- 1Department of Orthopedics, Affiliated Hospital of Jiangnan University, Wuxi, Jiangsu, China
- 2Wuxi School of Medicine, Jiangnan University, Wuxi, Jiangsu, China
- 3Department of Endocrinology, Affiliated Hospital of Jiangnan University, Wuxi, Jiangsu, China
- 4Department of Nutrition, Affiliated Hospital of Jiangnan University, Wuxi, Jiangsu, China
Objective: To explore the boost effect on ameliorating functional constipation in elderly patients through empowerment-based, healthy dietary behavioral intervention.
Design: In this randomized parallel group study, elderly patients with functional constipation were recruited and assigned to the experimental and control groups at a ratio of 1:1. The control group received routine intervention. The experimental group received 3-month empowerment-based intervention. The results were evaluated based on the Healthy Lifestyle and Personal Control Questionnaire (HLPCQ) and Cleveland Clinic Constipation Score (CCS). GraphPad Prism (Version 9) software was used for the statistical analysis.
Setting: As the world's population ages, functional constipation in the elderly has attracted widespread attention. The practical behavioral intervention to ameliorate constipation are worth exploring.
Participants: Sixty elderly patients with functional constipation.
Results: The study results showed no significant difference in the baseline data between the two groups (P > 0.05). After the intervention, the scores of HLPCQ (77.90 ± 14.57 vs. 61.11 ± 13.64) and CCS (7.48 ± 3.73 vs. 9.70 ± 3.07) in the experimental group were significantly higher than those in the control group (P < 0.05).
Conclusion: The results showed that empowerment-based intervention can effectively strengthen the healthy dietary behavior of elderly patients. Through patient empowerment, the subjective initiative and willingness to communicate were boosted in the experimental group. Their symptoms of functional constipation improved considerably better than in the control group.
Introduction
Constipation, as one of the geriatric syndromes, affects up to 11.7% of older citizens every year, and its prevalence is still rising (1). The global prevalence of functional constipation without organic lesions is about 8.7–11.6% when Rome IV criteria were used (2). Complications of functional constipation, such as fecal impaction, hemorrhoids and anal fissures, can easily lead to impaired ability to work. About 70% of patients complain that constipation will bring trouble to their daily life and social relations (3). Regardless, no exact cause of functional constipation, which may be the result of multiple factors, has been identified. In general, the potential risk factors associated with functional constipation are not only demographic factors (mainly higher age, women and low education) but also lifestyle factors and behaviors (mainly lacking fiber and liquids) (4). For example, survey results showed that patients have the intention of eating healthily, but they lack a certain level of cognition about dietary choices (5).
Therefore, a concept of empowerment is introduced here. In the medical field, empowerment means that people have the ability to control their own lives and improve their health by enhancing their ability to solve important problems (6). Responding to the challenge of chronic disease, the Chinese government has integrated patient empowerment into chronic disease management programs (7). Intervention based on empowerment theory has been widely used in the management of chronic diseases, such as hypertension (8), chronic kidney disease (9) and diabetes mellitus (10). Nevertheless, the existing health education and empowerment methods for the elderly patients are obscure and boring, and difficult to adhere to for a long time. Dietary intervention is usually listed as the first-line or the first step of treatment for constipation (11), which is also consistent with the Chinese preference for dietary therapy (12). In addition, a high dietary fiber diet has long been recommended for the improvement of constipation (13). Accordingly, this study aimed to empower patients to adopt healthy dietary behaviors by combining the educated demonstration of high-fiber food models and cards, and ultimately achieved the outcome of amelioration of constipation.
Methods
Study design
This randomized parallel group study was conducted at a tertiary hospital in Wuxi, China from 2020 to 2021. The study was single-blinded for the participants but not for the researchers, and a randomized list was generated by a statistician who used a computer to determine the group assignment of every participant. The main outcome indicator was healthy behavior, and the secondary outcome indicators were constipation symptoms. See Figure 1 for the flow chart of this study.
Participants
Sixty participants with functional constipation were recruited from July to October 2020. A total of 30 participants were allocated to the experimental group, which received empowerment-based behavioral intervention for 3 months and 30 participants in the control group were given routine care.
The inclusion criteria were as follows: (1) older adults (more than 65 years of age), (2) the Rome IV criteria for functional constipation including dyssynergic defecation and slow colonic transit, officially published by the American Gastroenterology Association in 2016 (14), (3) availability for telephone follow-up; (4) capability to give written informed consent.
The exclusion criteria were patients (1) with evolving cancer, serious cognitive problems, a psychiatric disease, or a serious medical or health condition that would hinder their ability for defecation, (2) having received abdominal and intestinal surgery, (3) with intestinal obstruction by electronic enteroscopy, (4) with rectal prolapse and internal hemorrhoids rated as grade 3–4 and (5) taking drugs affecting the intestinal motility.
Sample size
The healthy behavioral score of HLPCQ was used to estimate sample size, which was calculated on PASS software (version 15) and based on the following formula: n1 = n2 = [(Z1 – Zα/2 + Z1−β)2 ∗ ( + )]/δ2. In the formula, n1 and n2 are the sample content required by the two groups of samples. In the pilot experiment, the HLPCQ score of the experimental group and control group after intervention were 66.15 ± 13.84 and 46.58 ± 6.36, respectively. The standard deviation σ1 of conventional measures to improve HLPCQ score was about 6, and the standard deviation σ2 of empowerment intervention to improve HLPCQ score was estimated to be 14. If the HLPCQ score was 10 points higher than that of control group after intervention, the intervention was considered to be popularized. Thus, δ = 10. With α = 0.05, β = 0.10, Power = 90%, two-sided test, and checking the statistical table, values of Z1-α/2 = 1.96 and Z1−β = 1.28 were obtained. Therefore, the required number of samples was 26 cases. Considering that the attrition rate was 10%, the actual number of subjects recruited into the groups was 30 cases.
Interventions description
The intervention was mainly based on empowerment theory and was conducted around three elements of empowerment. Patients in the experimental group diagnosed with functional constipation were managed by a constipation treatment panel, which consisted of 6 nurses, 4 doctors and 3 nutritionists who had qualification certificates and rich work experience. In addition, 4 graduate students provided assistance. The research contents to meet the three elements of empowerment were as follows:
(1) Internal factors: improve patients' internal beliefs and attitudes
Patients are encouraged to express their feelings and dietary preferences. Through explanation and goal setting, patients can obtain a clear understanding of functional constipation and establish confidence in overcoming constipation.
(2) Interaction elements: enhances the interaction between patients and the environment and promotes the acquisition of patients' knowledge, skills and resources
Medical staffs and patients worked together to analyse the causes and mainly sorted out the following factors of functional constipation: (1) Medical staff: lack of cooperation of specialized nurses, doctors and nutritionists; (2) patient: the general diet regulation failed, the large adjustment cannot be adhered to and the healthy dietary behavior was poor; (3) methods: lack of individualized home assessment and professional guidance; (4) resources: lack of health education materials for constipation; lack of resources and skills to effectively ameliorate constipation.
The corresponding intervention to promote patient empowerment were as follows: (1) medical staff: establishment of a constipation treatment panel; (2) patient: establishment of a plan based on empowerment theory, interaction with patients by high-fiber food models and cards during health education and testing of patients' knowledge and familiarity diet matching skills; (3) methods: the patients were required to record their 24 h fluid intake, dietary intake, defecation and exercise contents in the healthy dietary behavior log. In addition, health lectures were carried out and a WeChat official account pushed relevant knowledge on the phone; (4) resources: provided patients with paper and electronic education materials and prebiotic food.
(3) Behavior elements: promote patients to adopt healthy dietary behavior
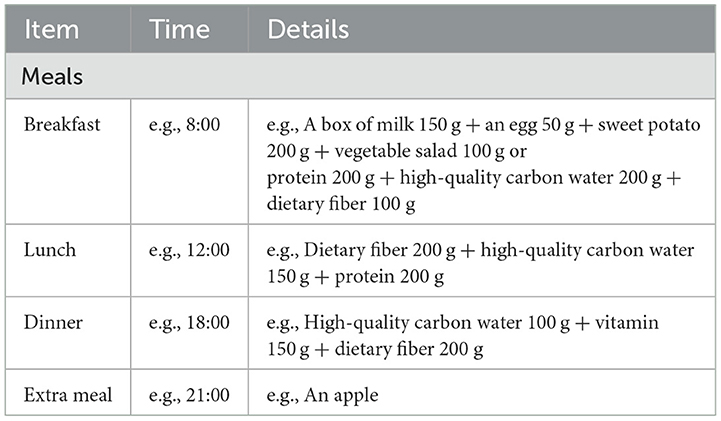
The nutritionist designed the patient's recipe based on the recommended nutrient intake in the Table 1. Health dietary behaviors were logged by patients at home as shown in Table 1 and the medical staff evaluated whether the patient adhered to the health dietary behavior. The total dietary fiber intake recommended by the US Food and drug administration is 20–35 g/day, in which the insoluble and soluble dietary fibers account for 70–75% and 25–30%, respectively (15). On this basis, the doctors provided diet matching demonstration and functional food selection suggestions based on the degree and characteristics of patients' constipation. For example, for patients with normal body mass index (BMI) and without hyperglycaemia, the proportion of insoluble fiber diet from roots and grains must be increased. Patients with high BMI or hyperglycaemia are suggested to increase their intake of soluble fiber diet from apple, kelp and flaxseed. The slightly sweet xylooligosaccharides are given to patients who cannot accept meal replacement powder and fruit and vegetable diets. In this study, xylooligosaccharides were provided to all participants free of charge. The patients followed the recipe and completed a 24-h dietary recall questionnaire. According to the weekly repeated evaluation, the patients were reminded once their diet was not met the requirement of the recommended nutrient intake. In addition, abdominal massage and exercise guidance were the same as those in the control group. In general, the physician's intervention was individualized for each patient and the same treatment was given to each of the subjects included in the study.
Evaluation tools
The Healthy Lifestyle and Personal Control Questionnaire (HLPCQ) was developed by Darviri in 2014, and it focuses on the evaluation of the healthy behavior of patients (16). The total score of HLPCQ was 104 points, with higher scores indicating better behavior of patients in managing their symptoms. It has been reported that the Chronbach's α coefficient of HLPCQ was 0.827, and the result of Bartlett's test of Sphericity was P < 0.001, and the KMO value was 0.797 by Kaiser-Meyer-Olkin measurement, suggesting a good reliability and validity in applying HLPCQ (16). In addition, the Cleveland Clinic Constipation Score (CCS) was designed by the American Gastroenterology Society, and it is used to assess patients' gastrointestinal and anorectal symptoms (17). The total score of CCS was 30 points, with higher scores indicating more severe constipation of patients. The Chronbach's α coefficient of CCS was 0.839, and the result of Bartlett's test of Sphericity was P < 0.001, and the KMO value was 0.831, which confirmed a high reliability in applying CCS (17). The tools were rated using Likert's 5-level points, with higher scores indicating better health behavior and more severe constipation.
Data collection
The distribution and collection of questionnaires were the responsibility of five designated researchers. In order to reduce the bias in the research process, the researchers were able to unify the guidance language and accurately master the knowledge related to functional constipation, scale content and data collection methods. General information about patients can also be obtained through medical care records and archives of the community. Besides, all subjects included in the study completed the 3-month trial, and all data collection was completed.
Statistical analysis
The statistical analysis of the data obtained from the study was performed using GraphPad Prism(Version 9) software. The measurement data with normal distribution were expressed as mean (M) and standard deviation (SD) and a Student's t-test was performed. The enumeration data were statistically described by frequency and percentage and analyzed using the Chi-square test, and P < 0.05 was defined as statistically significant.
Results
Sociodemographic characteristics and medical status
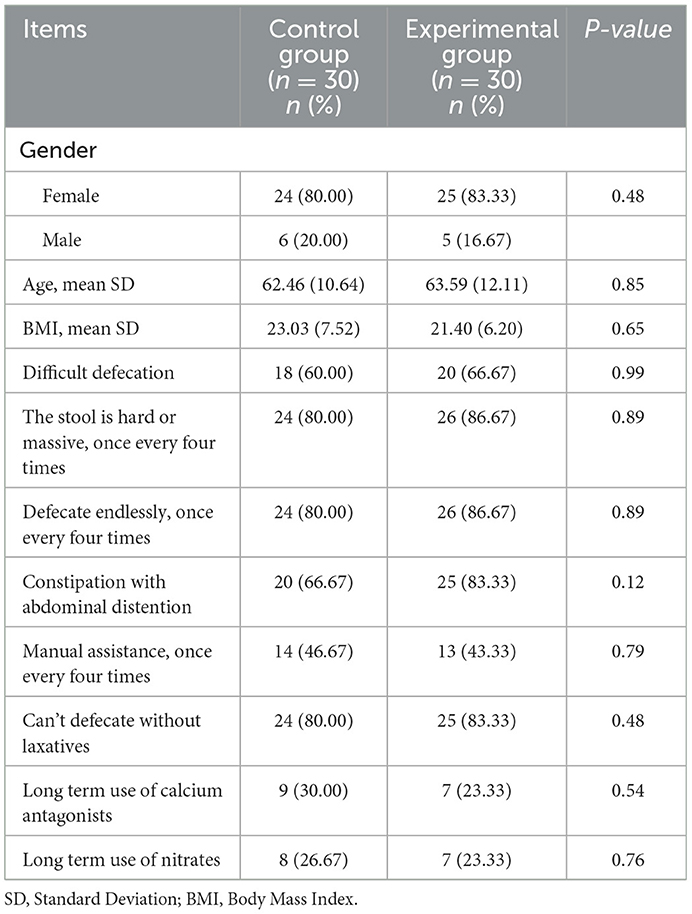
The Table 2 shows that the majority of participants were female, who accounted for 80.00% of the control group and 83.33% of the experimental group. The average age of participants was 67.46 ± 10.64 years in the control group and 68.59 ± 12.11 years in the experimental group. The BMI calculated by height and weight of the two groups was close to 22. More than 80% of the participants defecated hard and massive stool and could not defecate without laxatives. More than 50% of the participants complained about difficult defecation and abdominal distention. More than 23% of participants had taken calcium antagonists and nitrates for a long time. All the differences were not statistically significant in sociodemographic characteristics and medical data (P > 0.05) (Table 2).
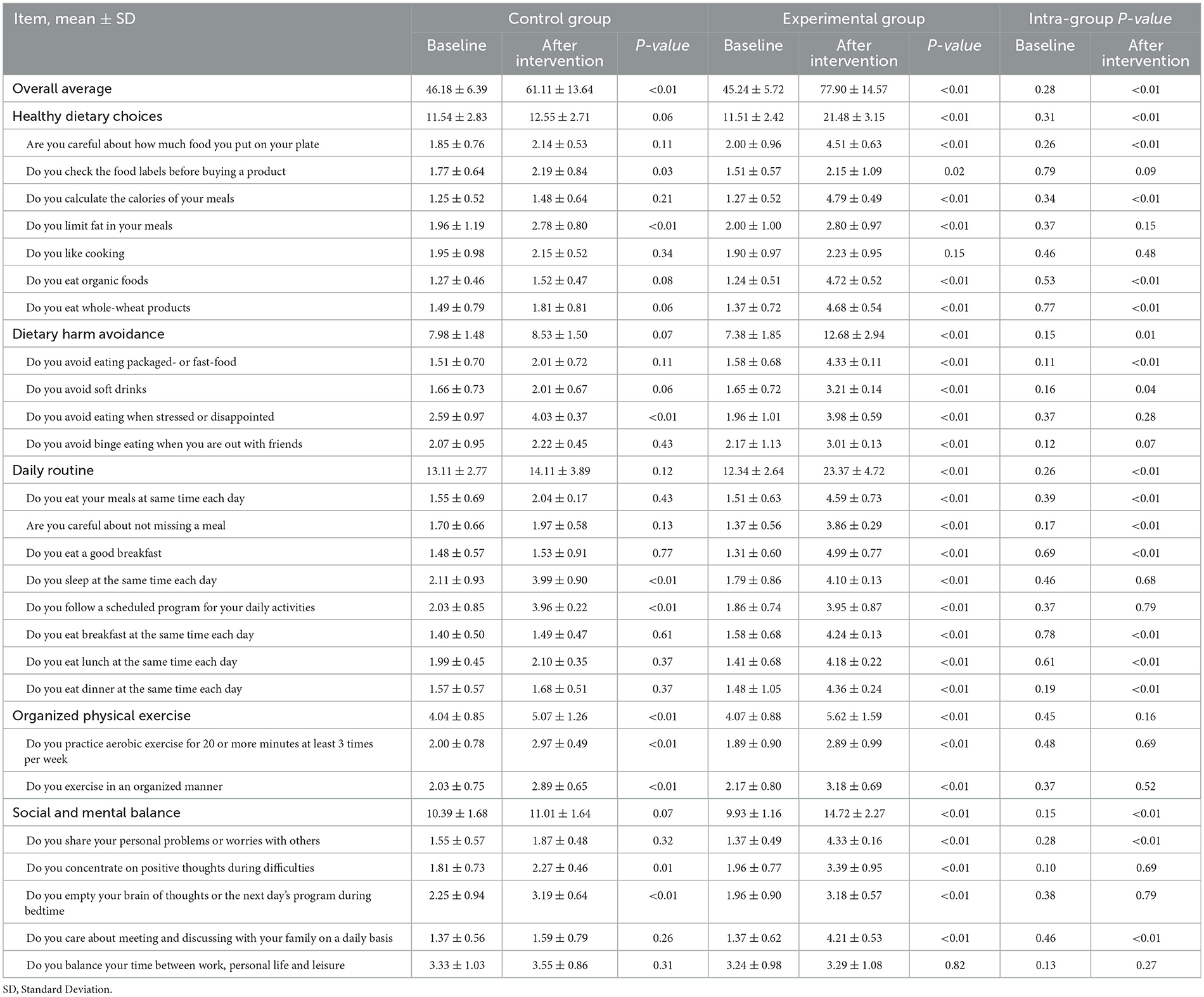
Health dietary behavior improved after the intervention in HLPCQ
Table 3 presents the comparison of healthy behavior of patients with functional constipation in the experimental and control groups. As shown in the Table 3, the scores before and after the intervention for the same patient were compared. Besides, intra-group comparisons were performed, that is, between control and experimental groups at baseline and between control and experimental groups after intervention. No difference was observed in the baseline health behavior between the two groups (P > 0.05). The overall average in the experimental group (77.90 ± 14.57) was significantly greater than that in the control group (61.11 ± 13.64) after the intervention (P < 0.05). The scores in four out of five dimensions, including healthy dietary choices (21.48 ± 3.15 vs. 12.55 ± 2.71), dietary harm avoidance (12.68 ± 2.94 vs. 8.53 ± 1.50), daily routine (23.37 ± 4.72 vs. 14.11 ± 3.89) and social and mental balance (14.72 ± 2.27 vs. 11.01 ± 1.64), showed that the empowerment results of the experimental group were significantly better than those of the control group (P < 0.05). Among these, 14/26 questions received higher scores in the experimental group than in the control group (P < 0.05).
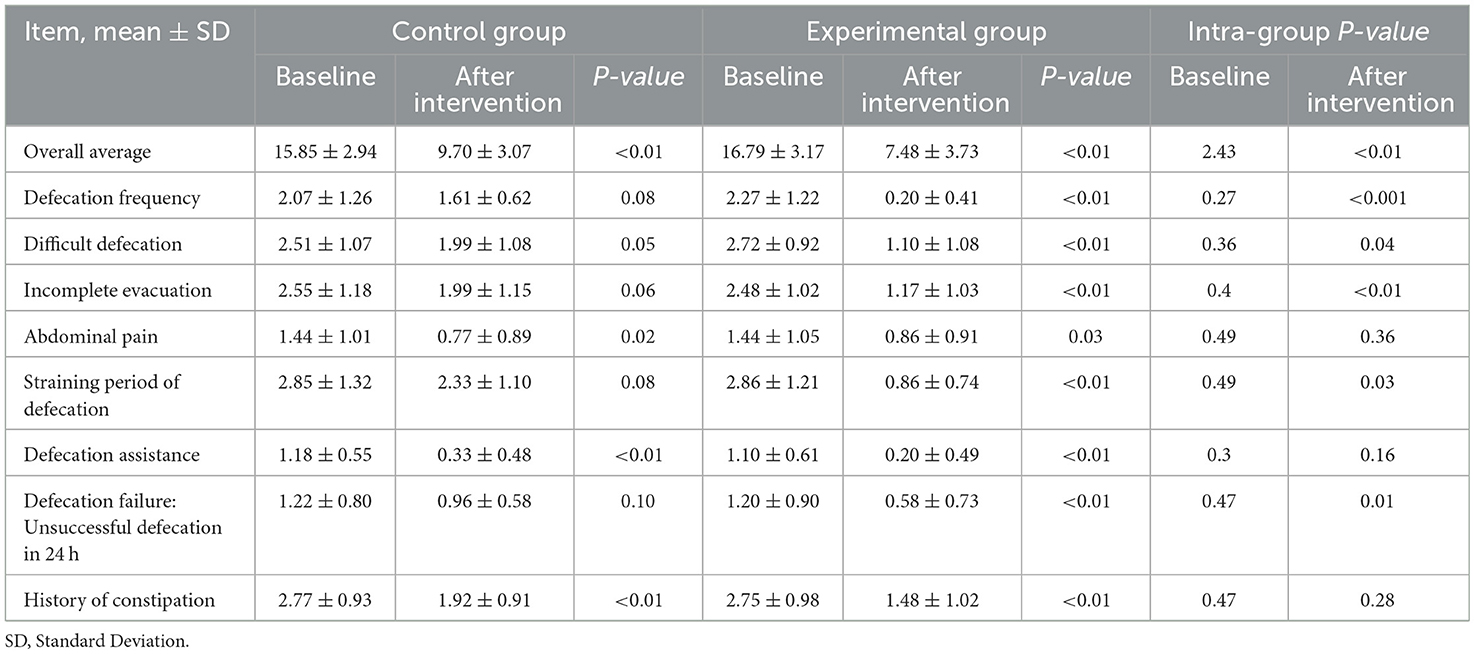
Symptoms of constipation improved after the intervention in CCS
Table 4 shows that no difference was observed in the baseline constipation symptoms between the two groups (P > 0.05). After intervention, the overall mean score of the experimental group decreased to 7.48 ± 3.73, which was less than that of the control group (9.70 ± 3.07) (P > 0.05). Significantly, 5/8 clinical problems, including defecation frequency (0.20 ± 0.41 vs. 1.61 ± 0.62), difficult defecation (1.10 ± 1.08 vs. 1.99 ± 1.08), incomplete evacuation (1.17 ± 1.03 vs. 1.99 ± 1.15), straining period of defecation (0.86 ± 0.74 vs. 2.33 ± 1.10) and defecation failure (0.58 ± 0.73 vs. 0.96 ± 0.58), in the experimental group received lower scores than those in the control group (P < 0.05).
Discussion
In this study, the majority of patients with functional constipation were women, which is consistent with the domestic and international epidemiological data (18). The reason why women are more likely to suffer from functional constipation than men is mainly related to hormones; that is, it may be caused by the decrease in the colonic smooth muscle motility resulting from the increased level of progesterone (19). The average age of the patients was ~68 years old. Studies have shown that as the colonic epithelium and pelvic floor muscle and nerve cells degenerate with age, the intestinal muscle strength and the secretion of intestinal cells decrease (20); thus, the elderly are more prone to constipation. In addition, some participants used calcium antagonists and nitrates, which is consistent with the literature discussing the positive relevance of constipation and cardiovascular disease (21). In addition, the baseline sociodemographic characteristics, healthy behavior and constipation symptoms of the patients with functional constipation showed no difference between the experimental and control groups.
The overall average scores of healthy behavior of 60 patients with functional constipation were lower than Darviri's survey results on the healthy population (16), indicating the poor overall level of lifestyle behavior and personal control of patients with functional constipation in this study and the need to strengthen their healthy behavior, especially in healthy diet choice, avoid diet injury and daily living habits. Healthy diet choice, avoidance of diet injury and daily life management were mainly reflected in the patients' diet management behavior, indicating that a good diet structure has not been formed. A high dietary fiber diet, as a functional food, has been recommended for the treatment and alleviation of constipation by normalizing the structure of intestinal flora to improve the intestinal ecology (22). Therefore, high dietary fiber food models and cards should be used in education demonstrations to promote the empowering effect for patients with functional constipation.
On the basis of the 24-h review, the patient adhered to our recommendations. After the intervention of empowerment-based behavioral intervention, improvements were observed in the patients' healthy dietary behaviors, such as being careful about the amount of food put on their plate, calculating meal calories, consuming organic foods and whole-wheat products and avoiding packaged or fast food. Individuals who do not eat whole grains, fresh fruits and vegetables every day have a high prevalence of constipation (23). In the dimension of daily routine, the patients' meals were usually irregular; they either eat on time, do not eat, or only eat perfunctorily. This irregular behavior is usually related to the patients' lack of awareness and attention to constipation. Moreover, the modern fast-paced lifestyle exacerbates this behavior (24). In addition, the survey on the social and psychological balance dimensions showed that patients with functional constipation rarely share personal problems or concerns with others nor discuss constipation with their families. Some investigations have shown that psychological stress and social disorder easily cause constipation (25, 26) and anxiety tends to have a negative impact on their daily life (27). However, patients in the control group diagnosed with functional constipation were managed by their responsible nurse and doctor, their specific treatment measures were dominated by medical personnel. Through patient empowerment, patients in the experimental group have exhibited stronger desire for knowledge and interpersonal interaction. Their subjective initiative and willingness to communicate were boosted. The results of this study suggest that only when patients are in a positive psychological state will they take on healthy behavior.
The main purpose of patient empowerment is to encourage patients to adopt healthy dietary behavior and the final outcome is the improved symptoms of constipation. Compared with the control group, the constipation symptoms of patients in the experimental group, including defecation frequency, difficult defecation, incomplete evacuation, straining period of defecation and defecation failure, significantly improved. Rasmussen reported that the defecation frequency during daytime is the most prominently associated with health-related quality of life (28). Therefore, empowering patients' health dietary behavior, from a long-term perspective, is conducive to improving patients' constipation symptoms and quality of life. Nevertheless, dealing with a larger scale and different types of patients with functional constipation, how to improve the healthy dietary behavior of patients through high-efficiency empowerment intervention deserves further research. Overall, the results of this study have shown that patient empowerment can strengthen subjective initiative and healthy behavior of elderly patients with functional constipation and promote active participation in self-care. Future research is also recommended to test the effectiveness of the empowerment-based intervention with an educated demonstration among a broad range of population groups.
Conclusion
This study showed that empowerment-based intervention plays a considerable role in improving the healthy dietary behavior of elderly patients with functional constipation. The intervention yielded a significant positive performance in the experimental group, addressed the problems experienced by elderly patients due to functional constipation, resulted in a decreased constipation severity and improved the quality of life. Besides, strengthening the subjective initiative of elderly patients through patient empowerment can reduce patients' over-dependence on medical resources. Therefore, this study provides a non-pharmacological treatment reference for elderly patients suffering from functional constipation.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Wuxi Third People's Hospital (Renamed later as Affiliated Hospital of Jiangnan University) (No. IEC201803001). The patients/participants provided their written informed consent to participate in this study.
Author contributions
XZ, FZ, DL, and JC designed the trial. YX and XZ conducted the study. YX, XZ, DL, and QW analyzed and interpreted the data. XW, FZ, DL, and HC were responsible for project administration and supervision. XW, XZ, FZ, and DL wrote the first draft of the manuscript and had primary responsibility for the manuscript's final content. All authors critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the Natural Science Foundation of Jiangsu Province (SBK2022023007) and Wuxi Municipal Bureau on Science and Technology (2021ZHYB05).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Komiya H, Umegaki H, Asai A, Kanda S, Maeda K, Nomura H, et al. Prevalence and risk factors of constipation and pollakisuria among older home-care patients. Geriatr Gerontol Int. (2019) 19:277–81. doi: 10.1111/ggi.13610
2. Barberio B, Judge C, Savarino EV, Ford AC. Global prevalence of functional constipation according to the Rome criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. (2021) 6:638–48. doi: 10.1016/S2468-1253(21)00111-4
3. Hishida Y, Nagai Y, Tsukiyama H, Nakamura Y, Nakagawa T, Ishizaki S, et al. Effects of elobixibat in patients with diabetes and concomitant chronic constipation: an 8-week, prospective, single-center, single-arm study. Adv Ther. (2022) 39:4205–17. doi: 10.1007/s12325-022-02243-w
4. Otani K, Watanabe T, Takahashi K, Nadatani Y, Fukunaga S, Hosomi S, et al. Prevalence and risk factors of functional constipation in the Rome IV criteria during a medical check-up in Japan. Gastroenterol. (2021) 36:2157–64. doi: 10.1111/jgh.15436
5. Malek L, Umberger WJ, Makrides M, ShaoJia Z. Predicting healthy eating intention and adherence to dietary recommendations during pregnancy in Australia using the Theory of Planned Behaviour. Appetite. (2017) 116:431–41. doi: 10.1016/j.appet.2017.05.028
6. Tengland PJH. Empowerment: a conceptual discussion. Health Care Anal. (2008) 16:77–96. doi: 10.1007/s10728-007-0067-3
7. Xue-Juan W, Hao W, Cai-Ying G, Xin-Ying L, Hong-Yan J, Li W, et al. Impact of an intelligent chronic disease management system on patients with type 2 diabetes mellitus in a Beijing community. BMC Health Serv Res. (2018) 18:821–8. doi: 10.1186/s12913-018-3610-z
8. Jarvis H, Oprinovich S, Guthrie K. Implementation of a self-measured blood pressure program in a community pharmacy: a pilot study. J Am Pharm Assoc. (2022) 62:41–6. doi: 10.1016/j.japh.2021.10.032
9. Kalantar-ZK, Li Philip KT, Tantisattamo E, et al. Living well with kidney disease by patient and care-partner empowerment: Kidney health for everyone everywhere. Patient Educ Couns. (2022) 105:243–45. doi: 10.1016/j.pec.2021.04.039
10. Ching SM, Yee A, Lee PY, Ramachandran V, Shum KM, Ismael NF, et al. Psychometric properties of the Malay version of the diabetes empowerment scale among hospital Serdang type 2 diabetes mellitus patients using exploratory factor analysis. Health Qual Life Outcomes. (2020) 18:23. doi: 10.1186/s12955-020-1280-0
12. Zeng Y, Zhang J, Zhang Y, Men Y, Zhang B, Sun Y. Prebiotic, immunomodulating, and antifatigue effects of konjac oligosaccharide. J Food Sci. (2018) 83:3110–7. doi: 10.1111/1750-3841.14376
13. Lu D, Pi Y, Ye H, Wu Y, Bai Y, Lian S, et al. Consumption of dietary fiber with different physicochemical properties during late pregnancy alters the gut microbiota and relieves constipation in sow model. Nutrients. (2022) 14:124–37. doi: 10.3390/nu14122511
14. Schiller L. Chronic constipation: new insights, better outcomes? Lancet Gastroenterol Hepatol. (2019) 4:873–82. doi: 10.1016/S2468-1253(19)30199-2
15. Kranz S, Dodd KW, Juan WY, Johnson LK, Jahns L. Whole grains contribute only a small proportion of dietary fiber to the U. S Diet Nutr. (2017) 9:1–8. doi: 10.3390/nu9020153
16. Darviri C, Alexopoulos EC, Artemiadis AK, Tigani X, Kraniotou C, Darvyri P, et al. The healthy lifestyle and personal control questionnaire (HLPCQ): a novel tool for assessing self-empowerment through a constellation of daily activities. BMC Public Health. (2014) 14:995. doi: 10.1186/1471-2458-14-995
17. Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. (1996) 39:681–5. doi: 10.1007/BF02056950
18. Chen Z, Peng Y, Shi Q, Chen Y, Cao L, Jia J, et al. Prevalence and risk factors of functional constipation according to the Rome criteria in China: a systematic review and meta-analysis. Front Medi. (2022) 9:815156. doi: 10.3389/fmed.2022.815156
19. Heitkemper M, Jarrett M. Pattern of gastrointestinal and somatic symptoms across the menstrual cycle. Gastroenterol. (1992) 102:505–13. doi: 10.1016/0016-5085(92)90097-I
20. Chandramowlishwaran P, Vijay A, Abraham D, Li G, Mwangi SM, Srinivasan S. Role of sirtuins in modulating neurodegeneration of the enteric nervous system and central nervous system. Front Neurosci. (2020) 14:614331. doi: 10.3389/fnins.2020.614331
21. Ueberall MA, Essner U, Müller-Schwefe G, Horlemann J, Storr M. Prevalence of drug-induced constipation and severity of associated biopsychosocial effects in patients with non-malignant pain: a cross-sectional review of depersonalized data from the German Pain e-Registry. Curr Medi Res Opin. (2021) 1:1–21. doi: 10.1080/03007995.2021.1990032
22. Illippangama AU, Jayasena DD, Jo C, Mudannayake DC. Inulin as a functional ingredient and their applications in meat products. Carbohydr Polym. (2022) 275:118706. doi: 10.1016/j.carbpol.2021.118706
23. Malcomson FC, Willis ND, McCallum I, Xie L, Shivappa N, Wirth MD. Diet-associated inflammation modulates inflammation and WNT signaling in the rectal mucosa, and the response to supplementation with dietary fiber. Cancer Prev Res. (2021) 14:337–46. doi: 10.1158/1940-6207.CAPR-20-0335
24. Huang C, Li X, Wu L, Wu G, Wang P, Peng Y, et al. The effect of different dietary structure on gastrointestinal dysfunction in children with cerebral palsy and epilepsy based on gut microbiota. Brain Dev. (2021) 43:192–9. doi: 10.1016/j.braindev.2020.09.013
25. Hendrix J, Ranginani D, Montero AM, Lockett C, Xu H, James-Stevenson T, et al. Early adverse life events and post-traumatic stress disorder in patients with constipation and suspected disordered defecation. Neurogastroenterol Motil. (2022) 34:e14195. doi: 10.1111/nmo.14195
26. Kayaoglu S, Sert O. Constipation in the period of limited isolation during COVID-19 pandemic. Rev Assoc Med Bras. (2022) 68:196–201. doi: 10.1590/1806-9282.20211007
27. Paans NPG, Gibson-Smith D, Bot M, van Strien T, Brouwer IA, Visser M, et al. Depression and eating styles are independently associated with dietary intake. Appetite. (2019) 13:103–10. doi: 10.1016/j.appet.2018.12.030
Keywords: empowerment, behavior, constipation, intervention, diet
Citation: Wang X, Zhong X, Liu D, Cao H, Chen J, Wang Q, Xia Y and Zhang F (2023) An empowerment-based, healthy dietary behavioral intervention to ameliorate functional constipation. Front. Nutr. 10:1043031. doi: 10.3389/fnut.2023.1043031
Received: 14 September 2022; Accepted: 08 March 2023;
Published: 27 March 2023.
Edited by:
Lilia Castillo-Martinez, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), MexicoReviewed by:
Eva Gabriela Guerrero Cadenas, Superior de Medicina del Instituto Politécnico Nacional, MexicoFarah Sameer Yahya, University of Mosul, Iraq
Copyright © 2023 Wang, Zhong, Liu, Cao, Chen, Wang, Xia and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Zhang, emY5OTU4QDE2My5jb20=
†These authors have contributed equally to this work
 Xuesong Wang
Xuesong Wang Xiaohui Zhong2†
Xiaohui Zhong2† Qinyue Wang
Qinyue Wang Feng Zhang
Feng Zhang