- 1School of Chinese Medicine, Beijing University of Chinese Medicine, Beijing, China
- 2School of Traditional Chinese Medicine, Anhui University of Traditional Chinese Medicine, Hefei, China
- 3National Institute of TCM Constitution and Preventive Medicine, Beijing University of Chinese Medicine, Beijing, China
- 4School of Chinese Medicine, Nanjing University of Chinese Medicine, Nanjing, Jiangsu, China
- 5Institute of Basic Theory for Chinese Medicine, China Academy of Chinese Medical Sciences, Beijing, China
Background: Based on the Chinese Medicine constitution, this study developed a questionnaire specifically tailored for preschool children.
Methods: First, a TCM constitution scale for children aged 3–6 years was developed using face-to-face interviews, Delphi expert consultation, and Classical Test Theory (CTT). The Delphi method was conducted via email, and five CTT indicators were selected: decision value–critical ratio, dispersion trend, item–total correlation, internal consistency, and factor loading. Second, the psychometric properties of the scale were assessed, including reliability (internal consistency, test–retest reliability, and split-half reliability) and content validity. Exploratory factor analysis (EFA) was used to evaluate the structural validity of the items.
Results: The CCMQ 2.0 consisted of 47 items selected from the original 49 items of version 1.0. Exploratory factor analysis yielded a Kaiser–Meyer–Olkin (KMO) value of 0.886, and Bartlett’s test of sphericity was significant (χ2 = 5308.679, p < 0.001), indicating that the data were suitable for factor analysis. Nine common factors were extracted, accounting for a cumulative variance contribution of 52.853%. The internal consistency of the CCMQ 2.0 was high, with a Cronbach’s α of 0.924, and the test–retest reliability was satisfactory, with an intraclass correlation coefficient (ICC) of 0.86. Overall, the scale showed promising preliminary psychometric properties, although further validation is needed.
Conclusion: This study developed and preliminarily evaluated a 47-item Traditional Chinese Medicine (TCM) constitution scale for assessing the physical and mental health of children aged 3 to 6 years. The scale demonstrated good reliability and validity, providing a promising alternative tool for large-scale pediatric health assessments.
1 Introduction
The physical and mental development of children stems from parental genetic inheritance and postnatal nurturing. There is a reciprocal interaction between physical health and emotional states/personality traits. During the preschool period, characterized by social adaptation, children experience alterations in dietary patterns and social environments that differ from their previous familial contexts, potentially leading to developmental shifts in their psychosomatic constitution (1–3). It is imperative for parents to understand preschool children’s developmental status in both physical and psychological domains to facilitate predictive assessments of future growth parameters (height/weight), personality development, and disease susceptibility, thereby enabling proactive prevention of potential developmental challenges (3). Therefore, a scale that integrates four evaluation dimensions—physiological, psychological, natural, and social adaptation—and pathological tendencies is necessary for investigating the physical and mental health development of preschool children.
The constitutional theory of Traditional Chinese medicine has established a new concept of health, which proposes that health refers to the good physical and mental adaptation to the natural and social environment in the whole life cycle, which is exactly what mental and physical health needs now (4). It reflects the current and future individual health trends in four aspects, including physical differences, life processes, psychological conditions, and adaptability to natural and social environments (5). On this basis, nine kinds of BC types are developed: Balance constitution (BC), Qi-deficiency constitution (QDC), Yang-deficiency constitution (YaDC), Yin-deficiency constitution (YiDC), Phlegm-dampness constitution (PDC), Dampness-heat constitution (DHC), Blood-stasis constitution (BSC), Qi-stagnation constitution (QSC), and Special constitution (SC). Each constitution has its representative subjective reaction, objective symptoms, and personality characteristics. The constitution is formed by innate heredity and acquired knowledge. The different constitutions of individuals show some differences in response and adaptability to external stimuli in physiological states, as well as in susceptibility to certain pathogenic factors and the tendency for disease development during pathogenesis (6).
In order to differentiate body constitution, Professor Wang Qi’s research group has developed the Constitution in Chinese Medicine Questionnaire (CCMQ) to assess nine types of constitution and provide guidance on managing body and mental health for people with different constitutions. The psychometric properties of CCMQ have been confirmed (7). At the same time, health management based on constitution identification has been promoted and is well applied in China. Different versions of CCMQ for cross-cultural adaptation have also been promoted and applied in multiple countries, such as the UK and South Korea (8–10). Because the differentiation method of the scale is simple and easy, and it does not harm children, many pediatric experts and educational institutions hope that a children’s version of the CCMQ will be developed (11). However, part of the CCMQ is not applicable to children who have not yet developed secondary sexual characteristics. Therefore, Professor Wang Qi’s research group began to develop scales for different age groups (12). The scales for ages 7–14 and 0–3 have been developed, and psychometric properties have been confirmed (13, 14). Based on the previous study of the research group, the expert experience of preschool children’s physical status was paid more attention than before, and in combination with CTT, the version of the scale for children aged 3–6 years was developed to provide a simple and effective tool for constitution differentiation in early childhood.
2 Materials and methods
This study was divided into scale development and evaluation. The development of CCMQ was an iterative and collaborative process involving item generation, item refinement, item finalization, and scale validation. As a pragmatic process, the study flow is shown in Figure 1. The study was approved by the Ethics Committee of Beijing University of Chinese Medicine (2021BZYLL0102). Preliminary validation has been completed.
2.1 Scale development
To develop the items for the 3–6 years version of the TCM constitution, a research group was initially established, consisting of a core group, an expert group, and a survey group. The core group included eight TCM constitution experts, scale research experts, and principal investigators who were responsible for quality control at all stages of the process.
2.1.1 Item generation
This stage aimed to determine the scale’s dimensions and establish an item pool. The scale’s dimensions use nine constitution classification methods, a measurement system with validated psychometric properties (15). The initial draft of the scale was carefully developed by an expert group, drawing on previous research, insights from comprehensive literature reviews and parent interviews, and clinical experience. This also marks the first step in our modified Delphi method. The following is an introduction to each step of our article.
Given the underdeveloped literacy and verbal expression skills of preschool children, parental input should serve as a crucial reference for optimizing item wording in childhood assessment scales. Although a questionnaire for children aged 1–6 years was previously developed, two primary limitations were identified in this version: an excessive number of items and ambiguities in item wording. This existing scale was therefore used as the foundation for conducting parental interviews in the current study. Through face-to-face interviews with 20 parents using the preliminary scale, we systematically compiled and analyzed the findings to formulate reference recommendations, which were subsequently submitted to expert reviewers.
In the literature review, search strategies incorporating keywords such as “preschool,” “children,” “3–6,” “child,” “scales,” “TCM constitution,” and “constitution” were employed across medical literature databases, including CNKI, Wanfang, VIP, PubMed, and Web of Science. The literature search was conducted up to December 2021. Studies were screened and categorized into three thematic categories: (1) theory exploration of children’s constitution, (2) application exploration of constitution scales based on diverse classification methods in children, and (3) relationships between children’s constitution and associated diseases. During this phase, our analysis revealed significant associations between constitution and several age-specific recurrent diseases or single symptoms (such as dental caries, nocturnal enuresis, and rickets). These constitution-related symptoms were subsequently incorporated into the item pool for scale development.
The integration of literature review and interview findings with structured expert discussions serves as an effective preparatory measure to streamline the Delphi expert consultation process (16). Recognizing the inherent disciplinary boundaries of experts from diverse fields, parental feedback, and synthesized literature data were systematically organized and presented as contextual reference materials during expert deliberations. Ultimately, through structured expert brainstorming sessions, we developed an item pool comprising 51 items (as shown in Column 2 of Table 1), with no further elaboration on individual results provided separately.
2.1.2 Qualitative item screening
This phase employed a Delphi expert survey to further screen and refine scale items using both qualitative and quantitative approaches.
2.1.2.1 Participants
A total of 21 experts were invited from a pre-established expert database and met the following inclusion criteria: 1. holding a bachelor’s degree or higher, with ≥10 years of research experience in their discipline and mid-level or higher professional titles; 2. demonstrated expertise or research background in TCM constitutional theory; 3. the experts’ primary workplace locations were equitably distributed across different administrative regions; 4. high engagement, willingness, and availability to complete two rounds of Delphi consultations; and 5. enough pediatric specialists who can cover comprehensive clinical domains.
Demographic characteristics of the experts are summarized in Table 2. To address the unique demands of pediatric practice, the selection prioritized clinicians with extensive pediatric experience and multidisciplinary expertise, thereby ensuring the authority of the expert panel.
2.1.2.2 Consultation process and statistical analysis
The Delphi expert consultations were conducted via email. The questionnaire solicited expert opinions on key methodological components, including dimensional classification, item scoring methodology, and the temporal design of the scale. Each domain encompassed distinct functional aspects and hierarchical levels, with all items evaluated using a 5-point Likert scale. These were all recognized by the experts in Round 1.
2.1.2.2.1 Computational methodology
Quantitative indices of importance and rationality were operationalized through the following metrics: mean scores, full-score ratio, coefficient of variation (CV), and Kendall’s W coefficient. The core group applied predetermined thresholds for item selection and refinement: a mean score of > 3.50 (moderate-critical threshold), a full-score ratio of > 0.20 (substantial agreement criterion), and a CV of ≤ 0.25 (low dispersion requirement) (17). These analytical procedures ensured methodological rigor in optimizing the scale’s psychometric properties, as detailed in Table 1.
2.1.3 Quantitative item screening
2.1.3.1 Participants and procedures
Between November and December 2022, parents or guardians (including biological parents, grandparents, or other primary caregivers) of children aged 3–6 years were recruited from Beijing, Shijiazhuang, Shandong, and Yunnan to complete an online survey. Inclusion criteria: 1. children aged 3–6 years; 2. caregivers providing long-term care with a comprehensive understanding of the child’s health status; and 3. voluntary participation with signed informed consent. Exclusion criteria: 1. non-eligible caregivers per inclusion standards; 2. families with psychiatric disorders or consciousness-related behavioral impairments; and 3. severe medical conditions precluding survey participation.
Participants were recruited through flyers distributed by universities and local schools. Informed consent was obtained and filled out by WJX (an online questionnaire survey platform). After cleaning the data to remove incomplete or duplicate responses, the final analytical sample comprised 357 participants.
2.1.3.2 Data processing and statistical analysis
Valid responses collected via the WJX platform were organized in Excel and analyzed using SPSS 28.0. By employing online questionnaires, multiple data sources, and age-stratified sampling, this study minimized the potential influence of social bias to the greatest extent possible. However, the possibility of bias cannot be completely ruled out, particularly for subjective items. The items were psychometrically evaluated through the following analytical methods: item discrimination was assessed using the high-low group comparison method (27% extreme scores method) (critical ratio [CR] via extreme score differentiation); item representativeness was determined through item-total correlation coefficients; internal consistency of both the composite scale and subscales was evaluated using Cronbach’s α coefficient; item sensitivity was measured via the coefficient of variation (CV) to quantify dispersion trends; and construct contribution was examined through factor loadings in dimensional analyses (17, 18). Items satisfying the four analytical methods were retained. The remaining items were appropriately trimmed as required for the scale construction.
2.2 Part 2: psychometric properties analysis
Following the development of the CCMQ for Children, Version 2.0, we preliminarily evaluated its psychometric properties. Participant inclusion and exclusion criteria, data collection protocols, and analytical software (SPSS 28.0) remained consistent with Section 2.1.3.1 and are therefore not reiterated.
Internal consistency was evaluated using Cronbach’s α coefficient; test–retest reliability was assessed using the intraclass correlation coefficient (ICC), and split-half reliability was evaluated via the Guttman split-half coefficient; for validity assessment, construct validity was validated through exploratory factor analysis (EFA) (15, 18).
3 Results
As described in the Methods section, the research results are presented in two parts: scale development and psychometric property analysis.
3.1 Item screening
3.1.1 Delphi method item screening
The expert consultation process involved two rounds, with both achieving a 100% valid response rate for the questionnaires. The experts’ authority coefficients were 0.86 and 0.826, respectively. The Kendall coefficient of concordance (W) for rationality was 0.24 (p = 0.00) and 0.282 (p = 0.00), while those for importance were 0.21 (p = 0.00) and 0.299 (p = 0.00). The experts demonstrated high authority and active engagement. Based on their feedback, items were revised and adjusted. After the first round of adjustments, 49 items were retained. In the second round, expert opinions showed strong convergence and coordination. Following the discussion, the number of items remained unchanged, with only minor wording modifications. The outcomes of item adjustments and retention are presented in Table 1.
3.1.2 Results of classical test theory (CTT) screening
Items meeting ≥4 analytical criteria were retained, while others were appropriately revised based on scale construction requirements: High-Low Grouping Method: All items showed statistical significance (p < 0.05). Item 16 had t = 2.523 (p = 0.013), while other items exhibited t > 3.0. Item-Total Correlation: Items 1, 4, 15, 16, 24, and 35 had corrected item-total correlations < 0.3, though all correlations were statistically significant (p < 0.05). Cronbach’s α Coefficient: Items 15 and 16 reduced the α coefficient of the Yang-deficiency constitution subscale. Deletion of items 33 (Damp-heat), 38/42 (Qi-stagnation), and 49 (Special diathesis) caused negligible α fluctuations (Δα < 0.02). Dispersion Trend: CV > 0.25 for all items, indicating items have adequate sensitivity. Factor Loadings: Item 15 loading = 0.173; Item 16 loading = 0.297 (both < 0.40 threshold). After panel review, Item 4 (“Does your child have a normal stool?”) and Item 15 (“Does your child often wet the bed?”) were removed, retaining 47 items (Table 3).
3.2 Psychometric evaluation
In this stage, 350 questionnaires were distributed, and 332 completed questionnaires were returned. The scale recovery rate was 94.85%, and the response rate reached 96.98%, indicating a high feasibility of the scale.
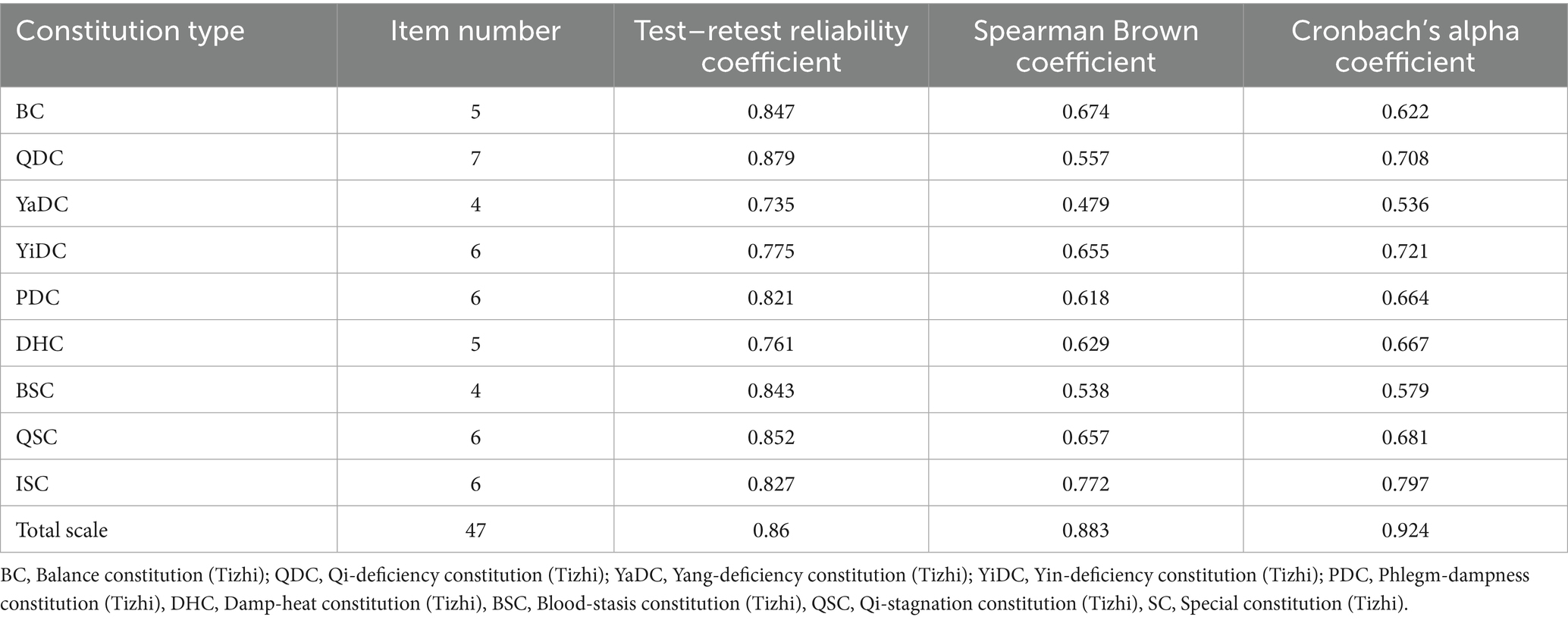
3.2.1 Internal consistency
Cronbach’s α coefficient for the full scale was 0.924, indicating good internal consistency. The Cronbach’s α coefficients for the subscales ranged from 0.536 to 0.797, suggesting acceptable reliability across all nine subscales.
3.2.2 Split-half reliability
The Spearman-Brown coefficient for the full scale was 0.883, indicating satisfactory split-half reliability. Subscale Spearman-Brown coefficients ranged from 0.479 to 0.772, reflecting moderate split-half reliability for individual subscales.
3.2.3 Test–retest reliability
The test–retest analysis included 49 participants. The intraclass correlation coefficient (ICC) for the full scale was 0.86, with ICC values for the subscales ranging from 0.735 to 0.879.
The results of Sections 3.2.1 to 3.2.3 are comprehensively presented in Table 4.
3.2.4 Content validity
The Delphi expert consultation method was employed to validate the rationality and importance of the scale items. Both the concentration and coordination of expert opinions were high. Additionally, the satisfactory test–retest reliability results obtained in later stages further supported the good content validity of the scale.
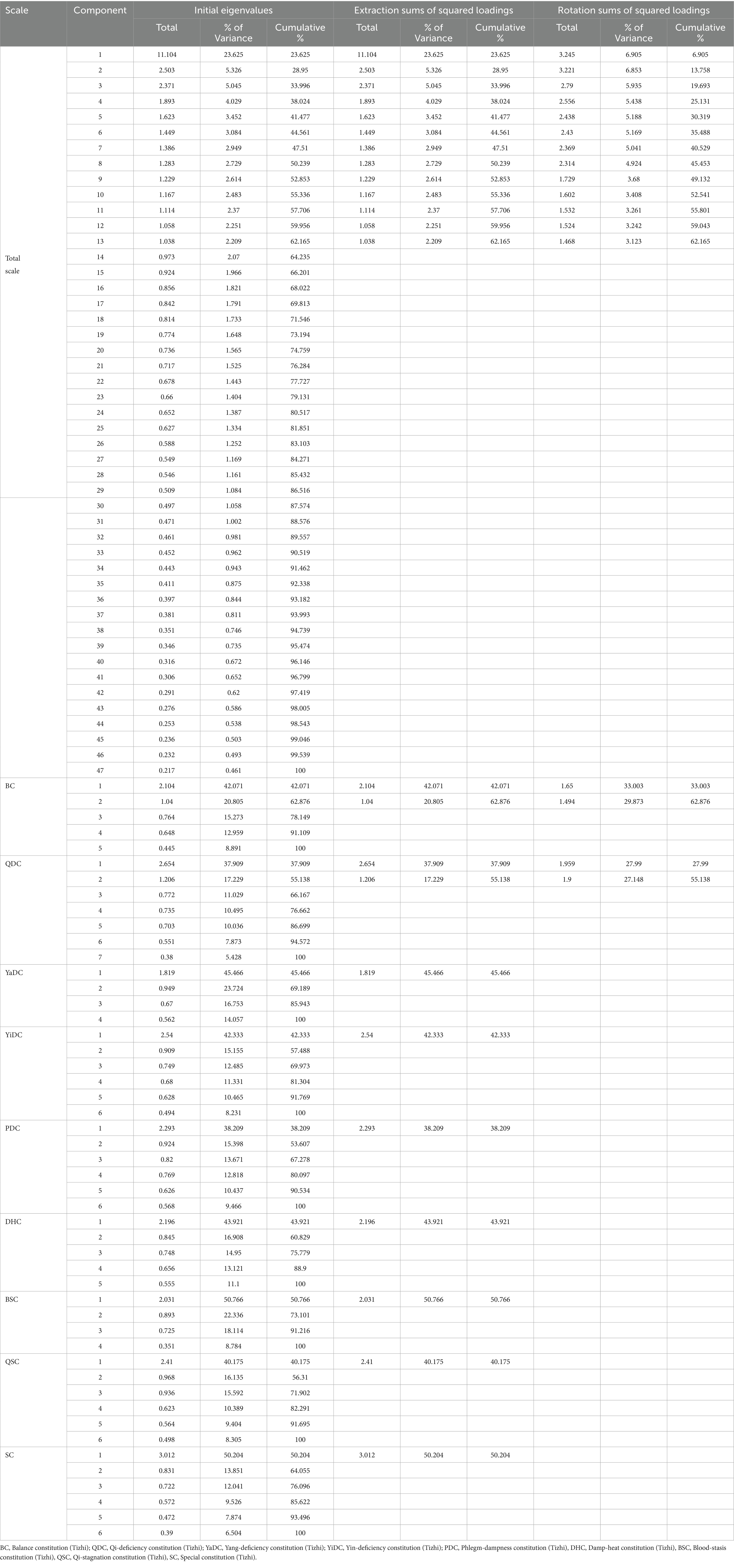
3.2.5 Construct validity
The KMO measure for the scale was 0.886, and Bartlett’s test of sphericity yielded χ2 = 5308.679 (p < 0.001), confirming the suitability for factor analysis. Under natural extraction conditions, 13 common factors were identified, accounting for 62.156% of the cumulative variance. When specifying nine factors (aligned with the subscale design), the cumulative variance explained was 52.853%, indicating adequate explanatory power for constitution-type classification. Detailed results for the full scale and subscales are provided in Table 5, while rotated factor loadings and distribution patterns are presented in Table 6.
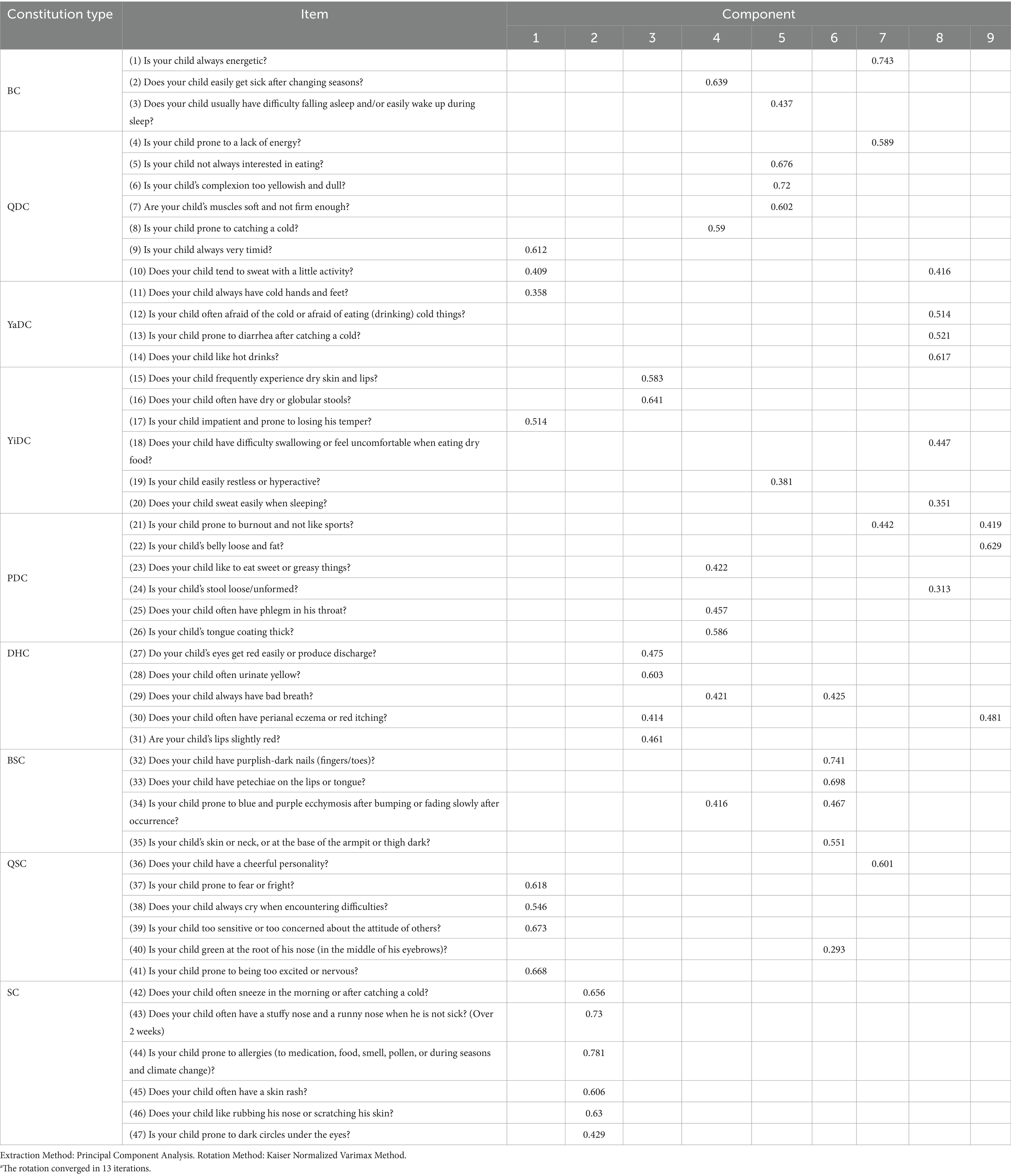
Table 6. Rotated component matrixa.
4 Discussion
The majority of existing assessment tools for preschool children primarily focus on specific domains such as cognitive development, physical growth, motor impairments, and the diagnosis of psychological disorders (19). These tools are generally designed for singular diagnostic purposes, aiming to accurately identify children with particular medical or developmental conditions. However, there has been a notable lack of comprehensive instruments that integrate both physical and mental health assessments, especially for the early detection and prevention of sub-healthy states in children. The scale developed in this study addresses this gap effectively by providing a holistic evaluation framework for preschool children’s overall well-being.
Through the aforementioned steps, this study successfully developed a scale demonstrating high feasibility, sound validity and reliability, and reasonable diagnostic utility. However, several aspects still require further exploration and discussion.
Cronbach’s α coefficient is one of the most commonly used indices for assessing the internal consistency of a scale. In general, a Cronbach’s α value above 0.80 for the total scale and above 0.60 for subscales is considered acceptable, indicating good internal reliability. Several researchers have noted that both excessive and insufficient numbers of items can influence the stability of Cronbach’s α (20). Specifically, a reduction in the number of items tends to lower the α coefficient; for scales containing only four items, the α value may sometimes fall below 0.60 or even 0.50 (21). In the second phase of this study, the YaDC and BSC subscales each consisted of four items, with Cronbach’s α coefficients of 0.536 and 0.579, respectively. Considering the limited number of items and their conceptual coherence, these values can still be regarded as acceptable, suggesting that the internal consistency of the subscales remains within a reasonable range.
Structural validity analysis indicated that the cumulative variance contribution rate of the extracted common factors reached 60% (Table 5), suggesting that the overall structural validity of the scale is acceptable. However, the validity indices of individual subscales did not reach ideal levels, primarily due to the unique diagnostic features of Traditional Chinese Medicine (TCM) syndromes—namely, the multidimensional and interrelated nature of symptom clusters. This is a very common situation in medicine, and numerous researchers have demonstrated the rational differentiation between syndromes from perspectives such as intestinal flora distribution (22). Specific item combinations could effectively distinguish between different syndrome patterns (e.g., phlegm-dampness vs. damp-heat constitutions, as shown in Table 6). Symptom overlap among syndromes led to cross-loading issues within the subscale factor structures. For example, due to the presence of “dampness” factors, both phlegm-dampness and dampness-heat types easily manifest as sticky stools. This issue has also been reported in a previous study (13, 15). Although earlier analyses, including discrete trend analysis, homogeneity testing, and item-total correlation (coefficients > 0.4), demonstrated acceptable item discriminative validity, the polysemous nature of core symptoms—often key to clinical differentiation—inevitably contributes to increased structural complexity.
In the development of questionnaires or rating scales, statistical analysis is typically regarded as a key foundation, as it directly influences the scale’s reliability, validity, and structural modeling. Structural validity is considered particularly crucial. At present, psychometric evaluation of structural validity primarily relies on confirmatory factor analysis (CFA), or a combination of exploratory factor analysis (EFA) followed by CFA. Moreover, CFA is based on hypothetical models (such as single factor, multi factor, second-order factor), requiring that the relationships between items highly conform to statistical patterns (23). However, as mentioned above, clinical symptoms are often multidimensional, intersecting, and dynamic, making it difficult to fully explain by a fixed factor model. This method often encounters model-fitting issues in the development and validation of clinical and psychological scales. Several scales that are currently considered the “gold standard” in psychiatry, such as the Hamilton Depression Scale, have encountered these problems. However, the poor CFA results did not affect the clinical efficacy (24).
Therefore, considering that the confirmatory factor analysis (CFA) conducted in this study yielded unsatisfactory model fit indices, and in view of the methodological limitations of further CFA-based exploration as well as the complexity of analyzing constitution-related items in children, exploratory factor analysis (principal component analysis) was ultimately adopted as the primary analytical approach. This method allowed for a more comprehensive examination of the underlying factor structure. The analysis revealed classification deviations in certain constitution-related items, which may be attributed to pediatric-specific factors. First, constitution-sensitive indicators validated in adult scales—such as typical symptoms of Yang deficiency—tend to be less pronounced in children. Second, several pediatric-specific items exhibited cross-loading across multiple constitution types during factor analysis, likely due to the unique physiological characteristics of children. Through expert consensus, these items were designated as auxiliary diagnostic items. In expert consultations, TCM pediatric specialists also noted that the prevalence of Yin deficiency in children is relatively low, which may explain the consistently low factor loadings for related items.
In this study, expert opinions received more attention and application. We tried to make the experts see the original items, and the set of expert references to these original situations quickly concentrated the expert advice. Under the advice of experts, we tried to do further clinical research on the items with TCM particularity or characteristics, or what experts thought was more important or meaningful, even if these items did not perform well in the statistical analysis:
A. Item 16 in Table 3—“Does your child like hot drinks?”—is rooted in the TCM pathophysiological concept of “Yang deficiency leading to internal cold.” Although experts unanimously agreed (100% agreement) that the item effectively captures the diagnostic feature of “aversion to cold and preference for warmth,” there were concerns about how clearly parents could understand and interpret this item (Kendall’s W = 0.62). After two rounds of clinical testing and iterative revision of the item’s wording, principal component analysis revealed a factor loading of 0.429. The item was significantly correlated with the total score of the Yang-deficiency subscale (r = 0.53, p < 0.01) and demonstrated acceptable internal consistency (Cronbach’s α = 0.71). These empirical findings support the theoretical validity of cold–heat differentiation in TCM. Therefore, the item was retained, with the hope that it may also be of reference value to other researchers working on pediatric constitution assessment.
B. Item 15 in Table 3 – “Does your child often wet the bed?” – was developed based on the TCM theory of “kidney yang deficiency leading to failure of bladder control.” Although supported by 76% of Delphi panel experts, factor analysis showed cross-loading across multiple constitution types: the factor loading for Yang deficiency was moderate and significant (λ = 0.549), while the loadings for Qi stagnation (λ = 0.333) and damp-heat constitution (λ = 0.357) were low. In the forced extraction of nine factors, the item even demonstrated a negative loading under the damp-heat constitution (λ = −0.382), suggesting structural inconsistency. A subgroup analysis of children aged 3–6 years with enuresis (n = 127) revealed that the most prevalent constitution types were Yin deficiency (38.6%) and Qi stagnation (29.1%), which notably differ from prior clinical findings that predominantly associate enuresis with Yang deficiency (25).
This divergence may be attributed to two key factors:
Differences in study populations: Our research was based on large-scale community screening in kindergartens, while existing clinical studies primarily sampled children who sought medical treatment. These clinical subjects may represent more severe cases of enuresis. In contrast, our sample may include children with milder symptoms, possibly already relieved by early intervention. Notably, in our factor analysis, Yang deficiency remained the only constitution type with a factor loading above the conventional threshold (λ > 0.4), suggesting some level of theoretical and structural consistency.
Influence of emotional factors: According to both modern psychological studies and Traditional Chinese Medicine (TCM) theory, emotional dysregulation can contribute to the development of enuresis. Structural equation modeling (SEM) in our study demonstrated a significant association between enuresis symptoms and scores on a pediatric anxiety scale (β = 0.41, p = 0.003), supporting the emerging concept of “emotional enuresis” (26). This finding aligns with TCM perspectives, wherein Yin deficiency often manifests as irritability, restlessness, and internal heat, while Qi stagnation is associated with introversion, emotional repression, and heightened sensitivity. In our factor analysis, enuresis showed meaningful loadings on items related to Yin deficiency, dampness, and Qi stagnation—patterns that may underlie functional or stress-induced enuresis in preschool children.
Although Item 15 passed content validation by TCM experts and retained some empirical support (i.e., its association with Yang deficiency), its overall discriminative power was relatively low (Youden index = 0.31, significantly lower than that of other items). Considering the unique characteristics of the kindergarten assessment environment—including potential parental reporting bias—the item was ultimately removed from the general pediatric scale. However, due to its theoretical value and potential clinical applicability, we recommend retaining this item in the specialized version of the scale intended for use by trained TCM practitioners in medical or hospital settings.
Although this study has not yet fully verified the model’s robustness through confirmatory factor analysis (CFA) and cross-validation, the exploratory factor analysis (EFA) results demonstrated strong theoretical and clinical alignment with the core concepts of traditional Chinese medicine (TCM) syndromes. This indicates that the extracted nine-factor model possesses good theoretical interpretability and practical potential at this stage. Due to the limitations of sample size and the exploratory nature of this research phase, further investigation into the factor structure could not be conducted. Future studies will employ larger and independent samples to perform CFA and cross-validation, thereby enhancing the verification of the stability and generalizability of the proposed nine-factor model. Such efforts will contribute to the refinement of the pediatric constitution scale and the advancement of theoretical understanding in this field.
4.1 Strengths and limitations
The development and optimization of scale items integrated expert consensus with statistical validation, taking into account multidimensional influencing factors such as children’s psychology, lifestyle habits, behavioral characteristics, and developmental status. The scale combines subjective perceptions with objective symptoms, requires a short measurement time, and is designed for completion by parents/caregivers, making it suitable for general population application.
This study has several limitations. First, it is a preliminary investigation. Participants for psychometric analysis were recruited from schools, which may limit the generalizability of the scale. Future studies should involve larger-scale and more rigorous designs. Second, this study did not include criterion validity analysis, mainly because research on traditional Chinese medicine (TCM) constitutions in children aged 3–6 years remains limited. At present, no widely recognized and validated instrument in China can serve as a “gold standard” for comparative validation. Therefore, criterion-related validity analysis could not be conducted in this study. Future research will consider using expert-based clinical judgments as a reference to compare with the scale assessment results in order to further examine and enhance the validity and practical applicability of this instrument. Third, while the original CCMQ has been translated into multiple languages and widely used globally, the cross-cultural applicability of the pediatric CCMQ requires further validation. Finally, in the preliminary analysis phase, we attempted confirmatory factor analysis (CFA), but it did not pass statistical tests. Therefore, only exploratory factor analysis (EFA) was conducted for structural validity analysis, and no adequate statistical support was obtained. As a result, while the psychometric properties of the current scale are still acceptable, there are limitations in the scale development method based on Traditional Chinese Medicine (TCM), particularly due to the long-standing structural contradictions related to the principle of syndrome differentiation in TCM. Future studies could attempt sample cross-validation based on larger-scale research while gradually improving the development and validation system for TCM-specific statistical methods. We also suggest increasing the involvement of statistical experts in this interdisciplinary research.
5 Conclusion
This study developed and evaluated a 47-item pediatric health assessment questionnaire called the Wang’s TCM Constitution Questionnaire (3–6 years). It successfully retains the original nine constitution-type structure from the CCMQ, demonstrates acceptable reliability and validity through psychometric evaluation, and can be widely applied to 3–6-year-old Chinese preschoolers. This tool provides a simple and practical questionnaire for large-scale screening of children’s TCM constitutions, supporting primary healthcare and health management.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author. Requests to access these datasets should be directed to bGl3ZW5sZTE5OTJAcXEuY29t.
Ethics statement
The studies involving humans were approved by the authors confirm that all procedures contributing to this work were approved by the Ethics Committee of Beijing University of Chinese Medicine (Approval No. 2021BZHYLL0102). The guardians of the participants provided written informed consent to participate in this study. The studies were conducted in accordance with the local legislation and institutional requirements.
Author contributions
WL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SD: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. ZL: Conceptualization, Formal analysis, Methodology, Software, Writing – review & editing. SC: Conceptualization, Data curation, Methodology, Project administration, Validation, Writing – review & editing. YC: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing. M-hB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. J-XC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. JW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work is supported by the National Key R&D Program of China (2024YFC3506300, 2024YFC3506301) High level Key Discipline of National Administration of Traditional Chinese Medicine - Traditional Chinese constitutional medicine (No. zyyzdxk-2023251). This study did not receive any specific funding from public, commercial, or non-profit funding agencies. All authors reported no financial relationship with commercial interests.
Acknowledgments
We would like to express our gratitude to all researchers, institutions, and participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TCM, Traditional Chinese Medicine; CCMQ, Constitution in Chinese Medicine Questionnaire; BC, Balance constitution; QDC, Qi-deficiency constitution; YaDC, Yang-deficiency constitution; YiDC, Yin-deficiency constitution; PDC, Phlegm-dampness constitution; DHC, Damp-heat constitution; BSC, Blood-stasis constitution; QSC, Qi-stagnation constitution; SC, Special constitution; CTT, Classical test theory; EFA, Exploratory factor analysis; CFA, Confirmatory Factor Analysis; KMO, Kaiser–Meyer–Olkin.
References
1. Loveday, S, White, N, Constable, L, Gates, A, Sanci, L, Goldfeld, S, et al. Lessons learned from the implementation of an integrated health and social care child and family hub - a case study. Int J Integr Care. (2024) 24:9. doi: 10.5334/ijic.8631
2. Ortega, FB, Ruiz, JR, Castillo, MJ, and Sjöström, M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes. (2008) 32:1–11. doi: 10.1038/sj.ijo.0803774
3. Haav, A, Oja, L, and Piksööt, J. The influence of kindergarten environment on the development of preschool children’s physical fitness. Int J Environ Res Public Health. (2024) 21:761. doi: 10.3390/ijerph21060761
4. Wang, J, Yu, RX, and Wang, Q. New concept of health with perspective of Chinese medicine. Chin J Integr Med. (2019) 25:712–5. doi: 10.1007/s11655-016-2671-2
5. Wang, J, Wang, T, Shuai, LY, Fei, ZY, Ru, LL, and Wang, Q. Research on constitution of Chinese medicine and implementation of translational medicine. Chin J Integr Med. (2015) 21:389–93. doi: 10.1007/s11655-014-2019-8
7. Sun, W, Bai, M, Wang, J, Wang, B, Liu, Y, Wang, Q, et al. Machine learning-assisted rapid determination for traditional Chinese medicine constitution. Chin Med. (2024) 19:127. doi: 10.1186/s13020-024-00992-0
8. Jing, H. The development of constitution questionnaire of Chinese medicine in English edition and the epidemiological investigation of TCM constitution in American and Canadian population. Beijing: Beijing University of Chinese Medicine (2012).
9. Li, B, Cao, H, Tian, E, and Wang, Q. A cross-sectional study of a Korean population using the standardized constitution in Chinese medicine questionnaire (Korean version). J Anhui Univ Chin Med. (2015) 34:25–8. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=IPzr95zWmwThQujCAzZfGsVPXIPRBA4md26w1fJiMJUX4_IOOq476ANgpQmBjX6527kuXsd6VjUUXMJ8FO8VJ373kOfB0yzqjdah3ug3zVoahsCEG4hQn4i3Z_Q46JJstGeF95b5wKx2r65Uuj8ldLtM63ObQy7zygKciHdYRCpFTlDjBa6wc9MiU8sNWEu-&uniplatform=NZKPT&language=CHS
10. Lai, Y. Network survey research and result analysis of body constitution of TCM among overseas population. Beijing: Beijing University of Chinese Medicine (2014).
11. Li, Y. Research progress of children’s constitution of traditional Chinese medicine. China Modern Dist Educ Tradit Chin Med. (2024) 22:165–8. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=IPzr95zWmwT3PcG7EqW-ktbkuz8T-VpziVFw9AprcjJ8s5_XUN7aYQ1YRRnxa20-SBA5ipGsGmssUZZ_hjKEaD6itwH73SgI-Fu1QbEbQl9TIR6qHcbu9yh0oSpoDqatW0Uv30uVAGIRtnDHvLCvhkl31DVwLuWgOVguq0q9s0DKJL0nq14fDKro3Pql2S4z&uniplatform=NZKPT&language=CHS
12. Cao, H, Chen, X, Song, Y, Li, SX, Ma, H, Zhang, G, et al. A comprehensive study of psychological well-being and traditional Chinese medicine constitutions among model workers in Beijing. Front Psych. (2024) 15:1425757. doi: 10.3389/fpsyt.2024.1425757
13. Li, Z. Development and evaluation of Wang’s nine TCM constitution questionnaire (0–3 version). Beijing: Beijing University of Chinese Medicine (2021).
14. Yang, Y. Development of TCM constitution questionnaire for children aged 7–14 years. Beijing: Beijing University of Chinese Medicine (2015).
15. Bai, M, Li, Z, Wang, HY, Ma, XL, Wang, ZL, Li, SJ, et al. Development and evaluation of short-form version of the constitution in Chinese medicine questionnaire: study a new and best brief instrument of Chinese medicine for health management. Chin Med. (2023) 18:140. doi: 10.1186/s13020-023-00844-3
16. Zeng, G. Modern epidemiological methods and applications. Beijing: Joint Publishing House of Beijing Medical University and Peking Union Medical College (1994).
17. Wang, Y. Development and evaluation of medical scales: theories, methods, and case studies. Beijing: Peking University Medical Press (2020).
18. Wu, M. Questionnaire statistical analysis practice: SPSS operation and application. Chongqing: Chongqing University Press (2010).
19. Yang, Y. Child developmental behavioral and psychological assessment scales. Beijing: People’s Medical Publishing House (2016).
21. Jiang, X, Shen, Z, Zhang, N, Liao, H, and Xu, H. Reliability and validity analysis of questionnaire. Modern Prev Med. (2010) 37:429–31. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=IPzr95zWmwSeuNt3gO60ZL7AzdDJj4uI0kYGta1DGmyP6dm8Z3ewBbXqpsSTGB4VygHmGe1Ve6vNsMGOmh22xbcBQjJK8vViKhSYVHwy67k-7SYRy1q9TAQRiqv9Q2pgNWx3618dztk2WKhESAwsH1KrI_8aLu2u1Yn7uGM-9vtvoEc8-Jk6KQiFiaJudHiC&uniplatform=NZKPT&language=CHS
22. Yuan, S, Zhang, R, Zhu, Z, Zhou, X, Zhang, H, Li, X, et al. Potential metabolic markers in the tongue coating of chronic gastritis patients for distinguishing between cold dampness pattern and damp heat pattern in traditional Chinese medicine diagnosis. J Inflamm Res. (2025) 18:9717–34. doi: 10.2147/JIR.S480405
23. Richardson, GB, Bates, DG, McLaughlin, LE, McGee, N, Tse, WWY, and Lai, MHC. Are higher-order constructs in evolutionary psychology attributable to omitted cross-loading bias? An exploratory structural equation modeling approach. Hum Nat. (2025) 36:257–80. doi: 10.1007/s12110-025-09497-7
24. Cole, JC, Motivala, SJ, Dang, J, Lucko, A, Lang, N, Levin, MJ, et al. Structural validation of the Hamilton depression rating scale. J Psychopathol Behav Assess. (2004) 26:241–54. doi: 10.1023/B:JOBA.0000045340.38371.04
25. Tao, M. Correlation between TCM syndrome types and constitution in children with enuresis and clinical study on TCM treatment. Zhejiang: Zhejiang Chinese Medical University (2014).
26. Gao, L. Clinical research progress on pediatric enuresis. Modern Med Health Res Electr J. (2023) 7:138–41. Available online at: https://kns.cnki.net/kcms2/article/abstract?v=IPzr95zWmwT2nU-jy-Rj0vDigg9XCYNySYCt2HU35TisjHz_YWbw1wL4ufUu2dQG9zooNNB-roHN7aixT1ta45gjHDmbi49KieIRSboSAADRXz39firIfBvwgQ_x_QEEAO6UqRkpPl02EcIw4NAFzgMIslT61Bxceq0OvYNZgQLJNAhJPhtSRwEg1Qve66nS&uniplatform=NZKPT&language=CHS
Keywords: constitution in Chinese medicine scale, body constitution, 3-6 year, psychometric property evaluation, diagnostic validity
Citation: Li W, Dong S, Li Z, Chen S, Cai Y, Bai M-h, Chen J-X and Wang J (2025) A scale for assessing the health of children aged 3–6 years in China: development and validation of the TCM constitution scale (3–6 years). Front. Public Health. 13:1690212. doi: 10.3389/fpubh.2025.1690212
Edited by:
Xin Li, Sichuan University, ChinaReviewed by:
Huy Khanh Tang, University of Medicine and Pharmacy at Ho Chi Minh City, VietnamGabriela Maldonado Muñiz, Universidad de Colima Facultad de Enfermeria, Mexico
Copyright © 2025 Li, Dong, Li, Chen, Cai, Bai, Chen and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming-hua Bai, MTUxMDExNjEwOTVAMTYzLmNvbQ==; Jia-Xu Chen, Y2hlbmppYXh1QGhvdG1haWwuY29t; Ji Wang, ZG9jdG9yd2FuZzIwMDlAMTI2LmNvbQ==
 Wenle Li
Wenle Li Siying Dong
Siying Dong Zhuqing Li
Zhuqing Li Shunqi Chen
Shunqi Chen Yuyang Cai
Yuyang Cai Ming-hua Bai
Ming-hua Bai Jia-Xu Chen
Jia-Xu Chen Ji Wang
Ji Wang