- 1Department of Inflammation and Ageing, School of Infection, Inflammation and Immunology, College of Medicine and Health, University of Birmingham, Birmingham, United Kingdom
- 2University Hospitals Birmingham NHS Foundations Trust, Birmingham, United Kingdom
- 3Centre for Trauma Sciences Research, University of Birmingham, Birmingham, United Kingdom
- 4Institute for Mental Health, University of Birmingham, Birmingham, United Kingdom
Background: Traumatic brain injury (TBI) has been known to cause physical and psychological dysfunction among patients. Most family members face numerous physical and psychological difficulties in caregiving, yet effective interventions remain limited. This study aims to (a) identify the effects of caregiver interventions on caregiver burden for traumatic brain injury patients, (b) evaluate the effects of these programs on caregivers' psychological distress.
Methods: A systematic search was conducted in Pubmed, Medline and PsycINFO to search for randomized control trials (RCTs) that report the effects of caregiver interventions on care partners of TBI patients above the age of 18. The primary outcome was caregiver burden, which was measured mainly using the Zarit Burden Interview (ZBI). The secondary outcome was psychological distress, with the Brief Symptom Inventory-18 (BSI-18) as the main assessment used. The RoB-2 tool was used to assess the risk of bias.
Results: Thirteen RCTs were identified after screening. Meta-analysis of the primary outcome (ZBI) showed significant improvements (p < 0.05) favoring intervention despite high heterogeneity in the 5 studies. Meta-analysis of the secondary outcome (BSI-18) indicated smaller but significant improvement (p = 0.02) with low heterogeneity in 3 studies.
Conclusion: Results suggest that caregiver interventions are effective in improving caregiver burden and psychological distress in the future. However, due to high risk of bias in studies, the conclusion should be interpreted with caution before clinical application. Higher quality research should be conducted to ensure the effectiveness of caregiver programs.
1 Introduction
Traumatic brain injury (TBI) is one of the most common causes of trauma worldwide, affecting 20.8 million people worldwide (1). It causes physical, cognitive, functional and psychological difficulties among individuals with TBI, which makes caregiving challenging as it takes on the form of a chronic disease (2). About 70% of familial caregivers experience significant caregiver burden in the various populations, as most informal caregivers, i.e. family members including a spouse or a parent, are not ready to take up the role of caregiving after trauma hits (3). Studies have shown that caregivers encounter daily struggles in balancing their own needs and those of the person with TBI (4). They often experience psychological distress, changes in daily routines and relationships, physical strain, financial difficulties and shortage of resources, especially for moderate to severe TBI patients (5). Feeling overburdened by daily responsibilities is commonly reported among caregivers, with up to 20% caregivers experiencing significant depressive and somatic symptoms clinically (6). Social isolation also becomes a major challenge as social support is reduced (4). Substantial financial burden adds to caregivers' psychological stress as well (7). Although multiple factors contribute to caregiver burden, resilience could be built as long as caregivers have the perception that their needs are being met (8). Therefore, various caregiver interventions have been developed over the years to offer support to TBI caregivers in different stages of caregiving.
Conceptualisations of caregiver interventions have evolved from a predominantly problem-solving approach to a more strengths based approach during the 1990s to 2010s. Intervention content fell into two main categories: caregiving skills for supporting individuals with TBI and strategies for maintaining caregivers' health and well-being. Early sessions often focused on recognizing the symptoms of TBI, addressing cognitive and behavioral challenges and enhancing communication with the patient. A consistent finding across the literature was that effective programs combined educational information with opportunities for reflection and sharing in supportive environments. Thus structured programs that incorporate both practical skill building and emotional support were found to yield the most positive results (9). In recent decades, caregiver interventions for TBI have evolved from face-to face sessions to include a range of online methods of learning. Reported modalities include mobile health applications with online chat functions, telephone consultations, online problem solving interventions and video support groups aimed at improving accessibility for caregivers in remote areas (10, 11). While there was some controversy regarding the comparability of online and in-person interventions, studies have proved that online interventions can achieve equivalent outcomes when tailored to specific needs (12). For example, the Caregiver Wellness after Traumatic Brain Injury Program (CG-Well) has incorporated interactive games, inspirational quotes, supportive videos and photographs as creative methods of offering emotional support (13). Moreover, flexibility appears to be a recurrent advantage, allowing users to access the content at their own pace (14, 15).
In recent years, researchers have proposed several recommendations for designing personalized programs for caregivers of individuals with TBI, one of which emphasizes the principle of “respecting cultural differences” (16). An increasing trend of TBI caregiver interventions has been spotted over the last few years in middle income countries, such as Mexico, India and Indonesia (10, 17, 18). Another pilot study for Latino American caregivers was conducted to tailor to their needs, improving somatic symptoms and caregiver burden (19). These differences in cultural values can significantly influence how families engage with individuals living with TBI. Although numerous studies have examined the needs of TBI caregivers, there appears to be a notable gap in literature since 2018, when the most recent systematic review was published (20). The review identified methodological limitations in the existing evidence, including the need for more rigorous study designs and the adoption of outcome measures with higher validity and reliability. A separate systematic review on online TBI caregiver interventions further stated that small sample sizes limit the overall generalizability of results (12). Since 2018, several higher quality studies have been published, including interventions targeting different ethnic minorities and employing a range of delivery methods. Hence, the emerging body of research warrants comprehensive analysis to inform clinical thinking and guide the development of rehabilitation programs.
At present, no consensus exists on general guidelines for TBI caregiver interventions, underscoring the need to determine which program characteristics yield the most beneficial outcomes. The aim of this study is to evaluate the effectiveness of TBI caregiver interventions in alleviating caregiver burden and psychological distress through a systematic review and meta-analysis. Intervention effectiveness will be compared against standard hospital care to examine whether recently published randomized controlled trials differ from results in earlier reviews. Caregivers for adult TBI patients were included in the systematic review, excluding those caring for children and adolescents. The primary outcome of this study is caregiver burden while the secondary outcome includes measures of psychological distress, indicating symptoms of depression and anxiety. Both outcome measures were considered to determine whether caregiver programs effectively bring about positive changes in caregiver burden and stress.
2 Methods
2.1 Search strategy
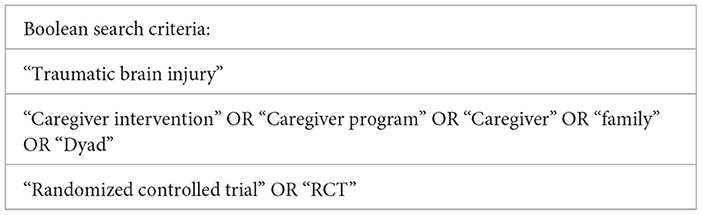
The systematic review was conducted according to the Preferred Reporting of Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (21). The literature search was completed on 22nd April 2025 in three databases, namely Pubmed, MEDLINE and PsycINFO. For search terms, (“traumatic brain injury”) AND (“caregiver intervention” OR “caregiver program” OR “Caregiver” OR “family” OR “Dyad”) AND (“randomized controlled trial” OR “RCT”) were used. Gray literature was also sourced from searches in ProQuest Dissertations and Theses and OpenGrey databases, conference proceedings as well as from scanning the references in previous systematic reviews that included studies of TBI caregiver interventions (20, 22) (Table 1).
2.2 Inclusion and exclusion criteria
Studies were included if the following criteria were met: (1) written in English; (2) the study design is an RCT; (3) described an intervention for TBI caregivers or a program involving both TBI survivors and caregivers, with comparison to a control group; (4) enrolled adult patients as participants; (5) full text was available.
Exclusion criteria of the studies included the following: (1) did not involve caregivers in the study; (2) enrolled adolescents or children as participants (<18 years old); (3) included other brain injury patients as participants; (4) program involving caregivers of adolescents/ children with TBI (<18 years old); (5) full text was unavailable; (6) not an RCT.
Studies involving caregivers of adolescents/children with TBI were excluded as their needs differ from that of adult TBI patients due to anatomical and physiological differences of the brain (23). Papers with studies were not filtered by date to include all studies up to April 2025.
2.3 Data collection
A manual search was conducted on each database, where titles and abstracts were screened to identify suitable articles. Covidence software was used to identify duplicates and track the process of screening (24). Studies were then sought for full text analysis according to the inclusion and exclusion criteria. The initial screening was done by the primary author (CYT) and then reviewed by the co-author (ZA). Any discrepancies were discussed between the two authors and resolved through mutual agreement.
2.4 Data extraction
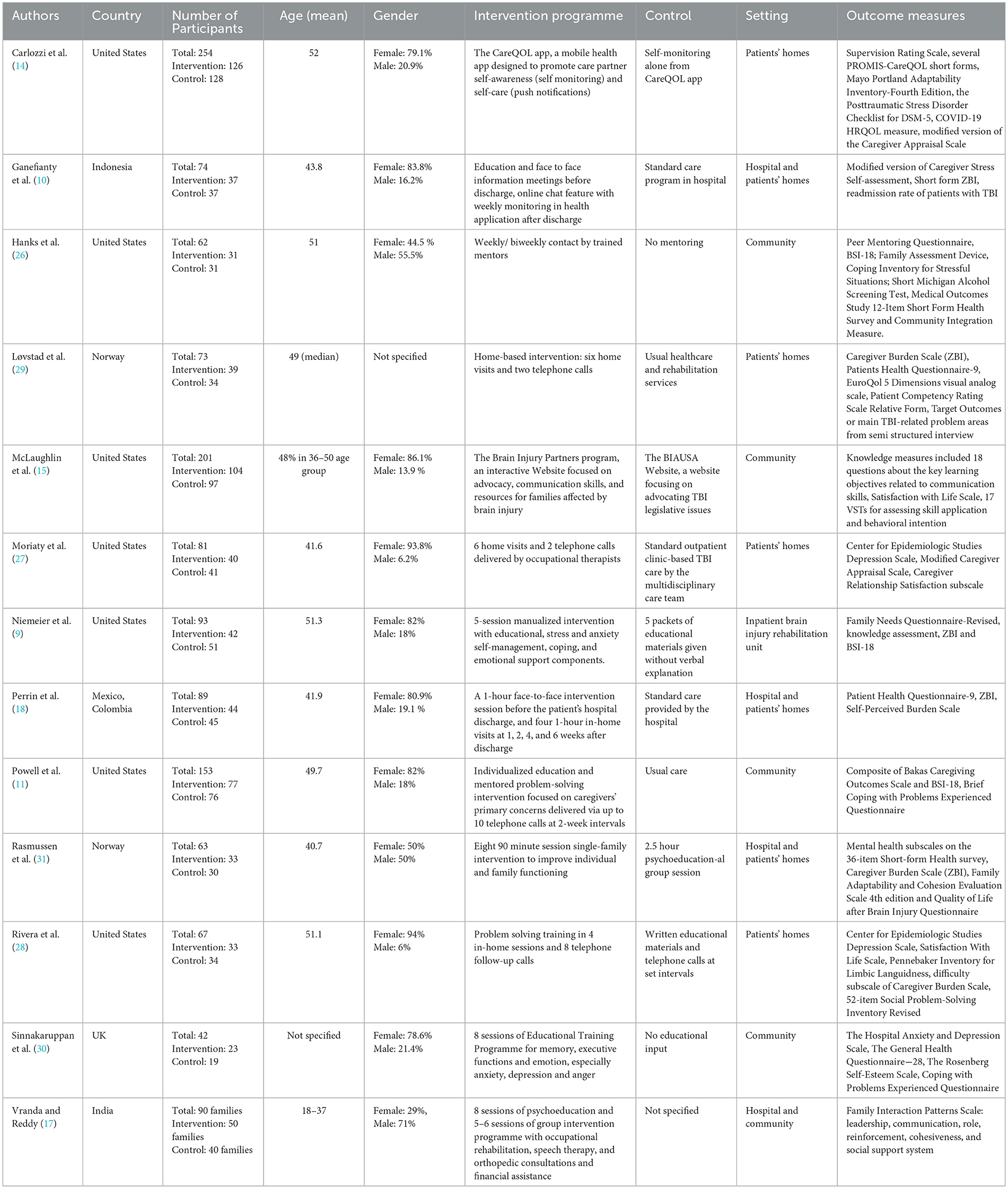
Data was extracted by the primary author (CYT) to a spreadsheet for further analysis. The data was then reviewed by the co-author (ZA) for verification. The characteristics of the studies, characteristics of participants, characteristics of intervention and control groups and their respective outcome measures were extracted (Table 2).
Authorship, the country where the study was conducted and the number of participants in the intervention and control group were included in the characteristics of the studies. The characteristics of participants were also recorded, such as whether they were civilians/ veterans, mean age and the percentage of each gender. In addition to the above data, the mode of delivery of the intervention, intervention programme, control, setting, duration and frequency of intervention, the timepoint which the intervention was conducted during the patient's journey were documented.
Caregiver burden was selected as the primary outcome, which consisted of either the 22 item and 12 item Zarit Burden Interview (ZBI), modified version of the Caregiver Appraisal Scale, Caregiver Burden Scale, Self-Perceived Burden Scale and the Bakas Caregiving Outcomes Scale. The secondary outcome measured psychological and somatic symptoms of caregivers. Four categories of other outcome measures were reported as well, namely overall health and quality of life (QoL), family functioning, TBI patients' assistance level and others. Although follow up data was frequently reported in most studies, only data collected immediately after the intervention was analyzed.
2.5 Risk of bias
Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB-2) was used to assess the quality of the RCTs (25). RoB-2 documents 5 domains of bias, namely bias from the randomization process, deviations from the intended interventions, missing data, measurement of outcomes and selection of the reported results. The two reviewers (CYT and ZA) screened the RCTs independently and rated each domain for low, unclear or high risk of bias across each study. The quality of all studies was then assessed to give an overall risk of bias. Any discrepancies between the assessors were discussed to reach a mutual consensus.
2.6 Statistical analysis
The mean and standard deviation (SD) of ZBI and BSI-18 was extracted from the results of the studies as there was sufficient homogeneity between at least three studies for both assessments. As two studies reported the mean and SD of the average score of ZBI, the data was calculated by the authors to extract the mean and SD of the total score of ZBI. A meta-analysis was conducted using RevMan 4.0 software (Cochrane Collaboration, London, UK) employing a random effects model. The mean difference and the 95% confidence interval were reported with I2, Chi2, and Tau2 to indicate the heterogeneity across studies. Forest plots were also created to show whether the results favored the intervention or the control group. As studies used a variety of outcome measures, outcomes other than ZBI and BSI-18 were analyzed using a narrative synthesis of the data.
3 Results
3.1 Search results
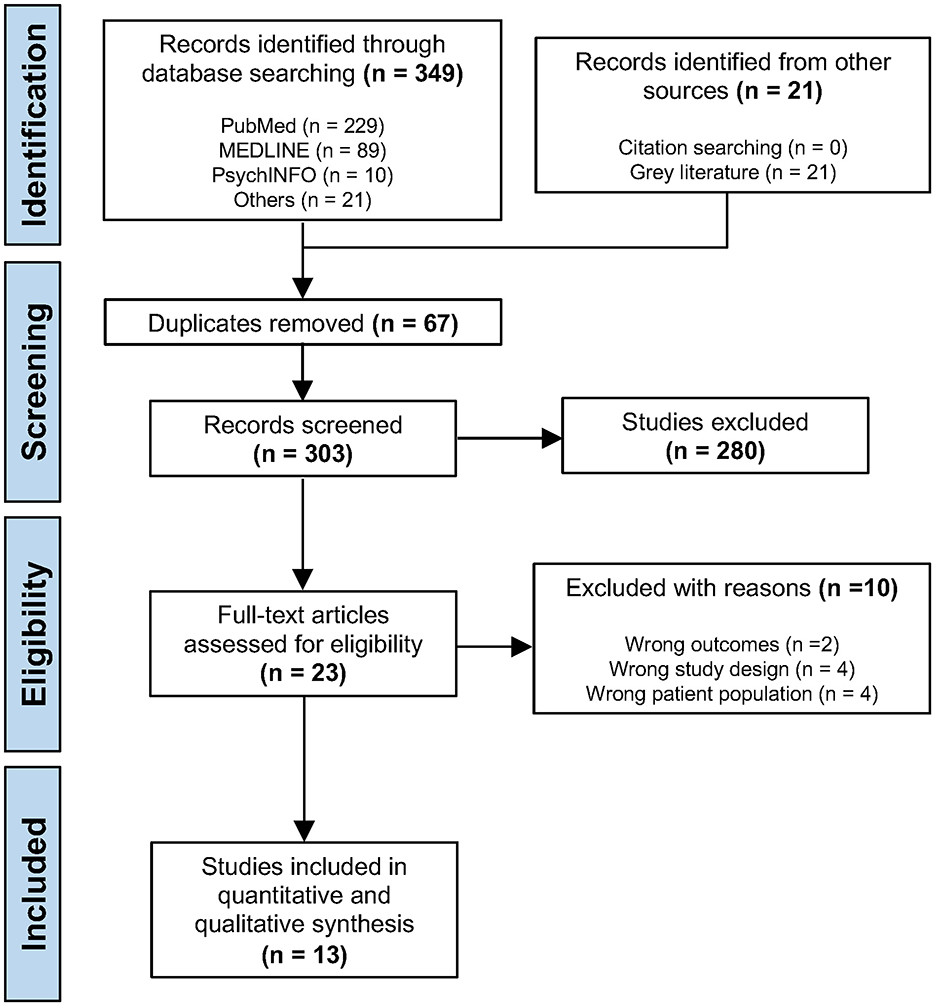
The initial search yielded a total of 370 papers, comprising 349 results from three databases and 21 references from gray literature. 67 references were identified as duplicates by Covidence (https://www.covidence.org/; Melbourne, Victoria, Australia) and were removed. 303 studies were screened according to title and abstract by the primary reviewer (CT), resulting in the exclusion of 280 studies. The remaining 23 full text studies were assessed for eligibility in the second stage of screening. Out of the 10 studies excluded, two were due to having wrong outcomes, four due to wrong study design and four for including the wrong patient population. Ultimately, 13 studies were included for the meta-analysis (Table 2). The entire process was reviewed by the co-author (ZA), including performing independent searches in the same database using the same search strings and the searches and included studies were confirmed by the co-author. The process is summarized in Figure 1 in the form of a PRISMA flowchart.
3.2 Study characteristics
Data extracted from the studies was summarized in Table 2. RCTs were selected to ensure potentially high methodological quality across the studies. The 13 studies were published from 2005 to 2025, encompassing a total of 1,252 participants and 90 families. 629 participants and 50 families took part in the interventions while 623 participants and 40 families took part in the control groups. The majority of studies were conducted in Western countries, with eight studies based in North and South America (9, 11, 14, 15, 18, 26–28), three in Europe (29–31) and two in Asia (10, 17). Caregiver age mostly ranged from 36–52, with only 1 study having younger participants (aged 18–37) (17). Most of the studies had >75 % participants as females (9–11, 14, 15, 18, 27, 28, 30) while three studies had female percentages lower than 50% (17, 26, 31). Most caregivers were at the age of 36–50, except for 1 study (17). The time of injury of TBI patients ranged from acute post-injury to 10 years. One study specifically focused on veterans with TBI while others recorded interventions for civilians.
Interventions differed considerably in program structure, duration and content. The interventions lasted from 10 days to 2 years. Intervention methods involved face to face interactions, remote programs based on web or telephone communication or a combination of both. Six studies had their intervention delivered face to face (9, 17, 18, 26, 30, 31), four had blended approaches (10, 27–29), and three were conducted using remote interventions only (11, 14, 15). The types of remote interventions included mobile health apps with online chat functions, telephone follow up, interactive websites. In contrast, in-person interventions encompassed psychoeducational sessions delivered by medical staff, problem solving training, group intervention programs, individual peer mentoring and home visits. All face to face interventions were conducted in hospitals or in patients' homes. In-person interventions were conducted weekly, or biweekly or once a month, usually spacing out during the end of the treatment. On the other hand, remote interventions tend to allow caregivers higher flexibility in using the medical applications, generally at their own pace. Control groups were either given standard care at the local hospital or written materials without additional explanation from medical staff.
3.3 Risk of bias assessment
The risk of bias-2 tool (RoB-2) was used to assess the quality of the included RCT studies (Figure 2). Most studies had an overall moderate to high level of bias, with seven studies rated as high (9, 15, 17, 18, 27, 29, 30) while six studies had some concerns (10, 11, 14, 26, 28, 31). Due to the nature of the interventions, all studies were not able to blind the participants to their allocated interventions. The staff implementing the programs were also aware of the caregivers' allocated interventions as blinding could not be conducted. Thus all studies had a high risk of bias due to deviations from the intended interventions (D2). Two studies were rated high in bias from the randomization process (D1) as the details of the randomization processes were not specified (17, 18). Six studies had an unclear risk of bias as the randomization process was not described in detail (9, 14, 15, 27, 28, 30). There were three studies rated as high for bias due to missing data (D3) as they had >25% of missing data (9, 18, 27) while five studies raised some concerns due to a 10%−25% attrition rate (11, 14, 15, 26, 30). Most dropouts were lost to follow-up or caregiver withdrawal, raising concerns on the sustained participation and effectiveness of the interventions. There were also concerns related to bias in measurement of outcomes (D4) as most outcome measures were subjectively rated by caregivers themselves. Given the subjective nature of the primary outcome, the potential for measurement bias was notable. Objective measures were typically included as secondary outcomes, such as psychological metrics and vital signs, knowledge in caregiving and health measures for TBI patients. Finally, bias in selection of the reported result (D5) was mostly rated as low to moderate risk of bias without evidence of selective reporting amongst studies.
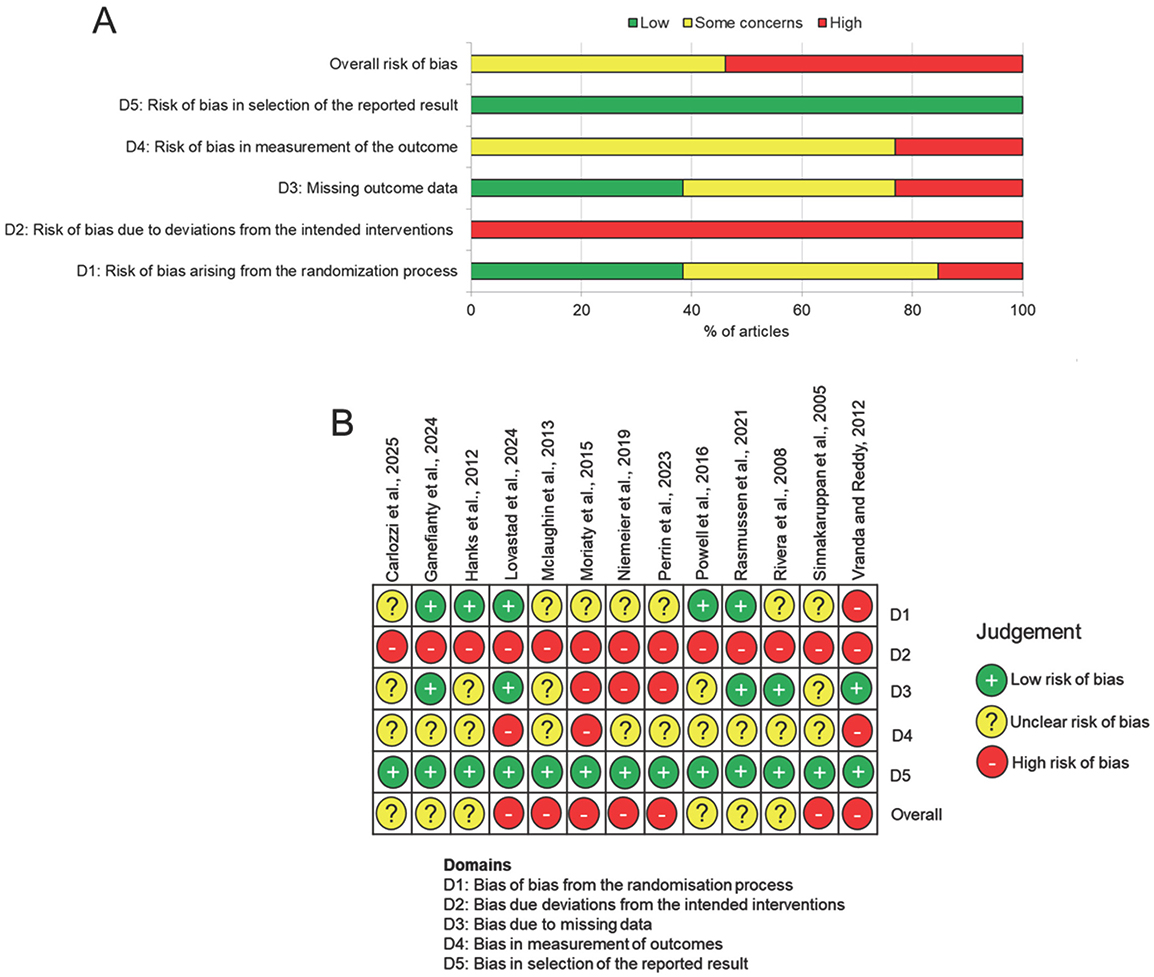
Figure 2. Risk of bias assessment. (A) Summary chart for risk of bias in all studies. (B) Risk of bias in individual studies for each domain.
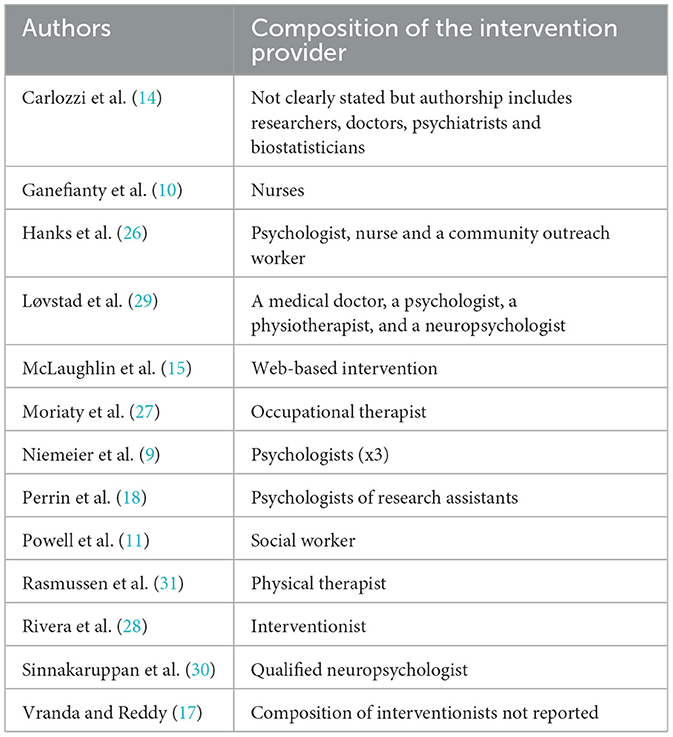
3.4 Composition of the intervention providers
In considering the composition of the team that provided the intervention to the carer's, three studies did not clearly state the qualifications of the interventionists (14, 17, 28), whilst one study was a web-based intervention developed by the Brain Injury Partners (15) (Table 3). However, many studies had one specialist that included a nurse, social worker, psychologist or researcher, occupational therapist of a neuropsychologist (10, 11, 18, 27, 30, 31). Only two studies reported that a multidisciplinary team delivered the interventions, including medical doctors, nurses, community worker, physiotherapist and a neuropsychologist (26, 29). One study reported that a team of three psychologists delivered the intervention (9).
3.5 Outcomes
3.5.1 Primary outcome data: caregiver burden
The primary outcome measures (caregiver burden) were mostly self-reported. Five studies utilized the ZBI (9, 10, 18, 29, 31), one study reported a subscale of the ZBI (28) and two studies used the modified version of Caregiver Appraisal Scale (14, 27). In the five studies, the term “Caregiver Burden Scale” is used interchangeably with “The Zarit Burden Interview”. The ZBI is a self-reported assessment that measures the subjective burden in caregiver experiences, indicating the strain on personal, social and financial aspects of life (32). Caregivers are required to answer 22 items on a 5-point Likert scale of 0–4, where lower scores indicate a lower caregiver burden.
A meta-analysis for studies that reported the ZBI results showed a mean difference of 6.34 favoring the intervention group (p < 0.00001), but with high heterogeneity displayed (I2 = 97%, Chi2 = 158.85). In addition, a high degree of between study variability in effect sizes across studies was reflected. Two out of the five studies reported statistically significant outcomes (10, 18), while the results of the other three studies were non-significant (9, 29, 31). However, an overall positive effect favoring the intervention was detected (Figure 3).
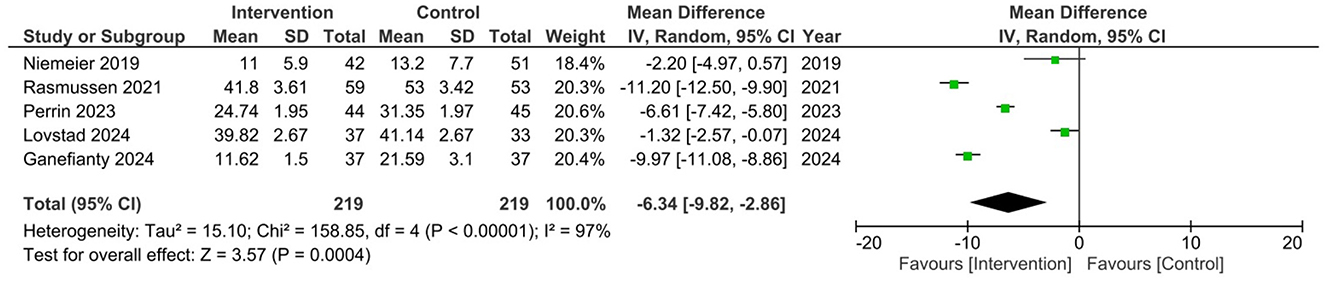
Figure 3. Meta-analysis of primary outcome data for ZBI scores in appropriate studies (9, 10, 18, 29, 31).
3.5.2 Secondary outcome data: psychological symptoms
For psychological symptoms, three studies utilized the BSI-18 (9, 11, 26), two studies used the Center for Epidemiologic Studies Depression Scale (CESD) (27, 28), another two used the Patient Health Questionnaire (PHQ-9) (18, 29) while three others used other assessments (14, 30, 31). The BSI-18 is a 18-item self-reported checklist that assesses the psychological status in patient populations. The global severity index of the BSI-18 reports the results on all 18 items, which could be further divided into three 6 items scales, measuring somatisation, anxiety and depression.
The global severity index of BSI-18 was used to perform a meta-analysis. A mean difference of 2.84 favoring the intervention group was detected, indicating a statistically significant effect (p = 0.02). Low heterogeneity among studies was found (I2 = 0%, Chi2 = 1.27), demonstrating consistent intervention effects in different programs. Although a fixed effect model was appropriate for the statistical analysis, a random effects model was still used as a conservative approach to detect heterogeneity across studies. Two studies reported non-significant results (9, 26) while one study had positive effects on caregivers' mental health (11). However, an overall positive effect favoring the intervention was detected (Figure 4).
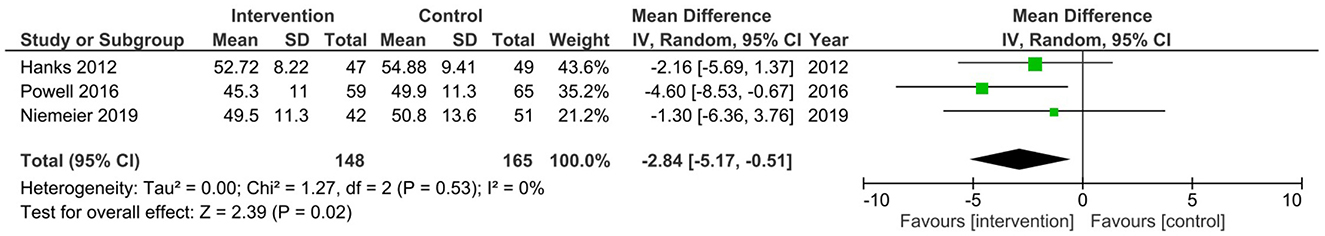
Figure 4. Meta-analysis of secondary outcome data for BSI-18 scores in appropriate studies (9, 11, 26).
Only one study stated that the primary outcome of caregiver burden in male carers was associated with an increased risk of negative outcomes after the intervention (14). However, none of the other studies reported any differences in outcomes when carers were male as opposed to female (9–11, 15, 17, 18, 26–31).
4 Discussion
The primary objective of this study was to determine whether caregiver interventions are effective in reducing caregiver burden and psychological distress. We identified 13 studies that met our inclusion/exclusion criteria, encompassing a total of 1,252 participants and 90 families. Interventions differed considerably in structure, duration and content and lasted for 10 days to 2 years. The risk of bias was judged as moderate to high since some studies were not able to blind allocation of participants to groups due to the nature of the study. The primary outcome measure for caregiver burden was either the Zarit Burden Interview (ZBI) or the Caregiver Burden Scale and a meta-analysis from pooled data from some of the studies evaluated using the ZBI favored the intervention group. The global severity index of BSI-18 was also significant and favored the intervention. These results suggest that caregiver burden is significant and intervention helped reduce this burden significantly. Due to the high risk of bias, however, more high quality studies are required to make definitive conclusions.
Based on the findings of this study, it can be concluded that TBI caregiver interventions are effective in reducing caregiver burden. Nevertheless, the results should be interpreted with caution. The high heterogeneity observed in ZBI results likely reflects real world variations due to differences in population characteristics and intervention types, which enhances the generalizability of the results across diverse settings. Four out of eight studies reported significant reduction in caregiver burden. Of the four studies that reported a significant reduction in caregiver burden, three incorporated psychoeducation and skills training, suggesting that improvements in practical caregiving abilities and knowledge may be essential components of effective interventions (10, 18, 27, 31). Both face-to-face and blended delivery modes appeared effective in reducing caregiver burden. All four studies were conducted in hospital and home settings, with intervention durations ranging from 1 to 4 months. Three studies involved weekly or biweekly contact with caregivers (18, 27, 31) and three studies were implemented during the transition from hospital to patients' homes within 1 year of injury (10, 18, 31). These findings, paired with the meta-analysis result for ZBI, indicate caregiver interventions may lessen caregiver burden significantly. However, the inconsistency of results from the studies complicates the interpretations as overall methodological limitations and small sample sizes reduces certainty of these results. Therefore, while interventions may be beneficial, the variability in study quality requires careful consideration and further investigation for the application of interventions.
Findings of the secondary outcome are consistent with current literature, which reports small improvements in psychological symptoms following caregiver interventions. The low heterogeneity of results reflects statistical consistency, increasing the confidence in the robustness of the findings. Despite variations in delivery methods, the positive effects of interventions were consistent across different contexts. This suggests that the observed benefits of multi-component TBI caregiver interventions were stable. Given that all 3 studies were done in the United States in the meta-analysis, the homogeneity might partly reflect the similarity of study contexts, which limits generalisability to lower or middle income countries. Eight out of ten RCTs in this study reported improvements in depression and anxiety scores in various outcome measures, which matched with the findings in BSI-18. The interventions lasted from 1 month to 2 years while contacts were arranged at least once a month. All interventions that improved depression and overall mental health outcomes included an emotional support component, such as follow-up contact with medical staff or educational sessions on emotional regulation that facilitated sharing. Blended and face to face interventions worked most effectively in alleviating psychological distress. Interventions that support caregivers during the transition from hospital to home tend to lead to better psychological outcomes as well. As many caregivers feel unprepared for this change, convenient and easily accessible programs can alleviate anxiety and ease the transition. The results suggest that home visits and telephone follow-ups facilitate a smoother transition and enable timely resolution of problems as they arise. This highlights the importance of providing both psychological and practical support to improve caregivers' wellbeing. However, due to the small number and the modest quality of studies, the results should be considered alongside the broader body of literature before making definitive practice recommendations.
Placing the results of this study in wider literature, comparison with the previous systematic review must be considered, as notable advancements in intervention studies have been observed (20). The findings suggest that intervention approaches applied predominantly in Western countries may also be effective in Asian contexts when adapted to place greater emphasis on social and emotional support. Cultural contexts appeared to influence intervention priorities, where studies from Asian countries more frequently emphasized family functioning and support, whereas studies from Western countries tended to focus on individual-level outcomes, reflecting differing societal values. The differences in content also lead to the variety of outcome measures. Compared to previous systematic reviews, outcome measures have become more standardized, allowing a meta-analysis to be done, yet they have also grown more diverse. Family functioning outcome measures have become increasingly common in current intervention studies, reflecting that support should extend beyond the individual caregiver to the family unit as a whole. Nevertheless, current literature still contains relatively few outcome measures specifically validated for TBI caregivers. One such tool, the Traumatic Brain Injury Caregiver Quality of Life (TBI-CareQOL), was validated in 2020 but it has yet to be widely adopted in interventions studies (33).
In terms of assessing how easy the interventions were for both participants and providers, this was difficult as interventions were delivered in a variety of way, ranging from web-based, app-based, face-to-face, online chats, home visits and telephone calls. However, interventions can be delivered in a variety of settings, including in patient's own homes which may be easier to follow without the need for repeat in-person visits. However, this relies on patients making sure that they adhere to the intervention plan, which may be hard to follow. Future research should assess how best to deliver these interventions and whether remote or web-based platforms may offer improved adherence due to their flexibility.
Several limitations should be considered when interpreting the findings of this review. Although a comprehensive multi-database search was conducted, relevant studies may have been missed due to publication bias and language restrictions as those without English full text manuscripts were excluded. Second, there is moderate to high risk of bias in the studies, with common issues including high attrition rate, inadequate blinding and incomplete reporting of randomization processes. Third, the predominance of studies conducted in high-income countries, where healthcare systems and caregiver support services may differ substantially from those in low and middle income countries. This limits the generalisability of findings to global contexts. Cultural differences in caregiving roles, family values and coping mechanisms may also influence the acceptability and effectiveness of interventions. Thus, interventions focusing on the needs of TBI caregivers with different ethnicities should also be developed to generalize interventions to other populations. Finally, as there are no standardized outcome measures for TBI caregivers specifically, conclusions should be drawn cautiously and considered alongside the broader literature. Future updates to this review should aim to incorporate these developments, standardize outcome measures and assess the long-term effects of caregiver programs.
Another limitation is that across the 13 studies, there was a variety of specialists, ranging from nurses to psychologists, that delivered the intervention and so there is considerable methodological heterogeneity and comparisons of potential caregiver burden improvements across the included studies must be interpreted with caution. Future studies should look to standardize the composition of the team that delivers the intervention, with perhaps first identifying which specialist or a multidisciplinary team of specialist might provide the best training for the intervention.
5 Conclusion
This systematic review found that multi-component interventions are beneficial in reducing caregiver burden and psychological distress among TBI caregivers. Interventions with both practical and psychological support, implemented at least once a month should be considered during the TBI patient's transition from hospital to community. Sessions using a blended or face to face approach are encouraged to facilitate caregivers in meeting the needs of their loved one. However, while benefits were observed over various populations and delivery modes, results should be interpreted with caution due to methodological limitations, which are consistent with previous systematic reviews. The heterogeneity of studies makes it difficult to develop definitive clinical guidelines as differences in intervention design, delivery and outcome measures limit the ability to establish universally applicable recommendations. Future research should prioritize rigorous study designs and the validation of standardized outcome measures in TBI caregiving to enable clearer comparisons between interventions. Overall, well-structured caregiver interventions appear promising for integration into hospital standard care and rehabilitation pathways, but higher quality research is required to confirm their effectiveness, determine the best specialist or teams of specialists to deliver the intervention and thus guide broader implementation.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CYT: Investigation, Conceptualization, Writing – original draft, Formal analysis, Data curation. ZA: Conceptualization, Supervision, Methodology, Writing – review & editing, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to thank Dr. Paul Perrin for providing additional information regarding their study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gu L, Zhang L, Li C, Jiang L, Zhou J, Xie Y, et al. Global, regional, and national burden of traumatic brain injury, 1990–2021: a systematic analysis for the global burden of disease study 2021. J Neurotrauma. (2025) 42:19–20. doi: 10.1089/neu.2025.0039
2. Dams-O'Connor K, Juengst SB, Bogner J, Chiaravalloti ND, Corrigan JD, Giacino JT, et al. Traumatic brain injury as a chronic disease: insights from the United States Traumatic Brain Injury Model Systems Research Program. Lancet Neurol. (2023) 22:517–28. doi: 10.1016/S1474-4422(23)00065-0
3. Lieshout K, Oates J, Baker A, Unsworth CA, Cameron ID, Schmidt J, et al. Burden and preparedness amongst informal caregivers of adults with moderate to severe traumatic brain injury. Int J Environ Res Public Health. (2020) 17:6386. doi: 10.3390/ijerph17176386
4. Brickell TA, Cotner BA, French LM, Carlozzi NE, O'Connor DR, Nakase-Richardson R, et al. Severity of military traumatic brain injury influences caregiver health-related quality of life. Rehabil Psychol. (2020) 65:377–89. doi: 10.1037/rep0000306
5. Qadeer A, Khalid U, Amin M, Murtaza S, Khaliq MF, Shoaib M. Caregiver's burden of the patients with traumatic brain injury. Cureus. (2017) 9:e1590. doi: 10.7759/cureus.1590
6. Kratz AL, Sander AM, Brickell TA, Lange RT, Carlozzi NE. Traumatic brain injury caregivers: a qualitative analysis of spouse and parent perspectives on quality of life. Neuropsychol Rehabil. (2017) 27:16–37. doi: 10.1080/09602011.2015.1051056
7. Malec JF, Van Houtven CH, Tanielian T, Atizado A, Dorn MC. Impact of TBI on caregivers of veterans with TBI: burden and interventions. Brain Inj. (2017) 31:1235–45. doi: 10.1080/02699052.2016.1274778
8. Klyce DW, Marwitz JH, Perera RA, Dreer LE, Agtarap SD, Abbasi K, et al. Caregiver resilience through the first 2 years after traumatic brain injury: a traumatic brain injury model systems study. Arch Phys Med Rehabil. (2025) 106:1217–26. doi: 10.1016/j.apmr.2025.01.464
9. Niemeier JP, Kreutzer JS, Marwitz JH, Sima AP. A randomized controlled pilot study of a manualized intervention for caregivers of patients with traumatic brain injury in inpatient rehabilitation. Arch Phys Med Rehabil. (2019) 100:S65–75. doi: 10.1016/j.apmr.2018.07.422
10. Ganefianty A, Songwathana P, Damkliang J, Imron A, Latour JM, A. Mobile health transitional care intervention delivered by nurses improves postdischarge outcomes of caregivers of patients with traumatic brain injury: a randomized controlled trial. World Neurosurg. (2024) 184:191–201. doi: 10.1016/j.wneu.2024.01.078
11. Powell JM, Fraser R, Brockway JA, Temkin N, Bell KR. A telehealth approach to caregiver self-management following traumatic brain injury: a randomized controlled trial. J Head Trauma Rehabil. (2016) 31:180. doi: 10.1097/HTR.0000000000000167
12. Suntai Z, Laha-Walsh K, Albright DL. Effectiveness of remote interventions in improving caregiver stress outcomes for caregivers of people with traumatic brain injury. Rehabil Psychol. (2021) 66:415–22. doi: 10.1037/rep0000402
13. Nichols LO, Martindale-Adams J, Seel RT, Zuber JK, Perera R, Perrin PB. Reducing burden and anxiety for caregivers of veterans with traumatic brain injury and dementia: randomized controlled trial of the resources for enhancing all caregivers' health—Hope intervention. Rehabil Psychol. (2025) doi: 10.1037/rep0000632 [Epub ahead of print].
14. Carlozzi NE, Troost JP, Sen S, Choi SW, Wu Z, Miner JA, et al. Improving outcomes for care partners of individuals with traumatic brain injury: results for a mHealth randomized control trial of the CareQOL app. Arch Phys Med Rehabil. (2025) 106:548–61. doi: 10.1016/j.apmr.2024.12.022
15. McLaughlin KA, Glang A, Beaver SV, Gau JM, Keen S. Web-based training in family advocacy. J Head Trauma Rehabil. (2013) 28:341. doi: 10.1097/HTR.0b013e31824e1d43
16. Oyesanya TO, Ibemere SO, Loflin C, McReynolds V, Anaya B, Huang M, et al. “If you respect me, you are respecting my culture”: methods and recommendations for personalizing a TBI transitional care intervention. Brain Inj. (2023) 37:746–57. doi: 10.1080/02699052.2023.2208881
17. Vranda MN, Reddy NK. Efficacy of family intervention in acquired head-injury cases in India. Disabil CBR Incl Dev. (2012) 23:137–49. doi: 10.5463/dcid.v23i3.120
18. Perrin PB, Rodriguez-Agudelo Y, Plaza SLO, Quijano-Martinez MC, Trujillo MA, Smith ER, et al. Multi-site, multi-country randomized clinical trial of an acute traumatic brain injury caregiver transition assistance program in Latin America. NeuroRehabilitation. (2023) 52:137–47. doi: 10.3233/NRE-220121
19. Linton KF, Kim BJ. A pilot study of Trabajadora de salud, a lay health worker intervention for Latinas/os with traumatic brain injuries and their caregivers. Disabil Health J. (2018) 11:161–4. doi: 10.1016/j.dhjo.2017.04.009
20. Kreitzer N, Kurowski BG, Bakas T. Systematic review of caregiver and dyad interventions after adult traumatic brain injury. Arch Phys Med Rehabil. (2018) 99:2342–54. doi: 10.1016/j.apmr.2018.04.016
21. PRISMA Statement (2025). Available online at: https://www.prisma-statement.org (Accessed August 14, 2025).
22. Baker A, Barker S, Sampson A, Martin C. Caregiver outcomes and interventions: a systematic scoping review of the traumatic brain injury and spinal cord injury literature. Clin Rehabil. (2017) 31:45–60. doi: 10.1177/0269215516639357
23. Figaji AA. Anatomical and physiological differences between children and adults relevant to traumatic brain injury and the implications for clinical assessment and care. Front Neurol. (2017) 8:685. doi: 10.3389/fneur.2017.00685
24. Marshall IJ, Wallace BC. Toward systematic review automation: a practical guide to using machine learning tools in research synthesis. Syst Rev. (2019) 8:163. doi: 10.1186/s13643-019-1074-9
25. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
26. Hanks RA, Rapport LJ, Wertheimer J, Koviak C. Randomized controlled trial of peer mentoring for individuals with traumatic brain injury and their significant others. Arch Phys Med Rehabil. (2012) 93:1297–304. doi: 10.1016/j.apmr.2012.04.027
27. Moriarty H, Winter L, Robinson K, Piersol CV, Vause-Earland T, Iacovone DB, et al. A randomized controlled trial to evaluate the veterans' in-home program for military veterans with traumatic brain injury and their families: report on impact for family members. PM&R. (2016) 8:495–509. doi: 10.1016/j.pmrj.2015.10.008
28. Rivera PA, Elliott TR, Berry JW, Grant JS. Problem-solving training for family caregivers of persons with traumatic brain injuries: a randomized controlled trial. Arch Phys Med Rehabil. (2008) 89:931–41. doi: 10.1016/j.apmr.2007.12.032
29. Løvstad M, Borgen IMH, Hauger SL, Kleffelgård I, Brunborg C, Røe C, et al. Family member reported symptom burden, predictors of caregiver burden and treatment effects in a goal-oriented community-based randomized controlled trial in the chronic phase of traumatic brain injury. BMC Neurol. (2024) 24:333. doi: 10.1186/s12883-024-03841-7
30. Sinnakaruppan I, Downey B, Morrison S. Head injury and family carers: A pilot study to investigate an innovative community-based educational programme for family carers and patients. Brain Inj. (2005) 19:283–308. doi: 10.1080/02699050400003924
31. Rasmussen M, Andelic N, Pripp AH, Nordenmark TH, Soberg HL. The effectiveness of a family-centred intervention after traumatic brain injury: a pragmatic randomised controlled trial. SAGE J Clin Rehabil. (2021) 35:1428–41. doi: 10.1177/02692155211010369
32. Siegert RJ, Jackson D, Tennant A, Turner-Stokes L. Factor analysis and Rasch analysis of the Zarit Burden Interview for acquired brain injury carer research. J Rehabil Med. (2010) 42:302–9. doi: 10.2340/16501977-0511
Keywords: caregiver interventions, caregiver programs, traumatic brain injury, caregiver burden, psychological distress, rehabilitation
Citation: Ting CY and Ahmed Z (2025) Impact of caregiver interventions on caregiver burden in adult traumatic brain injury: a systematic review and meta-analysis. Front. Public Health 13:1698592. doi: 10.3389/fpubh.2025.1698592
Received: 22 September 2025; Revised: 23 October 2025; Accepted: 13 November 2025;
Published: 03 December 2025.
Edited by:
Margarida Vilaça, University of Minho, PortugalReviewed by:
Anand Kumar, Banaras Hindu University, IndiaAloysia Ispriantari, Institut Teknologi Sains dan Kesehatan RS dr Soepraoen Kesdam V, Indonesia
Copyright © 2025 Ting and Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zubair Ahmed, ei5haG1lZC4xQGJoYW0uYWMudWs=
 Chung Yan Ting
Chung Yan Ting Zubair Ahmed
Zubair Ahmed