- 1School of Basic Medical Sciences & School of Nursing, Chengdu University, Chengdu, China
- 2Department of Pediatrics, Deyang People's Hospital, Deyang, China
- 3Department of Psychosomatic Medicine, Deyang People's Hospital, Deyang, China
- 4Department of Nursing, Deyang People's Hospital, Deyang, China
- 5Department of Emergency, Deyang People's Hospital, Deyang, China
Objective: This study aims to investigate the current status of caregiver burden among parents of children with asthma comorbidities and to identify its associated factors.
Methods: We conducted a cross-sectional study from May to July 2025, involving 325 parents of children with asthma and comorbidities from two tertiary hospitals in Sichuan Province, China. Sociodemographic and clinical characteristics were collected through structured questionnaires. The Zarit caregiver burden interview (ZBI) and perceived social support scale (PSSS) were used to assess caregiver burden and social support levels, respectively. Statistical analyses included Pearson correlation, t-tests, analysis of variance (ANOVA), and multiple linear regression.
Results: The total caregiver burden score was 40.44 ± 6.86, with 61.8% of the parents experiencing a moderate level of burden. Perceived social support was negatively correlated with caregiver burden (r = −0.621, P < 0.01). Multiple linear regression analysis revealed the child's age, asthma course, asthma comorbidity course, number of comorbidities, payment methods of healthcare costs, employment status, asthma control status, and perceived social support as factors significantly associated with caregiver burden, collectively explaining 55.2% of the total variance. This indicates that nearly half of the variance in caregiver burden could not be explained.
Conclusions: The caregiver burden among parents of children with asthma and comorbidities is substantial. Factors associated with higher burden levels include longer asthma course, greater number of comorbidities, longer comorbidity course, part-time employment status, and poor asthma control. Conversely, higher levels of perceived social support, older child age, and medical insurance and commercial insurance coverage were associated with lower burden levels. These findings provide an empirical basis for clinical institutions, communities, and relevant departments to inform the development of targeted interventions aimed at alleviating this caregiver burden. It should be noted that this study employed a cross-sectional design, and future longitudinal research is needed to verify causal relationships.
1 Introduction
Asthma is a heterogeneous disease characterized by chronic airway inflammation and heightened airway responsiveness, clinically manifested as recurrent episodes of wheezing, coughing, and shortness of breath, which often occur or worsen at night or in the early morning (1). As a chronic airway hyperresponsiveness condition that severely affects the physical and mental health of children worldwide, the prevalence of pediatric bronchial asthma has been increasing (2, 3), posing a substantial burden on global public health systems. According to the 2021 Global Initiative for Asthma (GINA) report, asthma affects over 300 million children globally (4), posing a critical and increasing public health burden that demands urgent attention worldwide (5–7).
In recent years, clinical practice and research have revealed that childhood asthma is often accompanied by comorbidities, a situation that further increases the complexity and challenges of disease management. In 2008, the World Health Organization (WHO) defined “comorbidity” as the coexistence of two or more chronic non-communicable diseases in the same patient (8). Common comorbidities of childhood asthma include allergic rhinitis (AR), chronic rhinosinusitis (CRS), and obstructive sleep apnea (OSA), among others (9). Studies indicate that 85%−95% of children with asthma have comorbid AR (10), 63% have comorbid OSA (11), and 49.2% experience anxiety-related issues (12). These comorbidities not only directly and negatively impact the condition of children with asthma, such as increasing the difficulty of asthma diagnosis and reducing treatment effectiveness (13, 14), but also lead to a higher frequency of asthma exacerbations, as well as increased emergency department visits and hospitalizations (13, 15), substantially consuming medical resources. Furthermore, the long-term management of comorbidities requires parents to invest more time in monitoring multiple disease symptoms and coordinating multidisciplinary treatments. Simultaneously, higher treatment costs and concerns about the child's prognosis impose significant physical, psychological, and economic pressures on parents (16). Given that caring for children with asthma and comorbidities is a long-term and continuous process, and that parents play a critical role in disease management, with the quality of care they provide determining the disease progression and recovery of the child, it is crucial to recognize and address the caregiver burden experienced by parents of children with asthma comorbidities.
Caregiver burden refers to the negative reactions experienced by caregivers in physical, psychological, and economic aspects due to the perceived stress of providing care to patients (17). Studies have shown that caring for children with chronic diseases presents greater challenges than caring for healthy children, and the high-quality care required by affected children is more likely to impose a heavy burden on caregivers (18). As the primary caregivers of children with asthma (19), parents bear multiple disease-related pressures, and the presence of asthma comorbidities further exacerbates this burden. On the physical level, caring for children with asthma comorbidities requires parents to expend considerable time and energy over the long term: asthma comorbidities are prone to triggering acute episodes or causing persistent symptoms in children, thereby increasing the need for emergency visits and hospitalizations (20). Parents must accompany their children throughout diagnosis and treatment, and this significant time investment often leads to physical fatigue and exacerbates exhaustion (21). On the psychological level, long-term care commonly leads to anxiety and depressive symptoms among parents (22). Studies report that 67.57% of parents of children with asthma experience varying degrees of depression (23). Additionally, concerns about the child's physical and mental impairment, uncertainty about disease prognosis, and pressures from social and work responsibilities further compound their psychological and emotional burden. On the economic level, children with asthma comorbidities require more complex health management and greater use of medical services. Long medication cycles and high treatment costs (16), coupled with the fact that comorbidities increase asthma-related treatment expenses (24), place a substantial financial strain on families.
Given that asthma comorbidities severely affect children's health and impose multiple burdens on their caregivers, addressing parental caregiver burden in this population is crucial. However, existing literature primarily focuses on asthma as a single disease (25–28), thereby overlooking the cumulative impact of multiple comorbidities. Specifically, there is a notable lack of studies investigating how the coexistence of several comorbidities amplifies caregiver burden, creating a significant gap in understanding the challenges faced by parents of this complex patient population. To address this gap, this cross-sectional study aims to investigate the current status of caregiver burden and its associated factors among parents of children with asthma and comorbidities, and employs the total number of comorbidities per child to operationalize this cumulative impact in our analysis. The findings will provide an empirical basis for developing targeted intervention strategies aimed at alleviating this caregiver burden and improving disease management outcomes.
2 Materials and methods
2.1 Survey participants
In this study, A convenience sampling method was employed to recruit parents of children with asthma and comorbidities who visited the pediatric outpatient departments of two Grade A tertiary hospitals in Sichuan Province from May 2025 to July 2025 as participants.
Inclusion criteria: parents of children diagnosed with asthma and at least one comorbidity (including allergic rhinitis, chronic sinusitis, obesity, gastroesophageal reflux disease, obstructive sleep apnea, anaphylaxis, anxiety and depression issues) based on the diagnostic criteria specified in Guidelines for the Diagnosis and Management of Bronchial Asthma in Children by the Respiratory Subspecialty Group of the Pediatrics Society, Chinese Medical Association (1); parents of children aged 0–18 years; parents with normal thinking and verbal communication abilities, as well as adequate reading and comprehension skills; parents who voluntarily agreed to participate in the study and signed the informed consent form.
Exclusion criteria: parents with mental illness or other severe chronic conditions that prevented them from completing the questionnaire independently; parents or their children who had experienced major life changes or stressful events (e.g., the death of a family member, a serious traffic accident, etc.) within the past 3 months.
Based on Kendall's rough estimation principle for sample size, the sample size of a study should be at least 5–10 times the number of variables (29). In this study, a total of 25 variables were included. Accounting for potential invalid questionnaires, the sample size was increased by 10%−20%, resulting in a calculated required sample size of 138–300 participants. To ensure more reliable statistical results, we attempted to collect as much data as possible. Ultimately, 340 questionnaires were distributed in this study, with 325 valid ones recovered, yielding an effective response rate of 95.59%.
This study has obtained approval from the Ethics Committee of Deyang People's Hospital (No. 2025-04-043-K01) and the Medical Ethics Committee of the Affiliated Hospital of Chengdu University (No. PJ2025-056-03). All participants were fully informed about the study, provided their informed consent, and voluntarily participated.
2.2 Survey instruments and measures
2.2.1 General information questionnaire
The questionnaire consists of two sections: one for the children and one for their parents. The child's general information questionnaire includes items such as gender, age, duration of asthma, duration of asthma comorbidities, asthma control status, number of comorbidities, family history of asthma, medical expense payment method, and the child's annual medical expenses. The parents' general information questionnaire covers items like gender, age, educational level, marital status, number of children, employment status, and monthly family income.
2.2.2 Zarit caregiver burden inventory (ZBI)
The Zarit Caregiver Burden Inventory (ZBI), developed by Zarit et al. (17), is used to assess the level of burden experienced by caregivers. The ZBI questionnaire used in this study was translated and revised by Chinese scholar Wang et al. (30). The Chinese version of the questionnaire consists of 22 items, divided into two dimensions: personal burden and responsibility burden. Specifically, it includes 12 items related to personal burden (Items 1, 4, 5, 8, 9, 14, 16–21) and 6 items addressing other forms of burden (Items 2, 3, 6, 11–13). Items 7, 10, and 15 are not categorized under any dimension, while Item 22 serves as an overall evaluation of the caregiver's perceived burden. The questionnaire uses a 5-point Likert scale, with responses ranging from 0 to 4, corresponding to “never”, “rarely”, “sometimes”, “often”, and “always” respectively. Total scores range from 0 to 88, with higher scores indicating greater caregiver burden. Scores of 0 to 19 indicate no burden, 20 to 39 indicate mild burden, 40 to 59 indicate moderate burden, and scores above 60 indicate severe burden. The Cronbach's alpha coefficient of the original scale is 0.870, and in the present study, the Cronbach's alpha coefficient for the scale was 0.832.
2.2.3 Perceived social support scale (PSSS)
The perceived social support scale (PSSS), developed by Zimet et al. (31), is used to assess an individual's level of perceived social support. The PSSS questionnaire used in this study was translated and revised by Chinese scholar Jiang et al. (32). The Chinese version of the questionnaire consists of 12 items across three dimensions: family support, friend support, and other support. Specifically, there are 4 items for family support (Items 3, 4, 8, 11), 4 items for friend support (Items 6, 7, 9, 12), and 4 items for other support (Items 1, 2, 5, 10). The questionnaire uses a 7-point Likert scale, with responses ranging from 1 to 7, corresponding to “strongly disagree”, “disagree”, “slightly disagree”, “neutral”, “slightly agree”, “agree”, and “strongly agree” respectively. Total scores range from 12 to 84, with higher scores indicating a higher level of perceived social support. Scores of 12–36 indicate a low level of perceived social support, 37–60 indicate a moderate level, and 61–84 indicate a high level. The Cronbach's alpha coefficient of the original scale is 0.840, and in the present study, the Cronbach's alpha coefficient for the scale was 0.814.
2.2.4 Data collection
This study employed a convenience sampling method, which is a core type of non-probability sampling. Convenience sampling is characterized by the accessibility and ease of participant selection, allowing researchers to prioritize individuals who are readily available, easily recruited, and meet the inclusion criteria in a specific research setting, without adhering to randomization principles to cover all individuals in the population (33). The reasons for selecting convenience sampling are as follows: first, as a cross-sectional study requiring sample collection within a limited timeframe, this method effectively reduces the difficulty of sample screening and shortens the data collection cycle. Second, for cross-sectional studies focusing on target populations in specific settings, this approach ensures that enrolled participants can provide the core information required for the research, balancing feasibility and data completeness. It should be noted that while this method offers advantages in efficiency and practicality, its reliance on convenience rather than randomization may limit sample representativeness, thereby restricting the generalizability and broader applicability of the findings. Participants were selected in strict accordance with the predefined inclusion and exclusion criteria. Questionnaires were collected through on-site surveys with immediate retrieval. To ensure consistency in the research process, the research team first provided uniform training to its members on interview techniques, key points for questionnaire completion, and relevant protocols. Before distributing the questionnaires, researchers thoroughly explained the purpose and significance of the study to the participants. Questionnaires were only distributed after participants had a clear understanding of the study and signed the informed consent form. During questionnaire completion, participants could ask researchers questions at any time; researchers provided on-site explanations but only for clarification purposes, avoiding suggestive or deliberate guidance and refraining from interfering with participants' responses. Once the questionnaires were completed, researchers collected them on the spot and reviewed the responses. If any errors or omissions were identified, participants were immediately asked to supplement or correct the information to minimize data loss.
2.3 Statistical analysis
Data from the questionnaires were entered using Microsoft Excel 2019 to establish and organize the database. Statistical analyses were performed with SPSS 25.0 software. During the data cleaning phase, following an overall assessment of data quality, missing values were addressed using listwise deletion. Only complete cases without any missing values were included in the analysis to ensure both the sample size and reliability of subsequent analyses. Qualitative data are presented as frequencies and percentages. For quantitative data, the descriptive approach was determined based on their distribution. The normality of continuous variables was assessed using the Shapiro-Wilk test. Quantitative data that were normally or approximately normally distributed are described as means and standard deviations, while those not meeting the normality assumption are reported as medians and interquartile ranges. Independent samples t-tests and one-way analysis of variance were used to examine differences in caregiver burden scores among parents of children with asthma comorbidities based on demographic characteristics of both the parents and the children. Pearson correlation analysis was conducted to explore the correlation between parental caregiver burden and perceived social support, as well as the relationships between numerical demographic variables and caregiver burden. Multiple linear regression analysis was employed to identify factors influencing the caregiver burden among parents of children with asthma comorbidities. Nominal variables were converted into dummy variables before being entered into the regression model. Multicollinearity among the independent variables was assessed using the variance inflation factor (VIF) and tolerance to ensure the stability and accuracy of the regression model. A VIF < 10 and a tolerance > 0.1 indicated the absence of severe multicollinearity, allowing for the regression analysis to proceed. If VIF ≥10 or tolerance ≤ 0.1, remedial measures such as removing redundant variables or merging variables were applied before further analysis. The independence of residuals was verified using the Durbin-Watson test. To quantify the magnitude of the associations, the effect size (standardized coefficient β) along with its 95% confidence interval (CI) are reported. A P-value < 0.05 was considered statistically significant.
3 Results
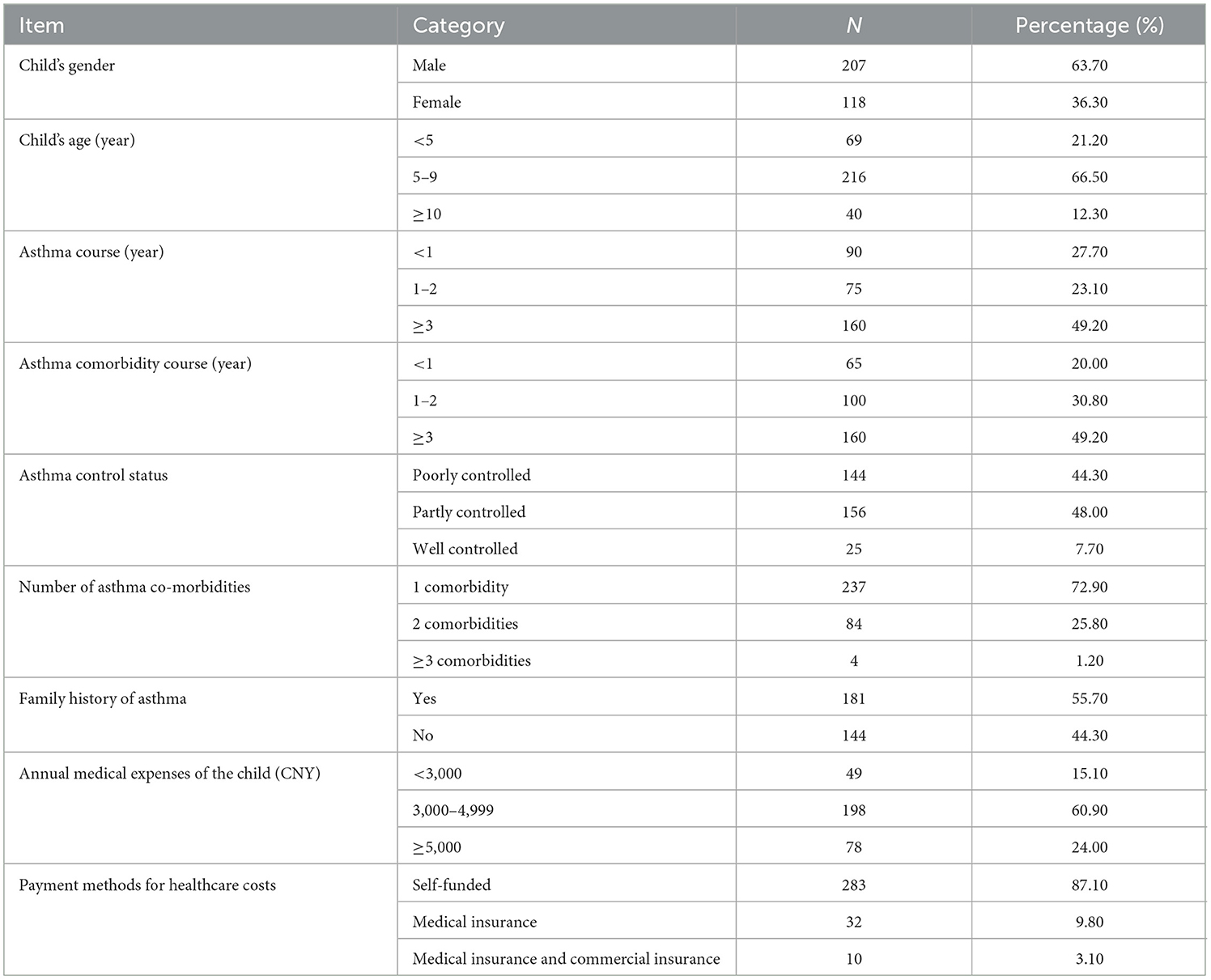
3.1 Demographic characteristics of children with asthma comorbidities
Among 325 children with asthma comorbidities, there were 207 boys (55.50%) and 118 girls (39.30%). The average age of children was (6.43 ± 2.49) years. Course of asthma < 1 year: 90 (27.70%), 1–2 years: 75 (23.10%), ≥3 years: 160 (49.20%). Course of comorbidities of asthma < 1 year: 65 (20.00%), 1–2 years: 100 (30.80%), ≥3 years: 160 (49.20%). In terms of the number of comorbidities, there were 237 children (72.90%) who had 1 comorbidity, 84 (25.80%) had 2 comorbidities, and 4 (1.20%) had ≥ 3 comorbidities. There were 181 (55.70%) with a family history of asthma and 144 (44.30%) without such a history. See Table 1 for details.
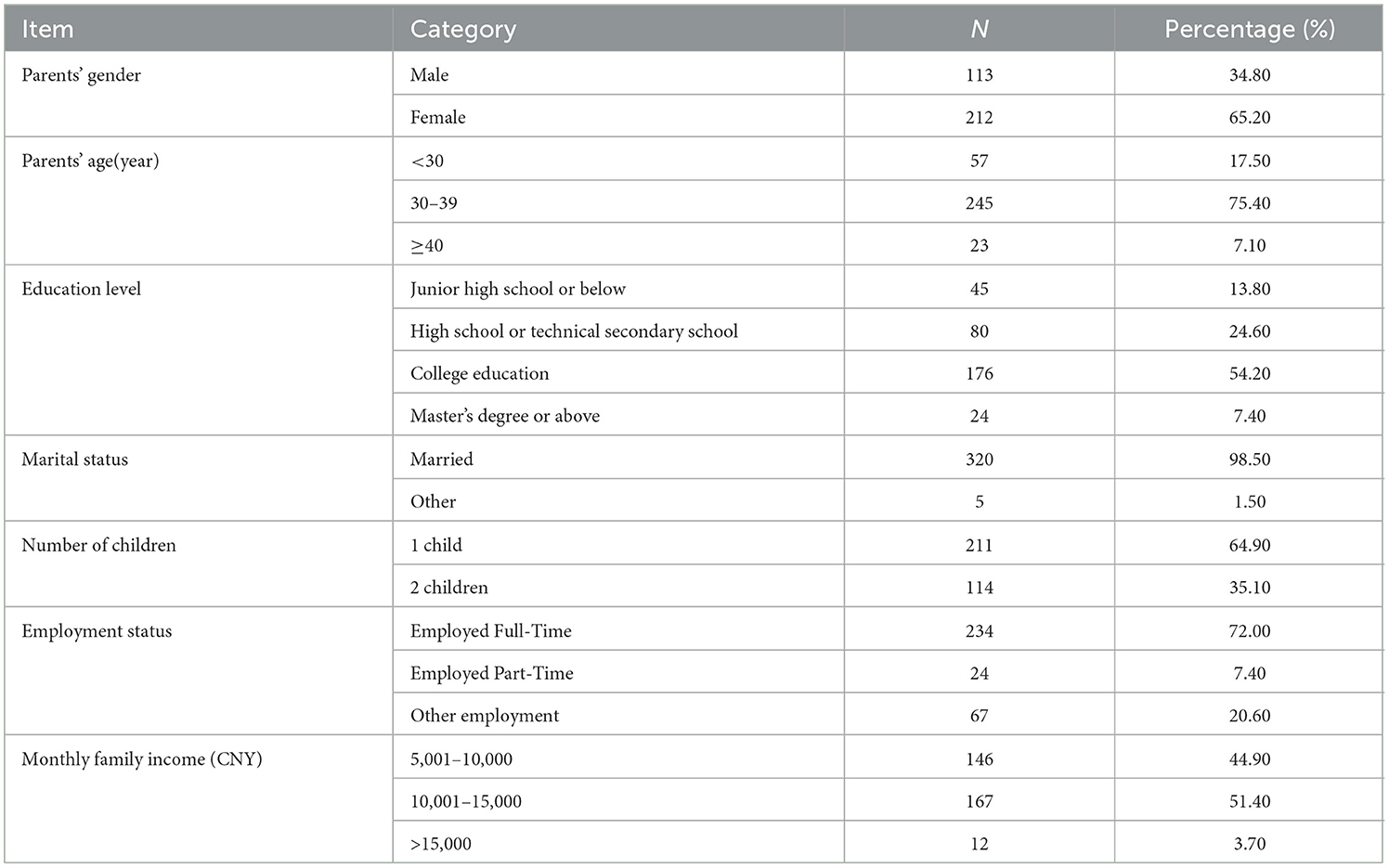
3.2 Demographic characteristics among parents of children with asthma comorbidities
Among the 325 parents of children with asthma comorbidities, 113 were male (34.80%) and 212 were female (65.20%), with a higher proportion of females. The average age of the parents was (34.17 ± 3.57) years. In terms of educational level, 176 (54.20%) had a college education, 80 (24.60%) had a high school or technical secondary school education, 45 (13.80%) had a Junior high school or below, and 24 (7.40%) had a master's degree or above. Among the employment statuses, 234 parents (72.00%) were employed full-time, 24 parents (7.40%) were employed part-time, and 67 (20.60%) were in other employment statuses. See Table 2 for details.
3.3 Caregiver burden and perceived social support scores among parents of children with asthma comorbidities
The caregiver burden score among parents of children with asthma comorbidities was 40.44 ± 6.86, with 61.8% (n = 201) experiencing a moderate level of burden. The perceived social support score was 46.23 ± 4.20, indicating a moderate level of support. The scores of each dimension of the caregiver burden scale and the perceived social support scale. See Table 3 for details.
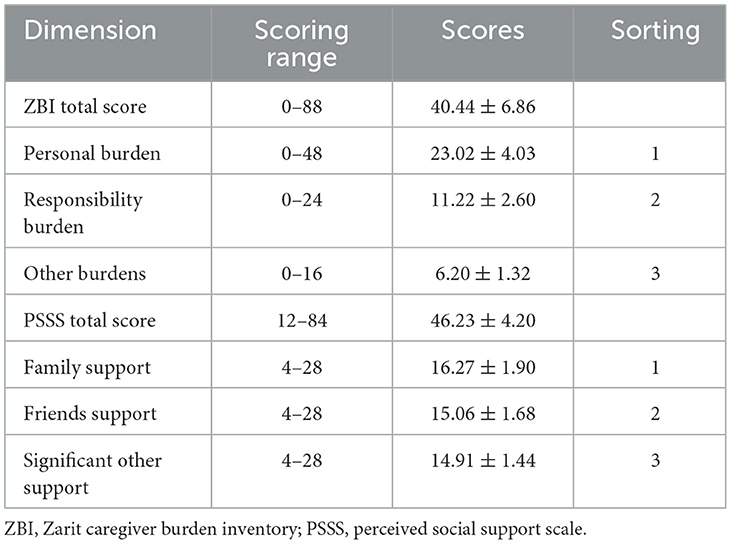
Table 3. Caregiver burden and perceived social support scores in parents of children with asthma comorbidities.
3.4 Correlation analysis of caregiver burden Score and perceived social support Score
Pearson correlation analysis revealed significant negative correlations between caregiver burden (total and dimension scores) and perceived social support (total and dimension scores) (all P < 0.01). Specifically, a strong negative correlation was found between the total scores of caregiver burden and perceived social support (r = −0.621, P < 0.01). See Table 4 for details.
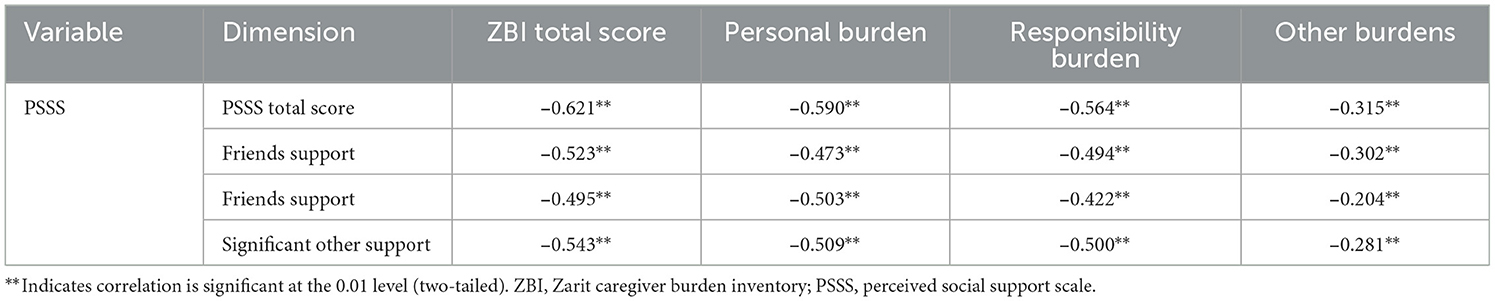
Table 4. Correlation analysis of caregiver burden and perceived social support scores for parents of children with asthma comorbidities.
3.5 Univariate analysis of the caregiver burden among parents of children with asthma comorbidities
Univariate analysis identified several factors significantly associated with caregiver burden, including the child's age, asthma course, asthma comorbidity course, asthma control status, number of comorbidities, family history of asthma, annual medical expenses, payment methods of healthcare costs, parent's gender, educational level, employment status, and monthly family income (all P < 0.05). See Table 5 for details.
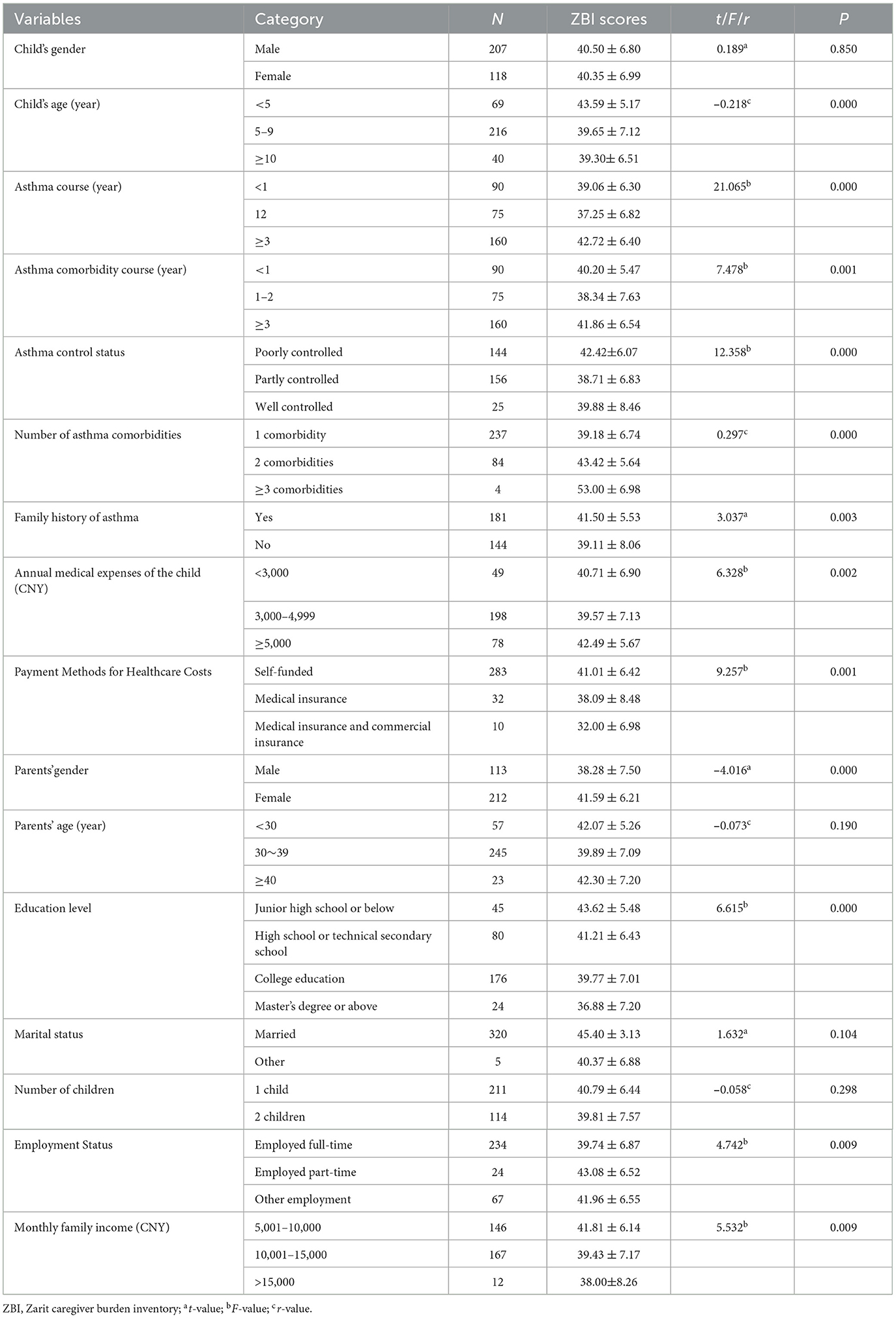
Table 5. Univariate analysis of caregiver burden among parents of children with asthma comorbidities (N = 325).
3.6 Multiple linear regression analysis of caregiver burden among parents of children with asthma comorbidities
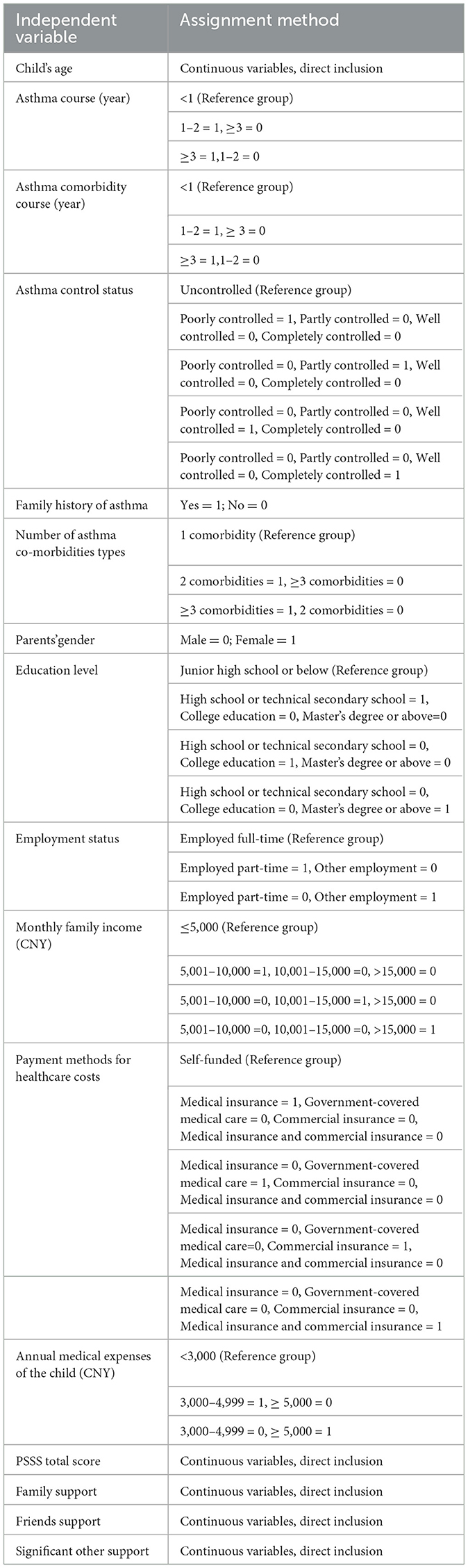
Multiple linear regression analysis was performed with the total caregiver burden score as the dependent variable. The independent variables were those identified through univariate analysis and Pearson correlation analysis. The analysis revealed that perceived social support, the child's age, asthma course, number of comorbidities, payment methods of healthcare costs, asthma comorbidity course, employment status, and asthma control status were significantly associated with caregiver burden. These factors collectively explained 55.2% of the variance in caregiver burden (R2 = 0.552). The assignments of the independent variables are shown in Table 6, and the results of the multiple linear regression analysis are shown in Table 7.
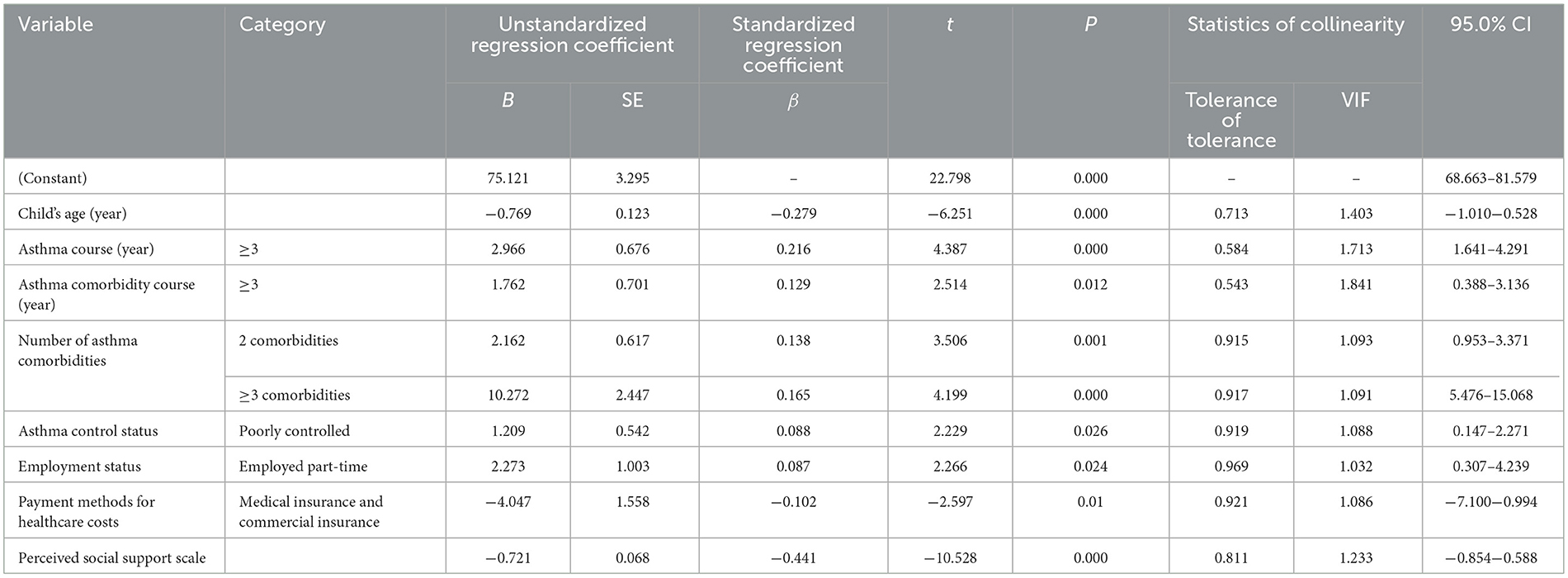
Table 7. Multiple linear regression analysis of caregiver burden among parents of children with asthma comorbidities (N = 325).
4 Discussion
4.1 Levels of caregiver burden among parents of children with asthma comorbidities
This study found that the total caregiver burden score for parents of children with asthma comorbidities was 40.44 ± 6.86, indicating a moderate level of burden. This level of burden was higher than that previously reported for parents of children with asthma alone (34), caregivers of children with general chronic diseases (35), and caregivers of children with diabetes (36). Several factors may explain these findings: compared to children with asthma only or general chronic diseases, the condition of children with asthma comorbidities is more complex. In addition to managing asthma symptoms, parents must also provide care for other comorbidities, significantly increasing the volume and difficulty of caregiving tasks. This often leads to a burden due to mental and physical exhaustion. The recurrent nature of asthma comorbidities may cause parents to feel uncertain about treatment effectiveness. Coupled with frequent medical visits and the financial pressure from overlapping treatment costs for multiple diseases, it can easily trigger emotions such as anxiety and fatigue (37), thereby increasing psychological burden.
Furthermore, this study revealed that 61.2% of parents of children with asthma comorbidities experienced a moderate level of caregiver burden. Among the dimensions of caregiver burden, personal burden ranked higher than role strain. This suggests that during the caregiving process, parents' physical and mental exhaustion is more pronounced than the burden derived from specific care tasks. The reasons for this may be that the complex condition of children with asthma comorbidities requires substantial time and energy investment in care. Parents often sacrifice personal rest, social activities, and even work, leading to long-term neglect of their own needs and accumulation of personal burden (38). At the same time, facing the potential recurrence of the child's illness or interactions among multiple diseases, parents are prone to self-blame, which further exacerbates psychological pressure at the personal level. Therefore, relevant departments can reduce the overall caregiver burden on parents by establishing temporary care support channels to provide short-term respite opportunities, implementing targeted psychological interventions to help alleviate negative emotions, and offering care pathway guidelines for comorbidities to simplify daily care processes.
4.2 Factors associated with caregiver burden among parents of children with asthma comorbidities
4.2.1 Perceived social support
This study demonstrated that perceived social support among parents of children with asthma comorbidities is negatively correlated with caregiver burden, meaning that higher levels of social support are associated with lower levels of burden, which is consistent with previous studies (34, 39). Ding et al. (40) also noted that social support is a crucial factor influencing caregivers' care activities and supportive behaviors. High levels of social support can not only directly alleviate parents' physical, psychological, and financial pressures but also promote positive coping mechanisms, thereby enhancing mental health and reducing the risk of anxiety and depression (41). Additionally, access to resources such as medical information and care benefits can directly reduce care-related concerns and lessen physical and financial strain (42). Conversely, parents with low perceived social support are more likely to face caregiving alone due to a lack of external support, experiencing difficulties in obtaining emotional guidance and practical assistance, leading to an accumulated burden. This survey revealed that only 12.7% of parents of affected children reported a high level of perceived social support. Therefore, clinical institutions and communities should prioritize supporting populations with low social support by implementing targeted interventions. These may include conducting one-on-one assessments to identify specific deficiencies (e.g., lack of emotional or informational support), encouraging parents to proactively strengthen communication with relatives and friends and participate in mutual support groups for caregivers of children with chronic illnesses, and promoting the establishment of diversified community support platforms, such as organizing family support lectures and creating online experience-sharing groups. These efforts would help parents build a robust social support network, thereby enhancing their perceived social support and alleviating caregiver burden.
4.2.2 Child's age
This study demonstrated that the age of the child was significantly associated with caregiver burden among parents. A negative correlation was observed between the child's age and the level of caregiver burden experienced by parents of children with asthma comorbidities, a result consistent with the report by Yang et al. (43). Older children demonstrated greater physiological and psychological maturity, enhanced self-care capacity, improved cognitive and self-management abilities, as well as decreased anxiety and resistance toward treatment and nursing care. These developments reduced the demand for parental assistance in daily care and disease management, thereby alleviating physical and psychological stress (43). In contrast, younger children were more prone to poor cooperation, distress behaviors such as crying, and limited self-management awareness due to their illness and therapeutic regimens, thereby increasing caregiving difficulty (44). Furthermore, parents of very young children assumed nearly complete responsibility for both daily living and medical care (45), which consumed considerable time and energy. This often resulted in diminished social participation, restricted access to informational and emotional support, and heightened perceptions of social isolation, collectively contributing to elevated caregiver burden (46). Therefore, it is suggested that relevant departments and healthcare institutions prioritize parents of young children with asthma comorbidities, implementing targeted interventions focusing on three aspects: competence, resources, and psychology. Collaborate with healthcare professionals to conduct practical training sessions, teaching parents how to use toys to guide their children's cooperation during treatment and symptom monitoring, while also distributing care manuals. For older children, provide simultaneous self-management education through interactive lessons to teach basic care skills, gradually reducing parental caregiving pressure. Utilize community-based platforms to establish short-term care support, organize mutual aid groups, and integrate lectures by psychologists to help parents share experiences and manage care-related stress.
4.2.3 Payment methods for healthcare costs
This study demonstrated that the payment methods for healthcare costs were associated with lower levels of caregiver burden among parents of children with asthma comorbidities. Parents from families utilizing a combination of “medical insurance and commercial insurance” reported significantly lower levels of caregiver burden, a finding consistent with the results reported by Tu et al. (47). Several factors may explain these findings: the long-term treatment required for pediatric asthma comorbidities entails substantial medical expenditures. The dual coverage provided by medical and commercial insurance can complementarily offset these costs, significantly reducing out-of-pocket expenses for families. This reduction in financial pressure alleviates cost-related anxiety, thereby mitigating caregiver burden. In contrast, families relying solely on out-of-pocket payments or single medical insurance schemes face heightened economic and psychological strain. Out-of-pocket payers bear the full cost of treatment, while those with only basic medical insurance may find that coverage limitations fail to meet the comprehensive demands of multimorbidity management, as supported by previous studies (48, 49). Jiang et al. (48) suggested that the payment methods for healthcare costs influence caregivers' positive perceptions. Out-of-pocket payment imposes a heavy economic burden on caregivers, leading to a decline in their positive attitudes toward themselves and society. In contrast, insurance reimbursement can alleviate some of the financial pressure and have a protective effect on caregivers' physical and mental health. Therefore, it is suggested that multi-faceted intervention strategies be implemented at the national level: improve the healthcare security system, encourage families to adopt a combination of “medical insurance and commercial insurance,” and promote the establishment of specialized medical insurance programs for children with asthma (50). It is also essential to optimize reimbursement policies for the diagnosis and treatment of comorbidities to further reduce medical expenses. By alleviating the financial pressure on families, the caregiver burden on parents can be reduced.
4.2.4 Number of asthma comorbidities
This study demonstrated that the number of comorbidities was significantly associated with caregiver burden among parents of children with asthma comorbidities, indicating that a higher number of comorbidities are associated with a greater level of caregiver burden. This suggests that the coexistence of multiple comorbidities may significantly increase caregiver burden by exacerbating the difficulty of asthma control and complicating treatment management processes. The underlying reason for this is that an increase in the number of comorbidities complicates the clinical condition of children with asthma (51). On one hand, parents must simultaneously address the dual care demands of asthma and multiple other diseases, resulting in an increased caregiving workload. On the other hand, potential interactions between different diseases may prolong treatment cycles and increase the frequency of medical visits, thereby amplifying parents' practical and psychological burdens. Additionally, investigations have demonstrated that the frequency of asthma attacks and emergency department visits significantly rises with an increasing number of comorbidities (52), and multiple comorbidities represent a major risk factor for poor asthma control (53). Other studies have also pointed out that asthma comorbidities directly contribute to a higher frequency of asthma deterioration (13). These negative changes in disease status ultimately translate into parental concerns regarding disease prognosis, further exacerbating the caregiver burden. Therefore, healthcare providers and community workers should prioritize parents of children with a higher number of comorbidities and regularly assess changes in their caregiver burden. Personalized care guidance plans can be developed for such families. For example, by simplifying multi-disease care processes and providing coordinated one-stop follow-up services to reduce the complexity of care. Additionally, collaboration with health insurance and social support systems should be strengthened to offer medical expense subsidies or assistance channels, thereby mitigating the compounded impact of financial pressure and alleviating parental caregiver burden.
4.2.5 The disease course of asthma and asthma comorbidities
This study demonstrated that the disease course of asthma and asthma comorbidities was positively correlated with caregiver burden among parents, indicating that a longer disease course was associated with a higher level of burden, which is consistent with previous studies (54). Several factors may explain these findings: a longer disease course implies a prolonged period during which caregivers must invest time in caregiving (55). Over time, the continuous focus of time and energy on the child leads caregivers to gradually abandon their original lifestyles, as leisure and rest time are occupied, resulting in a cumulative increase in psychological load (56). As chronic conditions, asthma and its comorbidities require long-term management, sometimes throughout the child's life, and are prone to recurrence. During extended care, caregivers inevitably experience emotional and psychological burdens, often accompanied by anxiety regarding treatment efficacy (57). Additionally, a longer disease course often indicates a more complex clinical condition and greater difficulty in disease control, necessitating more frequent treatments. This not only increases medical expenses but may also lead to treatment resistance in children due to unmet long-term expectations. Consequently, parents must expend additional effort to guide and persuade their children to cooperate with treatment, further exacerbating the caregiver burden. Therefore, clinical institutions and community departments should prioritize families with long-term disease courses and implement stratified interventions. This can be achieved by establishing a case manager system for such families, where dedicated personnel track disease progression and streamline multidisciplinary diagnosis and treatment processes. Additionally, regular mutual support activities should be organized, involving psychological experts to provide emotional counseling, thereby helping parents alleviate long-term care pressure and ultimately reducing the caregiver burden on families across different stages of the disease.
4.2.6 Asthma control status
This study demonstrated that the asthma control status of the children was significantly associated with caregiver burden, indicating that poorer asthma control was associated with greater caregiver burden among parents, which is consistent with previous findings (58). Furthermore, a correlation was observed between the degree of disease control in children and parental caregiving burden, with suboptimal disease management increasing the perceived burden among parents (59). Several factors may explain these findings: asthma comorbidities are a risk factor for decreased asthma control in children (60) and are closely associated with increased asthma exacerbations and poor control (61). This implies that parents must simultaneously manage both asthma and comorbid conditions, leading to increased care complexity and perceived burden. Furthermore, children with poorly controlled asthma often experience recurrent symptoms, reduced drug efficacy, and repeated hospitalizations, necessitating that parents invest more time and effort in closely monitoring symptoms and managing acute episodes. This prolonged state of high vigilance gradually accumulates psychological strain. Additionally, as the primary caregivers, parents also face dual pressures from both disease management and medical expenses (62).
Therefore, clinical institutions and community departments should prioritize families of children with poorly controlled asthma and implement targeted interventions. These may include collaborating with healthcare professionals to provide disease management training for parents, enhancing their ability to monitor symptoms and respond to emergencies; establishing a follow-up mechanism for asthma control to facilitate timely adjustment of treatment plans and reduce disease recurrence; and organizing regular psychological support and family mutual-aid activities to help alleviate parental anxiety, thereby mitigating the caregiver burden associated with poor asthma control.
4.2.7 Employment status
This study demonstrated that the employment status of the parents was associated with their caregiver burden. Specifically, parents engaged in part-time employment reported relatively higher levels of caregiving burden. The study also indicated that poorer family economic status was associated with greater caregiver burden (63). The need for long-term treatment and regular follow-up visits for asthma comorbidities often leads to work absenteeism, reduced working hours, and income loss among caregivers, significantly increasing the financial strain on families. Under such economic pressure, some parents may resort to working overtime or taking on part-time jobs to supplement household income (64).
Several factors may explain these findings: asthma comorbidities require regular management, while part-time work often involves fragmented schedules, making it difficult to establish a stable care routine. Parents may need to frequently interrupt work to care for their children, leading to reduced work efficiency and compressed rest time. In cases of fluctuations in the child's condition, the time constraints of part-time work may force parents to face the dilemma of either losing income due to missed work or delaying necessary care. Moreover, the income stability and level from part-time work are generally lower than those of full-time employment, often insufficient to fully cover the long-term medical expenses and care-related costs of the child. This amplifies parents' concerns about inadequate care resources and intensifies the psychological burden. Additionally, these parents must balance part-time work, childcare, and daily household responsibilities such as supporting older adult(s) family members. Under multiple role pressures, they are prone to neglect their own health (65), remaining in a prolonged state of physical and mental exhaustion, which further exacerbates the caregiver burden. Therefore, it is suggested that policy and service-level interventions be implemented to provide more care-friendly employment options for parents, including remote work opportunities and flexible scheduling (66), to help them better balance occupational demands with caregiving responsibilities and ultimately reduce caregiver burden.
5 Limitations
This study has several limitations. First and most importantly, the cross-sectional nature of the study design precludes the determination of causal relationships between the identified factors and caregiver burden. The associations observed only indicate relationships at a single point in time. Second, the data were collected exclusively through self-reported questionnaires, which introduces the potential for self-report bias. For instance, parents' assessments of their psychological state, social support, and burden level may be influenced by social desirability or transient mood states. Third, the generalizability of the findings is limited by the convenience sampling method and the recruitment of participants from only two tertiary hospitals in a single province of China. The experiences of caregivers in other regions or healthcare settings may differ. Finally, while the study examined several key factors, it may not have encompassed all relevant variables, such as specific caregiver coping strategies or detailed clinical markers of disease severity.
Future research should therefore prioritize longitudinal or prospective cohort designs to establish temporal precedence and better infer causality. Expanding to multi-center, multi-regional studies with larger and more diverse samples is essential to enhance the external validity of the findings. Incorporating objective measures, such as healthcare utilization records or clinical biomarkers of asthma control, would help mitigate self-report bias. Furthermore, investigating a broader range of psychosocial variables, including resilience, caregiver self-efficacy, and family functioning, could provide a more comprehensive understanding of the determinants of caregiver burden.
6 Conclusion
In conclusion, this study demonstrates that parents of children with asthma comorbidities experience a considerable level of caregiver burden, with over 60% experiencing moderate burden. Factors associated with higher caregiver burden in this group include asthma course (≥3 years), number of asthma comorbidities (2 or ≥3 comorbidities), asthma comorbidity course (≥3 years), employment status (part-time employment), and poor asthma control. Conversely, perceived social support, the child's age, and having both medical and commercial insurance are associated with lower caregiver burden.
The caregiver burden status of these parents requires focused attention from clinical institutions, communities, and relevant authorities. Going forward, an intervention system can be built around the influencing factors: enhancing parents' perceived social support by establishing community mutual-aid platforms and organizing family support activities; developing integrated disease management plans for families of children with long disease duration, multiple comorbidities, or poorly controlled asthma, simplifying care procedures, and strengthening skill training; addressing role conflict issues among part-time parents by collaborating with communities and enterprises to provide care support and psychological counseling; and working with medical insurance departments to optimize medical security policies for children with asthma and comorbidities, expanding the coverage of “dual insurance.” Through multi-level collaboration involving families, medical institutions, communities, and policy sectors, alleviating the care burden of these parents will not only improve the caregivers' quality of life but also provide family-level safeguards for the children's standardized treatment and health outcomes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved Ethical Committee of Deyang People's Hospital (No. 2025-04-043-K01) and the Medical Ethics Committee of Affiliated Hospital of Chengdu University (No. PJ2025-056-03). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
XY: Methodology, Formal analysis, Writing – review & editing, Data curation, Writing – original draft, Investigation, Visualization, Validation, Conceptualization. KS: Methodology, Writing – original draft, Software, Data curation, Investigation, Writing – review & editing. JL: Investigation, Funding acquisition, Writing – review & editing, Resources, Data curation. FY: Project administration, Conceptualization, Writing – review & editing, Supervision. XW: Methodology, Investigation, Validation, Writing – review & editing. DB: Data curation, Writing – review & editing, Investigation. QH: Supervision, Resources, Writing – review & editing, Funding acquisition. LD: Writing – review & editing, Investigation, Data curation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Safeguarding Tibetan Youth, Together Building a Dream of Health. The Creation of a Tibetan & Mandarin Bilingual First Aid Science Popularization Video Series (Grant No. 2025JDKP0172), and the Deyang Municipal Bureau of Science and Technology (Grant No. 2024SZS220).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hong J, Bao Y. Attach importance to the standardized diagnosis and treatment of bronchial asthma in children. Chin J Pediatr. (2016) 54:161–2. doi: 10.3760/cma.j.issn.0578-1310.2016.03.001
2. Asher MI, Rutter CE, Bissell K, Chiang CY, El Sony A, Ellwood E, et al. Worldwide trends in the burden of asthma symptoms in school-aged children: global asthma network phase I cross-sectional study. Lancet. (2021) 398:1569–80. doi: 10.1016/s0140-6736(21)01450-1
3. Hammoudeh S, Hani Y, Alfaki M, Omar N, El Dimassi D, Nowir K, et al. The prevalence of asthma, allergic rhinitis, and eczema among school-aged children in Qatar: a global asthma network study. Pediatr Pulmonol. (2022) 57:1440–6. doi: 10.1002/ppul.25914
4. Santamaria F, Borrelli M, Baraldi E. Gina 2021: the missing pieces in the childhood asthma puzzle. Lancet Respir Med. (2021) 9:e98. doi: 10.1016/S2213-2600(21)00275-7
5. Guo X, Li Z, Ling W, Long J, Su C, Li J, et al. Epidemiology of childhood asthma in Mainland China (1988–2014): a meta-analysis. Allergy Asthma Proc. (2018) 39:15–29. doi: 10.2500/aap.2018.39.4131
6. Zhou S, Huang J, Liang Y, Wei L, Guo Z. Huang Ye. Prevalence and risk factors of asthma in Chinese children: a meta-analysis. Int J Epidemiol Infect Dis. (2020) 47:253–9. doi: 10.3760/cma.j.cn331340-20191231-00234
7. Prevention CfDCa. Centers for Disease Control and Prevention (2022). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/asthma.html (Cited April 18, 2022).
9. Boulet LP, Boulay M. Asthma-related comorbidities. Expert Rev Respir Med. (2011) 5:377–93. doi: 10.1586/ers.11.34
10. Wang R, Liang J, Han W, Wang W, Lu Y, Gu Q. Prevalence of allergic rhinitis in Chinese children from 2001 to 2021: meta analysis. Chin J Preventive Med. (2022) 56:784–93. doi: 10.3760/cma.j.cn112150-20220315-00242
11. Kong DL, Qin Z, Shen H, Jin HY, Wang W, Wang ZF. Association of obstructive sleep apnea with asthma: a meta-analysis. Sci Rep. (2017) 7:4088. doi: 10.1038/s41598-017-04446-6
12. Bardach NS, Neel C, Kleinman LC, McCulloch CE, Thombley R, Zima BT, et al. Depression, anxiety, and emergency department use for asthma. Pediatrics. (2019) 144:e20190856. doi: 10.1542/peds.2019-0856
13. Denlinger LC, Phillips BR, Ramratnam S, Ross K, Bhakta NR, Cardet JC, et al. Inflammatory and comorbid features of patients with severe asthma and frequent exacerbations. Am J Respir Crit Care Med. (2017) 195:302–13. doi: 10.1164/rccm.201602-0419OC
14. Liu Y, Liu S, Xu Z, Yin J, Shen K. Progress of comorbidities of asthma in children. Int J Pediatr. (2023) 50:575–9. doi: 10.3760/cma.j.issn.1673-4408.2023.09.001
15. Kulikova A, Lopez J, Antony A, Khan DA, Persaud D, Tiro J, et al. Multivariate association of child depression and anxiety with asthma outcomes. J Allergy Clin Immunol Pract. (2021) 9:2399–405. doi: 10.1016/j.jaip.2021.02.043
16. Licari A, Andrenacci B, Di Cicco ME, Leone M, Marseglia GL, Tosca M. Respiratory comorbidities in severe asthma: focus on the pediatric age. Expert Rev Respir Med. (2023) 17:1–13. doi: 10.1080/17476348.2023.2168261
17. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. (1980) 20:649–55. doi: 10.1093/geront/20.6.649
18. Adib-Hajbaghery M, Ahmadi B. Caregiver burden and its associated factors in caregivers of children and adolescents with chronic conditions. Int J Commun Based Nurs Midwifery. (2019) 7:258–69. doi: 10.30476/ijcbnm.2019.73893.0
19. Hua K, Yu M, Xu S. The mediating effect of primary caregivers' self-efficacy on the influence of coping style on quality of life in children with asthma. Mod Clin Nurs. (2021) 20:14–8. doi: 10.3969/j.issn.1671-8283.2021.9.03
20. Alduraywish SA, Lodge CJ, Campbell B, Allen KJ, Erbas B, Lowe AJ, et al. The march from early life food sensitization to allergic disease: a systematic review and meta-analyses of birth cohort studies. Allergy. (2016) 71:77–89. doi: 10.1111/all.12784
21. Özçeker D, Uçkun U, Islamova D, Tamay Z, Güler N. Corticosteroid phobia among parents of asthmatic children. Turk J Pediatr. (2018) 60:142–6. doi: 10.24953/turkjped.2018.02.004
22. Hou F, Bai Y, Li F, Wu X, Wei Q, Sun Z. The relationship between social support, family closeness, adaptability and depression in caregivers of children with bronchial asthma. J Int Psychiatry. (2024) 51:594–6, 602. Available online at: https://d.wanfangdata.com.cn/periodical/ChVQZXJpb2RpY2FsQ0hJMjAyNTA2MjISEmd3eXgtanNieDIwMjQwMjA2MhoIa3h6eHA5dWc%3D
23. Chen J, Chu X, Li Y, Wu L, Song F. The influence of social support on the family cohesion adaptability and depression level of parents of children with bronchial asthma. Mater Child Health Care China. (2021) 36:1865–8. doi: 10.19829/j.zgfybj.issn.1001-4411.2021.08.051
24. Gibson PG, McDonald VM, Granchelli A, Olin JT. Asthma and comorbid conditions-pulmonary comorbidity. J Allergy Clin Immunol Pract. (2021) 9:3868–75. doi: 10.1016/j.jaip.2021.08.028
25. Li Q, Zhang L, Xi X. Analysis of influencing factors related to the burden felt by caregivers of children with asthma. Sichuan J Physiol Sci. (2021) 43:385–7. Available online at: https://d.wanfangdata.com.cn/periodical/ChVQZXJpb2RpY2FsQ0hJMjAyNTA2MjISEXNjc2xreHp6MjAyMTAzMDExGgh6dzJpdDMxcw%3D%3D
26. Zhang J, Xu Y, Ao Z, Li C, Liao C, Huang Y, et al. An analysis of the current situation of the caregiving burden of caregivers of children with asthma in heyuan city and related factors. China Health Ind. (2021) 18:28–31, 5. doi: 10.16659/j.cnki.1672-5654.2021.16.028
27. Chang M, Xu S. Analysis of the current status and influencing factors of the care burden of the main caregivers of children with asthma. Jilin Med J. (2022) 43:1106–10. doi: 10.3969/j.issn.1004-0412.2022.04.096
28. Yang F, Zhou J, Xiao H, Wu X, Cui Y, Huang H, et al. Caregiver burden among parents of school-age children with asthma: a cross-sectional study. Front Public Health. (2024) 12:1368519. doi: 10.3389/fpubh.2024.1368519
29. Ni P, Chen J, Liu N. The sample size estimation in quantitative nursing research. Chin J Nurs. (2010) 45:378–80. doi: 10.3761/j.issn.0254-1769.2010.04.037
30. Wang L, Yang X, Hou Z, Feng Q, Marui E. Application and evaluation of Chinese version of zarit caregiver burden interview. Chin J Public Health. (2006) 22:970–2. doi: 10.3321/j.issn:1001-0580.2006.08.040
31. Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. (1990) 55:610–7. doi: 10.1207/s15327752jpa5503&;4_17
33. China NBoSo. Convenience Sampling in Statistical Surveys (2023). Available online at: https://www.stats.gov.cn/WZWSREL3pzL3RqbGwvdGp4amJnbi8yMDIzMTEvdDIwMjMxMTE0XzE5NDQ0OTQuaHRtbA== (Accessed October 5, 2025).
34. Lu S, Xie W. Influencing factors of caregiving burden of parents of children with acute exacerbation of bronchial asthma and its relationship with coping mode. Henan Med Res. (2022) 31:3103–7. doi: 10.3969/j.issn.1004-437X.2022.17.008
35. Liu W, Lin X, Shao X, Wu X, Wang D, Liu L, et al. Study on the correlation between care burden, fatigue and coping styles of caregivers of children with chronic lung disease. Acad J Guangzhou Med College. (2022) 50:156–60. doi: 10.3969/j.issn.2095-9664.2022.03.31
36. Kobos E, Imiela J. Factors affecting the level of burden of caregivers of children with type 1 diabetes. Appl Nurs Res. (2015) 28:142–9. doi: 10.1016/j.apnr.2014.09.008
37. Yang L, Cui Y. Investigation on mental health status of parents of asthmatic children and its association with social factors. Mod Med J. (2018) 46:930–2. doi: 10.3969/j.issn.1671-7562.2018.08.022
38. Griva K, Goh CS, Kang WCA Yu ZL, Chan MC, Wu SY, et al. Quality of life and emotional distress in patients and burden in caregivers: a comparison between assisted peritoneal dialysis and self-care peritoneal dialysis. Qual Life Res. (2016) 25:373–84. doi: 10.1007/s11136-015-1074-8
39. Chiou CJ, Chang HY, Chen IP, Wang HH. Social support and caregiving circumstances as predictors of caregiver burden in Taiwan. Arch Gerontol Geriatr. (2009) 48:419–24. doi: 10.1016/j.archger.2008.04.001
40. Ding L, Lin M, Zhang Q, Wang ZH, Shi JH. Survey and analysis of the present situation of caregivers' caring activities and supportive behaviors of family caregivers for patients with diabetic kidney disease. Chin J Mod Nurs. (2021) 27:2981–7. doi: 10.3760/cma.j.cn115682-20201021-05843
41. Akbar Z, Aisyawati MS. Coping strategy, social support, and psychological distress among university students in Jakarta, Indonesia during the covid-19 pandemic. Front Psychol. (2021) 12:694122. doi: 10.3389/fpsyg.2021.694122
42. Lee KC, Yiin JJ, Chao YF. Effect of integrated caregiver support on caregiver burden for people taking care of people with cancer at the end of life: a cohort and quasi-experimental clinical trial. Int J Nurs Stud. (2016) 56:17–26. doi: 10.1016/j.ijnurstu.2016.01.002
43. Yang T, Huang X, Cai K, Zhou X. The psychological stress status of the main caregivers of children with bronchial asthma. South China J Prev Med. (2021) 47:105–8. doi: 10.12183/j.scjpm.2021.0105
44. Gao G, Guo M, Guo J, Wen L, Li J. Qualitative study on burden of caregiver of children with asthma. Chin J Pract Nurs. (2015) 31:984–7. doi: 10.3760/cma.j.issn.1672-7088.2015.13.015
45. McCann D, Bull R, Winzenberg T. The daily patterns of time use for parents of children with complex needs: a systematic review. J Child Health Care. (2012) 16:26–52. doi: 10.1177/1367493511420186
46. Li S, Lu Q, Huang L. Research progress on the care burden of primary caregivers of children with bronchial asthma. Chin General Pract Nurs. (2024) 22:2238–42. doi: 10.12104/j.issn.1674-4748.2024.12.014
47. Tu S, Miao X, Geng D, Zeng Y, Li Y, Yang R. The influencing factors of burdens in caregivers of patients with amyotrophic lateral sclerosis. Mod Clin Nurs. (2018) 17:7–13. doi: 10.3969/j.issn.1671-8283.2018.11.002
48. Jiang F, Wang W, Wang Q, Tang S. The care feelings of caregivers of elderly patients with dementia. Chin J Gerontol. (2014) 34:759–62. doi: 10.3969/j.issn.1005-9202.2014.03.089
49. Chen R, Yang W, Wu L. Influence factor of primary burden in family members of hospitalized brain tumor patients. Mod Oncol Med. (2016) 24:1633–6. doi: 10.3969/j.issn.1672-4992.2016.10.035
50. Ughasoro MD, Eze JN, Oguonu T, Onwujekwe EO. Burden of childhood and adolescence asthma in Nigeria: disability adjusted life years. Paediatr Respir Rev. (2022) 41:61–7. doi: 10.1016/j.prrv.2021.07.004
51. Liu W, Jiang N, Li Y, Cheng S. Status and influencing factors of learned helplessness in patients with multiple chronic conditions in the community. J Nurs Sci. (2025) 40:12–59. doi: 10.3870/j.issn.1001-4152.2025.07.012
52. Patel MR, Leo HL, Baptist AP, Cao Y, Brown RW. Asthma outcomes in children and adolescents with multiple morbidities: findings from the national health interview survey. J Allergy Clin Immunol. (2015) 135:1444–9. doi: 10.1016/j.jaci.2014.11.008
53. Mirabelli MC, Hsu J, Gower WA. Comorbidities of asthma in US children. Respir Med. (2016) 116:34–40. doi: 10.1016/j.rmed.2016.05.008
54. Kantipuly A, Pillai MR, Shroff S, Khatiwala R, Raman GV, Krishnadas SR, et al. Caregiver burden in primary congenital glaucoma. Am J Ophthalmol. (2019) 205:106–14. doi: 10.1016/j.ajo.2019.05.003
55. Dai M, Zhao X, Li J, Chen C, Zheng J, Wang Q, et al. Research on the current situation and influencing factors of caregivers' burden and social support for children with autism in Mianyang area. Chin General Pract Nurs. (2024) 22:4307–11. doi: 10.12104/j.issn.1674-4748.2024.22.037
56. Xu W, Li H. Analysis of the current status and influencing factors of the care burden for the main caregivers of patients with idiopathic pulmonary fibrosis*. China J Mod Med. (2021) 31:58–64. doi: 10.3969/j.issn.1005-8982.2021.04.010
57. Qi S, Dong M. Research status on the care burden of the main caregivers of children with chronic diseases in pediatrics. Tianjin J Nurs. (2020) 28:244–7. doi: 10.3969/j.issn.1006-9143.2020.02.041
58. Pedraza AM, Rodríguez-Martínez CE, Acuña R. [Initial validation of a scale to measure the burden for parents/caregivers of children with asthma and factors associated with this burden in a population of asthmatic children]. Biomedica. (2013) 33:361–9. doi: 10.7705/biomedica.v33i3.813
59. Peay HL, Meiser B, Kinnett K, Furlong P, Porter K, Tibben A. Mothers' psychological adaptation to Duchenne/Becker muscular dystrophy. Eur J Hum Genet. (2016) 24:633–7. doi: 10.1038/ejhg.2015.189
60. Tay TR, Radhakrishna N, Hore-Lacy F, Smith C, Hoy R, Dabscheck E, et al. Comorbidities in difficult asthma are independent risk factors for frequent exacerbations, poor control and diminished quality of life. Respirology. (2016) 21:1384–90. doi: 10.1111/resp.12838
61. Dixon AE, Kaminsky DA, Holbrook JT, Wise RA, Shade DM, Irvin CG. Allergic rhinitis and sinusitis in asthma: differential effects on symptoms and pulmonary function. Chest. (2006) 130:429–35. doi: 10.1378/chest.130.2.429
62. Parikh K, Paul J, Fousheé N, Waters D, Teach SJ, Hinds PS. Barriers and facilitators to asthma care after hospitalization as reported by caregivers, health providers, and school nurses. Hosp Pediatr. (2018) 8:706–17. doi: 10.1542/hpeds.2017-0182
63. Paller AS, Weidinger S, Capozza K, Pink AE, Tang M, Guillaume X, et al. Similarities and differences in the perception of atopic dermatitis burden between patients, caregivers, and independent physicians (ad-gap survey). Dermatol Ther. (2023) 13:961–80. doi: 10.1007/s13555-022-00850-7
64. Foronda CL, Kelley CN, Nadeau C, Prather SL, Lewis-Pierre L, Sarik DA, et al. Psychological and socioeconomic burdens faced by family caregivers of children with asthma: an integrative review. J Pediatr Health Care. (2020) 34:366–76. doi: 10.1016/j.pedhc.2020.02.003
65. Li N, Chen L, Ding L, Chen X, Yao D, Wu Y, et al. Analysis of the burden of main caregivers of preschool children with scoliosis and its influencing factors. World Latest Med Inform. (2019) 19:177–9. doi: 10.19613/j.cnki.1671-3141.2019.20.088
Keywords: asthma, comorbidity, caregiver burden, parents, caregivers
Citation: Yi X, Sunzi K, Liu J, Yang F, Wu X, Bi D, Huang Q and Dai L (2025) Caregivers' burden and its influencing factors among parents of children with asthma and comorbidities: a cross-sectional study. Front. Public Health 13:1698723. doi: 10.3389/fpubh.2025.1698723
Received: 04 September 2025; Accepted: 23 October 2025;
Published: 07 November 2025.
Edited by:
Margherita Neri, University of Ferrara, ItalyReviewed by:
Stephen Hughes, The University of Sydney, AustraliaUshapriya Mathiazhakan, SRM Institute of Science and Technology (Deemed to be University) College of Nursing, India
Copyright © 2025 Yi, Sunzi, Liu, Yang, Wu, Bi, Huang and Dai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Yang, MzI5ODcxNTgwQHFxLmNvbQ==; Qin Huang, ODY1MTcwNzE1QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xin Yi
Xin Yi Kejimu Sunzi
Kejimu Sunzi Jie Liu3
Jie Liu3 Fang Yang
Fang Yang Lifei Dai
Lifei Dai