- 1Affiliated Hospital (School of Clinical Medicine), Hangzhou Normal University, Hangzhou, China
- 2School of Public Health and Nursing, Hangzhou Normal University, Hangzhou, China
Objective: Current diagnostic frameworks for pathological personality are shifting from categorical to dimensional models. While the Personality Inventory for DSM-5 represents the most extensively validated dimensional measure across Western and Eastern cultures, its length limits practical utility. This study developed the Parker Personality Measure Short Form (PERM-SF) to facilitate efficient screening of pathological personality traits.
Methods: Two samples of college students (Sample 1: N = 1,768; 937 women and 831 men, aged 20.59 years ± 1.95, ranging from 16 to 27 years; Sample 2: N = 1,614; 887 women and 727 men, aged 20.38 years ± 1.59, 17–27 years) were recruited consecutively from one university in China through online random sampling. Exploratory factor analysis in Sample 1 identified items with robust psychometric properties for inclusion in the PERM-SF. Confirmatory factor analysis in Sample 2 validated the factor structure. Subsequent analyses evaluated internal consistency, longitudinal measurement invariance, and construct validity.
Results: Thirty-eight of the 92 items of PERM were deleted due to low factor loadings or high cross loadings, resulting in a five-factor model consisting of 54 items (F1: Dissociality, F2: Self-doubt-Detachment, F3: Disinhibition-Negative affectivity, F4: Anankastia, F5: Borderline pattern). All factors demonstrated good internal consistency (McDonald’s ω = 0.834–0.932). Longitudinal measurement invariance held at strict level (ΔCFI ≤ 0.001, ΔRMSEA ≤ 0.001) and two-way random-effects ICCs ranged from 0.488 to 0.759. Validity analyses revealed significant weak-to-moderate correlations with the Symptom Checklist-90 and established discriminant validity for all factor pairs, as supported by the Heterotrait-Monotrait Ratio test.
Conclusion: The PERM-SF exhibits adequate preliminary psychometric properties for rapid assessment of pathological personality dimensions, supporting its utility for research and screening applications at least among Chinese young adults.
1 Introduction
Personality is a composite reflecting an individual’s stable cognitive, emotional-affective, and behavioral patterns, encompassing past influences, interpretations of the present, and constructs for the future (1). The spectrum from a healthy personality to severe personality disorders forms a continuum that reflects varying degrees of pathological personality (2). A recent global systematic review and meta-analysis estimated the worldwide pooled prevalence of personality disorders (PDs) at 7.8% (3). Despite marked regional variations with reported prevalence rates of 4.1% in Asian populations (4), significantly lower than the 12.16% observed in Western countries (5), PDs contribute substantially to functional impairment, reduced productivity, and disease burden (6). Furthermore, PDs exhibit high comorbidity with other psychiatric conditions, exacerbating risks of premature mortality and suicidal behavior (2). Primary and secondary prevention strategies on personality disorders can monitor of risk factors operating at the population level, e.g., use of scales, and are needed to reduce the individual and societal burdens in the community (7). Therefore, to optimize patient outcomes and recovery, it is essential to assess pathological personality and identify personality disorders at an early stage.
Personality disorder (PD) diagnostic systems fall into two main categories. The first is the categorical diagnostic system of PD based on typical experiences and behaviors, with representative assessment tools such as the Personality Diagnostic Questionnaire-5 (8) and the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Personality Disorders (9), based on the widely used DSM-5. However, this categorical system faces many practical problems [(e.g., 6, 10)]. Firstly, the number of independent PD types is uncertain, and there are no clear boundaries between types and severity of PD. Additionally, the clinical presentation of patients with specific types of PD varies across cultures. For example, patients with borderline personality disorder under religious cultures had fewer addictive behaviors (11). Similarly, while obsessive-compulsive personality disorder in Western contexts is characterized by order, perfectionism, and control stemming from internal conflicts, its manifestation in Chinese patients is often associated with culturally shaped traits such as dependency, conformity, and self-restraint (12). Furthermore, different types of PD diagnosis present various issues of clinical utility (13). For instance, although effective evidence-based therapies are available for borderline personality disorder, there is a stigma attached to this group by mental health professionals (14), which might delay effective treatment and pose a lethal risk (15). Conversely, for other personality disorder types like antisocial, narcissistic, and avoidant, evidence of effective psychotherapy is limited (16).
Therefore, an alternative model has been adopted in both the DSM-5 Section III [the alternative model, DSM-5-AMPD, (9)] and the latest International Classification of Diseases-11 [ICD-11, (17)], namely the PD dimensional diagnostic system. This system places greater emphasis on assessing a patient’s core personality traits and the degree of impaired functioning rather than meeting specific PD symptoms (18, 19). Current instruments for assessing pathological personality traits mainly include the Personality Inventory for DSM-5 [PID-5, (18)], serial questionnaires based on the ICD-11 by Oltmanns and Widiger (20–22), and the Personality Assessment Questionnaire for ICD-11 (23), etc. The PID-5 is possibly the best available dimensional trait assessment tool, validated across diverse Western and Eastern cultures (24), demonstrating reliability and validity in capturing pathological personality traits per both DSM-5-AMPD and ICD-11 criteria (25), and it has both self-report (18) and informant-report (26) versions. However, the PID-5 comprises 220 items. During self-report, patients with PD often exhibit emotional instability, low treatment adherence (2), and may become irritable and uncooperative when required to complete time-consuming measurement tools, impacting the accuracy of the results.
The PID Brief Form [PID-5-BF, 25 items, (9)] and the Short Form [PID-SF, 100 items, (27)] addressed this issue effectively by reducing the number of items. So far, the PID-5-BF has been translated and adapted into Brazilian Portuguese (28), American (29), French (30), Portuguese (31), Italian (32) and Chinese (33) versions, and proved to be reliable and valid in general. However, the criterion-related validity of its Antagonism factor for typical personality disorder types was not satisfactory in the sole Asian sample (33), which therefore needs further validation. Unlike the PID-5-BF, which targets the five higher-order domains (9), the PID-5-SF efficiently assesses both DSM-5-AMPD traits and facets (27). However, its psychometric properties have mainly been reported in European countries [(31, 34–37)], and its structure has been inconsistent across some of these reports (34–36). Hence, a self-report instrument for rapid pathological personality trait screening in Asian cultures is demanding to complement the PID-5 in clinic settings, especially when an informant is unavailable.
The Parker Personality Measure [PERM, (38)] is a reliable and validated instrument for assessing pathological personality in Western culture, containing 92 clinical descriptions of impaired personality functioning across 11 personality disorder types, ten of which are consistent with DSM-5 classifications (9). The mean Cronbach’s α values for its 11 factors were 0.81 and 0.83 by self-report and corroborative witness, respectively (38). Studies involving college students and clinical populations have further demonstrated the reliability and validity of its Chinese version (39), reporting good internal consistency (alpha coefficients > 0.70) and adequate criterion-related validity with other personality measures like the Five-Factor Normal Personality Questionnaire and the Zuckerman–Kuhlman–Aluja Personality Questionnaire (39–41). Interestingly, the PERM also reflects a five-factor dimensional structure of pathognomonic personality. The authors named these domains “entitled/dissocial,” “inhibited,” “borderline,” “schizoid/schizotypal” and “obsessional” (38). The first four essentially correspond to most of the personality disorder dimensions in the ICD-11 and the Borderline pattern specifier (2, 24) and the last partially reflecting a feature of the Antagonism domain in the DSM-5-AMPD (24). Thus, the PERM could facilitate an understanding of the transition from categorical to dimensional diagnostic systems and pathological personality characteristics in specific populations. However, no study has yet fully validated the measurement properties of the five-factor dimensional structure of the PERM when categorical diagnostic criteria were in widespread use.
In recent years, mental health issues such as anxiety, depression, and insomnia have been frequently reported among college students [(e.g., 42, 43)], along with phenomena like suicide and self-injury [(e.g., 44)], cyberbullying (45), and cyber-addiction (46). These issues indicate that some students experience persistent psychological symptoms leading to impaired interpersonal and social functioning, often associated with dysfunctional personality [(e.g., 47)]. Furthermore, typical personality disorders account for a certain percentage of Chinese college students (48, 49), especially among those with internet addiction (50). Therefore, the college student population may well reflect the continuum of personality functioning impairment from normal personality to personality disorder. Considering their ability to understand the questionnaires and sample accessibility, we chose college students as subjects.
The aim of this study is to further refine the items with the highest factor loadings, develop the Short Form of PERM (PERM-SF), and validate its measurement properties in Chinese. This facilitates rapid assessment and early intervention for pathological personality traits, thereby reducing the economic and social burden on patients and families, and further optimizing the allocation of public health resources. We will also discuss whether its structure complies with the dimensional model of ICD-11 or DSM-5-AMPD, and cross-cultural stability of its factor connotations.
2 Methods
2.1 Participants
Sample 1 (N = 1,768; 937 women and 831men, aged 20.59 years ± 1.95, ranging from 16 to 27 years) and Sample 2 (N = 1,614; 887 women and 727 men, aged 20.38 years ± 1.59, 17 to 27 years) were recruited from one comprehensive university in Zhejiang Province, China in September 2021 to January 2023 and March 2023 to January 2024 with random sampling, respectively. Both samples completed the online electronic version of the questionnaire via Chinese public questionnaire platform “Questionnaire Star”.1 The exclusion criteria for the fillers were as follows: (1) incomplete completion of the questionnaire; (2) identical answers to all items; (3) less than 5 min to complete the questionnaire; or (4) a standardized score of more than 65 on the Lie factor of the PERM, indicating possible masking of psychological symptoms. After excluding these cases one by one (4.21, 1.55, 3.06, and 2.74%, respectively), the overall valid response rate to the questionnaire was 88.44%.
Additionally, a cohort of 339 subjects in Sample 2 was drawn from March to June 2023 to complete the Symptom Checklist-90 [SCL-90, (51)] to further assess the divergent validity of the PERM-SF. Given the convenience and accessibility of the study, 202 subjects from Sample 2 were randomly invited to retake the PERM-SF questionnaire, with a mean measurement interval of 64.40 (±21.05) days, to assess longitudinal measurement invariance. The purpose, voluntariness, and privacy measures of the study were clearly explained in the study guidelines (survey results would be used for research purposes only; names could be replaced by initials), and feedback on results based on the original PERM was provided according to the needs of the subjects.
2.2 Measurement instruments
2.2.1 The Parker personality measure
The PERM (38) is a self-reported personality scale with 92 clinical symptom items and 10 validity items designed to assess 11 different functioning styles of personality disorder, including Paranoid (10 items), Schizoid (8 items), Schizotypal (5 items), Antisocial (10 items), Borderline (10 items), Performative (6 items), Narcissistic (8 items), Avoidant (10 items), Dependent (10 items), Obsessive-Compulsive (6 items) and Passive-Aggressive (9 items). Each item is measured on a 5-point Likert scale (1 = very unlike me, 2 = moderately unlike me, 3 = somewhat like and unlike me, 4 = moderately like me, and 5 = very like me). Higher PERM factor scores indicate more severe personality disorder functioning styles. In this study, we revised the Chinese version of PERM with the permission of Gordon Parker, the lead author of the original questionnaire. The PERM-SF was developed following the Chinese Version of the PERM (PERM-C) by Wang et al. (39), which has good reliability and validity in previous studies (39–41).
2.2.2 The Symptom Checklist-90
The SCL-90 (51) is a self-rating scale consisting of 90 items assessing nine dimensions of symptoms, namely somatization, depression, paranoid ideation, anxiety, psychosis, anxiety, hostility, interpersonal sensitivity, and obsessive-compulsive symptoms. Each item is scored on a 5-point scale from 1 (no) to 5 (severe). A higher total score reflects greater overall severity of psychological distress in the past week. The scale has shown good psychometric properties in a population of Chinese college students (52), and its Cronbach’s α in this study was 0.982 (n = 339).
2.3 Statistical analysis
Structural validity, internal consistency, longitudinal measurement invariance, and construct validity of the PERM-SF were assessed in accordance with the COnsensus-based Standards for the selection of health status Measurement Instruments (COSMIN) guidelines (53–55). All analyses were conducted using SPSS 21.0, JASP 0.19.3 and R 4.5.1.
2.3.1 Structural validity
Exploratory factor analysis (EFA) was performed on the 92 clinical symptom items of the PERM-C using Sample 1 to validate its factor structure. Data factorability was first assessed via the Kaiser-Meyer-Olkin (KMO) measure and Bartlett’s test of sphericity. Principal component analysis was subsequently conducted, with the optimal number of factors determined through combined application of eigenvalue criterion with scree plot inspection (56), and Horn’s parallel analysis (57). Varimax rotation (maximum variance method) accounted for potential factor correlations. Items were systematically excluded according to these criteria: (1) target loadings were less than 0.450; (2) cross-loadings were greater than 0.400 (58, 59); and (3) assignment to factors containing fewer than three items.
After excluding ineligible items, the remaining ones were evaluated to construct a revised structural model of the PERM-SF. Confirmatory factor analysis (CFA) was applied to validate the factor model in Sample 2 using the Diagonally Weighted Least Squares estimator in R4.5.1, with model fit assessed via goodness-of-fit indices and the root mean square error of approximation (RMSEA) (60, 61). If the comparative fit index (CFI) and the Tucker-Lewis index (TLI) were greater than 0.900, and the standardized root mean square residual (SRMR) and RMSEA were less than 0.080, the GOF metrics would be considered to be good, and the model would be considered good, and the model would be well-fitted (62). The finalized factor model would be used for further analyses.
2.3.2 Internal consistency
Cronbach’s α and McDonald’s ω were used to assess internal consistency of the PERM-SF. However, since the use of α as an indicator of internal consistency suffered from several problems, e.g., inconsistency of results with hypotheses affecting the assessment (63), McDonald’s ω, which has less demanding assumptions and captured the effect of deleted items on overall reliability (64), was mainly considered in the current study.
2.3.3 Longitudinal measurement invariance
The longitudinal measurement invariance (configural, metric, scalar, strict) of the PERM-SF was rigorously tested using longitudinal CFA with temporally repeated measurements to ensure scale stability over time. In configural invariance model, all parameters were free to test whether the proposed factor structure fitted uniformly across groups. In metric invariance model, the factor loadings of each group were constrained to be equal. In the scalar invariance model, the factor loadings and the observed variable intercepts were constrained to test whether they were equal across groups. Finally, in strict invariance model, factor loadings, intercepts, and residuals were constrained to be equal across groups. Longitudinal measurement invariance was assessed based on the variance of fit metrics such as CFI, TLI, and RMSEA (65). Models were considered acceptable if ΔCFI was less than 0.010, ΔTLI was less than 0.010, and ΔRMSEA was less than 0.015 (66–68).
2.3.4 Test–retest reliability
Using data from 202 subjects in Sample 2, we assessed the test–retest reliability of the PERM-SF factors by calculating the Intraclass Correlation Coefficient (ICC) under a two-way random-effects model for absolute agreement. The level of agreement was interpreted according to Cicchetti’s (69) criteria: below 0.40 indicated poor agreement; 0.40–0.59, fair; 0.60–0.74, good; and 0.75–1.00, excellent. Per COSMIN guideline (55), reliability (ICC) > 0.7, Rating +.
2.3.5 Construct validity
To assess divergent validity, bivariate Spearman correlations were examined. Specifically, correlations were calculated, respectively, between the PERM-SF factors (where a correlation of r > 0.50 was expected), and between these PERM-SF factors and the SCL-90 total score. |r| < 0.30 indicates a weak correlation, 0.30 ≤ |r| < 0.70 indicates a moderate correlation, and 0.70 ≤ |r| ≤ 1.00 indicates a strong correlation (70, 71). For factor intercorrelations, above 0.80 or 0.85 implies poor discriminant validity (72). Given the related yet dissimilar constructs of the PERM-SF and the SCL-90, the former assesses core personality traits and personality dysfunction, whereas the latter one screening for a broader range of psychological symptoms and their severity (52), a low to moderately significant positive correlation between the two was expected (73). On the other hand, the SCL-90-Revised Personality Severity Index (PSI), which is calculated with the total score of the subscales addressing interpersonal problems (i.e., interpersonal sensitivity, hostility, and paranoid ideation), indicating the severity of personality disorder (74). Inspired by studies related to the SCL-90-R PSI (75), a moderate positive correlation between the PSI index calculated using the SCL-90 and the PERM-SF was expected. Construct validity was deemed satisfactory if at least 75% of the correlations aligned with these expectations (55). Discriminant validity was further evaluated using the Heterotrait-Monotrait Ratio (HTMT), with values below 0.85 considered acceptable.
3 Results
3.1 Structural validity
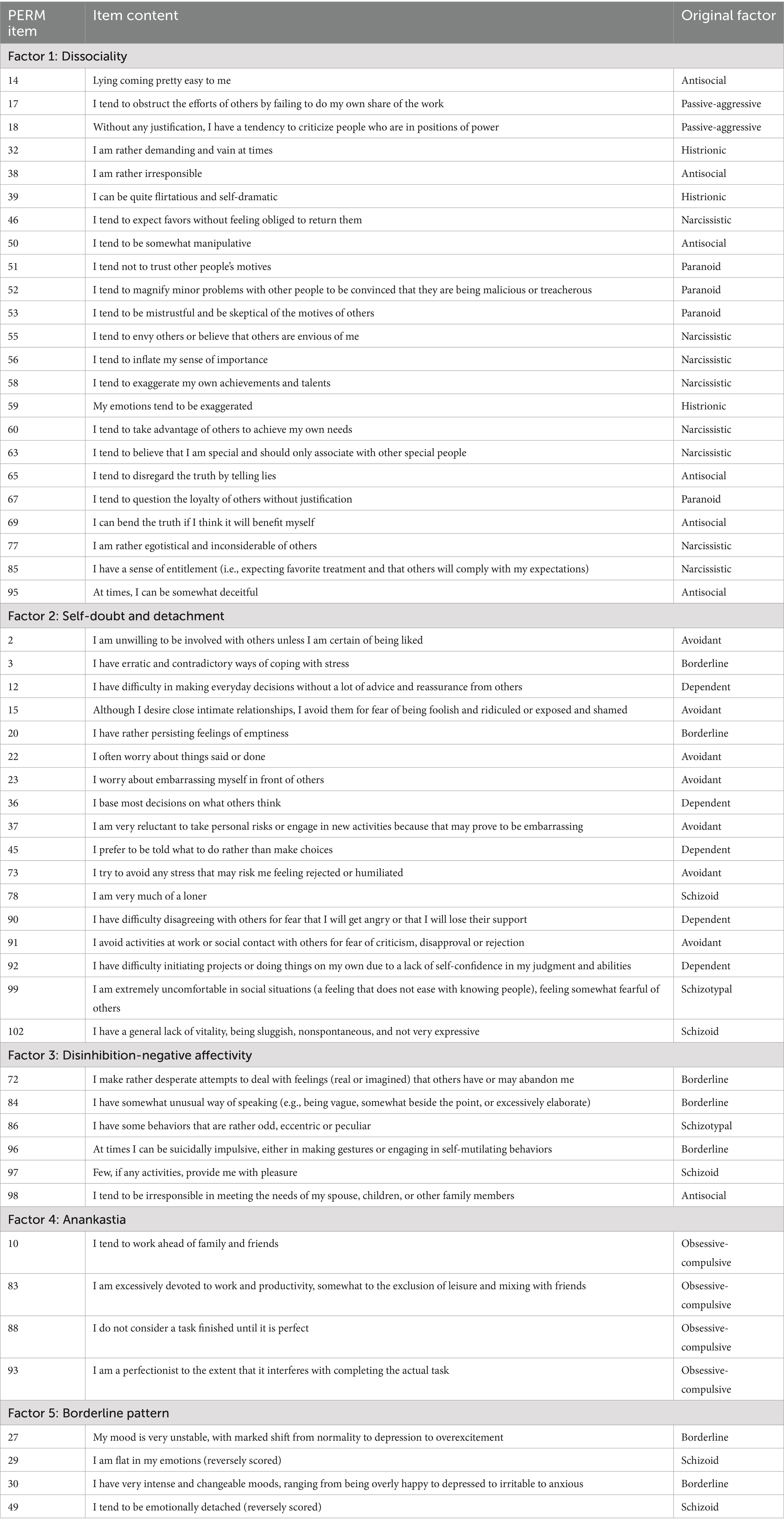
Using the eigenvalue criterion and scree plot, EFA was conducted on Sample 1 (college students), initially yielding a six-factor structure with maximum rotation (KMO = 0.975; Bartlett’s test: χ2 = 79597.179, p < 0.001), which explained 44.73% of the total variance. Items 01, 05, 06, 07, 08, 09, 13, 16, 19, 21, 24, 25, 26, 31, 33, 34, 40, 41, 42, 43, 47, 48, 54, 61, 62, 64, 66, 68, 70, 71, 74, 76, 79, 81, 82, 87, 94, and 100 were subsequently excluded based on low factor loadings (<0.45) or substantial cross-loadings (>0.40). Analysis of the remaining 54 items revealed a stable five-factor structure (KMO = 0.963; Bartlett’s test: χ2 = 45010.892, p < 0.001), accounting for 49.06% of the total variance. As all retained items met the criteria for factor loading and cross-loading, the EFA supported a five-factor solution comprising 54 items. The factor composition was as follows: Factor I (F1): Items 14, 17, 18, 32, 38, 39, 46, 50, 51, 52, 53, 55, 56, 58, 59, 60, 63, 65, 67, 69, 77, 85, 95; Factor II (F2): Items 02, 03, 12, 15, 20, 22, 23, 36, 37, 45, 73, 78, 90, 91, 92, 99, 102; Factor III (F3): Items 72, 84, 86, 96, 97, 98; Factor IV (F4): Items 10, 83, 88, 93; Factor V (F5): Items 27, 29 (reverse-scored), 30, 49 (reverse-scored). Factor loadings are presented in Table 1. This refined instrument was designated the Short Form of PERM (PERM-SF; see Table 2 for item details). Parallel analysis initially suggested nine factors. However, applying the retention criteria (≥3 items with loadings > 0.45 and cross-loadings < 0.40) also supported a five-factor solution.
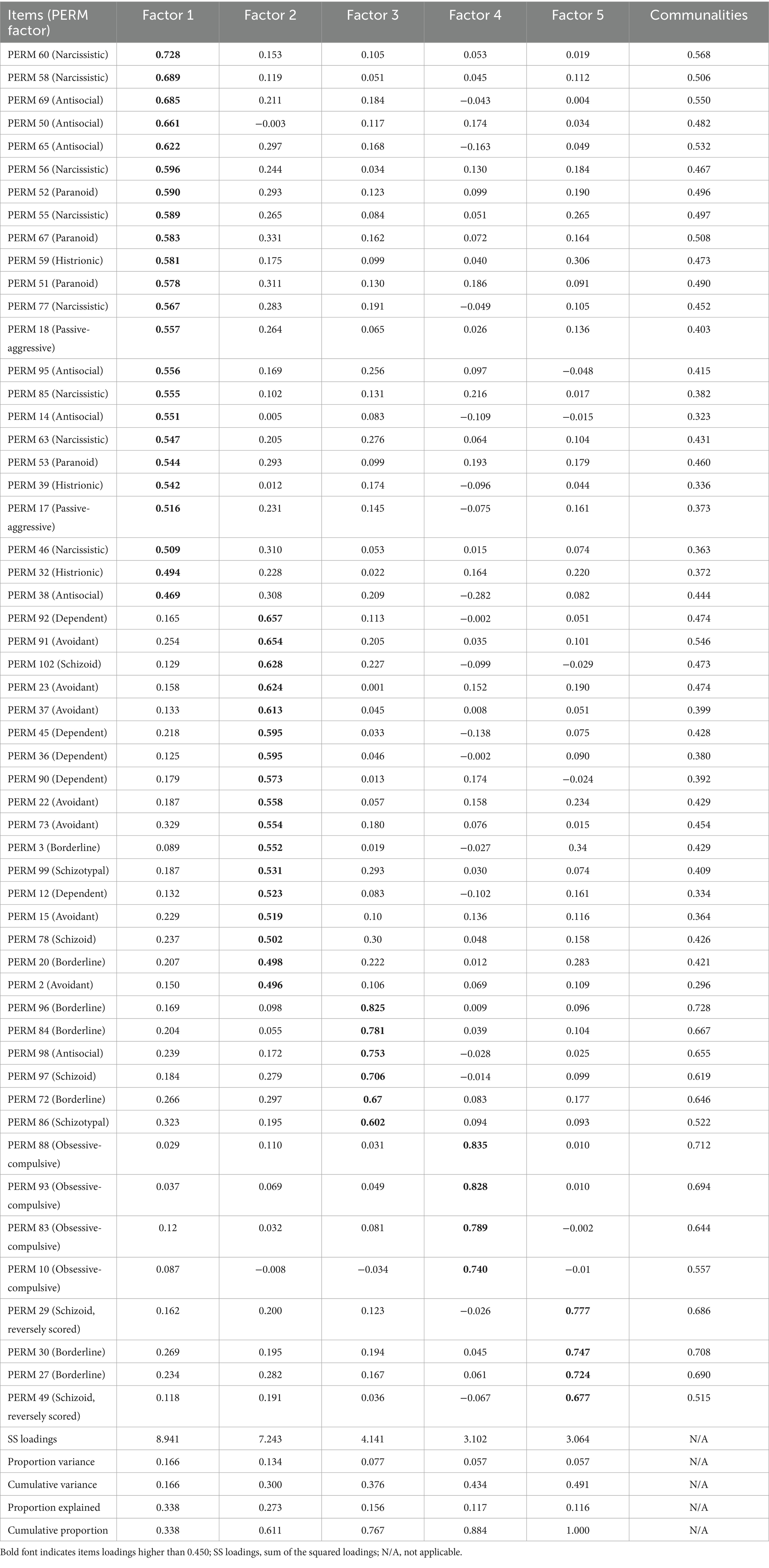
Table 1. Factor loadings for each item in the exploratory factor analysis (with Sample 1, N = 1,768).
CFA results for Sample 2 (college students) are presented in Table 3 and Figure 1. The five-factor PERM-SF model demonstrated a superior fit to Parker and Hadzi-Pavlovic’s (38) original 11-factor model, as evidenced by the following indices: CFI = 0.971, TLI = 0.970, SRMR = 0.059, and RMSEA = 0.063. In contrast, although formally identifiable, the 11-factor model suffered from severe statistical limitations, most notably near-perfect correlations between multiple latent variables (e.g., Histrionic–Narcissistic, r = 0.974). These high correlations indicate a lack of discriminant validity and directly contradict the model’s assumption of independent constructs. Given these issues, the more parsimonious five-factor model is statistically preferable. The five factors were named sequentially as Dissociality, Self-doubt-Detachment, Disinhibition-Negative Affectivity, Anankastia, and Borderline Pattern.
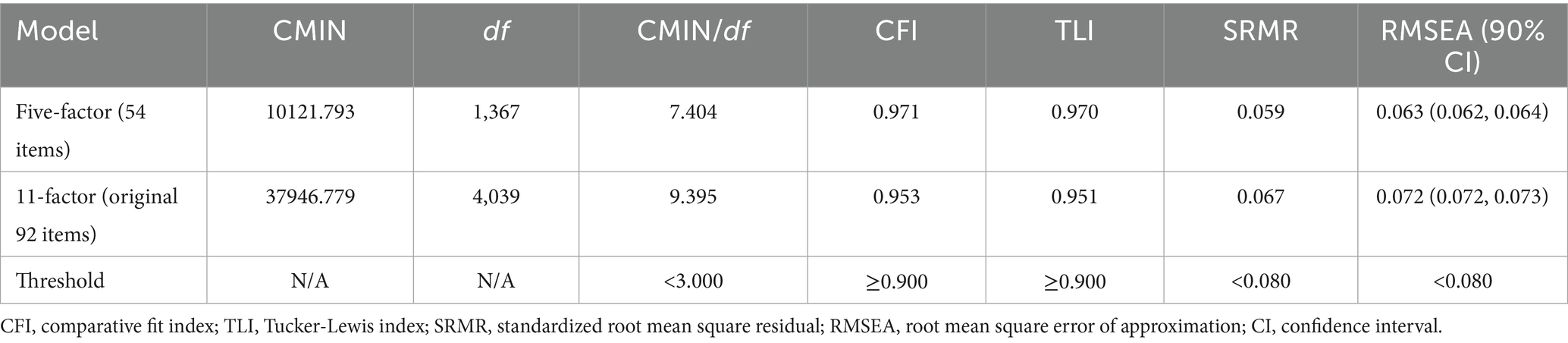
Table 3. Confirmatory factor analysis of alternative factorial solutions of the Short Form of Parker Personality Measure (with Sample 2, N = 1,614).
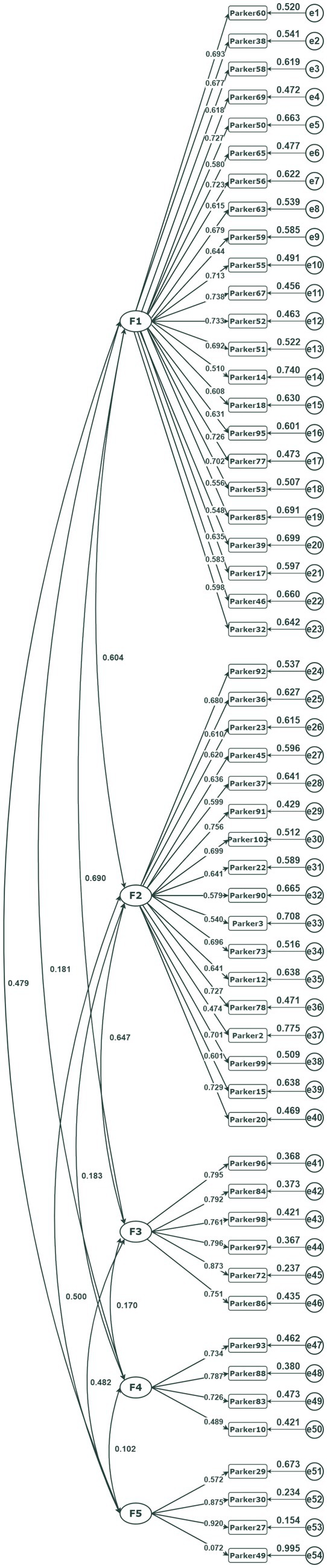
Figure 1. Standardized coefficients of confirmatory factor analysis results for a five-factor model of the Short Form of Parker Personality Measure (with Sample 2, N = 1,614).
3.2 Internal consistency
Internal consistency estimates for the PERM-SF are detailed in Table 4. Both McDonald’s ω and Cronbach’s α demonstrated good internal consistency in Sample 1, with ω ranging from 0.834 to 0.932 and α from 0.832 to 0.932.

Table 4. Internal consistency of the Short Form of Parker Personality Measure (PERM-SF, with Sample 1, N = 1,768).
3.3 Longitudinal measurement invariance
As presented in Table 5, measurement invariance testing in the Sample 2 subsample (n = 202) demonstrated all incremental fit index differences (ΔCFI, ΔTLI, ΔRMSEA) fell within established thresholds. These results suggest temporal stability of the measurement model across assessment points.
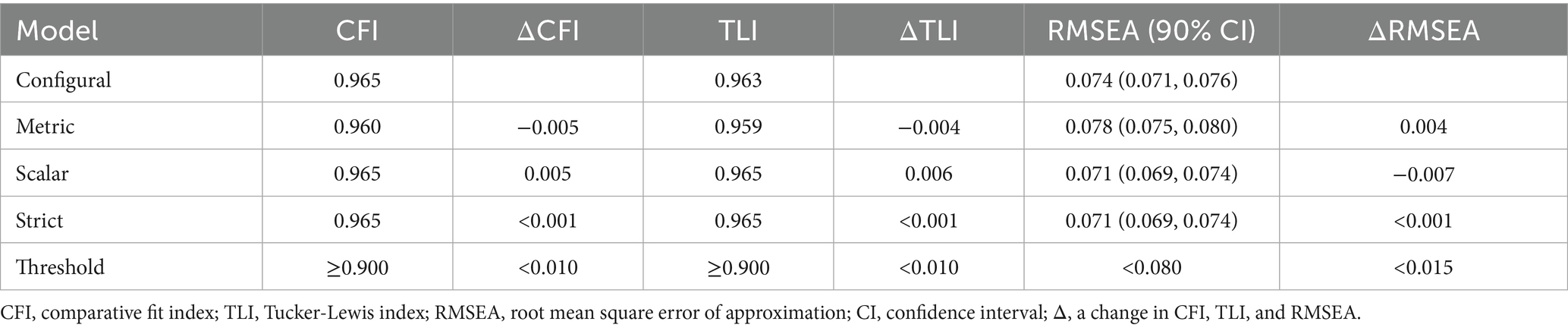
Table 5. Test of measurement invariance of the Short Form of Parker Personality Measure across time (with part of Sample 2, n = 202).
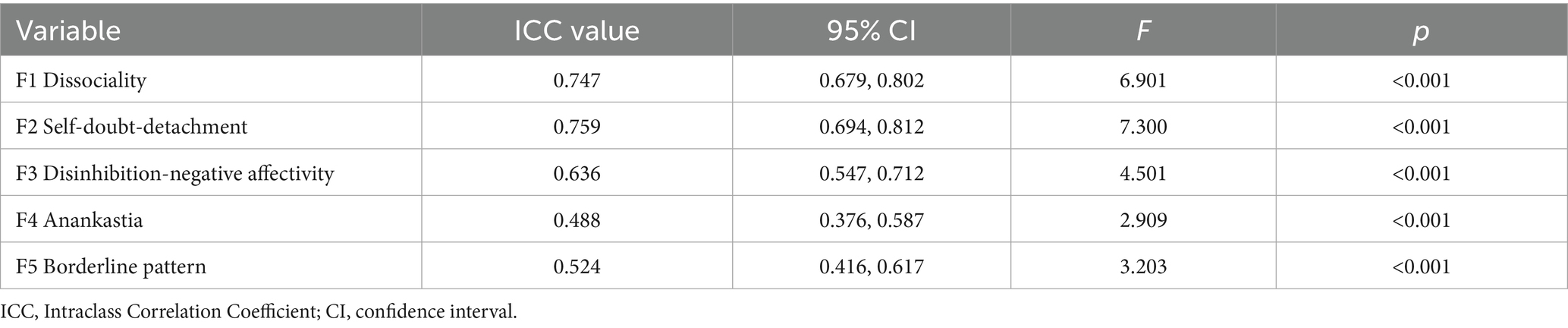
3.4 Test–retest reliability
As shown in Table 6, two-way random-effects ICCs ranged from 0.488 to 0.759 for the five factors of PERM-SF, indicating acceptable test–retest reliability.
3.5 Construct validity
As shown in Table 7, weak to moderate positive intercorrelations were observed among PERM-SF factors (rs = 0.104–0.630, Ps < 0.01), except for the non-significant association between Anankastia and Borderline Pattern (r = 0.047, p = 0.060). Additionally, each PERM-SF factor showed weak to moderate positive correlations with the SCL-90 total score and PSI (rs = 0.182–0.494, Ps < 0.01). Finally, discriminant validity was supported by the HTMT analysis, in which all values remained below the 0.85 threshold, as confirmed by bootstrap confidence intervals.
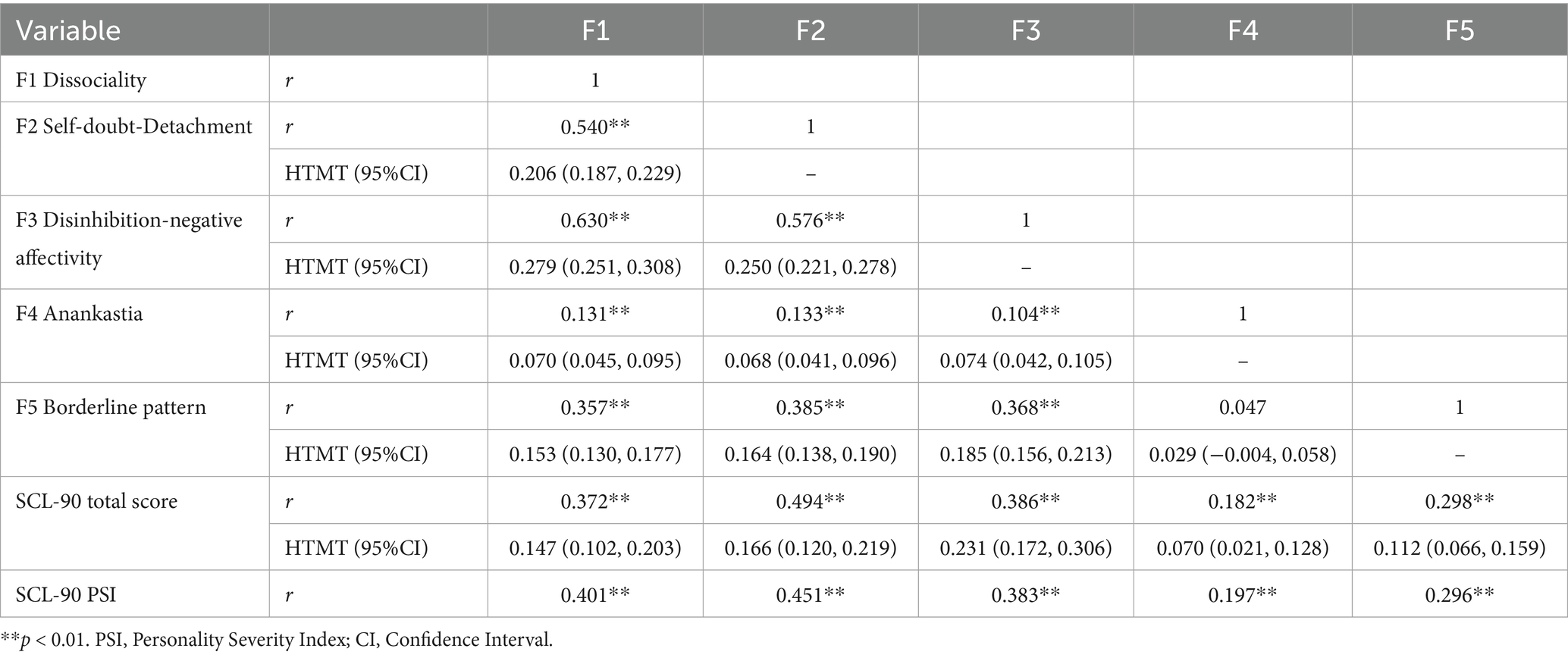
Table 7. Bivariate correlations and Heterotrait-Monotrait Ratio (HTMT) for the Short Form of Parker Personality Measure (PERM-SF) and Symptom Checklist-90 (SCL-90) (with Sample 2, N = 1,614; for correlations and HTMTs of SCL-90, with part of Sample 2, n = 339).
4 Discussion
This study investigated the measurement properties of the PERM-SF in a Chinese college student sample. Compared to the original PERM’s retention threshold [items with loadings ≥ 0.30; (38)], we implemented more stringent criteria, resulting in substantial item reduction. Notably, five-factor structure of the PERM-SF basically covered all the personality disorder dimensional features of ICD-11, including the borderline pattern specifier. This differs somewhat from the structure of the widely used PID (18), which captured different facets in both DSM-5-AMPD and ICD-11 criteria (76). Furthermore, the PERM-SF demonstrated acceptable internal consistency and construct validity while satisfying longitudinal measurement invariance requirements. Collectively, these findings provide preliminary evidence for the PERM-SF’s reliability and utility in assessing pathological personality dimensions.
4.1 Structural validity
EFA provided initial evidence for the PERM-SF’s five-factor structure, subsequently supported by CFA. The current factor composition demonstrated both continuity and expansion relative to Parker and Hadzi-Pavlovic’s (38) original PERM: F1 Dissociality retained narcissistic, antisocial, and histrionic features from the original dissocial factor, while incorporating additional passive-aggressive and paranoid traits. F2 Self-doubt-Detachment preserved dependent and avoidant characteristics akin to the original inhibited factor, but expanded to include schizoid, schizotypal, and borderline features. F3 Disinhibition-Negative Affectivity incorporated schizoid/schizotypal traits from the original counterpart, while integrating additional borderline and antisocial expressions. F4 Anankastia maintained obsessive-compulsive features consistent with the original factor. F5 Borderline Pattern conserved core borderline characteristics while assimilating schizotypal elements. This empirical alignment supports the structural plausibility of the five-factor personality disorder model. The observed trait overlaps across factors are consistent with diagnostic convergence between DSM-5-AMPD and ICD-11 dimensional frameworks (76). Notably, these findings echo Parker and Hadzi-Pavlovic’s (38) original observation that paranoid traits predominantly loaded onto Cluster B personality disorders.
The five factors in this study were under the dimensions of PD covered by the ICD-11, except that Factor 2 was changed from Interpersonal Detachment to Self-doubt-Detachment. Compared with that in the ICD-11, the PERM-SF Self-doubt-Detachment reflects social withdrawal, avoidance of intimacy, lack of self-confidence and reduced emotional expression but not indifference to others. This suggests that in Chinese culture, self-doubt or low self-confidence rather than emotional indifference is the primary cause of interpersonal detachment in individuals with pathological personality traits. This may lead to uncertainty about the attitudes of others in interpersonal relationships and fear of being devalued, resulting in a tendency to distance oneself from others. Cross-cultural studies of social behavior have also found that people with self-doubt who were different from the dominant culture tended to be more reserved and averse to stares (77), and that the expression of social anxiety in the context of cultural difference was related to the degree to which one defined him/herself as independent or in need of interdependence (78). This finding also made a clearer distinction between Factor II and Factor I (Dissociality) in the PERM-SF compared to the two factors Dissociality and Detachment in the ICD-11, i.e., they reflect more passive and more active causes of interpersonal problems, respectively. In addition, the Disinhibition and Negative Affectivity factors were combined into Factor III, which embodied impulsivity without regard to risks and consequences, irresponsibility, and negative emotional feelings such as loss of pleasure and feelings of abandonment, but not distraction. While there was already a precedent for combining Impulsive and Borderline into Emotionally unstable in ICD-10 (2), the results of the present study suggested a stronger association between lack of inhibition and negative affectivity rather than the borderline pattern, which contributed to pathological personality in Chinese culture. Previous evidence also suggested a strong relationship between the Inhibition domain and its various aspects and negative affect such as anxiety and depression (79, 80). Factor IV Anankastia in the current study exemplifies behavioral control over self, emotional discipline and perfectionism, but not control over others. Previous research has found a bipolar relationship between Anankastia and Disinhibition (81), and the emphasis on social role obligations and the need for hierarchical obedience relationships in traditional Chinese Confucian culture may make socially maladjusted individuals more prone to internal emotion regulation in order to conform to social norms (82–84). The borderline pattern was the fifth factor that embodied unstable emotions, but not unstable interpersonal relationships and self-image. This was partly because the latter was more highly correlated with Factor 2, and partly because Chinese culture was subtle and implicit and promoted a high degree of interpersonal harmony (85), which made individuals more inclined to minimize the external expression of their emotions to avoid possible damage to their relationships (86).
Notably, prior research extracting metrics from three personality instruments (PERM-C, Five-Factor Nonverbal Personality Questionnaire, Zuckerman-Kuhlman Personality Questionnaire) in Chinese populations similarly identified a five-factor structure (39). The current solution demonstrates both convergence and divergence with this earlier model. Namely, Dissocial (FI), Inhibition (FIV), and Compulsivity (FV) align with pathological dimensions identified here; Emotional Dysregulation (FIII) is superseded by the Borderline Pattern; Experience Seeking (FII), which showed minimal PERM-C loadings previously, is replaced by Self-doubt-Detachment. These structural differences may stem from measurement focus variation. Whereas the items of Wang et al. (39) primarily captured normal personality variation, the current instrument exclusively operationalizes pathological personality descriptors.
4.2 Internal consistency
The PERM-SF demonstrated good internal consistency, with both McDonald’s ω and Cronbach’s α coefficients exceeding 0.80 for all five factors, indicating acceptable reliability. Importantly, item reduction enhanced reliability coefficients compared to the original PERM. Thus, given its psychometric properties and assessment efficiency, the PERM-SF represents a psychometrically sound option when time constraints prioritize brief self-assessment protocols.
4.3 Longitudinal measurement invariance
Longitudinal measurement invariance of the PERM-SF was supported through the longitudinal CFA. Model comparisons revealed non-significant Δχ2 values across configural, metric, scalar, and strict invariance levels, while ΔCFI, ΔTLI, and ΔRMSEA remained within established thresholds (67). As preliminary evidence for temporal stability, the current measurement intervals (40 days to 3 months) provide a foundation for subsequent invariance studies, though future research should systematically vary retest durations. Further validation across broader age cohorts would strengthen invariance evidence.
4.4 Test–retest reliability
The temporal stability of the scale was assessed using a two-month test–retest interval in a subsample of 202 participants. The resulting ICCs indicate a moderate level of reliability. While these values are more modest than the excellent stability reported for established measures like the PID-5 over both short and extended periods (87), they fall within the acceptable range for the initial validation of a novel personality instrument. It may be attributable to our longer retest interval than the typical one-week interval used in many high-reliability benchmarks, which allows for greater natural fluctuation, and the potential state-sensitivity of the constructs measured.
4.5 Construct validity
The weak-to-moderate positive intercorrelations among PERM-SF factors, alongside similar associations between all factors and SCL-90 PSI/total scores, collectively indicate adequate discriminant validity and sensitivity to pathological personality severity, as evidenced through interpersonal dysfunction and psychological distress markers of SCL-90. No significant association was observed between the PERM-SF Borderline Pattern and Anankastia factors. Notably, the Borderline Pattern is characterized by core traits of high disinhibition and negative affectivity (24). First, Borderline Pattern and Anankastia map onto orthogonal dimensions within the big-five traits, specifically, high Neuroticism with low Conscientiousness versus high Conscientiousness (24, 81). This structural independence has been replicated in international samples (88). Second, within Chinese cultural contexts, this distinction may be further amplified by cultural norms that promote control-oriented (Anankastic) coping strategies while suppressing disinhibited emotional expression (associated with the Borderline Pattern) (82–84). In general, the PERM-SF demonstrates acceptable construct validity.
A key finding of this study is the established discriminant validity among the PERM-SF factors. Although some factors were moderately to highly correlated—reflecting shared variance within the personality pathology spectrum—the HTMT supported their statistical distinctiveness. For example, despite a substantive correlation between Dissociality and Disinhibition-Negative Affectivity, their distinction met modern psychometric standards for discriminant validity (89). These results indicate that the PERM-SF effectively captures multifaceted yet discrete aspects of personality pathology in Chinese college students.
4.6 Limitations
Several limitations warrant consideration when interpreting the findings of this study. First, while initial validation focused on college students, a population demonstrating non-negligible personality disorder prevalence (48, 49) and frequent personality-related functional impairment (47), generalizability requires verification across clinical samples, diverse age cohorts (e.g., adolescents, older adults), and varied cultural contexts. This necessity is underscored by documented cross-cultural variability in personality disorder manifestation (9). Second, to reduce participant burden, we did not administer the classical personality disorder measures that support the DSM-5-AMPD or the ICD-11 criteria, such as the PID-5 (18). This constraint limited comprehensive evaluation of convergent and discriminant validity. Third, although the present study allowed for anonymous completion and the PERM questionnaire had a separate Lie factor for screening to improve the validity of the results, the possibility of subject reporting bias could not be ruled out, as the questioning mainly involved negative descriptions of personality. Fourth, the test–retest reliability warrants further investigation with larger samples and varying retest durations. Future validation should therefore incorporate multi-method assessments, particularly observer-rated measures of personality pathology dimensions and severity in broader and more diverse samples.
5 Conclusion
In this study, we developed the PERM-SF and established its substantial alignment with the core dimensions of personality disorders outlined in the latest ICD-11. Its measurement properties, including structural validity, internal consistency, longitudinal measurement invariance, and construct validity, were successfully validated within a sample of Chinese college students. The significantly abbreviated item count of this short form renders it particularly well-suited for the efficient screening of pathological personality traits. Further validation, however, is warranted in clinical populations and broader community samples. The application of the PERM-SF holds considerable promise that it could facilitate the early detection and effective treatment of PD while simultaneously offering new avenues for research and intervention into common mental illnesses and serious psychosocial problems (e.g., suicide and self-harm), optimizing the distribution of finite public health resources.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Hangzhou Normal University Affiliated Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YZ: Validation, Writing – original draft, Writing – review & editing. JH: Formal Analysis, Validation, Visualization, Writing – review & editing. YC: Resources, Validation, Writing – review & editing. JX: Formal Analysis, Validation, Writing – review & editing. RM: Formal Analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – review & editing. BZ: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Resources, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Bingren Zhang was supported by grants from the National Natural Science Foundation of China (No. 82101595) and Scientific Research Fund of Zhejiang Provincial Education Department (No. Y202558066). Three undergraduate students (Yihua Zhang, Jing Huang, and Yangjie Chen) were supported by the Starlight Program of Hangzhou Normal University.
Acknowledgments
We are grateful to Prof. Gordon Parker and Prof. Wei Wang for their previous work that inspired this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Pervin, LA. Personality: Theory, assessment, and research. New York, NY: John Wiley & Sons, Inc (2001).
2. Tyrer, P, Reed, GM, and Crawford, MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. (2015) 385:717–26. doi: 10.1016/S0140-6736(14)61995-4
3. Winsper, C, Bilgin, A, Thompson, A, Marwaha, S, Chanen, AM, Singh, SP, et al. The prevalence of personality disorders in the community: a global systematic review and meta-analysis. Br J Psychiatry. (2020) 216:69–78. doi: 10.1192/bjp.2019.166
4. de Bernier, GL, Kim, YR, and Sen, P. A systematic review of the global prevalence of personality disorders in adult Asian populations. Personal Ment Health. (2014) 8:264–75. doi: 10.1002/pmh.1270
5. Volkert, J, Gablonski, TC, and Rabung, S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. Br J Psychiatry. (2018) 213:709–15. doi: 10.1192/bjp.2018.202
7. Samuels, J. Personality disorders: epidemiology and public health issues. Int Rev Psychiatry. (2011) 23:223–33. doi: 10.3109/09540261.2011.588200
8. Hyler, SE. Personality diagnostic Questionnaire-5 (PDQ-5). New York: New York State Psychiatric Institute (2016).
9. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edition. DSM-5. Arlington, VA: American Psychiatric Association (2013).
10. Balsis, S, Segal, DL, and Donahue, C. Revising the personality disorder diagnostic criteria for the diagnostic and statistical manual of mental disorders-fifth edition (DSM-V): consider the later life context. Am J Orthopsychiatry. (2009) 79:452–60. doi: 10.1037/a0016508
11. Khan, SH, Pucker, HE, Temes, CM, and Zanarini, MC. The relationship between religion and health-related behaviours in patients with borderline personality disorder. Mental Health Religion Cult. (2019) 22:416–22. doi: 10.1080/13674676.2019.1625036
12. Pribram, ED. A cultural approach to emotional disorders: Psychological and aesthetic interpretations. New York: Routledge (2016).
13. Calliess, IT, Machleidt, W, and Ziegenbein, M. Personality disorders in a cross-cultural perspective. Eur Psychiatry. (2007) 22:S177–7. doi: 10.1016/j.eurpsy.2007.01.580
14. Baker, J, and Beazley, PI. Judging personality disorder: a systematic review of clinician attitudes and responses to borderline personality disorder. J Psychiatr Pract. (2022) 28:275–93. doi: 10.1097/PRA.0000000000000642
15. Schmeck, K. Debate: should CAMHs professionals be diagnosing personality disorder in adolescents–‘no rationale to deprive adolescents of effective treatment’. Child Adolesc Mental Health. (2022) 27:192–3. doi: 10.1111/camh.12553
16. Euler, S, Stalujanis, E, and Spitzer, C. Aktueller Stand der Psychotherapie von Persönlichkeitsstörungen. Z Psychiatr Psychol Psychother. (2018) 66:95–105. doi: 10.1024/1661-4747/a000345
17. World Health Organization (2019). International classification of diseases 11th revision. Available online at: https://www.who.int/classifications/icd/en/ (Accessed April 14, 2024).
18. Krueger, RF, Derringer, J, Markon, KE, Watson, D, and Skodol, AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol Med. (2012) 42:1879–90. doi: 10.1017/S0033291711002674
19. Reed, GM, First, MB, Kogan, CS, Hyman, SE, Gureje, O, Gaebel, W, et al. Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders. World Psychiatry. (2019) 18:3–19. doi: 10.1002/wps.20611
20. Oltmanns, JR, and Widiger, TA. A self-report measure for the ICD-11 dimensional trait model proposal: the personality inventory for ICD-11. Psychol Assess. (2018) 30:154–69. doi: 10.1037/pas0000459
21. Oltmanns, JR, and Widiger, TA. The five-factor personality inventory for ICD-11: a facet-level assessment of the ICD-11 trait model. Psychol Assess. (2020) 32:60–71. doi: 10.1037/pas0000763
22. Oltmanns, JR, and Widiger, TA. The self-and informant-personality inventories for ICD-11: agreement, structure, and relations with health, social, and satisfaction variables in older adults. Psychol Assess. (2021) 33:300–10. doi: 10.1037/pas0000982
23. Kim, YR, Tyrer, P, and Hwang, ST. Personality assessment questionnaire for ICD-11 personality trait domains: development and testing. Personal Ment Health. (2021) 15:58–71. doi: 10.1002/pmh.1493
24. Pan, B, and Wang, W. Practical implications of ICD-11 personality disorder classifications. BMC Psychiatry. (2024) 24:191. doi: 10.1186/s12888-024-05640-3
25. Fang, S, Ouyang, Z, Zhang, P, He, J, Fan, L, Luo, X, et al. Personality inventory for DSM-5 in China: evaluation of DSM-5 and ICD-11 trait structure and continuity with personality disorder types. Front Psych. (2021) 12:635214. doi: 10.3389/fpsyt.2021.635214
26. Markon, KE, Quilty, LC, Bagby, RM, and Krueger, RF. The development and psychometric properties of an informant-report form of the personality inventory for DSM-5 (PID-5). Assessment. (2013) 20:370–83. doi: 10.1177/1073191113486513
27. Maples, JL, Carter, NT, Few, LR, Crego, C, Gore, WL, Samuel, DB, et al. Testing whether the DSM-5 personality disorder trait model can be measured with a reduced set of items: an item response theory investigation of the personality inventory for DSM-5. Psychol Assess. (2015) 27:1195–210. doi: 10.1037/pas0000120
28. Zatti, C, Oliveira, SESD, Guimarães, LSP, Calegaro, VC, Benetti, SPDC, Serralta, FB, et al. Translation and cultural adaptation of the DSM-5 personality inventory–brief form (PID-5-BF). Trends Psychiatry Psychother. (2020) 42:291–301. doi: 10.1590/2237-6089-2019-0073
29. Anderson, JL, Sellbom, M, and Salekin, RT. Utility of the personality inventory for DSM-5–brief form (PID-5-BF) in the measurement of maladaptive personality and psychopathology. Assessment. (2018) 25:596–607. doi: 10.1177/1073191116676889
30. Combaluzier, S, Gouvernet, B, Menant, F, and Rezrazi, A. Validation d’une version française de la forme brève de l’inventaire des troubles de la personnalité pour le DSM-5 (PID-5 BF) de Krueger. L'Encéphale. (2018) 44:9–13. doi: 10.1016/j.encep.2016.07.006
31. Pires, R, Sousa Ferreira, A, Guedes, D, Gonçalves, B, and Henriques-Calado, J. Estudo das propriedades psicométricas-Formas Longa, Reduzida e Breve-da Versão Portuguesa do Inventário da Personalidade para o DSM-5 (PID-5). Revista Iberoamericana de Diagnóstico y Evaluación – e Avaliação Psicológica. (2018) 47:197–212. doi: 10.21865/RIDEP47.2.14
32. Fossati, A, Somma, A, Borroni, S, Markon, KE, and Krueger, RF. The personality inventory for DSM-5 brief form: evidence for reliability and construct validity in a sample of community-dwelling Italian adolescents. Assessment. (2017) 24:615–31. doi: 10.1177/1073191115621793
33. Hu, C, Hu, J, Lai, J, Yu, Y, Huang, M, Li, S, et al. The reliability and validity of the Chinese version of PID-5 brief form and its preliminary application in the Chinese population. Zhejiang Med. (2020) 42:2037–41. doi: 10.12056/j.issn.1006-2785.2020.42.19.2019-1822
34. García, LF, Aluja, A, Urieta, P, and Gutierrez, F. High convergent validity among the five-factor model, PID-5-SF, and PiCD. Personal Disord Theory Res Treat. (2022) 13:119–32. doi: 10.1037/per0000486
35. See, AY, Klimstra, TA, Cramer, AO, and Denissen, JJ. The network structure of personality pathology in adolescence with the 100-item personality inventory for DSM-5 short-form (PID-5-SF). Front Psychol. (2020) 11:823. doi: 10.3389/fpsyg.2020.00823
36. Somma, A, Krueger, RF, Markon, KE, Borroni, S, and Fossati, A. Item response theory analyses, factor structure, and external correlates of the Italian translation of the personality inventory for DSM-5 short form in community-dwelling adults and clinical adults. Assessment. (2019) 26:839–52. doi: 10.1177/1073191118781006
37. Thimm, JC, Jordan, S, and Bach, B. The personality inventory for DSM-5 short form (PID-5-SF): psychometric properties and association with big five traits and pathological beliefs in a Norwegian population. BMC Psychol. (2016) 4:1–11. doi: 10.1186/s40359-016-0169-5
38. Parker, G, and Hadzi-Pavlovic, D. A question of style: refining the dimensions of personality disorder style. J Personal Disord. (2001) 15:300–18. doi: 10.1521/pedi.15.4.300.19186
39. Wang, W, Hu, L, Mu, L, Chen, D, Song, Q, Zhou, M, et al. Functioning styles of personality disorders and five-factor normal personality traits: a correlation study in Chinese students. BMC Psychiatry. (2003) 3:11. doi: 10.1186/1471-244X-3-11
40. Fan, H, Wang, C, Shao, X, Jia, Y, Aluja, A, and Wang, W. Short form of the Zuckerman–Kuhlman–Aluja personality questionnaire: its trait and facet relationships with personality disorder functioning styles in Chinese general and clinical samples. Psychiatry Res. (2019) 271:438–45. doi: 10.1016/j.psychres.2018.12.028
41. Fan, H, Zhu, Q, Ma, G, Shen, C, Zhang, B, and Wang, W. Predicting personality disorder functioning styles by the Chinese adjective descriptors of personality: a preliminary trial in healthy people and personality disorder patients. BMC Psychiatry. (2016) 16:1–7. doi: 10.1186/s12888-016-1017-0
42. Duan, H, Gong, M, Zhang, Q, Huang, X, and Wan, B. Research on sleep status, body mass index, anxiety and depression of college students during the post-pandemic era in Wuhan, China. J Affect Disord. (2022) 301:189–92. doi: 10.1016/j.jad.2022.01.015
43. Wu, X, Tao, S, Zhang, Y, Li, S, Ma, L, Yu, Y, et al. Geographic distribution of mental health problems among Chinese college students during the COVID-19 pandemic: nationwide, web-based survey study. J Med Internet Res. (2021) 23:e23126. doi: 10.2196/23126
44. Lew, B, Kõlves, K, Osman, A, Abu Talib, M, Ibrahim, N, Siau, CS, et al. Suicidality among Chinese college students: a cross-sectional study across seven provinces. PLoS One. (2020) 15:e0237329. doi: 10.1371/journal.pone.0237329
45. Jin, X, Zhang, K, Twayigira, M, Gao, X, Xu, H, Huang, C, et al. Cyberbullying among college students in a Chinese population: prevalence and associated clinical correlates. Front Public Health. (2023) 11:1100069. doi: 10.3389/fpubh.2023.1100069
46. Duc, TQ, Chi, VTQ, Huyen, NTH, Quang, PN, Thuy, BT, and Di, KN. Growing propensity of internet addiction among Asian college students: meta-analysis of pooled prevalence from 39 studies with over 50,000 participants. Public Health. (2024) 227:250–8. doi: 10.1016/j.puhe.2023.11.040
47. Liao, Y, He, W, and Wu, ZA. Meta-analysis of the factors affecting mental health of Chinese college students. J Yangzhou Univ. (2017) 21:41–6. doi: 10.19411/j.cnki.1007-8606.2017.05.009
48. Lin, H, Huang, XT, Dou, G, Chen, YG, and Wang, XG. A cross-sectional study of Chinese college students' personality disorders. J Psychol Sci. (2008) 31:277–81. doi: 10.16719/j.cnki.1671-6981.2008.02.059
49. Ma, QG. Analysis of the current situation of personality disorders in college students and discussion of countermeasures. Ideol Theor Educ. (2016) 5:89–93. doi: 10.16075/j.cnki.cn31-1220/g4.2016.05.016
50. Ko, HC, Wu, JYW, and Lane, HY. Personality disorders in female and male college students with internet addiction. J Nerv Ment Dis. (2017) 205:740–1. doi: 10.1097/NMD.0000000000000708
51. Derogatis, LR, Lipman, RS, and Covi, L. SCL-90: an outpatient psychiatric rating scale–preliminary report. Psychopharmacol Bull. (1973) 9:13–28.
52. Yu, Y, Wan, C, Huebner, ES, Zhao, X, Zeng, W, and Shang, L. Psychometric properties of the symptom check list 90 (SCL-90) for Chinese undergraduate students. J Ment Health. (2019) 28:213–9. doi: 10.1080/09638237.2018.1521939
53. Mokkink, LB, Terwee, CB, Gibbons, E, Stratford, PW, Alonso, J, Patrick, DL, et al. Inter-rater agreement and reliability of the COSMIN (COnsensus-based standards for the selection of health status measurement instruments) checklist. BMC Med Res Methodol. (2010) 10:1–11. doi: 10.1186/1471-2288-10-82
54. Mokkink, LB, Terwee, CB, Patrick, DL, Alonso, J, Stratford, PW, Knol, DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. (2010) 63:737–45. doi: 10.1016/j.jclinepi.2010.02.006
55. Prinsen, CA, Mokkink, LB, Bouter, LM, Alonso, J, Patrick, DL, De Vet, HC, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. (2018) 27:1147–57. doi: 10.1007/s11136-018-1798-3
56. Floyd, FJ, and Widaman, KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess. (1995) 7:286–99. doi: 10.1037/1040-3590.7.3.286
57. Timmerman, ME, and Lorenzo-Seva, U. Dimensionality assessment of ordered polytomous items with parallel analysis. Psychol Methods. (2011) 16:209–20. doi: 10.1037/a0023353
58. Price, B. A first course in factor analysis. Technometrics. (1993) 35:453–3. doi: 10.1080/00401706.1993.10485363
59. Tabachnick, B. G., Fidell, L. S., and Ullman, J. B. (2013). Using multivariate statistics (6, pp. 497–516). Boston, MA: Pearson.
60. Kline, RB. Principles and practice of structural equation modeling. New York, NY: Guilford Publications (2023).
61. Satorra, A, and Bentler, PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. (2001) 66:507–14. doi: 10.1007/BF02296192
62. Hu, LT, and Bentler, PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. (1999) 6:1–55. doi: 10.1080/10705519909540118
63. Kalkbrenner, MT. Choosing between Cronbach’s coefficient alpha, McDonald’s coefficient omega, and coefficient H: confidence intervals and the advantages and drawbacks of interpretive guidelines. Meas Eval Couns Dev. (2024) 57:93–105. doi: 10.1080/07481756.2023.2283637
64. Dunn, TJ, Baguley, T, and Brunsden, V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. (2014) 105:399–412. doi: 10.1111/bjop.12046
65. Beckett, C, Eriksson, L, Johansson, E, and Wikström, C. Multivariate data analysis (MVDA) In: Pharmaceutical quality by design: A practical approach. Hoboken, NJ: John Wiley & Sons (2018). 201–25.
66. Chen, FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Modeling. (2007) 14:464–504. doi: 10.1080/10705510701301834
67. Cheung, GW, and Rensvold, RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Modeling. (2002) 9:233–55. doi: 10.1207/S15328007SEM0902_5
68. Meade, AW, Johnson, EC, and Braddy, PW. Power and sensitivity of alternative fit indices in tests of measurement invariance. J Appl Psychol. (2008) 93:568–92. doi: 10.1037/0021-9010.93.3.568
69. Cicchetti, DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. (1994) 6:284–90. doi: 10.1037/1040-3590.6.4.284
70. Hair, JF Jr, Black, WC, Babin, BJ, and Anderson, RE. Exploratory factor analysis In: Multivariate data analysis. 7th ed. Harlow, Essex: Pearson New International Edition (2014). 101–2.
72. Brown, TA. Confirmatory factor analysis for applied research. 2nd ed. New York, NY: Guilford Press (2015).
73. DeVon, HA, Block, ME, Moyle-Wright, P, Ernst, DM, Hayden, SJ, Lazzara, DJ, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. (2007) 39:155–64. doi: 10.1111/j.1547-5069.2007.00161.x
74. Karterud, S, Friis, S, Irion, T, Mehlum, L, Vaglum, P, and Vaglum, S. A SCL-90-R derived index of the severity of personality disorders. J Personal Disord. (1995) 9:112–23. doi: 10.1521/pedi.1995.9.2.112
75. Pedersen, G, and Karterud, S. Using measures from the SCL-90-R to screen for personality disorders. Personal Ment Health. (2010) 4:121–32. doi: 10.1002/pmh.122
76. Bach, B, Sellbom, M, Skjernov, M, and Simonsen, E. ICD-11 and DSM-5 personality trait domains capture categorical personality disorders: finding a common ground. Aust N Z J Psychiatry. (2018) 52:425–34. doi: 10.1177/0004867417727867
77. Hsu, L, Woody, SR, Lee, HJ, Peng, Y, Zhou, X, and Ryder, AG. Social anxiety among east Asians in North America: east Asian socialization or the challenge of acculturation? Cult Divers Ethn Minor Psychol. (2012) 18:181–91. doi: 10.1037/a0027690
78. Zentner, KE, Lee, H, Dueck, BS, and Masuda, T. Cultural and gender differences in social anxiety: the mediating role of self-construals and gender role identification. Curr Psychol. (2023) 42:21363–74. doi: 10.1007/s12144-022-03116-9
79. Kulacaoglu, F, and Izci, F. The effect of emotional dysregulation and impulsivity on suicidality in patients with bipolar disorder. Psychiatr Danub. (2022) 34:706–14. doi: 10.24869/psyd.2022.706
80. Ro, E, Vittengl, JR, Jarrett, RB, and Clark, LA. Disinhibition domain and facets uniquely predict changes in depressive symptoms and psychosocial functioning. Personal Ment Health. (2023) 17:363–76. doi: 10.1002/pmh.1585
81. Strus, W, Łakuta, P, and Cieciuch, J. Anankastia or psychoticism? Which one is better suited for the fifth trait in the pathological big five: insight from the Circumplex of personality Metatraits perspective. Front Psych. (2021) 12:648386. doi: 10.3389/fpsyt.2021.648386
82. Chang, L, Mak, MC, Li, T, Wu, BP, Chen, BB, and Lu, HJ. Cultural adaptations to environmental variability: an evolutionary account of east–west differences. Educ Psychol Rev. (2011) 23:99–129. doi: 10.1007/s10648-010-9149-0
83. Hwang, KK. Chinese relationalism: theoretical construction and methodological considerations. J Theory Soc Behav. (2000) 30:155–78. doi: 10.1111/1468-5914.00124
84. Wei, M, Su, JC, Carrera, S, Lin, SP, and Yi, F. Suppression and interpersonal harmony: a cross-cultural comparison between Chinese and European Americans. J Couns Psychol. (2013) 60:625–33. doi: 10.1037/a0033413
85. Zhang, B, Fan, H, and Wang, W. Social elite in Imperial China: their destinies as documented by the historical literature and their personality as defined by the contemporary five-factor model. Psychiatry Int. (2023) 4:35–44. doi: 10.3390/psychiatryint4010006
86. Deng, X, Sang, B, and Luan, Z. Up-and down-regulation of daily emotion: an experience sampling study of Chinese adolescents' regulatory tendency and effects. Psychol Rep. (2013) 113:552–65. doi: 10.2466/09.10.PR0.113x22z4
87. Al-Dajani, N, Gralnick, TM, and Bagby, RM. A psychometric review of the personality inventory for DSM–5 (PID–5): current status and future directions. J Pers Assess. (2016) 98:62–81. doi: 10.1080/00223891.2015.1107572
88. Gutiérrez, F, Aluja, A, Ruiz, J, García, LF, Gárriz, M, Gutiérrez-Zotes, A, et al. Personality disorders in the ICD-11: Spanish validation of the PiCD and the SASPD in a mixed community and clinical sample. Assessment. (2021) 28:759–72. doi: 10.1177/1073191120936357
89. Henseler, J, Ringle, CM, and Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. (2015) 43:115–35. doi: 10.1007/s11747-014-0403-8
Glossary
CFA - Confirmatory factor analysis
CFI - Comparative fit index
COSMIN - COnsensus-based Standards for the selection of health status Measurement Instruments
DSM-5 - Diagnostic and statistical manual of mental disorders, fifth edition
DSM-5-AMPD - DSM-5 Section III (the alternative model)
EFA - Exploratory factor analysis
GOF - Goodness of fit
HTMT - Heterotrait-Monotrait ratio
ICC - Intraclass correlation coefficient
ICD-11 - International classification of diseases-11
KMO - Kaiser-Meyer-Olkin
PD - Personality disorder
PERM - Parker personality measure
PERM-C - Chinese version of the Parker personality measure
PERM-SF - Short form of the Parker personality measure
PID-5 - Personality inventory for DSM-5
PID-5-BF - Personality inventory for DSM-5-brief form
PID-5-SF - Personality inventory for DSM-5-short form
PSI - Personality severity index
RMSEA - Root mean square error of approximation
SCL-90 - Symptom Checklist-90
SRMR - Standardized root mean square residual
TLI - Tucker-Lewis index
Keywords: Parker personality measure, college students, pathological personality, psychometric properties, cross-cultural validation
Citation: Zhang Y, Huang J, Chen Y, Xu J, Meng R and Zhang B (2025) Development and validation of the short form of the Parker personality measure among Chinese college students. Front. Public Health. 13:1685858. doi: 10.3389/fpubh.2025.1685858
Edited by:
Seetharaman Hariharan, The University of the West Indies St. Augustine, Trinidad and TobagoReviewed by:
Kay Brauer, Martin Luther University of Halle-Wittenberg, GermanyMenglin Xu, The Ohio State University, United States
Copyright © 2025 Zhang, Huang, Chen, Xu, Meng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bingren Zhang, YmluZ3JlbnpAaHpudS5lZHUuY24=; Runtang Meng, bWVuZ3J1bnRhbmdAaHpudS5lZHUuY24=
†These authors have contributed equally to this work
 Yihua Zhang1†
Yihua Zhang1† Runtang Meng
Runtang Meng Bingren Zhang
Bingren Zhang