- 1Department of Emergency Medicine, The People’s Hospital of Atushi City, Atushi, China
- 2Department of Urology Surgery, The People’s Hospital of Atushi City, Atushi, China
- 3Department of Cardiovascular Medicine, The People’s Hospital of Atushi City, Atushi, China
Background: Cardiopulmonary resuscitation (CPR) is a critical, life-saving intervention that is especially important in school settings. This study assessed the levels of CPR knowledge, training, and rescue willingness among school teachers in Xinjiang, China.
Methods: We conducted an online cross-sectional survey among 368 full-time teachers across primary, middle, and high schools (May–June 2025). A composite CPR readiness score (0–100) combined self-reported knowledge, training (formal or self-study vs. none), four core technical items (golden time, compression location, depth, rate), and rescue willingness. Group differences were assessed by Kruskal–Wallis with FDR-adjusted Mann–Whitney post hoc tests; categorical associations used chi-square with Cramer’s V; multivariable correlates of readiness were examined by OLS with robust SEs.
Results: Overall, 37.0% were trained (self-study or formal); 10.9% reported “very clear” knowledge. Technical knowledge accuracy was uneven: compression location 78.0%, golden time within 4 min 68.5%, compression rate 100–120/min 44.8%, and depth 5–6 cm 39.7%. Mean readiness was 55.7 ± 17.4 (95% CI: 53.9–57.4) and was higher in trained than untrained teachers (69.8 ± 13.3 vs. 47.4 ± 13.8; p < 0.0001). Readiness differed by age (p = 0.019; lower in 46–60 years) and ethnicity (Han 57.2 ± 16.6 vs. other minorities 52.8 ± 18.5; p = 0.027), and was higher among those aware of AED locations (69.3 ± 16.0; p < 0.0001). In OLS, training (+20.39 points [95% CI: 17.54–23.23]; p < 0.0001), AED awareness (+8.35 [4.09–12.62]; p = 0.000124), and often worrying about emergencies (+12.09 [4.37–19.81]; p = 0.002) were independent positive correlates; male sex (−3.54 [−6.91 to −0.18]; p = 0.039) and other minority ethnicity (−5.57 [−8.99 to −2.14]; p = 0.001) were negative.
Conclusion: The findings demonstrate an urgent need for systematic and culturally adapted CPR training programs among school teachers in Xinjiang, China.
Introduction
Out-of-hospital cardiac arrest (OHCA) remains one of the leading causes of mortality worldwide, with survival being heavily dependent on immediate intervention (1–3). The concept of the “chain of survival” indicates that early recognition, prompt initiation of cardiopulmonary resuscitation (CPR), and rapid defibrillation within the first few minutes can significantly increase survival probabilities from less than 10% to over 50% (4–10). In school environments where professional medical assistance is rarely immediately available, teachers are unlikely to have more than a few minutes to respond to life-threatening emergencies, making their ability to perform CPR essential. In China, where student-to-teacher ratios are high and school hours are long, the likelihood of witnessing a cardiac emergency is non-negligible.
International studies have documented wide variability in teacher CPR preparedness. While CPR training rates in high-income countries with mandatory training policies can exceed 50%, reports from other regions suggest substantially lower rates (11–17). In the ethnically and culturally diverse region of Xinjiang, China, unique challenges such as geographical isolation, limited access to quality healthcare training, and language barriers may further impede the acquisition and retention of CPR skills.
Against this backdrop, we conducted a cross-sectional survey to characterize CPR knowledge, training experience, and overall readiness among school teachers in Xinjiang. We further examined differences across demographic and contextual subgroups, mapped associations among key categorical factors, and identified multivariable correlates of CPR readiness to inform targeted, scalable interventions. Unlike many prior studies, we operationalized readiness as a composite construct integrating knowledge, training, core technical accuracy, and willingness—thus capturing preparedness more holistically than any single domain alone.
Methods
Study design and participants
We administered an online, anonymous, cross-sectional survey to full-time teachers across primary, middle, and high schools in Atushi, Xinjiang province, China from May to June 2025. The survey was distributed through WeChat groups associated with regional teacher associations. Eligibility criteria included active classroom teaching, direct student contact, Chinese literacy, and informed consent. Of 373 responses, 368 were retained after data cleaning and completeness checks.
Measures
The survey instrument was developed based on validated international CPR knowledge assessments and adapted for the Chinese context. The questionnaire underwent translation and back-translation by independent bilingual team members to ensure conceptual equivalence. English translations of all key survey items are provided in Supplementary Methods. The questionnaire comprised five sections. Demographics comprised gender, age, ethnicity (analyzed as Han vs. other minorities), education, and teaching level (primary, middle, and high). CPR knowledge and awareness included self-reported knowledge level, recognition of appropriate indications for CPR, awareness of school automated external defibrillator (AED) locations, and related perceptions. Training experience captured any prior training (self-study or formal), time since last training, and self-assessed skill mastery among those trained. Technical knowledge items assessed golden rescue time, chest compression location, depth, rate, and AED use timing. Emergency-related attitudes encompassed worry about emergencies, rescue willingness, volunteer willingness, and perceived necessity of teacher CPR training.
CPR readiness score
The primary outcome was a composite CPR readiness score (0–100) defined a priori from four domains: (1) self-reported CPR knowledge (0–30); (2) training experience (0–20: formal 20, self-study 10, none 0); (3) technical accuracy on four core items (0–30: golden time, compression location, depth, rate; 7.5 points each if correct); and (4) rescue willingness (0–20: willing & competent 20; willing but worried 15; need legal protection 10; not willing 0). The weighting scheme was developed through expert consensus involving three emergency physicians, aligning with international CPR assessment frameworks. Internal consistency was assessed using Cronbach’s alpha. To test robustness, we conducted sensitivity analyses with ±20% variations in component weights.
Statistical analysis
We summarized categorical variables as n (%) and continuous variables as mean ± SD with 95% confidence intervals (CI). Baseline characteristics were described overall and by training status (untrained vs. trained). Group differences for readiness used Kruskal–Wallis tests with Mann–Whitney post hoc comparisons when overall p < 0.05. Effect sizes were calculated using Cramer’s V for categorical associations, with values of 0.1, 0.3, and 0.5 representing small, medium, and large effects, respectively. To identify independent correlates of readiness, we fitted ordinary least squares (OLS) models with robust (HC3) standard errors; predictors included training (any vs. none), gender, age group, ethnicity, education, teaching level, AED location awareness, and worry about emergencies. Model assumptions were verified through comprehensive residual diagnostics including Q-Q plots, residuals versus fitted values plots, and scale-location plots. Multicollinearity was assessed using variance inflation factors (VIF), with values exceeding 5.0 considered problematic. All regression coefficients are reported with 95% confidence intervals. Statistical significance was set at p < 0.05.
Results
Participant characteristics
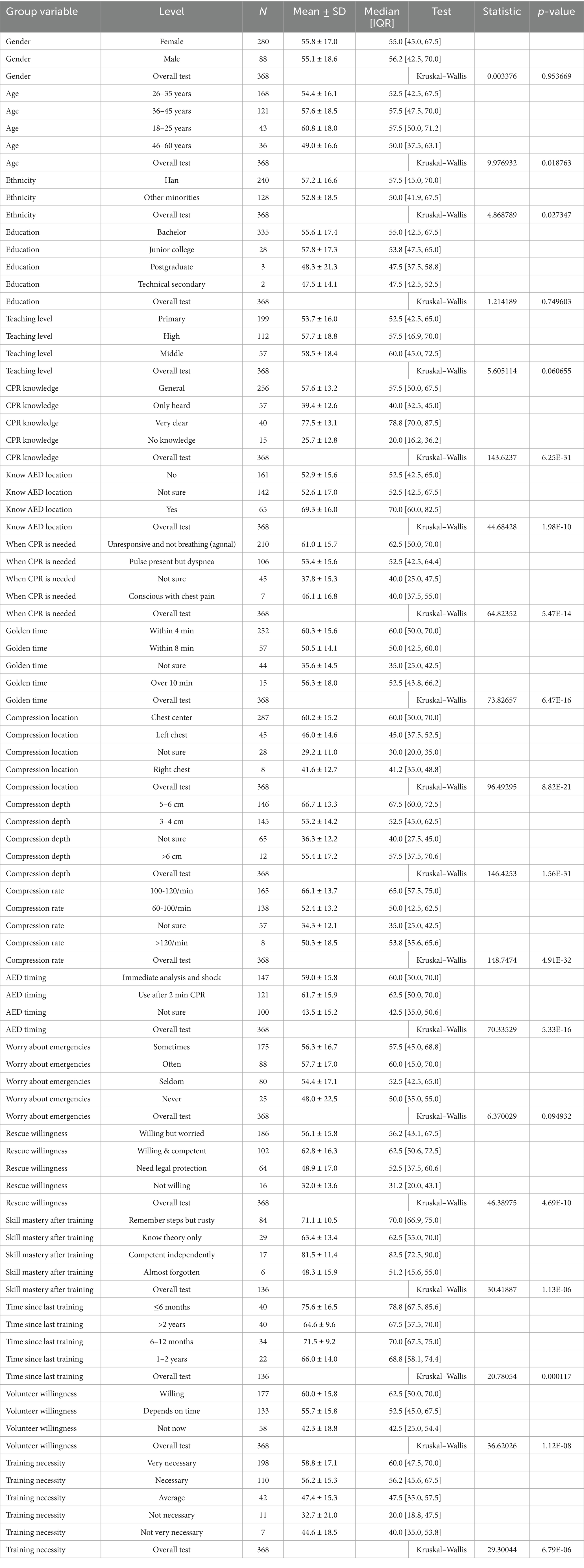
Among 368 teachers, 280 (76.1%) were female and 88 (23.9%) male (Table 1). Age distribution was 18–25 years 11.7%, 26–35 years 45.7%, 36–45 years 32.9%, and 46–60 years 9.8%. Ethnicity was Han 65.2% and other minorities 34.8%. Most held a bachelor’s degree (91.0%). Teaching levels were primary 54.1%, high 30.4%, and middle 15.5%. Overall, 37.0% were trained (self-study or formal).
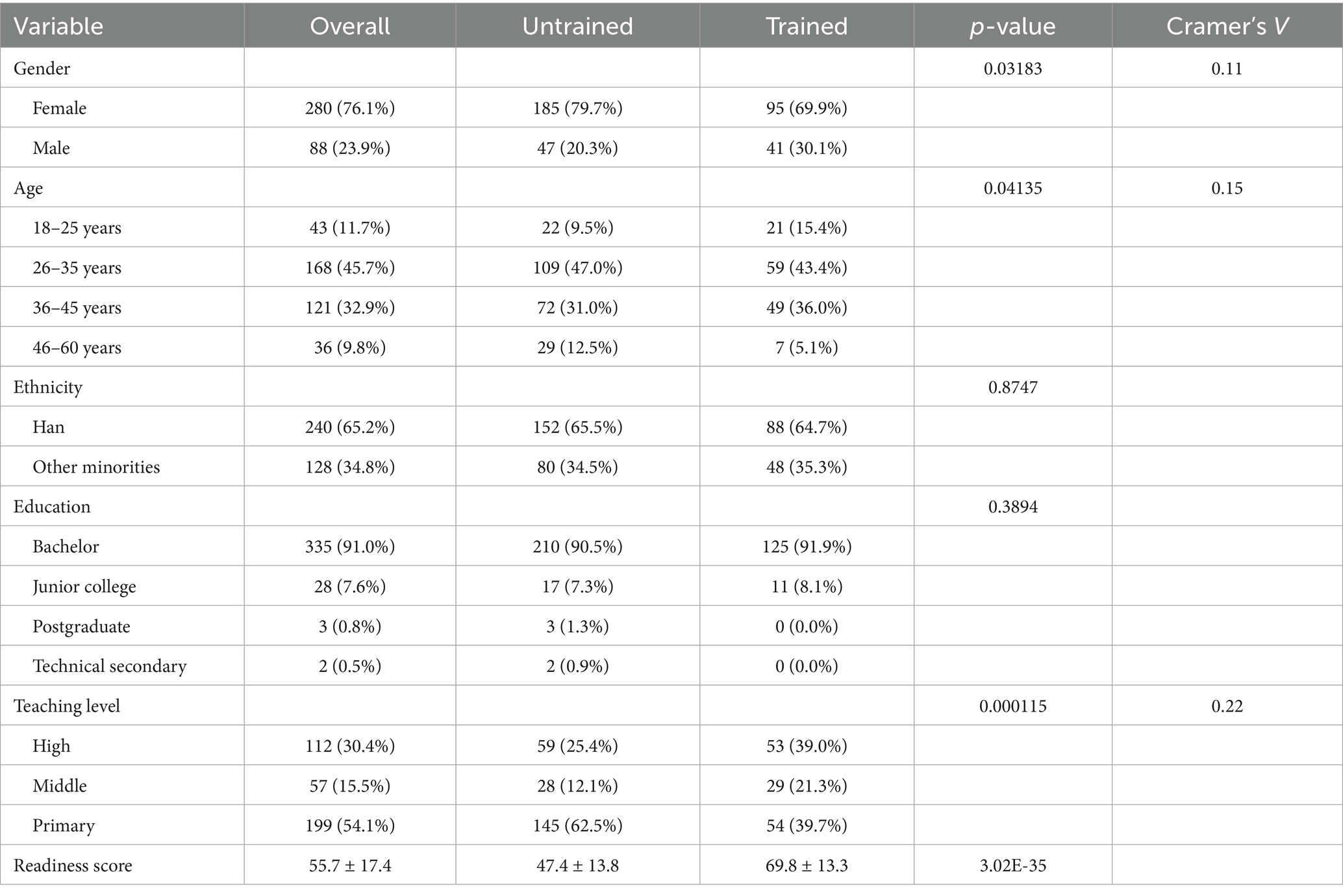
Table 1. The demographic information of the participants and the characteristics of the questionnaire (N = 368).
CPR knowledge and awareness
Self-reported CPR knowledge levels revealed concerning gaps: only 10.9% of teachers reported “very clear” knowledge enabling complete procedure description, while 69.6% had “general understanding but unclear details,” 15.5% had “only heard of the concept,” and 4.1% reported “no knowledge” (Table 1). Recognition of appropriate CPR application scenarios was moderate, with 57.1% correctly identifying “unresponsive with absent or abnormal breathing” as requiring immediate CPR. Awareness of AED device locations was limited, with only 17.7% knowing their school’s AED locations.
Training experience and skill retention
Overall CPR training rate was 37.0%, comprising 10.9% formal training through hospitals or Red Cross organizations and 26.8% self-study through videos or books (Supplementary Table 1). Among trained individuals (n = 136), training recency varied: within 6 months (29.4%), 6–12 months (25.0%), 1–2 years (16.2%), and over 2 years (29.4%). Skill retention among trained personnel was suboptimal: 12.5% felt capable of independent operation, 61.8% remembered steps but felt rusty, 21.3% retained only theoretical knowledge, and 4.4% had almost forgotten their training. Training status varied by gender (p = 0.032, Cramer’s V = 0.11), age (p = 0.041, Cramer’s V = 0.15), and teaching level (p < 0.001, Cramer’s V = 0.22), but not by ethnicity or education level.
CPR technical knowledge accuracy
Technical CPR knowledge was unevenly distributed among the respondents: 78.0% correctly identified the center of the chest as the optimal compression site, 68.5% recognized the recommended “golden time” interval of approximately 4 min for effective resuscitation, yet only 44.8 and 39.7% correctly reported the recommended compression rate (100–120/min) and depth (5–6 cm), respectively (Supplementary Table 1). On average, respondents answered 3.26 ± 1.52 of the six key technical questions correctly, with only 8.6% answering all items accurately and 23.9% responding correctly to two or fewer items.
Rescue willingness and barriers
While 78.2% of teachers expressed willingness to perform CPR, confidence levels varied significantly: 27.7% felt “willing and capable,” 50.5% were “willing but worried about mistakes,” 17.4% would act only with “legal protection,” and 4.3% were “unwilling to participate” (Supplementary Table 1). Concerns about encountering CPR situations were prevalent: 23.9% “frequently worried,” 47.6% “occasionally worried,” 21.7% “rarely worried,” and 6.8% “never worried.” Legal concerns emerged as a significant barrier, with 17.4% requiring legal protection before performing CPR.
Training preferences and perceived needs
The most preferred training methods were regular hands-on practice sessions (69.3%), expert lectures with certification (53.0%), and online courses with simulation (49.5%). Willingness to join CPR promotion teams was moderate: 48.1% willing, 36.1% depending on schedule, and 15.8% not considering (Supplementary Table 1). Notably, 83.7% of participants rated CPR training for teachers as “necessary” or “very necessary,” with only 3.0% considering it “unnecessary.” This high perceived need contrasted sharply with the low actual training rate.
The correlation between CPR training and CPR readiness
Training status was associated with multiple dimensions of preparedness in baseline comparisons. Trained teachers were more likely to report “very clear” CPR knowledge (21.3% vs. 4.7%) and less likely to report “only heard” (4.4% vs. 22.0%) or “no knowledge” (1.5% vs. 5.6%; p < 0.0001, Cramer’s V = 0.34) (Supplementary Table 1). They more often knew the location of AEDs (Yes: 33.1% vs. 8.6%; Not sure: 33.1% vs. 41.8%; No: 33.8% vs. 49.6%; p < 0.0001, Cramer’s V = 0.31). Technical knowledge distributions also favored trained teachers: correct chest compression location (88.2% vs. 72.0%; p = 0.000136, Cramer’s V = 0.24), correct depth 5–6 cm (54.4% vs. 31.0%) with far fewer “not sure” responses (2.2% vs. 26.7%; p < 0.0001, Cramer’s V = 0.34), correct rate 100–120/min (52.9% vs. 40.1%) with markedly fewer “not sure” (1.5% vs. 23.7%; p < 0.0001, Cramer’s V = 0.30), and golden time within 4 min (74.3% vs. 65.1%; p = 0.0045, Cramer’s V = 0.19). Recognition of correct CPR indications was higher among the trained (“unresponsive and not breathing (agonal)”: 67.6% vs. 50.9%; p < 0.0001, Cramer’s V = 0.25). Volunteer willingness also differed (willing: 55.9% vs. 43.5%; not now: 9.6% vs. 19.4%; p = 0.017, Cramer’s V = 0.15). Training status varied modestly by gender and age distributions (p = 0.0318 and p = 0.0413, respectively), whereas education and ethnicity did not.
CPR readiness score
Mean readiness was 55.7 ± 17.4 (95% CI: 53.9–57.4) (Figure 1). By training status, trained teachers scored higher than untrained (69.8 ± 13.3 [67.5–72.0] vs. 47.4 ± 13.8 [45.6–49.2]; Kruskal–Wallis p < 0.0001) (Table 2). Readiness did not differ by gender (p = 0.954) or education (p = 0.750) and showed a non-significant trend across teaching levels (p = 0.061). Age differences were significant overall (p = 0.0188); FDR-adjusted pairwise tests indicated lower readiness among 46–60 years compared with 18–25 years (p = 0.0339) and 36–45 years (p = 0.0339), with other contrasts not significant. Ethnicity was associated with readiness (Han 57.2 ± 16.6 vs. other minorities 52.8 ± 18.5; p = 0.0273; pairwise p = 0.0274).
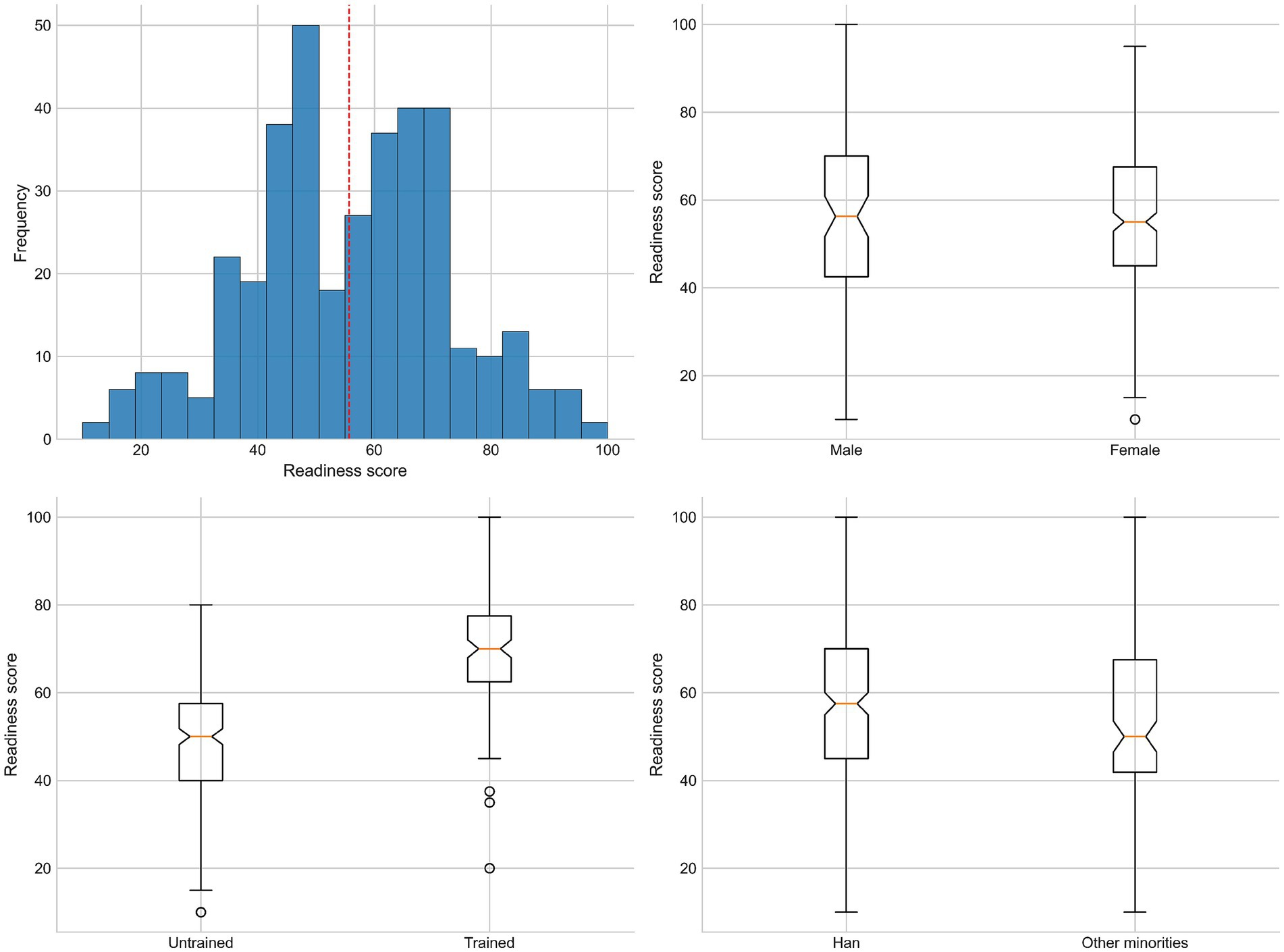
Figure 1. Statistical analysis of CPR readiness scores. Overall distribution (histogram) and group comparisons by gender, training status, and ethnicity.
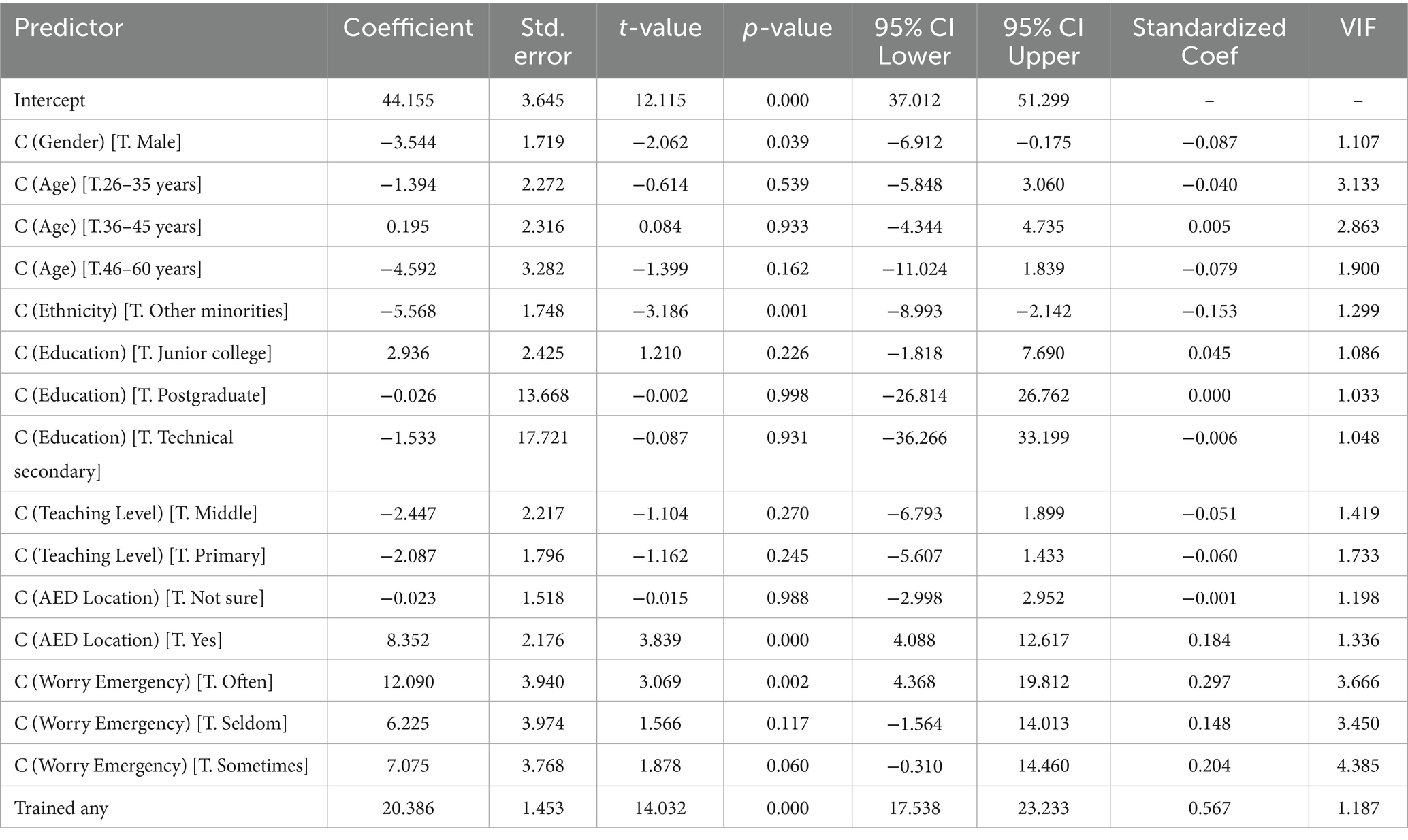
Multivariable correlates of CPR readiness
In the OLS model with robust (HC3) standard errors (adjusted R2 = 0.49), independent positive correlates of readiness were training (any vs. none: +20.39 points [95% CI: 17.54–23.23], standardized β = 0.57; p < 0.0001), AED location awareness (Yes vs. No: +8.35 [4.09–12.62], standardized β = 0.18; p = 0.000124), and often worrying about emergencies (Yes vs. never: +12.09 [4.37–19.81], standardized β = 0.30; p = 0.00215). Male gender (−3.54 [REVISED] [−6.91 to −0.18], standardized β = −0.09; p = 0.039) and other minority ethnicity (−5.57 [−8.99 to −2.14], standardized β = −0.15; p = 0.00145) were independently associated with lower readiness (Table 3 and Supplementary Figure 1). Age group, education, teaching level, and being “not sure” about AED location were not significant after adjustment. Variance inflation factors ranged from 1.03 to 4.39, all below the threshold of 5.0, indicating acceptable levels of multicollinearity. Stratified analyses showed that the positive effect of AED awareness persisted even among untrained teachers (+8.63 points, p = 0.023), suggesting independent contributions beyond training effects.
Discussion
This study provides a comprehensive, contemporary appraisal of CPR preparedness among school teachers in Xinjiang, China. Overall readiness was modest (55.7 ± 17.4), and only 37.0% of teachers had ever received CPR training, underscoring a critical implementation gap in a setting where teachers may be the first or only responders during the initial minutes of cardiac arrest. Although nearly 78% of educators expressed willingness to perform CPR, only a fraction felt capable when confronted with an emergency, a discrepancy that is likely to have significant implications for outcomes during actual cardiac arrest events. Against the backdrop of the international “chain of survival” concept, which demonstrates that early bystander CPR and defibrillation can dramatically improve survival rates, our findings suggest that even modest improvements in training coverage and skill sustainability could yield measurable benefits in school settings (4–10, 18, 19).
The comparison with international standards shows that the current training rate of 37.3% among teachers in Xinjiang, China is considerably lower than that reported in regions with mandatory training policies (17, 20–23). The uneven performance on technical questions is particularly disconcerting given that incorrect knowledge regarding compression rate and depth may detract from the overall quality of resuscitative efforts. Cultural factors such as language barriers and differing perceptions of legal responsibility for bystander intervention may contribute to both the low training uptake and the reluctance to act, despite high willingness levels.
The observed differences in readiness scores between Han teachers and those from other minority groups (57.2 ± 16.6 vs. 52.8 ± 18.5, p = 0.027) warrant careful interpretation within the complex socio-cultural context of Xinjiang. These disparities should not be interpreted as reflecting inherent differences between ethnic groups, but rather as indicators of systemic inequities in access to resources and opportunities for professional development. The independent negative association of minority ethnicity with readiness in multivariable analysis (β = −0.15, p = 0.001) persisted after controlling for other factors, suggesting that unmeasured structural barriers contribute to these disparities.
Our composite readiness score showed modest internal consistency (Cronbach’s α = 0.44), which is below the conventional threshold of 0.70. This likely reflects the multidimensional nature of CPR readiness, encompassing distinct domains of knowledge, training, technical skills, and psychological willingness that may not form a unidimensional construct. In addition, legal concerns emerged as a significant systemic barrier, with 17.4% of teachers requiring legal protection before being willing to perform CPR. This finding reflects broader societal concerns in China about legal liability for good-faith emergency interventions.
While the study was limited by its cross-sectional design, reliance on self-reported measures (which may overestimate actual CPR competency), and the single geographic region from which the questionnaire sample was drawn, it nonetheless provides critical insights that are directly applicable to the design of future educational interventions. Our data strongly advocate for the institution of mandatory, standardized CPR training programs within the educational system. With the proper deployment of training, AED infrastructure, and legal safeguards, teachers can be empowered to serve as confident and capable first responders, ultimately ensuring greater safety for students and the broader community.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of the People’s Hospital of Atushi City. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JM: Writing – review & editing, Writing – original draft, Data curation, Software, Investigation, Conceptualization. LK: Writing – review & editing, Writing – original draft, Data curation. XZ: Writing – review & editing, Data curation, Investigation, Conceptualization. QT: Writing – review & editing, Data curation, Investigation, Conceptualization. SL: Writing – review & editing, Data curation, Investigation, Conceptualization. WZ: Writing – review & editing, Writing – original draft, Data curation, Supervision, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1683122/full#supplementary-material
References
1. Kumar, A, Avishay, DM, Jones, CR, Shaikh, JD, Kaur, R, Aljadah, M, et al. Sudden cardiac death: epidemiology, pathogenesis and management. Rev Cardiovasc Med. (2021) 22:147–58. doi: 10.31083/j.rcm.2021.01.207
2. Sawyer, KN, Camp-Rogers, TR, Kotini-Shah, P, Del Rios, M, Gossip, MR, Moitra, VK, et al. Sudden cardiac arrest survivorship: a scientific statement from the American Heart Association. Circulation. (2020) 141:e654–85. doi: 10.1161/CIR.0000000000000747
3. Al-Khatib, SM, Stevenson, WG, Ackerman, MJ, Bryant, WJ, Callans, DJ, Curtis, AB, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the american College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Heart Rhythm. (2018) 15:e73–e189. doi: 10.1016/j.hrthm.2017.10.036
4. Ewy, GA. Cardiopulmonary resuscitation — strengthening the links in the chain of survival. N Engl J Med. (2000) 342:1599–601. doi: 10.1056/NEJM200005253422109
5. Bobrow, BJ, Panczyk, M, and Subido, C. Dispatch-assisted cardiopulmonary resuscitation: the anchor link in the chain of survival. Curr Opin Crit Care. (2012) 18:228–33. doi: 10.1097/MCC.0b013e328351736b
6. Ong, MEH, Perkins, GD, and Cariou, A. Out-of-hospital cardiac arrest: prehospital management. Lancet. (2018) 391:980–8. doi: 10.1016/S0140-6736(18)30316-7
7. Vallianatou, L, Kapadohos, T, Polikandrioti, M, Sigala, E, Stamatopoulou, E, Kostaki, EM, et al. Enhancing the chain of survival: the role of smartphone applications in cardiopulmonary resuscitation. Cureus. (2024) 16:e68600. doi: 10.7759/cureus.68600
8. Bunch, TJ, Hammill, SC, and White, RD. Outcomes after ventricular fibrillation out-of-hospital cardiac arrest: expanding the chain of survival. Mayo Clin Proc. (2005) 80:774–82. doi: 10.1016/S0025-6196(11)61532-2
9. Berdowski, J, Berg, RA, Tijssen, JGP, and Koster, RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. (2010) 81:1479–87. doi: 10.1016/j.resuscitation.2010.08.006
10. Herlitz, J, Svensson, L, Holmberg, S, Ängquist, KA, and Young, M. Efficacy of bystander CPR: intervention by lay people and by health care professionals. Resuscitation. (2005) 66:291–5. doi: 10.1016/j.resuscitation.2005.04.003
11. Cave, DM, Aufderheide, TP, Beeson, J, Ellison, A, Gregory, A, Hazinski, MF, et al. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: a science advisory from the American Heart Association. Circulation. (2011) 123:691–706. doi: 10.1161/CIR.0b013e31820b5328
12. Al Enizi, BA, Saquib, N, Zaghloul, MS, Alaboud, MS, Shahid, MS, and Saquib, J. Knowledge and attitudes about basic life support among secondary school teachers in Al-Qassim, Saudi Arabia. Int J Health Sci. (2016) 10:415–22. doi: 10.12816/0048736
13. Tamur, S, Alasmari, RM, Alnemari, MA, Altowairgi, MA, Altowairqi, AH, Alshamrani, NM, et al. Knowledge and attitudes around first aid and basic life support of kindergarten and elementary school teachers and parents in Taif City, Saudi Arabia. Children. (2023) 10:1266. doi: 10.3390/children10071266
14. Alahmed, YS, Alzeadi, HS, Alghumayzi, AK, Almarshad, LA, Alharbi, AS, and Alharbi, AS. Knowledge and attitudes of first aid and basic life support among public school teachers in Qassim, Saudi Arabia. Cureus. (2023) 15:e42955. doi: 10.7759/cureus.42955
15. Vaillancourt, C, Lui, A, de Maio, VJ, Wells, GA, and Stiell, IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. (2008) 79:417–23. doi: 10.1016/j.resuscitation.2008.07.012
16. van Nieuwenhuizen, BP, Oving, I, Kunst, AE, Daams, J, Blom, MT, Tan, HL, et al. Socio-economic differences in incidence, bystander cardiopulmonary resuscitation and survival from out-of-hospital cardiac arrest: a systematic review. Resuscitation. (2019) 141:44–62. doi: 10.1016/j.resuscitation.2019.05.018
17. Juul Grabmayr, A, Andelius, L, Bo Christensen, N, Folke, F, Bundgaard Ringgren, K, Torp-Pedersen, C, et al. Contemporary levels of cardiopulmonary resuscitation training in Denmark. Resusc Plus. (2022) 11:100268. doi: 10.1016/j.resplu.2022.100268
18. Shekhar, A, and Narula, J. Globally, GDP per capita correlates strongly with rates of bystander CPR. Ann Glob Health. (2022) 88:36. doi: 10.5334/aogh.3624
19. Sasson, C, Rogers, MAM, Dahl, J, and Kellermann, AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. (2010) 3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576
20. Sipsma, K, Stubbs, BA, and Plorde, M. Training rates and willingness to perform CPR in King County, Washington: a community survey. Resuscitation. (2011) 82:564–7. doi: 10.1016/j.resuscitation.2010.12.007
21. Perkins, GD, Gräsner, JT, Semeraro, F, Olasveengen, T, Soar, J, Lott, C, et al. European resuscitation council guidelines 2021: executive summary. Resuscitation. (2021) 161:1–60. doi: 10.1016/j.resuscitation.2021.02.003
22. Salvatierra, GG, Palazzo, SJ, and Emery, A. High school CPR/AED training in Washington state. Public Health Nurs. (2017) 34:238–44. doi: 10.1111/phn.12293
Keywords: cardiopulmonary resuscitation, school teachers, emergency preparedness, CPR training, Xinjiang, China
Citation: Ma J, Kuai L, Zhu X, Tang Q, Liu S and Zhou W (2025) Cardiopulmonary resuscitation knowledge and skills among school teachers in Xinjiang, China: a cross-sectional survey. Front. Public Health. 13:1683122. doi: 10.3389/fpubh.2025.1683122
Edited by:
Adriano Friganovic, University of Applied Health Sciences, CroatiaReviewed by:
Mouhajir Mohamed, Mohammed V University, MoroccoStjepan Petričević, Alma Mater Europaea - ECM, Slovenia
Copyright © 2025 Ma, Kuai, Zhu, Tang, Liu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiwei Zhou, d2VpZ29vMTIyNEAxNjMuY29t
†These authors have contributed equally to this work
 Jin Ma
Jin Ma Liuniu Kuai2†
Liuniu Kuai2†