- 1School of Nursing, Bouvé College of Health Sciences, Northeastern University, Boston, MA, United States
- 2Health Promotion Research Center, School of Public Health, University of Washington, Seattle, WA, United States
- 3Herbert Wertheim School of Public Health and Human Longevity Science, University of California, San Diego, San Diego, CA, United States
- 4Department of Population & Community Health, College of Public Health, University of North Texas Health Science Center, Fort Worth, TX, United States
- 5School of Human Services, University of Cincinnati, Cincinnati, OH, United States
- 6Human Performance and Nutrition Research Institute, Oklahoma State University, Stillwater, OK, United States
- 7Center for Community Health and Aging, Department of Environmental and Occupational Health, School of Public Health, Texas A&M University, College Station, TX, United States
- 8Center for Community Health and Aging, Department of Health Behavior, School of Public Health, Texas A&M University, College Station, TX, United States
Background: Rates of social disconnectedness and depression have intensified in recent years. Yet, little is known about how they relate to one another across different age groups. This study assessed the relationship between social disconnectedness and depressive symptoms among U. S. adults of varying ages using an internet-delivered survey data collected between November 2021 and January 2022 from a non-probabilistic national sample of 2,496 employed adults aged 18–89 years.
Methods: Participants completed Upstream Social Interaction Risk Scale (U-SIRS-13) and the Patient Health Questionnaire short version (PHQ-2). Within each of five age groups (18–29, 30–39, 40–49, 50–59, 60+), descriptive statistics and Pearson’s r correlations were calculated for U-SIRS-13 and PHQ-2. Subsequently, logistic regression models were fitted to assess the relationship between the U-SIRS-13 and PHQ-2 (a score of 3 or greater indicated possible depression), controlling for sociodemographic covariates.
Results: The prevalence of possible depression among participants was 31.6%, which ranged from 46.8% (ages 18–29) to 10.5% (ages 60+). U-SIRS-13 and PHQ-2 had significant associations in all age groups (Pearson’s r range: 0.283–0.275, p < 0.001). Holding sociodemographic covariates constant, higher U-SIRS-13 scores were consistently associated with increased odds of possible depression across age groups (Odds Ratio range: 1.24–1.50, p < 0.001). While possible depression was more prevalent among younger age groups (18-29 and 30-39), the relationship between social disconnectedness and possible depression was stronger among older age groups (40–49, 50–59, and 60+).
Conclusion: This finding supports that regardless of age, individuals who experience higher levels of social disconnectedness are more likely to have possible depression Coordinated efforts are needed to address depressive symptomology and facilitate meaningful interactions with others in all age groups.
Introduction
Recent years have seen a notable increase in the prevalence of depression, social isolation, and loneliness in various age groups in the United States (U.S.) (1, 2). Depression is a pervasive mental health condition that affects millions of people globally across all ages, contributing significantly to the burden of disease (3). The onset of major depression occurs in early or late life. Nearly 40% of individuals experience their first episode of depression before the age of 20, with prevalence peaking during the second and third decades of life (3). Over half of major depression cases occur in older age (age 60 or older), also known as the late onset depression (4). Depression affects well-being and physical health and also increases risky health behaviors including alcohol and substance use (5). Concurrently, current national reports from 2022 estimate that about 25% of U.S. older adults and about 40% of U.S. young adults experience social isolation or loneliness (6). Prior studies also indicate that nearly half of U.S. adults report feeling lonely (7, 8), with most recent 2023 survey showing that nearly 30% of U.S. adults ages 18 and 34 report feeling lonely at least weekly compared to about 17% older adults report loneliness (9). Conversely, older adults ages 65 and older report more social isolation than their younger counterparts (10, 11).
A large body of research has demonstrated that social constructs (e.g., such as social isolation, loneliness, and low social support) are robustly associated with depressive symptoms across age groups (12–14). Social isolation typically refers to the objective lack or infrequency of social contacts, such as living alone or having limited interaction with others, while loneliness refers to a subjective perception of inadequate social connection (15). Both of these constructs captures important but distinct dimensions of social experience, and together, they have informed much of what we know about the social determinants of mental health. However, these narrower constructs are often used in silo, either on the objective absence of social ties (e.g., social isolation) or the subjective experience of unmet social needs (e.g., loneliness), limiting the understanding of other relevant dimensions of risk that stem from the broader, everyday social interactions that combine multidimensional constructs. More recently, researchers have begun to explore broader, integrative concept of social disconnectedness—an umbrella term that encompasses the concepts of social isolation and loneliness as well as social interactions and engagement (16–18)—which has emerged as a critical determinant of physical and mental health (19). Social disconnectedness is a broader construct that encompasses dimensions of both social isolation and loneliness, capturing a wide range of structural and perceived deficits in social engagement and support. Use of this umbrella term may offer greater utility in identifying at-risk individuals, particularly among groups where social risk manifests differently, which is especially relevant for prevention and intervention efforts.
The interplay between social disconnectedness and depressive symptoms is complex and may be bidirectional (12). Existing evidence about the association between social disconnectedness and depressive symptoms suggests that people who are socially disconnected (i.e., feel lonely or isolated, report low social support, and experience strain in their relationships) are more likely to develop symptoms of depression (14, 20). However, depressive symptoms themselves can contribute to reduced social motivation, avoidance of interaction, and negative social cognitions, which in turn may increase the likelihood of further social withdrawal and subsequent disconnection (21, 22). This reciprocal pattern may create a reinforcing cycle in which poor mental health and increased social disconnectedness exacerbate one another over time.
Factors such as the replacement of personal communication channels with technology-mediated ones, the advent of technology communication, changes in family dynamics and structure, and the impact of the COVID-19 pandemic have been implicated in these rising trends (23, 24). Despite the evidence demonstrating a significant relationship between social disconnectedness and depressive symptoms in specific age groups (i.e., adolescents or older adults), there is a paucity of research examining how this association varies across early adulthood to older age (18–89 years), and much of this work has focused on single, narrowly defined constructs. Less is known about how broader construct of social disconnectedness, which may holistically capture a wider array of social interactions, relate to depressive symptoms across age cohorts.
Closing the research gap regarding the age-specific dynamics of social disconnectedness and depressive symptoms may contribute to the broader understanding of social and mental health across the age cohorts. As such, this study seeks to address that gap by examining how the strength of the association between social disconnectedness and depressive symptoms varies across five age groups spanning early adulthood to older age (i.e., 18–29, 30–39, 40–49, 50–59, 60+). Based on prior literature that utilized narrower constructs, we hypothesized that, while the prevalence rates of social disconnectedness and depressive symptoms would vary by age, their association would be significant across all age groups even after controlling for sociodemographic covariates.
Methods
Data were analyzed from a cross-sectional sample of employed adults collected using an internet-delivered questionnaire. Participants were recruited through Qualtrics Online Panels (25) using a non-probability sampling approach between November 22, 2021, and January 4, 2022. The overall purpose of the study was to identify the wellness of working Americans following the COVID-19 pandemic and identify perceptions about work culture. Given the study focus, eligibility criteria required all participants to be age 18 years or older, a full-time employee, and a resident of the United States. After eligible participants were identified by Qualtrics, they were presented with a link to the online questionnaire, which required acknowledgment of an Institutional Review Board (IRB)-approved information sheet. Participation in the study was voluntary, and participants could choose to stop taking the survey at any time. While attention-check questions were not incorporated into the instrument, initial data quality checks were performed by Qualtrics to ensure participants met eligibility criteria, completed all questionnaire items, and thoughtfully completed the instrument (e.g., time taken to complete, pattern responding, duplicate respondents) (26). Qualtrics maintains a network of managed panels composed of U.S. adults who voluntarily opt in to participate in online surveys. Eligibility for this study required participants to be currently employed, reside in the United States, and be between the ages of 18 and 60. Quotas were applied to approximate national demographic distributions (e.g., age, gender, race/ethnicity, and U.S. Census quartiles). Potential participants were recruited by Qualtrics to complete the online questionnaire. A total of 2,932 participants initiated the questionnaire, of which 2,508 completed the questionnaire (85.6%). Of those, 12 participants were omitted from analyses for missing data on specific variables of interest, resulting in an analytic sample of 2,496 employed adults. The Texas A&M University IRB reviewed and approved all components of this study (#IRB2021-1127 M).
Measures
Depressive symptoms
The Patient Health Questionnaire-2 (PHQ-2) was used to identify depressive symptoms among participants (27, 28). This two-item scale contains the first two items of the PHQ-9, a validated screening measure for depression (29), which measures the two cardinal symptoms of depression: depressed mood and anhedonia. The PHQ-2 asked participants to report the frequency they “felt down, sad, or hopeless” and “had little interest or pleasure in doing things” in the past 2 weeks. Response choices were on a 4-point Likert scale and ranged from “not at all” (scored 0) to “nearly every day” (scored 3). These items were summed, with a total score ranging from 0 to 6. The scores were dichotomized using the recommended cutoff of ≥3, indicating those with possible depression (30). The PHQ-2 was selected for its efficiency and validated use in large-scale population studies, including online and survey-based research, where minimizing participant burden is important. The PHQ-2 has demonstrated strong correlation with the PHQ-9 and high diagnostic accuracy in identifying major depressive disorder across diverse populations, including adults in community and primary care settings (27, 31).
Social disconnectedness
The Upstream Social Interaction Risk Scale (U-SIRS-13) was used to identify the risk of social disconnectedness among participants (32, 33). This 13-item scale was developed to specifically assess the broader concept of social disconnectedness among older adults in clinical and community settings (32, 33). asked participants to report the frequency of feeling disconnected in terms of physical opportunities to interact with others and the emotional fulfillment of such interactions (or lack thereof). Response choices were on a 3-point Likert scale, including “never” (scored 1), “sometimes” (scored 2), and “often” (scored 3). Based on the practical scoring recommendations provided by Smith and Barrett (33), each item was then dichotomized based on the directionality of the wording to create items scored as “no risk” (scored 0) and “risk” (scored 1). Items were then summed to generate a continuous score from 0 to 13, with higher scores indicating higher risk for social disconnectedness. Cronbach’s alpha for the U-SIRS-13 in the sample was 0.78, which aligns with reliability coefficients identified in other studies (33). Unlike scales that focus either on loneliness or social isolation, the U-SIRS-13 includes items that assess structural, functional, and quality aspects of social connection (33)—such as frequency of social and religious participation, access to social support, and feelings of companionship or belonging. This multidimensional scale allows for a more comprehensive assessment of individuals at risk for poor social connectedness across multiple life contexts.
Sociodemographic covariates
Analyses were performed across five participant age groups (i.e., ages 18–29 years, 30–39 years, 40–49 years, 50–59 years, 60 + years). Age was also analyzed continuously within each age group, respectively. Other sociodemographic characteristics included in analyses were sex (i.e., male, female), ethnicity (i.e., non-Hispanic, Hispanic), and race (i.e., White, Black, Asian, Other/Multiple Races).
Data analysis
All analyses were performed using the IBM SPSS version 29. Descriptive statistics were calculated for all variables of interest, which were initially compared by participant age group and PHQ-2 score ≥3. When comparing across age groups, chi-square tests were used for categorical variables and one-way ANOVA were used for continuous variables. When comparing across PHQ-2 score ≥3, chi-square tests were used for categorical variables and two-tailed independent sample t-tests were used for continuous variables. Cronbach’s alpha coefficients were calculated to identify the reliability of the U-SIRS-13 for the total sample and each age group. Point-biserial correlation coefficients were calculated to identify the strength and direction of relationships between U-SIRS-13 (continuous) and PHQ-2 score ≥3 (dichotomous) for the total sample and each age group. Then, a series of logistic regression models were fitted to assess the associations of U-SIRS-13 and covariates (i.e., age, sex, ethnicity, and race) on PHQ-2 score ≥3 for all participants, then separately within each age group. For each model, PHQ-2 score <3 served as the referent category with statistical significance set at p < 0.05. Collinearity statistics were calculated (i.e., Variance Inflation Factor (VIF) and tolerance), which indicated no multicollinearity among independent variables. To account for multiple analyses and reduce risks for Type I errors, a Benjamini Hochberg False Detection Rate of 95% was used (34). All significant findings met these criteria.
Results
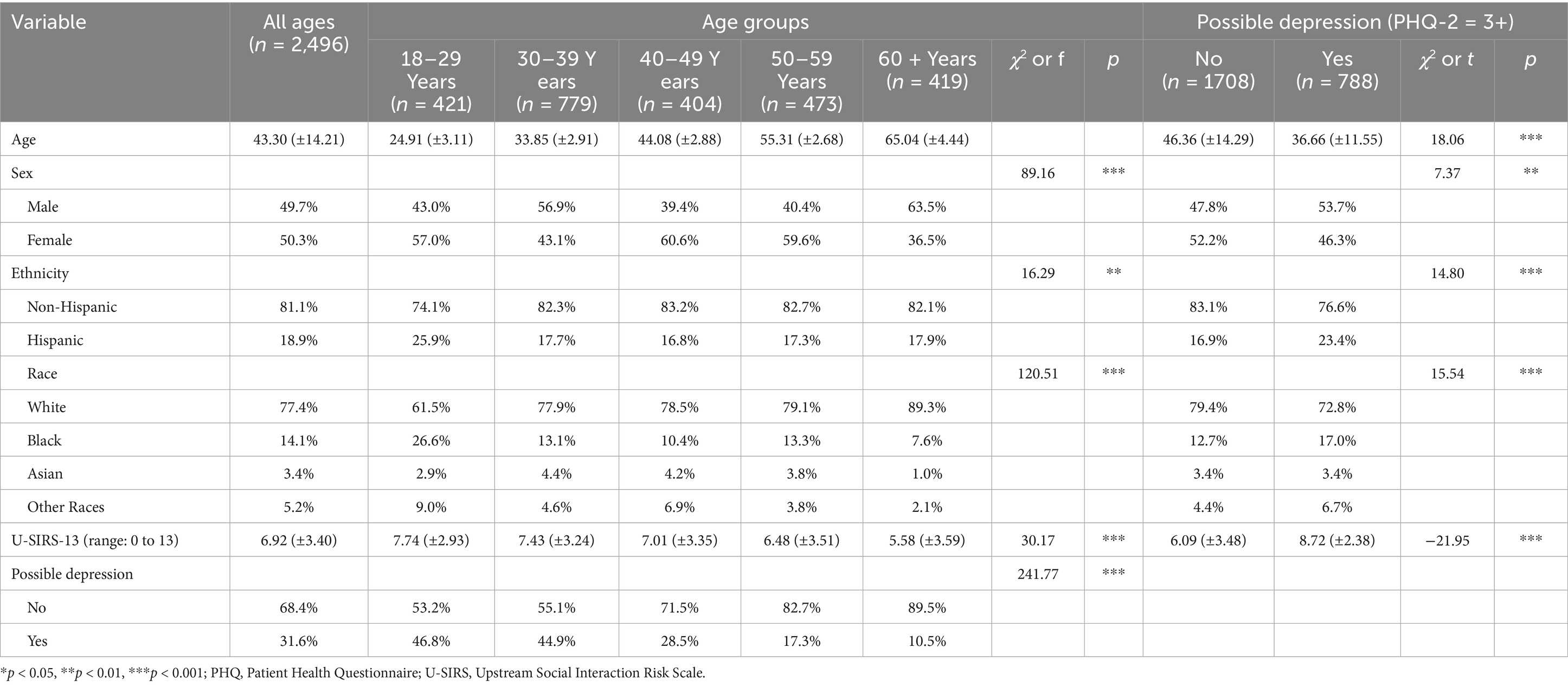
Table 1 reports sample characteristics stratified by age group and possible depression (PHQ-2 score ≥3). Ages ranged from 18 to 89 years. On average (±SD), participants were aged 43.30 (±14.21) years, with 16.9% being ages 18–29 years, 31.2% ages 30–39 years, 16.2% ages 40–49 years, 19.0% ages 50–59 years, and 16.9% ages 60 years and older. About half of the sample (50.3%) was female, and 81.1% identified as non-Hispanic. About 77.4% of participants identified as White, 14.1% were Black, 3.4% were Asian, and 5.2% another race or multiple races. A total of 31.6% participants had possible depression. On average, participants reported a U-SIRS-13 score of 6.92 (±3.40) on a scale from 0 to 13.
When comparing sample characteristics by age groups, significantly smaller proportions of participants ages 30–39 years and 60 years and older were female. A significantly larger proportion of participants ages 18–29 years identified as Hispanic. In terms of race, a significantly larger proportion of participants ages 18–29 years identified as Black or another or multiple races, whereas a larger proportion of participants ages 60 years and older identified as White. Significantly larger proportions of participants ages 18–29 years and 30–39 years had possible depression. On average, participants of younger age groups reported significantly higher U-SIRS-13 scores.
When comparing sample characteristics by possible depression, participants reporting possible depression were significantly younger than those without depression. Significantly larger proportions of men and participants who identified as Hispanic had possible depression. Relative to those without possible depression, a significantly larger proportion of participants who reported being Black or another or multiple races reported possible depression. On average, participants reporting possible depression had significantly higher U-SIRS-13 scores than those without possible depression.
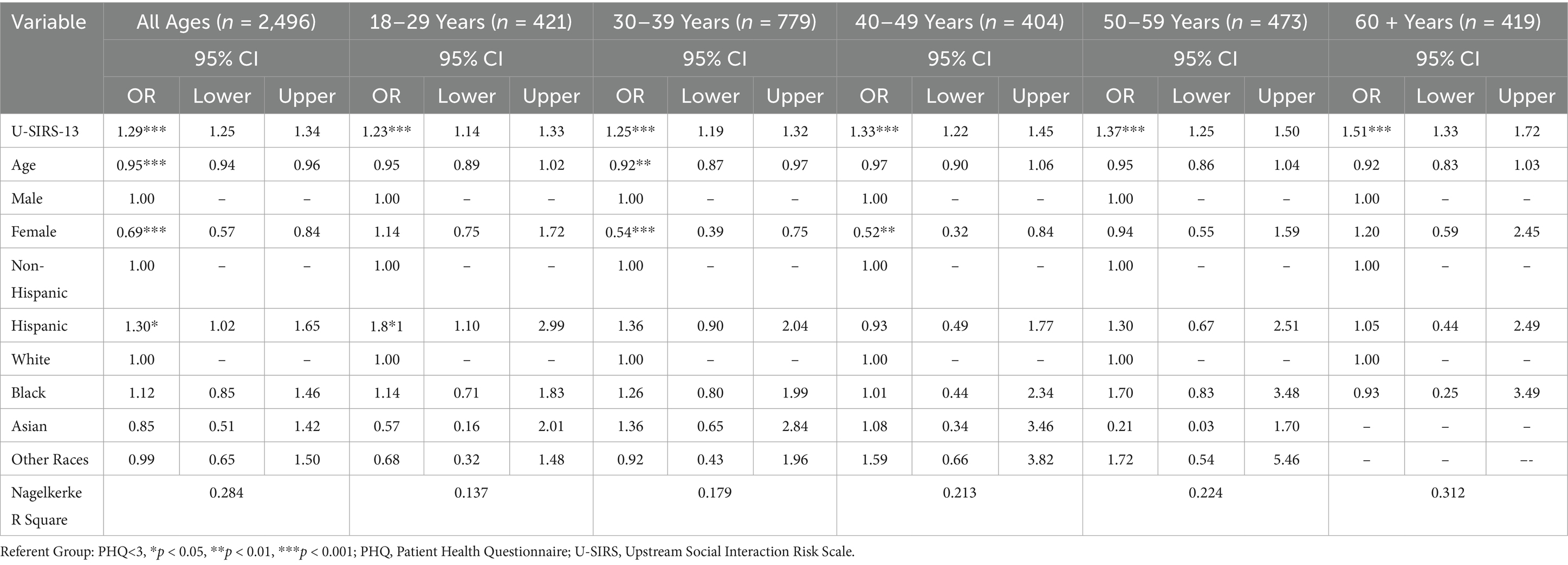
Table 2 reports the Cronbach’s alpha reliability coefficients for the U-SIRS-13 as well as the point-biserial r coefficients between the U-SIRS-13 and PHQ-2, for all participants and within each age group. For the total sample, the Cronbach’s alpha coefficient for the U-SIRS-13 data was 0.78, and the point-biserial r revealed a significantly positive association between the U-SIRS-13 and PHQ-2 (rpb = 0.36, p < 0.001). The Cronbach’s alpha coefficients for the U-SIRS-13 data increased across older age groups. The correlation between the U-SIRS-13 and PHQ-2 remained significantly positive across age groups and increased across older age groups.
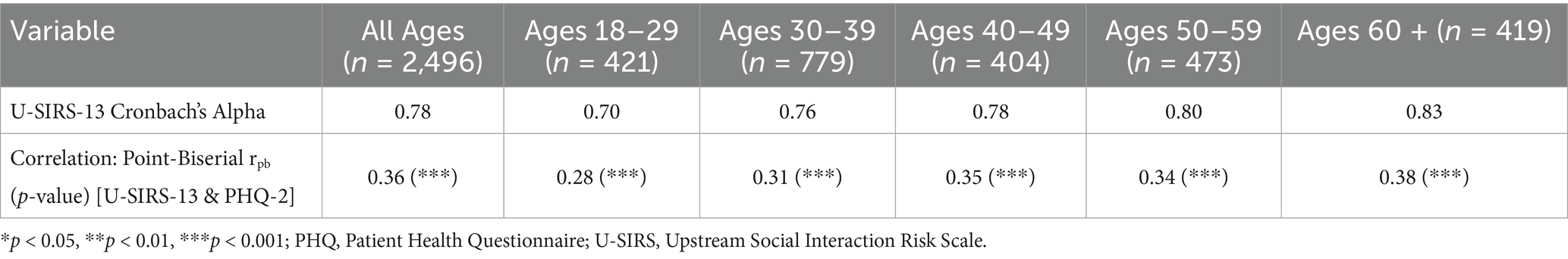
Table 2. U-SIRS-13 internal reliability and correlations between social disconnectedness and possible depression.
Table 3 reports the binary logistic regression models examining the factors associated with possible depression (PHQ-2 score ≥3) by age groups, controlling for age (continuous), sex, ethnicity, and race. In the model with all participants, each additional unit increase of the U-SIRS-13 increased the odds of possible depression. In this model, each additional year of age decreased the odds of possible depression. Relative to male participants, female participants were less likely to have possible depression. Relative to non-Hispanic participants, Hispanic participants were more likely to have possible depression. Across regression models for each age group, each additional unit increase of the U-SIRS-13 increased the odds of possible depression, with odds ratios increasing across older age groups. For participants ages 18–29 years, Hispanic participants were more likely to have possible depression compared to their non-Hispanic counterparts. In the model for participants ages 30–39 years, each additional year of age decreased the odds of possible depression. In the models for participants ages 30–39 years and 40–49 years, female participants were less likely to have possible depression compared to male participants.
Discussion
This study assessed the risk prevalence for social disconnectedness and possible depression, and the association between them, across adults in different age ranges. Results provide robust evidence of a positive relationship between social disconnectedness and possible depression across all age groups. Notably, while younger adults (ages 18–39 years) exhibited the highest prevalence of depressive symptoms, the strength of the association between social disconnectedness and depression appeared stronger among midlife and older adults. These findings underscore the importance of age-sensitive strategies to mitigate social disconnectedness as part of mental health promotion efforts.
Aligned with prior studies (35–37), we found that the prevalence of social disconnectedness and possible depression were significantly higher among young adults aged 18–39 years. Their respective prevalence rates gradually decreased across age groups, reaching their lowest points among individuals aged 60 years and older. This finding may suggest the presence of age-related disparities in mental health and social well-being, with younger adults having a higher risk for both social disconnectedness and possible depression. A recent report demonstrates that the health and wellbeing of younger people is largely impacted by the pervasiveness of digital communication and smart devices on daily lives (38). For example, while technology has provided opportunities for consistent communication and connection with others, its ubiquitous nature may generate the need for ongoing stimulation and the feelings of incompleteness without its presence (39). The higher rates of social disconnectedness and depression observed among younger adults in the current study could be attributed to their higher level of technology use (40, 41); however, future studies are needed to examine how technology utilization influences these outcomes across age ranges.
The association between social disconnectedness and possible depression was significant across all age groups, confirming our study hypothesis. This finding supports that regardless of age, individuals who experience higher levels of social disconnectedness are more likely to have possible depression (12, 42, 43). Interestingly, the strength of the positive correlation coefficients between these two factors gradually increased with increasing age (40–49, 50–59, and 60+) and was notably stronger in older age groups. Several factors may contribute to this pattern. First, older adults often experience significant life changes— such as reduced social networks due to loss of loved ones, bereavement, retirement (44, 45), health challenges, and functional limitations (46)—that can disrupt social roles and diminish opportunities for meaningful engagement. As a result, disconnectedness may be felt more acutely and have a stronger emotional impact in later life. The Socioemotional Selectivity Theory posits that as one grows older, they view the time left in life as more limited and, as such, selectively choose to narrow and focus their social relationships that bring meaning and purpose instead of broadening their social ties (47). It might be that as one grows older, the need for meaningful relationships increases, and when this expectation is not reached (i.e., more socially disconnected), individuals may be more likely to experience mental distress (i.e., depressive symptoms). However, given the cross-sectional nature of this study with a convenience sample, future research is needed to complement these exploratory findings and validate these age-related patterns observed in the current study. Second, coping strategies may differ by age group; younger adults may be more likely to use technology to maintain connection, while older adults may rely more heavily on in-person interactions that are disrupted by health or mobility constraints (48). Generational norms around mental health expression and help-seeking could influence how depression is experienced and reported. Older adults, particularly those from historically stoic or self-reliant cohorts, may underreport emotional distress or delay seeking support, potentially amplifying the psychological burden of social disconnectedness (43, 49). These factors highlight the need for age-sensitive strategies that measure and mitigate the impacts of social disconnectedness on mental health across the lifespan.
The association between social disconnectedness and depression across all age groups underscores the need for intervention strategies targeting to reduce social disconnectedness tailored for specific age groups in different life context to improve effectiveness and accessibility. Prior literature suggests a range of risk factors for loneliness and isolation that may differ in magnitude at specific age groups (36, 37). For example, interventions for young adults may focus on skills to enhance relationship-building with friends and coworkers in educational and workplace settings as frequent contact with friends and relationship in workplace mattered more for loneliness in this age group compared to older age groups (50). For midlife adults, interventions could be integrated into workplace wellness or parenting support programs as this age group is faced with changing social roles and work-life-balance (44). As such, practical solutions for these age groups may include integrating mental health resources into employee wellness programs, creating informal peer-support networks, or embedding social connection components into digital mental health apps and employee onboarding processes. For older adults, approaches such as intergenerational activities and digital literacy support may help reduce barriers to connection (51, 52). These approaches could include community-based technology training, telehealth support, or programs that match older adults with digital mentors to reduce barriers to social participation using technology and mitigate the negative consequences of disconnectedness. Interventions that integrate social prescribing, structured group activities, or neighborhood-level social infrastructure (e.g., senior centers, transportation services) may also be effective. Healthcare providers should consider assessing social connectedness as part of routine depression screenings and offering interventions that foster social interaction alongside traditional treatments for depression. Similarly, employers should offer opportunities for more social interaction and approaches to enhance mental health in the workplace. At the policy level, efforts to address digital equity, invest in community-based mental health and aging services, and incentivize intergenerational or workplace-based connection models are warranted. These age-tailored approaches acknowledge that social disconnectedness is not experienced uniformly and that the pathways to prevention and support must align with life stage, access, and context (53).
Our findings revealed a novel result that male participants were more likely to report possible depression compared to female participants, with this significant association driven by younger age groups (ages 30–49). This result contrasts with prior studies that demonstrate that women are more likely to report depression than men, a phenomenon known as the “female preponderance in depression” (54, 55). Traditionally, men were far less likely to report depression or mental health symptoms due to societal expectations and mental health stigma that may provoke masculinity (56). In fact, our oldest age group that was predominantly comprised of White men, reported the lowest rates of possible depression, which aligns with previous research showing that men tend to underreport depressive symptoms (54). As such, the discrepancy in our findings may reflect a generational shift, with younger men becoming more expressive about their mental health as societal stigma surrounding mental health issues for males have decreased with an increase in awareness of its importance (43, 49). Further studies are needed to explore these gendered and age-varying patterns on mental health outcomes across different generations in a greater detail.
Consistent with previous studies (57, 58), participants in the current study who identified as racial and ethnic minorities had higher rates of probable depression. These findings likely reflect a complex interplay of social, structural, and health-related factors. One explanation is that race often serves as a proxy for exposure to systemic racism (59), which has been consistently linked to poorer mental health outcomes (60, 61). These stressors may exacerbate the feelings of hopelessness and emotional distress, further compounding the risk of depression. In addition, structural barriers, such as limited availability of culturally competent clinicians, financial constraints, and systemic inequalities in healthcare access, may contribute to the underutilization of mental health services by these minoritized groups (62). Studies indicate that individuals from these communities are less likely to receive accurate diagnoses and adequate treatment for depression, which may result in unmet mental health needs (63, 64). Stigma surrounding mental health, compounded by historical and ongoing medical mistrust, may further limit health-seeking behaviors for these minoritized groups. Black and Hispanic individuals often face dual stigmatization—both for experiencing mental health issues and for seeking treatment—which may serve as barriers to timely intervention and can lead to misdiagnosis or under-diagnosis of depression (62–64). Stigma, coupled with the historical medial distrust, underscores the need for culturally sensitive approaches to mental health care that directly address the unique challenges faced by these populations. Addressing these systemic factors is warranted for reducing the observed disparities in depression risk and improving mental health outcomes in these marginalized communities across all ages.
There are several limitations to consider when interpreting the study’s findings. It is important to note that the cross-sectional study design precludes inferences about causality. Although prior literature suggests a potentially bidirectional relationship between social disconnectedness and depression, our analysis modeled social disconnectedness as the independent variable and depression as the outcome. Therefore, assessment of the association operating in both directions using longitudinal research designs is warranted to examine causal pathways. Future studies should also consider examination of between- and within-person differences that are reflective of the true developmental and life course changes in the cross-sectional relationship found in this study. All data were self-reported, which may have introduced social desirability or recall biases. Generalizability may be limited because the data were drawn from a non-probability sample of employed U.S. adults recruited via Qualtrics Online Panels. As such, the findings may not generalize to unemployed individuals, those with more severe health or functional limitations, or populations with lower digital access or literacy. These populations may be at elevated risk for social disconnectedness or depression, suggesting that our findings may not be fully representative of the broader U.S. adult population. Additionally, the study’s inclusion requirement of employment status may have skewed the sample toward individuals who were more functionally able or socially integrated, which could have suppressed the prevalence or severity of outcomes of interest. The observed pattern of higher depressive symptoms among men, particularly those aged 30–49 years, should be interpreted with caution given the non-probability sampling strategy of employed Americans. As described previously, this sample may reflect generational or contextual differences in depression reporting, but it may also be influenced by selection biases related to workforce participation and digital access. Moreover, individuals with more severe depressive symptoms and/or social disconnectedness may have been less likely to participate, potentially leading to underestimates of its respective prevalence rates and overestimating the association strength between these variables, especially among the oldest age group (i.e., 60 + years). While about 15% of the current sample was age 60 years or older, there were limited number of participants ages 70 years and older (n = 61), which constrained our ability to further stratify analyses by finer age subgroups within the older adult population (e.g., 60–69 years, 70–79 years, 80–89 years). Future research should specifically focus on older adults, particularly those beyond traditional working age, to better understand how aging influences the relationship between social disconnectedness and mental health in later life. Such studies could offer valuable insights into how life stage, retirement, and aging-related shifts in social roles may interact with these variables. Depression was assessed using the PHQ-2, a brief screening tool, which limited the ability to fully capture diagnostic criteria, symptom chronicity, or severity. Although the PHQ-2 is a validated and widely used screening tool, its brevity may underestimate depression prevalence, particularly among older adults or individuals with milder or somatic symptom presentations. Future studies should employ more comprehensive diagnostic tools and inclusive sampling strategies to examine these relationships across broader and more diverse populations. Moreover, race, ethnicity, sex, and age were assessed as discrete categories rather than its intersectional factors in relation to risk for depression (65). Further research assessing the interplay between these various identities on mental health outcomes is needed to gauge more nuanced understanding of the associations to reduce health inequalities (66). The current study used practical scoring recommendations for the U-SIRS-13 (33), which yielded robust findings. However, using alternative U-SIRS-13 scoring methods to explore its relationship with depression may further validate the robustness of observed relationships in the current study. The U-SIRS-13 was originally validated with older adults and has been used with other adult populations (e.g., middle-aged caregivers) (33), thus its use with younger populations in the current study is exploratory and provides preliminary indications of its appropriateness for those ages 18 to 60 + years. Lastly, although we adjusted for several sociodemographic variables, we did not include important confounders such as life stressors, substance use, and personality traits, all of which are known to affect depressive symptoms (67). The omission of these factors may bias the observed associations and limit the internal validity of the findings. Future studies should aim to include a more comprehensive set of covariates to better isolate the unique impact of social disconnectedness on depression.
Despite these limitations, this study’s findings show that there is a significant relationship between social disconnectedness and possible depression across different age ranges, highlighting the importance of multidimensional, upstream social risk factors for mental health. These results underscore the importance of fostering social connectedness and managing depression. Efforts are warranted to understand age-informed intervention strategies to address social disconnectedness and depressive symptoms across the adult life span.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board at Texas A&M University. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because After eligible participants were identified by Qualtrics, they were presented with a link to the online questionnaire, which required acknowledgment of an Institutional Review Board-approved information sheet. Participants needed to click ‘I agree’ to acknowledge receipt and continue taking the actual survey.
Author contributions
MY-J: Writing – original draft, Writing – review & editing. LS: Writing – review & editing. AN: Writing – review & editing. MN: Writing – review & editing. AM: Writing – review & editing. AB: Writing – review & editing. MO: Writing – review & editing. IU: Writing – review & editing. MLS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Goodwin, RD, Dierker, LC, Wu, M, Galea, S, Hoven, CW, and Weinberger, AH. Trends in U.S. depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. (2022) 63:726–33. doi: 10.1016/j.amepre.2022.05.014
2. Hansen, T, Nes, RB, Hynek, K, Nilsen, TS, Reneflot, A, Stene-Larsen, K, et al. Tackling social disconnection: an umbrella review of RCT-based interventions targeting social isolation and loneliness. BMC Public Health. (2024) 24:1917. doi: 10.1186/s12889-024-19396-8
3. Malhi, GS, and Mann, JJ. Depression. Lancet. (2018) 392:2299–312. doi: 10.1016/S0140-6736(18)31948-2
4. Fiske, A, Wetherell, JL, and Gatz, M. Depression in older adults. Annu Rev Clin Psychol. (2009) 5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621
5. Pozuelo, JR, Desborough, L, Stein, A, and Cipriani, A. Systematic review and meta-analysis: depressive symptoms and risky behaviors among adolescents in low-and middle-income countries. J Am Acad Child Adolesc Psychiatry. (2022) 61:255–76. doi: 10.1016/j.jaac.2021.05.005
6. Town, MEP, Zhao, G, Town, M, Eke, P, Thomas, CW, Hsia, J, et al. Racial and ethnic differences in social determinants of health and health-related social needs among adults—behavioral risk factor surveillance system, United States, 2022. MMWR Morb Mortal Wkly Rep. (2024) 73:204–8. doi: 10.15585/mmwr.mm7309a3
7. Bruce, LD, Wu, JS, Lustig, SL, Russell, DW, and Nemecek, DA. Loneliness in the United States: a 2018 national panel survey of demographic, structural, cognitive, and behavioral characteristics. Am J Health Promot. (2019) 33:1123–33. doi: 10.1177/0890117119856551
8. Shovestul, B, Han, J, Germine, L, and Dodell-Feder, D. Risk factors for loneliness: the high relative importance of age versus other factors. PLoS One. (2020) 15:e0229087. doi: 10.1371/journal.pone.0229087
9. Healthy Minds Monthly Poll from the American Psychiatric Association (APA). Ment Heal Wkly. (2024) 34:7–8. doi: 10.1002/mhw.33938
10. Kannan, VD, and Veazie, PJ. US trends in social isolation, social engagement, and companionship ⎯ nationally and by age, sex, race/ethnicity, family income, and work hours, 2003–2020. SSM Popul Health. (2023) 21:101331. doi: 10.1016/j.ssmph.2022.101331
11. Cudjoe, TKM, Roth, DL, Szanton, SL, Wolff, JL, Boyd, CM, and Thorpe, RJ. The epidemiology of social isolation: national health and aging trends study. J Gerontol B Psychol Sci Soc Sci. (2020) 75:107–13. doi: 10.1093/geronb/gby037
12. Cacioppo, JT, Hughes, ME, Waite, LJ, Hawkley, LC, and Thisted, RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. (2006) 21:140–51. doi: 10.1037/0882-7974.21.1.140
13. Holt-Lunstad, J, Smith, TB, Baker, M, Harris, T, and Stephenson, D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
14. Wang, J, Mann, F, Lloyd-Evans, B, Ma, R, and Johnson, S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156. doi: 10.1186/s12888-018-1736-5
15. National Academies of Sciences Engineering, and Medicine. Social isolation and loneliness in older adults: opportunities for the health care system. Washington, DC: The National Academies Press (2020). 316 p.
16. Necka, EA, Rowland, LM, and Evans, JD. Social disconnection in late life mental illness - commentary from the National Institute of Mental Health. Am J Geriatr Psychiatry. (2021) 29:727–30. doi: 10.1016/j.jagp.2020.08.013
17. Cornwell, EY, and Waite, LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. (2009) 50:31–48. doi: 10.1177/002214650905000103
18. Holt-Lunstad, J. Social connection as a critical factor for mental and physical health: evidence, trends, challenges, and future implications. World Psychiatry. (2024) 23:312–32. doi: 10.1002/wps.21224
19. Office of the Surgeon General Publications and reports of the surgeon general. Our epidemic of loneliness and isolation: the US surgeon general’s advisory on the healing effects of social connection and community Washington (DC) US Department of Health and Human Services (2023).
20. Chen, Y, and Feeley, TH. Social support, social strain, loneliness, and well-being among older adults: an analysis of the health and retirement study. J Soc Pers Relat. (2014) 31:141–61. doi: 10.1177/0265407513488728
21. Teo, AR, Choi, H, and Valenstein, M. Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS One. (2013) 8:e62396. doi: 10.1371/journal.pone.0062396
22. Joiner, T E, Jr., & Timmons, K. A. (2009). Depression in its interpersonal context. In: Handbook of depression. eds. I. H. Gotlib and C. L. Hammen New York: The Guilford Press; 295–313.
23. Burholt, V, Windle, G, Gott, M, and Morgan, DJteam obotCW. Technology-mediated communication in familial relationships: moderated-mediation models of isolation and loneliness. Gerontologist. (2020) 60:1202–12. doi: 10.1093/geront/gnaa040
24. Hall, JA, Pennington, N, and Merolla, AJ. Which mediated social interactions satisfy the need to belong? J Comput-Mediat Commun. (2022) 28:1–12. doi: 10.1093/jcmc/zmac026
25. Qualtrics. Online Panels 2025 Available online at: https://www.qualtrics.com/support/survey-platform/distributions-module/online-panels/ (Accessed September 3, 2025).
26. Qualtrics. Response quality 2025 Available online at: https://www.qualtrics.com/support/survey-platform/survey-module/survey-checker/response-quality/ (Accessed September 3, 2025).
27. Kroenke, K, Spitzer, RL, and Williams, JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
28. Spitzer, RL, Kroenke, K, and Williams, JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
29. Arroll, B, Goodyear-Smith, F, Crengle, S, Gunn, J, Kerse, N, Fishman, T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. (2010) 8:348–53. doi: 10.1370/afm.1139
30. Manea, L, Gilbody, S, Hewitt, C, North, A, Plummer, F, Richardson, R, et al. Identifying depression with the PHQ-2: a diagnostic meta-analysis. J Affect Disord. (2016) 203:382–95. doi: 10.1016/j.jad.2016.06.003
31. Löwe, B, Kroenke, K, and Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. (2005) 58:163–71. doi: 10.1016/j.jpsychores.2004.09.006
32. Smith, ML, Steinman, LE, and Casey, EA. Combatting social isolation among older adults in a time of physical distancing: the COVID-19 social connectivity paradox. Front Public Health. (2020) 8:403. doi: 10.3389/fpubh.2020.00403
33. Smith, ML, and Barrett, ME. Development and validation of the upstream social interaction risk scale (U-SIRS-13): a scale to assess threats to social connectedness among older adults. Front Public Health. (2024) 12:1454847. doi: 10.3389/fpubh.2024.1454847
34. Benjamini, Y, and Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. (1995) 57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x
35. Victor, CR, and Yang, K. The prevalence of loneliness among adults: a case study of the United Kingdom. J Psychol. (2012) 146:85–104. doi: 10.1080/00223980.2011.613875
36. Hawkley, LC, Buecker, S, Kaiser, T, and Luhmann, M. Loneliness from young adulthood to old age: explaining age differences in loneliness. Int J Behav Dev. (2022) 46:39–49. doi: 10.1177/0165025420971048
37. Collier Villaume, S, Chen, S, and Adam, EK. Age disparities in prevalence of anxiety and depression among US adults during the COVID-19 pandemic. JAMA Netw Open. (2023) 6:e2345073-e. doi: 10.1001/jamanetworkopen.2023.45073
38. National Academies of Sciences Engineering, and Medicine In: S Galea, GJ Buckley, and A Wojtowicz, editors. Social media and adolescent health. Washington, DC: The National Academies Press (2024). 274.
39. Fryman, S, and Romine, W. Measuring smartphone dependency and exploration of consequences and comorbidities. Comput Human Behav Rep. (2021) 4:100108. doi: 10.1016/j.chbr.2021.100108
40. Cunningham, S, Hudson, CC, and Harkness, K. Social media and depression symptoms: a Meta-analysis. Res Child Adolesc Psychopathol. (2021) 49:241–53. doi: 10.1007/s10802-020-00715-7
41. Bonsaksen, T, Ruffolo, M, Price, D, Leung, J, Thygesen, H, Lamph, G, et al. Associations between social media use and loneliness in a cross-national population: do motives for social media use matter? Health Psychol Behav Med. (2023) 11:2158089. doi: 10.1080/21642850.2022.2158089
42. Lee, SL, Pearce, E, Ajnakina, O, Johnson, S, Lewis, G, Mann, F, et al. The association between loneliness and depressive symptoms among adults aged 50 years and older: a 12-year population-based cohort study. Lancet Psychiatry. (2021) 8:48–57. doi: 10.1016/S2215-0366(20)30383-7
43. Achterbergh, L, Pitman, A, Birken, M, Pearce, E, Sno, H, and Johnson, S. The experience of loneliness among young people with depression: a qualitative meta-synthesis of the literature. BMC Psychiatry. (2020) 20:415. doi: 10.1186/s12888-020-02818-3
44. Infurna, FJ, Gerstorf, D, and Lachman, ME. Midlife in the 2020s: opportunities and challenges. Am Psychol. (2020) 75:470–85. doi: 10.1037/amp0000591
45. Kristensen, K, König, HH, and Hajek, A. The empty nest, depressive symptoms and loneliness of older parents: prospective findings from the German ageing survey. Arch Gerontol Geriatr. (2021) 95:104425. doi: 10.1016/j.archger.2021.104425
46. Huxhold, O, Fiori, KL, and Windsor, T. Rethinking social relationships in adulthood: the differential investment of resources model. Personal Soc Psychol Rev. (2022) 26:57–82. doi: 10.1177/10888683211067035
47. Carstensen, LL. Motivation for social contact across the life span: a theory of socioemotional selectivity In: Nebraska symposium on motivation. University of Nebraska Press. (1993) 209–254.
48. Chopik, WJ. The benefits of social technology use among older adults are mediated by reduced loneliness. Cyberpsychol Behav Soc Netw. (2016) 19:551–6. doi: 10.1089/cyber.2016.0151
49. Yeo, TED. “Do you know how much I suffer?”: how young people negotiate the Tellability of their mental health disruption in anonymous distress narratives on social media. Health Commun. (2021) 36:1606–15. doi: 10.1080/10410236.2020.1775447
50. Nicolaisen, M, and Thorsen, K. What are friends for? Friendships and loneliness over the lifespan—from 18 to 79 years. Int J Aging Hum Dev. (2017) 84:126–58. doi: 10.1177/0091415016655166
51. Knight, RL, Chalabaev, A, Mackintosh, KA, McNarry, MA, and Hudson, J. Moving together: increasing physical activity in older adults with an intergenerational technology-based intervention. A feasibility study. PLoS One. (2024) 19:e0301279. doi: 10.1371/journal.pone.0301279
52. Batra, R, Flatt, JD, Pharr, JR, Sharma, M, Khubchandani, J, Kanekar, A, et al. Exploring social support strategies and socio-cultural factors influencing social isolation and loneliness: the role of digital literacy. Healthcare. (2024) 21:2149. doi: 10.3390/healthcare12212149
53. Holt-Lunstad, J. Social connection as a public health issue: the evidence and a systemic framework for prioritizing the “social” in social determinants of health. Annu Rev Public Health. (2022) 43:193–213. doi: 10.1146/annurev-publhealth-052020-110732
54. Shi, P, Yang, A, Zhao, Q, Chen, Z, Ren, X, and Dai, Q. A hypothesis of gender differences in self-reporting symptom of depression: implications to solve under-diagnosis and under-treatment of depression in males. Front Psych. (2021) 12:589687. doi: 10.3389/fpsyt.2021.589687
55. Piccinelli, M, and Wilkinson, G. Gender differences in depression: critical review. Br J Psychiatry. (2000) 177:486–92. doi: 10.1192/bjp.177.6.486
56. Smith, DT, Mouzon, DM, and Elliott, M. Reviewing the assumptions about men's mental health: an exploration of the gender binary. Am J Mens Health. (2018) 12:78–89. doi: 10.1177/1557988316630953
57. Bailey, RK, Mokonogho, J, and Kumar, A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatr Dis Treat. (2019) 15:603–9. doi: 10.2147/NDT.S128584
58. Vyas, CM, Donneyong, M, Mischoulon, D, Chang, G, Gibson, H, Cook, NR, et al. Association of Race and Ethnicity with Late-Life Depression Severity, symptom burden, and care. JAMA Netw Open. (2020) 3:e201606-e. doi: 10.1001/jamanetworkopen.2020.1606
59. Lett, E, Asabor, E, Beltrán, S, Cannon, AM, and Arah, OA. Conceptualizing, contextualizing, and operationalizing race in quantitative health sciences research. Ann Fam Med. (2022) 20:157–63. doi: 10.1370/afm.2792
60. Mouzon, DM, and McLean, JS. Internalized racism and mental health among African-Americans, US-born Caribbean blacks, and foreign-born Caribbean blacks. Ethn Health. (2017) 22:36–48. doi: 10.1080/13557858.2016.1196652
61. Mouzon, DM, Taylor, RJ, Keith, VM, Nicklett, EJ, and Chatters, LM. Discrimination and psychiatric disorders among older African Americans. Int J Geriatr Psychiatry. (2017) 32:175–82. doi: 10.1002/gps.4454
62. González, HM, Tarraf, W, Whitfield, KE, and Vega, WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res. (2010) 44:1043–51. doi: 10.1016/j.jpsychires.2010.03.017
63. Bailey, RK, Blackmon, HL, and Stevens, FL. Major depressive disorder in the African American population: meeting the challenges of stigma, misdiagnosis, and treatment disparities. J Natl Med Assoc. (2009) 101:1084–9. doi: 10.1016/S0027-9684(15)31102-0
64. Jimenez, DE, Park, M, Rosen, D, Joo, J, Garza, DM, Weinstein, ER, et al. Centering culture in mental health: differences in diagnosis, treatment, and access to care among older people of color. Am J Geriatr Psychiatry. (2022) 30:1234–51. doi: 10.1016/j.jagp.2022.07.001
65. Seens, H, Lu, Z, Fraser, J, MacDermid, JC, Walton, DM, and Grewal, R. An intersectional approach to identifying factors associated with anxiety and depression following the COVID-19 pandemic. Sci Rep. (2022) 12:11393. doi: 10.1038/s41598-022-15695-5
66. Fagrell Trygg, N, Gustafsson, PE, and Månsdotter, A. Languishing in the crossroad? A scoping review of intersectional inequalities in mental health. Int J Equity Health. (2019) 18:115. doi: 10.1186/s12939-019-1012-4
Keywords: social disconnectedness, loneliness, depressive symptom, young adults, midlife adults
Citation: Yoo-Jeong M, Steinman LE, Nguyen AL, Neelamegam M, Merianos AL, Boolani A, Ory MG, Udoh I and Smith ML (2025) Social disconnectedness and depressive symptoms across age groups: findings from a non-probability sample of employed U.S. adults. Front. Public Health. 13:1716553. doi: 10.3389/fpubh.2025.1716553
Edited by:
Nan Jiang, Southern Medical University, ChinaReviewed by:
Myrna Weissman, New York State Psychiatric Institute (NYSPI), United StatesZixian Liu, Southern Medical University, China
Copyright © 2025 Yoo-Jeong, Steinman, Nguyen, Neelamegam, Merianos, Boolani, Ory, Udoh and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Moka Yoo-Jeong, bS55b28tamVvbmdAbm9ydGhlYXN0ZXJuLmVkdQ==
 Moka Yoo-Jeong
Moka Yoo-Jeong Lesley E. Steinman
Lesley E. Steinman Annie L. Nguyen3
Annie L. Nguyen3 Malinee Neelamegam
Malinee Neelamegam Ashley L. Merianos
Ashley L. Merianos Ali Boolani
Ali Boolani Marcia G. Ory
Marcia G. Ory Matthew Lee Smith
Matthew Lee Smith