- School of Economics, Qingdao University, Qingdao, China
Introduction: Although the co-morbidity of chronic diseases and depression has been widely documented, its psychosocial mechanisms have not been systematically explored. This study analyzed the impact of chronic disease on depression, while emphasizing the mediating roles that income satisfaction, job safety satisfaction, and social cognitive capital play in the psychosocial mechanism.
Methods: Using the 2022 China Family Tracking Survey (CFPS) data, this study conducted a baseline regression using an ordered logit model, and explored the pathways of chronic illnesses on depressive symptoms through mechanism tests and heterogeneity analyses (n = 7,896).
Results: Chronic conditions are associated with a considerable increase in the risk of depressive symptoms (OR = 1.671, p < 0.01). Mechanistic analyses showed that income satisfaction, job safety satisfaction and social cognitive capital all played partial mediating roles. Heterogeneity analyses indicated that the impact of chronic illness on depression was stronger among males, individuals with less robust social support, and non-users of the Internet.
Discussion: This research reveals that chronic illness constitutes a notable risk factor for depression and underscores its indirect impacts on mental health through three psychosocial pathways: financial strain, job safety, and insufficient interpersonal trust. The results emphasize the importance of integrating socioeconomic support, workplace improvement and digital health resources in chronic disease management to mitigate the risk of depression.
1 Introduction
As a major global public health issue, chronic diseases not only inflict long-term harm on patients’ physical health but also exert a profound influence on their psychological well-being. Studies have revealed a strong connection between chronic pain and depression. In addition, patients with chronic diseases—including diabetes, cancer, stroke, chronic liver disease, kidney disease, and COPD—have a notably higher incidence of mental disorders and a greater likelihood of developing depression (1–12). Chronic illnesses not only lead to a decrease in the patient’s ability to perform daily living tasks, but may also exacerbate the depressive condition (13). The long duration of the disease, complex treatment, and numerous complications not only bring financial burden to the family, but also may induce or aggravate depressive symptoms through physiological mechanisms such as neuroendocrine dysregulation (14). Conversely, depression can itself contribute to a higher susceptibility to chronic illnesses, adversely affecting their prognosis and diminishing the overall quality of life. This bidirectional interaction—where chronic diseases exacerbate depression and depression increases susceptibility to chronic diseases—often creates a self-perpetuating cycle that is challenging to overcome (15, 16). Beck’s cognitive model of depression posits that patients with chronic diseases are forced to abandon valued activities due to illness-related limitations. This creates a profound sense of psychological loss and burden, representing a key mechanism in the onset of depression (17). Consequently, it is essential—from both clinical and public health angles—to detect and manage depression early in patients suffering from chronic diseases.
More notably, compared to a single chronic disease, co-morbidity typically implies a longer disease course, more complex treatment processes, and poorer health outcomes. Regarding chronic comorbidities and depression, a meta-analysis indicates that those with two or more chronic conditions experience an approximately twofold higher risk of depression than individuals without any (6). The coexistence of multiple diseases not only leads to diminished physical function and deteriorated quality of life but also significantly increases mortality risk (18, 19). The impact of chronic diseases extends beyond the medical sphere, profoundly affecting psychological and social functioning. Patients and their families often bear heavy economic burdens and psychological stress (20). Studies reveal that chronic illnesses have become the primary driver behind the reduction in health status among people in China (21). Depression, as a highly disabling mental disorder, can cause emotional disturbances, sleep problems, and even suicidal behavior, further exacerbating the disease burden. By 2017, depression had affected over 258 million people globally, including 56 million in China (22, 23).
Although the comorbidity of chronic diseases and depression has been widely documented (9, 24–26), its underlying mechanisms—particularly the psychosocial pathways—remain insufficiently explored. Existing research predominantly focuses on biological mechanisms such as inflammatory responses and neuroendocrine dysregulation (27, 28), while rarely conducting systematic analyses of the mediating processes through which chronic diseases lead to depression from multidimensional perspectives including social, psychological, and behavioral factors. For instance, patients with limited physical activity often become more dependent on others, experience reduced social engagement, and exhibit diminished interpersonal trust (29). These shifts in psychosocial factors may serve as crucial mediators for depression onset. Conversely, modern information technologies like the internet provide chronic disease patients with novel avenues for social support and information access (30). Research indicates that internet users exhibit lower chronic disease risk (31), as patients can utilize online platforms for social interaction, medical information retrieval, and recreational activities—thereby enhancing psychological well-being. Therefore, the psychosocial mechanisms within the digital society context warrant further exploration. Economic pressures also represent a significant mediating factor. Most chronic diseases require long-term management or lifelong treatment, imposing sustained financial burdens and labor force losses (32, 33). Low income coupled with high expenditures may lead to a loss of perceived control over life, thereby inducing feelings of helplessness and depressive symptoms. Consequently, constructing a comprehensive psychosocial mechanism analysis framework encompassing socioeconomic status, job safety, and social cognitive capital not only helps elucidate the complex pathways linking chronic diseases and depression but also provides a theoretical foundation for developing targeted psychological interventions.
This study employs an ordered logit model to investigate the impact of chronic diseases on depressive symptoms, placing emphasis on the mediating effects of income satisfaction, job safety, and interpersonal trust. Furthermore, the study performed heterogeneity analyses across three dimensions—gender, social support, and internet usage—to explore variations in the chronic illness-depression association among different subgroups. The results provide a scientific foundation for developing psychological interventions in chronically ill patients, emphasizing the integration of psychosocial support into long-term care to enhance well-being and alleviate the combined burden of physical and mental health conditions.
2 Datasets
2.1 Sample selection
This study makes use of data from the 2022 China Family Panel Studies (CFPS), which is a nationally representative survey carried out by the Institute of Social Science Survey affiliated with Peking University (34). Fieldwork was conducted between May and December 2022, which encompasses four key survey instruments (community, household, adult, and child modules) within the framework of stratified multi-stage probability sampling.
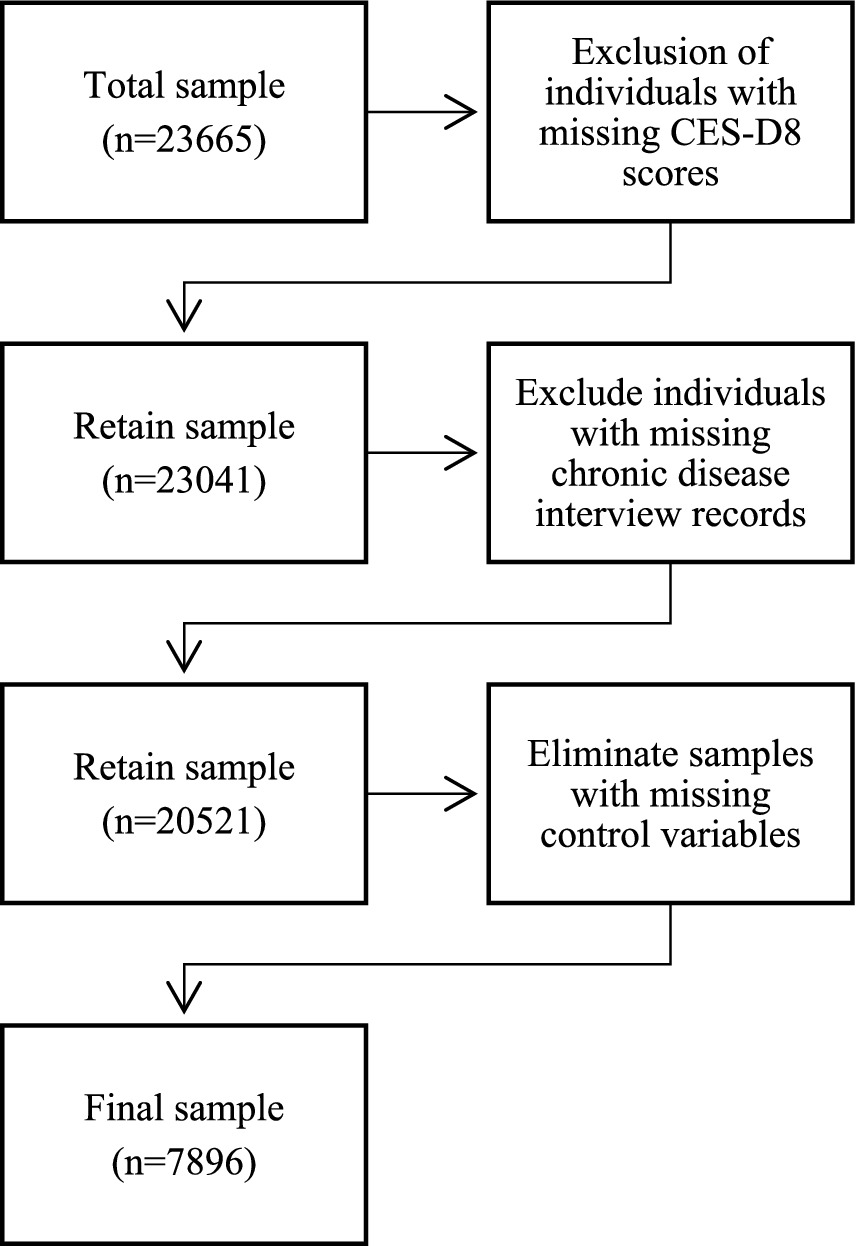
During the sample selection process, the study included individuals of legal working age1 (males: aged 18–60; females: aged 18–55) and excluded individuals with unclear educational characteristics and mental health data. The analytical framework incorporated 7,896 eligible participants meeting inclusion criteria, with sample attrition pathways and exclusion rationales systematically visualized in Figure 1 to ensure methodological transparency.
2.2 Measure
2.2.1 Explained variable: depressive symptoms
Depressive symptoms were evaluated using the 8-item Center for Epidemiologic Studies Depression Scale, a shortened version of the original CES-D created by Radloff (35). The scale measures the frequency of eight symptoms experienced in the past week, including: low mood, trouble starting tasks, sleep disturbances, lack of positive feelings, social isolation, reduced happiness, prolonged sadness, and loss of motivation. Responses were scored on a 4-point scale, ranging from 1 (rarely; <1 day) to 4 (most of the time; 5–7 days). Two positive items (e.g., happiness) were reverse-scored. The total score ranges from 8 to 32, with higher scores indicating more severe depressive symptoms.
2.2.2 Explanatory variable: chronic
Chronic disease prevalence was measured in this study using the following question: “Have you received a diagnosis of a chronic disease from a doctor in the past 6 months?” This variable is binary, coded as 1 for “yes” and 0 for “no.” This self-reported method based on physician diagnosis accurately identifies clinically confirmed chronic disease status within the past 6 months, providing a reliable empirical foundation for subsequent analysis.
2.2.3 Mechanism variables
To further elucidate how chronic diseases influence the onset and progression of depression through psychosocial mechanisms, this study introduces income satisfaction, job satisfaction, and social cognitive capital as mediating variables, constructing a multidimensional mechanism analysis framework. These variables aim to explain the psychological adaptation challenges chronic disease patients may face when confronting long-term health pressures—and their ultimate impact on depressive states—not only from the perspective of objective material conditions but also from subjective cognitive and emotional experiences.
First, income satisfaction serves as a key indicator reflecting individuals’ subjective evaluation of their economic status. Its level directly relates to patients’ psychological resilience when coping with additional medical expenses, income reduction, or diminished work capacity stemming from chronic illness. This study employs a 5-point scale to measure this indicator, with scores ranging from 1 (very dissatisfied) to 5 (very satisfied). Chronic illness may reduce labor participation rates and work efficiency, thereby impacting personal and household finances. Low income satisfaction may intensify patients’ perceived economic strain, inducing feelings of helplessness and anxiety, ultimately increasing depression risk. Thus, income satisfaction plays a crucial mediating role between chronic illness and depression: chronic illness constrains economic capacity, lowers income satisfaction, and subsequently affects mental health status.
Second, job safety satisfaction serves as another critical psychosocial mediating variable. This study measured it using the CFPS questionnaire item “Are you satisfied with the safety of your current job?.” This variable reflects individuals’ subjective perceptions regarding workplace physical safety conditions, protection against physical hazards, and labor safety measures. Chronic disease patients often exhibit heightened sensitivity to safety risks in the workplace due to compromised health. For instance, physical discomfort may increase the risk of operational errors or accidents, or physical limitations may hinder their ability to handle high-risk tasks. Such concerns and dissatisfaction regarding safety issues significantly increase psychological burden, triggering anxiety and tension, which in turn indirectly exacerbate depressive symptoms. Therefore, perceived workplace safety acts as a conduit between chronic illness and depressive symptoms.
Third, social cognitive capital—reflecting core trust and social cognition—is defined as the “tendency to trust others.” It adopts a binary coding method: “trust” is coded as 1, and “distrust” as 0. Chronic disease patients, due to prolonged illness, may experience reduced social interaction and even impaired interpersonal trust stemming from disease stigma. Trust constitutes a core component of social capital. Higher social cognitive capital facilitates effective acquisition of social support, helping patients better integrate into social networks and strengthen psychological resilience. Conversely, patients who tend to distrust others are more likely to engage in social avoidance and experience emotional isolation, thereby amplifying the negative psychological impacts of chronic illness. Thus, social cognitive capital acts as a cognitive mediator between chronic illness and depression. A lack of trust may intensify patients’ feelings of helplessness and loneliness, subsequently increasing the likelihood of depression.
2.2.4 Control variables
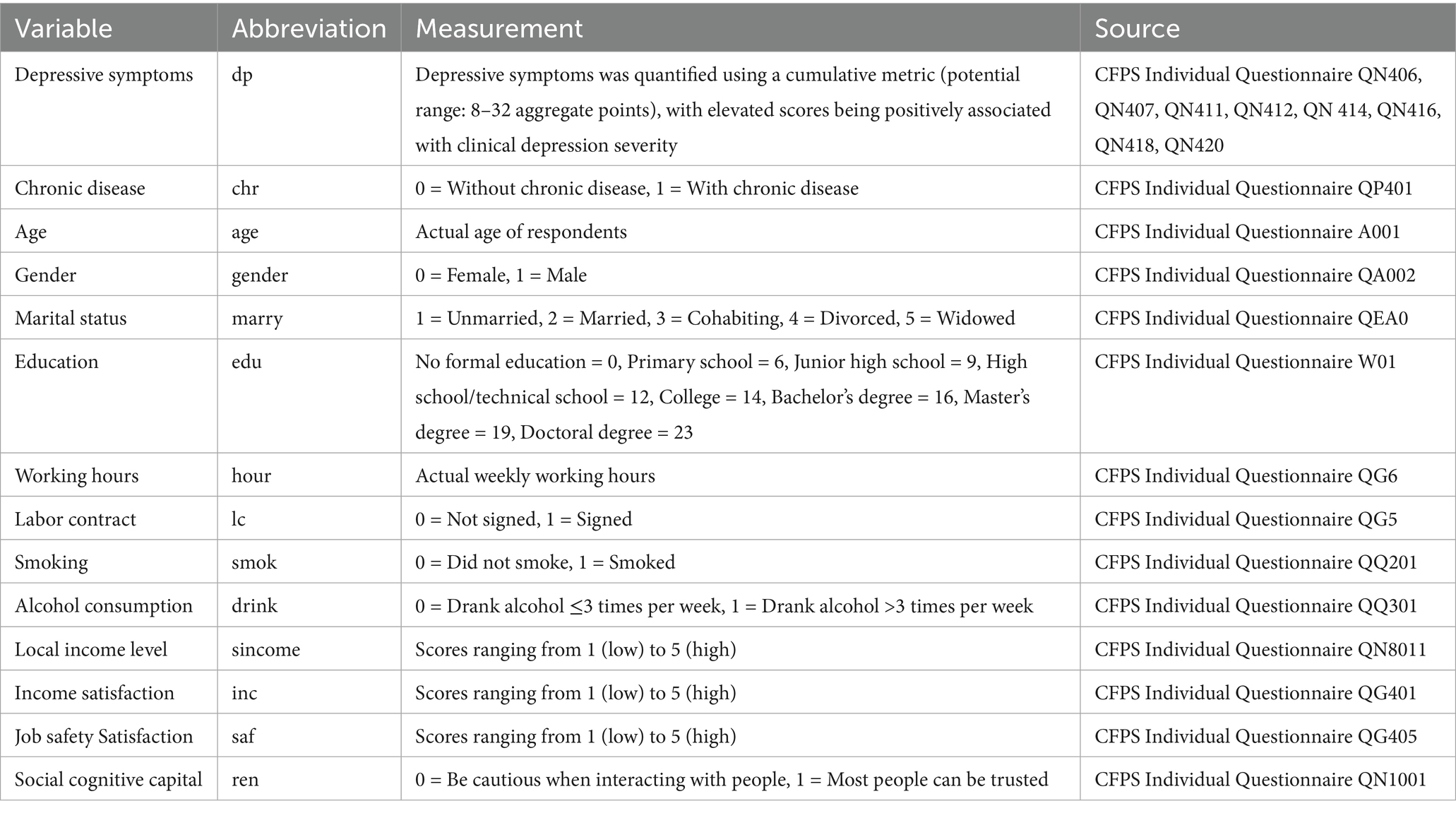
Given the numerous factors influencing individual depressive symptoms, the following four control variables were selected based on relevant studies (36, 37). (1) Individual characteristics: age, gender, marital status, and education. (2) Employment characteristics: labor contract status and weekly working hours. (3) Health behaviors: smoking in the past month and frequent drinking (≥3 times/week). (4) Socioeconomic status: self-rated local income level. Variable descriptions are provided in Table 1.
3 Methods
3.1 Benchmark regression model
In this study, data were cleaned and analysed using Stata 17.0 software. Since the explanatory variable (dp) is an 8–12 ordered variable, this paper uses an ordered logit model rather than OLS (Ordinary Least Squares) to evaluate the link between the explained variable (dp) and the explanatory variable (chr) (37–39). Benchmark regression model is shown below:
Where denotes an individual, denotes a province, and denotes an occupation; dp is an explanatory variable representing an individual’s level of depression; chr is a dummy variable for chronic; represents control variables including individual characteristics, job characteristics, health behavior, biomedical status, and socioeconomic prositioning; is a dummy variable for an occupation; and is a random error term.
3.2 Mechanism model
To examine how chronic diseases influence depressive symptoms through psychosocial factors, we employed the following mechanistic model for regression analysis.
Equation 1 first examines whether chronic has an effect on mechanism variables, Equation 2 further examines the role of mechanism variables on depressive symptoms, and finally Equation 3 is designed to examine whether the inclusion of mechanism variables attenuates the effect of chronic diseases on depressive symptoms. Where represents mechanism variables including income satisfaction, job safety satisfaction, and social cognitive capital.
4 Results
4.1 Descriptive statistics
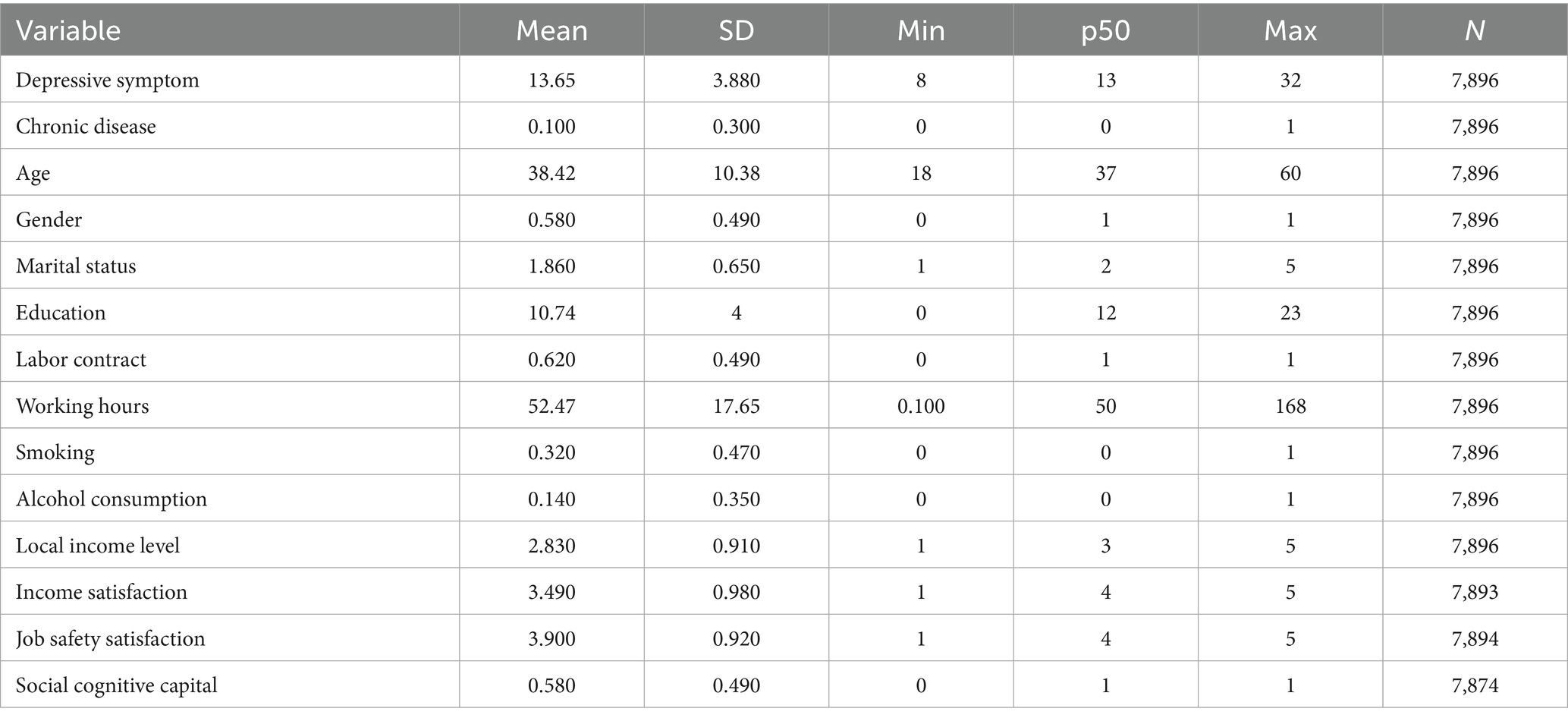
The average score for depressive symptoms was 13.65 (SD = 3.88). This mean indicates that the overall depression level of the sample population falls below the theoretical median (20 points), presenting an overall characteristic of mild depressive tendencies. The core independent variable—chronic disease (chr)—had a mean of 0.10. This indicates that approximately 10% of workers in the final sample self-reported being diagnosed by a physician with at least one chronic disease within the past 6 months. This proportion underscores chronic disease as a significant public health issue that cannot be overlooked. Regarding demographic characteristics, the sample’s average age was 38.42 years (SD = 10.38), indicating a predominantly young-to-middle-aged population. Gender distribution showed 58% males and 42% females. The mean marital status score of 1.86 corresponded to the “married” category in the classification variable, suggesting most individuals in the sample were in marital relationships. The average years of education (edu) was 10.74 years, roughly equivalent to a high school diploma, reflecting that the proportion of individuals with higher education qualifications in China may still be relatively limited. Regarding work characteristics, the average weekly working hours reached 52.47 h, far exceeding the national statutory 40-h standard workweek, clearly revealing the widespread phenomenon of “overwork” among the sample. This aligns with the work culture prevalent in certain industries during China’s current rapid economic development phase. Concurrently, only 62% of workers have signed labor contracts (LC mean = 0.62), indicating that a proportion of the labor market remains informal. The instability and lack of safeguards in such employment may pose threats to mental health. Regarding health behaviors, 32% of respondents reported smoking within the past month (smok), while 14% consumed alcohol more than three times weekly (drink). These behaviors themselves may serve as negative coping strategies for psychological stress, forming a complex bidirectional relationship with depressive symptoms. The mean subjective assessment of local income level (sincome) was 2.83, indicating a moderately low level. Meanwhile, the mean scores for income satisfaction (inc) and job safety satisfaction (saf) were 3.49 and 3.90, respectively, falling between “average” and “relatively satisfied.” This indicates that workers’ subjective assessments of their economic circumstances and job stability are generally neutral to positive. Crucially, social cognitive capital (ren), or generalized trust, showed that 58% of the sample tended to trust others. This proportion serves as a key indicator of social capital levels, with higher trust typically associated with better social integration and psychological well-being.
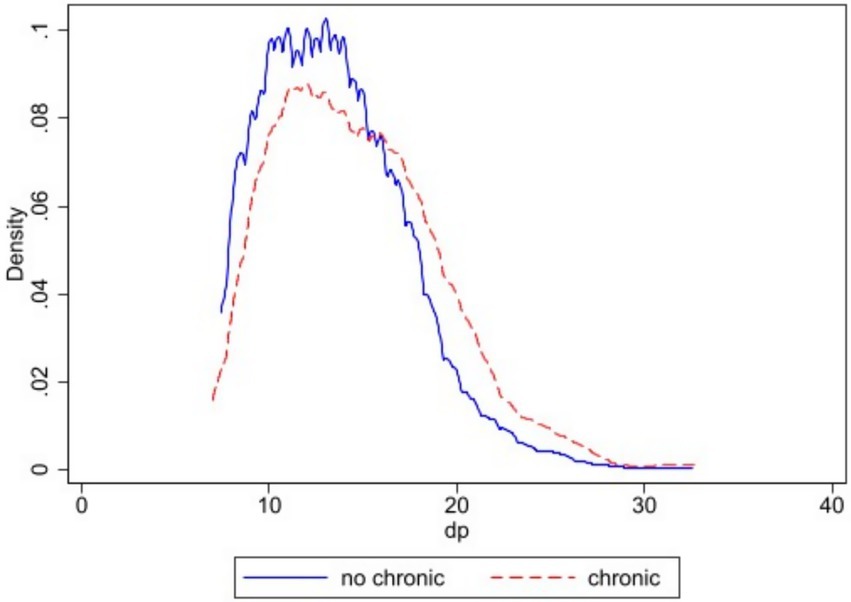
Figure 2 uses kernel density estimation (KDE) curves to compare the distribution of depressive symptoms scores between participants, employing a nonparametric approach. The figure clearly shows a significant distributional shift between the two density curves. The depression score density curve for the non-chronic disease group is overall shifted to the left of the coordinate axes, i.e., toward the lower score range. Its peak is higher and the curve steeper, indicating that depression scores within this group are more concentrated. Most individuals in this group exhibit relatively good mental health, with depression scores clustered in the lower range. In contrast, the density curve for the chronic disease group is markedly shifted to the right, with distribution skewed toward higher score regions. This curve exhibits a lower peak and a flatter, rightward-extending tail, revealing two key characteristics: First, depression scores within this group are less concentrated, indicating greater individual variation; Second, a substantial proportion of individuals fall into higher score ranges, indicating a significantly higher proportion of individuals at risk of moderate to severe depressive symptoms within the chronic disease patient group. Furthermore, the long tail on the right side of the curve signifies the presence of a non-negligible “high-risk” tail group within this cohort. These individuals exhibit particularly severe depressive symptoms and represent a population requiring focused attention and intervention (Table 2).
4.2 Depressive symptoms and chronic diseases
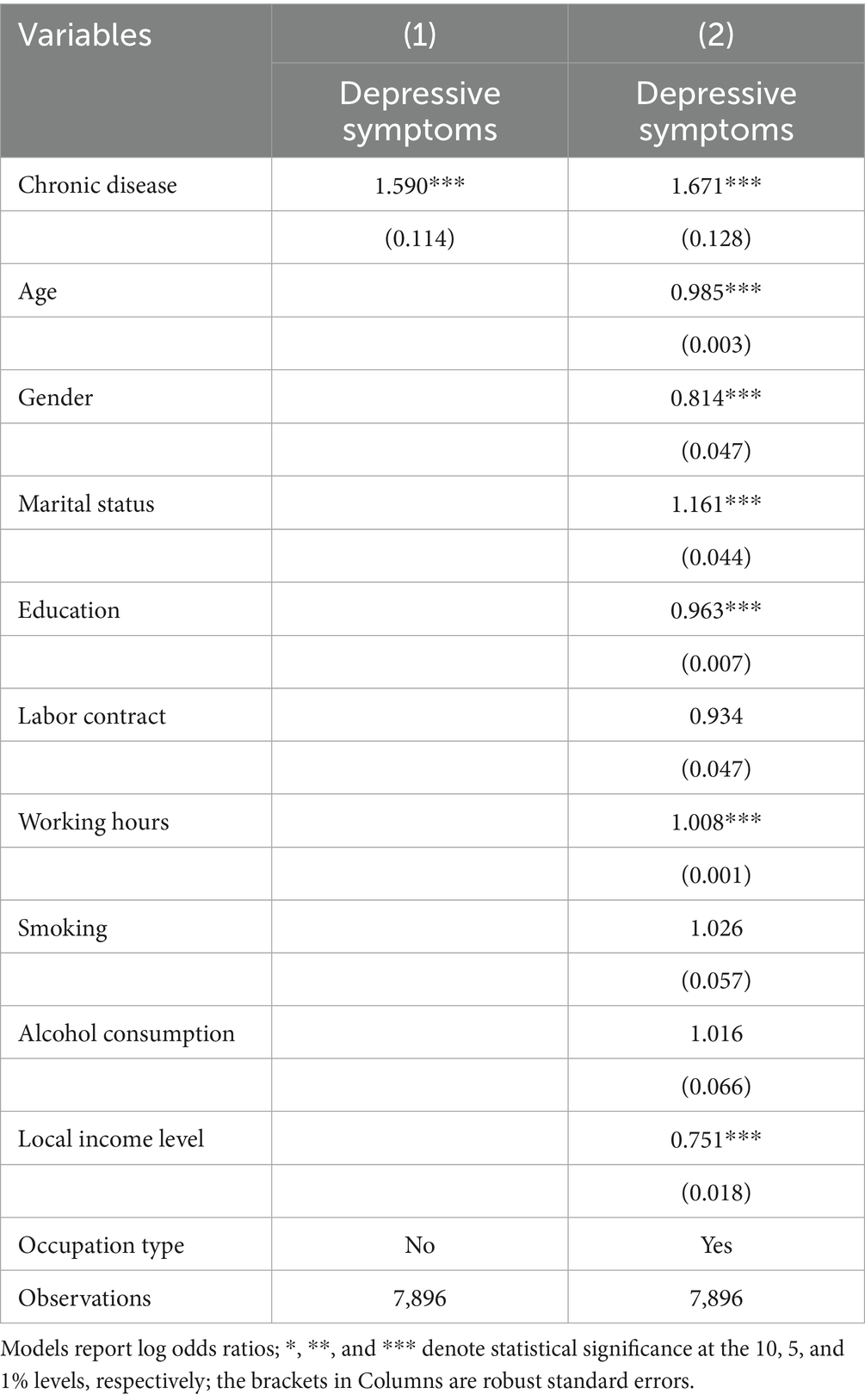
Table 3 reveals a positive association between chronic diseases and depressive symptoms in the baseline regression analysis. In the model without control variables, patients with chronic illness were significantly more depressive than those without chronic illness (OR = 1.590, p < 0.01). After the introduction of a range of control variables, the positive effect of chronic illness on depressive symptoms remained significant, with the OR rising to 1.671 and significant at the 1% level, suggesting that patients with chronic illness had a risk of depression that was approximately 67.1% higher than non-patients.
Among the control variables, age exhibited a negative association with depression (OR = 0.985, p < 0.01), indicating a slight decline in depressive symptoms with age; for gender, males were less depressive compared to females (OR = 0.814, p < 0.01); and higher levels of education were associated with lower depressive symptoms (OR = 0.963, p < 0.01), indicating a psychoprotective effect of education. Local income ratings correlated negatively with depression (OR = 0.751, p < 0.01).
4.3 Robustness test
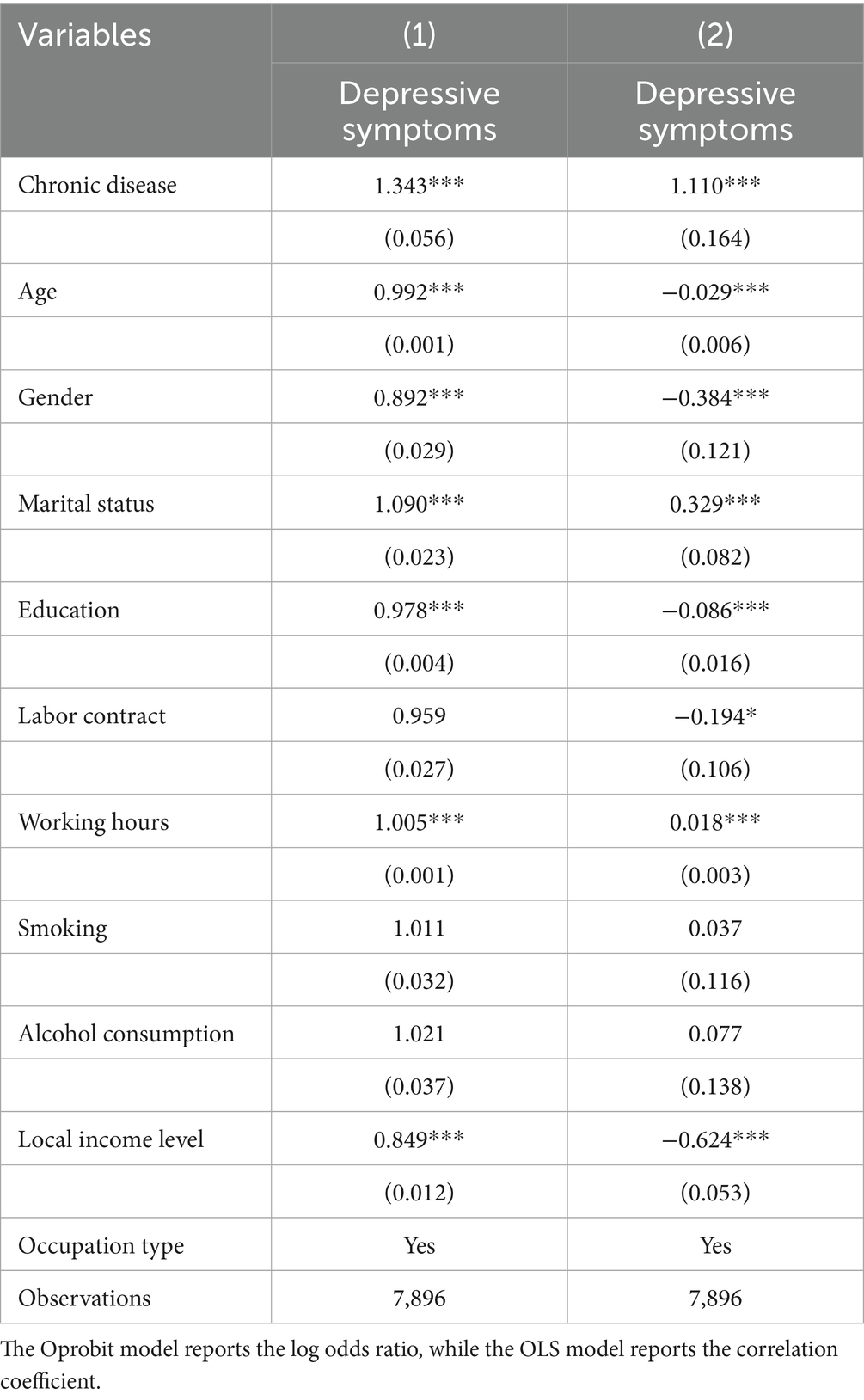
First, both the ordered Probit and benchmark ordered Logit models fall under Generalized Ordered Response Models (GORMs). Structurally isomorphic, they are suited for ordered categorical dependent variables. Their key difference lies in the assumption regarding the random error term’s distribution: Logit uses a logistic distribution, while Probit assumes a standard normal distribution. Although parameter estimates are generally incomparable due to differing distribution scales, the direction and statistical significance of variable effects should be consistent. Thus, applying the Ordered Probit model serves as a sensitivity analysis concerning distributional assumptions. As displayed in Column 1 of Table 4, the coefficient of chronic diseases remains significantly positive at the 1% level, which confirms the robustness of the findings under different distributional assumptions.
Second, the depression score—ranging broadly and evenly from 8 to 32—can be treated as an approximately continuous variable (40). Although the OLS model ignores the ordinal nature of the dependent variable, potentially introducing measurement error, its estimation results still serve as an important reference benchmark. If the significance of core variables remains consistent across different model specifications, interference from the dependent variable’s measurement scale on the conclusions can be largely ruled out. As illustrated in Column 2 of Table 4, the coefficient for chronic diseases remained statistically significant at the 1% level, indicating a consistent positive association with depressive symptoms across different model specifications.
Furthermore, the estimated results for control variables in both models showed high consistency with the benchmark model. The direction and significance of coefficients for variables such as age, gender, education, and working hours remained largely unchanged, indicating that model specification had minimal impact on the results and that the estimates were robust.
4.4 Mechanism test results
4.4.1 Income satisfaction
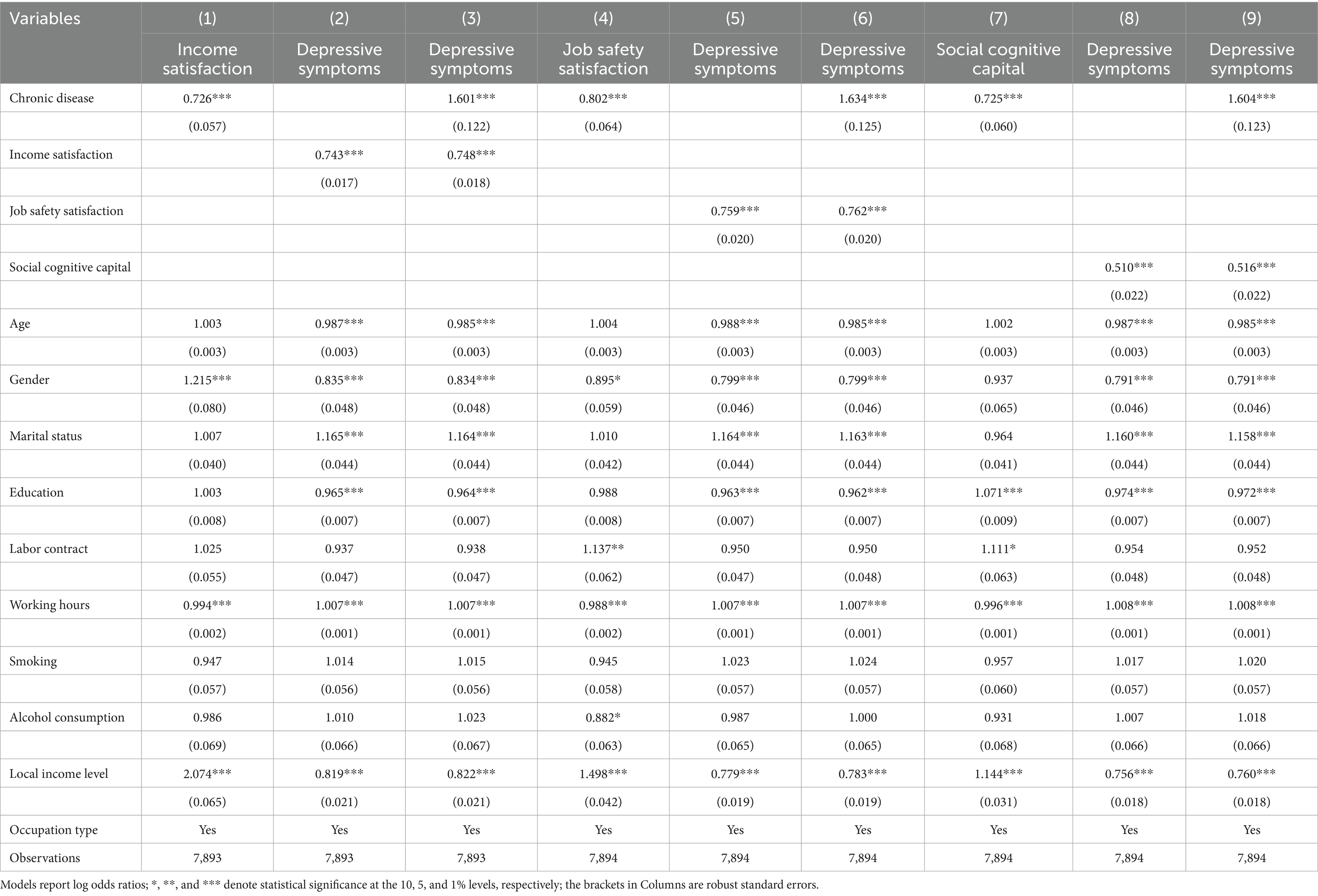
Column 1 of Table 5 indicates that chr exert a negative impact on inc (OR = 0.726, p < 0.01). This finding supports theoretical expectations that chronic diseases often impose substantial economic pressures on patients through increased healthcare expenditures, reduced labor force participation, decreased working hours, or impaired work efficiency, thereby diminishing their income satisfaction. Further analysis reveals that income satisfaction itself exerts a negative influence on depressive symptoms (OR = 0.743, p < 0.01). Specifically, a one-unit increase in income satisfaction reduces the odds ratio for elevated depressive symptoms by approximately 25.7%.
More importantly, after simultaneously incorporating chronic disease and income satisfaction variables, the odds ratio for chronic disease affecting depressive symptoms decreased from 1.671 to 1.601 while remaining statistically significant. This implies that chronic diseases directly adversely affect mental health while also indirectly exacerbating depression by diminishing patients’ satisfaction with their income status.
4.4.2 Job safety satisfaction
The findings in Column 4 of Table 5 suggest that chronic diseases exert a significant negative impact on job safety satisfaction (OR = 0.802, p < 0.01), suggesting that chronic conditions markedly reduce individuals’ satisfaction with workplace safety conditions. Further analysis indicates that job safety satisfaction itself has an independent negative effect on depressive symptoms (OR = 0.759, p < 0.01).
After controlling for both chronic disease and job safety satisfaction variables, the direct effect coefficient of chr on dp decreased from 1.671 in the baseline model to 1.634 (p < 0.01). Chronic disease not only directly exacerbates depressive symptoms but also indirectly impacts mental health by reducing patients’ subjective evaluations of workplace physical safety.
4.4.3 Cognitive social capital
Column 7 of Table 5 indicates that chronic illness exerts a significant negative impact on social cognitive capital (OR = 0.725, p < 0.01). The disease state markedly reduces individuals’ fundamental trust in others and society. This effect likely stems from the chronic pain, functional limitations, and stigma associated with chronic illness. These factors collectively reduce patients’ social participation, diminish the quality of interpersonal interactions, and may even reinforce defensive and distancing tendencies due to experiences of discrimination or misunderstanding, ultimately eroding their sense of universal trust.
Social cognitive capital was also negatively associated with depressive symptoms (OR = 0.510, p < 0.01). Specifically, for each unit increase in an individual’s interpersonal trust level, the odds ratio for experiencing higher-level depression decreased by approximately 49%. After controlling for both chronic disease and interpersonal trust variables, the OR of chronic disease on depressive symptoms significantly decreased from 1.671 to 1.604 (p < 0.01), indicating that social cognitive capital partially mediated the influence pathway from chronic disease to depression. This finding reveals that chronic disease not only directly harms mental health but also indirectly increases depression risk by eroding patients’ trust in others through a social cognitive process.
4.5 Heterogeneity analysis
4.5.1 Gender
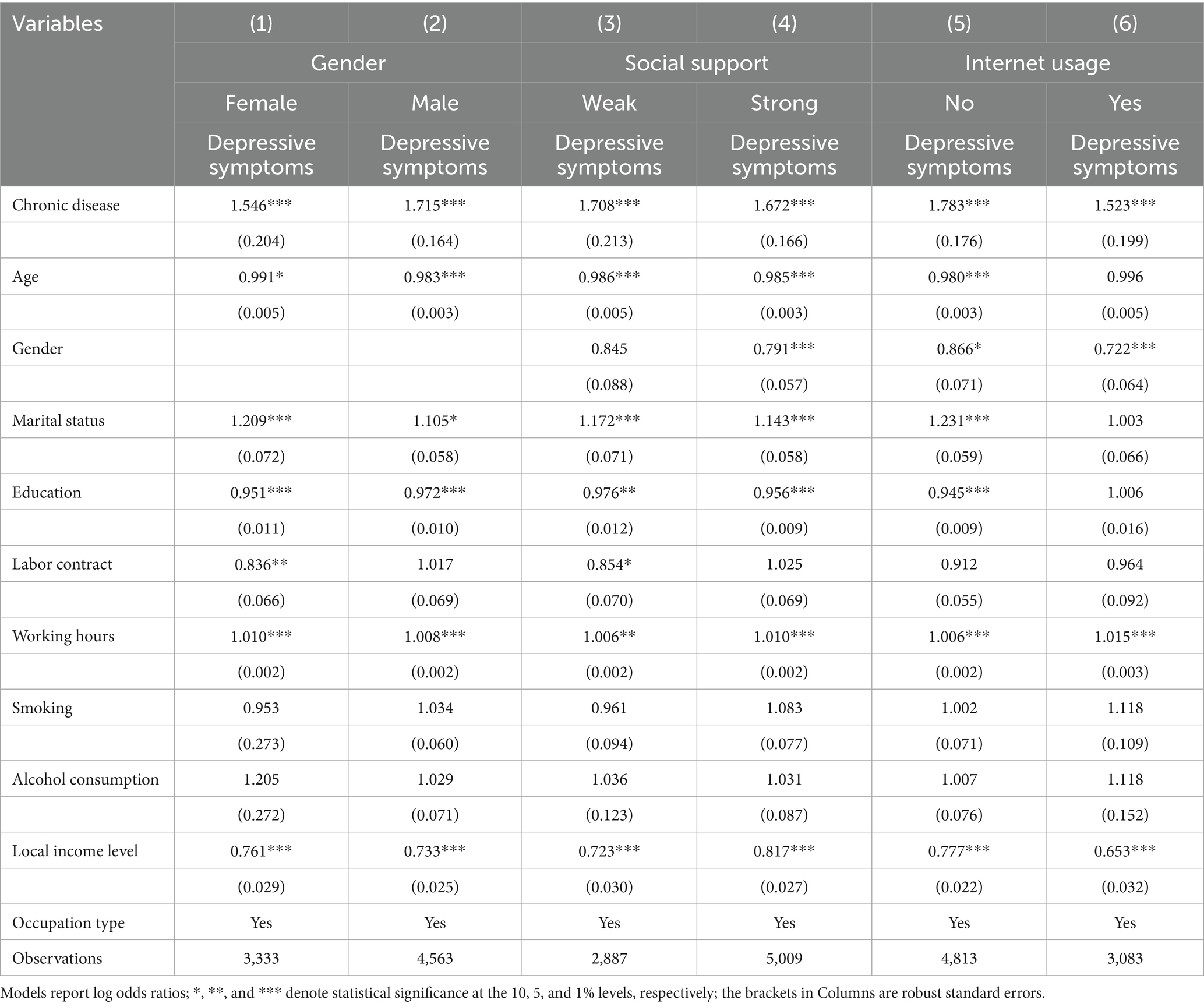
As shown in Columns 1 and 2 of Table 6, chronic diseases significantly increase depressive symptoms in both males and females, although the magnitude of the effect varies. Specifically, among females, the odds ratio for depression among chronic disease patients was 1.546 times higher than among non-patients (OR = 1.546, p < 0.01). Among men, this ratio was even higher, with an odds ratio of 1.715 times (OR = 1.715, p < 0.01). This indicates that while chronic diseases pose a significant threat to mental health for both genders, their negative impact on male depression is slightly greater than on female depression.
4.5.2 Social support
This study measured social support using the single-item indicator “quality of personal relationships.” This binary variable was created by coding respondents as 1 if their unprocessed scores exceeded 6 (signifying greater support) and 0 otherwise (denoting lesser support). As illustrated in columns 3 and 4 of Table 6, chronic disease exerted a statistically significant positive impact on depressive symptoms across both social support subgroups, albeit with marked differences in the magnitude of this effect. In particular, within the group of people with limited social support, the likelihood of depression in those with chronic conditions was 1.708 times greater than in non-patients (OR = 1.708, p < 0.01). In contrast, among those with stronger social support, this incidence ratio was 1.672 times higher (OR = 1.672, p < 0.01).
4.5.3 Internet usage
Internet usage, as a vital channel for information access and social participation in modern society, is increasingly recognized for its role in chronic disease management and mental health maintenance. This research classifies participants into two groups according to their answers to the question “Have you ever used the internet?”: internet users (coded as 1) and non-users (coded as 0). Among non-internet users, the odds ratio (OR) for depression occurrence among chronic disease patients was 1.783 times higher than among non-patients (OR = 1.783, p < 0.01). Among internet users, this OR decreased to 1.523 times higher (OR = 1.523, p < 0.01). These findings indicate that while chronic diseases significantly increase depression risk across all populations, their psychological impact is more severe among non-internet users.
5 Discussion
Using data from the 2022 China Family Panel Studies (CFPS), this research examined the association between chronic illnesses and depressive symptoms, as well as the underlying psychosocial mechanisms. Findings indicate that chronic diseases significantly elevate individuals’ risk of depression, a result that remains robust after controlling for a series of confounding variables and adjusting model specifications. More importantly, this study reveals three mediating pathways through which chronic diseases influence depressive symptoms: income satisfaction, job safety satisfaction, and social cognitive capital. Significant heterogeneous effects were also identified across different genders, levels of social support, and internet usage groups. The following sections provide a comprehensive discussion of these key findings.
First, this study found that individuals with chronic illnesses exhibit significantly higher depression risk than those without chronic conditions, consistent with existing research findings (4, 10, 11). This study further proposes and validates three influence pathways from a psychosocial perspective: financial stress exacerbates depression by reducing income satisfaction (41); occupational insecurity, increases depression risk by diminishing job safety satisfaction (42); and social isolation coupled with lack of trust indirectly causes emotional problems by damaging social cognitive capital (43).
Second, mechanism analysis indicated that income satisfaction, job safety satisfaction, and social trust partially mediated the association between chronic illnesses and depressive symptoms. Chronic disease patients, facing increased medical expenses and diminished work capacity, are more prone to dissatisfaction with their economic circumstances, which in turn triggers anxiety and depression (44, 45). Simultaneously, the threat chronic illness poses to employment stability significantly reduces patients’ job safety. This insecurity, is particularly amplified in China’s labor market, where long working hours and informal employment are prevalent (average weekly work hours: 52.47; only 62% of workers have formal contracts). Furthermore, chronic illness often leads to reduced social participation, “sickness stigma,” and diminished interpersonal trust, further diminishing social cognitive capital and thereby heightening depression risk (46). These three pathways collectively form a psychosocial transmission network, revealing the complex mechanisms through which chronic illness impacts mental health.
Heterogeneity analysis indicates that male chronic disease patients face a higher risk of depression than females (47), potentially linked to traditional cultural expectations of men as “breadwinners” and their emotional expression patterns. Among individuals with weaker social support networks, chronic diseases exert a more pronounced impact on depression, underscoring social support as a crucial buffer against the psychological toll of illness (48). As a vital psychosocial resource, social support offers multifaceted protection when individuals face health-related stress: First, at the emotional support level, care, understanding, and outlets for emotional expression from friends and family help alleviate negative emotions stemming from illness (49); Second, at the instrumental support level, practical assistance (such as accompanying patients to medical appointments or providing financial aid) alleviates tangible difficulties (50). Finally, at the informational support level, access to disease management knowledge and medical advice enhances patients’ sense of control (51). For those with weaker social support networks, the absence of these protective factors forces them to cope alone with the physical, mental, and financial burdens of chronic illness, leading to heightened depression risk (52). Notably, internet usage demonstrated a significant protective effect: chronic disease patients who used the internet exhibited markedly lower depression risk than non-users. The internet provides patients with channels for information access, social connection, and psychological adjustment, partially compensating for deficiencies in offline social support (53). Internet use may mitigate chronic diseases’ negative effects on mental health through multiple mechanisms. To begin with, it offers easy access to information, allowing patients to gain a better grasp of disease-related knowledge, treatment approaches, and self-management techniques—thereby boosting their sense of control and self-efficacy (54). Second, online platforms—such as social media, health forums, and support groups—offer spaces for social support and emotional exchange, helping alleviate loneliness and stigma associated with illness while promoting psychological adaptation (55). Additionally, the internet provides abundant recreational resources and online services (e.g., telemedicine, mental health courses) that help patients divert attention, relieve stress, and improve emotional well-being (56).
Several limitations are associated with this study. First, the depressive symptoms are self-reported, potentially introducing common method bias. Second, the data failed to identify the specific purpose of Internet use, making it difficult to completely rule out its negative effect of exacerbating the risk of depression, such as amplifying fear of illness through online information. Future research is necessary to differentiate between different types of Internet use in order to more fully assess their impact. Third, the findings of this paper need to be treated with more caution as the data used in this paper are cross-sectional and it is not possible to establish that there is a causal relationship between the variables.
Despite these limitations, the study offers both theoretical and practical value. The study integrates social psychology and health economics to propose a multiple mediation framework. Practically, this paper recommends greater attention to patients’ psychosocial needs in chronic disease management. This involves establishing a multidimensional mental health promotion system through enhanced economic security, strengthened employment support, increased social participation, and expanded healthy internet usage. Particularly in the digital age, governments and healthcare institutions can collaborate to develop online support platforms for chronic disease patients. These platforms ought to offer information, counseling, and community-based services to enhance psychological well-being and disrupt the illness-depression vicious cycle.
6 Conclusion
This study analyzes how chronic diseases affect depressive symptoms and underlying psychosocial mechanisms, using data from the 2022 China Family Panel Studies (CFPS). Findings indicate that chronic diseases significantly elevate workers’ risk of depression, with affected individuals exhibiting approximately 1.67 times higher incidence rates than non-affected counterparts. This result remains robust after controlling for multiple confounding variables and adjusting model specifications, confirming chronic diseases as a key predictor of depressive symptoms.
Further mechanistic analysis revealed that chronic diseases indirectly influence depressive symptoms through three psychosocial pathways: income satisfaction, job safety satisfaction, and social cognitive capital all partially mediate this relationship. Chronic diseases exacerbate depressive symptoms by intensifying economic pressures, weakening perceptions of job safety, and reducing interpersonal trust levels. Heterogeneity analysis reveals that the effect of chronic diseases on depression is stronger among males, individuals with low social support, and those lacking internet access. These findings highlight the importance of gender roles, social support networks, and digital resources in mitigating illness-related psychological distress.
This research broadens the understanding of chronic disease-depression comorbidity through a psychosocial lens. It underscores the importance of economic safety, improved work environments, rebuilding social trust, and internet-based health applications in chronic disease management. Future policy development should prioritize multidimensional psychosocial support, particularly in the digital context. By integrating online and offline resources, a more comprehensive mental health promotion system for chronic disease patients can be established. This approach will effectively break the vicious cycle of “disease-depression,” thereby enhancing patients’ quality of life.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://opendata.pku.edu.cn/dataverse/CFPS.
Ethics statement
The studies involving humans were approved by Institutional Review Board (or Ethics Committee) of Peking University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
QX: Data curation, Resources, Visualization, Writing – original draft. RS: Conceptualization, Data curation, Methodology, Writing – original draft. XJ: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the Province Social Science Fund of Shandong, grant number 25CRKJ02.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^According to Article 15 of the Labor Law of the People’s Republic of China, there is a prohibition against employers employing adults under 16 years of age. This paper chooses a sample of 18 years of age or older because workers who are 16 years of age or older, but under the age of 18, are considered to be ‘underage workers’ and enjoy special protection. In addition, China’s delayed retirement policy, which will take effect from 1 January 2025, will not affect the legal working age during the sample period.
References
1. Wojtasik-Bakalarz, K, Woroń, J, Siwek, M, and Krupa, AJ. Patient with pain and depression – practical therapeutic implications. ResearchGate. (2025) 22:33–41. doi: 10.5604/01.3001.0015.4555
2. Yang, C-M, Sung, F-C, Mou, C-H, Liao, C-H, Wang, P-H, and Shieh, S-H. Anxiety and depression risk in Taiwan women with breast cancer and cervical cancer. Front Oncol. (2022) 12:946029. doi: 10.3389/fonc.2022.946029
3. Ojagbemi, A, Akpa, O, Elugbadebo, F, Owolabi, M, and Ovbiagele, B. Depression after stroke in sub-Saharan Africa: a systematic review and Meta-analysis. Behav Neurol. (2017) 2017:1–9. doi: 10.1155/2017/4160259
4. Olvera, RL, Fisher-Hoch, SP, Williamson, DE, Vatcheva, KP, and McCormick, JB. Depression in Mexican Americans with diagnosed and undiagnosed diabetes. Psychol Med. (2016) 46:637–46. doi: 10.1017/S0033291715002160
5. Chang, WH, Foster, GR, Kelly, DA, and Lai, AG. Depression, anxiety, substance misuse and self-harm in children and young people with rare chronic liver disease. BJPsych Open. (2022) 8:e146. doi: 10.1192/bjo.2022.550
6. Read, JR, Sharpe, L, Modini, M, and Dear, BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disord. (2017) 221:36–46. doi: 10.1016/j.jad.2017.06.009
7. Xiao, T, Qiu, H, Chen, Y, Zhou, X, Wu, K, Ruan, X, et al. Prevalence of anxiety and depression symptoms and their associated factors in mild COPD patients from community settings, Shanghai, China: a cross-sectional study. BMC Psychiatry. (2018) 18:89. doi: 10.1186/s12888-018-1671-5
8. Zheng, X, Wu, W, and Shen, S. Prospective bidirectional associations between depression and chronic kidney diseases. Sci Rep. (2022) 12:10903. doi: 10.1038/s41598-022-15212-8
9. Bi, Y-H, Pei, J-J, Hao, C, Yao, W, and Wang, H-X. The relationship between chronic diseases and depression in middle-aged and older adults: a 4-year follow-up study from the China health and retirement longitudinal study. J Affect Disord. (2021) 289:160–6. doi: 10.1016/j.jad.2021.04.032
10. Diderichsen, F, and Andersen, I. The syndemics of diabetes and depression in Brazil – an epidemiological analysis. SSM Popul Health. (2019) 7:100318. doi: 10.1016/j.ssmph.2018.11.002
11. Xuan, L, Zhao, Z, Jia, X, Hou, Y, Wang, T, Li, M, et al. Type 2 diabetes is causally associated with depression: a mendelian randomization analysis. Front Med. (2018) 12:678–87. doi: 10.1007/s11684-018-0671-7
12. Yuan, J, Wang, Y, and Liu, Z. Chronic disease and depression among the elderly in China: the mediating role of instrumental activities of daily living and the moderating role of area of residence. Curr Psychol. (2023) 42:27186–93. doi: 10.1007/s12144-022-03782-9
13. Li, A, Rosella, LC, Kurdyak, P, and Wodchis, WP. Depression as a risk factor for physical illness and multimorbidity in a cohort with no prior comorbidity. Can J Psychiatr. (2021) 66:726–36. doi: 10.1177/0706743720974832
14. Huang, C-Q, Dong, B-R, Lu, Z-C, Yue, J-R, and Liu, Q-X. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res Rev. (2010) 9:131–41. doi: 10.1016/j.arr.2009.05.005
15. Ciprandi, G, Schiavetti, I, Rindone, E, and Ricciardolo, FLM. The impact of anxiety and depression on outpatients with asthma. Ann Allergy Asthma Immunol. (2015) 115:408–14. doi: 10.1016/j.anai.2015.08.007
16. Jiang, C, Zhu, F, and Qin, T. Relationships between chronic diseases and depression among middle-aged and elderly people in China: a prospective study from CHARLS. Curr Med Sci. (2020) 40:858–70. doi: 10.1007/s11596-020-2270-5
18. Singh, K, Patel, SA, Biswas, S, Shivashankar, R, Kondal, D, Ajay, VS, et al. Multimorbidity in south Asian adults: prevalence, risk factors and mortality. J Public Health (Oxf). (2019) 41:80–9. doi: 10.1093/pubmed/fdy017
19. Yao, S-S, Meng, X, Cao, G-Y, Huang, Z-T, Chen, Z-S, Han, L, et al. Associations between multimorbidity and physical performance in older Chinese adults. Int J Environ Res Public Health. (2020) 17:4546. doi: 10.3390/ijerph17124546
20. Khera, R, Valero-Elizondo, J, and Nasir, K. Financial toxicity in atherosclerotic cardiovascular disease in the United States: current state and future directions. J Am Heart Assoc. (2020) 9:e017793. doi: 10.1161/JAHA.120.017793
21. Zhou, M, Wang, H, Zeng, X, Yin, P, Zhu, J, Chen, W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
22. Ren, X, Yu, S, Dong, W, Yin, P, Xu, X, and Zhou, M. Burden of depression in China, 1990-2017: findings from the global burden of disease study 2017. J Affect Disord. (2020) 268:95–101. doi: 10.1016/j.jad.2020.03.011
23. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
24. Zhou, P, Wang, S, Yan, Y, Lu, Q, Pei, J, Guo, W, et al. Association between chronic diseases and depression in the middle-aged and older adult Chinese population-a seven-year follow-up study based on CHARLS. Front Public Health. (2023) 11:1176669. doi: 10.3389/fpubh.2023.1176669
25. Zhang, Y, Wang, Y, Fan, X, He, Y, Li, R, Cheng, X, et al. American Heart Association’s new “life’s essential 8” score and depression in adults with chronic diseases and comorbidity: NHANES, 2007 through 2018. J Psychiatr Res. (2025) 181:188–96. doi: 10.1016/j.jpsychires.2024.11.061
26. Ambe, DA, Voshaar, RCO, Marijnissen, RM, de Kam, H, Rius-Ottenheim, N, Kok, AAL, et al. Interaction of chronic diseases and levels of mastery on the course of depression. J Psychosom Res. (2025) 189:112000. doi: 10.1016/j.jpsychores.2024.112000
27. Yue, L, and Yao, H. Mitochondrial dysfunction in inflammatory responses and cellular senescence: pathogenesis and pharmacological targets for chronic lung diseases. Br J Pharmacol. (2016) 173:2305–18. doi: 10.1111/bph.13518
28. Navarro-Ledesma, S. Frozen shoulder as a metabolic and immune disorder: potential roles of leptin resistance, JAK-STAT dysregulation, and fibrosis. J Clin Med. (2025) 14:1780. doi: 10.3390/jcm14051780
29. Boelhouwer, IG, Vermeer, W, and van Vuuren, T. Work ability, burnout complaints, and work engagement among employees with chronic diseases: job resources as targets for intervention? Front Psychol. (2020) 11:1805. doi: 10.3389/fpsyg.2020.01805
30. Wang, Z, Fan, Y, Lv, H, Deng, S, Xie, H, Zhang, L, et al. The gap between self-rated health information literacy and internet health information-seeking ability for patients with chronic diseases in rural communities: cross-sectional study. J Med Internet Res. (2022) 24:e26308. doi: 10.2196/26308
31. Li, P, Zhang, C, Gao, S, Zhang, Y, Liang, X, Wang, C, et al. Association between daily internet use and incidence of chronic diseases among older adults: prospective cohort study. J Med Internet Res. (2023) 25:e46298. doi: 10.2196/46298
32. Zhou, M, Sun, X, and Huang, L. Chronic disease and medical spending of Chinese elderly in rural region. Int J Qual Health Care. (2021) 33:mzaa142. doi: 10.1093/intqhc/mzaa142
33. Guo, J, Wu, Y, Deng, X, Liu, Z, Chen, L, and Huang, Y. Association between social determinants of health and direct economic burden on middle-aged and elderly individuals living with diabetes in China. PLoS One. (2021) 16:e0250200. doi: 10.1371/journal.pone.0250200
34. Xie, Y, and Hu, J. An introduction to the China family panel studies (CFPS). Chin Sociol Rev. (2014) 47:3–29. doi: 10.2753/CSA2162-0555470101.2014.11082908
35. Radloff, LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
36. Lin, W, Wang, H, Gong, L, Lai, G, Zhao, X, Ding, H, et al. Work stress, family stress, and suicide ideation: a cross-sectional survey among working women in Shenzhen, China. J Affect Disord. (2020) 277:747–54. doi: 10.1016/j.jad.2020.08.081
37. Pengcheng, L, Longfei, Z, Shujuan, C, and Xiaojie, W. Association between household overcrowding and depressive mood among Chinese residents. J Affect Disord. (2021) 290:74–80. doi: 10.1016/j.jad.2021.04.066
38. Cai, Y, Kong, W, Lian, Y, and Jin, X. Depressive symptoms among Chinese informal employees in the digital era. Int J Environ Res Public Health. (2021) 18:5211. doi: 10.3390/ijerph18105211
39. Xu, Q, Wang, L, Zhang, Y, and Jiang, X. On-call work and depressive mood: a cross-sectional survey among rural migrant workers in China. Front Psychol. (2023) 13:1068663. doi: 10.3389/fpsyg.2022.1068663
40. Zhonglin, W, Kit-Tai, H, and Lei, C. A comparison of moderator and mediator and their applications. Acta Psychol Sin. (2005) 37:268. https://journal.psych.ac.cn/acps/EN/Y2005/V37/I02/268
41. Potasova, M, Moraucikova, E, Rusnak, R, Melisova, A, Pilarcikova, S, Sutvajova, M, et al. Associations between prevalence of chronic diseases and socio-economic status in adult population of Slovakia. Bratisl Med J. (2023) 124:383–9. doi: 10.4149/BLL_2023_091
42. Portune, R. Psychosocial risks in the workplace: an increasing challenge for German and international health protection. Arh Hig Rada Toksikol. (2012) 63:123–31. doi: 10.2478/10004-1254-63-2012-2212
43. Li, X, Li, J, Shao, W, Ma, J, Zhou, A, Song, Y, et al. The relationship between family doctor contract services policy and perceived participation in primary health care among chronic disease patients in China: the mediating role of the patient trust. Health Soc Care Community. (2023) 2023:1–11. doi: 10.1155/2023/6854131
44. Coughlin, SS, Datta, B, Berman, A, and Hatzigeorgiou, C. A cross-sectional study of financial distress in persons with multimorbidity. Prev Med Rep. (2021) 23:101464. doi: 10.1016/j.pmedr.2021.101464
45. Becker, N, Scott, JW, Moniz, MH, Carlton, EF, and Ayanian, JZ. Association of chronic disease with patient financial outcomes among commercially insured adults. JAMA Intern Med. (2022) 182:1044–51. doi: 10.1001/jamainternmed.2022.3687
46. O’Brien, ME. Effective social environment and hemodialysis adaptation: a panel analysis. J Health Soc Behav. (1980) 21:360–70. doi: 10.2307/2136412
47. Valdez, LA, Gubrium, AC, Markham, J, Scott, L, Hubert, A, Meyer, J, et al. A culturally and gender responsive stress and chronic disease prevention intervention for low/no-income African American men: the MOCHA moving forward randomized control trial protocol. Contemp Clin Trials. (2021) 101:106240. doi: 10.1016/j.cct.2020.106240
48. Zou, H, Liu, J, Jiang, D, Hou, L, Wang, W, and Zhang, L. The effect of health literacy on disease management self-efficacy in chronic disease patients: the mediating effects of social support and the moderating effects of illness perception. Patient Prefer Adherence. (2024) 18:657–66. doi: 10.2147/PPA.S447320
49. Shi, Y, Liang, Z, Zhang, Y, Zhou, Y, Dong, S, Li, J, et al. Latent profiles of psychological resilience in patients with chronic disease and their association with social support and activities of daily living. BMC Psychol. (2025) 13:792. doi: 10.1186/s40359-025-03115-y
50. Okoro, RN. Cushioning the economic burden of chronic kidney disease for patients in LMICs: the heightened need for a government-driven financial support policy. Health Policy Technol. (2021) 10:100507. doi: 10.1016/j.hlpt.2021.100507
51. Walters, JAE, Courtney-Pratt, H, Cameron-Tucker, H, Nelson, M, Robinson, A, Scott, J, et al. Engaging general practice nurses in chronic disease self-management support in Australia: insights from a controlled trial in chronic obstructive pulmonary disease. Aust J Prim Health. (2012) 18:74–9. doi: 10.1071/PY10072
52. Bouchard, V, Robitaille, A, Perreault, S, Cyr, M-C, Tardif, J-C, Busseuil, D, et al. Psychological distress, social support, and use of outpatient care among adult men and women with coronary artery disease or other non-cardiovascular chronic disease. J Psychosom Res. (2023) 165:111131. doi: 10.1016/j.jpsychores.2022.111131
53. Chen, K-C, Liu, S, Lin, M-P, Lee, Y-T, Wu, JY-W, Lin, C-A, et al. A moderated mediation model of the relationship between depression and internet addiction: mediation by refusal self-efficacy of internet use and moderation by online and real-life social support. Int J Ment Health Addict. (2024) 22:1649–61. doi: 10.1007/s11469-022-00949-0
54. Pereira, V, Hadjielias, E, Christofi, M, and Vrontis, D. A systematic literature review on the impact of artificial intelligence on workplace outcomes: a multi-process perspective. Hum Resour Manage Rev. (2023) 33:100857. doi: 10.1016/j.hrmr.2021.100857
55. Bold, E, Richardson, KL, Al-Uzri, A, Craven, SF, Clark, K, Grzesek, K, et al. Internet use and health literacy among pediatric chronic kidney disease patients and their caregivers. J Nephrol. (2024) 37:2561–8. doi: 10.1007/s40620-024-02136-x
56. Palermo, TM, Dudeney, J, Santanelli, JP, Carletti, A, and Zempsky, WT. Feasibility and acceptability of internet-delivered cognitive Behavioral therapy for chronic pain in adolescents with sickle cell disease and their parents. J Pediatr Hematol Oncol. (2018) 40:122–7. doi: 10.1097/MPH.0000000000001018
Keywords: chronic diseases, depressed symptoms, income satisfaction, job safety satisfaction, social cognitive capital, ordinal logistic model
Citation: Xu Q, Shang R and Jiang X (2025) Chronic diseases and depressive symptoms in China: a psychosocial mechanism perspective. Front. Public Health. 13:1696199. doi: 10.3389/fpubh.2025.1696199
Edited by:
Anna Julia Krupa, Jagiellonian University Medical College, PolandReviewed by:
Giulio Longo, Marche Polytechnic University, ItalyCristiana Tapoi, Prof. Dr. Alexandru Obregia Psychiatry Hospital, Romania
Copyright © 2025 Xu, Shang and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xia Jiang, eGlhamlhbmcwMkBob3RtYWlsLmNvbQ==
 Qingqing Xu
Qingqing Xu Ruizhe Shang
Ruizhe Shang Xia Jiang
Xia Jiang