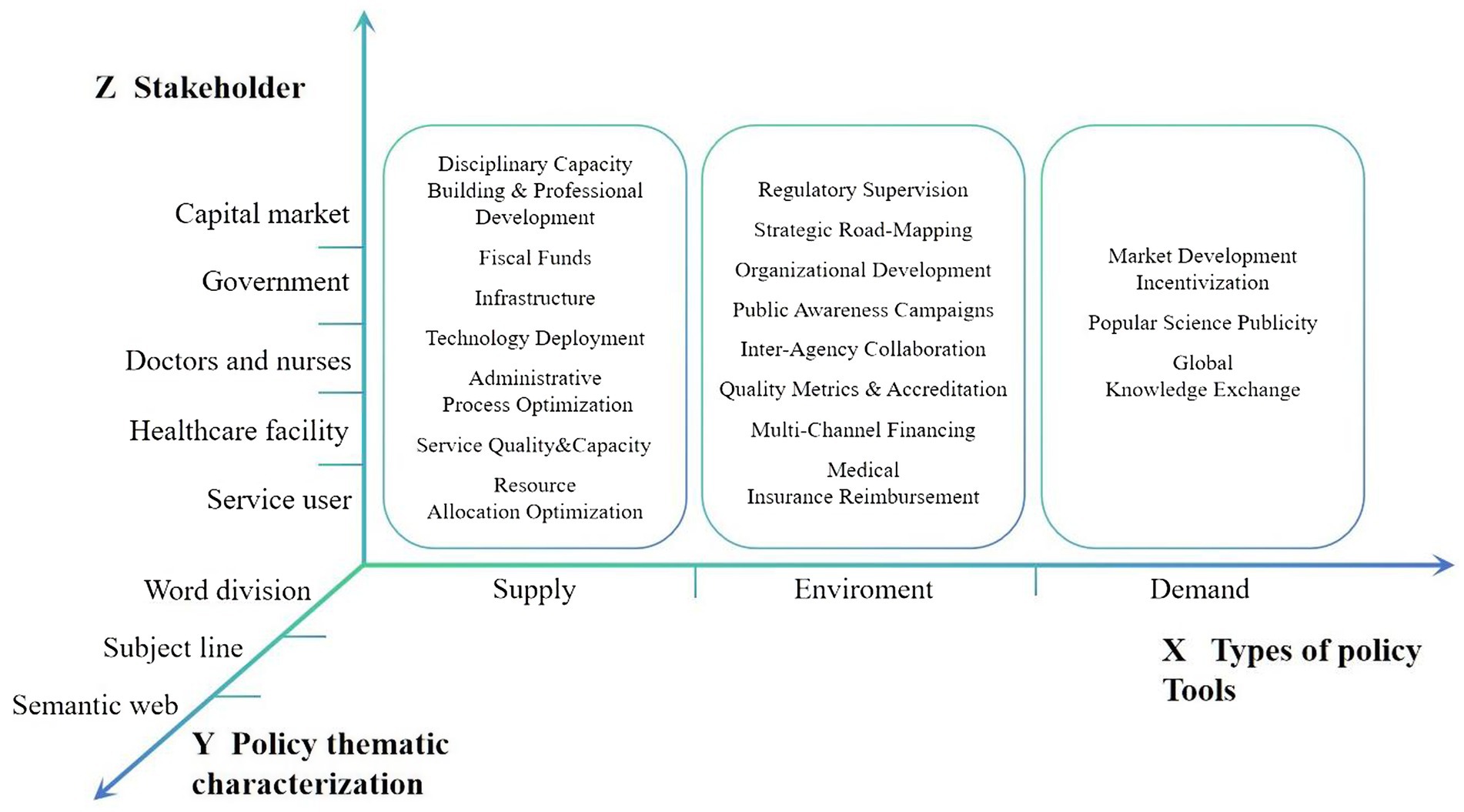
The constructed policy analysis framework for rehabilitation medical services comprised three constitutive dimensions: types of policy tools, thematic characterization of policies, and stakeholders (Figure 1).
2.4.1 X-dimension: types of policy tools
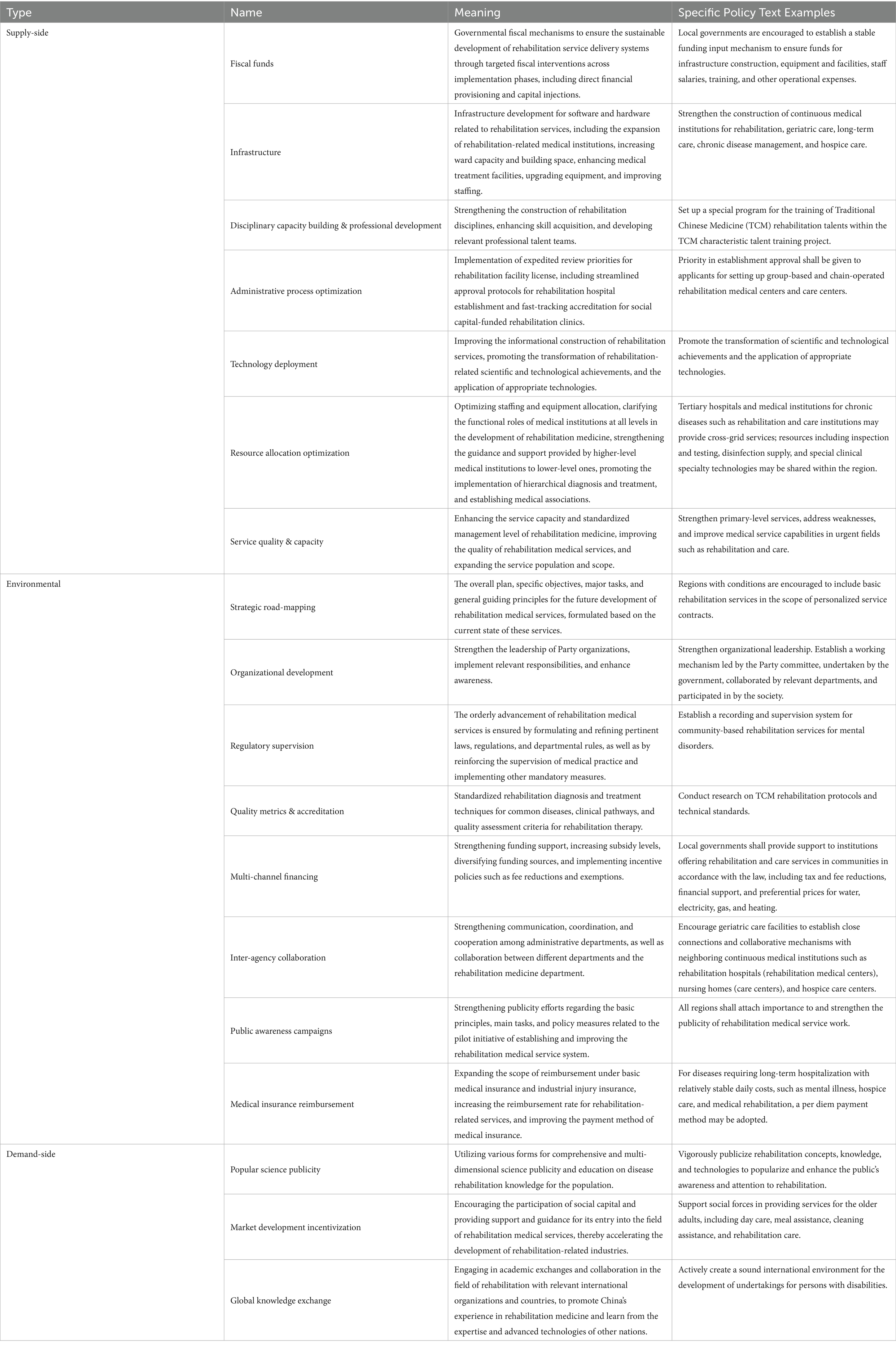
This analytical component adopts the tripartite taxonomy of policy tools conceptualized by Rothwell and Zegveld (27)—supply-side, environmental, and demand-side tools—to systematically examine rehabilitation medical service policy documents.
From an international perspective, this framework has been widely applied in policy analysis within fields such as healthcare and industrial development, boasting a well-established theoretical foundation and operational paradigm. The 2010–2023 period represents a critical phase in the transformation of China’s rehabilitation medical services from scattered exploration to systematic development. Policy interventions during this period need to simultaneously address three aspects: the establishment of an institutional framework (environment), the supply of resource factors (supply), and the stimulation of service demand (demand).
Supply-side tools refer to the direct supply and support provided by the government for activities related to the construction and development of rehabilitation medical services, focusing on addressing weaknesses and strengthening foundations. For instance, fiscal funds can include special subsidies for primary-level rehabilitation equipment and transfer payments to poverty-stricken areas. Environmental tools denote a series of measures adopted by the government to create a favorable development environment for the growth of rehabilitation medical services, emphasizing framework construction and collaboration promotion. A case in point is the joint promotion of the “Integration Initiative for Mental Health and Rehabilitation Services” by multiple ministries and commissions. Demand-side tools refer to the approaches employed by the government, such as popular science publicity, market development, and international exchanges, to enhance the public’s demand for rehabilitation medical services.
After subdividing the specific categories in the rehabilitation medical service policy texts, a total of 18 tool categories were identified. The specific categories, their definitions, and illustrative examples are presented in Table 3.
2.4.2 Y-dimension: thematic policy characterization
Thematic policy characterization effectively reflects the prioritization logic of policy-promulgating entities during the policymaking process. Based on established analytical frameworks (28), thematic characterization in this study was deconstructed into three methodological components, including lexical segmentation, thematic keyword extraction, and semantic network analysis. A term frequency analysis was conducted using ROST CM 6.0 (developed by Wuhan University’s Big Data Research Team) on the 41 rehabilitation service policy documents to identify high-frequency keywords, construct a co-word matrix. Based on this co-word matrix, Gephi 0.10 was used to build a semantic network (29). The co-occurrence matrix algorithm was applied to map the lexical relationship patterns and reveal potential policy focus areas. This hierarchical analytical approach enables multilevel interpretation of policy texts, from surface-level lexical patterns to deeper semantic configurations.
2.4.3 Z-dimension: stakeholder
Policy implementation requires collaborative engagement among multiple stakeholders to achieve strategic objectives (30). Stakeholder theory posits that organizational success depends on effectively managing relationships with key groups, including clients, employees, suppliers, communities, funders, and other entities influencing goal attainment (31). Since the 1990s, this framework has demonstrated strong applicability in health-sector research (32).
In alignment with rehabilitation policy characteristics, this study identified five core stakeholder categories as the Z dimension: regulatory authorities (government agencies), provider organizations (healthcare institutions), clinical practitioners (medical professionals), service recipients (patients), and rehabilitation capital markets (including equipment manufacturers and suppliers).
3 Results
3.1 X-dimension analytical findings
Analysis of the 41 policy documents yielded 298 coded segments. Frequency distribution across policy tool categories revealed significant disparities in their deployment (Table 4). Environmental tools dominated policy implementation (58.05%), followed by supply-side (32.98%) and demand-side tools (9.06%).
Quantitative analysis of environmental tool subtypes revealed significant disparities in their application. Further analysis of specific policy tool subcategories revealed that within environmental policy tools, strategic road-mapping constituted the largest proportion (33.89%), followed by inter-agency collaboration mechanisms (8.39%) and governance infrastructure enhancement (5.37%). Strategic road-mapping primarily involves the government’s formulation of developmental blueprints, specific objectives, and operational frameworks tailored to the current landscape rehabilitation service delivery. A representative example is the Precision Rehabilitation Service Initiative articulated in the National Health Commission’s policy documents: “Implement targeted rehabilitation interventions prioritizing children with disabilities and certified disabled individuals, achieving 80% coverage of essential rehabilitation services for the disabled population with rehabilitation needs.” Inter-agency collaboration mechanisms encompass both vertical administrative coordination (e.g., inter-ministerial task forces under State Council Directive 2021–19) and horizontal clinical integration models (e.g., multidisciplinary consultation systems linking rehabilitation departments to other clinical specialties).
Supply-side policy tools emphasize three strategic dimensions: rehabilitation resource allocation optimization (9.73%), service quality enhancement (8.72%), and disciplinary capacity building (8.72%). This finding indicates that the government prioritized equitable and rational allocation of rehabilitation medical resources, promoted service development through hierarchical diagnosis and treatment systems, and supported resource decentralization through the establishment of healthcare consortia. Additionally, it emphasized service quality and talent development to ensure these three strategic dimensions work synergistically.
Although demand-side interventions constituted the smallest proportion (9.06%) of policy tool categories, they reflect a notable policy emphasis on market development incentives (7.05%). This aligns with China’s decade-long policy trajectory of promoting social capital participation in rehabilitation services, as outlined by the State Council’s Guidelines on Social Capital Participation in Healthcare (2019). Implementing rehabilitation health literacy initiatives among the general population, alongside establishing international knowledge exchange frameworks, particularly with nations demonstrating advanced rehabilitation service systems, holds substantial potential for advancing the field. These endeavors align with the World Health Organization’s Rehabilitation 2030 Initiative (33).
3.2 Y-dimension analytical findings
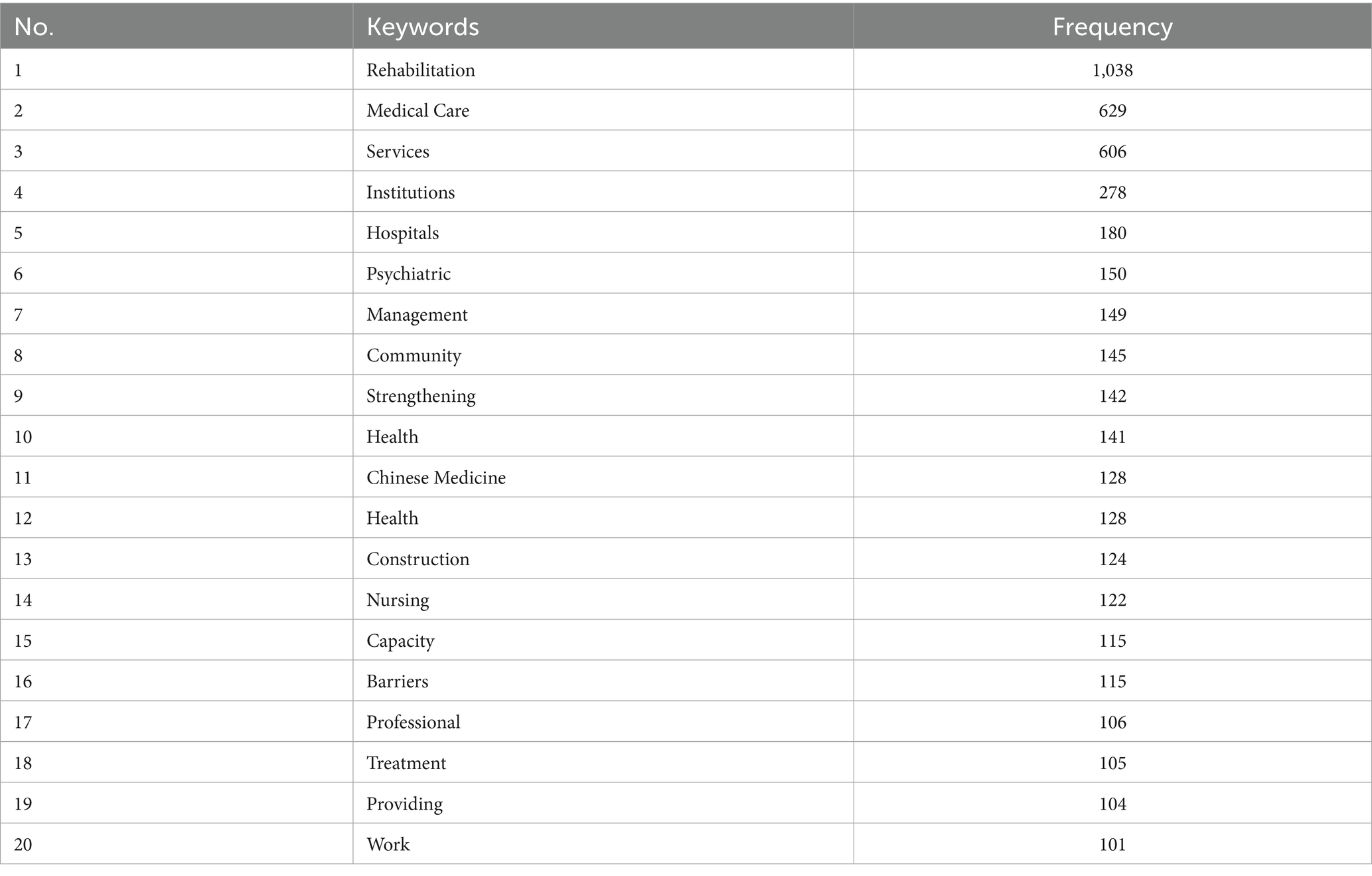
3.2.1 Lexical frequency analysis
The analytical protocol involved a systematic term frequency analysis of the 41 policy documents using ROST CM 6.0. Lexical segmentation and frequency quantification yielded a ranked list of the top 20 high-frequency keywords. The lexical segmentation outcomes are listed in Table 5.
3.2.2 Semantic network analysis of themes
Building on the word frequency analysis, further semantic network analysis of theme words in the rehabilitation policy documents was conducted. As shown in Figure 2, strong similarities and correlations were observed among the theme words in the policy text. The core terms, service, medical care, rehabilitation, strengthening, and institution, highlight the policy emphasis on enhancing the provision and development of rehabilitation services in medical and health institutions. The secondary keywords included management, health, construction, establishment, development, improvement, and technology, indicating that China’s rehabilitation medical services remain in the developmental phase, with ongoing improvements in terms of both technological capacity and institutional infrastructure.
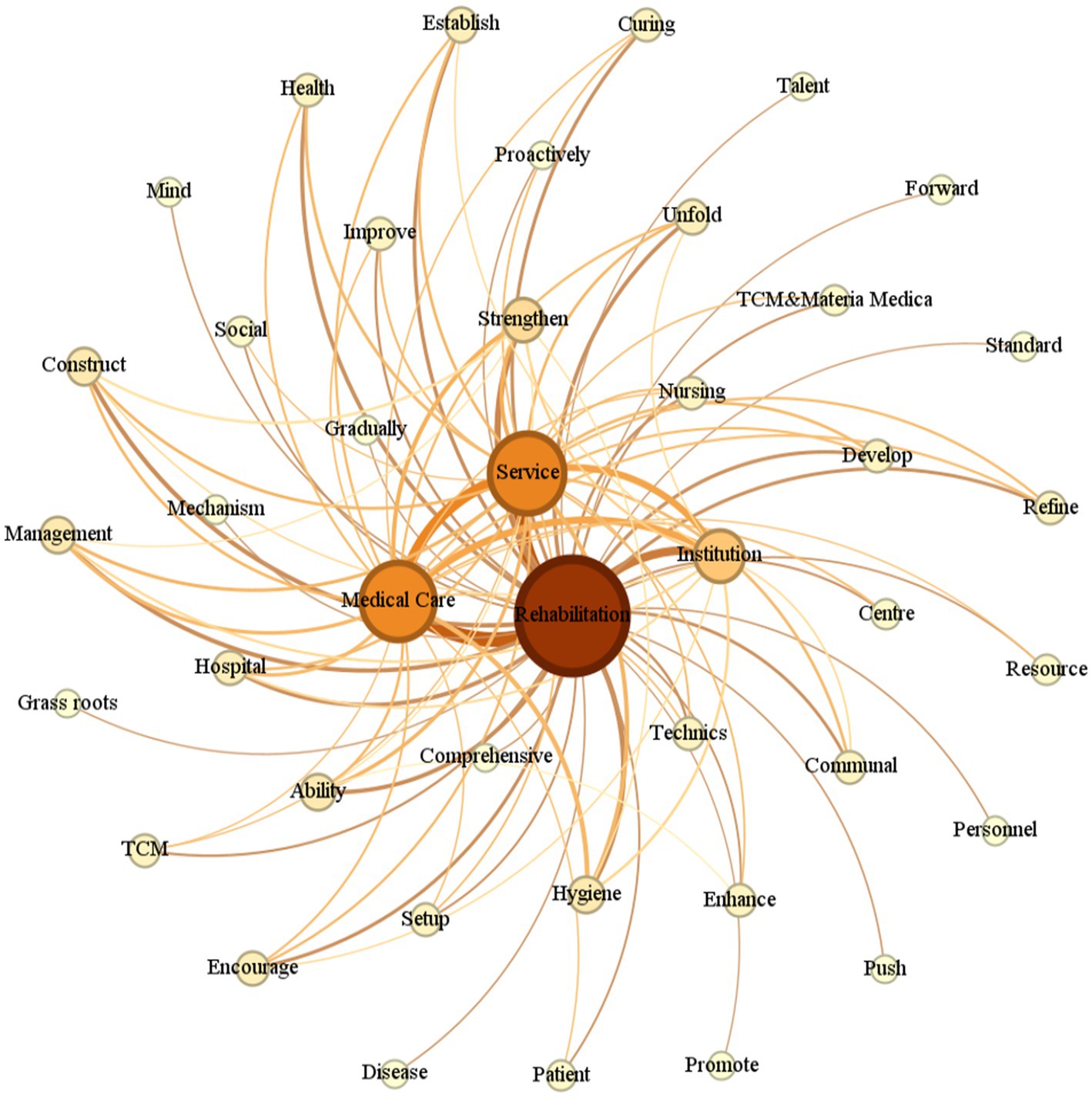
Figure 2. Semantic network map of keywords for China rehabilitation healthcare policy text. Key association pathways: rehabilitation and medical care, rehabilitation and institution, rehabilitation and strengthening, rehabilitation and service.
3.3 Z-dimension analytical findings
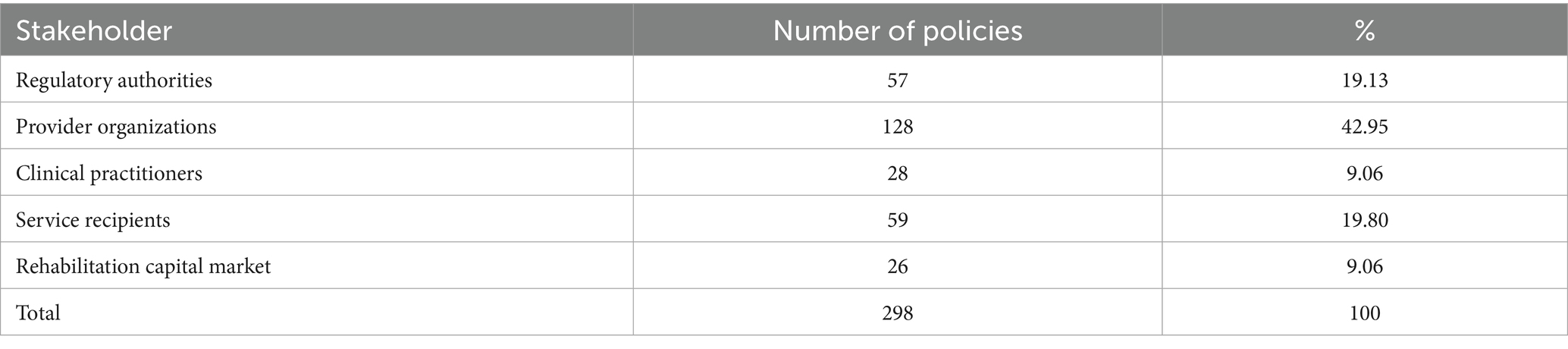
The analytical framework revealed that provider organizations were the predominant direct stakeholders in rehabilitation service delivery, accounting for 42.95% of policy interventions. Service recipients (patients) and regulatory authorities represented secondary stakeholder groups, while rehabilitation capital markets and clinical practitioners exhibited limited policy engagement (Table 6).
3.4 Results of cross-sectional analysis
Based on the single-dimensional analysis of rehabilitation medical service policies, a cross-dimensional analysis between specific policy tool categories and stakeholders was conducted. The two-dimensional quantitative results are shown in Table 7.

Table 7. Two-dimensional statistics of ‘specific categories–stakeholders’ in rehabilitation policy tools.
The X–Z analysis revealed that supply-side policy tools are mostly applied to healthcare institutions, healthcare workers, and patients. Additionally, environmental policy tools are mostly applied to healthcare institutions, government agencies, and patients, while demand-side tools are concentrated within the rehabilitation capital market, with minimal application to healthcare workers, healthcare institutions, and government agencies.
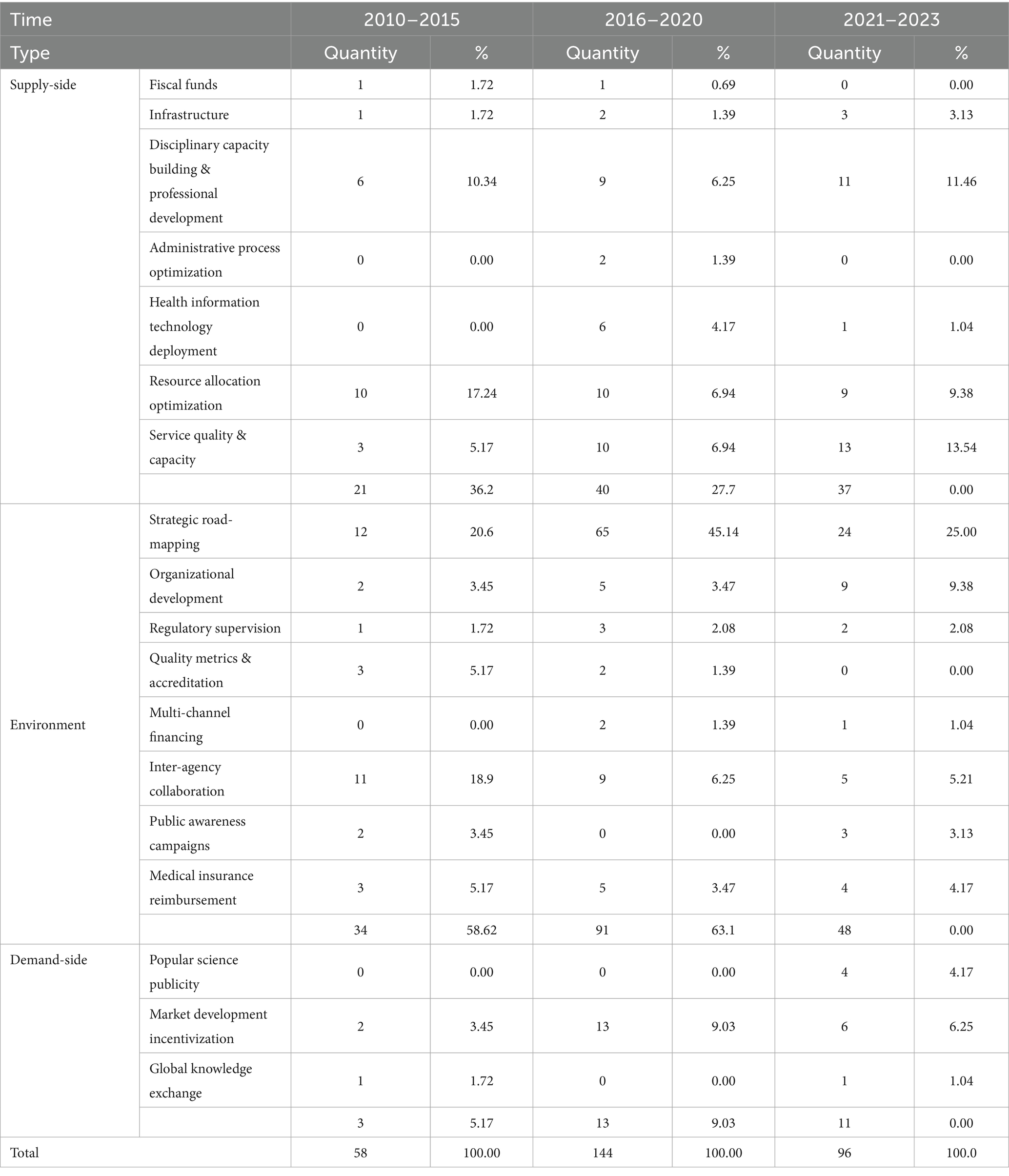
3.5 Results of temporal dimension analysis
To further reveal the dynamic development trajectory of China’s rehabilitation medical service policies, this study incorporated a temporal dimension and divided the policy samples into three phases based on China’s Five-Year Plans for National Economic and Social Development: the initial exploration phase (2010–2015, covering the 12th Five-Year Plan period and prior), the accelerated development phase (2016–2020, the 13th Five-Year Plan period), and the in-depth integration phase (2021–2023, the 14th Five-Year Plan period). The results are presented in Tables 8, 9.
In the initial exploration phase, environmental tools dominated. By frequently utilizing tools such as goal planning and inter-departmental collaboration, efforts were focused on establishing a basic institutional framework. From the perspective of stakeholders, policy focus was highly concentrated on government agencies and healthcare institutions, reflecting a path dependence on driving the initial development of rehabilitation initiatives through the internal administrative system.
During the accelerated development phase, the proportion of environmental tools further increased. Among supply-side tools, the use of information technology support and optimized administrative approval grew significantly, indicating a shift in resource allocation toward efficiency and innovation. The proportion of demand-side tools rose to 9.03%, with a focus on market development to encourage social capital participation in the rehabilitation sector. Among stakeholders, the proportion of policies targeting healthcare institutions jumped to 54.86%, making them the core of policy implementation. Concurrently, attention to patients (20.83%) and capital market participation (10.42%) increased, marking a shift in policy focus from institutional establishment to scale expansion.
In the in-depth integration phase, policy focus shifted from framework construction to connotative development, and the use of tools became more balanced. Among supply-side tools, service quality improvement, disciplinary development, and talent education emerged as core priorities. For the first time, popular science publicity was introduced under demand-side tools, signifying a policy orientation toward stimulating public demand. During this phase, policy attention to healthcare providers and patients continued to rise, reflecting a transition from emphasizing system construction to focusing on the capabilities of service suppliers and the experience of end beneficiaries.
4 Discussion
4.1 Outcomes
In this study, we established an analytical framework encompassing tool typology, thematic salience, and stakeholder configurations, based on Rothwell and Zegveld’s policy tool theory. Key insights were derived through bibliometric and content analyses of 41 rehabilitation medical service policies issued in mainland China over a 13-year period. The findings revealed that China’s rehabilitation medical service policy framework demonstrates institutional completeness, characterized by well-defined objectives, multifaceted implementation modalities, and favorable developmental ecosystems.
Environmental policy tools are predominantly utilized, with the “strategic road-mapping” subcategory receiving considerably high emphasis compared to other components within the same category. In contrast, both the supply-side and demand-side policy tools exhibited suboptimal deployment levels and notable internal structural imbalances. These findings align with those of a previous study (34).
Thematic analysis revealed that China’s rehabilitative healthcare system remains in an early developmental phase across both technological and institutional dimensions. Current strategic priorities are primarily concentrated in institutional rehabilitation frameworks, community-based intervention models, and Traditional Chinese Medicine (TCM) rehabilitation paradigms. Lexical frequency mapping identified psychotherapeutic interventions and TCM-based rehabilitation as pivotal developmental vectors. Notably, the ongoing structural integration of nursing support systems with rehabilitative protocols underscores the need for specialized therapeutic competencies in service delivery.
Based on stakeholder and cross-analysis results, provider organizations (42.95%) emerged as the core target of policies, followed by regulatory authorities (19.13%) and service recipients (19.80%). Clinical practitioners and the rehabilitation capital market each accounted for only 9.06%. The policy content directed at these latter groups is predominantly passive and response-oriented (e.g., skills training for medical staff or equipment configuration requirements for the capital market). In contrast, proactive and incentive-based clauses (e.g., career development support for medical staff or innovation subsidies for the capital market) are largely absent. This reflects a structural pattern characterized by a “focus on core entities and absence of vulnerable entities.”
4.2 Underlying reasons
Analyzing from the triangular dimension of “Outcome–Subject–Governance,” the observed imbalance in policy tool use and stakeholder representation may stem from adaptive responses corresponding to the development stage of rehabilitation services in China. From 2010 to 2023, China’s rehabilitation medicine sector was in an early, developmental phase, essentially “starting from scratch.” Guided by the incremental decision-making theory (35), the government prioritized the use of environmental policy tools (58.05%) to rapidly establish a policy framework. These tools are characterized by broad coverage, low cost, and high flexibility, and may guide development directions through strategic road-mapping (33.89%). In contrast, supply-side tools (32.98%) require long-term resource investment, whereas demand-side tools (9.06%) rely on multi-stakeholder collaboration. Both were challenging to implement on a large scale in the early development phase, leading to a stage-specific imbalance in policy tool application.
Second, the uneven representation of stakeholders may stem from significant disparities in their power positions and participation levels throughout the policy process. Drawing on the “Ladder of Citizen Participation” theory (36), government agencies and healthcare institutions occupy the “citizen power” tier at the top of the ladder, serving as policy formulators and core implementers, respectively. Cross-analysis of policy texts reveals that environmental tools are largely directed toward these two entities (48 entries for the government and 82 entries for healthcare institutions), which confirms their dominant status. Patients reside in the “symbolic participation” tier in the middle of the ladder: while they are beneficiaries of policies, they are not endowed with substantive authority to influence decision-making. Rehabilitation medical staff and the rehabilitation capital market occupy an even lower tier at the bottom of the ladder, functioning as passive respondents who are merely informed unilaterally. Relevant policies mostly consist of requirements imposed on them rather than provisions to motivate their initiative, and their core demands lack institutionalized channels for expression and influence.
Finally, limitations within the governance structure have constrained both the optimization of policy tools and collaboration among stakeholders. Influenced by the “administrative-led” tradition in China’s healthcare sector (37, 38), rehabilitation medical services have developed a “government–medical institution” dual governance model. A total of 48 “environmental tools–government” codes and 82 “environmental tools–medical institution” codes constitute the core policy chain, while collaborative participation mechanisms for medical staff, capital, and the public are absent (e.g., no policies mention medical staff participation in policy revision). This governance structure not only limits the efficiency of resource allocation in supply-side tools but also makes it difficult for demand-side tools to stimulate market and public demand. As a result, it reinforces existing patterns of tool imbalance and stakeholder differences.
Compared with developed countries, the Chinese rehabilitation policy model identified in this study presents distinct characteristics. The rehabilitation policy systems in European and American countries have become relatively mature through long-term development, driven by a robust market mechanism, diversified insurance payment schemes, active industry associations, and patient organizations in a collaborative manner. China’s model, characterized by “dominance of environmental tools and a dual core of government-medical institutions,” represents a typical “top-down” system construction path. This reflects the strategic choice of a developing country like China to rapidly establish a policy framework “from scratch” during a specific stage of development.
4.3 Recommendations
To address the prominent issue that demand-side tools account for only 9.06%, priority measures can be advanced in the later stage of the 14th Five-Year Plan. For instance, a rehabilitation service voucher system should be established: issue universal rehabilitation service vouchers to key groups such as post-operative patients and older adults, clarify the voucher amount, scope of use, and redemption procedures. By directly subsidizing the demand side, this system reduces the threshold for rehabilitation consumption, guides the public to actively use rehabilitation services, and converts potential demand into effective demand. Additionally, the coverage of rehabilitation science popularization can be expanded: collaborate with medical institutions, communities, and new media platforms to develop a rehabilitation knowledge popularization program, design differentiated science content for different groups, and enhance public awareness of rehabilitation through public lectures, community free clinics, and other forms—thereby driving rehabilitation service consumption from the source of demand.
Focusing on the core dimensions of supply-side tools such as resource allocation and disciplinary development, two aspects of work can be promoted. First, the rehabilitation resource allocation mechanism can be optimized: centering on hierarchical medical system, establish a connection system of “upper-level hospital assessment + community rehabilitation training + home-based rehabilitation guidance,” and use special fiscal funds to subsidize the update of primary-level rehabilitation equipment. Second, a special program for rehabilitation talent training should be implemented: conduct regular training on rehabilitation skills for existing medical staff, set up special allowances for rehabilitation talents, and attract talents to flow to primary-level and remote areas.
To tackle the problems of excessively high proportion of goal planning and insufficient implementation in environmental tools, refinements can be made in two aspects. First, an assessment mechanism for rehabilitation policies could be established: incorporate indicators such as rehabilitation service coverage into the health work assessment system of local governments, and conduct regular evaluations of policy implementation effects. Second, the coordination of medical insurance reimbursement policies can be strengthened: further expand the coverage of rehabilitation programs under medical insurance, explore pilot medical insurance payment for new service models such as home-based rehabilitation and tele-rehabilitation. Leveraging the medical insurance lever to drive the development of the rehabilitation service market will also provide institutional support for the implementation of demand-side and supply-side tools.
4.4 Limitations
The transferability of the research findings to other contexts may be limited. Additionally, potential bias from researcher subjectivity may influence data interpretation, although this was mitigated through interaction checks within the research team.
4.5 Conclusion
From the perspective of policy tools, this study reveals the structural imbalance of China’s rehabilitation policies—characterized by “the dominance of environmental tools and insufficient supply-side and demand-side tools”—as well as the governance feature of “government-medical institution” as the core with insufficient participation of other stakeholders. Compared with international rehabilitation and nursing policies, China’s policy framework still needs to be strengthened in terms of the improvement of service systems and the diversification of tool utilization. This study provides a new perspective for international policy research.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XJ: Data curation, Methodology, Software, Writing – original draft, Writing – review & editing. LL: Conceptualization, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by Shanghai Center for Emerging Technologies Governance in Medicine and Public Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Introduction to rehabilitation-the Chinese Society of Physical Medicine and Rehabilitation. Available online at: https://cspmr.cma.org.cn/cn/page.asp?pageid=18.html#1 (Accessed December 24, 2024).
2. Taylor, RS, Sadler, S, Dalal, HM, Warren, FC, Jolly, K, Davis, RC, et al. The cost effectiveness of REACH-HF and home-based cardiac rehabilitation compared with the usual medical care for heart failure with reduced ejection fraction: a decision model-based analysis. Eur J Prev Cardiol. (2019) 26:1252–61. doi: 10.1177/2047487319833507
3. Chen, YW, Wang, CY, Lai, YH, Liao, YC, Wen, YK, Chang, ST, et al. Home-based cardiac rehabilitation improves quality of life, aerobic capacity, and readmission rates in patients with chronic heart failure. Medicine (Baltimore). (2018) 97:e9629. doi: 10.1097/MD.0000000000009629
4. Oddy, M, and da Silva, RS. The clinical and cost-benefits of investing in neurobehavioural rehabilitation: a multi-Centre study. Brain Inj. (2013) 27:1500–7. doi: 10.3109/02699052.2013.830332
5. Bachmann, S, Finger, C, Huss, A, Egger, M, Stuck, AE, and Clough-Gorr, KM. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ. (2010) 340:c1718. doi: 10.1136/bmj.c1718
6. Duscha, BD, Ross, LM, Hoselton, AL, Piner, LW, Pieper, CF, and Kraus, WE. A detailed analysis of cardiac rehabilitation on 180-day all-cause hospital readmission and mortality. J Cardiopulm Rehabil Prev. (2024) 44:99–106. doi: 10.1097/HCR.0000000000000835
7. Puhan, MA, Scharplatz, M, Troosters, T, and Steurer, J. Respiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality-a systematic review. Respir Res. (2005) 6:54. doi: 10.1186/1465-9921-6-54
8. Radford, K, Phillips, J, Drummond, A, Sach, T, Walker, M, Tyerman, A, et al. Return to work after traumatic brain injury: cohort comparison and economic evaluation. Brain Inj. (2013) 27:507–20. doi: 10.3109/02699052.2013.766929
9. Guo, C, and Li, H. Application of 5G network combined with AI robots in personalized nursing in China: a literature review. Front Public Health. (2022) 10:948303. doi: 10.3389/fpubh.2022.948303
10. Zhao, J, and Gereffi, G. Upgrading of Chinese domestic firms in advanced manufacturing: evidence from industrial robots and high-tech medical devices In: China’s new development strategies. Gereffi, G, Bamber, P, and Fernandez-Stark, K, eds. Singapore: Palgrave Macmillan (2022). 195–233.
11. Huo, Y. Current status and development of percutaneous coronary intervention in China. J Zhejiang Univ Sci B. (2010) 11:631–3. doi: 10.1631/jzus.B1001012
12. Tao, C, Nogueira, RG, Zhu, Y, Sun, J, Han, H, Yuan, G, et al. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. (2022) 387:1361–72. doi: 10.1056/NEJMoa2206317
13. Zhou, M, Ta, S, Hahn, RT, Hsi, DH, Leon, MB, Hu, R, et al. Percutaneous intramyocardial septal radiofrequency ablation in patients with drug-refractory hypertrophic obstructive cardiomyopathy. JAMA Cardiol. (2022) 7:529–38. doi: 10.1001/jamacardio.2022.0259
14. Cieza, A, Causey, K, Kamenov, K, Hanson, SW, Chatterji, S, and Vos, T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2021) 396:2006–17. doi: 10.1016/S0140-6736(20)32340-0
15. Hall, CD, Herdman, SJ, Whitney, SL, Anson, ER, Carender, WJ, Hoppes, CW, et al. Vestibular rehabilitation for peripheral vestibular hypofunction: an updated clinical practice guideline from the academy of neurologic physical therapy of the American Physical Therapy Association. J Neurol Phys Ther. (2022) 46:118–77. doi: 10.1097/NPT.0000000000000382
16. Andrade, R, Pereira, R, van Cingel, R, Staal, JB, and Espregueira-Mendes, J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br J Sports Med. (2020) 54:512–9. doi: 10.1136/bjsports-2018-100310
17. Wade, SL, Narad, ME, Shultz, EL, Kurowski, BG, Miley, AE, Aguilar, JM, et al. Technology-assisted rehabilitation interventions following pediatric brain injury. J Neurosurg Sci. (2018) 62:187–202. doi: 10.23736/S0390-5616.17.04277-1
18. Coscia, M, Wessel, MJ, Chaudary, U, Millán, JR, Micera, S, Guggisberg, A, et al. Neurotechnology-aided interventions for upper limb motor rehabilitation in severe chronic stroke. Brain. (2019) 142:2182–97. doi: 10.1093/brain/awz181
19. McGlinchey, MP, James, J, McKevitt, C, Douiri, A, McLachlan, S, and Sackley, CM. The effect of rehabilitation interventions on physical function and immobility-related complications in severe stroke-protocol for a systematic review. Syst Rev. (2018) 7:197. doi: 10.1186/s13643-018-0870-y
20. Cruise, CM, Sasson, N, and Lee, MH. Rehabilitation outcomes in the older adult. Clin Geriatr Med. (2006) 22:257–67. doi: 10.1016/j.cger.2005.12.015
21. Burstrom, B, Nylen, L, Clayton, S, and Whitehead, M. How equitable is vocational rehabilitation in Sweden? A review of evidence on the implementation of a national policy framework. Disabil Rehabil. (2011) 33:453–66. doi: 10.3109/09638288.2010.493596
22. Costa, N, Blyth, FM, Parambath, S, and Huckel, SC. What's the low back pain problem represented to be? An analysis of discourse of the Australian policy directives. Disabil Rehabil. (2023) 45:3312–22. doi: 10.1080/09638288.2022.2125085
23. Capano, G, and Howlett, M. The knowns and unknowns of policy instrument analysis: policy tools and the current research agenda on policy mixes. SAGE Open. (2020) 10:215824401990056. doi: 10.1177/2158244019900568
24. Bali, AS, Howlett, M, Lewis, JM, and Ramesh, M. Procedural policy tools in theory and practice. Polic Soc. (2021) 40:295–311. doi: 10.1080/14494035.2021.1965379
25. Lyu, Z. The choice of public policy instruments: a new perspective on policy implementation research. Pac J. (2006) 5:7–16.
26. von Granitz, H, Sonnander, K, and Winblad, U. Tracing the refinement of policy tools for disability rights: a content analysis of how the granting process of state-funded personal assistance in Sweden is aligned with the LSS act. Disabil Rehabil. (2025) 47:926–35. doi: 10.1080/09638288.2024.2362954
27. Rothwell, R., and Zegveld, W. Industrial innovation and public policy: preparing for the 1980s and 1990s London Frances Printer 1981 10–12
28. Wang, C, Duan, Y, and Ren, L. Quantitative research on rural revitalization policy texts of central ministries and commissions: a three-dimensional analytical framework based on the perspective of policy instruments. Agric Econ Manag. (2021) 3:15–27.
30. Tang, S, and Si, Y. Quantitative research on medical consortium-related policies in China: a policy instruments perspective. Health Soft Sci. (2020) 34:32–6.
31. Edward Freeman, R, and Phillips, RA. Stakeholder theory: a libertarian defense. Bus Ethics Q. (2002) 12:331–49. doi: 10.2307/3858020
32. Fang, H, Jiang, K, Ma, H, Bai, X, Anastasia, G, and Jiao, M. Integrating primary healthcare service systems based on stakeholder theory. Chin Health Econ. (2018) 37:72–5.
33. Rehabilitation 2030: a call for action-World Health Organization. Available online at:https://www.who.int/rehabilitation/rehabilitation-2030-call-for-action (Accessed December 14, 2024).
34. Li, W, Zhu, Y, and Zhu, X. Text analysis of rehabilitation nursing policy in China from the perspective of policy tools. Front Public Health. (2025) 13:1562889. doi: 10.3389/fpubh.2025.1562889
35. Lindblom, CE. The science of ‘muddling through.’. Public Adm Rev. (1959) 19:79–88. doi: 10.2307/973677
36. Arnstein, SR. A ladder of citizen participation. J Am Plan Assoc. (2019) 85:24–34. doi: 10.1080/01944363.2018.1559388
37. Yip, W, and Hsiao, WC. What drove the cycles of Chinese health system reforms? Health Syst Reform. (2015) 1:52–61. doi: 10.4161/23288604.2014.995005
Keywords: rehabilitation, China, policy tool, policy analysis, rehabilitation policy
Citation: Jiang X and Luo L (2025) A quantitative study of China’s rehabilitation policies from the perspective of policy tools. Front. Public Health. 13:1676931. doi: 10.3389/fpubh.2025.1676931
Edited by:
Chao Ma, Southeast University, ChinaReviewed by:
Sureshkumar Kamalakannan, Northumbria University, United KingdomHai xia Wang, The Second Qilu Hospital of Shandong University, China
Ricardo De Moraes E. Soares, Naval School, Portugal
Copyright © 2025 Jiang and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Luo, bGlsdW9mdWRhbkAxNjMuY29t
 Xinyang Jiang
Xinyang Jiang Li Luo*
Li Luo*