- 1Department of Emergency Medicine, West China Hospital, Sichuan University/West China School of Nursing, Sichuan University, Chengdu, China
- 2Disaster Medical Center, Sichuan University, Chengdu, China
Aim: The purpose of this study was to explore the correlation between the mental health status and professional identity of Chinese nurses after the COVID-19 public health emergency.
Method: An e-questionnaire survey was designed, and nurses from 4 Chinese hospitals were included in our study. The questionnaires were used to measure nurses’ professional identity, mental health, and sleep quality. Logistic regression analyses were used to explore their relationships.
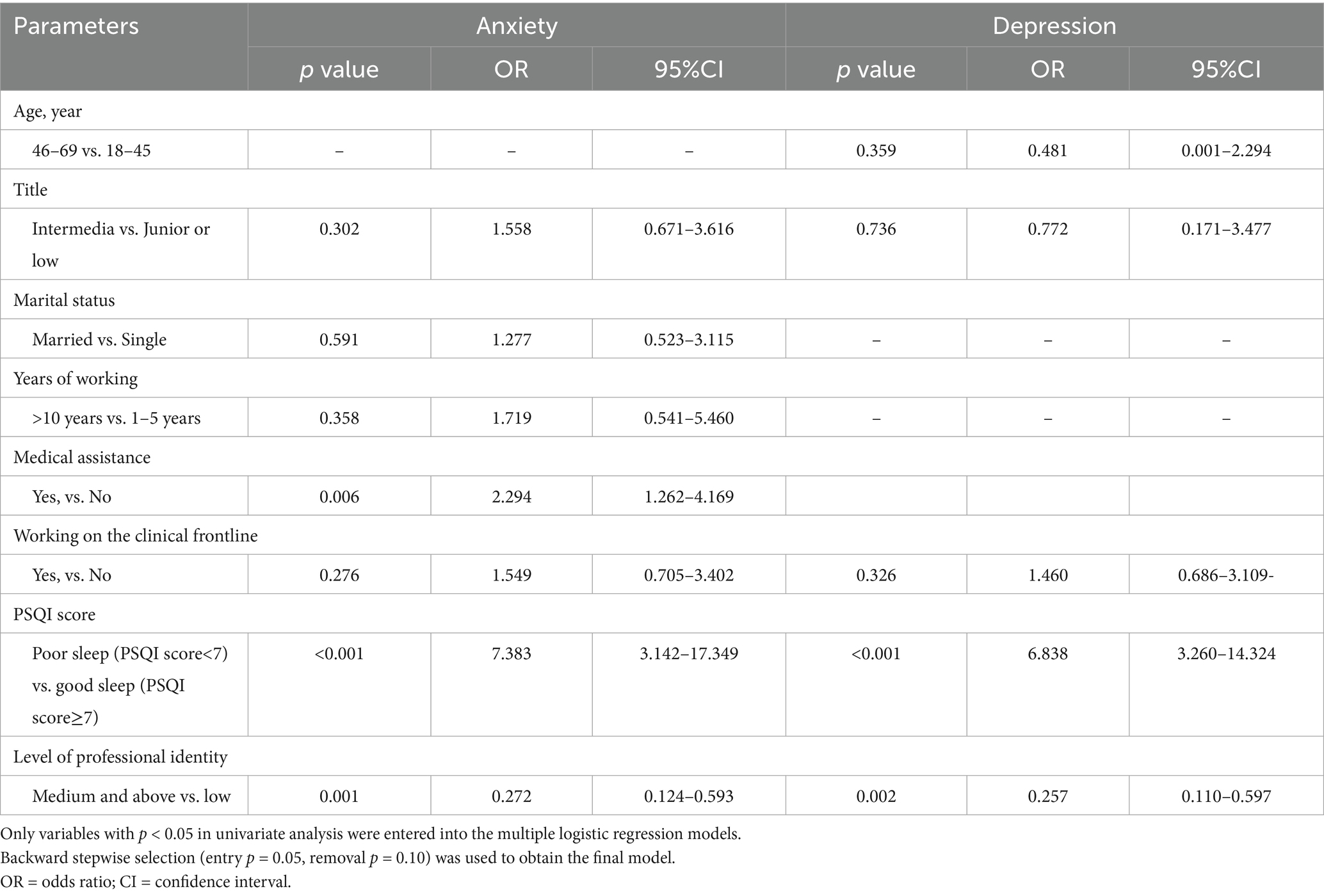
Results: The multiple logistic regression analysis suggested that medical assistance, PSQI score, and level of professional identity were independent risk factors for anxiety, and the results of multiple logistic regression analysis suggested that a medium level of professional identity and the PSQI score were independent factors for depression.
Discussion: The results show that nurses’ professional identity is negatively related to anxiety and depression after experiencing the COVID-19 public health emergency.
Implications for practice: After the COVID-19 public health emergency, managers urgently need to pay attention to nurses’ mental health issues, which may help improve nurses’ professional identity, increase their work enthusiasm, and benefit their career development.
Introduction
The COVID-19 pandemic, declared a Public Health Emergency of International Concern (PHEIC) by the World Health Organization, serves as a critical context for this study, providing a unique lens to examine the interplay between professional identity and mental health among nurses during a global health crisis. It is a special event of disease spread that will cause health, economic and social consequences and require coordinated actions by the government and society. Nurses play a key role in health caring, with more than half of health workers still on the clinical frontline, which increases the mental health risks in health workers (1). However, nurses are also considered assistants to doctors, which results in a poor impression and low social status of nursing work in the modern social environment (2). It has been shown that the COVID-19 public health emergency has increased heavy pressure on nurses, which has caused higher turnover and reduced the level of nurses’ professional identity level. Professional identity is the best predictor of the departure rate from nursing (3). The aging population is a severe issue, and nurses are shorthanded in China. These reasons lead to the heavy shortage of nursing staff (4).
Professional identity was defined as “one’s professional self-concept based on attributes, beliefs, values, motives, and experience” (5, 6), which plays a crucial role in nurses, and it has been changing constantly in nursing careers (7). One study reported that nurses are more likely to be mobile during major public health emergency (8). Previous research argued that nurses’ high level of professional identity can improve clinical performance (9), increase job retention (10, 11), and provide high-quality services (12).
Mental health is a multidimensional construct that includes emotional, cognitive, and behavioral well-being, and its disturbances commonly manifest as anxiety, depression, and sleep disorders in nurses after major public health events. Anxiety and depression are among the most prevalent and well-validated indicators of post-crisis psychological burden in nursing populations; therefore, the GAD-7 and SDS were selected in this study as standardized and widely used tools. Furthermore, a growing body of longitudinal and review evidence indicates a strong bidirectional relationship between sleep disturbance and psychological distress (13, 14): insomnia not only commonly co-occurs with anxiety and depression, but longitudinal studies and meta-analyses show that insomnia symptoms predict future onset of depressive and anxiety symptoms. For example, Baglioni et al. (15) reported that insomnia roughly doubles the risk of later depression in prospective studies, and mechanistic reviews identify disrupted sleep and circadian functioning as core processes in mood and anxiety disorders (16). Therefore, we included the PSQI to assess sleep quality as an integral dimension of mental health rather than limiting mental health to emotional symptoms alone.
Furthermore, sleep disturbance has a strong bidirectional relationship with psychological distress, and insomnia is both a predictor and a consequence of anxiety and depression. For this reason, the PSQI was included to assess sleep quality as an integral dimension of mental health, rather than limiting mental health to emotional symptoms alone.
This study draws upon Social Identity Theory and Professional Identity Formation Theory to understand the relationship between professional identity and mental health (6). According to Social Identity Theory (17), individuals derive part of their self-concept from their membership in social and professional groups. A strong and positive professional identity contributes to psychological resilience, helping individuals maintain a coherent and valued sense of self during times of stress or crisis. Conversely, when professional identity is weakened or threatened—as during public health emergencies—individuals may experience increased psychological distress such as anxiety and depression. By applying this theoretical lens, we examine how variations in nurses’ professional identity relate to their mental health status following a major public health crisis like COVID-19.
Although prior studies have examined links between professional identity and mental health in nursing populations (18), relatively few quantitative studies have examined this relationship specifically in the aftermath of a major public health emergency. The present study therefore aimed to examine the association between nurses’ professional identity and symptoms of anxiety and depression following the COVID-19 public health emergency. Our primary objective was to test whether professional identity scores were associated with concurrent symptoms of anxiety and depression in a sample of Chinese nurses surveyed in February 2023.
Methods
Study design and population
A cross-sectional survey was conducted among registered nurses working in four hospitals in Sichuan Province, China between February 2 and February 28, 2023.
Inclusion criteria were: (1) registered nurses; (2) participated in clinical work during the COVID-19 public health emergency; (3) provided informed consent. Exclusion criteria were: non-nursing staff and questionnaires with incomplete key variables. All nurses in this study had direct pandemic-related work experience; therefore, no unexposed nurses were included. Sample size adequacy was evaluated using G*Power, and our final sample exceeded the minimum requirement. The questionnaire did not set an answer-time exclusion rule because the survey content was straightforward, and completion time was expected to vary across individuals. Working-year differences were analyzed in univariate and adjusted models to compare mental health between nurse groups with different experience levels.
Recruitment and data collection
Recruitment was conducted using internal hospital communication channels (email or WeChat groups). The survey was hosted on Wenjuanxing (www.wjx.cn), a widely used online survey tool in China similar to Qualtrics or SurveyMonkey, providing secure and user-friendly interfaces for data collection. All participants were voluntary and anonymous. The questionnaire could be completed only once per participant using the same Internet Protocol (IP) address to prevent duplicate submissions; however, IP addresses were not stored in the exported dataset, preserving anonymity. All participants could withdraw at any time without giving any reason. There were minimal missing values (<2% per item), and cases with incomplete key variables were excluded from the final analysis (n = 5).
Sample size calculation
A priori sample size calculation was performed using G*Power 3.1.9.7 for logistic regression. We designated the primary outcome as presence of anxiety (GAD-7 ≥ 5). This choice was made because the GAD-7 is a validated, brief screening instrument widely used in healthcare worker studies during the COVID-19 pandemic (19), and a cut-point of 5 is commonly used to denote presence of any clinically relevant anxiety symptoms (mild or greater) in population and occupational studies (20), thereby capturing a clinically meaningful burden while maximizing the observed event rate for regression modeling. Using GAD-7 ≥ 5 as the binary outcome also aligns with prior COVID-era HCW studies that used the same threshold for reporting anxiety prevalence (1). Assuming a medium effect size approximated by an odds ratio of 1.5 for a binary predictor, α = 0.05, power (1 − β) = 0.80, and inclusion of up to 10 candidate predictors in multiple models, the minimum required sample size was estimated at 142. Our final sample of 253 participants exceeds this requirement. We acknowledge that convenience sampling limits generalizability; therefore, the sample size calculation is reported for transparency rather than implying population representativeness.
Ethics statement
This study received unified ethics approval from the Ethics Committee of West China Hospital (No. 2023/177), and the approval covered all participating sub-centers. Written informed consent was obtained electronically from all participants prior to participation. This study was performed in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Measures
The e-questionnaire comprised a demographic questionnaire, Nurses’ Professional Identity Scale, Generalized Anxiety Disorder (GAD-7), Self-rating Depression Scale (SDS), and Pittsburgh Sleep Quality Index (PSQI).
Demographics
Participants completed a demographic questionnaire including age, gender, education level, professional title, marital status, child status, years of working, medical assistance experience (defined as deployment to support other regions or hospitals during the COVID-19 response), department, working on the clinical frontline and underlying medical conditions.
Professional identity scale for nurses
The Professional Identity Scale for Nurses developed by Liu et al. (21) consists of 30 items grouped into five dimensions (professional identity evaluation, professional social support, professional social proficiency, dealing with professional frustration, and professional self-reflection). Each item is rated on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), with higher scores indicating a stronger professional identity. The total score ranges from 30 to 150. A professional identity norm (21) classifies total scores of ≤90 as low, 91–120 as medium, and > 120 as high professional identity. In this study, we re-checked all item codings (including reverse-scored items) and recalculated reliability. The total-scale Cronbach’s α was 0.938, indicating excellent internal consistency. Subscale α coefficients were professional identity evaluation = 0.913, professional social support = 0.876, professional social proficiency = 0.892, dealing with professional frustration = 0.905, and professional self-reflection = 0.881. These values are consistent with prior Chinese nurse validation studies (21).
Generalized anxiety disorder 7-item
The GAD-7 is a 7-item self-report measure of generalized anxiety severity developed by Spitzer et al. (20). Each item is rated 0 (not at all) to 3 (nearly every day), yielding a total score of 0–21; cut-off values of 5, 10, and 15 represent mild, moderate, and severe anxiety, respectively. The Chinese version has demonstrated strong reliability and validity (22). In our sample, Cronbach’s α was 0.915.
Self-rating depression scale
The Zung SDS (23) comprises 20 items, each rated 1–4 (a little of the time to most of the time). Ten items are reverse scored. The raw total (20–80) is multiplied by 1.25 to obtain the standard score (25–100); a standard score ≥ 50 indicates possible depressive symptoms. In our sample, Cronbach’s α was 0.874.
Pittsburgh sleep quality index
The Chinese version of the PSQI (20) scale was used to evaluate anxiety in the previous month, and it has been most widely used to evaluate sleep quality in many studies. It contains 19 self-reported items and is divided into seven components. Each component was scored from 0 = No difficulty to 3 = Severe difficulty; component scores were summed to produce the global PSQI (0–21), and a total score ≥ 7 indicates poor sleep quality (24). Higher scores indicate poor sleep quality. In this study, Cronbach’s α was 0.821.
Statistical analysis
IBM SPSS Statistics for Windows, Version 25.0, was used for data analyses. Continuous variables are presented as mean ± SD or median [IQR] depending on distribution. Categorical variables are presented as n (%). Group comparisons used Student’s t-test or Mann–Whitney U test for continuous variables and Chi-square or Fisher’s exact test for categorical variables. Spearman rank correlation was used to examine the association between professional identity and GAD-7/SDS scores.
To identify independent factors associated with anxiety and depression, multiple logistic regression analyses were conducted. Candidate variables with p < 0.05 in univariate analyses were entered into multiple logistic regression models. Multicollinearity was assessed using VIF (values >5 considered indicative of problematic collinearity). Backward stepwise selection (entry p = 0.05, removal p = 0.10) was used to derive the final model. Model fit was evaluated with the Hosmer-Lemeshow test and receiver operating characteristic (ROC) AUC. All tests were two-tailed and p < 0.05 was considered statistically significant.
Results
Characterization and distribution of anxiety and depression
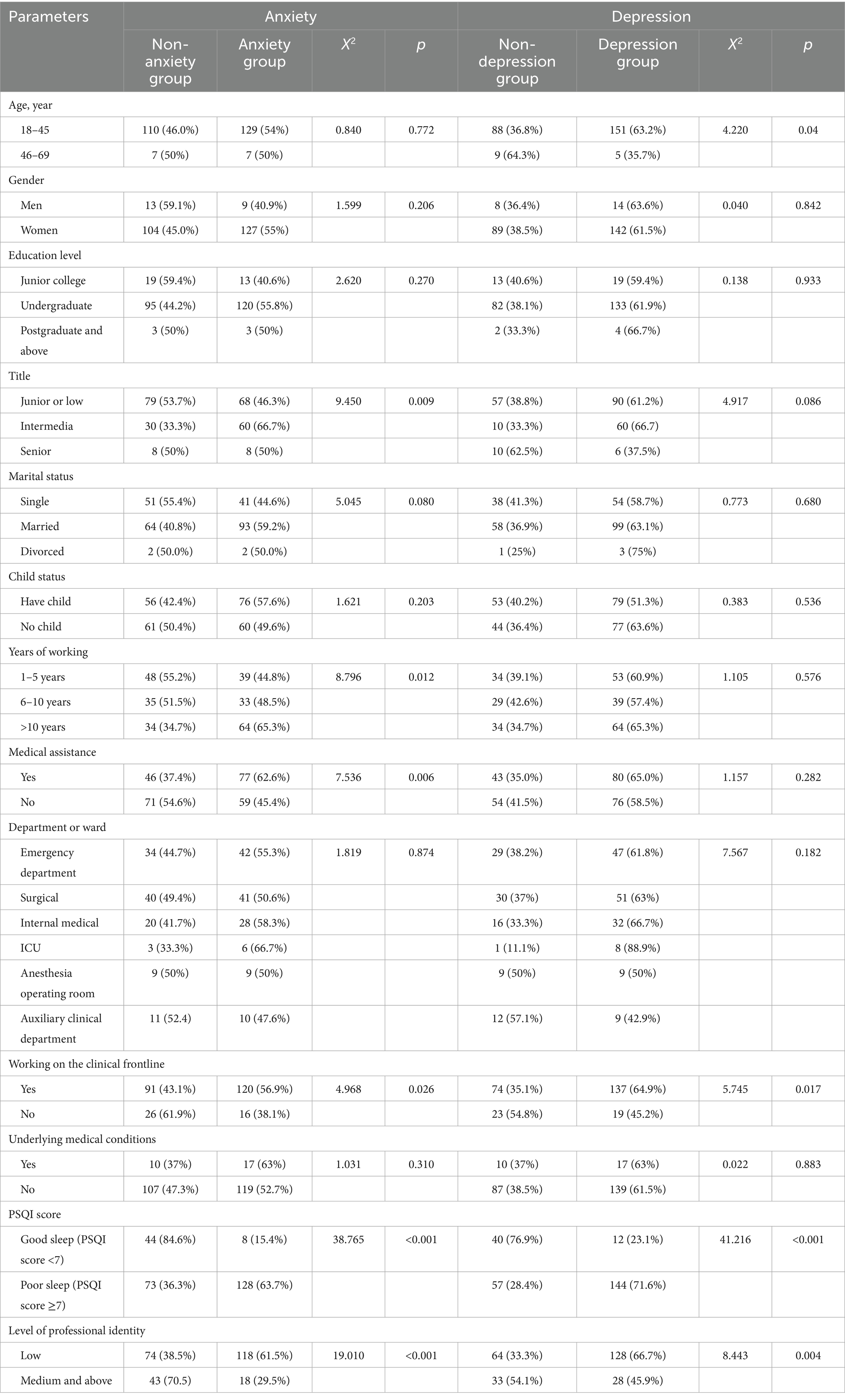
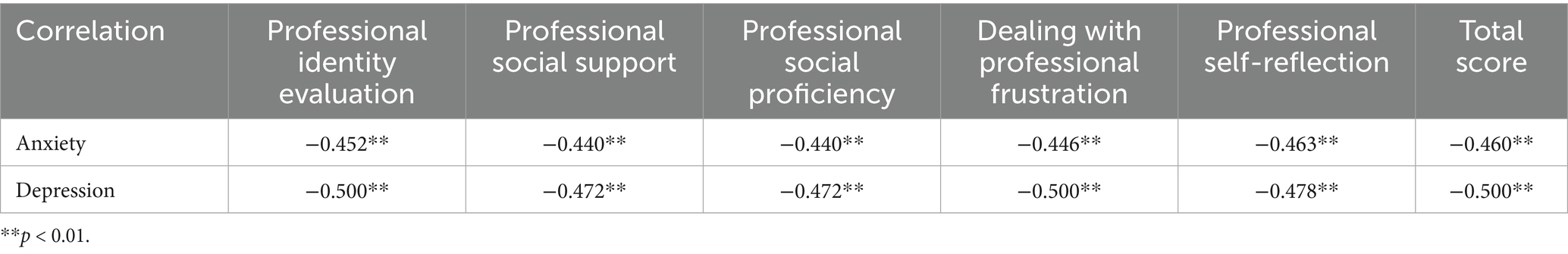
As shown in Table 1, a total of 136 nurses had anxiety, and while 117 did not. There were significant differences in job titles (p = 0.009), marital status (p = 0.080), years of working (p = 0.012), medical assistance (p = 0.006), working on the clinical frontline (p = 0.026), PSQI score (p < 0.001) and level of professional identity (p < 0.001) between the groups with and without anxiety. Additionally, a total of 156 nurses had depression, and while 97 did not. Age distribution (p = 0.040), working on the clinical frontline (p = 0.017), PSQI score (p < 0.001) and the level of professional identity (p = 0.004) were significantly different between the depression groups and non-depressing groups. Spearman correlation analysis showed that the scores of all dimensions and the total score of nurses’ professional identity were negatively correlated with the scores of anxiety and depression (all p < 0.01), indicating that higher professional identity was associated with lower anxiety and depression (Table 2).
Professional identity and comparison with Liu’s study
The mean score of professional identity was 105.25 ± 20.32 in all included nurses. The total mean scores of this study and Liu’s study were 105.15 ± 20.32 and 96.83 ± 14.99, respectively. This study showed a medium level of professional identity, which is the same as Liu’s study. The mean score of professional identity showed a significant difference in the dimensions of professional identity evaluation (3.34 ± 0.79) compared with Liu’s study (2.88 ± 0.66), and the other four dimensions showed the same levels (as shown in Table 3).
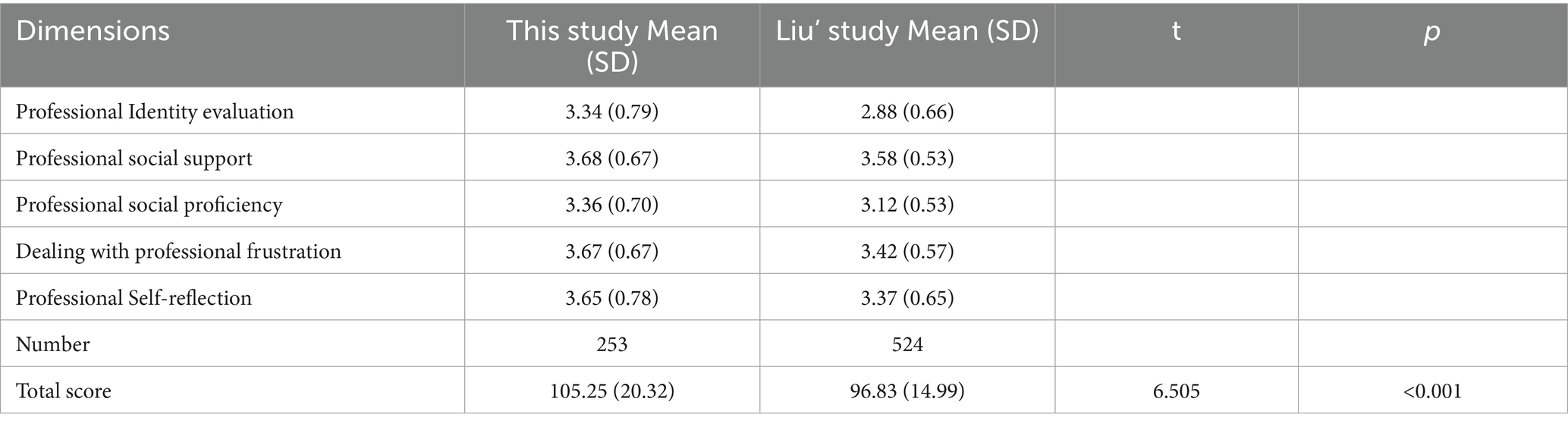
Table 3. Comparison the scores on professional identity for nurse between this study and the Liu’ study.
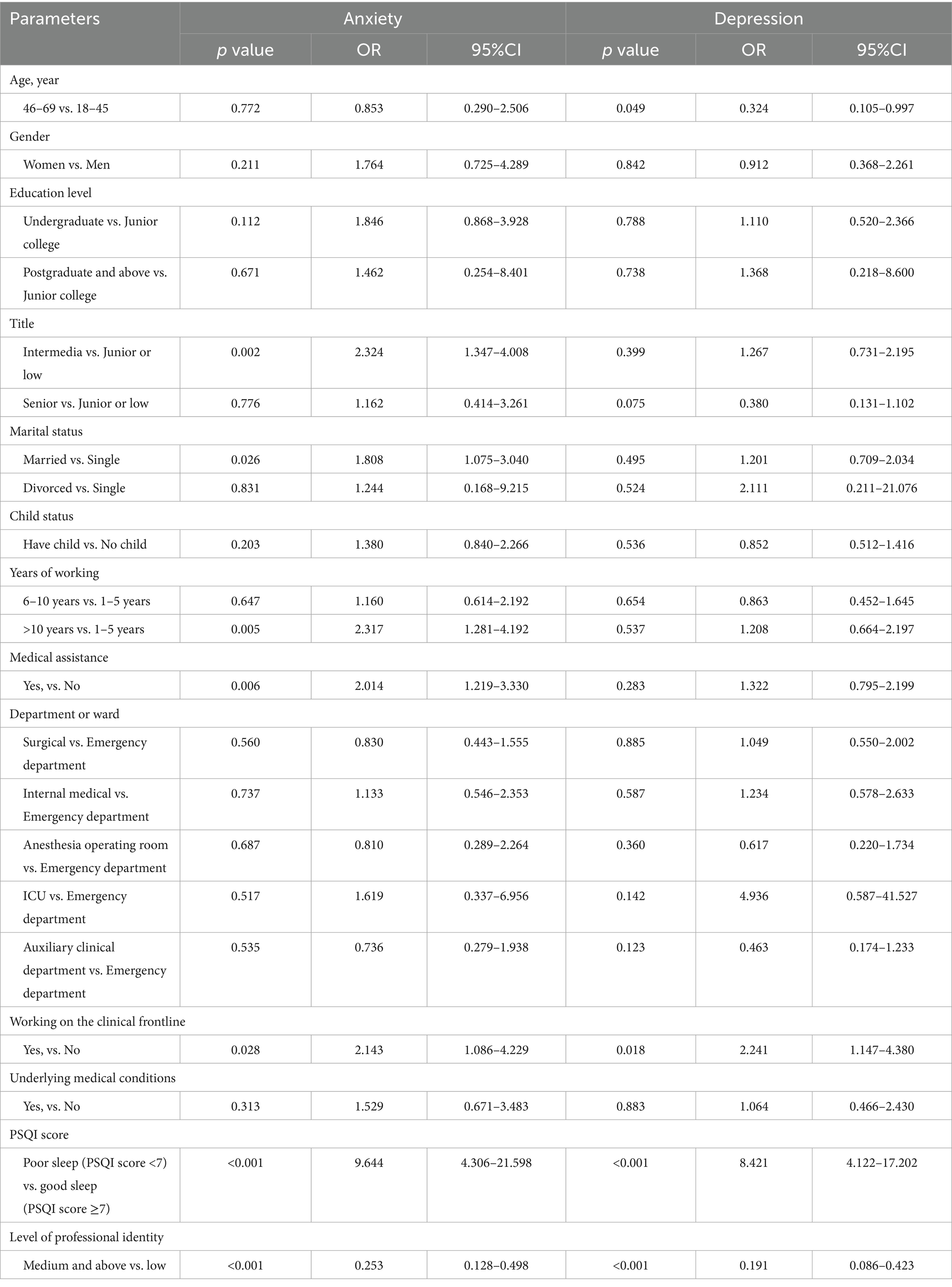
Univariate and multiple logistic regression analysis of anxiety and depression
To further investigate the factors contributing to anxiety and depression, univariate and multiple logistic regression analyses were performed. In Table 4, the results of univariate analysis showed that intermediate titles (OR 2.324, 95%CI: 1.347–4.008; p = 0.002), married (OR 1.808, 95%CI: 1.075–3.040; p = 0.026), more than 10 years of working experience (OR 2.317, 95%CI: 1.281–4.192; p = 0.005), and poor sleep quality (OR 9.644, 95%CI: 4.306–21.598; p < 0.001) increased the risk of anxiety compared with junior or low titles, single, young nurses, and good sleep quality. Nurses who had medical assistance (OR 2.014, 95%CI: 1.219–3.330; p = 0.006) and working on the clinical frontline (OR 2.143, 95.0% CI: 1.086–4.229; p = 0.028) had an increased risk of anxiety compared with those who did not. A medium level of professional identity was associated with a lower risk of anxiety than a low level of professional identity (OR 0.253, 95%CI: 0.128–0.498; p < 0.001). In Table 5, the results of multiple analysis suggested that medical assistance (OR 2.294, 95%CI: 1.262–4.169; p = 0.006), PSQI score (OR 7.383, 95%CI: 3.142–17.349; p < 0.001), and level of professional identity (OR 0.272, 95% CI: 0.124–0.593; p = 0.001) were independent risk factors for anxiety.
In the univariate logistic regression analysis of depression, participants aged 46–69 years had a higher risk of depression than those aged 18–45 years (OR 0.324, 95% CI: 0.105–0.997; p = 0.049). In addition, the front-line of working (OR 2.241, 95%CI: 1.147–4.380; p = 0.018) and poor sleep (OR 8.421, 95%CI: 4.122–17.202; p < 0.001) contributed to a higher risk of depression. However, a medium level of professional identity was associated with a lower risk of depression than a low level of professional identity (OR0.191, 95% CI: 0.086–0.423; p < 0.001). In Table 5, the results of multiple analyses suggested that the PSQI score (OR 6.838, 95.0%CI: 3.260–14.324; p < 0.001) and a medium level of professional identity (OR 0.257, 95%CI: 0.110–0.597; p = 0.002) were independent factors for depression. The association between professional identity and depression was attenuated after adjustment for sleep quality (PSQI), suggesting that sleep quality may partially mediate the observed bivariate association between professional identity and depression.
Discussion
To our knowledge, this is one of relatively few quantitative studies have examined the relationship between professional identity and nurses’ mental health specifically in the aftermath of the COVID-19 public health emergency. Our findings add to this literature by examining cross-sectional associations between professional identity, sleep quality and symptoms of anxiety and depression in nurses surveyed in February 2023. Firstly, the characteristics of the anxious group and the non-anxious group were analyzed, reporting professional title, marital status, working years, external support experience, working on the clinical frontline, PSQI score, and professional identity level had increased the risk of anxiety. In addition, age distribution, working on the clinical frontline, PSQI score, and professional identity level will increase the risk of depression in the depressed and non-depressed groups. Nurses working on the clinical frontline may be at higher risk for anxiety and depression. A previous study reported that nurses working in SARS wards were at higher risk of depression and anxiety than nurses working in non-SARS wards (25), which is consistent with our study. Interestingly, the prevalence rates of anxiety and depression after experiencing the COVID-19 public health emergency in this study were 53.8 and 46.2%, respectively, while results from a study reported that the prevalence rates of anxiety and depression were 46 and 40%, respectively (26). Infected nurses may be more concerned about prognosis than about the possibility of infection. Managers should assess the mental health status of nurses and take more timely measures to reduce the occurrence of anxiety and depression. To identify psychological distress early, voluntary and confidential mental health screenings could be implemented. In addition, psychological counseling resources and peer support groups should be made readily available.
The findings revealed that nurses’ professional identity was negatively correlated with anxiety and depression. This aligns with Social Identity Theory, which posits that individuals derive a sense of self-esteem and emotional stability from their group membership. A strong identification with one’s professional group—such as being a nurse—may buffer psychological distress by reinforcing personal value and purpose during times of crisis. Additionally, according to Professional Identity Formation Theory, the development and reinforcement of a stable professional identity over time can enhance psychological resilience. The loss of statistical significance of professional identity in the fully adjusted depression model likely reflects partial overlap between sleep disturbance and professional identity as predictors of depressive symptoms. In our cross-sectional data PSQI showed a particularly strong association with depression and including PSQI in multivariable models attenuated the professional identity coefficient. This attenuation may reflect mediation (sleep as a pathway), shared variance (overlapping constructs), or both; longitudinal mediation analysis is required to disentangle these possibilities. We therefore interpret the depression model results cautiously. Nurses who view their role positively and consistently are less likely to internalize stress or uncertainty, thereby experiencing lower levels of anxiety and depression. Therefore, more attention should be given to identifying nurses’ professional identity.
The results of this study also showed that the mean score of professional identity was 105.25 ± 20.32. Nurses in the ICU have a lower level of professional identity than those in other departments. The phenomenon may be attributed to the critical patients in the ICU with high mortality rates, although they have received the best medical care. However, this finding should be interpreted with caution, as the cross-sectional design does not allow causal inference, and the difference may also reflect contextual factors such as staffing levels or workplace culture. Therefore, the departmental variation observed in this study should be considered exploratory and warrants further investigation in longitudinal or qualitative research.
The results of this study showed that nurses had a medium level of professional identity after experiencing the COVID-19 public health emergency, which is consistent with Liu’s study but lower than Li’s study (21). The mean scores of the five professional identity dimensions were higher than those in Liu’s study, especially in professional identity evaluation. This may be because under the careful care of nurses, the prognosis of patients has greatly improved, which greatly enhanced the professional identity of nurses. During the COVID-19 public health emergency, nurses’ professional identity has been improved. Therefore, active and effective measures were suggested to maintain the high professional identity of nurses. However, due to the heavy workload, deteriorating working environment, and worry about the poor prognosis, nurses’ professional identity had relatively declined at this stage compared with the beginning of the COVID-19 public health emergency. In addition, due to the strong support from government, populations and society associations, the professional identity of medical workers has been greatly enhanced.
This study also found that nurses who were married, had worked more than 10 years, or had an intermediate job title were more likely to be anxious than those who were single, had worked 1–5 years, or had junior or low job titles. This may be explained by married nurses needing to care more about their families, and senior nurses and nurses with high professional titles usually do not engage in front-line clinical work in China. After the COVID-19 public health emergency, many of their operating skills were not proficient, and their ability to accept new things was relatively lower than that of newly recruited nurses. At the same time, professional titles and positions are often related, and nurses with high professional titles often invested more energy and time in management in China.
The results showed that medical assistance, PSQI score, and level of professional identity were independent factors of the anxiety groups. Nurses who had medical assistance of the COVID-19 public health emergency were more likely to have worse anxiety status than those who did not. Medical assistance in this study denotes deployment of nursing staff to assist other regions or hospitals during the COVID-19 response (for example, nurses who were sent to support facilities in harder-hit locations). One possible reason is that most of them had direct contact with patients during the COVID-19 public health emergency. A variety of studies have shown that it may induce mental health problems (27), and medical staff may have higher rate of mental health problems than residents (28). In addition, many studies have reported that health workers had a higher risk of poor sleep quality than others (29). Additionally, only the PSQI score was an independent factor for depression. Some studies have shown that anxiety and depression are both significantly associated with poor sleep quality (30–32). Beyond rotation systems, hospitals should consider increasing staffing ratios, particularly in high-intensity units such as ICU and emergency departments. Studies have shown that insufficient staffing and high patient acuity significantly contribute to nurse burnout and anxiety (30). Moreover, institutions should provide on-site mental health professionals or hotlines for timely psychological support.
Finally, the observed lower mean professional identity in ICU nurses should be interpreted with caution because the ICU subgroup in our sample was small (n = 9). We have deleted strong inferences from this underpowered subgroup analysis and now present it only as an exploratory observation that requires confirmation in larger, purposefully sampled studies. Recent qualitative work has documented identity disruption, role strain and resilience among nurses during the COVID-19 pandemic which complements our quantitative findings and suggests directions for future mixed-methods work (33). Based on the observed associations, hospitals could consider (1) routine, confidential mental-health screening of nursing staff after major public health events; (2) accessible psychological counseling and peer-support programs; (3) targeted sleep hygiene interventions for staff with poor PSQI scores; and (4) staffing adjustments such as temporary rotation/relief to reduce continuous high-acuity exposure. These are proposed pending evaluation in interventional or longitudinal research.
Conclusion
Nurses’ professional identity was inversely associated with symptoms of anxiety and depression in this cross-sectional survey conducted after the COVID-19 public health emergency. Because of the cross-sectional design causal inferences cannot be drawn; longitudinal and qualitative studies are needed to clarify causal pathways and to test whether interventions to support professional identity reduce psychological symptoms. In addition, psychometric evaluation of the professional identity scale in post-emergency contexts is recommended.
Limitations
The limitations of this study should be noted. Because this study was cross-sectionally designed, selection bias cannot completely be ruled out. In addition, compared with our large population nurses in China, the sample size of our study was relatively small. Furthermore, the sample was drawn from four hospitals using convenience sampling, the findings may not be fully generalizable to all Chinese nurses. Future studies using stratified random sampling across regions and hospital levels are recommended.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
NX: Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing – original draft. LZ: Project administration, Supervision, Writing – review & editing. ZY: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kang, L, Ma, S, Chen, M, Yang, J, Wang, Y, Li, R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
2. Poorgholami, F, Ramezanli, S, Jahromi, MK, and Jahromi, ZB. Nursing students' clinical performance and professional self-concept. Bangladesh J Med Sci. (2016) 15:57–61. doi: 10.3329/bjms.v15i1.22118
3. Hetherington, D, Murphy, G, Wilson, N, and Dixon, K. Issues: emergency department nurses' narratives of burnout: blurring of roles and professional identity. Aust Nurs Midwifery J. (2020) 26:40–1.
4. Slattery, MJ, Logan, BL, Mudge, B, Secore, K, Von Reyn, LJ, and Maue, RA. An undergraduate research fellowship program to prepare nursing students for future workforce roles. J Prof Nurs. (2016) 32:412–20. doi: 10.1016/j.profnurs.2016.03.008
5. Crossley, J, and Vivekananda-Schmidt, P. The development and evaluation of a professional self identity questionnaire to measure evolving professional self-identity in health and social care students. Med Teach. (2009) 31:e603–7. doi: 10.3109/01421590903193547
6. Slay, HS, and Smith, DA. Professional identity construction: using narrative to understand the negotiation of professional and stigmatized cultural identities. Hum Relat. (2011) 64:85–107. doi: 10.1177/0018726710384290
7. Mcneese-Smith, DK, and Crook, M. Nursing values and a changing nurse workforce: values, age, and job stages. JONA J Nurs Adm. (2003) 33:260–70. doi: 10.1097/00005110-200305000-00002
8. Nashwan, AJ, Abujaber, AA, Villar, RC, Nazarene, A, Al-Jabry, MM, and Fradelos, EC. Comparing the impact of Covid-19 on nurses' turnover intentions before and during the pandemic in Qatar. J Pers Med. (2021) 11:456. doi: 10.3390/jpm11060456
9. Cowin, LS, and Hengstberger-Sims, C. New graduate nurse self-concept and retention: a longitudinal survey. Int J Nurs Stud. (2006) 43:59–70. doi: 10.1016/j.ijnurstu.2005.03.004
10. Kristoffersen, M. Does professional identity play a critical role in the choice to remain in the nursing profession? Nurs Open. (2021) 8:1928–36. doi: 10.1002/nop2.862
11. Neishabouri, M, Ahmadi, F, and Kazemnejad, A. Iranian nursing students' perspectives on transition to professional identity: a qualitative study. Int Nurs Rev. (2017) 64:428–36. doi: 10.1111/inr.12334
12. Hensel, D, and Laux, M. Longitudinal study of stress, self-care, and professional identity among nursing students. Nurse Educ. (2014) 39:227–31. doi: 10.1097/NNE.0000000000000057
13. Fang, H, Tu, S, Sheng, J, and Shao, A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. (2019) 23:2324–32. doi: 10.1111/jcmm.14170
14. Shi, C, Wang, S, Tang, Q, Liu, X, and Li, Y. Cross-lagged relationship between anxiety, depression, and sleep disturbance among college students during and after collective isolation. Front Public Health. (2022) 10:1038862. doi: 10.3389/fpubh.2022.1038862
15. Baglioni, C, Battagliese, G, Feige, B, Spiegelhalder, K, Nissen, C, Voderholzer, U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
16. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, E, and Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
17. Tajfel, H., Turner, J., Austin, W. G., and Worchel, S. (2001). An integrative theory of intergroup conflict. Intergroup relations: Essential readings, 94–109.
18. Zeng, Z, Wang, X, Bi, H, Li, Y, Yue, S, Gu, S, et al. Factors that influence perceived organizational support for emotional labor of Chinese medical personnel in Hubei. Front Psychol. (2021) 12:684830. doi: 10.3389/fpsyg.2021.684830
19. Gupta, B, Sharma, V, Kumar, N, and Mahajan, A. Anxiety and sleep disturbances among health care workers during the Covid-19 pandemic in India: cross-sectional online survey. JMIR Public Health Surveill. (2020) 6:e24206. doi: 10.2196/24206
20. Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
21. Liu, LZ, and Liu, X. The correlation between job stressors, job burnout and professional identity of nurses. J Nurs Adm (Chinese). (2009) 9:1–2.
22. Tong, X, An, D, Mcgonigal, A, Park, S-P, and Zhou, D. Validation of the generalized anxiety Disorder-7 (gad-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31–6. doi: 10.1016/j.eplepsyres.2015.11.019
23. Zung, WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
24. Liu, X, Tang, M, and Hu, L. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiatry. (1996) 29:103–7.
25. Su, TP, Lien, TC, Yang, CY, Su, YL, Wang, JH, Tsai, SL, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. (2007) 41:119–30. doi: 10.1016/j.jpsychires.2005.12.006
26. Tu, ZH, He, JW, and Zhou, N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during Covid-19 outbreak: a cross-sectional study. Medicine (Baltimore). (2020) 99:e20769. doi: 10.1097/MD.0000000000020769
27. Fountoulakis, KN, Apostolidou, MK, Atsiova, MB, Filippidou, AK, Florou, AK, Gousiou, DS, et al. Self-reported changes in anxiety, depression and suicidality during the Covid-19 lockdown in Greece. J Affect Disord. (2021) 279:624–9. doi: 10.1016/j.jad.2020.10.061
28. Zhao, Y, Tao, Y, Bao, X, Ding, Q, Han, C, Luo, T, et al. A study on differences about the influencing factors of depressive symptoms between medical staff and residents during 2022 city-wide temporary static management period to fighting against Covid-19 pandemic in Shanghai. Front Public Health. (2022) 10:1083144. doi: 10.3389/fpubh.2022.1083144
29. Huang, Y, and Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during Covid-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. (2020) 288:112954. doi: 10.1016/j.psychres.2020.112954
30. Ernstsen, L, and Havnen, A. Mental health and sleep disturbances in physically active adults during the Covid-19 lockdown in Norway: does change in physical activity level matter? Sleep Med. (2021) 77:309–12. doi: 10.1016/j.sleep.2020.08.030
31. Harvey, AG. Sleep and circadian functioning: critical mechanisms in the mood disorders? Annu Rev Clin Psychol. (2011) 7:297–319. doi: 10.1146/annurev-clinpsy-032210-104550
32. Paterson, JL, Dorrian, J, Ferguson, SA, Jay, SM, Lamond, N, Murphy, PJ, et al. Changes in structural aspects of mood during 39-66 h of sleep loss using matched controls. Appl Ergon. (2011) 42:196–201. doi: 10.1016/j.apergo.2010.06.014
Keywords: China, nursing staff, professional identity, anxiety, depression, sleep quality, COVID-19, cross-sectional study
Citation: Xie N, Zou L and Yuan Z (2025) The impact of professional identity on nurses’ mental health status after the COVID-19 public health emergency: a cross-sectional survey. Front. Public Health. 13:1678636. doi: 10.3389/fpubh.2025.1678636
Edited by:
Petros Galanis, National and Kapodistrian University of Athens, GreeceReviewed by:
Esmaiel Maghsoodi, Maragheh University of Medical Sciences, IranYehong Wei, The Second Affiliated Hospital of Zhejiang Chinese Medical University, China
Kui Jia, The First Affiliated Hospital of Guangxi Meidical University, China
Copyright © 2025 Xie, Zou and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liqun Zou, eno5MjEyMjExQDEyNi5jb20=; Zhenfei Yuan, aHhqenl6ZkAxNjMuY29t
 Nan Xie
Nan Xie Liqun Zou
Liqun Zou Zhenfei Yuan
Zhenfei Yuan