- 1Department of Health Policy and Management, School of Public Health, Peking University, Beijing, China
- 2Department of Immunization Program, Zhejiang Provincial Center for Disease Control and Prevention, Zhejiang, China
Objectives: We aim to analyze equity in maternal, newborn, and child health (MNCH) interventions in Jilin, a northeastern province of China, 2008–2018.
Study design: Cross-sectional study.
Methods: We used provincially representative survey data from 2008, 2013, and 2018. We included 18 essential MNCH interventions, analyzed equity, and calculated the composite coverage score. We used logistic and multiple linear regressions to adjust sampling clusters and covariates.
Results: Coverage of hospital-based interventions, such as hospital delivery and antenatal B-ultrasound tests, was nearly universal in Jilin province. Cesarean sections persisted at alarmingly high rates (57.6%). Enormous unmet needs and rural–urban inequalities existed for community-based interventions, such as improved drinking water sources (85.4 vs. 97.9%, p < 0.01), improved sanitation facilities (52.5 vs. 94.2%, p < 0.01), four government-funded antenatal care services (55.8 vs. 84.1%, p < 0.01), and at least eight antenatal care sessions (26.8 vs. 46.3%, p < 0.05). Compared to rural–urban inequity, individual-level disparities across income and education were either small in scale or statistically insignificant. The inequity in coverage of maternal and newborn care shrank during 2008–2018.
Conclusions: Despite its success in reducing mortality, China's unique obstetrician-led safe motherhood strategy may come at the cost of over-medicalization and health inequity. Jilin province's recent efforts to revitalize primary health care show the potential to make a change. An integrated system that links families, communities, and all levels of health care organizations seems to be the most effective and efficient model to offer continuing MNCH care.
Introduction
Global health initiatives, such as the Millennium Development Goals (MDGs) and the Sustainable Development Goals (SDGs), prioritize maternal, newborn, and child health (MNCH) (1, 2). Consensus was reached to extend health coverage along the MNCH care continuum with the rationale of effectively linking families, communities, and all levels of health care providers as a means to universal coverage (3–5). Focusing on 75 prioritized countries, the Countdown to 2015 (now Countdown to 2030) represents a decade of efforts to monitor the trends of coverage and equity in a series of essential MNCH interventions (6, 7). However, China is the only country that has not yet reported its equity profiles (8, 9).
Notably, China adopted a unique hospital-based birth strategy in the 1990s and successfully achieved MDGs 4 and 5, which required each country to reduce its maternal mortality by three quarters and under-five mortality by two thirds between 1990 and 2015 (10–12). Endorsing the Law of Maternal and Infant Health in 1995, the Chinese government established several policies and programs to promote universal hospital births. Hospital deliveries are heavily subsidized with both demand- and supply-side financing mechanisms; community-based traditional birth attendants are abandoned, midwives are marginalized by obstetricians, and certification of birth-attendance services is gradually centralizing from primary care providers to county hospitals and above (10, 13–15). National data in China show that hospital births increased from <50% to almost 100% during 1988 and 2008 (16). The rise in hospital births fully account for the descending trends in maternal mortality and may prevent 48–70% of neonatal deaths in China (10, 17). Although these are positive trends, there are concerns that such a doctor-led approach may usher in over-medicalization and health system fragmentation, which may exacerbate health inequity (12, 18).
Interestingly, China experienced dramatic changes in its health system development. During the 1960s−1980s, China adopted a community-based, people-centered, and de-professionalized health development approach. The World Health Organization (WHO) recognized China's experience in scaling up essential health care coverage, which inspired many principles of primary health care that were promoted in the Alma Ata Declaration (18, 19). However, after the 1980s, China experienced a substantial shift to a laissez-faire paradigm and medicalization, moving the health provision focus from primary health care to disease-centered, highly specialized, and high-cost tertiary care (19, 20). Aware of these problems, the Chinese government has been proposing a new round of health reform since 2009 with health equity as a core issue. This reform aims to reorient the country's health system to primary health care (21–23). One milestone is the National Essential Public Health Services program. In this program, the government offers free access to a package of essential health care services and pays particular attention to MNCH (24–26). Previous studies on China's health system reform mainly focused on the general uptake of inpatient or outpatient care, while few reports incorporated the aforementioned contextual changes when specifically analyzing China's safe-motherhood policies (12, 27).
With a land area of 187,000 square kilometers and a population of 27.5 million, Jilin province is located in northeastern China and can be considered a typical province of China in terms of socioeconomic and health system development (please see Appendix 1 for the mapped location and detailed socio-demographic profiles). In this study, we aim to describe the equity of Jilin province in the context of China's health system reform using three waves of provincially representative health survey data from 2008, 2013, and 2018. We attempt to draw lessons for both China and other low- and middle-income countries (LIMCs) on how to strengthen a country's health system effectively and efficiently to extend coverage of essential MNCH interventions.
Methods
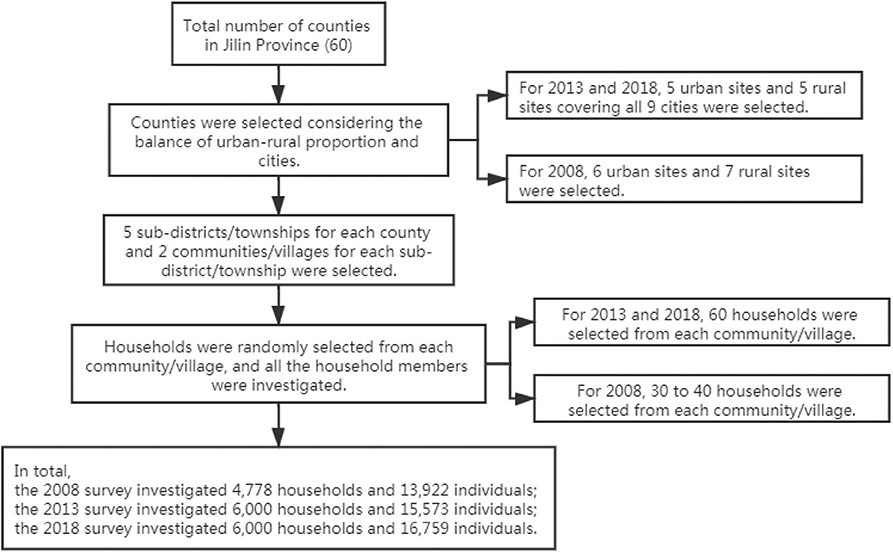
We used data from three cross-sectional waves of the National Health Service Survey (NHSS) that were conducted in Jilin province, China in 2008, 2013, and 2018. For each wave, expanded provincially representative household samples were obtained using a four-stage, stratified, clustered, random sampling procedure (28). The sampling procedure is shown in Figure 1 (for details of the sampling maps and the population covered, please see Appendix 2). Qualified investigators conducted the household interviews using structured questionnaires. Basic information on households, health status of household members, demands and utilization of health services, and information on maternal and child care was collected. In our study, we used parts of households, mothers with live births in the past 5 years and children under 5 years old.
We included 18 essential MNCH interventions building on the Countdown, the latest WHO recommendations on quality antenatal care services that were released in 2016, and China's National Essential Public Health Services program (8, 29). The interventions were classified into three domains along the MNCH care continuum according to the target population: water and sanitation, maternal and newborn care, and child care. Within the first domain, we analyzed coverage of improved drinking water sources and sanitation facilities using the Countdown definitions (8). Within the maternal and newborn care domain, we analyzed coverage of the following eight interventions: at least one, four, five, and eight sessions of antenatal care; four types of government-funded antenatal services; hospital delivery; cesarean section; and at least one session of postnatal care. We defined a mother as receiving four types of government-funded antenatal services if she received all four types of services that are freely provided in China's National Essential Public Health Services program at least once during her antenatal period. The four services are blood testing, blood pressure monitoring, urine testing, and B-ultrasound examination; the former three were analyzed as antenatal care quality in a recent study (30). Note that these services were not included in the 2018 survey. Within the child care domain, we analyzed coverage of growth monitoring services (≥1 check) for all 3 years, early initiation of breastfeeding and exclusive breastfeeding within 6 months in specific years considering comparable definitions of the interventions and the following five vaccinations in 2008 and 2013: one dose of BCG, one dose of measles, three doses of DPT, hepatitis B, and polio vaccines. The intervention variables for households and women had no missing data. For the child-related intervention variables, we excluded missing data. We assumed that the effect was negligible because missing data accounted for only 3.8% of all the survey data although more missing data occurred for children living in rural areas.
To better compare the coverage and equity of MNCH interventions, we additionally constructed an overall MNCH care composite coverage score and three specific composite coverage scores for different domains of the MNCH care continuum, adopting the Countdown approach: (31, 32) water and sanitation coverage score, maternal and newborn care coverage score, and child immunization coverage score (Figure 2). The three specific composite coverage scores were calculated for each target object. The intervention in the formulas had a value of 1 if used and 0 otherwise. The overall composite coverage score was calculated for the population using the average scores of the specific composite coverage scores in the target population. All the composite scores were transformed to proportions ranging from 0 to 100%. We excluded interventions that were not surveyed in all 3 years from the overall composite coverage score calculation. Cesarean sections were also excluded because there is no consensus on the ideal rates (31), and the actual rates are all higher than 50% in Jilin province. We analyzed correlations between different composite coverage scores and child health outcomes (under-five mortality rates and under-five stunting rates) at the county level to check the validation. The water and sanitation coverage score showed significantly negative correlations with both outcomes. The maternal and newborn care coverage score and the overall composite coverage score showed significantly negative correlations with under-five stunting rates. The child immunization coverage score showed no significant correlations with either outcome, but we retained it because it is still a concern for other LIMCs. For more details on the correlation analysis, please see Appendix 3.
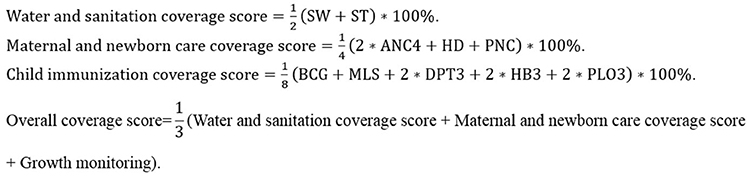
Figure 2. Formulas for building composite coverage scores for essential interventions along the MNCH care continuum. SW, Improved drinking water sources; ST, Improved sanitation facilities; ANC4, At least four antenatal care sessions; HD, Hospital delivery; PNC, At least one postnatal care session; BCG, BCG vaccination; MSL, Measles vaccination; DPT3, DPT vaccination (3 doses); HB3, Hepatitis B vaccination (3 doses); PLO3, Polio vaccination (3 doses). The child immunization coverage score was only available for 2008 and 2013 and was thus not calculated in the overall coverage score.
We focused on the coverage equity for different rural–urban settings, educational achievements, and household income groups. We used the rural–urban classification of the National Bureau of Statistics of the People's Republic of China, which defines townships as rural and subdistricts as urban. We grouped households' economic status as poor vs. rich, separated by the median per capita annual income for each survey separately ($730, $1,977, and $2,171 in 2008, 2013, and 2018, respectively). We grouped educational achievements into primary and below and secondary and above.
The survey also collected information on household heads' or mothers' educational achievement, ethnicity, households' distance to the nearest health facility, mothers' and children's health insurance coverage, and other covariates, such as mothers' age at childbirth, parity, and children's age in months and sex. These variables were adjusted in the equity analysis considering the unequal distributions in different groups.
We described the trends of the 18 essential interventions and the composite coverage scores using bar graphs and used chi-square tests to test the differences. We analyzed the equity gaps for these interventions, adopting the dots-plot approach that was developed by the Countdown (32). In the Countdown, mean coverage rates in each wealth quintile are displayed intuitively by differently colored dots in a line. We used logistic regressions (for each intervention) and multiple linear regressions (for composite coverage scores) adjusting for relevant variables and calculated marginal means for rural–urban settings, poor and rich, and different educational achievement groups. We display the marginal means in each group instead of the unadjusted mean coverage rates used in the Countdown. We used multiple linear regressions, accounting for sampling clusters, to analyze the trends and factors associated with the composite coverage scores. These analyses were all implemented in Stata 13.0.
Results
In total, we analyzed data from 16,778 households, 1,534 mothers, and 1,725 children (Table 1). Household income per capita tripled during 2008–2018 with medians ranging from $730 to $2,171 in Jilin province, China. Almost all of the mothers achieved primary and above education. Social insurance coverage increased from 70% to nearly universal from 2008 to 2018 for mothers, but for children, it was relatively low at 81.6% in 2018. Multiparity increased from below 30% in 2008 and 2013 to 41.8% in 2018, and 85% of the mothers gave birth at the age of 20–34.
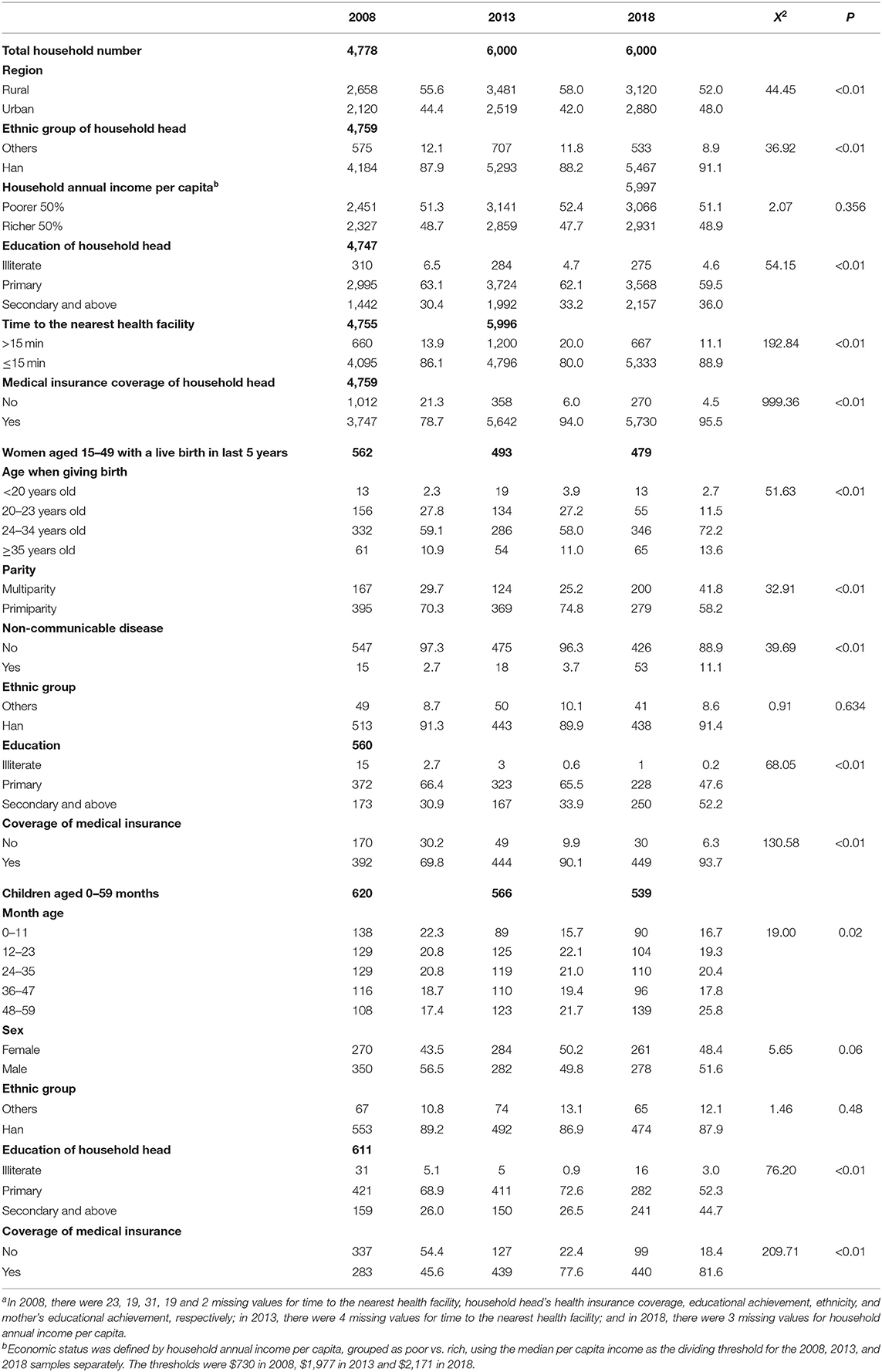
Table 1. Characteristics of investigated households, mothers, and children, Jilin province, China (2008–2018)a.
As Figure 3 shows, coverage of hospital delivery and each of the five child vaccinations had already been above 90.0% since 2008. The proportions of mothers who received at least four antenatal care sessions (from 73.0% in 2008 to 92.9% in 2018), at least five antenatal care sessions (from 61.6% in 2008 to 85.4% in 2018), at least eight antenatal care sessions (from 25.1% in 2008 to 58.9% in 2018), and at least one postnatal care session (from 56.0% in 2008 to 74.7% in 2018) were relatively low but increased significantly since 2013 (p < 0.01). The proportion of cesarean sections increased from 51.8 to 64.9% during 2008–2013 and decreased to 56.8% in 2018. Falls after a rise were observed for coverage of improved drinking water sources (from 86.7% in 2008 to 93.7% in 2013 and to 90.2% in 2018, p < 0.01), improved sanitation facilities (from 64.1% in 2008 to 75.0% in 2013 and to 64.6% in 2018 again, p < 0.01), and at least one session of growth monitoring (from 70.6% in 2008 to 74.5% in 2013 and to 51.0% in 2018, p < 0.01). Additionally, the four types of government-funded antenatal care services increased significantly from 50.4 to 82.2% during 2008–2013. Coverage of early initiation of breastfeeding (~30%) and exclusive breastfeeding within 6 months (~65%) seemed sluggish during 2008–2018. In sum, the water and sanitation coverage score rose from 75.4% in 2008 to 84.3% in 2013 and then fell back to 77.4% in 2018; the maternal and newborn care coverage score increased from ~75% during 2008–2013 to 90.1% in 2018; and the overall coverage scores were 73.6, 78.4, and 72.8% in 2008, 2013, and 2018, respectively. The child immunization coverage scores were all higher than 90%.
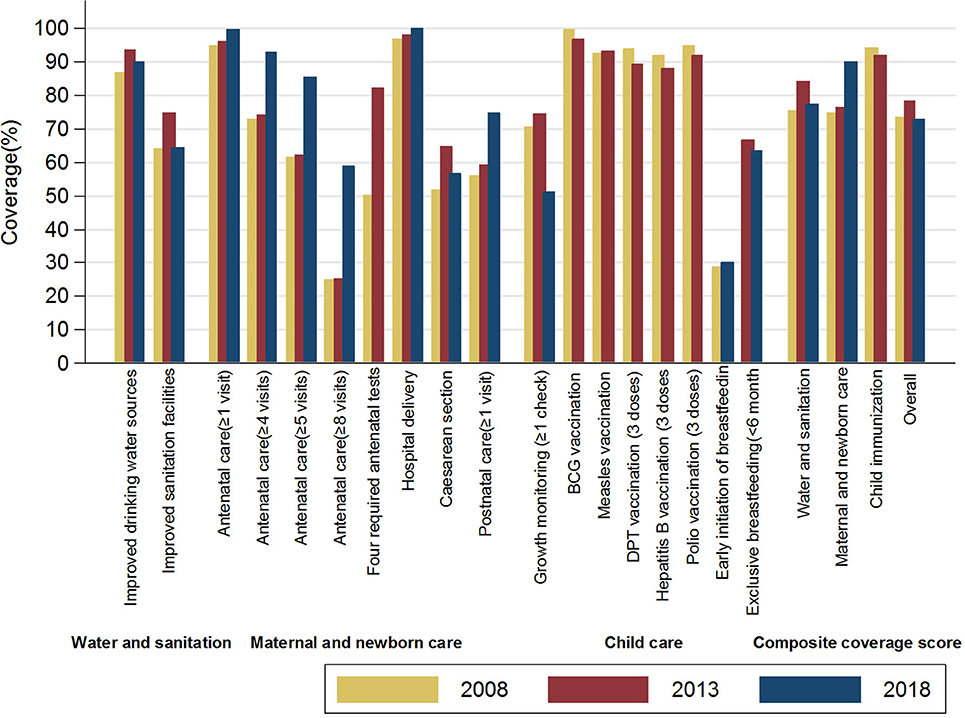
Figure 3. Essential MNCH intervention coverage along the care continuum, Jilin province, China (2008–2018).
(a) Four government-funded antenatal services, defined as whether the mother received all four types of services at least once during her antenatal period. These services are freely provided by China's National Essential Public Health Services program and include blood testing, blood pressure monitoring, urine testing, and B-ultrasound examinations.
(b) Water and sanitation coverage score is the composite coverage score for improved drinking water sources and improved sanitation facilities.
(c) Maternal and newborn care coverage score is the composite coverage score for antenatal care, hospital delivery, and postnatal care.
(d) Child immunization coverage score is the composite coverage score for five types of child immunization.
(e) Overall coverage score is the composite coverage score for water and sanitation, maternal and newborn care, and child growth monitoring. Child immunization coverage scores were excluded because we lacked data in 2018.
Figures 4–6 illustrate the equity gaps for the 18 essential MNCH interventions and the composite coverage scores between urban and rural settings, poor and rich households, and women with above and below primary education (all these values were predicted by logistic regression models adjusting for other covariates. For details of the regression analyses, please see Appendix 4). The results reveal different types of inequity in different domains. In the water and sanitation domain, substantial rural–urban equity gaps exist for coverage of improved drinking water sources (85.4 vs. 97.9%, p < 0.01) and improved sanitation facilities (52.5 vs. 94.2%, p < 0.01), whereas the adjusted equity gaps were relatively small across rich vs. poor and household heads with high vs. low educational achievement. In the maternal and newborn care domain, most interventions had similarly small equity gaps except for four government-funded antenatal care services (55.8 vs. 84.1% for rural vs. urban, p < 0.01) and at least eight antenatal care sessions (26.8 vs. 46.3% for rural vs. urban, p < 0.05). In the child care domain, most of the differences were either small in scale or statistically insignificant.
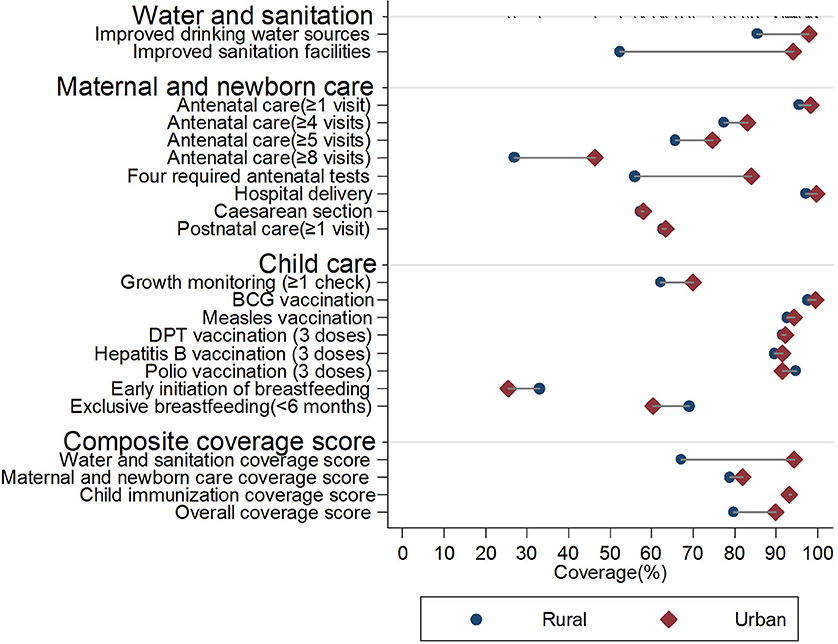
Figure 4. Equity gaps between rural and urban settings in essential MNCH interventions, Jilin province, China (2008–2018). For details of the regression results for each specific intervention, please see Appendix 4.
(a) In the water and sanitation domain, the interventions were adjusted for setting, household economic status, time to the nearest health facility, household head educational achievement, health insurance coverage, and ethnicity.
(b) In the maternal and newborn domain, the interventions were adjusted for setting, household economic status, time to the nearest health facility, mother's educational achievement, health insurance coverage, age when giving birth, parity, and ethnicity.
(c) In the child care domain, the interventions were adjusted for setting, household economic status, household head educational achievement, time to the nearest health facility, children's health insurance, age in months, sex, and ethnicity.
(d) Hospital delivery and BCG vaccination were not adjusted because the proportions were near 100%.
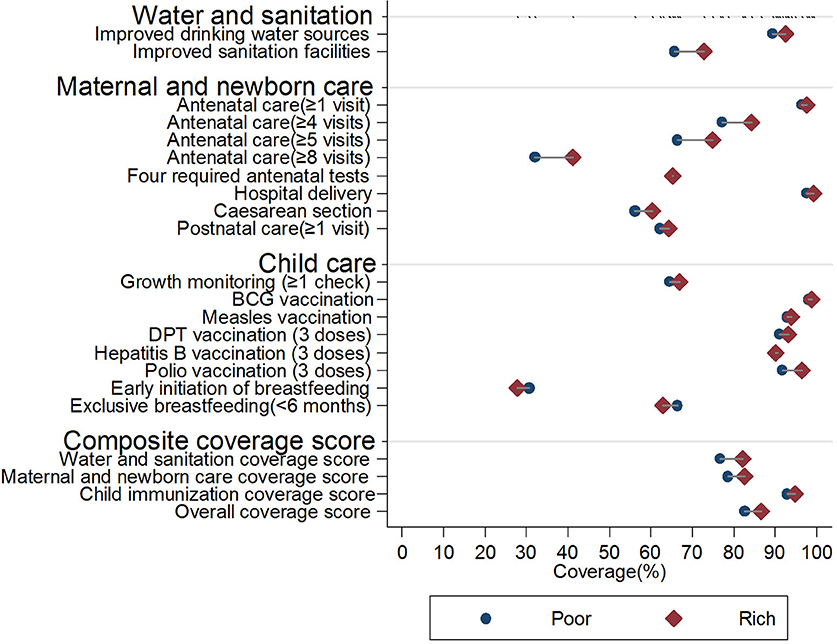
Figure 5. Equity gaps between poor and rich essential MNCH interventions, Jilin province, China (2008–2018). For details of the regression results for each specific intervention, please see Appendix 4.
(a) In the water and sanitation domain, the interventions were adjusted for setting, household economic status, time to the nearest health facility, household head educational achievement, health insurance coverage, and ethnicity.
(b) In the maternal and newborn domain, the interventions were adjusted for setting, household economic status, time to the nearest health facility, mother's educational achievement, health insurance coverage, age when giving birth, parity, and ethnicity.
(c) In the child care domain, the interventions were adjusted for settings, household economic status, household head educational achievement, time to the nearest health facility, children's health insurance, age in months, sex, and ethnicity.
(d) Hospital delivery and BCG vaccination were not adjusted because the proportions were near 100%.
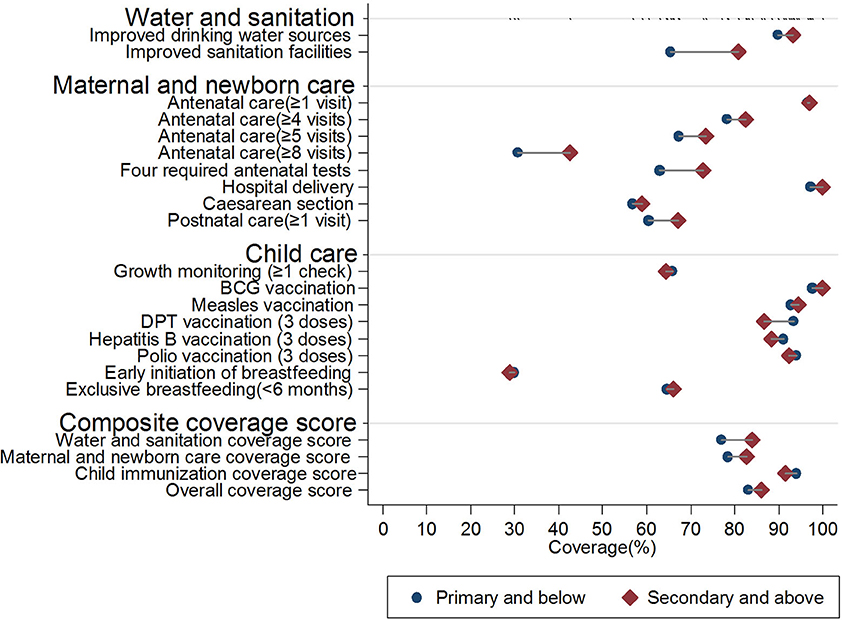
Figure 6. Equity gaps between low and high educational achievements in essential MNCH interventions, Jilin province, China (2008–2018). For details of the regression results for each specific intervention, please see Appendix 4.
(a) In the water and sanitation domain, the interventions were adjusted for setting, household economic status, time to the nearest health facility, household head educational achievement, health insurance coverage, and ethnicity.
(b) In the maternal and newborn domain, the interventions were adjusted for setting, household economic status, time to the nearest health facility, mother's educational achievement, health insurance coverage, age when giving birth, parity, and ethnicity.
(c) In the child care domain, the interventions were adjusted for setting, household economic status, household head educational achievement, time to the nearest health facility, children's health insurance, age in months, sex, and ethnicity.
(d) Hospital delivery and BCG vaccination were not adjusted because the proportions were near 100%.
Table 2 shows the factors associated with the composite coverage scores and the trends. For the water and sanitation coverage score, the adjusted urban–rural difference was 27.3% (95% CI 22.3–32.3%), whereas the effects of household-level economic status and educational achievement were substantially attenuated by other factors (adjusted differences 5.4%, 95% CI 3.3–7.5% comparing rich and poor and 6.6%, 95% CI 4.2–9.0% comparing above and below primary education). For maternal and newborn care coverage scores, the adjusted urban–rural, poor–rich, and high–low educational differences were relatively small. In addition, mothers who could access a health facility in 15 min had higher composite coverage scores than those who could access a health facility in more than 15 min (adjusted difference 9.4%, 95% CI 2.7–16.1%).
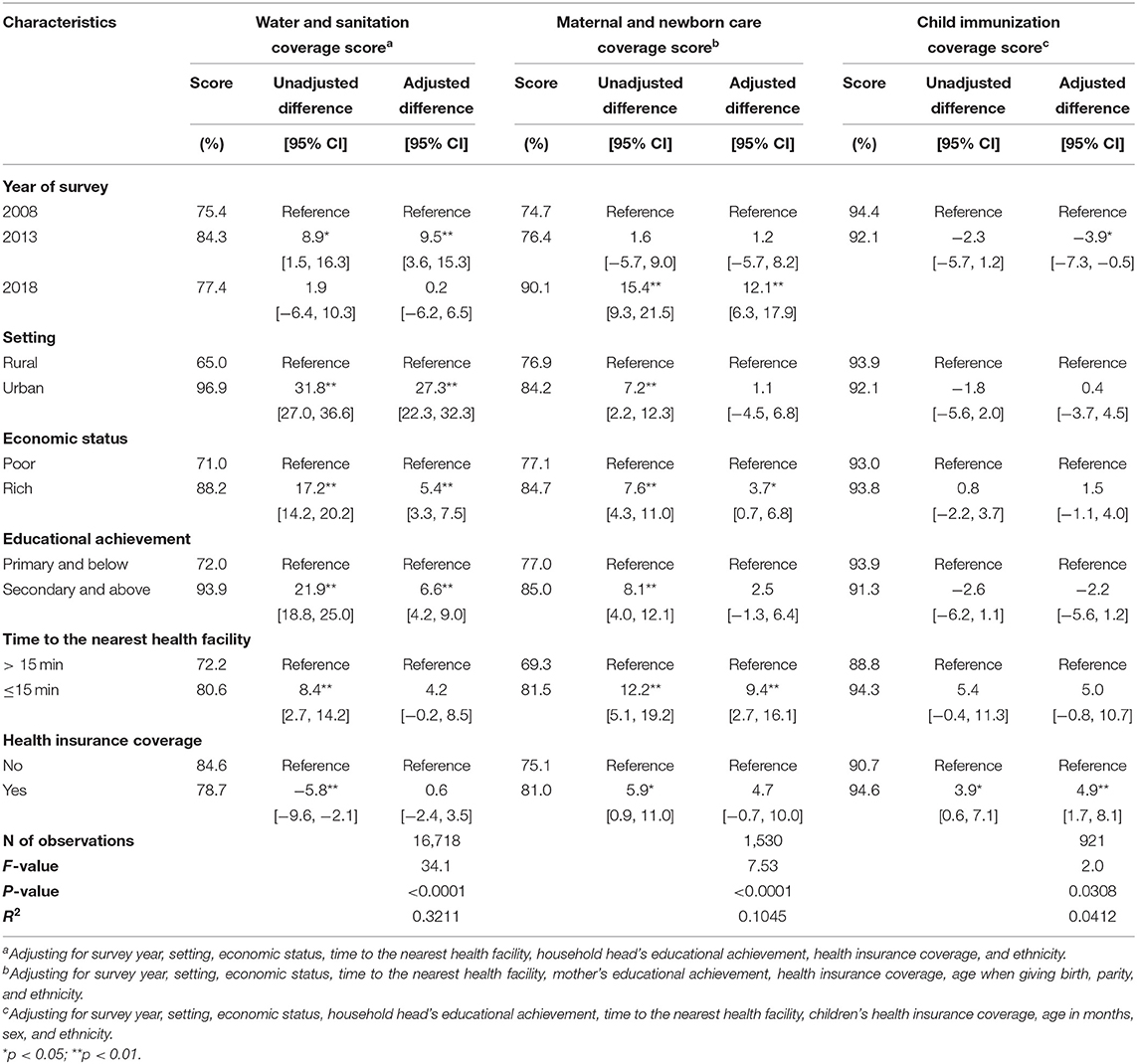
Table 2. Factors associated with the composite coverage scores for essential MNCH interventions in Jilin province, China (2008–2018).
The changing trends were particularly evident among those living in rural settings. When adjusting for other covariates, the water and sanitation coverage score increased by 14.1 percentage points (95% CI 4.7–23.6%) from 2008 to 2013 but returned to the 2008 level in 2018, which made the rural–urban gap first shrink and then expand. For maternal and newborn care coverage, a significant rising trend occurred (adjusted differences 12.1%, 95% CI 6.3–17.9% comparing 2008 and 2018). For figure on the trends, please see Appendix 5.
Discussion
Using provincially representative survey data, we reported the coverage and equity of 18 interventions along the MNCH care continuum in Jilin province, China, during 2008 and 2018. Given its size and socioeconomic development level, Jilin province accommodates the population of a middle-level country globally and can be considered a typical region in China. We found high coverage of hospital-based interventions in this region. Some interventions, such as cesarean section, presented alarmingly high rates—among the highest rates worldwide—indicating over-coverage (33). However, substantial unmet needs exist in many community-based interventions that are delivered in primary care settings or rely on wider systems, such as antenatal and postnatal care, child growth monitoring, child feeding, and water and sanitation. Such inequity mainly presented as urban–rural disparities rather than household- or individual-level inequalities across people's income and educational status, especially in the water and sanitation domain and quality coverage of maternal and newborn care interventions.
Compared to other LMICs, the main difference is that, in other resource-insufficient countries, improvements have mainly involved scaling up community-based MNCH interventions although substantial gaps persist in intrapartum care and other hospital-based interventions (1, 7, 34–37). The findings demonstrate China's health system development process and hospital-based strategy to improve maternal and newborn care in recent decades.
In the 1960s−1980s, China built a community-oriented and integrated health system that focused on effectively linked three-tier systems, barefoot doctors, and community-based financing mechanisms. The system provides information for many LIMCs due to its ability to provide essential health services with high cost-effectiveness given resource constraints (19). However, China moved away from this model after the economic reform in the 1980s. Decentralization provided more autonomy as well as profit-making pressure on hospitals. Users were given freedom to choose public hospitals as their first contact, and resources were redistributed among different health service providers. Great achievements were made in constructing many modern advanced hospitals. However, there are two concerns about such a paradigm shift. First, boosted by an increasingly common belief in science and technology and distorted by incentives to maximize revenue, Chinese hospitals were considered to be part of a “medical arms race” that focused on developing high-technology and costly examinations and procedures, which might usher in the overuse of curative care and uncontrolled rising medical expenditures (18, 20, 38). Second, the promotion of market-oriented financing mechanisms changed providers' relationships from collaborative to competitive (39, 40). In the competition with advanced and profitable hospital care, community-based care was gradually marginalized (41). Consequently, the primary care system that used to provide collaborative and continuing care was dismantled in China in the 1990s (18, 19, 27).
We found that hospital-based interventions, such as hospital delivery and antenatal B-ultrasound examination, were almost universal in Jilin province, China. On the one hand, the cesarean section rate was as high as 51.8% in 2008 and increased to 64.9% in 2013, similar to the rates reported from the government's annual report data (42). In our study, most mothers were primiparas and gave birth at <30 years of age. Considering such a high level of prevalence and low risk, the high cesarean section rate could certainly be seen as an indication of over-medicalization. By contrast, most community-based interventions that are delivered in primary care settings, such as antenatal and postpartum care as well as child growth monitoring, presented low coverage and revealed unmet needs. For example, the proportions of mothers who received at least one session of postnatal care were lower than 65%, and coverage of at least four sessions of antenatal care was no higher than 80%. Unlike hospital delivery, these services warrant lower requirements for equipment and personnel skills and could be effectively delivered by township and village health providers.
Especially for water and sanitation and the quality coverage of maternal and newborn care interventions, urban–rural inequalities were more profound than individual-level disparities across ethnicity, education, income, and health insurance status. These patterns are different from other Countdown countries, where social status, mother's educational achievement, and families' ability to pay are considered to be main barriers in accessing quality MNCH care (43–47). Jilin province has moderate economic development and ranked 11th out of 31 provinces in China in terms of rural household per capita income (48). In our study, most of the mothers achieved primary education and above, which means they have the ability to acquire basic health information and make health decisions. These findings suggest that, once basic wealth and education are guaranteed, individual-level social determinants may be less important barriers that undermine access to essential MNCH services, and regional-level system endowment or deficiency might have a more considerable impact.
Encouragingly, coverage of maternal and newborn care interventions was improved and the inequity shrank substantially during 2008–2018, such as the four types of government-funded antenatal care services (from 50.4% in 2008 to 82.2% in 2013) and at least five antenatal care sessions (from 61.6% in 2008 to 85.4% in 2018). These interventions were included in China's National Essential Public Health Services program initiated in 2009. In the program, the government offers free access to antenatal and postnatal care, growth monitoring, and maternal health education as well as free vaccinations for BCG, measles, DPT, hepatitis B, and polio (24–26). Special funds are allocated to purchase these services from community health care providers on a per capita basis. The government also made additional efforts to improve rural infrastructures. In contrast, water and sanitation involved more multi-sector coordination interventions and had no specific subsidy, which made their improvement more difficult (49, 50). However, even in the program, improvements were not observed in all interventions, and sluggish coverage was observed for interventions such as at least one session of growth monitoring and child feeding. Taken together, these results suggest that China's recent efforts to revitalize its primary health care system are partly effective in reducing health inequity. In fact, although the reform made efforts to strengthen the primary care system, hospitals still perform nearly 50% of outpatient services (48).
The data and analysis in this study warrant scrutiny. First, the Jilin province NHSS is provincially representative. Given the size, socioeconomic situation, and health system development in Jilin province, the findings can somewhat depict the situation in China. However, China is very large, and the situation in the western part is quite different from other regions (12). Second, we built on the Countdown approach but made some changes due to the data and China's specific contexts. For example, we analyzed hospital delivery instead of skilled birth attendants and postnatal care within 42 days instead of 2 days. Unlike many international health surveys, such as the Demographic and Health Surveys (DHSs), which only surveyed children aged 12–23 months for vaccination coverage, children 12–59 months were used to define vaccination coverage in this analysis to maximize the sample size. We performed a sensitivity analysis and found no changes for the findings (Appendix 6). Furthermore, we added some interventions that were not included in the Countdown, such as at least eight antenatal care sessions, four types of government-funded antenatal services, BCG vaccination, hepatitis B vaccination (three doses), polio vaccination (three doses), and growth monitoring (≥1 check). These indicators are included in either the WHO 2016 recommendations on quality antenatal care services or China's National Essential Public Health Services program. Third, China's NHSS provided very limited information in performing the same principal component analysis as the DHS (51). Thus, we used household annual income per capita instead of the wealth index as used in the Countdown for equity analysis. Fourth, recall bias may occur in the household surveys, but we believe the coverage and equity of interventions were still comparable among different years since the same survey method was used.
Other LIMCs could draw lessons from China. The obstetrician-led MNCH care strategy may come at the cost of over-medicalization and health inequity. Taking Jilin province as an example, we also find that recent efforts in China to revitalize primary health care exhibit the potential for change. An integrated system that links families, communities, and all levels of health care organizations seems to be the most effective and efficient model to offer continuing MNCH care.
Data Availability Statement
The data analyzed in this study was obtained from the Jilin Health Information and Statistics Center. No individual private information could be released to the public domain. Requests to access these datasets should be directed to Yaoguang Zhang, emhhbmd5Z0BuaGZwYy5nb3YuY24=.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
XF conceived the study. YW did the analysis and made the first draft under XF's supervision. RL helped to refine the report and XF finalized the report. All authors contributed to critical interpretation of the results and development of the report, and approved the final version.
Funding
The research was funded by Newton Advanced Fellowship Program (grant ref No. 71761130083) and China National Natural Science Foundation Excellent Young Scientist Program (grant ref No. 71422009).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00212/full#supplementary-material
References
1. Countdown Coverage Writing Group, Countdown to Core Group, Bryce J, Daelmans B, Dwivedi A, Fauveau V, et al. Countdown to 2015 for maternal, newborn, and child survival: the 2008 report on tracking coverage of interventions. Lancet. (2008) 371:1247–58. doi: 10.1016/S0140-6736(08)60559-0
2. Lim SS, Allen K, Bhutta ZA, Dandona L, Forouzanfar MH, Fullman N, et al. Measuring the health-related sustainable development goals in 188 countries: a baseline analysis from the global burden of disease study 2015. Lancet. (2016) 388:1813–50. doi: 10.1016/S0140-6736(16)31467-2
3. World Health Organization. World Health Report 2005: Make Every Mother and Child Count. Geneva: World Health Organization (2005). doi: 10.30875/8466f5ca-en
4. Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. (2007) 370:1358–69. doi: 10.1016/S0140-6736(07)61578-5
5. Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, et al. Global health 2035: a world converging within a generation. Lancet. (2013) 382:1898–955. doi: 10.1016/S0140-6736(13)62105-4
6. Bryce J, Terreri N, Victora CG, Mason E, Daelmans B, Bhutta ZA, et al. Countdown to 2015: tracking intervention coverage for child survival. Lancet. (2006) 368:1067–76. doi: 10.1016/S0140-6736(06)69339-2
7. Victora CG, Requejo JH, Barros AJ, Berman P, Bhutta Z, Boerma T, et al. Countdown to 2015: a decade of tracking progress for maternal, newborn, and child survival. Lancet. (2016) 387:2049–59. doi: 10.1016/S0140-6736(15)00519-X
8. Countdown to 2015. A Decade of Tracking Progress for Maternal, Newborn and Child Survival: The 2015 Report. Geneva: United Nations International Children's Emergency Fund and World Health Organization (2015). Available online at: http://countdown2030.org/documents/2015Report/Countdown_to_2015_final_report.pdf (accessed May 25, 2017).
9. Hogan DR, Stevens GA, Hosseinpoor AR, Boerma T. Monitoring universal health coverage within the sustainable development goals: development and baseline data for an index of essential health services. Lancet Glob Health. (2017) 6:E152–68. doi: 10.1016/S2214-109X(17)30472-2
10. Feng XL, Guo S, Hipgrave D, Zhu J, Zhang L, Song L, et al. China's facility-based birth strategy and neonatal mortality: a population-based epidemiological study. Lancet. (2011) 378:1493–500. doi: 10.1016/S0140-6736(11)61096-9
11. He C, Liu L, Chu Y, Perin J, Dai L, Li X, et al. National and subnational all-cause and cause-specific child mortality in China, 1996-2015: a systematic analysis with implications for the sustainable development goals. Lancet Glob Health. (2017) 5:e186–97. doi: 10.1016/S2214-109X(16)30334-5
12. Gao Y, Zhou H, Singh N, Powell-Jackson T, Nash S, Yang M, et al. Progress and challenges in maternal health in western China: a countdown to 2015 national case study. Lancet Glob Health. (2017) 5:e523–36. doi: 10.1016/S2214-109X(17)30100-6
13. Harris A, Belton S, Barclay L, Fenwick J. Midwives in China: 'jie sheng po' to 'zhu chan shi'. Midwifery. (2009) 25:203–12. doi: 10.1016/j.midw.2007.01.015
14. Cheung NF. Chinese midwifery: the history and modernity. Midwifery. (2009) 25:228–41. doi: 10.1016/j.midw.2007.03.001
15. China's National Health and Family Planning Commission. Standards for Maternal and Newborn Care. Beijing: China's National Health and Family Planning Commission (2011). Available online at: http://www.nhc.gov.cn/zwgkzt/wsbysj/201107/52320.shtml (accessed May 25, 2017).
16. Feng XL, Xu L, Guo Y, Ronsmans C. Socioeconomic inequalities in hospital births in China between 1988 and 2008. Bull World Health Organ. (2011) 89:432–41. doi: 10.2471/BLT.10.085274
17. Feng XL, Zhu J, Zhang L, Song D, Hipgrave S, Guo C, et al. Socio-economic disparities in maternal mortality in China between 1996 and 2006. BJOG. (2010) 117:1527–36. doi: 10.1111/j.1471-0528.2010.02707.x
18. Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. (2008) 372:1493–501. doi: 10.1016/S0140-6736(08)61364-1
19. Feng XL, Martinez-Alvarez M, Zhong J, Xu J, Yuan B, Meng Q, et al. Extending access to essential services against constraints: the three-tier health service delivery system in rural China (1949-1980). Int J Equity Health. (2017) 16:49. doi: 10.1186/s12939-017-0541-y
20. Hu S, Tang S, Liu Y, Zhao Y, Escobar ML, de Ferranti D. Reform of how health care is paid for in China: challenges and opportunities. Lancet. (2008) 372:1846–53. doi: 10.1016/S0140-6736(08)61368-9
21. Chen Z. Launch of the health-care reform plan in China. Lancet. (2009) 373:1322–24. doi: 10.1016/S0140-6736(09)60753-4
22. Yip WC, Hsiao WC, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China's huge and complex health-care reforms. Lancet. (2012) 379:833–42. doi: 10.1016/S0140-6736(11)61880-1
23. Li X, Lu J, Hu S, Cheng KK, De Maeseneer J, Meng Q, et al. The primary health-care system in China. Lancet. (2017) 390:2584–94. doi: 10.1016/S0140-6736(17)33109-4
24. China's National Health and Family Planning Commission. National Essential Public Health Services Standards. (2009) Beijing: China's National Health and Family Planning Commission. Available online at: www.nhc.gov.cn/zwgk/wtwj/201304/b175eb09dfd240f6bae36d2fb67c8619.shtml (accessed May 25, 2017).
25. China's National Health and Family Planning Commission. National Essential Public Health Services Standards. (2011) Beijing: China's National Health and Family Planning Commission. Available online at: http://www.nhc.gov.cn/jws/s3577/201105/51780.shtml (accessed May 25, 2017).
26. China's National Health and Family Planning Commission. National Essential Public Health Services Standards. (2017) Beijing: China's National Health and Family Planning Commission. Available online at: http://www.nhc.gov.cn/jws/s3578/201703/d20c37e23e1f4c7db7b8e25f34473e1b.shtml (accessed May 25, 2017).
27. Yip W, Hsiao W. Harnessing the privatisation of China's fragmented health-care delivery. Lancet. (2014) 384:805–18. doi: 10.1016/S0140-6736(14)61120-X
28. Niu JD, Zhang QJ, Feng XL, Wang QY, Wang Y, He YH, et al. An Analysis Report of the Fifth Health Services Survey in Jilin Province. Beijing: Peking University Medical Press (2016).
29. World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization (2016). Available online at: http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf (accessed May 25, 2017).
30. Arsenault C, Jordan K, Lee D, Dinsa GD, Manzi F, Marchant T, et al. Equity in antenatal care quality: an analysis of 91 national household surveys. Lancet Global Health. (2018) 6:e1186–95. doi: 10.1016/S2214-109X(18)30389-9
31. Boerma JT, Bryce J, Kinfu Y, Axelson H, Victora CG. Mind the gap: equity and trends in coverage of maternal, newborn, and child health services in 54 Countdown countries. Lancet. (2008) 371:1259–67. doi: 10.1016/S0140-6736(08)60560-7
32. Barros AJ, Ronsmans C, Axelson H, Loaiza E, Bertoldi AD, Franca GVA, et al. Equity in maternal, newborn, and child health interventions in countdown to 2015: a retrospective review of survey data from 54 countries. Lancet. (2012) 379:1225–33. doi: 10.1016/S0140-6736(12)60113-5
33. Vogel JP, Betran AP, Vindevoghel N, Souza JP, Torloni MR, Zhang J, et al. Use of the robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Health. (2015) 3:e260–70. doi: 10.1016/S2214-109X(15)70094-X
34. Bhutta ZA, Chopra M, Axelson H, Berman P, Boerma T, Bryce J, et al. Countdown to 2015 decade report (2000-10): taking stock of maternal, newborn, and child survival. Lancet. (2010) 375:2032–44. doi: 10.1016/S0140-6736(10)60678-2
35. Kumar C, Singh PK, Rai RK. Coverage gap in maternal and child health services in India: assessing trends and regional deprivation during 1992-2006. J Public Health UK. (2013) 35:598–606. doi: 10.1093/pubmed/fds108
36. Mangham-Jefferies L, Pitt C, Cousens S, Mills A, Schellenberg J. Cost-effectiveness of strategies to improve the utilization and provision of maternal and newborn health care in low-income and lower-middle-income countries: a systematic review. BMC Pregnancy Childbirth. (2014) 14:243. doi: 10.1186/1471-2393-14-243
37. Requejo JH, Bryce J, Barros AJ, Berman P, Bhutta Z, Chopra M, et al. Countdown to 2015 and beyond: fulfilling the health agenda for women and children. Lancet. (2015) 385:466–76. doi: 10.1016/S0140-6736(14)60925-9
38. Yip WC, Hsiao W, Meng Q, Chen W, Sun X. Realignment of incentives for health-care providers in China. Lancet. (2010) 375:1120–30. doi: 10.1016/S0140-6736(10)60063-3
39. Eggleston K, Ling L, Qingyue M, Lindelow M, Wagstaff A. Health service delivery in China: a literature review. Health Econ. (2008) 17:149–65. doi: 10.1002/hec.1306
40. Yip W, Hsiao WC. The Chinese health system at a crossroads. Health Aff . (2008) 27:460–68. doi: 10.1377/hlthaff.27.2.460
41. Bhattacharyya O, Delu Y, Wong ST, Bowen C. Evolution of primary care in China 1997-2009. Health Policy. (2011) 100:174–80. doi: 10.1016/j.healthpol.2010.11.005
42. Li HT, Luo S, Trasande L, Hellerstein S, Kang C, Li JX, et al. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. JAMA. (2017) 317:69–76. doi: 10.1001/jama.2016.18663
43. LeVine RA, LeVine SE, Rowe ML, Schnell-Anzola B. Maternal literacy and health behavior: a nepalese case study. Soc Sci Med. (2004) 58:863–77. doi: 10.1016/S0277-9536(03)00261-2
44. Gabrysch S, Campbell OM. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. (2009) 9:34. doi: 10.1186/1471-2393-9-34
45. Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. (2007) 85:812–9. doi: 10.2471/BLT.06.035659
46. Anwar I, Nababan HY, Mostari S, Rahman A, Khan JAM. Trends and inequities in use of maternal health care services in Bangladesh, 1991-2011. PLoS ONE. (2015) 10:e120309. doi: 10.1371/journal.pone.0120309
47. Langlois EV, Miszkurka M, Zunzunegui MV, Ghaffar A, Ziegler D, Karp I. Inequities in postnatal care in low- and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ. (2015) 93:259–70. doi: 10.2471/BLT.14.140996
48. National Bureau of Statistics of the People's Republic of China. China Statistical Yearbook. (2018) Beijing: National Bureau of Statistics of the People's Republic of China. Available online at: http://www.stats.gov.cn/tjsj/ndsj/2018/indexch.htm (accessed October 25, 2019).
49. Bei E, Wu X, Qiu Y, Chen C, Zhang X. A tale of two water supplies in China: finding practical solutions to urban and rural water supply problems. Acc Chem Res. (2019) 52:867–75. doi: 10.1021/acs.accounts.8b00605
50. Cheng S, Li Z, Uddin SMN, Mang H-P, Zhou X, Zhang J, et al. Toilet revolution in China. J Environ Manage. (2018) 216:347–56. doi: 10.1016/j.jenvman.2017.09.043
51. Rutstein SO. The DHS Wealth Index: Approaches for Rural and Urban Areas. (2008) Available online at: http://dhsprogram.com/pubs/pdf/WP60/WP60.pdf (accessed May 27, 2017).
Keywords: China, maternal newborn and child health, primary care, health system, equity
Citation: Wang Y, Liao R and Feng XL (2020) Equity in Essential Maternal, Newborn, and Child Health Interventions in Northeastern China, 2008 to 2018. Front. Public Health 8:212. doi: 10.3389/fpubh.2020.00212
Received: 06 November 2019; Accepted: 07 May 2020;
Published: 02 July 2020.
Edited by:
Edward I. Broughton, Bristol Myers Squibb, United StatesReviewed by:
Mindaugas Stankunas, Lithuanian University of Health Sciences, LithuaniaLaura Cacciani, Regional Health Service of Lazio, Italy
Copyright © 2020 Wang, Liao and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xing Lin Feng, ZnhsQGJqbXUuZWR1LmNu
 Ying Wang
Ying Wang Ran Liao
Ran Liao Xing Lin Feng
Xing Lin Feng