- 1Orthopedics Department, Changzhi People’s Hospital, Changzhi, China
- 2Department of Physical Education, Changzhi University, Changzhi, China
- 3School of Acupuncture and Tuina, Nanjing University of Chinese Medicine, Nanjing, China
Objective: This study aimed to evaluate the effectiveness of ultrasound-guided acupotomy (UgA) in treating Cervical spondylosis (CS), particularly in pain relief, improvement in cervical range of motion (CROM), and overall clinical efficacy, through a systematic review and meta-analysis based on GRADE quality assessment.
Methods: Following PRISMA guidelines, we searched databases including PubMed, Embase, Cochrane Library, Web of Science, and CNKI, Wanfang, Weipu, and Sinomed, identifying 33 randomized controlled trials (RCTs). Inclusion criteria were: patients aged 18–70 with a diagnosis of CS, intervention with UgA, and control groups receiving placebo, physical therapy, or other conventional treatments. Primary outcomes included clinical effective rate and Visual Analog Scale (VAS) for pain, while secondary outcomes encompassed Neck Disability Index (NDI), CROM, and mean flow velocity of vertebral and basilar arteries (MFV-VA/BA). Study quality was assessed using the Cochrane Risk of Bias 2.0 tool, and meta-analysis was conducted using Stata 15.0. The GRADE approach was used to evaluate evidence quality.
Results: Meta-analysis revealed that UgA significantly improved the clinical effective rate compared to control treatments (RR = 1.17, 95% CI: 1.13–1.21), with low heterogeneity (I2 = 12%). UgA also demonstrated significant pain reduction (WMD = −0.96, 95% CI: −1.25 to −0.67), albeit with high heterogeneity (I2 = 91.6%). For secondary outcomes such as NDI, CROM, and MFV-VA/BA, UgA showed moderate improvements, but with considerable heterogeneity. GRADE assessment indicated high-quality evidence for the clinical effective rate, while evidence for VAS, NDI, and CROM was rated as low or very low due to heterogeneity and publication bias.
Conclusion: UgA shows superior efficacy for pain and disability in cervical spondylosis compared to non-UgA and other acupuncture related therapies. However, heterogeneity and potential publication bias exist. It requires skilled practitioners and real-time ultrasound guidance for treatment. Future multinational randomized trials with standardized protocols are needed.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/PROSPERO, PROSPERO CRD42025649835.
Introduction
Cervical spondylosis (CS), or cervical degenerative disc disease, is a prevalent musculoskeletal disorder of the cervical spine1 (1, 2), driven by aging and modern lifestyle factors such as prolonged use of smartphones, computers, and other electronic devices (3). The global prevalence of CS estimated that 30% to 50% of individuals over the age of 40 experience some form of cervical degeneration (4, 5). Furthermore, the disease is considered a significant cause of disability, affecting up to 20% of individuals in their lifetime (5).
CS is characterized by neck pain and stiffness, often accompanied by radicular pain, numbness, tingling, headache, nausea, gastrointestinal discomfort, blurred vision, tinnitus, hypomnesia, palpitations, and, in severe cases, motor and sensory deficits in the upper limbs (2, 6). With aging, degenerative changes develop, including intervertebral disc herniation, osteophyte formation, and ligament calcification. These changes can cause nerve root compression, spinal cord impingement, and inflammation (7). This degeneration results in reduced flexibility of the cervical spine, leading to mechanical stress and causing pain, dysfunction, and neurological deficits (8). Factors such as poor posture, repetitive neck movements, and trauma may accelerate the degenerative process, exacerbating the symptoms of CS (9).
CS can be classified into different clinical subtypes based on the nature and severity of the symptoms. These include cervical axial syndrome, cervical radiculopathy, cervical myelopathy, and cervicogenic headache (10). The clinical presentation can vary significantly depending on the type and location of the degenerative changes. Diagnosis is typically made based on a comprehensive assessment that includes a thorough clinical history, physical examination, and imaging studies, such as x-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans (11). Treatment options for CS include conservative measures such as physical therapy, pharmacological management (analgesics, anti-inflammatory drugs, muscle relaxants), and interventional procedures like epidural steroid injections (12). If conservative treatments fail, surgery may be considered. Options include discectomy and spinal fusion.
Given the limitations of conventional treatments, there has been growing interest in exploring alternative and complementary therapies for CS. One such treatment is acupuncture, which has been used in Traditional Chinese Medicine (TCM) for thousands of years to alleviate pain and promote healing. In recent years, acupuncture techniques have advanced. A modern approach, known as “acupotomy therapy,” has been introduced (13, 14). The procedure involves inserting an acupotomy at the site of pain or spasm to release soft-tissue tension. This improves blood circulation and reduces inflammation (15). Ultrasound-guided Acupotomy (UgA) has shown promise in treating CS and its associated symptoms, such as pain, muscle tension, and reduced mobility (16). The ultrasound guidance ensures accurate localization of the anatomical structures and facilitates the targeting of specific regions of the cervical spine affected by degenerative changes. UgA delivers mechanical stimulation that may restore tissue function by promoting collagen synthesis and activating fibroblasts (17).
Compared with landmark-based (non-guided) acupotomy or other conservative interventions, ultrasound guidance provides real-time visualization of the target soft tissues and adjacent neurovascular structures, enabling more precise release and safer manipulation (18). This precision reduces repeated passes and iatrogenic injury while improving the likelihood of complete adhesiolysis at the affected cervical levels. Despite the promising results of UgA, there remains a lack of consensus regarding its efficacy and safety compared to other conventional treatments. The purpose of this study is to conduct a systematic review and meta-analysis to evaluate the effectiveness of UgA in treating CS, specifically focusing on pain relief, improvement in range of motion, and overall treatment efficacy.
Methods
Study design and protocol
This study adheres to the guidelines established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (19). A systematic review and meta-analysis were conducted to evaluate the effectiveness of UgA therapy in treating CS, focusing on pain relief, improvement in the range of motion, and overall clinical efficacy. The protocol for this systematic review and meta-analysis was registered with PROSPERO (CRD42025649835) prior to the commencement of the study.
Literature search
A comprehensive literature search was performed in the following databases: PubMed, Embase, Cochrane Library, Web of Science, CNKI, Weipu, Sinomed and Wanfang. We searched Mesh terms related to “Ultrasonography” and “Spondylosis”. Then we applied a subject-heading + free-text + near-synonym/variant strategy across title, abstract, and keyword fields, such as “ultrasound”, “ultrasonic imaging”, “ultrasonographic imaging”, “ultrasonics”, “cervical spondylosis”, “cervical syndrome”, “cervical spondylopathy”, “acupotomy”, “acupotomology”, “needle knife”, and “needle-knife”. The search was conducted without language restrictions. The literature search was updated through October 2024. The search strategy for PubMed can be found in Supplementary Material.
Eligibility criteria
Inclusion Criteria:
(1) Study Design: Only randomized controlled trials (RCTs) were included, as RCTs minimize selection bias and provide the highest level of evidence for evaluating intervention efficacy.
(2) Population: Studies must involve human participants aged 18–70 years with a clear diagnosis of CS (20), regardless of the subtype or severity of the disease. Studies that include participants with CS as the primary condition were eligible for inclusion.
(3) Intervention: The intervention must be Ultrasound-guided Acupotomy (UgA) for the treatment of CS. The studies must compare this intervention with a placebo, standard physical therapy, pharmacological treatments, or other conventional therapeutic modalities.
(4) Primary Outcomes: Studies must report at least one of the following primary outcomes:
Efficacy: Improvement in clinical efficacy, as defined by the number of patients achieving “cure,” “significant improvement,” or “effective response.”
Pain Reduction: Changes in Visual Analog Scale (VAS) scores for pain relief.
(5) Secondary Outcomes: Studies must report at least one of the following secondary outcomes:
Neck Disability Index (NDI): Evaluation of functional disability related to CS.
Cervical Range of Motion (CROM): Improvement in the cervical spine's range of motion.
Symptom and Function Assessment (SFA): Assessments that evaluate changes in symptoms and functional status.
Mean Flow Velocity of Vertebral and Basilar Arteries (MFV-VA/BA): Measurement of the average flow velocity in the vertebral and basilar arteries as assessed by Doppler ultrasound or similar techniques.
(6) Publication Type: Studies must be published in peer-reviewed journals with available full-text data. There were no restrictions based on language.
Exclusion Criteria:
(1) Study Design: Studies that are not randomized controlled trials (RCTs) (e.g., observational studies, case series, case reports) were excluded.
(2) Population: Studies that involve participants outside the age range of 18–70 years or those with conditions other than CS were excluded. Studies focusing on subgroups with additional severe comorbidities or disorders unrelated to CS were also excluded.
(3) Intervention: Studies that do not use UgA therapy as an intervention or studies that do not include a valid control group (e.g., placebo, conventional treatments) were excluded.
(4) Outcomes: Studies that do not report on the primary outcomes of efficacy or VAS scores, or fail to report any of the predefined secondary outcomes (NDI, CROM, CASCS, or MFV-VA/BA) were excluded.
(5) Data Quality: Studies that do not provide sufficient data for statistical analysis (e.g., incomplete outcome reporting, lack of baseline or follow-up data) or those with significant methodological flaws that cannot be addressed were excluded.
(6) Publication Type: Conference abstracts, editorials, letters to the editor, and case reports were excluded due to insufficient data for inclusion in a meta-analysis.
Study selection and data extraction
The study selection and data extraction processes were carried out by two independent reviewers (LJ and Z). In the first stage, they screened titles and abstracts, followed by a full-text review in the second stage. Any discrepancies between the reviewers were resolved through discussion, and if consensus could not be reached, a third reviewer (YY) was consulted. Only studies that met the predefined inclusion criteria were included in the final analysis. A flowchart depicting the study selection process was created according to the PRISMA guidelines.
After selecting the studies, the two reviewers independently extracted relevant data using a standardized form. The extracted data included study characteristics such as the first author, year of publication, study design, sample size, and follow-up duration. Patient characteristics, including age, sex, disease duration, and baseline severity of CS, were also collected. Details of the interventions, such as the type of acupotomy therapy, including needle specifications, ultrasound guidance, frequency, and duration of treatment, along with the comparison group (placebo, pharmacological treatment, or physical therapy), were documented. The primary and secondary outcomes were recorded, including pain reduction (measured by VAS), improvement in range of motion, and overall clinical efficacy as reported in terms of cure, significant improvement, or effective response. Lastly, any adverse events related to UgA therapy, such as hematomas or infections, were extracted for analysis.
Risk of bias assessment
The risk of bias in the included studies was assessed using the Risk of Bias 2.0 (ROB 2.0) tool for randomized controlled trials (RCTs) (21). This tool evaluates bias in five key domains: randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results. Each study was assessed for risk of bias in each domain, and classified as having low, high, or some concerns regarding bias. Discrepancies between reviewers were resolved through discussion and consensus.
Statistical analysis
Meta-analysis was conducted using Stata version 15.0. For continuous outcomes (e.g., VAS scores and NDI), the mean difference (MD) with 95% confidence intervals (CI) was calculated. For other continuous outcomes, such as cervical range of motion, standardized mean differences (SMD) were used. For dichotomous outcomes (e.g., clinical efficacy), the risk ratio (RR) with 95% CI was used. All analyses were conducted using a random-effects model. Heterogeneity among studies was assessed using the I2 statistic, with I2 values of 25%, 50%, and 75% indicating low, moderate, and high heterogeneity, respectively. A fixed-effect model was used for data synthesis when heterogeneity was below 50%; otherwise, a random-effects model was applied. Subgroup analyses were performed to explore potential sources of heterogeneity, including study design, type of comparison group, and follow-up duration. Publication bias was evaluated using funnel plots and Egger's test for studies with more than 10 included trials. Sensitivity analysis was conducted by excluding studies with a high risk of bias to assess the robustness of the results.
Certainty of evidence
The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach was used to assess the certainty of evidence for the primary outcomes (22). The quality of evidence was rated as high, moderate, low, or very low, based on factors such as study limitations, inconsistency, indirectness, imprecision, and publication bias.
Results
Included studies and basic characteristics
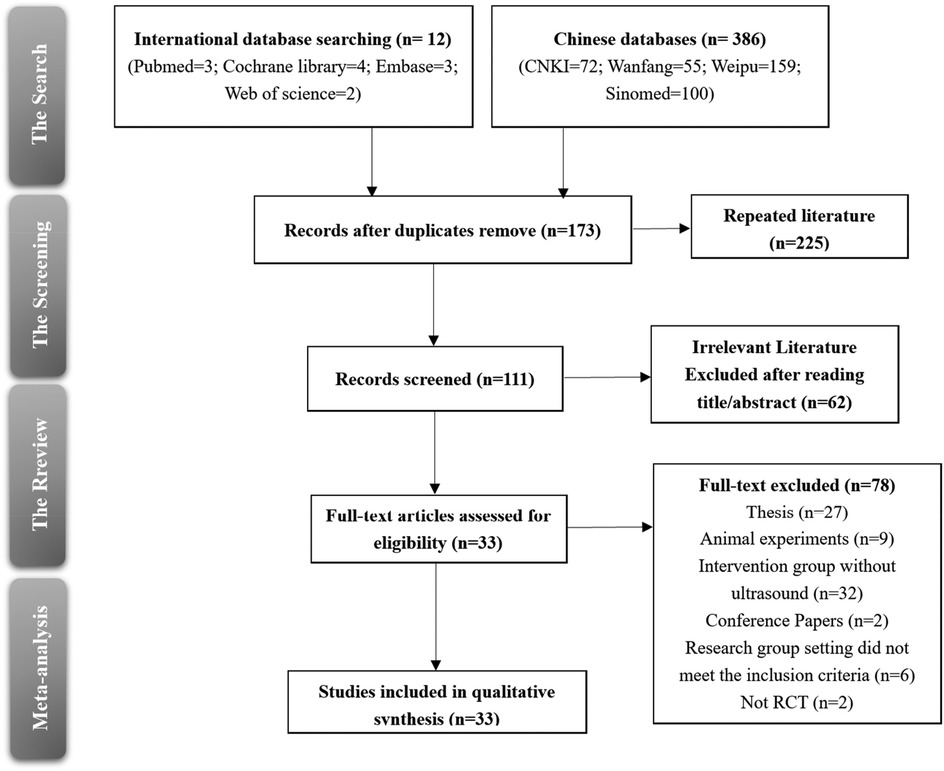
In this systematic review, a total of 33 randomized controlled trials (RCTs) were included after a thorough screening and selection process. The search initially yielded 12 records from international databases (PubMed, Cochrane Library, Embase, and Web of Science) and 386 records from Chinese databases (CNKI, Wanfang, Weipu, and Sinomed). After removing duplicates, 173 records were retained for further screening. Of these, 111 records were reviewed, and 33 studies met the inclusion criteria for qualitative synthesis (Figure 1).
The included studies focused on the effect of UgA interventions for CS compared to various control treatments. The characteristics of the participants in these studies ranged from 20 to 100 individuals per trial, with a mean age ranging from 34 to 79 years. The majority of participants were middle-aged and older adult individuals, reflecting the typical demographic affected by CS. The specific characteristics of the study are shown in Table 1.
The interventions in the included studies involved UgA, non- UgA, and combinations with other therapies such as pulsed radiofrequency (PRF), traction, and traditional Chinese medicine (TCM). In the studies by Pu et al. (23), Cai et al. (24), Du et al. (27), and Deng et al. (25), the control groups received ultrasound-guided nerve root block (UgNRB) treatment. Additionally, in the studies by Fu and Huang (28), Zhang and Yao (51), and Huang et al. (31), the control groups received non-ultrasound-guided acupotomy or acupotomy procedures. Other studies, such as those by Wang et al. (46) and Luo et al. (42), involved comparison with combinations of non-ultrasound-guided acupotomy and other therapies, such as PRF and traction. The interventions ranged from 2 to 8 weeks, with treatment durations and frequencies varying across studies. All trials reported at least one primary outcome.
Risk of bias results
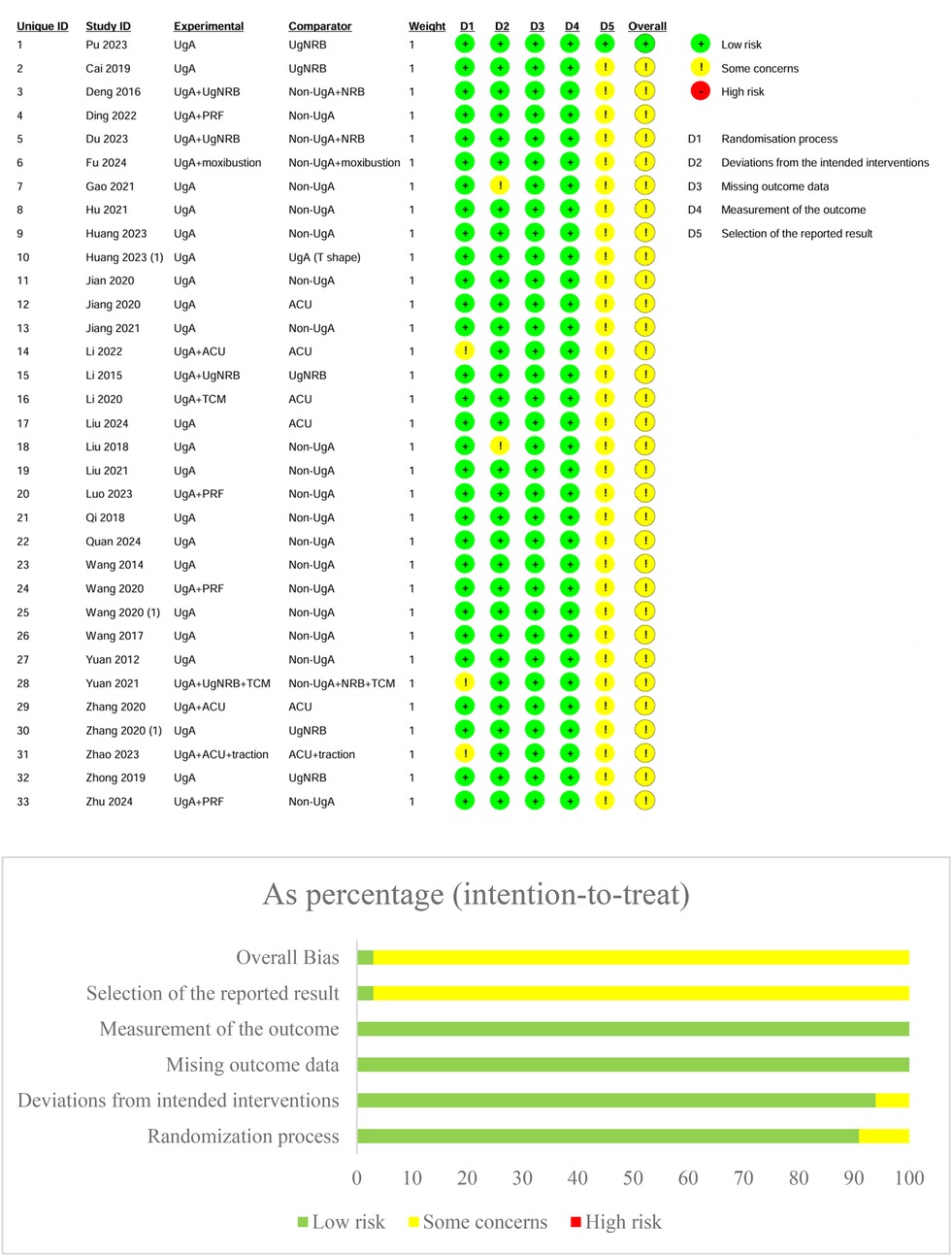
The risk of bias in the included studies was assessed using the Cochrane Risk of Bias 2.0 tool. In terms of the randomization process, the majority of studies were classified as having low risk [e.g., Pu et al. (23), Cai et al. (24), Deng et al. (25)], although some studies raised concerns regarding randomization, especially when allocation concealment was unclear [e.g., Jiang and Ke (35)]. The deviations from intended interventions domain showed that most studies adhered to the interventions as planned, with minimal concerns or high-risk deviations in a few cases [e.g., Du et al. (27)]. Regarding missing outcome data, a few studies had incomplete data, raising concerns [e.g., Li and Cheng (38), Yuan et al. (50)], though the majority maintained low risk. For measurement of outcomes, most studies used appropriate, blinded methods for outcome assessment, but a few studies raised concerns over the risk of detection bias [e.g., Zhang and Yao (51), Huang et al. (31)]. Selection of the reported results generally had low risk (Figure 2).
Meta-analysis of effective rate
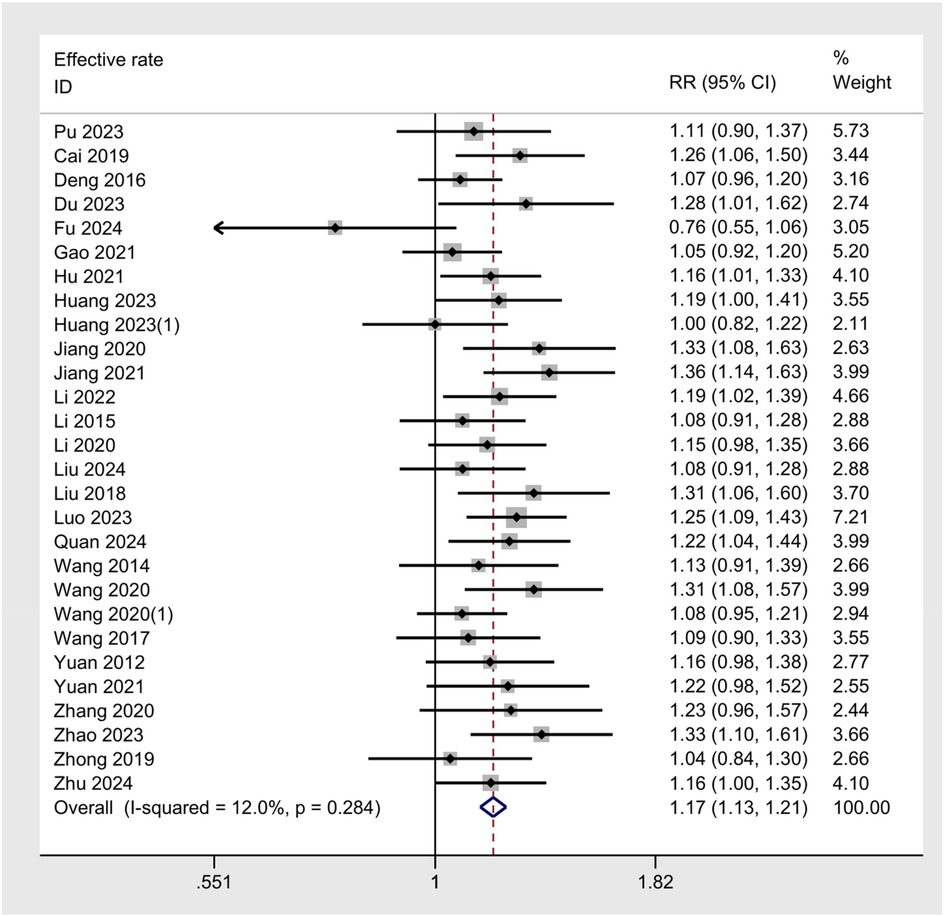
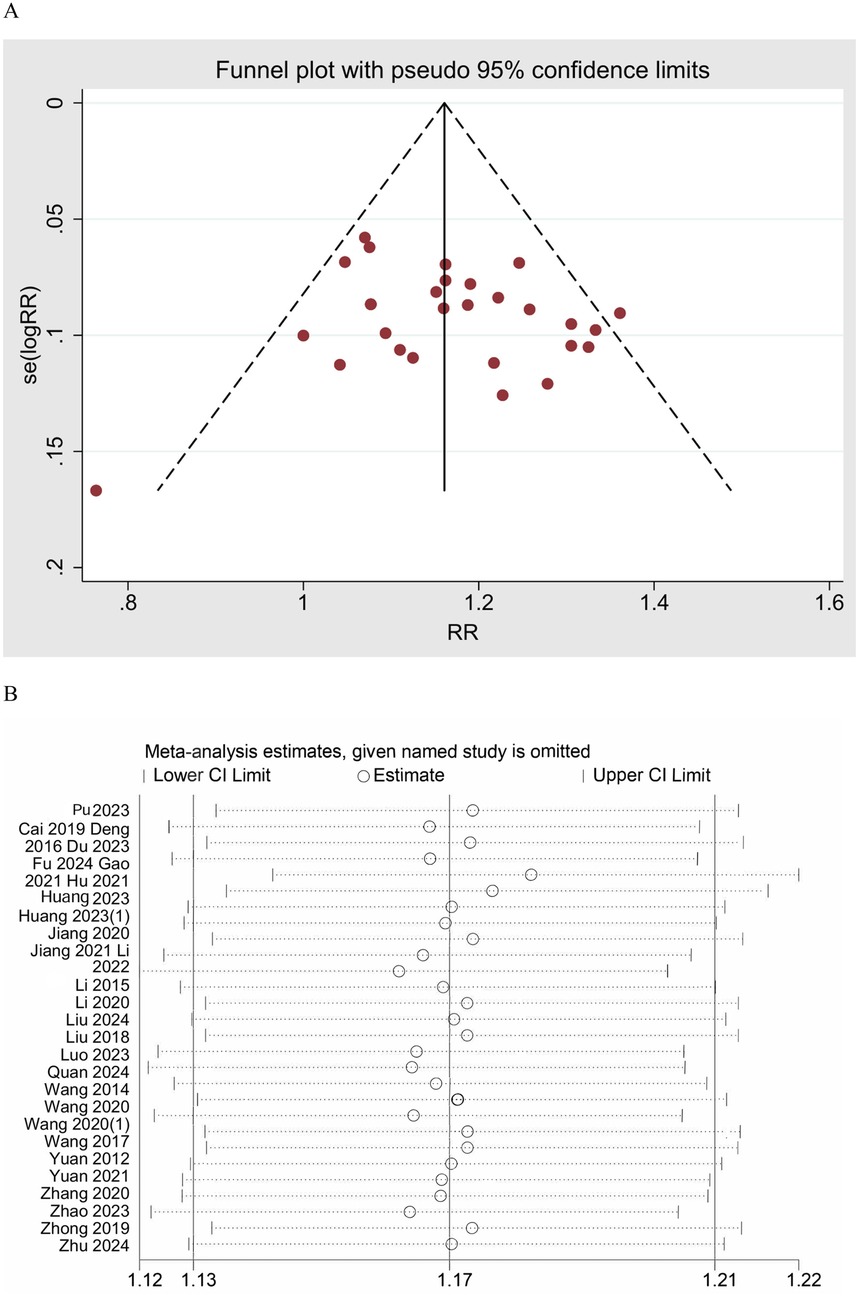
The meta-analysis of the effective rate across 28 studies yielded a pooled RR of 1.17 (95% CI: 1.13–1.21, z = 8.8, p < 0.001), indicating a statistically significant improvement in the effective rate for UgA compared to control treatments (Figure 3). The I2 value was 12.0%, indicating good consistency between studies. A funnel plot was generated to assess publication bias, and no clear asymmetry was observed, suggesting a low risk of bias in the published studies (Figure 4A). Additionally, sensitivity analysis was performed by sequentially omitting individual studies, and the pooled effect estimate remained stable, further supporting the robustness of the results. (Figure 4B)
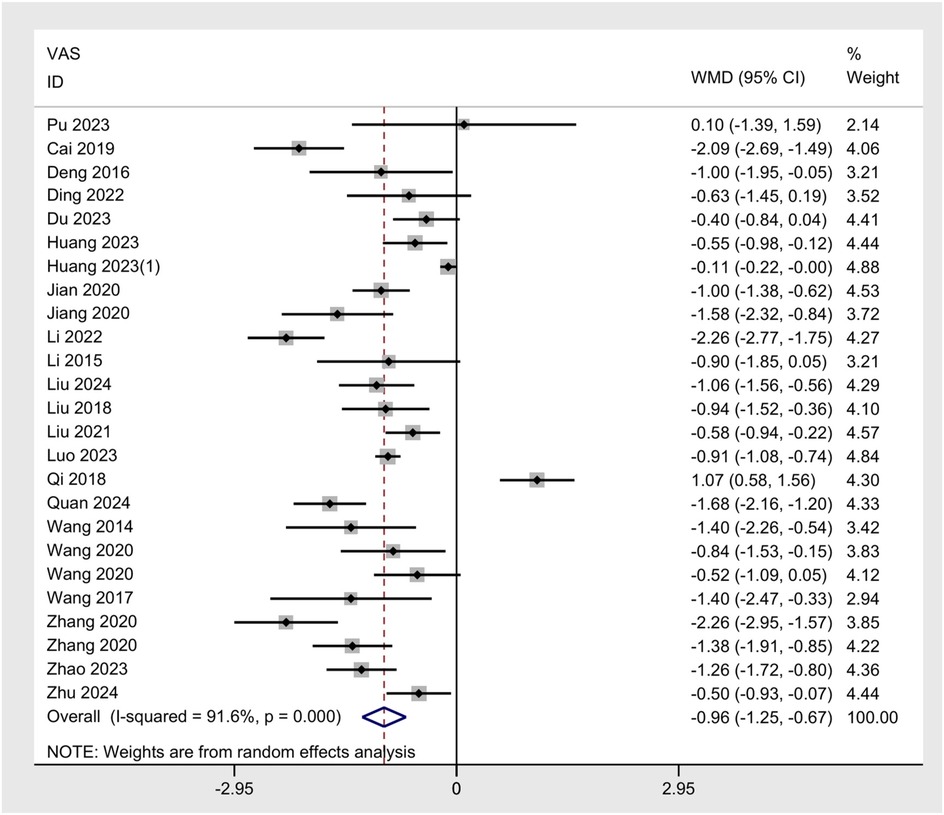
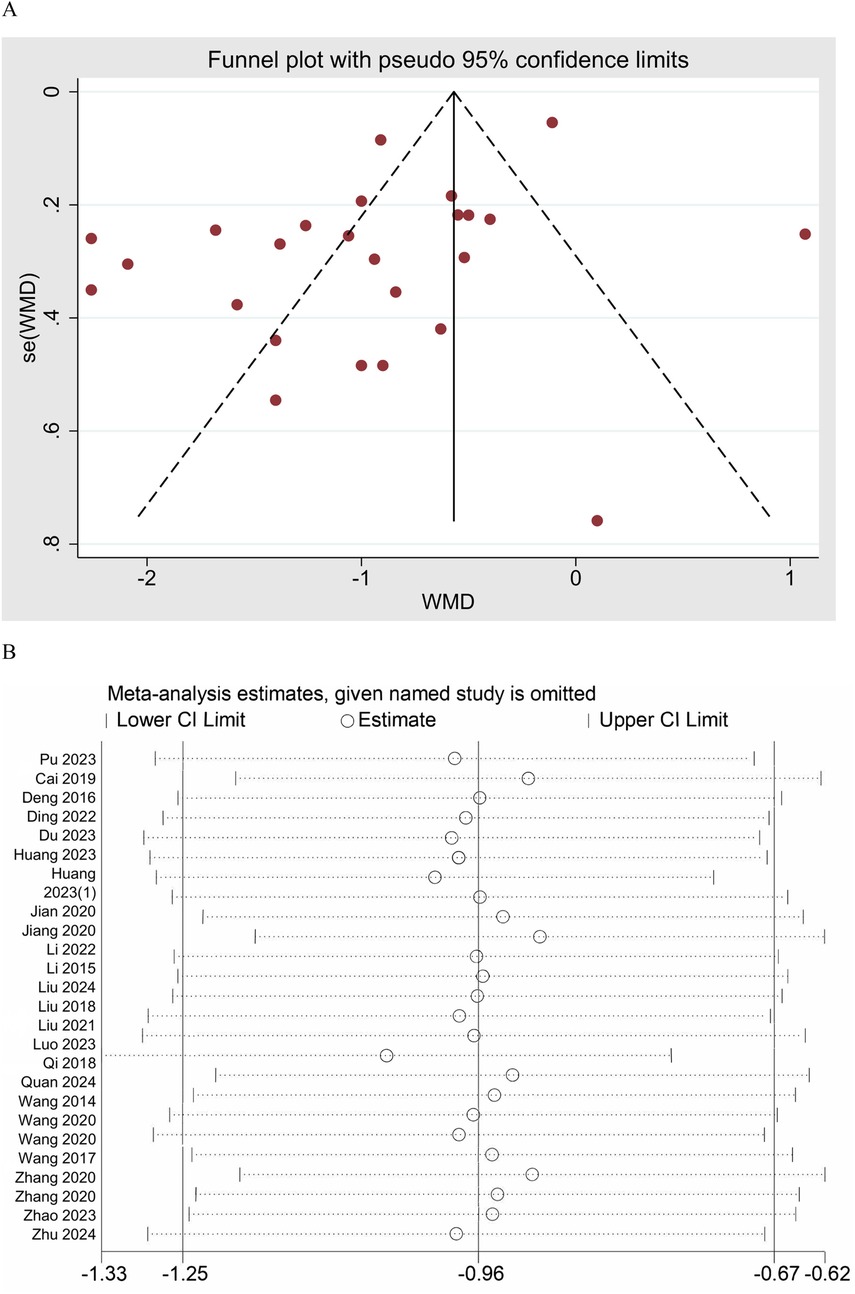
Meta-analysis of VAS scores
The meta-analysis of the VAS across 25 studies demonstrated a significant reduction in pain intensity following UgA compared to control interventions. The pooled WMD was −0.96 (95% CI: −1.25 to −0.67), indicating that the UgA group can significantly reduce VAS scores compared to the control group (Figure 5). Substantial heterogeneity was observed across the model, with an I2 value of 91.6%. Publication bias was assessed using both Begg's and Egger's tests. Begg's test showed no significant bias (p = 0.889), and Egger's test suggested the presence of some bias (p = 0.007), indicating potential small-study effects (Figure 6A). The trim and fill method did not impute any missing studies. The sensitivity analysis showed that excluding individual studies did not significantly alter the pooled estimate (Figure 6B).
Meta-analysis of NDI scores
The meta-analysis of NDI scores from 10 studies showed a pooled WMD of −4.55 (95% CI: −6.72 to −2.39), indicating significant improvement in disability. High heterogeneity was observed (I2 = 94.4%). Publication bias was not significant (Begg's p = 0.929, Egger's p = 0.186). Sensitivity analysis confirmed the robustness of the results.
Meta-analysis of CROM
The meta-analysis on CROM of 10 studies revealed a pooled SMD of 0.96 (95% CI: 0.60–1.31), indicating a significant improvement in cervical flexibility following UgA. However, substantial heterogeneity was observed, with an I-squared value of 84.5%, suggesting high variability across studies. To assess publication bias, Begg's test indicated significant bias (p = 0.009), while Egger's test showed no significant bias (p = 0.459). The trim and fill analysis imputed one missing study to address asymmetry, resulting in an adjusted random-effects estimate of SMD = 0.80 (95% CI: 0.40 to 1.21), which remained statistically significant. Sensitivity analysis revealed that the pooled estimate remained robust after omitting individual studies.
Meta-analysis of SFA
The meta-analysis of SFA across 8 studies yielded a pooled SMD of 1.33 (95% CI: 0.85–1.81), indicating a significant improvement in symptom and functional outcomes following ultrasound-guided needling compared to controls. High heterogeneity was observed with an I2 value of 87.9%. Begg's test indicated potential publication bias (p = 0.013), and Egger's test suggested the presence of bias (p = 0.016). The trim and fill method imputed 2 potentially missing studies to adjust for publication bias. The adjusted random-effects estimate decreased from SMD = 1.33 to SMD = 1.05 but remained statistically significant, suggesting that the original effect may have been overestimated yet robust. Sensitivity analysis, excluding individual studies, confirmed the stability of the pooled estimate.
Meta-analysis of MFV-VA/BA
The meta-analysis of MFV-VA revealed a pooled SMD of 1.13 (95% CI: 0.61, 1.64), suggesting the difference between the UgA group and the control group was statistically significant. Significant heterogeneity was observed (I2 = 87.8%). Begg's test (p = 0.573) and Egger's test (p = 0.262) did not indicate significant publication bias. Sensitivity analysis showed stable results. The meta-analysis of MFV-BA indicated a pooled SMD of 1.83 (95% CI: 0.76, 2.91), suggesting the difference was statistically significant. Notable heterogeneity was found (I2 = 95.9%). Publication bias was not detected by Begg's test (p = 1.000) and Egger's test (p = 0.928). The results remained consistent through sensitivity analysis.
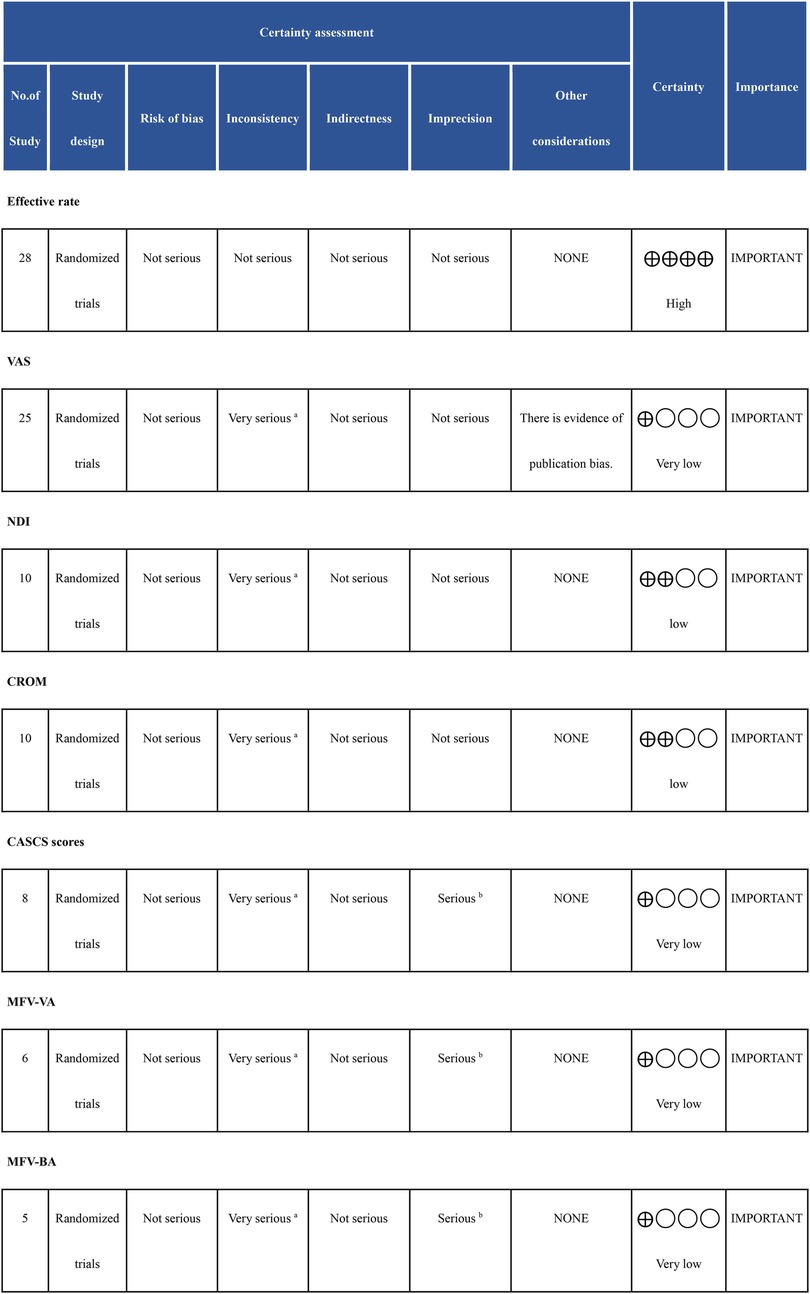
GRADE assessment
For the effective rate across 28 randomized trials, the certainty of evidence is high. There were no serious concerns regarding risk of bias, inconsistency, indirectness, or imprecision. In contrast, the certainty of evidence for the VAS, based on 25 randomized trials, was rated as very low. This downgrading was primarily due to serious inconsistency, as indicated by an I2 > 70%. Additionally, publication bias was identified, which further impacts the robustness of the evidence. For the NDI and CROM, both based on 10 randomized trials, the certainty of evidence is low. The primary concern was serious inconsistency (I2 > 70%), though there were no issues related to bias or imprecision. Outcomes such as SFA, MFV-VA, and MFV-BA, based on small sample sizes (8, 6, and 5 studies, respectively), also received a very low certainty rating. The reasons for downgrading included serious inconsistency and serious imprecision due to the small sample sizes and significant variability in the studies. These outcomes are still considered important but with very low certainty in their findings (Figure 7).
Discussion
Our results demonstrates that UgA provides significant clinical benefits across multiple outcomes in cervical spondylosis. UgA significantly increased the effective rate, reduced pain intensity, and improved neck disability. Secondary outcomes confirmed notable improvements in cervical range of motion, symptoms and function, and vertebral-basilar artery hemodynamics. These findings are consistent with prior literature, confirming its positive impact (56–58). This study presents the first meta-analysis on the effects of UgA on vertebrobasilar artery blood flow velocity, seeking to elucidate potential mechanisms of this therapy. The results observed increase in vertebrobasilar artery blood flow velocity following UgA treatment. Physiologically, increases in vertebrobasilar flow could plausibly reflect improved regional perfusion and reduced ischemia of pain-generating soft tissues, thereby supporting symptom relief (59). This may be particularly beneficial for patients with cervical spondylosis who often experience vertebrobasilar insufficiency due to mechanical compression or sympathetic stimulation (60). UgA may not only address musculoskeletal dysfunction but also promote neurovascular recovery.
The consistently high heterogeneity observed in most outcomes raises important methodological considerations. This variability may reflect fundamental differences in treatment protocols, including acupoint selection, treatment frequency, and technique, as well as divergent outcome assessment methods. Furthermore, some results were detected potential publication bias, especially in patient-reported outcomes like VAS, underscores the need for cautious interpretation. These factors collectively diminish the certainty of the evidence and highlight an imperative for more rigorously designed. Implications for practice are therefore cautious. Where ultrasound equipment and trained operators are available, UgA may be considered for patients with pain and mobility limitations, with shared decision-making that prioritizes outcomes meaningful to patients (pain, function, return to activity).
Most trials assessed outcomes immediately or shortly after treatment, providing robust evidence for acute efficacy but insufficient data on long-term sustainability. Future research incorporating prolonged follow-up periods is essential to determine the persistence of benefits in pain relief, functional improvement, and hemodynamic changes. Establishing the long-term efficacy will be crucial for positioning UgA within chronic management strategies.
As most included trials were conducted in China, the generalizability of the findings to other health systems may be limited. Contextual factors such as differences in provider training, access to ultrasound equipment, usual care practices, and patient attitudes toward TCM could influence the outcomes and applicability of UgA elsewhere. Clinicians outside China should consider local feasibility and prioritize patient-centered outcomes such as pain, function, and quality of life when evaluating UgA.
Conclusion
UgA has a higher overall efficacy compared to non-UgA and other complementary alternative therapies such as traditional acupuncture, and is beneficial for pain and disability. However, substantial heterogeneity and suspected publication bias reduce certainty. In practice, UgA may be considered for adults with CS who remain symptomatic with restricted cervical motion after conservative care, in settings with real-time ultrasound and trained operators. Future work should comprise preregistered, multicenter randomized trials—including sites outside China—with standardized UgA parameters, clearly defined comparators, blinded outcome assessment, and complete adverse events reporting.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
ZL: Writing – original draft, Writing – review & editing. ZZ: Writing – original draft. YY: Writing – original draft. ZN: Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2025.1654265/full#supplementary-material
References
1. Rao RD, Currier BL, Albert TJ, Bono CM, Marawar SV, Poelstra KA, et al. Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management. J Bone Joint Surg. (2007) 89(6):1360–78. doi: 10.2106/00004623-200706000-00026
2. Rao R. Neck pain, cervical radiculopathy, and cervical myelopathy: pathophysiology, natural history, and clinical evaluation. J Bone Joint Surg Am. (2002) 84(10):1872–81. doi: 10.2106/00004623-200210000-00021
3. Chu EC. Preventing the progression of text neck in a young man: a case report. Radiol Case Rep. (2022) 17(3):978–82. doi: 10.1016/j.radcr.2021.12.053
4. Fehlings MG, Tetreault L, Nater A, Choma T, Harrop J, Mroz T, et al. The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery. (2015) 77:S1–5. doi: 10.1227/NEU.0000000000000953
5. Lv Y, Tian W, Chen D, Liu Y, Wang L, Duan F. The prevalence and associated factors of symptomatic cervical Spondylosis in Chinese adults: a community-based cross-sectional study. BMC Musculoskelet Disord. (2018) 19:1–12. doi: 10.1186/s12891-018-2234-0
6. Chu EC. Cervical radiculopathy as a hidden cause of angina: cervicogenic angina. J Med Cases. (2022) 13(11):545–50. doi: 10.14740/jmc4025
7. Fotakopoulos G, Georgakopoulou V, Lempesis I, Papalexis P, Sklapani P, Trakas N, et al. Pathophysiology of cervical myelopathy. Biomed Rep. (2023) 19(5):84. doi: 10.3892/br.2023.1666
8. Iorio JA, Jakoi AM, Singla A. Biomechanics of degenerative spinal disorders. Asian Spine J. (2016) 10(2):377. doi: 10.4184/asj.2016.10.2.377
9. Baucher G, Taskovic J, Troude L, Molliqaj G, Nouri A, Tessitore E. Risk factors for the development of degenerative cervical myelopathy: a review of the literature. Neurosurg Rev. (2022) 45(2):1675–89. doi: 10.1007/s10143-021-01698-9
10. Rhee JM, Yoon T, Riew KD. Cervical radiculopathy. J Am Acad Orthop Surg. (2007) 15(8):486–94. doi: 10.5435/00124635-200708000-00005
11. Hussain S, Mubeen I, Ullah N, Shah SSUD, Khan BA, Zahoor M, et al. Modern diagnostic imaging technique applications and risk factors in the medical field: a review. BioMed Res Int. (2022) 2022(1):5164970. doi: 10.1155/2022/5164970
12. Al-Mutairi AMF, Almutairi STF, Alruaidan AR, Almutairi DM, Alqthami AMG. Cervical spondylosis: innovative techniques for physical therapy-an updated review. J Ecohumanism. (2024) 3(8):13195–209. doi: 10.62754/joe.v3i8.6215
13. Yoon S-H, Kwon C-Y, Jo H-G, Sul J-U, Lee H, Won J, et al. Safety of acupotomy in a real-world setting: a prospective pilot and feasibility study. J Integr Med. (2022) 20(6):514–23. doi: 10.1016/j.joim.2022.08.003
14. Luan GR, Shang X, Meng DH, Liu CB, Luo SY, Yang YH, et al. Ultrasound-guided acupotomy release combined with corticosteroid injection for carpal tunnel syndrome: a multicenter retrospective study. Asian J Surg. (2025) 48(10):6054–61. doi: 10.1016/j.asjsur.2025.06.066
15. Qiu Z, Jia Y, Shen Y, Zhou Q, Sun X, Zhu X, et al. Acupotomy by an ultrasound-guided technique: a protocol for a systematic review. Medicine (Baltimore). (2019) 98(42):e17398. doi: 10.1097/MD.0000000000017398
16. Liang Y-s, Chen L-y, Cui Y-y, Du C-x, Xu Y-x, Yin L-h. Ultrasound-guided acupotomy for trigger finger: a systematic review and meta-analysis. J Orthop Surg Res. (2023) 18(1):678. doi: 10.1186/s13018-023-04127-3
17. Hu J, Tong H, Zhang J, Jiang L. Acupotomy for musculoskeletal pain: exploring therapeutic potential and future directions. J Pain Res. (2025) 18:3027–36. doi: 10.2147/JPR.S518705
18. Bader KB, Padilla F, Haworth KJ, Ellens N, Dalecki D, Miller DL, et al. Overview of therapeutic ultrasound applications and safety considerations: 2024 update. J Ultrasound Med. (2025) 44(3):381–433. doi: 10.1002/jum.16611
19. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. (2010) 8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007
20. Theodore N. Degenerative cervical spondylosis. N Engl J Med. (2020) 383(2):159–68. doi: 10.1056/NEJMra2003558
21. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken: Wiley (2019). p. 4.
22. Schünemann HJ, Mustafa RA, Brozek J, Steingart KR, Leeflang M, Murad MH, et al. GRADE Guidelines: 21 part 2. Test accuracy: inconsistency, imprecision, publication bias, and other domains for rating the certainty of evidence and presenting it in evidence profiles and summary of findings tables. J Clin Epidemiol. (2020) 122:142–52. doi: 10.1016/j.jclinepi.2019.12.021
23. Pu J, Cao W, Chen Y, Fan Y, Cao Y. Ultrasound-guided injection acupotomy as a minimally invasive intervention therapy for cervical spondylotic radiculopathy: a randomized control trial. Ann Med. (2023) 55(1):2233556. doi: 10.1080/07853890.2023.2233556
24. Xiaoshan C, Yijin R, Xiangping L, Zhaoli L, Xiaoling Z. Clinical observation of ultrasound-guided acupotomy for cervical nerve root release in the treatment of cervical spondylotic radiculopathy. J Hubei Univ Trad Chinese Med. (2019) 21(05):101–4.
25. Fang D, Qinghua L, Ying L, Zhikai L, Liang Y, Jianliang S. Observation on the efficacy of ultrasound-guided acupotomy release in the treatment of cervical spondylotic radiculopathy. Zhejiang J Traumat Surg. (2016) 21(02):206–8. doi: 10.3969/j.issn.1009-7147.2016.02.002
26. Ding D, Chen S, Li R. Effects of ultrasound-guided cervical nerve root pulsed radiofrequency combined with acupotomy on pain and cervical joint mobility in elderly patients with cervical spondylotic radiculopathy. Chin J Gerontol. (2022) 42(07):1666–70. doi: 10.3969/j.issn.1005-9202.2022.07.038
27. Wei D, Yu D, Feng L, Tusheng L, Wen L, He R, et al. Efficacy observation of ultrasound-guided acupotomy combined with nerve root block in the treatment of cervical spondylotic radiculopathy. Chin J Pain Med. (2023) 29(12):948–52.
28. Fu C, Huang Y. Clinical study on musculoskeletal ultrasound-guided acupotomy combined with heat-sensitive moxibustion in the treatment of cervical spondylotic radiculopathy. Mod Diagn Treat. (2024) 35(15):2232–3. +2236. https://kns.cnki.net/kcms2/article/abstract?v=6VlBgy5--50i2KjSxSyp9p7AZTEvsGrRKkfTQHvaAgrz5A2ORMQGXZTWuHYKmmpNw4uJD9dLxKBxf3s4MPSrBcZ0D4XZxzhvip8Bq1vi7x0AA8oKw8ltj7rvR9_uPwkgZv_jTs-bE2RcKkTYizA-rCjW8RDcNs6pfj5o85hukgBTMKsazXFaFA==&uniplatform=NZKPT&language=CHS
29. Gao X, Zhang S. Clinical study on musculoskeletal ultrasound-guided blade needle release in the treatment of cervical spondylotic radiculopathy. Hebei J Tradit Chin Med. (2021) 43(04):662–5. doi: 10.3969/j.issn.1002-2619.2021.04.030
30. Hu N. Study on the therapeutic effect of ultrasound-guided cervical nerve root acupotomy release in the treatment of cervical spondylotic radiculopathy. Chin J Trauma Disability Med. (2021) 29(20):38–9. doi: 10.13214/j.cnki.cjotadm.2021.20.023
31. Na H, Zhanping L, Yanwei W, Zhantao Z, Yangfu L. Effects of ultrasound-guided acupotomy soft tissue release on pain and cervical mobility in patients with cervical spondylosis. Shenzhen J Integr Tradit Chin West Med. (2023) 33(13):25–8. doi: 10.16458/j.cnki.1007-0893.2023.13.008
32. Yuebin H, Zeyu W, Lingling Z, Changyin J, Juan Z, Runze T, et al. Efficacy observation of ultrasound-guided acupotomy based on “neck-sacrum simultaneous treatment” for cervical spondylosis. Her Med. (2023) 29(10):60–4. doi: 10.13862/j.cn43-1446/r.2023.10.011
33. Jian F, He J, Yi K. Clinical value of ultrasound-guided acupotomy in the release of cervical facet joints. Kang Yi. (2020) (19):184. doi: 10.12332/j.issn.2095-6525.2020.19.182
34. Hao JZ, Yun JL, Hua TZ, Jun K, Li Z. Clinical study on ultrasound-guided acupotomy for vertebral artery type cervical spondylosis guided by meridian theory. Contemp Med. (2020) 26(21):124–6. doi: 10.3969/j.issn.1009-4393.2020.21.048
35. Jiang Z, Ke J. Ultrasound-guided acupotomy for vertebral artery type cervical spondylosis: a report of 50 cases guided by meridian theory. J Jiangxi Univ Tradit Chinese Med. (2021) 33(04):69–72. https://kns.cnki.net/kcms2/article/abstract?v=6VlBgy5--52-Pv-a_Os89wiOLJ1szRjqlW7KwWCUoB4HCPliCnVEWHIASFdtsEIbNan6N72ZCUGT1iV5utyEGsKeQyGvNbuljYrBgXZbjwZ7GpmADzPERu41kWB9UNfaP2ArDPKdBJlsy0sdCxlmyGoeJ5N1S20WoJR8Z7J2udj1XXjUGCwnHw==&uniplatform=NZKPT&language=CHS
36. Li H, Li Y, He H. Clinical efficacy of ultrasound-guided acupotomy release combined with acupuncture in the treatment of cervical spondylotic radiculopathy. Mod Diagn Treat. (2022) 33(05):702–5. https://kns.cnki.net/kcms2/article/abstract?v=6VlBgy5--52j66on9A2G3vhs0F_2Z0nXGrpfaA7qF64YFi_07s21qyvZ-qqfKj9EH5d1Xiah4INmdj9Ieb98ReNMH3WCu2wGy1bJYexvRT4--xOZJz02e-943cGYUjvppbDpGpVUQh9iwpedaPWHqLJSt5nkEbUAd8TCQmKCbJ4KZu8-DN6kIw==&uniplatform=NZKPT&language=CHS
37. Qinghua L, Fang D, Zhikai L, Jianling S. Ultrasound-guided acupotomy release of the cervical intervertebral foramen for the treatment of cervical spondylotic radiculopathy. Zhejiang J Integr Tradit Chin West Med. (2015) 25(06):588–9. CNKI:SUN:ZJZH.0.2015-06-024
38. Li Y, Cheng J. Efficacy study of ultrasound-guided acupotomy combined with modified gegen decoction in the treatment of cervical spondylotic radiculopathy. Acta Chin Med. (2020) 2020(35):145–6.
39. Fushui L, Dan L, Gang H, Xiaole W, Ting F, Jiaming Q, et al. Clinical observation of ultrasound-guided acupotomy nerve stimulation in the treatment of cervical spondylotic radiculopathy. J Jiangxi Univ Tradit Chinese Med. (2024) 36(02):61–5. doi: 10.20140/j.2095-7785.2024.02.17
40. Hong L, Zhongbiao X, Liangzhi Z, Yurong G, Mengwei Y, Xia L. Clinical observation of ultrasound-guided acupotomy release therapy for cervical spondylosis. Fujian J Tradit Chin Med. (2018) 49(03):8–10. doi: 10.13260/j.cnki.jfjtcm.011617
41. Hong L, Zesheng Z, Liangzhi Z, Renpan Z, Ziqian J, Jing L. Clinical efficacy of ultrasound-visualized acupotomy technique in the treatment of cervical spondylosis. China Med Herald. (2021) 18(15):180–3. +196. doi: 10.20047/j.issn1673-7210.2021.15.043
42. Luo H, Huang Y, Wu D. Analysis of the efficacy of ultrasound-guided cervical nerve root pulsed radiofrequency combined with acupotomy in the treatment of elderly patients with cervical spondylotic radiculopathy. Chin J Pract Med. (2023) 50(01):62–5. doi: 10.3760/cma.j.cn115689-20221004-04722
43. Qi L, Li L, Li X. Observation on the efficacy of ultrasound-guided acupotomy release in the treatment of cervical spondylotic Radiculopathy. Electron J Clin Med Lit. (2018) 5(A4):45. doi: 10.16281/j.cnki.jocml.2018.a4.034
44. Quan B, Liu C, Ma C. Observation on the efficacy of ultrasound-guided acupotomy release of the cervical transverse process in the treatment of cervical spondylotic radiculopathy. Chin Foreign Med Res. (2024) 22(09):56–9. doi: 10.14033/j.cnki.cfmr.2024.09.014
45. Jianguang W, Shucan X, Xinjie Z, Chenhui H, Yu C, Haijian L. Clinical study on ultrasound-guided acupotomy in the treatment of cervical spondylotic radiculopathy. Her Med. (2014) 20(07):6–7. +10. doi: 10.13862/j.cnki.cn43-1446/r.2014.07.003
46. Jing W, Xiaodan Z, Miao Z, Junqiang Z. Effects of ultrasound-guided cervical nerve root pulsed radiofrequency combined with acupotomy on pain and cervical joint mobility in patients with cervical spondylotic radiculopathy. Curr Med Res Pract. (2020) 5(08):97–8. +115. doi: 10.19347/j.cnki.2096-1413.202008041
47. Junwei W, Juan C, Lifeng C, Jianming C, Jinbo A. Clinical study on musculoskeletal ultrasound-guided acupotomy release in the treatment of greater occipital nerve entrapment syndrome. Med J Natl Def Forces Southwest China. (2020) 34(08):527–30. doi: 10.13730/j.issn.1009-2595.2020.08.001
48. Wang L, Wang Y. Observation on the efficacy of ultrasound-guided acupotomy in the treatment of cervical spondylotic radiculopathy. Her Med. (2017) 23(15):65–7. doi: 10.13862/j.cnki.cn43-1446/r.2017.15.020
49. Caidi Y, Weixing F, Min L, Gang C, Liang D, Guoyuan X. Application of ultrasound localization technology in acupotomy nerve stimulation for the treatment of cervical spondylotic radiculopathy. J Med Imaging. (2012) 22(12):2008–10. doi: 10.3969/j.issn.1006-9011.2012.12.013
50. Yuan T, Yao M, Zhang H. Clinical study on ultrasound-guided acupotomy release combined with cervical formula granules in the treatment of cervical spondylotic radiculopathy. Liaoning J Tradit Chin Med. (2021) 48(04):99–102. +221. doi: 10.13192/j.issn.1000-1719.2021.04.029
51. Zhang S, Yao T. Clinical analysis of ultrasound-guided acupotomy release combined with acupuncture in the treatment of cervical spondylotic radiculopathy. J Hubei Univ Trad Chinese Med. (2020) 22(02):102–5. doi: 10.3969/j.issn.1008987x.2020.02.29
52. Zhang W. Clinical observation of ultrasound-guided minimally invasive acupotomy in the treatment of cervical spondylotic radiculopathy. China’s Naturopathy. (2020) 28(15):27–9. doi: 10.19621/j.cnki.11-3555/r.2020.1512
53. Zhao G. Effects of ultrasound-guided cervical acupotomy release on cervical joint mobility in elderly patients with cervical spondylotic radiculopathy. J Med Theor Pract. (2023) 36(14):2409–11. doi: 10.19381/j.issn.1001-7585.2023.14.024
54. Zhinian Z, Hua G, Kang J, Shaoguo D, Xiaoqing L, Qingfu W. Observation on the efficacy of ultrasound-guided acupotomy stimulation of the stellate ganglion in the treatment of vertebral artery type cervical spondylosis. Her Med. (2019) 25(10):82–4. +114. doi: 10.13862/j.cnki.cn43-1446/r.2019.10.021
55. Qiyu Z, Congcong H, Gang Z, Ting X, Fanghua W. Observation on the clinical efficacy and safety of ultrasound-guided cervical nerve root pulsed radiofrequency combined with acupotomy in the treatment of cervical spondylotic radiculopathy. Reflexology Rehabil Med. (2024) 5(01):71–4.
56. Yu W-Y, Liu J, Lin Z-H, Liu H, Zhang L-Z, Feng X-L, et al. Characterization of rectus femoris lesions in knee osteoarthritis at different stages and the effect of ultrasound-guided acupotomy. Front Physiol. (2025) 15:1496425. doi: 10.3389/fphys.2024.1496425
57. Kwon C-Y, Yoon S-h, Lee B, Leem J. Acupotomy for the treatment of lumbar spinal stenosis: a systematic review and meta-analysis. Medicine (Baltimore). (2019) 98(32):e16662. doi: 10.1097/MD.0000000000016662
58. Chae H, Chu H, Lee J, Kim H, Kim D, Park S, et al. Effectiveness and safety of acupotomy treatment on shoulder pain: 25 multicenter retrospective study. J Pain Res. (2023) 16:1367–80. doi: 10.2147/JPR.S398711
59. Wang Y, Huang J, Qian G, Jiang S, Miao C. Study on the correlation between different levels of patients with vertebrobasilar dolichoectasia and posterior circulation blood perfusion. J Stroke Cerebrovasc Dis. (2022) 31(5):106378. doi: 10.1016/j.jstrokecerebrovasdis.2022.106378
Keywords: cervical spondylosis, ultrasound-guided acupotomy, meta-analysis, systematic review, grade
Citation: Lijian Z, Zhen Z, Yuan Y and Nachuan Z (2025) Ultrasound-guided acupotomy for cervical spondylosis: a systematic review and meta-analysis based on GRADE quality assessment. Front. Pain Res. 6:1654265. doi: 10.3389/fpain.2025.1654265
Received: 17 July 2025; Accepted: 28 October 2025;
Published: 14 November 2025.
Edited by:
Tony L. Yaksh, University of California, San Diego, United StatesReviewed by:
Eric Chu, EC Healthcare, Hong Kong SAR, ChinaBrian E. Cairns, University of British Columbia, Canada
Copyright: © 2025 Lijian, Zhen, Yuan and Nachuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhang Lijian, MTUyMzQ1ODA5OTlAMTYzLmNvbQ==
 Zhang Lijian
Zhang Lijian Zhang Zhen1
Zhang Zhen1