- 1Department of Nutrition and Health, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates
- 2Department of Statistics and Business Analytics, College of Business and Economics, United Arab Emirates University, Al Ain, United Arab Emirates
- 3Department of Food Science, College of Agriculture and Veterinary Medicine, United Arab Emirates University, Al Ain, United Arab Emirates
Introduction: Camel milk, with its resemblance to human milk and therapeutic properties, has potential as a substitute/complementary food for infants. To commercialize camel milk and its products specifically for infants, this research was imperative to explore the knowledge, attitudes, and practices among mothers about the acceptance of camel milk and its products for babies (0–2 years old) in the United Arab Emirates (UAE).
Methods: Using convenience sampling, a bilingual structured questionnaire with Cronbach-alpha-tested reliability of 0.865 was completed by 502 mothers, both UAE Nationals and expatriates.
Results: Results showed an inadequate awareness about exclusive breastfeeding, with only 54.7% aware of its correct duration. However, most participants (59.8%) did not know if it was suitable for use in babies, and 76.1% were not aware of any health benefits associated with its use in babies. Based on a five-point Likert scale (from 0–4), mean score exceeding neutral score of 2 indicated mothers’ positive attitudes toward camel milk and its products: culturally acceptable (2.77) and acceptable to their babies (3.09). Moreover, the current practice of using camel milk as an alternative to human milk was not reported in those mothers who did not breastfeed their babies. Furthermore, mothers’ employment, lower birth order of the babies, mothers’ knowledge about camel milk use for babies, its use in complementary foods, and associated health benefits emerged as factors significantly influencing their decision to use camel milk, its infant formula, and products in complementary feeds for the 0–2 years old babies.
Discussion: Overall, promoting camel milk and its products as a sustainable nutritional alternative for 0–2 years old babies necessitates a multifaceted approach that includes raising awareness and fostering a positive attitude among mothers to support its acceptance. Future research should systematically explore consumer demand, maternal perceptions, and safety considerations, with a focus on establishing evidence-based guidelines for the appropriate use of camel milk products in early childhood nutrition.
1 Introduction
Exclusive breastfeeding for the first 6 months of life is widely recommended due to its unparalleled nutritional and immunological benefits for infants (Dieterich et al., 2013; World Health Organization, and United Nations Children’s Fund, 2020; Meek et al., 2022). Human milk provides a complete source of nutrition tailored to an infant’s needs, containing an ideal balance of proteins, fats, carbohydrates, vitamins, and minerals that support healthy growth and development. Human milk not only meets essential nutrient requirements but also provides antimicrobial, anti-inflammatory, and immunoregulatory components that support immune system development (Meek et al., 2022; Szyller et al., 2024). In the absence of human milk, particularly under circumstances where breastfeeding is not possible due to medical conditions, maternal health concerns, or logistical barriers, alternative feeding options must be considered to ensure infants receive adequate nutrition (Tomori, 2022).
Infant formulas serve as a crucial alternative when breastfeeding is not possible or insufficient, ensuring proper nutrition for infants (Baker and Merritt, 2022). However, their use may lead to potential side effects, particularly in relation to allergies. Early introduction of complementary foods and human milk substitutes before the age of 4–6 months has frequently been linked to an increased risk of food hypersensitivities and other allergic conditions in infants (Vandenplas et al., 2014; Mathias et al., 2019; Wong, 2024). Cow’s milk-based formulas, the most common type, is known to trigger cow’s milk protein allergy (CMPA) in some infants (Edwards and Younus, 2024). Similarly, soy-based formulas, often used as an alternative, may also cause allergies in sensitive infants (Merritt and Jenks, 2004). The risk of developing food allergies later in life is higher in formula-fed infants compared to those exclusively breastfed (Zong et al., 2020). Additionally, the absence of certain immune-boosting components found in breast milk may leave formula-fed infants more susceptible to infections (Shamsia, 2009; Barile and Rastall, 2013). While modern formulas are designed to closely mimic breast milk, they cannot fully replicate its complex composition and adaptive nature, potentially impacting the infant’s gut microbiome and immune system development (Bode, 2015). Therefore, careful consideration and medical guidance are essential when choosing and using infant formulas, especially for infants with a family history of allergies (Koletzko et al., 2012; Vandenplas et al., 2014).
As a result, many infants rely on hypoallergenic formulae, which are specially designed for babies who are allergic to or cannot tolerate standard cow’s milk-based formulas. These formulas contain partially or extensively hydrolysed proteins to minimize allergenic reactions (Koletzko et al., 2012). While hypoallergenic formulas offer substantial benefits for allergic infants, they are associated with certain limitations, such as, they do not replicate the complex immunological properties of breast milk, reduced palatability, high production costs causing financial burden for some families, and some infants can still be allergic to residual protein fragments (American Academy of Pediatrics, 2000; Koletzko et al., 2012; Vandenplas et al., 2014; Zibaee et al., 2015).
These limitations underscore the importance of ongoing research and development of naturally hypoallergenic, nutritionally complete, palatable, affordable, and sustainable infant formula. In line with this, redirecting research efforts toward naturally hypoallergenic sources may lead to the development of more affordable, palatable, and nutritionally balanced alternatives (Nayak et al., 2020). Such sources may include specific plant-based proteins or hypoallergenic animal milk varieties that require minimal processing (EFSA Panel on Dietetic Products and Allergies, 2012; Rubino et al., 2014; Le Roux et al., 2020). This approach could potentially preserve more natural nutrients and bioactive compounds, thereby improving both the nutritional value and acceptability of hypoallergenic options for infants with allergies or intolerance.
In this quest for hypoallergenic alternatives to cow milk, goat and camel milk, have sparked the interest of the scientific community (Nayak et al., 2020; Muthukumaran et al., 2022). These alternative milk sources have unique compositional characteristics and contain bioactive compounds that may contribute to reduced allergenic responses in sensitive individuals. Goat milk, for instance, possesses several distinct features that set it apart from cow’s milk (Albenzio et al., 2012). One of the most notable differences is the size of its fat globules, which are significantly smaller than those found in cow’s milk (Zhao et al., 2022). This structural difference may contribute to improved digestibility, as the smaller fat globules are more easily broken down by digestive enzymes. Additionally, goat milk has a different casein profile compared to cow’s milk, with a higher proportion of β-casein and lower levels of αs1-casein (Xiao et al., 2023). This altered protein composition may result in the formation of softer curds in the stomach, potentially reducing the likelihood of allergic reactions and improving overall digestibility. Similarly, camel milk has attracted recent interest for its potential in managing milk allergies, owing to its distinctive protein profile (Al-Ayadhi and Elamin, 2013; Rubino et al., 2014; Zibaee et al., 2015). Unlike cow’s milk, camel milk lacks the allergenic protein β-lactoglobulin and has a higher proportion of β-casein (65%), which facilitates easier digestion (Konuspayeva et al., 2009; Nayak et al., 2020; Muthukumaran et al., 2022; Zou et al., 2022). Additionally, camel milk is reported to have immune-protective properties, with approximately five times the immunoglobulin content of cow’s milk (Konuspayeva et al., 2007). A recent study highlights camel milk’s suitability for newborn consumption, attributing its benefits to a high water content, unsaturated fatty acids, and vitamin C, as well as its lower lactose and fat content (Algaithi et al., 2022; Mudgil et al., 2022; Zou et al., 2022). Moreover, camel milk contains higher levels of lactoferrin, lysozyme, and vitamin C than cow’s milk, making it a promising alternative for hypoallergenic infant formula (Ali Redha et al., 2022). Its production also requires fewer resources, making it a sustainable solution in regions facing climate-related water scarcity challenges (Chikha and Faye, 2025).
The United Arab Emirates (UAE) is well-positioned to capitalize on the benefits of camel milk, given its strong cultural significance, easy accessibility, and established camel farming industry (Nagy and Juhasz, 2016; Ismail et al., 2022). Further, the COVID-19 pandemic has highlighted concerns regarding food security, sustainable production, and the need to minimize carbon footprints, leading to a growing interest in local products that are responsibly produced and support sustainable agriculture (Nagy et al., 2022). These concerns align with the United Nations Sustainable Development Goals (SDGs), particularly SDG 2 (“Zero Hunger”) and SDG 3 (“Good Health and Well-being”), which emphasize the importance of food security, improved nutrition, and reduced childhood mortality (Gil et al., 2019). Given that the UAE relies on imports for 80–90% of its food supply, there is an urgent need to explore self-sustaining indigenous food production solutions (Pirani and Arafat, 2016; Sundarakani and Ghouse, 2024). Therefore, promoting indigenous, nutrient-rich dietary options, such as camel milk, may support both public health and cultural sustainability.
However, the UAE’s rapid economic and social development has led to dietary transitions, with an increasing reliance on commercialized foods of various ethnic origins (Al Sabbah et al., 2023). Despite being the second-largest producer of camel milk in the Middle East after Saudi Arabia, consumer demand remains limited (Konuspayeva and Faye, 2021; Ismail et al., 2022). A recent study in the UAE reported that only a quarter of adults consume camel milk regularly (Ismail et al., 2022).
Expanding the commercialization of camel milk and locally produced camel milk-based infant formula holds significant potential to enhance national food security and promote infant and paediatric health (Ait El Alia et al., 2025; Chikha and Faye, 2025). However, understanding consumer perceptions is a prerequisite to the successful commercialization of any product. This study therefore explored the knowledge, attitudes, and practices (KAP) of mothers regarding the acceptance of camel milk and its products for babies (0–2 years old) in the UAE.
2 Materials and methods
2.1 Ethical approval
The research protocol was approved by the UAE University (UAEU) Social Sciences Ethics Committee (ERS_2021_8428), in accordance with legal requirements related to ethical principles of research with human participants (Declaration of Helsinki and Belmont Report). All participants provided electronic consent to participate, prior to completing the online survey.
2.2 Study design and participants
This was an observational study with a cross-sectional research design. Data collection took place between January 2022 and March 2022. To elicit information about KAP related to camel milk and its products for 0–2 years old babies, a sample size of 640 mothers from the UAE population was estimated based on the sample size calculation with a 5% margin of error and 95% confidence interval, and a response rate of 60%. Considering the targeted age-group, convenience sampling method was adopted. A total of 584 mothers originally responded. However, after removing the data of those mothers (n = 82) who either did not complete the questionnaire or had erroneous information, data for 502 mothers were used for analysis.
2.3 Questionnaire
A structured bilingual questionnaire was developed for ease of understanding by the participants. The questionnaire was divided into five sections: (1) socio-demographic information of mothers and their babies, including age, nationality, education, employment, number of children, and baby’s age, sex, birth order, and medical conditions (9 items); (2) mothers’ knowledge about infant feeding practices, such as ideal newborn nutrition, exclusive breastfeeding duration, camel milk use, timing of its introduction, and perceived health benefits (7 items); (3) attitudes toward feeding options, including factors influencing camel milk use, preferred sources and forms, and purchasing considerations for camel milk formula (5 items); (4) actual feeding practices, covering breastfeeding status, alternatives used, and reasons for choosing them (3 items); and (5) perceptions of camel milk’s potential contribution to food security in the UAE (2 items).
Knowledge domain items included either binary (Yes/No), or multiple options with one being the most appropriate response. Each of these items were interpreted in the text of the results section in terms of their frequency distribution (N and/or %) for correct awareness. No scoring method was used to calculate their overall knowledge score.
Attitude domain items were evaluated using a five-point Likert scale from 0 to 4. Point 2 was considered as the neutral score. The mean score for each item above the neutral score of 2 indicated a positive attitude. To elaborate,
i. Likert Scale options: Never (0), Rarely (1), Sometimes (2), Often (3), Always (4) were consistently applied to the following items:
-Which of the following milk alternatives you would consider using if you were not able to breastfeed your baby exclusively or partially?
-Which of the following sources of camel milk would you prefer?
-What form would you include camel milk in the diet of your baby?
ii. Likert Scale options: Not important (0), Slightly important (1), Moderately important (2), Important (3), Very important (4) were consistently applied to the following items:
-How the factors listed would influence your above decision?
-How the following factors will affect your choice when buying an infant formula made from camel milk?
Practice domain items included either binary (Yes/No), or multiple options. Each of these items were interpreted in the text of the results section in terms of their frequency distribution (N and/or %) for the mothers’ practices.
The bilingual questionnaire was developed through the standard protocol. The forward and backward translations, conducted by native English and Arabic-speaking experts, were reviewed by five subject-matter experts to assess content validity in terms of relevance and clarity. Based on their feedback, the research team made minor adjustments to ensure conceptual and linguistic equivalence. The revised version was pilot-tested with 10 mothers before finalization. The individual and scale content validity indices ranged between 0.8–1.0 for both- relevance and clarity. The Cronbach’s alpha value of 0.865 indicated excellent internal consistency of the questionnaire.
2.4 Statistical analysis
Data was statistically analyzed using IBM SPSS Statistics version 28 (SPSS Inc., Chicago, IL, United States). Categorical variables for socio-demographic characteristics, knowledge, practices, and perceptions regarding camel milk in promoting food security were expressed in frequencies and percentages. The Wilcoxon Signed Rank Test was used to analyze the attitudes of mothers. This test aimed to determine if the mean score for each option and the average score per question exceeded the neutral score of 2 (Sometimes) or was less than 2 (Never/Rarely) on a scale ranging from 0 (Never) to 4 (Always), as an example. The logistic regression analysis was performed for the use of camel milk-based infant formula on characteristics of participants, mothers’ knowledge, and attitudes about feeding 0-2-year-old babies. Statistical significance was tested at the 0.05 level of significance.
3 Results
3.1 Socio-demographic characteristics of participants
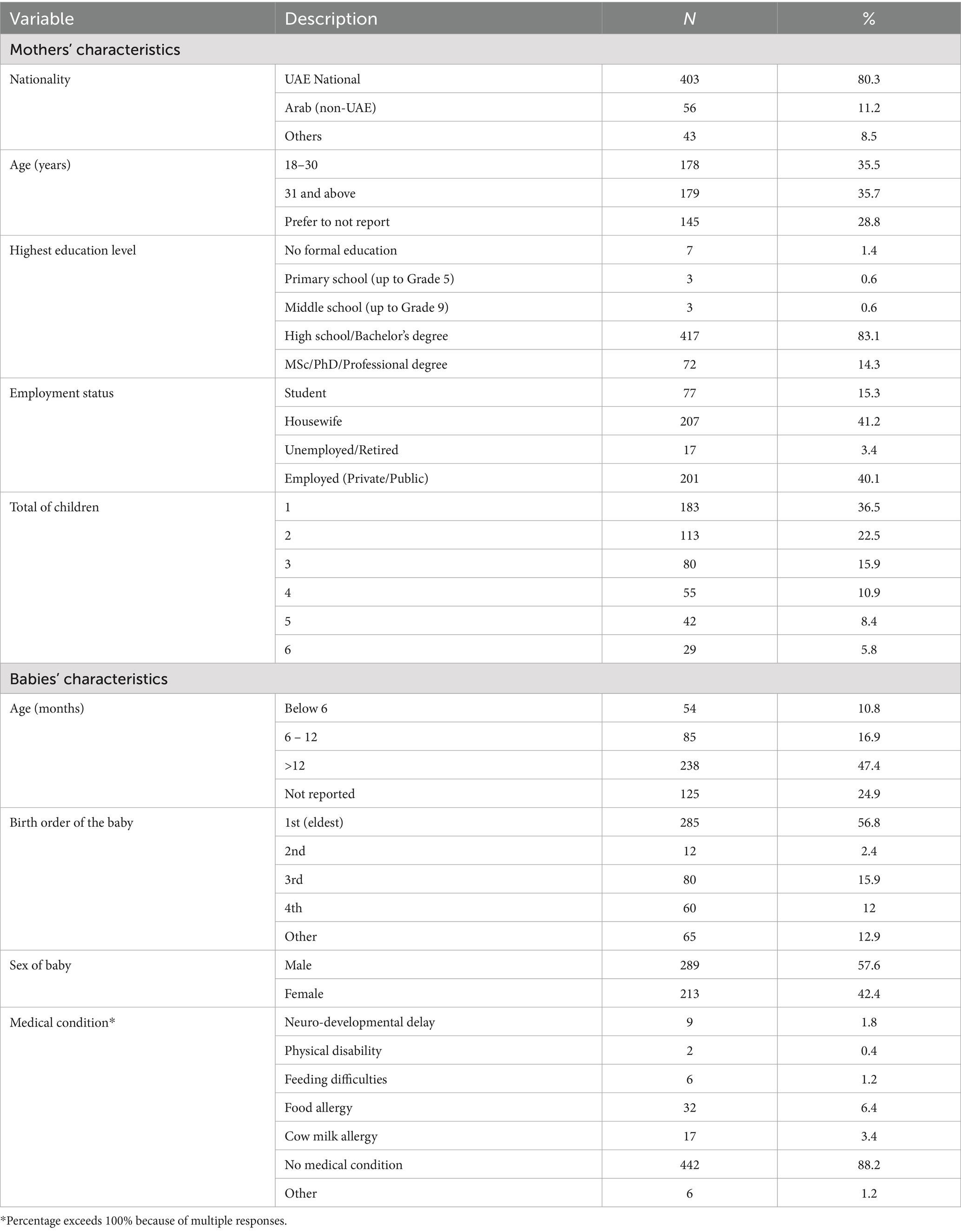
Table 1 shows that the majority of the participants were UAE nationals (80.3%). The mean age of the mothers was 31.03 ± 6.7 years, with almost equal distribution in the age groups of 18–30 years and 31 or above years. Mostly, mothers had completed high school education or a university degree program (97.4%), and almost equal proportions of the mothers were either housewives (41.2%) or employed (40.1%), the remaining 15.3% were students, and 3.4% were retired. Nearly 59.0% of mothers were reported to have 1–2 children during the study period, whereas 41.0% had 3–6 children.
Table 1 also presents the characteristics of babies. Mothers had their last babies either in the age group of 0–12 months (36.8%) or above 12 months (47.4%), although nearly one-fourth of the mothers did not report the age of their babies. Nearly 57% of the 0–2 years old babies were the 1st born to these mothers. More mothers of male (57.6%) than female babies (42.4%) responded to the questionnaire. Most of the babies were not reported to have a diagnosed medical condition (88.2%). However, some mothers reported medically diagnosed conditions in their babies, including food allergies (6.4%) and cow’s milk allergy (3.4%), neuro-developmental delays (1.8%), physical disabilities (0.4%), or other medical conditions not specified by the mothers (1.2%).
3.2 Mothers’ knowledge about feeding 0–2 years old babies
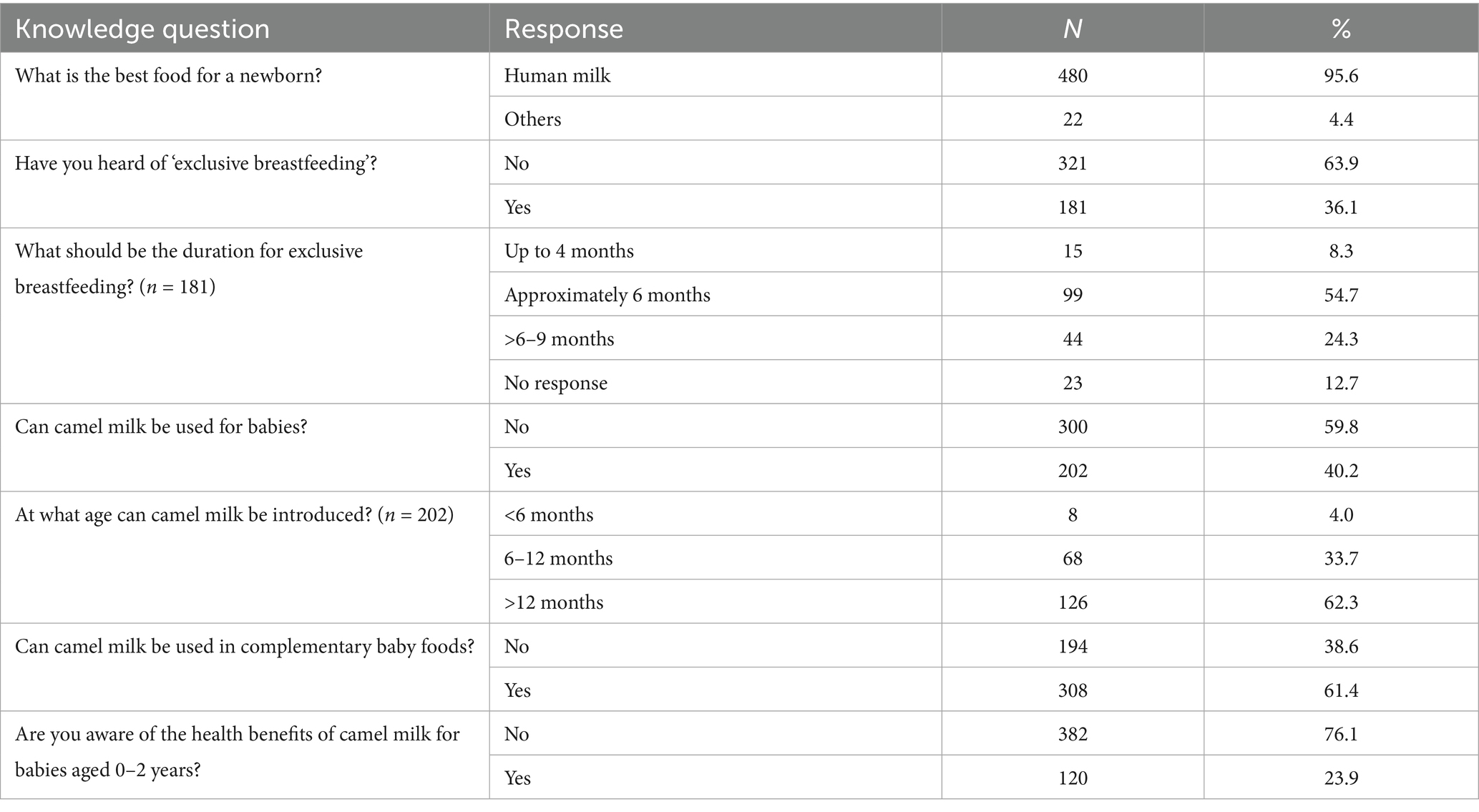
Table 2 illustrates the mothers’ knowledge regarding the feeding of 0–2 years old babies. The first question inquired about the optimal feeding for newborns, with the majority of respondents (95.6%) indicating that human milk is the best choice. The remaining 4.4% of mothers reported alternative options, including specialized/infant formula, and a combination of human milk and infant formula as the best feed for the young babies.
An inadequate awareness level was evident among the mothers for ‘exclusive breastfeeding’, reflected in only 36.1% of mothers, in contrast to 63.9% who knew of ‘exclusive breastfeeding’. From those who had heard (n = 181) of the term, more than half (54.7%) correctly responded that the duration of exclusive breastfeeding should be for approximately 6 months. However, about one-fourth of them (n = 44) considered it to be for 6–9 months, 8.3% for less than 4 months, and 12.7% of the mothers did not respond.
Mixed responses were obtained regarding the mothers’ awareness of using camel milk for babies. Approximately 40.2% (n = 202) of the total respondents considered it suitable, with differing views regarding the recommended age for its introduction to babies. The majority of these mothers (62.3%) believed that camel milk could be introduced only after 12 months of age, followed by 33.7% mothers who considered the appropriate age for introducing camel milk between 6 and 12 months, and a small proportion (4.0%) believed it could be introduced before 6 months. Moreover, out of the 502 mothers, 61.4% of the respondents reported camel milk could be used in complementary baby foods. However, only 23.9% of the total participating mothers were aware of any health benefits of camel milk for babies aged 0–2 years, indicating low awareness among mothers about the importance of camel milk for 0–2 years old babies.
3.3 Mothers’ attitudes toward feeding 0–2 years old babies
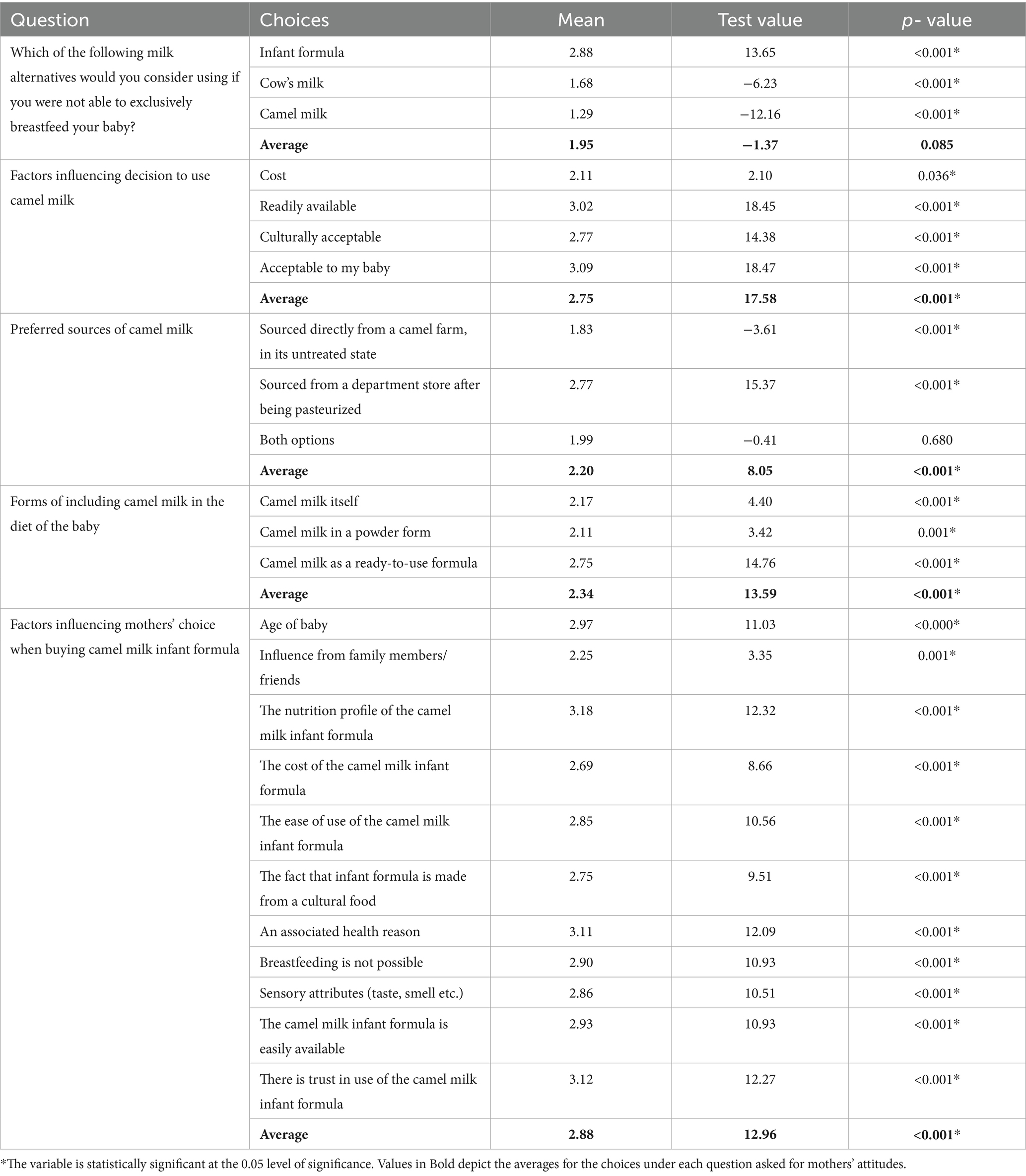
Table 3 presents the attitudes of mothers toward feeding options for 0–2 years old babies. The first question was about the mothers’ views on different milk alternatives if they were not able to exclusively breastfeed their babies. As evident, a mean score of 2.88 and test value of 13.65 (p < 0.001) indicated that mothers had a positive view and significant likelihood of using infant formula as a milk alternative. On the other hand, mothers expressed an unfavorable view and less likelihood of using cow’s milk or camel milk as milk alternatives for 0–2 years old babies. Further, the overall mean score of 1.95 for all milk alternative options indicated that mothers had a generally negative view of milk alternatives as a replacement for human milk, although this trend was not statistically significant (t = −1.37; p = 0.085).
The four factors selected in the study were considered to significantly influence the decisions of mothers for using camel milk for their babies, with mean scores above 2 and p-values <0.001. The factor “Acceptable to my baby” had the strongest preference for responses above 2, followed by being “Readily available,” “Culturally acceptable,” and finally “Cost”.
The mothers significantly preferred sourcing camel milk from a departmental store after pasteurization, with a mean value of 2.77 (t = 15.37; p < 0.001). In contrast, sourcing directly from a camel farm in an untreated state was significantly less preferred with a (mean value of 1.83; t = −3.61; p < 0.001).
Mothers were asked about their likelihood of including camel milk in a baby’s diet in three different forms: camel milk itself, camel milk in a powder form, or camel milk as a ready-to-use formula. Camel milk in a ready-to-use formula was significantly more preferred with a (mean value of 2.75 t = 14.76; p < 0.001), followed by camel milk itself (mean value of 2.17; t = 4.40; p < 0.001), and lastly in powder form (mean value of 2.11; t = 3.42; p = 0.001). The average mean value of 2.34 (t = 13.59; p < 0.001) indicated a preference for including camel milk in a baby’s diet in any form.
Regarding the factors influencing the choice of mothers for buying specifically camel milk infant formula, all 11 factors were significantly favorably responded by the mothers with mean values above 2. The strongest preferences for factors with the highest mean responses above 2, test values, and p-values were less than 0.001: “The nutrition profile of the camel milk infant formula,” “There is trust in use of the camel milk infant formula,” and “An associated health reason”.
3.4 Mothers’ practices toward feeding 0–2 years old babies
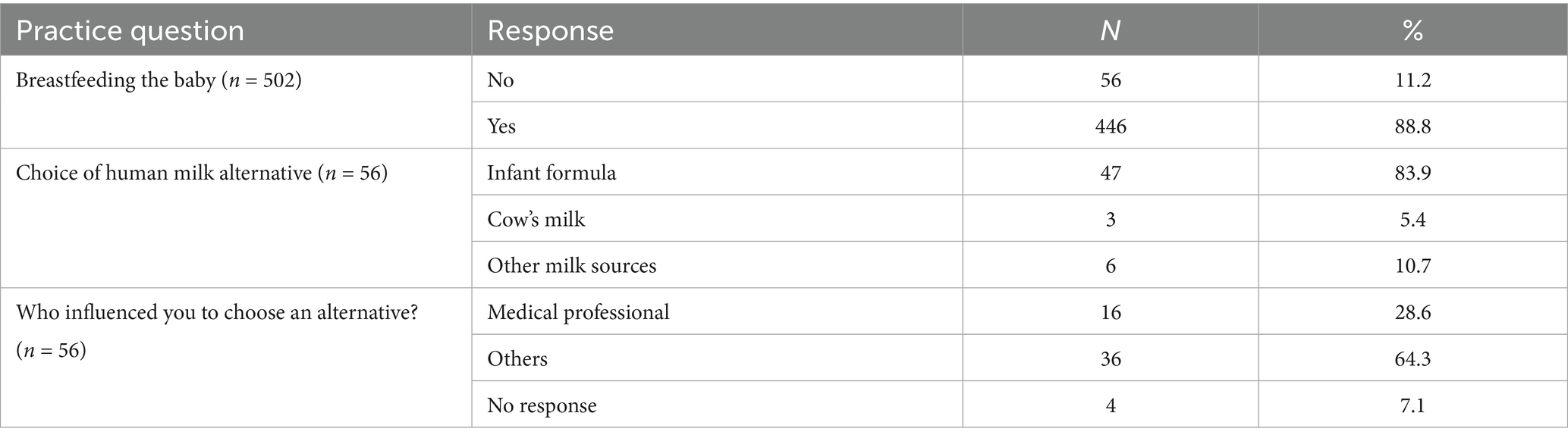
Table 4 provides a summary of survey responses related to the feeding practices adopted by the mothers for their 0–2 years old babies. A large majority of mothers (88.8%) reported breastfeeding their babies. Among the 11.2% (n = 56) who did not, the most commonly used alternative was infant formula (83.9%), followed by unspecified types of milk other than cow’s milk (10.7%), and cow’s milk (5.4%). Only 28.6% of mothers consulted medical professionals in contrast to 64.3% who relied on the advice of others, such as family members/friends, articles, and social media.
3.5 Camel milk and food security
Mothers were asked about their perceptions of the use of camel milk in addressing food security challenges in the context of the UAE. Figure 1 shows that the majority (85.7%) of the mothers believed that camel milk can favorably contribute to the country’s food security, attributed to several reasons by mothers, mainly because camel milk is a “Local ingredient” (66.0%), followed by its “Nutritional content” (60.2%), being “Culturally acceptable” (57.2%), “Readily available” (57.0%) and “Easily accessible,” (52.1%).
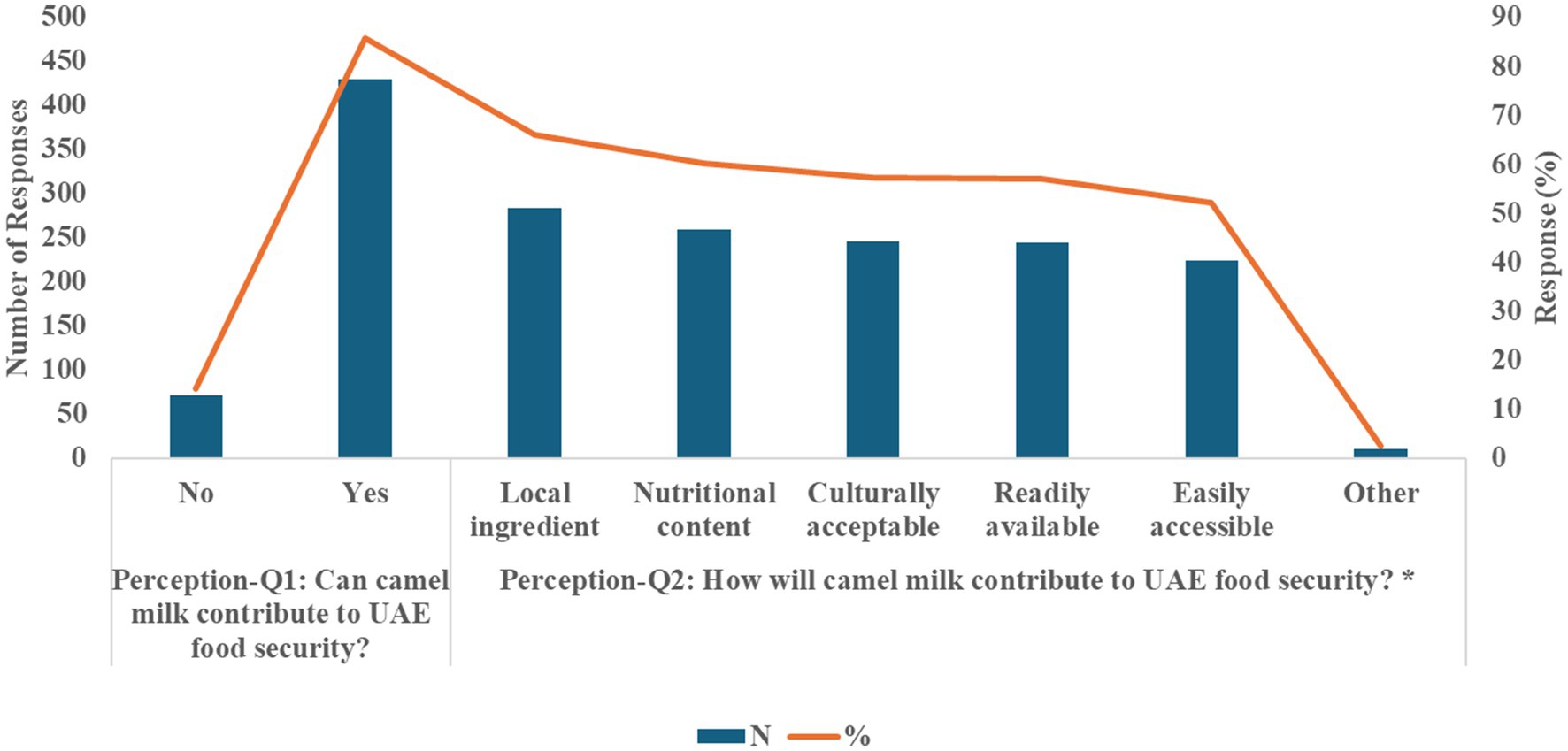
Figure 1. Perceptions of mothers in using camel milk for promoting UAE food security (n = 502). *Total percentage for each question exceeds 100% because of multiple responses.
3.6 Logistic regression analysis for the use of camel milk or infant formula on characteristics of participants, mothers’ knowledge and attitudes about feeding 0–2 years old babies
The logistic regression model goodness-of-fit was evaluated using several criteria. First, the initial classification results without any independent variables included in the model equal 52%, which is the percentage of participants who did not consider camel milk or infant formula. After including independent variables in the logistic regression model, the overall percentage of correctly classified participants in both categories is 80.7%. This accuracy rate is greater than the proportional by chance accuracy criteria of 80.7% (1.25 × 50.1% = 62.6%), indicating that the criteria for classification accuracy are satisfied.
Second, the logistic analysis reveals that the probability of the block chi-square (248.27) was p-value < 0.001, reflecting that the relationship between the independent variables and the dependent variable was supported. Finally, the Nagelkerke R2 method shows that 52.0% of the variation in the dependent variable “Consider using camel milk-based formula” is explained by the independent variables included in the model. All of these criteria provide sufficient evidence to conclude that the model is a good fit.
The logistic regression analysis for the use of camel milk or infant formula made from camel milk on characteristics of participants and mothers’ knowledge and attitudes about feeding 0–2 years old babies is presented in Table 5. Among the variables examined, nationality, sex of babies, number of children, and preferred sources of camel milk were not statistically significant (p > 0.05). On the other hand, mothers’ employment, birth order of the 0–2 years old babies, mothers’ knowledge if camel milk can be used for the babies, camel milk use in complementary foods, knowledge of health benefits associated with camel milk, their views on factors influencing their decision for using camel milk-based infant formula and including camel milk in the complementary feeds of the babies were highly statistically significant (p < 0.05). The details of the significant results are given below.
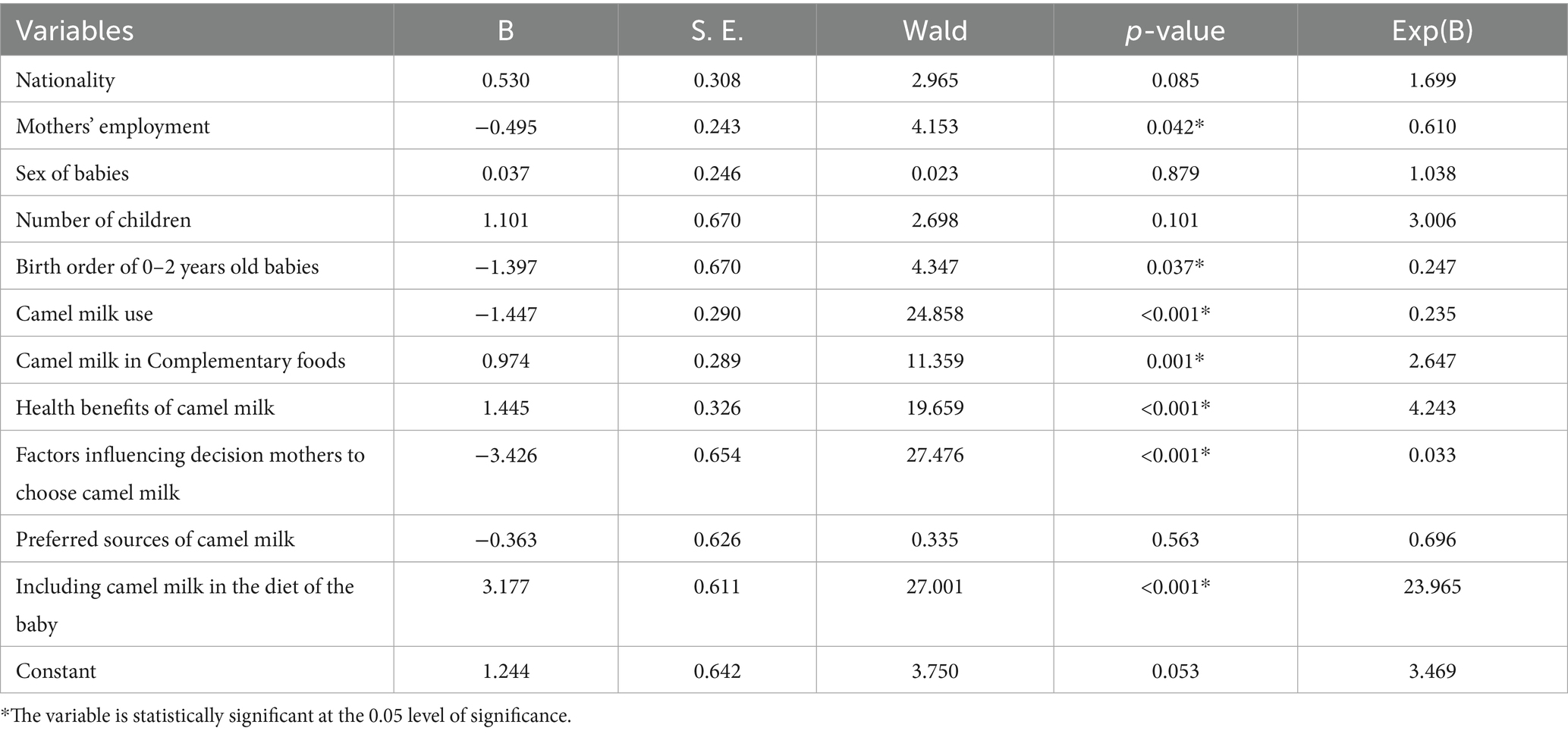
Table 5. The logistic regression analysis for the use of camel milk-based formula on characteristics of participants, mothers’ knowledge and attitudes about feeding 0–2 years old babies (N = 502).
Mothers’ employment had an exponential coefficient of 0.61 (p = 0.042), indicating that employed mothers were 0.61 times less likely to consider camel milk or infant formula compared to unemployed mothers.
In contrast, the birth order of 0–2 years old babies had an exponential coefficient of 0.247 (p-value = 0.037), suggesting that participants with 1–2 birth orders of the babies were 0.247 times less likely to consider camel milk or infant formula compared to those with a higher birth order of children.
Mothers’ knowledge about the use of camel milk for babies had a significant impact on the likelihood of considering camel milk or infant formula. Mothers who were not aware had an exponential coefficient of 0.235 (p < 0.001), implying that they were 0.235 times less likely to consider camel milk or infant formula compared to those who were aware of it. In contrast, those who perceived that camel milk can be used as part of complementary foods had an exponential coefficient of 2.647 (p = 0.001), indicating that they were 2.647 times more likely to consider camel milk or infant formula compared to those who did not.
Knowledge of health benefits associated with giving camel milk to babies had an exponential coefficient of 4.243 (p < 0.001), indicating that mothers who associated benefits with the consumption of camel milk or its formula were 4.243 times more likely to have the outcome compared to those who did not.
The average of factors influencing the mothers’ attitudes toward feeding 0–2 years old babies, such as cost, availability, cultural acceptability, and acceptability to their babies, had a significant impact on whether they considered using camel milk or formula as a substitute or complement to breastfeeding. The exponential coefficient of 0.033 (p < 0.001) indicates that the mothers were 0.033 times less likely to consider these influencing factors when deciding to use camel milk or infant formula.
Furthermore, the average of factors related to including camel milk in the baby’s diet, such as the cost of camel milk itself, in a powder form, or as a ready-to-use formula, had a significant impact on mothers’ decision to consider camel milk or formula. The Exponential coefficient of 23.965 (p < 0.001) indicates that the mothers were 23.97 times more likely to consider including camel milk in their babies’ diet when deciding to use camel milk or infant formula.
4 Discussion
To the best of our knowledge, the present study is one among the first to assess the knowledge, attitudes, and practices among mothers about the acceptance of camel milk and its products for babies (0–2 years old) in the UAE. Overall, the mothers exhibited inadequate knowledge about exclusive breastfeeding, and health benefits of camel milk for 0–2 years old babies, and generally regarded camel milk and its products as unsuitable for infants. Moreover, the current practice of using camel milk as an alternative to human milk was not reported in those mothers who did not breastfeed their babies. Furthermore, mothers’ employment, lower birth order of the babies, mothers’ knowledge about the camel milk use for babies, its use in complementary foods, and associated health benefits emerged as factors significantly influencing their decision for using camel milk, its infant formula, and products in complementary feeds for the 0–2 years old babies.
Camels hold importance to the desert’s ecological system, and their milk contributes to the nutritional needs of those living in arid and semi-arid regions (Shori, 2012). The socioeconomic significance of camel milk has extended to other countries where camels are not a conventional part of the food system, evident in increased global production by 5-fold in the past 60-year period (Mohan et al., 2020; Nagy et al., 2022). Nonetheless, high availability of camel milk in the market is not aligned with its consumption, as recently reported among UAE adults (Ismail et al., 2022). Further, the camel milk products and formula targeting infants are not popular in the UAE market.
It is well-established that human milk is the gold-standard for infant nutrition, providing benefits beyond somatic growth, such as improved cognitive development, chronic disease prevention, and the development and maturation of the immune system (Binns et al., 2016; Martin et al., 2016). However, breastfeeding may not always be possible or solely adequate; in fact, globally, 38% of the infants are exclusively breastfed, making infant formula a necessary and effective substitute (Martin et al., 2016). It is expected that the infant formula market will continue to rapidly expand, with annual growth rates of 7–9%, further boosting the manufacturing of more innovative products with ingredients that confer safety and additional health benefits (Martin et al., 2016; Ahern et al., 2019).
In 2018, a UAE-based company was the first to launch a camel milk formula targeted for children aged 1–3 years, as an alternative for those with CMPA (Cornall, 2018). However, later it was discontinued owing to lesser demand. Additionally, researchers from the UAE have developed and investigated the in-vitro effects of a camel milk-based infant formula and concluded its viability as an option for formulating infant formulas (Algaithi et al., 2022; Mudgil et al., 2022). The present study was therefore conducted to assess the mothers’ knowledge, attitudes, and practices for the acceptability of camel milk and its products for babies’ 0–2 years old babies in the UAE, the findings of which would lay the foundation for investigating the consumer need for commercializing the camel milk-based formula, and its products for infants.
We observed a widespread awareness (95.6%) regarding human milk as the best feed for a baby after birth, and 88.8% of the mothers reported breastfeeding/having breastfed their 0–2 years old babies. On the contrary, a much smaller proportion of mothers (36.1%) had heard about the term exclusive breastfeeding, of whom a little above half (54.7%) correctly responded to a duration of approximately 6 months for exclusive breastfeeding. A systematic review reported an average of 70.9% (3.1 to 100%) of mothers correctly defining exclusive breastfeeding, being commonly misunderstood as not mixing two milks, not offering human milk, and/or the use of water during exclusive breastfeeding (Still et al., 2017). A high rate of initiation of breastfeeding (98%) with only 25% rate of exclusive breastfeeding was earlier reported in the UAE (Radwan, 2013). Data from the Gulf Cooperation Council (GCC) countries also showed that exclusive breastfeeding practices were suboptimal in the region and supplementing breastfeeding with other forms of nutrition was commonly practiced, sometimes as early as the first month of life (Al-Nuaimi et al., 2017). This creates a need to offer safe, sustainable, and viable infant milk alternatives for those mothers who are either not able to or not willing to (knowingly or unknowingly) exclusively breastfeed their young infants.
Secondly, our results indicate that camel milk and its products were generally viewed as unsuitable for babies (59.8%), with the majority (62.3%) supporting its introduction after the first year of life. Participants may have attributed it to the nutritional advice of not introducing cow’s milk before 12 months due to its unsuitability to the infant’s intestines (Bennett et al., 2014; Busnel et al., 2023). However, camel milk can be modified to serve as an alternative infant formula (Algaithi et al., 2022; Mudgil et al., 2022), although further research is required to validate the age and safety of its introduction to 0–2 years old babies. Additionally, nearly three-fourths (76.1%) of our participants were not aware of the health benefits of camel milk and identified key influencing factors to the decision of using camel milk for 0–2 years old babies, including its acceptability for the baby, cost, nutritional profile, associated health benefits, trust in the use of the formula, ready availability, and cultural acceptability.
Demand for camel milk may not be solely driven by the perspective of its use as a food source, as options are already available and accepted in the global market. However, its medicinal value has resulted in a greater willingness to try such products (Mohan et al., 2020). Therefore, awareness of the benefits of the product would be of significance to its acceptability. As mentioned earlier, our results showed a low level of awareness in less than one-fourth of the mothers about the benefits of camel milk for babies 0–2 years old.
Nonetheless, the nutritional profile and associated health benefits of camel milk were ranked highly among the reasons influencing the mothers’ choice for their babies. Similarly, nutritional values and medicinal properties were identified as the top drivers of its consumption among adults in the UAE (Ismail et al., 2022). Further, a study in Kenya showed that camel milk demand was driven by the perceived high nutritional profile, followed by the belief of its superior medicinal properties (Akweya et al., 2012). Our results showed that knowledge of health benefits was associated with a significant 4.2-fold increase in considering camel milk for 0–2 years old babies. Increasing knowledge about the beneficial effects of camel milk was shown to establish demand, and low levels of knowledge may lead to consumers perceiving a risk with buying and using this product (Emukule et al., 2011). Specifically, in a market where more participants are satisfied and not actively searching for an alternative, they need to be convinced of the added health benefits to consider the option of camel milk (Profeta et al., 2022).
This cultural acceptability of camel milk was reflected in our study, as UAE citizens are significantly more likely to consider camel milk. A factor that may influence its acceptability in the region may stem from more religious beliefs and adherence to religious practices, as camel milk is mentioned with its medicinal value in the Quran and sayings from Prophet Muhammad ﷺ (Galali and Al-Dmoor, 2019). Practically, however, it was reportedly consumed in about a quarter of the households and mainly by adults, and rarely given to infants and children in the UAE (Ismail et al., 2022). In another study on school children from grades 4–6 in the UAE, only 9.6% reported drinking camel milk, in comparison to 93.2% who consumed cow’s milk. However, this study was conducted before camel milk was commercially available (Hashim, 2002). Findings from focus groups conducted in non-camel milk producing countries showed that participants were willing to try camel milk despite its unfamiliarity, because of its plausible health characteristics (Profeta et al., 2022).
In our study, the availability of camel milk and in a ready-to-use formula were reported to positively influence the decision to use it. Channels that have been found to increase accessibility and awareness of the availability of these products include supermarkets, cafes, family and friend recommendations, health professionals, and social media advertising (Profeta et al., 2022). The use of multiple channels is recommended as our study found only a small proportion of mothers consulted medical professionals for human milk alternatives, while the majority relied on other sources, including family/friends, social media, and articles.
Mothers reported “acceptable to my baby” as one of the strongest factors affecting their preference for camel milk for their 0–2 years old babies. As infants’ acceptance is critical in decision-making, some negative attributes reported in camel milk include a fatty mouthfeel, aftertaste, saltiness, astringency, fishy flavor and sourness while infant formula with a rich aroma and sweet flavor was considered better accepted (Fleischer et al., 2016; Fazzino and Kong, 2023).
Another important criterion was the source of the camel milk. Our respondents showed a higher preference for pasteurized camel milk, sourced from departmental stores, and had an overall negative attitude toward milk sourced directly from a camel farm. In contrast, a recent UAE survey findings revealed that the adults showed a greater likelihood of obtaining camel milk from a family farm (51.4%) compared to a supermarket (36.4%), possibly due to its affordability and convenience, followed by the farmers’ market (12.1%) (Ismail et al., 2022; Nagy et al., 2022). Although the reason behind the mothers’ preference warrants further investigation, it is plausible that this stemmed from the fact that the question was directed toward newborns and infants, raising concerns about food safety in mothers’ minds.
A social factor influencing the decision was the baby’s birth order. Mothers with children with 1–2 birth orders were less likely to report considering camel milk for their young babies. This factor was not previously studied, but prior breastfeeding experience influenced the mothers’ breastfeeding self-efficacy, and exclusive breastfeeding practices for longer durations (Kramer and Kakuma, 2012). However, first-time mothers reported more breastfeeding problems and were more anxious about insufficient feed intake (Hines et al., 2022; Oktarianita et al., 2024). Additionally, a United States of America national survey showed that mothers were more likely to choose the same feeding method for each child (Taylor et al., 2008).
The current study focused on a relatively unexplored topic, evaluating the factors that influence the acceptability of camel milk and its potential use as an infant formula, in the UAE, where camel husbandry holds cultural significance. Distributing an online questionnaire increased our outreach, inclusive of a diverse population. However, this may have introduced sampling and reporting bias. The cross-sectional design and convenience sampling method limited the establishment of causal relationships and representativeness of the data. Future research should employ cluster-based sampling covering the UAE population based on the rural–urban and camel-rearing areas and non-rearing areas, include both individual surveys and focus group interviews for mixed-methods research analysis for better understanding of perspectives on the socio-cultural factors that influence the decision-making process related to use of camel milk and infant formula for feeding 0–2 years old babies. It would be relevant to conduct economic evaluations for cost-effectiveness and cost–benefit analyses of the sales volume of camel milk as an infant milk compared to other commercial infant formulas for prediction of the viability of camel milk formula and related products for infant nutrition in the UAE market.
Overall, this study lays the groundwork triggering further investigations for developing targeted programs to enhance awareness about camel milk, formulation of commercial camel milk infant formula, and comprehensive analysis of its acceptability and market viability for the 0–2 years old babies. Future research can also be directed to experiment with developing other camel milk-based products targeting young babies, including yogurt, custard, among others.
The inherent hypoallergenic, immune-boosting, and gut health-enhancing properties of camel milk present strong potential for promoting camel milk-based infant formula and related products to diverse populations in the UAE and beyond. Prioritizing clinical trials and comprehensive product analyses is essential to substantiate health benefits and support regulatory approval for nutrition and health claims, thereby enhancing consumer trust. Additionally, food technology innovations should focus on optimizing the sensory qualities of camel milk products, particularly those formulated for babies aged 0–2 years.
Furthermore, the use of camel milk and its products in infant feeding must be grounded in scientific evidence and regulated practices. Public health policy and infant nutrition programs in the UAE should focus on education, regulation, and evidence-based integration to ensure their safe and beneficial use in promoting national food sustainability.
5 Conclusion
This study explored mothers’ knowledge, attitudes, and practices regarding camel milk and its products for 0–2 years old babies. While camel milk holds cultural acceptance, overall knowledge among participants was limited, and most mothers did not consider it suitable for infants under 1 year of age. These findings highlight the need for increased awareness of camel milk’s nutritional and health benefits, particularly among mothers of young children in the UAE. The acceptability of camel milk-based infant formula was shaped by perceived benefits, cultural familiarity, sensory characteristics, cost, and the child’s birth order. Promoting such products will require targeted education campaigns, improvements in sensory appeal, clear nutritional messaging, and accessible pricing strategies. Ultimately, collaboration among researchers, healthcare professionals, and industry stakeholders is essential to position camel milk as a credible and sustainable alternative to conventional cow milk-based infant formulas.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study involving humans was approved by UAEU Social Sciences Ethics Committee (ERS_2021_8428). The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their electronic consent to participate in this study.
Author contributions
MP: Data curation, Methodology, Investigation, Writing – original draft, Writing – review & editing. SS: Data curation, Formal analysis, Software, Writing – review & editing. MoK: Investigation, Writing – original draft, Writing – review & editing. HD: Investigation, Writing – original draft, Writing – review & editing. MuK: Writing – original draft, Writing – review & editing. MA: Investigation, Writing – original draft, Writing – review & editing. HA: Investigation, Writing – original draft, Writing – review & editing. PM: Conceptualization, Visualization, Writing – review & editing, Writing – original draft. SM: Conceptualization, Methodology, Visualization, Writing – review & editing, Writing – original draft. AA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the UAEU-SDGs Research Program 2022 Grant#G00003808.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahern, G. J., Hennessy, A., Ryan, C. A., Ross, R. P., and Stanton, C. (2019). Advances in infant formula science. Annu. Rev. Food Sci. Technol. 10, 75–102. doi: 10.1146/annurev-food-081318-104308
Ait El Alia, O., Zine-Eddine, Y., Chaji, S., Boukrouh, S., Boutoial, K., and Faye, B. (2025). Global camel milk industry: a comprehensive overview of production, consumption trends, market evolution, and value chain efficiency. Small Rumin. Res. 243:107441. doi: 10.1016/j.smallrumres.2025.107441
Akweya, B., Gitao, C., and Okoth, M. (2012). The acceptability of camel milk and milk products from north eastern province in some urban areas of Kenya. Afr. J. Food Sci. 6, 465–473. doi: 10.5897/AJFS10.061
Al Sabbah, H., Assaf, E. A., Al-Jawaldeh, A., Alsammach, A. S., Madi, H., Khamis Al Ali, N., et al. (2023). Nutrition situation analysis in the UAE: a review study. Nutrients 15:363. doi: 10.3390/nu15020363
Al-Ayadhi, L. Y., and Elamin, N. E. (2013). Camel milk as a potential therapy as an antioxidant in autism spectrum disorder (ASD). Evid. Based Complement. Alternat. Med. 2013:602834, 1–8. doi: 10.1155/2013/602834
Albenzio, M., Campanozzi, A., D’apolito, M., Santillo, A., Mantovani, M. P., and Sevi, A. (2012). Differences in protein fraction from goat and cow milk and their role on cytokine production in children with cow's milk protein allergy. Small Rumin. Res. 105, 202–205. doi: 10.1016/j.smallrumres.2012.02.018
Algaithi, M., Mudgil, P., Hamdi, M., Redha, A. A., Ramachandran, T., Hamed, F., et al. (2022). Lactobacillus reuteri-fortified camel milk infant formula: effects of encapsulation, in vitro digestion, and storage conditions on probiotic cell viability and physicochemical characteristics of infant formula. J. Dairy Sci. 105, 8621–8637. doi: 10.3168/jds.2022-22008
Ali Redha, A., Valizadenia, H., Siddiqui, S. A., and Maqsood, S. (2022). A state-of-art review on camel milk proteins as an emerging source of bioactive peptides with diverse nutraceutical properties. Food Chem. 373:131444. doi: 10.1016/j.foodchem.2021.131444
Al-Nuaimi, N., Katende, G., and Arulappan, J. (2017). Breastfeeding trends and determinants: implications and recommendations for gulf cooperation council countries. Sultan Qaboos Univ. Med. J. 17:e155, –e161. doi: 10.18295/squmj.2016.17.02.004
American Academy of Pediatrics (2000). Committee on Nutrition. Hypoallergenic infant formulas. Pediatrics 106, 346–349. doi: 10.1542/peds.106.2.346
Baker, R. D., and Merritt, R. J. (2022). Welcome to a new infant formula. J. Pediatr. Gastroenterol. Nutr. 75, 389–390. doi: 10.1097/MPG.0000000000003572
Barile, D., and Rastall, R. A. (2013). Human milk and related oligosaccharides as prebiotics. Curr. Opin. Biotechnol. 24, 214–219. doi: 10.1016/j.copbio.2013.01.008
Bennett, W. E., Hendrix, K. S., Thompson-Fleming, R. T., Downs, S. M., and Carroll, A. E. (2014). Early cow's milk introduction is associated with failed personal-social milestones after 1 year of age. Eur. J. Pediatr. 173, 887–892. doi: 10.1007/s00431-014-2265-y
Binns, C., Lee, M., and Low, W. Y. (2016). The long-term public health benefits of breastfeeding. Asia Pac. J. Public Health 28, 7–14. doi: 10.1177/1010539515624964
Bode, L. (2015). The functional biology of human milk oligosaccharides. Early Hum. Dev. 91, 619–622. doi: 10.1016/j.earlhumdev.2015.09.001
Busnel, A., Domet, M., Ramchani Ben Othman, K., Desclée De Maredsous, C., Ghomari-Boukhatem, H., Bouchenak, M., et al. (2023). Food consumption, nutritional intakes and the role of milk formulas in nutrient adequacy among young children from birth to 2 years living in urban Algeria. Public Health Nutr. 26, 171–181. doi: 10.1017/S1368980022000957
Chikha, M., and Faye, B. (2025). Camel milk: white gold and its contribution to the sustainable development goals—a review. Outlook Agric. 54, 42–54. doi: 10.1177/00307270251315472
Cornall, J. (2018). Camelicious launches world’s first camel milk based baby formula at GULFOOD. UAE: Dairy Reporter.
Dieterich, C. M., Felice, J. P., O’sullivan, E., and Rasmussen, K. M. (2013). Breastfeeding and health outcomes for the mother-infant dyad. Pediatr. Clin. N. Am. 60, 31–48. doi: 10.1016/j.pcl.2012.09.010
Edwards, C. W., and Younus, M. A. (2024). Cow milk allergy. Treasure Island, FL: StatPearls Publishing.
EFSA Panel on Dietetic Products and Allergies. (2012). Scientific opinion on the suitability of goat milk protein as a source of protein in infant formulae and in follow-on formulae. EFSA Journal 10, 2603.
Emukule, J., Ngigi, M., and Guliye, A. (2011). Analysis of socio-economic factors influencing willingness to pay for camel milk in Nakuru district, Kenya. Religion 13, 7.4.
Fazzino, T. L., and Kong, K. L. (2023). A new paradigm for investigating the etiology of obesity in early childhood: exposure to added sugars and hyper-palatable foods in infancy and dysregulation of food reinforcement processes. Obes. Rev. 24:e13526. doi: 10.1111/obr.13526
Fleischer, D. M., Venter, C., and Vandenplas, Y. (2016). Hydrolyzed formula for every infant. Nestle Nutr Inst Workshop Ser, pp. 51–65.
Galali, Y., and Al-Dmoor, H. (2019). Miraculous properties of camel milk and perspective of modern science. J. Fam. Med. Dis. Prev. 5, 1–7. doi: 10.23937/2469-5793/1510095
Gil, J. D. B., Reidsma, P., Giller, K., Todman, L., Whitmore, A., and Van Ittersum, M. (2019). Sustainable development goal 2: improved targets and indicators for agriculture and food security. Ambio 48, 685–698. doi: 10.1007/s13280-018-1101-4
Hashim, I. (2002). Acceptance of camel milk among elementary school students in Al Ain city, United Arab Emirates. Emir. J. Food Agric. 14, 54–59. doi: 10.9755/ejfa.v14i1.4985
Hines, M., Hardy, N., Martens, A., and Zimmerman, E. (2022). Birth order effects on breastfeeding self-efficacy, parent report of problematic feeding and infant feeding abilities. J. Neonatal Nurs. 28, 16–20. doi: 10.1016/j.jnn.2021.07.003
Ismail, L. C., Osaili, T. M., Mohamad, M. N., Zakaria, H., Ali, A., Tarek, A., et al. (2022). Camel milk consumption patterns and perceptions in the UAE: a cross-sectional study. J. Nutr. Sci. 11:e59. doi: 10.1017/jns.2022.55
Koletzko, S., Niggemann, B., Arató, A., Dias, J., Heuschkel, R., Husby, S., et al. (2012). Diagnostic approach and management of cow's-milk protein allergy in infants and children: ESPGHAN GI committee practical guidelines. J. Pediatr. Gastroenterol. Nutr. 55, 221–229. doi: 10.1097/MPG.0b013e31825c9482
Konuspayeva, G., and Faye, B. (2021). Recent advances in camel milk processing. Animals 11:1045. doi: 10.3390/ani11041045
Konuspayeva, G., Faye, B., and Loiseau, G. (2009). The composition of camel milk: a meta-analysis of the literature data. J. Food Compos. Anal. 22, 95–101. doi: 10.1016/j.jfca.2008.09.008
Konuspayeva, G., Faye, B., Loiseau, G., and Levieux, D. (2007). Lactoferrin and immunoglobulin contents in camel’s milk (Camelus bactrianus, Camelus dromedarius, and hybrids) from Kazakhstan. J. Dairy Sci. 90, 38–46. doi: 10.3168/jds.S0022-0302(07)72606-1
Kramer, M. S., and Kakuma, R. (2012). Optimal duration of exclusive breastfeeding. Cochrane Database Syst. Rev. 2012:3517. doi: 10.1002/14651858.CD003517.pub2
Le Roux, L., Mejean, S., Chacon, R., Lopez, C., Dupont, D., Deglaire, A., et al. (2020). Plant proteins partially replacing dairy proteins greatly influence infant formula functionalities. LWT 120:108891. doi: 10.1016/j.lwt.2019.108891
Martin, C. R., Ling, P.-R., and Blackburn, G. L. (2016). Review of infant feeding: key features of breast milk and infant formula. Nutrients 8:279. doi: 10.3390/nu8050279
Mathias, J. G., Zhang, H., Soto-Ramirez, N., and Karmaus, W. (2019). The association of infant feeding patterns with food allergy symptoms and food allergy in early childhood. Int. Breastfeed. J. 14, 1–12. doi: 10.1186/s13006-019-0241-x
Meek, J. Y., Noble, L., and Breastfeeding, S. O. (2022). Policy statement: breastfeeding and the use of human milk. Pediatrics 150:e2022057988. doi: 10.1542/peds.2022-057988
Merritt, R. J., and Jenks, B. H. (2004). Safety of soy-based infant formulas containing isoflavones: the clinical evidence. J. Nutr. 134, 1220S–1224S. doi: 10.1093/jn/134.5.1220S
Mohan, G., Gupta, V., Raj, A., and Kaur, R. (2020). Consumer acceptance of camel milk in emerging economy. J. Int. Food Agribus. Mark. 32, 54–68. doi: 10.1080/08974438.2018.1549521
Mudgil, P., Baba, W. N., Alneyadi, M., Ali Redha, A., and Maqsood, S. (2022). Production, characterization, and bioactivity of novel camel milk-based infant formula in comparison to bovine and commercial sources. LWT 154:112813. doi: 10.1016/j.lwt.2021.112813
Muthukumaran, M. S., Mudgil, P., Baba, W. N., Ayoub, M. A., and Maqsood, S. (2022). A comprehensive review on health benefits, nutritional composition and processed products of camel milk. Food Rev. Intl. 1, 1–37. doi: 10.1080/87559129.2021.2008953
Nagy, P., and Juhasz, J. (2016). Review of present knowledge on machine milking and intensive milk production in dromedary camels and future challenges. Trop. Anim. Health Prod. 48, 915–926. doi: 10.1007/s11250-016-1036-3
Nagy, P. P., Skidmore, J. A., and Juhasz, J. (2022). Intensification of camel farming and milk production with special emphasis on animal health, welfare, and the biotechnology of reproduction. Anim. Front. 12, 35–45. doi: 10.1093/af/vfac043
Nayak, C., Ramachandra, C., and Kumar, G. (2020). A comprehensive review on composition of donkey milk in comparison to human, cow, buffalo, sheep, goat, camel and horse milk. Mysore J. Agric. Sci. 54:11.
Oktarianita, O., Wulandari, R. D., and Supriyanto, S. (2024). Exploring the determinants of exclusive breastfeeding practices among first-time mothers: a narrative review. Afr. J. Reprod. Health 28, 239–248. doi: 10.29063/ajrh2024/v28i10s.28
Pirani, S. I., and Arafat, H. A. (2016). Interplay of food security, agriculture and tourism within GCC countries. Glob. Food Secur. 9, 1–9. doi: 10.1016/j.gfs.2016.05.002
Profeta, A., Enneking, U., Claret, A., Guerrero, L., and Heinz, V. (2022). Consumer acceptance and preference for camel milk in selected European and Mediterranean countries. Sustain. For. 14:1. doi: 10.3390/su142215424
Radwan, H. (2013). Patterns and determinants of breastfeeding and complementary feeding practices of Emirati mothers in the United Arab Emirates. BMC Public Health 13, 1–11. doi: 10.1186/1471-2458-13-171
Rubino, M., Mazza, G. A., Rubino, S., Mahdi, A. M., Zurlo, F., Dolceamore, R. T., et al. (2014). Camel milk: a possible alternative to infant formulas for patients with allergy to cow milk proteins. Dig. Liver Dis. 46:e116. doi: 10.1016/j.dld.2014.07.136
Shamsia, S. (2009). Nutritional and therapeutic properties of camel and human milks. Int J Genet Mol Biol 1, 52–58.
Shori, A. B. (2012). Comparative study of chemical composition, isolation and identification of micro-flora in traditional fermented camel milk products: gariss, suusac, and shubat. J. Saudi Soc. Agric. Sci. 11, 79–88. doi: 10.1016/j.jssas.2011.12.001
Still, R., Marais, D., and Hollis, J. L. (2017). Mothers’ Understanding of the Term ‘Exclusive Breastfeeding’: A Systematic Review. Matern. Child Nutr. 13:e12336. doi: 10.1111/mcn.12336
Sundarakani, B., and Ghouse, A. (2024). A systematic literature review and bibliometric analysis of Blockchain technology for food security. Food Secur. 13:3607. doi: 10.3390/foods13223607
Szyller, H., Antosz, K., Batko, J., Mytych, A., Dziedziak, M., Wrześniewska, M., et al. (2024). Bioactive components of human milk and their impact on child’s health and development, literature review. Nutrients 16:1487. doi: 10.3390/nu16101487
Taylor, J. S., Geller, L., Risica, P. M., Kirtania, U., and Cabral, H. J. (2008). Birth order and Breastfeeding initiation: results of a National Survey. Breastfeed. Med. 3, 20–27. doi: 10.1089/bfm.2007.0006
Tomori, C. (2022). Overcoming barriers to breastfeeding. Best Pract. Res. Clin. Obstet. Gynaecol. 83, 60–71. doi: 10.1016/j.bpobgyn.2022.01.010
Vandenplas, Y., Abuabat, A., Al-Hammadi, S., Aly, G. S., Miqdady, M. S., Shaaban, S. Y., et al. (2014). Middle east consensus statement on the prevention, diagnosis, and management of cow's milk protein allergy. Pediatr. Gastroenterol. Hepatol. Nutr. 17, 61–73. doi: 10.5223/pghn.2014.17.2.61
Wong, G. W.-K. (2024). Food allergies around the world. Front. Nutr. 11:1373110. doi: 10.3389/fnut.2024.1373110
World Health Organization, and United Nations Children’s Fund (2020). Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: The revised baby-friendly hospital initiative 2018 implementation guidance. Geneva: World Health Organization.
Xiao, T., Zeng, J., Zhao, C., Hou, Y., Wu, T., Deng, Z., et al. (2023). Comparative analysis of protein digestion characteristics in human, cow, goat, sheep, mare, and camel milk under simulated infant condition. J. Agric. Food Chem. 71, 15035–15047. doi: 10.1021/acs.jafc.3c03123
Zhao, L., Wang, J., and Mao, X. (2022). Composition and interfacial properties play key roles in different lipid digestion between goat and cow milk fat globules in vitro. Food Chem. 374:131538. doi: 10.1016/j.foodchem.2021.131538
Zibaee, S., Yousefi, M., Taghipour, A., Kiani, M. A., and Noras, M. R. (2015). Nutritional and therapeutic characteristics of camel milk in children: a systematic review. Electron. Physician 7:1523. doi: 10.19082/1523
Zong, X.-N., Li, H., Wu, H.-H., and Zhang, Y.-Q. (2020). Growth performance comparison of exclusively breastfed infants with partially breastfed and formula fed infants. PLoS One 15:e0237067. doi: 10.1371/journal.pone.0237067
Keywords: camel milk, pediatric, complementary food, infant formula, milk allergy
Citation: Padayachee M, Safi SKH, Kittana M, Al Derei HS, Khajjah M, Aldhanhani MSOK, Alrashedi HMH, Mudgil P, Maqsood S and Attlee A (2025) Is camel milk protein suitable for infants? Understanding mothers’ knowledge, attitudes, and practices. Front. Sustain. Food Syst. 9:1613806. doi: 10.3389/fsufs.2025.1613806
Edited by:
Shalander Kumar, International Crops Research Institute for the Semi-Arid Tropics, IndiaReviewed by:
Eugenia Bezirtzoglou, Democritus University of Thrace, GreeceHeba H. Salama, National Research Centre, Egypt
Ibrahim Bakry, Zagazig University, Egypt
Copyright © 2025 Padayachee, Safi, Kittana, Al Derei, Khajjah, Aldhanhani, Alrashedi, Mudgil, Maqsood and Attlee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amita Attlee, YW1pdGEuYXR0bGVlQHVhZXUuYWMuYWU=
 Morgambal Padayachee
Morgambal Padayachee Samir K. H. Safi
Samir K. H. Safi Monia Kittana
Monia Kittana Hessa Salem Al Derei
Hessa Salem Al Derei Muneera Khajjah
Muneera Khajjah Mozah Salem Obaid Khameis Aldhanhani3
Mozah Salem Obaid Khameis Aldhanhani3 Hessa Mohammed Helal Alrashedi
Hessa Mohammed Helal Alrashedi Priti Mudgil
Priti Mudgil Sajid Maqsood
Sajid Maqsood Amita Attlee
Amita Attlee