- 1EPI Department, Chongqing Center for Disease Control and Prevention (Chongqing Academy of Preventive Medicine), Chongqing, China
- 2School of Public Health, Southwest Medical University, Luzhou, China
Background: The human papillomavirus (HPV) vaccine is essential for preventing sexually transmitted infections and HPV-related cancers in both men and women. Vaccinating boys directly protects them and contributes to herd immunity. It also indirectly protects their future partners. As parents’ intentions strongly influence adolescents’ HPV vaccination, this study aimed to investigate the factors that influence their vaccination intentions for sons. The results of this study will provide a theoretical basis and practical recommendations for improving parental acceptance of HPV vaccination.
Methods: A multi-stage, non-random, cross-sectional survey was conducted, targeting guardians of male junior high school students across various districts and counties in Chongqing.
Results: A total of 3,481 valid responses were collected. Among the guardians, nearly 40% had never heard of HPV or the HPV vaccine. Overall, 71.3% of guardians expressed willingness to vaccinate their sons against HPV, while 28.7% were unwilling. Personal characteristics of the guardians, such as age and number of children, were associated with vaccination intention. Higher levels of knowledge about HPV were positively correlated with willingness to vaccinate, while vaccine hesitancy was associated with reduced acceptance.
Conclusion: This study suggests that guardians in Chongqing have a high willingness to vaccinate their sons against HPV, and vaccine knowledge is one of the influencing factors. However, concerns about vaccine safety and efficacy remain significant barriers to vaccine acceptance. Awareness of the HPV vaccine should be improved, especially in groups with limited knowledge, through targeted educational campaigns and advice from healthcare professionals to address vaccine hesitancy.
Introduction
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection and is closely associated with genital warts as well as cancers of the cervix, anus, throat, and other sites (1). Although HPV is often considered a women’s health issue, men are equally susceptible (2) and play an important role in transmitting the virus to their partners, thereby increasing their risk of developing associated diseases (3–6). Vaccination is an effective strategy for preventing HPV infection and related diseases. The American Advisory Committee on Immunization Practices (ACIP) recommends HPV vaccination for women aged 13–26 and men aged 13–21 (7). As evidence of the vaccine’s benefits in disease prevention and herd immunity accumulates, many countries have begun including boys in their national vaccination programs (8, 9). In 2020, the World Health Organization launched the Global Strategy to Eliminate Cervical Cancer, proposing to increase the HPV vaccination rate among girls under 15 years old to 90% by 2030 (10). In China, several pilot programs to vaccinate adolescent girls have been implemented in recent years, including a subsidy program for schoolgirls launched by the Chongqing municipality in 2022 (11).
However, no equivalent program currently exists for boys, resulting in limited vaccine accessibility and suboptimal coverage among male adolescents. This gender disparity may hinder the overall effectiveness of HPV prevention strategies, given the important role of males in HPV transmission and their risk of developing HPV-related cancers (12). Therefore, expanding vaccination programs to include boys could yield significant public health benefits. Since the HPV vaccine is most effective before the initiation of sexual activity, and minors require parental or guardian consent for vaccination, it is important to understand guardians’ attitudes toward vaccinating boys.
This study aims to assess the willingness of the guardians of male junior high school students in Chongqing to vaccinate their sons against HPV and identify the factors influencing their decision. The findings will provide a scientific basis for improving vaccine acceptance and coverage among adolescent boys, as well as offering practical strategies.
Methods
Study design and participants
This study conducted a cross-sectional observational study on guardians of male junior high school students in Chongqing between February to May 2023.
The target population was parents or legal guardians of male junior high school students. A multistage, non-probability sampling method was used. To ensure feasibility, selection was made by local CDC staff based on factors such as geographic location, school size, and willingness to participate. At the time the study began, HPV vaccination for males had not yet been implemented in China. According to published studies, parental willingness to vaccinate their sons against HPV ranged from 41% to 87% (13). Thus, we conservatively assumed an expected acceptance rate of 50%. Taking into account a design effect of 2.5, stratified sampling, and an anticipated 20% non-response rate, the required sample size was calculated to be 2,400 parents.
Ethics statement
This study was approved by the ethics committee of the Chongqing Center for Disease Control and Prevention (KY-2022-013). Informed consents were obtained from participants at the beginning of the survey.
Questionnaire
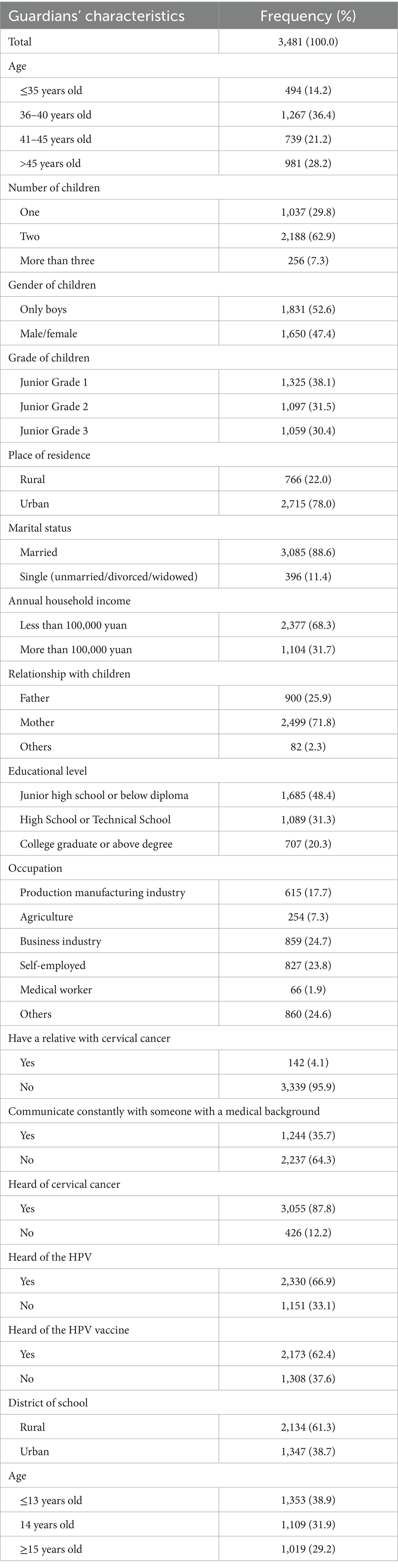
A questionnaire was designed, and the socio-demographic information (such as age, number of children, residence, education, occupation, marital status, income, and relationship with children) of the respondents was collected as shown in Table 1. In addition, it covers knowledge about HPV and the HPV vaccine and the degree of vaccine hesitation. HPV and HPV vaccine awareness of vaccination was measured through a number of general knowledge questions. Vaccine hesitation was measured by the Vaccine Hesitation Scale (VHS), which was developed by the Strategic Advisory Expert Group (SAGE) Vaccine Hesitation Working Group (14). The main outcome was whether the guardian was willing to vaccinate the child against HPV. Options include “The child has been or is being vaccinated,” “willing to be vaccinated,” “unwilling to be vaccinated,” and “later.” With only one option to choose from, we combined the last two responses, both of which indicate no recent intention to get the HPV vaccine.
Before making the questionnaire available to all participants, researchers surveyed a small portion of parents to ensure that it was easy to understand and complete. We conducted a reliability and validity analysis. Cronbach’s alpha coefficients are ≥0.6, indicating that the questionnaire is reliable.
Data collection
The final survey was distributed online via the mini application ‘Wen Juan Xing’, a widely used online survey platform with functions equivalent to Amazon Mechanical Turk. Researchers commissioned the class teachers to send out the questionnaire in WeChat groups, the most commonly used means of communication among Chinese parents and teachers. The questionnaire began with informed consent, and all participants were allowed to proceed with the survey items only if they agreed to continue the survey. The data of 3,481 parents who completed the questionnaire were recorded in our study, while the other uncompleted questionnaires cannot be recorded on the platform. All the records were anonymous and without any personal identifiers.
Statistical analysis
Descriptive statistics were calculated for sociodemographic characteristics, HPV and HPV vaccine awareness, and the number and percentage of vaccine hesitations. Knowledge scores (KS) were calculated to evaluate HPV and HPV vaccine knowledge, with one point assigned to each correct answer. Overall, KS were categorized into “low,” “medium,” and “high” levels. Vaccine hesitancy was assessed using a 10-item 5-point Likert scale, with responses ranging from 1 (strongly disagree) to 5 (strongly agree), resulting in a total score from 10 to 50. Based on the median, vaccine hesitancy was dichotomized into “low” and “high” for bivariate analyses. Willingness to vaccinate was assessed by the question: “Are you willing to get the HPV vaccine for your child right now?” Variables significantly associated with willingness to vaccinate in univariate analyses were included as covariates in the multivariable logistic regression model. Prior to fitting the model, multicollinearity among covariates was assessed using variance inflation factors (VIFs). All covariates had VIF values well below 5, indicating that multicollinearity was not a concern. Logistic regression was then used to identify factors independently associated with willingness to vaccinate, and results were reported as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was determined using two-tailed tests, with a significance level of 0.05. All analyses were conducted using R (version 4.4.2).
Results
A total of 3,481 parents of male junior high school students were included in this study, of whom two children were the majority (62.9%), followed by only children (29.8%). Among the respondents, most are mothers (71.8%), have a junior high school education or below (48.4%), and have an annual household income of less than 100,000 yuan (68.3%).
Characteristics of guardians
The characteristics of guardians and children are shown in Table 1. The average age of guardians was 41.8 ± 6.4 years old, and 78.0% of guardians lived in cities and towns. The majority (71.8%) were 45 years of age or younger, the majority (48.4%) had a junior high school diploma or less, and 20.3% had a university diploma or higher. In addition, 88.6% are married, 24.7% work as commercial or service workers, 23.8% are self-employed, and 17.7% work in manufacturing. Only 1.9% work in the medical field. A total of 68.3% of households have an annual income of less than 100,000 yuan. Most of the people who participated in the survey had two children. A total of 29.8% were only children.
Awareness of HPV
Of the 3,481 guardians who participated in the survey, the vast majority (87.8%) had heard of cervical cancer, and 66.9% had heard of HPV. More than half learned about HPV through radio, television, or the Internet, and approximately half learned about HPV through introductions from family or friends (Figure 1). The study designed eight questions to assess guardians’ knowledge of HPV, with one point for each correct answer. Among guardians who had heard of HPV, the average score was 3.4 ± 2.2, with the lowest score being 0 and the highest score being 8. KS is divided into three grades: ‘low’ (less than 3 points), ‘medium’ (3–5 points), and ‘high’ (more than 5 points). Among guardians who had heard of HPV, 37.3% had low awareness of HPV, 44.9% had moderate awareness, and 17.8% had high awareness.
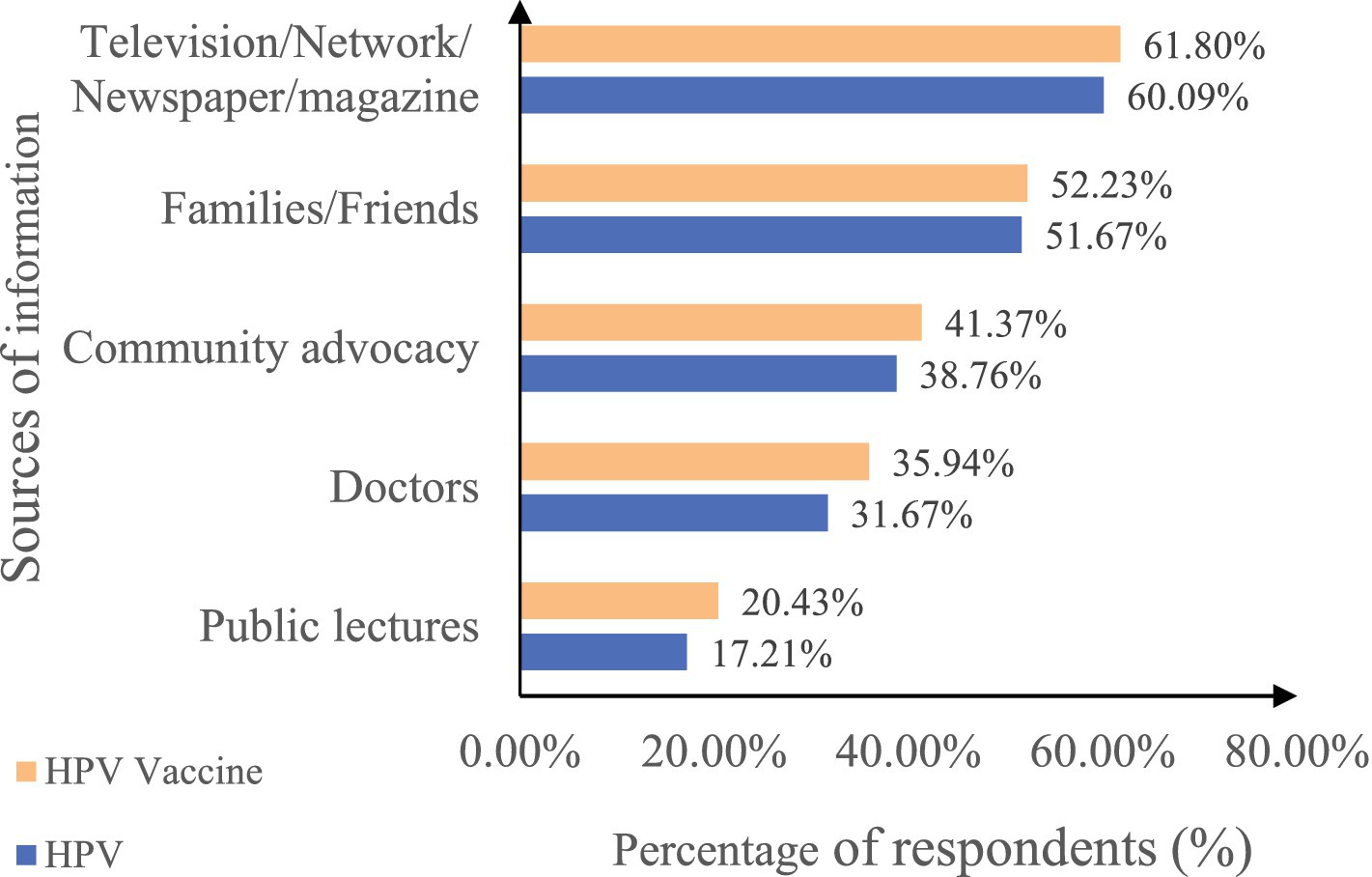
Figure 1. Main sources of information about HPV and HPV vaccine among guardians. The horizontal axis represents the percentage of respondents, and the vertical axis indicates the source of information. HPV, human papillomavirus; HPV vaccine, HPV vaccine. Different colors indicate the proportion of respondents who learned about HPV (blue) and HPV vaccine (orange) from each source. The questions were multiple choices in the survey.
Awareness of the HPV vaccine
In the survey, more than half (62.4%) of guardians had heard of the HPV vaccine. Of the guardians who had heard about the HPV vaccine, 61.8% learned about it through television, the Internet, newspapers, magazines, and 35.9% learned about it through doctors in hospitals or schools (Figure 1). We designed six questions to measure guardians’ awareness of the HPV vaccine, with one point awarded for each correct answer. Among guardians who had heard of the HPV vaccine, the average score was 3.5 ± 1.6, the lowest score was 0, and the highest score was 6. KS is divided into three grades: ‘low’ (less than 3 points), ‘medium’ (3–4 points), and ‘high’ (more than 4 points). Of the guardians who had heard about the HPV vaccine, 24.7% had a low level of cognitive knowledge about the HPV vaccine, 44.3% had a moderate level of cognitive knowledge about the HPV vaccine, and 31.0% had a high level of cognitive knowledge about the HPV vaccine.
Degree of vaccine hesitancy
WHO’s SAGE Working Group on Immunization defined vaccine hesitancy as the act of delaying or refusing vaccines despite vaccine availability, and the VHS was developed to assess vaccine hesitancy (15). The VHS consists of 10 items that are rated on a 5-point Likert scale, ranging from ‘strongly disagree’ to ‘strongly agree.’ Among the 3,481 guardians, the average score was 22.4 ± 4.3, the lowest score was 10, and the highest score was 50.
Vaccine hesitancy was divided into two groups, with ‘low’ indicating ≤25 points and ‘high’ indicating more than 26 points. The sample median was used as the cutoff value. Among the guardians we surveyed, 78.7% had low vaccine hesitancy and 21.3% had high vaccine hesitancy.
Attitude toward the HPV vaccine
A total of 71.3% of the guardians were willing to vaccinate their children against HPV, while only 28.7% were unwilling to vaccinate their children against HPV. Among them, 44.9% are worried that the child is too small and has an impact on its growth and development, 40.7% are worried about whether the vaccine really has a protective effect on the child after vaccination, 37.5% are worried about safety, and 81.2% are willing to vaccinate the child if the HPV vaccine is free of charge. Doctors’ and government recommendations for vaccination were the motivating factors for most of the respondents. A total of 54.9% did not know how to choose the vaccine, 20.8% chose the imported nine-valent vaccine, 15.6% chose the domestic two-valent vaccine, and 5.1% chose the imported four-valent vaccine.
Factors associated with guardians’ willingness to vaccinate their children
Table 2 shows the results of the binary logistic regression analysis investigating the relationship between vaccination intention and various individual characteristics. The analysis revealed that guardians residing in rural areas were 1.268 (95% CI: 1.074–1.497, p = 0.005) times more likely to vaccinate their children with the HPV vaccine compared to those in urban areas. Guardians with both sons and daughters were 1.654 (95% CI: 1.346–2.031, p < 0.001) times more likely to vaccinate their children than those with only sons. Guardians who had vaccinated their children with all the free HPV vaccines were less willing to vaccinate their children than those who had not; the proportion was 0.574 (95% CI: 0.440–0.744, p < 0.001) times. Additionally, those who had heard of HPV were 1.418 (95% CI: 1.083–1.862, p = 0.01) times more likely to vaccinate their children than those who had not. Those with moderate HPV knowledge were 2.265 (95% CI: 1.739–2.953, p < 0.001) times more likely to vaccinate than those with low knowledge, and those with high knowledge were 2.683 (95% CI: 1.634–4.531, p < 0.001) times more likely. Guardians with high vaccine hesitancy were 0.193 (95%CI: 0.160–0.231, p < 0.001) times less likely than those with low vaccine hesitancy to vaccinate HPV vaccine for their children.
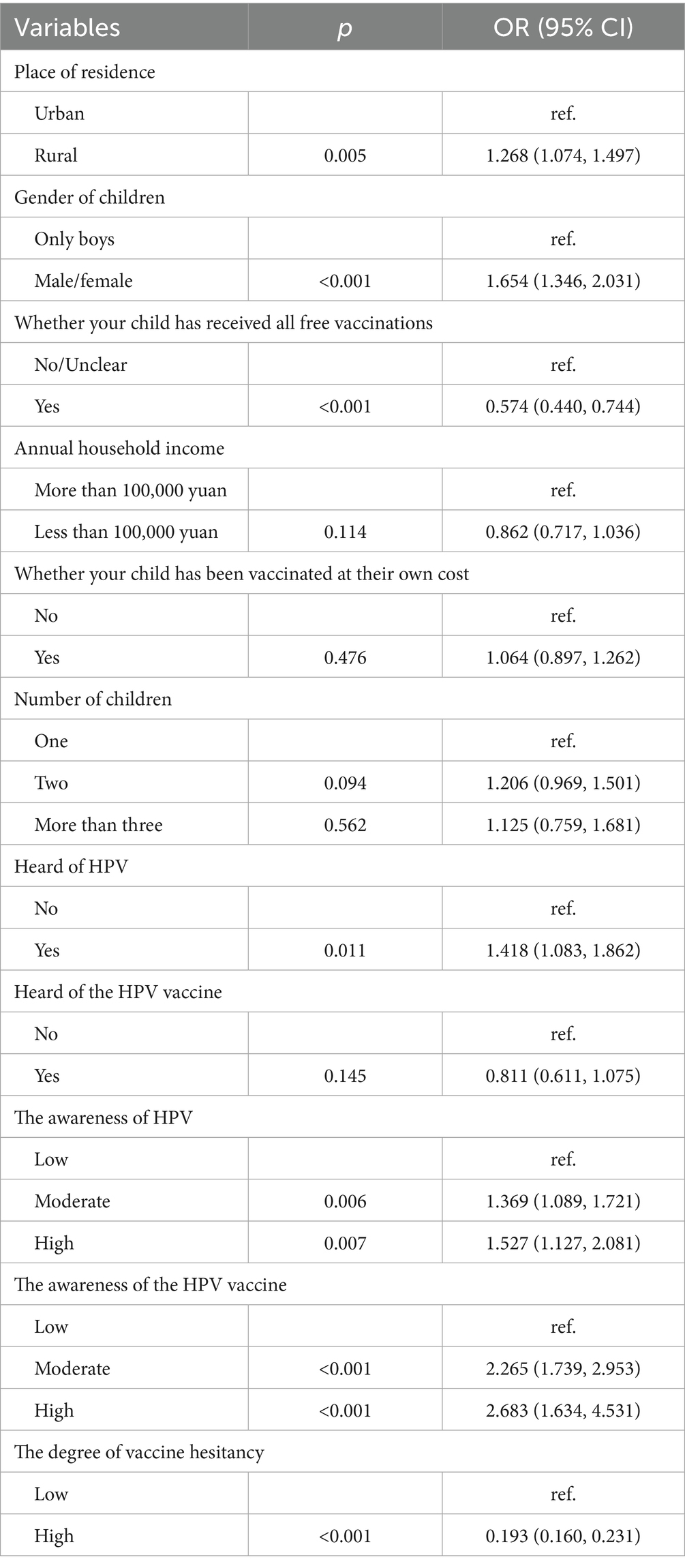
Table 2. Binary logistic regression analysis of attitude to the HPV vaccine to vaccinate their children among guardians.
Discussion
This study involved a cross-sectional survey in Chongqing, China, to investigate guardians’ willingness to have their sons vaccinated against HPV. The results showed that 71.3% of guardians were willing to vaccinate their sons, a proportion significantly higher than that reported among French parents of teenagers (16) and Greek guardians of children (17), and also higher than that among college students in China (18). In the United States and Canada, parental willingness ranges from 55% to 68% (19, 20), while in Spain, only approximately 24% of young Hispanic men believed the HPV vaccine could prevent future health problems (21). These cross-national differences likely reflect variations in vaccination policies, public health campaigns, and cultural or healthcare-related factors. The relatively high willingness observed in this study indicates that Chinese guardians—particularly in Chongqing—are receptive to HPV vaccination for boys when adequate information and policy support are provided. Strengthening health education and expanding HPV vaccination programs to include males could help translate this positive attitude into higher vaccination uptake.
Among the respondents, 36.4% of guardians were aged 36–40, an age group that pays particular attention to health issues. Studies indicate that the HPV infection rates are higher among men aged 26–35 (22), suggesting that guardians in this age group realize the importance of HPV vaccination and are therefore more willing to have their children vaccinated. This increase in willingness may be related to a deeper understanding of HPV-related diseases. Beyond age-related differences, rural guardians, despite generally having lower educational levels, were more willing to vaccinate their children than urban guardians. This finding aligns with research in Vietnam, where rural residents also demonstrated greater willingness to vaccinate (23). This pattern may reflect rural guardians’ perception of higher HPV risk and its potential consequences due to limited access to healthcare. Such heightened perception of severity and susceptibility could motivate stronger preventive behavior, thereby increasing their willingness to vaccinate sons.
In this study, 47.1% of guardians had some knowledge of HPV vaccines, higher than figures reported in systematic reviews and meta-analyses (37%) (24), and Nigeria (36.5%) (25), but lower than Romania (85.8%) (26), the United Kingdom (54.8%) (27), Kenya (48%) (28), and Thailand (60%) (29). Guardians familiar with HPV and HPV vaccines were more likely to choose vaccination. Those with a high level of knowledge were significantly more willing to vaccinate than those with lower knowledge, consistent with previous studies (30). This suggests that a better understanding of HPV and its link to cervical cancer leads to greater vaccine acceptance (31). Raising awareness of HPV and its vaccines among parents of junior high students, particularly those with low awareness, is therefore key to increasing vaccination rates.
Guardians with both sons and daughters were significantly more willing to vaccinate their children against HPV than those with only sons. Previous studies indicate that parents generally accept HPV vaccination for daughters more readily than for sons, and mothers are more inclined to vaccinate daughters (32). This reflects the perception that HPV vaccines are “female-only,” ignoring their protective effects for males against diseases such as anal and laryngeal cancers and condyloma acuminatum. HPV infection affects both males and females, and men are both at risk and important in transmission.
The quadrivalent and nine-valent HPV vaccines have been approved by China’s National Medical Products Administration (NMPA) for males aged 9 to 26, highlighting the country’s commitment to HPV prevention in men. Targeted health education should be strengthened to increase coverage. For example, Tianjin has integrated HPV vaccination into its public health program, providing subsidized vaccines for eligible females and promoting male vaccination following the nine-valent approval. Universities have also run campaigns to encourage a gender-neutral vaccination approach. Such efforts could serve as a model for other regions seeking to expand coverage across genders.
The survey found that vaccine hesitancy among guardians may prevent their sons from receiving HPV vaccines. In 2019, the World Health Organization (WHO) listed vaccine hesitancy as one of the “Top Ten Global Health Threats” and described it as “a potential serious challenge to immunization programmes.” The reasons given by guardians who participated in the survey for refusing HPV vaccines were generally concerns about the vaccine’s impact on children’s growth and development due to their young age, or doubts about its protective effect and safety. These findings are largely consistent with the results of similar research (33, 34). Overall, safety concerns are a key reason for HPV vaccine hesitancy (35, 36). Parents of vaccinated children stated that recommendations from doctors or healthcare authorities increased the likelihood of their children receiving the HPV vaccine. Doctors’ recommendations were an important factor in addressing vaccine hesitancy (37, 38). Similarly, in Spain, HPV vaccination among adolescent girls was strongly associated with advice from health professionals, highlighting that nurse and physician recommendations are key drivers of uptake (39). Promoting HPV vaccination should therefore involve clinical doctors through routine check-ups and vaccination clinics, which can reduce information barriers and enhance parental trust.
This survey revealed that 54.9% of guardians were uncertain about which vaccine to choose. Among recognized vaccine types, only 20.8% opted for the imported nine-valent vaccine, and 15.6% chose the domestic two-valent vaccine. This discrepancy between intention and choice may result from insufficient information, limited understanding of vaccine types, and concerns about cost and effectiveness. More systematic health education and information dissemination are recommended, with targeted publicity, particularly for urban and low-income families, to support informed decision-making. Improving information channels and providing professional consultation can enhance both vaccination intention and uptake, promoting wider HPV vaccine coverage.
This study has several limitations. First, its cross-sectional design allows only associations, not causal inferences. Second, the multistage non-probability sampling may introduce selection bias, though the sample was structured to reflect Chongqing’s demographic composition—a predominantly rural and mountainous region—ensuring reasonable representativeness. Third, while participants’ socioeconomic profiles generally matched census data, some subgroup imbalances may remain. Finally, self-reported information could be affected by socially desirable responses.
Despite these limitations, the study’s strengths include a structured and population-focused questionnaire, diverse guardian participation, and systematic assessment of key factors influencing male HPV vaccination willingness. Conducted before the official rollout of the male HPV vaccine in China, this research provides valuable real-world insights to support evidence-based policymaking and tailored vaccination education and promotion strategies in similar settings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the ethics committee of the Chongqing Center for Disease Control and Prevention (KY-2022-013). Informed consents were obtained from participants at the beginning of the survey. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XH: Writing – original draft, Writing – review & editing. NB: Investigation, Writing – review & editing, Writing – original draft. JX: Conceptualization, Validation, Supervision, Writing – review & editing. NW: Project administration, Writing – review & editing, Methodology. YX: Investigation, Writing – review & editing, Validation. BX: Resources, Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Chongqing Municipal Health Commission, Chongqing Municipal Science and Technology Bureau [2024MSXM021].
Acknowledgments
The authors wish to express great appreciation for the assistance of all the participants in the schools and the Centers for Disease Control and Prevention in the data collection of the survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Williamson, AL. Recent developments in human papillomavirus (HPV) vaccinology. Viruses. (2023) 15:1440. doi: 10.3390/v15071440
2. Garolla, A, Graziani, A, Grande, G, Ortolani, C, and Ferlin, A. HPV-related diseases in male patients: an underestimated conundrum. J Endocrinol Investig. (2024) 47:261–74. doi: 10.1007/s40618-023-02192-3
3. Hu, J, Ji, L, Li, P, Ni, X, Huang, Y, Tao, J, et al. Genital HPV prevalence, follow-up and persistence in males and HPV concordance between heterosexual couples in Wenzhou, China. Infect Drug Resist. (2022) 15:7053–66. doi: 10.2147/idr.S387226
4. Falcaro, M, Castañon, A, Ndlela, B, Checchi, M, Soldan, K, Lopez-Bernal, J, et al. The effects of the National HPV Vaccination Programme in England, UK, on cervical Cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet. (2021) 398:2084–92. doi: 10.1016/s0140-6736(21)02178-4
5. Lopez-Diez, E, Perez, S, Carballo, M, Iñarrea, A, de la Orden, A, Castro, M, et al. Lifestyle factors and oncogenic papillomavirus infection in a high-risk male population. PLoS One. (2017) 12:e0184492. doi: 10.1371/journal.pone.0184492
6. Bruni, L, Albero, G, Rowley, J, Alemany, L, Arbyn, M, Giuliano, AR, et al. Global and regional estimates of genital human papillomavirus prevalence among men: a systematic review and meta-analysis. Lancet Glob Health. (2023) 11:e1345–62. doi: 10.1016/s2214-109x(23)00305-4
7. Petrosky, E, Bocchini, JA Jr, Hariri, S, Chesson, H, Curtis, CR, Saraiya, M, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. (2015) 64:300–4.
8. Giuliano, AR, Palefsky, JM, Goldstone, S, Moreira, ED Jr, Penny, ME, Aranda, C, et al. Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. N Engl J Med. (2011) 364:401–11. doi: 10.1056/NEJMoa0909537
9. Spînu, AD, Anghel, RF, Marcu, DR, Iorga, DL, Cherciu, A, and Mischianu, DLD. HPV vaccine for men: where to? (Review). Exp Ther Med. (2021) 22:1266. doi: 10.3892/etm.2021.10701
10. Human papillomavirus vaccines. (2020) WHO position paper. Geneva: World Health Organization, Available online at: https://www.who.int/news/item/19-08-2020-world-health-assembly-adopts-global-strategy-to-accelerate-cervical-cancer-elimination?utm_source=chatgpt.com
11. Bai, N, Wang, Q, Shao, J, Chen, L, Wang, C, Xiao, X, et al. HPV vaccination intention among guardians of female secondary school students in Chongqing, China. Hum Vaccin Immunother. (2024) 20:2381293. doi: 10.1080/21645515.2024.2381293
12. Li, Y, Zhao, F, Wu, D, Qin, C, Lu, Y, Yang, Y, et al. Prevalence of human papillomavirus and genotype distribution in Chinese men: a systematic review and meta-analysis. Cancer Med. (2025) 14:e70686. doi: 10.1002/cam4.70686
13. Zhao, Y, Sun, Y, Li, Z, Ma, J, Wang, F, and Jia, B. HPV vaccination willingness among 3,081 secondary school parents in China's capital. Hum Vaccin Immunother. (2025) 21:2477383. doi: 10.1080/21645515.2025.2477383
14. Ogilvie, G, Anderson, M, Marra, F, McNeil, S, Pielak, K, Dawar, M, et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. (2010) 7:e1000270. doi: 10.1371/journal.pmed.1000270
15. Larson, HJ, Jarrett, C, Schulz, WS, Chaudhuri, M, Zhou, Y, Dube, E, et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. (2015) 33:4165–75. doi: 10.1016/j.vaccine.2015.04.037
16. Rivera, AF, Dussault, JM, Oudin Doglioni, D, Chyderiotis, S, Sicsic, J, Barret, AS, et al. Sociodemographic determinants of HPV vaccine awareness, uptake, and intention among parents of adolescents in France 2021-22. Hum Vaccin Immunother. (2024) 20:2381300. doi: 10.1080/21645515.2024.2381300
17. Toska, A, Latsou, D, Paraskeuopoulou, C, Fradelos, E, Albani, E, Milionis, C, et al. Knowledge and beliefs of Greek parents towards HPV infection and vaccination—are they willing to vaccinate their sons? Int J Adolesc Med Health. (2024) 36:61–8. doi: 10.1515/ijamh-2023-0144
18. Ran, H, Chen, Y, Gao, J, Guo, H, and Peng, S. Low awareness of HPV infection and willingness of HPV vaccination among Chinese male college students in the east of China. Front Public Health. (2022) 10:971707. doi: 10.3389/fpubh.2022.971707
19. Achimaș-Cadariu, T, Pașca, A, Nicoară, D, and Dumitrașcu, DL. Exploring vulnerable, ethnic minority, and low socioeconomic children's knowledge, beliefs, and attitudes regarding HPV vaccination in Romania. Healthcare. (2025) 13:2010. doi: 10.3390/healthcare13162010
20. Choi, Y, Seo, HJ, Seo, J, Park, E, and Yang, HJ. Perceptions of human papillomavirus vaccination among adolescent boys and their parents in high-income countries: a scoping review protocol. BMJ Open. (2025) 15:e092705. doi: 10.1136/bmjopen-2024-092705
21. Thomas, TL, Stephens, DP, Johnson-Mallard, V, and Higgins, M. Young Hispanic men and human papillomavirus vaccination choices. J Transcult Nurs. (2016) 27:103–8. doi: 10.1177/1043659614526759
22. Yi, X, Chen, H, Wu, G, Hu, Y, and Tang, X. Trends in human papillomavirus infection and genotype distribution among males in Chongqing, China (2017-2022): an observational study. Eur J Clin Microbiol Infect Dis. (2024) 43:2127–35. doi: 10.1007/s10096-024-04933-5
23. Tran, NT, Phan, TNT, Pham, TT, Le, TT, Le, HM, Nguyen, DT, et al. Urban-rural disparities in acceptance of human papillomavirus vaccination among women in Can Tho. Vietnam Ann Ig. (2023) 35:641–59. doi: 10.7416/ai.2023.2575
24. Trim, K, Nagji, N, Elit, L, and Roy, K. Parental knowledge, attitudes, and behaviours towards human papillomavirus vaccination for their children: a systematic review from 2001 to 2011. Obstet Gynecol Int. (2012) 2012:921236. doi: 10.1155/2012/921236
25. Okunade, KS, Sunmonu, O, Osanyin, GE, and Oluwole, AA. Knowledge and acceptability of human papillomavirus vaccination among women attending the gynaecological outpatient clinics of a university teaching hospital in Lagos, Nigeria. J Trop Med. (2017) 2017:8586459. doi: 10.1155/2017/8586459
26. Voidăzan, S, Tarcea, M, Morariu, SH, Grigore, A, and Dobreanu, M. Human papillomavirus vaccine—knowledge and attitudes among parents of children aged 10-14 years: a cross-sectional study, Tîrgu Mureş, Romania. Cent Eur J Public Health. (2016) 24:29–38. doi: 10.21101/cejph.a4287
27. Sherman, SM, and Nailer, E. Attitudes towards and knowledge about human papillomavirus (HPV) and the HPV vaccination in parents of teenage boys in the UK. PLoS One. (2018) 13:e0195801. doi: 10.1371/journal.pone.0195801
28. Masika, MM, Ogembo, JG, Chabeda, SV, Wamai, RG, and Mugo, N. Knowledge on HPV vaccine and cervical Cancer facilitates vaccine acceptability among school teachers in Kitui County, Kenya. PLoS One. (2015) 10:e0135563. doi: 10.1371/journal.pone.0135563
29. Songthap, A, Pitisuttithum, P, Kaewkungwal, J, Fungladda, W, and Bussaratid, V. Knowledge, attitudes, and acceptability of a human papilloma virus vaccine among students, parents and teachers in Thailand. Southeast Asian J Trop Med Public Health. (2012) 43:340–53.
30. Ganczak, M, Owsianka, B, and Korzeń, M. Factors that predict parental willingness to have their children vaccinated against HPV in a country with low HPV vaccination coverage. Int J Environ Res Public Health. (2018) 15:645. doi: 10.3390/ijerph15040645
31. Dereje, N, Ashenafi, A, Abera, A, Melaku, E, Yirgashewa, K, Yitna, M, et al. Knowledge and acceptance of HPV vaccination and its associated factors among parents of daughters in Addis Ababa, Ethiopia: a community-based cross-sectional study. Infect Agent Cancer. (2021) 16:58. doi: 10.1186/s13027-021-00399-8
32. Heyde, S, Osmani, V, Schauberger, G, Cooney, C, and Klug, SJ. Global parental acceptance, attitudes, and knowledge regarding human papillomavirus vaccinations for their children: a systematic literature review and Meta-analysis. BMC Womens Health. (2024) 24:537. doi: 10.1186/s12905-024-03377-5
33. Karafillakis, E, Simas, C, Jarrett, C, Verger, P, Peretti-Watel, P, Dib, F, et al. HPV vaccination in a context of public mistrust and uncertainty: a systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum Vaccin Immunother. (2019) 15:1615–27. doi: 10.1080/21645515.2018.1564436
34. Borena, W, Luckner-Hornischer, A, Katzgraber, F, and Holm-von, LD. Factors affecting HPV vaccine acceptance in West Austria: do we need to revise the current immunization scheme? Papillomavirus Res. (2016) 2:173–7. doi: 10.1016/j.pvr.2016.10.001
35. Joshi, R, and Kilinsky, A. HPV vaccine hesitancy in the United States. Curr Opin Pediatr. (2025) 37:198–204. doi: 10.1097/mop.0000000000001441
36. Kyei, GK, Kyei, EF, and Ansong, R. HPV vaccine hesitancy and uptake: a conceptual analysis using Rodgers' evolutionary approach. J Adv Nurs. (2025) 81:2368–81. doi: 10.1111/jan.16653
37. Baumann, A, Andersen, B, Østergaard, L, and Larsen, MB. Sense & sensibility: decision-making and sources of information in mothers who decline HPV vaccination of their adolescent daughters. Vaccine X. (2019) 2:100020. doi: 10.1016/j.jvacx.2019.100020
38. Achimaș-Cadariu, T, Pașca, A, Jiboc, NM, Puia, A, and Dumitrașcu, DL. Vaccine hesitancy among European parents-psychological and social factors influencing the decision to vaccinate against HPV: a systematic review and Meta-analysis. Vaccines. (2024) 12:127. doi: 10.3390/vaccines12020127
Keywords: HPV vaccine, vaccination willingness, vaccine hesitancy, male adolescents, guardianship
Citation: He X, Bai N, Xu J, Wan N, Xiao Y and Xu B (2025) HPV vaccination intention among guardians of male junior high school students in Chongqing, China. Front. Public Health. 13:1692814. doi: 10.3389/fpubh.2025.1692814
Edited by:
Marco Dettori, University of Sassari, ItalyReviewed by:
Enver Envi Roshi, University of Medicine, AlbaniaDaniel Enterria Morales, University of California, San Diego, United States
Copyright © 2025 He, Bai, Xu, Wan, Xiao and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Binyue Xu, NTYzMjk4NTMwQHFxLmNvbQ==
†These authors have contributed equally to this work
 Xiaoqin He
Xiaoqin He Ningpei Bai1†
Ningpei Bai1†