- 1Department of Nursing, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China
- 2Department of Geriatrics, Peking Union Medical College, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
- 3Department of Nursing, Sichuan Provincial People's Hospital, Chengdu, China
- 4Department of Nursing, The Second Affiliated Hospital Zhejiang University School of Medicine, Hangzhou, China
- 5Department of Nursing, Tongji Medical College, Tongji Hospital, Huazhong University of Science and Technology, Wuhan, China
- 6Department of Nursing, The Second Affiliated Hospital of Haerbin Medical University, Haerbin, China
- 7Department of Nursing, Qinghai Provincial People's Hospital, Xining, China
- 8Department of Epidemiology and Statistics, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences & School of Basic Medicine, Peking Union Medical College, Beijing, China
Background: Studies that explore the nutritional status, sociodemographic factors, mental health variables, and physical health variables that affect the health-related quality of life (HRQoL) of elderly patients are scarce in China.
Objective: This study aimed to examine the association between health-related quality of life (HRQoL) and nutritional status, sociodemographic characteristics, and health-related variables among Chinese elderly patients.
Materials and Methods: Participants were recruited from six tertiary-level hospitals in six provinces or municipalities/cities throughout China from October 2018 to February 2019: a total of 9,996 participants aged 65 years and older were enrolled. The nutritional status and HRQoL were measured using the Mini Nutritional Assessment—Short Form (MNA-SF) and the EuroQoL Five-Dimension Visual Analog Scale, respectively. BMI was taken using standard measurement protocols. Sociodemographic characteristics included age, sex, education, marital status, ethnicity, smoking, alcohol drinking, and current residence. Mental and physical health variables such as frailty and depression were assessed using validated tested instruments. Multiple linear regression analysis was used to analyze whether the nutritional status, sociodemographic characteristics, and health-related variables were associated with HRQoL.
Results: According to the MNA-SF scores at the 30- and 90-day follow-up, 9.7% and 9.1% of participants were malnourished, respectively. Higher MNA-SF scores were related to higher HRQoL scores in older patients (regression coefficient; 95% confidence interval) both at the 30-day (0.660; 0.499–0.821) and 90-day (0.622; 0.434–0.809) follow-up. However, there were no significant associations between the body mass index values and HRQoL. Sociodemographic characteristics (such as age, smoking, and current residence), physical health variables (frailty, urinary function, defecation function, sleeping condition, and falling accidents in the past 12 months), and mental health variables (depression) were the main factors influencing HRQoL in this group.
Conclusion: There are several factors associated with HRQoL among the population derived from this investigation of a representative sample of the Chinese hospitalized elderly population in tertiary hospitals. These findings could have major importance for the planning of “active aging” policies and programs.
Trial Registration: Chinese Clinical Trial Registry, ChiCTR1800017682, registered August 9, 2018.
Introduction
The aging population is growing rapidly worldwide and looks set to continue to increase even further in the future (1, 2). For example, by 2050, one-fifth of the world's population will be aged 60 years or older, and the proportion of the older population is expected to double from about 11% in 2000 to 22% in 2050 (3). In 2018, the number of Chinese older adults approached 241 million, accounting for 17.2% of the total population, and this figure is expected to approach 480 million by 2050 (1, 4).
Aging in humans may be accompanied by physiological and pathological changes relevant to nutrition, social, psychological, and physical factors, such as weight loss, impaired appetite, depression, and functional disability (5–9). There is growing evidence that malnutrition is a common health problem among older adults in hospital, community, and nursing home settings (5, 10, 11). The burden of malnutrition among the Chinese elderly is serious, and in 2017, for example, malnutrition increased hospital costs by RMB 214 (14% increase) per older adult (12). Also, poor mental health and physical functioning contributes to a progressive decline in health, hindering recovery from illness and leading to increased utilization of health care services and premature institutionalization (6, 13, 14).
Health-related quality of life (HRQoL) is a subjective, multidimensional measure reflecting functional status and emotional and social well-being as well as general health (8, 15). HRQoL has become a main goal in the promotion and development of health among older adults (8, 16, 17). Deterioration of physical functioning can result in difficulties with daily activities including cooking and eating, which may affect nutritional status (2, 4). Malnutrition and declining functional status are two critical factors related to loss of independence with aging (18). Therefore, low HRQoL in older adults can reflect potential health problems contributing to functional disability and dependence as well as a risk of malnutrition (19, 20).
Previous studies have shown a direct association between poor nutritional status and worse HRQoL in some groups, such as adults aged 80 years and older (16). Most previous studies have used differing nutritional screening tools, such as the Mini Nutritional Assessment (MNA) and Malnutrition Universal Screening Tool (MUST) (8, 17), as well as estimated nutritional status and HRQoL in older adults using data from only a single hospital or a smaller sample size (8, 16, 17, 21). Studies conducted in China have explored frailty, depression, and the association between HRQoL and functional abilities among the elderly (22–25), but only a few studies have focused on the association between nutrition and HRQoL among elderly patients. Therefore, studies that explore the sociodemographic factors, nutritional status, mental health variables, and physical health variables that affect the HRQoL of the elderly are scarce in China. To address this issue, we conducted a study designed to examine the association between nutritional status, sociodemographic characteristics, health-related variables, and HRQoL in Chinese elderly patients aged 65 years and above based on a large-scale prospective national survey.
Materials and Methods
Study Design and Participants
The participants were derived from a large-scale cohort study in a representative sample of the Chinese hospitalized elderly population in tertiary hospitals, which is an ongoing survey of the physiological and psychological conditions in elderly patients nationwide (Chinese Clinical Trial Registry number ChiCTR1800017682). The baseline data collected from the period from October 2018 to February 2019 represent the baseline survey data used in this study.
The target population is all older inpatients in tertiary hospitals. Eligible participants were recruited using a two-stage cluster sampling method to ensure the representativeness of the study sample. In the first stage, five provinces and one municipality/city in China (southwest: Sichuan Province; northeast: Heilongjiang Province; south central: Hubei Province; northern: Beijing municipality/city; northwest: Qinghai Province; eastern: Zhejiang Province) were selected. A simple random sampling method was used in this stage. In the second stage, one tertiary hospital was selected in each province or municipality/city: The Peking Union Medical College Hospital (PUMCH), where the author works, as a form of convenience sampling. In addition to this hospital, five other hospitals were selected through simple random sampling. All eligible elderly patients from the surgical, internal medicine, neurology, and orthopedics departments and the intensive care unit (ICU) of the selected hospitals were continuously enrolled.
A sample size of 7,299 can produce a two-sided 95% confidence interval with a tolerance error equal to 0.005 when the predicted prevalence rate is 5% (26). Considering the potential non-response and loss to follow, 10,000 participants will be recruited in this study. The inclusion criteria were as follows: aged 65 years and older; signed the consent form; understood the aims of the study; and with sufficient mental ability to answer the interview questionnaire.
Measurement Instruments
The Mini Nutritional Assessment—Short Form (MNA-SF) is a six-item scale that assesses nutritional risk. Assessment is a validated test with sensitivity and specificity for the diagnosis of malnutrition, especially for the elderly (5). Responses yield a score from 0 to 14 points. The participants were then categorized into normal nutritional status (12–14 points), at risk for malnutrition (8–11 points), or malnourished (0–7 points) (6). The MNA-SF has been validated in the Chinese population and has excellent test characteristics (27).
Weight (in kilograms), height (in centimeters), and body mass index (BMI) were recorded. The participants were weighed in light clothing with the footwear removed. The weight of the participants was measured to the nearest 0.1 kg using digital electronic chair scales and the height to the nearest 1 mm using a portable stadiometer. BMI was calculated by dividing the body weight by the height squared (in kilograms per square meter) (28) and was used to classify participants into groups of emaciation (<18.5 kg/m2), normal (18.5–23.9 kg/m2), overweight (24–27.9 kg/m2), and obesity (≥28 kg/m2) according to the Chinese guidelines for the prevention and control of adult overweight and obesity (29) and the Chinese criteria by the Working Group on Obesity in China (WGOC) (30).
HRQoL was measured using the EuroQoL Five-Dimension Visual Analog Scale (EQ5DVAS), in which the participants were asked to rate their overall health status. Possible scores range from 0 to 100, in which 0 represents the worst imaginable health state and 100 the best imaginable health state (8, 13, 16, 31). This scale has been validated among the Chinese population (32, 33).
Data Collection and Quality Control
The data on nutritional status, sociodemographic characteristics, and health-related variables were collected by 589 well-trained and certified registered nurses who conducted face-to-face questionnaire interviews, health assessment, and physical examinations and reviewed clinical records. To ensure data quality, firstly, the research group developed the project survey manual, operation manual, and training manual. Secondly, a database was built using an electronic data collection (EDC) system to guarantee the accuracy and integrity of the data. Also, to ensure accurate data collection, all nurses received systematic training on completing the case report form (CRF) before they recorded the patients' information daily on the web-based online CRF; they were proficient in the investigation process, the method of using the EDC system, and the application of the depression assessment, frailty assessment, and other health assessment scales. Data on HRQoL were collected at both 30 and 90 days in a telephone follow-up.
Definition of Covariates
We developed a multiple linear regression model including factors potentially associated with HRQoL: age, sex, education, marital status, ethnicity, smoking, alcohol consumption, falling accidents in the past 12 months, sleeping condition, urinary function, defecation function, frailty, depression, and current residence. Sleeping condition, urinary function, and defecation function were dichotomized as normal function or dysfunction. Frailty was assessed using the Frailty Scale (34), with a higher total score indicating a more severely frail condition, which represents frail (3–5), pre-frail (1, 2), and robust (0). The FRAIL scale has been validated for use in older Chinese population (22). Depression assessment was based on the 15-item Geriatric Depression Scale 15 (GDS-15) (35). The total GDS score was the sum of the responses of the 15 depression questions (range, 0–15). If the total GDS score is above 5, the patient was considered as depressed, with a larger GDS-15 score denoting more severe depression. The GDS-15 has been validated for use in Chinese elderly (36).
Statistical Analysis
A descriptive analysis of the participants' characteristics was performed using proportions and measures of central tendency and dispersion, in accordance with the nature of the variables. Normality probability plots showed that the EQ5DVAS scores were normally distributed. Multiple linear regression analysis was used to predict EQ5DVAS scores according to the sociodemographic characteristics, health-related variables, and nutritional status. Variables that were not multicollinear were entered into the multiple linear regression model. Regression coefficients and 95% confidence intervals (CIs) were used to assess the strength of the relationships. All statistical analyses were conducted using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA). Statistical significance was accepted at the level of 0.05.
Ethics
This study received approval from the ethics committee of the Peking Union Medical College Hospital (S-K540). All participants signed a form consenting to participate in this study, which adhered to the principles of the Declaration of Helsinki. The participants and their families were provided detailed information about the aim of the study, the terms of participation in the study, the rights of the participants, and questions to be asked. The interview language used is standard Mandarin/Putonghua. If the participants had specific conditions, such as cognitive decline, the nurse interviewed a legal guardian or representative who took care of him to provide consent to participate in this study. Participants were excluded if they had persistent unconsciousness or were unable to provide ethical consent for their participation and if their caregivers were unable to provide effective information.
Results
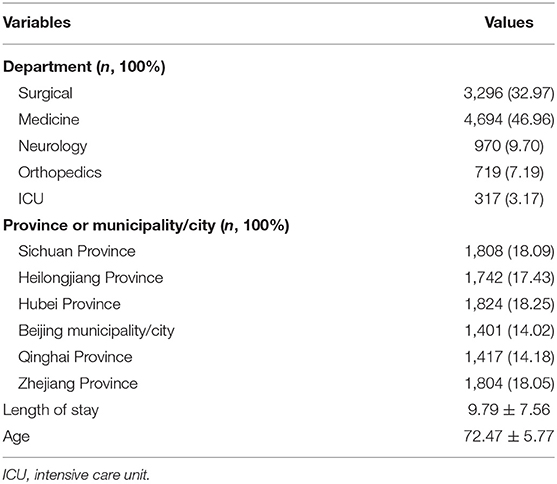
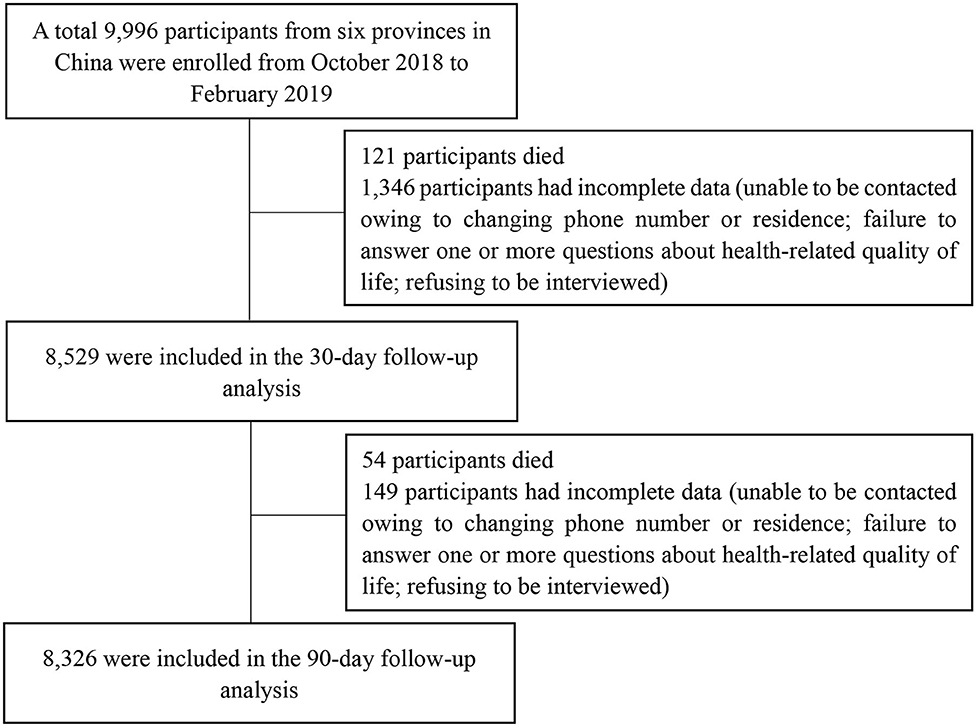
A total of 9,996 elder patients from 314 wards of six hospitals were enrolled in this study. Descriptive statistics and the frequencies of demographics are shown in Table 1. The mean age of this population was 72.47 ± 5.77 years. The average length of stay in the hospital was 9.79 ± 7.56 days. The study flowchart is presented in Figure 1. At the 30-day follow-up, 8,529 (85.3%) participants remained in the study, 121 (1.2%) participants died, and 1,346 (13.5%) had incomplete data (changing phone number or residence permanently, failure to respond to one or more questions about HRQoL, and refusal to be interviewed). At the 90-day follow-up, 8,326 (83.3%) completed the study, 54 (0.5%) participants died, and 149 (1.5%) had incomplete data. At the 30- and 90-day follow-up, the baseline characteristics of those who dropped out of the study (age, sex, frailty, depression, current residence, and nutritional status) did not differ significantly from those who completed it.
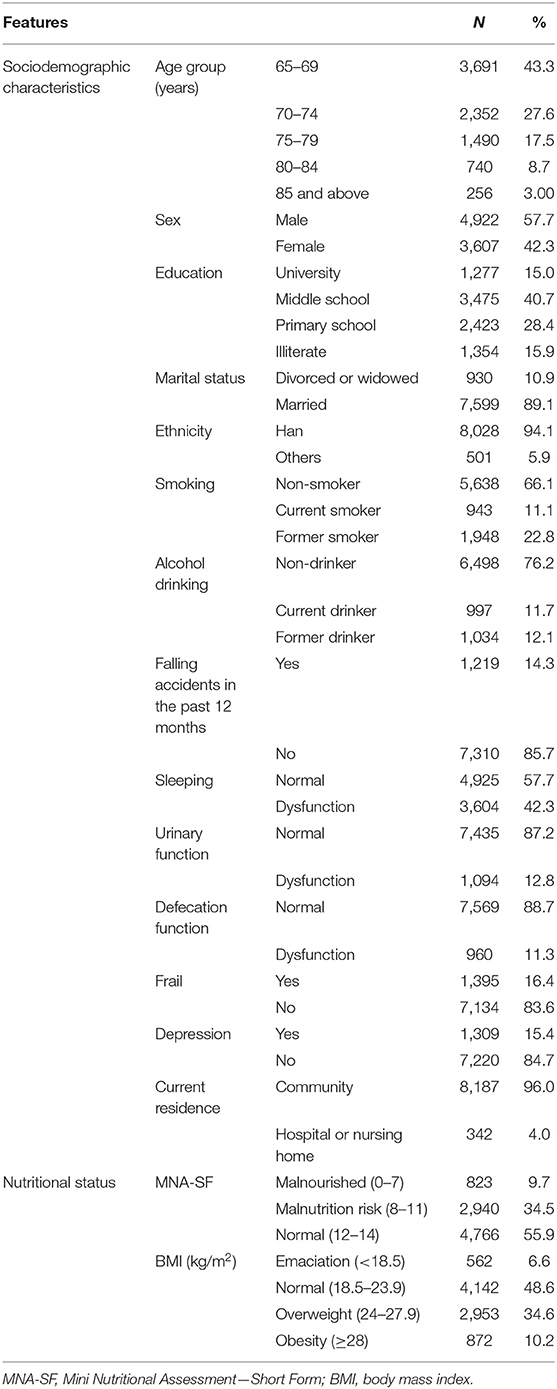
The general characteristics and nutritional status of the participants completing the study at 30-day follow-up are shown in Table 2. A total 56.7% of the participants were aged 70 years and 57.7% were men; 94.1% of the participants were of Han ethnicity. A total 66.1 and 76.2% of the participants were non-smokers and non-drinkers, respectively. A total 14.3% of the participants had a falling accident in the past 12 months, 42.3% had sleeping difficulties, 12.8% had urinary dysfunction, and 11.3% had defecation dysfunction. The prevalence rates of frailty and depression were 16.4 and 15.4%, respectively. The proportion of participants living in the community was 96.0%. According to the MNA-SF scores, 9.7% of the participants were found to be malnourished; only 6.6% were emaciated, according to the BMI values.
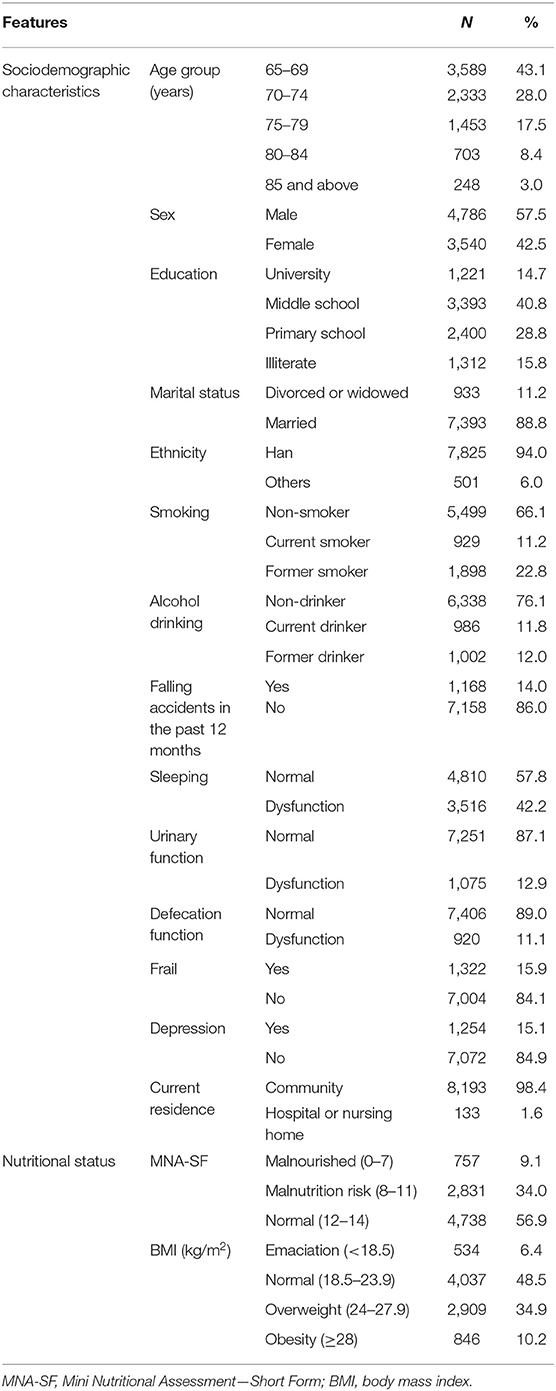
The descriptive characteristics and nutritional status of the participants completing the study at the 90-day follow-up are presented in Table 3. A total 56.9 and 57.5% of the participants were aged 70 years and are males, respectively. In total, 94.0% of the participants were of Han ethnicity; 66.1 and 76.1% were non-smokers and non-drinkers, respectively. Of the participants, 14.0% had a falling accident in the past 12 months. The proportion of participants with sleeping difficulties was 42.2%, those with urinary dysfunction was 12.9%, and the proportion with defecation dysfunction was 11.1%. The prevalence rates of frailty and depression were 15.9 and 15.1%, respectively. The percentage of participants living in the community was 98.4%. In total, 9.1% of the participants were found to be malnourished, according to the MNA-SF scores; only 6.4% were emaciated, according to the BMI values.
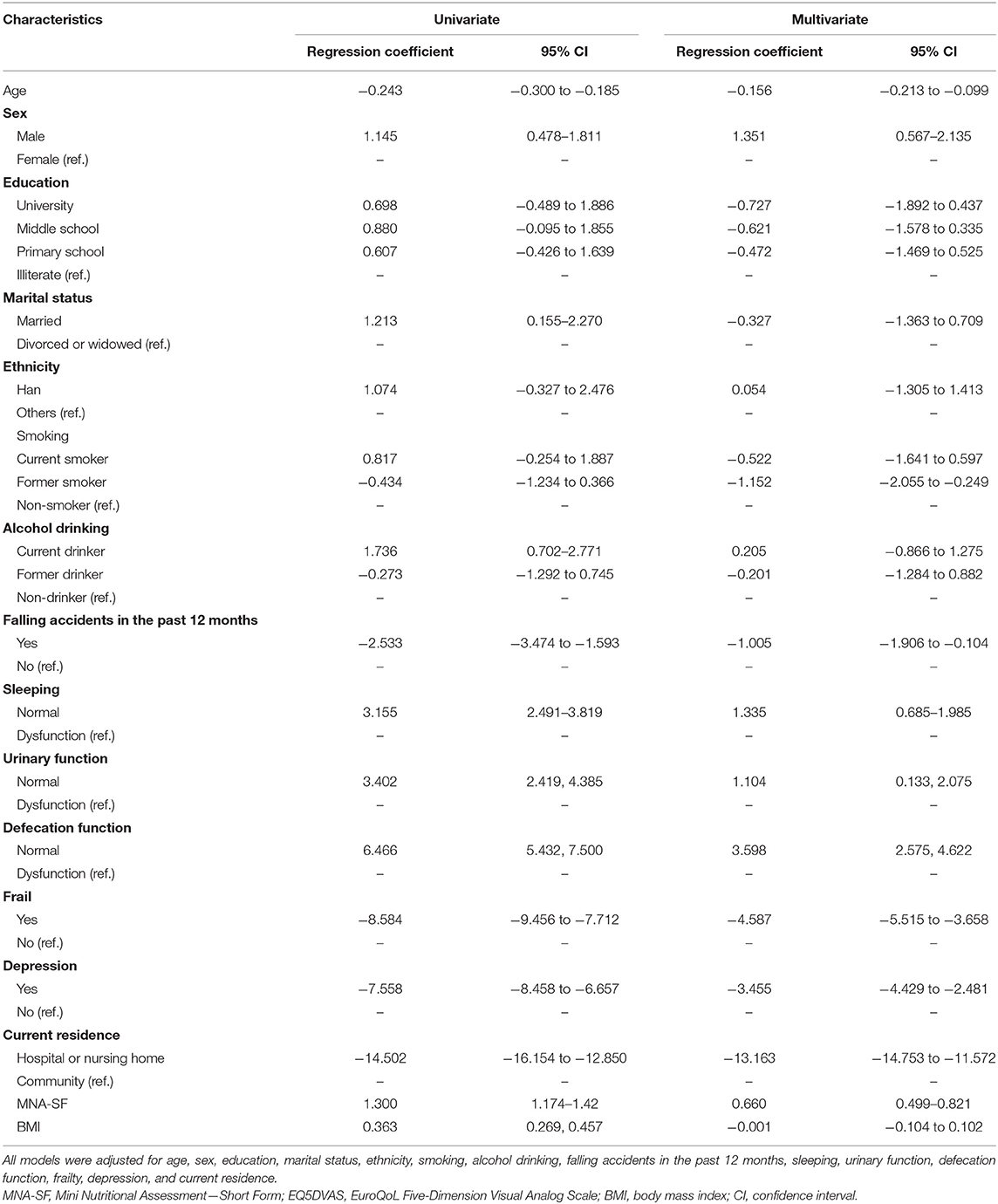
At the 30-day follow-up, male sex (regression coefficient, 1.351; 95% CI, 0.567–2.135), normal sleeping (1.335; 0.685–1.985), normal urinary function (1.104; 0.133–2.075), normal defecation function (3.598; 2.575–4.622), and a higher MNA-SF score (0.660; 0.499–0.821) were associated with higher EQ5DVAS scores in the multiple linear regression model. In contrast, age (−0.156; −0.213 to −0.099), former smoker (−1.152; −2.055 to −0.249), falling accidents in the past 12 months (−1.005; −1.906 to −0.104), frailty (−4.587; −5.515 to −3.658), depression (−3.455; −4.429 to −2.481), and living in a hospital or nursing home setting (−13.163; −14.753 to −11.572) were associated with lower EQ5DVAS scores. Contrary to the results of the univariate analysis, the association with BMI values was not significant in the multivariate model (Table 4).
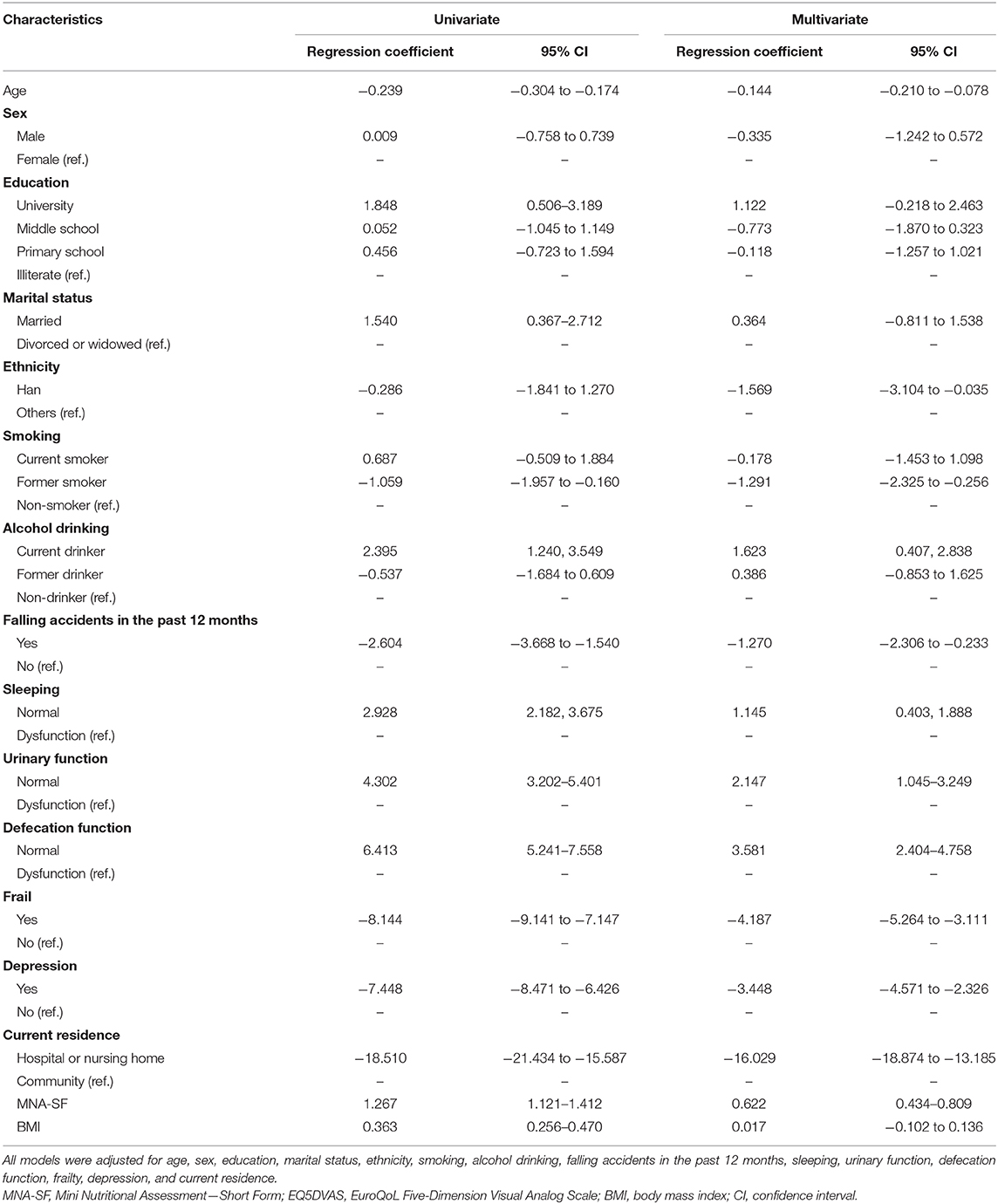
At the 90-day follow-up, current drinker (regression coefficient, 1.623; 95% CI, 0.407–2.838), normal sleeping (1.145; 0.403–1.888), normal urinary function (2.147; 1.045–3.249), normal defecation function (3.581; 2.404–4.758), and a higher MNA-SF score (0.622; 0.434–0.809) were associated with higher EQ5DVAS scores in the multiple linear regression model. Age (−0.144; −0.210 to −0.078), Han ethnicity (−1.569; −3.104 to −0.035), former smoker (−1.291; −2.325 to −0.256), falling accidents in the past 12 months (−1.270; −2.306 to −0.233), frailty (−4.187; −5.264 to −3.111), depression (−3.448; −4.571 to −2.326), and living in hospital or a nursing home (−16.029; −18.874 to −13.185) were associated with lower EQ5DVAS scores. Contrary to the results of the univariate analysis, the association with BMI values was not significant in the multivariate model (Table 5).
Discussion
To our knowledge, this is the first study to examine the associations between nutritional status, sociodemographic characteristics, and health-related variables and HRQoL among a nationally representative sample of Chinese hospitalized elderly population in tertiary hospitals. The main finding was that higher MNA-SF scores were related to higher HRQoL scores in elderly patients, both at the 30- and 90-day follow-up. However, we found no significant associations between the BMI values and HRQoL. Sociodemographic characteristics (such as age, smoking, and current residence), physical health variables (frailty, urinary function, defecation function, sleeping condition, and falling accidents in the past 12 months), and mental health variables (depression) were the main factors influencing HRQoL in this group.
The MNA-SF scores showed significant associations with the HRQoL scores, suggesting that nutritional status may have an important influence on the HRQoL among the elderly. This finding is consistent with previous studies reporting that the HRQoL scores decrease with the decline of the MNA-SF scores (6, 8, 13). Poor nutrition leads to ill health and ill health to poor nutrition, so identifying priorities for management is a key issue as well as a challenge. One study from Turkey reported that a 12-week intervention with oral nutritional supplementation plus physical exercise improved the nutritional status and HRQoL in older adults (13). Therefore, developing targeted nutritional supplementation plans to help older people to improve their HRQoL is fundamental to the management of healthy aging among older individuals in China. In addition, despite growing evidence that nutritional support improves HRQoL in older people, more data are urgently needed regarding the effects of nutritional support on HRQoL in the elderly.
In this study, MNA-SF and BMI were assessed at the time of admission to the hospital, and HRQoL was recorded at 30 and 90 days after admission via follow-up regardless of whether the participant is hospitalized or discharged. Generally, MNA-SF may reflect the nutritional status in the past 3 months; thus, the MNA-SF is more representative of the long-term nutritional status of participants than does BMI. Accordingly, the potential association between MNA-SF and HRQoL is more convincing in reflecting the relationship between nutritional status and clinical outcomes. BMI is prone to changes owing to weight gain or loss during hospitalization, which could explain the statistically non-significant results between BMI and HRQoL (8). Still, we believe that controlling BMI is essential to improving the clinical outcomes, as many researchers have shown that BMI is closely related to patients' inflammation and oxidation levels. Further research is required to confirm the relationships between nutritional status and clinical outcomes in this regard.
Similar to the present results, some studies have shown that HRQoL indicators decrease with aging in older adults (25, 37–39). In addition, our results suggest that the HRQoL scores among the participants in the hospital or nursing home settings were lower compared to the participants living in the community. This is perhaps because the community-dwelling elderly can receive support from family, friends, and neighbors and assistance with activities of daily living, such as the sourcing and preparation of meals and help with eating, when necessary (40), which means that such individuals have a better quality of life. Therefore, investing in adequate geriatric care sources, developing a home care-dominated system, supported by community care, and supplemented with institutional care aimed at helping the elderly to self-manage their daily activities and improving their HRQoL are warranted.
Apart from age and residence, former smokers had lower HRQoL scores than non-smokers. Previous studies have also demonstrated a negative relationship between smoking and HRQoL and that smoking cessation significantly improves HRQoL (41).
With regard to the health-related variables, our results suggest that physical and mental health variables including frailty, depression, and falling accidents in the past 12 months can bring about a series of negative effects on HRQoL; other research support these findings. In a study conducted among older adults, frail participants had leaner body mass, lower HRQoL scores, greater depression, and greater vulnerability to falls than the non-frail participants (9). Schoene et al. (42) demonstrated that a history of falling accidents might greatly affect HRQoL in older people. Other studies have reported that depression has a major influence on HRQoL, which can affect general appetite, and the HRQoL scores decrease with decreased general appetite (8, 39, 43). Besides, HRQoL was positively correlated with urinary function, defecation function, and sleeping condition in the present study. Regarding these factors, early assessment, identification, and prevention are important. More advanced risk factor assessment scales, standardized nursing care measures, and nutrition and physical activity interventions may be useful in improving the HRQoL among elderly patients in the future.
Compared with women, the men in our study had a lower risk of poor HRQoL at the 30-day follow-up; in addition, HRQoL was poorer in women than in men, as reported in other studies (44–46). This is perhaps because men generally have better muscle storage than women, and that may affect physical conditions (such as frailty), appetite, and other factors linked to HRQoL (47–49). At the 90-day follow-up, Han ethnicity was associated with lower HRQoL scores than did other ethnicities, which might be owing to differences in the ethnic distribution of our participants. In addition, current drinkers had higher HRQoL scores than non-drinkers; this can be ascribed to the fact that older adults who consume small to moderate amounts of alcohol are more likely to maintain physical functioning than non-drinkers, as moderate alcohol consumption has been associated with a decreased risk of cardiovascular disease (19). However, detailed assessments based on the amount and frequency of alcohol consumption are needed.
This study has some limitations that should be considered when interpreting the results. First, because of convenience sampling, the patients enrolled in our study were selected from tertiary hospitals and from only one hospital in each province or municipality/city, which limited the generalizability of this study. Second, there were a considerable number of potential participants who were unable to be contacted, most of whom were in distant provinces or were migrant workers; this may have led to selection bias. Thirdly, although nutritional status and HRQoL can be assessed using several different assessment scales, our use of a limited number of measurement tools restricted the comparison of our results with those of other studies. Fourth, the participants enrolled in this study were relatively young—nearly half of the participants were 65–69 years old—which limited the generalizability of this study. Fifth, the reason for the admission might be a major factor influencing HRQoL. The target population in this study involved multiple wards or departments; we did not analyze the reason for the admission, nor did we analyze the application of medical and nursing care in older patients. Finally, chronic diseases (such as cancer, diabetes, and cardiovascular diseases) could be associated with poor HRQoL among elderly patients. The participants in this study covered many departments, and we did not analyze the impact of chronic diseases in this paper. Prospective studies with more sophisticated evaluations are required in the future.
Conclusion
This study suggests that higher MNA-SF scores were associated with higher HRQoL scores in Chinese elderly patients, whereas there were no significant associations between BMI and HRQoL. Sociodemographic characteristics and physical and mental health variables were the main factors influencing HRQoL in this group. Investing in adequate geriatric care sources, developing a home care-dominated system, supported by community care, and supplemented with institutional care aimed at improving HRQoL are warranted. In light of the factors associated with HRQoL, attention should be paid to risk assessment, preventive measures, nutrition, and physical activity intervention. These findings could have major importance in the planning of “active aging” policies and programs.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committee of Peking Union Medical College Hospital (S-K540). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XWu conceived and designed this study. HL prepared and edited the manuscript and drafted the tables. JJia and TX performed the statistical analyses and reviewed the manuscript. CZ, MZ, XWe, JJin, HW, DL, and SZ recruited participants, collected data, and edited the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Special Research Fund for Central Universities, Peking Union Medical College (grant number 2018PT33001). The funding bodies had no specific role in the study design or data collection, analysis, and interpretation or in manuscript conception and writing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the research participants and nursing staff for their kind and efficient contribution to the study. We thank Hugh McGonigle, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of the manuscript.
Abbreviations
MNA-SF, Mini Nutritional Assessment—Short Form; BMI, body mass index; ICU, intensive care unit; CI, confidence interval; EQ5DVAS, EuroQoL five-dimension visual analog scale; HRQoL, health-related quality of life.
References
1. The Lancet. Global elderly care in crisis. Lancet. (2014) 383:927. doi: 10.1016/S0140-6736(14)60463-3
2. The Lancet. Ageing and health—an agenda half completed. Lancet. (2015) 386:1509. doi: 10.1016/S0140-6736(15)00521-8
3. The Lancet. How to cope with an ageing population. Lancet. (2013) 382:1225. doi: 10.1016/S0140-6736(13)62080-2
4. Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. (2015) 24(Pt. B):197–205. doi: 10.1016/j.arr.2015.08.003
5. Fernández-Barrés S, García-Barco M, Basora J, Martínez T, Pedret R, Arija V. The efficacy of a nutrition education intervention to prevent risk of malnutrition for dependent elderly patients receiving home care: a randomized controlled trial. Int J Nurs Stud. (2017) 70:131–41. doi: 10.1016/j.ijnurstu.2017.02.020
6. Verlaan S, Aspray TJ, Bauer JM, Cederholm T, Hemsworth J, Hill TR, et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: a case-control study. Clin Nutr. (2017) 36:267–74. doi: 10.1016/j.clnu.2015.11.013
7. Durazzo M, Campion D, Fagoonee S, Pellicano R. Gastrointestinal tract disorders in the elderly. Minerva Med. (2017) 108:575–91. doi: 10.23736/S0026-4806.17.05417-9
8. Rasheed S, Woods RT. An investigation into the association between nutritional status and quality of life in older people admitted to hospital. J Hum Nutr Diet. (2014) 27:142–51. doi: 10.1111/jhn.12072
9. Adame Perez SI, Senior PA, Field CJ, Jindal K, Mager D, Frailty R. Health-related quality of life, cognition, depression, vitamin D and health-care utilization in an ambulatory adult population with type 1 or type 2 diabetes mellitus and chronic kidney disease: a cross-sectional analysis. Can J Diabetes. (2019) 43:90–7. doi: 10.1016/j.jcjd.2018.06.001
10. Naruishi K, Yumoto H, Kido J-I. Clinical effects of low body mass index on geriatric status in elderly patients. Exp Gerontol. (2018) 110:86–91. doi: 10.1016/j.exger.2018.05.017
11. Win AZ, Ceresa C, Arnold K, Allison TA. High prevalence of malnutrition among elderly veterans in home based primary care. J Nutr Health Aging. (2017) 21:610–3. doi: 10.1007/s12603-017-0918-z
12. Wei JM, Zhang YH, Jamie P, Xu L, Li X, Suela S, et al. The impact of malnutrition on health outcomes and healthcare cost among Chinese older adults. Chin J Geriatr. (2017) 36:929. doi: 10.1016/S0261-5614(17)31099-3
13. Abizanda P, López MD, García VP, Estrella Jde D, da Silva González Á, Vilardell NB, et al. Effects of an oral nutritional supplementation plus physical exercise intervention on the physical function, nutritional status, and quality of life in frail institutionalized older adults: the ACTIVNES study. J Am Med Dir Assoc. (2015) 16:439.e9–16. doi: 10.1016/j.jamda.2015.02.005
14. Evans C. Malnutrition in the elderly: a multifactorial failure to thrive. Perm J. (2005) 9:38–41. doi: 10.7812/TPP/05-056
15. Development of the World Health Organization WHOQOL-BREF quality of life assessment. the WHOQOL group. Psychol Med. (1998) 28:551–8. doi: 10.1017/S0033291798006667
16. Jimenez-Redondo S, Beltran de Miguel B, Gavidia Banegas, Guzman Mercedes L, Gomez-Pavon J, Cuadrado Vives C. Influence of nutritional status on health-related quality of life of non-institutionalized older people. J Nutr Health Aging. (2014) 18:359–64. doi: 10.1007/s12603-013-0416-x
17. Kostka J, Borowiak E, Kostka T. Nutritional status and quality of life in different populations of older people in Poland. Eur J Clin Nutr. (2014) 68:1210–15. doi: 10.1038/ejcn.2014.172
18. Kiesswetter E, Pohlhausen S, Uhlig K, Diekmann R, Lesser S, Heseker H, et al. Malnutrition is related to functional impairment in older adults receiving home care. J Nutr Health Aging. (2013) 17:345–50. doi: 10.1007/s12603-012-0409-1
19. Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. (1999) 48:445–69. doi: 10.1016/S0277-9536(98)00370-0
20. Akosile CO, Mgbeojedo UG, Maruf FA, Okoye EC, Umeonwuka IC, Ogunniyi A. Depression, functional disability and quality of life among Nigerian older adults: prevalences and relationships. Arch Gerontol Geriatr. (2018) 74:39–43. doi: 10.1016/j.archger.2017.08.011
21. Eriksson BG, Dey DK, Hessler RM, Steen G, Steen B. Relationship between MNA and SF-36 in a free-living elderly population aged 70 to 75. J Nutr Health Aging. (2005) 9:212–20.
22. Ye B, Gao J, Fu H. Associations between lifestyle, physical and social environments and frailty among Chinese older people: a multilevel analysis. BMC Geriatr. (2018) 18:314. doi: 10.1186/s12877-018-0982-1
23. Yu J, Li J, Cuijpers P, Wu S, Wu Z. Prevalence and correlates of depressive symptoms in Chinese older adults: a population-based study. Int J Geriatr Psychiatry. (2012) 27:305–12. doi: 10.1002/gps.2721
24. Ran L, Jiang X, Li B, Kong H, Du M, Wang X, et al. Association among activities of daily living, instrumental activities of daily living and health-related quality of life in elderly Yi ethnic minority. BMC Geriatr. (2017) 17:74. doi: 10.1186/s12877-017-0455-y
25. Sun W, Aodeng S, Tanimoto Y, Watanabe M, Han J, Wang B, et al. Quality of life (QOL) of the community-dwelling elderly and associated factors: a population-based study in urban areas of China. Arch Gerontol Geriatr. (2015) 60:311–6. doi: 10.1016/j.archger.2014.12.002
26. Agarwal E, Miller M, Yaxley A, Isenring E. Malnutrition in the elderly: a narrative review. Maturitas. (2013) 76:296–302. doi: 10.1016/j.maturitas.2013.07.013
27. Lei Z, Qingyi D, Feng G, Chen W, Hock RS, Changli W. Clinical study of mini-nutritional assessment for older Chinese inpatients. J Nutr Health Aging. (2009) 13:871–5. doi: 10.1007/s12603-009-0244-1
28. Weir CB, Jan A. BMI Classification Percentile And Cut Off Points. Treasure Island, FL: StatPearls (2019).
29. Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases–report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci. (2002) 15:245–52.
30. World Health Organization. Obesity: Preventing and Managing the Global Epidemic Report of a WHO Consultation (WHO Technical Report Series 894). (2000) 894, i-xii, 1–253.
31. EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. (1990) 16:199–208. doi: 10.1016/0168-8510(90)90421-9
32. Bao XY, Xie YX, Zhang XX, Peng X, Huang JX, Du QF, et al. The association between multimorbidity and health-related quality of life: a cross-sectional survey among community middle-aged and elderly residents in southern China. Health Qual Life Outcomes. (2019) 17:107. doi: 10.1186/s12955-019-1175-0
33. Wang H, Kindig DA, Mullahy J. Variation in Chinese population health related quality of life: results from a EuroQol study in Beijing, China. Qual Life Res. (2005) 14:119–32. doi: 10.1007/s11136-004-0612-6
34. Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. (2012) 16:601–8. doi: 10.1007/s12603-012-0084-2
35. Arthur AJ, Jagger C, Lindesay J, Matthews RJ. Evaluating a mental health assessment for older people with depressive symptoms in general practice: a randomised controlled trial. Br J Gen Pract. (2002) 52:202–7.
36. Zhao H, He J, Yi J, Yao S. Factor structure and measurement invariance across gender groups of the 15-item geriatric depression scale among chinese elders. Front Psychol. (2019) 10:1360. doi: 10.3389/fpsyg.2019.01360
37. Acar Tek N, Karacil-Ermumcu MS. Determinants of health related quality of life in home dwelling elderly population: appetite and nutritional status. J Nutr Health Aging. (2018) 22:996–1002. doi: 10.1007/s12603-018-1066-9
38. Chen H-M, Chen C-M. Factors associated with quality of life among older adults with chronic disease in Taiwan. Int J Gerontol. (2017) 11:12–5. doi: 10.1016/j.ijge.2016.07.002
39. Gallegos-Carrillo K, Garcia-Pena C, Mudgal J, Romero X, Duran-Arenas L, Salmeron J. Role of depressive symptoms and comorbid chronic disease on health-related quality of life among community-dwelling older adults. J Psychosom Res. (2009) 66:127–35. doi: 10.1016/j.jpsychores.2008.07.007
40. Marshall S, Agarwal E, Young A, Isenring E. Role of domiciliary and family carers in individualised nutrition support for older adults living in the community. Maturitas. (2017) 98:20–9. doi: 10.1016/j.maturitas.2017.01.004
41. Goldenberg M, Danovitch I, William IsHak W. IsHak: quality of life and smoking. Am J Addict. (2014) 23:540–62. doi: 10.1111/j.1521-0391.2014.12148.x
42. Schoene D, Heller C, Aung YN, Sieber CC, Kemmler W, Freiberger E. A systematic review on the influence of fear of falling on quality of life in older people: is there a role for falls? Clin Interv Aging. (2019) 14:701–19. doi: 10.2147/CIA.S197857
43. Pilgrim AL, Robinson SM, Sayer AA, Roberts HC. An overview of appetite decline in older people. Nurs Older People. (2015) 27:29–35. doi: 10.7748/nop.27.5.29.e697
44. Kvamme JM, Olsen JA, Florholmen J, Jacobsen BK. Risk of malnutrition and health-related quality of life in community-living elderly men and women: the Tromso study. Qual Life Res. (2011) 20:575–82. doi: 10.1007/s11136-010-9788-0
45. Konig HH, Heider D, Lehnert T, Riedel-Heller SG, Angermeyer MC, Matschinger H, et al. Health status of the advanced elderly in six European countries: results from a representative survey using EQ-5D and SF-12. Health Qual Life Outcomes. (2010) 8:143. doi: 10.1186/1477-7525-8-143
46. Guallar-Castillon P, Sendino AR, Banegas JR, Lopez-Garcia E, Rodriguez-Artalejo F. Differences in quality of life between women and men in the older population of Spain. Soc Sci Med. (2005) 60:1229–40. doi: 10.1016/j.socscimed.2004.07.003
47. Ribeiro RV, Hirani V, Senior AM, Gosby AK, Cumming RG, Blyth FM, et al. Le couteur, diet quality and its implications on the cardio-metabolic, physical and general health of older men: the concord health and ageing in men project (CHAMP). Br J Nutr. (2017) 118:130–43. doi: 10.1017/S0007114517001738
48. Das A, Cumming RG, Naganathan V, Blyth F, Ribeiro RV, Le Couteur DG, et al. Prospective associations between dietary antioxidant intake and frailty in older australian men: the concord health and ageing in men project. J Gerontol A Biol Sci Med Sci. (2020) 75:348–56. doi: 10.1093/gerona/glz054
Keywords: aging, malnutrition, depression, frailty, health-related quality of life, China
Citation: Liu H, Jiao J, Zhu C, Zhu M, Wen X, Jin J, Wang H, Lv D, Zhao S, Wu X and Xu T (2020) Associations Between Nutritional Status, Sociodemographic Characteristics, and Health-Related Variables and Health-Related Quality of Life Among Chinese Elderly Patients: A Multicenter Prospective Study. Front. Nutr. 7:583161. doi: 10.3389/fnut.2020.583161
Received: 14 July 2020; Accepted: 31 August 2020;
Published: 16 October 2020.
Edited by:
Rosa Sammarco, University of Naples Federico II, ItalyReviewed by:
Lina Ma, Capital Medical University, ChinaRosilene Ventura Ribeiro, The University of Sydney, Australia
Copyright © 2020 Liu, Jiao, Zhu, Zhu, Wen, Jin, Wang, Lv, Zhao, Wu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinjuan Wu, d3V4aW5qdWFuQHNpbmEuY29t; Tao Xu, eHV0YW9zZEAxMjYuY29t
†These authors have contributed equally to this work
 Hongpeng Liu
Hongpeng Liu Jing Jiao
Jing Jiao Chen Zhu1
Chen Zhu1 Jingfen Jin
Jingfen Jin