- Department of nursing, Women’s Hospital School of Medicine, Zhejiang University, Hangzhou, Zhejiang, China
Background: More than a quarter of women aged 15 to 49 who have had a partner worldwide have experienced varying degrees of intimate partner violence (IPV). Cultural differences lead to different perceptions of intimate relationship violence among women, as well as varying degrees and forms of intimate relationship violence they experience.
Aim: This study aimed to systematically evaluate the psychological experiences and needs of women who experienced intimate relationship violence during the perinatal period, helping clinical nursing staff identify manifestations of violence and provide targeted assistance.
Methods: We systematically searched PubMed, Cochrane Library, Web of Science, CINAHL, PsycINFO, Embase, CNKI, Wanfang Database, VIP Database, China Biomedical Literature Service System to involve relevant literature on the experience and needs of intimate relationship violence among perinatal women. The search period was from the establishment of the database to July 2025. An initial search using the keywords “intimate partner violence,” “pregnancy,” “perinatal,” and “qualitative research” retrieved 2,980 articles. We used JBI quality evaluation criteria to assess the quality of the included studies. This study followed the Enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) guidelines.
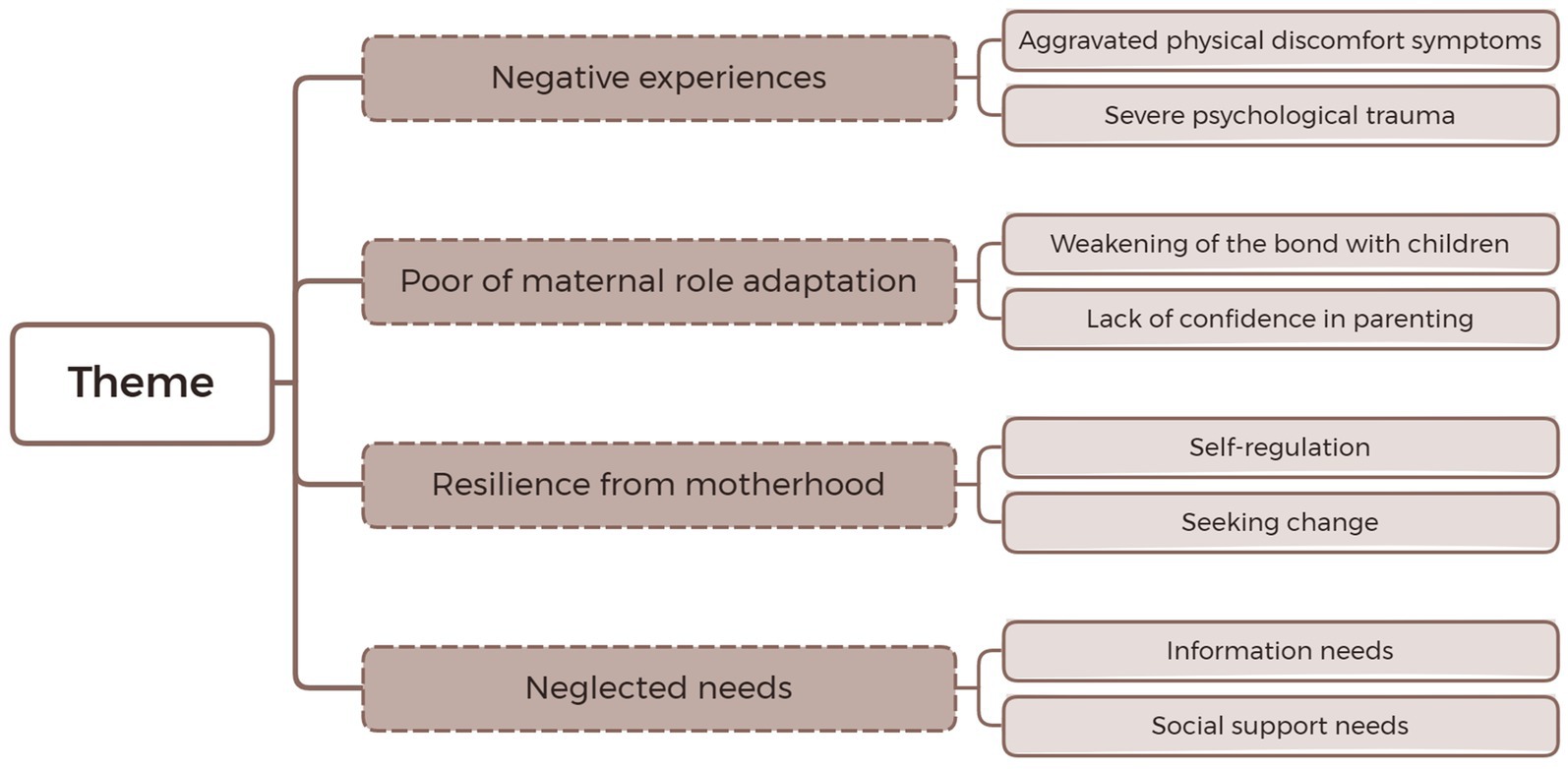
Results: A total of 16 studies were included. Four themes and nine sub themes were summarized and synthesized: Theme 1: Negative experiences (① aggravated physical discomfort symptoms, ② severe psychological trauma); Theme 2: Poor of maternal role adaptation (① Weakening of the bond with children, ② Lack of confidence in parenting), Theme 3: Resilience from motherhood (① Self-regulation, ② Seeking change); Theme 4: Neglected needs (① Information needs, ② Social support needs).
Conclusion: Perinatal women are prone to various forms of violence. This can lead to severe physical and psychological trauma as well as adverse pregnancy outcomes. Medical healthcare personnel should be trained to identify violent behaviors. Appropriate communication skills should be employed to expose intimate relationship violence. Training in skills such as parenting and psychological counseling should be provided to perinatal women. Social support organizations should offer economic, policy, legal and psychological assistance to perinatal women.
1 Introduction
Intimate relationship violence (IPV) refers to physical, sexual, or psychological harm inflicted by an intimate partner. It includes physical assault, sexual coercion, psychological abuse and controlling behavior (1). According to the World Health Organization, over a quarter (27%) of women aged 15 to 49 who have had a partner worldwide have experienced varying degrees of IPV (2). A systematic review study covering 40 + countries around the world indicates that physical violence accounts for 10%, psychological violence for 26%, sexual violence for 9%, verbal violence for 16%, and economic violence for 26%. Considering all types of violence together, the event rate for any IPV was 26% (3). IPV is a global public health issue. It seriously violates women’s human rights and has infiltrated individuals and families of different cultures, races, social classes, and economic levels around the world. It has caused serious consequences such as family instability and social conflicts (4).
WHO guidelines state the perinatal period refers to the duration of pregnancy and the year after birth (5). When women experience intimate partner violence during the perinatal period, it is referred to as perinatal intimate partner violence (6). The perinatal period is an important stage in a woman’s entire life cycle. The demands in terms of physiology, psychology, and the social support system have all changed. Therefore, experiencing IPV during the perinatal period will exacerbate the adverse consequences brought about by the violence. Research showed that 32.7% of women have experienced at least one IPV throughout the entire perinatal period (7). IPV can cause severe physical and psychological trauma and long-term sequelae for pregnant women during the perinatal period. For instance, injuries, gestational hypertension, chronic pain, gynecological diseases, pre-natal and post-natal depression, anxiety disorders, and post-traumatic stress syndrome (8–11). It also caused serious adverse pregnancy outcomes. Such as miscarriage, stillbirth, premature birth, low birth weight of newborns, and decreased rates of exclusive breastfeeding (2, 12–15). Exposure to IPV during the perinatal period can lead to some unhealthy behaviors, such as drug use, alcohol abuse, and suicidal tendencies. The offspring of women who suffered from IPV were at a higher risk of developing depression, anxiety, and other problems. This may have potential long-term effects on children’s health and social and psychological well-being (16). History of trauma was associated with a more severe clinical phenotype of perinatal depression (PND) and decreased resilience level (17).
Research showed that only half of all perinatal women who suffered from IPV choose to seek help. The majority of them obtain assistance from informal institutions such as family and friends (18). In Japan, only 6.9% of perinatal care institutions have implemented IPV screening (19). The reasons for society’s neglect of IPV are quite complex. For instance, there is the stigmatization of women who have suffered from IPV. Lack of relevant knowledge (20). Fear of revealing the consequences of domestic violence. The neglect of the importance of domestic violence by health service institutions and other departments (21). And concerns about the vulnerability of the fetus or pregnancy (22).
Many studies have shown that attention should be paid to and early prevention of perinatal IPV and intervention should be given to women who suffer from IPV, many research topics focused on epidemiological studies of perinatal IPV, such as the incidence of perinatal IPV, risk factor studies, and correlation studies (7, 23–27). But many perinatal women who suffer from IPV say they are not asked by obstetricians or midwives about intimate violence (28). This incongruity underscores the urgent need to re-evaluate support frameworks by critically analyzing lived experiences. A nuanced understanding of lived experiences is essential in informing effective, empathetic interventions. Qualitative research is particularly well-suited to capturing the Inner feelings and experiences of perinatal women suffering from IPV (29). And providing a contextualized framework for clinical practice. Meta-synthesis offers a valuable method for synthesizing qualitative evidence, allowing for a deeper exploration of complex emotional and psychological processes.
Therefore, this study aims to systematically integrate the real psychological experiences and needs of perinatal women who have experienced or are currently experiencing IPV. It seeks to answer the following questions: (1) What are the experiences and needs of perinatal women who experience intimate relationship violence? (2) What recommendations can be drawn from these studies to inform clinical practice, education, and future research to better support Perinatal women who experience intimate relationship violence?
2 Methods
2.1 Study design
This study is a meta integrated research on the real psychological experiences and needs of women who have experienced or are currently experiencing IPV during the perinatal period, and followed the guidelines for improving the transparency of qualitative research synthesis reports (ENTREQ) (30) for reporting.
2.2 Data sources
We retrieved qualitative studies on intimate relationship violence experienced by perinatal women from Chinese and English databases PubMed, Cochrane Library, Web of Science, CINAHL, PsycINFO, Embase, Ovid, as well as China National Knowledge Infrastructure, Wanfang Database, VIP Database, and China Biomedical Literature Service System using computer systems. The retrieval deadline is from the establishment of the database to July 2025. Searches were based on a combination of free-text keywords and indexed terms (MeSH) related to the terms: intimate partner violence, violence against women, domestic violence, pregnancy, perinatal, qualitative research etc. (The search strategy is shown in Supplementary File 1).
2.3 Eligibility criteria
According to PICoS, the inclusion criteria for research literature are as follows. Inclusion criteria: (1) The research subjects (population, P) are perinatal women, including family members or non-family members (friends or medical personnel) of perinatal women, and only the inner experiences, feelings, and coping strategies of perinatal women themselves are extracted; (2) The phenomenon of interest (I) refers to the true psychological experiences, feelings, needs, and coping strategies of pregnant women who have experienced or are currently experiencing intimate relationship violence throughout the entire perinatal period; (3) Context (Co) refers to women experiencing intimate relationship violence during the perinatal period; and (4) The research design (S) is qualitative research, including phenomenological research, narrative research, grounded theory, ethnography, and as well as the qualitative research part in mixed research. Exclusion criteria: (1) inability to retrieve full-text, incomplete data, and duplicate publications; (2) Non-Chinese and English literature; (3) Adopting mixed research methods but unable to separate qualitative data; and (4) Conference abstracts, dissertations. Data collection continued until feasible sample size was met.
2.4 Study selection and data extraction
Literature screening and data extraction were independently completed by two researchers, followed by cross checking. In case of any discrepancies, the decision was made by a third researcher. If a decision still cannot be reached, the research team will discuss the matter and reach a consensus before making a decision. Firstly, we used Endnote X9 software to remove duplicate literature, then read the title and abstract to exclude obviously unrelated literature. Finally, we read the entire text and included literature that was relevant to this study. The data extracted by two individuals using an Excel spreadsheet, including author, publication year, region, qualitative research methods, research subjects and number, interested phenomena, and main research results. Enter the main research results into Nvivo20 software for text content synthesis and integration.
2.5 Quality assessment
Two researchers conducted literature quality evaluations separately, and if the evaluation results were inconsistent, a third researcher made a decision. The qualitative research quality evaluation criteria published by the Australian JBI Evidence based Healthcare Center were adopted (31). The evaluation consists of 10 items, each evaluated as “yes,” “no,” “not applicable,” or “unclear.” The literature quality is divided into three levels: A, B, and C. Fully meet the evaluation criteria, with a low possibility of bias, rated as Class A; Partially meets the evaluation criteria, with a moderate possibility of deviation, classified as level B; Completely unsatisfied, with a high possibility of offset, classified as level C. The final inclusion of studies with quality evaluation levels of A and B.
2.6 Research team and reflexivity
The research team consisted of the four authors. The authors conceived this study. All four authors worked in maternity hospitals. The four authors have a relatively in-depth understanding of the physiology and psychology of perinatal women. And trained in systematic qualitative research. The researchers’ first language and sociocultural background differed from those of the study participants. To fully understand the context of the qualitative studies included in the research. The researchers completed the study under the guidance of team members who were proficient in English. Read repeatedly and understand the meaning of the participant’s words. Efforts were made to minimize bias caused by the researchers themselves. After repeated discussions, the research team reached a consensus on the research results.
2.7 Data analysis
This study adopted the Thomas and Hardens’ thematic synthesis method (32): (1) Repeatedly read, analyze, and interpret the meaning of relevant research results based on a full understanding of the philosophical ideas and methodology of qualitative research; (2) Combine and summarize similar results together to form a general category; and (3) Further categorize and form integrated concepts or explanations. Through these three steps, the reports incorporated into the literature were reported as a whole, and new core themes were distilled and given new interpretations. Two researchers independently coded and then aggregated the codes. In cases where there was disagreement, we consulted a third researcher for discussion and decision-making. The research team held multiple discussions on the final results until we reached a consensus. The details of the encoding formation process are shown in Table 1.
3 Results
3.1 Study characteristics
A preliminary search obtained 2,980 Chinese and English literature, and after removing duplicate literature, 2,154 were obtained. By reading the literature titles and abstracts, 31 literatures were obtained after excluding literature unrelated to the topic and non-Chinese English literature; After reading the full text, 15 articles that cannot be obtained and had low quality (with a quality evaluation level of C) were excluded. Finally, 16 articles were included, and the literature screening process is shown in Figure 1. 16 articles are all in English (20–22, 28, 29, 33–43), and the basic characteristics of the included articles are shown in Table 2. All included studies were published between 2016 and 2024 and conducted in 13 different countries, with a total of 388 participants. Participants were recruited through purposive sampling or convenience sampling methods, and the interview locations involved in the study included prenatal care facilities, prenatal clinics, participants’ homes, or other private rooms. Three studies (33, 39, 41) adopted a mixed method design, in which only qualitative data was extracted. Other studies (20–22, 28, 29, 34–38, 40, 42, 43) are qualitative studies that use case analysis, content analysis, exploratory research, grounded theory, explanatory phenomenology, and descriptive phenomenology methods. Qualitative data was collected through semi-structured interviews.
3.2 Quality assessment results
The quality evaluation of five articles was rated as A (20, 28, 29, 38, 40), and the quality evaluation of eleven articles was rated as B (21, 22, 33–37, 39, 41–43). Fifteen studies did not mention whether the philosophical foundation and methodology were consistent; Eleven studies (21, 22, 33–37, 39, 41–43) did not explain the researchers’ own situation from the perspective of cultural background and values; Twelve studies (21, 22, 33–39, 41–43) did not elaborate on the impact of researchers on the research or the influence of research on researchers. Of the sixteen studies, five studies were from Africa (20, 21, 39, 40, 42), four studies from Asia (28, 35, 37, 41), three studies from Europe (22, 29, 34), three studies from North America (36, 38, 43) and one study from South America (33). The results of the literature quality evaluation are shown in Table 3.
3.3 Key findings of the meta-synthesis
Thematic analysis of 56 key quotes from the 16 included studies generated four overarching themes: Theme 1: Negative experiences (① aggravated physical discomfort symptoms, ② severe psychological trauma); Theme 2: Poor of maternal role adaptation (① Weakening of the bond with children, ② Lack of confidence in parenting), Theme 3: Resilience from motherhood (① Self-regulation, ② Seeking change); Theme 4: Neglected needs (① Information needs, ② Social support needs). A chart was created to summarize the main themes and their interrelationships (Figure 2).
3.4 Qualitative meta-synthesis
3.4.1 Negative experience
3.4.1.1 Aggravated physical discomfort symptoms
There were various forms of IPV, among which the most serious and harmful was physical violence, which caused irreversible physical and mental trauma to women during the perinatal period (33, 37). Forms of physical violence include slapping, pushing, pulling, kicking, stepping, etc. (21), which leaved serious bruises on women and pose a serious threat to the safety of women and/or fetuses (42, 44). Sexual violence was also one of the important reasons for exacerbating women’s physical discomfort (21). The decrease in women’s willingness to engage in sexual activity during the perinatal period made it a high-risk period for sexual violence (21). Some women expressed that they were often forced or uncomfortable to have sexual intercourse with their husbands (21). Due to long-term stress, many perinatal women who suffered from IPV experience varying degrees of physical discomfort symptoms, such as headaches, insufficient or excessive sleep, nightmares, and decreased attention (40, 41). Physical violence leads to serious adverse pregnancy outcomes such as miscarriage, complications of pregnancy, fetal loss, and maternal deaths (20).
“My husband is lying on top of me when he wants to have sex, but I’m pregnant and I feel a lot of pain… makes me very sad (21).” “I always have a headache. I think too much, and whenever I think of my husband, I lose my appetite to eat (41).”
3.4.1.2 Severe psychological trauma
Emotional violence such as verbal attacks, indifference, manipulation, and control was more common and covert than physical violence, causing serious psychological trauma to women in the perinatal period (33, 37). Some women have expressed that their needs have been ignored (21, 41). Some women have reported experiencing neglect and verbal attacks from their intimate partners (20, 41). Some women expressed that their freedom was restricted (41). The husband controls their social activities, clothing choices, movements and finances (21, 40, 43). Their husbands monitor their phones and restrict their travel, this placed the women in a situation of existential isolation (41). They want to have social relationships with friends or relatives (41). Neglect, control and verbal insults caused long-lasting psychological trauma to women in the perinatal period, increases risk of perinatal depression (43, 45).
“I started crying after I got pregnant because my husband was always angry or scolding me, maybe I had depression (41).” “When I was playing social media, he immediately threw away my phone… he no longer allows me to use my phone (41).” “I want to go to work, and then he stopping me from going to work. Then he starts saying abusive words to me (43).”
3.4.2 Poor of maternal role adaptation
3.4.2.1 Weakening of the bond with children
Experiencing IPV during the perinatal period can lead to role transition disorders (36, 38). This makes it difficult to adapt to the role of a mother. It is not conducive to the formation of a good mother child attachment relationship (38). Some women expressed that the bond between themselves and their children has weakened (37). Some women believe that children are the result of their husbands’ violence (35). And because they detest their husbands, they also detest their children. Even by punishing the children to vent one’s dissatisfaction (35). As a result, they are unable to establish an emotional connection with their children (38).
“For me, he represented the domestic violence. The product of… a bad relationship. It was… wow. No, I did not love that child (38).” “When I was angry because of my husband’s violent behavior, I hit the baby in my stomach and empty myself in such a way (35).”
3.4.2.2 Lack of confidence in parenting
Some women frequently suffer from violence from their husbands (29). They are unable to fulfill their responsibilities as mothers (29, 36, 38). They cannot properly take care of their children (40). They lack the knowledge and skills for parenting, and ultimately lose confidence in parenting (38, 40). Some women expressed great guilt about their children (36). Some women have reported that their partners use their children to attack, manipulate, and threaten them (35). These dilemma all led to their inability to fully engage in their new roles, interact with children, and fulfill their responsibilities of raising children (38).
“I’m trying not to let my insecurities rule my parenting (36).” “After the birth, I was constantly doubting myself as a mother… Maybe I’m not doing enough? … I lost my bearings. Because him, he was constantly criticizing me (38).” “He (husband) now knows that the best way he can hurt me, attack me, or retaliate against me is through his children (35).”
3.4.3 Resilience from motherhood
3.4.3.1 Self-regulation
Perinatal women exposed to IPV apply situation improvement strategies to protect themselves and their children (35, 38). Some women choose to improve their situation through self-regulation. Self-regulation through self-actualization, comprehensive self-care skills, promoting positive self-concepts, resilience and strengthening spirituality (21, 35). And creating a good mood, self-relaxation, return attention through enjoyable activities, positive mental imagery and maintain authority, skills and empowerment (21, 35, 40). Maintaining and promoting self-confidence, self-esteem and self-control (35).
“I tried to calm down by shifting my focus, thinking about myself and the child in my belly, which made me stop thinking about violent things (35).” “Some pregnant women lost their self-confidence during pregnancy…I always told I’m very good and I have no problems (35).”
3.4.3.2 Seeking change
Out of the mother’s instinct to protect the fetus or the newborn. Women who have suffered from long-term IPV during the perinatal period are eager to change this undesirable situation (35, 36, 38). Some women ultimately chose to end unhealthy intimate relationships (33, 34, 36). Some women said they fought back against their husbands’ abuse and sought help from their families of origin (21).
“I should make a decision (to leave my husband) because I do not want my daughter to live in such an environment after giving birth (33).” “When my husband abused me, I retaliated against him. He wanted to hit me in the abdomen, so I fought back in self-defense (35).” “My father once said: Daughter, please leave him (your partner), we will take care of these children and send them to school (42).”
3.4.4 Neglected needs
3.4.4.1 Information needs
IPV related knowledge: Most women who suffered from IPV during the perinatal period expressed a lack of knowledge about IPV (20–22, 29, 39). They were eager to learn about it in order to identify and seek help as early as possible (20, 28, 35). When seeking help through online or mobile app platforms, it is necessary to ensure sufficient security and privacy during use (34). Legal and psychological counseling information: Perinatal women who had experienced intimate relationship violence hoped to receive legal and psychological support (21, 28, 34, 43). They also want to understand issues such as divorce, property division, and custody (34, 43). Meanwhile, the respondents hoped that society can provide them with multilingual legal publicity services (43).
“I wish I could know that not having financial support is also a form of abuse (43).” “We should have a flowchart… with a route for seeking help (22).” “I want to know how to get a divorce and about custody issues (34).” “I do not know if the health center has a psychologist who provides free counseling for me. I need psychological counseling (28).” “Abused mothers should be informed about support systems. What services can they receive from the health centers? Where can they go for psychological counseling? (35).”
3.4.4.2 Social support needs
Most informal social support system support from family and friends (21, 42). Perinatal women who have suffered from IPV long for support and assistance from the trustworthy people around them (42, 43). The support of family members, such as providing emotional support, advice, and practical assistance, can help them avoid the harm caused by violence (42). Formal social support system support from the health care system, welfare organization, social emergency, social work, forensic medicine, judicial and legal system, and police (28, 43). Some of the participants recognized the causes of violence in historical, cultural and structural elements (33). Therefore, a formal institution is needed to carry out strong intervention, such as taking measures to get women back into the job market (21, 28, 43). Or introduce policies aimed at changing the public’s perception of gender inequality (28, 33). Some women during the perinatal period craved support and assistance from professional medical institutions (43). Many women expressed that they hoped healthcare professionals can take their pain seriously and understand it (34).
“He (father) asked me to go home because he still loves me very much (42). “They (medical staff) should ask us what happened… who abused us (37).” “There should be a 24- hour telephone counseling center so that they can call for psychological advice (28),” “Society should react to violence against pregnant women… (28).” “The woman must be the person who takes care of the children and does not have the kind of support network that allows her to return to the job market, right? It’s always the woman who ends up giving up (33).”
4 Discussion
This study systematically synthesized 16 qualitative articles to explore the experiences and needs of perinatal women who have experienced or are currently experiencing IPV. Through coding, constant comparison, and analysis, these experiences were organized into four themes (Negative experiences, poor of maternal role adaptation, resilience from motherhood; and neglected needs).
The respondents in this study came from countries in Europe, Asia, Africa, North America and South America. This indicates that intimate relationship violence is widespread in most parts of the world. The research focuses on the countries in Africa and Asia (20, 21, 28, 35, 37, 39–42). This is consistent with the research results of Jean et al. (46). The rate of IPV is the highest in the Eastern Mediterranean region (46). Social and cultural factors have contributed to the increase in the incidence rate in this region. The countries in this region share many common social and cultural characteristics, including the “silence” surrounding IPV. Brunelli et al. (3) indicates that physical violence and sexual violence occur more frequently in Africa and the Middle East. Psychological violence is more common in the Americas and the Eastern Mediterranean region (3). Countries with higher incomes have a lower rate of violence (3). The research conducted by Chen et al. (47) indicate IPV prevalence in urban slums was notably high. Tran et al.’s (48) study also pointed out that young people from low-income families, those living in rural areas, and those with low educational attainment tend to be more tolerant of IPV.
Gender inequality resulting from factors such as race, history, economy, culture and social structure is an important influencing factor for perinatal women to suffer from IPV (33). And the constraints of traditional culture, religious beliefs, imperfect social systems, the fear of exposing the consequences of IPV, and the economic and emotional dependence on the abusers… all these complex factors have led them to choose to remain silent about IPV (33, 37, 41, 42). At the same time, the issue of basic sustenance makes it even more difficult for women to escape the predicament of IPV (20, 40). This is consistent with Park’s research (49) findings. Improving perceptions of gender inequality (at the individual level) and emphasizing democratic values (at the national level) are of great significance in reducing intimate relationship violence.
Intimate relationship violence encompasses physical, psychological, sexual and economic violence. It causes severe trauma to the physical and mental health of pregnant women during the perinatal period. Moreover, it leads to serious adverse pregnancy outcomes (21). Perinatal women who have suffered from IPV have demonstrated remarkable resilience and recovery ability in order to protect their children. Most women choose to endure IPV in an attempt to preserve the integrity of their families, which is consistent with the research findings of Gilliam et al. (50). The frequent occurrence and intensification of violence forced them to adopt other coping methods. For instance, diverting attention, praying to God, and enhancing spirituality can enable mothers to remain calm when dealing with domestic violence (21, 35). Some other women, in the end, chose to divorce their partners in order to protect their children. Most of these women are educated, financially capable, and have family members providing support (42).
IPV has affected the parenting experiences and responsibilities of women during the perinatal period. Their violent partners used a variety of strategies to attack the mother’s parenting practices. For example by undermining her authority, interrupting her sleep as well as the baby’s, using the children to manipulate her, abusing the children directly, and more (38, 51). The crying or screaming of the children can bring back traumatic memories of violence for them. This has dampened their confidence in parenting and made them unable to fully focus on taking care of their children (38). This is consistent with the research results of Chiesa et al. (52), IPV victimization diminished levels of communication, connectedness, lack of effective parenting skills, as well as higher levels of physical aggression, neglect and authoritarian parenting styles. Living in an environment of IPV for a long time can easily lead to the intergenerational transmission of violence. Children tend to imitate their fathers’ behaviors in conflict situations, which seriously affects their growth (53). Therefore, it is necessary to assist pregnant and postpartum women in ending IPV, while also providing them with parenting knowledge and skills assistance.
Perinatal women who have suffered from IPV encounter significant obstacles when seeking help. Many women lack awareness of the forms of mental violence, economic violence and sexual violence. They are not aware that they have suffered IPV (22). Firstly, relevant knowledge about IPV should be provided to pregnant and postpartum women. They should be made aware that they have suffered from IPV. And they should take immediate measures and seek help to protect themselves and their children. Secondly, provide training on violence prevention and perinatal health care knowledge to the spouses. This helps men enhance their understanding of pregnancy-related matters (28). Studies (21, 39) have shown that the majority of IPV survivors rely on their informal support networks, such as family, friends, acquaintances, relatives, neighbors, etc. Raise public awareness of IPV. This can enable members of informal support organizations to recognize the dangers of IPV. Provide assistance to women and children.
The World Health Organization proposed that routine questioning of IPV was a right of perinatal women, a responsibility of healthcare providers, and a part of safe and complete routine prenatal care (29). Develop intervention guidelines for healthcare professionals to identify and manage perinatal IPV and eliminate violent behavior (35). Midwives should establish a more trusting and close relationship with pregnant women during the perinatal period (29). Their cultural values and language should be respected. Cultural security is a factor that determines whether they are willing to disclose information about IPV (54). At the same time, they should ensure safety and privacy during the conversation (37). Healthcare personnel can use simple questionnaire surveys or euphemistic questions such as “How have you been living recently?” and “What happens when you have different opinions with your partner?” as entry points to inquire about the sensitive topic of IPV (34, 55). Consultation via a questionnaire from an obstetric clinic or video on an online platform is acceptable. For example, video counseling is provided through e-health, and some “quick exit” buttons are set to ensure that women can use it safely (34). Provide written information materials related to IPV for women in the perinatal period, including response procedures and contact information for supporting organizations, such as placing written materials on bulletin boards in hospitals or health service centers (22).
Women who suffered from IPV during the perinatal period often bore significant physical and mental pressure for a long time. Taghizadeh (56) offered “problem-solving” skills training courses for women suffering from IPV at health centers, taught by systematically trained midwives on the best ways to cope with IPV. Can establish peer support groups to alleviate the loneliness of women suffering from IPV during the perinatal period by sharing stories from other women (34). Mercier et al. (57) systematically reviewed intervention measures for intimate relationship violence experienced by perinatal women, including cash assistance, family visits, counseling and education. Provide life skills training for perinatal women who have suffered from IPV (58). This can reduce IPV and improve the quality of the relationship. The specific training contents including conflict management, effective communication, anger management, problem-solving, emotional regulation, and stress management. Enhancing spirituality can enhance maternal–infant attachment behaviors (59). It helps protect mothers from the negative impacts of IPV.
Social formal organizations should also be aware of the dangers of IPV. The healthcare system, welfare organizations, forensic medicine, social work and legal institutions should collaborate together (28). Provide personalized and implementable assistance to women. For instance, providing employment, housing, child-rearing, and insurance-related policies. Offering cash assistance, training programs and education. Help women to end unhealthy relationships with their partners as soon as possible. Provide psychological counseling services. Conduct training on dealing with violence to enhance women’s safety (28, 39).
5 Limitations
Some limitations in our study should be considered. The inclusion of only English and Chinese publications may have introduced language bias. Additionally, the relatively small number of studies included (n = 16) may also reflect publication bias or gaps in qualitative research on Perinatal IPV in different regions contexts. Most studies do not mention the race, religion, and economic status of respondents, so there may be cultural differences in the results of this study.
6 Conclusion
This meta-analysis provides a systematic review of the psychological experiences and needs of perinatal women who experience intimate relationship violence, revealing that they suffer from severe psychological and physiological trauma Unable to adapt to the role of a mother, she longed to change the situation in order to provide protection for her child. And crave a comprehensive social support network to provide support and assistance. Perinatal IPV screening should be included in routine maternal and child health services, and healthcare workers need to receive training to remain sensitive and alert to issues that may be related to IPV. Provide them with timely psychological counseling and referral services. Strengthen the publicity and education on IPV, and enhance public awareness of this issue. The social support system should provide assistance to women who have experienced IPV during the perinatal period from multiple aspects such as economy, policies, laws and regulations, and psychological support. In the future, qualitative studies with large samples, multi-centers and trans-regions should be carried out. To explore the influence of different culture, race and economic level on perinatal IPV. This in turn provides more targeted clinical interventions.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
RW: Writing – original draft, Conceptualization, Data curation, Methodology, Supervision, Writing – review & editing. SW: Data curation, Methodology, Writing – review & editing. KY: Data curation, Methodology, Writing – review & editing. HX: Conceptualization, Data curation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1678360/full#supplementary-material
References
1. Kyle, J. Intimate partner violence. Med Clin North Am. (2023) 107:385–95. doi: 10.1016/j.mcna.2022.10.012
2. White, SJ, Sin, J, Sweeney, A, Salisbury, T, Wahlich, C, Montesinos Guevara, CM, et al. Global prevalence and mental health outcomes of intimate partner violence among women: a systematic review and Meta-analysis. Trauma Violence Abuse. (2024) 25:494–511. doi: 10.1177/15248380231155529
3. Brunelli, L, Pennisi, F, Pinto, A, Cella, L, Parpinel, M, Brusaferro, S, et al. Prevalence and screening tools of intimate partner violence among pregnant and postpartum women: a systematic review and Meta-analysis. Eur J Investig Health Psychol Educ. (2025) 15:161. doi: 10.3390/ejihpe15080161
4. Babatope, AE, Ibirongbe, DO, Adewumi, IP, Ajisafe, DO, Fadipe, OA, Popoola, GO, et al. Spatial variation of intimate partner violence and its public health implication: a cross-sectional study. BMC Public Health. (2025) 25:2744. doi: 10.1186/s12889-025-24123-y
5. World Health Organization. Guide for integration of perinatal mental health in maternal and child health services. Geneva: World Health Organization (2022).
6. Sharps, PW, Laughon, K, and Giangrande, SK. Intimate partner violence and the childbearing year: maternal and infant health consequences. Trauma Violence Abuse. (2007) 8:105–16. doi: 10.1177/1524838007302594
7. Laughon, K, Hughes, RB, Lyons, G, Roarty, K, and Alhusen, J. Disability-related disparities in screening for intimate partner violence during the perinatal period: a population-based study. Womens Health Issues. (2025) 35:97–104. doi: 10.1016/j.whi.2024.12.001
8. Özkan-Şat, S, and Söylemez, F. The Association of Domestic Violence during Pregnancy with maternal psychological well-being in the early postpartum period: a sample from women with low socioeconomic status in eastern Turkey. Midwifery. (2024) 134:104000. doi: 10.1016/j.midw.2024.104000
9. Thompson, NN, Mumuni, K, Oppong, SA, Sefogah, PE, Nuamah, MA, and Nkyekyer, K. Effect of intimate partner violence in pregnancy on maternal and perinatal outcomes at the Korle Bu teaching hospital, Ghana: an observational cross sectional study. Int J Gynaecol Obstet. (2023) 160:297–305. doi: 10.1002/ijgo.14375
10. Hou, F, Zhang, X, Cerulli, C, He, W, Mo, Y, and Gong, W. The impact of intimate partner violence on the trajectory of perinatal depression: a cohort study in a Chinese sample. Epidemiol Psychiatr Sci. (2020) 29:e133. doi: 10.1017/S2045796020000463
11. Gürkan, ÖC, Ekşi, Z, Deniz, D, and Çırçır, H. The influence of intimate partner violence on pregnancy symptoms. J Interpers Violence. (2020) 35:523–41. doi: 10.1177/0886260518789902
12. Khalid, N, Zhou, Z, and Nawaz, R. Exclusive breastfeeding and its association with intimate partner violence during pregnancy: analysis from Pakistan demographic and health survey. BMC Womens Health. (2024) 24:186. doi: 10.1186/s12905-024-02996-2
13. Lockington, EP, Sherrell, HC, Crawford, K, Rae, K, and Kumar, S. Intimate partner violence is a significant risk factor for adverse pregnancy outcomes. AJOG Glob Rep. (2023) 3:100283. doi: 10.1016/j.xagr.2023.100283
14. Do, HP, Vo, TV, Murray, L, Baker, PRA, Murray, A, Valdebenito, S, et al. The influence of childhood abuse and prenatal intimate partner violence on childbirth experiences and breastfeeding outcomes. Child Abuse Negl. (2022) 131:105743–13. doi: 10.1016/j.chiabu.2022.105743
15. Kana, MA, Safiyan, H, Yusuf, HE, Musa, ASM, Richards-Barber, M, Harmon, QE, et al. Association of intimate partner violence during pregnancy and birth weight among term births: a cross-sectional study in Kaduna, northwestern Nigeria. BMJ Open. (2020) 10:e036320. doi: 10.1136/bmjopen-2019-036320
16. Wolfe, DA, Crooks, CV, Lee, V, McIntyre-Smith, A, and Jaffe, PG. The effects of children's exposure to domestic violence: a Meta-analysis and critique. Clin Child Fam Psychol Rev. (2003) 6:171–87. doi: 10.1023/a:1024910416164
17. Bianciardi, E, Barone, Y, Lo Serro, V, De Stefano, A, Giacchetti, N, Aceti, F, et al. Inflammatory markers of perinatal depression in women with and without history of trauma. Riv Psichiatr. (2021) 56:237–45. doi: 10.1708/3681.36671
18. Stiller, M, Wilson, ML, Bärnighausen, T, Adedimeji, A, Lewis, E, and Abio, A. Help-seeking behaviors among survivors of intimate partner violence during pregnancy in 54 low- and middle-income countries: evidence from demographic and health survey data. BMC Public Health. (2025) 25:413. doi: 10.1186/s12889-025-21421-3
19. Maruyama, N, and Horiuchi, S. Views from midwives and perinatal nurses on barriers and facilitators in responding to perinatal intimate partner violence in Japan: baseline interview before intervention. BMC Health Serv Res. (2024) 24:1234. doi: 10.1186/s12913-024-11737-y
20. Hatcher, AM, Woollett, N, Pallitto, CC, Mokoatle, K, Stöckl, H, and Garcia-Moreno, C. Willing but not able: patient and provider receptiveness to addressing intimate partner violence in Johannesburg antenatal clinics. J Interpers Violence. (2019) 34:1331–56. doi: 10.1177/0886260516651094
21. Katushabe, E, Ndinawe, J, Editor, A, Agnes, K, Nakidde, G, Asiimwe, JB, et al. “He stepped on my belly” an exploration of intimate partner violence experience and coping strategies among pregnant women in southwestern-Uganda. (2023).
22. Garnweidner-Holme, LM, Lukasse, M, Solheim, M, and Henriksen, L. Talking about intimate partner violence in multi-cultural antenatal care: a qualitative study of pregnant women's advice for better communication in south-East Norway. BMC Pregnancy Childbirth. (2017) 17:1–10. doi: 10.1186/s12884-017-1308-6
23. Dai, X, Chu, X, Qi, G, Yuan, P, Zhou, Y, Xiang, H, et al. Worldwide perinatal intimate partner violence prevalence and risk factors for post-traumatic stress disorder in women: a systematic review and Meta-analysis. Trauma Violence Abuse. (2024) 25:2363–76. doi: 10.1177/15248380231211950
24. Lévesque, S, Medvetskaya, A, Julien, D, Clément, M, and Laforest, J. Prevalence and correlates of intimate partner violence in the perinatal period in a representative sample of Quebec mothers. Violence Vict. (2025) 40:19–38. doi: 10.1891/vv-2022-0069
25. Naseem, H, Park, S, Rowther, AA, Atif, N, Rahman, A, Perin, J, et al. Perinatal intimate partner violence and maternal-infant bonding in women with anxiety symptoms in Pakistan: the moderating role of breastfeeding. J Interpers Violence. (2025) 40:1934–58. doi: 10.1177/08862605241271364
26. Galbally, M, Watson, S, MacMillan, K, Sevar, K, and Howard, LM. Intimate partner violence across pregnancy and the postpartum and the relationship to depression and perinatal wellbeing: findings from a pregnancy cohort study. Arch Womens Ment Health. (2024) 27:807–15. doi: 10.1007/s00737-024-01455-z
27. Jackson, KT, Marshall, C, and Yates, J. Health-related maternal decision-making among perinatal women in the context of intimate partner violence: a scoping review. Trauma Violence Abuse. (2024) 25:1899–910. doi: 10.1177/15248380231198876
28. Barez, MA, Najmabadi, KM, Roudsari, RL, Bazaz, MM, and Babazadeh, R. "family and society empowerment": a content analysis of the needs of Iranian women who experience domestic violence during pregnancy: a qualitative study. BMC Womens Health. (2023) 23:370. doi: 10.1186/s12905-023-02525-7
29. Kirwan, C, Meskell, P, Biesty, L, Dowling, M, and Kirwan, A. Ipv routine enquiry in antenatal care: perspectives of women and healthcare professionals-a qualitative study. Violence Against Women. (2024) 31:10778012241231784. doi: 10.1177/10778012241231784
30. Tong, A, Sainsbury, P, and Craig, J. Consolidated criteria for reporting qualitative research (Coreq): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
31. Min, M, Hancock, DG, Aromataris, E, Crotti, T, and Boros, C. Experiences of living with juvenile idiopathic arthritis: a qualitative systematic review. JBI Evid Synth. (2022) 20:60–120. doi: 10.11124/jbies-21-00139
32. Thomas, J, and Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. (2008) 8:45. doi: 10.1186/1471-2288-8-45
33. Sánchez, ODR, Zambrano, E, Dantas-Silva, A, and Surita, FG. Perceptions of Brazilian women at a public obstetric outpatient clinic regarding domestic violence: a qualitative study. BMJ Open. (2023) 13:e071838. doi: 10.1136/bmjopen-2023-071838
34. Fernández López, R, de- León-de-León, S, Martin-de-las-Heras, S, Torres Cantero, JC, Megías, JL, and Zapata-Calvente, AL. Women survivors of intimate partner violence talk about using e-health during pregnancy: a focus group study. BMC Womens Health. (2022) 22:98. doi: 10.1186/s12905-022-01669-2
35. Barez, MA, Babazadeh, R, Roudsari, RL, Bazaz, MM, and Najmabadi, KM. Women's strategies for managing domestic violence during pregnancy: a qualitative study in Iran. Reprod Health. (2022) 19:58. doi: 10.1186/s12978-021-01276-8
36. Herbell, K, Li, Y, Bloom, T, Sharps, P, and Bullock, LFC. Keeping it together for the kids: new mothers’ descriptions of the impact of intimate partner violence on parenting. Child Abuse Negl. (2020) 99:99. doi: 10.1016/j.chiabu.2019.104268
37. Rishal, P, Joshi, SK, Lukasse, M, Schei, B, Swahnberg, K, Bjorngaard, JH, et al. They just walk away' - women's perception of being silenced by antenatal health workers: a qualitative study on women survivors of domestic violence in Nepal. Glob Health Action. (2016) 9:31838. doi: 10.3402/GHA.V9.31838
38. Lévesque, S, Rousseau, C, Lessard, G, Bigaouette, M, Fernet, M, Valderrama, A, et al. Qualitative exploration of the influence of domestic violence on motherhood in the perinatal period. J Fam Violence. (2022) 37:275–87. doi: 10.1007/s10896-021-00294-1
39. Yirgu, R, Wondimagegnehu, A, Qian, J, Milkovich, R, Zimmerman, LA, Decker, MR, et al. Needs and unmet needs for support Services for Recently Pregnant Intimate Partner Violence Survivors in Ethiopia during the Covid-19 pandemic. BMC Public Health. (2023) 23:725. doi: 10.1186/s12889-023-15634-7
40. Keynejad, RC, Bitew, T, Mulushoa, A, Howard, LM, and Hanlon, C. Pregnant women and health workers’ perspectives on perinatal mental health and intimate partner violence in rural Ethiopia: a qualitative interview study. BMC Pregnancy Childbirth. (2023) 23:78. doi: 10.1186/s12884-023-05352-8
41. Nhi, TT, Hanh, NTT, and Gammeltoft, TM. Emotional violence and maternal mental health: a qualitative study among women in northern Vietnam. BMC Womens Health. (2018) 18:58. doi: 10.1186/s12905-018-0553-9
42. Sigalla, GN, Mushi, D, and Gammeltoft, T. "staying for the children": the role of Natal relatives in supporting women experiencing intimate partner violence during pregnancy in northern Tanzania - a qualitative study. PLoS One. (2018) 13:e0198098. doi: 10.1371/journal.pone.0198098
43. Scott, SE, Laubacher, C, Chang, J, Miller, E, Bocinski, SG, and Ragavan, MI. Perinatal economic abuse: experiences, impacts, and needed resources. J Womens Health (Larchmt). (2024) 33:1536–53. doi: 10.1089/jwh.2024.0119
44. Guo, C, Wan, M, Wang, Y, Wang, P, Tousey-Pfarrer, M, Liu, H, et al. Associations between intimate partner violence and adverse birth outcomes during pregnancy: a systematic review and Meta-analysis. Front Med (Lausanne). (2023) 10:1140787. doi: 10.3389/fmed.2023.1140787
45. Dutta, I, and Sharma, D. Mothers at risk of postpartum depression and its determinants: a perspective from the urban Jharkhand, India. J Family Med Prim Care. (2025) 14:2853–60. doi: 10.4103/jfmpc.jfmpc_303_25
46. Jean Simon, D, Kondo Tokpovi, VC, Ouedraogo, A, Dianou, K, Kiragu, A, Olorunsaiye, CZ, et al. Intimate partner violence during pregnancy against 601,534 women aged 15 to 49 years in 57 Lmics: prevalence, disparities, trends and associated factors using demographic and health survey data. EClinicalMedicine. (2025) 86:103382. doi: 10.1016/j.eclinm.2025.103382
47. Chen, S, Ma, N, Kong, Y, Chen, Z, Niyi, JL, Karoli, P, et al. Prevalence, disparities, and trends in intimate partner violence against women living in urban slums in 34 low-income and middle-income countries: a multi-country cross-sectional study. EClinicalMedicine. (2025) 81:103140. doi: 10.1016/j.eclinm.2025.103140
48. Tran, TD, Nguyen, H, and Fisher, J. Attitudes towards intimate partner violence against women among women and men in 39 low- and middle-income countries. PLoS One. (2016) 11:e0167438. doi: 10.1371/journal.pone.0167438
49. Park, Y, Song, J, Wood, B, Gallegos, T, and Childress, S. A global examination on the attitudes toward intimate partner violence against women: a multilevel modeling analysis. Violence Against Women. (2025):10778012251338388. doi: 10.1177/10778012251338388
50. Gilliam, HC, Martinez-Torteya, C, Carney, JR, Miller-Graff, LE, and Howell, KH. "my cross to bear": mothering in the context of intimate partner violence among pregnant women in Mexico. Violence Against Women. (2024):10778012241289433. doi: 10.1177/10778012241289433
51. Bancroft, L, Silverman, J, and Ritchie, D. The batterer as parent: Addressing the impact of domestic violence on family dynamics. Thousand Oaks, California: SAGE Publications, Inc. (2012). Available online at: https://sk.sagepub.com/book/mono/the-batterer-as-parent/toc (Accessed July 30, 2025).
52. Chiesa, AE, Kallechey, L, Harlaar, N, Rashaan Ford, C, Garrido, EF, Betts, WR, et al. Intimate partner violence victimization and parenting: a systematic review. Child Abuse Negl. (2018) 80:285–300. doi: 10.1016/j.chiabu.2018.03.028
53. Meinck, F, Lu, M, Suresh, D, Cetin, M, Neelakantan, L, Hemady, C, et al. What are the mechanisms underpinning intergenerational transmission of violence perpetration? A realist review. Trauma Violence Abuse. (2025):15248380251361468. doi: 10.1177/15248380251361468
54. Spangaro, J, Herring, S, Koziol-Mclain, J, Rutherford, A, Frail, MA, and Zwi, AB. 'They Aren't really black fellas but they are easy to talk to': factors which influence Australian aboriginal women's decision to disclose intimate partner violence during pregnancy. Midwifery. (2016) 41:79–88. doi: 10.1016/j.midw.2016.08.004
55. Stewart, DE, Vigod, SN, MacMillan, HL, Chandra, PS, Han, A, Rondon, MB, et al. Current reports on perinatal intimate partner violence. Curr Psychiatry Rep. (2017) 19:26. doi: 10.1007/s11920-017-0778-6
56. Taghizadeh, Z, Pourbakhtiar, M, Ghasemzadeh, S, Azimi, K, and Mehran, A. The effect of training problem-solving skills for pregnant women experiencing intimate partner violence: a randomized control trial. Pan Afr Med J. (2018) 30:79. doi: 10.11604/pamj.2018.30.79.14872
57. Mercier, O, Fu, SY, Filler, R, Leclerc, A, Sampsel, K, Fournier, K, et al. Interventions for intimate partner violence during the perinatal period: a scoping review: a systematic review. Campbell Syst Rev. (2024) 20:e1423. doi: 10.1002/cl2.1423
58. Pazandeh, F, Askari, S, Fakari, FR, Safarzadeh, A, Haghighizadeh, MH, and Nasab, MB. Effect of life skills training on marital relations, self-esteem and anxiety levels of Iranian pregnant women exposed to intimate partner violence: a randomized controlled trial. BMC Psychol. (2025) 13:988. doi: 10.1186/s40359-025-03352-1
59. Tork Zahrani, S, Haji Rafiei, E, Hajian, S, Alavi Majd, H, and Izadi, A. The correlation between spiritual health and maternal-fetal attachment behaviors in pregnant women referring to the health centers in Qazvin, Iran. Int J Community Based Nurs Midwifery. (2020) 8:84–91. doi: 10.30476/ijcbnm.2019.81668.0
Keywords: intimate relationship violence, perinatal period, experience, demand, qualitative meta-synthesis
Citation: Wen R, Wang S, Yang K and Xu H (2025) Psychological experiences and needs of perinatal women experiencing intimate partner violence: a qualitative meta-synthesis. Front. Public Health. 13:1678360. doi: 10.3389/fpubh.2025.1678360
Edited by:
Dominic Azuh, Covenant University, NigeriaReviewed by:
Emanuela Bianciardi, University of Rome Tor Vergata, ItalyMalikeh Amel Barez, Islamic Azad University, Mashhad, Iran
Copyright © 2025 Wen, Wang, Yang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyan Xu, eHVob25neUB6anUuZWR1LmNu
 Ruifang Wen
Ruifang Wen Shanshan Wang
Shanshan Wang