- 1Department of Art, Southeast University, Nanjing, Jiangsu, China
- 2Department of Art, Nanjing University of the Arts, Nanjing, Jiangsu, China
Introduction: Hospital cleaning involves unique risk factors including chemical exposures, infection control procedures, and physically demanding tasks that may have greater impact on older workers compared to their younger counterparts. While existing systematic reviews have examined musculoskeletal disorders among cleaning workers, none have specifically focused on older hospital cleaners. With global workforce aging and increasing employment of older adults in healthcare settings, understanding musculoskeletal disorder prevalence and specific risk factors in this population is essential for developing targeted prevention strategies. The primary objective of this systematic review is to determine the prevalence of musculoskeletal disorders among older hospital cleaners and identify associated risk factors.
Methods: We searched PubMed, MEDLINE, Web of Science, and Google Scholar from inception to July 11, 2025. Two reviewers independently screened titles, abstracts, and full texts. Data extraction included study characteristics, participant demographics, prevalence data, and risk factors. Quality assessment was conducted using the Joanna Briggs Institute checklist.
Results: Eleven studies were included. Among older hospital cleaners (aged 50+ years), musculoskeletal disorder prevalence ranged from 49.1% to 68.96% across age-stratified studies. Several factors appeared to be associated with MSD risk in this population, including work demands, individual factors (age, gender, inadequate rest time, stress, and posture), technology-related factors, and organizational factors.
Discussion: This systematic review identified multiple risk factors for musculoskeletal disorders among older hospital cleaners. The findings provide evidence to inform occupational health policies and targeted prevention strategies for this vulnerable population.
1 Introduction
Musculoskeletal disorders (MSDs) encompass a range of inflammatory and degenerative conditions affecting muscles, tendons, joints, ligaments, and other musculoskeletal structures (1). As one of the most commonly reported occupational injuries globally (2–4), MSDs are characterized by high prevalence (5). These conditions are associated with absenteeism and early retirement, which negatively affect daily activities, productivity, and quality of life, and in severe cases may lead to disability (6–8). Beyond the direct health impacts, MSDs impose a substantial economic burden: indirect costs often exceed direct medical expenses, making MSDs among the most expensive occupational diseases worldwide (9–11). When combined with productivity losses and increased strain on public healthcare systems (12–16), MSDs have become an urgent global public-health challenge (17).
Previous studies have identified four major categories of risk factors for work-related musculoskeletal disorders: biomechanical, individual, mental, and organizational (2, 5). Biomechanical risk factors include poor working postures (18–20), repetitive motions (21, 22), vibrations (23), heavy physical demands such as lifting or carrying loads (18, 20, 24, 25). Individual risk factors include age (26), gender (27), smoking (18), BMI (18, 24, 28, 29), sleep habits (5, 30), and prior medical history (29). Mental risk factors include negative emotions (31) and workload (18, 32, 33). Organizational risk factors include shift work (5, 34) and lack of workplace support (22, 25). Collectively, these determinants form a multidimensional framework encompassing biomechanical, individual, mental, and organizational domains. These four categories of risk factors are particularly pronounced among hospital cleaners, who face unique occupational challenges due to the nature of their work environment and task demands.
The vulnerability of hospital cleaners to MSDs has been further amplified by demographic changes in the workforce (35). In recent years, global population aging has prompted retirement-policy reforms across various regions (36). These policies have extended retirement age (37), particularly for individuals in physically demanding occupations. As a result, the proportion of older workers in the service industry has steadily increased (38, 39). Hospital cleaning work have become an increasingly common employment option among older adults (40). According to the U.S. Bureau of Labor Statistics, hospital cleaning positions in general medical and surgical hospitals constitute one of the largest employment sectors (41). The proportion of cleaners working in hospitals and educational institutions is significantly higher than that of other types of cleaners (42). In this review, the term “hospital cleaners” refers specifically to cleaning workers in general medical and surgical hospitals.
Given their increasing numbers and combined exposure to multiple risk domains, MSDs pose a critical occupational-health challenge for hospital cleaners (6, 43, 44). Healthcare cleaning personnel bear substantial responsibility for disrupting infection-transmission chains (6, 36, 45–47). Consequently, they must perform cleaning tasks at higher frequencies, with high-risk hospital areas sometimes requiring cleaning every 4 h (48). Moreover, the 24-h operation demands of hospitals necessitates prolonged and irregular shifts, further elevating musculoskeletal risk compared with cleaners in other environments (44). In routine operations, their standard duties include preparing cleaning products and sanitizing various surfaces throughout the hospital (44, 49). These tasks involve high physical demands, including prolonged standing, repetitive movements, distance walking, and sustained cardio-respiratory exertion (50). This growing demographic shift underscores an urgent need to understand the prevalence and risk factors of MSDs within this essential yet understudied workforce.
Multiple studies have demonstrated a high prevalence of MSDs among hospital cleaners, particularly affecting the back, shoulders, neck, and knees (1, 5, 22, 26, 27, 51, 52). Within the cleaning workforce, there is a substantial proportion of older individuals and those with limited skills (40, 53–55). In particular, individuals aged 50–59 years face higher risks of developing MSDs (56). Numerous studies have shown that risk factors such as age, gender, poor posture, and prior medical history are associated with musculoskeletal disorders among older hospital cleaners (26, 55). Six systematic reviews on MSDs among cleaners have been published between 1979 and 2024, consistently identifying cleaning workers as a high-risk occupational group for MSDs. The focus of these reviews has evolved from identifying MSD risk factors (57, 58) to developing intervention strategies (53, 59–61). However, despite the rapidly aging workforce in healthcare cleaning services, the intersection between age-related vulnerability and hospital-specific exposures remains poorly understood, representing a critical research gap.
There is currently no universal consensus regarding the definition of “older.” Public policies apply varying age thresholds ranging from 45 to 65 years (62, 63). For instance, the World Health Organization defines “older adults” as 65 and above in general-population contexts (64). Such thresholds are commonly tied to pension eligibility in different national contexts (65). However, aging is a dynamic, multidimensional process (66). In occupational contexts, the concept of “older workers” extends beyond chronological age to include organizational and career-stage dimensions (67). Its social definition continues to evolve in different workplace contexts (65). Empirical evidence showed that decision-makers perceive workers as “older” at a mean age of 52.40 years, with younger decision-makers (≤35 years) setting this threshold even lower at 50.91 years (65).
Given this complexity, this review establishes 50 years as the age criterion based on three lines of evidence from occupational musculoskeletal health research. First, the Global Burden of Disease study reported a significant increase in MSDs case numbers and prevalence specifically among the 50–59 age group (56). This indicates that workers aged 50+ who remain employed represent a critical population for understanding how to support continued productive engagement despite age-related health challenges. Second, the prevalence and risk factors of MSDs across different body regions among older hospital cleaners may differ substantially from those observed in younger workers (68). Third, this threshold aligns with age-stratifications practices commonly used in occupational-health studies (69–71). Despite the growing body of literature on MSDs among hospital cleaners, to our knowledge, no systematic review has specifically synthesized evidence on prevalence and risk factors among older workers (≥50 years) in this occupation. This is a critical gap given the unique vulnerabilities of aging workers and the increasing proportion of older adults in the cleaning workforce.
Therefore, this systematic review aims to (1) synthesize the prevalence of musculoskeletal disorders among older hospital cleaners, (2) identify associated risk factors, and (3) provide recommendations for intervention strategies in general medical and surgical hospitals.
2 Methods
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (72). The PRISMA checklist is listed in Supplementary material S2.
The study protocol was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO; registration number: CRD420251102052). Initially, the age threshold for inclusion was set at 55 years; however, due to the limited number of relevant articles, the threshold was adjusted to 50 years to ensure adequate study inclusion. Studies involving hospital cleaners aged 50 years and above were included in this review.
2.1 Data sources
A comprehensive literature search was performed in PubMed, MEDLINE, Web of Science, and Google Scholar from inception to July 11, 2025.
2.2 Inclusion and exclusion criteria
We applied the PICO framework to establish inclusion criteria (73): Population (P): Hospital cleaning workers aged 50 years and older employed in general medical and surgical hospitals. Studies providing age-stratified data for hospital cleaning workers aged 50+ within mixed-age populations were also included; Intervention (I): Hospital cleaning work activities; Comparison (C): Any comparison group or no comparison; Outcomes (O): Musculoskeletal disorder prevalence and risk factors associated with musculoskeletal disorders.
During the screening process, studies were excluded according to the following criteria. Records not relevant to the topic were removed during initial database searches, and duplicate records across databases were eliminated. Studies without accessible full text were excluded. To ensure inclusion of primary research only, all review or synthesis papers were excluded. Non-English publications were excluded from the analysis. Finally, studies with participants below 50 years of age or reporting mean ages under 50 years without age-stratified data were excluded to maintain focus on older hospital cleaners.
2.3 Search strategy
A systematic search was conducted in PubMed, MEDLINE, Web of Science, and Google Scholar from inception to July 11, 2025. Search strategies were tailored for each database and are presented in Supplementary Table S1.
2.4 Literature screening and data extraction
Two reviewers independently screened all titles, abstracts, and full-text articles using inclusion and exclusion criteria. Disagreements between reviewers were resolved through discussion with a third reviewer to reach consensus. Additionally, we used a study characteristics form to capture prevalence data for musculoskeletal disorders and to identify risk factors.
2.5 Data items
Two reviewers extracted data including country, study design, study period, hospital setting, sample size (% female), primary outcome, MSD assessment method; risk factors, prevalence (%), sample selection, confounding control, and limitations.
2.6 Risk of bias assessment
The methodological quality of each included study was assessed using the Joanna Briggs Institute (JBI) critical appraisal checklist for cross-sectional studies (74). This checklist has been widely used for assessing the quality of studies included in systematic reviews (58, 75). Each item was scored as “Yes,” “No,” or “Unclear.” Two reviewers independently conducted the assessments, and consensus was reached through discussion when disagreements occurred. The JBI quantitative critical appraisal tool was applied to assess the risk of bias in the included studies (76). Included studies were classified based on the number of JBI checklist items answered with “Yes”: studies answering 0–3 items were categorized as “poor quality,” those answering 4–6 items as “moderate quality,” and studies answering 7–8 items were considered “high quality” (58).
2.7 Task categorization
Given the heterogeneity in task descriptions, two reviewers independently extracted all reported cleaning tasks from the included studies. Through iterative discussion and consensus building, we grouped similar tasks according to three criteria: (1) primary biomechanical demands, (2) equipment and tools used, and (3) work environment characteristics. Any disagreements between reviewers were resolved through discussion with a third reviewer until consensus was achieved.
2.8 Data synthesis
Owing to substantial heterogeneity among the included studies, meta-analysis was not feasible, and a descriptive synthesis approach was employed instead. This heterogeneity was primarily attributed to several factors: (1) the wide age range of participants aged 50 years and above across studies; (2) only six studies provided age-stratified data, with two lacking prevalence data; and (3) among the remaining four studies with age stratification and prevalence data, two assessed musculoskeletal disorders over the last 7 days, while two examined prevalence over the last 12 months, making statistical pooling inappropriate. Data extraction focused on study design, participant demographics, outcome measures, prevalence rates, and identified risk factors. Results were presented using narrative synthesis.
During data synthesis, a conceptual model grounded in the Person–Environment (P–E) Fit theory was constructed to illustrate the interactions between work demands, individual characteristics, and environmental factors contributing to musculoskeletal disorders among older hospital cleaners (Figure 2). This conceptual framework was developed inductively based on the synthesis of identified risk factors and existing theoretical foundations from occupational health and organizational psychology literature.
3 Results
3.1 Literature search results
We searched multiple databases including PubMed, MEDLINE, Web of Science, and Google Scholar from inception to July 11, 2025. After screening and eligibility assessment, 11 studies met the inclusion criteria and were included in this review (Figure 1).
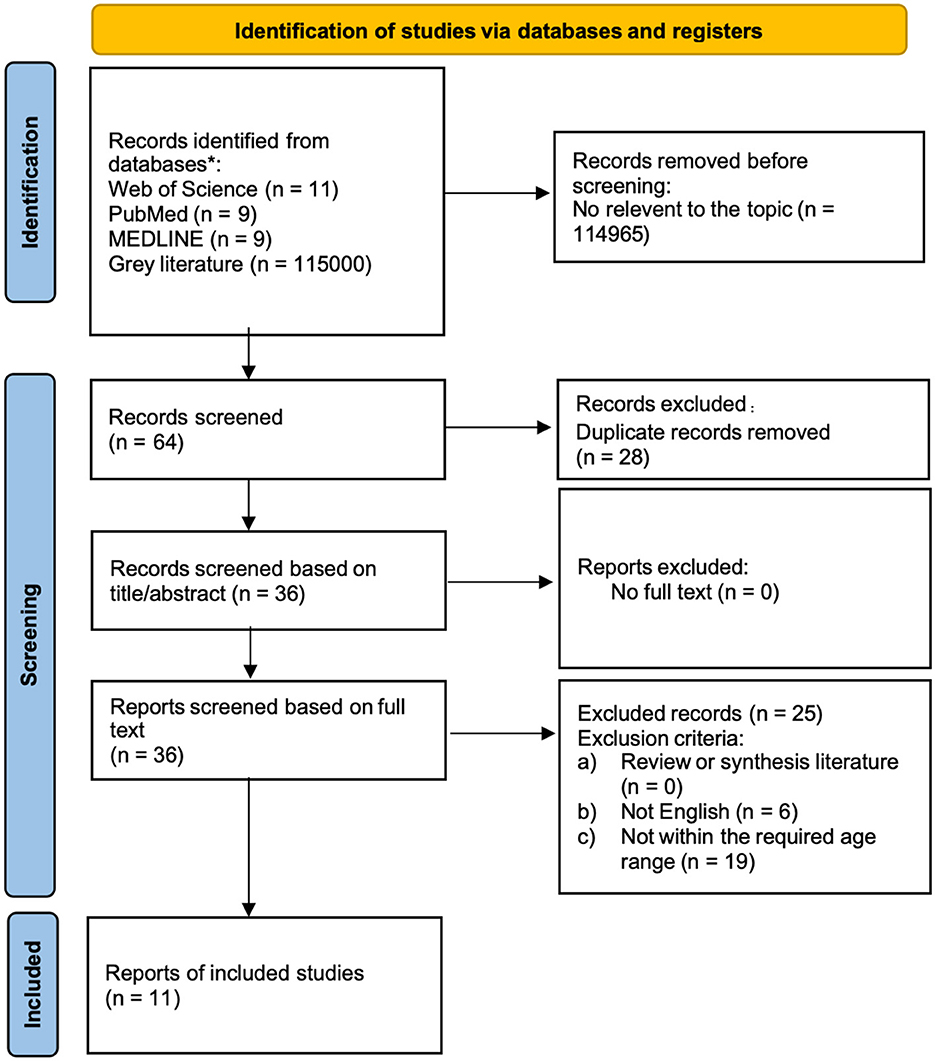
Figure 1. PRISMA flow diagram (72).
3.2 Baseline characteristics
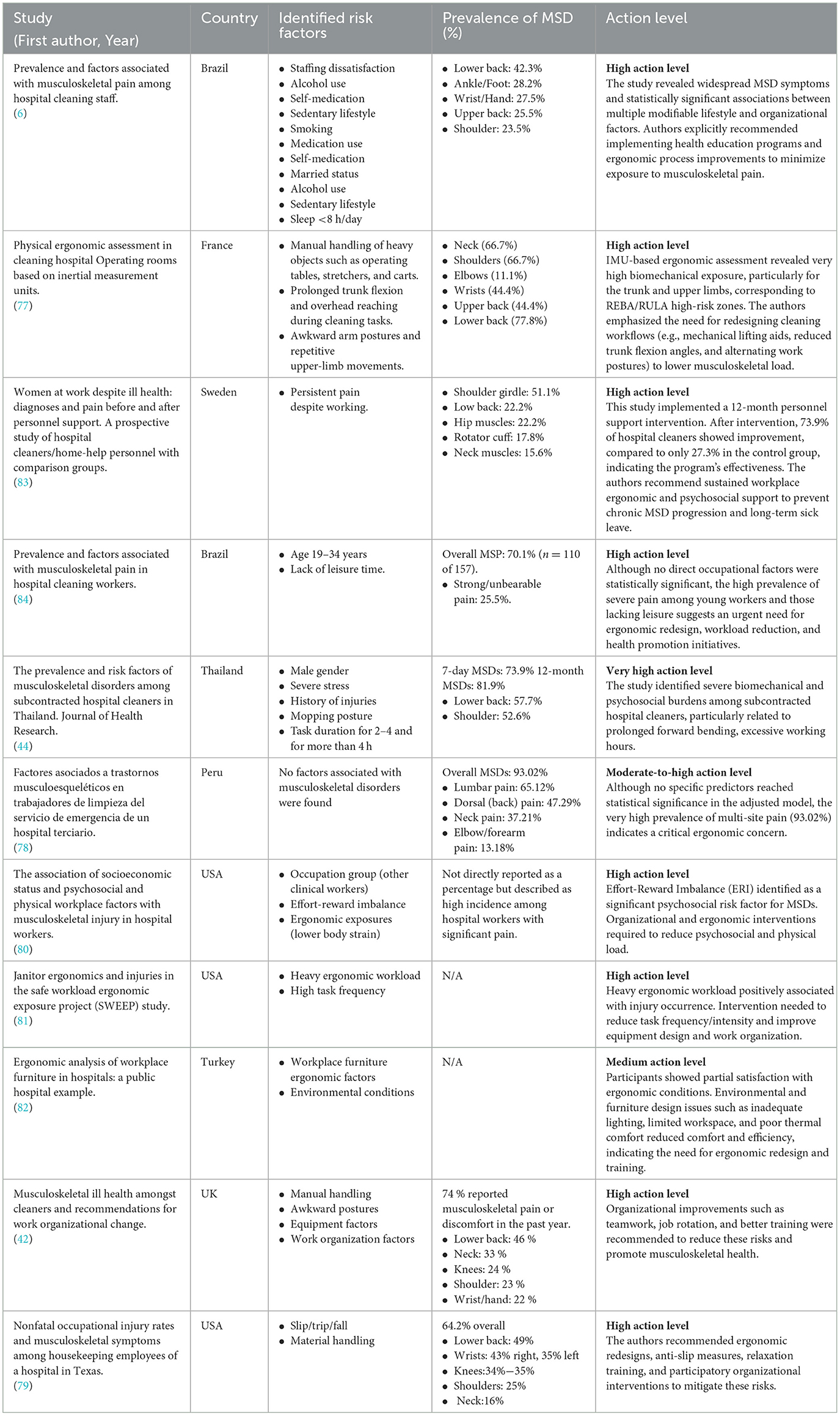
Table 1 presents the baseline characteristics of the included studies, including country, study design, study period, hospital setting, sample size, age, sample size, proportion of females (%), primary outcome, MSD assessment method, risk factors, prevalence (%), sample selection, confounding control, and study limitations.
Among the 11 included studies, seven (63.6%) were conducted in Global North regions, comprising three studies from the United States and one each from France, Sweden, the United Kingdom, and Turkey. The remaining four studies (36.4%) were conducted in Global South regions, including two studies from Brazil and one each from Thailand and Peru (Table 1).
The majority of studies (n = 8, 72.7%) were conducted in public healthcare settings. Five studies were conducted in public hospitals, two in public university hospitals, and one in the broader public healthcare sector; hospital setting information was unavailable for three studies.
Study designs included eight cross-sectional studies (72.7%), two prospective cohort studies (18.2%), and one case-control study (9.1%).
Publication years ranged from 2001 to 2024, spanning two decades of research. The distribution showed three studies (27.3%) from 2001–2010, while the 2011–2020 and 2021–2024 periods each contributed four studies (36.4%), indicating sustained and increasing research interest in recent years.
Age distributions varied widely across studies, though specific sample sizes for older worker subgroups were not consistently reported across all studies. Gender distribution was available for nine studies, revealing a predominantly female workforce with female participation rates ranging from 12.5% to 100%.
The primary outcomes of the included studies were grouped into two main categories. Eight studies (72.7%) focused on determining the prevalence of musculoskeletal disorders or pain and assessing multidimensional risk factors, including economic, organizational, psychosocial, and physical determinants among hospital cleaning staff. The remaining three studies (27.3%) examined ergonomic assessment.
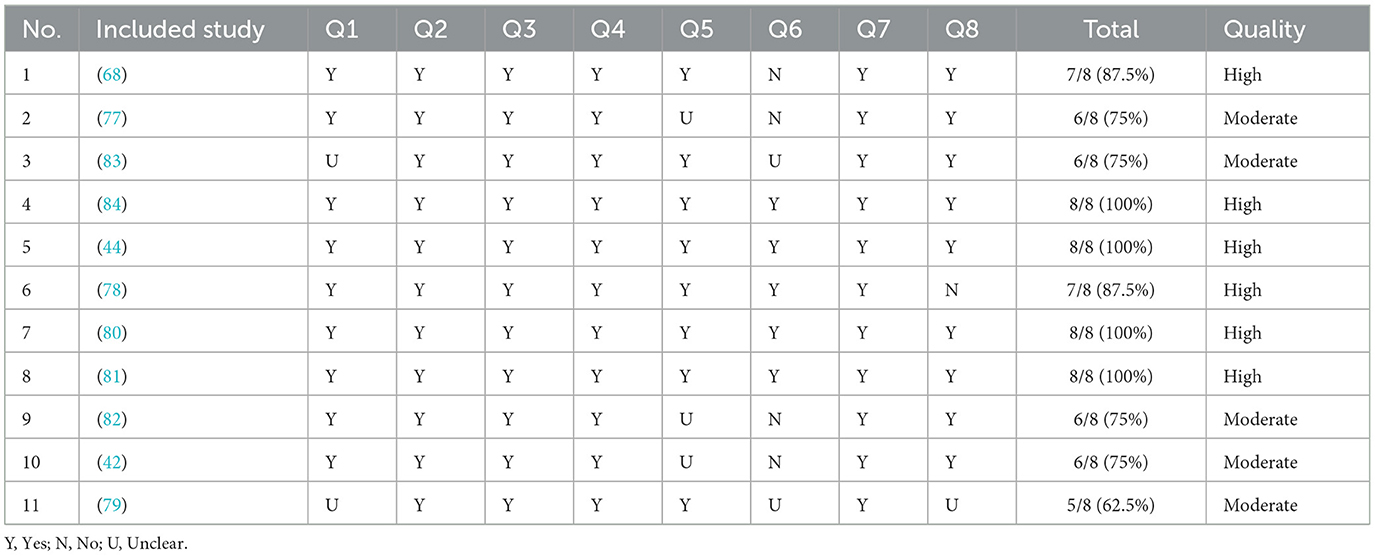
3.3 Risk of bias
We used the JBI checklist to evaluate the risk of bias in included studies (Table 2). The risk of bias assessment comprised eight questions (58). Two reviewers independently assessed each study, with disagreements resolved through discussion. Detailed risks of bias assessments for individual studies are summarized in Table 3. The assessment revealed that all 11 included studies demonstrated high and moderate quality. The main source of bias was related to confounding factor management. Six studies failed to clearly identify potential confounders or implement appropriate statistical adjustment strategies.
3.4 Outcome measurement
Five studies employed the Nordic Musculoskeletal Questionnaire (NMQ) or the Standardized Nordic Questionnaire (SNQ) to assess MSD prevalence and related factors (44, 68, 77–79). Both NMQ and SNQ are widely used to collect data on work-related musculoskeletal problems or pain in specific body regions. Four studies utilized self-reported structured questionnaires to conduct ergonomic assessments or workplace evaluations (42, 80–82). Additionally, two studies employed the Visual Analogue Scale (VAS) to measure individuals' perceived intensity or changes in specific sensations, symptoms, or conditions (83, 84).
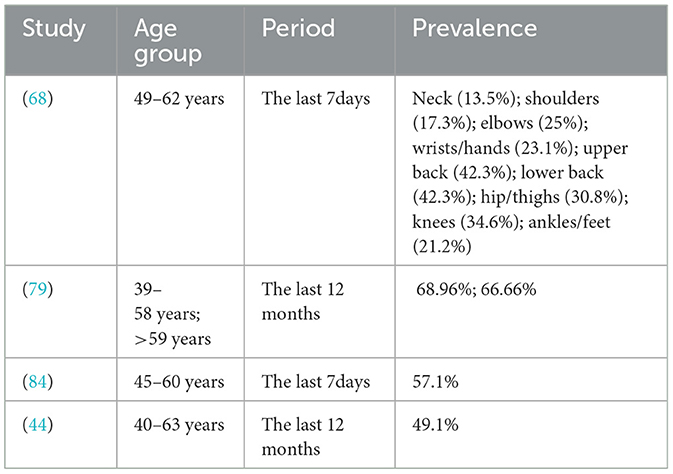
Due to substantial heterogeneity among study participants, a meta-analysis was not feasible; therefore, a descriptive analysis was employed to synthesize the results. All 11 articles included hospital cleaners aged 50 years and above. Among these, six studies provided age-stratified data (44, 68, 79, 81, 82, 84), of which four studies reported prevalence rates (Table 3). Results from the four studies with age-stratified data showed that older hospital cleaners (aged 39–62 years across studies) had overall MSD prevalence rates ranging from 49.1% to 68.96%. Prevalence rates varied across different body regions, with the upper back and lower back showing the highest prevalence rates, both reaching 42.3%. Importantly, different studies employed varying time windows (7 days vs. 12 months), which may affect prevalence comparisons. The 12-month prevalence was generally higher than the 7-day prevalence, which is consistent with the chronic and recurrent nature of MSDs in this population.
4 Discussion
Previous systematic reviews on musculoskeletal disorders among cleaners have established theoretical foundations. One review developed a conceptual model that identified potential factors contributing to musculoskeletal disorders among cleaners (53). This model posits that load, tissue response, and modifying factors jointly govern musculoskeletal adaptation and injury risk, shaping cleaners' health and work ability (53). Subsequently, another review built upon this foundation to identify five key components of work structure (individual, technology, organization, environment, and outcome) based on balance theory (61).
However, no systematic reviews have specifically focused on MSDs among older hospital cleaners. Additionally, previous models have not adequately addressed the dynamic relationship between cleaner characteristics and MSDs. Older workers generally face age-related degenerative changes, with declining muscular strength being a key manifestation of this deterioration. Previous literature has demonstrated that muscular strength may be a critical factor in determining MSD risk when performing physically demanding work tasks. Lower muscle strength in vulnerable body regions may increase the risk of MSDs during heavy physical labor (85). Conversely, higher muscle strength may enhance cleaners' tolerance for heavy physical work and provide a protective balance against the development of musculoskeletal symptoms (86).
This suggests that an individual's adaptive capacity when performing work tasks may influence MSD outcomes. Based on these findings, this study developed a conceptual model based on Person-Environment Fit (P-E Fit) theory (Figure 2). P-E Fit is typically defined as the compatibility between individual and work environment characteristics (87). The P-E Fit model is widely applied in organizational psychology and occupational health fields, and has increasingly been used in work-health relationship research. Multiple studies have emphasized that good P-E Fit can help workers adapt to work and return to work through dynamic, phased, and cyclically adjustable processes, ultimately reducing the prevalence of MSDs (88–90).
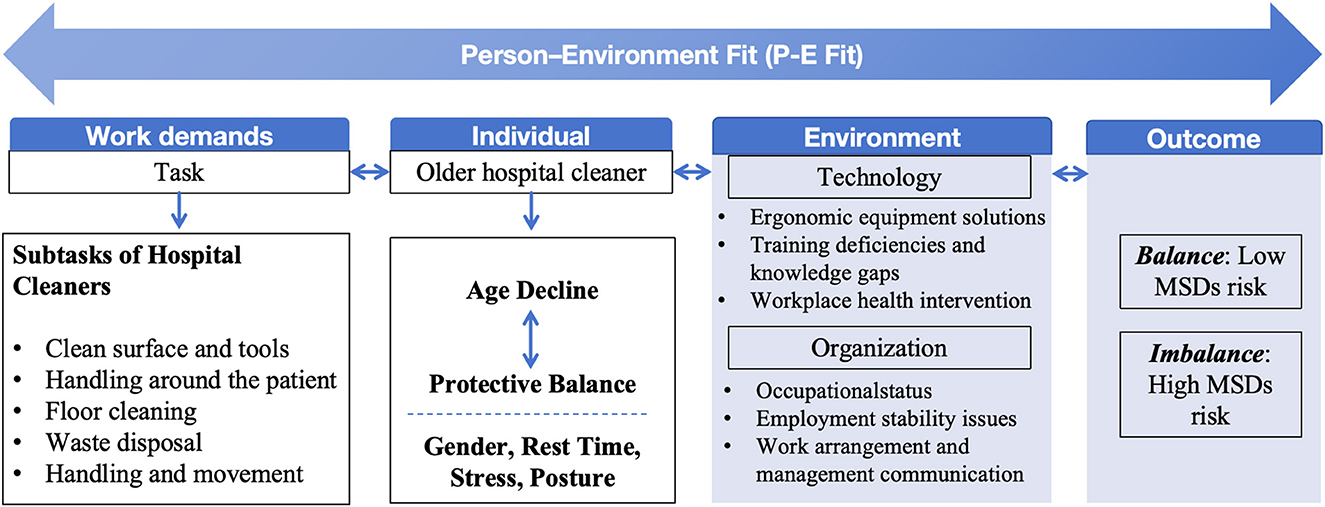
Figure 2. A conceptual model of musculoskeletal disorder risk factors in older hospital cleaners based on Person-Environment Fit (P-E Fit) theory.
The population aged 50 and above generally corresponds to individuals from the later Baby Boomer and early Generation X cohorts. A study based on the P-E Fit model explored person-environment fit from three perspectives: individual-work, individual-group, and individual-supervisor relationships (91). This study indicated that person-environment fit for individuals over 50 can be predicted through person-job fit (91), emphasizing that ensuring alignment between job content and characteristics of this population is critical (92).
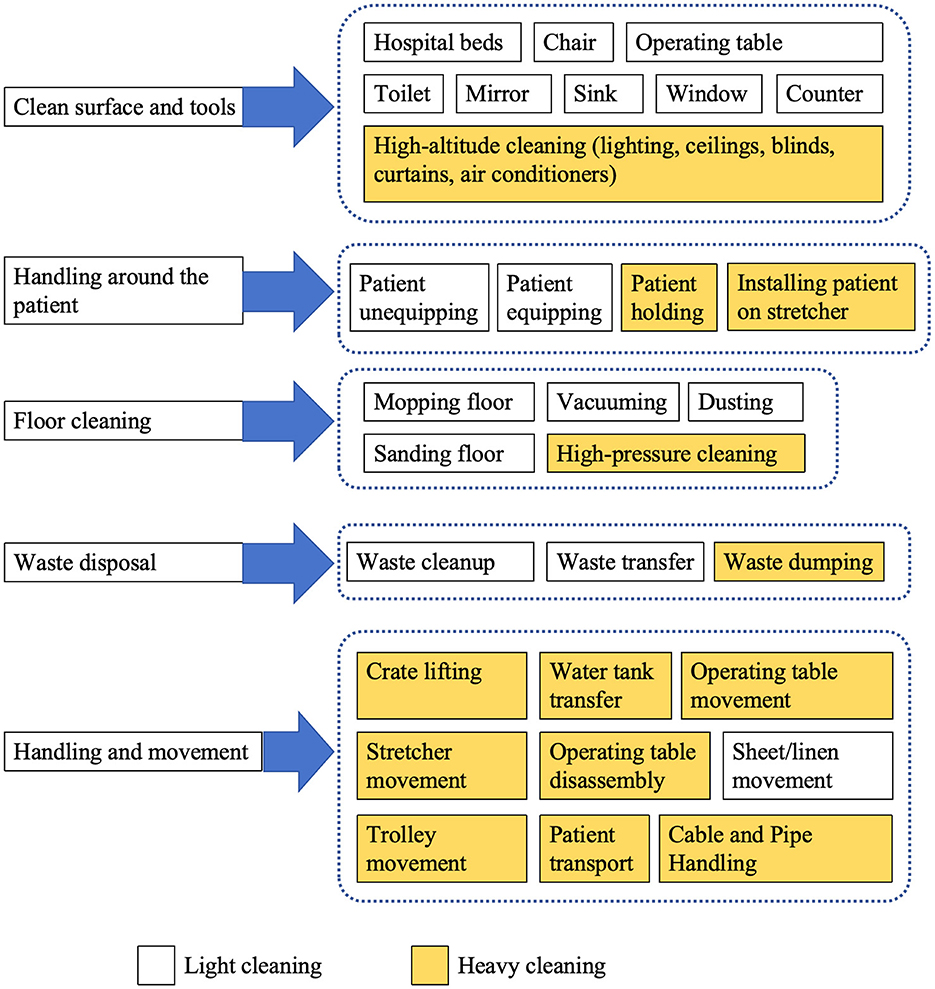
4.1 Subtasks of hospital cleaners
Hospitals encompass diverse workspaces and represent high-risk environments for musculoskeletal disorders (80). Each phase of hospital cleaning work presents specific MSD risk factors (93). One study identified eight daily tasks performed by cleaners, including emptying large trash bins, emptying small (less than 25 pounds) trash bins, mopping, vacuuming, dusting, cleaning toilets, cleaning mirrors, and cleaning sinks; Through Rapid Entire Body Assessment scoring, all tasks were classified as high-risk categories (81). The study by Bello et al. (49) showed that hospital cleaning tasks included preparing cleaning solutions, floor cleaning, window cleaning, mirror cleaning, toilet cleaning, sink cleaning, and countertop cleaning. A study conducted by Laithaisong et al. (44) categorized cleaning work into five main space subcategories: inpatient department, outpatient department, high-level space, office/dormitory, and waste disposal. Another study listed subtasks including waste disposal, lighting management, handling situations around patients, cable and pipe management, patient transport, surface and tool cleaning, various object movement, floor cleaning, box lifting, water tank handling, high-pressure cleaning, operating table movement, stretcher movement, operating table cleaning, operating table disassembly, sheet movement, and cart movement (77).
Given the lack of consensus regarding hospital cleaners' work tasks, we synthesized findings from multiple studies to identify five main categories of hospital cleaning tasks: surface and tool cleaning, handling around patients, floor cleaning, waste disposal, and handling and movement (Figure 3).
Each cleaning task has its unique musculoskeletal disorder risk factors. For example, dusting and scrubbing tasks often involve awkward postures such as overhead reaching, bending, kneeling, squatting, and wrist flexion (93). Based on physical demands, cleaning tasks are typically categorized as light or heavy cleaning in recent occupational studies. Light cleaning includes dusting and cleaning countertops, while heavy cleaning encompasses tasks with higher physical demands (94). One study suggested that high physical demand activities are the primary risk sources for musculoskeletal disorders among hospital cleaners (84). Therefore, heavy cleaning tasks require more attention and intervention measures, including equipment improvements and training in relevant ergonomic knowledge.
4.2 Individual factors associated with MSDs
4.2.1 Age
Previous studies have demonstrated that advancing age is associated with degeneration of the musculoskeletal system and is one of the most common risk factors for MSDs (64, 95). However, regarding hospital cleaners, the impact of age on musculoskeletal disorders has yielded mixed conclusions.
Some studies support age as a risk factor for MSDs. Older cleaners face a contradiction between high physical work demands and declining physical work capacity, making them more susceptible to musculoskeletal injury risks (96). Age-stratified analysis showed that the prevalence of MSDs in the 39–62 age group ranged from 49.1% to 68.96%, while hospital cleaners over 59 years old had a prevalence rate of 66.66%, with particular attention needed for upper back and lower back MSD risks (42, 68, 79). Another study showed that healthcare workers aged 47 and above had approximately twice the risk of developing upper extremity musculoskeletal pain compared to younger employees aged 34 and below (97).
However, other studies have reached opposite conclusions, suggesting that age may sometimes act as a protective factor, which may be explained by lighter work tasks and greater work experience among older cleaners. One study showed that the MSP prevalence in the 45–60 age group (57.1%) was lower than in the 19–34 age group (76.5%) and 35–44 age group (78.0%), which may be because younger employees often handle more physically demanding activities, while older cleaners possess more extensive professional experience (84). This finding is consistent with a US study showing that hospital cleaners aged 39–58 years (68.96%) had higher prevalence rates than those over 59 years (66.66%), while the 18–38 age group had lower prevalence (51.85%) (79). This pattern may be explained by the latency period from musculoskeletal pain symptoms to diagnosis, which can span months to years (78). One study identifie the middle-age period (35–50 years) as a critical prevention window for musculoskeletal disorders, when some physical problems begin to manifest but workers have not yet left their positions (98). Some hospital cleaners choose to continue working despite ill health (83).
Organizations and governments could consider providing occupational screening for hospital cleaners around age 35 and implement preventive interventions during this period. Such screening and interventions may help avoid long-term sick leave in the workplace. During earlier career stages, musculoskeletal training and guidance should be incorporated to promote proper body posture (84).
Some studies found no significant association between age and MSDs (44, 78). One possible explanation is that the smaller number of older cleaners reduced statistical power. Additionally, the selection of adjustment variables may have been overly conservative, which could partially explain why significant risk factors were not identified. Another possibility is the healthy worker effect, where high-risk individuals may have already left employment.
Age-related physiological decline may further amplify the risk of WMSDs among older cleaners. However, the findings across studies remain contradictory (79). Several investigations suggest that WMSD prevalence increases with age, peaks during midlife and then declines thereafter (68, 84). This apparent paradox can be partly explained by the “healthy worker effect,” whereby workers who cannot tolerate pain or physical strain leave employment earlier, resulting in a relatively healthier remaining workforce (99). In addition, older cleaners who remain employed may benefit from lighter work assignments, accumulated experience, and adaptive coping strategies that mitigate physical strain (84). Considering the latency between symptom onset and clinical diagnosis, as well as older workers' higher pain tolerance and greater economic dependence on work, a considerable number of symptomatic but untreated individuals may exist in this group (78, 83, 98). Therefore, older hospital cleaners represent a distinct subgroup shaped by both health selection and age-related physiological decline, whose WMSD patterns and risk factors differ from those of younger workers. Future epidemiological studies focusing specifically on this population are needed to better understand their true disease burden and inform targeted preventive measures.
4.2.2 Gender
Evidence on gender-related MSD risk remains inconsistent across studies (78). Higher MSD prevalence among females may be attributed to gendered division of labor, lower upper-body strength, and additional domestic workload, which increase cumulative physical strain (84). Conversely, male cleaners may experience greater exposure to heavy lifting and forceful exertion, leading to different injury patterns (44). These gendered risk patterns align with findings from other physically demanding occupations, such as surgeons (100), dentists (101) and other occupation (102, 103), where gender-specific task allocation and ergonomic mismatch contribute to differential MSD risks (104).
A study further showed that the two most common types of injuries or disorders among both male and female were sprains/strains and general soreness or pain. Specifically, male cleaners had higher rates of sprains/strains or tears; female cleaners more frequently experienced bruises and contusions (105). These distinctions likely reflect the division between heavy and light cleaning duties.
Future preventive strategies should incorporate gender-sensitive approaches. For female cleaners, interventions should focus on mitigating cumulative musculoskeletal strain and preventing contusions, particularly among those balancing work and childcare responsibilities; for male cleaners, emphasis should be placed on safe lifting techniques and reducing acute sprain and strain injuries.
4.2.3 Rest time
One study indicated that insufficient rest time was associated with a higher prevalence of musculoskeletal disorders. After multivariable adjustment: no leisure time, PRa = 1.14 (95% CI = 1.03–1.27, p = 0.013), occasional leisure time, PRa = 1.10 (95% CI = 1.02–1.20, p = 0.021) (84). These findings suggest a dose-response relationship between rest time and MSD risk, highlighting that insufficient recovery may lead to the accumulation of muscle fatigue and delayed tissue repair. This is consistent with evidence from other physically demanding occupations (e.g., nursing and manufacturing), which has shown that inadequate rest disrupts recovery cycles and increases the likelihood of chronic musculoskeletal pain (106–110).
4.2.4 Stress
In physically demanding work, stress can lead to fatigue while increasing the biomechanical load on muscles and tendons (44). One study indicated that hospital cleaners with a history of severe stress and injury in the past year had higher associations with MSDs occurrence (44), suggesting that screening rates should be increased for this population.
Additionally, the hospital work environment presents unique psychosocial factors, including pressures from the fast-paced medical environment and life-and-death work responsibilities (80). These findings are consistent with other occupational studies showing that high job stress, shift work, and insufficient social support can exacerbate musculoskeletal symptoms through chronic physiological stress responses (5, 111–114).
4.2.5 Posture
A Thai study identified repetitive forward-bending postures of the back as one of the risk factors for MSDs (44). Research has shown that high physical load, repetitive movements, and uncomfortable postures increase the risk of developing musculoskeletal symptoms (51). Specifically, a French study used Rapid Upper Limb Assessment (RULA) to evaluate the ergonomic scores of cleaners' bodies, finding that elbows and forearms face higher risk levels in hospital cleaning work. Tasks such as “moving stretchers” and “moving operating tables” involve heavy object displacement, exposing cleaners to more adverse postures (77). However, some mechanical assistive devices can help alleviate these problems (115). Poor posture leads to uneven load distribution and localized muscle fatigue, explaining its strong link with MSDs. To address this issue, improvements in mop handle design and training for cleaning staff on proper work postures and tool usage are necessary. Similar ergonomic interventions in healthcare and industrial settings have demonstrated reductions in MSD prevalence (116, 117), supporting the need for posture-specific training among hospital cleaners.
4.3 Technology factors associated with MSDs
New technologies and ergonomic equipment can mitigate individual risks in the cleaning occupation (93). For example, a US study designed an improved hospital waste bin that limited the degree of shoulder and trunk flexion required to remove garbage bags, thereby reducing repetitive overhead movements and thereby decreasing the risk of muscle strains or sprains (118). Additionally, another study reported ergonomic solutions for long-handled tools, gloves, vacuum cleaners, mops, buckets, furniture, and waste bins. These improved tools can help cleaners minimize awkward postures and repetitive strain (93). These findings suggest that healthcare facilities should prioritize ergonomic equipment procurement and regular technology upgrades to create safer working environments for cleaning staff.
Training and supervision are fundamental safeguards for ensuring hospital cleaners' health. A Turkish cross-sectional study revealed that most participants in public hospitals had only partial understanding (52.6%) or complete lack of understanding (29.9%) of ergonomic working conditions, with over half (56.2%) expressing a desire to receive relevant training (82). Similarly, a UK study found that approximately 26% of workplace cleaners indicated inadequate cleaning training (42). Additionally, a study targeting female cleaning workers demonstrated that workplace health intervention programs (ergonomic equipment, professional instruction, and designated work time) were more cost-effective than home exercise guidance alone in reducing musculoskeletal pain, enhancing muscle strength, and reducing analgesic use, ultimately improving employee health and reducing sick leave (119). These findings highlight the need for comprehensive ergonomic training programs, structured workplace health interventions, and systematic supervision to address knowledge gaps and reduce MSD risks among hospital cleaners.
4.4 Organizational factors associated with MSDs
Hospital cleaners frequently face complex and demanding work situations. However, their work is often underrecognized, characterized by low social status (47, 48). This occupation also tends to exist within unstable employment relationships (6). One study found that positive organizational factors were associated with lower physical workloads and healthier musculoskeletal conditions among hospital cleaners (51).
Several organizational issues may increase exposure to ergonomic risk factors and consequently elevate the risk of injury and illness among cleaners. These include a lack of influence or control over daily work, monotonous tasks, lack of respect or appreciation, effort-reward imbalance, insufficient supervisor or colleague support, inadequate family support, lack of training or preparation, unclear responsibilities, and poor communication (93). Therefore, comprehensive organizational improvements including enhanced job control, recognition programs, adequate training, and strengthened social support systems are essential for reducing MSD risks in this vulnerable population.
Additionally, research has indicated that task durations exceeding 2 h may expose hospital cleaners to higher MSD risks (44). Conversely, a UK study found that despite cleaners having limited autonomy in choosing cleaning tasks or rest times, reported MSD symptoms did not increase (42). However, focus group discussions in the same study emphasized that regular communication between management and cleaners plays a critical role in improving work performance and overall wellbeing (42). This discrepancy may reflect contextual differences in management practices, workload distribution, and psychosocial support across healthcare settings, highlighting that organizational communication and participatory management can buffer the physical strain associated with cleaning tasks.
4.5 Limitations
This systematic review has several important limitations that should be acknowledged. First, the evidence base was limited, with only 11 studies meeting the inclusion criteria, thereby limiting the comprehensiveness of our findings. The small number of studies with age-stratified data (n = 6) and prevalence reporting (n = 4) further constrained our ability to draw robust conclusions about MSDs in older hospital cleaners. Second, the literature search was restricted to English-language publications. This language limitation may have excluded relevant studies published in other languages and potentially introduced language bias. Future reviews could include non-English databases or employ translation support to reduce this limitation. Third, substantial heterogeneity existed across studies in terms of study designs, outcome measures, and assessment timeframes (7 days vs. 12 months), which precluded meta-analysis and limited comparability of findings.
Fourth, most included studies were cross-sectional in design, which only allows identification of associations rather than causal relationships between risk factors and MSDs. Regarding review process limitations, we initially set the age threshold at 55 years but adjusted it to 50 years due to insufficient studies, which may have introduced selection bias. The varying definitions of “older workers” across studies posed challenges in data synthesis. Additionally, the quality of included studies was variable, with some studies showing methodological limitations in sample selection, confounding control, and outcome measurement. Finally, self-reported outcome measures in most studies may have introduced recall bias and measurement error.
Therefore, these limitations suggest that findings should be interpreted cautiously, and future research with standardized methodologies, larger sample sizes, and longitudinal designs is needed to strengthen the evidence base for this vulnerable population.
5 Conclusion
This systematic review synthesized available evidence on musculoskeletal disorders among older hospital cleaners aged 50 years and above. Across 11 studies, MSD prevalence ranged from 49.1% to 68.96%, with the lower and upper back being the most affected regions. Based on the available evidence, this review proposed a preliminary conceptual model based on P-E Fit theory to understand the complex interactions between individual and environmental factors affecting MSDs in older hospital cleaners. However, further empirical research is needed to validate this theoretical framework in the future. To ensure sustainable employment for older hospital cleaners, task design and assignment require greater attention to achieve optimal person-environment fit (90). Guided by the P-E Fit theory, the findings reveal that the development of MSDs in this population results from the interaction between work demands, individual capacity, and environmental conditions.
Work demands (repetitive cleaning tasks, handling around patients, waste disposal, and prolonged standing) impose continuous physical stress on the musculoskeletal system. Individual factors, including age-related decline, gender differences, insufficient rest, psychological stress, and poor posture, further influence vulnerability to MSDs. Environmental and organizational elements, such as limited ergonomic equipment, inadequate training, unstable employment relationships, and weak managerial communication, exacerbate the imbalance between personal capacity and task requirements.
When work demands exceed individual capacity in a poorly supported environment, this imbalance increases the risk of MSDs; conversely, balance between these dimensions can reduce musculoskeletal strain and promote sustainable employability. Therefore, strategies to improve person–environment fit should focus on ergonomic equipment upgrades, task rotation, rest scheduling, targeted training, and strengthened communication between management and cleaners. Although heterogeneity among studies precluded quantitative synthesis, the findings underscore the need for integrated ergonomic, organizational, and psychosocial interventions to reduce MSD risks and promote the health of aging hospital cleaning staff. Future research with standardized methodologies and larger sample sizes is needed to strengthen the evidence base and establish more definitive risk factors for this vulnerable population.
Author contributions
WZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. YC: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the Jiangsu Provincial Social Science Foundation (Grant No. 22YSC007) and the Fundamental Research Funds for the Central Universities (Grant Nos. 3213042305B2 and 2242024S30013).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1711097/full#supplementary-material
References
1. Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol. (2004) 14:13–23. doi: 10.1016/j.jelekin.2003.09.015
2. Darvishi E, Ghasemi F, Sadeghi F, Abedi K, Rahmati S, Sadeghzade G. Risk assessment of the work-related musculoskeletal disorders based on individual characteristics using path analysis models. BMC Musculoskelet Disord. (2022) 23:616. doi: 10.1186/s12891-022-05573-6
3. Mahdavi N, Motamedzade M, Jamshidi AA, Darvishi E, Moghimbeygi A, Heidari Moghadam R. Upper trapezius fatigue in carpet weaving: the impact of a repetitive task cycle. Int J Occup Safety Ergon. (2018) 24:41–51. doi: 10.1080/10803548.2016.1234706
4. Wang K, Zeng X, Li J, Guo Y, Wang Z. The prevalence and risk factors of work-related musculoskeletal disorders among nurses in China: a systematic review and meta-analysis. Int J Nurs Stud. (2024) 157:104826. doi: 10.1016/j.ijnurstu.2024.104826
5. Darvishi E, Osmani H, Aghaei A, Moloud EA. Hidden risk factors and the mediating role of sleep in work-related musculoskeletal discomforts. BMC Musculoskelet Disord. (2024) 25:256. doi: 10.1186/s12891-024-07387-0
6. Luz EMFd, Munhoz OL, Greco PBT, Santos JLGd, Camponogara S, Magnago TSBdS. Ergonomic risks and musculoskeletal pain in hospital cleaning workers: convergent care research with mixed methods. Rev Latin Am Enferm. (2024) 32:e4176. doi: 10.1590/1518-8345.7048.4176
7. Roberts S, Colombier P, Sowman A, Mennan C, Rölfing JH, Guicheux J, et al. Ageing in the musculoskeletal system: cellular function and dysfunction throughout life. Acta Orthop. (2016) 87:15–25. doi: 10.1080/17453674.2016.1244750
8. Buckle P. Ergonomics and musculoskeletal disorders: overview. Occup Med. (2005) 55:164–7. doi: 10.1093/occmed/kqi081
9. Bernard BP, Putz-Anderson V. Musculoskeletal Disorders and Workplace Factors: A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. Cincinnati, OH: National Institute for Occupational Safety and Health (1997).
10. Briggs AM, Cross MJ, Hoy DG, Sànchez-Riera L, Blyth FM, Woolf AD, et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization world report on ageing and health. Gerontologist. (2016) 56:S243–S55. doi: 10.1093/geront/gnw002
11. Pleho D, HadŽiomerović AM, Pleho K, Pleho J, Remić D, Arslanagić D, et al. Work caused musculoskeletal disorders in health professionals. J Health Sci. (2021) 11:7–16. doi: 10.17532/jhsci.2021.1209
12. Flores LY, Deal JZ. Work-related pain in Mexican American custodial workers. Hisp J Behav Sci. (2003) 25:254–70. doi: 10.1177/0739986303025002007
13. Yassi A. Work-related musculoskeletal disorders. Curr Opin Rheumatol. (2000) 12:124–30. doi: 10.1097/00002281-200003000-00006
14. Amell T, Kumar S. Work-related musculoskeletal disorders: design as a prevention strategy. A review. J Occup Rehab. (2001) 11:255–65. doi: 10.1023/A:1013344508217
15. Sebbag E, Felten R, Sagez F, Sibilia J, Devilliers H, Arnaud L. The world-wide burden of musculoskeletal diseases: a systematic analysis of the World Health Organization Burden of Diseases Database. Ann Rheum Dis. (2019) 78:844–8. doi: 10.1136/annrheumdis-2019-215142
16. Jia N, Zhang H, Ling R, Liu Y, Li G, Ren Z, et al. Epidemiological data of work-related musculoskeletal disorders—China, 2018–2020. China CDC weekly. (2021) 3:383. doi: 10.46234/ccdcw2021.104
17. Bevan S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract Res Clin Rheumatol. (2015) 29:356–73. doi: 10.1016/j.berh.2015.08.002
18. Da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. (2010) 53:285–323. doi: 10.1002/ajim.20750
19. Fung B, Chan K, Lam L, Cheung S, Choy N, Chu K, et al. Study of wrist posture, loading and repetitive motion as risk factors for developing carpal tunnel syndrome. Hand Surg. (2007) 12:13–8. doi: 10.1142/S0218810407003341
20. Eriksen W, Natvig B, Bruusgaard D. Smoking, heavy physical work and low back pain: a four-year prospective study. Occup Med. (1999) 49:155–60. doi: 10.1093/occmed/49.3.155
21. Fredriksson K, Alfredsson L, Thorbjörnsson CB, Punnett L, Toomingas A, Torgén M, et al. Risk factors for neck and shoulder disorders: a nested case–control study covering a 24-year period. Am J Ind Med. (2000) 38:516–28. doi: 10.1002/1097-0274(200011)38:5<516::AID-AJIM4>3.3.CO;2-S
22. Weigall F, Simpson K, Bell A, Kemp L. An assessment of the repetitive manual tasks of cleaners (2005).
23. Sharma A, Mandal BB. 49 Risk of lumbar injury from whole-body vibration exposure: epidemiological insights from field studies on dumper operators. In Occupational and Environmental Medicine. Barcelona: BMJ Publishing Group Ltd. (2025). p. 82.
24. Engkvist I-L, Hjelm EW, Hagberg M, Menckel E, Ekenvall L. Risk indicators for reported over-exertion back injuries among female nursing personnel. Epidemiology. (2000) 11:519–22. doi: 10.1097/00001648-200009000-00006
25. Ariëns GA, Bongers PM, Hoogendoorn WE, Houtman IL, van der Wal G, van Mechelen W. High quantitative job demands and low coworker support as risk factors for neck pain: results of a prospective cohort study. Spine. (2001) 26:1896–901. doi: 10.1097/00007632-200109010-00016
26. Chu PC, Lee CH, Wang J, editors. Work-related and personal factors in musculoskeletal disorders among elderly hospital cleaning workers. in ISEE Conference Abstracts (2023). Research Triangle Park, NC: EHP Publishing.
27. Sharma NK, Tiwari M, Thakur A, Ganguli AK, editors. An ergonomic study of the cleaning workers to identify the prevalence of musculoskeletal disorders in India. in International Conference of the Indian Society of Ergonomics. New York: Springer. (2020).
28. Descatha A, Leclerc A, Chastang J-F, Roquelaure Y. Incidence of ulnar nerve entrapment at the elbow in repetitive work. Scand J Work Environ Health. (2004) 30:234. doi: 10.5271/sjweh.784
29. Coggon D, Croft P, Kellingray S, Barrett D, McLaren M, Cooper C. Occupational physical activities and osteoarthritis of the knee. Arthritis Rheumat Off J Am Coll Rheumatol. (2000) 43:1443–9. doi: 10.1002/1529-0131(200007)43:7<1443::AID-ANR5>3.0.CO;2-1
30. Topaloglu-Ak A, Kurtulmus H, Basa S, Sabuncuoglu O. Can sleeping habits be associated with sleep bruxism, temporomandibular disorders and dental caries among children? Dent Med Prob. (2022) 59:517–22. doi: 10.17219/dmp/150615
31. Gheldof EL, Vinck J, Vlaeyen JW, Hidding A, Crombez G. Development of and recovery from short-and long-term low back pain in occupational settings: a prospective cohort study. Eur J Pain. (2007) 11:841–54. doi: 10.1016/j.ejpain.2006.12.012
32. Darvishi E, Maleki A, Giahi O, Akbarzadeh A. Subjective mental workload and its correlation with musculoskeletal disorders in bank staff. J Manipul Physiol Ther. (2016) 39:420–6. doi: 10.1016/j.jmpt.2016.05.003
33. Chang JH, Wu JD, Liu CY, Hsu DJ. Prevalence of musculoskeletal disorders and ergonomic assessments of cleaners. Am J Ind Med. (2012) 55:593–604. doi: 10.1002/ajim.22064
34. Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses' aides. Occup Environ Med. (2004) 61:398–404. doi: 10.1136/oem.2003.008482
35. Rahman A, Palaneeswaran E, Kulkarni A, Zou P, editors. Musculoskeletal health and safety of aged workers in manual handling works. in 2015 International Conference on Industrial Engineering and Operations Management (IEOM). Dubai: IEEE (2015).
36. Cross S, Gon G, Morrison E, Afsana K, Ali SM, Manjang T, et al. An invisible workforce: the neglected role of cleaners in patient safety on maternity units. Glob Health Action. (2019) 12:1480085. doi: 10.1080/16549716.2018.1480085
37. Goderis B, Muns S. Decent old-age incomes for all? A microdata analysis of poverty amossng older adults in the Netherlands. Int J Soc Welfare. (2025) 34:e70020. doi: 10.1111/ijsw.70020
38. Hofäcker D, Naumann E. The emerging trend of work beyond retirement age in Germany. Zeit Gerontol Geriatr. (2015) 48:473–9. doi: 10.1007/s00391-014-0669-y
39. Yeo H. Are there sufficient jobs for older workers in a local market? Educ Gerontol. (2025) 51:1038–100. doi: 10.1080/03601277.2025.2450135
40. Oakman J, Clays E, Jørgensen MB, Holtermann A. Are occupational physical activities tailored to the age of cleaners and manufacturing workers? Int Arch Occup Environ Health. (2019) 92:185–93. doi: 10.1007/s00420-018-1364-x
41. Labor USDo. Janitors and Cleaners, Except Maids and Housekeeping Cleaners. Washington, DC.: US Government Printing Office (2023).
42. Woods V, Buckle P. Musculoskeletal ill health amongst cleaners and recommendations for work organisational change. Int J Ind Ergon. (2006) 36:61–72. doi: 10.1016/j.ergon.2005.08.001
43. Lasrado OE, Møllerløkken OJ, Moen BE, Van den Bergh G. Musculoskeletal symptoms among hospital cleaners. Arch Environ Occup Health. (2017) 72:87–92. doi: 10.1080/19338244.2016.1160862
44. Laithaisong T, Aekplakorn W, Suriyawongpaisal P, Tupthai C, Wongrathanandha C. The prevalence and risk factors of musculoskeletal disorders among subcontracted hospital cleaners in Thailand. J Health Res. (2022) 36:802–12. doi: 10.1108/JHR-01-2021-0040
45. Matlow AG, Wray R, Richardson SE. Attitudes and beliefs, not just knowledge, influence the effectiveness of environmental cleaning by environmental service workers. Am J Infect Control. (2012) 40:260–2. doi: 10.1016/j.ajic.2011.02.024
46. Berni LB, Beck CLC, Prestes FC, Silva RMd, Bublitz S, Lamb F. Indicators of pleasure/pain in hygiene and cleaning outsourced workers of a university hospital. Rev Rene. (2016) 17:155–64. doi: 10.15253/2175-6783.2016000200002
47. Dancer SJ. Hospital cleaning: past, present, and future. Antimicrob Resist Infect Control. (2023) 12:80. doi: 10.1186/s13756-023-01275-3
48. Dancer SJ. Hospital cleaning in the 21st century. Eur J Clin Microbiol Infect Dis. (2011) 30:1473–81. doi: 10.1007/s10096-011-1250-x
49. Bello A, Quinn MM, Perry MJ, Milton DK. Characterization of occupational exposures to cleaning products used for common cleaning tasks-a pilot study of hospital cleaners. Environ Health. (2009) 8:11. doi: 10.1186/1476-069X-8-11
50. Korshøj M, Krustrup P, Jespersen T, Søgaard K, Skotte JH, Holtermann A, et al. 24-h assessment of physical activity and cardio-respiratory fitness among female hospital cleaners: a pilot study. Ergonomics. (2013) 56:935–43. doi: 10.1080/00140139.2013.782427
51. Unge J, Ohlsson K, Nordander C, Hansson G-Å, Skerfving S, Balogh I. Differences in physical workload, psychosocial factors and musculoskeletal disorders between two groups of female hospital cleaners with two diverse organizational models. Int Arch Occup Environ Health. (2007) 81:209–20. doi: 10.1007/s00420-007-0208-x
52. Johansson EE, Hamberg K, Lindgren G. Westman G. “How could I even think of a job?”-Ambiguities in working life in a group of female patients with undefined musculoskeletal pain. Scand J Primary Health Care. (1997) 15:169–74. doi: 10.3109/02813439709035022
53. Kumar R, Kumar S. Musculoskeletal risk factors in cleaning occupation—A literature review. Int J Ind Ergon. (2008) 38:158–70. doi: 10.1016/j.ergon.2006.04.004
54. Park J, Kim SG. Park J-s, Han B, Kim KB, Kim Y. Hazards and health problems in occupations dominated by aged workers in South Korea. Ann Occup Environ Med. (2017) 29:27. doi: 10.1186/s40557-017-0177-9
55. Wang M-H, Chen Y-L, Chiou W-K. Using the OVAKO working posture analysis system in cleaning occupations. Work. (2019) 64:613–21. doi: 10.3233/WOR-193022
56. Zhou J, Xie S, Xu S, Zhang Y, Li Y, Sun Q, et al. From pain to progress: comprehensive analysis of musculoskeletal disorders worldwide. J Pain Res. (2024) 3455–72. doi: 10.2147/JPR.S488133
57. Charles LE, Loomis D, Demissie Z. Occupational hazards experienced by cleaning workers and janitors: a review of the epidemiologic literature. Work. (2009) 34:105–16. doi: 10.3233/WOR-2009-0907
58. Sánchez-Rodríguez C, Capitán-Moyano L, Malih N, Yanez AM, Bennasar-Veny M, Velasco-Roldán O, et al. Prevalence of musculoskeletal disorders among hotel housekeepers and cleaners: a systematic review with meta-analysis. Musculoskelet Sci Pract. (2024) 69:102890. doi: 10.1016/j.msksp.2023.102890
59. Luz EMFd, Munhoz OL, Morais BX, Silva SCd, Almeida FO, Magnago TSBdS. Strategies to minimize ergonomic risks in the cleaning staff: an integrative review. Cogitare Enfermagem. (2021) 26:e71073. doi: 10.5380/ce.v26i0.71073
60. Van Kampen V, Hoffmeyer F, Seifert C, Brüning T, Bünger J. Occupational health hazards of street cleaners–a literature review considering prevention practices at the workplace. Int J Occup Med Environ Health. (2020) 33:701–32. doi: 10.13075/ijomeh.1896.01576
61. Lin J-H, Lee W, Smith CK, Yragui NL, Foley M, Shin G, et al. Cleaning in the 21st Century: the musculoskeletal disorders associated with the centuries-old occupation–A literature review. Appl Ergon. (2022) 105:103839. doi: 10.1016/j.apergo.2022.103839
62. Agency UNR. Older Persons (2025). Available online at: https://emergency.unhcr.org/protection/persons-risk/older-persons (Accessed September 20, 2025).
63. World Health Organization. Ageing (2025). Available online at: https://www.who.int/health-topics/ageing#tab=tab_1 (Accessed September 20, 2025).
65. McCarthy J, Heraty N, Cross C, Cleveland JN. Who is considered an ‘older worker'? Extending our conceptualisation of ‘older'from an organisational decision maker perspective. Hum Resourc Manag J. (2014) 24:374–93. doi: 10.1111/1748-8583.12041
66. Cleveland JN, Lim AS. Employee age and performance in organizations. Aging and work in the 21st century. (2007) 109–37.
67. Cleveland JN, Hanscom M. What is old at work? Moving past chronological age. In Parry E, McCarthy J, editors. The Palgrave Handbook of Age Diversity and Work. New York: Springer (2016). p. 17–46.
68. Luz EMFd, Munhoz OL, Greco PBT, Morais BX, Camponogara S, Magnago TSBdS. Prevalence and factors associated with musculoskeletal pain among hospital cleaning staff. Rev Bras Enferm. (2024) 77:e20230237. doi: 10.1590/0034-7167-2023-0237
69. Oakman J, Neupane S, Nygård C-H. Does age matter in predicting musculoskeletal disorder risk? An analysis of workplace predictors over 4 years. Int Archiv Occup Environ Health. (2016) 89:1127–36. doi: 10.1007/s00420-016-1149-z
70. Man H, Vinstrup J, Andersen LL. Work and lifestyle factors associated with musculoskeletal pain among professional cleaners: a cross-sectional study. Int J Occup Safety Ergon. (2025) 31:522–8. doi: 10.1080/10803548.2025.2453319
71. Paggi ME, Jopp DS. Outcomes of occupational self-efficacy in older workers. Int J Aging Hum Dev. (2015) 80:357–78. doi: 10.1177/0091415015607640
72. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
73. Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Library Assoc JMLA. (2018) 106:420. doi: 10.5195/jmla.2018.345
74. Porritt K, Gomersall J, Lockwood C. JBI's systematic reviews: study selection and critical appraisal. AJN Am J Nurs. (2014) 114:47–52. doi: 10.1097/01.NAJ.0000450430.97383.64
75. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Systematic reviews of etiology and risk. JBI Manual Evidence Synthesis. (2020) 1:217–69. doi: 10.46658/JBIRM-17-06
76. Munn Z, Stone JC, Aromataris E, Klugar M, Sears K, Leonardi-Bee J, et al. Assessing the risk of bias of quantitative analytical studies: introducing the vision for critical appraisal within JBI systematic reviews. JBI Evidence Synthesis. (2023) 21:467–71. doi: 10.11124/JBIES-22-00224
77. Koskas D, Vignais N. Physical ergonomic assessment in cleaning hospital operating rooms based on inertial measurement units. Bioengineering. (2024) 11:154. doi: 10.3390/bioengineering11020154
78. Zamora-Chávez SC, Vásquez-Alva R, Luna-Muñoz C, Carvajal-Villamizar LL. Factores asociados a trastornos musculoesqueléticos en trabajadores de limpieza del servicio de emergencia de un hospital terciario. Rev Facult Med Hum. (2020) 20:388–96. doi: 10.25176/RFMH.v20i3.3055
79. Salwe K, Kumar S, Hood J. Nonfatal occupational injury rates and musculoskeletal symptoms among housekeeping employees of a hospital in Texas. J Environ Public Health. (2011) 1:382510. doi: 10.1155/2011/382510
80. Gillen M, Yen IH, Trupin L, Swig L, Rugulies R, Mullen K, et al. The association of socioeconomic status and psychosocial and physical workplace factors with musculoskeletal injury in hospital workers. Am J Ind Med. (2007) 50:245–60. doi: 10.1002/ajim.20429
81. Schwartz A, Gerberich SG, Kim H, Ryan AD, Church TR, Albin TJ, et al. Janitor ergonomics and injuries in the safe workload ergonomic exposure project (SWEEP) study. Appl Ergon. (2019) 81:102874. doi: 10.1016/j.apergo.2019.102874
82. Gedik T. Ergonomic analysis of workplace furniture in hospitals: a public hospital example. Wood Indus Eng. (2021) 3:23–30. doi: 10.1080/165019701750419617
83. Landstad BJ, Schüldt K, Ekholm J, Broman L, Bergroth A. Women at work despite ill health: diagnoses and pain before and after personnel support. A prospective study of hospital cleaners/home-help personnel with comparison groups. J Rehab Med. (2001) 33:216–24. doi: 10.1080/165019701750419617
84. Luz EMFd, Magnago TSBdS, Greco PBT, Ongaro JD, Lanes TC, Lemos JC. Prevalence and factors associated with musculoskeletal pain in hospital cleaning workers. Texto Contexto Enfermagem. (2017) 26:e00870016. doi: 10.1590/0104-07072017000870016
85. Hamberg-van Reenen HH, Ariëns GA, Blatter BM, Van Der Beek AJ, Twisk JW, Van Mechelen W, et al. Is an imbalance between physical capacity and exposure to work-related physical factors associated with low-back, neck or shoulder pain? Scand J Work Environ Health. (2006) 190–7. doi: 10.5271/sjweh.998
86. Holtermann A, Blangsted A, Christensen H, Hansen K, Søgaard K. What characterizes cleaners sustaining good musculoskeletal health after years with physically heavy work? Int Arch Occup Environ Health. (2009) 82:1015–22. doi: 10.1007/s00420-009-0401-1
87. Kristof-Brown A, Guay RP. Person–environment fit. In Zedeck S, editor. Handbook of Industrial and Organizational Psychology. Washington, DC: American Psychological Association (2011). p. 3–50.
88. Popa AE, Bejenaru A, Mitrea EC, Morândău F, Pogan L. Return to work after chronic disease: a theoretical framework for understanding the worker-employer dynamic. Chronic Illn. (2023) 19:704–18. doi: 10.1177/17423953221117852
89. Oakman J, de Wind A, van den Heuvel SG, van der Beek AJ. Work characteristics predict the development of multi-site musculoskeletal pain. Int Arch Occup Environ Health. (2017) 90:653–61. doi: 10.1007/s00420-017-1228-9
90. Karwowski W. Managing workloads to optimize performance, health, and well-being. in International Encyclopedia of Ergonomics and Human Factors. Vol. 3. Boca Raton, FL: CRC Press (2006). p. 2223–7.
91. Deschênes A-A. Satisfaction with work and person–environment fit: are there intergenerational differences? An examination through person–job, person–group and person–supervisor fit. Int J Organ Theory Behav. (2021) 24:60–75. doi: 10.1108/IJOTB-02-2020-0025
92. Oakman J, Wells Y. Working longer: what is the relationship between person–environment fit and retirement intentions? Asia Pac J Hum Resourc. (2016) 54:207–29. doi: 10.1111/1744-7941.12075
93. Goggins R. Hazards of cleaning strategies for reducing exposures to ergonomic risk factors. Prof Saf. (2007) 52.
94. Calvet B, Riel J, Couture V, Messing K. Work organisation and gender among hospital cleaners in Quebec after the merger of ‘light'and ‘heavy'work classifications. Ergonomics. (2012) 55:160–72. doi: 10.1080/00140139.2011.576776
95. Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. (2010) 24:769–81. doi: 10.1016/j.berh.2010.10.002
96. Lim MC, Lukman KA, Giloi N, Lim JF, Avoi R, Rahim SSSA, et al. Prevalence of upper limb musculoskeletal disorders and its associated risk factors among janitorial workers: a cross-sectional study. Ann Med Surg. (2022) 73:103201. doi: 10.1016/j.amsu.2021.103201
97. Barbosa REC, Assunção AÁ, de Araújo TM. Musculoskeletal pain among healthcare workers: an exploratory study on gender differences. Am J Ind Med. (2013) 56:1201–12. doi: 10.1002/ajim.22215
98. Mozafari A, Vahedian M, Mohebi S, Najafi M. Work-related musculoskeletal disorders in truck drivers and official workers. Acta Med Iran. (2015) 432–8.
99. Shah D. Healthy worker effect phenomenon. Indian J Occup Environ Med. (2009) 13:77–9. doi: 10.4103/0019-5278.55123
100. Abo-Naser L, Leibner G, Vilenski RG, Luria S, Kriger Y. Gender differences in prevalence of musculoskeletal disorders (MSDs) among surgeons. Perioperat Care Operat Room Manag. (2025) 40:100542. doi: 10.1016/j.pcorm.2025.100542
101. Berniyanti T, Palupi R, Alkadasi BA, Setyowati D, Sari KP, Fitrihana RN, et al. Gender-Specific risk of MSDs in Dentists: the impact of work posture. Malays J Med Health Sci. (2025) 21. doi: 10.47836/mjmhs.21.s2.11
102. Das B. Gender differences in prevalence of musculoskeletal disorders among the rice farmers of West Bengal, India. Work. (2015) 50:229–40. doi: 10.3233/WOR-131694
103. Park J, Kim Y, Han B. Work sectors with high risk for work-related musculoskeletal disorders in Korean men and women. Saf Health Work. (2018) 9:75–8. doi: 10.1016/j.shaw.2017.06.005
104. Estryn-Behar M, Kaminski M, Peigne E, Maillard M, Pelletier A, Berthier C, et al. Strenuous working conditions and musculo-skeletal disorders among female hospital workers. Int Arch Occup Environ Health. (1990) 62:47–57. doi: 10.1007/BF00397848
105. USDL. Nonfatal Occupational Injuries and Illnesses Requiring Days Away From Work, 2015. Washington, DC: U.S. Department of Labor (2016).
106. Tang L, Wang G, Zhang W, Zhou J. The prevalence of MSDs and the associated risk factors in nurses of China. Int J Ind Ergon. (2022) 87:103239. doi: 10.1016/j.ergon.2021.103239
107. Attarchi M, Raeisi S, Namvar M, Golabadi M. Association between shift working and musculoskeletal symptoms among nursing personnel. Iran J Nurs Midwifery Res. (2014) 19:309–14.
108. Onovughe EC. Musculoskeletal disorders among nurses: a systematic literature review (bachelor's thesis). Vaasa: Vaasa University (2025).
109. Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am J Ind Med. (2006) 49:964–71. doi: 10.1002/ajim.20330
110. Santos A, Ramos H, Ramasamy G, Fernandes C. Musculoskeletal pain among migrant workers in the Malaysian manufacturing industry: the impact of the physical environment, workload and work patterns. Pertanika J Soc Sci Hum. (2015) 23:315–24. https://www.researchgate.net/publication/314121074_Musculoskeletal_Pain_among_Migrant_Workers_in_the_Malaysian_Manufacturing_Industry_The_Impact_of_the_Physical_Environment_Workload_and_Work_Patterns
111. Torp S, Riise T, Moen BE. The impact of social and organizational factors on workers' coping with musculoskeletal symptoms. Phys Ther. (2001) 81:1328–38. doi: 10.1093/ptj/81.7.1328
112. Warren N. Work stress and musculoskeletal disorder etiology: the relative roles of psychosocial and physical risk factors. Work. (2001) 17:221–34. doi: 10.3233/WOR-2001-00191
113. Bezzina A, Austin E, Nguyen H, James C. Workplace psychosocial factors and their association with musculoskeletal disorders: a systematic review of longitudinal studies. Workplace Health Saf. (2023) 71:578–88. doi: 10.1177/21650799231193578
114. Asuquo EG, Murphy-Tighe S, Ryan R, O'Sullivan K. How is social support defined, categorized and measured in studies of work-related musculoskeletal disorders among hospital nurses: a scoping review. J Adv Nurs. (2025) 81:1130–41. doi: 10.1111/jan.16356
115. Cristoforetti A, Tessarolo F, Rigoni M, Nollo G, editors. Remote center of motion and synchronized rotation for a motorized surgical table. in 2020 IEEE 20th Mediterranean Electrotechnical Conference (MELECON). Palermo: IEEE (2020).
116. Jin X, Dong Y, Yang L, Huang W, Cao L, Zhang Z, et al. Ergonomic interventions to improve musculoskeletal disorders among vehicle assembly workers: a one-year longitudinal study. BMC Public Health. (2025) 25:824. doi: 10.1186/s12889-025-21798-1
117. Hawke AL. Patient Handling Interventions and Their Role in Reducing Musculoskeletal Disorders Among Healthcare Workers. [Ph.D Thesis]. Michigan Technological University, Houghton, MI, United States (2025).
118. Padilla R, Baltich J, Fathallah F, editors. Development of an ergonomic waste container for hospitals. in Proceedings of the Human Factors and Ergonomics Society Annual Meeting. Los Angeles, CA: SAGE Publications (2008).
Keywords: musculoskeletal disorders, older hospital cleaners, prevalence, risk factors, systematic review
Citation: Zhou W, Gu K and Chen Y (2025) Musculoskeletal disorders among older hospital cleaners: a systematic review of prevalence and risk factors. Front. Public Health 13:1711097. doi: 10.3389/fpubh.2025.1711097
Received: 23 September 2025; Accepted: 03 November 2025;
Published: 24 November 2025.
Edited by:
Dragan Mijakoski, Institute of Occupational Health of RNM, North MacedoniaReviewed by:
Ebrahim Darvishi, Kurdistan University of Medical Sciences, IranMilad Gholami, Arak University of Medical Sciences, Iran
Copyright © 2025 Zhou, Gu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaizhi Gu, OTk0MDk1NDQzQHFxLmNvbQ==
 Wei Zhou
Wei Zhou Kaizhi Gu2*
Kaizhi Gu2*