- 1School of Economics, Faculty of Humanities and Social Sciences, University of Nottingham, Ningbo, China
- 2College of Accounting, Ningbo University of Finance and Economics, Ningbo, China
- 3Kelley School of Business, Indiana University, Bloomington, IN, United States
- 4Department of Applied Health Sciences, University of Birmingham, Birmingham, United Kingdom
- 5Smartsteps Data Technology Co., Ltd., Beijing, China
- 6Nottingham University Business School, University of Nottingham, Ningbo, China
- 7Department of Health Policy and Management, College of Public Health, University of Georgia, Athens, GA, United States
Mobile phone data provide high-resolution, near real-time measurements of population mobility and have become an increasingly valuable source for public health research, enabling rapid evaluation of policy impacts on human movement and pandemic control. However, the methodological challenges surrounding the extraction, governance, and validation of mobile phone data for the public health community remain insufficiently explored. Following the PRISMA-ScR framework, we conduct a scoping review to synthesize major research themes, opportunities, and challenges in the use of mobile phone data for public health, particularly pandemic-related studies. Our findings highlight limitations in the empirical use of these datasets, including demographic and population coverage, representativeness, and equity issues, as well as the transparency of data extraction and processing. We also provide guidance for future research, including the development of standardized frameworks for data curation and validation, a clear understanding of algorithms that extract mobility information, and rigorous interpretation of mobility metrics.
Introduction
Human mobility, the movement of human beings across space and time, is a fundamental determinant of disease transmission and public health dynamics (1, 2). However, measuring and monitoring human mobility has traditionally been challenging due to limited data availability and granularity (3). The widespread use of mobile phones and advances in big data technologies have transformed this landscape, enabling large-scale, near-real-time tracking of human mobility (4), offering insights that were previously unattainable (5). Capturing location information at high spatial and temporal resolutions (6), mobile phone data allows continuous, rapid, and detailed analysis of human behavior far beyond the capacity of traditional survey data (3).
In recent years, mobile phone data have attracted significant attention within the public health community, as they provide valuable information for assessing the impact of health policies and understanding transmission dynamics of infectious diseases (4, 7). They support surveillance, forecasting, and evaluation of pandemics and have been widely used to analyze the effects of Non-Pharmaceutical Interventions (NPIs) on population mobility (8). Diverse analytical perspectives and models have been developed to study human behavior based on spatiotemporal features extracted from various types of mobile phone data, facilitating research on mobility patterns, social networks, disease transmission, and the evaluation of control strategies (5). Despite these advances in mobile phone data, concerns regarding personal privacy, data governance, and methodological challenges persist, alongside the potential for misuse of the data (5, 9).
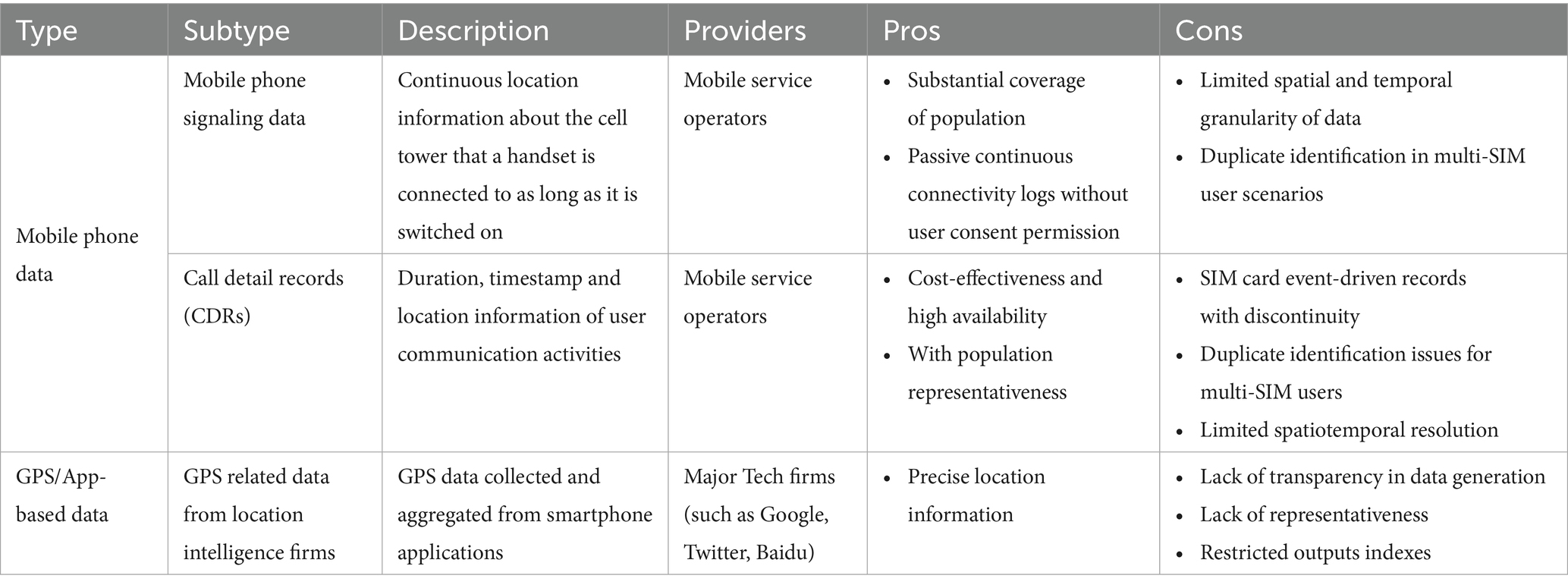
Mobile phone generated data can be broadly categorized into two types based on the source and the method of collection: signaling data (and call detail records, CDRs) generated by phones during communication with cell towers, and GPS/App-based data generated by mobile Apps (Table 1). Mobile phones frequently ping nearby cell towers, leaving a record of the signal data that can be used to triangulate the phone’s location based on antenna connections (10). A key advantage of mobile phone signaling data is that it provides location information as long as the mobile phone is switched on, even if it is not actively being used. CDRs typically contain the user ID, timestamp, and cell tower location associated with calls, texts, or other activities tied to the SIM card (7). In another way, GPS/App-based data generated by Apps such as Google Maps and Baidu Maps, often use global positioning system (GPS) services to record a device’s location over time. GPS/App-based data offer greater accuracy in terms of spatial precision and provide more frequent observations than mobile signaling data (7). However, these data are usually aggregated for privacy protection, often presented as population-level data at specific point-of-interest (POIs) or locations. While GPS/App-based data provide finer location details than mobile phone signaling data, the latter is more representative of the broader population since it is not limited to users of specific applications.
Despite the growing interest in and utilization of mobile phone data in public health, significant methodological challenges are associated with data extraction, data governance, and data quality for mobile phone signaling data (3, 6). While there has been extensive research using mobile phone data, no comprehensive review has focused specifically on the empirical use of mobile phone signaling data in public health. To address this gap, this article conducts a scoping review on the use of mobile phone signaling data in public health. Our review focuses on the mobile phone signaling data, while the GPS/App-based mobile phone data warrants a separate review. We have curated an extensive list of publications on the use of mobile phone data in public health, synthesizing key themes, highlighting both the opportunities and challenges of its application in pandemic response efforts, and suggesting avenues for future research.
Methods
Overview
The scoping review follows the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) guidelines and adopts the Arksey and O’Malley methodology framework (11).
Identifying the research question
The primary aim of this review was to examine the classification, application, and methodological, societal, and data-related challenges and opportunities of the empirical use of mobile phone data in public health. The core research questions are:
(1) How have mobile phone data been used in public health research, specifically for pandemic control?
(2) What are the key opportunities and challenges associated with the use of mobile phone data for public health research?
Identifying relevant studies
The search strategy was developed by WJ, XC, and ZC. We conducted a search across four major citation databases: MEDLINE, PubMed, ScienceDirect, and Web of Science, covering publications in English from January 1, 2012, to June 30, 2024. The search strategy combined keywords related to mobile phone data (“Cell phone” OR “Mobile Phone”) and mobility terms (“Mobility” OR “Flow”) along with the pandemic (“COVID” OR “Pandemic”). The search strategy was refined to ensure comprehensive coverage of relevant themes (see Appendix Table 1 for details).
Study selection
Inclusion criteria of the review were: (1) studies focused on population mobility, human movement, or related patterns; (2) studies clearly described the applications of mobile phone data for illustrating or measuring mobility patterns; (3) studies provided empirical evidence in the context of the pandemic. Two reviewers (XC and WJ) independently conducted the blind review process, screening titles and abstracts to exclude studies that did not pertain to mobility, pandemics, or healthcare utilization, secondary studies (e.g., review articles), theoretical studies without empirical applications, and studies lacking details on data sources. The full texts were assessed by the two reviewers based on the metrics of the mobile phone data and the study outcomes. Discrepancies when there was uncertainty (44%†) or inconsistent decisions (9%†) were resolved by a senior reviewer (ZC).
Charting the data
Data from the included studies were charted by two reviewers (XC and WJ), who identified key characteristics, including study title, research theme, study region, study population, data source, mobility metrics, main outcomes, and study findings. According to scoping review guidelines, no studies were excluded based on quality, as the aim was to identify gaps in the literature rather than assess methodological rigor (11).
Collating, summarizing, and reporting the findings
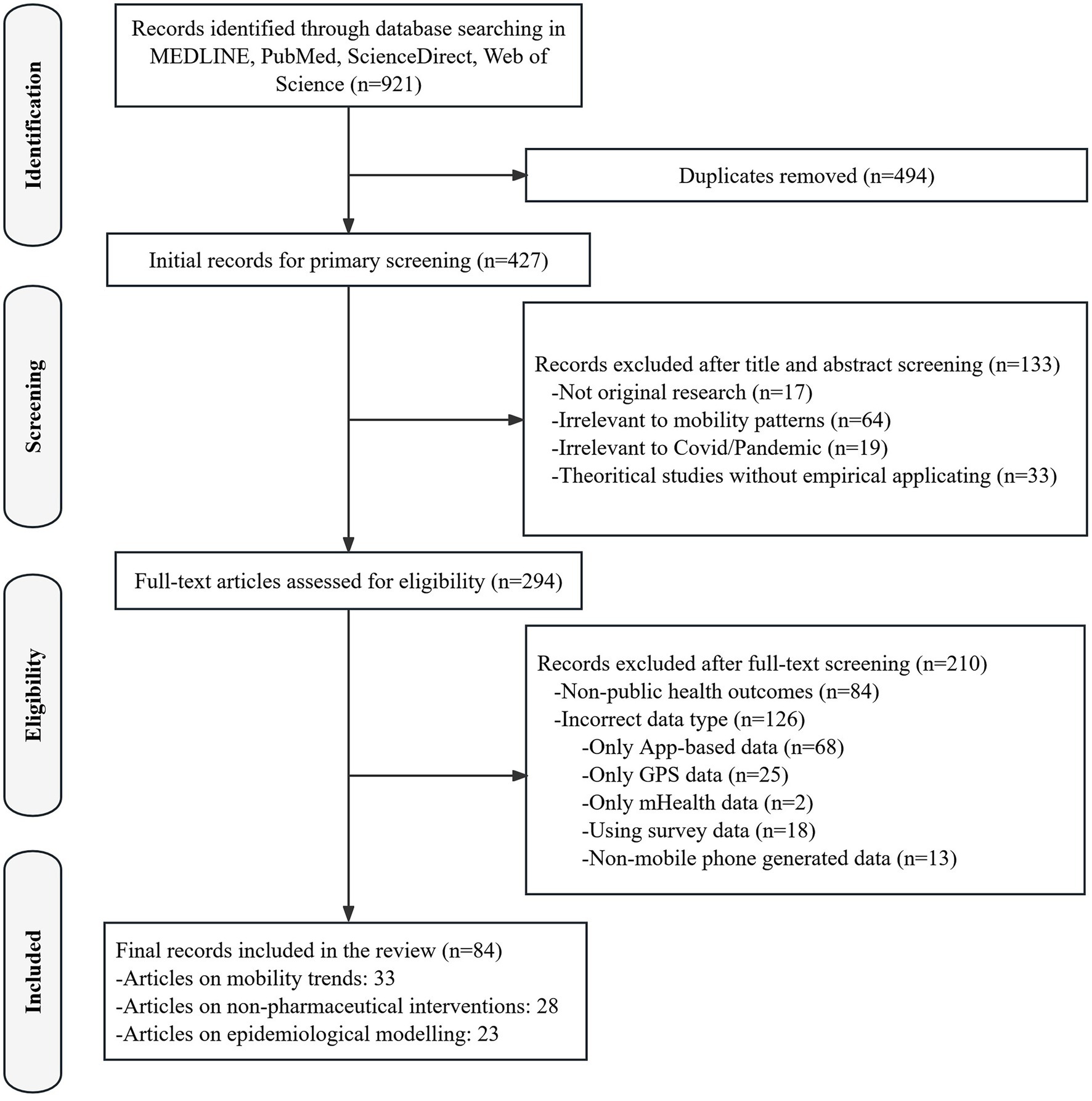
A PRISMA flowchart (Figure 1) was developed to track the selection process. The findings were synthesized to identify key patterns and relationships across studies, and a Sankey diagram was used to visualize the distribution of research themes, mobility metrics, and outcome domains.
Results
Overview
A total of 921 records were retrieved from database searches and imported into a local citation database via Zotero 6.0. After de-duplication, it yielded a list of 427 citations. Following an initial screening of titles and abstracts, 133 citations were excluded due to irrelevance. Among the remaining 294 full-text articles, 210 were excluded because of non-public health outcomes (n = 84) or incorrect data type (n = 126; specific reasons for exclusion are presented in Figure 1). Ultimately, 84 articles met the inclusion criteria and were included in the final review. A narrative and numerical summary of study characteristics was presented and tabulated in the Appendix Table 2. Four key themes with important implications emerged from our review of mobile phone data applications in pandemic control-related research.
Tracking population mobility
A total of 25 studies (30%) focused on analyzing mobility patterns using mobile phone data. Jia and colleagues were the first to use real-time mobile phone data to assess the spatio-temporal dynamics of the COVID-19 spread in China (12). Using national aggregated mobile operator data, Lu et al. established the correlation between population mobility and disease transmission (1). Luo et al. analyzed the mobility patterns among different populations and how they influence the risks of disease transmission (13). Aside from China, an extensive list of research used mobile phone signaling data in public health research exists, analyzing the associations between human mobility and coronavirus spread in the US (14–19), Latin America (20), Ireland (4), Spain (6, 21), Brazil (22), Ecuador (23), Japan (24), Finland (25), and globally (26). However, in the later stages of the pandemic, the association between mobility metrics derived from mobile phone data and COVID-19 incidence growth rates gradually weakened following the lifting of initial stay-at-home orders (27). Other studies explored the socioeconomic impacts of mobility changes, linking mobility data with demographic characteristics (21, 28), economic distress (16), and health outcome indicators (29).
Evaluation of non-pharmaceutical interventions
Thirty-six studies (43%) evaluated the effectiveness of multiple NPIs using mobile phone data, which were adapted as primary measures to restrain the spread of COVID-19 globally before the introduction of effective vaccinations. Many studies assessed social distancing (30–39) and lockdown policies (40–46) across different countries, highlighting their role in mitigating the spread of COVID-19. Research also showed that less aggressive interventions, such as remote working and closures of non-essential businesses, had varied impacts depending on the country (47–54). Notably, a study covering 135 countries found significant reductions in mobility due to travel restrictions during the first wave of the pandemic (55); however, other studies emphasized spontaneous reductions in mobility that occurred regardless of government actions and a ‘floor’ phenomenon (19).
Predictive modeling of disease transmission
Incorporating mobility parameters—either tuned or estimated from mobile phone data—into epidemiological models enhances their ability to simulate outbreak dynamics under varying conditions. A total of 23 studies (27%) integrated mobile phone data into epidemiological models to predict disease spread. These models helped simulate outbreak trajectories in various regions, including Chinese cities and worldwide (56–69). A notable study combined mobile phone data with genomics to track coronavirus variants in Bangladesh, revealing how large-scale human migration from urban to rural areas influenced viral diversity (70). Social factors, such as sociodemographic characteristics, were also examined, showing how mobility differences contributed to infection rates in disadvantaged groups (56, 71). Other researchers highlighted that socioeconomic factors, such as education, household size, and the proportion of the Latinx population, have consistent positive relationships with COVID-19 prevalence over time (72).
Implications for health equity
A sheer body of studies highlighted the potential of mobile phone data to analyze health inequality issues. Research on gender-specific mobility patterns (73), age-group mobility (74–76), and socioeconomic status (SES) (77–79) revealed disparities in COVID-19 transmission risks. Studies also showed that NPIs affected populations and communities differently based on SES, influencing the mobility responses and, consequently, infection rates (44, 80, 81). For instance, using mobility measures derived from mobile phone data, Carranza et al. showed that the impact of NPIs on mobility varied widely across communities, depending on their socioeconomic levels, which also contributes to disparities in infection rates between high- and low-income areas (53).
Discussion
Our scoping review highlights the emerging role of mobile phone signaling data as a valuable alternative for population mobility analysis in public health. The aggregation and analysis of such large-scale, routinely generated data represent a major advancement in digital epidemiology (38). Mobile phone data have increasingly been adopted in modeling population flows, simulating the spatiotemporal transmission dynamics, thereby enhancing the accuracy of risk assessments and informing public health response strategies. More importantly, our review underscores several key considerations and challenges that must be aware to fully realize the potential of mobile phone data in public health.
Measurement of mobility
Mobile phone data enable the measurement of human mobility through diverse metrics, supporting multidisciplinary research. As illustrated in the Sankey diagram (Figure 2), we summarize mobility metrics into four major categories. Population flow metrics, such as origin–destination flow indicators, can track the movement of infected individuals across regions, revealing transmission pathways (1, 6, 62). Population density metrics, including the number of visits or hourly population density to POIs, help evaluate the implementation and effectiveness of pandemic control policies across different population groups (56, 82). Geographical movement indicators, such as the radius of gyration or entropy of movement, can be used to refine epidemiological models and simulate disease transmission (9, 59). Time- or distance-related metrics—such as duration spent at specific locations, distance traveled, travel frequency, and activity space—capture behavioral response to public health interventions (31, 40, 48). Additional information is presented in Appendix Table 3.
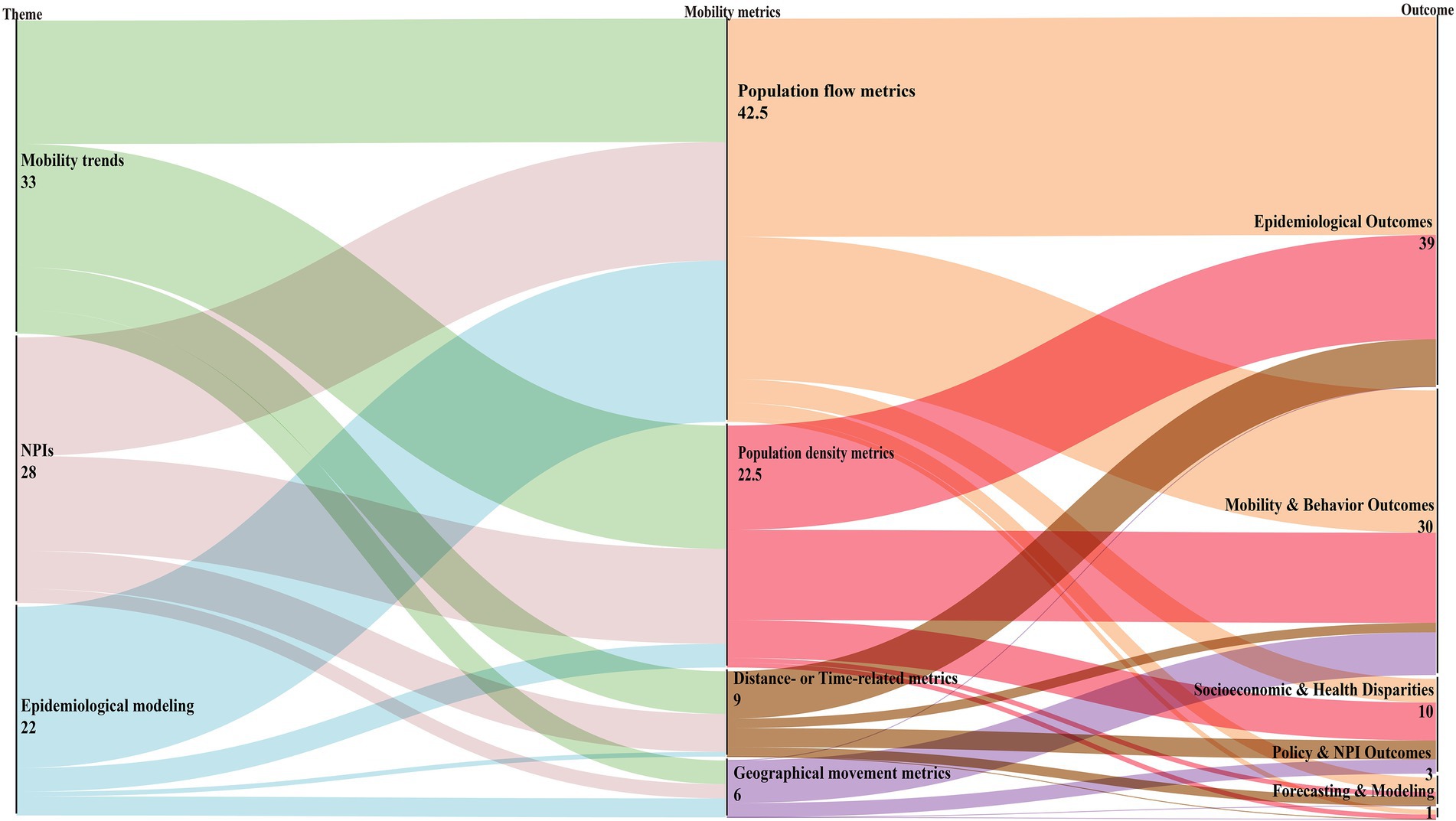
Figure 2. Sankey diagram illustrating the distribution of included studies from research themes (left) through mobility metric classes (middle) to main outcome domains (right). Link widths are proportional to the number of studies. We categorized mobility metrics into four non-exclusive classes: Population flow, Population density, Geographical movement, and Distance/Time. Because individual studies often used multiple classes, we applied fractional counting: if a study used k classes, each Theme-to-Metric link received a weight of 1/k. Duplicates within the same class were counted once per study. For transparency, a full-counting version of metric co-usage is provided in Appendix Table 2.
However, the diversity of mobility metrics also introduces challenges. Comparisons between studies become complicated, and the predictive power of different mobility indicators in empirical models varied substantially across regions and time period (15, 83). The reliability of mobility metrics derived from mobile phone data as proxies for disease transmission is inconsistent, temporally and geographically. For instance, the correlation between alternative mobility metrics and the effective reproductive number of the coronavirus fluctuated during the early stages of COVID-19 (59). These findings underscore the importance for researchers of carefully selecting appropriate mobility indicators and ensuring their robustness when interpreting results or informing health policymaking.
Lack of transparency in data generation
The procedures and algorithms used to collect and process mobile phone raw data are often opaque to public health and social science researchers. Many studies do not provide a detailed description of how the raw data is generated. For example, the frequency of mobile signal pings used to define a device’s location (e.g., every 5 min versus every 10 min) can significantly impact mobility estimates and the inferred effect of interventions (59). Data generation is also influenced by factors such as cell tower distribution and the types of mobile applications used, which can vary from urban to rural areas and across countries (35). This complexity and lack of transparency in data generation hinder the ability to link mobility data to human behavior (59), which may reduce the reliability and trustworthiness of subsequent analyses.
Data privacy
As the large-scale use of mobile phone data becomes more common, protecting individual privacy remains a central concern (84). To minimize privacy risks, data providers often aggregate and preprocess data through methods such as statistical thresholds, differential privacy, and appropriate security controls (35), providing researchers with spatially and temporally aggregated datasets. While these approaches safeguard privacy, they reduce data granularity and can introduce uncertainties in data quality (7), which may limit the comparability and generalizability of results across studies.
Representativeness and equity implications
Mobile phone data enable rapid, large-scale, and context-specific data collection (85), but representativeness requires careful consideration. Representativeness of mobile phone data depends on market share, user demographics, and geographic coverage. Data from a single operator or regions with uneven network coverage may systematically underrepresent children, older adults, and rural or low-income populations, limiting the generalizability of results and potentially biasing conclusions about behavioral responses to NPIs (84–86). During the COVID-19 pandemic, mobility reductions were found to be smaller in low-income communities due to occupational and structural constraints, suggesting that operator coverage biases may distort inferences on health equity and assessments of policy effectiveness (53, 80). To mitigate these issues, recent studies have recommended corrective strategies such as reweighting using census covariates, small-area estimation to improve spatial representativeness, and integrating multiple mobility and demographic data sources (14, 84, 85, 87). Strengthening such representativeness adjustments is crucial to ensure that mobility-derived evidence makes a meaningful contribution to equity-oriented public health research.
Time and spatial scales for aggregation
Selecting the appropriate spatial and temporal scales is critical for striking a balance between privacy protection and analytical utility. Spatial units may include grids or an administrative area, which should reflect population density differences between urban and rural regions. Temporal scales should align with study designs and research objectives; for example, daily measures can better indicate short-term disease transmission, whereas weekly measures can better reflect seasonal or migration patterns (35). Flexible aggregation ensures mobility metrics are informative, actionable, and ethically responsible.
Future research directions
Our review shows that mobile phone data have been extensively used to measure population mobility, model disease transmission, and guide and assess public health interventions for pandemic control. These data offer near-real-time insights into large-scale population behavior, and hold promise for both retrospective and prospective public health analyses (88). However, practical challenges highlighted in our review and previous study (84) underscore the need for cautious and informed application. The following directions may help better harness these data for public health outcomes of interest, enabling a more effective understanding of population behaviors and responses in rapidly changing situations.
Understanding the data generation process
A major challenge is the limited understanding of how these data are collected, processed, and transformed into usable metrics. Current preprocessing methods for mobile phone mobility data often operate as black boxes for researchers, which may lead to biases in analyses with ambiguous directions (84). Researchers must critically examine the assumptions underlying default conditions and thoroughly understand the critical decision rules (35), such as the spatial boundaries of POI, the minimum interactions required to register activity, and the criteria defining “stay” or “pass-by” actions. Transparent reporting of these technical details is crucial for replicating, validating, and scaling findings across academia, industry, and policy contexts. A list of recommended reporting items is in Appendix Table 4.
Exploring more granular data
Current uses of mobile phone datasets are typically anonymized and aggregated to preserve privacy. Although useful for broad mobility trends, such aggregates may be insufficient for targeted public health responses, especially in the post-pandemic era, where sustained surveillance is required (84, 85). In addition, there is a growing need to access finer, sub-population-level mobility data to capture the heterogeneous transmission patterns and disproportionate epidemic burdens, as our review identified. Therefore, there is a need to bolster open discussions and collaborations among mobile operators, policymakers, and researchers to develop frameworks that ensure privacy while enabling legally compliant extraction of detailed, actionable mobility information.
Linkage with other data sources
A new and growing body of literature explores the integration of mobile phone data with complementary datasets, such as census demographics (20, 21, 79), social media (33, 82), internet search volume (16), or genomics (70). With its extensive coverage and spatiotemporal scale, integrating mobile phone data with other data sources can overcome user-based selection bias, provide a more comprehensive picture of population activity (84), and enhance understanding of the profound social and health equity implications. Linking mobility data with socioeconomic and behavioral information at an appropriate geographic scale (e.g., census block group level) enables a more comprehensive view of transmission patterns, disparities, and intervention effectiveness (7), supporting more effective and informed public health decision-making.
Limitations
This review has three main limitations. First, it focuses primarily on the use of mobile phone data for pandemic control, potentially overlooking applications in other public health areas such as influenza or tuberculosis control. Second, the review is limited to English-language health literature, excluding studies published in languages other than English or in engineering and technical fields. Third, mobile phone data also has significant analytical value in other research fields, such as urban planning, emergency evacuation, and economic resilience and forecasting (84), while our review concentrates on public health applications.
Conclusion
Mobile phone data have become an increasingly valuable tool for studying human mobility across multidisciplinary research and practices, as evidenced by the expanding body of literature referring to this data. Our review shows that these data are primarily used to characterize spatial and temporal mobility patterns, assess the role of human movement in disease spread, and perform simulation and predictive modeling of outbreaks. Despite their substantial potential, as we reviewed, challenges remain in ensuring inclusive, transparent, and sustainable use (9). Critical information on user demographics, population coverage, device usage differences, and data processing remains incomplete (59), complicating comparisons across studies and settings. Future work should prioritize validation, standardized frameworks for data curation, and transparent reporting of processing algorithms to strengthen the interpretability and reliability of mobility metrics in public health research.
Author contributions
XC: Data curation, Formal analysis, Software, Validation, Writing – original draft, Writing – review & editing. WJ: Data curation, Methodology, Software, Visualization, Writing – review & editing. SL: Data curation, Methodology, Software, Writing – review & editing. XL: Project administration, Supervision, Validation, Writing – review & editing. YL: Project administration, Supervision, Validation, Writing – review & editing. LL: Supervision, Validation, Writing – review & editing. ML: Project administration, Supervision, Writing – review & editing. XW: Resources, Supervision, Writing – review & editing. YC: Resources, Supervision, Writing – review & editing. AC: Funding acquisition, Project administration, Writing – review & editing. ZC: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the National Natural Science Foundation of China (Grant# 72174098). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
XW and YC are employed by the company Smartsteps Data Technology Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2025.1728985/full#supplementary-material
Abbreviations
NPIs, Non-Pharmaceutical Interventions; PRISMA-ScR, Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews; CDRs, Call Detail Records; GPS, Global Positioning System; POI, Point-of-Interest; SES, Socioeconomic Status.
References
1. Lu, X, Tan, J, Cao, Z, Xiong, Y, Qin, S, Wang, T, et al. Mobile phone-based population flow data for the COVID-19 outbreak in mainland China. Health Data Sci. (2021) 2021:9796431. doi: 10.34133/2021/9796431
2. Barbosa, H, Barthelemy, M, Ghoshal, G, James, CR, Lenormand, M, Louail, T, et al. Human mobility: models and applications. Phys Rep. (2018) 734:1–74. doi: 10.1016/j.physrep.2018.01.001
3. Wu, L, and Shimizu, T. Analysis of the impact of non-compulsory measures on human mobility in Japan during the COVID-19 pandemic. Cities. (2022) 127:103751. doi: 10.1016/j.cities.2022.103751
4. Madden, JM, More, S, Teljeur, C, Gleeson, J, Walsh, C, and McGrath, G. Population mobility trends, deprivation index and the Spatio-temporal spread of coronavirus disease 2019 in Ireland. Int J Environ Res Public Health. (2021) 18:6285. doi: 10.3390/ijerph18126285
5. Okmi, M, Por, LY, Ang, TF, and Ku, CS. Mobile phone data: a survey of techniques, features, and applications. Sensors. (2023) 23:908. doi: 10.3390/s23020908
6. Osorio Arjona, J, and De Las Obras-Loscertales Sampériz, J. Estimation of mobility and population in Spain during different phases of the COVID-19 pandemic from mobile phone data. Sci Rep. (2023) 13:8962. doi: 10.1038/s41598-023-36108-1
7. Yabe, T, Jones, NKW, Rao, PSC, Gonzalez, MC, and Ukkusuri, SV. Mobile phone location data for disasters: a review from natural hazards and epidemics. Comput Environ Urban Syst. (2022) 94:101777. doi: 10.1016/j.compenvurbsys.2022.101777
8. Oliver, N, Oliver, N, and Lepri, B. Mobile phone data for informing public health actions across the COVID-19 pandemic life cycle. Sci Adv. (2020) 6:1–10. doi: 10.1126/sciadv.abc0764
9. Yabe, T, Tsubouchi, K, Fujiwara, N, Wada, T, Sekimoto, Y, and Ukkusuri, SV. Non-compulsory measures sufficiently reduced human mobility in Tokyo during the COVID-19 epidemic. Sci Rep. (2020) 10:18053. doi: 10.1038/s41598-020-75033-5
10. Drane, CR, and Rizos, C. Positioning Systems in Intelligent Transportation Systems Artech House, Inc. (1998).
11. Arksey, H, and O’Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
12. Jia, JS, Lu, X, Yuan, Y, Xu, G, Jia, J, and Christakis, NA. Population flow drives spatio-temporal distribution of COVID-19 in China. Nature. (2020) 582:389–94. doi: 10.1038/s41586-020-2284-y
13. Luo, M, Qin, S, Tan, B, Cai, M, Yue, Y, and Xiong, Q. Population mobility and the transmission risk of the COVID-19 in Wuhan, China. ISPRS Int J Geo Inf. (2021) 10:395. doi: 10.3390/ijgi10060395
14. Gao, S, Rao, J, Kang, Y, Liang, Y, Kruse, J, Dopfer, D, et al. Association of Mobile Phone Location Data Indications of travel and stay-at-home mandates with COVID-19 infection rates in the US. JAMA Netw Open. (2020) 3:e2020485. doi: 10.1001/jamanetworkopen.2020.20485
15. Gatalo, O, Tseng, K, Hamilton, A, Lin, G, and Klein, E. Associations between phone mobility data and COVID-19 cases. Lancet Infect Dis. (2021) 21:E111. doi: 10.1016/S1473-3099(20)30725-8
16. Gimbrone, C, Rutherford, C, Kandula, S, Martínez-Alés, G, Shaman, J, Olfson, M, et al. Associations between COVID-19 mobility restrictions and economic, mental health, and suicide-related concerns in the US using cellular phone GPS and Google search volume data. PLoS One. (2021) 16:e0260931. doi: 10.1371/journal.pone.0260931
17. Paredes, MI, Perofsky, AC, Frisbie, L, Moncla, LH, Roychoudhury, P, Xie, H, et al. Local-scale phylodynamics reveal differential community impact of SARS-CoV-2 in metropolitan US county. PLoS Pathog. (2022) 20:e1012117. doi: 10.1101/2022.12.15.22283536
18. Verma, R, Yabe, T, and Ukkusuri, SV. Spatiotemporal contact density explains the disparity of COVID-19 spread in urban neighborhoods. Sci Rep. (2021) 11:10952. doi: 10.1038/s41598-021-90483-1
19. Xiong, C, Hu, S, Yang, M, Luo, W, and Zhang, L. Mobile device data reveal the dynamics in a positive relationship between human mobility and COVID-19 infections. Proc Natl Acad Sci USA. (2020) 117:27087–9. doi: 10.1073/pnas.2010836117
20. Kephart, JL, Delclòs-Alió, X, Rodríguez, DA, Sarmiento, OL, Barrientos-Gutiérrez, T, Ramirez-Zea, M, et al. The effect of population mobility on COVID-19 incidence in 314 Latin American cities: a longitudinal ecological study with mobile phone location data. Lancet Digit Health. (2021) 3:e716–22. doi: 10.1016/S2589-7500(21)00174-6
21. Levin, R, Chao, DL, Wenger, EA, and Proctor, JL. Insights into population behavior during the COVID-19 pandemic from cell phone mobility data and manifold learning. Nature Computational Sci. (2021) 1:588–97. doi: 10.1038/s43588-021-00125-9
22. Silva, JCS, de Lima Silva, DF, Delgado Neto, A d S, Ferraz, A, Melo, JL, Ferreira Júnior, NR, et al. A city cluster risk-based approach for Sars-CoV-2 and isolation barriers based on anonymized mobile phone users’ location data. Sustain Cities Soc. (2021) 65:102574. doi: 10.1016/j.scs.2020.102574
23. Cuellar, L, Torres, I, and Romero-Severson, E. Assessing the impact of human mobility to predict regional excess death in Ecuador. Sci Rep. (2022) 12:370. doi: 10.1038/s41598-021-03926-0
24. Kawakami, Y, Nojiri, S, Nakamoto, D, Irie, Y, Miyazawa, S, Kuroki, M, et al. Novel indicator for the spread of new coronavirus disease 2019 and its association with human mobility in Japan. Sci Rep. (2023) 13:115. doi: 10.1038/s41598-022-27322-4
25. Willberg, E, Järv, O, Väisänen, T, and Toivonen, T. Escaping from cities during the COVID-19 crisis: using mobile phone data to trace mobility in Finland. ISPRS Int J Geo Inf. (2021) 10:103. doi: 10.3390/ijgi10020103
26. Venter, ZS, Sadilek, A, Stanton, C, Barton, DN, Aunan, K, Chowdhury, S, et al. Mobility in blue-Green spaces does not predict COVID-19 transmission: a global analysis. Int J Environ Res Public Health. (2021) 18:12567. doi: 10.3390/ijerph182312567
27. Gottumukkala, R, Katragadda, S, Bhupatiraju, RT, Kamal, AM, Raghavan, V, Chu, H, et al. Exploring the relationship between mobility and COVID- 19 infection rates for the second peak in the United States using phase-wise association. BMC Public Health. (2021) 21:1669. doi: 10.1186/s12889-021-11657-0
28. Valsecchi, M. Internal migration networks and mortality in home communities: evidence from Italy during the Covid-19 pandemic. Eur Econ Rev. (2021) 140:103890. doi: 10.1016/j.euroecorev.2021.103890
29. Yarmol-Matusiak, EA, Cipriano, LE, and Stranges, S. A comparison of COVID-19 epidemiological indicators in Sweden, Norway, Denmark, and Finland. Scand J Public Health. (2021) 49:69–78. doi: 10.1177/1403494820980264
30. Amiri, A. Role of social distancing in tackling COVID-19 during the first wave of pandemic in Nordic region: evidence from daily deaths, infections and needed hospital resources. Int J Nurs Sci. (2021) 8:145–51. doi: 10.1016/j.ijnss.2021.03.010
31. Badr, HS, Du, H, Marshall, M, Dong, E, Squire, MM, and Gardner, LM. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect Dis. (2020) 20:1247–54. doi: 10.1016/S1473-3099(20)30553-3
32. Barberia, LG, Cantarelli, LGR, de Claro Faria Oliveira, ML, Moreira, N d P, and Costa Rosa, IS. The effect of state-level social distancing policy stringency on mobility in the states of Brazil. Rev Adm Publica. (2021) 55:27–49. doi: 10.1590/0034-761220200549
33. Jeffrey, B, Walters, CE, Ainslie, KEC, Eales, O, Ciavarella, C, Bhatia, S, et al. Anonymised and aggregated crowd level mobility data from mobile phones suggests that initial compliance with COVID-19 social distancing interventions was high and geographically consistent across the UK. Wellcome Open Res. (2020) 5:170. doi: 10.12688/wellcomeopenres.15997.1
34. Khataee, H, Scheuring, I, Czirok, A, and Neufeld, Z. Effects of social distancing on the spreading of COVID-19 inferred from mobile phone data. Sci Rep. (2021) 11:1–9. doi: 10.1038/s41598-021-81308-2
35. Kishore, N, Kiang, MV, and Engø-Monsen, K. Measuring mobility to monitor travel and physical distancing interventions: a common framework for mobile phone data analysis. Lancet Digit Health. (2020) 2:e622–8. doi: 10.1016/S2589-7500(20)30193-X
36. Lyu, Z, and Takikawa, H. The disparity and dynamics of social distancing Behaviors in Japan: investigation of Mobile phone mobility data. JMIR Med Inform. (2022) 10:e31557. doi: 10.2196/31557
37. Sanchez, JN, Reyes, GA, Martinez-Lopez, B, and Johnson, CK. Impact of social distancing on early SARS-CoV-2 transmission in the United States. Zoonoses Public Health. (2022) 69:746–56. doi: 10.1111/zph.12909
38. Szocska, M, Pollner, P, Schiszler, I, Joo, T, Palicz, T, McKee, M, et al. Countrywide population movement monitoring using mobile devices generated (big) data during the COVID-19 crisis. Sci Rep. (2021) 11:5943. doi: 10.1038/s41598-021-81873-6
39. Zhang, L, Darzi, A, Ghader, S, Pack, ML, Xiong, C, Yang, M, et al. Interactive COVID-19 mobility impact and social distancing analysis platform. Transportation Res Record: J Transportation Res Board. (2023) 2677:168–80. doi: 10.1177/03611981211043813
40. Pullano, G, Valdano, E, Scarpa, N, Rubrichi, S, and Colizza, V. Evaluating the effect of demographic factors, socioeconomic factors, and risk aversion on mobility during the COVID-19 epidemic in France under lockdown: a population-based study. Lancet Digital Health. (2020) 2:e638–49. doi: 10.1016/S2589-7500(20)30243-0
41. Pepe, E, Bajardi, P, Gauvin, L, Privitera, F, Lake, B, Cattuto, C, et al. COVID-19 outbreak response, a dataset to assess mobility changes in Italy following national lockdown. Sci Data. (2020) 7:230. doi: 10.1038/s41597-020-00575-2
42. Vinceti, M, Filippini, T, Rothman, KJ, Ferrari, F, Goffi, A, Maffeis, G, et al. Lockdown timing and efficacy in controlling COVID-19 using mobile phone tracking. EClinicalMedicine. (2020) 25:100457. doi: 10.1016/j.eclinm.2020.100457
43. Vinceti, M, Balboni, E, Rothman, KJ, Teggi, S, Bellino, S, Pezzotti, P, et al. Substantial impact of mobility restrictions on reducing COVID-19 incidence in Italy in 2020. J Travel Med. (2022) 29:taac081. doi: 10.1093/jtm/taac081
44. Heiler, G, Hanbury, A, and Filzmoser, P. The impact of COVID-19 on relative changes in aggregated mobility using mobile-phone data. Austrian J Stat. (2023) 52:163–79. doi: 10.17713/ajs.v52i4.1510
45. Campbell, M, Marek, L, Wiki, J, Hobbs, M, Sabel, CE, McCarthy, J, et al. National movement patterns during the COVID-19 pandemic in New Zealand: the unexplored role of neighbourhood deprivation. J Epidemiol Community Health. (2021) 75:903–5. doi: 10.1136/jech-2020-216108
46. Carlitz, RD, and Makhura, MN. Life under lockdown: illustrating tradeoffs in South Africa’s response to COVID-19. World Dev. (2021) 137:105168. doi: 10.1016/j.worlddev.2020.105168
47. Nagata, S, Nakaya, T, Adachi, Y, Inamori, T, Nakamura, K, Arima, D, et al. Mobility change and COVID-19 in Japan: Mobile data analysis of locations of infection. J Epidemiol. (2021) 31:387–91. doi: 10.2188/jea.JE20200625
48. Kamineni, M, Engø-Monsen, K, Midtbø, JE, Forland, F, de Blasio, BF, Frigessi, A, et al. Effects of non-compulsory and mandatory COVID-19 interventions on travel distance and time away from home, Norway, 2021. Eurosurveillance. (2023) 28:2200382. doi: 10.2807/1560-7917.ES.2023.28.17.2200382
49. Gibbs, H, Liu, Y, Abbott, S, Baffoe-Nyarko, I, Laryea, DO, Akyereko, E, et al. Association between mobility, non-pharmaceutical interventions, and COVID-19 transmission in Ghana: a modelling study using mobile phone data. PLOS Global Public Health. (2022) 2:e0000502. doi: 10.1371/journal.pgph.0000502
50. Loisate, S, Mutembo, S, Arambepola, R, Makungo, K, Kabalo, EN, Sinyange, NB, et al. Changes in mobility patterns during the COVID-19 pandemic in Zambia: implications for the effectiveness of NPIs in sub-Saharan Africa. PLOS Glob Public Health. (2023) 3:e0000892. doi: 10.1371/journal.pgph.0000892
51. Dekker, MM, Coffeng, LE, Pijpers, FP, Panja, D, and De Vlas, SJ. Reducing societal impacts of SARS-CoV-2 interventions through subnational implementation. eLife. (2023) 12:e80819. doi: 10.7554/eLife.80819
52. Sabbatini, CE, Pullano, G, Di Domenico, L, Rubrichi, S, Bansal, S, and Colizza, V. The impact of spatial connectivity on NPIs effectiveness. BMC Infect Dis. (2024) 24:21. doi: 10.1186/s12879-023-08900-x
53. Carranza, A, Goic, M, Lara, E, Olivares, M, Weintraub, GY, Covarrubia, J, et al. The social divide of social distancing: shelter-in-place behavior in Santiago during the Covid-19 pandemic. Manag Sci. (2022) 68:2016–27. doi: 10.1287/mnsc.2021.4240
54. Castells-Quintana, D, Herrera-Idárraga, P, Quintero, LE, and Sinisterra, G. Unequal response to mobility restrictions: evidence from COVID-19 lockdown in the city of Bogotá. Spat Econ Anal. (2024) 19:206–24. doi: 10.1080/17421772.2023.2235377
55. Lai, S, Ruktanonchai, NW, Carioli, A, Ruktanonchai, CW, Floyd, JR, Prosper, O, et al. Assessing the effect of global travel and contact restrictions on mitigating the COVID-19 pandemic. Engineering. (2021) 7:914–23. doi: 10.1016/j.eng.2021.03.017
56. Chang, S, Pierson, E, Koh, PW, Gerardin, J, Redbird, B, Grusky, D, et al. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. (2021) 589:82–7. doi: 10.1038/s41586-020-2923-3
57. Guan, G, Dery, Y, Yechezkel, M, Ben-Gal, I, Yamin, D, and Brandeau, ML. Early detection of COVID-19 outbreaks using human mobility data. PLoS One. (2021) 16:e0253865. doi: 10.1371/journal.pone.0253865
58. Kain, MP, Childs, ML, Becker, AD, and Mordecai, EA. Chopping the tail: how preventing superspreading can help to maintain COVID-19 control. Epidemics. (2021) 34:100430. doi: 10.1016/j.epidem.2020.100430
59. Kishore, N, Taylor, AR, Jacob, PE, Vembar, N, Cohen, T, Buckee, CO, et al. Evaluating the reliability of mobility metrics from aggregated mobile phone data as proxies for SARS-CoV-2 transmission in the USA: a population-based study. Lancet Digit Health. (2022) 4:27–36. doi: 10.1016/S2589-7500(21)00214-4
60. Muller, SA, Balmer, M, Charlton, W, Ewert, R, Neumann, A, Rakow, C, et al. Predicting the effects of COVID-19 related interventions in urban settings by combining activity-based modelling, agent-based simulation, and mobile phone data. PLoS One. (2021) 16:e0259037. doi: 10.1371/journal.pone.0259037
61. Villanueva-Miranda, I, Hossain, MS, and Akbar, M “Human mobility driven Modeling of an infectious disease.” In: 2022 IEEE International Conference on Data Mining Workshops (ICDMW) Orlando, FL, USA (2022)
62. Gan, T, Li, W, He, L, and Li, J. Intracity pandemic risk evaluation using mobile phone data: the case of Shanghai during COVID-19. ISPRS Int J Geo Inf. (2020) 9:715. doi: 10.3390/ijgi9120715
63. Huang, Q, Liu, Q, Song, C, Liu, X, Shu, H, Wang, X, et al. Urban spatial epidemic simulation model: a case study of the second COVID-19 outbreak in Beijing, China. Trans GIS. (2022) 26:297–316. doi: 10.1111/tgis.12850
64. Shi, Z, Qian, H, Li, Y, Wu, F, and Wu, L. Machine learning based regional epidemic transmission risks precaution in digital society. Sci Rep. (2022) 12:20499. doi: 10.1038/s41598-022-24670-z
65. Zhou, Y, Xu, R, Hu, D, Yue, Y, Li, Q, and Xia, J. Effects of human mobility restrictions on the spread of COVID-19 in Shenzhen, China: a modelling study using mobile phone data. Lancet Digital Health. (2020) 2:e417–24. doi: 10.1016/S2589-7500(20)30165-5
66. Aràndiga, F, Baeza, A, Cordero-Carrión, I, Donat, R, Martí, MC, Mulet, P, et al. A spatial-temporal model for the evolution of the COVID-19 pandemic in Spain including mobility. Mathematics. (2020) 8:1677. doi: 10.3390/math8101677
67. Brown, TS, Engø-Monsen, K, Kiang, MV, Mahmud, AS, Maude, RJ, and Buckee, CO. The impact of mobility network properties on predicted epidemic dynamics in Dhaka and Bangkok. Epidemics. (2021) 35:100441. doi: 10.1016/j.epidem.2021.100441
68. Schwabe, A, Persson, J, and Feuerriegel, S. “Predicting COVID-19 spread from large-scale mobility data.” Proceedings of the 27th ACM SIGKDD Conference on Knowledge Discovery & Data Mining (2021); 3531–3539.
69. Selinger, C, Choisy, M, and Alizon, S. Predicting COVID-19 incidence in French hospitals using human contact network analytics. Int J Infect Dis. (2021) 111:100–7. doi: 10.1016/j.ijid.2021.08.029
70. Cowley, LA, Afrad, MH, Rahman, SIA, Mamun, MMA, Chin, T, Mahmud, A, et al. Genomics, social media and mobile phone data enable mapping of SARS-CoV-2 lineages to inform health policy in Bangladesh. Nat Microbiol. (2021) 6:1271–8. doi: 10.1038/s41564-021-00955-3
71. Yechezkel, M, Weiss, A, Rejwan, I, Shahmoon, E, Ben-Gal, S, and Yamin, D. Human mobility and poverty as key drivers of COVID-19 transmission and control. BMC Public Health. (2021) 21:1–13. doi: 10.1186/s12889-021-10561-x
72. Kashem, SB, Baker, DM, González, SR, and Lee, CA. Exploring the nexus between social vulnerability, built environment, and the prevalence of COVID-19: a case study of Chicago. Sustain Cities Soc. (2021) 75:103261. doi: 10.1016/j.scs.2021.103261
73. Reisch, T, Heiler, G, Hurt, J, Klimek, P, Hanbury, A, and Thurner, S. Behavioral gender differences are reinforced during the COVID-19 crisis. Sci Rep. (2021) 11:19241. doi: 10.1038/s41598-021-97394-1
74. He, S, Niu, C, Wei, Y, Cai, Y, Zhang, W, Xiao, Y, et al. COVID-19 impacts on cross-border mobility of senior population between Shenzhen and Hong Kong. Front Public Health. (2023) 11:1285288. doi: 10.3389/fpubh.2023.1285288
75. Jiang, W-M, Wen, T-H, Huang, Y-C, Chiou, H-Y, Chen, WJ, Hsiung, CA, et al. Interregional mobility in different age groups is associated with COVID-19 transmission in the Taipei metropolitan area, Taiwan. Sci Rep. (2023) 13:17285. doi: 10.1038/s41598-023-44474-z
76. Xia, J, Yin, K, Yue, Y, Li, Q, Wang, X, Hu, D, et al. Impact of human mobility on COVID-19 transmission according to mobility distance, location, and demographic factors in the Greater Bay Area of China: population-based study. JMIR Public Health Surveill. (2023) 9:e39588. doi: 10.2196/39588
77. Iio, K, Guo, X, Kong, X, Rees, K, and Bruce Wang, X. COVID-19 and social distancing: disparities in mobility adaptation between income groups. Transportation Res Interdis Perspectives. (2021) 10:100333. doi: 10.1016/j.trip.2021.100333
78. Lee, WD, Qian, M, and Schwanen, T. The association between socioeconomic status and mobility reductions in the early stage of England’s COVID-19 epidemic. Health Place. (2021) 69:102563. doi: 10.1016/j.healthplace.2021.102563
79. Lamb, MR, Kandula, S, and Shaman, J. Differential COVID-19 case positivity in new York City neighborhoods: socioeconomic factors and mobility. Influenza Other Respir Viruses. (2021) 15:209–17. doi: 10.1111/irv.12816
80. Gauvin, L, Bajardi, P, Pepe, E, Lake, B, Privitera, F, and Tizzoni, M. Socio-economic determinants of mobility responses during the first wave of COVID-19 in Italy: from provinces to neighbourhoods. J R Soc Interface. (2021) 18:20210092. doi: 10.1098/rsif.2021.0092
81. Yücel, SG, Pereira, RHM, Peixoto, PS, and Camargo, CQ. Impact of network centrality and income on slowing infection spread after outbreaks. Appl Netw Sci. (2023) 8:16. doi: 10.1007/s41109-023-00540-z
82. Liu, Y, Wang, Z, Rader, B, Li, B, Wu, CH, Whittington, JD, et al. Associations between changes in population mobility in response to the COVID-19 pandemic and socioeconomic factors at the city level in China and country level worldwide: a retrospective, observational study. Lancet Digit Health. (2021) 3:E349–59. doi: 10.1016/S2589-7500(21)00059-5
83. Jewell, S, Futoma, J, Hannah, L, Miller, AC, Foti, NJ, and Fox, EB. It’s complicated: characterizing the time-varying relationship between cell phone mobility and COVID-19 spread in the US. NPJ Digital Med. (2021) 4:152. doi: 10.1038/s41746-021-00523-3
84. Okmi, M, Ang, TF, Mohd Zaki, MF, Ku, CS, Phan, KY, Wahyudi, I, et al. Mobile phone network data in the COVID-19 era: a systematic review of applications, socioeconomic factors affecting compliance to non-pharmaceutical interventions, privacy implications, and post-pandemic economic recovery strategies. PLoS One. (2025) 20:e0322520. doi: 10.1371/journal.pone.0322520
85. Grantz, KH, Meredith, HR, Cummings, DAT, Metcalf, CJE, Grenfell, BT, Giles, JR, et al. The use of mobile phone data to inform analysis of COVID-19 pandemic epidemiology. Nat Commun. (2020) 11:4961. doi: 10.1038/s41467-020-18190-5
86. Tizzoni, M, Bajardi, P, Decuyper, A, Kon Kam King, G, Schneider, CM, Blondel, V, et al. On the use of human mobility proxies for modeling epidemics. PLoS Comput Biol. (2014) 10:e1003716. doi: 10.1371/journal.pcbi.1003716
87. Dong, E, Du, H, and Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. (2020) 20:533–4. doi: 10.1016/S1473-3099(20)30120-1
Keywords: mobile phone data, public health, mobile signaling data, population mobility, pandemic
Citation: Cheng X, Jiang W, Liu S, Lou X, Li Y, Liu L, Li M, Wang X, Cen Y, Chong A and Chen Z (2025) Mobile phone data analyses for public health research: a scoping review. Front. Public Health. 13:1728985. doi: 10.3389/fpubh.2025.1728985
Edited by:
Hai-Feng Pan, Anhui Medical University, ChinaReviewed by:
Por Lip Yee, University of Malaya, MalaysiaCopyright © 2025 Cheng, Jiang, Liu, Lou, Li, Liu, Li, Wang, Cen, Chong and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhuo Chen, emh1by5jaGVuQG5vdHRpbmdoYW0uZWR1LmNu; emNoZW4xQHVnYS5lZHU=
 Xuening Cheng
Xuening Cheng Wei Jiang
Wei Jiang Siyi Liu3
Siyi Liu3 Yang Li
Yang Li Molin Li
Molin Li Zhuo Chen
Zhuo Chen