- 1Faculty of Health Sciences, Ludwik Rydygier Collegium Medicum in Bydgoszcz of the Nicolaus Copernicus University in Toruń, Bydgoszcz, Poland
- 2Tadeusz Borowicz Provincial Infectious Diseases Hospital in Bydgoszcz, Bydgoszcz, Poland
- 3Collegium Medicum, The Mazovian University in Płock, Płock, Poland
Background: Diabetes management strongly depends on patient adherence to treatment, which is influenced by psychological factors such as illness acceptance.
Objective: This study aimed to assess the levels of illness acceptance and medication adherence among patients with diabetes and to examine the relationship between these factors.
Methods: A cross-sectional study was conducted among 190 adult patients with type 1 or type 2 diabetes attending outpatient clinics in Poland. Patients were approached and invited to participate in the study when they attended their scheduled outpatient clinic appointments. A total of 256 patients were invited, of whom 36 declined. Out of the 220 questionnaires returned, 190 were fully completed and included in the final statistical analysis. The study was conducted between May 16, 2017, and the end of 2017. Illness acceptance was measured using the Acceptance of Illness Scale (AIS), and adherence was assessed with the Morisky Medication Adherence Scale (MMAS-8). Sociodemographic and clinical data were also collected.
Results: The mean illness acceptance score was 29.16 ± 6.53, with 53.2% of participants demonstrating a high level of acceptance. Medication adherence was moderate according to the MMAS-8 classification (6.49 ± 1.5 points). Illness acceptance was positively correlated with adherence (R = 0.29, p < 0.001). Patients who reported a preference for structured education and psychological support showed higher adherence scores, emphasizing the importance of patient-centered interventions.
Conclusion: The findings indicate that higher illness acceptance is associated with better adherence in patients with diabetes. In our sample, preferences for structured diabetes education and psychological support were linked with higher adherence scores, suggesting these patient-centered components may be particularly effective. Tailored education, brief psychological counselling, and shared decision-making should be incorporated into diabetes care to strengthen acceptance and support long-term self-management. Further studies are recommended to examine the effectiveness of acceptance-based interventions and to confirm these findings in larger and more diverse samples.
Background
Diabetes is a chronic illness that significantly impacts both individual well-being and public health. It is often referred to as a civilization-related illness due to its growing prevalence worldwide. According to the International Diabetes Federation, approximately 537 million adults globally were diagnosed with diabetes in 2021 (1), with an increasing trend observed in many countries, including Poland. In 2023, an estimated 3 million Poles were affected by diabetes, underscoring the importance of effective prevention and management strategies (2).
The development of diabetes is affected by various genetic, environmental, and lifestyle factors. Major risk factors include an unhealthy diet, low physical activity, obesity, an aging population, stress, and environmental influences (3). The rising incidence of diabetes challenges healthcare systems, as it demands long-term medical treatment and lifestyle changes to prevent complications (2).
A crucial part of managing diabetes is the patient’s acceptance of their illness. Illness acceptance involves the mental and emotional process through which a person adapts to the restrictions caused by the disease, affecting their psychological health and how well they follow treatment (4). Greater levels of illness acceptance are linked to better self-care, increased adherence to medical advice, and overall treatment success. Patients who accept their condition more are more likely to actively participate in their therapy, resulting in better disease outcomes (4–6).
Another key factor in diabetes management is medication adherence, which refers to the extent to which patients follow prescribed treatment regimens. While adherence is often used interchangeably with compliance, these terms have distinct meanings. Adherence emphasizes the patient’s active participation in their treatment plan, whereas compliance suggests passive obedience to medical instructions. In the literature, adherence is generally preferred, as it reflects a collaborative approach to disease management (6).
Illness acceptance plays a crucial role in how patients manage chronic conditions such as diabetes. Higher levels of acceptance have been associated with better adherence to treatment regimens, including medication use and lifestyle modifications. Illness acceptance is considered a constructive psychological process that enables patients to adjust to their condition and actively participate in its management.
Coordinated care understood as coherent, team-based patient management by an interdisciplinary workforce (physician, nurse, diabetes educator, pharmacist, and psychologist) integrates the principles of holistic care, which addresses the patient’s biological, psychological, and social needs. Within this framework, self-management, i.e., the patient’s capacity to live with and manage the disease, is of central importance. However, observed shifts in the epidemiology of diabetes, changes in individual patient profiles, and rapid technological advances necessitate a transition toward a more individualized model of patient collaboration. This approach aligns with contemporary strategies for combating diabetes and can be described as a coordinated care model tailored to the individual with diabetes (7).
Given the significant role of both illness acceptance and medication adherence in diabetes management, this study aims to evaluate their levels among patients with diabetes and to identify factors influencing these aspects. Understanding the relationship between acceptance and adherence can inform healthcare professionals and policymakers about the need for targeted interventions, including psychological support and educational programs to enhance diabetes care. In this study, we posit that higher illness acceptance facilitates the implementation of treatment recommendations (adherence) by enhancing motivation, emotion regulation, and collaboration with the multidisciplinary care team, as well as engagement in one’s treatment. These studies concern research on a group of patients with diabetes and align with the concept of patient collaboration, referred to as preparing the patient for self-care.
Materials and methods
Subjects
The study involved 190 individuals, including 101 female and 89 male patients with type 1 and type 2 diabetes. Patients were approached consecutively during their scheduled outpatient clinic visits. Of 256 patients invited, 36 declined. Of the 220 questionnaires returned, 190 were fully completed and included in the final analysis (completion rate: 86%; usable rate: 74%). Data were collected from May 16, 2017 to December 31, 2017.
The study was conducted among patients of the Multispecialty Healthcare Center “GRYF-MED” in Bydgoszcz and the Endocrinology and Diabetology Outpatient Clinic of the Dr. Antoni Jurasz University Hospital No. 1 in Bydgoszcz. Participation was anonymous and voluntary.
Inclusion criteria: age ≥18 years; clinical diagnosis of diabetes (type 1 or type 2); minimum diabetes duration of at least 6 months since diagnosis; current use of at least one prescribed antidiabetic medication; ability to provide informed consent.
The study utilized an original questionnaire of its own design, consisting of 24 questions regarding sociodemographic factors, medical conditions, lifestyle, and treatment methods. Patients self-assessed their health status on a scale ranging from very good to very poor.
Standardized research tools were used in the study:
• The Acceptance of Illness Scale (AIS) questionnaire by Felton et al.—Polish adaptation by Juczyński (8)—included 8 statements accompanied by a 5-point response scale: 1—I strongly agree, 2—I agree, 3—I do not know, 4—I disagree, 5—I strongly disagree. The measure of the degree of acceptance of the current health status was the sum of all points, ranging from 8 to 40 points. The scores were divided into three ranges to determine the level of acceptance, grouped as follows: 8–18—no acceptance, 19–29—moderate acceptance, and 30–40—good acceptance of the illness.
• The eight-item Morisky Medication Adherence Scale (MMAS-8) was used as a diagnostic instrument to assess the level of adherence and compliance with medical recommendations—Polish adaptation by Jankowska-Polańska et al. (9). Respondents were asked to address 8 statements regarding them medication-taking routine. The total result obtained for all statements allowed us to assess the degree of adherence to the recommended drug regimen, where a score of <6 points indicated a low level, a score of ≥6 and <8 points indicated a moderate level, and 8 points indicated a high level of adherence and compliance (9–11).
Study protocol
The study was conducted in accordance with the guidelines of the Declaration of Helsinki. The protocol received approval from the Bioethics Committee at Nicolaus Copernicus University Collegium Medicum in Bydgoszcz, Poland (consent number KB 362/2017). Each participant provided informed consent to take part in the study.
The consent for publication section is not applicable.
Statistical analysis
Statistical analysis was performed using the Statistica v. 13 software (StatSoft, TULSA, USA). Basic qualitative (nominal) data were presented as the population size (n) and percentage (%). Non-parametric tests were applied for statistical analysis. The Spearman rank correlation test was used to assess correlations. The Mann–Whitney U test was used for comparisons between two groups, and the Kruskal–Wallis test was applied for comparisons among three or more groups. Quantitative (measurable) variables were presented as mean and standard deviation (M ± SD).
A total of 256 patients were invited to participate in the study, and 36 declined. Out of the 220 questionnaires returned, 190 were fully completed and were included in the final statistical analysis.
Results
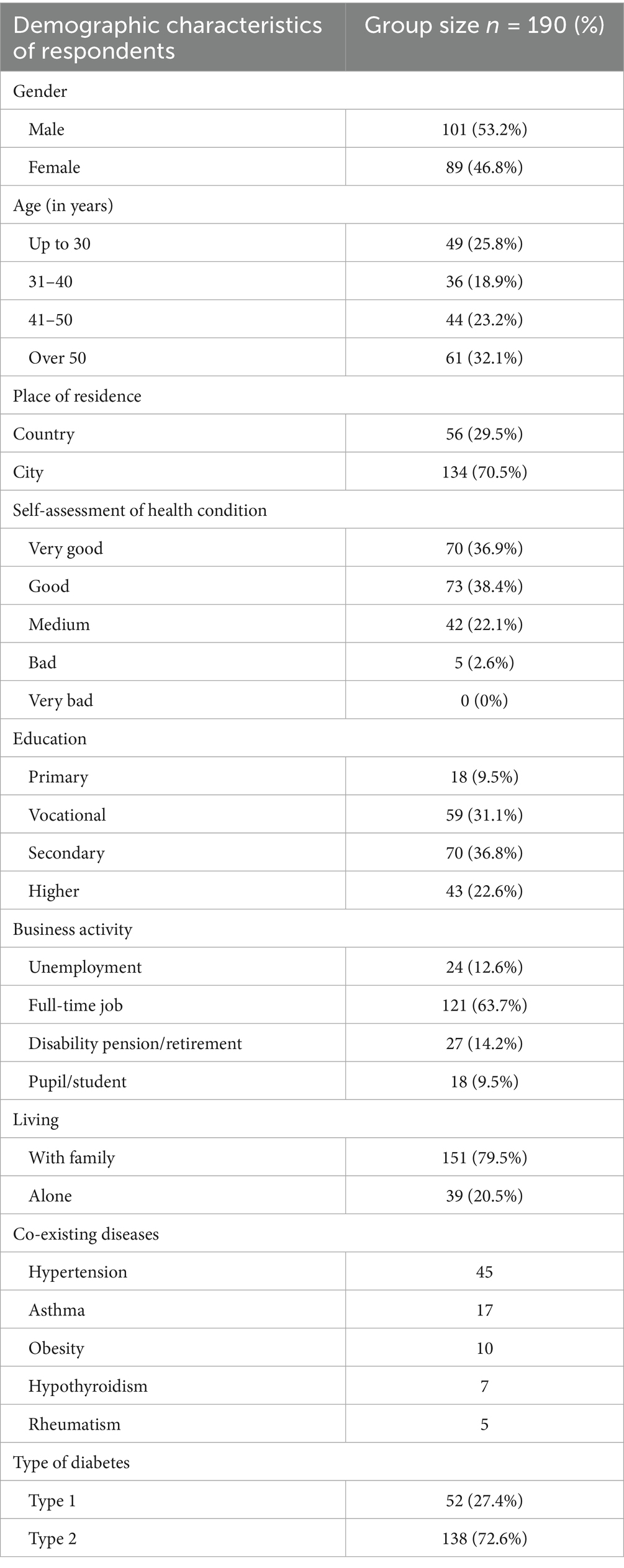
The general characteristics of the study population are presented in Table 1. The study involved 190 individuals, including 101 female and 89 male patients. The mean age of the participants was 42.2 ± 13.4 years: 41.3 years ± 13.9 for female patients, and 43.2 years ± 12.9 for male patients. The largest group of respondents had a secondary education (36.8%), while the smallest group had a primary education (9.5%). Among the respondents, 63.7% were employed. One-fifth of the patients (20.5%) lived alone. Among the study participants, 72.6% had type 2 diabetes. The mean time since the diagnosis of diabetes was 7.7 ± 5.7 years. In the study population, 87 patients (45.8%) declared the presence of coexisting diseases. When answering the question about the type of coexisting diseases, respondents were allowed to select more than one statement. Thus, a total of 122 responses were registered from 87 individuals. The most commonly reported coexisting conditions were hypertension (36.9%), followed by asthma (13.9%), obesity (8.2%), hypothyroidism (5.7%), and rheumatism (4.1%).
The average illness acceptance score among the patients was 29.16 ± 6.53 points. The study population was divided into three groups based on the degree of acceptance of their illness. The largest group consisted of individuals with a high level of illness acceptance—101 individuals (53.2%). Among the respondents, moderate acceptance of illness was reported by 75 individuals (39.5%). Fourteen individuals (7.4%) did not accept their illness.
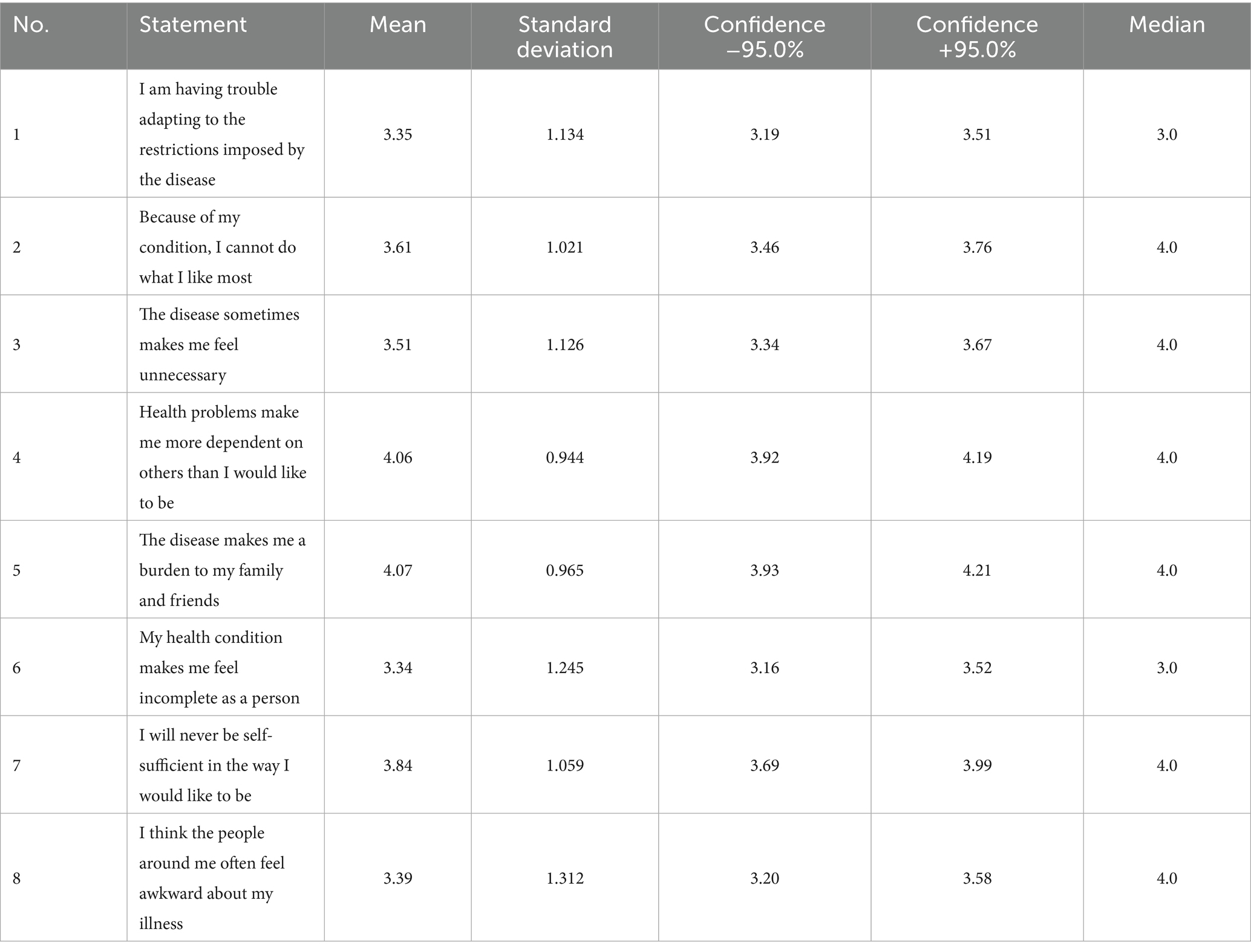
Table 2 presents the mean values for individual statements on the Acceptance of Illness Scale, ranging from 3.34 to 4.07 points. The lowest average, and thus the lowest level of illness acceptance, was obtained for the statements: “My health condition makes me feel incomplete as a person” (3.34 points) and “I am having trouble adapting to the restrictions imposed by the disease” (3.35 points). The highest average, and consequently the highest level of acceptance of illness, was scored for the statements: “The disease makes me a burden to my family and friends” (4.07 points) and “Health problems make me more dependent on others than I would like to be” (4.06 points).
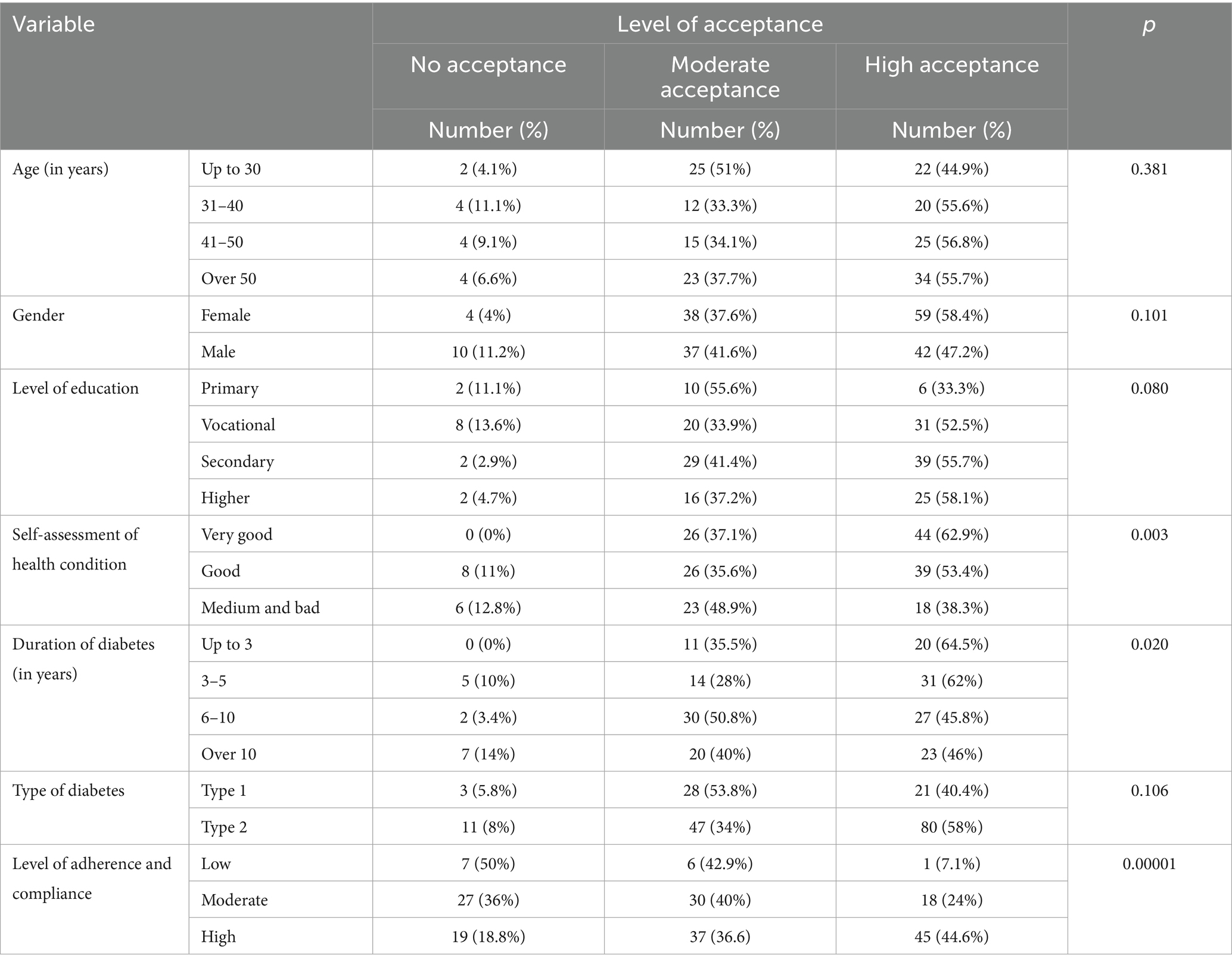
A detailed set of results on the levels of acceptance of illness in the study population is presented in Table 3. The highest average score for acceptance of illness was observed in the age group of 41–50 years, 29.75 points, and in those above 50 years of age, 29.56 points. The lowest score was observed in individuals aged up to 30 years, 28.43 points. Participants’ age, gender, education level, and type of diabetes did not show statistically significant correlations with the results of illness acceptance (p > 0.05).
When reporting the diabetes duration correlation (R = −0.168; p = 0.020), acknowledge this represents a small effect size. Statistical analysis revealed that the level of illness acceptance increased along with the self-assessment of health status (R = 0.35; p < 0.001). The highest average score for acceptance of illness was noted in individuals who rated their health as very good, 30.64 points, while the lowest was in the group who rated their health status as moderate, 27.28 points. In the study, the duration of diabetes was negatively correlated with illness acceptance (r = −0.168; p = 0.020), representing a small effect size. The highest average acceptance was observed among individuals with diabetes duration ≤3 years (30.94 points) and 3–5 years (29.7 points), and the lowest among those with duration >10 years (28.0 points). Therapeutic adherence and compliance in the study population were assessed using the MMAS-8 (Polish version). The results of illness acceptance showed a statistically significant positive correlation with the level of adherence and compliance (R = 0.29; p < 0.001), indicating a medium effect size. Consistent with this association, Table 3 shows a clear gradient: the highest mean adherence and compliance occurred in the high-acceptance group (6.88 points), whereas the lowest was observed in the low-acceptance group (5.23 points), with the medium group falling in between.
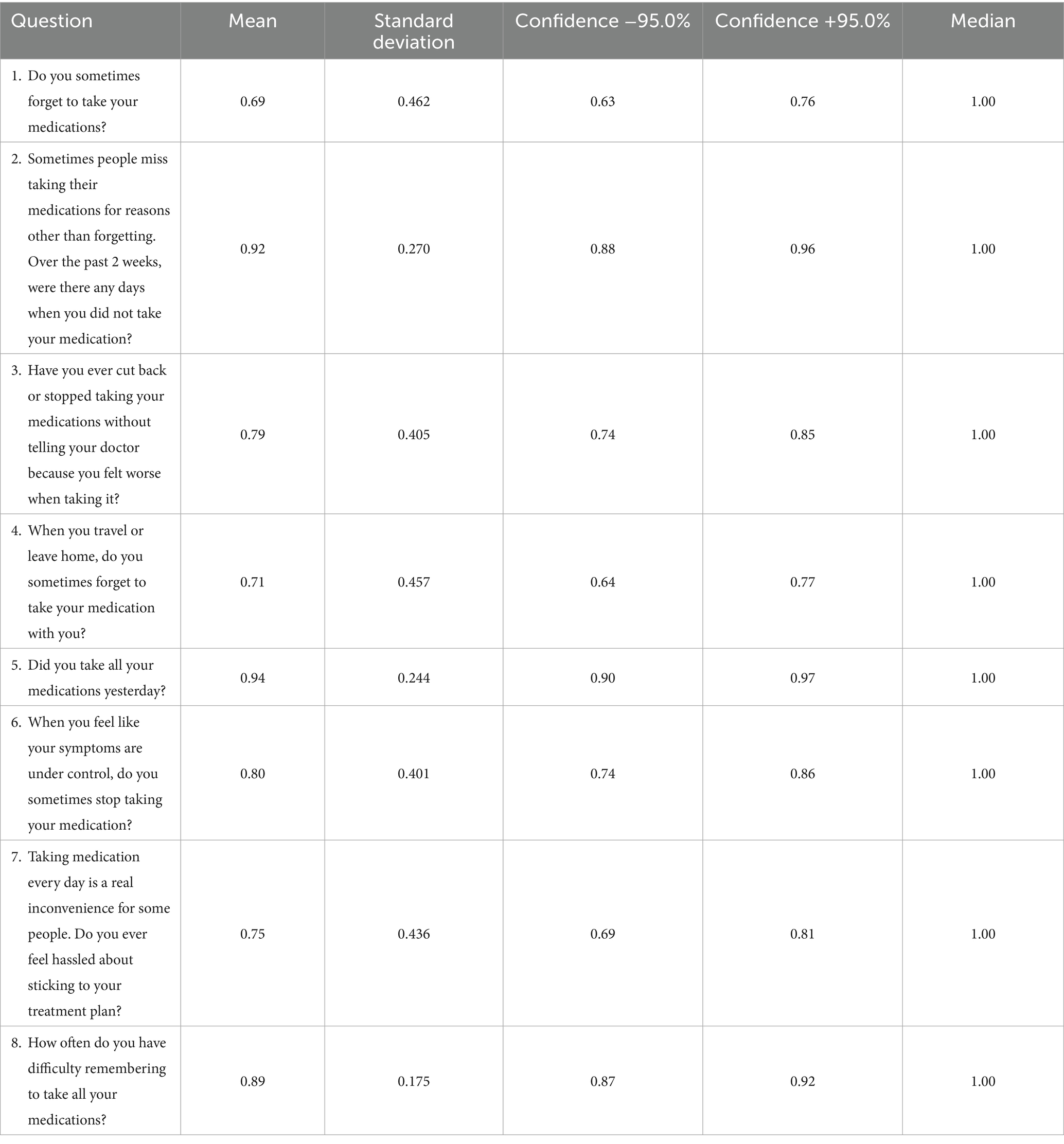
Answers to individual questions of the Morisky Medication Adherence Scale questionnaire are presented in Table 4. The mean total score was 6.49 ± 1.5, indicating a moderate level of adherence and compliance among the patients. Moderate level of adherence means that the patient generally follows medical recommendations regarding medication use, but does not always do so consistently. This level of adherence does not imply a lack of cooperation with the physician, but it may reduce the effectiveness of therapy, leading to fluctuations in blood glucose levels, poorer diabetes control, and an increased risk of complications.
Among all items assessing medication adherence, the highest average score was given to question 5: “Did you take all your medications yesterday?” (0.94 points). This was followed closely by question 2: “Sometimes people miss taking their medications for reasons other than forgetting. Over the past 2 weeks, were there any days when you did not take your medication?” (0.92 points) (Table 4 for detailed responses).
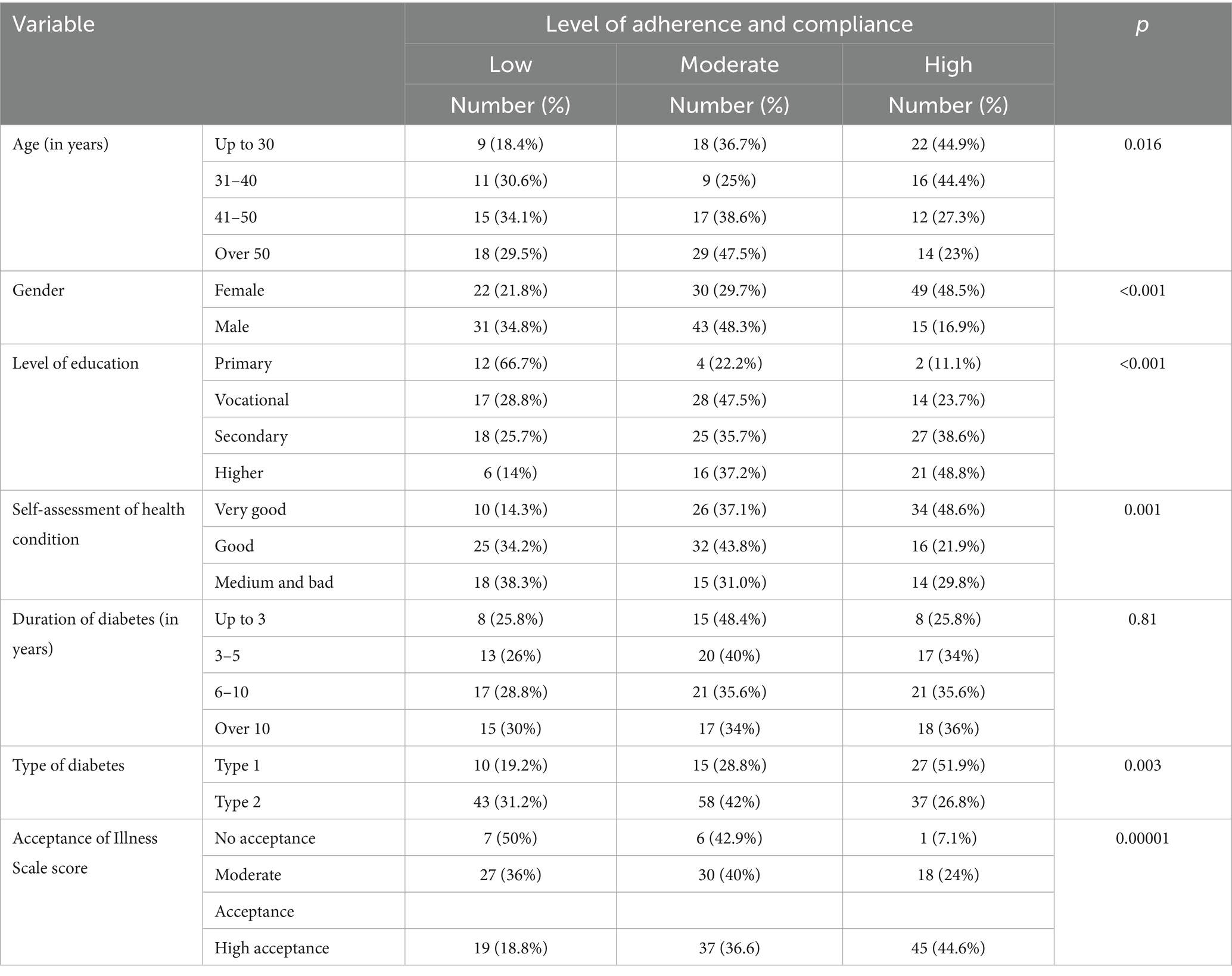
Table 5 presents the detailed results of therapeutic adherence and compliance assessed using the Morisky Medication Adherence Scale. Statistical analysis showed that with increasing age of the participants, the level of adherence and compliance decreased (R = −0.17; p = 0.016). A higher mean score for adherence and compliance was observed in the female group, as compared to males (6.85 ± 1.36 vs. 6.08 ± 1.59 points, p < 0.001). With higher levels of education of the participants and self-assessment of their health status, the level of adherence and compliance also increased (R = 0.29; p < 0.001 for both). The duration of diabetes treatment did not affect the level of adherence and compliance (p > 0.05). A higher mean score for adherence and compliance was observed in individuals with type 1 diabetes, as compared to those with type 2 (6.99 vs. 6.31 points, p = 0.003). The level of acceptance of illness influenced the level of adherence and compliance (R = 0.29; p < 0.0001).
For a patient with diabetes, it is important to monitor and control their glucose levels at home. Among those surveyed, the vast majority (76.8%) declared that they performed such monitoring. Patients most commonly measured their glucose levels once a day (33.6%), then three times a day (26.7%), and lastly twice a day (26.0%). As many as 65.8% of the respondents reported receiving assistance from family members in glucose monitoring. Monitoring glucose and blood pressure is associated with keeping a self-monitoring diary where these values are recorded. Keeping such a diary was declared by 64.7% of the patients. Among 76 patients treated with subcutaneous insulin, 76.3% indicated self-preparation and administration of injections. All patients receiving insulin through an insulin pump (39 individuals) were able to independently operate the equipment thanks to the training they had received.
Discussion
Diabetes is a chronic condition in which treatment effectiveness largely depends on active patient participation. In such a model of care, adherence and compliance are pivotal, as they determine the maintenance of recommendations in everyday practice.
The primary aim of this study was to evaluate the level of illness acceptance and adherence to therapeutic recommendations among patients with diabetes and to identify the factors influencing these aspects. Our findings demonstrate a significant positive correlation between illness acceptance and medication adherence (R = 0.29; p < 0.001), supporting previous research (12, 13). Patients with higher illness acceptance scores (mean: 6.88 points) exhibited better adherence compared to those with low acceptance (5.23 points). These findings highlight the crucial role of psychological adaptation in managing diabetes.
Cognitive function -are an important determinant of adherence to therapeutic recommendations, although cognitive decline likely did not play a major role in our relatively young study sample (14, 15). Deficits in memory, executive functions, and health literacy (reading and writing skills) are associated with poorer adherence (16–18). Patients with type 1 diabetes demonstrated higher mean adherence scores than those with type 2 diabetes (6.99 ± 1.36 vs. 6.31 ± 1.59 points, p = 0.003). This aligns with earlier findings that dependence on insulin for survival promotes greater adherence (19). At the same time, psychosocial aspects—including health beliefs, perceived severity, and self-efficacy—play a crucial role in adherence differences (20–25). According to the Health Belief Model, patients are more likely to comply when they perceive a high risk of complications and believe in treatment efficacy (23), while psychological insulin resistance (PIR) may emerge when insulin initiation is perceived as a failure, reducing adherence (26, 27).
Our study found a statistically significant negative correlation between diabetes duration and illness acceptance (R = −0.168; p = 0.020), indicating that patients with a longer disease duration had lower acceptance levels. A study of 298 Turkish patients reported a similar lack of correlation between age and illness acceptance, but higher acceptance among women, more educated patients, and those without comorbidities (12). Khazew and Faraj (28) also found no consistent sociodemographic predictors, suggesting that cultural or contextual factors may influence illness perception. Future studies should include larger and more diverse populations to explore these associations further.
Socioeconomic factors such as education, healthcare access, and financial barriers also shape adherence (29, 30). Our results confirmed the positive association between higher education and adherence (R = 0.29; p < 0.001), consistent with reports that health literacy improves treatment engagement (31). Patients with type 1 diabetes often benefit from more structured education and early training, while those with type 2 may lack adequate support, increasing the risk of non-adherence (31). Addressing these disparities through targeted education and support programs may help bridge this gap.
Future research should investigate psychosocial determinants such as health beliefs, self-efficacy, and barriers to adherence, and assess the effectiveness of tailored interventions, including cognitive-behavioral, motivational, educational, and acceptance-based approaches, in larger and more diverse populations (32). Given the rising incidence of both type 1 and type 2 diabetes, a coordinated care model is being implemented in response to system-level needs. This model directs resources toward individualized education, continuous follow-up, and psychosocial support, aligning with the patient needs identified in our findings.
Coordinated diabetes care may also enhance both acceptance and adherence. In Poland, the coordinated care model introduced in 2023 integrates physicians and nurses in continuous patient-centered care, aligning with current clinical recommendations of the Polish Diabetes Association.
Conclusion
In the present study, it was found that patients with diabetes exhibited a moderate level of adherence and compliance and a high level of acceptance of illness. Patients who accepted their diabetes tended to demonstrate better self-care and adherence to medical recommendations. Higher education of patients correlated with a greater level of acceptance of illness and better adherence to medical recommendations. Patients with type 1 diabetes showed a higher level of adherence to recommendations than those with type 2 diabetes, which may result from intensive education on insulin therapy.
Monitoring disease acceptance and adherence to treatment recommendations can be an important element of diabetes care. Periodic monitoring, especially during health and family crisis situations, would be beneficial. Coordinated diabetes care aims to minimize or delay complications, maintain a good quality of life for the patient, and reduce healthcare costs for both the patient and the healthcare system.
Practice implications
Identification of patients with diabetes who experience difficulties adhering to therapeutic recommendations allow for the development of individual treatment plans and the provision of additional education and support, and also reduces the risk of diabetes complications. Based on the findings of this study, strategies for diabetes patient care can be tailored to focus on promoting acceptance of illness and supporting self-management. Educational programs and psychosocial support initiatives can be implemented to enhance diabetes management among patients. The study results can be valuable for healthcare policymakers and administrators involved in planning the provision of healthcare services to patients with diabetes, as they indicate the need to increase access to educational programs and psychological support for these patients.
In the Polish context, the Self-Care of Diabetes Inventory (SCODI)—in its Polish adaptation—can be used to assess areas of self-care, alongside the MMAS-8 (medication adherence) and AIS (illness acceptance).
Limitations
The authors were unable to utilize glycemia and glycosylated hemoglobin values in the study because patients used various equipment for self-monitoring of glycemia. Authors were also unable to perform glycemia and glycosylated hemoglobin assays because patients attended medical appointments at different times of the day (patients were not fasted). Therefore, such test results would not be reliable.
Given the cross-sectional design, we cannot draw causal conclusions about the relationship between illness acceptance and adherence, nor determine its directionality. We did not assess the presence or severity of diabetes complications, which could influence both illness acceptance and adherence; thus, we could not adjust for potential confounding by disease burden.
Author’s note
The results of this study were presented at the International Conference on Research in Life-Sciences & Healthcare, Paris, France, 23-24 April 2021.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Bioethics Committee at Nicolaus Copernicus University Collegium Medicum in Bydgoszcz, Poland (consent number KB 362/2017). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AP: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. AM: Writing – original draft, Formal analysis, Writing – review & editing. MH: Writing – original draft, Formal analysis. EK: Data curation, Methodology, Writing – original draft. MG: Formal analysis, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. Generative AI (ChatGPT, OpenAI) was used only for language editing. All study design, data collection, analysis, and interpretation were performed exclusively by the authors.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. OECD. Health at a glance: Europe 2022. State of health in the EU cycle. Paris: OECD Publishing; (2022). Available online at: https://www.oecd-ilibrary.org/docserver/507433b0-en.pdf
2. mZdrowie.pl. Światowy Dzień Cukrzycy 2023: wczesne wykrycie, nowoczesne leczenie. (2023). Available online at: https://www.mzdrowie.pl/medycyna/swiatowy-dzien-cukrzycy-2023-wczesne-wykrycie-nowoczesne-leczenie/ (Accessed May 15, 2025).
3. Centers for Disease Control and Prevention. Diabetes risk factors. (2021). Available online at: https://www.cdc.gov/diabetes/basics/risk-factors.html (Accessed May 15, 2025).
4. Pereira, G, Bergamin, M, Granacher, U, and Ribeiro, F. Psychological adjustment to diabetes and adherence to self-care behaviors in type 2 diabetes: associations with self-compassion. J Diabetes Res. (2019) 2019:3289203. doi: 10.1155/2019/3289203
5. Rusin-Pawełek, EI, Galińska, I, Wierzba, W, Dykowska, G, Gołębiak, I, and Śliwczyński, A. The level of disease acceptance in patients with type 2 diabetes during hospitalization and selected socio-demographic and medical factors. Pielęgniarstwo w Opiece Długoterminowej. (2022) 7:5–17. doi: 10.19251/pwod/2022.1(1)
6. World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: WHO (2003).
7. Mastalerz-Migas, A. Standard postępowania w cukrzycy w POZ z uwzględnieniem opieki koordynowanej. Lek POZ. (2022) 8:395–9.
8. Juczyński, Z. Narzędzia pomiaru w promocji i psychologii zdrowia. Warszawa: Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego (2000).
9. Jankowska-Polańska, B, Uchmanowicz, I, Chudiak, A, Dudek, K, Morisky, DE, and Szymańska-Chabowska, A. Psychometric properties of the polish version of the eight-item Morisky medication adherence scale in hypertensive adults. Patient Prefer Adherence. (2016) 10:1759–66. doi: 10.2147/PPA.S101904
10. Morisky, DE, Ang, A, Krousel-Wood, M, and Ward, HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. (2008) 10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x
11. Berlowitz, DR, Foy, CG, Kazis, LE, Bolin, LP, Conroy, MB, Fitzpatrick, P, et al. Effect of intensive blood-pressure treatment on patient-reported outcomes. N Engl J Med. (2017) 377:733–44. doi: 10.1056/NEJMoa1611179
12. Dogan, DA, Ek, H, Zengi, S, Pehlivan, S, and Ersoy, C. Association between the effect of acceptance of illness and medication adherence, metabolic control, and risk of diabetic foot in individuals with diabetes. Prim Care Diabetes. (2023) 17:334–40. doi: 10.1016/j.pcd.2023.05.003
13. Bonikowska, I, Szwamel, K, and Uchmanowicz, I. Analysis of the impact of disease acceptance, demographic, and clinical variables on adherence to treatment recommendations in elderly type 2 diabetes mellitus patients. Int J Environ Res Public Health. (2021) 18:8658. doi: 10.3390/ijerph18168658
14. He, X, Wang, X, Wang, B, and Zhu, A. The association between mild cognitive impairment and medication non-adherence among elderly patients with chronic diseases. Cureus. (2023) 15:e47756. doi: 10.7759/cureus.47756
15. Park, DC, Lodi-Smith, J, Drew, L, Haber, S, Hebrank, A, Bischof, GN, et al. The impact of sustained engagement on cognitive function in older adults: the synapse project. Psychol Sci. (2014) 25:103–12. doi: 10.1177/0956797613514919
16. Sun, X, Wang, L, Shen, X, Huang, C, Wei, Z, Su, L, et al. Correlates of adherence to multimodal non-pharmacological interventions in older adults with mild cognitive impairment: a cross-sectional study. Front Psych. (2022) 13:833767. doi: 10.3389/fpsyt.2022.833767
17. Rohde, D, Merriman, NA, Doyle, F, Bennett, K, Williams, D, and Hickey, A. Does cognitive impairment impact adherence? A systematic review and meta-analysis of the association between cognitive impairment and medication non-adherence in stroke. PLoS One. (2017) 12:e0189339. doi: 10.1371/journal.pone.0189339
18. Smith, D, Lovell, J, Weller, C, Kennedy, B, Winbolt, M, Young, C, et al. A systematic review of medication adherence in older people with dementia or cognitive impairment. PLoS One. (2017) 12:e0170668. doi: 10.1371/journal.pone.0170668
19. García-Pérez, LE, Álvarez, M, Dilla, T, Gil-Guillén, V, and Orozco-Beltrán, D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. (2013) 4:175–94. doi: 10.1007/s13300-013-0034-y
20. Kirkman, MS, Rowan-Martin, MT, Levin, R, Fonseca, VA, Schmittdiel, JA, Herman, WH, et al. Determinants of adherence to diabetes medications: findings from a large pharmacy claims database. Diabetes Care. (2015) 38:604–9. doi: 10.2337/dc14-2098
21. Young-Hyman, D, de Groot, M, Hill-Briggs, F, Gonzalez, JS, Hood, K, and Peyrot, M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care. (2016) 39:2126–40. doi: 10.2337/dc16-2053
22. McSharry, J, McGowan, L, Farmer, AJ, and French, DP. Perceptions and experiences of taking oral medications for the treatment of type 2 diabetes mellitus: a systematic review and meta-synthesis of qualitative studies. Diabet Med. (2016) 33:1330–8. doi: 10.1111/dme.13128
23. Lim, S, Oh, TJ, Dawson, J, and Fritschi, C. Psychosocial interventions to improve adherence in type 2 diabetes mellitus: a systematic review. Psychosom Med. (2022) 84:500–12. doi: 10.1097/PSY.0000000000001057
24. Johnson, SB, Seidenberg, M, and Van Gorp, W. Cognitive factors in diabetes self-management. Curr Diab Rep. (2019) 19:21. doi: 10.1007/s11892-019-1209-7
25. Polonsky, WH, Fisher, L, Hessler, D, and Edelman, SV. Improving diabetes self-care through a comprehensive telemedicine-based program: evidence from the TELEDIABE study. Diabetes Care. (2015) 38:627–34. doi: 10.2337/dc14-2011
26. Grady, PA, and Gough, LL. Self-management: a comprehensive approach to the management of chronic conditions. Am J Public Health. (2014) 104:e25–31. doi: 10.2105/AJPH.2014.302041
27. Bailey, CJ, and Kodack, M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract. (2014) 68:444–52. doi: 10.1111/ijcp.12376
28. Khazew, HR, and Faraj, RK. Illness acceptance and its relationship to health behaviors among patients with type 2 diabetes: a mediating role of self-hardiness. Curr Probl Cardiol. (2024) 49:102606. doi: 10.1016/j.cpcardiol.2024.102606
29. Peyrot, M, Rubin, RR, Lauritzen, T, Skovlund, SE, Snoek, FJ, Matthews, DR, et al. Resistance to insulin therapy among patients and providers: results of the cross-national diabetes attitudes, wishes, and needs (DAWN) study. Diabetes Care. (2015) 38:2495–503. doi: 10.2337/dc15-0545
30. Walker, RJ, Smalls, BL, and Egede, LE. Social determinants of health in diabetes and cardiovascular risk. Curr Diab Rep. (2017) 17:76. doi: 10.1007/s11892-017-0900-y
31. Powers, MA, Bardsley, J, Cypress, M, Duke, S, Funnell, MM, Fischl, AH, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement. Diabetes Care. (2017) 40:1409–19. doi: 10.2337/dc17-0745
Keywords: illness acceptance, medication adherence, health psychology, type 2 diabetes, self-management, illness perception, psychological adaptation
Citation: Pluta A, Marzec A, Humańska M, Kobus E and Głowacka M (2025) Illness acceptance and medication adherence in patients with diabetes in Poland: a cross-sectional study. Front. Public Health. 13:1690434. doi: 10.3389/fpubh.2025.1690434
Edited by:
Tomoya Tachi, Nagoya City University, JapanReviewed by:
Snežana Knežević, Academy of Applied Studies Polytechnic, SerbiaAli Malik Tiryag, University of Basrah, Iraq
Copyright © 2025 Pluta, Marzec, Humańska, Kobus and Głowacka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Agnieszka Pluta, YWduaWVzemthLnBsdXRhQGNtLnVtay5wbA==
 Agnieszka Pluta
Agnieszka Pluta Alicja Marzec1
Alicja Marzec1