Abstract
Background: Arab Americans are a historically understudied minority group in the United States and their health needs and risks have been poorly documented. We aim to provide an updated comprehensive review of the literature on Arab American physical and mental health and provide suggestions for future work in this field.
Methods: A comprehensive review of the English language medical and public health literature published prior to 2017 identified through multiple database searches was conducted with search terms describing Arab Americans and health outcomes and behaviors. The literature was qualitatively summarized by health behavior (vaccination, tobacco use, drug and alcohol use, and physical activity), health outcome (diabetes, mental health, cardiovascular disease, cancer, women's, and child health), and populations at increased risk of poor health outcomes (adolescents and the elderly).
Results: The majority of studies identified exploring Arab American health have been published since 2009 with an increase in the number of longitudinal and intervention studies done with this population. The majority of research is being undertaken among individuals living in ethnic enclaves due to the lack of an ethnic or racial identifier that may help identify Arab Americans from population-based studies. Studies highlight the conflicting evidence in the prevalence of diabetes and cardiovascular disease based on study sample, an increased understanding of cancer incidence and barriers to identification, and an increased level of knowledge regarding mental health and sexual health needs in the population. Information on health behaviors has also increased, with a better understanding of physical activity, alcohol and drug use, and vaccination.
Conclusion: More research on Arab American health is needed to identify risks and needs of this marginalized population given the current social and political climate in the United States, especially with regard to acculturation status and immigrant generation status. We provide recommendations on approaches that may help improve our understanding of Arab American health.
Introduction
Race and ethnicity are a dominant part of national and academic conversations in the United States. One group that is historically represented but largely absent from national and academic conversations about race and ethnicity are Arab Americans. Arab Americans' classification within the United States' racial schema as White makes them invisible as a minority group. This is at odds with politics, war, and violence in the Middle East and the stigmatizing representation of Arabs in the media. Additionally, a recent report by the Arab American Institute Foundation has found that in line with the general surge of bias-motivated violence in the past few years, Arab Americans are at increased risk for hate crimes (1). This discrepancy between having a highly visible and stigmatized group that also has a general lack of visibility in official documents or health records places Arab Americans in an unusual position in the American healthcare system—they are a group that both exists in the public consciousness but is also un-counted and hence has not been a part of a national reckoning with its needs and particularities (2). Aiming to address this gap, we set out to comprehensively review the Arab American health literature, updating a previous review that was conducted a decade ago (3). We examine literature on the health behaviors (actions taken to maintain, attain, or regain good health and prevent illness), health outcomes (an illness, condition, or state that impacts the length or quality of a person's life), and sub-populations within the large Arab American population with particular health needs.
Arab Americans are those individuals with ancestral, cultural, ethnic, linguistic, familial, or heritage ties to one or more of the 22 Arab League countries. It is estimated that there are approximately 3.5 million Arab Americans living in the United States (4). Arabs are disproportionately represented among recent immigrants to the United States due to war and instability in the Middle East. The diversity in country of origin of Arab immigrants makes understanding health indicators difficult, as the differences in health outcomes among Arabic League countries can be disparate. Social determinants in these countries vary dramatically from high poverty and war torn to highly affluent and stable. Arab Americans have varied nativity in the United States: foreign-born (first generation), U.S. born children of immigrants (1.5 and second generation), or U.S. born to U.S. born parents (third and greater generations) (5). The diversity in country of origin, geographic location, tenure in the United States, and acculturation makes studying Arab Americans difficult and the task of generally understanding Arab American health monumental.
A history of Arab American immigration to the United States has been published elsewhere (6). Prior to the 1940's the position of Arab immigrants in the United States' racial system was unclear if not ambiguous (2). The Census Bureau decided in the 1940's that Arab Americans were to be treated like other European immigrant communities (7). The Office of Management and Budget of the United States government has outlined that Arab Americans belong to the “White” racial category, as having origins from the Middle East (8). Arab American's place in society was complicated by developments in the Middle East that led to increased discrimination and exclusion of this population since the 1960's and 1970's (1). Arab American organizations and community members began advocating for a dedicated Middle East and North African (MENA) identifier on the U.S. Census in the 1990's (9). A test of this category was done on the 2015 Census but recently the U.S. Census decided not to include the MENA category on the 2020 Census1.
The aim of this review is to provide an updated assessment of the peer-reviewed literature concerned with the health of Arab Americans living in the United States and to summarize key health indicators in this population. A previous review of Arab American health literature published in 2009 reviewed 34 research studies and found little consensus regarding the burden of cardiovascular disease and diabetes in Arab Americans, little information about cancer or mental health disorders, and mixed information regarding whether social determinants of health differed for Arab Americans when compared to other populations (3). We aim to update this review with information on more recently published studies in this population and to synthesize current knowledge about health risks facing Arab Americans to better inform interventions for this vulnerable population and to encourage additional research.
Methods
The main aim of this study is to summarize the state of the medical and public health literature describing the mental and physical health outcomes and needs of Arab Americans published prior to January 1, 2017. We conducted a comprehensive review following many of the reporting guidelines and criteria set forth by the Preferred Reporting Items of Systematic Reviews (PRISMA) (10). A search was conducted using PubMed/Medline, BIOSYS Previews, CINAHL, Cochrane Reviews, and Web of Science on Arab Americans (specified by a combination of terms including country of origin and regional identifiers) and health related outcomes including tobacco use, cardiovascular disease, stroke, cancer, diabetes, maternal and child health, depression, mental health, trauma, substance abuse and general mental and physical health terms (Supplemental Material). These health behaviors and outcome categories were chosen based on the outcomes most prevalently represented in the previous review and on the authors' expertise. For inclusion, articles needed to describe a study in a population of Arab Americans in the United States. Studies also needed to include a health outcome (defined broadly as physical or mental well-being), be written in English, and be published before January 1, 2017. Qualitative and quantitative research studies were included. Endnote (X8) was the bibliographical data management software used for this review.
After removing duplicates, each article's title and abstract were read and evaluated by two members of the research team against the inclusion criteria set above. Articles that did not meet the criteria were excluded after conferring with a third research team member. Based on the evaluation process with the titles and abstracts, 7424 articles were removed yielding 445 articles (Figure 1). Full texts of 445 articles were evaluated to ensure each article was a true match to the study criteria. This resulted in the further exclusion of 198 articles, yielding 247 articles in the review. All decisions were agreed upon through review and consensus by at least three research team members (Figure 1).
Figure 1
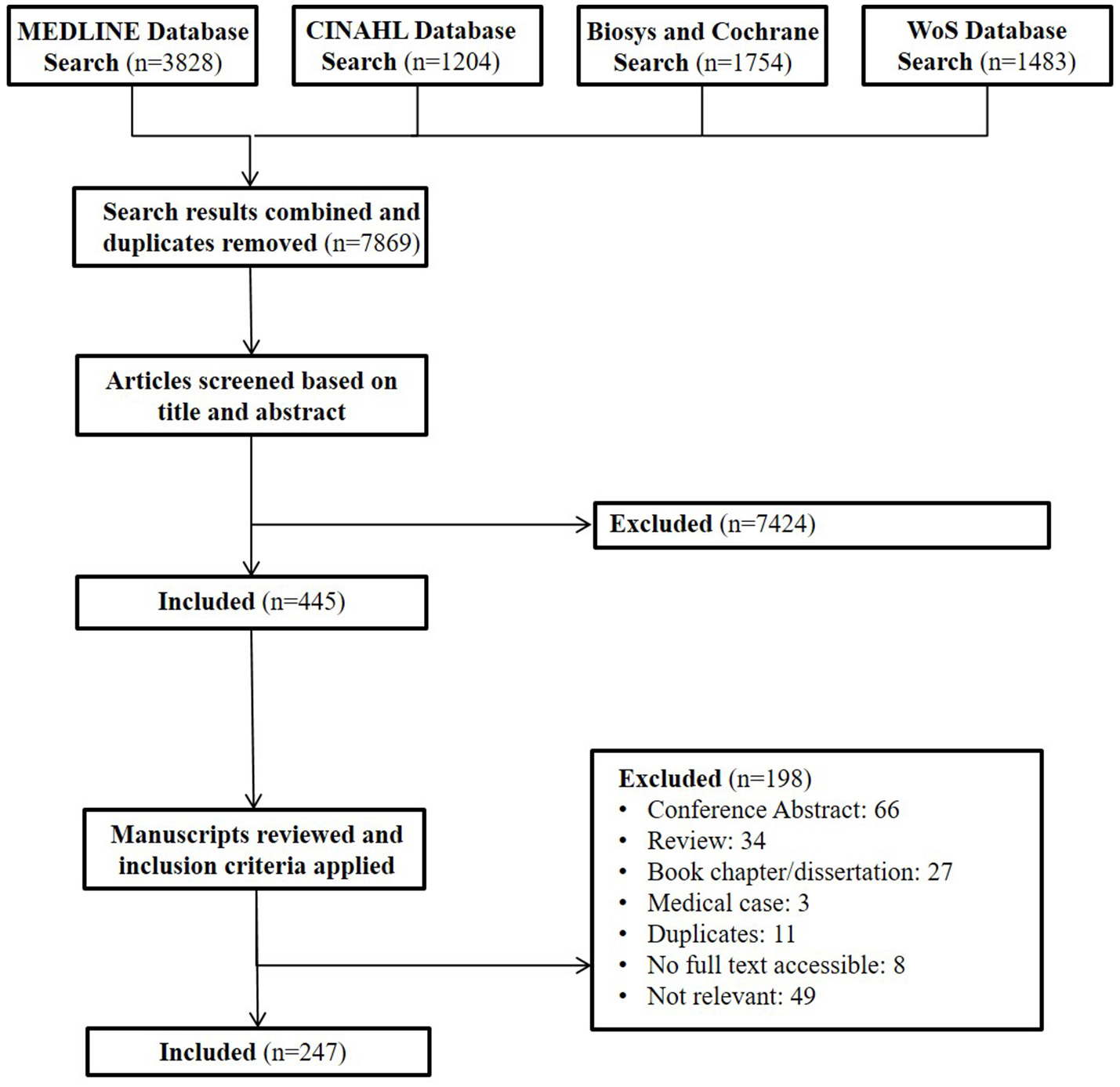
Review cascade for Arab American health. This cascade describes the process through which papers were identified and reviewed for our comprehensive review of Arab American health in the public health and medical literature.
Epidemiological information on study design, sampling characteristics, study period, geographic origin of samples, and study location were extracted from all papers by multiple investigators. When estimates of prevalence or incidence were reported across studies for the same health outcome, these estimates were recorded as a range. Data points that provided an understanding of the magnitude of illness or disease in Arab Americans were extracted along with notable study designs and observations from qualitative studies. Results are summarized descriptively to help inform readers of the most rigorous, generalizable, and notable takeaways from studies with large sample sizes and rigorous sampling frames (when possible) within health outcomes, behaviors, and vulnerable populations. Quality of data and potential for bias was assessed epidemiologically by more than one investigator and notable exceptions (both positive and negative) are described descriptively within each outcome section of the Results and the Discussion. Due to the heterogeneity in study type and quality of the Arab American literature a systematic quality assessment was not conducted.
Results
Since the publication of the last review 169 papers were published accounting for 68% of all publications reviewed. We organized our findings around health behaviors, health outcomes, and populations of interest. We examined health behaviors among Arab Americans including tobacco use, physical activity, alcohol and drug use, and vaccination. We examined seven morbidity clusters for health outcomes including diabetes, mental health, women's and child health, cancer, cardiovascular disease, and other health outcomes. Finally, we highlighted two distinct populations of interest for Arab American health: adolescents and the elderly.
Papers describing the health of Somali immigrants and their descendants in the United States (N = 66, 27%) accounted for the largest immigrant subgroup, while Iraqi immigrants (N = 39, 16%) accounted for the second largest identified subgroup. Nearly half of all papers examined the health of a mix of countries of origin or did not specify the composition of the groups they included (N = 122, 49%). The number of United States cities and regions in which Arab American health research is taking place has expanded since the last review. While the majority of studies were still being undertaken in Michigan (N = 90, 36%), many other states are represented in the literature including Minnesota (N = 30, 12%), California (N = 11, 5%), New York (N = 8, 3%) and Virginia (N = 4, 2%). Eight studies have examined national samples of Arab Americans (3%) while some examined Arab Americans from multiple cities (N = 9, 4%).
The epidemiologic composition of publications examined has shifted dramatically since the last review was written. The number of studies testing interventions (N = 15, 6%) and the number of longitudinal studies (N = 30, 12%) among Arab Americans increased since 2009. Novel methodologies like snowball sampling (N = 13, 5%) and web-based surveys (N = 3, 1%) were also used in addition to more traditional qualitative methods like focus groups (N = 77, 31%). The majority of the literature focused on describing health outcomes in a sample (N = 136, 55%) as opposed to examining the relationship between an exposure and outcome.
Health behaviors
Tobacco use
Research regarding tobacco use and addiction among Arab Americans has had a strong foothold and publishing record in Arab American health literature since the early 1990's. The first study on Arab American smoking prevalence occurred in 1992 and aimed to estimate community prevalence among Arab Americans (38.9%) in Michigan (11). Since that first study was published, a number of other studies have examined the prevalence of smoking among Arab American populations, primarily in the Michigan area (12, 13), but also in Houston, Minnesota, and Virginia (14–16) with smoking prevalence ranging from 6 to 45%. Generally, it has been found that less assimilated Arab Americans had a higher dependence on nicotine and tobacco products with the use of tobacco correlating negatively with time spent in the United States (17). More recent literature aims to understand the predictors of water-pipe smoking and of quitting smoking in Arab American populations. Generally, very little evidence was found that Arab Americans desire to quit water-pipe smoking (14). An intervention study performed in a Midwest school aimed at discouraging high school students from starting smoking or continuing smoking showed improvements in non-Arab American and Arab American teens (18).
Physical activity
Most of the studies on physical activity were from small convenience samples often performed at religious sites or from religious communities. Further, many of these samples were taken from ethnic enclaves and areas where a large number of Arab immigrants live. Some studies have examined the impact of acculturation on physical activity and found that individuals with lower American acculturation tended to have less physical activity (19) while those found to be more acculturated participated in more physical activities (20). Further, some barriers to physical activity have been identified including a lack of knowledge about how to use machines at the gym (21), lack of money for gym memberships (22), and mixed cultural messaging on body image (19).
Alcohol and drug use
A study aimed at estimating the prevalence of binge drinking among Arab Americans at both national and state levels found that nationally Arab Americans had lower prevalence of lifetime alcohol consumption and consumption in the last month than non-Hispanic Whites (23). The national data also showed that Arab American men were 1.78 times more likely to have had alcohol in their lifetime than women (23). An exploratory qualitative study performed by the same investigators aimed to understand the potential reasons for this discrepancy found that alcohol was easily accessible in Arab American communities and environments in Michigan, that social pressures encouraged people to drink at social gatherings, and that populations that were more highly acculturated tended to have higher drinking prevalence than those who were not (24). Some research has been done to understand the low representation of Arab Americans in substance abuse treatment and the presence of language and cultural barriers to Arab Americans enrolling in these programs was uncovered (25).
Vaccination
Research on vaccination behavior among Arab Americans lags behind our knowledge of vaccination behavior in other immigrant and minority groups (26–28). A study with data from a national health survey found that Arab Americans had lower estimated rates of recommended vaccinations (flu and pneumonia) when compared to non-Hispanic Whites (29). Only one study among Somali adolescents in Minnesota examined the uptake of human papilloma virus vaccinations. This study showed that while Somali adolescents were accepting of the vaccine, they were less likely to complete the vaccine series when compared to non-Arab, non-Hispanic Whites in the same area (30).
Morbidity clusters
Diabetes
Estimates of diabetes prevalence in Arab American populations range from 4.8 to 23% (31–33). Due to the high prevalence of diabetes and higher odds of diabetes when compared to non-Arab, non-Hispanic Whites found in many Arab American populations, including Somali Americans (34), researchers have examined biological and genetic pathways for these differences. Specifically, work has found that vitamin D insufficiency and hypovitaminosis D were common among Arab Americans and were linked to insulin resistance, metabolic syndrome and glucose intolerance in Arab American men (35). Researchers have also hypothesized that differences in disease burden may also be a result of lack of knowledge and care in this marginalized population.
A number of studies found a lack of appropriate diabetes education tools for Arab Americans (36, 37). Cultural and linguistic deficiencies in the existing educational literature may be preventing Arab Americans from fully understanding their risk for diabetes and their ability to improve their health. Cost and access to appropriate healthcare were barriers identified in a number of studies (38). Acculturation was found to influence diabetes control differently for men than for women. Negative associations between Arab acculturation and diabetes risk were found among Arab American men while American acculturation was found to be associated with diabetes risk among women (39). There were some religious barriers to diabetes control. Some woman cited concerns about modesty that prevented them from exercising properly (36). Ramadan poses a potential barrier to diabetes control in this population as well (40).
One of the first intervention studies implemented among Arab Americans was the adapted Diabetes Prevention Program (DPP) group lifestyle intervention (41, 42). The DPP was tailored linguistically and culturally to Arab American populations in the Dearborn Michigan area to encourage individuals to lose weight and understand their risk for diabetes. The program was successful, with individuals losing weight if they had family support and were appropriately educated on the benefits of the program. This intervention was one of the first successful implementations of intervention research in the Arab American community. The authors attribute their success to targeting gaps in knowledge and reducing misconceptions in recruiting and promoting participation. Arab Americans who perceived they were at increased risk of diabetes were more willing to participate in a lifestyle intervention than those who did not perceive they were at risk (43).
Mental health
Research on mental health outcomes and the needs of Arab Americans with regard to mental health has increased since September 11th. While discrimination against Arab Americans is not new, discrimination, and stigmatization have increased in the United States over the past two decades (1, 44). Additionally, many Arab immigrants come to the United States from war torn and conflict-ridden regions increasing their exposure to traumatic and stressful experiences. Studies have documented higher incidence of psychological distress in the years following September 11th among Arab Americans (45). The overall prevalence of depression and other adverse mental health outcomes in Arab Americans is still relatively unknown. Recent studies among Arab American adolescents estimate that 14% of Arab Americans living in the Dearborn ethnic enclave were diagnosed with depression (46), while another online study found that 50% of Arab-American respondents met criteria for depression (44). In particular, studies among Iraqi refugees suggested that this group was at particularly high risk for PTSD and overall health problems (47) and that a longer tenure in the United States was associated with increased depression for this population (48). The effort to estimate this psychological burden is deterred by a number of methodological challenges including the inability to easily identify Arab populations (49), the negative cultural attitudes toward counseling and psychotherapy (50–54), and the lack of targeted and culturally competent mental health services (52, 55) for Arab Americans.
Anti-Arab sentiment was associated with poor mental health outcomes including depression, distress, and unhappiness in Arab American populations (45, 56). Stress, specifically related to migration and the immigration experience, was examined among a group of Arab immigrant woman and found that post-immigration related stressors were correlated with depression and PTSD (57). In a study of Iraqi immigrants, pre-migration trauma was associated with higher rates of depression and PTSD (58). In one of a few randomized clinical trials reviewed, Iraqi refugees who had experienced post-traumatic stress were randomized to brief narrative exposure therapy or control (59). Investigators found that those who received brief narrative exposure therapy had greater posttraumatic growth and increased well-being alongside reduced symptomology for depression (59). Evidence suggests that there were challenges to psychotherapy for Arab Americans including hesitancy in discussing family problems outside of the family and a hesitancy to seek treatment. When individuals sought therapy, therapists reported a large amount of intergenerational conflicts and a difficulty to adjust to mainstream culture as primary complaints (50).
Women's and child health
The research in Arab American women's and child health is primarily focused on intimate partner violence, sexual health, obstetrics, and birth outcomes.
Intimate partner violence
Some studies found high prevalence of intimate partner violence in Arab American communities (60). Generally, Arab American woman exposed to intimate partner violence were at higher risk of depression (61). Woman who experienced intimate partner violence had many barriers to receiving care and support including language barriers, fear associated with discrimination, lack of culturally sensitive help, and a lack of trust of American providers (60, 62). There was mixed evidence for police intervention and the use of shelters for Arab American women (62). Some work has been done to understand the structural causes of intimate partner violence in Arab American populations including dependence on male relationships for stability and safety post immigration (62), patriarchal Arab culture, the lack of cultural support for seeking marital help outside of the family (61), and family honor, and blaming (62, 63). There is generally a critical need for domestic violence awareness and prevention programs in Arab American populations (64). Additionally, educating women about their rights and the care available to them may improve health seeking behavior alongside the increase in culturally competent health care providers for Arab American patients (60, 62, 63).
Female genital mutilation and sexual health
The majority of the literature regarding the sexual health care needs of Arab American women focused on Somali women and those who experienced female genital mutilation. Female genital mutilation is the practice of partially or totally removing external genitalia of young girls and woman for nonmedical reasons (65). This practice is common in 30 countries in Africa, the Middle East and Asia (65). The prevalence and practice of female genital mutilation practices in the United States was low and rare (66, 67), but the number of those who come to the United States having experienced this in other countries was high (66). More research is needed in more diverse populations to understand the FGM practices in the United States and their impact on Arab American women's sexual health.
Knowledge and care for sexually transmitted diseases and HIV among Arab Americans was relatively low. While few research studies examined the sexual health needs of Arab American women, a study performed among Somali immigrants found low knowledge of STI/HIV risk factors, low condom use, and low incidence of extra-marital sex (66).
Obstetrics
All studies aiming to understand the obstetric needs of Arab Americans focused on Somali American populations. Among Somali refugees, women preferred little obstetric intervention (68) and clinicians who were more conservative with the use of C-sections (69, 70). Some authors noted that this was due to the fact that many women felt that in Somalia death after obstetric intervention was common (68) and many believed that there was a risk of not having future children after intervention (71). Prenatal education and programs helping mothers understand the options for obstetric care and reducing language barriers between patients and providers could reduce adverse obstetric outcomes (72–74).
Birth
Arab immigrants had lower odds of pre-term birth than U.S.-born mothers (75). This trend is not unique to Arab Americans but to many immigrant groups (76). Some theorize that the reasons for this difference in pre-term birth includes the fact that immigrants who are able to immigrate to the United States are those that are healthy (77). Arab mothers tended to be healthier than non-Arab mothers with less tobacco use (78), less pregnancy-related hypertension and diabetes (79), lower rates of birth defects (80), and more consistent prenatal care (81). Somali women in particular faced poor obstetric outcomes due to poorer prenatal care (70) and feeling vulnerable and uninformed, but their outcomes improved with doula support (82). While there is great interest in whether or not adverse birth outcomes increased after September 11th, (83) did not find evidence of increased adverse birth outcomes after September 11th despite showing that stress and discrimination increase this risk among Arab mothers (84).
Cancer
Cancer rates among Arab American populations are relatively unknown, although the majority of work in this field has focused on breast cancer.
Breast cancer
Whether or not Arab Americans have a higher breast cancer associated mortality rate than non-Arab, non-Hispanic Whites is unclear. Evidence was found in both directions (85, 86). Arab American women tend to be diagnosed at a later stage of breast cancer and yet had higher overall survival than European and American women (87, 88). Barriers to breast cancer screening for Arab Americans included immigration-related barriers, fear, lack of knowledge, and access issues (89–94). Arab American women with higher levels of education and who have lived in the United States for long periods of time were more likely to get screened for breast cancer than their counterparts (95). Fatalism and religious beliefs have been cited by some authors as barriers to breast cancer screening (96). A recent study by Padela et al. found no correlation between fatalism and screening rates among Arab Americans (95).
Other cancer
Studies examining the perceptions of cancer among Arab Americans found that education, employment status, and the length of time one spends in the United States affected knowledge of cancer and screening (97). Many Arab Americans generally feared cancer (98) and some believed in keeping cancer diagnoses a secret in order to protect the image of the family in social settings (99). In one study of Arab American men and women, women were found to be more knowledgeable about the modifiable risk factors associated with cancer but that changing food habits was a point of concern (98). To improve perceptions and knowledge about cancer in Arab American populations, community educational programs targeting practices and knowledge within the Arab American community may help create change and awareness of risks (97, 99).
The barriers to screening and treatment of cancer among Arab Americans included lack of knowledge (100–103), religious and cultural beliefs about sickness (100, 104), fear and embarrassment (98, 103), language (101, 104), lack of culturally sensitive healthcare providers (100), lack of access to healthcare (105), and a need to maintain secrecy of sickness or disease (99). Community based participatory research was conducted among Arab Americans to address cancer education, prevention, and screening (106). This type of research was successful and found to increase cancer screening rates among an Arab American community in Detroit and can be used in future studies aiming to improve education and screening of other diseases.
Studies which include Arab Americans that aimed to estimate the incidence of particular cancers primarily focused on two comparisons: comparisons within Arab Americans (place of birth, gender, and country of origin) and comparing Arab American incidence to non-Hispanic, non-Arab White cancer incidence. Differences were observed in the incidence of cancer between foreign-born and U.S.-born Arab Americans and also between male and female Arab Americans (107). Differences of cancer incidence by country of origin were also found (108). Arab Americans, especially women, were at increased risk for thyroid cancer (107–110). Arab American men were found to be at increased risk of lung and prostate cancer when compared to Hispanic men, but had lower rates when compared to Black men (110). Manifestations of cancer also differed with Arab American men suffering from higher urinary incontinence associated with prostate cancer than White men (111). Arab American men had higher rates of bladder cancer than both Hispanic and black men (110). Risk factors for cancers differed between Arab American and non-Hispanic, non-Arab White women. White women tended to have a higher incidence of hormone, tobacco, and alcohol use while Arab American women had high vitamin D related deficiency and radiation exposure (109).
Cardiovascular disease
There is a surprising lack of reliable and nationally representative data on cardiovascular disease among Arab Americans. Despite the fact that Arab Americans are generally cited to have higher cardiovascular disease risk than the general population, there is little evidence for this from the existing literature.
Prevalence of self-reported hypertension among Arab Americans (13.4%) was found to be lower than prevalence among non-Hispanic Whites (24.5%) in an analysis of the 2000–2003 National Health Interview Survey (33). A cross-sectional descriptive study among Arab Americans in Southern California found a high prevalence of hypertension (36.5 and 39.7% pre-hypertensive) (112).
A cross-sectional study among Arab Americans in Michigan found an overall prevalence of self-reported heart disease of 7.1% and that Arab Americans were four times more likely to have heart disease than Black Americans in this sample (113). Studies of hypercholesterolemia found prevalence ranged from 24.6 to 44.8% among Arab Americans in various national and community-level convenience samples (39, 114). These numbers were well below the national average of 50.4% hypercholesterolemia in the United States population, but were not rigorously estimated using national and representative sampling methods (114).
Tailakh et al. attempted to understand the awareness of hypertension among a cross-sectional sample of Arab Americans in Southern California and determined that only 67.4% were aware of their hypertension and 52.2% were taking their antihypertensive medication (with 46% of those on medication having controlled blood pressure) (112). To our knowledge, no interventions have been tested to alter cardiovascular status among Arab Americans or influence the risk of developing cardiovascular disease in this population. This is in contrast to the numerous studies developing interventions to improve cardiovascular disease in the United States. While there is no mechanistic reason why interventions developed in other communities would not be transferrable to Arab Americans, it will be important to develop culturally relevant cardiovascular disease interventions for this population.
Other health issues
Infectious disease
The majority of research on infectious disease outcomes among Arab Americans focused on Somali immigrant populations in the Minnesota area (115, 116). More recent literature examined Hepatitis C among Somali immigrants in Minnesota and among Arabs in Southeast Michigan. Somali immigrants in Minnesota had high rates of hepatitis and hepatocellular carcinoma suggesting targeted interventions were needed for this population (117). The prevalence of Hepatitis C virus antibodies among Arab Americans in Southeast Michigan was found to be triple the national average (5.4%) suggesting the need for more studies assessing the burden of Hepatitis C in this community (118).
Asthma
Asthma prevalence has been found to vary by racial and ethnic groups in the United States (119). Evidence from recent studies shows that Arab Americans tended to have lower prevalence of asthma (9.4%) than other racial and ethnic minorities including non-Hispanic Whites and Black Americans (14.4%) (120). An important initiative, the Arab American Environmental Health Project (AAEHP) aimed to understand the impact of the environment on health among Arab Americans populations. One of the first studies published from this interdisciplinary project suggested that asthma prevalence was higher than previously reported among Arab Americans (16%) but that asthma was more strongly correlated with environmental exposure among those with hypertension (121). Asthma management was also found to vary by English language fluency and acculturation variables, suggesting targeted interventions may need to be put in place to help those Arab Americans affected by asthma (122).
Populations of interest
While many studies focused attention on the adult Arab American population in the United States, there are at-risk populations within this community that have been explicitly studied.
Elderly
Global demographics have shifted such that life expectancies are longer and many countries and populations are experiencing aging. The attention paid to the needs of elderly Arab Americans was minimal suggesting this as a future area of research. Better understanding the healthcare, social, and medical needs of the aging Arab American population in the United States is an important and urgent area of study. In our literature review, only three papers examined the needs of older Arab Americans. While Dallo et al. found a reduced likelihood of reporting a disability among Arab Americans when compared to other groups of color in the United States (123), Ajrouch synthesized information from a face-to-face survey and found that well-being varied with social capital for Arab American elders (124). More work is needed in this area to understand how to best care for aging Arab Americans and ensure their mental and physical well-being.
Adolescents
Adolescent Arab Americans are mostly composed of second generation Arab Americans, born in the United States to immigrant parents. In a large sample of Arab American adolescents, Ahmed et al. found that there was a strong relationship between perceived discrimination and poor mental health. Further, adolescents reporting more religious coping, strong ethnic identity, and religious support were found less likely to be psychologically distressed (125). An analysis by Aroian et al. (126) found that the quality of the mother-adolescent relationship was the most important predictor of adolescent behavior and stress (127). Adolescents experienced a great deal of discrimination from teachers, school administrators, and their classmates suggesting the need for more dedicated research on how discrimination impacts adolescents (128). A recent analysis by Munro-Kramer et al. found two distinct subgroups of Arab American adolescents in their sample from the Midwest: those with multiple high risk behaviors and those with minimal risk behaviors and more positive life experiences (129). This analysis of high risk behaviors like sexual activity, tobacco use, and physical activity provides a perspective on the potential health needs of Arab American adolescents. The research on Arab American adolescents and their unique health risks requires further exploration and research.
Discussion
In this updated comprehensive literature review of Arab American health, we found that the literature describing Arab American health outcomes and needs in the past decade has increased and expanded in geographic representation (Table 1). Publications discussing the health behaviors (especially physical activity, alcohol and drug use, and vaccination) of Arab Americans have increased in frequency since the publication of the literature review in 2009 alongside studies focusing on sexual health and female genital mutilation. Since the publication of the last review, a more substantial number of studies have examined the mental health needs of the Arab American population (44, 46, 48, 50, 51, 56, 195–202). Recent studies have improved upon the past literature by providing estimates of depression and depression symptoms among larger groups of Arab Americans alongside the examination of the risk factors (and resiliency factors) associated with this improved mental health but very few studies report on interventions to reduce mental health outcomes. Studies of cancer among Arab Americans have also increased in number since the last review, with a number of studies identifying incidence of a variety of cancers in Arab Americans (106–110) and another set of studies identifying barriers to screening, care and treatment in this population (97–105, 203). There have been more studies examining the risk of diabetes and cardiovascular disease in Arab Americans since 2009 (34–43, 112, 121, 141, 204–206), and more recent studies have examined successful targeted interventions to reduce risk factors for these diseases in ethnic enclaves (41–43). The implementation of intervention studies in Arab American populations is an improvement to the literature reported since the last review.
Table 1
| Number of studies identified (N = 247) | Proportion | References | |
|---|---|---|---|
| TIME PERIOD | |||
| 1980–1989 | 4 | 1.6% | (130–133) |
| 1990–1999 | 10 | 4.0% | (11, 64, 69, 134–140) |
| 2000–2009 | 80 | 32.4% | (12, 13, 17, 25, 31–33, 47, 52, 55, 63, 74, 78, 79, 83, 85, 86, 98, 108, 113–116, 122, 124, 127, 141–194) |
| 2010–2017 | 153 | 61.9% | (14–16, 18–24, 29, 30, 34–46, 48, 50, 51, 53, 54, 56–62, 66–68, 70–73, 75, 80–82, 84, 87–97, 99–107, 109–112, 117, 118, 120, 121, 123, 125, 126, 128, 129, 195–265) |
| COUNTRY OF ORIGIN OF SAMPLE (NOT EXCLUSIVE) | |||
| Egypt | 11 | 4.5% | (54, 55, 79, 135, 146, 151, 152, 185, 186, 240, 245) |
| Iraq | 39 | 15.8% | (11, 31, 47, 48, 54, 58–61, 79, 93, 94, 99, 109, 124–126, 143, 151, 152, 171, 172, 180, 183–186, 193–195, 197, 198, 207, 208, 244, 248, 249, 253, 256) |
| Jordan | 8 | 3.2% | (54, 79, 86, 90, 137, 152, 185, 249) |
| Kuwait | 3 | 1.2% | (151, 185, 249) |
| Lebanon | 28 | 11.3% | (11, 31, 36, 54, 55, 61, 79, 99, 102, 109, 124–126, 143, 151, 152, 180, 183–186, 193, 194, 198, 207, 238, 249, 260) |
| Palestine | 15 | 6.1% | (11, 54, 55, 61, 79, 86, 90, 143, 146, 151, 152, 180, 185, 186, 207) |
| Saudi Arabia | 6 | 2.4% | (54, 79, 146, 151, 152, 249) |
| Somalia | 66 | 26.7% | (15, 21, 22, 30, 34, 51, 53, 54, 66–74, 82, 89, 94, 100, 101, 103–105, 115–117, 144, 149, 158, 159, 163, 167, 177, 178, 182, 191, 192, 199, 201, 204, 206, 209, 210, 212, 214, 218, 219, 222, 224, 226, 227, 230–233, 235, 237, 241, 243, 254, 255, 257, 261, 263) |
| Sudan | 9 | 3.6% | (54, 98, 140, 152, 153, 164, 209, 253, 257) |
| Syria | 11 | 4.5% | (11, 54, 79, 99, 124, 143, 151, 152, 185, 186, 249) |
| Yemen | 22 | 8.9% | (11, 31, 36, 61, 79, 102, 125, 135, 139, 143, 146, 151, 175, 180, 185, 186, 194, 198, 207, 238, 249, 260) |
| Mixed/Unspecified | 122 | 49.4% | (12–14, 16–20, 23, 25, 29, 32, 33, 35, 37–46, 50, 52, 54–57, 62–64, 75, 78, 80, 81, 83, 84, 87, 88, 91, 92, 95–97, 106–108, 110–112, 114, 118, 120–123, 125, 127–134, 136, 138, 141, 145, 147, 148, 150, 154–157, 162, 165, 166, 168–170, 173, 174, 176, 181, 187–190, 193, 196, 200, 202, 203, 205, 211, 213, 215–217, 220, 221, 223, 225, 228, 229, 234, 236, 239, 242, 246, 247, 251, 252, 258, 259, 262, 264, 265) |
| UNITED STATES LOCATION (NOT EXHAUSTIVE) | |||
| California | 11 | 4.5% | (19, 20, 69, 110, 112, 133, 162, 211, 228, 252, 254) |
| Washington D.C. | 2 | 0.8% | (86, 90) |
| Illinois | 3 | 1.2% | (95, 264, 265) |
| Louisiana | 2 | 0.8% | (39, 81) |
| Maine | 3 | 1.2% | (73, 212, 226) |
| Massachusetts | 4 | 1.6% | (71, 93, 94, 235) |
| Michigan | 90 | 36.4% | (11–13, 24, 25, 31, 32, 36–38, 41–43, 45–47, 56–63, 75, 78, 79, 83–85, 87, 92, 97, 99, 102, 106–111, 113, 118, 120–122, 124–127, 136, 139, 142, 145, 147, 154, 156, 157, 160, 161, 165, 166, 168, 174, 176, 179–181, 183, 184, 187, 190, 193, 194, 196, 197, 202, 207, 208, 217, 220, 221, 223, 225, 234, 238, 243, 246, 248, 258) |
| Minnesota | 30 | 12.2% | (15, 21, 30, 34, 66, 72, 74, 100, 101, 103–105, 115–117, 140, 144, 158, 163, 170, 178, 192, 201, 210, 218, 222, 224, 237, 257, 263) |
| New Jersey | 2 | 0.8% | (110, 152) |
| New York | 8 | 3.2% | (52, 68, 152, 167, 185, 213, 215, 245) |
| Texas | 2 | 0.8% | (14, 229) |
| Virginia | 4 | 1.6% | (16, 146, 236, 242) |
| Washington | 3 | 1.2% | (89, 149, 214) |
| National | 8 | 3.2% | (23, 29, 33, 123, 155, 189, 247, 259) |
| Multiple Cities | 9 | 3.6% | (44, 48, 54, 55, 88, 91, 96, 153, 216) |
| SAMPLING CHARACTERISTICS (NOT EXCLUSIVE) | |||
| Convenience sample | 171 | 69.2% | (12–14, 16, 17, 20–22, 25, 36, 37, 39–42, 46, 50–55, 57, 59–64, 67–74, 81, 82, 85–87, 89–106, 111–114, 118, 120, 121, 124–126, 128–135, 137, 139–141, 143–146, 148–154, 157–159, 164, 167–173, 175, 177–186, 188, 190–195, 197–204, 207, 209–214, 216, 219, 220, 223, 226–233, 235, 236, 238–241, 243, 245, 248, 249, 251–257, 260, 262–265) |
| Population based sample | 69 | 27.9% | (11, 12, 15, 23, 29–35, 38, 43–45, 47, 48, 56, 58, 75, 78–80, 83–85, 88, 107, 108, 110, 115–117, 122, 123, 136, 138, 142, 147, 155, 156, 160–163, 165, 166, 174, 176, 180, 187–189, 196, 205, 206, 208, 215, 218, 221, 222, 225, 234, 237, 246, 247, 250, 258, 259) |
| Snowball sampling | 13 | 5.3% | (22, 54, 91, 127, 135, 167, 177, 199, 203, 232, 235, 244, 261) |
| Web-based sampling | 3 | 1.2% | (54, 55, 177) |
| STUDY CHARACTERISTICS (NOT EXCLUSIVE) | |||
| Cross-sectional | 196 | 79.4% | (11–25, 32–40, 43–46, 48, 50–57, 60–64, 66, 71, 72, 74, 81, 82, 86, 89, 91, 93–96, 98–100, 102, 103, 109–114, 117, 118, 120–122, 124, 125, 127–161, 163, 164, 166–195, 197–202, 204–211, 213, 214, 216, 217, 219–221, 223–225, 227–233, 235, 237–242, 244–246, 249, 251–263, 265) |
| Longitudinal | 30 | 12.2% | (29, 30, 42, 59, 75, 78–80, 83, 84, 88, 92, 105–108, 115, 116, 123, 126, 162, 165, 196, 217, 218, 234, 236, 247, 248, 250) |
| Intervention | 15 | 6.1% | (18, 41, 42, 46, 59, 87, 92, 97, 104, 106, 150, 215, 223, 236, 243) |
| Focus groups or interviews | 77 | 31.2% | (19, 21, 24, 36–38, 51–53, 62–64, 66–71, 73, 74, 81, 82, 89, 90, 93, 94, 96, 98–101, 103, 126, 128–130, 136, 137, 139, 143, 144, 148, 158, 159, 167, 169, 171, 178, 185, 191, 192, 195, 199, 201, 207, 210, 212, 214, 215, 219, 224, 227, 229–233, 235, 241, 242, 248, 253, 254, 256, 257, 263, 264) |
Characteristics of Arab American health studies identified through comprehensive review are summarized by number of studies identified and proportion of all studies identified.
Methodological limitations in the literature
This review highlighted some methodological shortcomings of the existing literature on Arab American health that may prevent comparisons of health indicators to other ethnic groups in the United States. First is our inability to generalize findings from ethnic enclaves to areas where Arab Americans may be dispersed among other ethnic populations. The majority of studies aiming to understand health outcomes and health needs of Arab Americans took place within ethnic enclaves, primarily Dearborn Michigan, and Somali enclaves within Minnesota. In fact, regionally representative data sets using rigorous sampling methodologies (that have been invaluable for our understanding of Arab American health needs) have been overused and overpublished in the literature, suggesting that much of the information we have on Arab populations stems from a few datasets (ex. Detroit Arab American 2003 survey) within ethnic enclaves. While the identification and recruitment of Arab individuals in this area is made easier by social and cultural community connections, the lived experiences of these Arabs likely differs from those living in other parts of the country. Further, the large diversity of Arab populations residing in the United States with regard to country of origin, immigrant generation, and religion necessitates the study of diverse and nationally representative Arab samples in future studies.
Second, almost all studies were recruited through convenience sampling and very few studies used rigorous sampling methodologies to recruit samples of Arab Americans. This is in large part due to the absence of an easy way to identify Arab Americans on a wider scale and is a previously mentioned concern by other authors (3, 266). Investigators have used a variety of methods to isolate Arab Americans from larger datasets including Arab surname algorithms, using place of birth and Arabic language as indicators. Little is known about the generalizability of the findings from each of these methods.
Third, there were a general lack of prospective and longitudinal studies performed in this population- most studies were cross-sectional in nature. Longitudinal studies are able to follow individuals for longer periods of time to understand disease development. The longitudinal studies that were performed in this population have aimed to increase education, screening, or knowledge. Very few aim to alter disease status or examine interventions specific to disease reduction. The United States public health community has a long history of successful longitudinal studies aimed at understanding the burden of chronic diseases within particular populations (ex. Framingham Heart Study, Nurses' Health Study etc.) but the richness of these datasets cannot be used to understand Arab American health because, despite their likely presence in these datasets, Arab Americans cannot be isolated. These methodological challenges should be considered in the context of the future research directions recommended.
Unfortunately, many of the methodological shortcomings in the literature have persisted since the publication of the last review (3), suggesting the need for more active collaboration among researchers and institutions to overcome these limitations. These methodological shortcomings made a rigorous quality assessment of the literature difficult to conduct due to heterogeneity in the rigor of studies and the relatively recent nascence of the Arab American health literature. In the absence of a systematic quality assessment of the literature, our literature review could not be considered systematic, a limitation of our work.
While progress has been made in expanding the geographic representation of studies and the inclusion of a few randomized trials, more longitudinal studies with population-representative samples will help improve our understanding of Arab Americans.
Future research directions
Future studies should aim to understand the diverse healthcare needs of Arab Americans and to better understand how to improve their experiences in healthcare. All institutions and organizations with an interest in helping improve minority health should identify Arab American populations in their databases and provide culturally competent services for improved care. Information taken on intake forms should include expanded information on race, religion, and cultural practices that may inform the care or health decision making of minority populations. Community based participatory research can be used by these institutions to develop interventions and to understand the health needs and desires of Arab American populations alongside the cultural nuances that influence health.
Second, understanding the needs of vulnerable sub-populations within the Arab American community should be prioritized. Understanding health needs within elderly Arab populations and the impact that increased life expectancy will have on these populations is important to our understanding of Arab American health more generally. The cultural processes and traditions associated with elder care and medical care may influence the health needs and resources available to this vulnerable populations over time. Another vulnerable population in need of active study are adolescents, and particularly adolescent women. Due to the compounding issues of acculturation, stress, and puberty, the health behaviors of this population should be better understood to develop targeted interventions. Studies aiming to examine Arab American sexual health should expand beyond the realm of female genital mutilation and attempt to provide culturally competent care and culturally relevant solutions to sexual health issues in this population.
Third, increasing the amount of information collected about acculturation status including immigration generation is important and necessary. Understanding the factors that make Arab American and Arab immigrants resilient will help contextualize Arab American health in the minority health landscape in the United States. Collecting data on religion should become a regular part of studies on mental health among Arab Americans. Evidence shows that assimilated Muslim Arab Americans experience higher levels of discrimination compared to their less assimilated counterparts and assimilated Christian Arab Americans (54). A better understanding of the role of religion could lead to productive collaborations between mental health providers and faith based institutions.
Finally, more creative studies using natural, political, or environmental experiments will also help the medical community understand the needs of this population in relation to the changing social and political environment in the United States. Using novel data streams to more rigorously sample Arab Americans nationally will help the medical community understand the contexts in which Arab Americans are accessing healthcare and may help improve their social experience in the United States overall. Ensuring the security and confidentiality of Arab Americans in these studies should be prioritized and emphasized to continue increasing the confidence of this community with medical and public health research.
Conclusion
Arab Americans are a socially and politically important immigrant group in the United States that has been increasing in size due to increased immigration over the past decade. More attention is needed to better understand the social and health needs of this population in the context of the changing political climate. Public health and medical researchers can improve their understanding of the health needs of Arab Americans through the identification and active recruitment of Arab Americans, the focus on vulnerable sub-populations, collecting data on acculturation and religion, and using novel longitudinal data streams. Understanding Arab American health needs in the context of the existing racial and minority health landscape in the United States will be important to better understanding immigrant health in the United States.
Statements
Author contributions
NA, AE-S, and SG contributed to the design of the research. NA implemented the research and analyzed the results. NA, AE-S, and SG contributed to the writing of the manuscript.
Acknowledgments
We thank the undergraduate research fellows from the Boston College W. F. Connell School of Nursing who assisted in the sorting of abstracts and full texts and for their assistance in the preliminary analysis for this comprehensive review: Margaret Dauer, Amanda Dulla, Amy Lu, and Kimberly Bretta. We would also like to thank the reviewers for their helpful comments in shaping the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2018.00262/full#supplementary-material
Footnotes
1.^Using Two Separate Questions for Race and Ethnicity in 2018 End-to-End Census: Hearing before the 2020 Census Program Memorandum Series (February 2, 2018, 2018).
References
1.
Arab American Institute Foundation. Underreported, Under Threat: Hate Crime in the United States and the Targeting of Arab Americans 1991-2016 (2018). Available online at: https://d3n8a8pro7vhmx.cloudfront.net/aai/pages/14141/attachments/original/1532368901/EXECUTIVE_SUMMARY.pdf?1532368901 (Accessed July 30, 2018)
2.
JamalAANaberNC. Race and Arab Americans Before and After 9/11: From Invisible Citizens to Visible Subjects.Syracuse, NY: Syracuse University Press (2008).
3.
El-SayedAMGaleaS. The health of Arab-Americans living in the United States: a systematic review of the literature. BMC Public Health (2009) 9:272. 10.1186/1471-2458-9-272
4.
Arab American Demographics. Arab American Institute Foundation (2014). Available online at: http://www.aaiusa.org/demographics
5.
BrittinghamADela Cruz GP. We the People of Arab Ancestry in the United States.Washington, DC: US Census Bureau (2005).
6.
OrfaleaG. The Arab Americans: A History. Ithaca, NY: Interlink Books (2006).
7.
HassanSD. Arabs, race and the post-September 11 national security state. Middle East Rep. (2002) 32:16–21.
8.
Executive Office of the President Office of Management and Budget (OMB) Office of Information and Regulatory Affairs. Standard for the Classification of Federal Data on Race and Ethnicity (1995). Available online at: https://www.whitehouse.gov/omb/fedreg_race-ethnicity
9.
KaroubJ. Census Bureau may count Arab-Americans for the first time in 2020 (2015). Available online at: http://www.pbs.org/newshour/rundown/census-bureau-considering-new-category-arab-americans-2020-count/
10.
MoherDShamseerLClarkeMGhersiDLiberatiAPetticrewMet al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. 10.1186/2046-4053-4-1
11.
RiceVHKulwickiA. Cigarette use among Arab Americans in the Detroit metropolitan area. Public Health Rep. (1992) 107:589–94.
12.
KulwickiASmileyKDevineS. Smoking behavior in pregnant Arab Americans. MCN Am J Matern Child Nurs. (2007) 32:363–7. 10.1097/01.NMC.0000298132.62655.0d
13.
TemplinTRiceVHGadelrabHWeglickiLHammadAKulwickiAet al. Trends in tobacco use among Arab/Arab-American adolescents: preliminary findings. Ethn Dis. (2005) 15(1 Suppl. 1):8.
14.
AthamnehLSansgirySSEssienEJAbughoshS. Predictors of intention to quit waterpipe smoking: a survey of arab americans in houston, Texas. J Addict. (2015) 2015:575479. 10.1155/2015/575479
15.
GiulianiKKWMireOLeinberger-JabariAEhrlichLCStiglerMHPryceDJet al. Cigarettes and the somali diaspora tobacco use among somali adults in Minnesota. Am J Prev Med. (2012) 43(5. Suppl. 3): S205–13. 10.1016/j.amepre.2012.08.002
16.
El-ShahawyOHaddadL. Correlation between nicotine dependence and barriers to cessation between exclusive cigarette smokers and dual (water pipe) smokers among Arab Americans. Subst Abuse Rehabil. (2015) 6:25–32. 10.2147/SAR.S72360
17.
Al-OmariHScheibmeirM. Arab Americans' acculturation and tobacco smoking. J Transcult Nurs. (2009) 20:227–33. 10.1177/1043659608330353
18.
RiceVHWeglickiLSTemplinTJamilHHammadA. Intervention effects on tobacco use in Arab and non-Arab American adolescents. Addict Behav. (2010) 35:46–8. 10.1016/j.addbeh.2009.07.005
19.
KahanD. Arab American college students' physical activity and body composition: reconciling middle east-west differences using the socioecological model. Res Q Exerc Sport. (2011) 82:118–28. 10.1080/02701367.2011.10599728
20.
AqtashSVanServellen G. Determinants of health-promoting lifestyle behaviors among arab immigrants from the region of the levant. Res Nurs Health. (2013) 36:466–77. 10.1002/nur.21555
21.
MohamedAAHassanAMWeisJASiaIGWielandML. Physical activity among Somali men in Minnesota: barriers, facilitators, and recommendations. Am J Mens Health. (2014) 8:35–44. 10.1177/1557988313489132
22.
DharodJMCroomJESadyCG. Food insecurity: its relationship to dietary intake and body weight among somali refugee women in the United States. J Nutr Educ Behav. (2013) 45:47–53. 10.1016/j.jneb.2012.03.006
23.
ArfkenCArnetzBFakhouriMVentimigliaMJamilH. Alcohol use among arab americans: what is the prevalence?J Immigr Minor Health (2011) 13:713–8. 10.1007/s10903-011-9447-8
24.
ArfkenCLOwensDSaidM. Binge drinking among arab/chaldeans: an exploratory study. J Ethn Subst Abuse (2012) 11:277–93. 10.1080/15332640.2012.735163
25.
ArfkenCLBerryAOwensD. Pathways for Arab Americans to substance abuse treatment in southeastern Michigan. J Muslim Ment Health (2009) 4:31–46. 10.1080/15564900902785457
26.
BurgerAEReitherENHofmannETMamelundS-E. The influence of hispanic ethnicity and nativity status on 2009 H1N1 pandemic vaccination uptake in the United States. J Immigr Minor Health (2017) 20:561–8. 10.1007/s10903-017-0594-4
27.
FryCASilvermanEPMillerS. Addressing pneumococcal vaccine uptake disparities among african-american adults in the United States. Public Health Nurs. (2016) 33:277–82. 10.1111/phn.12257
28.
GalbraithKVLechugaJJeneretteCMMooreLADPalmerMHHamiltonJB. Parental acceptance and uptake of the HPV vaccine among African-Americans and Latinos in the United States: a literature review. Soc Sci Med. (2016) 159:116–26. 10.1016/j.socscimed.2016.04.028
29.
DalloFJKindrattTB. Disparities in vaccinations and cancer screening among USand Foreign-Born Arab and European American Non-Hispanic White Women. Womens Health Issues (2015) 25:56–62. 10.1016/j.whi.2014.10.002
30.
PruittCNReeseCSGrossardtBRShireAMCreedonDJ. Completion of the human papillomavirus vaccination series lags in Somali adolescents. J Low Genit Tract Dis. (2013) 17:280–8. 10.1097/LGT.0b013e3182759a64
31.
JaberLABrownMBHammadAHowakSNZhuQGhafoorAet al. Epidemiology of diabetes among Arab Americans. Diabetes Care (2003) 26:308–13. 10.2337/diacare.26.2.308
32.
JaberLABrownMBHammadAZhuQHermanWH. The prevalence of the metabolic syndrome among Arab Americans. Diabetes Care (2004) 27:234–8. 10.2337/diacare.27.1.234
33.
DalloFJBorrellLN. Self-reported diabetes and hypertension among Arab Americans in the United States. Ethn Dis. (2006) 16:699–705. 10.1093/aje/163.suppl_11.S185-b
34.
NjeruJWTanEMStSauver JJacobsonDJAgunwambaAAWilsonPMet al. High rates of diabetes mellitus, pre-diabetes and obesity among somali immigrants and refugees in minnesota: a retrospective chart review. J Immigr Minor Health (2016) 18:1343–9. 10.1007/s10903-015-0280-3
35.
PinelliNRJaberLABrownMBHermanWHPinelliNRJaberLAet al. Serum 25-hydroxy vitamin d and insulin resistance, metabolic syndrome, and glucose intolerance among Arab Americans. Diabetes Care (2010) 33:1373–5. 10.2337/dc09-2199
36.
BertranEAFritzHAbbasMTarakjiSDiZazzo-MillerRPociaskFDet al. The impact of arab american culture on diabetes self-management education. Diabetes Educ. (2015) 41:748–54. 10.1177/0145721715607356
37.
FritzHDiZazzo-MillerRBertranEAPociaskFDTarakjiSArnetzJet al. Diabetes self-management among Arab Americans: patient and provider perspectives. BMC Int Health Hum Rights (2016) 16:22. 10.1186/s12914-016-0097-8
38.
BertranEAPinelliNRSillsSJJaberLA. The Arab American experience with diabetes: Perceptions, myths and implications for culturally-specific interventions. Prim Care Diabetes (2017) 11:13–9. 10.1016/j.pcd.2016.07.004
39.
Al-DahirSBraktaFKhalilABenrahlaM. The impact of acculturation on diabetes risk among Arab Americans in Southeastern Louisiana. J Health Care Poor Underserved. (2013) 24:47–63. 10.1353/hpu.2013.0038
40.
PinelliNRJaberLA. Practices of Arab American patients with type 2 diabetes mellitus during ramadan. J Pharm Pract. (2011) 24:211–5. 10.1177/0897190010367432
41.
PinelliNRBrownMBHermanWHJaberLA. Family support is associated with success in achieving weight loss in a group lifestyle intervention for diabetes prevention in Arab Americans. Ethn Dis. (2011) 21:480–4.
42.
JaberLAPinelliNRBrownMBFunnellMMAndersonRHammadAet al. Feasibility of group lifestyle intervention for diabetes prevention in Arab Americans. Diabetes Res Clin Pract. (2011) 91:307–15. 10.1016/j.diabres.2010.11.032
43.
PinelliNRHermanWHBrownMBJaberLAPinelliNRHermanWHet al. Perceived risk and the willingness to enroll in a diabetes prevention lifestyle intervention in Arab-Americans. Diabetes Res Clin Pract. (2010) 90:27. 10.1016/j.diabres.2010.08.010
44.
AmerMMHoveyJD. Anxiety and depression in a post-September 11 sample of Arabs in the USA. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:409–18. 10.1007/s00127-011-0341-4
45.
PadelaAIHeislerM. The association of perceived abuse and discrimination after September 11, 2001, with psychological distress, level of happiness, and health status among Arab Americans. Am J Public Health (2010) 100:284–91. 10.2105/AJPH.2009.164954
46.
JaberRMFarroukhMIsmailMNajdaJSobhHHammadAet al. Measuring depression and stigma towards depression and mental health treatment among adolescents in an Arab-American community. Int J Cult Ment Health (2015) 8:247–54. 10.1080/17542863.2014.953188
47.
JamilHHakim-LarsonJFarragMKafajiTDuqumIJamilLH. A retrospective study of Arab American mental health clients: trauma and the Iraqi refugees. Am J Orthopsychiatry (2002) 72:355–61. 10.1037/0002-9432.72.3.355
48.
TaylorEYanniEPezziCGuterbockMRothneyEHartonEet al. Physical and mental health status of iraqi refugees resettled in the United States. J Immigr Minor Health (2014) 16:1130–7. 10.1007/s10903-013-9893-6
49.
AbuelezamNNEl-SayedAMGaleaS. Arab American health in a racially charged US. Am J Prev Med. (2017) 52:810–2. 10.1016/j.amepre.2017.02.021
50.
MartinU. Psychotherapy with Arab Americans: an exploration of therapy-seeking and termination behaviors. Int J Cult Ment Health (2014) 7:162–7. 10.1080/17542863.2012.742121
51.
EllisBHLincolnAKCharneyMEFord-PazRBensonMStruninL. Mental health service utilization of somali adolescents: religion, community, and school as gateways to healing. Transcult Psychiatry (2010) 47:789–811. 10.1177/1363461510379933
52.
Abu-RasWAbu-BaderSH. The impact of the September 11, 2001, attacks on the well-being of Arab Americans in New York City. J Muslim Ment Health (2008) 3:217–39. 10.1080/15564900802487634
53.
EllisBHMacDonaldHZKlunk-GillisJLincolnAStruninLCabralHJ. Discrimination and mental health among Somali refugee adolescents: the role of acculturation and gender. Am J Orthopsychiatry (2010) 80:564–75. 10.1111/j.1939-0025.2010.01061.x
54.
AwadGH. The impact of acculturation and religious identification on perceived discrimination for Arab/Middle Eastern Americans. Cultur Divers Ethnic Minor Psychol. (2010) 16:59–67. 10.1037/a0016675
55.
AmerMMHoveyJD. Socio-demographic differences in acculturation and mental health for a sample of 2nd generation/early immigrant Arab Americans. J Immigr Minor Health (2007) 9:335–47. 10.1007/s10903-007-9045-y
56.
AbdulrahimSJamesSAYamoutRBakerW. Discrimination and psychological distress: does Whiteness matter for Arab Americans?Soc Sci Med. (2012) 75:2116–23. 10.1016/j.socscimed.2012.07.030
57.
NorrisAEAroianKJNickersonDM. Premigration persecution, postmigration stressors and resources, and postmigration mental health: a study of severely traumatized U.S. Arab Immigrant Women. J Am Psychiatr Nurses Assoc. (2011) 17:283–93. 10.1177/1078390311408900
58.
ArnetzBBTemplinTSaudiWJamilHArnetzBBTemplinTet al. Obstructive sleep apnea, posttraumatic stress disorder, and health in immigrants. Psychosom Med. (2012) 74:824–31. 10.1097/PSY.0b013e31826bf1ec
59.
HijaziAMLumleyMAZiadniMSHaddadLRapportLJArnetzBB. Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: a preliminary randomized clinical trial. J Trauma Stress (2014) 27:314–22. 10.1002/jts.21922
60.
BarkhoEFakhouriMArnetzJE. Intimate partner violence among Iraqi immigrant women in Metro Detroit: a pilot study. J Immigr Minor Health (2011) 13:725–31. 10.1007/s10903-010-9399-4
61.
KulwickiABalloutSKilgoreCHammadADervartanianH. Intimate partner violence, depression, and barriers to service utilization in arab American Women. J Transcult Nurs. (2015) 26:24–30. 10.1177/1043659614524000
62.
KulwickiAAswadBCarmonaTBalloutS. Barriers in the utilization of domestic violence services among Arab immigrant women: perceptions of professionals, service providers & community leaders. J Fam Violence (2010) 25:727–35. 10.1007/s10896-010-9330-8
63.
Abu-RasW. Cultural beliefs and service utilization by battered Arab immigrant women. Violence Against Women (2007) 13:1002–28. 10.1177/1077801207306019
64.
KulwickiADMillerJ. Domestic violence in the Arab American population: transforming environmental conditions through community education. Issues Ment Health Nurs. (1999) 20:199–215.
65.
Organization WH. Female Genital Mutilation, Fact Sheet (2018). Available online at: http://www.who.int/mediacentre/factsheets/fs241/en/
66.
ConnorJJHuntSFinsaasMCiesinskiAAhmedARobinsonBBE. Sexual health care, sexual behaviors and functioning, and female genital cutting: perspectives from somali women living in the United States. J Sex Res. (2016) 53:346–59. 10.1080/00224499.2015.1008966
67.
McNeelySChristie-deJong F. Somali refugees' perspectives regarding FGM/C in the US. Int J Migr Health Soc Care (2016) 12:157–69. 10.1108/IJMHSC-09-2015-0033
68.
BrownECarrollJFogartyCHoltC. 'They get a C-section…they gonna die': Somali women's fears of obstetrical interventions in the United States. J Transcult Nurs. (2010) 21:220–7. 10.1177/1043659609358780
69.
BeineKFullertonJPalinkasLAndersB. Conceptions of prenatal care among Somali women in San Diego. J Nurse Midwifery (1995) 40:376–81. 10.1016/0091-2182(95)00024-E
70.
Johnson-AgbakwuCEHelmTKillawiAPadelaAI. Perceptions of obstetrical interventions and female genital cutting: insights of men in a Somali refugee community. Ethn Health (2014) 19:440–57. 10.1080/13557858.2013.828829
71.
AmeresekereMBorgRFrederickJVragovicOSaiaKRajA. Somali immigrant women's perceptions of cesarean delivery and patient-provider communication surrounding female circumcision and childbirth in the USA. Int J Gynaecol Obstet. (2011) 115:227–30. 10.1016/j.ijgo.2011.07.019
72.
DeStephanoCCFlynnPMBrostBC. Somali prenatal education video use in a United States obstetric clinic: a formative evaluation of acceptability. Patient Educ Couns. (2010) 81:137–41. 10.1016/j.pec.2009.12.003
73.
JacobySDLucarelliMMusseFKrishnamurthyASalyersV. A mixed-methods study of immigrant somali women's health literacy and perinatal experiences in maine. J Midwifery Womens Health (2015) 60:593–603. 10.1111/jmwh.12332
74.
HerrelNOlevitchLDuBoisDKTerryPThorpDKindEet al. Somali refugee women speak out about their needs for care during pregnancy and delivery. J Midwifery Womens Health (2004) 49:345–9. 10.1016/j.jmwh.2004.02.008
75.
El-SayedAGaleaS. Interethnic mating and risk for preterm birth among Arab-American mothers: Evidence from the Arab-American Birth Outcomes Study. J Immigr Minor Health (2011) 13:445–52. 10.1007/s10903-010-9341-9
76.
SinghGKYuSM. Adverse pregnancy outcomes: differences between US-and foreign-born women in major US racial and ethnic groups. Am J Public Health (1996) 86:837–43.
77.
WingateMSAlexanderGR. The healthy migrant theory: variations in pregnancy outcomes among US-born migrants. Soc Sci Med. (2006) 62:491–8. 10.1016/j.socscimed.2005.06.015
78.
El-SayedAMGaleaS. Explaining the low risk of preterm birth among Arab Americans in the United States: an analysis of 617451 births. Pediatrics (2009) 123:438. 10.1542/peds.2008-1634
79.
ElReda DKGrigorescuVPosnerSFDavis-HarrierA. Lower rates of preterm birth in women of Arab ancestry: an epidemiologic paradox–Michigan, 1993-2002. Matern Child Health J. (2007) 11:622–7. 10.1007/s10995-007-0199-y
80.
YanniEACopelandGOlneyRS. Birth defects and genetic disorders among Arab Americans – Michigan, 1992-2003. J Immigr Minor Health (2010) 12:408–13. 10.1007/s10903-008-9203-x
81.
MaPMagnusMMagnusJ. Perception of pregnancy related health issues among arab women living in the United States. J Immigr Minor Health (2013) 15:273–80. 10.1007/s10903-012-9589-3
82.
WojnarDM. Perinatal experiences of somali couples in the United States. J Obstet Gynecol Neonatal Nurs. (2015) 44:358–69. 10.1111/1552-6909.12574
83.
El-SayedAHadleyCGaleaS. Birth outcomes among Arab Americans in Michigan before and after the terrorist attacks of September 11, 2001. Ethn Dis. (2008) 18:348–56.
84.
El-SayedAMGaleaS. Community context, acculturation and low-birth-weight risk among Arab Americans: evidence from the Arab-American birth-outcomes study. J Epidemiol Community Health (2010) 64:155–60. 10.1136/jech.2008.084491
85.
HensleyAlford SSchwartzKSolimanAJohnsonCCGruberSBMerajverSD. Breast cancer characteristics at diagnosis and survival among Arab-American women compared to European- and African-American women. Breast Cancer Res Treat. (2009) 114:339–46. 10.1007/s10549-008-9999-z
86.
KawarLN. Jordanian and palestinian immigrant women's knowledge, affect, cultural attitudes, health habits, and participation in breast cancer screening. Health Care Women Int. (2009) 30:768–82. 10.1080/07399330903066111
87.
ArshadSWilliamsKPMabisoADeySSolimanAS. Evaluating the knowledge of breast cancer screening and prevention among Arab-American women in Michigan. J Cancer Educ. (2011) 26:135–8. 10.1007/s13187-010-0130-x
88.
HirkoKASolimanASBanerjeeMRuterbuschJHarfordJBChamberlainRMet al. Characterizing inflammatory breast cancer among Arab Americans in the California, Detroit and New Jersey Surveillance, Epidemiology and End Results (SEER) registries (1988-2008). Springerplus (2013) 2:3. 10.1186/2193-1801-2-3
89.
Al-AmoudiSCañasJHohlSDDistelhorstSRThompsonB. Breaking the silence: breast cancer knowledge and beliefs among somali muslim women in seattle, Washington. Health Care Women Int. (2015) 36:608–16. 10.1080/07399332.2013.857323
90.
KawarLN. Barriers to breast cancer screening participation among Jordanian and Palestinian American women. Eur J Oncol Nurs. (2013) 17:88–94. 10.1016/j.ejon.2012.02.004
91.
Petro-NustasWNortonMEVilhauerRPConnellyAD. Health beliefs associated with breast cancer screening among Arab women in the Northeastern United States. Int J Health Promot Educ. (2012) 50:273–7. 10.1080/14635240.2012.723374
92.
WilliamsKPMabisoATodemDHammadAHill-AshfordYHamadeHet al. Differences in knowledge of breast cancer screening among African American, Arab American, and Latina women. Prev Chronic Dis. (2011) 8:A20. Available online at: www.cdc.gov/pcd/issues/2011/jan/09_0185.htm (Accessed on August 30, 2018).
93.
SaadiABondBPercac-LimaS. Perspectives on preventive health care and barriers to breast cancer screening among iraqi women refugees. J Immigr Minor Health (2012) 14:633–9. 10.1007/s10903-011-9520-3
94.
SaadiABondBEPercac-LimaS. Bosnian, iraqi, and somali refugee women speak: a comparative qualitative study of refugee health beliefs on preventive health and breast cancer screening. Women's Health Issues (2015) 25:501–8. 10.1016/j.whi.2015.06.005
95.
PadelaAMurrarSAdvientoBLiaoCHosseinianZPeekMet al. Associations between religion-related factors and breast cancer screening among american muslims. J Immigr Minor Health (2015) 17:660–9. 10.1007/s10903-014-0014-y
96.
ObeidatRFLallyRMDickersonSS. Arab american women's lived experience with early-stage breast cancer diagnosis and surgical treatment. Cancer Nurs. (2012) 35:302–11. 10.1097/NCC.0b013e318231db09
97.
DalloFJZakarTBorrellLNFakhouriMJamilH. Cancer knowledge increases after a brief intervention among Arab Americans in Michigan. J Cancer Educ. (2011) 26:139–46. 10.1007/s13187-010-0179-6
98.
ElmubarakEBromfieldEBovell-BenjaminACElmubarakEBromfieldEBovell-BenjaminA. Focused interviews with Sudanese Americans: perceptions about diet, nutrition, and cancer. Prev Med. (2005) 40:502–9. 10.1016/j.ypmed.2004.09.021
99.
MellonSGauthierJCichonMHammadASimonM. Knowledge, Attitudes, and Beliefs of Arab-American Women Regarding Inherited Cancer Risk. J Genet Couns. (2013) 22:268–76. 10.1007/s10897-012-9546-2
100.
GhebreRSewaliBOsmanSAdaweANguyenHOkuyemiKet al. Cervical cancer: barriers to screening in the somali community in minnesota. J Immigr Minor Health (2015) 17:722–8. 10.1007/s10903-014-0080-1
101.
SewaliBPrattRAbdiwahabEFahiaSCallKTOkuyemiKS. Understanding cancer screening service utilization by somali men in Minnesota. J Immigr Minor Health (2015) 17:773–80. 10.1007/s10903-014-0032-9
102.
TalaatN. Adherence and barriers to colorectal cancer screening varies among Arab Americans from different countries of origin. Arab J Gastroenterol. (2015) 16:116–20. 10.1016/j.ajg.2015.07.003
103.
RaymondNCOsmanWO'BrienJMAliNKiaFMohamedFet al. Culturally informed views on cancer screening: a qualitative research study of the differences between older and younger Somali immigrant women. BMC Public Health (2014) 14:1–16. 10.1186/1471-2458-14-1188
104.
SewaliBOkuyemiKSAskhirABelinsonJVogelRIJosephAet al. Cervical cancer screening with clinic-based Pap test versus home HPV test among Somali immigrant women in Minnesota: a pilot randomized controlled trial. Cancer Med. (2015) 4:620–31. 10.1002/cam4.429
105.
MorrisonTBFlynnPMWeaverALWielandML. Cervical cancer screening adherence among somali immigrants and refugees to the United States. Health Care Women Int. (2013) 34:980–8. 10.1080/07399332.2013.770002
106.
ViciniFAShahCWallaceMJonesPDykesVTullJet al. Strategies for reducing cancer incidence and mortality in African American and Arab American and Chaldean communities in the Detroit metropolitan area. Am J Clin Oncol. (2012) 35:316–21. 10.1097/COC.0b013e318210f9b5
107.
KhanFRuterbuschJJGomezSLSchwartzK. Differences in the cancer burden among foreign-born and US-born Arab Americans living in metropolitan Detroit. Cancer Causes Control. (2013) 24:1955–61. 10.1007/s10552-013-0271-4
108.
SchwartzKLKulwickiAWeissLKFakhouriHSakrWKauGet al. Cancer among Arab Americans in the metropolitan Detroit area. Ethn Dis. (2004) 14:141–6.
109.
PetersonLSolimanARuterbuschJSmithNSchwartzK. Comparison of exposures among arab american and non-hispanic white female thyroid cancer cases in metropolitan detroit. J Immigr Minor Health (2011) 13:1033–40. 10.1007/s10903-011-9485-2
110.
BergmansRSolimanASRuterbuschJMezaRHirkoKGraffJet al. Cancer incidence among arab americans in california, detroit, and new jersey SEER registries. Am J Public Health (2014) 104:83. 10.2105/AJPH.2014.301954
111.
MoussawiAYassineMDeySSolimanA. Clinical profile, quality of care, and recurrence in arab-american and caucasians prostate cancer patients in michigan. J Immigr Minor Health (2013) 15:803–9. 10.1007/s10903-012-9662-y
112.
TailakhAMentesJCMoriskyDEPikeNAPhillipsLREvangelistaLS. Prevalence, awareness, treatment, and control of hypertension among arab Americans. J Cardiovasc Nurs. (2013) 28:330–7. 10.1097/JCN.0b013e31825638ae
113.
JamilHFakhouriMDalloFTemplinTKhouryRFakhouriH. Self-reported heart disease among Arab and Chaldean American women residing in southeast Michigan. Ethn Dis. (2008) 18:19–25.
114.
JamilHTemplinTFakhouriMRiceVHKhouriRFakhouriH. Comparison of personal characteristics, tobacco use, and health states in Chaldean, Arab American, and non-Middle Eastern white adults. J Immigr Minor Health (2009) 11:310–7. 10.1007/s10903-008-9125-7
115.
KempainenRNelsonKWilliamsDNHedemarkL. Mycobacterium tuberculosis disease in Somali immigrants in Minnesota. Clinical Investigations (2001) 119:176–80. 10.1378/chest.119.1.176
116.
RockRBSutherlandWMBakerCWilliamsDN. Extrapulmonary tuberculosis among Somalis in Minnesota. Emerg Infect Dis. (2006) 12:1434–6. 10.3201/eid1209.050295
117.
ShireAMSandhuDSKaiyaJKOseiniAMYangJDChaiteerakijRet al. Viral hepatitis among somali immigrants in minnesota: association of hepatitis C with hepatocellular carcinoma. Mayo Clin Proc. (2012) 87:17–24. 10.1016/j.mayocp.2011.08.001
118.
JamilLHDuffyMCFakhouriMJamilHJ. Prevalence of antibodies to the hepatitis C virus among arab and chaldean Americans in Southeast Michigan, Usa. Ethn Dis. (2013) 23:18–21.
119.
GoldDRWrightR. Population disparities in asthma. Annu Rev Public Health (2005) 26:89–113. 10.1146/annurev.publhealth.26.021304.144528
120.
JamilHRaymondDFakhouriMTemplinTKhouryRFakhouriHet al. Self-reported asthma in chaldeans, arabs, and african Americans: factors associated with asthma. J Immigr Minor Health (2011) 13:568–75. 10.1007/s10903-010-9390-0
121.
JohnsonMNriaguJHammadASavoieKJamilH. Asthma, environmental risk factors, and hypertension among arab Americans in metro detroit. J Immigr Minor Health (2010) 12:640–51. 10.1007/s10903-008-9205-8
122.
JohnsonMNriaguJHammadASavoieKJamilH. Asthma prevalence and severity in Arab American communities in the Detroit area, Michigan. J Immigr Health (2005) 7:165–78. 10.1007/s10903-005-3673-x
123.
DalloFBoozaJNguyenN. Functional limitations and nativity status among Older Arab, Asian, Black, Hispanic, and White Americans. J Immigr Minor Health (2015) 17:535–42. 10.1007/s10903-013-9943-0
124.
AjrouchKJ. Resources and well-being among Arab-American elders. J Cross Cult Gerontol. (2007) 22:167–82. 10.1007/s10823-006-9033-z
125.
AhmedSRKia-KeatingMTsaiKH. A structural model of racial discrimination, acculturative stress, and cultural resources among Arab American adolescents. Am J Community Psychol. (2011) 48:181–92. 10.1007/s10464-011-9424-3
126.
AroianKJTemplinTNHoughEERamaswamyVKatzA. A longitudinal family-level model of Arab Muslim adolescent behavior problems. J Youth Adolesc. (2011) 40:996–1011. 10.1007/s10964-010-9615-5
127.
AroianKHoughESTemplinTNKulwickiARamaswamyVKatzA. A model of mother-child adjustment in Arab Muslim immigrants to the US. Soc Sci Med. (2009) 69:1377–86. 10.1016/j.socscimed.2009.08.027
128.
AroianKJ. Discrimination against muslim american adolescents. J Sch Nurs. (2012) 28:206–13. 10.1177/1059840511432316
129.
Munro-KramerMFavaNMSaftnerMADarling-FisherCTateNHStoddardSAet al. What are we missing? Risk behaviors among Arab-American adolescents and emerging adults. J Am Assoc Nurse Pract. (2016) 28:493–502. 10.1002/2327-6924.12352
130.
Abu-SaadH. Cultural components of pain: the Arab-American child. Issues Compr Pediatr Nurs. (1984) 7:91–9. 10.3109/01460868409009047
131.
LipsonJGReizianAEMeleisAI. Arab-American patients: a medical record review. Soc Sci Med. (1987) 24:101–7. 10.1016/0277-9536(87)90242-5
132.
ReizianAMeleisAI. Symptoms reported by Arab-American patients on the Cornell Medical Index (CMI). West J Nurs Res. (1987) 9:368–84. 10.1177/019394598700900308
133.
LaffreySCMeleisAILipsonJGSolomonMOmidianPA. Assessing Arab-American health care needs. Soc Sci Med. (1989) 29:877–83. 10.1016/0277-9536(89)90087-7
134.
MayKM. Middle-Eastern immigrant parents' social networks and help-seeking for child health care. J Adv Nurs. (1992) 17:905–12.
135.
MeleisAILipsonJGPaulSM. Ethnicity and health among five Middle Eastern immigrant groups. Nurs Res. (1992) 41:98–103. 10.1097/00006199-199203000-00008
136.
KulwickiACassPS. An assessment of Arab American knowledge, attitudes, and beliefs about AIDS. Image J Nurs Sch. (1994) 26:13–7. 10.1111/j.1547-5069.1994.tb00288.x
137.
HattarpollaraMMeleisAI. The stress of immigration and the daily lived experiences of jordanian immigrant women in the United-States. West J Nurs Res. (1995) 17:521–39. 10.1177/019394599501700505
138.
JaberLASlaughterRLGrunbergerG. Diabetes and related metabolic risk-factors among arab-americans. Ann Pharmacother. (1995) 29:573–6. 10.1177/106002809502900603
139.
KulwickiA. An ethnographic study of illness perceptions and practices of Yemeni-Arabs in Michigan. J Cult Divers. (1996) 3:80–9.
140.
PowerDVShandyDJ. Sudanese refugees in a Minnesota family practice clinic. Fam Med. (1998) 30:185-9.
141.
ChatkoffDKLeonardMT. A preliminary investigation of cognitive appraisal and cardiovascular reactivity and recovery in Arab Americans. Ethn Dis. (2009) 19:258–64.
142.
DalloFJJamesSA. Acculturation and blood pressure in a community-based sample of Chaldean-American women. J Immigr Health. (2000) 2:145–53. 10.1023/A:1009560903668
143.
KulwickiADMillerJSchimSM. Collaborative partnership for culture care: enhancing health services for the Arab community. J Transcult Nurs. (2000) 11:31–9. 10.1177/104365960001100106
144.
GreesonCJVeachPMLeRoyBS. A Qualitative investigation of somali immigrant perceptions of disability: implications for genetic counseling. J Genet Couns. (2001) 10:359–78. 10.1023/A:1016625103697
145.
HatahetWKhoslaPFungweTV. Prevalence of risk factors to coronary heart disease in an Arab-American population in southeast Michigan. Int J Food Sci Nutr. (2002) 53:325–35. 10.1080/09637480220138124
146.
IslamSMSJohnsonCA. Correlates of smoking behavior among Muslim Arab-American adolescents. Ethn Health. (2003) 8:319–37. 10.1080/13557850310001631722
147.
JaberLABrownMBHammadAZhuQHermanWH. Lack of acculturation is a risk factor for diabetes in Arab immigrants in the U.S.Diabetes Care (2003) 26:2010–4. 10.2337/diacare.26.7.2010
148.
KulwickiARiceVH. Arab American adolescent perceptions and experiences with smoking. Public Health Nurs. (2003) 20:177–83. 10.1046/j.0737-1209.2003.20304.x
149.
ReadRWChenPPBhandariAMillsRPCinciripiniGSTaylorCC. Intraocular pressure in a Somali population living in the United States. J Glaucoma (2003) 12:365–9. 10.1097/00061198-200308000-00012
150.
RiceVHTemplinTKulwickiA. Arab-American adolescent tobacco use: four pilot studies. Prev Med. (2003) 37:492–8. 10.1016/S0091-7435(03)00175-0
151.
BarryDT. Measuring acculturation among male Arab immigrants in the United States: an exploratory study. J Immigr Health (2005) 7:179–84. 10.1007/s10903-005-3674-9
152.
BeitinBKAllenKR. Resilience in Arab American couples after September 11, 2001: a systems perspective. J Marital Fam Ther. (2005) 31:251–67. 10.1111/j.1752-0606.2005.tb01567.x
153.
GeltmanPLGrant-KnightWMehtaSDLloyd-TravagliniCLustigSLandgrafJMet al. The 'lost boys of Sudan': functional and behavioral health of unaccompanied refugee minors resettled in the United States. Arch Pediatr Adolesc Med. (2005) 159:585–91. 10.1001/archpedi.159.6.585
154.
JohnsonMHammadANriaguJOSavoieKJamilH. Environmental disease burden in Arab-American communities in the Detroit area: prevalence and severity. Ethn Dis. (2005) 15(1 Suppl. 1):6.
155.
ReadJnGAmickBDonatoKM. Arab immigrants: a new case for ethnicity and health?Soc Sci Med. (2005) 61:77–82. 10.1016/j.socscimed.2004.11.054
156.
SlotnickMJNriaguJOJohnsonMMLinderAMSavoieKLJamilHJet al. Profiles of trace elements in toenails of Arab-Americans in the Detroit area, Michigan. Biol Trace Elem Res. (2005) 107:113–26. 10.1385/BTER:107:2:113
157.
RiceVHWeglickiLSTemplinTHammadAJamilHKulwickiA. Predictors of Arab American adolescent tobacco use. Merrill Palmer Q. (Wayne StateUniv. Press) (2006). 52:327–42.
158.
WissinkLJones-WebbRDuBoisDKrinkeBIbrahimQ. Improving health care provision to Somali refugee women. Minn Med. (2005) 88:36–40.
159.
DeShawPJ. Use of the emergency department by Somali immigrants and refugees. Minn Med. (2006) 89:42–5.
160.
KridliSA-OHermanWHBrownMBFakhouriHJaberLA. The epidemiology of diabetes and its risk factors among Chaldean Americans. Ethn Dis. (2006) 16:351–6.
161.
KridliSA-OHermanWHBrownMBFakhouriHJaberLA. For the patient. Diabetes and its risk factors among Chaldean Americans. Ethn Dis. (2006) 16:588.
162.
LauderdaleDS. Birth outcomes for Arabic-named women in California before and after September 11. Demography (2006) 43:185–201. 10.1353/dem.2006.0008
163.
RobertsonCLHalconLSavikKJohnsonDSpringMButcherJet al. Somali and Oromo refugee women: trauma and associated factors. J Adv Nurs. (2006) 56:577–87. 10.1111/j.1365-2648.2006.04057.x
164.
TompkinsMSmithLJonesKSwindellsS. HIV education needs among Sudanese immigrants and refugees in the Midwestern United States. AIDS Behav. (2006) 10:319–23. 10.1007/s10461-005-9060-8
165.
WeiSFeldmanGLMonaghanKG. Cystic fibrosis testing among Arab-Americans. Genet Med. (2006) 8:255–8. 10.1097/01.gim.0000214453.74456.f3
166.
BerlieHDHammadAJaberLA. The use of glucose-lowering agents and aspirin among Arab Americans with diabetes. Ethn Dis. (2007) 17(2, Suppl. 3):S45.
167.
CarrollJEpsteinRFiscellaKVolpeEDiazKOmarS. Knowledge and beliefs about health promotion and preventive health care among Somali women in the United States. Health Care Women Int. (2007) 28:360–80. 10.1080/07399330601179935
168.
El-EssawiDMusialJLHammadALimHW. A survey of skin disease and skin-related issues in Arab Americans. J Am Acad Dermatol. (2007) 56:933–8. 10.1016/j.jaad.2007.01.031
169.
HassounehDMKulwickiA. Mental health, discrimination, and trauma in Arab Muslim women living in the US: a pilot study. Ment Health Relig Cult. (2007) 10:257–62. 10.1080/13694670600630556
170.
HuWTFoleyTAWilcoxRAKozeraRMMorgensternBZJuhnYJ. Childhood obesity among Head Start enrollees in southeastern Minnesota: Prevalence and risk factors. Ethn Dis. (2007) 17:23–8.
171.
JamilHFarragMHakim-LarsonJKafajiTAbdulkhaleqHHammadA. Mental health symptoms in Iraqi refugees: posttraumatic stress disorder, anxiety, and depression. J Cult Divers. (2007) 14:19–25.
172.
JamilHNassar-McMillanSCLambertRG. Immigration and attendant psychological sequelae: a comparison of three waves of Iraqi immigrants. Am J Orthopsychiatry (2007) 77:199–205. 10.1037/0002-9432.77.2.199
173.
WeglickiLSTemplinTHammadAJamilHAbou-MedieneSFarroukhMet al. Tobacco use patterns among high school students: do Arab American youth differ?Ethn Dis. (2007) 17(2, Suppl. 3):S24.
174.
ArfkenCLKubiakSPFarragM. Arab Americans in publicly financed alcohol/other drug abuse treatment. Alcohol Treat Q. (2008) 26:229–40. 10.1080/07347320802071547
175.
BakerOGRiceV. Predictors of narghile (water-pipe) smoking in a sample of American Arab Yemeni adolescents. J Transcult Nurs. (2008) 19:24–32. 10.1177/1043659607309141
176.
BerlieHDHermanWHBrownMBHammadAJaberLA. Quality of diabetes care in Arab Americans. Diabetes Res Clin Pract. (2008) 79:249–55. 10.1016/j.diabres.2007.09.003
177.
EllisBHMacDonaldHZLincolnAKCabralHJ. Mental health of Somali adolescent refugees: the role of trauma, stress, and perceived discrimination. J Consult Clin Psychol. (2008) 76:184–93. 10.1037/0022-006X.76.2.184
178.
GiulianiKKWMireOAJamaSDuBoisDKPryceDFahiaSet al. Tobacco use and cessation among somalis in minnesota. Am J Prev Med. (2008) 351(6, Suppl. S):S462. 10.1016/j.amepre.2008.09.006
179.
JamilHFakhouriMDalloFTemplinTKhouryRFakhouriH. Disparities in self-reported diabetes mellitus among Arab, Chaldean, and Black Americans in Southeast Michigan. J Immigr Minor Health. (2008) 10:397–405. 10.1007/s10903-007-9108-0
180.
JamilHGrzybowskiMHakim-LarsonJFakhouriMSahutogluJKhouryRet al. Factors associated with self-reported depression in Arab, Chaldean, and African Americans. Ethn Dis. (2008) 18:464-70.
181.
KulwickiAKhalifaRMooreG. The effects of September 11 on Arab American nurses in metropolitan Detroit. J Transcult Nurs. (2008) 19:134–9. 10.1177/1043659607313071
182.
NilssonJEBrownCRussellEBKhamphakdy-BrownS. Acculturation, partner violence, and psychological distress in refugee women from Somalia. J Interpers Violence (2008) 23:1654–63. 10.1177/0886260508314310
183.
NorrisAEAroianKJNorrisAEAroianKJ. Avoidance symptoms and assessment of posttraumatic stress disorder in Arab immigrant women. J Trauma Stress. (2008) 21:471–8. 10.1002/jts.20363
184.
SchwartzKFakhouriMBartocesMMonsurJYounisA. Mammography screening among Arab American women in metropolitan Detroit. J Immigr Minor Health (2008) 10:541–9. 10.1007/s10903-008-9140-8
185.
ShahSMAyashCPharaonNAGanyFM. Arab American immigrants in New York: health care and cancer knowledge, attitudes, and beliefs. J Immigr Minor Health (2008) 10:429–36. 10.1007/s10903-007-9106-2
186.
WeglickiLSTemplinTNRiceVHJamilHHammadAWeglickiLSet al. Comparison of cigarette and water-pipe smoking by Arab and non-Arab-American youth. Am J Prev Med. (2008) 35:334–9. 10.1016/j.amepre.2008.06.037
187.
AbdulrahimSBakerW. Differences in self-rated health by immigrant status and language preference among Arab Americans in the Detroit Metropolitan Area. Soc Sci Med. (2009) 68:2097–103. 10.1016/j.socscimed.2009.04.017
188.
ArfkenCLKubiakSPFarragM. Acculturation and polysubstance abuse in Arab-American treatment clients. Transcult Psychiatry (2009) 46:608–22. 10.1177/1363461509351364
189.
DalloFJAlSnih SAjrouchKJ. Prevalence of disability among US- and foreign-born Arab Americans: results from the 2000 US Census. Gerontology (2009) 55:153–61. 10.1159/000151538
190.
HobbsRDHabibZAlromaihiDIdiLParikhNBlockiFet al. Severe vitamin D deficiency in Arab-American women living in Dearborn, Michigan. Endocr Pract. (2009) 15:35–40. 10.4158/EP.15.1.35
191.
JohnsonCEAliSAShippMPL. Building community-based participatory research partnerships with a somali refugee community. Am J Prev Med. (2009) 37(6, Suppl. 1):S236. 10.1016/j.amepre.2009.09.036
192.
NessSM. Pain expression in the perioperative period: insights from a focus group of Somali women. Pain Manag Nurs. (2009) 10:65–75. 10.1016/j.pmn.2008.05.001
193.
RamaswamyVAroianKJTemplinT. Adaptation and psychometric evaluation of the multidimensional scale of perceived social support for Arab American adolescents. Am J Community Psychol. (2009) 43:49–56. 10.1007/s10464-008-9220-x
194.
WrobelNHFarragMFHymesRW. Acculturative stress and depression in an elderly Arabic sample. J Cross Cult Gerontol. (2009) 24:273–90. 10.1007/s10823-009-9096-8
195.
KiraIALewandowskiLTemplinTRamaswamyVOzkanBMohaneshJ. The effects of perceived discrimination and backlash on Iraqi refugees' mental and physical health. J Muslim Ment Health (2010) 5:59–81. 10.1080/15564901003622110
196.
El-SayedAMTracyMScarboroughPGaleaS. Suicide among Arab-Americans. PLoS ONE (2011) 6:e14704. 10.1371/journal.pone.0014704
197.
ArnetzJRofaYArnetzBVentimigliaMJamilH. Resilience as a protective factor against the development of psychopathology among refugees. J Nerv Ment Dis. (2013) 201:167–72. 10.1097/NMD.0b013e3182848afe
198.
KiraIALewandowskiLAshbyJSTemplinTRamaswamyVMohaneshJ. The traumatogenic dynamics of internalized stigma of mental illness among arab American, Muslim, and Refugee Clients. J Am Psychiatr Nurses Assoc. (2014) 20:250–66. 10.1177/1078390314542873
199.
BettmannJEPenneyDClarksonFreeman PLecyN. Somali refugees' perceptions of mental illness. Soc Work Health Care (2015) 54:738–57. 10.1080/00981389.2015.1046578
200.
KulwickiABalloutS. Post traumatic stress disorder (Ptsd) in arab American refugee and recent immigrant women. J Cult Divers (2015) 22:9–12.
201.
PrattRFadumoAHangMOsmanSRaymondN. Perceptions of mental illness in the Somali community in Minnesota. Int J Migr Health Soc Care (2016) 12:16–25. 10.1108/IJMHSC-04-2014-0011
202.
SamariG. Cross-border ties and Arab American mental health. Soc Sci Med. (2016) 155:93–101. 10.1016/j.socscimed.2016.03.014
203.
SalmanKF. Health beliefs and practices related to cancer screening among arab muslim women in an urban community. Health Care Women Int. (2012) 33:45–74. 10.1080/07399332.2011.610536
204.
WielandMMorrisonTChaSRahmanAChaudhryR. Diabetes care among somali immigrants and refugees. J Community Health (2012) 37:680–4. 10.1007/s10900-011-9499-7
205.
SalinitriFDPinelliNRMartinETJaberLA. Insulin sensitivity and secretion in arab americans with glucose intolerance. Diabetes Technol Ther. (2013) 15:1019–24. 10.1089/dia.2013.0045
206.
NjeruJWHagi-SalaadMFHajiHChaSSWielandML. Diabetes health literacy among somali patients with diabetes mellitus in a US primary care setting. J Racial Ethn Health Disparities (2016) 3:210–6. 10.1007/s40615-015-0129-4
207.
AbdulrahimSAjrouchK. Social and cultural meanings of self-rated health: Arab immigrants in the United States. Qual Health Res. (2010) 20:1229–40. 10.1177/1049732310371104
208.
JamilHNassar-McMillanbSLambertRWangdYAgerJArnetzB. Pre- and post-displacement stressors and time of migration as related to self-rated health among Iraqi immigrants and refugees in Southeast Michigan. Med Confl Surviv. (2010) 26:207–22. 10.1080/13623699.2010.513655
209.
OgunleyeOSheltonJAIrelandAGlickMYehJ. Preferences for labor and delivery practices between pregnant immigrants and U.S.-born patients: a comparative prospective antenatal survey study. J Natl Med Assoc. (2010) 102:481–4. 10.1016/S0027-9684(15)30555-1
210.
PavlishCLNoorSBrandtJ. Somali immigrant women and the American health care system: discordant beliefs, divergent expectations, and silent worries. Soc Sci Med. (2010) 71:353–61. 10.1016/j.socscimed.2010.04.010
211.
QahoushRStottsNAlawnehMSFroelicherES. Physical activity in Arab women in Southern California. Eur J Cardiovasc Nurs. (2010) 9:263–71. 10.1016/j.ejcnurse.2010.03.002
212.
RotheEHoltCKuhnCMcAteerTAskariIO'MearaMet al. Barriers to outdoor physical activity in wintertime among somali youth. J Immigr Minor Health (2010) 12:726–36. 10.1007/s10903-009-9287-y
213.
SarsourLTongVSJaberOTalbiMJulliardK. Health assessment of the arab american community in southwest brooklyn. J Community Health (2010) 35:653–9. 10.1007/s10900-010-9260-7
214.
SteinmanLDoescherMKeppelGAPak-GorsteinSGrahamEHaqAet al. Understanding infant feeding beliefs, practices and preferred nutrition education and health provider approaches: an exploratory study with Somali mothers in the USA. Matern Child Nutr. (2010) 6:67–88. 10.1111/j.1740-8709.2009.00185.x
215.
AyashCAxelrodDNejmeh-KhourySAzizAYusrAGanyF. A community intervention: AMBER: Arab American breast cancer Education and referral program. J Immigr Minor Health (2011) 13:1041–7. 10.1007/s10903-011-9481-6
216.
BrittinHCObeidatBA. Food practices, changes, preferences and acculturation of Arab students in US universities. Int J Consum Stud. (2011) 35:552–9. 10.1111/j.1470-6431.2011.01023.x
217.
El-SayedAMTracyMScarboroughPGaleaS. Ethnic inequalities in mortality: the case of Arab-Americans. PLoS ONE (2011) 6:e29185. 10.1371/journal.pone.0029185
218.
FlynnPMFosterEMBrostBC. Indicators of acculturation related to somali refugee women's birth outcomes in minnesota. J Immigr Minor Health (2011) 13:224–31. 10.1007/s10903-009-9289-9
219.
GurnahKKhoshnoodKBradleyEYuanC. Lost in translation: reproductive health care experiences of somali bantu women in Hartford, Connecticut. J Midwifery Womens Health (2011) 56:340–6. 10.1111/j.1542-2011.2011.00028.x
220.
NriaguJSenthamarai-KannanRJamilHFakhoriMKorponicS. Lead poisoning among Arab American and African American children in the Detroit metropolitan area, Michigan. Bull Environ Contam Toxicol. (2011) 87:238–44. 10.1007/s00128-011-0346-4
221.
PadelaAIRasheedSWarrenGJWChoiHMathurAK. Factors associated with positive attitudes toward organ donation in Arab Americans. Clin Transplant. (2011) 25:800–8. 10.1111/j.1399-0012.2010.01382.x
222.
SalemWFlynnPWeaverABrostB. Fertility After Cesarean Delivery Among Somali-Born Women Resident in the USA. J Immigr Minor Health (2011) 13:494–9. 10.1007/s10903-010-9362-4
223.
SmithBDSilkK. Cultural competence clinic: an online, interactive, simulation for working effectively with arab american muslim patients. Acad Psychiatry (2011) 35:312–6. 10.1176/appi.ap.35.5.312
224.
BenbenekMMGarwickAW. Enablers and barriers to dietary practices contributing to bone health among early adolescent Somali girls living in Minnesota. J Spec Pediatr Nurs. (2012) 17:205–14. 10.1111/j.1744-6155.2012.00334.x
225.
DalloFSchwartzKRuterbuschJBoozaJWilliamsD. Mortality Rates Among Arab Americans in Michigan. J Immigr Minor Health (2012) 14:236–41. 10.1007/s10903-011-9441-1
226.
DevlinJTDhalacDSuldanAAJacobsAGuledKBankoleKA. Determinants of physical activity among somali women living in maine. J Immigr Minor Health (2012) 14:300–6. 10.1007/s10903-011-9469-2
227.
HillNHuntEHyrkäsK. Somali Immigrant Women's Health Care experiences and beliefs regarding pregnancy and birth in the United States. J Transcult Nurs. (2012) 23:72–81. 10.1177/1043659611423828
228.
JadallaALeeJ. The relationship between acculturation and general health of Arab Americans. J Transcult Nurs. (2012) 23:159–65. 10.1177/1043659611434058
229.
TamiSHReedDBBoylanMZvonkovicA. Assessment of the effect of acculturation on dietary and physical activity behaviors of Arab mothers in Lubbock, Texas. Ethn Dis. (2012) 22:192–7.
230.
BeatsonJE. Supporting refugee Somali Bantu mothers with children with disabilities. Pediatr Nurs. (2013) 39:142–5.
231.
CaronRTshabangu-SokoTFinefrockK. Childhood lead poisoning in a somali refugee resettlement community in new hampshire. J Community Health (2013) 38:660–9. 10.1007/s10900-013-9661-5
232.
ClarksonFreeman PAPenneyDSBettmannJELecyN. The intersection of health beliefs and religion among somali refugees: a qualitative study. J Relig Spiritual Soc Work (2013) 32:1–13. 10.1080/15426432.2013.749141
233.
DeckysCSpringerP. The elderly somali bantu refugees' adjustment to american healthcare. Online J Cult Competence Nurs Healthc. (2013) 3:3–15. 10.9730/ojccnh.org/v3n1a1
234.
FinktonDEl-SayedAGaleaS. Infant mortality among arab-americans: findings from the arab-american birth outcomes study. Matern Child Health J. (2013) 17:732–45. 10.1007/s10995-012-1049-0
235.
GeltmanPLAdamsJHCochranJDorosGRybinDHenshawMet al. The impact of functional health literacy and acculturation on the oral health status of Somali refugees living in Massachusetts. Am J Public Health (2013) 103:1516–23. 10.2105/AJPH.2012.300885
236.
HaddadLCorcoranJ. C ulturally tailored smoking cessation for arab american male smokers in community settings: a pilot study. Tob Use Insights. (2013) 6:17–23. 10.4137/TUI.S11837
237.
Henning-SmithCShippeeTPMcAlpineDHardemanRFarahF. Stigma,discrimination, or symptomatologydifferences in self-reported mental health between us-born and somalia-born black Americans. Am J Public Health (2013) 103:861–7. 10.2105/AJPH.2012.301184
238.
TalaatNHarbW. Reluctance to screening colonoscopy in Arab Americans: a community based observational study. J Community Health (2013) 38:619–25. 10.1007/s10900-013-9688-7
239.
AlkhateebHMAbushihabEF. Self-esteem and Arab-American elementary students. Psychol Rep. (2014) 115:805–9. 10.2466/07.11.PRO.115c27z9
240.
BekhetAKZauszniewskiJA. Individual characteristics and relocation factors affecting adjustment among relocated american and egyptian older adults. Issues Ment Health Nurs. (2014) 35:80–7. 10.3109/01612840.2013.842620
241.
FilippiMFaseruBBairdMNdikum-MofforFGreinerKDaleyC. A pilot study of health priorities of somalis living in kansas city: laying the groundwork for CBPR. J Immigr Minor Health (2014) 16:314–20. 10.1007/s10903-012-9732-1
242.
HaddadLEl-ShahawyOGhadbanR. Comparison of barriers to cessation among Arab American smokers of cigarettes and waterpipe. Int J Environ Res Public Health (2014) 11:9522–31. 10.3390/ijerph110909522
243.
HearstMOKehmRShermanSLechnerKE. increasing fruit and vegetable consumption and offerings to somali children: The FAV-S pilot study. J Prim Care Community Health (2014) 5:139–43. 10.1177/2150131913513269
244.
KiraIALewandowskiLAshbyJSSomersCChiodoLOdenatL. Does bullying victimization suppress IQ? the effects of bullying victimization on IQ in Iraqi and African American Adolescents: a traumatology perspective. J Aggress Maltreat Trauma (2014) 23:431–53. 10.1080/10926771.2014.904463
245.
PerumalswamiPVMillerFDOrabeeHRegabAAdamsMKapelusznikLet al. Hepatitis C screening beyond CDC guidelines in an Egyptian immigrant community. Liver Int. (2014) 34:253–8. 10.1111/liv.12259
246.
PoolerJGleasonSF. Comparison of WIC benefit redemptions in michigan indicates higher utilization among Arab American Families. J Nutr Educ Behav. (2014) 46:(Suppl. 3):S45–52. 10.1016/j.jneb.2014.02.019
247.
DalloFJKindrattTB. Disparities in preventive health behaviors among non-Hispanic White men: heterogeneity among foreign-born Arab and European Americans. Am J Mens Health (2015) 9:124–31. 10.1177/1557988314532285
248.
ElsouhagDArnetzBJamilHLumleyMBroadbridgeCArnetzJ. factors associated with healthcare utilization among arab immigrants and iraqi refugees. J Immigr Minor Health (2015) 17:1305–12. 10.1007/s10903-014-0119-3
249.
GoforthANPhamAVOkaER. Parent–child conflict, acculturation gap, acculturative stress, and behavior problems in Arab American Adolescents. J Cross Cult Psychol. (2015) 46:821–36. 10.1177/0022022115585140
250.
HouseyMDeGuirePLyon-CalloSWangLMarderWMcCuneWJet al. Incidence and prevalence of systemic lupus erythematosus among Arab and Chaldean Americans in southeastern Michigan: the Michigan Lupus Epidemiology and Surveillance Program. Am J Public Health (2015) 105:74. 10.2105/AJPH.2014.302423
251.
JadallaAAHattarMSchubertCC. Acculturation as a predictor of health promoting and lifestyle practices of Arab Americans: a Descriptive Study. J Cult Divers. (2015) 22:15–22.
252.
KassemNOFKassemNOJacksonSRDaffaRMLilesSHovellMF. Arab-american hookah smokers: initiation, and pros and cons of hookah use. Am J Health Behav. (2015) 39:680–7. 10.5993/AJHB.39.5.10
253.
MikalJPWoodfieldB. Refugees, post-migration stress, and internet use: a qualitative analysis of intercultural adjustment and internet use among iraqi and sudanese refugees to the United States. Qual Health Res. (2015) 25:1319–33. 10.1177/1049732315601089
254.
MurrayKEMohamedASDawsonDBSymeMAbdiSBarnack-TaviarisJ. Somali perspectives on physical activity: photovoice to address barriers and resources in San Diego. Prog Commun Health Partnersh (2015) 9:83–90. 10.1353/cpr.2015.0011
255.
OdunukanOWAbdulaiRMHagiSalaad MFLahrBDFlynnPMWielandML. Provider and interpreter preferences among somali women in a primary care setting. J Prim Care Community Health (2015) 6:105–10. 10.1177/2150131914552846
256.
SalmanKResickL. The Description of health among iraqi refugee women in the United States. J Immigr Minor Health (2015) 17:1199–205. 10.1007/s10903-014-0035-6
257.
WielandMTiedjeKMeiersSMohamedAFormeaCRidgewayJet al. Perspectives on physical activity among immigrants and refugees to a small urban community in Minnesota. J Immigr Minor Health (2015) 17:263–75. 10.1007/s10903-013-9917-2
258.
DalloFRuterbuschJKirmaJSchwartzKFakhouriM. A Health profile of arab Americans in Michigan: a novel approach to using a hospital administrative database. J Immigr Minor Health (2016) 18:1449–54. 10.1007/s10903-015-0296-8
259.
DalloFJKindrattTB. Disparities in chronic disease prevalence among non-hispanic whites: heterogeneity among foreign-born arab and European Americans. J Racial Ethn Health Disparities (2016) 3:590–8. 10.1007/s40615-015-0178-8
260.
GoforthANPhamAVChunHCastro-OlivoSMYosaiER. Association of acculturative stress, Islamic practices, and internalizing symptoms among Arab American adolescents. Sch Psychol Q. (2016) 31:198–212. 10.1037/spq0000135
261.
LincolnAKLazarevicVWhiteMTEllisBH. The impact of acculturation style and acculturative hassles on the mental health of somali adolescent refugees. J Immigr Minor Health (2016) 18:771–8. 10.1007/s10903-015-0232-y
262.
McClellandMLWeekesCVNBazziHWarwinskyJAbouarabiWSnellFet al. Perception of Obesity in African-American and Arab-American Minority Groups. J Racial Ethn Health Disparities (2016) 3:160–7. 10.1007/s40615-015-0127-6
263.
MissalBClarkCKovalevaM. Somali immigrant new mothers' childbirth experiences in Minnesota. J Transcult Nurs. (2016) 27:359–67. 10.1177/1043659614565248
264.
PadelaAIVuMMuhammadHMarfaniFMallickSPeekMet al. Religious beliefs and mammography intention: findings from a qualitative study of a diverse group of American Muslim women. Psychooncology (2016) 25:1175–82. 10.1002/pon.4216
265.
VuMAzmatARadejkoTPadelaAI. Predictors of delayed healthcare seeking among American Muslim Women. J Womens Health (2016) 25:586–93. 10.1089/jwh.2015.5517
266.
DalloFJ. Health Disparities. New York, NY: Handbook of Arab American Psychology; Routledge (2015).
Summary
Keywords
health disparities, arab american, stress, diabetes, mental health, women's health, child health, infectious disease
Citation
Abuelezam NN, El-Sayed AM and Galea S (2018) The Health of Arab Americans in the United States: An Updated Comprehensive Literature Review. Front. Public Health 6:262. doi: 10.3389/fpubh.2018.00262
Received
03 May 2018
Accepted
22 August 2018
Published
11 September 2018
Volume
6 - 2018
Edited by
Yasser Khazaal, Université de Genève, Switzerland
Reviewed by
Jacqueline Sin, University of Reading, United Kingdom; Shervin Assari, University of Michigan, United States
Updates
Copyright
© 2018 Abuelezam, El-Sayed and Galea.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nadia N. Abuelezam nadia.abuelezam@bc.edu
This article was submitted to Public Mental Health, a section of the journal Frontiers in Public Health
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.