- Robert F Stempel College of Public Health and Social Work, Florida International University, Miami, FL, United States
Editorial on the Research Topic
Biosocial determinants and solutions of mental health conditions in low and middle-income countries
Introduction
Mental health conditions represent a significant and growing public health challenge, especially in low- and middle-income countries (LMICs). These settings are characterized by numerous factors that foster social inequities and vulnerabilities, which increase the burden of mental disorders (1) However, public mental health spending in LMICs averages only 2.1% of total health budgets (2), limiting the capacity to develop detection, prevention, and care programs to address the rapidly expanding mental health issues.
Mental health conditions often develop early in life, affect people throughout their lives, and are heavily influenced by poverty, gender inequality, and exposure to violence. Depression and anxiety are the leading contributors to the global burden of mental disorders (3). Both are usually linked to unemployment, financial struggles, food and job insecurity, poor housing conditions, exposure to violence, and discrimination (4). They are associated with long-term disability and the risk of suicide, which is a major cause of death among young people worldwide. Therefore, they pose a significant public health challenge and require a stronger health system, investment in community-based care, and efforts to address the social factors that lead to mental distress (3).
Addressing a gap in global evidence
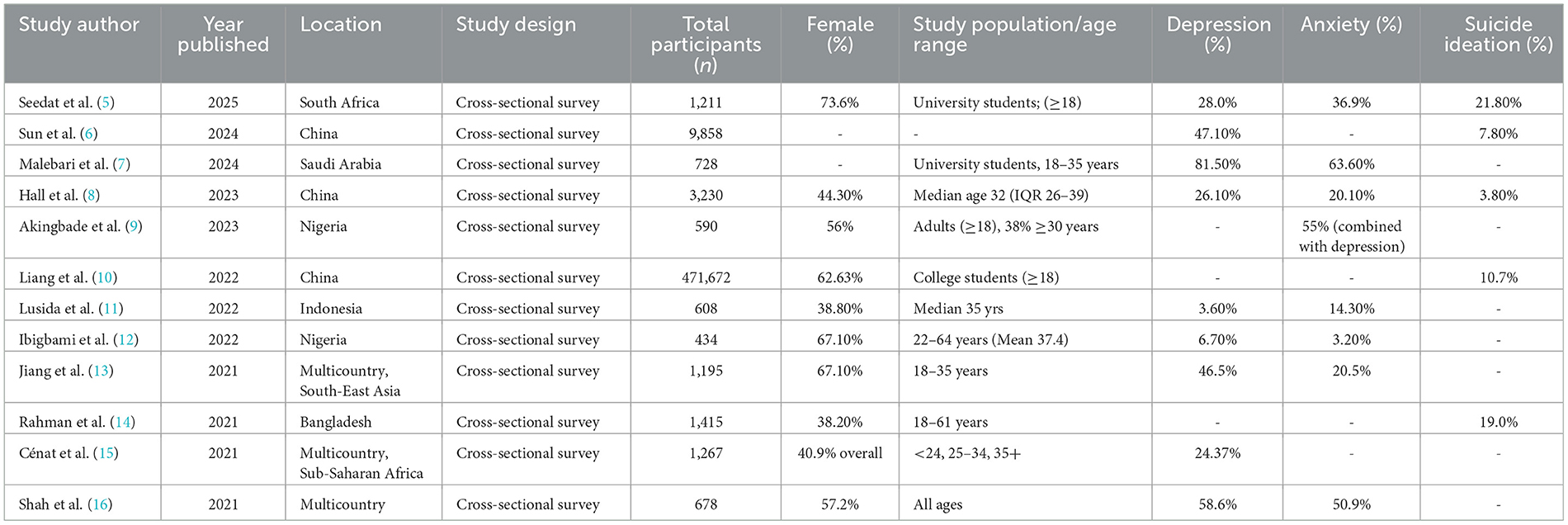
Over the past few years, the COVID-19 pandemic has revealed significant gaps in global mental health research, especially in resource-limited settings. Specifically, the pandemic has increased the prevalence of depression and anxiety symptoms and may have contributed to higher suicide rates worldwide. It has particularly affected the mental health of individuals from lower socio-economic backgrounds and those with limited access to social support and healthcare. Table 1 summarizes recent studies that assess the global psychological impact of the COVID-19 pandemic across various settings. These findings generally indicate a high worldwide prevalence of depression (up to 82%), anxiety (up to 64%), and suicidal ideation (up to 22%) during the pandemic.
To provide new research evidence from geographically diverse contexts, we previously launched a Research Topic on “Biosocial determinants and solutions for mental health conditions in low and middle-income countries: revealing the current evidence gaps”. This Research Topic includes several original studies that explore (a) the roles of social and demographic factors in mental health outcomes, especially during rapid changes like pandemics, armed conflict, and migration, and (b) offer guidance on cultural evidence necessary to shape public mental health initiatives in LMIC.
First, reports published in this Research Topic include an account of how COVID-19 restrictions impacted mental health. In a study with Chinese postgraduate students, Zhang et al. report higher stress and depression scores among students, especially rural female students. These scores were also associated with increased insomnia and suicidal ideation. The report calls for targeted psychological interventions and academic support systems that address students' specific needs. In Ghana, Nyawornota et al. investigate the impact of the COVID-19 pandemic on self-perceived health and physical activity levels among youth and adults. The results show significant sex differences in physical activity and self-perceived health during the pandemic, with women reporting lower activity levels and poorer health. These studies provide (1) a critical understanding of the evolution of health behaviors and perceptions under crisis conditions, (2) the psychosocial implications of being part of the healthcare workforce, and (3) the role of incorporating limited physical activity routines.
Second, several studies on this issue emphasize the importance of culturally sensitive research from Southeast Asia and the Middle East. In Ilam, Iran, Bazyar et al. present findings from a new population-based study that deepens our understanding of subjective health perceptions in low-resource settings. They examine the factors influencing self-rated health (SRH) and its value as a mental health indicator in conflict-affected and socioeconomically disadvantaged areas. The results show that poor SRH was predicted by hopelessness about the future and the presence of underlying chronic diseases. This research offers a scalable, low-cost alternative for identifying mental health issues to guide community health planning and policy in similar global contexts. In Northwest China, Niu and Wang conducted a study to understand better the psychological wellbeing of rural left-behind women (RLW). These women face significant challenges related to being the household head and raising children in vulnerable rural environments while their husbands migrate to urban areas for work. The study found that 35.7% of participants reported symptoms of depression, 37.6% experienced anxiety, and felt less secure. Notably, this study emphasizes the importance of integrating gender-sensitive approaches to assess the mental health impact of internal migration in similar LMIC settings. In Nepal, Mamidanna et al. explored the mental health effects of widowhood among women in a region where widowhood carries stigma and social isolation. The study revealed that widowed women exhibited high levels of emotional distress, anxiety, and depression, which could be worsened by age, poverty, and household income. These three studies highlight the critical intersection of gender, socioeconomic vulnerability, and cultural norms in societies that often experience social exclusion and economic hardship.
Third, studies in this issue highlight a significant, but often overlooked, role of environmental and economic stressors in impacting mental health outcomes. For example, during prolonged political and financial crises, El Khoury-Malhame et al. present new data from Lebanon showing that maladaptive coping strategies and intolerance of uncertainty are strongly linked to anxiety, depression, reduced wellbeing, and greater symptom expression among women. In contrast, adaptive coping strategies and social support are associated with better mental health outcomes. Additionally, in a longitudinal study in China, Liu and Zhang examine the psychological effects of household debt and find that indebtedness considerably worsens mental health. These studies underscore the importance of including mental health interventions that address structural (income, armed conflict) and relational (support, coping strategies) factors, especially in LMICs where financial insecurity is common.
Finally, since measurement gaps continue to be a major barrier to timely mental health assessment, Díaz-Castro et al. seek to improve pediatric mental health evaluation by validating the World Health Organization's Disability Assessment Schedule (2.0) for use with children and adolescents with mental disorders in specialized psychiatric care settings in Mexico. This study emphasizes the need for culturally appropriate assessment tools and scalable interventions.
In conclusion, this Research Topic presents new evidence on biosocial determinants of mental health in LMICs and highlights an unmet need for a coordinated, multifaceted approach. The studies will remind readers that (a) mental health must be incorporated into global health strategies, (b) such strategies should be developed through effective transdisciplinary collaboration supported by targeted funding, and (c) careful contextual implementation and community cohesion are crucial in addressing the rising burden of mental health issues worldwide.
Author contributions
RC: Writing – original draft, Investigation, Writing – review & editing, Supervision, Conceptualization. NT: Writing – original draft, Conceptualization, Investigation, Data curation, Writing – review & editing. SK: Data curation, Writing – review & editing, Writing – original draft, Investigation, Visualization.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization (2017). Available online at: https://apps.who.int/iris/handle/10665/254610 (Accessed August 22, 2025).
2. World Health Organization. Mental Health Atlas 2020. Geneva: World Health Organization (2021). Available online at: https://www.who.int/publications/i/item/9789240036703 (Accessed August 22, 2025).
3. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
4. Alegría M, Moyer A, Falgàs Bagué I, Wang Y, Alvarez K. Social determinants of mental health: where we are and where we need to go. Curr Psychiatry Rep. (2018) 20:95. doi: 10.1007/s11920-018-0969-9
5. Seedat S, Sengwayo M, Gani S, Mashego L, Ochayon J, Shepard A, et al. Prevalence and determinants of suicidal ideation among South African Health Sciences students at the onset of the COVID-19 pandemic. Front Psychiatry. (2025) 16:1492620. doi: 10.3389/fpsyt.2025.1492620
6. Sun HL, Chen P, Bai W, Zhang L, Feng Y, Su Z, et al. Prevalence and network structure of depression, insomnia and suicidality among mental health professionals who recovered from COVID-19: a national survey in China. Transl Psychiatry. (2024) 14:227. doi: 10.1038/s41398-024-02918-8
7. Malebari AM, Alamoudi SO, Al-Alawi TI, Alkhateeb AA, Albuqayli AS, Alothmany HN. Prevalence of depression and anxiety among university students in Jeddah, Saudi Arabia: exploring sociodemographic and associated factors. Front Public Health. (2024) 12:1441695. doi: 10.3389/fpubh.2024.1441695
8. Hall BJ Li G, Chen W, Shelley D, Tang W. Prevalence of depression, anxiety, and suicidal ideation during the Shanghai 2022 lockdown: a cross-sectional study. J Affect Disord. (2023) 330:283–90. doi: 10.1016/j.jad.2023.02.121
9. Akingbade O, Adeleye K, Fadodun OA, Fawole IO Li J, Choi EPH, Ho M, et al. eHealth literacy was associated with anxiety and depression during the COVID-19 pandemic in Nigeria: a cross-sectional study. Front Public Health. (2023) 11:1194908. doi: 10.3389/fpubh.2023.1194908
10. Liang SW, Liu LL, Peng XD, Chen JB, Huang AD, Wang XY, et al. Prevalence and associated factors of suicidal ideation among college students during the COVID-19 pandemic in China: a 3-wave repeated survey. BMC Psychiatry. (2022) 22:336. doi: 10.1186/s12888-022-03968-2
11. Lusida MAP, Salamah S, Jonatan M, Wiyogo IO, Asyari CH, Ali ND, et al. Prevalence of and risk factors for depression, anxiety, and stress in non-hospitalized asymptomatic and mild COVID-19 patients in East Java province, Indonesia. PLoS ONE. (2022) 17:e0270966. doi: 10.1371/journal.pone.0270966
12. Ibigbami OI, Akinsulore A, Opakunle T, Seun-Fadipe C, Oginni OA, Okorie VO, et al. Psychological distress, anxiety, depression, and associated factors among Nigerian healthcare workers during COVID-19 pandemic: a cross-sectional study. Int J Public Health. (2022) 67:1604835. doi: 10.3389/ijph.2022.1604835
13. Jiang N, Yan-Li S, Pamanee K, Sriyanto J. Depression, anxiety, and stress during the COVID-19 pandemic: comparison among higher education students in four countries in the Asia-Pacific region. J Popul Soc Stud. (2021) 29:370–83. doi: 10.25133/JPSSv292021.023
14. Rahman ME, Zubayer AA, Bhuiyan MRAM, Jobe MC, Khan MKA. Suicidal behaviors and suicide risk among Bangladeshi people during the COVID-19 pandemic: an online cross-sectional survey. Heliyon. (2021) 7:e05937. doi: 10.1016/j.heliyon.2021.e05937
15. Cénat JM, Noorishad PG, Kokou-Kpolou CK, Dalexis RD, Hajizadeh S, Guerrier M, et al. Prevalence and correlates of depression during the COVID-19 pandemic and the major role of stigmatization in low- and middle-income countries: a multinational cross-sectional study. Psychiatry Res. (2021) 297:113714. doi: 10.1016/j.psychres.2021.113714
16. Shah SMA, Mohammad D, Qureshi MFH, Abbas MZ, Aleem S. Prevalence, psychological responses, and associated correlates of depression, anxiety, and stress in a global population, during the coronavirus disease (COVID-19) pandemic. Community Ment Health J. (2021) 57:101–10. doi: 10.1007/s10597-020-00728-y
Keywords: global mental health, low and middle income countries, depression, anxiety, suicide
Citation: Chowdhury R, Trujillo N and Khalid S (2025) Editorial: Biosocial determinants and solutions of mental health conditions in low and middle-income countries. Front. Public Health 13:1691121. doi: 10.3389/fpubh.2025.1691121
Received: 22 August 2025; Accepted: 28 August 2025;
Published: 12 September 2025.
Edited and reviewed by: Wulf Rössler, Charité University Medicine Berlin, Germany
Copyright © 2025 Chowdhury, Trujillo and Khalid. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rajiv Chowdhury, cmFqY2hvd2RAZml1LmVkdQ==
†These authors share first authorship
 Rajiv Chowdhury
Rajiv Chowdhury Natalia Trujillo
Natalia Trujillo Samaun Khalid
Samaun Khalid