- 1College of Architecture and Urban Planning, Fujian University of Technology, Fuzhou, China
- 2Key Laboratory of New Technology for Construction of Cities in Mountain Area, Ministry of Education, Chongqing University, Chongqing, China
Population aging presents a critical challenge for urban sustainability and health equity. This study addresses the structural mismatch between the spatial distribution of older adults and health resources in Fuzhou, China, by developing an Agent-Based Model (ABM) to simulate the utilization of prevention, treatment, and long-term care facilities and its impact on health outcomes. The model, grounded in empirical questionnaire data and real-world spatial data, incorporates older adults as mobile agents with diverse health, economic, and living statuses, navigating a realistic urban environment over a 500-day simulation. This research designed a conceptual framework capturing the dynamic feedback between facility usage and health status. Four intervention scenarios, Multi-functional Community Centers (S1), Senior-Friendly Transportation Policies (S2), Community-based Health Education (S3), and a Comprehensive package (S4), were tested. Results indicate that spatial accessibility is the paramount driver of health improvement, with S2 (transport support) and S4 (comprehensive) demonstrating the most significant and rapid gains. Health equity, assessed via a weighted Gini coefficient, showed that while S4 achieved the most robust equity improvements across health and economic strata, its effect on residential disparities was limited. S1 risked exacerbating inequities if not precisely targeted, and S3 showed the least efficacy. The study concludes that optimizing health resources for aging populations requires a spatially-anchored, multi-dimensional strategy that prioritizes transportation accessibility, precision facility siting, and integrated service provision to effectively overcome “last-mile” barriers and address the complex needs of socioeconomically diverse older adults.
1 Introduction
Population aging has become a defining global challenge of the 21st century, profoundly reshaping societal development trajectories worldwide (1). As the developing country undergoing the most rapid and extensive demographic aging, China is compelled to evolve from providing basic support for older adults to ensuring high-quality aged care, a crucial objective in modernizing national governance (2). The Outline of the Healthy China 2030 Initiative identifies older adults as a priority group and explicitly calls for establishing an integrated health security system that spans prevention, diagnosis, treatment, rehabilitation, and long-term care (3). Achieving comprehensive health security throughout later life requires optimizing the allocation of health resources for older adults across prevention, treatment, and supportive care dimensions, thereby addressing the “last-mile” delivery challenges in health services (4).
Health resources for older adults encompass urban resources with social or natural attributes that promote physical and mental well-being in daily life. These include park spaces, medical institutions, and older adults care facilities, which older adults utilize either actively or passively to maintain health (5). Research on allocating these resources is grounded in public service distribution theory, often focusing on single-type facilities while incorporating the dual perspectives of “older adults” and “health resources” (6). Such studies span allocation standards (7), spatial distribution (8), evaluation and optimization (9), and service performance (10, 11). For instance, spatial equity of community-based care facilities in Shanghai was assessed using Gini coefficients and Lorenz curves (12), while embedded care facilities in Tianjin were shown to significantly improve life satisfaction through social and environmental factors (13). Recent behavioral studies have further explored how daily activities influence health, guiding contextualized facility planning (14). Examples include SEM modeling of park features affecting health behaviors in Zhengzhou (15) and machine learning analyses of health behaviors among ethnic older adults in rural Hunan (16).
Despite these advances, current research overly emphasizes spatial layout and service efficiency, paying insufficient attention to health outcomes (17), such as chronic disease intervention, and offering incomplete theoretical-practical frameworks for integrating full-chain health security into resource planning (18, 19). Crucially, health equity remains underexplored (20–22), particularly regarding systematic disparities in health opportunities and resource accessibility influenced by income, location, and baseline health (23, 24). In terms of methodological approaches to health equity assessment, a systematic comparison of various measurement tools, including the Gini coefficient and concentration index, has highlighted their respective applicability and limitations (25). Furthermore, growing attention has been directed toward the health effects of policy interventions. For instance, rigorous causal inference analyses have demonstrated that clean heating policies significantly reduced the incidence of respiratory diseases among residents. This finding not only provides empirical support for the synergistic optimization of environmental and health resources, but also underscores the necessity of multidimensional health intervention strategies. The observed disparities in the distribution of health benefits across different groups further offer critical evidence for evaluating the equity impacts of public policies (26).
Agent-Based Modeling (ABM) presents a promising approach to address these gaps (27, 28). ABM enables multi-scale simulation of human-environment interactions with minimal data input and supports low-cost, multi-scenario testing for spatial strategy optimization (29, 30). Its key strength lies in dynamically integrating behavioral theories with spatial contexts to simulate complex systems, thereby supporting empirical and applied studies (31). For instance, in a health policy application, a multi-theory ABM simulated health-seeking behaviors and diagnostic delays among diabetes patients. Scenario analyses demonstrated that targeted interventions, such as gender-specific health campaigns or improved primary care access, could substantially reduce late diagnosis rates, offering both theoretical insights and practical decision support for regional disease control strategies (32). Although ABM has been applied to simulate outdoor activities of older adults in Shenzhen (33) and demand-response in community care centers (34), few studies model the dynamic feedback between individual behaviors, such as facility use, and long-term health outcomes (35).
This study aims to bridge this gap by employing ABM, combined with questionnaire surveys and spatial analysis, to simulate health outcomes resulting from older adults’ utilization of prevention, treatment, and long-term care facilities in urban Fuzhou. It conceptualizes the “last mile” as the composite of bottlenecks occurring at the final stage of health resource access for older adults (36, 37). While recognizing the multidimensional nature of these barriers, the study operationalizes the concept by focusing specifically on spatial accessibility, thereby transforming a broad policy metaphor into a measurable and intervenable variable within the model, in alignment with China’s national aging strategy goals (2, 5, 38).
By incorporating bidirectional feedback between facility usage and health status, this study evaluate health impacts and equity under four intervention scenarios, offering spatiotemporally adaptive pathways for optimizing health resource allocation for older adults. The four intervention scenarios include: (1) Multi-functional Community Centers (S1): Upgrading community centers into comprehensive health hubs to provide daycare, preventive screenings, and social services; (2) Senior-Friendly Transportation Policies (S2): Overcoming travel challenge through health-dedicated lines, barrier-free bus retrofits, and pedestrian environment improvements; (3) Community-based Health Education Activities (S3): Conducting health lectures and family workshops to enhance chronic disease self-management skills and preventive healthcare awareness; (4) Comprehensive Intervention Package (S4): Integrating the aforementioned three strategies to test multi-dimensional synergistic effects. All scenarios are based on empirical data, aiming to improve the accessibility of health resources from spatial, social, and cognitive dimensions.
2 Study context
2.1 Study area
The study focuses on the central urban area of Fuzhou within the Third Ring Road (Figure 1). As the capital of Fujian Province and a key city in China’s economically dynamic eastern coastal region, Fuzhou serves as the political, economic, cultural, and transportation core of both the city and the province. The study area encompasses most of Gulou, Taijiang, Cangshan, and Jin’an districts, along with part of Minhou County, forming the most densely populated and highly urbanized zone in the city, with a total area of approximately 174.21 km2. According to the Seventh National Population Census, Fuzhou has a permanent population of 8.29 million, including 1.38 million people aged 60 and above, indicating an aging rate of 16.76% (39). Fuzhou exhibits urban characteristics, such as rapid urbanization, demographic transition, and ongoing spatial restructuring, that are representative of many Chinese cities (40). Its main urban area within the Third Ring Road constitutes a typical high-density urban core with a concentrated population distribution, making it a highly relevant context for examining accessibility challenges related to health resources for older adults (27, 41).
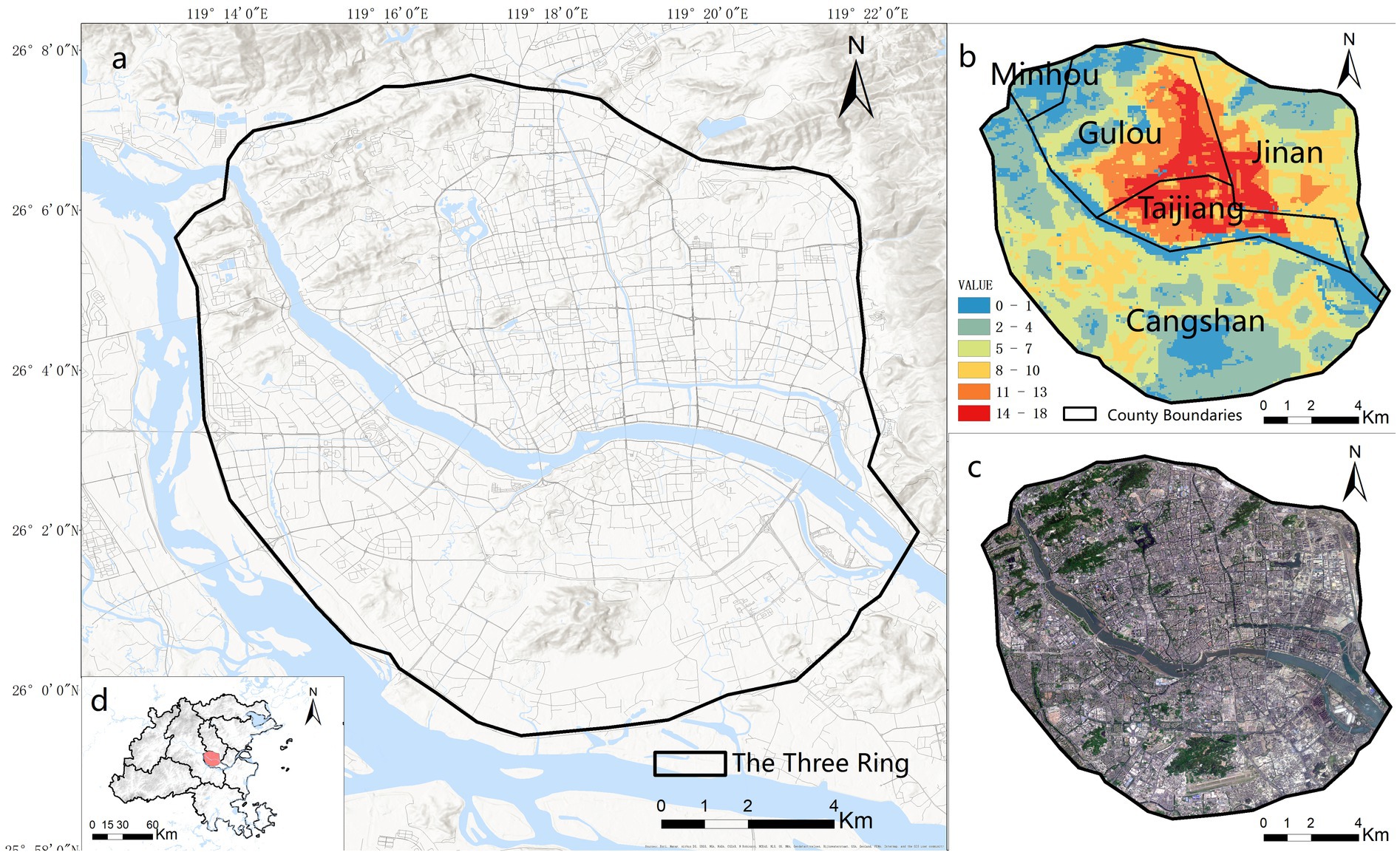
Figure 1. Location and overview of the study area. (a) Study area boundary; (b) spatial distribution of older adult population density; (c) satellite imagery; (d) geographical context of the study area within Fuzhou City. Figure 1 was generated by Esri ArcGIS 10.7 online platform (https://www.esri.com/zh-cn/arcgis/products/arcgis-desktop/overview). Sources: Esri, Maxar, Airbus DS, USGS, NGA, NASA, CGIAR, N Robinson, NCEAS, NLS, OS, NMA, Geodatastyrelsen, Rijkswaterstaat, GSA, Geoland, FEMA, Intermap, and the GIS user community.
The Fujian provincial guidelines for urban and rural older adults care facility planning and allocation proposed early guidance for tiered allocation of older adults’ care facilities across three dimensions: residential care, medical-nursing services, and recreational-cultural activities (42). As a typical aging city in Fujian, Fuzhou has implemented systematic policy adjustments for optimizing older adults health resources. The implementation plan for establishing a comprehensive older adults health service system in Fuzhou identifies preventive healthcare, disease diagnosis/treatment, and rehabilitation nursing as core tasks for building this system (43).
2.2 Conceptual framework of facility usage and health effects
Older adults, as a key target of health interventions, typically engage in limited daily activities, primarily involving physical and social interactions, medical visits, and rehabilitative care. Prevention, treatment, and long-term care facilities serve as spatial anchors for these activities, forming an integrated health promotion model that combines spatial resources and behavioral patterns to achieve closed-loop health interventions (44, 45). This study constructs a conceptual framework (Figure 2) to illustrate the dynamic relationships among older adults’ behaviors, facility usage, and health outcomes. Here, “+” denotes positive feedback that enhances health, while “–” indicates negative feedback that reduces demand. The framework incorporates three feedback mechanisms: (1) Reinforcing Loop R1: social and physical activities promote the use of preventive facilities, improving physical and mental health, which in turn encourages further activity engagement; (2) Balancing Loop B1: medical-seeking behavior leads to treatment, which improves health and reduces subsequent demand for medical services; and (3) Balancing Loop B2: use of rehabilitative care facilities aids recovery, decreasing the need for further care.
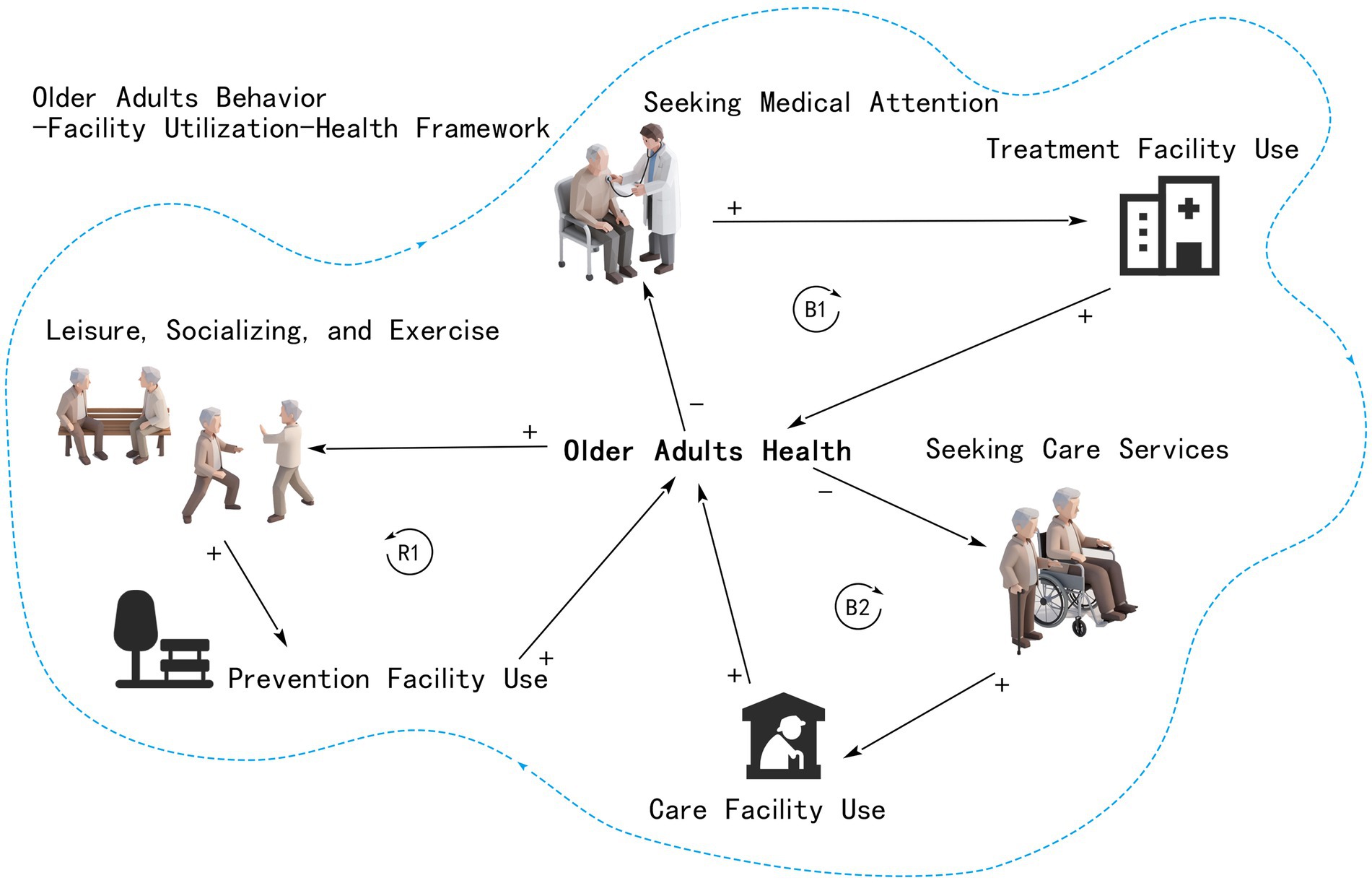
Figure 2. Conceptual framework of the feedback mechanisms between older adults’ facility usage and health outcomes. The icons and figure elements were generated using the AI image generation tool from iconfont (https://www.iconfont.cn/), and subsequently modified by the authors.
2.3 Data sources and calibration
Population data for adults aged 60 and above were sourced from WorldPop, utilizing a version calibrated with United Nations population estimates (46) and cross-validated against China’s Seventh National Population Census. Socioeconomic and health-related variables were derived from the Fuzhou population census and further supplemented and calibrated through a structured questionnaire survey.
The questionnaire data were collected using a multi-stage stratified sampling approach conducted on-site across Fuzhou’s main urban area. Sampling strata were defined by types of high-frequency activity venues commonly used by older adults, including parks and plazas, medical institutions, and older adults care facilities. A total of 350 questionnaires were distributed to adults aged 60 and above, resulting in 326 valid responses. The survey instrument captured key variables such as socioeconomic attributes, self-rated health status, travel behavior (e.g., outing frequency and travel distance), and facility usage preferences (see Appendix A1 for details). To ensure data reliability, portions of the survey responses were cross-validated with official census records, thereby strengthening sample representativeness and enhancing response validity.
Location data for public service facilities, initially classified under four major categories and eight subcategories, were acquired through the Amap POI (Point of Interest) service (https://www.amap.com). From this dataset, POIs were selected representing three key health-related functions - prevention, including parks and squares; treatment, including various medical institutions; and care, including older adults care service facilities.
3 Research methodology
The model was developed following the ODD (Overview, Design Concepts, and Details) protocol, a standardized framework for describing Agent-Based Models (ABM), which systematically outlines model structure, agent design, and operational mechanisms (47). To better capture behavioral complexity, the ODD+D extension was adopted, incorporating explicit descriptions of decision-making processes. The model was implemented using AnyLogic 8.7 Professional, leveraging its GIS capabilities to simulate agent mobility over real-road networks and to configure behavioral rules via parameter settings and Java coding.
3.1 Overview
3.1.1 Purpose
The model aims to analyze the health impacts of prevention, treatment, and long-term care facility usage among older adults with varying economic and living conditions, and to assess how interventions affect health outcomes and equity. It addresses demonstrated mismatches between the spatial distribution of older adluts populations and health resources in Fuzhou (Figure 3), where existing policies have yet to resolve persistent inequities (48).
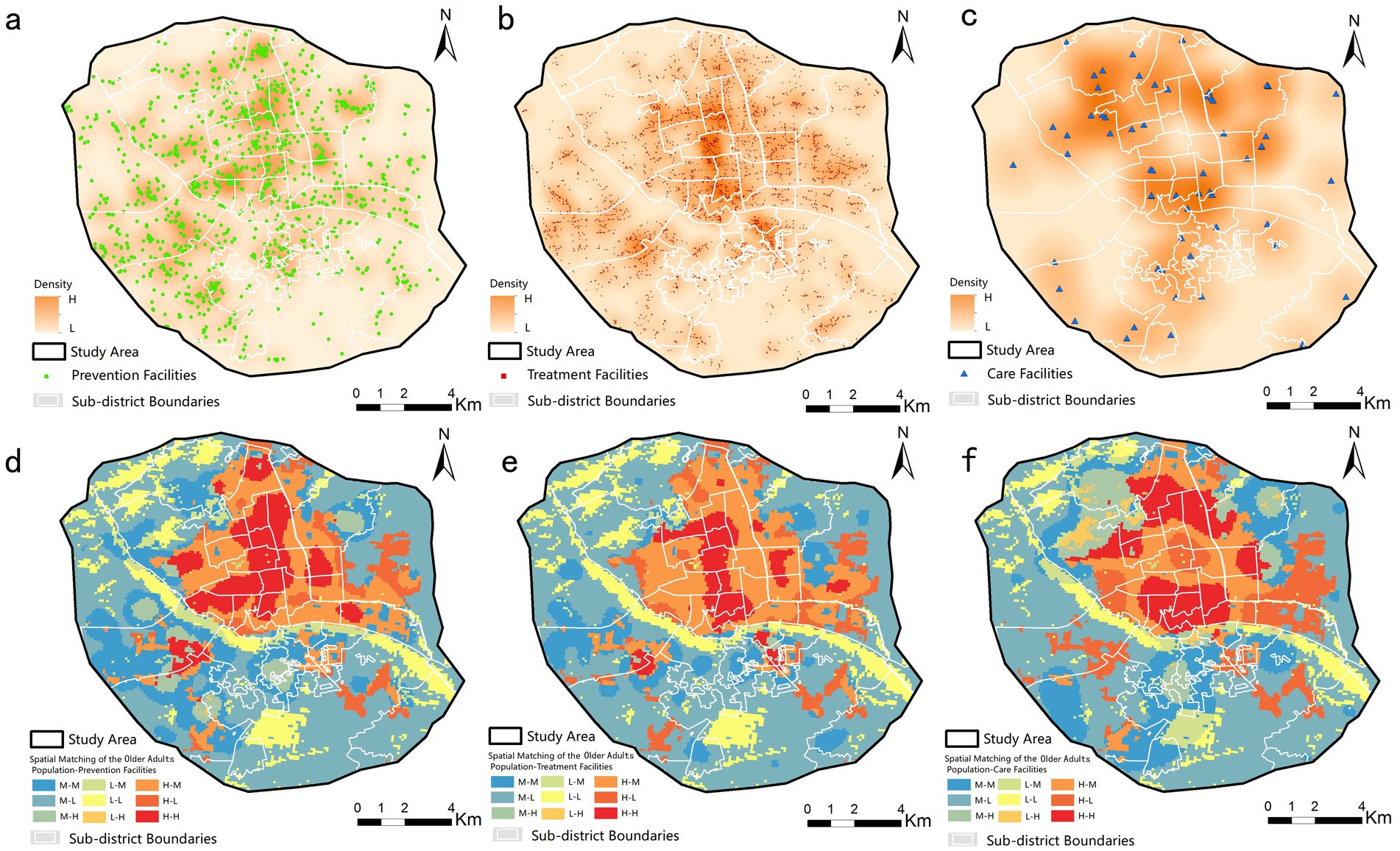
Figure 3. Spatial patterns and correlation analysis of health resources. Notes: Kernel density distribution of (a) prevention, (b) treatment, and (c) long-term care facilities. Spatial correlation between older adult population density and (d) prevention, (e) treatment, and (f) long-term care resources. Maps created with ArcGIS 10.7 (https://www.esri.com/zh-cn/arcgis/products/arcgis-desktop/overview).
3.1.2 Entities, state variables and scales
3.1.2.1 The environment
The model environment encompasses the physical and spatial context necessary for the movement of older adults and their utilization of health facilities (Figure 4). It covers the entire urban area inside the Third Ring Road in Fuzhou’s main urban zone, incorporating a real-world road network and the actual geographic distribution of health facilities based on Point of Interest (POI) data.
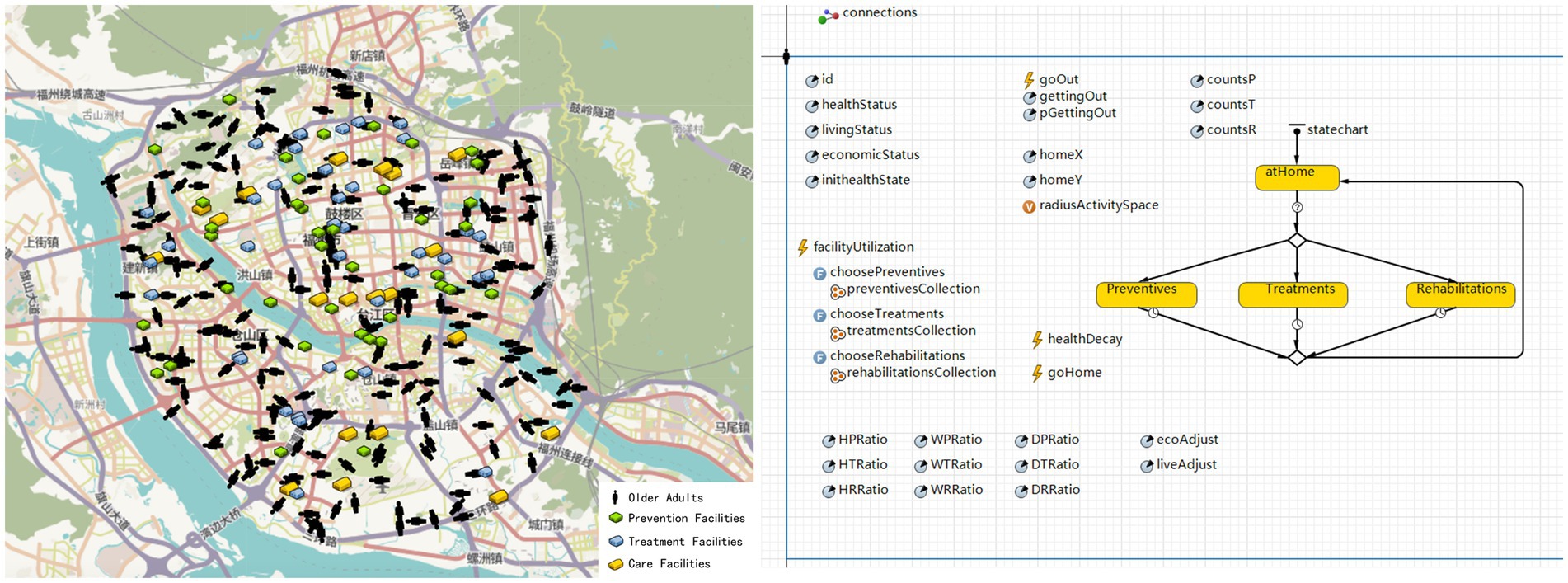
Figure 4. Model construction in AnyLogic GIS simulation environment. The base map and icons are all built-in components of the AnyLogic software.
3.1.2.2 Agents and scales
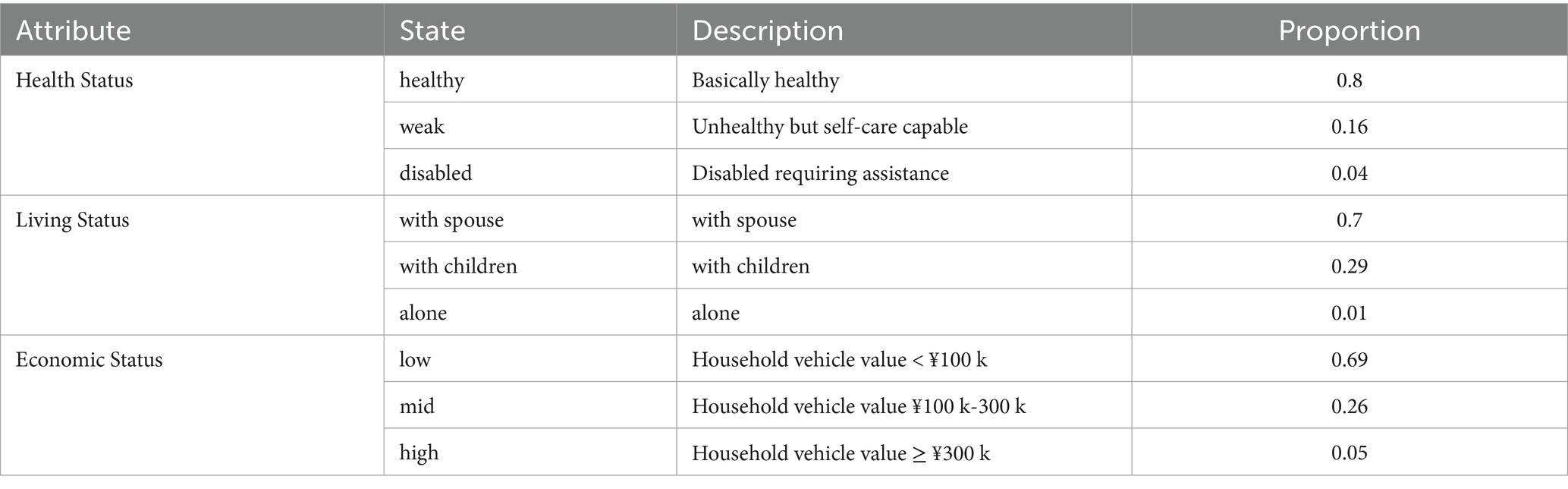
Within this environment, the model incorporates two main types of agents: older adults and health facilities. A total of 200 older adult agents are randomly generated within the study area. Each is assigned initial attributes, such as health status, economic status, and living status, based on proportions derived from Fuzhou census data and calibrated through questionnaire surveys (as summarized in Table 1). Economic status is proxied by household vehicle value, a durable good widely recognized as a proxy for wealth in survey-based studies due to its comparability and data availability (49). Value thresholds correspond to established market segments (50). For example, vehicles valued below ¥100,000 represent low-income groups (entry-level vehicles), those between ¥100,000 and ¥300,000 represent middle-income (mainstream family vehicles), and those above ¥300,000 indicate high-income households (premium vehicles). These agents navigate the real road network to make daily travel and facility choices, with their health status updating dynamically after facility visits.
In addition, the model includes 100 facility agents generated from real POI locations, distributed as 40 prevention, 40 treatment, and 20 long-term care facilities, reflecting actual urban service ratios. Each type of facility is designed to provide distinct health benefits.
The model operates at a daily time step over a simulation period of 500 days, capturing the travel behavior and facility usage patterns of the older adult agents.
3.2 Design concepts
3.2.1 Individual decision making
The decision-making processes for older adult agents in this model were designed based on empirical data obtained from questionnaires, with a primary focus on travel behavior. An analysis of 326 valid questionnaires collected from the main urban area of Fuzhou revealed that the health status of older adults exerts a significant gradient effect on both mobility and facility selection preferences. Statistical analyses—including the Kruskal-Wallis test, multivariate analysis of variance (MANOVA), and Dunn’s post hoc test—confirmed that health status significantly influences mobility capacity (Kruskal-Wallis test: p < 0.001). Specifically, healthier agents reported higher outing frequency (M = 4.69 days per week [Note: M denotes mean]) and broader travel ranges (M = 5.12 km), compared to those in the weak group (frequency M = 3.55 days, range M = 3.78 km) and the disabled group (frequency M = 2.01 days, range M = 1.02 km).
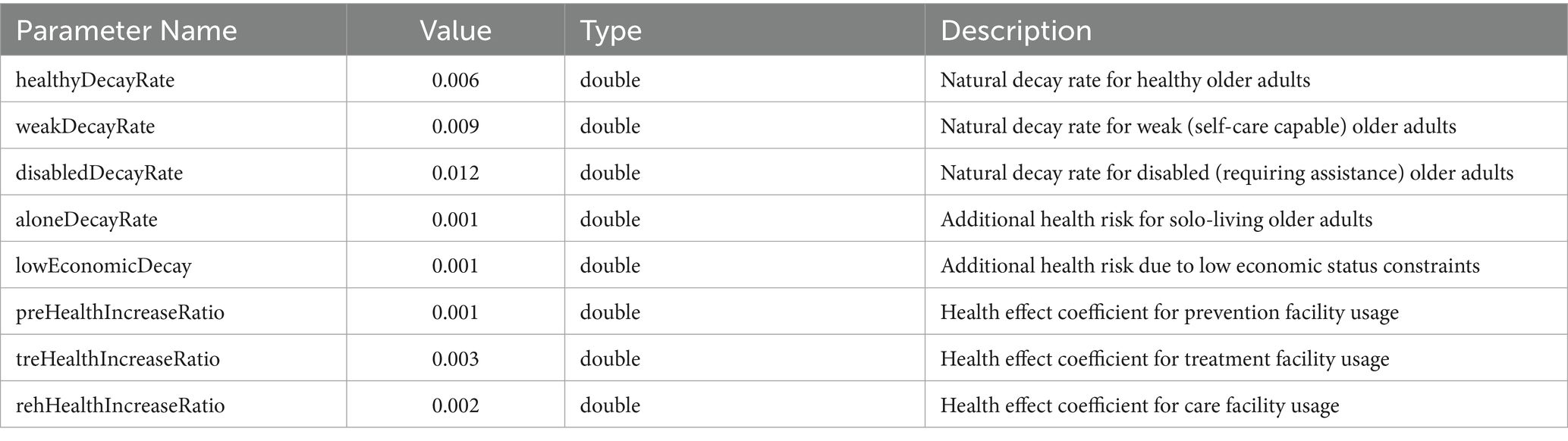
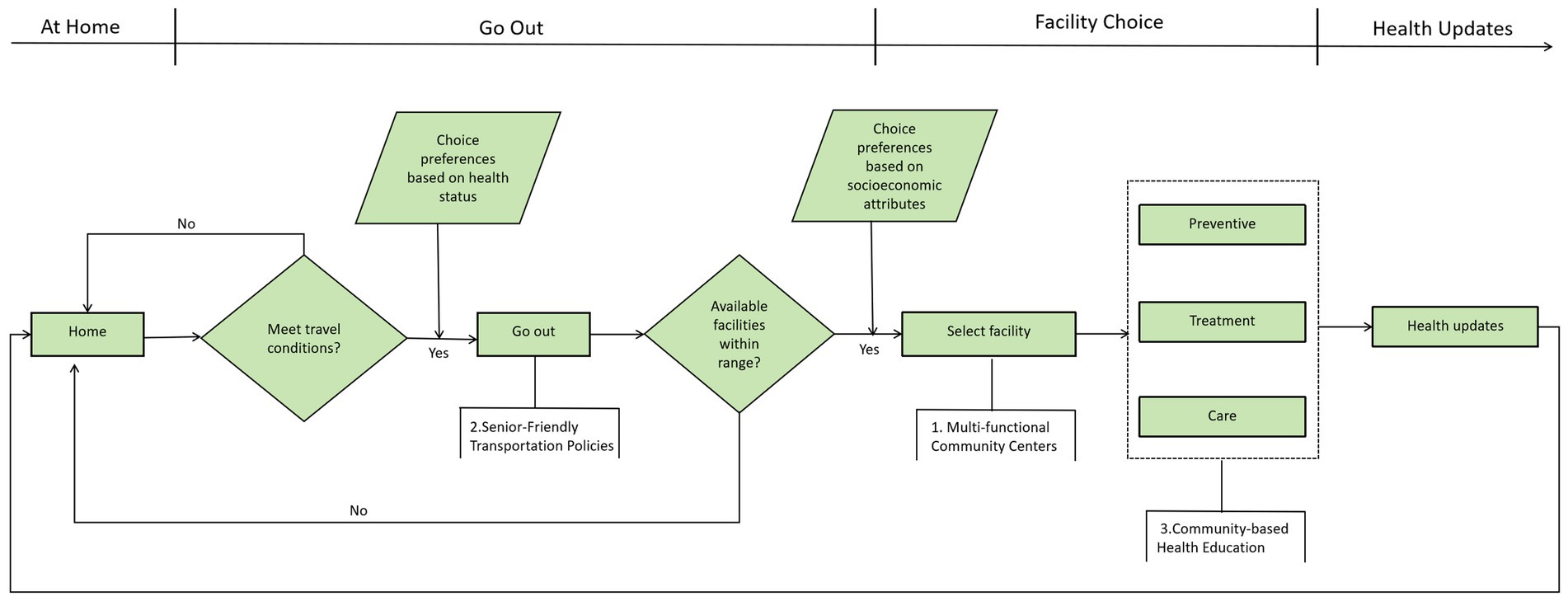
Based on these findings, the agents’ daily travel behavior is modeled according to their health status: healthy agents have a 70% probability of undertaking outings within a 5 km radius, weak agents have a 50% probability within 3 km, and disabled agents have a 30% probability within 1 km. When an outing is triggered, the agent first searches for available facilities within its activity radius and selects one at random. If no facilities are available within the radius, a secondary decision is invoked, with 50% probability, the agent will travel to the nearest facility outside the radius, otherwise, the outing is canceled.
3.2.2 Interactions
Based on empirical questionnaire data and existing literature, this study formulates agent interactions centered around the utilization of health facilities by older adults. The interactive process is defined as the use of these assistive facilities, with behavioral rules informed by evidence-based influences of health status, economic standing, and living arrangements on older adults’ preferences and demands for health resources. As summarized in Table 2, insights derived from literature review directly guide the model’s rule design. For instance, healthier older adults tend to prioritize preventive activities such as autonomous exercise and social engagement (51, 52); those with chronic conditions (categorized as “weak”) show greater dependence on treatment facilities, consistent with patterns observed in chronic care management (53, 54); while disabled older adults exhibit higher reliance on long-term care resources, reflecting necessities for sustained support (55, 56).
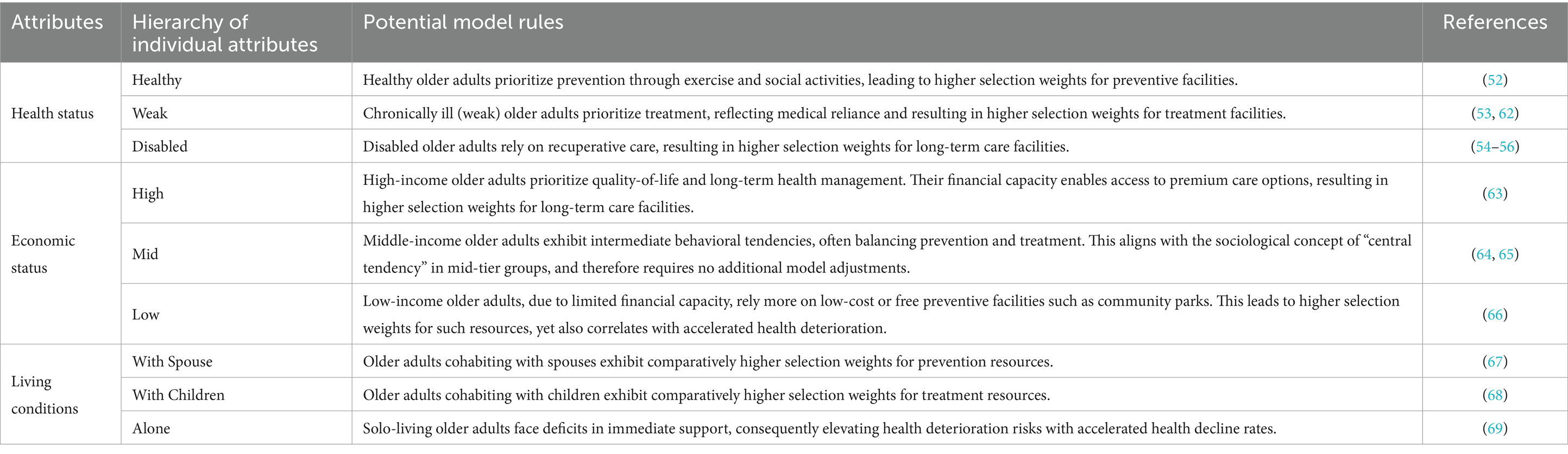
Table 2. Correspondence between influencing factors and agent-based decision rules for health resource selection.
These trends are corroborated by questionnaire findings, which confirm significant gradients in facility usage across health categories: healthier individuals prefer prevention facilities (mean usage frequency M = 4.69), those who are weak favor treatment facilities (M = 4.55), and disabled individuals predominantly use care facilities (M = 4.52), with MANOVA confirming statistically significant differences (F = 128.18, p < 0.001). Accordingly, the model operationalizes these patterns by dynamically assigning the facility-selection weights from Table 3 based on each agent’s current health status at every time step.
3.2.3 Emergence
The emergence process within the model is characterized by dynamic changes in the health status of older adult agents, represented by a continuous variable H bounded between 0 (complete unhealthiness) and 1 (optimal health) (28), which is calibrated against the older adult health assessment system of the Fuzhou Population Census following China’s Seventh National Population Census protocol (39, 57). This system classifies health status through a unified self-reported health question combined with Activities of Daily Living (ADL) criteria, with the model’s three health states corresponding precisely to census classifications: the “healthy” state (H ∈ [0.7, 1.0]) represents individuals with full functional independence requiring no help in core ADLs; the “weak” state (H ∈ [0.3, 0.7]) corresponds to those with mild to moderate impairment requiring assistance with 1–2 ADLs; and the “disabled” state (H ∈ [0.0, 0.3]) signifies severe functional limitation or dependency requiring help with 3 or more ADLs. Health updating follows a discrete-time process influenced by natural decline and facility-based improvements, formalized as:
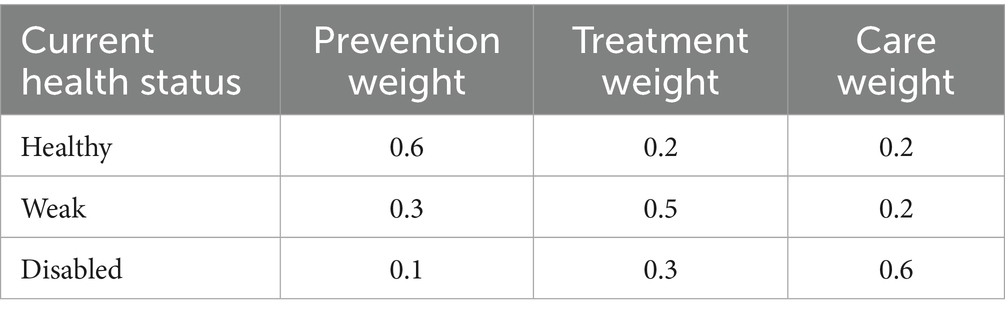
Here (Equation 1), Ht denotes the health value at day t; αHS represents the baseline health decay rate, stratified by health status; β and γ capture additional decay associated with solo living and low economic status, respectively; and δtype indicates the health gain coefficient specific to each type of health facility (prevention, treatment, or long-term care). All health values are clipped to the interval [0, 1] to enforce biological plausibility. Specific parameter values, including decay rates and facility effect coefficients, are provided in Table 4.
To evaluate equity implications emerging from agent interactions, a weighted Gini coefficient is applied across three core health equity indicators, improving upon conventional two-group inequality measures (58), formalized as:
This metric incorporates observations x₁, x₂, x₃, weighted by w₁, w₂, w₃, derived from demographic proportions reported in the Fuzhou population census, enabling a finer-grained assessment of distributional fairness in health outcomes (Equation 2). The observed values (x₁, x₂, x₃) represent the average health values of the model outputs for subpopulations of agents with different attributes. These subpopulations are categorized based on three types of individual attributes: initial health status (x₁-healthy, x₂-weak, x₃-disabled), income level (x₁-high, x₂-mid, x₃-low), and living status (x₁-with spouse, x₂-with children, x₃-alone). The calculation method is identical for each attribute and is performed separately. The weights (w₁, w₂, w₃) are derived from the actual census data of the main urban area of Fuzhou City, as shown in Table 1. They represent the actual proportion of each of the aforementioned subpopulations within the total population of the main urban area of Fuzhou City.
3.3 Design details
3.3.1 Initialization
During the initialization phase, older adult agents are randomly distributed across the area within Fuzhou’s Third Ring Road. Each agent follows a daily cycle that includes deciding whether to go out, selecting and traveling to a facility, returning home, and updating their health status accordingly. The travel and facility selection process is guided by the logic depicted in Figure 5.
3.3.2 Submodels
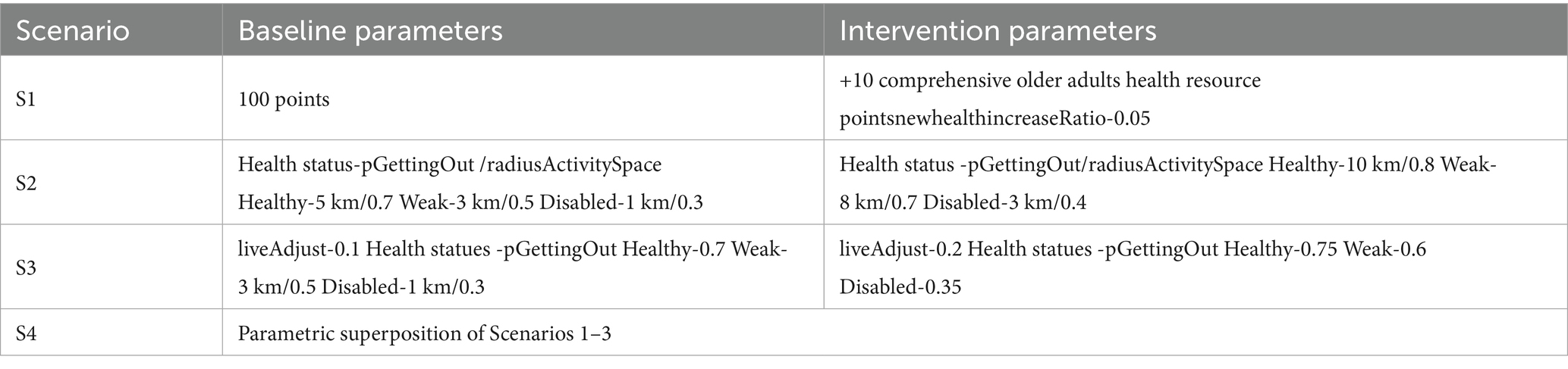
Building upon this baseline model, four intervention scenarios are implemented as submodels to evaluate the effects of policy interventions across spatial, social, and familial dimensions on health outcomes among older adults.
3.3.2.1 Scenario 1: multi-functional community centers
In line with China’s “aging-in-place” agenda, this scenario scales up Fuzhou’s flagship “Older-Adult Canteen + School” and “Community-Embedded Older-Adult Care” programs. Ten strategically chosen community centers are upgraded into one-stop health hubs, represented in the model by ten new facility agents whose placement algorithm priorities the largest service-coverage gaps. Each hub bundles daycare, recuperative care, preventive screenings and socialization spaces, delivering compound health benefits that exceed the sum of their parts.
3.3.2.2 Scenario 2: senior-friendly transportation policies
To dismantle the “last-mile” mobility barrier, this intervention deploys a comprehensive senior-friendly transportation package, such as free or low-fare dedicated health-transit lines, barrier-free bus retrofits (low-floor boarding, priority seating, audible/visual announcements), community micro-circulation shuttles with flexible routing and on-demand stops, and pedestrian upgrades, designed to create a low-stress travel chain from home to facility. In the agent-based model, these improvements are operationalized by increasing two core parameters: the daily outing probability (pGettingOut) and the activity radius (radiusActivitySpace). By explicitly translating the multidimensional “last-mile” concept into these measurable behavioral rules, S2 enhances spatial accessibility and facilitates the utilization of previously unreachable health facilities, enabling a precise assessment of its policy impact.
3.3.2.3 Scenario 3: community-based health education
This scenario deploys a multi-format curriculum, such as on-site workshops, short-form videos and family-oriented seminars, aimed simultaneously at older adults and their adult children. The content stresses chronic disease self-management and nurtures intergenerational support norms. Rather than adding new facilities, the model re-weights existing ones. For example, community centers offering recurrent health literacy sessions receive higher selection probabilities, translating gains in awareness into measurable upticks in preventive care uptake.
3.3.2.4 Scenario 4: comprehensive interventions
This scenario overlays the three preceding strategies (S1, S2, S3) through a rule-based parametric superposition. Specifically, for parameters of the same category present in multiple scenarios, the maximum value is selected (e.g., pGettingOut, radiusActivitySpace). The remaining parameters and model adjustments, such as the addition of new facility agents from S1, are cumulatively incorporated.
All resulting parameter adjustments are documented in full detail in Table 5, ensuring transparent replication of the integrated model run. Following multiple simulation runs with exclusion of the initial 60-day model burn-in period, results from the ABM were systematically evaluated across two core dimensions: (1)Health status, quantified by the health indicator H (range: 0–1; 0 = complete unhealthiness, 1 = optimal health); and (2) Health equity, measured via Gini coefficients (range: 0–1; 0 = perfect equity) across three socioeconomic status: initial health status (Healthy/Weak/Disabled), economic status (Low/Mid/High), and residential conditions (With spouse/With children/Alone). The results synthesize the impacts of four interventions—S1 (Multi-functional Community Centers), S2 (Senior-Friendly Transportation Policies), S3 (Community-based Health Education), and S4 (Comprehensive Intervention)—on health outcomes and equitable resource access for older adults in Fuzhou’s urban core.
4 Results
4.1 Spatial accessibility: the primary driver of population health gains
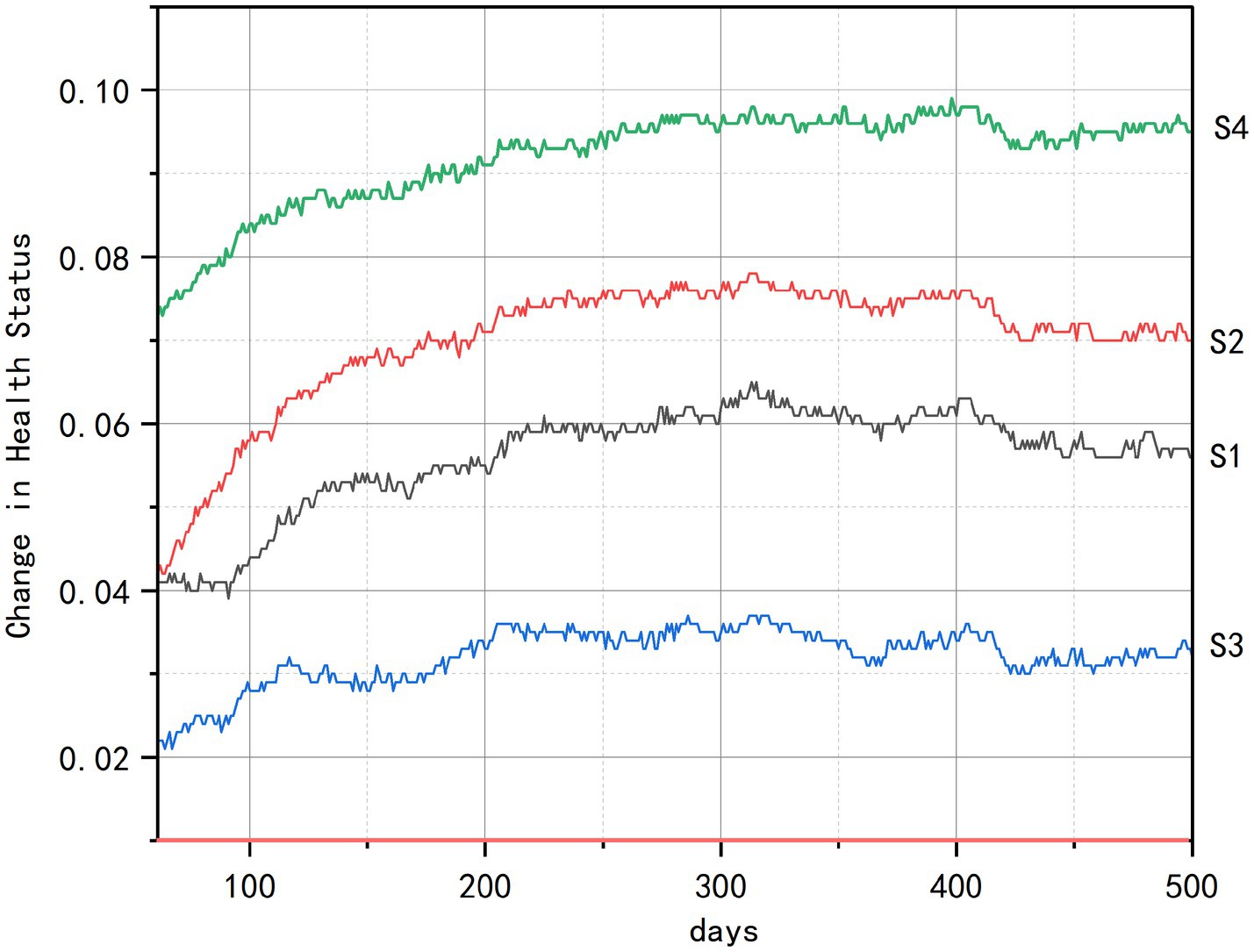
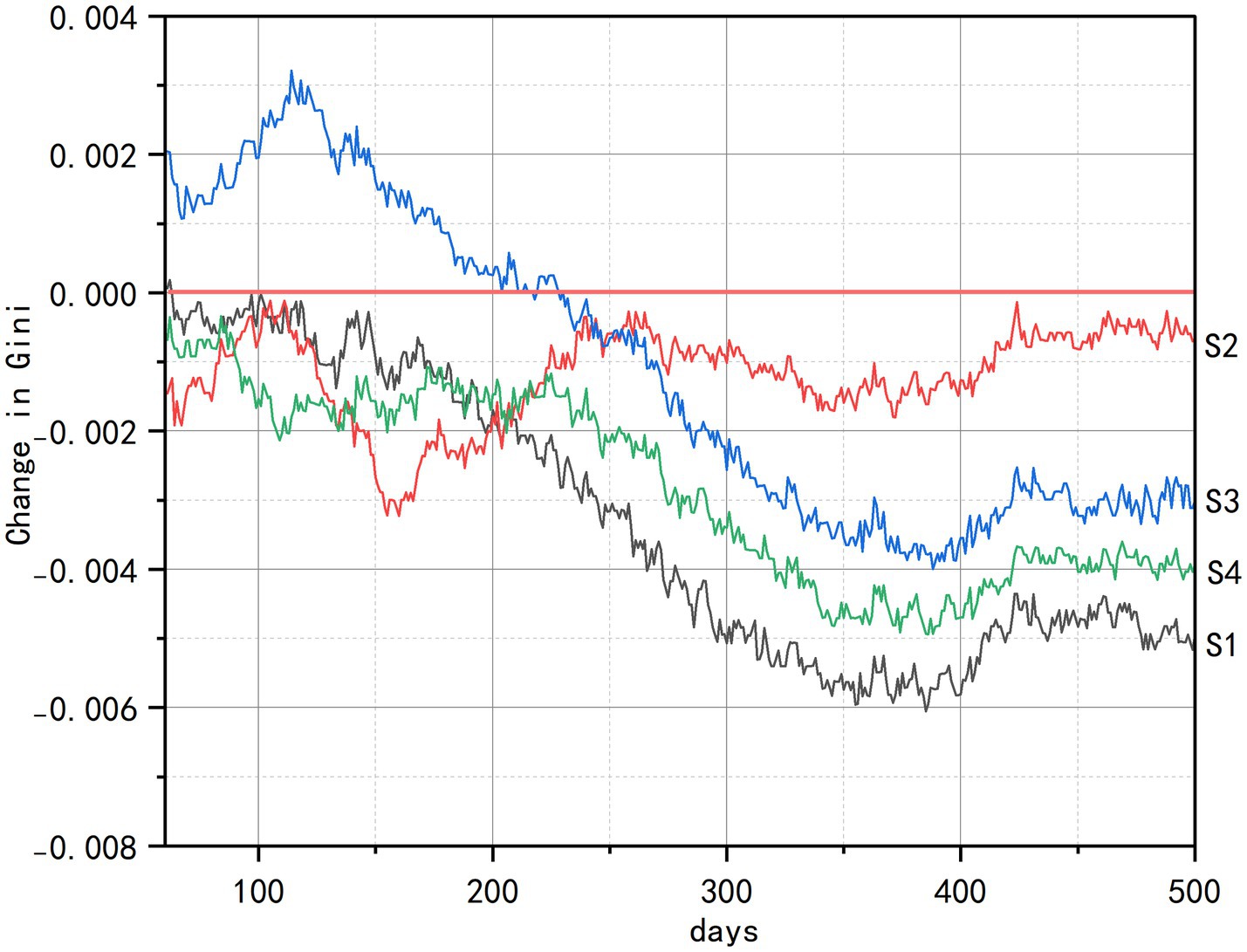
As evidenced in Figure 6, all intervention scenarios generated significant health improvements relative to the baseline (0.0), with spatial accessibility emerging as the paramount determinant of health gains. The comprehensive intervention (S4) achieved the most substantial overall improvement by synergistically integrating multidimensional strategies. Among the standalone interventions, the senior-friendly transportation policy (S2) demonstrated the most rapid health improvement, distinguished by the steepest ascent in its curve during the initial simulation period (approximately days 60–100).
These strong positive results, combined with consistent benefits across the older adult population, demonstrate the critical importance of improving spatial accessibility to overcome ‘last-mile’ mobility barriers. Community center repurposing (S1) ranked second in effectiveness by expanding daily health maintenance opportunities, though its impact remained constrained by service radius limitations that restricted usage frequency. In contrast, the community-based health education (S3) exhibited the weakest momentum and earliest stagnation plateau, reflecting significant vulnerability to individual variability in knowledge conversion efficiency driven by uncontrolled factors such as educational disparities. The consistent efficacy hierarchy observed (S4 > S2 > S1 > S3), further reinforces spatial accessibility as the foundational catalyst for health optimization.
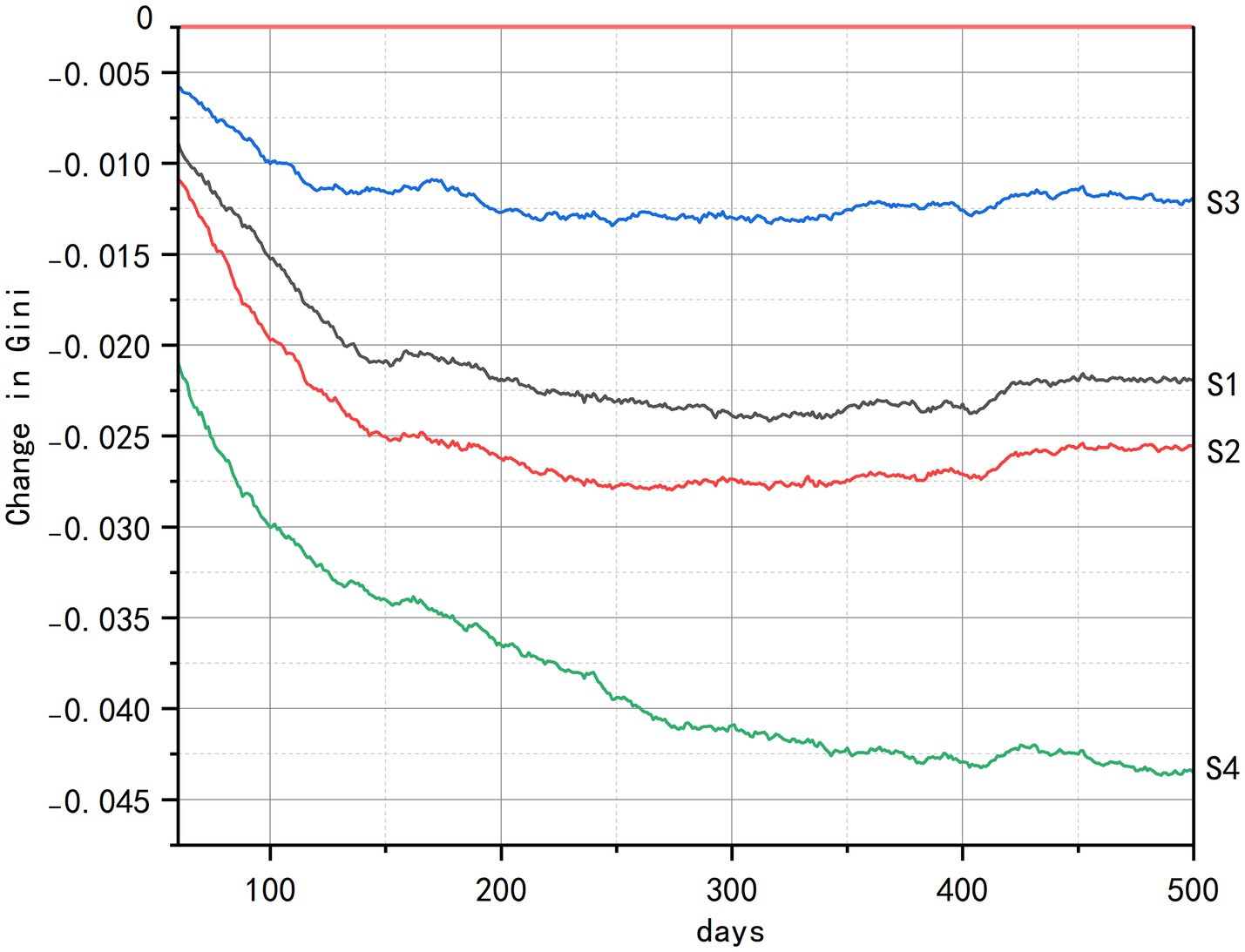
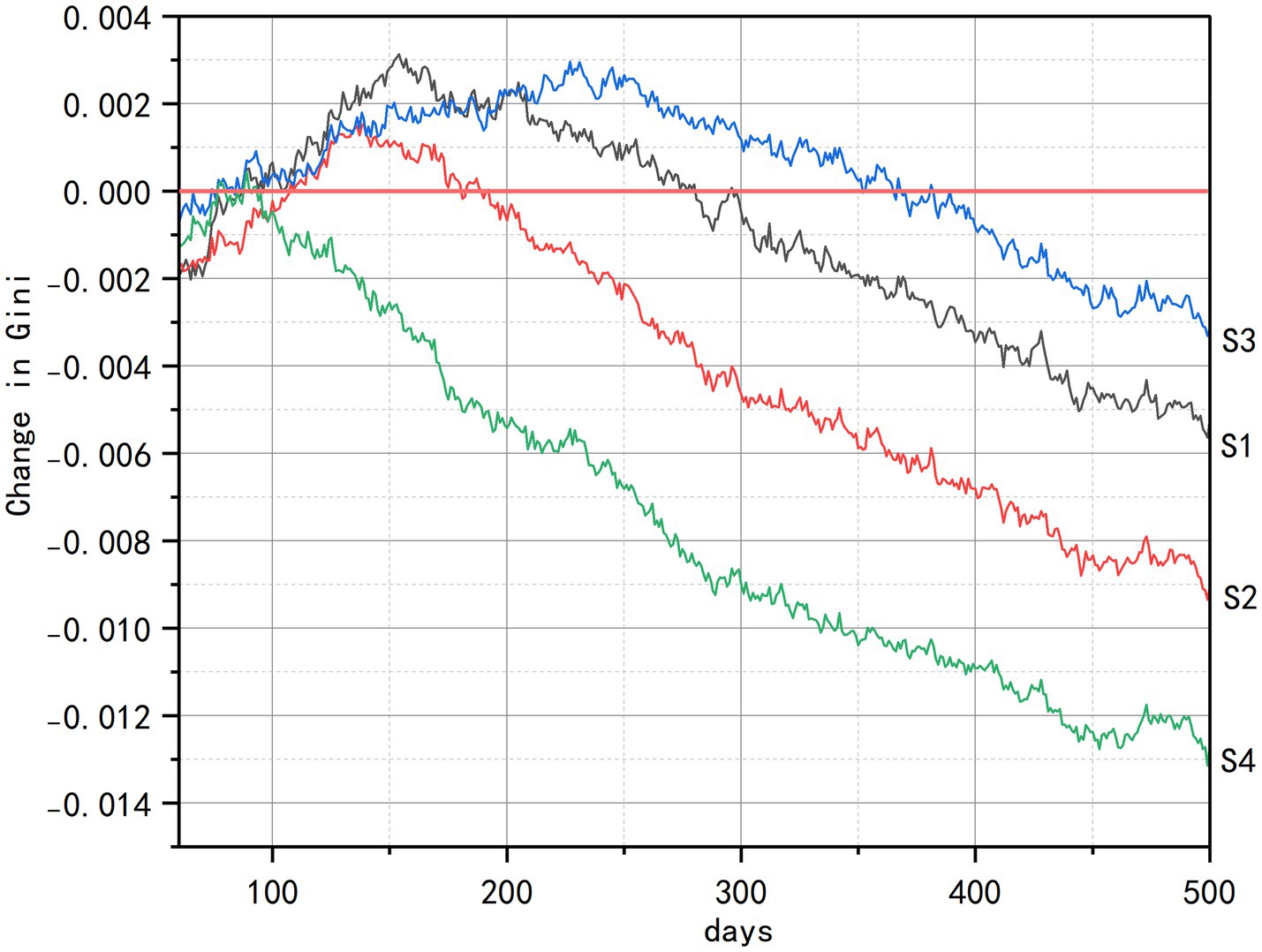
4.2 Multidimensional health equity: differential intervention impacts across socioeconomic status
Analysis of health equity impacts reveals consistent intervention hierarchies but context-dependent efficacy across socioeconomic dimensions, as quantified by Gini coefficient index (Figures 7–9). Across all strata, such as initial health status, economic status, and living status, comprehensive interventions (S4) demonstrated sustained equity improvements, achieving the largest Gini coefficient reductions through synergistic integration of spatial, cognitive, and social components. The senior-friendly transportation policies (S2) consistently ranked second in efficacy, generating rapid initial equity gains across health and economic subgroups by overcoming spatial accessibility barriers.
Across subgroups defined by baseline health status (Figure 7), the integrated intervention (S4) leveraged multidimensional coupling to produce a gradual yet durable reconstruction of equity. In contrast, senior-friendly transportation policies (S2) that rely primarily on improving spatial accessibility exhibited diminishing marginal returns over time. Critically, although the community-based health education (S3) nominally offered opportunities for participation, the persistent mobility constraints of disabled older adults meant that the actual benefits they derived were minimal.
For groups differentiated by economic status (Figure 8), all interventions triggered a transient deterioration in equity at the outset. This occurred because policy dividends were first captured by population segments with stronger resource-acquisition capacity, while disadvantaged groups, constrained by delayed penetration of resources into space, barriers to cognitive translation, and information asymmetry, experienced postponed gains, thereby temporarily widening gaps in access to health resources. Following the initial implementation shock, senior-friendly transportation policies (S2) emerged as the most effective standalone intervention. By physically expanding older adults’ activity spaces through sidewalk upgrades, strategically placed rest nodes, and dedicated senior transit loops, this approach directly dismantled concrete access barriers to health resources. The community-based health education (S3) eventually contributed to health gains, though its impact required an extended maturation period for knowledge translation and intergenerational support networks to develop fully. Most critically, the multi-functional community centers (S1) carried significant implementation risks. When deployment prioritized facility quantity over precise spatial targeting- specifically, failing to locate hubs within identified service deserts-these centers were disproportionately accessed by higher-income users. This “static hardware deployment” approach consequently amplified pre-existing inequities rather than alleviating them, demonstrating that infrastructure placement without equity-focused siting criteria can undermine intervention goals.
Among populations distinguished by living status (Figure 9), the multi-functional community centers (S1) became the single most effective intervention by directly compensating for the absence of family support—particularly for older adults living alone. This was achieved by expanding the physical supply of health resources, prioritizing the filling of service-coverage gaps, and providing day-care services. In comparison, the integrated intervention (S4) underperformed S1 overall, mainly because of unstable effects from spatial mobility enhancement (S2) and the behavior-change dependency of health education (S3), which jointly weakened synergy. The senior-friendly transportation policies (S2) displayed a brief but pronounced initial impact, yet their effectiveness declined continuously thereafter. More importantly, senior-friendly transportation policies (S2) failed to counter the inherent risk of accelerated health decline in isolated living environments such as solitary residence, and inadvertently intensified health inequities tied to differential living status.
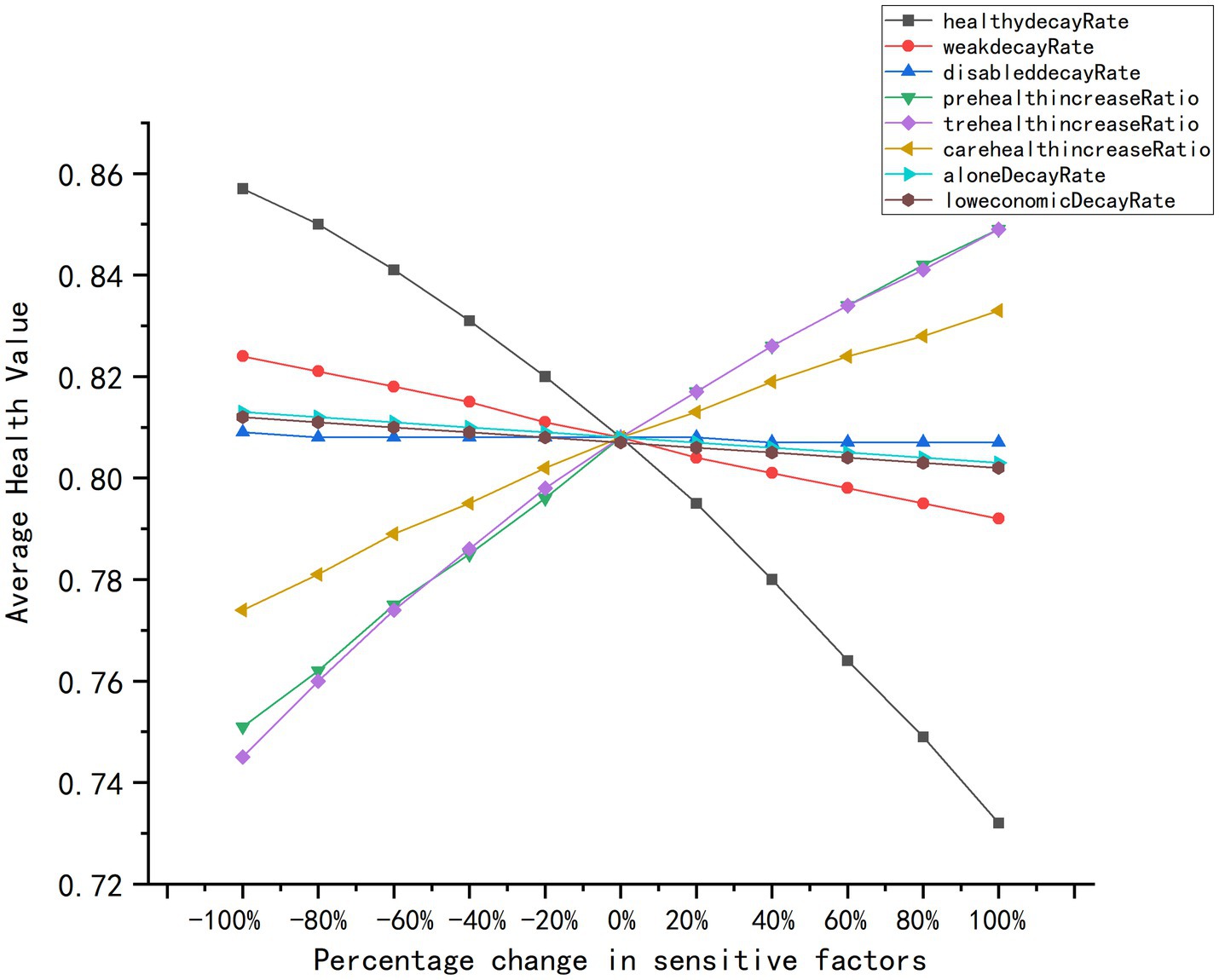
4.3 Model robustness and sensitivity analysis
This study established the model’s reliability for intervention assessment through rigorous robustness verification and sensitivity analysis. Univariate sensitivity testing (Figure 10) conducted across 100 independent simulation trials confirmed exceptional stability against input perturbations, with consistent predictive performance maintained throughout parameter variations. The smooth, continuous response curves, which were devoid of abrupt jumps or anomalous oscillations, demonstrated resilient output behavior under operational disturbances. Core parameters including health decay rates and preventive resource efficacy consistently aligned with theoretical expectations, validating the model’s mechanistic logic. Notably, while most parameters exhibited moderate sensitivity, select variables (e.g., decay rates for disabled subgroups) showed minimal responsiveness near baseline values, indicating strong tolerance to minor fluctuations. This balanced sensitivity profile, which avoids both excessive dependence on individual parameters and loss of critical effect detection, ultimately affirms the framework’s capacity for reliable policy extrapolation under uncertainty. The confirmed adaptability positions this ABM as a robust quantitative tool for forecasting multi-scenario health outcomes and optimizing aging-resource allocation strategies.
5 Discussion
The intervention scenarios evaluated in this study are strategically aligned with China’s active aging policy framework. Scenario S2 (Senior-Friendly Transportation) directly operationalizes the national mandate from the “14th Five-Year Plan for the Aging Cause and Older Adults Care System” to enhance age-adapted transformation of urban transportation (38). Similarly, Scenario S1 (Multi-functional Community Centers) implements the national “embedded older adults care” policy that promotes integrated community service hubs (2). Similarly, Scenario S3 (Community-based Health Education) is explicitly anchored in the “Healthy China 2030” blueprint and the “14th Five-Year Plan for Healthy Aging,” both of which prioritize health literacy promotion and chronic-disease self-management at the grassroots level by translating the national requirement for “community-based health education rooms and lecture series” into a scalable intervention (3, 38). This deliberate policy grounding ensures that our modeling exercise addresses real-world priorities.
In this context, the ABM simulation approach provides critical advantages for evidence-based policy formation. By creating a controlled “policy laboratory,” this study enable low-risk testing of intervention concepts before committing substantial public resources. The model identifies both leverage points and potential unintended consequences, such as the risk of S1 reinforcing spatial inequities, that might only emerge after costly implementation. This preemptive screening capacity is particularly valuable for aging cities like Fuzhou that face urgent resource allocation decisions amid demographic pressures.
The analysis demonstrates that transportation accessibility serves as the primary driver of health improvement, with S2 producing the most rapid gains by directly expanding older adults’ “mobility circles.” This finding highlights the critical importance of addressing the spatial dimension of the “last-mile” problem as a foundation for health equity in high-density urban environments. It is noteworthy that while this study focused on Fuzhou’s densely populated urban core, the fundamental mechanism through which transportation accessibility enables health resource utilization likely has broader applicability across diverse urban settings.
The relatively modest outcomes observed in the health education scenario (S3) highlight the significant influence of cognitive and socioeconomic factors in shaping the success of behavioral interventions. This finding reinforces the importance of situating educational initiatives within easily reachable physical settings and established social support systems—an approach consistent with China’s integrated care model, though one that demands adaptation to local conditions for effective implementation (59–61).
6 Conclusion
This study establishes that spatial accessibility constitutes the most critical determinant of health outcomes and equity for older adults in high-density urban cores like Fuzhou. Through an agent-based model capturing dynamic interactions across prevention-treatment-care resources, this study demonstrates that comprehensive interventions (S4), integrating spatial, transportation, and social dimensions, deliver the most significant and robust improvements. Such multidimensional strategies substantially elevate population-wide health while systematically dismantling barriers driven by “mobility circle collapse” among disadvantaged subgroups, achieving measurable equity gains across health and economic strata. However, their efficacy remains constrained in addressing residential inequities due to synergy limitations. Senior-friendly transportation policies (S2) emerge as potent catalysts for rapid health and equity improvements across health/economic groups, yet paradoxically exacerbate disparities among residential subgroups. While multi-functional community centers (S1) enhances health maintenance opportunities, its impact remains bounded by spatial distribution imbalances that risk solidifying disparities in underserved areas. Community-based health education (S3) yields minimal returns, underscoring how cognitive capacity, socioeconomic status, and family support act as persistent filters for knowledge conversion.
This study establishes agent-based modeling as a valuable tool for bridging national policy directives with local implementation planning. By translating policy concepts into computationally testable scenarios, this research provides a methodology for simulating intervention impacts across diverse urban contexts. Future research should expand this paradigm by incorporating multi-agent interactions with family and community networks, integrating cost-effectiveness analysis, and validating findings across cities with varying geographic and socioeconomic characteristics. Such efforts will further strengthen the evidence base for designing targeted, effective policies to address the complex challenges of population aging.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Science and Technology Ethics Committee of Fujian University of Technology. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
QZ: Funding acquisition, Writing – original draft, Conceptualization, Supervision, Writing – review & editing. XW: Methodology, Data curation, Software, Writing – original draft. SW: Formal analysis, Writing – original draft, Visualization. LH: Funding acquisition, Validation, Writing – review & editing, Supervision. CP: Conceptualization, Writing – review & editing, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the National Natural Science Foundation of China (No. 42201225) and the Youth Fund of the Ministry of Education for Humanities and Social Sciences (No. 22YJC840041). Publishing is also supported by the Natural Science Foundation of Fujian Province (No. 2025J01372) and the Open Fund of Key Laboratory of New Technology for Construction of Cities in Mountain Area, Ministry of Education (LNTCCMA-20240101).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. During the preparation of this work, the authors used GPT-4 Turbo to enhance readability and improve the language. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the publication’s content. In Figure 2, the icons and figure elements were generated using the AI image generationtool from iconfont (https://www.iconfont.cn/), and subsequently modified by the authors.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1698911/full#supplementary-material
References
1. Yang, H. Dynamic trend of China’s population ageing and new characteristics of the elderly. Population Res. (2022) 46:104–16. Available online at: https://rkyj.ruc.edu.cn/EN/Y2022/V46/I5/104
2. Zhou, X. Modernizing the governance of aged society: concepts, system and capacity construction. Population Soc. (2025) 41:1–9. doi: 10.14132/j.2095-7963.2025.02.001
3. Cui, S, and Yang, S. The "combination of medical care and nursing" from the perspective of healthy China. Dongyue Tribune. (2019) 40:42–51+191–192. doi: 10.15981/j.cnki.dongyueluncong.2019.06.005
4. Shao, Y, Fan, M, Cai, B, and Luo, J. An analysis of the evolution of China's policies on elderly healthcare services based on policy text mining. Modern Preven Med. (2024) 51:3570–5. doi: 10.20043/j.cnki.MPM.202403191
5. Chen, Q, Xing, L, Sun, G, and Mu, L. Spatial equity of urban health resources for the elderly from an active-passive health perspective: a case study of Central Wuhan City. Resour Sci. (2023) 45:1424–39. doi: 10.18402/resci.2023.07.11
6. Jiang, Z, Wu, C, and Chung, H. The 15-minute community life circle for older people: walkability measurement based on service accessibility and street-level built environment – a case study of Suzhou. China Cities. (2025) 157:105587. doi: 10.1016/j.cities.2024.105587
7. Yun, S, Gao, S, and Bao, Q. Public service facilities under the guidance of high quality development: an exploration on the chapter of public service facilities in the technical guidelines for the planning of xiong'an new area (for trial implementation). City Planning Rev. (2022) 46:77–83. doi: 10.11819/cpr20221805a
8. Li, B, Li, X, and Wang, Y. Research on the location and layout planning of community-based integrated elderly care facilities for rehabilitation. Architect J. (2019) 2:44–9. doi: 10.3969/j.issn.0529-1399.2019.02.008
9. Wang, F, Yu, L, and Zhang, Q. The function promoted and allocation optimized of Urban Community medical service facilities in the view of medical-pension combined. Architect J. (2018) S1:23–8.
10. Huang, Y, Zhang, H, and Zuo, X. Research Progress and reflection on senior living service system in China. Planner. (2024) 40:26–33. doi: 10.3969/j.issn.1006-0022.2024.05.004
11. Qiu, L. Research on the factors influencing satisfaction with community-based elderly care services: a case study of Shanghai. World Survey Res. (2016) 2:15–8. doi: 10.13778/j.cnki.11-3705/c.2016.02.003
12. Wang, L, Zhou, K, and Wang, Z. Spatial distribution of community pension facilities from the perspective of health equity: a case study of the central city of Shanghai. Hum Geogr. (2021) 36:48–55. doi: 10.13959/j.issn.1003-2398.2021.01.007
13. Hu, X, and Nakayama, T. Empirical research on the life satisfaction and influencing factors of users of community-embedded elderly care facilities. Buildings. (2025) 15:894. doi: 10.3390/buildings15060894
14. Sun, X, Wang, L, Wang, F, and Soltani, S. Behaviors of seniors and impact of spatial form in small-scale public spaces in Chinese old city zones. Cities. (2020) 107:102894. doi: 10.1016/j.cities.2020.102894
15. Zheng, H, Gao, Z, Wu, Z, and Tang, J. Impact of community parks on health behavioral activities of the elderly in Zhengzhou City. For Invent Plan. (2024) 49:181–7. doi: 10.3969/j.issn.1671-3168.2024.06.030
16. Tang, C, He, S, Qiu, T, He, C, Xu, J, Tang, W, et al. Predicting the health behavior of older adults in Western Hunan villages using machine learning algorithms. Buildings. (2024) 14:1895. doi: 10.3390/buildings14071895
17. Zhang, Q, Metcalf, SS, Palmer, HD, and Northridge, ME. Spatial analysis of Chinese American ethnic enclaves and community health indicators in new York City. Front Public Health. (2022) 10:Article 815169. doi: 10.3389/fpubh.2022.815169
18. Liu, B. Research on the spatial identities of public health service facilities in the suburban communities of metropolises: a case study of Jinshan District in Shanghai. hanghai Urban Plan Rev. (2017) 3:50.
19. Ni, C, Shao, B, Cong, Z, and Wang, Z. Impact of age-friendly community renovations on the elderly’s health. Chinese J Population Sci. (2024) 38:113–28. Available online at: http://ie.cass.cn/kygz/kycg/lw/202502/t20250207_5843380.shtml
20. Hu, ML, and Chen, SH. Measurement of healthcare resource allocation efficiency and spatiotemporal evolution analysis. Statistics Decision. (2023) 39:72–6. doi: 10.13546/j.cnki.tjyjc.2023.01.013
21. Gleeson, D, Townsend, B, Tenni, BF, and Phillips, T. Global inequities in access to COVID-19 health products and technologies: a political economy analysis. Health Place. (2023) 83:103051. doi: 10.1016/j.healthplace.2023.103051
22. Liu, J, Lai, Z, Meng, B, Guo, Z, and Liu, X. Assessing spatial configuration of barrier-free facilities from the perspective of age-friendliness: a case study of Beijing, China. Applied Geography. (2024) 172:103426. doi: 10.1016/j.apgeog.2024.103426
23. Luo, N, and Liao, Y. What types of government health investment methods are beneficial to equity in urban and rural health? Xitong Gongcheng Lilun yu Shijian/System Engineering Theory and Practice. (2024) 44:3169–89. doi: 10.12011/SETP2023-0981
24. Zhang, Q, Northridge, ME, Jin, Z, and Metcalf, SS. Modeling accessibility of screening and treatment facilities for older adults using transportation networks. Appl Geogr. (2018) 93:64–75. doi: 10.1016/j.apgeog.2018.02.013
25. Tao, Y, Henry, K, Zou, Q, and Zhong, X. Methods for measuring horizontal equity in health resource allocation: a comparative study. Heal Econ Rev. (2014) 4:10. doi: 10.1186/s13561-014-0010-x
26. Liao, L, Kong, S, and Du, M. The effect of clean heating policy on individual health: evidence from China. China Econ Rev. (2025) 89:102309. doi: 10.1016/j.chieco.2024.102309
27. Zhang, Q, Huang, B, Yu, B, and Wu, L. Enhancing sustainable urban mobility: a multi-agent analysis of low-carbon policy impacts on travel behavior in Fuzhou's main urban area, China. Human Soc Sci Commun. (2024) 11:1717. doi: 10.1057/s41599-024-04270-0
28. Zhang, Q, Metcalf, SS, Palmer, HD, and Northridge, ME. Developing an agent-based model of oral healthcare utilization by Chinese Americans in new York City. Health Place. (2022) 73:102740. doi: 10.1016/j.healthplace.2022.102740
29. Dai, D, Wang, Y, Bai, R, and Li, Y. Simulation analysis of outdoor leisure activities for the elderly in residential areas based on agent-based modeling: a case study of Shenzhen Taoyuan residential. Architect J. (2023) S2:108–13. Available online at: https://jzxb.cbpt.cnki.net/WKE/WebPublication/paperDigest.aspx?paperID=0dd755a5-c270-4e6c-bcf5-3722d0ad7de8
30. Motieyan, H, and Mesgari, MS. An agent-based modeling approach for sustainable urban planning from land use and public transit perspectives. Cities. (2018) 81:91–100. doi: 10.1016/j.cities.2018.03.018
31. Badham, J, Chattoe-Brown, E, Gilbert, N, Chalabi, Z, Kee, F, and Hunter, RF. Developing agent-based models of complex health behaviour. Health Place. (2018) 54:170–7. doi: 10.1016/j.healthplace.2018.08.022
32. Taghikhah, FR, Jabbari, A, Desouza, KC, Malik, A, and Khorshidi, HA. Understanding delayed diabetes diagnosis: an agent-based model of health-seeking behavior. Med Decis Mak. (2025) 45:399–425. doi: 10.1177/0272989X251326908
33. Bai, R. Study on outdoor leisure activity space of the elderly in residential areas based on agent-based modeling: A case study of Shenzhen Taoyuan residential [master’s thesis]. Harbin: Harbin Institute of Technology; (2019).
34. Ma, Y, Wu, R, Wang, Z, and Li, M. Study on the planning and layout of community geriatrics based on ABM: a case study of downtown Fuzhou. Urban Develop Studies. (2019) 26:18–25. doi: 10.3969/j.issn.1006-3862.2019.01.014
35. Cassidy, R, Singh, NS, Schiratti, PR, Semwanga, A, Binyaruka, P, Sachingongu, N, et al. Mathematical modelling for health systems research: a systematic review of system dynamics and agent-based models. BMC Health Serv Res. (2019) 19:845. doi: 10.1186/s12913-019-4627-7
36. Ji, J. The Last Mile of Elderly Care Service: Theory and Practice of Home-Based Elderly Care in China. China Social Sciences Press. (2021) 1:26–36. Available online at: https://www.sklib.cn/booklib/bookPreview?SiteID=122&ID=9232713&fromSubID=537
37. Sun, L, and Li, G. Integrating medical care and elderly support to uplift the “Most beautiful sunset glow”: bridging the “last mile” of health-based eldercare in communities. Population Health. (2022) 4:84–5. doi: 10.3969/j.issn.2096-7063.renkyujk202204045
38. State Council of the People’s Republic of China. The 14th five-year plan for National Aging Undertakings and elderly-care service system [internet]. Beijing: State Council of the People’s Republic of China (2022).
39. Fuzhou Municipal Bureau of Statistics. Fuzhou statistical yearbook 2020 [internet]. Beijing: China Statistics Press.
40. Xie, HL, Liu, SL, Dai, HX, You, MZ, Xiao, Y, Jiang, YJ, et al. Assessment of urban green space cooling benefits from a supply-demand matching perspective: a case study of Fuzhou city's main urban area. Acta Ecol Sin. (2025) 23:1–11. doi: 10.20103/j.stxb.202408252013
41. Wei, Y, and Wu, S. A method for identifying urban functional regions by integrating regional embedding representations. J Geo-Inform Sci. (2025) 27:424–40. doi: 10.12082/dqxxkx.2025.240484
42. Fujian Provincial Department of Housing and Urban-Rural Development. Fujian provincial guidelines for urban-rural older adults care facility planning and allocation [internet]. Fuzhou: The Department (2015).
43. Fuzhou Municipal People's Government Office. Implementation plan for establishing a comprehensive older adults health service system in Fuzhou [internet]. Fuzhou: The Office (2021).
44. Cao, L, Zhong, L, Fan, C, and Zhan, B. A practical study on the health promotion service model of integration of sport, medicine and health care in China. J Capital Univ Physical Educ Sports. (2022) 34:516–24. doi: 10.14036/j.cnki.cn11-4513.2022.05.006
45. Yang, F, Huang, Y, and Wang, F. Physical exercises of Chinese older adults and social participation: health promotion and network expansion. Population Res. (2021) 45:97–113. Available online at: https://rkyj.ruc.edu.cn/CN/Y2021/V45/I3/97
46. Bondarenko, M, Kerr, D, Sorichetta, A, and Tatem, AJ. Estimates of 2020 total number of people per grid square, adjusted to match the corresponding UNPD 2020 estimates and broken down by gender and age groupings, produced using built-settlement growth model (BSGM) outputs. WorldPop, University of Southampton: UK (2020).
47. Grimm, V, Berger, U, Bastiansen, F, Eliassen, S, Ginot, V, Giske, J, et al. A standard protocol for describing individual-based and agent-based models. Ecol Model. (2006) 198:115–26. doi: 10.1016/j.ecolmodel.2006.04.023
48. Xi, J. An analysis of the existing outdoor public space for senior citizens in old residential areas in Fuzhou and the adaptive renewal for the elderly. Architect Culture. (2019) 8:138–9. doi: 10.3969/j.issn.1672-4909.2019.08.049
49. Liu, J, Wu, C, Le Vine, S, and Jian, S. Panel data analysis of Chinese households’ car ownership and expenditure patterns. Transp Res Part D: Transp Environ. (2023) 123:103915. doi: 10.1016/j.trd.2023.103915
50. Le Vine, S, Wu, C, and Polak, J. A nationwide study of factors associated with household car ownership in China. IATSS Res. (2018) 42:128–37. doi: 10.1016/j.iatssr.2017.10.001
51. Chen, G, Xu, X, and Zhou, L. The impact of middle-aged and older adults’ proactive health behaviors on their health status: a latent profile analysis. Chinese Health Service Management. (2025) 42:344–8. doi: 10.3969/j.issn.1004-4663.2025.3.zgwssygl202503018
52. Hao, A, Chen, C, Lang, L, and Xu, N. The relationship between self-rated health and health service utilization among older adults. Chinese General Prac. (2021) 24:818–23. doi: 10.12114/j.issn.1007-9572.2021.00.032
53. Hu, H, Luan, W, and Li, J. Medical insurance, health services utilization and excessive demands for medical services: the impact of medical insurance on health service utilization among the elderly. J Shanxi Univ Finance Econ. (2015) 37:14–24. doi: 10.13781/j.cnki.1007-9556.2015.05.002
54. Zhang, P. Analysis of institutional elderly care demand and its influencing factors: A case study of Xiangcheng District. Nanjing: Nanjing Agricultural University (2016).
55. Jing, Y, and Li, Y. Analysis on the make-up of China's disabled seniors and the demand for long-term care. Population J. (2014) 36:55–63. doi: 10.3969/j.issn.1004-129X.2014.02.006
56. Ouyang, H. Study on the allocation mechanism and optimization of elderly care institutions in Changsha under the resilience city theory perspective [doctoral dissertation]. Changsha: Hunan University
57. National Bureau of Statistics of China. Office of the Leading Group of the State Council for the Seventh National Population Census. (2020) 1:1949–1950. Seventh National Population Census Program. Available online at: https://www.stats.gov.cn/sj/pcsj/rkpc/7rp/zk/html/fu06.pdf
58. Bleiberg, JF, Lyon, MA, and Schueler, BE. State takeover of school systems and Within-District fiscal equity. J Educ Human Resources. (2023) 41:172–204. doi: 10.3138/jehr-2021-0059
59. Turrell, G, Oldenburg, B, McGuffog, I, and Dent, R. Socioeconomic determinants of health: towards a national research program and a policy and intervention agenda. Queensland Univ Technol. (1999). doi: 10.5204/1329-4399.1329
60. Jiao, J, Wang, P, and He, H. Influence of community environment on cognitive function among older adults and the mediating role of social health. Chinese J Health Policy. (2025) 18:42–9. doi: 10.3969/j.issn.1674-2982.2025.05.007
61. Hao, X, Zheng, Y, Li, Y, Xu, J, and Sun, J. Research on the effect of the social support network on the health of the elderly migrant population. Chinese J Health Policy. (2022) 15:54–61. doi: 10.3969/j.issn.1674-2982.2022.10.008
62. Zuo, M, and Yang, Y. A study of smart senior care services: based on the dynamic needs of different age groups. J Sichuan Univ. (2025) 3:15–27+226–227. doi: 10.3969/j.issn.1006-0766.2025.03.002
63. Liu, L. Economic conditions, family form, and choice of elderly care for urban elderly: Analysis of elderly residents in the Yangtze River Delta urban agglomeration [doctoral dissertation]. Tempe (AZ): Arizona State University; (2025).
64. Hu, Y, Liu, H, Li, M, Zheng, X, and Liu, J. A survey on long-term care service demand and insurance intention in Ningbo City. Modern Manage. (2022) 12:648–58. doi: 10.12677/mm.2022.126089
65. Zhang, Y, and Liang, H. Socio-economic status and patterns of lifestyle of the older adults in China: convergence at lower levels while divergence at higher levels. Population Res. (2021) 45:114–28. Available online at: https://rkyj.ruc.edu.cn/CN/Y2021/V45/I3/114
66. Graves, JA, Hatfield, LA, Blot, W, Keating, NL, and McWilliams, JM. Medicaid expansion slowed rates of health decline for low-income adults in southern states. Health Aff. (2020) 39:67–76. doi: 10.1377/hlthaff.2019.00929
67. Oldenburg, B, McGuffog, ID, and Turrell, G. Socioeconomic determinants of health in Australia: policy responses and intervention options. The Medical journal of Australia. (2000) 172:489–92. doi: 10.5694/j.1326-5377.2000.tb124074.x
68. Wei, X, and Lu, J. The influence of living arrangement on the self-rated health of the elderly: based on CLASS 2014 data. Population Soc. (2021) 37:35–46. doi: 10.14132/j.2095-7963.2021.04.005
Keywords: agent-based modeling, older adults health equity, spatial accessibility, urban health planning, Fuzhou’s main urban area
Citation: Zhang Q, Wu X, Wu S, Huang L and Peng C (2025) Agent-based modeling of health resources for older adults: accessibility, equity, and last-mile solutions in Fuzhou, China. Front. Public Health. 13:1698911. doi: 10.3389/fpubh.2025.1698911
Edited by:
Chao Ma, Southeast University, ChinaReviewed by:
Liping Liao, Guangdong University of Finance and Economics, ChinaQihui Chen, China Agricultural University, China
Zicheng Jiang, Jiangyin People's Hospital, China
Copyright © 2025 Zhang, Wu, Wu, Huang and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiuyi Zhang, emhhbmdxeUBmanV0LmVkdS5jbg==; Liyun Huang, MTYzOTc1NjJAcXEuY29t; Chong Peng, cGVuZ2Nob25nQGZqdXQuZWR1LmNu
 Qiuyi Zhang
Qiuyi Zhang Xin Wu
Xin Wu Siying Wu
Siying Wu Liyun Huang2*
Liyun Huang2*