- Department of Otolaryngology Head and Neck Surgery, The Central Hospital of Enshi Tujia and Miao Autonomous Prefecture, Enshi, China
Background: Age-related hearing loss (ARHL) and tinnitus are common sensory symptoms that impair communication, psychosocial functioning, and QoL. Clinic-level investigations of QoL factors, comorbidities, and combination effects are scarce despite their public health importance.
Objective: This study examined the determinants of ARHL and tinnitus in older persons, their relationships with demographic, clinical, and psychosocial characteristics, and their effects on global and domain-specific health-related quality of life.
Methods: A retrospective study comprised of 1000 patients aged 60–85 years old. Structured interviews and medical records provided demographic, clinical, lifestyle, and psychosocial data. Hearing impairment was classified using established audiological standards based on pure-tone audiometry, and QoL was assessed with HRQOL measures. We used audiological standards to evaluate ARHL and tinnitus severity. Multivariable logistic regression assessed global and domain-specific QoL associations after covariate adjustment.
Results: Increasing severity of ARHL and tinnitus was strongly associated with older age, male sex, comorbidities, lifestyle risk factors, and psychological burden. Severe ARHL combined with tinnitus conferred the highest odds of impaired global QoL (OR 5.48, 95% CI 3.09–9.71), psychological distress (OR 6.89, 95% CI 3.82–12.43), and social limitations (OR 5.72, 95% CI 3.01–10.86; all p < 0.001). Tinnitus alone independently predicted poorer outcomes, while hearing aid use showed a modest but nonsignificant protective effect. Depression, anxiety, sleep disturbance, cognitive impairment, social isolation, and comorbid medical conditions further exacerbated QoL declines.
Conclusion: ARHL and tinnitus worsen physical, psychological, and social health, while intensity and duration increase risk. These findings emphasize the need for early detection, targeted therapies, and integrated care to reduce functional decline and improve QoL in older persons.
1 Introduction
Hearing loss and tinnitus can affect a person’s personal, social, and economic status. Tinnitus is ear ringing, whereas hearing loss is loss of hearing. Tinnitus, the feeling of sound (ringing, buzzing, hissing, or whooshing) without an external stimulation, usually occurs with hearing impairment and can be transitory or persistent. Tinnitus can cause hearing loss. Hearing loss can range from mild to total deafness and be genetic or acquired (1, 2). Together, these conditions reduce communication ability, impair social participation, and worsen overall quality of life, making them major public-health concerns worldwide. The global burden of hearing impairment is large and rising. Current estimates indicate that more than 1.5 billion people (roughly one in five worldwide) experience some degree of hearing loss, and around 430 million have disabling hearing loss (3, 4). Population aging and ongoing exposure to damaging noise are expected to further increase these numbers in the coming decades. Tinnitus is also highly prevalent (5). A large systematic review and meta-analysis estimated that approximately 14% of adults experience some form of tinnitus, and about 2% suffer a severe form that substantially interferes with daily life; incidence rises with age (6). Tinnitus affects hundreds of millions globally and represents an important, often under-recognized public health problem. Prevalence patterns vary by region and country. The WHO Western Pacific Region is estimated to have one of the highest prevalences of hearing loss globally, with about 7% of people experiencing some degree of hearing impairment (3). In Asia more broadly, the burden is also high, the prevalence of disabling hearing loss (defined as > 35 dB in the better ear) is estimated at 6.85% in East Asia and 7.37% in South Asia (4). In China, national studies estimate that in 2015, approximately 115 million people (about 8.4% of the population) had moderate-to-complete hearing loss, of whom around 85.7% were older than 50 years. Projections suggest that by 2060, this number could rise to 242 million individuals (roughly 18.6% of the population). Other data further highlight age-stratified trends: among adults aged 60 years or older in China, nearly two-thirds are estimated to have some hearing loss (7). Typically, the term “hearing loss” is broad and encompasses various forms of auditory impairment. Among these, sensorineural hearing loss (SNHL), resulting from damage to the inner ear (cochlea) or the auditory nerve, is the most common type and is most frequently associated with tinnitus. SNHL can arise from aging, noise exposure, ototoxic medications, or hereditary factors, and represents the primary focus in clinical and epidemiological studies examining the co-occurrence of hearing loss and tinnitus. The causes of hearing loss and tinnitus are multifactorial. Age-related sensorineural degeneration (presbycusis) and excessive noise exposure (occupational or recreational) are leading contributors worldwide. Other important causes include middle-ear disease and chronic ear infections, ototoxic medications, congenital and genetic conditions, head trauma, and certain systemic illnesses (e.g., cardiovascular disease, diabetes) (8, 9). Tinnitus is strongly associated with hearing loss but may also arise from otologic disorders, head/neck injuries, medications, and central nervous system changes (10–12). Targeting prevention and therapeutic management requires understanding these factors’ respective contributions in diverse groups. Hearing loss and tinnitus affect health beyond communication. They are linked to lower quality of life, social isolation, depression, anxiety, sleep disturbance, cognitive decline, and dementia in older persons (13–15). The resulting functional limitations and lost productivity generate substantial personal and societal costs and strain health systems, particularly in lower-resource settings where access to hearing care is limited. Despite the clear burden, many regions lack detailed, clinic-level analyses that identify modifiable and non-modifiable determinants of hearing loss and tinnitus, and how these determinants relate to severity, comorbidity, and service utilization. Retrospective analyses of audiology clinic and hospital records can efficiently generate hypotheses about risk factors (age, sex, exposure histories, comorbidities, otologic diagnoses, and medication exposures) and their association with outcomes such as the degree of hearing impairment and presence/severity of tinnitus. Such evidence can inform targeted prevention (noise control, safe-listening campaigns, rational use of ototoxic drugs), early detection strategies, and resource allocation for hearing rehabilitation (hearing aids, cochlear implants, tinnitus management). This retrospective study, therefore, aims to characterize the determinants of deafness/hearing loss and tinnitus in our patient population, quantify associations with key demographic and clinical variables, and identify priorities for public-health intervention and future prospective research.
2 Materials and methods
2.1 Ethical approval
The study protocol for the study was reviewed and approved by the Research Ethics Review Committee of The Central Hospital of Enshi Tujia and Miao Autonomous Prefecture. No. LC20240312. All participants gave written consent before data collection. Participants were promised confidentiality and anonymity throughout face-to-face interviews. The collected data were used only for scientific study and publishing.
2.2 Study design
A retrospective, cross-sectional study explored the causes and health implications of hearing loss and tinnitus in older adults. Participants aged 60–85 were recruited from The Central Hospital of Enshi Tujia and Miao Autonomous Prefecture in June 2023–2025. Female and male candidates from diverse socioeconomic and educational backgrounds were eligible. Participants had to be ≥60 years old, provide complete demographic and clinical information, and agree to face-to-face interviews to evaluate hearing health, tinnitus characteristics, and quality of life. Hearing loss was categorized by WHO audiometric criteria as normal (<20 dB HL), mild (20–34 dB), moderate (35–49 dB), fairly severe (50–64 dB), and severe (≥65 dB). The standard audiological evaluation found sensorineural, conductive, and mixed hearing loss. Based on patient history and clinical evidence, tinnitus patients were classified as subjective or objective, primary (idiopathic) or secondary (related to an identifiable cause), and acute (<6 months) or chronic (≥6 months). Concurrent severe neurological or psychiatric disorders that could impair reliable communication, active comorbidities that independently cause hearing impairment (e.g., ototoxic medications, traumatic ear injury, or chronic otitis media), and incomplete or missing clinical or interview data were excluded. This comprehensive diagnostic methodology assessed age-related hearing loss (ARHL), tinnitus subtypes, and health-related quality of life using internationally accepted standards.
2.3 Sample size
A total of 1,050 older adults were screened, and 1,000 met the inclusion criteria. The required minimum sample size (≈370), estimated through power analysis based on a 30% expected prevalence, 95% confidence level, and 5% margin of error, was exceeded. The larger sample enhanced analytical robustness and generalizability.
2.4 Reliability and validity of the questionnaire
A systematic questionnaire was designed and piloted for clarity and feasibility with professional assistance. The study met psychometric criteria for reliability, with satisfactory internal consistency (Cronbach’s α = 0.78–0.86) and subsample test–retest reliability (ICCs = 0.80–0.88) (16). Hearing loss, tinnitus severity, and health outcomes linkages confirmed construct validity. These findings demonstrate that the measure accurately assessed older people’s deafness/hearing loss, tinnitus, and health.
2.5 Statistical analysis
Data were analyzed using SPSS v.25 (IBM Corp., Armonk, NY, USA). ANOVA and chi-square described participants for continuous and categorical variables. The Shapiro–Wilk test established continuous data distribution normality before parametric analyses. Deafness/hearing loss and tinnitus risk variables and their global and domain-specific quality of life impacts were discovered by multivariable logistic regression. The study used a significance level of p < 0.05 and reported odds ratios (ORs) with 95% CIs. Tinnitus and ARHL were examined in interaction models (17).
3 Results and discussion
3.1 Demographic, clinical, and psychosocial correlates of ARHL and tinnitus
This 1,000-person study found substantial differences in age, sex, marital status, medical comorbidities, lifestyle choices, and psychological factors in connection to age-related hearing loss (ARHL)/deafness and tinnitus severity (Table 1). The trend was clear across all categories. Participants with severe ARHL and tinnitus were significantly older (78.1 ± 6.0 years) compared to those with normal hearing and no tinnitus (64.0 ± 3.4 years, p < 0.001). The severe ARHL with tinnitus group had 60% male sex (p = 0.04). Marital status dropped sequentially with worsening ARHL and tinnitus, from 83% in normal hearing to 50% in severe ARHL (p < 0.001). ARHL and tinnitus groups consistently had more chronic diseases. Hypertension, diabetes (type 1 and type 2), and cardiovascular disease were most common in severe ARHL with tinnitus (64, 43, and 41%, respectively), about two-to-fourfold higher than normal hearing controls. Obesity, noise exposure, and ototoxic drug use substantially increased with hearing loss severity (p < 0.01). All lifestyle risk variables (smoking, alcohol use, physical inactivity, and poor sleep quality) were considerably higher (p < 0.05) in severe ARHL with tinnitus compared to normal hearing. ARHL and tinnitus worsened cognitive and psychological issues. Depression increased from 7 to 45% in severe ARHL with tinnitus, whereas anxiety and cognitive impairment increased to 39 and 32%, respectively (p < 0.001). Hearing aid use was low overall but significantly increased with severity (2% in normal hearing vs. 33% in severe ARHL with tinnitus, p < 0.001), indicating underutilization despite necessity.
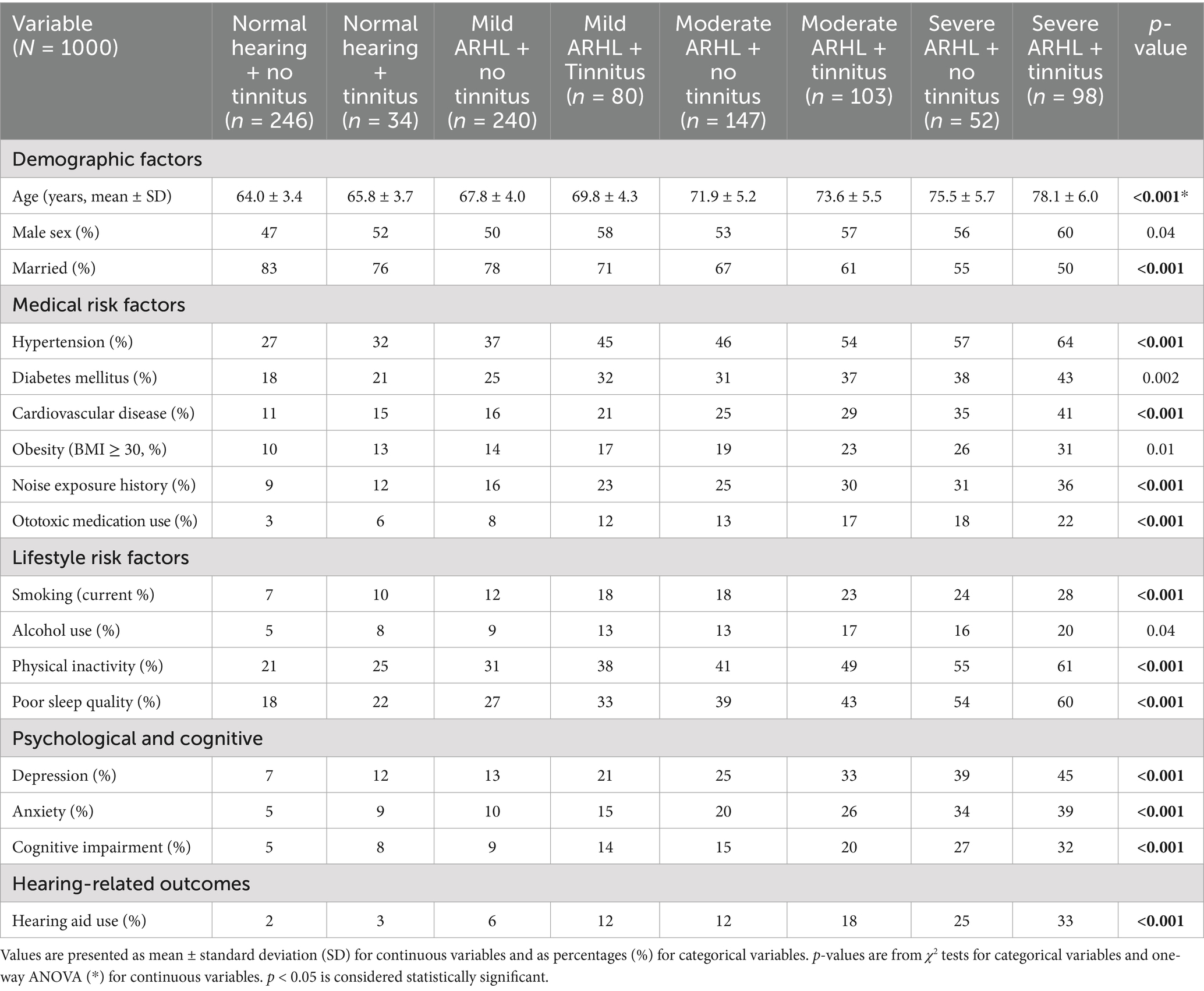
Table 1. Participant characteristics by severity of age-related hearing loss (ARHL) and tinnitus status.
3.2 Association of ARHL, tinnitus, and comorbid factors with quality of life
The association between age-related hearing loss, tinnitus, and comorbid factors plays a crucial role in determining the quality of life among older adults. Table 2, reveals adjusted ARHL, tinnitus severity, and QoL relationships. The hearing status gradient was strong. Mild ARHL with tinnitus was more likely to have poorer QoL than normal hearing without it (OR = 1.61, 95% CI: 1.08–2.41, p = 0.02), whereas moderate and severe ARHL had greater odds (OR = 1.74 and 2.18, respectively). ARHL with tinnitus conferred the highest risk, with an OR of 3.68 (95% CI: 2.25–6.02, p < 0.001) in severe cases. Sociodemographic and economic factors affected QoL. Age ≥75 years had approximately twice the risk of poor QoL (OR = 1.70, 95% CI: 1.24–2.34, β = 0.53, SE = 0.16, p = 0.001), with low education and income further increasing the risk (OR = 1.95 and 2.04, respectively). Marriage provided some protection (OR = 0.72, p = 0.07). Adverse lifestyle and health behaviors also decreased QoL. Although alcohol use (OR = 1.28, 95% CI: 0.89–1.85, p = 0.17) and obesity (OR = 1.26, 95% CI: 0.88–1.81, p = 0.20) were not statistically significant, both smoking (OR = 1.44, 95% CI: 1.01–2.05, β = 0.36, SE = 0.18, p = 0.04) and physical inactivity (OR = 1.49, 95% CI: 1.06–2.09, β = 0.40, SE = 0.17, p = 0.03) were significant predictors of reduced QoL. Strongest connections were with psychological and sleep states. Depression tripled the risks of reduced QoL (OR = 3.24, 95% CI: 2.10–5.01, β = 1.18, SE = 0.22, p < 0.001), followed by anxiety (OR = 2.52, 95% CI: 1.60–3.98 p < 0.001) and poor sleep quality (OR = 1.87, 95% CI: 1.27–2.77 p = 0.002). Among medical comorbidities, diabetes mellitus (OR = 1.57, 95% CI: 1.11–2.22, β = 0.45, SE = 0.18, p = 0.01), cardiovascular disease (OR = 1.71, 95% CI: 1.14–2.55, p = 0.009), cognitive impairment (OR = 2.10, 95% CI: 1.44–3.08, p < 0.001), and ototoxic medication use (OR = 1.46, 95% CI: 1.00–2.12, p = 0.048) were all significantly related to poorer QoL outcomes. Social isolation also emerged as a significant risk factor (OR = 1.54, 95% CI: 1.07–2.21, p = 0.019).
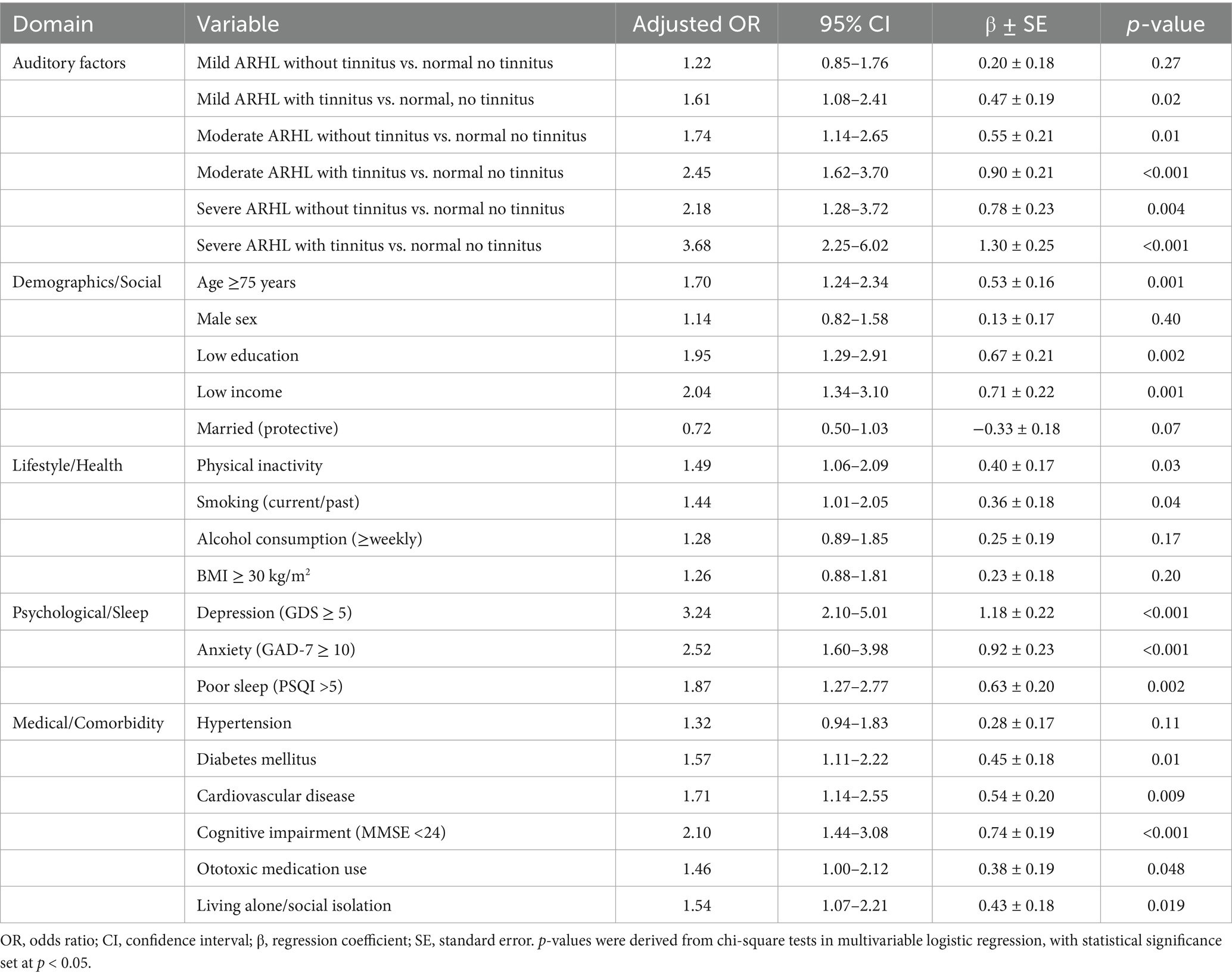
Table 2. Association of age-related hearing loss (ARHL) and tinnitus severity with quality of life (QoL).
3.3 Multivariable associations of ARHL and tinnitus with QoL and psychosocial outcomes
In the multivariable analysis, ARHL and tinnitus severity were consistently linked to lower quality of life, psychological health, and concurrent disorders. Severe impairment was linked to worse physical, psychological, social, and environmental QoL (OR = 3.04, 95% CI: 1.82–5.06, p < 0.001, p ≤ 0.002). Symptom outcomes were worse for severe cases, including poor sleep, fatigue, and tinnitus duration ≥5 years (OR = 3.98, 95% CI: 2.23–7.11, p < 0.001). Severe impairment was associated with higher odds of anxiety, depression, and cognitive impairment compared to milder conditions (OR = 3.62, 95% CI: 2.14–6.12, p < 0.001). Auditory outcomes showed growing relationships, especially for severe tinnitus (OR = 5.18, 95% CI: 3.02–8.87, p < 0.001) and severe ARHL (OR = 4.65, 95% CI: 2.64–8.18, p < 0.001). Hearing aid use may have a protective impact (OR = 0.65, 95% CI: 0.38–1.11, p < 0.001), but not statistically significant (p = 0.09). Severe impairment was linked to higher social isolation and loneliness (OR = 3.12, 95% CI: 1.88–5.18, p < 0.001), but low social participation was not statistically significant (p = 0.08). Medical comorbidities, such as hypertension, diabetes, and chronic pain/frailty, exhibited favorable relationships (OR = 1.82, 95% CI: 1.09–3.04, p = 0.02, 2.11, 95% CI: 1.21–3.68, p = 0.01, 3.01, 95% CI: 1.73–5.25, p < 0.001). Tinnitus-specific features indicate worse outcomes for abrupt onset (OR = 2.11, 95% CI: 1.21–3.66, p = 0.04) and high-pitch (OR = 2.84, 95% CI: 1.63–4.93, p < 0.001) (Table 3).
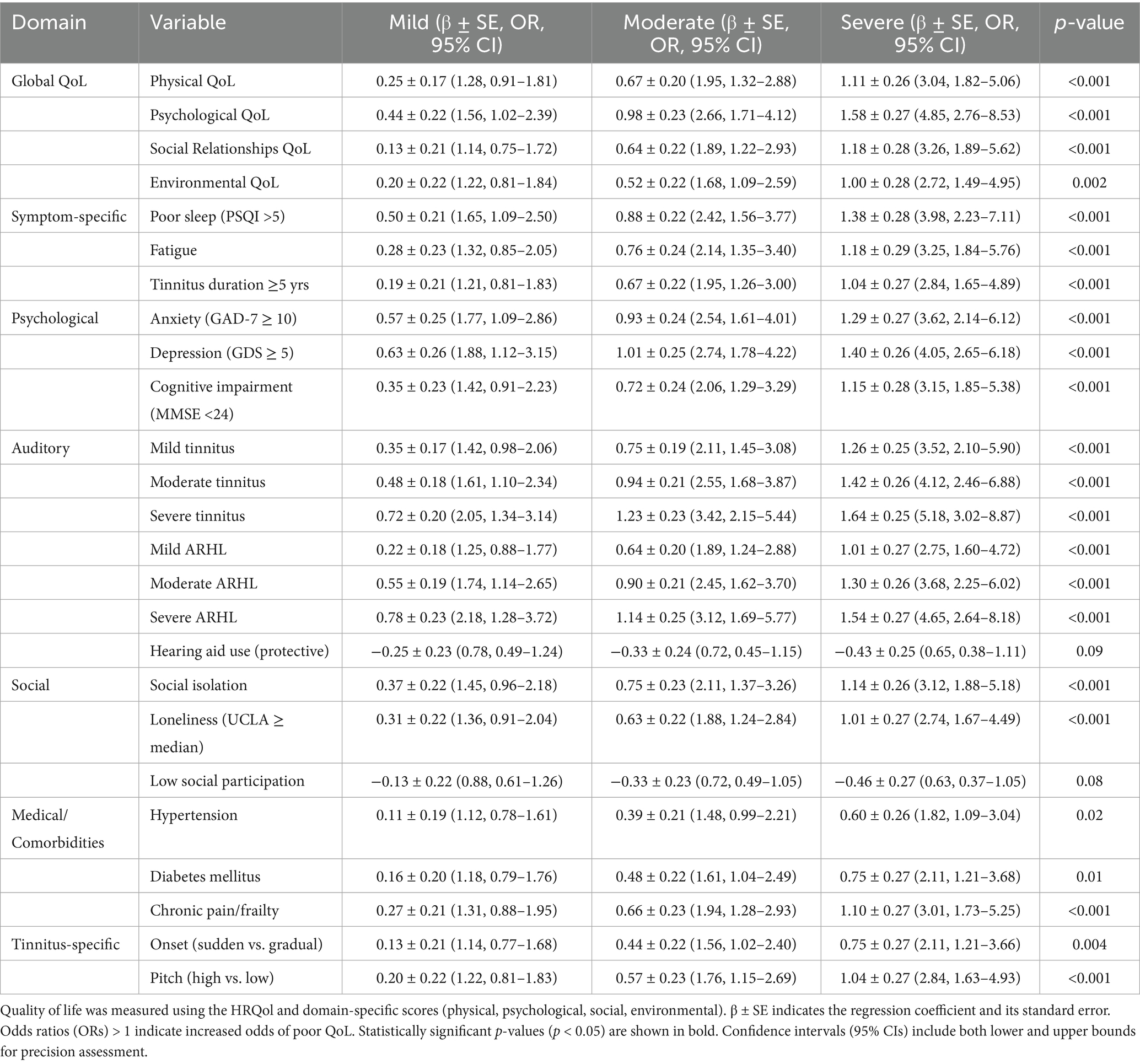
Table 3. Multivariable association of ARHL and tinnitus severity with QoL and psychosocial outcomes.
3.4 Impact of combined ARHL and tinnitus on health-related quality of life
The combined presence of age-related hearing loss and tinnitus has a compounded adverse effect on health-related quality of life in older adults. In the multivariate logistic regression analysis (Table 4), greater severity of ARHL and tinnitus was associated with lower global, psychological, and social HRQoL. Individuals with severe ARHL and tinnitus had higher odds of poor QoL, including a fivefold increase in global QoL impairment (OR 5.48, 95% CI 3.09–9.71, p < 0.001), nearly sevenfold increase in psychological distress (OR 6.89, 95% CI 3.82–12.43, p < 0.001), and over fivefold increase in social QoL limitations (OR 5.72, 95% CI 3.01–10.86, p < 0.001).
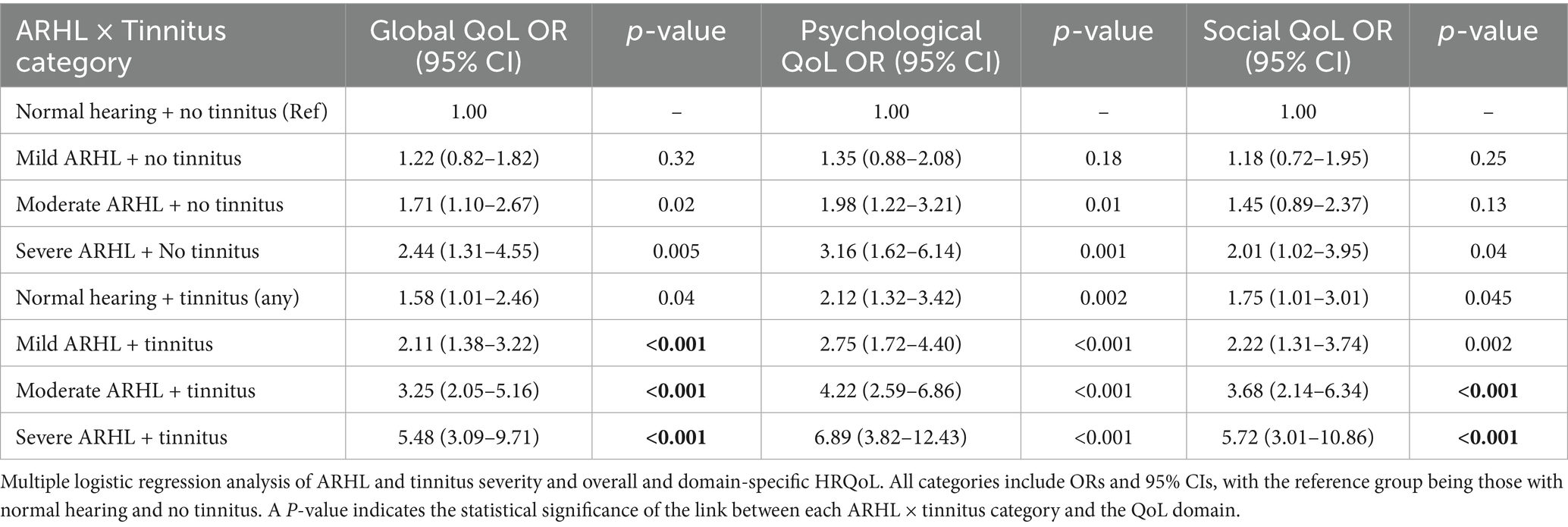
Table 4. Multiple logistic regression of combined ARHL and tinnitus severity in relation to global and domain-specific HRQoL.
4 Discussion
According to the findings of this study, there are a number of important factors that have a role in the development of hearing loss and tinnitus in older people. In addition, the study emphasizes the significance of these factors in terms of their influence on quality of life, as well as the importance of early screening and targeted treatments. The findings of this study have been found to be consistent with the findings of other population-based studies that have been conducted in the past. An advanced age, male gender, and vascular comorbidities are all factors that have been shown to have a significant contribution to the development of ARHL (18), mirroring the gradients observed in our data. It was also emphasized that the roles of noise exposure and ototoxic medications (19) were more common in our research patients with severe ARHL and tinnitus. ARHL, tinnitus, and psychological effects are strongly linked, as previously found (20, 21), which demonstrated increased risks of depression, anxiety, and cognitive decline in hearing-impaired individuals. Prior research has linked untreated hearing loss to poor sleep and physical inactivity, which has increased in our population (22, 23). Finally, our finding that hearing aid use rose with severity but remained low corresponds with a prior study that found hearing rehabilitation services underutilized despite their benefits (24). The findings of the present study are in line with previous research. Similar to our results, it was reported that both ARHL severity and tinnitus synergistically predict lower QoL and functional decline (21). The protective role of marital status, as was reflected in earlier studies as well, emphasized the importance of social support as a buffer against sensory impairment-related disability (25). Hearing impairment risk increases with factors like smoking and inactivity (26). The strong correlations to sorrow, anxiety, and poor sleep support previous research (27, 28), where psychological distress exacerbated hearing loss’s daily impact. Hearing loss independently predicted dementia risk in the cognitive impairment-ARHL association (29, 30). Lastly, studies demonstrate that diabetes and cardiovascular disease promote ARHL development and QoL decrease via vascular and metabolic pathways (31). These findings support and extend epidemiological evidence that ARHL and tinnitus negatively impact QoL through a complex interaction of auditory, physical, psychological (32), and social factors. ARHL and tinnitus severity are connected to lower quality of life, psychological and social distress, and medical comorbidities, showing their widespread impact. This study links severe ARHL and tinnitus to lower quality of life, mental health, social participation, and medical difficulties (32). These findings support previous evidence that hearing loss and tinnitus affect physical, mental, and social functioning. Moderate to severe ARHL patients showed lower physical and psychological QoL scores in earlier studies (33), typically comparable to those of other chronic debilitating diseases (34) and the epidemiology of Hearing Loss Study (11, 35). Severe ARHL and tinnitus were connected to sadness, anxiety, and cognitive impairment, increasing psychological morbidity concerns. These findings support epidemiological data linking untreated hearing loss to depression and anxiety (36), as well as long-term research showing hearing impairment accelerates cognitive decline and dementia risk (8, 37). Increased cognitive load, social isolation, and neuropathological pathways affect auditory and cognitive processing. Previous studies have shown that tinnitus severity increases depression and sleep problems (38). We identified strong associations between sleep disturbance and weariness, validating past findings that tinnitus-related hyperarousal and ARHL-related communication issues impair sleep and daytime functioning (23, 29). Cardiometabolic risk factors may cause microvascular and neurological alterations in auditory pathways (39), whereas chronic pain and frailty may worsen functional decline and limit coping methods. This study demonstrated that prompt amplification therapy may lessen hearing loss’s psychosocial and cognitive impacts. However, the benefit depends on impairment degree, device quality, and patient compliance with the treatment plan. Early hearing rehabilitation reduces depression, improves social connections, and prevents cognitive decline, according to clinical trials and meta-analyses (40). These studies reveal ARHL and tinnitus influence auditory, mental, social, and medical well-being. We conclude that these public health challenges require early screening, thorough care, and hearing health integration into aging and chronic disease prevention. Even in those with good hearing, tinnitus alone was associated with worse outcomes. This reinforces recent findings that age-related hearing loss and tinnitus significantly increase functional and psychological load. Tinnitus-related hearing loss predicted sadness, social isolation, and lower QoL (8). The Blue Mountains Hearing Project and Epidemiology of Hearing Loss Study indicated that ARHL and tinnitus increase emotional stress and social disengagement (37, 41). This study assessing graded risk throughout severity levels, stresses early ARHL and tinnitus detection and integrates therapy to promote quality of life. This study’s cross-sectional design and cultural and regional characteristics limit generalizability. Longitudinal and interventional research is needed to confirm these findings and understand processes.
5 Conclusion
Tinnitus and age-related hearing loss (ARHL) are widespread among older adults and have serious health consequences, according to this retrospective study. Both illnesses cause anxiety, depression, cognitive impairment, sleep deprivation, tiredness, and social isolation. ARHL and tinnitus severity separately and jointly significantly lower HRQoL, highlighting their effects. These studies demonstrate how sociodemographics, lifestyle, and medical conditions affect auditory, psychological, and social health. These findings emphasize the need of early detection, thorough hearing testing, and integrated therapy such as hearing rehabilitation, psychological support, and lifestyle adjustments to reduce ARHL and tinnitus. Quality of life as a health outcome can reveal the functional and psychological impact of sensory deficits in older persons. Finally, focused interventions for modifiable risk factors and symptom management are needed to sustain health, autonomy, and well-being in this increasing group.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by the study protocol for the study was reviewed and approved by the Research Ethics Review Committee of the Central Hospital of Enshi Tujia and Miao Autonomous Prefecture. No. LC20240312. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
LZ: Investigation, Methodology, Writing – review & editing, Writing – original draft, Formal analysis, Data curation. YL: Investigation, Writing – review & editing, Conceptualization, Writing – original draft, Data curation, Methodology.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript were used in the preparation, drafting, or editing of this manuscript. All content, analysis, and interpretations were completed solely by the authors.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Baracca, G, Del Bo, L, and Ambrosetti, U. Tinnitus and hearing loss In eds. Møller AR, Langguth B, DeRidder D, and Kleinjung T. Textbook of tinnitus. New York, NY: Springer Science+Business Media (2011) 285–91.
2. Shapiro, SB, Noij, KS, Naples, JG, and Samy, RN. Hearing loss and tinnitus. Med Clin North Am. (2021) 105:799–811. doi: 10.1016/j.mcna.2021.05.003
3. Jiang, C-Y, Han, K, Yang, F, Yin, S-Y, Zhang, L, Liang, B-Y, et al. Global, regional, and national prevalence of hearing loss from 1990 to 2019: a trend and health inequality analyses based on the global burden of disease study 2019. Ageing Res Rev. (2023) 92:102124. doi: 10.1016/j.arr.2023.102124
4. Li, W, Zhao, Z, Lu, Z, Ruan, W, Yang, M, and Wang, D. The prevalence and global burden of hearing loss in 204 countries and territories, 1990–2019. Environ Sci Pollut Res. (2022) 29:12009–16. doi: 10.1007/s11356-021-16582-8
5. Elgoyhen, AB, Langguth, B, De Ridder, D, and Vanneste, S. Tinnitus: perspectives from human neuroimaging. Nat Rev Neurosci. (2015) 16:632–42. doi: 10.1038/nrn4003
6. Jarach, CM, Lugo, A, Scala, M, van den Brandt, PA, Cederroth, CR, Odone, A, et al. Global prevalence and incidence of tinnitus: a systematic review and meta-analysis. JAMA Neurol. (2022) 79:888–900. doi: 10.1001/jamaneurol.2022.2189
7. Wang, Y, Xie, Y, Wang, M, Zhao, M, Gong, R, Xin, Y, et al. Hearing loss prevalence and burden of disease in China: findings from provincial-level analysis. Chin Med J. (2025) 138:41–8. doi: 10.1097/CM9.0000000000003096
8. Stegeman, I, Eikelboom, RH, Smit, AL, Baguley, DM, Bucks, RS, Stokroos, RJ, et al. Tinnitus and its associations with general health, mental health and hearing loss. Prog Brain Res. (2021) 262:431–50. doi: 10.1016/bs.pbr.2021.01.023
9. Gallus, S, Lugo, A, Garavello, W, Bosetti, C, Santoro, E, Colombo, P, et al. Prevalence and determinants of tinnitus in the Italian adult population. Neuroepidemiology. (2015) 45:12–9. doi: 10.1159/000431376
10. Boussaty, EC, Friedman, RA, Program, MV, and Clifford, RE. Hearing loss and tinnitus: association studies for complex-hearing disorders in mouse and man. Hum Genet. (2022) 141:981–90. doi: 10.1007/s00439-021-02317-9
11. Jansen, C, Le Prell, C, and Spankovich, C. Health determinants and modifiable risk factors of tinnitus In: Tinnitus: Advances in prevention, assessment, and management (2022). 41.
12. Panayiota, M, Maihoub, S, and Molnár, A. Speech recognition thresholds correlate with tinnitus intensity in individuals with primary subjective tinnitus. Front Neurol. (2025) 16:1672762. doi: 10.3389/fneur.2025.1672762
13. Phillips, OR, Baguley, DM, Pearson, SE, and Akeroyd, MA. The long-term impacts of hearing loss, tinnitus and poor balance on the quality of life of people living with and beyond cancer after platinum-based chemotherapy: a literature review. J Cancer Surviv. (2023) 17:40–58. doi: 10.1007/s11764-022-01314-9
14. de Graaf, R, and Bijl, RV. Determinants of mental distress in adults with a severe auditory impairment: differences between prelingual and postlingual deafness. Psychosom Med. (2002) 64:61–70. doi: 10.1097/00006842-200201000-00009
15. Molnár, A, Molnár, V, Mavrogeni, P, and Maihoub, S. Fasting glucose, Haemoglobin A1C (HbA1c), blood lipid, and triglyceride–glucose index parameters in relation to subjective tinnitus. Biomedicine. (2025) 13:824. doi: 10.3390/biomedicines13040824
16. Tavakol, M, and Dennick, R. Making sense of Cronbach's alpha. Int J Med Educ. (2011) 2:53–5. doi: 10.5116/ijme.4dfb.8dfd
18. Förster, CY, Shityakov, S, Scheper, V, and Lenarz, T. Linking cerebrovascular dysfunction to age-related hearing loss and Alzheimer’s disease—are systemic approaches for diagnosis and therapy required? Biomolecules. (2022) 12:1717. doi: 10.3390/biom12111717
19. Cannizzaro, E, Cannizzaro, C, Plescia, F, Martines, F, Soleo, L, Pira, E, et al. Exposure to ototoxic agents and hearing loss: a review of current knowledge. Hear Balance Commun. (2014) 12:166–75. doi: 10.3109/21695717.2014.964939
20. Chen, Z, Lu, Y, Chen, C, Lin, S, Xie, T, Luo, X, et al. Association between tinnitus and hearing impairment among older adults with age-related hearing loss: a multi-center cross-sectional study. Front Neurol. (2024) 15:1501561. doi: 10.3389/fneur.2024.1501561
21. Zhang, W, Ruan, J, Zhang, R, Zhang, M, Hu, X, Han, Z, et al. Association between age-related hearing loss with tinnitus and cognitive performance in older community-dwelling Chinese adults. Psychogeriatrics. (2022) 22:822–32. doi: 10.1111/psyg.12889
22. Han, SY, Seo, HW, Lee, SH, and Chung, JH. Physical inactivity and sedentariness in older hearing loss patients: restoration with hearing aids. Laryngoscope. (2024) 134:5109–15. doi: 10.1002/lary.31638
23. de Gruy, JA, Laurenzo, WW, Vu, T-H, Paul, O, Lee, C, and Spankovich, C. Prevalence and predictors of problematic tinnitus. Int J Audiol. (2025) 64:307–13. doi: 10.1080/14992027.2024.2378804
24. Yévenes-Briones, H, Caballero, FF, Estrada-deLeón, DB, Struijk, EA, Mesas, AE, Banegas, JR, et al. Duration and quality of sleep and risk of self-reported hearing loss: the UK biobank study. Ear Hear. (2023) 44:1182–9. doi: 10.1097/AUD.0000000000001360
25. Bertschi, I. Disability as an Interpersonal Experience: Stress and Dyadic Coping in Couples Facing Chronically Disabling Physical Health Problems: University of Zurich. (2022).
26. Liljas, AE, Wannamethee, SG, Whincup, PH, Papacosta, O, Walters, K, Iliffe, S, et al. Socio-demographic characteristics, lifestyle factors and burden of morbidity associated with self-reported hearing and vision impairments in older British community-dwelling men: a cross-sectional study. J Public Health. (2016) 38:e21–8. doi: 10.1093/pubmed/fdv095
27. Sullivan, K, and Ordiah, C. Association of mildly insufficient sleep with symptoms of anxiety and depression. Neurol Psychiatry Brain Res. (2018) 30:1–4. doi: 10.1016/j.npbr.2018.03.001
28. Ding, KR, Wang, SB, Xu, WQ, Lin, LH, Liao, DD, Chen, HB, et al. Low mental health literacy and its association with depression, anxiety and poor sleep quality in Chinese elderly. Asia Pac Psychiatry. (2022) 14:e12520. doi: 10.1111/appy.12520
29. Thomson, RS, Auduong, P, Miller, AT, and Gurgel, RK. Hearing loss as a risk factor for dementia: a systematic review. Laryngoscope Investigative Otolaryngology. (2017) 2:69–79. doi: 10.1002/lio2.65
30. Maihoub, S, Mavrogeni, P, Molnár, V, and Molnár, A. Tinnitus and its comorbidities: a comprehensive analysis of their relationships. J Clin Med. (2025) 14:1285. doi: 10.3390/jcm14041285
31. Zou, S, Liu, Y, Xu, B, Li, J, and He, Z. Age-related hearing loss: the complex interaction of carbohydrate metabolism in auditory and cognitive dysfunction during aging. Ageing Neurodegenerative Diseases. (2025) 5. doi: 10.1016/j.andd.2025.100035
32. Lampraki, C, Zuber, S, Turoman, N, Joly-Burra, E, Mack, M, Laera, G, et al. Profiles of social isolation and loneliness as moderators of the longitudinal association between uncorrected hearing impairment and cognitive aging. Communications psychology. (2025) 3:101. doi: 10.1038/s44271-025-00277-8
33. Nishimura, Y, Oikawa, M, and Motegi, H. What explains the difference in the effect of retirement on health? Evidence from global aging data. J Econ Surv. (2018) 32:792–847. doi: 10.1111/joes.12215
34. Chia, E-M, Wang, JJ, Rochtchina, E, Cumming, RR, Newall, P, and Mitchell, P. Hearing impairment and health-related quality of life: the Blue Mountains hearing study. Ear Hear. (2007) 28:187–95. doi: 10.1097/AUD.0b013e31803126b6
35. Quaranta, N, Coppola, F, Casulli, M, Barulli, MR, Panza, F, Tortelli, R, et al. Epidemiology of age related hearing loss: a review. Hear Balance Commun. (2015) 13:77–81. doi: 10.3109/21695717.2014.994869
36. Brüggemann, P, Szczepek, AJ, Rose, M, McKenna, L, Olze, H, and Mazurek, B. Impact of multiple factors on the degree of tinnitus distress. Front Hum Neurosci. (2016) 10:341. doi: 10.3389/fnhum.2016.00341
37. Cui, Y, and Du, H. The role of chronic tinnitus in hearing loss-related depression: insights for middle-aged and older adults. Clin Gerontol. (2025) 48:1–17. doi: 10.1080/07317115.2025.2482877
38. Ding, Z, Zhang, C, Wang, F, Wu, X, Chen, T, Wang, L, et al. The association between tinnitus sensation–level loudness and sleep quality in patients with subjective consecutive tinnitus: a mediation analysis. Am J Audiol. (2024) 33:433–41. doi: 10.1044/2024_AJA-23-00063
39. Xu, S, Jesdale, WM, Dubé, CE, Nielsen, NN, McPhillips, EA, and Lapane, KL. Social engagement and cognitive impairment among nursing home residents: the role of sensory impairment. Arch Gerontol Geriatr. (2024) 122:105397. doi: 10.1016/j.archger.2024.105397
40. Nixon, G, Sarant, J, Tomlin, D, and Dowell, R. Hearing aid uptake, benefit, and use: the impact of hearing, cognition, and personal factors. J Speech Lang Hear Res. (2021) 64:651–63. doi: 10.1044/2020_JSLHR-20-00014
Keywords: age-related hearing loss, tinnitus, quality of life, older adults, psychosocial outcomes, multivariable analysis
Citation: Zhang L and Liao Y (2025) Retrospective analysis of hearing loss and tinnitus determinants and their health impact among old adults. Front. Public Health. 13:1720441. doi: 10.3389/fpubh.2025.1720441
Edited by:
Agnieszka J. Szczepek, Charité University Medicine Berlin, GermanyCopyright © 2025 Zhang and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Liao, ZW5zaGlfemhhbmdAMTYzLmNvbQ==
 Lu Zhang
Lu Zhang Yong Liao
Yong Liao