- 1West China School of Medicine, Sichuan University, Sichuan University Affiliated Chengdu Second People's Hospital, Chengdu Second People's Hospital, Chengdu, China
- 2Department of Computing, The Hong Kong Polytechnic University, Kowloon, China
- 3Department of Oncology, Ziyang Central Hospital, Ziyang, China
- 4School of Health Policy and Management, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 5General Practice Ward/International Medical Center Ward, General Practice Medical Center, National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University, Chengdu, China
- 6Department of Endocrinology and Metabolism, West China Hospital, Sichuan University, Chengdu, China
China’s primary care system faced persistent challenges, including uneven resource distribution, a shortage of general practitioners, and a growing burden of chronic diseases. Artificial intelligence (AI) offered new tools to address these issues. This narrative review summarized the applications, benefits, challenges, and practical recommendations for DeepSeek. Literature searches were conducted across both Chinese and English databases, including China National Knowledge Infrastructure, Wanfang Data, and PubMed. In addition, official websites of provincial Health Commissions were searched for AI policies and reports related to DeepSeek deployment. Evidence showed that DeepSeek had been applied to assist clinical decision-making, support chronic disease management, and enhance medical education and research. Reported outcomes included improved diagnostic efficiency, guideline adherence, and patient engagement. However, challenges remained, such as limited model interpretability, potential reductions in humanistic care, unequal accessibility, technical constraints, and data privacy concerns.
1 Background
China faced uneven healthcare resource distribution, a shortage of general practitioners (GPs), and a growing burden of chronic disease (1, 2). Primary care institutions in China constituted the most widely distributed healthcare facilities (3). They delivered essential public health services, routine medical care, and chronic disease management to the majority of the population (3). However, they often faced limited specialty capabilities, particularly for vulnerable populations such as the older adults and children (4). Workforce shortages, insufficient equipment, and gaps in clinical experience hindered the delivery of high-quality care (5). Chronic diseases—including hypertension, type 2 diabetes, and malignancies—continued to rise (6). They contributed significantly to national morbidity and mortality and imposed substantial burdens on primary care providers (6).
Artificial intelligence (AI) offered novel approaches to support primary care and rapidly permeated clinical practice, pharmaceuticals, and health management, driving significant transformation across the healthcare system (7). AI demonstrated potential to address these challenges. It enhanced diagnostic accuracy, supported clinical decision-making, and streamlined workflow in primary care (7, 8). AI-powered systems integrated multi-source data, including electronic health records, laboratory tests, and wearable device measurements. They identified high-risk individuals, guided preventive interventions, and monitored treatment outcomes in real time (9). Early implementations in community hospitals and pilot studies showed that AI assistance improved guideline adherence, optimized chronic disease management, and reduced clinician workload (10).
In January 2025, Hangzhou Deeply Seeking Artificial Intelligence Basic Technology Research Co., Ltd. released DeepSeek-R1, a reasoning-optimized large language model based on DeepSeek-V3 and designed for complex inferential tasks (11). Many primary care settings in China adopted DeepSeek models to enhance clinical practice (12). This narrative review examined the benefits and challenges of DeepSeek across clinical practice, research, and education, highlighting lessons for the effective adoption of generative AI in China’s primary healthcare system.
2 Methods
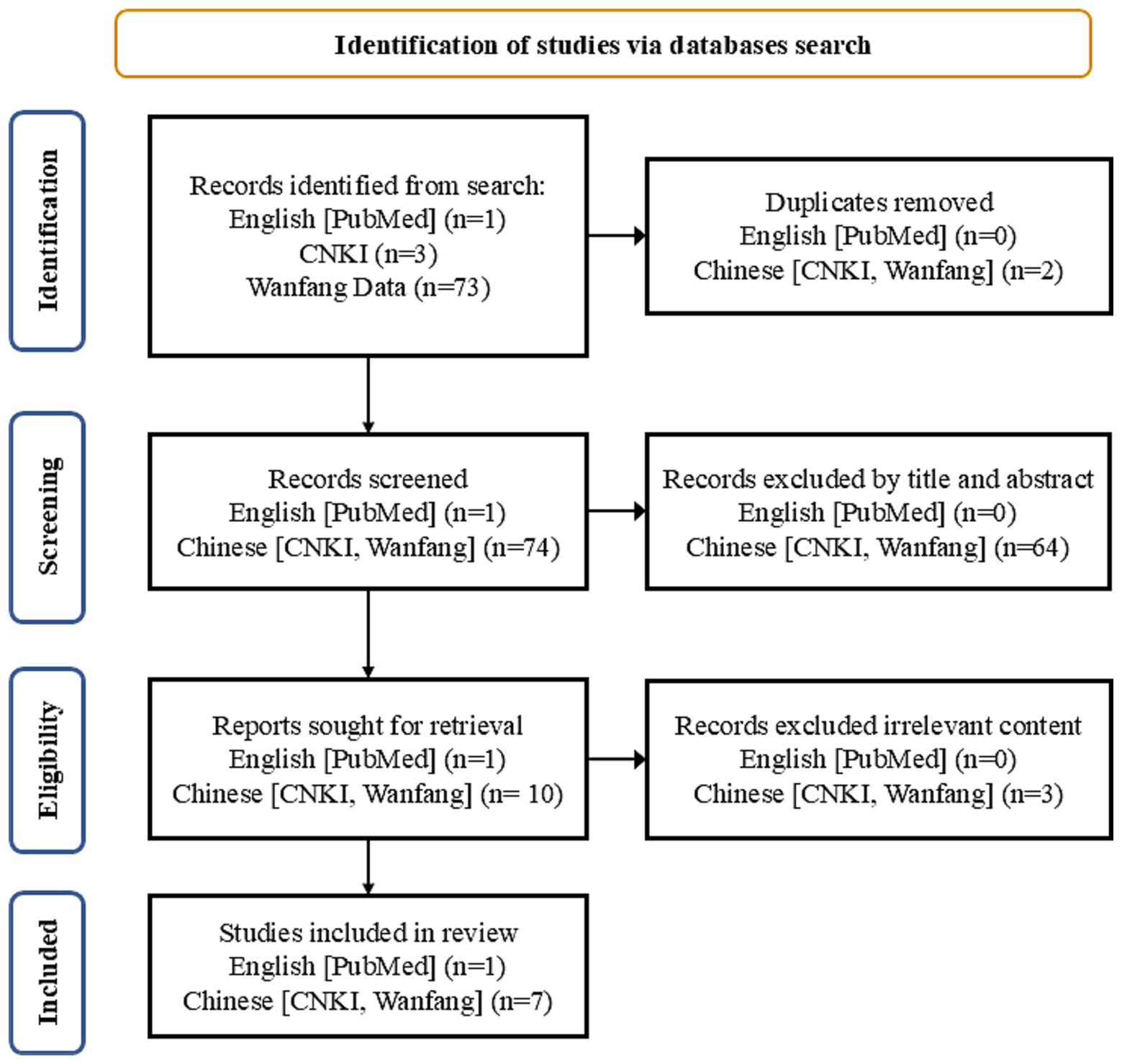
Searches were conducted in both Chinese and English databases, including China National Knowledge Infrastructure (CNKI), Wanfang Data, and PubMed. Primary search terms included ‘DeepSeek,’ ‘artificial intelligence,’ ‘primary care,’ ‘general practitioners,’ and MeSH term ‘Clinical Decision Support Systems.’ The search covered articles published between January 1, 2023, and April 14, 2025, reflecting the period when AI-based clinical decision tools were increasingly adopted in China. Inclusion criteria were: (1) publications in English or Chinese; (2) articles or reviews; (3) studies focused on the use of DeepSeek in primary care. Exclusion criteria were: (1) studies focused on medical education; (2) conference papers, theses, commentaries, editorials, and letters. Details of the literature search and screening process are presented in Figure 1. Furthermore, official websites of provincial Health Commissions were searched for AI policies and reports related to DeepSeek deployment.
3 Results
3.1 Chinese AI policy
China has been actively developing regulatory frameworks for AI, particularly generative AI. Key policies included the Algorithm Recommendation Management Provisions (2021) (13), the Deep Synthesis Management Provisions for Internet Information Services (2022) (14), the Interim Measures for the Management of Generative AI Services (2023) (15), and the Measures for the Identification of AI-Generated Content (2025) (16). The Measures for Ethical Review of Scientific and Technological Activities (Trial) (2023) mandate ethical assessment for algorithms with social influence (17). these regulations aim to promote the ethical and socially responsible use of AI while safeguarding data security, ensuring transparent content labeling, and defining the obligations of service providers.
3.2 DeepSeek technical overview
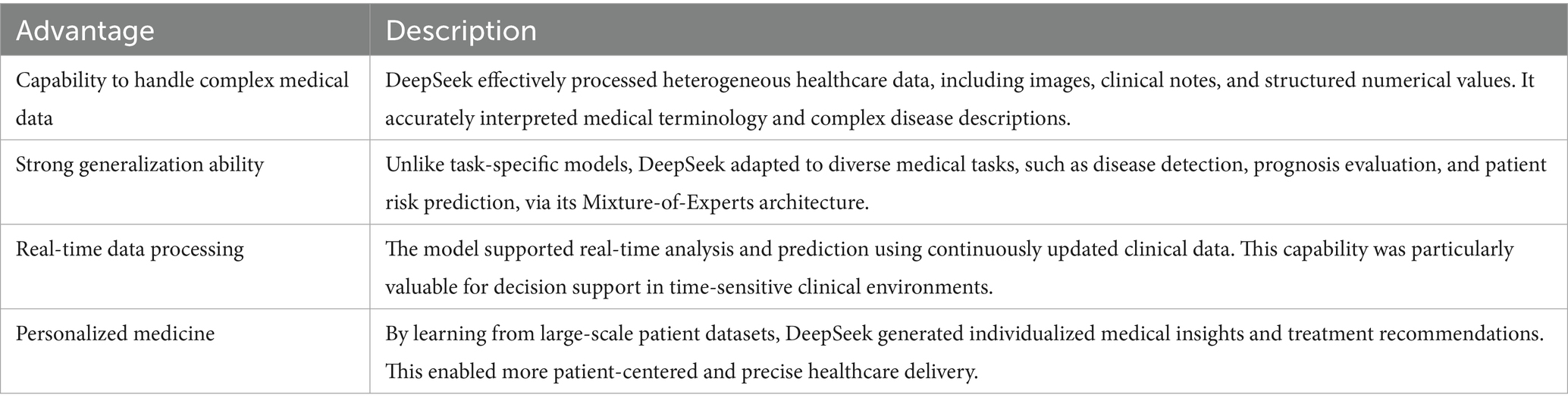
DeepSeek is an open-source platform licensed under the Massachusetts Institute of Technology (MIT) framework, providing a cost-effective alternative to proprietary AI systems (18). Its exceptional inferential capabilities derive from a Mixture-of-Experts architecture, reinforcement learning from human feedback (RLHF), an FP8 mixed-precision framework, and a multi-stage training regimen (18). In benchmark evaluations, DeepSeek-R1 outperformed both Generative Pre-trained Transformer (GPT-4o) and OpenAI’s o1 reasoning model (see Table 1) (19). Its capabilities extended into multimodal AI with the Janus-Pro-7B variant (11). DeepSeek demonstrated superior performance compared with other Chinese AI models (see Figure 2) (20).
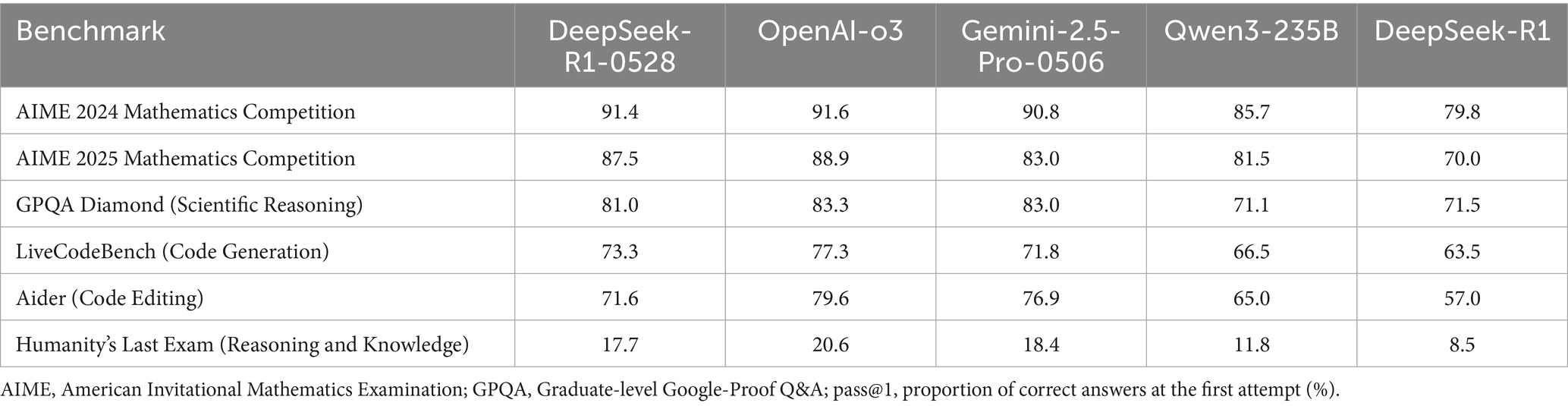
Table 1. Performance comparison of leading large language models across standardized benchmarks (pass@1, %).
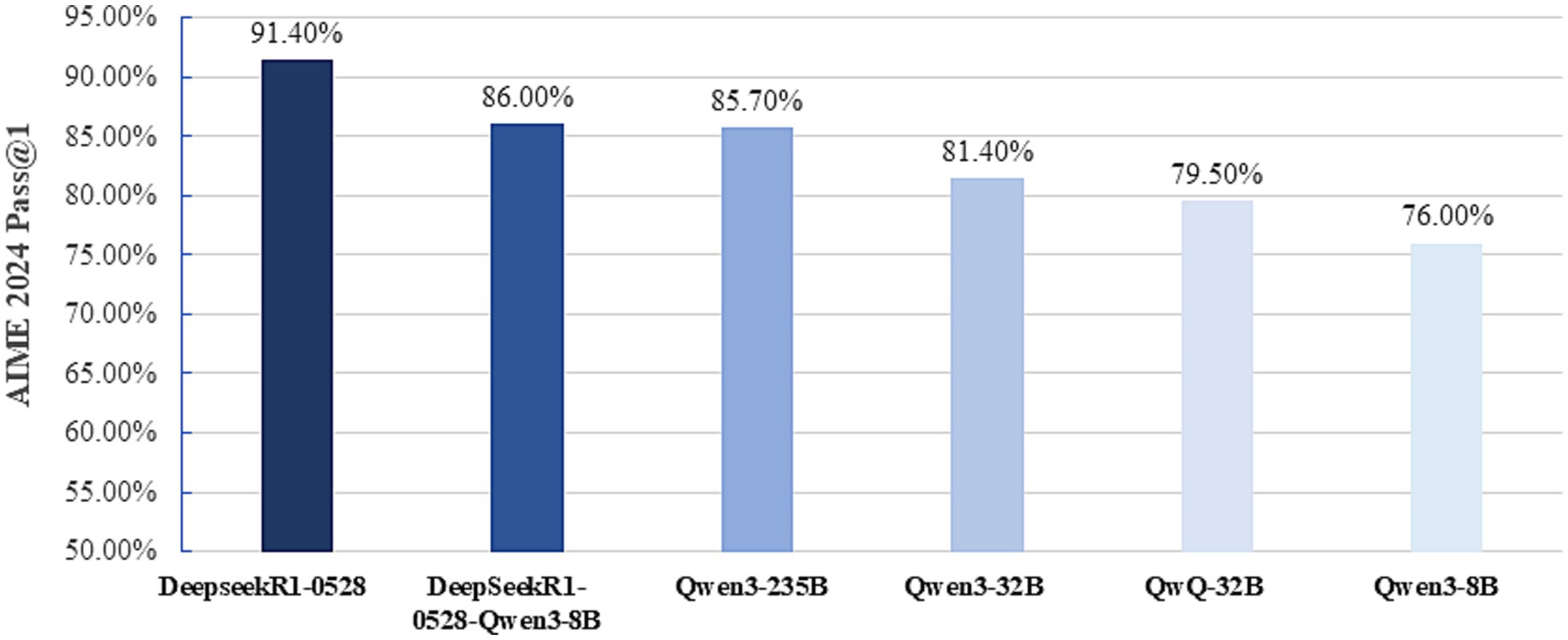
Figure 2. Performance of Chinese large language models on the 2024 American Invitational Mathematics Examination. AIME, American Invitational Mathematics Examination;pass@1, proportion of correct answers at the first attempt (%).
The model’s deep reasoning ability enables support for general practitioners in clinical practice, research, and educational training, particularly when augmented with high-quality, up-to-date knowledge during fine-tuning (21). DeepSeek offers flexibility via an application programming interface (API), allowing users to access its functions at lower cost than other large models and to run it locally (11). Unlike many general-purpose models, which often lack detailed version histories and transparent update logs, DeepSeek employs a dual identifier system of model version and training timestamp (22). During fine-tuning, all parameter adjustments are fully recorded, including supervised fine-tuning (SFT) datasets and RLHF ethical alignment strategies, ensuring traceability and accountability in model updates (18).
3.3 Advantages of DeepSeek
DeepSeek-R1 leveraged existing AI tools, including Mixture-of-Experts (MoE), reinforcement learning, and data distillation, to achieve breakthrough reasoning efficiency (18). It uniquely revealed the “chain of thought” during inference, enhancing transparency for users (see Table 2) (18). By deploying smaller, reliable, and open models on flexible infrastructures, the platform ensured effective and safe AI integration. DeepSeek strictly followed TRIPOD-LLM reporting guidelines, enabling full traceability from data de-identification to decision annotation, and establishing an ethically grounded technical framework (11, 12, 18).
3.4 Applications of DeepSeek in primary care
3.4.1 Empowering general practitioners
In primary care settings, diagnostic accuracy and timely decision-making were critical. DeepSeek assisted GPs by automating repetitive tasks, including standardized data entry, intelligent retrieval and integration of dispersed medical information, and generation of structured clinical documentation (23). The platform integrated multidimensional patient data—such as medical history, physical findings, and test results—and applied evidence-based reasoning to generate clinical recommendations (12). Logical inference modules reduced purely data-driven biases and supported personalized treatment planning, improving healthcare quality and outcomes (18). In a recent survey of GPs in Zhejiang Province, 64.3% reported actively using DeepSeek, and more than half (54.4%) perceived it as a collaborative decision-making tool rather than a replacement for clinicians (24).
A representative clinical case further illustrated the promise of DeepSeek-assisted diagnosis (25). A 57-year-old woman with recurrent epigastric pain consulted multiple surgeons and underwent extensive gastrointestinal and cardiologic workups, which yielded nonspecific findings. Dissatisfied with persistent symptoms, she subsequently engaged in more than 100 rounds of interaction with the DeepSeek system. The model suggested a possible diagnosis of somatic symptom disorder, prompting referral to the psychiatry department. Subsequent standardized psychological assessments confirmed the diagnosis, and targeted psychopharmacological and behavioral interventions led to marked symptom relief after 6 weeks. DeepSeek effectively compensated for the limitations of traditional episodic consultations by maintaining ongoing engagement.
Yuquan District Xicaiyuan Subdistrict Community Health Service Center implemented an AI-powered clinical system based on DeepSeek (26). The system integrated an intelligent knowledge graph covering 7,000 diseases and generated real-time diagnostic recommendations. It accurately identified 39 categories of critical and emergent conditions with an accuracy of 98.6%. Its drug database included over 1,400 medications, and during the trial phase, 136 inappropriate prescriptions were intercepted. AI automatically generated chronic disease follow-up plans, increasing response efficiency for abnormal indicators by 50% and improving public health data aggregation efficiency by 60%. Within 3 months of deployment, the system enhanced performance: outpatient diagnosis compliance reached 94.8%, medical record review time decreased by 70%, and patient satisfaction achieved 98.5% (26).
3.4.2 DeepSeek in health management
DeepSeek leveraged artificial intelligence and big data analytics to identify individuals at high risk for chronic diseases in primary healthcare (21). By integrating data from multiple sources—including wearable devices, telemedicine platforms, and electronic health records—DeepSeek facilitated early screening, risk stratification, and personalized health interventions (21). It constructed dynamic health profiles, monitored patient metrics in real time (e.g., blood glucose and blood pressure), and delivered individualized health guidance through smartphones or wearable devices. Meinian Onehealth used a DeepSeek-powered chatbot to provide diabetes education (27). Longgang District Maternity and Child Healthcare Hospital imported a 2.05-million-word prenatal diagnostic knowledge base into DeepSeek, enabling citizens to access evidence-based prenatal information interactively (28).
DS-Xiaobu Doctor 2.0, an AI-assisted system based on DeepSeek, was evaluated in pediatric outpatient care (29). The system reduced average consultation and diagnostic times to 2.16 and 5.86 min and achieved 92.4% overall diagnostic accuracy (29). Caregiver satisfaction was high, with a Net Promoter Score of +78. In the pediatric pneumonia scenario, DS-Xiaobu Doctor 2.0 (92.4%) outperformed GPT-4Med (89.1%) and Bio MedLM (88.6%) in diagnostic accuracy.
3.4.3 Bridging the urban–rural healthcare gap
DeepSeek enabled rapid deployment of hospital information systems (HIS) within a short period, supporting digital transformation in resource-limited primary care institutions (30). Its AI-assisted diagnostic system enhanced the specialty-level competencies of GPs, addressing challenges of workforce shortages and outdated clinical knowledge (31). In underserved regions, DeepSeek provided essential medical support through remote consultations and intelligent triage. The localized deployment model also improved data security and privacy protection. At the Fifth Affiliated Hospital of Southern Medical University, DeepSeek was used to optimize drug inventory and distribution systems for remote and low-income areas (32). In Yilong County, Nanchong, the system integrated electronic medical records and public health archives, automatically generating individualized “one person, one record” health profiles through dynamic data aggregation and analysis (33). At Youxian People’s Hospital in Mianyang, DeepSeek automatically generated personalized follow-up plans and delivered health reminders to patients (34). On average, each patient encounter saved 15–20 min, resulting in an approximate 30% increase in daily patient throughput for GPs (34).
DeepSeek provided real-time responses to health inquiries, offered guidance on personalized health planning, and delivered preventive recommendations (35). The system supported individuals with varying levels of health literacy through empathetic interactions and extended services to underserved populations. DeepSeek was free and available in multiple formats, including a web version, mobile applications, and a desktop client (11). By enabling scalable access to both health information and emotional support, DeepSeek complemented traditional healthcare delivery and enhanced patient engagement across diverse communities.
3.4.4 DeepSeek in medical education
Generative AI based on DeepSeek reshaped medical education. It enabled the creation of high-fidelity virtual patient cases that simulated the full clinical workflow, including history-taking, physical examination, and diagnosis. Inspur Group Co., Ltd. integrated DeepSeek technology to build diverse simulation scenarios, such as internal medicine emergencies and complex pediatric disorders (36). Through voice interaction and dynamic disease progression, the system trained medical students in diagnostic reasoning and emergency response. It also imitated patients’ emotional expressions and communication needs, helping trainees improve empathy and communication skills (37). At Shandong University QILU Hospital, the AI digital patient system improved the efficiency of standardized resident assessments (38). Using the MoE architecture and DeepSeek’s fine-tuning framework with multimodal reasoning, the time needed to build case-based knowledge databases was reduced by about 30% (38). The platform dynamically generated disease progression pathways, simulated complex clinical decisions, and supported AI-based performance evaluations.
3.4.5 Enhancing general practice research with DeepSeek
DeepSeek’s integrated knowledge base incorporated cutting-edge academic papers, patent databases, and global innovation case libraries, alongside the latest clinical guidelines and typical case examples, addressing the long-standing issue of outdated teaching resources (12, 18). DeepSeek enabled real-time retrieval of academic information, allowing researchers to rapidly access the latest scientific advances. Its data reasoning capabilities assisted general practitioners in various stages of research, including topic selection, study design, data processing, and analysis. DeepSeek efficiently mined large volumes of literature to identify research trends in general practice. It also provided automated literature review generation, experimental design optimization, and innovation assessment, thereby lowering the entry barrier for clinical research. Open-source nature reduced technological barriers, while lightweight model versions (e.g., 1.5B or 7B parameters) enabled cost-effective deployment in primary care institutions (11). When combined with retrieval-augmented generation (RAG), DeepSeek further enhanced the precision and depth of knowledge retrieval and application (39).
3.5 Challenges in the application of DeepSeek in primary care
3.5.1 Ethical risks
DeepSeek was susceptible to intrinsic limitations such as algorithmic bias, hallucination, and output unreliability, which raised multiple ethical concerns (40). DeepSeek-R1’s underlying architecture employed a multi-head latent attention mechanism (MLA) to extend contextual processing but retained limitations in long-range semantic modeling (18). This could lead to misinterpretation of complex medical terminology and semantic relationships. The training corpus was primarily derived from open internet sources, inevitably exposing the model to unverified or intentionally manipulated information, a phenomenon often referred to as “data pollution” (41). DeepSeek-R1 also showed biases in decoding metaphorical expressions and culturally embedded emotional content (41). These issues necessitated rigorous pre-deployment validation, human-in-the-loop oversight, and ongoing performance monitoring in clinical settings.
Such technical limitations can translate into real-world ethical dilemmas, as illustrated by a case in which AI-mediated insights challenged professional expertise. A 41-year-old female with a two-year history of a right lung ground-glass nodule (7 mm) actively engaged DeepSeek to analyze longitudinal CT imaging, receiving an AI assessment suggesting high malignancy risk (25). Despite the absence of clinical symptoms and guideline-based recommendations for conservative follow-up, she requested surgical intervention, diverging from the approach initially recommended by her clinicians (25). Postoperative pathology confirmed minimally invasive adenocarcinoma.
3.5.2 Lack of embedded clinical expertise
DeepSeek’s effectiveness depended heavily on the completeness and accuracy of medical data (42). However, electronic medical record data in China has been reported as suboptimal, with high rates of errors in demographic, surgical, and diagnostic information and pervasive issues in interoperability, unstructured entries, and coding inconsistencies (43–45). Such deficiencies could compromise AI systems like DeepSeek by introducing algorithmic bias, reducing diagnostic accuracy, and limiting interpretability. Incomplete or inconsistent real-world data may increase hallucinations, misclassification of medical terms, and errors in semantic inference, ultimately affecting clinical reliability and ethical use. When managing rare diseases (e.g., incidence <1/100,000) or complex cases, the limited availability of relevant data could prevent DeepSeek from accurately capturing disease characteristics, potentially leading to unreliable diagnoses (42). Furthermore, few randomized controlled trials or rigorous clinical validations had been conducted to confirm its clinical effectiveness.
DeepSeek-R1 improved primary care efficiency through lightweight deployment. AI-generated ‘optimal’ solutions represented statistical rather than holistic clinical optimality (46). Patient-specific factors, including psychological traits and cultural context, remained critical in decision-making (47). Continued dependence on AI recommendations without integrating professional expertise could therefore create ethical risks, including potential misdiagnoses and errors in critical clinical decisions (48).
3.5.3 Risk of eroding humanistic care
The increasing adoption of AI systems such as DeepSeek risked diminishing the role of humanistic care in clinical encounters. It could inadvertently reduce meaningful communication and emotional engagement between clinicians and patients (49). For health care professionals, the risks manifest in 2 distinct ways: some clinicians may develop overreliance on DeepSeek, leading to uncritical adoption of its outputs and subsequent diagnostic errors or treatment biases (30, 50). This concern was particularly pronounced in primary care, where continuity, coordination, personalization, and empathy were core service attributes.
When patients access Al-generated medical information without proper clinical context or guidance, they may use these outputs to evaluate the appropriateness of treatments recommended by their physicians. This can generate unwarranted skepticism and new sources of patient–physician conflict. A 54-year-old man had been admitted after routine imaging identified multiple gallstones with radiologic signs of cholecystitis; clinical examination and laboratory tests were unremarkable (25). He underwent an uneventful laparoscopic cholecystectomy and recovered without complication. Following discharge, however, the patient had repeatedly consulted DeepSeek and received conservative-management suggestions (watchful waiting and gallstone-preserving procedures). Citing these AI-sourced opinions, the patient subsequently challenged the surgical indication and filed a formal complaint against the operating team.
This episode illustrated several interrelated concerns. First, LLM outputs could amplify existing guideline ambiguity or present fragmentary evidence that patients may perceive as authoritative (51). Second, when patients acted on AI advice that conflicted with clinician judgment, it often resulted in erosion of clinical authority, breakdowns in informed consent, and new medico-legal disputes (52).
3.5.4 Data privacy and security concerns
DeepSeek’s effectiveness relied on large-scale data collection, raising concerns about privacy and misuse (53). Although regulatory frameworks such as the EU Artificial Intelligence Act and relevant Chinese regulations (15, 16) mandate transparency for high-risk AI systems, including traceable decision pathways, verifiable training data sources, and defined application boundaries (54). DeepSeek-R1 remained vulnerable to privacy breaches, particularly from data theft. Data minimization could partially reduce risks in centralized storage, yet distributed computing nodes remained susceptible to attacks, and data synchronization could be tampered with (41). Knowledge distillation from large to smaller models required feature extraction and transformation, increasing the risk of re-identifying de-identified data. Rapid deployment intensified these challenges, especially in resource-limited healthcare facilities lacking robust cybersecurity (41). Local deployment reduced cloud-related risks but shifted security responsibility to individual institutions, and integration with existing hospital information systems without adequate safeguards could introduce new vulnerabilities, given the model’s extensive parameter requirements and hardware demands (55).
3.5.5 Accessibility and usability across diverse populations
User adaptability varied across demographic groups. Older adults individuals, people with disabilities, and populations with lower educational attainment often faced greater challenges in interacting with AI-driven systems (56). Populations with lower educational attainment or limited health literacy were more likely to misinterpret AI outputs, overlook important recommendations, or struggle to integrate guidance into daily health management (57). These disparities created uneven adoption and utilization of AI systems, potentially exacerbating existing health inequities and limiting the overall effectiveness of digital health interventions in primary care settings (58).
3.5.6 Implementation costs
Deploying AI systems such as DeepSeek in resource-limited primary care settings involves not only direct costs but also substantial indirect expenditures, including hardware requirements (high-performance servers, secure data storage, reliable internet), staff training, and technical support (50).
3.6 Practical recommendations for implementing DeepSeek in primary care
3.6.1 Data mining and knowledge graph construction
To enhance DeepSeek’s interpretability and clinical relevance, primary care institutions should integrate multi-source healthcare data—including electronic health records, laboratory results, imaging studies, and wearable device data—into standardized, structured databases. Clinical knowledge graphs linking diseases, symptoms, treatments, and patient characteristics can then be constructed to provide semantic context. These knowledge graphs should be continuously updated with newly published guidelines and local clinical protocols. Fine-tuning DeepSeek on these graphs allows the model to generate evidence-based, transparent recommendations tailored to individual patients, enabling reproducible and clinically meaningful decision support.
Effective deployment of DeepSeek required deep integration of domain-specific medical knowledge (30). To ensure that model outputs aligned with real-world clinical practice, the development and interpretation of LLMs needed involvement from healthcare professionals with general practice expertise (40). Embedding clinical reasoning into model design was essential to improve interpretability and clinical relevance, particularly in primary care, where decision-making was multifactorial and highly individualized.
3.6.2 Clinical validation
Robust evaluation of DeepSeek’s clinical effectiveness requires well-designed multicentre studies. Primary care networks should implement pre–post intervention designs or randomized controlled trials comparing outcomes with and without DeepSeek assistance. Data collection should encompass diagnostic accuracy, treatment adherence, workflow efficiency, and patient-reported outcomes such as satisfaction and engagement (59). The findings can guide iterative model refinement, validate AI-driven recommendations in real-world settings, and provide a scientific basis for scaling deployment across diverse primary care environments.
To enhance inclusiveness, DeepSeek should support multimodal human-computer interaction, including voice commands, touch interfaces, and gesture recognition, alongside assistive features tailored to specific populations. Incorporating multilingual and localized content could mitigate comprehension issues arising from regional dialects or speech impairments, reducing risks of misinterpretation and diagnostic error (60).
3.6.3 Training programs for general practitioners
Successful adoption of DeepSeek depends on comprehensive clinician training. Health systems should establish structured programs that combine hands-on workshops, online modules, and case-based simulations to teach general practitioners how to interpret AI outputs, verify recommendations, and integrate insights into patient management. Training should include strategies for identifying model limitations, mitigating overreliance on AI, and maintaining professional judgment. Periodic assessments and refresher courses can ensure sustained proficiency and safe application of AI-assisted clinical decision-making. Developers were encouraged to deliberately integrate humanistic elements into AI systems to address patients’ emotional, psychological, and social needs, thereby preserving doctor–patient rapport (61).
3.6.4 Ethical and technical guidelines
To ensure responsible use, healthcare institutions should establish clear ethical and technical guidelines for DeepSeek deployment. These should define the boundaries for recommendation adoption, affirming that final clinical decisions rest with the physician. Policies must address data privacy, security, and governance, including protocols for handling sensitive patient information. Additionally, mechanisms for monitoring model performance, detecting biases, and ensuring fairness and transparency should be implemented (62). Clear documentation of model updates and decision logic will further support accountability and maintain trust in AI-assisted primary care.
3.6.5 Implementing a closed-loop primary care model with DeepSeek
DeepSeek supported a closed-loop primary care model, comprising pre-visit AI-assisted triage and data collection, in-visit clinical decision support and teleconsultation, and post-visit follow-up with automated reminders and continuous monitoring (23). Its intelligent health management system incorporated the latest clinical evidence and guidelines, enabling adaptive and individualized care, particularly for chronic disease management in community populations (23). The platform delivered targeted health education and real-time care recommendations, which promoted healthier lifestyles and facilitated timely clinical interventions (Figure 3) (23).
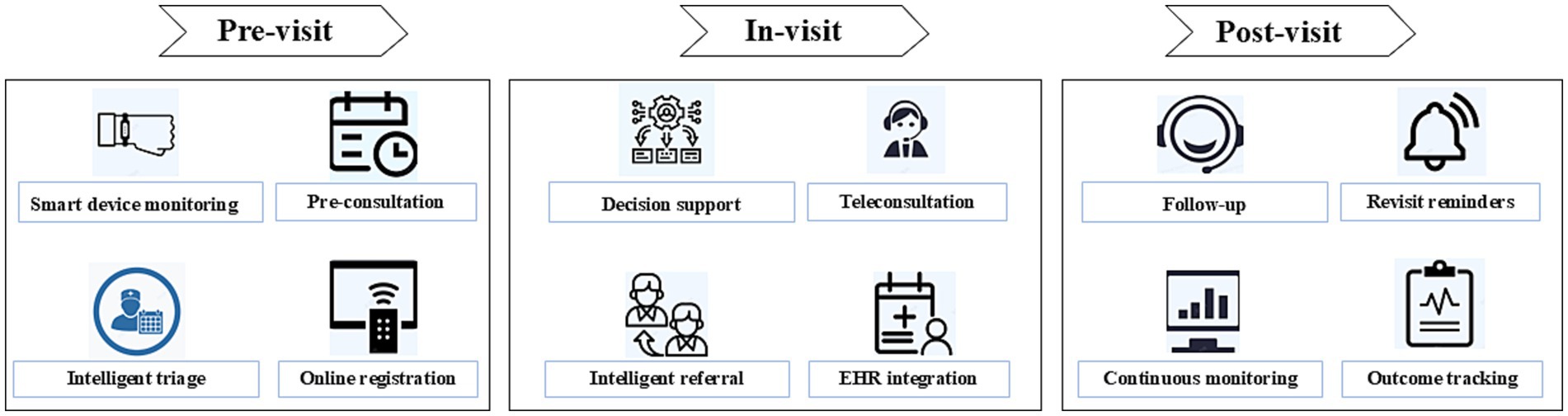
Figure 3. Digital health–enabled primary care workflow across pre-visit, in-visit, and post-visit stages.
4 Strengths and limitations
This review summarized the application of DeepSeek in Chinese primary care, covering clinical practice, research, education, and health management. It provided actionable recommendations for implementation. However, few original studies or multicenter trials directly evaluated its clinical effectiveness, particularly in real-world primary care settings. Most data came from pilot projects or institutional reports, limiting generalizability and the assessment of long-term impacts on patient outcomes and workflow efficiency.
5 Conclusion
DeepSeek demonstrated considerable potential in supporting primary care in China by enhancing clinical decision-making, chronic disease management, medical education, and research productivity. It was currently applied in primary care settings, where it assisted clinicians, supported health management, and facilitated training and research. However, challenges remained, including limited interpretability, potential reduction in humanistic care, accessibility issues, technical limitations, and data privacy concerns. To maximize the benefits of DeepSeek, future efforts should focus on rigorous clinical validation, structured training for general practitioners, robust ethical and technical guidelines, and integration with local healthcare data and knowledge systems. By addressing these challenges, DeepSeek and similar AI tools can empower primary care providers, promote equitable healthcare delivery, and contribute to a more intelligent and patient-centered healthcare system.
Author contributions
JZ: Conceptualization, Writing – original draft. DL: Writing – original draft. XW: Supervision, Writing – original draft. ZW: Conceptualization, Writing – original draft. QL: Writing – review & editing, Supervision, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The study team is grateful to all colleagues who participated in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. An, K, Zhang, R, Zhu, B, Liu, L, Tang, J, Ma, Y, et al. Familiarity of teaching skills among general practitioners transfer training trainers in China: a cross-sectional survey. BMC Med Educ. (2023) 23:949. doi: 10.1186/s12909-023-04945-3
2. An, K, Zhang, L, Qiao, RJ, Li, CZ, Zhong, Q, Ma, YR, et al. Training needs and curriculum of continuing medical education among general practitioners in Tibet, China: a cross-sectional survey. Front Public Health. (2022) 10:914847. doi: 10.3389/fpubh.2022.914847
3. An, K, Zhang, J, Wang, X, She, Y, Li, S, and Li, S. Integration and innovation: medical and health consortia improving continuing medical education in China. Front Public Health. (2025) 13:1633363. doi: 10.3389/fpubh.2025.1633363
4. Qin, J, Lin, C, Zhang, Y, and Zhang, L. The status and challenges of primary health care in China. Chin Gen Pract. (2024) 1:182–7. doi: 10.1016/j.cgpj.2024.07.005
5. Li, X, Krumholz, HM, Yip, W, Cheng, KK, De Maeseneer, J, Meng, Q, et al. Quality of primary health care in China: challenges and recommendations. Lancet. (2020) 395:1802–12. doi: 10.1016/S0140-6736(20)30122-7
6. An, K, Zhang, J, Wang, X, Qiao, R, and An, Z. The burden of type 2 diabetes in China from 1990 to 2021: a comparative analysis with G20 countries using the global burden of disease study 2021. Diabetes Res Clin Pract. (2025) 224:112188. doi: 10.1016/j.diabres.2025.112188
7. Fahim, YA, Hasani, IW, Kabba, S, and Ragab, WM. Artificial intelligence in healthcare and medicine: clinical applications, therapeutic advances, and future perspectives. Eur J Med Res. (2025) 30:848. doi: 10.1186/s40001-025-03196-w
8. Elhaddad, M, and Hamam, S. AI-driven clinical decision support systems: An ongoing pursuit of potential. Cureus. (2024) 16:e57728. doi: 10.7759/cureus.57728
9. Vaghari, D, Mohankumar, G, Tan, K, Lowe, A, Shering, C, Tino, P, et al. AI-guided patient stratification improves outcomes and efficiency in the AMARANTH Alzheimer’s disease clinical trial. Nat Commun. (2025) 16:6244. doi: 10.1038/s41467-025-61355-3
10. Maleki Varnosfaderani, S, and Forouzanfar, M. The role of AI in hospitals and clinics: transforming healthcare in the 21st century. Bioengineering. (2024) 11:337. doi: 10.3390/bioengineering11040337
11. DeepSeek. (2025). deepseek-ai/DeepSeek-R1. Available online at: https://github.com/deepseek-ai/DeepSeek-R1 (accessed June 10, 2025).
12. Chen, J, and Miao, C. DeepSeek deployed in 90 Chinese tertiary hospitals: how artificial intelligence is transforming clinical practice. J Med Syst. (2025) 49:53. doi: 10.1007/s10916-025-02181-4
13. The Central People's Government, of the People's Republic of China. (2022). Provisions on the Administration of Algorithmic Recommendation for internet information services. Available online at: https://www.gov.cn/zhengce/2022-11/26/content_5728941.htm (accessed November 11, 2025).
14. The Cyberspace Administration of China. (2022. Provisions on the Administration of Deep Synthesis of internet information services. Available online at: https://www.gov.cn/zhengce/zhengceku/2022-12/12/content_5731431.htm (accessed January 11, 2025).
15. China TCAo. (2023). Interim measures for the Administration of Generative Artificial Intelligence Services. Available online at: https://www.gov.cn/zhengce/zhengceku/202307/content_6891752.htm (accessed January 11, 2025).
16. The Cyberspace Administration of China. (2025). Notice on the issuance of the measures for the identification of artificial intelligence-generated content. Available online at: https://www.gov.cn/zhengce/zhengceku/202503/content_7014286.htm (accessed March 11, 2025).
17. Ministry of Science and Technology of the People’s Republic of China. (2023). Measures for the ethical review of scientific and technological activities (trial). Available online at: https://www.most.gov.cn/xxgk/xinxifenlei/fdzdgknr/fgzc/gfxwj/gfxwj2023/202310/t20231008_188309.html (accessed March 11, 2025).
18. Guo, D, Yang, D, Zhang, H, Song, J, Wang, P, Zhu, Q, et al. DeepSeek-R1 incentivizes reasoning in LLMs through reinforcement learning. Nature. (2025) 645:633–8. doi: 10.1038/s41586-025-09422-z
19. LLMDB. (2025). LLM Benchmarks. Available online at: https://llmdb.com/benchmarks (accessed June 10, 2025).
20. artificialanalysis.ai. (2024). AIME-2024. Available online at: https://artificialanalysis.ai/evaluations/ (accessed May 10, 2025).
21. MohanaSundaram, A, Sathanantham, ST, Ivanov, A, and Mofatteh, M. Deepseek's readiness for medical research and practice: prospects, bottlenecks, and global regulatory constraints. Ann Biomed Eng. (2025) 53:1754–6. doi: 10.1007/s10439-025-03738-7
22. Tu, X, He, Z, Huang, Y, Zhang, Z-H, Yang, M, and Zhao, J. An overview of large AI models and their applications. Visual Int. (2024) 2:34. doi: 10.1007/s44267-024-00065-8
23. Yan, WX, Liu, J, and Liang, WN. Deepseek empowers general medicine: potential application and prospect. Chin Gen Pract 2025; 28:2065–2069. doi: doi: 10.12114/j.issn.1007-9572.2025.0023.
24. Yan, FCQ, Liu, Y, Lü, J, Ren, JJ, and Chen, J. Analysis on evaluation attitudes and usage willingness of general practi-tioners towards DeepSeek. Chin Med Herald. (2025) 22:1–10. doi: 10.20047/j.issn1673-7210.2025.18.01
25. Yu, FWG, Li, Z, and Xie, Y. Deepseek empowering healthcare and the reflections on professional, legal, and ethical game. Med Philos. (2025) 46:25–9. doi: 10.12014/j.issn.1002-0772.2025.11.05
26. Xicaiyuan Subdistrict Community Health Service Center. (2025). Xicaiyuan subdistrict community health service center implemented the DeepSeek AI system. Available online at: http://www.yuquan.gov.cn/dtzx/zjdsq/202504/t20250409_1876031.html (accessed June 10, 2025).
27. Meinian Onehealth. (2025). AI + Medical. Available online at: https://www.meinian.cn/ (accessed February 10, 2025).
28. Shenzhen Longgang District Health Bureau. (2025). Deploy DeepSeek large model. Available online at: https://www.lg.gov.cn/lgwjj/gkmlpt/content/12/12001/post_12001653.html#6750 (accessed February 10, 2025).
29. Zhang, X, Fr,, Yang, R, Ye, C, Wang, X, Ge, X, et al. A DeepSeek-enabled intelligent pediatric healthcare system: construction and application effectiveness evaluation. Chin J Evid Based Pediatrics. (2025) 20:217–22. doi: 10.3969/j.issn.1673-5501.2025.03.010
30. Shen, T, Li, Y, Cao, Y, Du, X, Wang, X, Zhang, Y, et al. Rapid deployment of large language model DeepSeek in Chinese hospitals demands a regulatory response. Nat Med. (2025) 31:3233–8. doi: 10.1038/s41591-025-03836-y
31. Kong, Z, Kong, D, Kong, J, Xing, Y, and Liang, P. The performance evaluation of the AI-assisted diagnostic system in China. BMC Health Serv Res. (2025) 25:1179. doi: 10.1186/s12913-025-13344-x
32. Southern Medical University. DeepSeek practical exploration. (2025). Available online at: https://news.smu.edu.cn/info (accessed November 10, 2025).
33. Health Council of Yilong County. (2025). New paradigm of health management. Available online at: https://www.yilong.gov.cn/ (accessed November 10, 2025).
34. Health Commission of Sichuan Province. (2025). The province's first pilot district and county! Rural hospitals in youxian district, Mianyang, have access to“full blood Deepseek”. Available online at: https://wsjkw.sc.gov.cn/scwsjkw/szzsdwdt/2025/3/3/9f70959642ae49e28778c11cbf5194c1.shtml (accessed October 6, 2025).
35. Chen, J, and Zhang, Q. Deepseek reshaping healthcare in China's tertiary hospitals. Cham: Springer (2025).
36. Inspur Group. (2025). Inspur information launches metabrain R1 inference server. Available online at: https://www.inspur.com/lcjtww/gylc32/2315125/index.html (accessed October 7, 2025).
37. GMW Online. (2025). A new paradigm in medical education: Langchao Yunfan AI digital patients fully integrated with DeepSeek. Available online at: https://tech.gmw.cn/2025-02/19/content_37858199.htm (accessed October 9, 2025).
38. Shandong University QILU Hospital. (2025). QILU hospital successfully deploys DeepSeek large model, accelerates the construction of smart hospital. Available online at: https://www.qiluhospital.com/show-25-39572-1.html (accessed September 20, 2025).
39. Wang, Y, Wan, Y, Lei, X, Chen, Q, and Hu, H. A retrieval augmented generation based optimization approach for medical knowledge understanding and reasoning in large language models. Array. (2025) 28:100504. doi: 10.1016/j.array.2025.100504
40. Temsah, A, Alhasan, K, Altamimi, I, Jamal, A, Al-Eyadhy, A, Malki, KH, et al. DeepSeek in healthcare: revealing opportunities and steering challenges of a new open-source artificial intelligence frontier. Cureus. (2025) 17:e79221. doi: 10.7759/cureus.79221
41. Wang, S, and Li, M. From ChatGPT 4.0 to DeepSeek-R1: innovative applications and ethical governance paradigm shifts of artificial intelligence in healthcare. Chin J Med Ethics. (2025) 2:1–9.
42. Liang, W, Chen, P, Zou, X, Lu, X, Liu, S, Yang, J, et al. DeepSeek: the "Watson" to doctors-from assistance to collaboration. J Thorac Dis. (2025) 17:1103–5. doi: 10.21037/jtd-2025b-03
43. Jin, F, Yao, C, Yan, X, Dong, C, Lai, J, Li, L, et al. Gap between real-world data and clinical research within hospitals in China: a qualitative study. BMJ Open. (2020) 10:e038375. doi: 10.1136/bmjopen-2020-038375
44. Ge, D, Xia, Y, and Zhang, Z. Analyzing the medical record homepages quality in a Chinese EMR system. BMC Med Inform Decis Mak. (2025) 25:121. doi: 10.1186/s12911-025-02949-1
45. Zhong, J, Zhang, J, Fang, H, Liu, L, Xie, J, and Wu, E. Advancing the development of real-world data for healthcare research in China: challenges and opportunities. BMJ Open. (2022) 12:e063139. doi: 10.1136/bmjopen-2022-063139
46. Reddy, S. Generative AI in healthcare: an implementation science informed translational path on application, integration and governance. Implement Sci. (2024) 19:27. doi: 10.1186/s13012-024-01357-9
47. Lyu, Y, Xu, Q, and Liu, J. Exploring the medical decision-making patterns and influencing factors among the general Chinese public: a binary logistic regression analysis. BMC Public Health. (2024) 24:887. doi: 10.1186/s12889-024-18338-8
48. Elgin, CY, and Elgin, C. Ethical implications of AI-driven clinical decision support systems on healthcare resource allocation: a qualitative study of healthcare professionals’ perspectives. BMC Med Ethics. (2024) 25:148. doi: 10.1186/s12910-024-01151-8
49. Chen, D, Chauhan, K, Parsa, R, Liu, ZA, Liu, F-F, Mak, E, et al. Patient perceptions of empathy in physician and artificial intelligence chatbot responses to patient questions about cancer. NPJ Digital Med. (2025) 8:275. doi: 10.1038/s41746-025-01671-6
50. Zeng, D, Qin, Y, Sheng, B, and Wong, TY. Deepseek's "low-cost" adoption across China's hospital systems: too fast, too soon? JAMA. (2025) 333:1866–9. doi: 10.1001/jama.2025.6571
51. de Hond, A, Leeuwenberg, T, Bartels, R, van Buchem, M, Kant, I, Moons, KGM, et al. From text to treatment: the crucial role of validation for generative large language models in health care. Lancet Digital Health. (2024) 6:e441–3. doi: 10.1016/S2589-7500(24)00111-0
52. Mello, MM, Char, D, and Xu, SH. Ethical obligations to inform patients about use of AI tools. JAMA. (2025) 334:767–70. doi: 10.1001/jama.2025.11417
53. Xu, Z, Liu, S, Huang, W, Shi, J, Xu, F, Tang, X, et al. Deepseek: implications for data science and management in the AI era. Data Sci Manage. (2025). doi: 10.1016/j.dsm.2025.09.001
54. Cancela-Outeda, C. The EU'S AI act: a framework for collaborative governance. Int Things. (2024) 27:101291. doi: 10.1016/j.iot.2024.101291
55. Ali, T, Al-Khalidi, M, and Al-Zaidi, R. Information security risk assessment methods in cloud computing: comprehensive review. J Comput Inf Syst. (2024) 22:1–28. doi: 10.1080/08874417.2024.2329985
56. Stamate, A, Marzan, M-D, Velciu, M, Paul, C, and Spiru, L. Advancing user-centric design and technology adoption for aging populations: a multifaceted approach. Front Public Health. (2024) 12:1469815. doi: 10.3389/fpubh.2024.1469815
57. Marko, JGO, Neagu, CD, and Anand, PB. Examining inclusivity: the use of AI and diverse populations in health and social care: a systematic review. BMC Med Inform Decis Mak. (2025) 25:57. doi: 10.1186/s12911-025-02884-1
58. Estrela, M, Semedo, G, Roque, F, Ferreira, PL, and Herdeiro, MT. Sociodemographic determinants of digital health literacy: a systematic review and meta-analysis. Int J Med Inform. (2023) 177:105124. doi: 10.1016/j.ijmedinf.2023.105124
59. Crossnohere, NL, Anderson, N, Baumhauer, J, Calvert, M, Esparza, R, Gulbransen, S, et al. A framework for implementing patient-reported outcomes in clinical care: the PROTEUS-practice guide. Nat Med. (2024) 30:1519–20. doi: 10.1038/s41591-024-02909-8
60. Lin, C-H, Zhou, K, Li, L, and Sun, L. Integrating generative AI into digital multimodal composition: a study of multicultural second-language classrooms. Comput Compos. (2025) 75:102895. doi: 10.1016/j.compcom.2024.102895
61. Kirk, HR, Gabriel, I, Summerfield, C, Vidgen, B, and Hale, SA. Why human–AI relationships need socioaffective alignment. Humanit Soc Sci Commun. (2025) 12:728. doi: 10.1057/s41599-025-04532-5
Keywords: DeepSeek, primary care, artificial intelligence, clinical decision support, medical education
Citation: Zhang J, Li D, Wang X, Wu Z and Lyu Q (2025) Application and challenges of DeepSeek in primary care in China. Front. Public Health. 13:1721308. doi: 10.3389/fpubh.2025.1721308
Edited by:
Han Feng, Tulane University, United StatesReviewed by:
Heping Wang, University of Texas MD Anderson Cancer Center, United StatesMichel Abou Khalil, Tulane University, United States
Copyright © 2025 Zhang, Li, Wang, Wu and Lyu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingguo Lyu, bHZxaW5nZ3VvQHdjaHNjdS5lZHUuY24=
†These authors have contributed equally to this work
 Jinyi Zhang
Jinyi Zhang Dong Li
Dong Li Xingyou Wang
Xingyou Wang Zengxiang Wu
Zengxiang Wu Qingguo Lyu
Qingguo Lyu