- 1Department of Special Surgery, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
- 2Department of Basic Medical Sciences, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
- 3Ministry of Health, Amman, Jordan
- 4Faculty of Nursing, Al-Yarmouk University, Irbid, Jordan
- 5The Jordan University Hospital, Amman, Jordan
- 6AlKasr AlAiny Medical School, Cairo University, Cairo, Egypt
This study aimed to investigate eye makeup adverse reactions (ARs), habits and practices among Jordanian females. The research also sought to identify factors contributing to the risk of ARs to promote safer cosmetic practices and protect public health. A cross-sectional, web-based survey was conducted between March and May 2024, targeting Jordanian female residents. Data was collected using a self-administered questionnaire distributed via social media platforms using snowball sampling. The questionnaire covered social demographic characteristics, eye makeup habits, prevalence of cosmetic ARs, knowledge of eye makeup products, and the Ocular Surface Disease Index (OSDI). Logistic regression was used to assess predictors of eye makeup-related ARs. The study analyzed 1,741 valid surveys. Eye makeup users were generally younger (mean age 29.8 years) than non-users (mean age 36.8 years). A high proportion of eye makeup users (85%) reported at least one AR, with lacrimation being the most common symptom (59.2%). Significant predictors of ARs included young age (AOR = 0.968, p = 0.001), food/drug allergies (AOR = 1.602, p = 0.005), and allergic ocular disease (AOR = 4.401, p < 0.001). Unexpectedly, consistently removing eye makeup before sleep was associated with a higher risk of ARs (AOR = 4.718, p = 0.003). In conclusion, this study highlights the prevalence of adverse reactions associated with eye makeup use among Jordanian females and underscores the importance of cosmetovigilance. The high rate of self-reported adverse reactions indicates a need for increased awareness and education regarding safe cosmetic practices. Factors such as young age, pre-existing allergies were identified as significant predictors of adverse events, emphasizing the necessity of targeted interventions.
1 Introduction
The use of eye cosmetics is deeply rooted in human history, with archaeological evidence revealing their application in ancient Egypt to enhance physical appearance and convey social identity to both men and women-according to archaeological evidence: cosmetics, in general, have been used since prehistoric times (1–5). This tradition continues today, though modern formulations offer both beauty benefits and potential health risks. In modern times, eye cosmetics are often used to enhance the natural beauty of the eyes and to create an illusion of greater size and magnificence—thus increasing their perceived attractiveness (6–9). In addition, women lavishly spend money on popular cosmetics like eyeliner, mascara, and eyeshades—as an expression of their self-image (3, 5, 6, 10). While cosmetics empower women, they also pose risks of adverse reactions, especially with prolonged use (1, 6, 11).
Eye cosmetics are composed of a variety of substances, such as preservatives, vehicles (agents), antioxidants, humectants, fragrances, ultraviolet absorbers, emollients, emulsifiers, acrylates, and pigments (12, 13). Some of these products may be unsuited for use in close proximity to the eyes and may induce allergic reactions or irritation (12, 14). Likewise, microbial contamination can result from poor handling and storage, and the transmission of infections is further facilitated by the sharing of products (7, 14). Furthermore, the risk of injury increases with the use of aggressive application and removal techniques for instance: the use of fingers or cotton buds to rub eyelashes, which can inflict harm on the fragile ocular surface (15). Building upon the previous information, the risk of adverse reactions also increases with the prolonged use of contact eye makeup products-and these risks are further exacerbated by the lack of consumer awareness regarding ingredient safety, expiration dates, and proper application practices (1, 15, 16).
To address these risks, effective monitoring and regulation through cosmetovigilance is essential for monitoring adverse reactions and ensuring consumer safety (17). Through systematic data collection and analysis of cosmetic-related adverse events, it helps identify risks and implement preventive measures (4, 18, 19). Eye makeup poses particular risks due to factors such as harmful ingredients, poor hygiene, improper application and removal for example the use of fingers without hand washing, prolonged use defined as more than 6 months of regular use of eye makeup, and limited consumer awareness (1, 6, 12, 20).
Despite the wealth of information available globally, limited studies in Jordan have specifically addressed the patterns of cosmetic use among females. There were scarce studies conducted in Jordan in recent years exploring the cosmetics usage patterns and perceptions among females- this could be due to cultural factors or lack of resources. One study investigated skin-lightening products—it was not specific for the ocular area, but no research was published—specifically, on eye makeup use adverse reactions (48). Given the potential risks associated with eye makeup, this study aims to investigate the practices and reported adverse reaction of eye makeup use among Jordanian females. More specific aims: it seeks to determine the prevalence and nature of adverse reactions experienced from an ophthalmological point of view, and whether it is influenced by age, education level, or other socioeconomic factors. The findings of this research may contribute to a deeper understanding of the challenges and opportunities in promoting safer cosmetic guidelines and enhancing community awareness and protection.
2 Methods and results
2.1 Study design and ethics approval
A cross-sectional web-based survey was conducted between March and May 2024 to explore eye makeup practices and related adverse effects among women in Jordan. Data were collected via a self-administered questionnaire distributed through social media platforms. The study protocol received ethical approval from the Institutional Review Board of Al-Balqa Applied University (Ref No: 55/2023. Date 22/11/2023) and complied with the Declaration of Helsinki (2013) (21). Participation was voluntary and anonymous. Informed electronic consent was obtained prior to accessing the survey questions.
2.2 Study population and sampling
Eligible participants were female residents of Jordan aged 18 years or older. A non-probability sampling approach was employed, combining convenience and exponential non-discriminative snowball sampling. The questionnaire link was disseminated via university student forums and women's social media groups across various Jordanian governorates. Participants were encouraged to share the link within their networks to enhance reach. Eligibility was confirmed through screening questions embedded in the survey. Jordan has a population of approximately 11,734,000 people, with a median age of 22.9 years, with women accounting for 47.1% (22).
2.3 Survey instrument
The questionnaire was developed following a review of relevant literature and comprised seven sections (23–29): Introduction and Consent—including objectives, definitions of eye makeup, a confidentiality statement to ensure user privacy, and right to withdraw at anytime. Second section discussed the Eligibility Screening—two questions on gender and age; directing respondents to exit the survey if they did not meet the inclusion criteria of being female and older than 18 years old. Third section was on Sociodemographic Profile that included 14 items including age, education, marital status, occupation, smoking history, digital device use, and allergy history. Fourth part of the questionnaire focused on Makeup Practices— 18 items assessing frequency, method of application and removal, duration of use, and product expenditure. Fifty section inquired about the Adverse Reactions of using eye makeup consisted of 21 items covering symptoms such as eye redness, swelling, loss of eyelashes, abrasions of the cornea, seborrheic blepharitis, eye bibles, dermatitis, eye discharge, itchiness, etc. The sixth section was about the Knowledge Assessment of participants in the format of 10 questions on eye makeup ingredients, expiration dates, and labeling, with a scoring system. The last section consisted of the Ocular Surface Disease Index (OSDI) scale of 12 standardized questions in the Arabic language (30).
2.4 Development of the questionnaire
The majority of the questions in this study were extracted from previous research—please refer to previous paragraph, which was written in simple Arabic. Some questions required both forward and backward translations. Furthermore, the authors self-developed the questions, tested them for face and content validity, and made necessary amendments.
2.5 Pilot testing
A pilot study was carried out 1 month before distribution of the questionnaire to evaluate item clarity and content validity. Several face-to-face interviews were performed to collect participant feedback on the questionnaire's structure and wording. Based on this feedback, no substantive modifications were required for the final instrument. Data from pilot participants were not included in the primary analysis.
2.6 Sample size
Sample size was estimated using the formula n = 100 + 50i, where i is the number of independent variables. In general, a sample size of around 10% of the population, but not exceeding 1,000 participants, was considered appropriate. We used an event per variable (EPV) of 50 and the formula n = 100 + 50i, where i represents the number of independent variables in the final model. In our study, the minimum sample size would be 850, as we conducted logistic regression for 15 predictors (31). Although the intended upper limit was 1,000, a total of 1,837 responses were received, of which 1,741 met eligibility criteria and were included in the final analysis.
2.7 Data management and statistical analysis
Data were collected via Google Forms®, cleaned to remove incomplete or invalid responses (e.g., age < 18 or >90, non-differentiated responses), and exported to Google Sheets® for de-identification. Final datasets were imported into STATA SE v14 (2015) for analysis (32). Descriptive statistics summarized demographics, usage patterns, and reported symptoms. Bivariate associations were explored using Chi-square tests. Logistic regression analysis was conducted to identify predictors of self-reported adverse events. Variables significant in bivariate analysis were included in multivariate models. Both crude and adjusted odds ratios (COR, AOR) with 95% confidence intervals were reported. Significance threshold was set at p < .05 as appropriate.
2.8 Operational definitions and variables
Adverse reactions were defined as any ocular symptom perceived by the respondent to be linked to eye makeup use (26). Eye makeup referred to any cosmetic or applicator used on or around the eye and eyelids; articles that include perfumes, skin care, personal care, or hair care on the face or other body parts were excluded from the definition (3, 26). The primary outcome was the presence of one or more self-reported adverse effects. Independent variables included demographic factors, product usage behaviors, and hygiene practices.
3 Results
3.1 Descriptive statistics of the study population
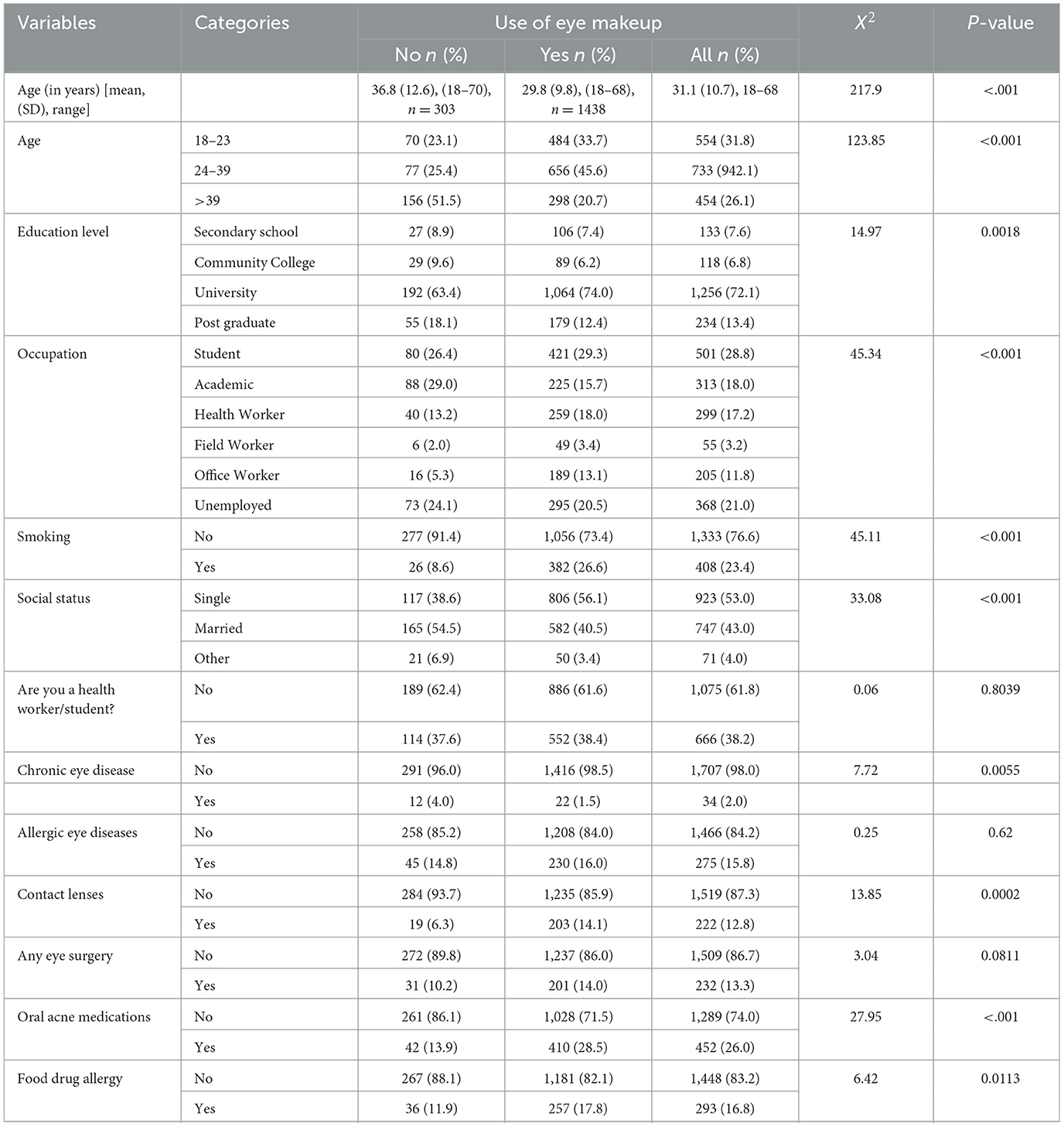
Among 1,741 valid surveys, eye makeup users (n = 1,438) were significantly younger than non-users (mean age: 29.8 ± 9.8 vs. 36.8 ± 12.6 years, p < 0.001) and more likely to be single (56.1%), university-educated (74.0%), and employed in office-based (13.1%) or health-related roles (18.0%) (p < 0.001). They reported higher rates of smoking (26.6%), contact lens use (14.1%), oral acne medication (28.5%), and food/drug allergies (17.8%) compared to non-users (all p < 0.05). Chronic eye disease was more prevalent among non-users (4.0% vs. 1.5%, p = 0.006), as demonstrated in Table 1.
3.2 Characteristics, practices, and habits of eye makeup users
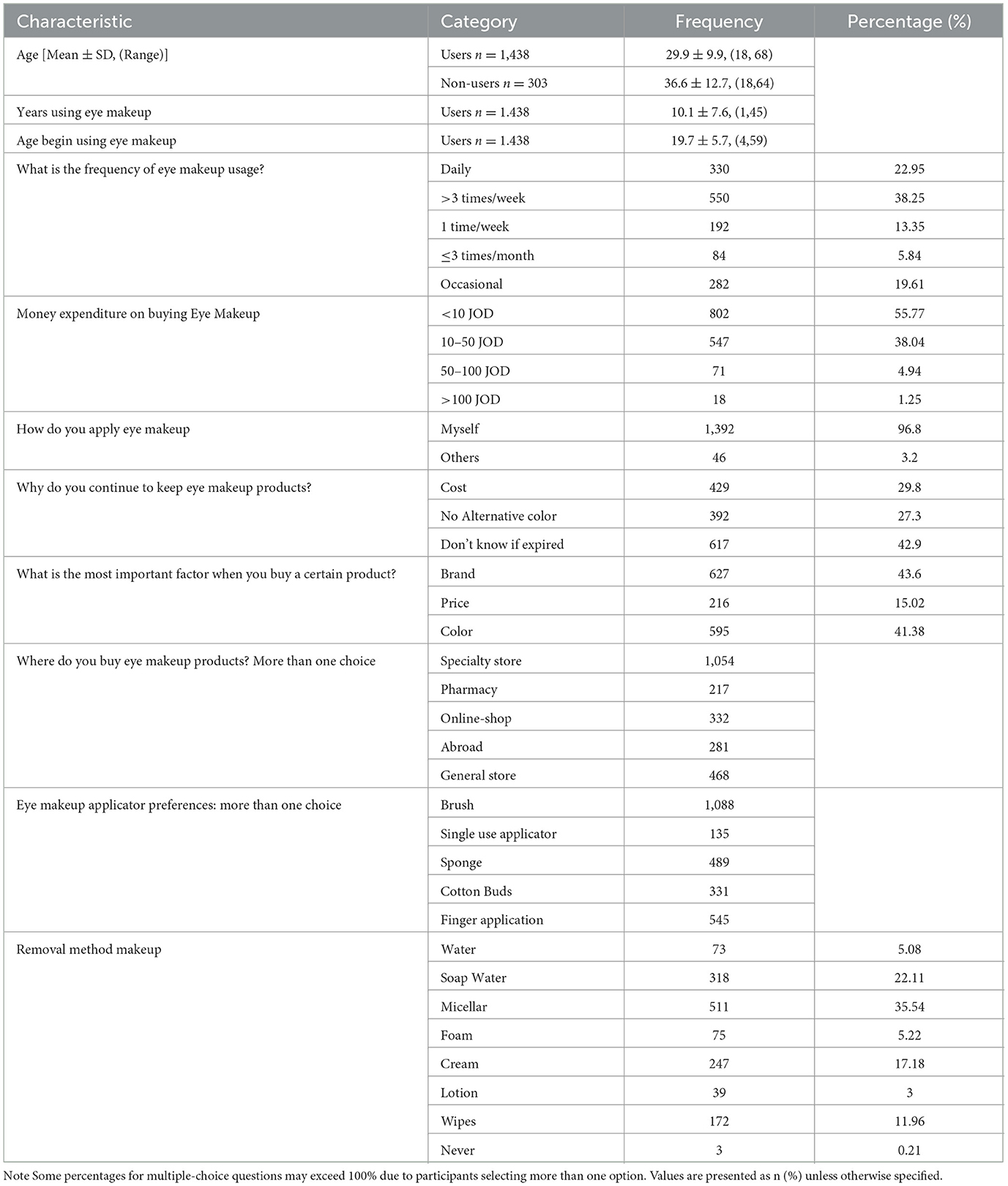
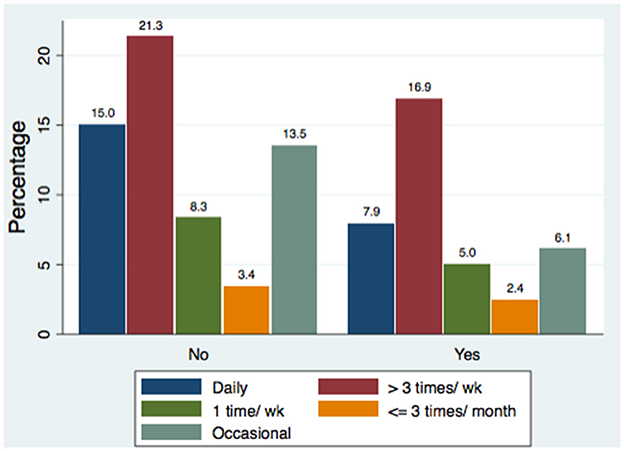
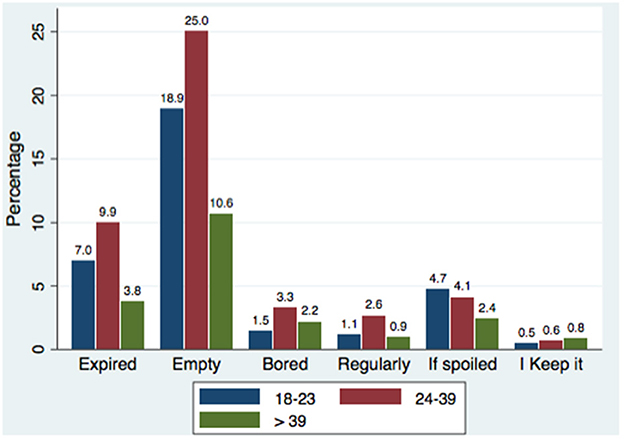
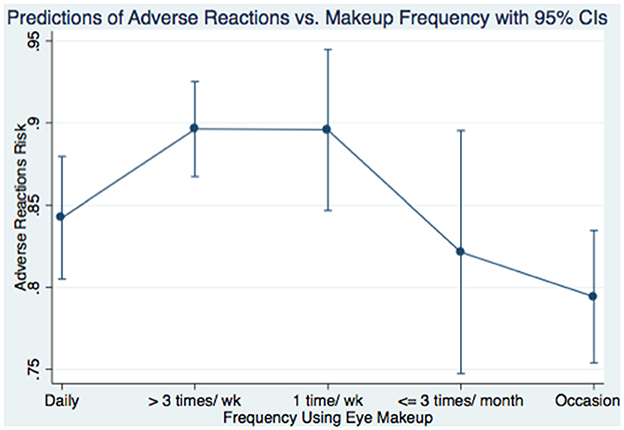
Table 2 illustrates that among 1,438 eye makeup users, the mean age of first use was 19.7 ± 5.7 years, with an average duration of use of 10.1 ± 7.6 years. Most eye makeup users applied makeup at least three times per week and spent less than 50 JOD per month. Spending was significantly associated with the employment category (χ2 = 32.61, p = 0.005), with healthcare and field workers spending more than unemployed participants. Most users applied makeup themselves using brushes or fingers and based purchasing decisions on brand and color. Specialist stores and online retailers were the preferred sources. A considerable proportion ignored product expiration dates. Micellar water and soap-based cleansers were the most common removers. Participants in health-related fields applied eye makeup less frequently than those outside such fields (Figure 1), especially among students.
3.3 Safety and Risk practices of participants
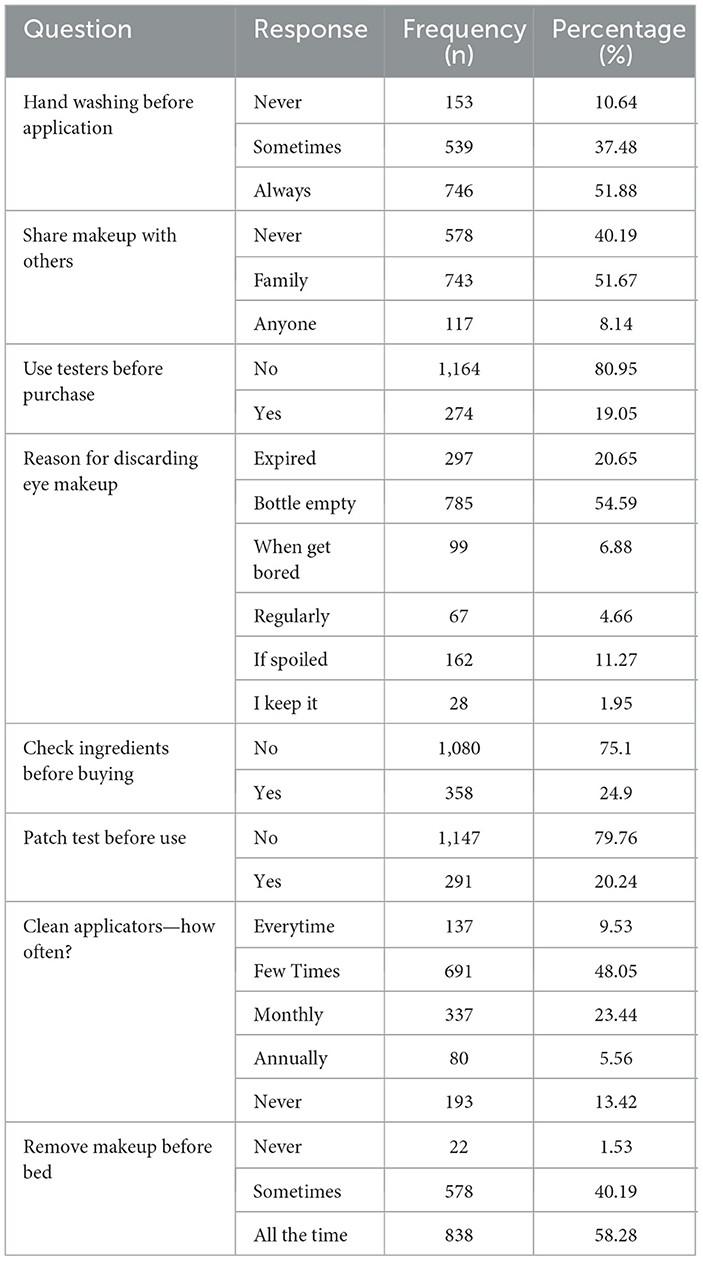
In general, hygiene practices were suboptimal, as demonstrated in Table 3. Although 89.4% of participants reported washing their hands before application and 58.2% removed makeup before sleep, it was common for them to share products, skip skin patch tests, and neglect ingredient lists. Only 19.1% checked expiration dates regularly.
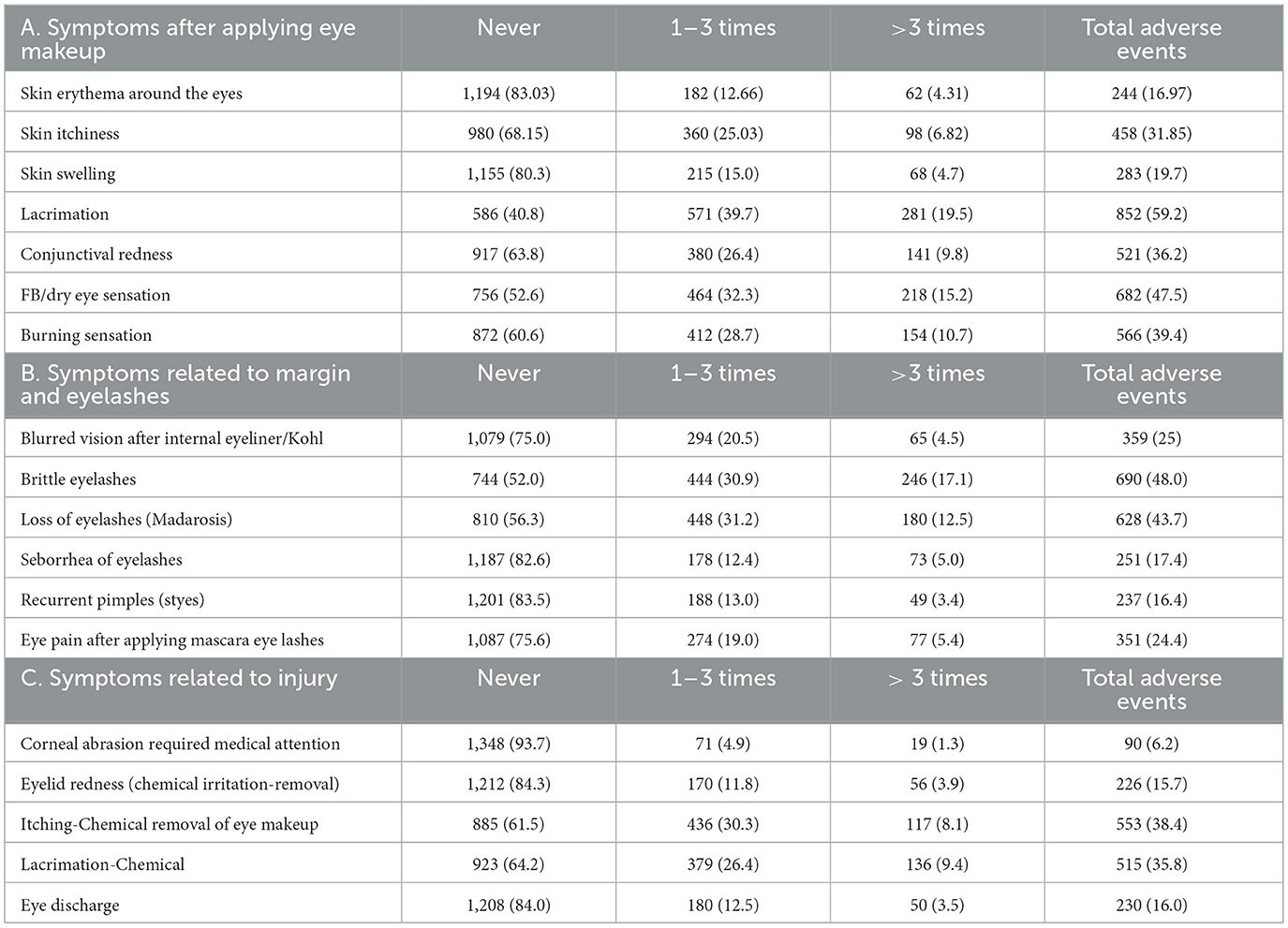
Product disposal behaviors varied by age (χ2 = 30.67, p = 0.001). Across all age groups, “product empty” was the most cited reason (54.6%). Disposal due to expiration was more common with increasing age (33.7% in 18–23 vs. 48.2% in 24–39 years). Older participants showed higher rates of discarding products due to disinterest/boredom (10.4%), while younger users more often cited spoilage (Figure 2).
3.4 Adverse reactions reported by eye makeup users
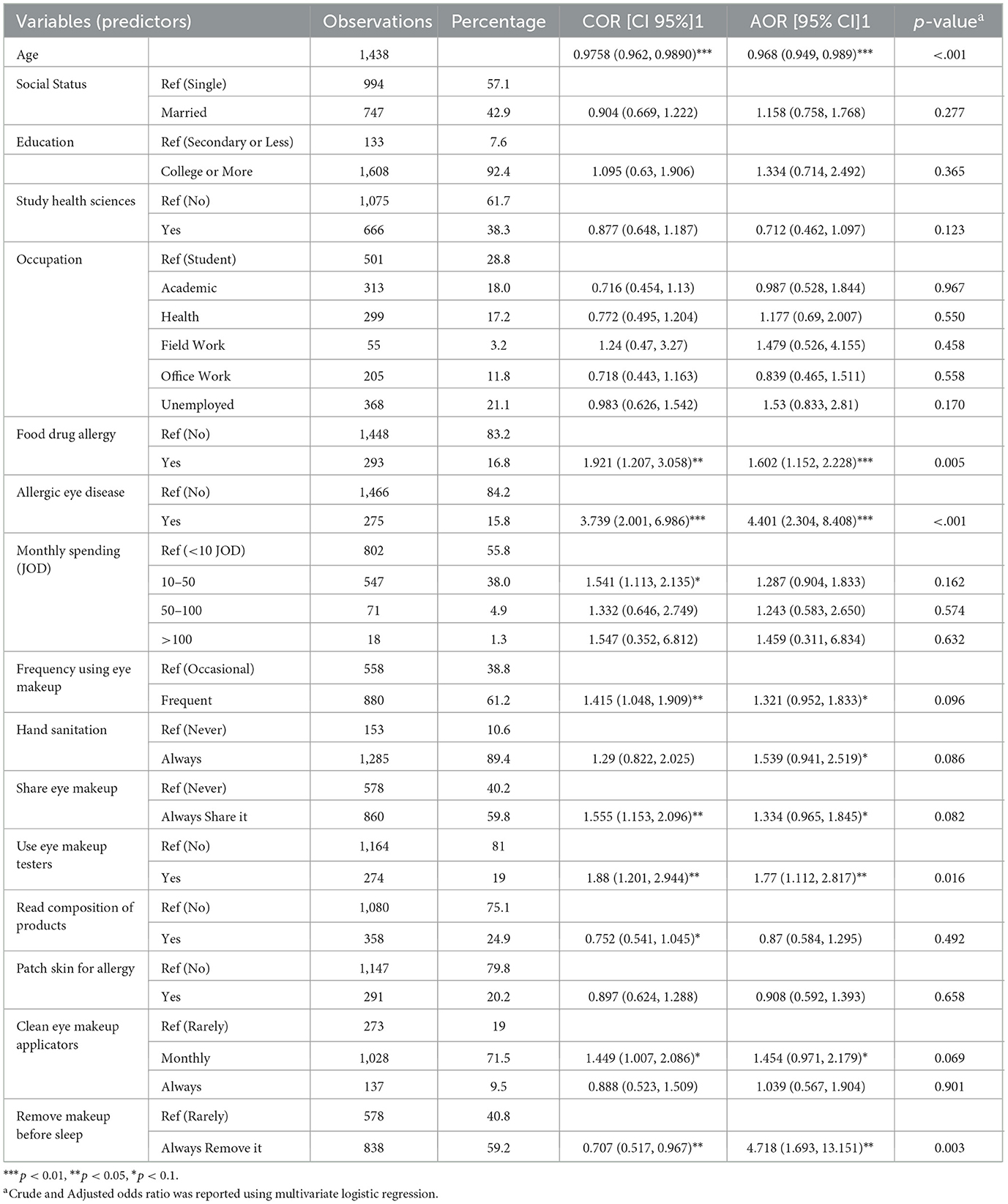
Among users, 59.2% reported lacrimation, 47.5% dry/foreign body sensation, 43.7% eyelash loss, and 39.4% burning sensation. Other symptoms included itching (38.4%), conjunctival hyperemia (36.2%), brittle lashes (48.0%), eye pain (24.4%), and blurred vision (25.0%). Corneal abrasion was reported by 6.2% of users, while 15.7% experienced chemical irritation. Skin rash around the eyes was reported in 16.97% (Table 4).
3.5 Predictors of occurrence of adverse reactions
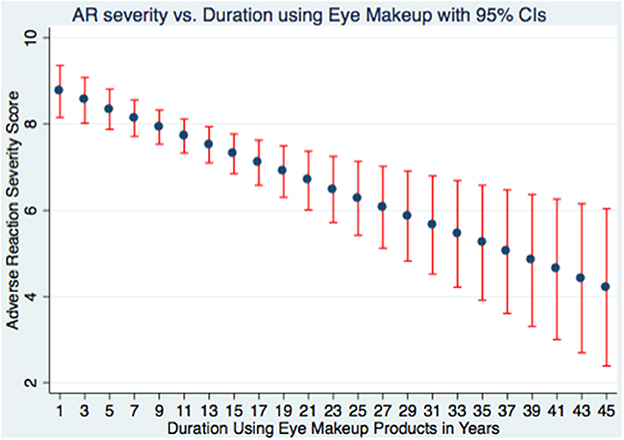
Multivariable logistic regression identified significant predictors of adverse reactions (Table 5). Younger age was protective (AOR = 0.968, p = 0.001). History of food/drug allergy (AOR = 1.602, p = 0.005) and allergic eye disease (AOR = 4.401, p < 0.001) increased risk. Unexpectedly, removing makeup before sleep was associated with greater odds of adverse reactions (AOR = 4.718, p = 0.003). Use of tester products also increased risk (AOR = 1.77, p = 0.016). Other behavioral and sociodemographic factors did not reach statistical significance. A regression plot (Figure 3) showed adverse reaction scores decreased with increasing years of use. Higher frequency of use was associated with greater adverse scores (Figure 4).
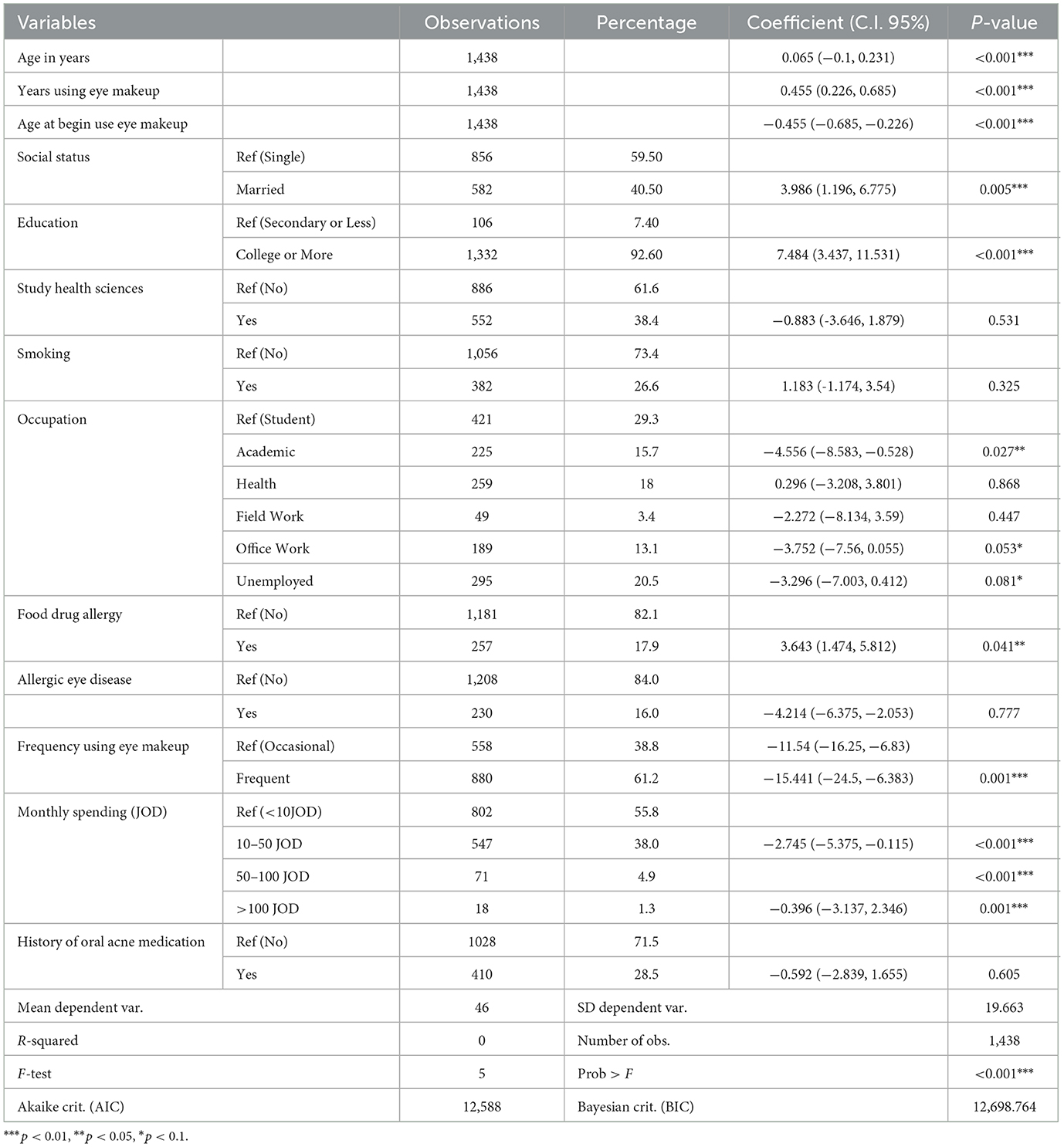
3.6 Predictors of malpractice habits vs. independent variables
A composite malpractice score was modeled against demographic and behavioral variables (Table 6). This score is based on the following malpractice habits that include not washing hands, sharing makeup, using tester products, not disposing of products regularly, not checking ingredients, not conducting skin patch tests, not cleaning applicators or brushes, and not removing makeup before bed as a single malpractice score value. We found that younger age groups (β = 0.065, p < 0.001) and longer duration of use (β = 0.455, p < 0.001) predicted higher malpractice scoring. Being married (β = 3.986, p = 0.005) and having higher education (β = 7.484, p < 0.001) were also associated with poorer safety practices. In contrast, frequent users had significantly lower malpractice scores (β = −15.441, p = 0.001), suggesting better hygiene awareness among this subgroup. Although the logistic regression model's overall explanatory power was limited, we demonstrated that multiple factors may play a role in malpractice scores related to eye makeup.
4 Discussion
This study showed that women who use eye makeup are significantly younger (mean age 29.8 ± 9.8 years) than non-users (36.8 ± 12.6 years), consistent with prior literature reporting higher cosmetic usage among younger age groups (2, 13, 33). Park et al. (13) found peak usage of eye and nail cosmetics among Korean women aged 20–29, which aligns with our age-stratified findings. Eye makeup users were also more likely to be single, university-educated, and employed in office or health-related sectors, mirroring demographic trends observed in similar populations (6).
Despite a lower prevalence of chronic eye diseases among users, they demonstrated higher rates of contact lens wear, smoking, oral acne medication use, and reported food or drug allergies (p < 0.001). These comorbidities may predispose individuals to heightened ocular sensitivity or increased susceptibility to cosmetic-related adverse reactions (12, 16, 34–36).
Regular cosmetic use, defined as ≥3 applications per week, was reported by 61.2% of respondents; in line with the 58.8% observed by (6), where 58.8% were classified as regular users (6). Interestingly, we observed an inverse correlation between usage frequency and adverse reaction scores (Figure 4), suggesting improved hygiene, adaptive tolerance, or informed product selection over time (17, 18). Several factors may explain this: (1) lower malpractice scores among regular users indicate better hygiene practices; (2) repeated exposure may induce ocular tolerance; and (3) experienced users may preferentially select less irritant products and utilize gentler removal techniques (1, 8). Furthermore, our data show an inverse relationship between years of cosmetic use and adverse symptom scores (Figure 3), indicating potential acclimation or avoidance of irritant products (8). Additionally, underreporting among long-term users due to recall bias or normalization of symptoms may play a role (26, 33).
We also noted behavioral variations in makeup removal practices by age and discipline. Among users aged 18–39, 61% preferred micellar or soapy water. In contrast, 51% of women over 39 favored creams or soaps. Health-related discipline participants reported higher usage of micellar water (47.75%) and lower reliance on potentially irritating wipes and foams (31.98% and 29.96%, respectively). This may reflect increased awareness of dermatologic safety and environmental impact. These trends are consistent with previous reports emphasizing the role of cleansing agents in maintaining periocular health (1, 37). Ozdemir et al. (38) similarly reported that although 77.7% of students prioritized makeup removal, only 46.9% used appropriate cleansing agents. Alarmingly, 66.8% of non-health discipline students in our cohort reported never removing makeup before sleep, a potential risk factor for ocular surface inflammation (1). This hygiene gap highlights the need for targeted education, particularly outside the health sciences.
Analysis of the relationship between participants' monthly expenditure on eye makeup products revealed that unemployed women in Jordan, expectedly, were more likely to spend the least amount (less than 10 JOD), whereas professionals in health and fieldwork were slightly more inclined to spend moderately (10–50 JOD) (χ2 = 32.6148, p = 0.005). The three most common methods of buying cosmetic products included specialty stores, general stores, and online shopping. Comparatively, Meharie et al. (24) reported that the primary source of cosmetics for female students at the Dessie campus, Wollo University in Ethiopia was local or ordinary shops (88.8%), followed by supermarkets (45.8%) and drug retail outlets (24.8%). Their findings also indicated a statistically significant association between monthly income and cosmetics utilization (OR = 2.280, 95% CI = 1.169–7.638) (24). They also reported that cosmetics utilization increased approximately twofold among students with a monthly income of 500 birr (equals 3.88 USD) or more compared to those earning less than 500 birr per month. Several other studies have suggested that income and access to different retail locations can influence cosmetic purchasing habits and utilization (1, 17, 23, 24, 29).
Our findings show that both the field of work and the total amount of disposable income a person has influence purchasing behavior and product choice. For instance, unemployed women were more likely to spend less than 10 JOD per month, whereas health and field professionals were much more inclined to spend between 10 and 50 JOD per month (χ2 = 32.6148, p = 0.005). These findings mirror those of Meharie et al. (24), who found that Ethiopian students who made more money were more likely to use cosmetics (OR = 2.28, 95% CI: 1.17–7.64). Several previous studies have reported that income and access to different retail locations can influence cosmetic purchasing habits and utilization (1, 17, 23, 24, 29).
Despite the widespread availability of cosmetic products, awareness of product safety remains suboptimal. In our sample, 75% did not read ingredient labels, and 79.8% did not perform skin patch testing prior to use. These findings are consistent with Meharie et al. (24), who found that 66.8% of users overlooked expiration labels. Dibaba et al. (17) and Nayak et al. (11) also noted low engagement in precautionary practices (23). Addis et al. (1) observed that users who routinely read labels had lower rates of adverse reactions. This emphasizes the need for targeted consumer education campaigns to improve safety practices, particularly among younger or less health-literate groups.
In this study, a substantial proportion of eye makeup users (85%) reported experiencing at least one adverse reaction (11, 17, 18, 23, 24, 26). The most frequently reported symptom was lacrimation, affecting 59.2% of users. This symptom, while often dismissed as mild, is clinically significant, as excessive tearing may reflect ocular surface irritation or early evaporative dry eye disease (DED) (2, 10). The second and third most common symptoms—foreign body sensation (47.5%) and burning sensation (39.4%)—are hallmark indicators of tear film instability and ocular surface inflammation (1–3, 18). These symptoms align with previous studies linking frequent cosmetic use, particularly of eyeliner and mascara, to dry eye symptomatology and meibomian gland dysfunction (3, 8, 39).
Hunter et al. (39) further demonstrated that certain eye cosmetics alter the biophysical properties of meibum, increasing its viscosity and contributing to evaporative dry eye. This aligns with our data showing that dry eye symptoms—particularly foreign body sensation and burning—were prevalent, especially among long-term users. These physiological changes reinforce the notion that product selection and application technique are central to ocular surface health in cosmetic users.
The anatomical proximity of eye makeup application to the lid margin and tear film puts the ocular surface at unique risk. Products such as pencil eyeliner, often applied directly to the waterline (mucocutaneous junction), are especially concerning. Albarrán et al. (40) demonstrated that cosmetic particles can migrate into the tear film, resulting in increased debris within the lipid layer. This interferes with meibomian gland output, a key factor in maintaining tear film stability. Such mechanical obstruction and contamination can accelerate tear evaporation, leading to chronic irritation and inflammation (3, 39, 41, 42).
Moreover, ocular itching (38.4%), conjunctival hyperemia (36.2%), and eye pain (24.4%) were frequently reported. These symptoms may be explained by hypersensitivity reactions to preservatives, dyes, and fragrance components in cosmetic products (11, 26). Repeated exposure to such allergens may induce subclinical inflammation and exacerbate underlying allergic conjunctivitis or meibomitis. These findings were echoed in a similar cohort by Addis et al. (1), who found strong associations between poor label awareness and increased incidence of ocular allergic symptoms.
A notable 25% of users reported blurred vision, a concerning symptom suggestive of significant optical disturbance, possibly caused by a compromised tear film or transient epithelial disruption (39). Chemical irritation, reported by 15.7%, may reflect direct toxic effects of cosmetic ingredients or improper removal techniques involving aggressive cleansers (9, 14, 43).
The most severe complication reported was corneal abrasion, identified in 6.2% of users. Though infrequent, corneal abrasions represent a clinically serious outcome, with potential for infection, scarring, and permanent visual impairment. This aligns with findings by Wang and Craig (10), who emphasized that seemingly innocuous cosmetic practices can result in sight-threatening injuries when proper hygiene is not maintained (33).
Another frequently overlooked issue was madarosis (eyelash loss) reported in 43.7% of participants. Chronic use of mascara, adhesive false lashes, and aggressive removal techniques can exert mechanical traction on lash follicles. Kadri et al. (37) found a significant positive association between long-term cosmetic use and milphosis (eyelash loss), with 19% of medical students reporting eyelash loss. This observation was supported by (author?) (3), who linked chronic blepharitis, frequently exacerbated by mascara residues, to follicular damage and lash weakening (3).
While dry eye disease (DED) symptoms were prevalent in our cohort, objective diagnostic tests such as tear breakup time (TBUT) or Schirmer's test were not conducted. Ercan et al. (41) found no significant difference in TBUT among users and non-users, whereas other studies reported increased OSDI (Ocular Surface Disease Index) scores in habitual users (5, 6, 12, 41, 44, 45). Interestingly, this study found no significant difference in OSDI scores (p = 0.083), despite increased subjective discomfort (P < 0.001), highlighting the complex interplay between symptom perception and objective disease markers. This could partially explained by Alison Ng et al. (8) and Hunter et al. (39) who demonstrated that cosmetic use, particularly layering multiple products, may create a cumulative effect on ocular surface stress. This additive exposure to foreign substances increases the risk of subclinical inflammation, disruption of mucin layer integrity, and delayed epithelial healing—mechanisms central to the chronicity of cosmetic-induced ocular surface disease (20, 27, 34, 36, 46, 47).
5 Limitations
The study has few limitations that should be considered when interpreting or generalizing its findings. First, the study relied on self-reporting of adverse reactions (ARs), which may be subject to recall bias and potential under- or over-reporting, and the management of these ARs was not captured—as it was not part of the aims of the study—making it difficult to ascertain the true impact or appropriate treatments utilized by the participants. Secondly, the study did not account for the frequency with which participants applied eye makeup during the day—although daily use was considered indicative of regular usage. Lastly, the study—intentionally—did not gather data on specific brands or types of eye makeup, which precludes any assessment of causality between particular products and observed adverse effects.
6 Conclusions
This study highlights the extensive use of eye cosmetics among Jordanian women and indicates a high incidence of self-reported ocular adverse responses, which range from moderate irritation to clinically important consequences, including madarosis and corneal abrasion. Regular users tended to be younger, more educated, and professionally active, yet exhibited notable deficiencies in product literacy, hygiene practices, and cosmetic removal behaviors. Some of the risk factors we reported included young age, pre-existing allergies, and improper application or removal habits; these findings highlighted the need for public health education interventions, particularly among non-health-discipline populations.
The results reinforce the public health importance of cosmetovigilance and call attention to the underreported ocular risks of eye makeup use. Given the association between suboptimal practices and adverse reactions, the policymakers in general need to prioritize standardized product labeling, public awareness campaigns, and the incorporation of routine screening for cosmetic-related ocular symptoms in clinical settings. Future longitudinal and interventional research is needed to find causal relationships between specific product types and ocular adverse reactions and to inform the development of evidence-based guidelines for safer cosmetic use.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Al-Balqa Applied University IRB committee Faculty of Medicine (55/2023 Date: 22/11/2023). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. AAl: Conceptualization, Data curation, Methodology, Resources, Visualization, Writing – original draft, Project administration. SI: Conceptualization, Formal analysis, Methodology, Resources, Supervision, Writing – original draft, Validation. AAb: Conceptualization, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. AM: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Software, Writing – original draft. HA: Conceptualization, Methodology, Writing – original draft, Data curation, Project administration, Visualization. YJ: Conceptualization, Methodology, Writing – original draft, Formal analysis, Investigation, Writing – review & editing. RA-A: Conceptualization, Methodology, Visualization, Writing – review & editing, Project administration, Resources, Writing – original draft. RH: Conceptualization, Data curation, Methodology, Writing – original draft, Resources, Visualization. LA-K: Conceptualization, Data curation, Methodology, Visualization, Software, Validation, Writing – review & editing. TA: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to thank Dr. Afaf Al-Ajarmeh, Dr. Yaqeen Majed Al Asoufi, Rasmieh Al-Amer PhD for their valuable assistance in data collection and survey distribution.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Gen AI was used in the creation of this manuscript. During the preparation of this work the author used ChatGPT (https://chat.openai.com/, accessed April 2025), Quilbot (https://quillbot.com/, accessed April 2025), Ref_n_write (https://www.ref-n-write.com/, Accessed April 2025) and Notebook LM (https://notebooklm.google.com/, Accessed April 2025) in order to proofread, summarize or help with rephrasing some language. After using this tool/service, the author reviewed and edited the content as needed and takes full responsibility for the content of the publication. These tools were not used to generate ideas or graphs.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Addis GT, Yimer YS, Dagnew SB, Moges TA, Assefa AN, Alemu MA, et al. Cosmetic use and related negative effects among graduate university female students in Ethiopia: a multicenter cross-sectional study. J Public Health. (2024) 32:237–45. doi: 10.1007/s10389-022-01815-y
2. Albdaya NA, Binyousef FH, Alrashid MH, Alajlan AA, Alsharif FA, Alfouzan SK, et al. Prevalence of dry eye disease and its association with the frequent usage of eye cosmetics among women. Cureus. (2022) 14:e27142. doi: 10.7759/cureus.27142
3. Sullivan DA, da Costa AX, Del Duca E, Doll T, Grupcheva CN, Lazreg S, et al. TFOS Lifestyle: Impact of cosmetics on the ocular surface. Ocul Surf. (2023) 29:77–130. doi: 10.1016/j.jtos.2023.04.005
4. Vickery SA, Kolas R, Dicko F. Eye cosmetics. In:Draelos ZD, , editor. Cosmetic Dermatology, 1st Edn. Hoboken, NJ: Wiley (2015). p. 199–206.
5. Yazdani M, Elgstøen KBP, Utheim TP. Eye make-up products and dry eye disease: a mini review. Curr Eye Res. (2022) 47:1–11. doi: 10.1080/02713683.2021.1966476
6. Ahmad Najmee NA, Abdul Hayy SH, Wan Mahmood WMA. Effects of eye cosmetics usage, knowledge, hygiene and management towards dry eye symptoms among university students. Malays J Med Health Sci. (2022) 18:213–20. doi: 10.47836/mjmhs.18.s15.29
7. Dimri AG, Singh D, Chatterjee R, Chaudhary S, Aggarwal DML. Evaluation of microbial contamination of eye make up product: mascara. J Biomed Pharm Res. (2016) 5(6):95–103
8. Alison Ng, Evans K, North R, Purslow C. Eye cosmetic usage and associated ocular comfort. Ophthalmic Physiol Opt. (2012) 32:501–7. doi: 10.1111/j.1475-1313.2012.00944.x
9. Alison Ng, Evans K, North RV, Jones L, Purslow C. Impact of eye cosmetics on the eye, adnexa, and ocular surface. Eye Contact Lens Sci Clin Pract. (2016) 42:211–20. doi: 10.1097/ICL.0000000000000181
10. Wang MT, Craig JP. Investigating the effect of eye cosmetics on the tear film: current insights. Clin Optom. (2018) 10:33–40. doi: 10.2147/OPTO.S150926
11. Nayak M, Ligade VS, Prabhu SS. Awareness level regarding adverse reactions caused by cosmetic products among female patients: a cross-sectional study. J Cosmet Dermatol. (2023) 22:2512–9. doi: 10.1111/jocd.15734
12. Nigam PK. Adverse reactions to cosmetics and methods of testing. Indian J Dermatol Venereol Leprol. (2009) 75:10. doi: 10.4103/0378-6323.45214
13. Park GH, Nam C, Hong S, Park B, Kim H, Lee T, et al. Socioeconomic factors influencing cosmetic usage patterns. J Expo Sci Environ Epidemiol. (2018) 28:242–50. doi: 10.1038/jes.2017.20
14. Coroneo MT, Rosenberg ML, Cheung LM. Ocular effects of cosmetic products and procedures. Ocul Surf. (2006) 4:94–102. doi: 10.1016/S1542-0124(12)70031-9
15. Alhamazani MA, Alnabri MS, Alreshidi MN, Alsulaiman HM, Strianese D, Althaqib RN. Assessing public awareness of daily eyelid hygiene habits in Saudi Arabia: an online survey study. Saudi J Ophthalmol. (2021) 35:304. doi: 10.4103/sjopt.sjopt_25_20
16. Dogra A, Minocha YC, Kaur S. Adverse reactions to cosmetics. Indian J Dermatol Venereol Leprol. (2003) 69:165.
17. Dibaba H, Yadesa D, Legesse B. Shewamene Z. Cosmetics utilization pattern and related adverse reactions among female university students. Int J Pharm Sci Res. (2013) 4:997–1004. doi: 10.13040/IJPSR.0975-8232.4(3).997-04
18. Bilal AI, Tilahun Z, Osman ED, Mulugeta A, Shekabdulahi M, Berhe DF. Cosmetics use-related adverse events and determinants among Jigjiga town residents, Eastern Ethiopia. Dermatol Ther. (2017) 7:143–53. doi: 10.1007/s13555-016-0157-y
19. Di Giovanni C, Arcoraci V, Gambardella L, Sautebin L. Cosmetovigilance survey: are cosmetics considered safe by consumers? Pharmacol Res. (2006) 53:16–21. doi: 10.1016/j.phrs.2005.08.003
20. Sautebin L. Understanding the adverse effects of cosmetics: a pilot project in cosmetovigilance. Drug Saf. (2008) 31:433–6. doi: 10.2165/00002018-200831050-00010
21. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
22. Department of Statistics. Jordan Population 2024 (2024). Available from: https://dosweb.dos.gov.jo/population/population-2/ (Accessed September 27, 2025).
23. Getachew M, Tewelde T. Cosmetic use and its adverse events among female employees of Jimma University, Southwest Ethiopia. Ethiop J Health Sci. (1970) 28:681–8. doi: 10.4314/ejhs.v28i6.6
24. Meharie BG, Ambaye AS, Atnafie SA. A cross sectional study on assessment of cosmetics utilization and self reported adverse reactions among Wollo University Dessie Campus Female Students. Dessie, North East Ethiopia. Eur J Pharm Med Res. (2014) 2:49–63.
25. Husain K, A. survey on usage of personal care products especially cosmetics among university students in Saudi Arabia. J Cosmet Dermatol. (2019) 18:271–7. doi: 10.1111/jocd.12773
26. Lucca JM, Joseph R, Hussain Al Kubaish Z, Mohammad Al-Maskeen S, Ali Alokaili Z. An observational study on adverse reactions of cosmetics: the need of practice the Cosmetovigilance system. Saudi Pharm J SPJ. (2020) 28:746–53. doi: 10.1016/j.jsps.2020.04.017
27. Upadhyay H, Parikh C, Nair PA. Awareness and practices about skin care among medical students: a cross-sectional study. J Clin Diagn Res. (2021) 15:OC01-5. doi: 10.31219/osf.io/cekxt
28. Chahine B, Hanna V, Ghandour I, Haydar S, Faddoul L. Knowledge and attitude of Lebanese women about cosmetics: a cross-sectional survey. Int J Womens Dermatol. (2023) 9:e091. doi: 10.1097/JW9.0000000000000091
29. Udayanga L, Subashini N, Udugama M, Silva P, Ranathunge T. Knowledge, perceptions, and consumption behaviour of cosmetics among undergraduates of Sri Lanka: a descriptive cross-sectional study. Front Public Health. (2024) 11:1184398. doi: 10.3389/fpubh.2023.1184398
30. Bakkar MM, El-Sharif AK, Al Qadire M. Validation of the Arabic version of the ocular surface disease index questionnaire. Int J Ophthalmol. (2021) 14:1595–601. doi: 10.18240/ijo.2021.10.18
31. Bujang MA. Sa'at N, Sidik TMITAB, Joo LC. Sample size guidelines for logistic regression from observational studies with large population: emphasis on the accuracy between statistics and parameters based on real life clinical data. Malays J Med Sci. (2018) 25:122–30. doi: 10.21315/mjms2018.25.4.12
32. Stata SE Release 14. Stata SE Release 14 (Stata Statistical Software). StataCorp.: College Station, TX (2015). Available from: https://www.stata.com/ (Accessed May 1, 2024).
33. Canbin Dong, Fang Liu, Zuda Liao, Lanmei Lin, Runnan Wang, Juan Du, et al. Analysis of adverse reactions of cosmetics in chinese han population in recent five years. Clin Cosmet Investig Dermatol. (2023) 16:2419–28. doi: 10.2147/CCID.S418591
34. Nohynek Gerhard, Antignac E, Re T, Toutain H. Safety assessment of personal care products/cosmetics and their ingredients. Toxicol Appl Pharmacol. (2010) 243:239–59. doi: 10.1016/j.taap.2009.12.001
35. Paikray E, Bisoyi D, Rout A, Mishra V, Sr EP, Bisoyi D, et al. Analysis and reporting of adverse drug reactions of cosmetics at a Tertiary Care Hospital. Cureus. (2024) 16(3). doi: 10.7759/cureus.56856
36. Sabhahit SV, Babu M. V D. Ocular effects of eye cosmetic formulations. Cutan Ocul Toxicol. (2024) 43:1–7. doi: 10.1080/15569527.2024.2360735
37. Kadri R, Achar A, Tantry TP, Parameshwar D, Kudva A, Hegde S. Mascara induced milphosis, an etiological evaluation. Int J Trichology. (2013) 5:144. doi: 10.4103/0974-7753.125611
38. Ozdemir A, Bostanci S, Cakmak B. Determination of factors affecting the selection and use of makeup materials. Int J Caring Sci. (2019) 12:823.
39. Hunter M, Bhola R, Yappert MC, Borchman D, Gerlach D. Pilot study of the influence of eyeliner cosmetics on the molecular structure of human meibum. Ophthalmic Res. (2015) 53:131–5. doi: 10.1159/000371852
40. Albarrán C, Pons AM, Lorente A, Montés R, Artigas JM. Influence of the tear film on optical quality of the eye. Contact Lens Anterior Eye. (1997) 20:129–35. doi: 10.1016/S1367-0484(97)80011-2
41. Ercan ZE. Effect of eyeliner and mascara use on tear film and meibomian glands. Saudi J Ophthalmol. (2022) 36:113–6. doi: 10.4103/sjopt.sjopt_170_21
42. Malik A, Claoué C. Transport and interaction of cosmetic product material within the ocular surface: Beauty and the beastly symptoms of toxic tears. Contact Lens Anterior Eye. (2012) 35:247–59. doi: 10.1016/j.clae.2012.07.005
43. Hadi H, Ai N, Zamli M, Awadh AI, Zafar MZ, Jamshed S. Cosmetic use-related adverse events: findings from lay public in Malaysia. Cosmetics. (2020) 7:41. doi: 10.3390/cosmetics7020041
44. Khan AZ, Fineide F, Magno MS, Hammer H, Chen X, Storås A, et al. Is eye makeup associated with poor ocular surface parameters in women with dry eyes? Invest Ophthalmol Vis Sci. (2023) 64:211.
45. Okereke JN, Udebuani AC, Ezeji EU, Obasi KO, Nnoli MC. Possible health implications associated with cosmetics: a review. Sci J Public Health. (2015) 3:58–63. doi: 10.11648/j.sjph.s.2015030501.21
46. Abusamak M, Jaber HM, Alrawashdeh HM. The effect of lockdown due to the COVID-19 pandemic on digital eye strain symptoms among the general population: a cross-sectional survey. Front Public Health. (2022) 10:895517. doi: 10.3389/fpubh.2022.895517
47. Mohammed AH, Hassan BAR, Wayyes AM, Al-Tukmagi HF, Blebil A, Dujaili J, et al. Exploring the quality of life of cosmetic users: a cross-sectional analysis from eight Arab countries in the Middle East. J Cosmet Dermatol. (2023) 22:296–305. doi: 10.1111/jocd.15085
Keywords: eye makeup, adverse reactions, cosmetovigilance, Jordanian females, web-based survey, ocular surface
Citation: Abusamak M, Al Zoubi S, Alomari AF, Issa SM, Abdul Aziz AA, Musleh A, Alrfooh H, Jarrar YB, Al-Amer R, Hamzeh R, Al-Kuran L and Abusamak TM (2025) Ocular adverse events associated with eye makeup: a cosmetovigilance-based cross-sectional study of prevalence and predictors among Jordanian women. Front. Public Health 13:1681656. doi: 10.3389/fpubh.2025.1681656
Received: 07 August 2025; Accepted: 25 September 2025;
Published: 16 October 2025.
Edited by:
Hasan Mahmud Reza, North South University, BangladeshReviewed by:
Watcharin Joemsittiprasert, New York Institution for Continuing Education, United StatesBarnali Chakraborty, North South University, Bangladesh
Copyright © 2025 Abusamak, Al Zoubi, Alomari, Issa, Abdul Aziz, Musleh, Alrfooh, Jarrar, Al-Amer, Hamzeh, Al-Kuran and Abusamak. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammad Abusamak, bUFidXNhbWFrQGJhdS5lZHUuam8=
 Mohammad Abusamak
Mohammad Abusamak Sura Al Zoubi
Sura Al Zoubi Amal F. Alomari
Amal F. Alomari Sara M. Issa
Sara M. Issa Ayman A. Abdul Aziz
Ayman A. Abdul Aziz Asma Musleh
Asma Musleh Hala Alrfooh3
Hala Alrfooh3 Yazun Bashir Jarrar
Yazun Bashir Jarrar Roa'a Hamzeh
Roa'a Hamzeh