- 1Metabolic Disease Center, Affiliated Hospital of Hangzhou Normal University, Hangzhou, China
- 2Department of Anesthesiology, The Second Hospital of Anhui Medical Unviersity, Hefei, China
- 3Department of Molecular & Cellular Physiology, Shinshu University School of Medicine, Matsumoto, Japan
- 4Neurological Department, Affiliated Hospital of Guizhou Medical University, Guiyang, China
- 5School of Public Health, Hangzhou Medical College, Hangzhou, China
Background: The coronavirus pneumonia is still spreading around the world. Much progress has been made in vaccine development, and vaccination will become an inevitable trend in the fight against this pandemic. However, the public acceptance of COVID-19 vaccination still remains uncertain.
Methods: An anonymous questionnaire was used in Wen Juan Xing survey platform. All the respondents were divided into healthcare workers and non-healthcare workers. Multinomial logistic regression analyses were performed to identify the key sociodemographic, cognitive, and attitude associations among the samples of healthcare workers and non-healthcare workers.
Results: A total of 2,580 respondents completed the questionnaire, including 1,329 healthcare workers and 1,251 non-healthcare workers. This study showed that 76.98% of healthcare workers accepted the COVID-19 vaccine, 18.28% workers were hesitant, and 4.74% workers were resistant. Among the non-healthcare workers, 56.19% workers received the COVID-19 vaccine, 37.57% workers were hesitant, and 6.24% workers were resistant. Among the healthcare workers, compared with vaccine recipients, vaccine-hesitant individuals were more likely to be female (AOR = 1.52, 95% CI: 1.12–2.07); vaccine-resistant individuals were more likely to live in the suburbs (AOR = 2.81, 95% CI: 1.44–3.99) with an income of 10,000 RMB or greater (AOR = 2.00, 95% CI: 1.03–3.90). Among the non-healthcare workers, vaccine-hesitant individuals were more likely to be female (AOR = 1.66, 95% CI: 1.31–2.11); vaccine-resistant individuals were also more likely to be female (AOR = 1.87, 95% CI: 1.16–3.02) and older than 65 years (AOR = 4.96, 95% CI: 1.40–7.62). There are great differences between healthcare workers and non-healthcare workers in their cognition and attitude toward vaccines.
Conclusions: Our study shows that healthcare workers are more willing to be vaccinated than non-healthcare workers. Current vaccine safety issues continue to be a major factor affecting public acceptance, and to expand vaccine coverage in response to the COVID-19 pandemic, appropriate vaccination strategies and immunization programs are essential, especially for non-healthcare workers.
Background
In the absence of a vaccine or effective treatment, all the countries around the world are trying to control the spread of COVID-19 by imposing quarantines and lockdowns, social distance measures, use of face masks in communities at all times, and travel restrictions. All these actions have caused enormous damage to people's physical and mental health and contributed to a significant global economic downturn (1–3). Therefore, there is a great need for an effective vaccine to control COVID-19. In fact, COVID-19 vaccines are being developed. According to the WHO, as of 12 March 2021, 81 vaccine candidates have been submitted for clinical evaluation, and 182 vaccine candidates have been submitted for preclinical evaluation (4, 5).
However, many side effects of vaccine have been reported in clinical evaluation, such as injection site pain (89.8%), fatigue (62.2%), headache (45.6%), and muscle pain (37.1%) (6). More serious side effects have also been reported, such as COVID-19 vaccine-associated immune thrombosis and thrombocytopenia (7). Despite great progress in vaccine development, there are still significant challenges in future immunization against COVID-19, one of which is uncertainty about the public acceptance of COVID-19 vaccination (8). A representative data from the general adult populations of Ireland and the United Kingdom showed that vaccine hesitancy/resistance was evident for 35 and 31% of these populations, respectively (9).
In fact, vaccine acceptance reflects the general perception of disease risk, vaccine attitudes, and needs of the general population, which is critical to the success of immunization programs to achieve a high vaccination coverage, especially for emerging infectious diseases (10, 11). Mathematical models showed that if the COVID-19 vaccine is 80% effective, then the coverage must be at least 75% to eliminate an ongoing pandemic (12). Therefore, it is extremely important to keep track of the public's views on vaccination, especially the views and acceptance of the vaccine among healthcare workers and non-healthcare workers.
Healthcare workers are often on the front lines of fight against epidemics, some of whom are required to carry out procedures with a high risk of contracting pathogens (13). In addition, previous studies reported that clinicians are an important source of vaccine information, and communication among clinicians can improve the adherence to vaccination recommendations (14–17). Certainly, healthcare workers are also concerned about the side effects of vaccines. Therefore, we need to know whether there is a difference in the acceptance of vaccines between the healthcare workers and non-healthcare workers in China. What factors affect the people's acceptance of the vaccine? This information is critical to prepare well for future vaccination strategies and immunization programs against COVID-19. Therefore, our study aimed to evaluate the acceptance of future COVID-19 vaccination, preference for vaccine attributes and schedules, and influencing factors for vaccination acceptance among healthcare workers and non-healthcare workers in China.
Methods
Population and Sampling
This study is a nation-wide cross-sectional study in China; the ethics committee of Affiliated Hospital of Hangzhou Normal University approved all the procedures performed. In January 2021, an anonymous online cross-sectional survey was conducted on Wen Juan network (https://www.wenjuan.com), founded by Shanghai Zhongyan Network Technology. It is the largest free online survey platform in China, which can provide questionnaire creation, release, management, collection, and analysis services for enterprises or individuals. Their personal information can be confirmed, and authentic, diverse, and representative samples can be obtained. The target population of this study is Chinese adults living in China, divided into healthcare workers and non-healthcare workers according to their occupation.
First, we calculated the sample size of the survey, according to a previous study, currently the average proportion of people accepted to be vaccinated is 64.9% (8). Therefore, an approximate value of 65% was selected for the calculation of sample size. The expected error rate was set to 1.5%. The sample size was calculated as follows (18, 19):
where ua = 1.96, p is the proportion of vaccinations accepted, and δ is the standard deviation (0.015). To reduce the sampling error and increase the study power, a rough estimation was made by multiplying the calculated sample size by 1.35 times, leading to a final sample size of 2,675. The validation of the questionnaire is 0.83. After sorting out the collected questionnaires, we excluded the invalid questionnaires (lack of information, filling errors) and finally included 2,580 valid questionnaires. Among them, 1,329 questionnaires were from the healthcare workers, and 1,251 questionnaires were from the non-healthcare workers.
Questionnaire Design
Informed consent has been designed. In the first part of the survey page, we have set that the respondents can continue to complete the questionnaire if they agree to response to it. If they do not agree, they can not go on. A self-administered questionnaire was designed based on previous study to evaluate the acceptance of vaccines for emerging infectious diseases (20). The questionnaire mainly includes two parts: social demographic characteristics and cognition and attitude toward vaccine. The first part focused on “gender, age, education level, living area, family income, and health status.” The second part featured eight questions about cognition and attitude toward vaccine. The scenario presented to the physicians was as follows: “Do you know about COVID-19 vaccine development and vaccination; do you think the COVID-19 vaccine has side effects; do you think it's better to get immunity to infectious diseases naturally than vaccinating; do you think vaccination is an effective way to prevent and control the epidemic; do you believe in the safety and effectiveness of vaccines; do you know the vaccination place in your residential area; does your work unit encourage you to get vaccinated; do you think vaccination has an effect on regional epidemic prevention.” Attitude toward vaccine including three types: resistance, hesitation, and acceptance. Resistance means rejection of vaccination. Hesitation means unwillingness to accept because of being uncertain, worried, or embarrassed about vaccination. Acceptance means agreeing with an inoculation. The three types of attitudes toward vaccines were investigated through questions: would you like to get the COVID-19 vaccine? The answer option set three options: resistance, hesitation, and acceptance.
Statistical Method
A descriptive statistical analysis was conducted on the social and demographic characteristics of the sample, and the corresponding proportion was calculated. Multiple logistic regression analysis was used, in which the dependent variable was the vaccine acceptance (resistance, hesitation, and acceptance), and the independent variable was the influencing factor (social population, cognition, and attitude). For these analyses, the vaccine acceptance group was set as the reference category to identity factors associated with vaccine hesitancy and vaccine resistance. All relationships between the predictor and criterion variables are represented as adjusted odds ratios (AOR) with 95% confidence intervals. The statistical tests were two-sided, and the effects with p < 0.05 were considered to be statistically significant. All statistical models were constructed using R software version 3.6.0 (R Foundation for Statistical Computing, version 3.6.1; http://www.Rproject.org).
Results
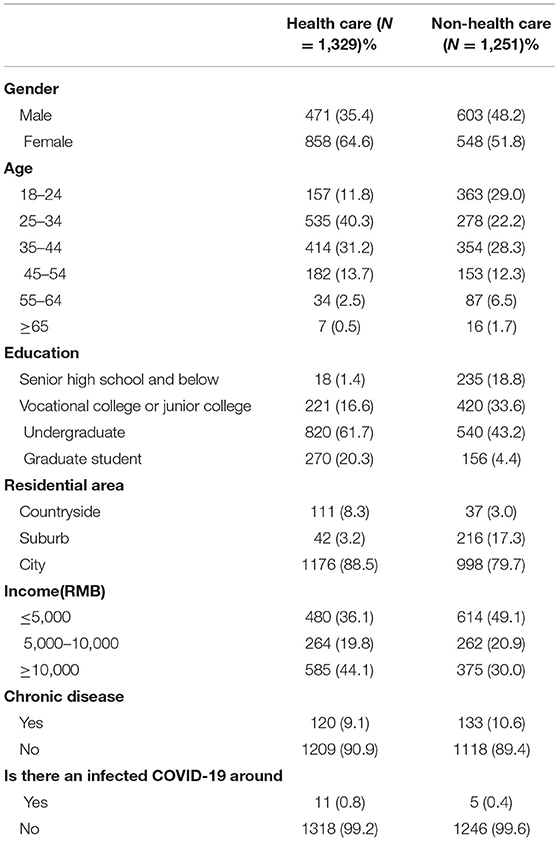
A total of 2,580 respondents completed the questionnaire, including 1,329 healthcare workers and 1,251 non-healthcare workers (Table 1). All of them were distributed in 33 provincial administrative regions in China (Supplementary Table 1).
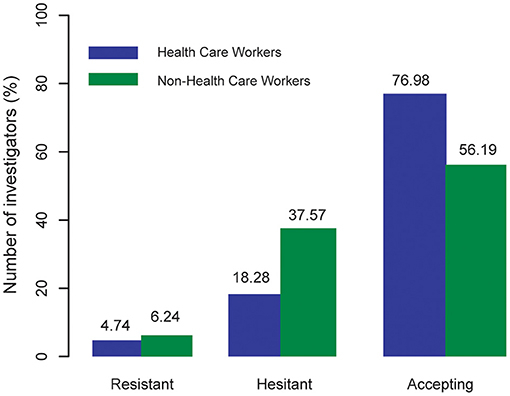
The basic characteristics of the respondents showed that 76.98% of healthcare workers accepted the COVID-19 vaccine; 18.28% of healthcare workers were hesitant; and 4.74% of healthcare workers were resistant. Among the non-healthcare workers, 56.19% of non-healthcare workers received the COVID-19 vaccine, significantly lower than that of healthcare workers; 37.57% non-healthcare workers were hesitant; and 6.24% non-healthcare workers were resistant, higher than that of healthcare workers (Figure 1).
The correlations of sociodemographic and health indicators among the samples of healthcare workers and non-healthcare workers showed that vaccine-hesitant individuals were more likely to be female (AOR = 1.52, 95% CI: 1.12–2.07) among the healthcare workers, comparing with vaccine recipients. Vaccine-resistant individuals were more likely to live in the suburbs (AOR = 2.81, 95% CI: 1.44–3.99) with an income of 10,000 RMB or greater (AOR = 2.00, 95% CI: 1.03–3.90). Among the non-healthcare workers, vaccine-hesitant individuals were more likely to be female (AOR = 1.66, 95% CI: 1.31–2.11). Vaccine-resistant individuals were also more likely to be female (AOR = 1.87, 95% CI: 1.16–3.02) and older than 65 years (AOR = 4.96, 95% CI: 1.40–7.62) (Table 2).
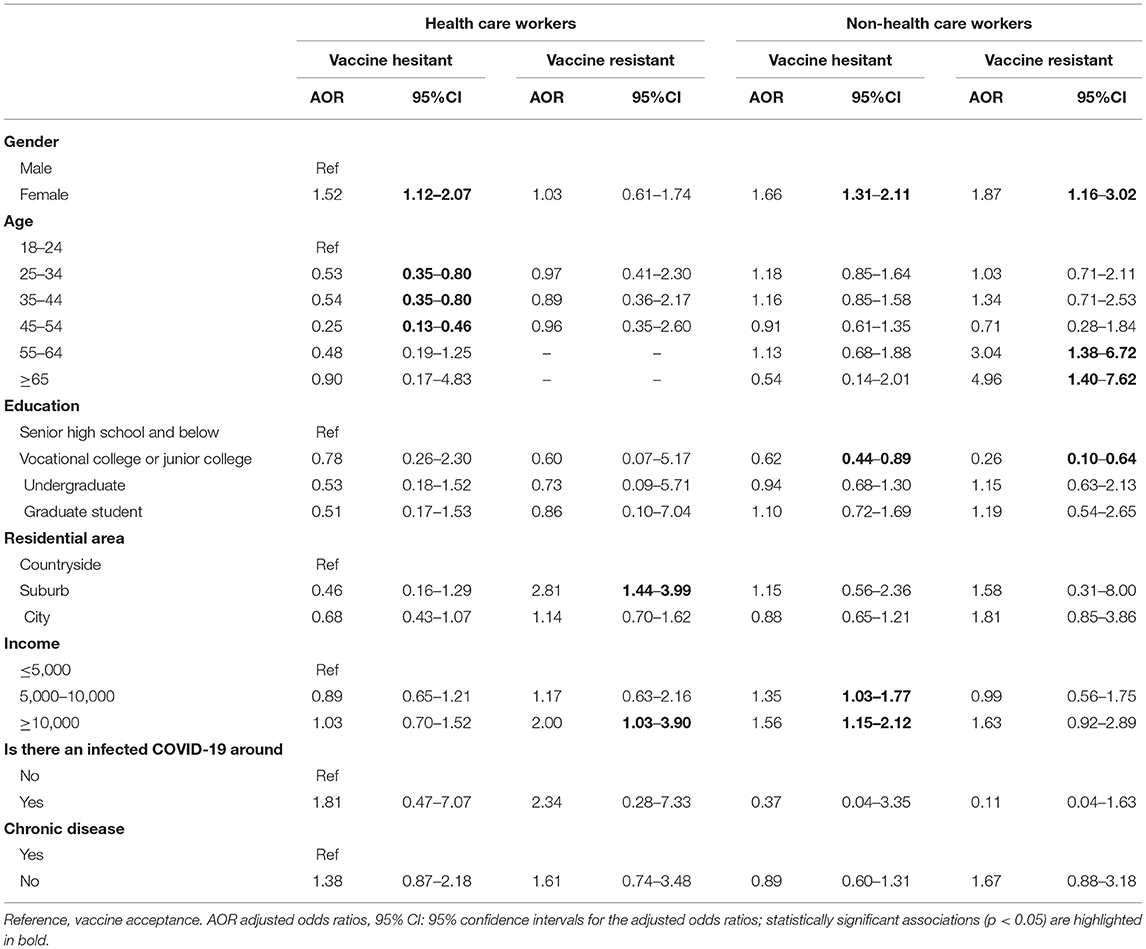
Table 2. Relationships of sociodemographic and health indicators among the samples of healthcare workers and non-healthcare workers.
The cognition and attitude of healthcare workers and non-healthcare workers are described in Table 3. The reasons for vaccine hesitation or resistance among healthcare workers are as follows: Adverse effects of vaccine were considered (AOR = 6.91, 95% CI: 4.73–10.1; 9.30, 95% CI: 4.20–20.6). Vaccines were not considered an effective method for controlling epidemics (AOR = 2.43, 95% CI: 1.52–3.88; 5.40, 95% CI: 2.85–10.2). The safety and efficacy of the vaccine were not convinced (AOR = 11.71, 95% CI: 6.78–20.23; 40.77, 95% CI: 22.0–83.1). Work unit had no vaccination requirements (AOR = 4.61, 95% CI: 3.32–6.41; 2.10, 95% CI: 1.04–3.89). In addition, people with vaccine resistance were more likely to perceive vaccination as having no significant or moderate impact on district prevention (AOR = 21.6, 95% CI: 11.6–27.5; 11.93, 95% CI: 8.0–17.2).
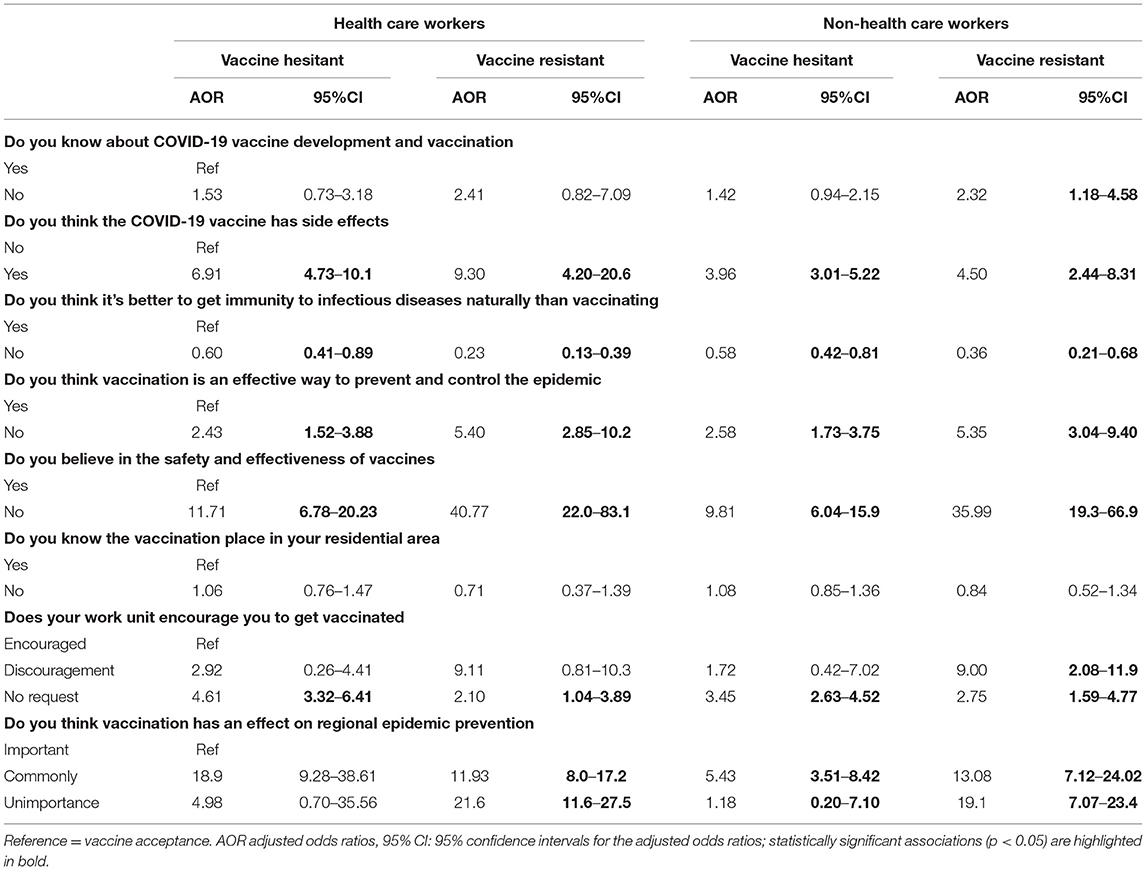
Table 3. Relationships of cognitive and attitude with the samples of healthcare workers and non-healthcare workers.
Among the non-healthcare workers, those with vaccine hesitation were more likely to believe that vaccination had an average impact on regional prevention (AOR = 5.43, 95% CI: 3.51–8.42), except for the above reasons which were similar to those of healthcare workers. Non-healthcare workers with vaccine resistance were more likely to be unaware of vaccine development and vaccination (AOR = 2.32, 95% CI: 1.18–4.58) and discouraged by their employer from getting vaccinated (AOR = 9.00, 95% CI: 2.08–11.9).
Discussion
Our results showed that the acceptance rate of vaccine was higher than 50% in both healthcare workers and non-healthcare workers. Although our study showed a high acceptance of vaccination among the healthcare workers, not all of them wanted to receive the vaccine. The acceptance rate of healthcare workers was significantly higher than that of non-healthcare workers (76.98 vs. 56.19%), while the rates of vaccine hesitation and resistance were lower than those of non-healthcare workers. We think they also have an attitude toward the vaccine and what concerns they might have although they had been vaccinated. Their experience might provide better suggestions for our vaccination strategy. Therefore, we did not exclude this part of the vaccinated population before the investigation.
Females were more likely to show signs of vaccine hesitancy and resistance than males, especially among non-healthcare workers. In terms of age, vaccine resistance among the non-healthcare workers was more common in people over 55 years old. In addition, we found that the education level and the presence of chronic diseases and COVID-19 infection had no significant influence on the acceptance of vaccine among the healthcare workers, while the residence and income level had some influence. In contrast, among the non-healthcare workers, education level had a certain effect on vaccine resistance and resistance. Therefore, to increase the vaccine coverage and eliminate the ongoing pandemic, non-healthcare workers should be encouraged to actively vaccinate themselves, while the acceptance of healthcare workers to vaccinate should not be ignored.
Previous reports indicated that the acceptance to get vaccinated lies between 60 and 90% among the doctors in Greece (February 2020) and France (March–July 2020), and between 40 and 60% among the nurses in Hong Kong, China (February–March 2020) (21–23). Numerous studies had reported that clinicians were an important source of vaccine information. Communication among physicians could improve the adherence to vaccination recommendations (24, 25), and vaccinated healthcare workers were more likely to recommend vaccines to friends, families, and their patients (26–29). Therefore, it is necessary to evaluate the acceptance of vaccination by healthcare workers and its influencing factors, and to motivate the non-healthcare workers to actively respond to vaccination through them.
Concerns about the safety or side effects of the vaccine were reported to be the main reason for the hesitation, and previous study on the acceptance of vaccination against emerging serious infectious diseases such as H1N1 had also emphasized that uncertainty about the new vaccine, particularly its safety, can reduce the confidence in the vaccine and thus the acceptance (30). Our findings were consistent with these findings. The common factors influencing vaccine hesitation or resistance among healthcare workers and non-healthcare workers were as follows: (1) They thought that the vaccine had side effects. (2) They did not think that vaccination was an effective way to prevent and control the epidemic. (3) They did not believe in the safety and effectiveness of the vaccine (the main reason). (4) The current cost of vaccines was unacceptable. (5) There was no requirement for vaccination in the work unit. We found that the reasons for vaccine hesitation and resistance among the non-healthcare workers were not only related to the above points, but also related to their lack of knowledge about the development and vaccination of COVID-19 vaccine.
We also found that the non-healthcare workers were less concerned about the side effects and safety of vaccines than the medical workers, probably because of the lack of medical knowledge and low understanding of COVID-19 vaccines. Universal vaccination is an important measure to control the epidemic. To control COVID-19 effectively and quickly and restore social activities, appropriate vaccination strategies, and immunization programs should be designed to increase the coverage, especially among those who are hesitant about vaccination (16). Currently, the cost of the vaccine should be affordable to the public, and China has long stated its goal is to make its COVID-19 vaccine a global good when it is ready for use (6, 31). In response to public concerns about the safety and efficacy of vaccines, health professionals, and credible authorities, such as governments or other sources, should actively organize health education and communication to combat disinformation and misinformation, and disseminate authoritative information in a transparent manner, especially about vaccine effectiveness, and adverse events (32–36). This will help to encourage community leaders of healthcare professionals and surrounding friends or relatives to share their personal experiences with COVID-19 vaccination to build vaccine confidence and trust (37). In addition, a high perception of benefits and low perceived barriers to receiving the vaccine were the two most important factors influencing a definite intention for COVID-19 vaccination; hence, public health intervention programs should focus on increasing the perception of benefits of vaccination (1).
This is the first study on a large-scale vaccination of healthcare workers and non-healthcare workers during the COVID-19 pandemic. This study provides guidance for the vaccination of Chinese population, especially for non-healthcare workers.
This study has some limitations. First, in this study, an online questionnaire was used, and the public may have problems such as information deviation or false filling when filling in the questionnaire, which requires further research. Second, we used a web push technology to make the survey. We could not obtain a balanced feedback from different cities in China. From S-table, the regional imbalance of responders was obvious. However, we have to point out that the number of medical staff and non-medical staff was relatively balanced.
Conclusions
Chinese adults have a high degree of acceptance of vaccination, and healthcare workers are more willing to be vaccinated than non-healthcare workers. Current vaccine safety issues are a major factor affecting public acceptance, and to expand vaccine coverage in response to the COVID-19 pandemic, appropriate vaccination strategies and immunization programs are essential.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
This study is a nation-wide cross-sectional study in China; the ethics committee of Affiliated Hospital of Hangzhou Normal University approved all the procedures performed.
Author Contributions
Y-RC and Z-HF conceived the study and designed the analysis. Y-RC and NW performed statistical analysis. M-WW and WW wrote the first draft of the manuscript. M-YZ, JN, J-jJ, C-yW, and X-wZ participate in revision the manuscript. All authors contributed to revision of the manuscript.
Funding
The presented study was supported by Youth fund of Zhejiang Academy of Medical Sciences (No. 2019Y009); Medical and Technology Project of Zhejiang Province (Nos. 2021HY127, 2020362651, and 2021KY890); Hangzhou science and Technology Bureau fund (Nos. 20191203B96 and 20191203B105); Clinical Research Fund of Zhejiang Medical Association (No. 2020ZYC-A13); Hangzhou Health and Family Planning Technology Plan key projects (2017ZD02).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.709056/full#supplementary-material
References
1. Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. (2020) 14:e0008961. doi: 10.1371/journal.pntd.0008961
2. WHO. World Health Data Platform. Available online at: https://www.who.int/data#reports (accessed March 15, 2021).
3. Zhang KC, Fang Y, Cao H, Chen H, Hu T, Chen YQ, et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: cross-sectional online survey. JMIR Pediatr Parent. (2020) 3:e24827. doi: 10.2196/24827
4. Carvalho Aguiar Melo M, de Sousa Soares D. Impact of social distancing on mental health during the COVID-19 pandemic: an urgent discussion. Int J Soc Psychiatry. (2020) 66:625–6. doi: 10.1177/0020764020927047
5. World Health Data Platform. Draft Landscape and Tracker of COVID-19 Candidate Vaccines. Available online at: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed March 15, 2021).
6. Riad A, Pokorná A, Attia S, Klugarová J, Koščík M, Klugar M. Prevalence of COVID-19 vaccine side effects among healthcare workers in the Czech Republic. J Clin Med. (2021) 10:1428. doi: 10.3390/jcm10071428
7. Franchini M, Liumbruno GM, Pezzo M. COVID-19 vaccine-associated immune thrombosis and thrombocytopenia (VITT): diagnostic and therapeutic recommendations for a new syndrome. Eur J Haematol. (2021) 107:173–80. doi: 10.1111/ejh.13665
8. Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. (2020) 8482. doi: 10.3390/vaccines8030482
9. Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. (2020) 13:1657–63. doi: 10.2147/JMDH.S276771
10. Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. (2021) 12:29. doi: 10.1038/s41467-020-20226-9
11. Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. (2014) 112:1–11. doi: 10.1016/j.socscimed.2014.04.018
12. Bartsch SM, O'Shea KJ, Ferguson MC, Bottazzi ME, Wedlock PT, Strych U, et al. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am J Prev Med. (2020) 59:493–503. doi: 10.1016/j.amepre.2020.06.011
13. Kwok KO, Li KK, Wei WI, Tang A, Wong SYS, Lee SS. Editor's choice: influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. (2021) 114:103854. doi: 10.1016/j.ijnurstu.2020.103854
14. Wheeler M, Buttenheim AM. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum Vaccin Immunother. (2013) 9:1782–9. doi: 10.4161/hv.25959
15. Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch Pediatr Adolesc Med. (2005) 159:470–6. doi: 10.1001/archpedi.159.5.470
16. Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. (2009) 360:1981–8. doi: 10.1056/NEJMsa0806477
17. Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. (2021) 9:119. doi: 10.3390/vaccines9020119
18. Schmidt SAJ, Lo S, Hollestein LM. Research techniques made simple: sample size estimation and power calculation. J Invest Dermatol. (2018) 138:1678–82. doi: 10.1016/j.jid.2018.06.165
19. Jiang Z, Wang J, Guo X, Feng L, Yu M, Zhou J, et al. Menstrual disorders and occupational exposures among female nurses: a nationwide cross-sectional study. Int J Nurs Stud. (2019) 95:49–55. doi: 10.1016/j.ijnurstu.2019.04.010
20. Irwin KL, Jalloh MF, Corker J, Alpha Mahmoud B, Alpha Mahmoud B, Li W, et al. Attitudes about vaccines to prevent Ebola virus disease in Guinea at the end of a large Ebola epidemic: results of a national household survey. Vaccine. (2017) 35:6915–23 doi: 10.1016/j.vaccine.2017.06.026
21. Napolitano F, Della Polla G, Angelillo IF. Knowledge, attitudes, and behaviors of parents towards recommended adult vaccinations: an explanatory survey in the geographic area of Naples, Italy. Int J Environ Res Public Health. (2019) 16:2070. doi: 10.3390/ijerph16122070
22. Detoc M, Touche C, Charles R, Lucht F, Gagneux-Brunon A, Botelho-Nevers E. Primary physicians' attitudes toward their patients receiving a proposal to participate in a vaccine trial. Hum Vaccin Immunother. (2019) 15:2969–79. doi: 10.1080/21645515.2019.1625646
23. Verger P, Scronias D, Dauby N, Lucht F, Gagneux-Brunon A, Botelho-Nevers E. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill. (2021) 26:2002047. doi: 10.2807/1560-7917.ES.2021.26.3.2002047
24. Papagiannis D, Malli F, Raptis DG, Papathanasiou IV, Fradelos EC, Danill Z, et al. Assessment of knowledge, attitudes, and practices towards new coronavirus (SARS-CoV-2) of health care professionals in Greece before the outbreak period. Int J Environ Res Public Health. (2020) 17:4925. doi: 10.3390/ijerph17144925
25. Gagneux-Brunon A, Detoc M, Bruel S, Tardy B, Rozaire O, Frappe P, et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. (2021) 108:168–73. doi: 10.1016/j.jhin.2020.11.020
26. Wang K, Wong ELY, Ho KF, Cheung AWL, Chan EYY, Yeoh EK, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. (2020) 38:7049–56. doi: 10.1016/j.vaccine.2020.09.021
27. Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. (2016) 34:6700–6. doi: 10.1016/j.vaccine.2016.10.042
28. Zhang J, While AE, Norman IJ. Nurses' knowledge and risk perception towards seasonal influenza and vaccination and their vaccination behaviours: a cross-sectional survey. Int J Nurs Stud. (2011) 48:1281–9. doi: 10.1016/j.ijnurstu.2011.03.002
29. LaVela SL, Smith B, Weaver FM, Legro MW, Goldstein B, Nichol K. Attitudes and practices regarding influenza vaccination among healthcare workers providing services to individuals with spinal cord injuries and disorders. Infect Control Hosp Epidemiol. (2004) 25:933–40. doi: 10.1086/502323
30. Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. (2020) 9:16. doi: 10.3390/vaccines9010016
31. Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. (2020) 21:977–82. doi: 10.1007/s10198-020-01208-6
32. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. (2020) 173:964–73. doi: 10.7326/M20-3569
33. Henrich N, Holmes B. The public's acceptance of novel vaccines during a pandemic: a focus group study and its application to influenza H1N1. Emerg Health Threats J. (2009) 2:e8. doi: 10.3134/ehtj.09.008
34. Determann D, Korfage IJ, Lambooij MS, Bliemer M, Richardus JH, Steyerberg EW, et al. Acceptance of vaccinations in pandemic outbreaks: a discrete choice experiment. PLoS ONE. (2014) 9:e102505. doi: 10.1371/journal.pone.0102505
35. Xinhua Net Update: China to Make COVID-19 Vaccine Global Public Good: Official. Available online at: http://www.xinhuanet.com/english/2020-06/07/c_139121625.htm (accessed March 15, 2020).
36. Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. (2020) 35:785–8. doi: 10.1007/s10654-020-00675-8
Keywords: COVID-19 vaccine, healthcare workers, non-healthcare workers, vaccine hesitant, vaccine resistant, vaccine acceptance
Citation: Wang M-W, Wen W, Wang N, Zhou M-Y, Wang C-y, Ni J, Jiang J-j, Zhang X-w, Feng Z-H and Cheng Y-R (2021) COVID-19 Vaccination Acceptance Among Healthcare Workers and Non-healthcare Workers in China: A Survey. Front. Public Health 9:709056. doi: 10.3389/fpubh.2021.709056
Received: 13 May 2021; Accepted: 05 July 2021;
Published: 02 August 2021.
Edited by:
Jonathan Ling, University of Sunderland, United KingdomReviewed by:
Fatima Saleh, Beirut Arab University, LebanonChundung Asabe Miner, University of Jos, Nigeria
Copyright © 2021 Wang, Wen, Wang, Zhou, Wang, Ni, Jiang, Zhang, Feng and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong-Ran Cheng, Y2hlbmd5ckB6amFtcy5jb20uY24=; Zhan-Hui Feng, aDk0NTAyMDNAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Ming-Wei Wang
Ming-Wei Wang Wen Wen1†
Wen Wen1† Meng-Yun Zhou
Meng-Yun Zhou Zhan-Hui Feng
Zhan-Hui Feng Yong-Ran Cheng
Yong-Ran Cheng