- 1Department of General Affairs, National Rehabilitation Center, Seoul, Republic of Korea
- 2Department of Gaitlab, National Rehabilitation Center, Seoul, Republic of Korea
- 3Department of Physical Education, Konkuk University, Seoul, Republic of Korea
- 4National Team Physical Fitness Assessment and Analysis Lab, Department of Sport Science, Sport Science Center for National Athletes with Disabilities, Icheon, Republic of Korea
- 5Department of Healthcare and Public Health, Rehabilitation Research Institute, National Rehabilitation Center, Seoul, Republic of Korea
- 6Department of Clinical Research for Rehabilitation, Rehabilitation Research Institute, National Rehabilitation Center, Seoul, Republic of Korea
- 7Department of Rehabilitation Medicine, Ewha Womans University Mokdong Hospital, Seoul, Republic of Korea
- 8Department of Sports and Leisure, Suseong University, Daegu, Republic of Korea
- 9Department of Physical Education, Korea National Sport University, Seoul, Republic of Korea
Purpose: This study aimed to compare the effects of high-intensity resistance training (HIRT) versus moderate-intensity resistance training (MIRT) on bone mineral density (BMD), body composition, and functional fitness in individuals with motor-complete paraplegia after spinal cord injury (SCI), and to propose a tailored exercise intervention for this population.
Methods: Participants with motor-complete paraplegia were randomized into HIRT (n = 8) or MIRT (n = 8) groups. Both groups completed an 8-week elastic resistance training program. The measured outcomes included extended body composition (BMD, T-scores, lean mass, and fat mass) and functional fitness components (cardiorespiratory endurance, muscular strength, endurance, and flexibility).
Results: No significant changes in BMD were observed in either group (p > 0.05). The HIRT group demonstrated significant improvements in lean mass (p < 0.001), chest press strength (p = 0.024), muscular endurance (p = 0.008), and VO₂peak (p = 0.001), while the MIRT group showed no significant changes. Flexibility and fat mass did not significantly differ in either group (p > 0.05).
Conclusion: High-intensity resistance training was more effective than MIRT in improving lean mass and functional fitness in individuals with motor-complete SCI. Although BMD did not change over the 8-week period, its assessment remains clinically relevant, and future studies should investigate longer-duration or higher-intensity protocols to promote skeletal adaptations.
1 Introduction
Individuals with spinal cord injury (SCI) represent a growing demographic, with over 2,000 new cases reported annually across all age groups and sexes (1). Due to high healthcare costs and susceptibility to secondary conditions, tailored health programs are essential (2). Loss of motor function in SCI leads to reduced physical activity, which is a primary contributor to poor health outcomes. Owing to their dependence on assistive devices such as wheelchairs, individuals with SCI exhibit significantly lower physical activity levels than those without disabilities. They also show markedly poorer physical fitness, including reduced muscular strength, flexibility, and cardiorespiratory endurance.
In individuals with SCI, cardiorespiratory endurance is approximately 70% of the typical level, while muscular strength ranges from 30 to 50% depending on injury severity (3). Flexibility is often limited by repetitive, constrained movements during wheelchair use, which increases the risk of musculoskeletal injury (4). Thus, maintaining and improving physical fitness is essential for preserving independence and overall health and requires continuous monitoring and effort. Achieving this necessitates the consideration of extended body composition, including bone mineral density (BMD) and body composition, alongside functional fitness, cardiorespiratory endurance, muscular strength, muscular endurance, and flexibility. Given the heightened risk of osteoporosis and fracture in SCI, BMD was included as a clinically meaningful component of extended body composition analysis, providing insights into long-term skeletal health beyond immediate effects of training.
Reduced activity in SCI increases the risk of osteoporosis and fractures (5). However, regular upper-body exercise may enhance bone health, with some studies reporting increased upper-limb BMD in active individuals with SCI (6). There is a strong relationship between physical fitness and BMD. Regular exercise promotes muscle fiber development and stimulates the musculoskeletal system, thereby improving BMD. High-intensity exercise, which imposes a greater mechanical load, can induce hypertrophy and enhance strength, leading to BMD gains in targeted areas. SCI affects the entire body, and interventions such as electrical stimulation, which induce repetitive contractions and mechanical stress, have been shown to improve BMD (7). Therefore, maintaining physical fitness is key to increasing BMD and improving the overall health of individuals with SCI.
Researchers continue to explore innovative training methods to maximize the effectiveness of exercise. One prime example is high-intensity interval training (HIIT), which has gained popularity for its time efficiency and high effectiveness. In the present study, the traditional aerobic-based HIIT and moderate intensity continuous training (MICT) formats were modified into resistance-based protocols using elastic bands, allowing participants to perform interval or continuous exercises with upper-limb muscle engagement rather than large-muscle aerobic movement. This approach was specifically designed to align with the functional needs and neuromuscular conditions of individuals with SCI.
A 12-week HIIT program improved muscular strength and cardiovascular and respiratory functions in patients with SCI (8). Compared with continuous moderate-intensity training, HIIT provides higher metabolic intensity and greater enjoyment, making it more suitable for this population (9). Although the exercise modality was resistance-based, the interval and continuous structures of HIIT and MICT were maintained, ensuring comparable intensity modulation and work-to-rest ratios consistent with conventional definitions. It also yields superior oxygen uptake and cardiovascular fitness, improving vascular and overall health (10). Nevertheless, most individuals with SCI still rely on arm ergometer-based MICT (11), Therefore, adapting both HIIT and MICT into resistance-based formats provides an opportunity to enhance muscular engagement and functional outcomes while preserving the established principles of exercise intensity control. This study aimed to evaluate the effects of High-Intensity Resistance Training (HIRT) and Moderate-Intensity Resistance Training (MIRT) on functional fitness and extended body composition in individuals with SCI, and to propose an effective training method tailored to their needs.
2 Materials and methods
2.1 Participants
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Konkuk University (IRB No. 7001355-202008-HR-397). Data collection was conducted from October 1, 2020, to March 31, 2021. Participants with chronic SCI were recruited from local disability centers. Inclusion criteria were: (1) wheelchair users with motor-complete paraplegia due to SCI, based on findings that individuals with American Spinal Injury Association Impairment Scale (AIS) grade B benefit from both short- and long-term training at various intensities (12); (2) no engagement in regular exercise within the past 6 months; (3) no use of medications that could affect study outcomes and no plans to initiate such medications during the study period; and (4) ability to complete the exercise program consistently. All participants were informed of the study’s purpose, protocol, and potential benefits and provided written informed consent.
Based on two comparable randomized controlled trials that showed clinically meaningful improvements with 7–10 participants per arm (11, 13), together with prior exercise-intervention studies in individuals with SCI (14, 15), we set a target of eight participants per group and, after allowing for an anticipated 20% attrition, enrolled 20 men. An investigator not involved in outcome assessments then used sealed opaque envelopes and a block size of 4 to allocate participants to either HIRT or MIRT.
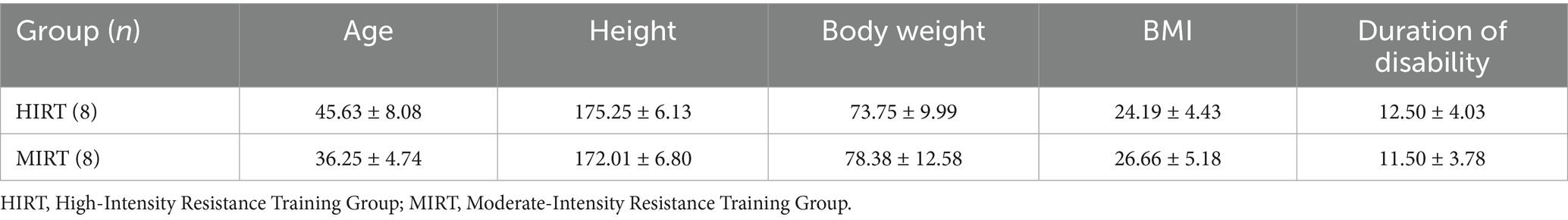
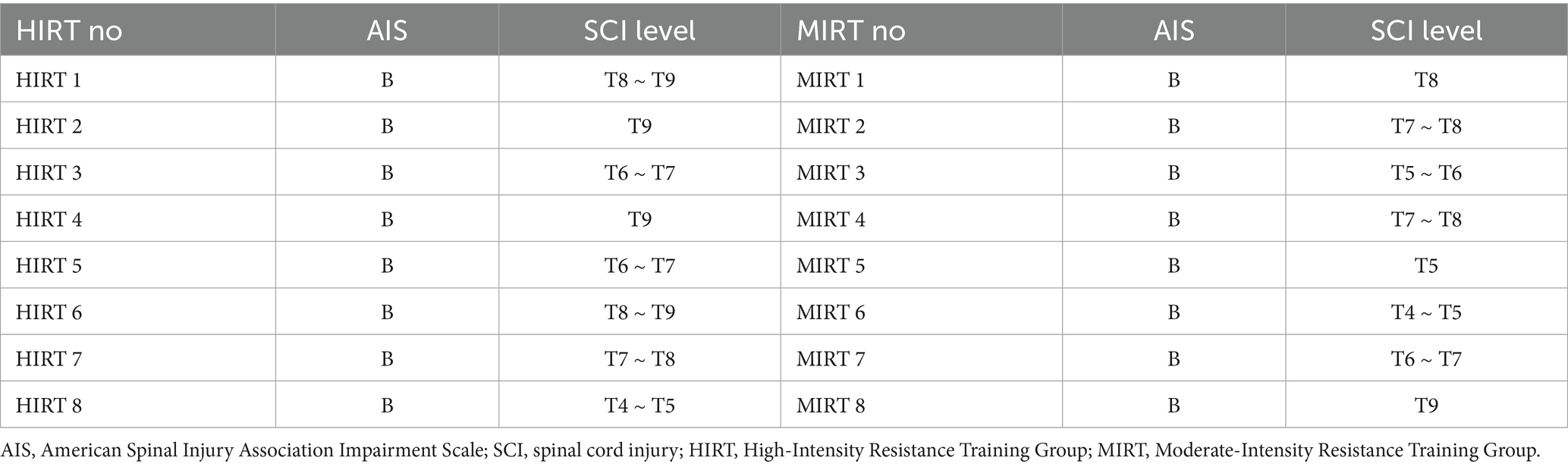
Four participants withdrew because of recurrent pressure ulcers (n = 2) or scheduling conflicts (n = 2), leaving 16 participants (HIRT = 8; MIRT = 8) who completed the program. Baseline characteristics and AIS classifications are presented in Tables 1, 2, respectively.
2.2 Procedure
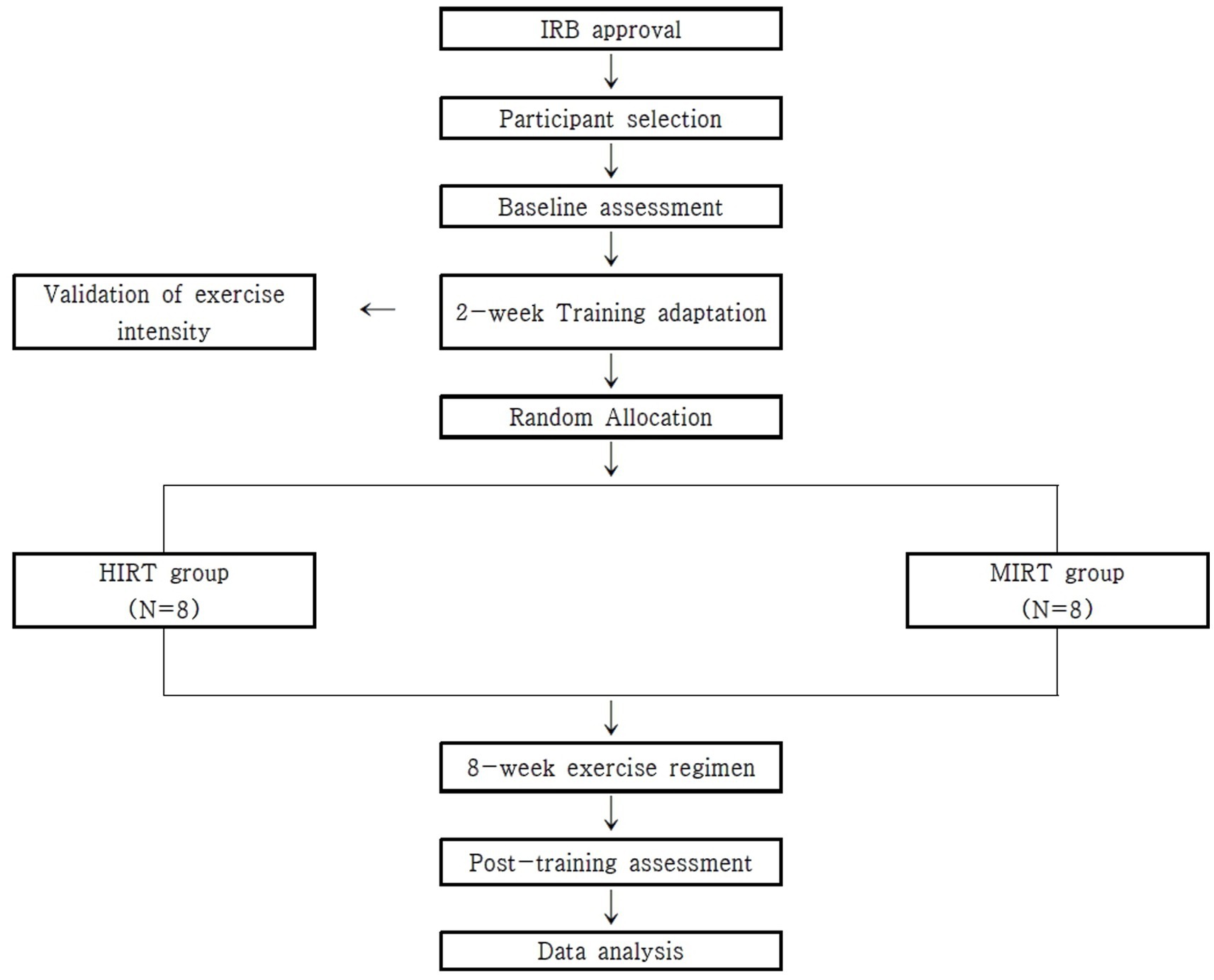
This study investigated the differences in outcomes between training methods in individuals with SCI. Participants were assessed at baseline and randomly assigned to the HIRT or MIRT groups. After 8 weeks of training, the same protocols were used to assess changes in BMD and fitness. The study design is illustrated in Figure 1. Outcome assessors were blinded to group allocation throughout the study period to reduce assessment bias.
2.3 Training methods
This study implemented two training protocols, HIRT and MIRT, to examine their effects on individuals with SCI. Before the intervention, a pre-training validation phase was conducted to directly measure energy expenditure during MIRT sessions using a portable gas analyzer (K5, COSMED, Italy). These measurements served as the basis for adjusting the HIRT protocol to ensure equivalent training volume between groups. Based on a previous study indicating that at least two sessions of high-intensity exercise per week over 6 weeks are required to improve physical fitness in individuals with SCI (16), participants first completed a 2-week validation and acclimation phase, This phase consisted of once-weekly training to adjust to the prescribed intensities, provide instruction and practice for interpreting the rating of perceived exertion (RPE), and measure energy expenditure during MIRT sessions for protocol matching. The final decision to implement an 8-week intervention period was informed by previous studies demonstrating improvements in overall physical function among individuals with SCI following 8 weeks of exercise training (17, 18). Given the limited physical activity associated with daily life in this population, this duration was considered sufficient. To ensure that both external intensity (%1RM) and internal load (subjective exertion) were accurately represented, training sessions were standardized based on one-repetition maximum (1RM) to unify resistance intensity. During the intervention, researchers monitored RPE in real time and provided feedback to maintain adherence to the target intensity. Training was conducted three times per week, as research indicates that 2–3 weekly sessions of moderate- to high-intensity exercise improve strength and physical function in individuals with chronic SCI (19). A minimum of 24 h of rest was maintained between sessions to ensure adequate recovery. All exercises were designed according to the frequency, intensity, time, and type principle of exercise prescription. All training sessions were supervised by a rehabilitation exercise specialist with over 10 years of experience in SCI-specific physical training, ensuring safety and appropriate guidance throughout the intervention.
The HIRT protocol was adapted from a previous upper-body HIIT case study in an individual with SCI using an arm crank ergometer (20). It included high-intensity intervals at 70% of one repetition maximum (1RM) with a rating of perceived exertion of 17 on Borg’s scale, lasting 4–5 min, alternating with low-intensity intervals at 20–25% of 1RM for 3–5 min. In previous resistance training studies involving individuals with spinal cord injury, 70% of 1RM has been classified as high intensity (21), and the original HIRT design that guided this study also applied 70% as the high-intensity threshold (20). Based on these precedents, this study defined 70% of 1RM as high-intensity resistance training. Each interval consisted of 2 to 3 sets of 30–45 s, adjusted to match the energy expenditure measured during the MIRT validation phase. Resistance bands enabled smooth transitions between intensities, and repetitions were tailored to match the energy expenditure measured in MIRT.
The MIRT group performed resistance exercises continuously, without rest between repetitions or sets, maintaining a steady pace throughout the 25 min sessions. This structure was intentionally designed to reflect the principles of continuous training, despite the use of resistance-based rather than aerobic modalities. The MIRT protocol was developed based on previous research applying moderate-intensity continuous training to individuals with SCI. It consisted of 25 min sessions performed at 45% of 1RM, with participants maintaining a perceived exertion level of 12 on Borg’s scale. Each session lasted approximately 30 min in total, including a 3 min warm-up and 2 min cool-down phase with standardized stretching exercises. This structure was maintained consistently across both groups to ensure uniform physiological preparation and recovery. The total energy expenditure of these MIRT sessions was measured and used as a reference to ensure matched training volume in the HIRT protocol. Resistance bands were calibrated according to the 2019 guidelines of the National Rehabilitation Center (22). Training intensity was adjusted at week 4, following 1RM reassessments, to align with progressive overload principles. Researchers monitored perceived exertion levels throughout each session to ensure participants exercised at the prescribed intensity.
Each training week included three sessions with one resistance exercise per day—chest press (day 1), lateral raise (day 2), and shoulder press (day 3). This structure was applied identically across both groups. In the chest press, participants positioned the resistance band behind the scapula, pushing forward to engage the chest and arm muscles. The lateral raise involved placing the band under the feet while seated in a wheelchair, lifting the hands to shoulder height to activate the shoulder muscles. The shoulder press required securing the band at the pelvic area in the wheelchair, either by sitting on it or looping it under the seat, and extending the arms upward.
To enhance adherence and accessibility, all sessions were conducted remotely at fixed times through a social network platform. Participants performed exercises simultaneously from their homes or workplaces according to pre-announced schedules. Real-time video monitoring ensured proper execution, and participants who missed a session were offered make-up opportunities.
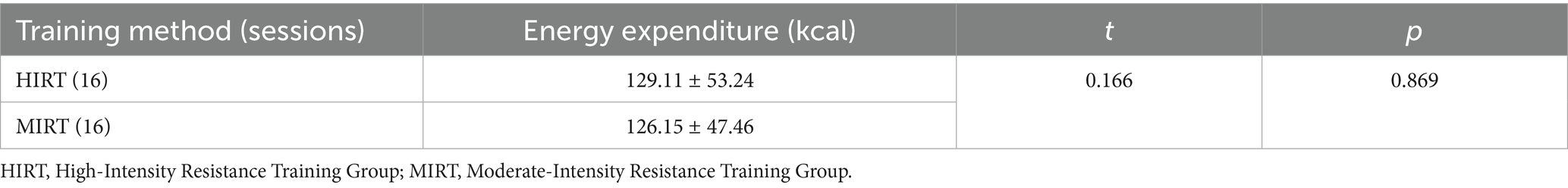
To control for confounding variables, training volume was analyzed based on energy expenditure and total oxygen consumption. An independent t-test confirmed no significant differences between the groups (t = 0.166, p = 0.869), indicating equivalent training volumes. Detailed statistical results are presented in Table 3.
2.4 Outcome measures
2.4.1 Extended body composition
Extended body composition, including BMD and body composition, was measured using dual-energy X-ray absorptiometry (Holyzonwi, United States). Scans were conducted at a certified facility with minimal radiation exposure (0.001 mSv) under professional supervision. Participants wore lightweight clothing and removed all metallic items. BMD and T-scores were assessed at the hip and lumbar spine, which are common sites of osteoporotic fractures (23). To ensure accuracy, the participants remained still during the scans. Body composition was recorded in grams and converted to kilograms.
2.4.2 Functional fitness
Functional fitness was evaluated across cardiorespiratory endurance, muscular strength, muscular endurance, flexibility, and body composition.
Cardiorespiratory endurance was assessed using the 6 Minute Wheelchair Ambulation Test on an 80-m marked course. Participants were instructed to cover as much distance as possible within 6 min while using their wheelchair. The total distance traveled and VO₂ peak were recorded using a portable gas analyzer (K5, COSMED, Italy). All participants received prior instruction and completed a warm-up to ensure maximal effort during the test.
Muscular strength was assessed with an isometric chest press using a device (HUR, Finland). Before testing, participants received instruction and demonstration to ensure proper technique and maximal voluntary effort. Each participant performed a single maximal contraction, and the peak value was recorded for analysis.
Muscular endurance was evaluated with the 1 min arm curl test at 60% of the individual’s pre-assessed 1RM. While seated, participants performed as many repetitions as possible within 1 min, following a consistent range of motion under verbal supervision.
Flexibility was assessed with the behind-the-back reach test to evaluate shoulder mobility. The shortest distance between the fingertips of both hands was measured using a standard measuring tape. The test was conducted on both the affected and unaffected sides. When both sides were impaired, the more functional or less symptomatic side was classified as unaffected.
A trained safety officer was present during all assessments, and all researchers involved had received prior safety training to ensure standardized measurement procedures and participant safety.
2.5 Statistical analysis
Data were analyzed using SPSS version 28.0 (IBM Corp., Armonk, NY, United States) to compute means and standard deviations. The Shapiro–Wilk test confirmed a normal distribution across all groups and time points (p > 0.05), validating the use of parametric tests. Its appropriateness for small samples supports this choice.
Two-way repeated measures analysis of variance was used to examine the effects of training group (HIRT vs. MIRT) and time (pre- vs. post-intervention) on BMD and physical fitness. Within-group changes were analyzed using a paired t-test. Statistical significance was set at p < 0.05. Per-protocol analysis was conducted, excluding participants who withdrew before post-testing. No imputation methods were applied for missing data.
3 Results
3.1 Participants’ physical characteristics
The Shapiro–Wilk test confirmed a normal distribution in the selected sample (p > 0.05). Due to irregular attendance or health issues, the final sample comprised 16 participants who completed either the HIRT or MIRT program. Physical characteristics are presented in Table 1, and AIS classifications are shown in Table 2. No statistically significant differences were observed between groups in age, height, body weight, body mass index, or duration of disability (p > 0.05) (Table 1).
Participants in both groups were classified as AIS grade B and presented with comparable levels of SCI, with neurological injury levels ranging from T4 to T9 (Table 2). No apparent differences in AIS classification or neurological level were observed between groups.
Training volume was monitored using energy expenditure metrics to ensure equivalent load across intervention types. Analysis revealed no statistically significant difference in mean energy expenditure between the HIRT and MIRT groups (p = 0.869), confirming comparability in training volume (Table 3).
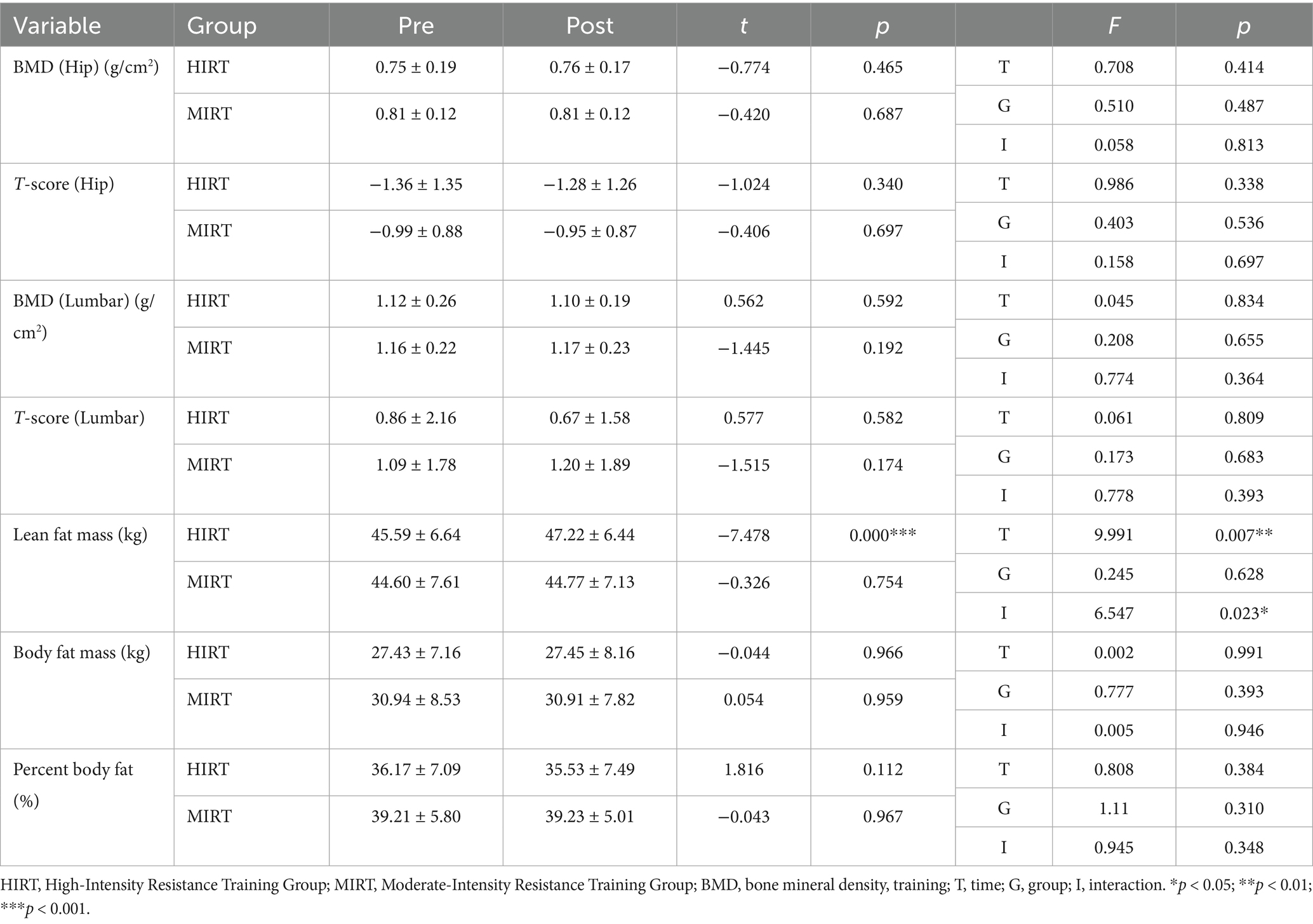
3.2 Extended body composition
A significant group-by-time interaction was observed for lean body mass (p < 0.05), along with a significant main effect of time (p < 0.01). The HIRT group demonstrated a significant post-training increase in lean mass (p < 0.001), whereas the MIRT group exhibited no change (p > 0.05) (Table 4).
In contrast, no significant changes were observed in fat mass or percent body fat (p > 0.05). Similarly, no significant group-by-time interaction or main effects were found for hip BMD or T-scores (p > 0.05). Lumbar BMD and T-scores also showed non-significant results across all effects (p > 0.05) (Table 4).
3.3 Functional fitness
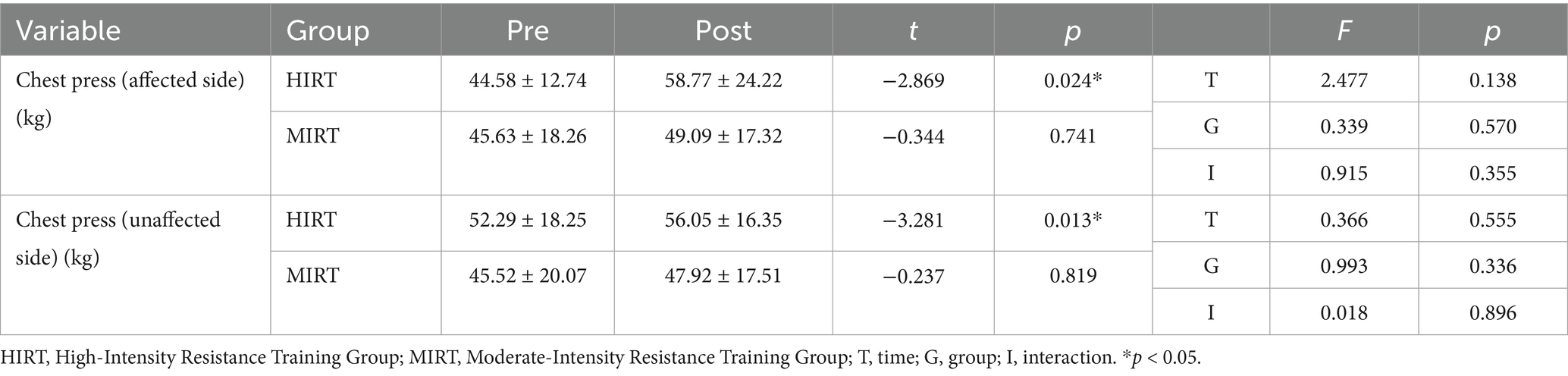
Functional fitness outcomes showed varied responses across domains. In muscular strength, chest press results revealed no significant group-by-time interaction or main effects (p > 0.05). However, paired t-tests indicated a significant within-group improvement in the HIRT group (p < 0.05), whereas no significant change was observed in the MIRT group (p > 0.05) (Table 5).
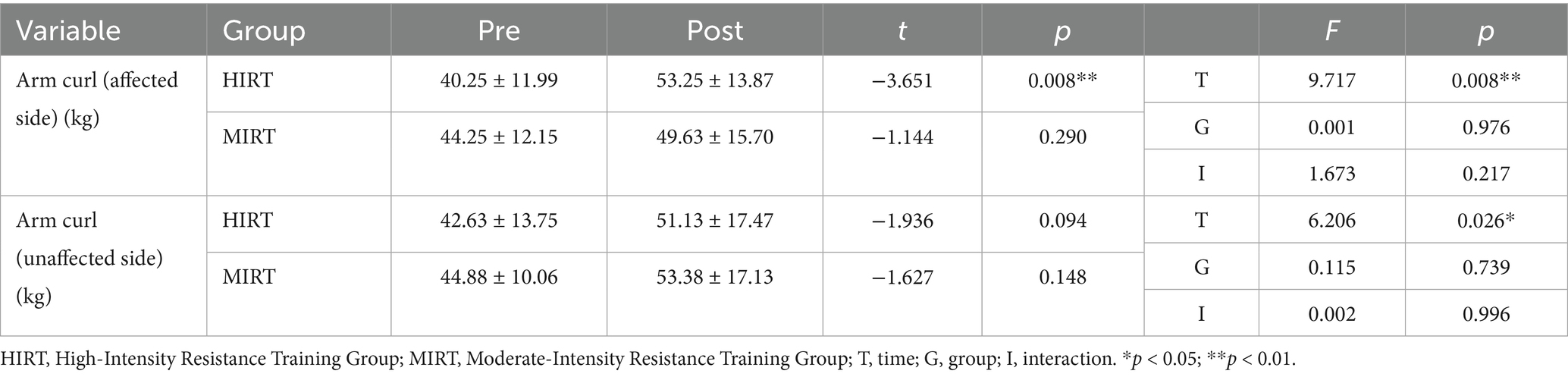
For muscular endurance, on the affected side, a significant main effect of time was found (p < 0.01), though no interaction or group effects were observed (p > 0.05). Only the HIRT group demonstrated a significant within-group improvement (p < 0.01). On the unaffected side, a significant main effect of time was also observed (p < 0.05); however, neither group showed significant changes in within-group comparisons (p > 0.05) (Table 6).
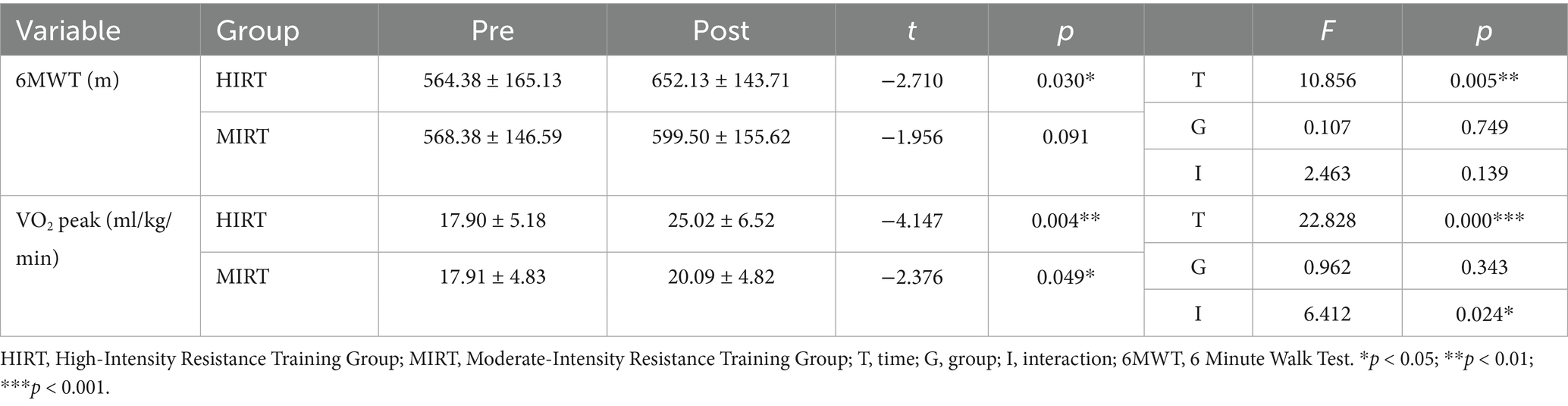
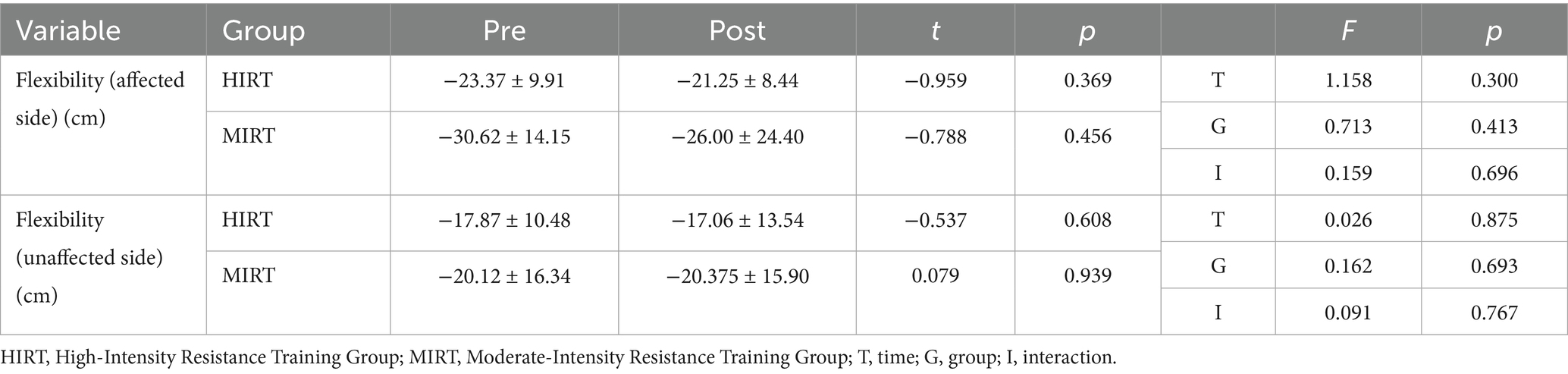
In terms of cardiorespiratory endurance, the 6 Minute Wheelchair Ambulation Test revealed a significant time effect (p < 0.01), with only the HIRT group showing significant post-training improvement (p < 0.05), while the MIRT group showed no change (p > 0.05). VO₂peak results demonstrated a significant group-by-time interaction (p < 0.05) along with a robust time effect (p < 0.001). Both groups improved significantly after training (HIRT: p < 0.01; MIRT: p < 0.05) (Table 7). Finally, flexibility measures showed no significant effects on either side (p > 0.05) (Table 8).
4 Discussion
The BMD in SCI is affected by physical inactivity, increased adiposity, and impaired nutrient absorption (24, 25). Regular physical activity remains one of the most effective strategies for improving BMD (26). Mechanical loading through repeated muscle contractions and relaxations generates stress on bones, which increases the load borne by the skeletal system. This process minimizes bone resorption and helps maintain or improve BMD (27). Individuals with SCI, however, typically have reduced BMD compared to those without SCI, predisposing them to a higher risk of osteoporosis and fractures (28). For this population, consistent exercise is critical for preserving good BMD.
No significant change in BMD (p > 0.05) was observed over the 8-week intervention, likely reflecting the need for longer durations. In this study, BMD was assessed at the hip and lumbar spine, which are among the most fracture-prone sites in individuals with SCI and are clinically relevant for monitoring skeletal health. Although upper extremity BMD was not included, the selected regions represent key weight-bearing sites and are commonly used as proxies for overall skeletal status in clinical practice. Furthermore, given the high prevalence of osteoporotic fractures in the hip and spine among individuals with motor-complete SCI, as noted in our methodology, the study prioritized these regions to ensure both clinical relevance and consistency with prior SCI-related BMD research. Previous studies suggest that measurable osteogenic adaptations in individuals with SCI require at least 12 months of sustained high intensity loading (29, 30). Future research employing longer interventions, potentially combined with nutritional or pharmacological support, may further clarify the capacity of for exercise to promote measurable skeletal adaptations in SCI.
Exercise intensity also plays a crucial role. Studies suggest that intensity may have a greater impact than frequency or modality on promoting bone metabolism (31). Moderate-to high-intensity resistance training increases growth hormone secretion and osteoblast activity, thereby enhancing bone strength (32, 33). Although the intensity was individualized in this study, future protocols should incorporate progressive overload to better induce musculoskeletal adaptation.
The HIRT participants showed significant increases in lean mass (p < 0.001), which, while not directly improving BMD in the current timeframe, may contribute to future skeletal integrity by increasing axial loading and promoting muscle-bone interaction—critical precursors for long-term osteogenesis in SCI. According to a previous study (34), regular exercise in individuals with SCI resulted in significant increases in muscle mass. Such changes benefit not only BMD but also metabolic health and functional independence, especially in those reliant on upper-body strength. By contrast, the lack of lean mass improvement in the MIRT group may be partly attributed to the relatively low intensity of the resistance component, which was likely insufficient to induce hypertrophic adaptations.
The muscular strength and endurance gains in the HIRT group likely resulted from hypertrophic adaptation to high-intensity training. These findings align with prior research showing that hypertrophy improves force output, delays fatigue, and enhances physical performance (35). Muscle gains may also underlie improvements in oxygen uptake and cardiorespiratory fitness, consistent with evidence that resistance and interval training increase capillary density and cardiac output (36).
Despite these benefits, fat mass did not significantly decrease in either group, supporting previous findings that short-term resistance training alone has limited effects on body fat, unless combined with diet or extended duration (37). Similarly, 6 weeks of moderate-to-high intensity interval training improved strength metrics but did not significantly alter fat mass (13). Programs integrated with nutritional strategies may be required for favorable changes in fat composition.
Flexibility results were similarly limited, likely due to repetitive upper-body training and wheelchair-related biomechanical constraints (4). Muscle tightness from upper limb dominance underscores the need for adjunct flexibility or mobility interventions. Resistance training alone may be insufficient for improving joint range of motion, highlighting the value of posture- and flexibility-focused programs.
While HIRT yielded modest gains in body composition, its superior time efficiency, approximately 40% greater than that of MIRT, makes it a practical and scalable option for individuals with SCI (38). Given their time and physical limitations, HIRT provides an efficient model for enhancing fitness. Therefore, careful monitoring of intensity progression and recovery is essential to ensure safety and long-term adherence, especially in populations with limited mobility and autonomic regulation. Furthermore, incorporating behavioral support strategies and adaptive equipment may enhance program accessibility and support sustainable engagement in everyday environments, aligning with community-based physical activity goals. These findings provide actionable insights for designing inclusive, time-efficient training strategies that address both physiological and environmental barriers to exercise in the SCI population.
In conclusion, this study suggests that HIRT effectively improves lean mass, muscular strength, endurance, and cardiorespiratory fitness in individuals with SCI. While flexibility may require joint-specific or postural interventions, the overall musculoskeletal improvements observed in the HIRT group suggest potential benefits for long-term functional independence and health. Given the importance of lean mass in reducing the risks associated with metabolic syndrome and osteoporosis, HIRT emerges as a time-efficient and scalable rehabilitation strategy. Moreover, its feasibility within limited timeframes makes it a promising option for promoting community-based physical activity and improving health outcomes in populations with mobility impairments. Although the sample size was modest, it reflects the inherent challenges of recruiting individuals with motor-complete SCI into controlled training trials, and the findings nevertheless provide clinically meaningful insights for this underserved population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board (IRB) of Konkuk University (IRB No. 7001355-202008-HR-397). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SK: Writing – original draft, Methodology. JL: Investigation, Writing – review & editing, Formal analysis. WK: Project administration, Writing – review & editing. SJ: Investigation, Writing – review & editing, Formal analysis. YB: Writing – review & editing, Investigation, Formal analysis. HL: Formal analysis, Investigation, Writing – review & editing. JK: Formal analysis, Writing – review & editing, Investigation. KA: Writing – review & editing, Data curation, Visualization. NP: Formal analysis, Investigation, Writing – review & editing. SS: Writing – original draft, Data curation, Formal analysis, Visualization, Conceptualization, Project administration, Supervision, Methodology, Writing – review & editing, Investigation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
This study was supported by the KU Research Professor Program of Konkuk University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BMD, bone mineral density; HIIT, high-intensity interval training; MICT, moderate-intensity continuous training; HIRT, high-intensity resistance training; MIRT, moderate-intensity resistance training; SCI, spinal cord injury.
References
1. Shin, HS. Etiology and epidemiology of spinal cord injury in Korea. J Korean Med Assoc. (2020) 63:589–95. doi: 10.5124/jkma.2020.63.10.589
2. Lu, Y, Shang, Z, Zhang, W, Pang, M, Hu, X, Dai, Y, et al. Global incidence and characteristics of spinal cord injury since 2000-2021: a systematic review and meta-analysis. BMC Med. (2024) 22:285. doi: 10.1186/s12916-024-03514-9
3. Haisma, JA, van der Woude, LH, Stam, HJ, Bergen, MP, Sluis, TA, and Bussmann, JB. Physical capacity in wheelchair-dependent persons with a spinal cord injury: a critical review of the literature. Spinal Cord. (2006) 44:642–52. doi: 10.1038/sj.sc.3101915
4. Trudel, D, Duley, J, Zastrow, I, Kerr, EW, Davidson, R, and MacDermid, JC. Rehabilitation for patients with lateral epicondylitis: a systematic review. J Hand Ther. (2004) 17:243–66. doi: 10.1197/j.jht.2004.02.011
5. Ramnemark, A, Nyberg, L, Lorentzon, R, Olsson, T, and Gustafson, Y. Hemiosteoporosis after severe stroke, independent of changes in body composition and weight. Stroke. (1999) 30:755–60. doi: 10.1161/01.str.30.4.755
6. Jones, LM, Legge, M, and Goulding, A. Intensive exercise may preserve bone mass of the upper limbs in spinal cord injured males but does not retard demineralisation of the lower body. Spinal Cord. (2002) 40:230–5. doi: 10.1038/sj.sc.3101286
7. Dolbow, DR, Gorgey, AS, Daniels, JA, Adler, RA, Moore, JR, and Gater, DR. The effects of spinal cord injury and exercise on bone mass: a literature review. Neurorehabil Neural Repair. (2011) 29:261–9. doi: 10.3233/NRE-2011-0702
8. Jacobs, PL, Nash, MS, and Rusinowski, JW. Circuit training provides cardiorespiratory and strength benefits in persons with paraplegia. Med Sci Sports Exerc. (2001) 33:711–7. doi: 10.1097/00005768-200105000-00005
9. Astorino, TA, and Thum, JS. Interval training elicits higher enjoyment versus moderate exercise in persons with spinal cord injury. J Spinal Cord Med. (2018) 41:77–84. doi: 10.1080/10790268.2016.1235754
10. Astorino, TA, and Thum, JS. Within-session responses to high-intensity interval training in spinal cord injury. Disabil Rehabil. (2018) 40:444–9. doi: 10.1080/09638288.2016.1260648
11. Mcleod, JC, Diana, H, and Hicks, AL. Sprint interval training versus moderate-intensity continuous training during inpatient rehabilitation after spinal cord injury: a randomized trial. Spinal Cord. (2020) 58:106–15. doi: 10.1038/s41393-019-0345-6
12. Wirz, M, Mach, O, Maier, D, Benito-Penalva, J, Taylor, J, Esclarin, A, et al. Effectiveness of automated locomotor training in patients with acute incomplete spinal cord injury: a randomized, controlled, multicenter trial. J Neurotrauma. (2017) 34:1891–6. doi: 10.1089/neu.2016.4643
13. Kim, DI, Lee, H, Lee, BS, Kim, J, and Jeon, JY. Effects of a 6-week indoor hand-bike exercise program on health and fitness levels in people with spinal cord injury: a randomized controlled trial study. Arch Phys Med Rehabil. (2015) 96:2033–40.e1. doi: 10.1016/j.apmr.2015.07.010
14. D’Oliveira, GL, Figueiredo, FA, Passos, MC, Chain, A, Bezerra, FF, and Koury, JC. Physical exercise is associated with better fat mass distribution and lower insulin resistance in spinal cord injured individuals. J Spinal Cord Med. (2014) 37:79–84. doi: 10.1179/2045772313Y.0000000147
15. Pelletier, CA, Totosy de Zepetnek, JO, MacDonald, MJ, and Hicks, AL. A 16-week randomized controlled trial evaluating the physical activity guidelines for adults with spinal cord injury. Spinal Cord. (2015) 53:363–7. doi: 10.1038/sc.2014.167
16. Eitivipart, AC, de Oliveira, CQ, Arora, M, Middleton, J, and Davis, GM. Overview of systematic reviews of aerobic fitness and muscle strength training after spinal cord injury. J Neurotrauma. (2019) 36:2943–63. doi: 10.1089/neu.2018.6310
17. Pooryamanesh, L, Daneshmandi, H, Hadžić, V, Sekulić, D, and Kondrič, M. Eight-week exercise intervention improves shoulder pain and body posture of wheelchair athletes with spinal cord injury. J Sports Med Phys Fitness. (2024) 64:483–9. doi: 10.23736/s0022-4707.23.15414-4
18. Martinache, F, de Crouy, AC, Boutin, A, Duranteau, J, and Vigué, B. Early functional proprioceptive stimulation in high spinal cord injury: a pilot study. Front Rehabilit Sci. (2025) 6:1490904. doi: 10.3389/fresc.2025.1490904
19. Hicks, AL, Martin Ginis, KA, Pelletier, CA, Ditor, DS, Foulon, B, and Wolfe, DL. The effects of exercise training on physical capacity, strength, body composition and functional performance among adults with spinal cord injury: a systematic review. Spinal Cord. (2011) 49:1103–27. doi: 10.1038/sc.2011.62
20. Harnish, CR, Daniels, JA, and Caruso, D. Training response to high-intensity interval training in a 42-year-old man with chronic spinal cord injury. J Spinal Cord Med. (2017) 40:246–9. doi: 10.1080/10790268.2015.1136783
21. Li, X, Li, Q, Li, C, Zhang, C, Qian, J, and Zhang, X. Effect of high-intensity exercise training on functional recovery after spinal cord injury. Front Neurol. (2025) 16:1442004. doi: 10.3389/fneur.2025.1442004
22. National Rehabilitation Center. Development of a resistance circuit exercise program to improve the health and physical fitness of people with spinal cord injuries and preliminary verification of its effectiveness (2019). Available online at: https://www.nrc.go.kr/nrc/board/boardView.do?no=21794&fno=63&menu_cd=06_01&board_id=NRC_NOTICE_BOARD&bn=newsView&search_item=1&search_content=&pageIndex=23 (Accessed June 25, 2025).
23. Hinton, PS, Nigh, P, and Thyfault, J. Effectiveness of resistance training or jumping-exercise to increase bone mineral density in men with low bone mass: a 12-month randomized, clinical trial. Bone. (2015) 79:203–12. doi: 10.1016/j.bone.2015.06.008
24. Buchholz, AC, McGillivray, CF, and Pencharz, PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr. (2003) 77:371–8. doi: 10.1093/ajcn/77.2.371
25. Wucher, H, Ciangura, C, Poitou, C, and Czernichow, S. Effects of weight loss on bone status after bariatric surgery: association between adipokines and bone markers. Obes Surg. (2008) 18:58–65. doi: 10.1007/s11695-007-9258-0
26. Langsetmo, L, Hitchcock, CL, Kingwell, EJ, Davison, KS, Berger, C, Forsmo, S, et al. Physical activity, body mass index and bone mineral density-associations in a prospective population-based cohort of women and men: the Canadian multicentre osteoporosis study (CaMos). Bone. (2012) 50:401–8. doi: 10.1016/j.bone.2011.11.009
27. Howe, TE, Shea, B, Dawson, LJ, Downie, F, Murray, A, Ross, C, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. (2011):CD000333. doi: 10.1002/14651858.CD000333.pub2
28. Lazo, MG, Shirazi, P, Sam, M, Giobbie-Hurder, A, Blacconiere, MJ, and Muppidi, M. Osteoporosis and risk of fracture in men with spinal cord injury. Spinal Cord. (2001) 39:208–14. doi: 10.1038/sj.sc.3101139
29. van der Scheer, JW, Martin Ginis, KA, Ditor, DS, Goosey-Tolfrey, VL, Hicks, AL, West, CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. (2017) 89:736–45. doi: 10.1212/WNL.0000000000004224
30. Chen, SC, Lai, CH, Chan, WP, Huang, MH, Tsai, HW, and Chen, JJ. Increases in bone mineral density after functional electrical stimulation cycling exercises in spinal cord injured patients. Disabil Rehabil. (2005) 27:1337–41. doi: 10.1080/09638280500164032
31. Vincent, KR, and Braith, RW. Resistance exercise and bone turnover in elderly men and women. Med Sci Sports Exerc. (2002) 34:17–23. doi: 10.1097/00005768-200201000-00004
32. Aloia, JF, Rasulo, P, Deftos, LJ, Vaswani, A, and Yeh, JK. Exercise-induced hypercalcemia and the calciotropic hormones. J Lab Clin Med. (1985) 106:229–32.
33. Notomi, T, Lee, SJ, Okimoto, N, Okazaki, Y, Takamoto, T, Nakamura, T, et al. Effects of resistance exercise training on mass, strength, and turnover of bone in growing rats. Eur J Appl Physiol. (2000) 82:268–74. doi: 10.1007/s004210000195
34. Mastropietro, A, Peruzzo, D, Taccogna, MG, Sanna, N, Casali, N, Nossa, R, et al. Multiparametric MRI assessment of morpho-functional muscle changes following a 6-month Fes-cycling training program: pilot study in people with a complete spinal cord injury. JMIR Rehabilit Assist Technol. (2025) 12:e64825. doi: 10.2196/64825
35. Durán, FS, Lugo, L, Ramírez, L, and Eusse, E. Effects of an exercise program on the rehabilitation of patients with spinal cord injury. Arch Phys Med Rehabil. (2001) 82:1349–54. doi: 10.1053/apmr.2001.26066
36. Ordonez, FJ, Rosety, MA, Camacho, A, Rosety, I, Diaz, AJ, Fornieles, G, et al. Arm-cranking exercise reduced oxidative damage in adults with chronic spinal cord injury. Arch Phys Med Rehabil. (2013) 94:2336–41. doi: 10.1016/j.apmr.2013.05.029
37. Griffin, L, Decker, MJ, Hwang, JY, Wang, B, Kitchen, K, Ding, Z, et al. Functional electrical stimulation cycling improves body composition, metabolic and neural factors in persons with spinal cord injury. J Electromyogr Kinesiol. (2009) 19:614–22. doi: 10.1016/j.jelekin.2008.03.002
Keywords: neurological impairment, disability, resistance exercise, health promotion, rehabilitation training
Citation: Kim S, Lee J, Kim W, Jin S, Bae Y, Lee H, Kim J, An K, Park N and Shin S (2025) Effects of high-intensity resistance training on extended body composition and functional fitness after spinal cord injury with motor complete paraplegia: a randomized controlled trial study. Front. Public Health. 13:1678313. doi: 10.3389/fpubh.2025.1678313
Edited by:
Alfonso Mastropietro, National Research Council (CNR), ItalyReviewed by:
Mauro Marzorati, National Research Council (CNR), ItalyLucas Vieira Santos, Federal University of Viçosa, Brazil
Giovanna Rizzo, National Research Council (CNR), Italy
Copyright © 2025 Kim, Lee, Kim, Jin, Bae, Lee, Kim, An, Park and Shin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seyoung Shin, aG5qbTE1NUBuYXZlci5jb20=
 Seckjin Kim1
Seckjin Kim1 Hyunjong Lee
Hyunjong Lee Junghwan Kim
Junghwan Kim Seyoung Shin
Seyoung Shin