- 1Department of Tropical Medicine and Global Health, School of Tropical Medicine and Global Health, Nagasaki University, Nagasaki, Japan
- 2Sustained Health Initiatives of the Philippines (SHIP), Mandaluyong, Philippines
- 3Faculty of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 4Institute of Molecular Biology and Biotechnology, National Institutes of Health, University of the Philippines, Manila, Philippines
- 5Institute of Tropical Medicine, (NEKKEN), Nagasaki University, Nagasaki, Japan
Introduction: Depression is the most frequently observed psychiatric disorder among HIV patients. The effect of depression on adherence among men who have sex with men (MSM) HIV patients has not been well studied in the Philippines. Depression is commonly undiagnosed and consequently untreated, which leads to a negative influence on antiretroviral therapy (ART) adherence. Other risk factors such as HIV-related stigma, self-body image satisfaction, and nutritional status are recognized as potential barriers to access HIV prevention and treatment services issues and poor adherence.
Methods: Hospital anxiety and depression scale (HADS) was used to screen depressive symptoms during scheduled clinic visits. ART adherence was self-reported using a visual analog scale questionnaire covering the last 30 days. Structured questionnaires were used for measuring risk factors and socio-demographic data. Anthropometry was conducted and body composition was assessed using bioelectrical impedance analysis.
Results: One-hundred and ninety-three participants were recruited from the SHIP clinic between 7th March and 30th September 2018, of whom, 42 (21.8%) screened positive for depression (HADS score ≥ 8) and 24 (12.4%) were non-adherent to ART (<95% of medication taken as prescribed). The most common reported reason for non-adherence was simply forgotten (18 out of 42, 42.9%). Increasing depressive symptoms were associated with non-adherence [crude odds ratio (OR) = 1.13; 95% CI: 1.02–1.26]. Social family support (SFS) and body image (BI) scores were also associated with non-adherence, but were not statistically significant in multivariable models. Factors significantly associated with depressive symptoms (but not non-adherence) included the following: using intravenous drugs, being in a relationship, anxiety, self-esteem, and stigma scores.
Conclusions: Increased depression symptoms, low social family support, and body image dissatisfaction may be interconnected risk factors for ART non-adherence among Filipino MSM HIV patients. Comprehensive mental health services beyond regular post-HIV testing counseling may increase adherence to ART and improve HIV treatment outcomes. Further prospective studies are needed to address the causal/reverse causal pathway between depression and non-adherence.
Introduction
The Filipino population of men who have sex with men (MSM) is estimated to be between 200,000 and 670,000, representing 1–3% of the total adult male population (1). The group most impacted by HIV in the Philippines is MSM, representing 85% of new sexually-acquired infections since 2011. The median age of new cases is 22 years old, and more than 60% of people living with HIV in the Philippines are under 25 (2).
The efficacy of antiretroviral therapy (ART) depends on compliance with daily medication regimens. Adherence is a cornerstone to suppress viral replication and improve immunological and clinical outcomes; decrease the risk of developing ART drug resistance; and reduce the risk of transmitting HIV (3). A recent surveillance study in the Philippines showed that 10.3% of patients experienced treatment failure on their first-line regimens, possibly due to incomplete adherence to ART (4). Also, a regional cohort study TREAT-Asia (Therapeutic Research, Education, and AIDS Training in Asia) found that out of 1,316 participants, 26% self-reported suboptimal adherence levels (<95%) during their first 6 months of treatment (5). More generally, one out of four ART users may fail to adhere to medication for reasons which can be categorized as relating to patient and family, medication, health delivery system, caregiver, and social/environmental factors (6).
People living with HIV may face many challenges including depression, low social and family support (SFS), widespread stigma, changes in nutritional status, and barriers to accessing mental and psychological care which may have a negative effect on ART adherence level (7). People living with HIV are more likely to be depressed compared with those who are HIV negative (8), and MSM are three times more at risk of depression compared with the general population of men (9). Depression has a severe negative impact on the quality of life (QOL), which can affect patient behaviors including medication adherence (10). Depression in people living with HIV could be triggered by stress, stigma, difficult life events, and side effects of medications (11, 12). A crosssectional study in Malawi reported depression to be associated with a 1.55 fold greater risk of being non-adherent to ART (13). A study in Vietnam found that several clinical and social factors were associated with depression among PLHIV, and these factors included having a lower number of CD4 cells at the start of ART, receiving ART in the clinic without HIV counseling and testing (HCT) services, having a physical health problem, and experiencing discrimination (14).
Stigma is another barrier for HIV patients. UNAIDS reported in October 2017 that across 19 countries, one in five persons living with HIV avoided going to health centers because they feared stigma related to their HIV status (13). PLHIV are often non-adherent to their ART to avoid being seen taking pills and avoid being perceived as HIV-positive (15). People living with HIV may experience social isolation, lose employment, and family and friends as major sources of support (3). Previous studies in Thailand, France, and South Africa have found a positive association between SFS and ART adherence (15–17).
Persons living with HIV are highly susceptible to malnutrition due to inadequate dietary intake, appetite loss, nutrition losses, metabolic changes, and increased requirements for both macro and micronutrients (18). Those who are undernourished [defined as body mass index (BMI) < 18.5 kg/m] are 10 times more likely to be non-adherent to ART (19). In a prospective cohort study in Haiti, receiving food assistance and subsequent improved nutritional status was associated with improved adherence to ART (18). Up to 60% of MSM HIV infected individuals experience moderate to severe changes in body fat composition (20, 21). It has been previously reported that MSM living with HIV are more likely to experience high levels of body dissatisfaction compared with heterosexual persons living with HIV (22).
A lack of data exists on depression in Filipino MSM persons living with HIV. The primary objective of this study was to assess the prevalence of depression and its association with ART adherence and with other risk factors, such as stigma, low self-esteem, alcohol abuse, body image, nutritional status, and low social and family support among Filipino MSM. We hypothesized that these risk factors would be correlated and associated with both depression and adherence.
Methods
Study Design
This was a nested crosssectional study within an ongoing single-arm, mobile health (mHealth) intervention study which used a self-reported questionnaire for adherence to assess the impact of the intervention on ART adherence.
Study Population
The inclusion criteria for participation in the nested study were as follows: (1) adult PLHIV (age 18 years); (2) male subjects who self-defined as having sex with males; (3) taking ART in the sustained health initiatives of the Philippines (SHIP) clinic in Manila; (4) enrolled into an existing, single-arm trial study: the Connect for Life Mobile Phone Adherence Demonstration Project (CFL) at the SHIP Clinic; (5) able to understand written and spoken English. The exclusion criteria were the following: (1) receiving primary HIV care at a facility other than SHIP; (2) late-stage HIV and/or hospitalized; (3) previous psychiatric disease before diagnosis of HIV or any significant clinical neurological disorder such as stroke or cerebral palsy.
Study Site
Sustained Health Initiatives of the Philippines Clinic is a low-cost, private facility in Metro Manila, a city of just under 13 million people in the predominantly Catholic country of the Philippines. SHIP Clinic provides HIV primary care and wrap-around services to approximately 900 patients as of April 2021. Between 2012 and 2018, SHIP was a satellite partner clinic of the STI/AIDS Guidance Intervention and Prevention Unit at the Philippine General Hospital (PGH-SAGIP), the largest hospital in the country. Approximately 98% of clients of SHIP are MSM, with an average age of 30 years at initial consultation. Most are employed full- or part-time. The patients come from all regions of Metro Manila and some live outside of Metro Manila in other provinces.
Study Enrolment Procedures
Participants in the CFL study were approached to participate in this nested study by a member of the study team during a routine clinic visit and written informed consent was obtained.
Data Collection
Data were collected using a self-reported questionnaire, including standardized data collection tools as described below, designed, and implemented through Open Data Kit (ODK) using an electronic tablet during a routine clinic visit. Trained clinical research assistants were available to answer any queries from participants while completing the questionnaire.
Antiretroviral therapy adherence data was extracted from CFL study records in which adherence was assessed using a self-administered “Visual Analog scale” question of the percentage of doses taken in the previous 30 days at four-time points, namely, baseline [Week 0 (within 60 days from Screening)] and 12, 24, and 48 weeks. Participants were defined as adherent at each time point if the participant reported 95% of medications taken in the prior 30 days.
CD4 data was extracted from participant records. In the study site, ART initiation was recommended for all patients with an AIDS-defining illness (Treat all policy), or when CD4 count is below 500. CD4 count is performed every 6 months and the viral load test is performed annually.
Depression/anxiety was assessed using the hospital anxiety and depression scale (HADS), a self-administrated questionnaire consisting of 14-items, seven questions assessing depressive symptoms and seven assessing anxiety. Each item contains four response options (from 0 to 3). The presence of anxiety or depressive symptoms was defined as a score of HADS ≥ 8 for each (23–25). The HADS questionnaire had been validated in several languages and countries, including the Philippines (26), and in general practice and community settings (26, 27).
Alcohol abuse was measured using the alcohol use disorder identification test (AUDIT) and is recommended for use in the Philippines (28). The AUDIT is a 10-item, self-rating questionnaire that assesses hazardous drinking, dependence symptoms, and harmful alcohol use (29). The presence of alcohol-related social problems and medical complications was defined as an AUDIT score ≥ 8 (29, 30).
Social and family support was measured using the multidimensional scale of perceived social support (MSPSS) which measures the extent to which an individual perceives social support from three different sides: family, friends, and a significant other (31, 32). The scale is 12 items, with each item using a 7-point Likert scale (32). MSPSS has been validated for use in lower-middle-income countries (33–36). High levels of perceived support were defined as total score 69–84; moderate 49–68; and low 12–48 (32, 36).
Stigma was measured using the Berger scale, designed to determine stigma in HIV patients. It includes 40 items rated on a 5-point scale from (37) assessing personalized stigma, disclosure concerns, negative self-image, and concern with the public attitude. Higher scores indicate more stigma (37, 38).
Self-esteem was measured using Rosenberg self-esteem scale (RSES). It is a validated tool used to assess positive and negative feelings of a patient to his own self (39, 40). It consists of 10 questions with a 4-point Likert scale ranging from very negative (1) to very positive (4) (41, 42). Higher scores indicate higher self-esteem.
Self-body image was measured by the body image quality of life inventory (BIQLI), developed to monitor both positive and negative effects of body image on a the psychosocial QOL of a patient, which includes beliefs and emotions (43). This scale has 19 items, each using a 5-point Likert scale. BIQLI assesses the specific domains of day-to-day emotions, self-esteem, sexuality, social interest/avoidance, interpersonal relations, eating and exercise, grooming habits, and general life satisfaction (44, 45). Higher scores indicate high satisfaction with body image (44).
Anthropometry was conducted by trained clinical research assistants at the time of the interview. Height was measured using a stadiometer (model Seca 213) to the nearest 0.1 cm. Mid upper arm circumference (MUAC) was measured using a non-elastic plastic tape at the midway between the olecranon and acromion process on the upper left arm. Body composition (body fat%, lean body mass, and visceral fat) was measured using bioelectrical impedance analysis (BIA) (model Tanita MC-780MA).
Ethics Statement
The primary intervention study (CFL) was approved by the University of the Philippines Manila (reference number UPMREB 2016-265-01) and London School of Hygiene and Tropical Medicine (reference number 11631). This nested crosssectional study was approved by Nagasaki University, School of Tropical Medicine, and Global Health (reference number 42) and the University of the Philippines Manila (reference number UPMREB 2017-453-01).
Data Analysis
Adherence data were used from the same time point as the current data collection. Data analysis was conducted using Stata 14.0. The proportion of study participants with depression or anxiety (HADS scores ≥ 8) are reported as percentages with corresponding 95% confidence intervals. Logistic regression was used to investigate associations between depressive or anxiety symptoms and being adherent/non-adherent as a binary outcome. A p-value of 0.05 was considered as statistically significant. Multivariable models were developed using a forward stepwise approach from factors associated in univariable analyses significant at p < 0.05 and models compared using likelihood ratio (LR) tests.
Results
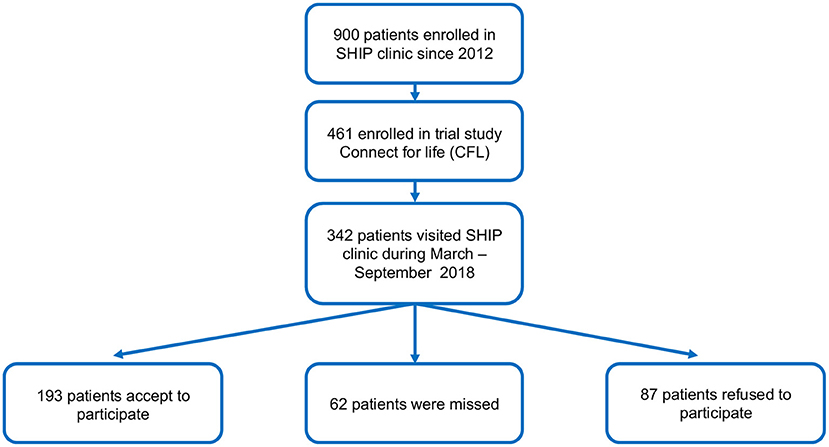
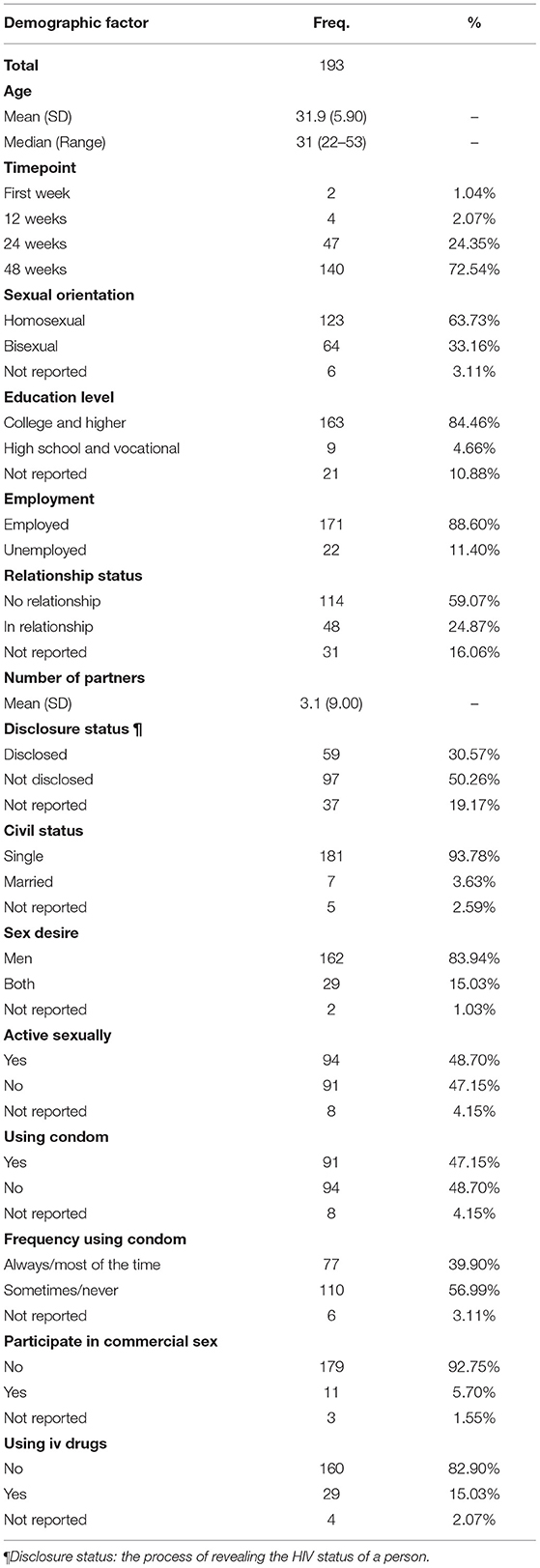
Figure 1 shows the flow of persons potentially eligible and those enrolled in the current study. Out of 342 participants in the CFL study with routine clinic visits during the nested study enrolment period, 193 Filipino MSM were enrolled between 7th March and 30th September 2018 (Figure 1). The characteristics of our study participants are shown in Table 1. The mean age was 31.95 years (range 22–53, SD 5.90). Only 48 (24.9%) reported being in a relationship. Most participants, 163 (84.5%) were highly educated at college or higher level. Fifty-nine (30.6%) had disclosed their HIV status and 91 (47.15%) reported using condoms, with consistent condom use in 77 participants (39.0%). The proportion reporting ever using IV drugs was 29 (15.0%).
The prevalence of non-adherence was 12.4% (24/193) with 125 (65%) of those adherent reporting 100% adherence in the previous 30 days. The prevalence of depression was 21.8% (42/193) and anxiety 37.3% (72/193) (Table 2). The prevalence of poor SFS, poor self-esteem, and potential alcohol misuse was 34.7, 46.1, and 15.0%, respectively (Table 2).
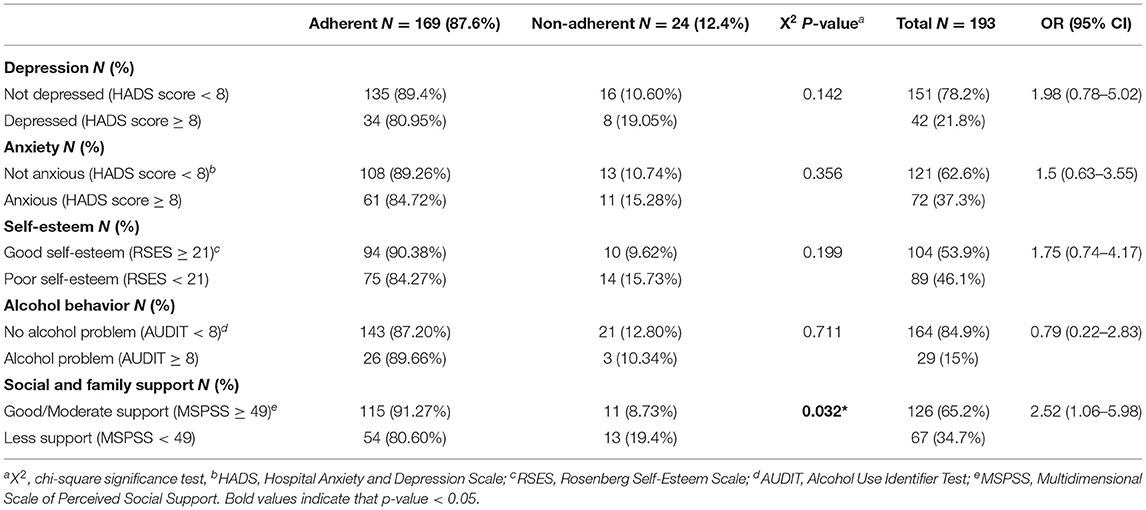
Table 2. Prevalence and associations between depression, anxiety, self-esteem alcohol misuse, and social family support and ART adherence.
No associations between age, timepoint, CD4 count, or demographic variables (as per those in Table 1) with adherence were observed (Supplementary Table 1).
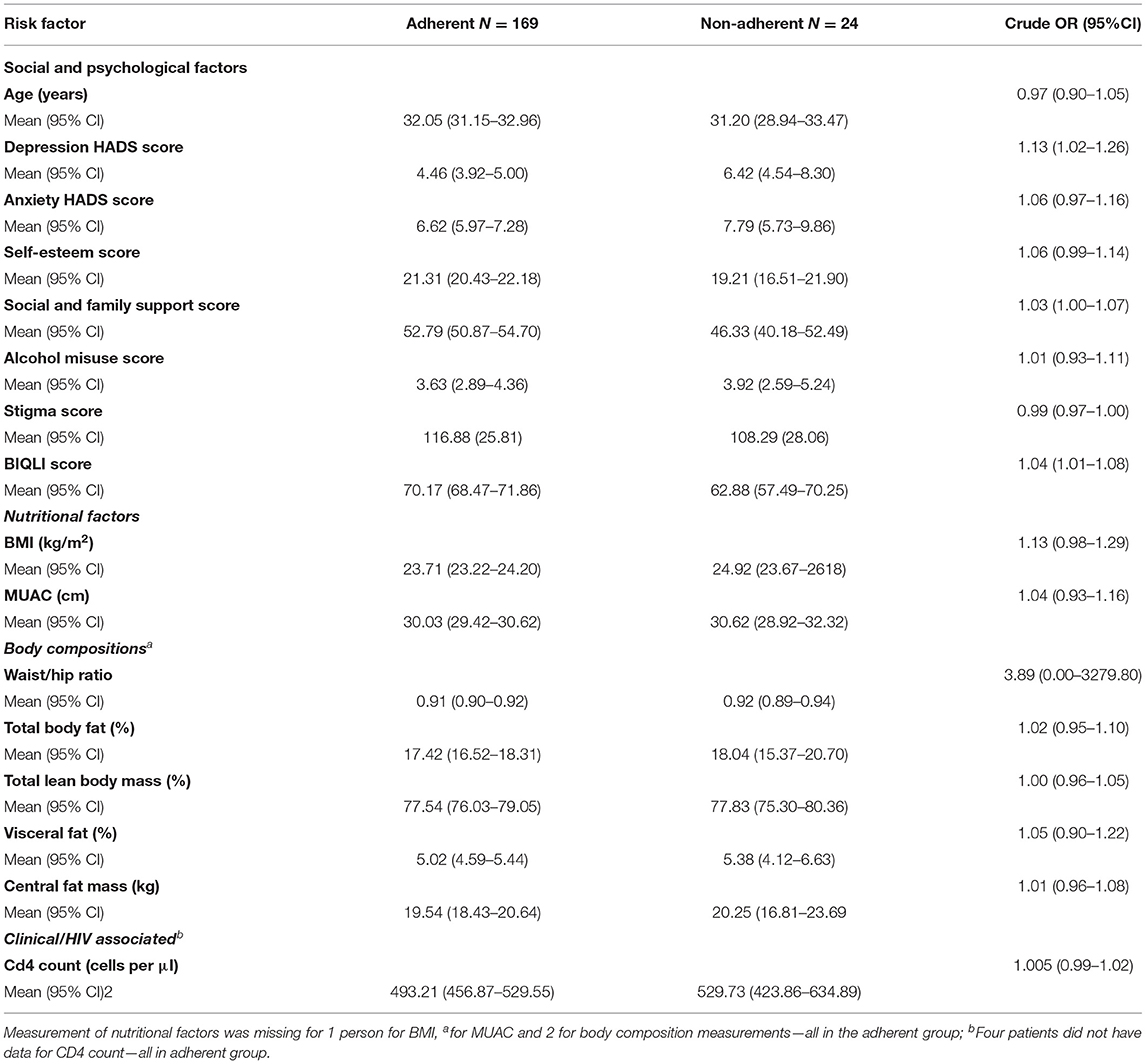
Effects of Psychological, Social, and Nutrition Factors on Non-adherence
For exposures with predefined cut-offs and analyzed as a binary exposure, only high/moderate SFS compared with low SFS was significantly associated with odds of non-adherence (OR = 2.52; 95% CI:1.06–5.98) (Table 2). Although there were more non-adherent participants amongst those who were depressed (19.05%) compared with non-depressed (10.60%), this did not reach statistical significance (Table 2). When analyzed as continuous scores, there was good evidence of an association between increased depression symptom score and non-adherence (OR:1.13; 95% CI 1.02–1.26) as well as poorer self-body image score [OR: 1.04; 95% CI (1.01–1.08)] and decreased perceived SFS (OR = 1.03; 95% CI:1.00–1.07) (Table 3). While higher BMI had weak evidence of association (p = 0.0818) with non-adherence, there was no evidence for an association between nutritional status assessed by MUAC (p = 0.4935) or with measures of body composition (Table 3).
We then investigated if any of the assessed psychosocial and nutritional measures were also associated with depression and could therefore be possible confounders of the association between HADS score and non-adherence. Higher HADs score for anxiety symptoms, higher stigma, lower self-esteem, lower perceived social family support, and lower body image scores were all significantly associated with depression as well as lower measures of body fat (Supplementary Table 2).
When adjusting for SFS or body image, the association between depression score and non-adherence, was not statistically significant (Table 4). However, when comparing the crude and adjusted models, no evidence of statistical difference between the models was observed (LRT p-values 0.27 and 0.23; Table 4).
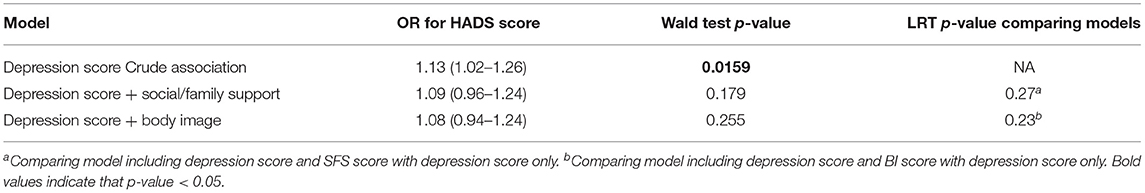
Table 4. Comparison of models of association between depression and non-adherence with and without adjustment for potential confounders.
Discussion
To our knowledge, this is the first study in Filipino MSM living with HIV to assess the prevalence of depressive symptoms with other risk factors, which was observed to be 21.8%, that has provided evidence to suggest an independent association between non-adherence to ART and depressive symptoms, perceived lower social family support, and poorer self-body image. The prevalence of depressive symptoms in this study was lower than that observed in a recent study of Chinese MSM living with HIV (36%, 95% CI 1.03–1.05) (46) which also used HADS. This difference may result from the higher educational status and lower prevalence of drug use in our population compared with the Chinese study population (46). In another study in Tanzania, the prevalence of depression among MSM persons living with HIV was also higher at 46.3% (47), possibly explained by the study in Tanzania using the Patient health questionnaire (PHQ) with cut-off point 4, which in a Swedish primary care population diagnosed 30% more as depressed compared with HADS (≥8) (48).
The prevalence of non-adherent persons in this study was 12.4%, lower than many other previous studies, but is perhaps not unsurprising in this study in which all the participants were recently enrolled into a mobile intervention study to improve ART adherence and were relatively young, urban, and highly educated. Furthermore, adherence may be higher in the newer easier to take ARV regimens, and or the finding is similar to a recent study in the urban Filipinos (4). In Cameroon, the prevalence of ART non-adherence in 300 HIV infected persons was 47.3% (49), defined using the Morisky scale ≥ 1. While in 418 Ethiopians with HIV, the prevalence of self-reported ART non-adherence (<95% of prescribed doses) over the previous 7 days was 53.4% (50). Differences may result from different methods of assessing and defining non-adherence, in study population characteristics (e.g., level of education; 69% in Ethiopia reported no education), and clinic settings, which may affect communication and relationships with health care providers (51, 52).
In this crosssectional study, we observed that an increase in 1 point of the HADS depression symptom score was associated with a 13% increase in the odds of reporting non-adherence, although the association with depression using HADS ≥ 8 did not reach statistical significance. This is consistent with previous findings in other populations. In a prospective study in 400 Ethiopians living with HIV, depression measured using a 13-item scale, widely used in the HIV/AIDS literature (≥10 defined as depressed), was significantly associated with non-adherence assessed using a self-reported scale over the last 7 days (OR 2.13; 95% CI: 1.18–3.81) (53). Two crosssectional studies, one in Thailand in 379 participants with depression assessed using the Beck depression inventory II (≥14 defined as depressed) was associated with non-adherence measured by self-reported scale over 30 days (<95%) (OR 4.68; 95% CI: 2.78–7.88) (54), and in Cameron in 300 participants, depression using the patient health question-9 (≥10 defined as depressed) was associated with adherence assessed by Morisky scale (≥1) (OR 5.04; CI: 2.84–8.97) (49).
Social family support and body image dissatisfaction were also strongly associated with non-adherence. This is consistent with the findings in the above Ethiopian study in which participants with higher perceived social family support were 1.82 times more likely to be adherent to ART (OR: 1.82, 95% CI:1.04–3.21) (53). Similar findings were observed In India, among 279, persons with high SFS score were 1.96 times more likely to be adherent (OR: 1.96; CI: 0.94–4.08) (55). Also, in a community-based study in 233 Nepalese living with HIV, negative emotional distance from family was associated with ART non-adherence (OR = 3.38, CI 1.28–8.91) (56). Therefore, social family support should be considered to be used to identify and prioritize those at high risk of non-adherence.
Body image dissatisfaction has been previously reported to have an adverse effect on ART adherence level (44). Generally, MSM, regardless of their HIV status, are more likely to have a high level of body dissatisfaction compared with heterosexuals (22, 57). Also, ART can cause body fat changes due to lipodystrophy (21, 44). Body image dissatisfaction may be an important indicator of non-adherence and cluster with other high-risk behaviors and psychosocial impacts that may benefit from interventions, including poor ART adherence (44, 45, 58), increased sexual behaviors that can transmit HIV (58), elevated levels of depressive symptoms (44, 58–60), increased methamphetamine use (61), and low self-esteem (62). In an Italian cohort study persons who had body tissue changes as a side effect of ART were almost five times more likely to be non-adherent (OR:4.67, 95% CI, 1.01–22.4) (63), and in an American cohort of 1,671 women self-perception of central fat gain was associated with a 1.5-fold increased odds of ART non-adherence (64). Finally, in a crosssectional study testing the impact of depression on the relationship between HAART adherence and body dissatisfaction in 124 HIV gay and heterosexual men, body dissatisfaction and depression independently predicted HAART non-adherence (44). Physical exercise might be a good intervention to improve depressive and anxiety symptoms and consequently adherence. A longitudinal study of three cohort studies done in the Netherlands among 7,076 participants showed that people who exercised were 1.47 times likely to recover from depression and anxiety (65).
There were several limitations of this study. Adherence was measured by self-report. Therefore, recall bias and social desirability bias may lead the participants to overreport their adherence level. Also, this crosssectional study was done within an intervention study with the aim of improving treatment adherence, and thus is not representative of those in standard care. Hence, level of adherence might be already enhanced compared with the general HIV population in the Philippines. The study population in SHIP clinic are also more highly educated than the general population in the Philippines and may not represent the general MSM population in the Philippines.
Conclusions
This study was the first to assess the association between depression or other risk factors and ART non-adherence among MSM persons living with HIV in the Philippines. The findings of this study documented that depression is a relatively common symptom among MSM persons with HIV. Comprehensive mental health services beyond post-HIV testing counseling may increase adherence to ART and improve HIV treatment outcome. This can be done through routine screening for depression and anxiety symptoms using standardized validated tools like HADS, which can enable early identification of patients with mild or moderate symptoms. Simple interventions such as peer support, supervised by clinic program staff may help prevent the progression of symptoms and the development of complications. Patients with severe symptoms should be ideally referred to psychiatrists (if available) for further evaluation and care. Previous studies have shown that peer support can improve depressive symptoms more than ordinary care, as PLWHIV may prefer to share their experiences with others who are facing similar obstacles rather than reporting their psychological difficulties to psychiatrists or doctors (66, 67). In the SHIP clinic, doctors have subsequently started to conduct routine depression/anxiety screening using this tool, and they report that it enables patients to express their feelings and concerns and helps develop a stronger relationship between doctors and patients. Further prospective studies are needed to address the causal/reverse causal pathway between depression and non-adherence.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The primary intervention study (CFL) was approved by the University of the Philippines Manila (reference number UPMREB 2016-265-01) London School of Hygiene and Tropical Medicine (reference number 11631). This nested cross-sectional study was approved by Nagasaki University, School of Tropical Medicine, and Global Health (reference number 42) The University of the Philippines Manila (reference number UPMREB 2017-453-01). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HE, SC, CO'C, and ES designed the study. HE and KL implemented the study and collected the data. CO'C shared the data from the main cohort study. HE and SC conducted the statistical analysis, sample size calculation and wrote the manuscript. All authors contributed to and approved the final version of the manuscript for submission.
Funding
This study was funded by Japan International Cooperation Agency through the ABE initiative scholarship to cover the salary of research nurses, ethical fees, and logistics.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are grateful to Kris Calica, Romil Jeffrey Juson, and Michelle Ann Savaadra who interviewed the participants. They are grateful to Dr. James Lewis, London School of Hygiene and Tropical Medicine for his support. Electronic data solutions were provided by LSHTM Open Research Kits (odk.lshtm.ac.uk). Funding for this work was supported by Japan International Cooperation Agency (JICA), whilst the Connect For Life (CFL) project at the SHIP clinic was supported by funding from Janssen Global Public Health.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.644438/full#supplementary-material
References
1. Farr AC, Wilson DP. An HIV epidemic is ready to emerge in the Philippines. J Int AIDS Soc. (2010) 13:1–8. doi: 10.1186/1758-2652-13-16
2. Department of Health in the Philippines (DOH). 2018 Integrated HIV Behavioral and Serologic Surveillance (IHBSS). (2018).
3. Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS ONE. (2014) 9:e88166. doi: 10.1371/journal.pone.0088166
4. Salvana EMT, Samonte GMJ, Telan E, Leyritana K, Tactacan-Abrenica RJ, Ching PR, et al. High rates of tenofovir failure in a CRF01_AE-predominant HIV epidemic in the Philippines. Int J Infect Dis. (2020) 95:125–132. doi: 10.1016/j.ijid.2020.02.020
5. Jiamsakul A, Kumarasamy N, Ditangco R, Li PC, Phanuphak P, Sirisanthana T, et al. Factors associated with suboptimal adherence to antiretroviral therapy in Asia. J Int AIDS Soc. (2014) 17:1–9. doi: 10.7448/IAS.17.1.18911
6. Zhang JA, Wei Z, Li CG, Sun CB. Adherence to long-term therapies. WHO. (2003) 321:1779–83. doi: 10.4028/www.scientific.net/AMM.321-324.1779
7. Samonte GMJ, Belimac JGB, Feliciano JS. Philippines Estimates of the Most at-Risk Population and People Living with HIV. Philippines: Department of Health (2011). p. 1–24.
8. Roberts JE, Ciesla JA. Meta-analysis of the relationship between hiv infection and risk for depressive disorders. Am J Psychiatry. (2001) 158:725–30. doi: 10.1176/appi.ajp.158.5.725
9. Mills TC, Paul J, Stall R, Pollack L, Canchola J, Chang YJ, et al. Distress and depression in men who have sex with men: the Urban men's health study. Am J Psychiatry. (2004) 161:278–85. doi: 10.1176/appi.ajp.161.2.278
10. Secor A, Wahome E, Micheni M, Rao D, Simoni J, Sanders E, et al. Prevalence of depression, substance abuse, and stigma among men who have sex with men in coastal Kenya. Ann Glob Heal. (2015) 81:101–2. doi: 10.1016/j.aogh.2015.02.735
11. Leserman J, Petitto JM, Perkins DO. Severe stress, depressive symptoms, and changes in lymphocyte subsets in human immunodeficiency virus—infected men a 2-year follow-up study. JAMA Psychiatry. (1997) 54:279–85. doi: 10.1001/archpsyc.1997.01830150105015
12. Page-Shafer K, Delorenze GN, Satariano WA, Winkelstein W Jr Comorbidity and survival in HIV-infected men in the San Francisco men's health survey. Ann Epidemiol. (1996) 6:420–30. doi: 10.1016/S1047-2797(96)00064-6
13. Kim MH, Mazenga AC, Yu X, Ahmed S, Paul ME, Kazembe PN, et al. High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: barriers and associated factors. J Int AIDS Soc. (2017) 20:1–12. doi: 10.7448/IAS.20.1.21437
14. Tran BX, Dang AK, Truong NT, Ha GH, Nguyen HLT, Do HN, et al. Depression and quality of life among patients living with HIV/AIDS in the era of universal treatment access in Vietnam. Int J Environ Res Public Health. (2018) 15:1–14. doi: 10.3390/ijerph15122888
15. Oconnor C, Leyritana K, Calica K, Gill R, Doyle AM, Lewis JJ, et al. Risk factors affecting adherence to antiretroviral therapy among HIV patients in Manila, Philippines: a baseline cross-sectional analysis of the Philippines connect for life study. Sex Health. (2021) 18:95–103. doi: 10.1071/SH20028
16. Rotheram-Borus MJ, Stein JA, Jiraphongsa C, Khumtong S, Lee SJ, Li L. Benefits of family and social relationships for Thai parents living with HIV. Prev Sci. (2010) 11:298–307. doi: 10.1007/s11121-009-0165-6
17. Sellier P, Clevenbergh P, Ljubicic L, Simoneau G, Evans J, Delcey V, et al. Comparative evaluation of adherence to antiretroviral therapy in sub-Saharan African native HIV-infected patients in France and Africa. Clin Infect Dis. (2006) 43:654–7. doi: 10.1086/506436
18. Ivers LC, Chang Y, Gregory Jerome J, Freedberg KA. Food assistance is associated with improved body mass index, food security and attendance at clinic in an HIV program in central Haiti: a prospective observational cohort study. AIDS Res Ther. (2010) 7:1–8. doi: 10.1186/1742-6405-7-33
19. Berhe N, Tegabu D, Alemayehu M. Effect of nutritional factors on adherence to antiretroviral therapy among HIV-infected adults: a case control study in Northern Ethiopia. BMC Infect Dis. (2013) 13:233. doi: 10.1186/1471-2334-13-233
20. Guaraldi G, Orlando G, Squillace N, De Santis G, Pedone A, Spaggiari A, et al. Multidisciplinary approach to the treatment of metabolic and morphologic alterations of HIV-related lipodystrophy. HIV Clin Trials. (2006) 7:97–106. doi: 10.1310/EYWJ-8B5K-X7VQ-9CPE
21. Cabrero E, Griffa L, Burgos A, HIV Body Physical Changes Study Group. Prevalence and impact of body physical changes in HIV patients treated with highly active antiretroviral therapy: results from a study on patient and physician perceptions. AIDS Patient Care STDS. (2010) 24:5–13. doi: 10.1089/apc.2009.0191
22. Morrison MA, Morrison TG, Sager CL. Does body satisfaction differ between gay men and lesbian women and heterosexual men and women? A meta-analytic review. Body Image. (2004) 1:127–38. doi: 10.1016/j.bodyim.2004.01.002
23. Olssøn I, Mykletun A, Dahl AA. The hospital anxiety and depression rating scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry. (2005) 5:46. doi: 10.1186/1471-244X-5-46
24. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. an updated literature review. J Psychosom Res. (2002) 52:69–77. doi: 10.1016/s0022-3999(01)00296-3
25. Aherrera JAM, Abrahan LL, Racaza GZ, Train CQ, Jara RD. Depression and anxiety in adults with congenital heart disease using the validated filipino version of the hospital anxiety and depression score (HADS-P). Phillippine J Intern Med. (2016) 54:1–8. doi: 10.1016/j.gheart.2015.03.029
26. Gauiran DTV, Samala KG, Lim JA, De Guzman ML. Measurement of anxiety and depression among HIV patients seen in the Philippines general hospital using the hospital anxiety and depression scale-Pilipino Version (HAdS-P). Acta Med Philipp. (2018) 52:40–52. doi: 10.47895/amp.v52i1.466
27. Jelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale: an updated literature review. Psychosom Res. (2002) 52:69–77. doi: 10.1016/S0022-3999(01)00296-3
28. United Nations Office on Drugs and Crime. Guidance for Community-Based Treatment and Care Services for People Affected by Drug Use and Dependence in the Philippines. (2014).
29. Lawford BR, Barnes M, Connor JP, Heslop K, Nyst P, Young RMD. The alcohol use disorders identification test guidelines for use in primary care. WHO. (2012) 26:324–9. doi: 10.1177/0269881110393051
30. Bohn MJ, Babor TF, Kranzler HR. The alcohol use disorders identification test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol. (1995) 56:423–32. doi: 10.15288/jsa.1995.56.423
31. Haber MG, Cohen JL, Lucas T, Baltes BB. The relationship between self-reported received and perceived social support: a meta-analytic review. Am J Community Psychol. (2007) 39:133–44. doi: 10.1007/s10464-007-9100-9
32. Zimet GD, Dahlem NW, Zimet SG, Gordon K, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (2010) 52:37–41. doi: 10.1207/s15327752jpa5201
33. Dambi JM, Corten L, Chiwaridzo M, Jack H, Mlambo T, Jelsma J. A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the multidimensional perceived social support scale (MSPSS). Health Qual Life Outcomes. (2018) 16:80. doi: 10.1186/s12955-018-0912-0
34. Bruwer B, Emsley R, Kidd M, Lochner C, Seedat S. Psychometric properties of the multidimensional scale of perceived social support in youth. Compr Psychiatry. (2008) 49:195–201. doi: 10.1016/j.comppsych.2007.09.002
35. Qadir F, Khalid A, Haqqani S, Zill-E-Huma, Medhin G. The association of marital relationship and perceived social support with mental health of women in Pakistan. BMC Public Health. (2013) 13:1150. doi: 10.1186/1471-2458-13-1150
36. Wongpakaran T, Wongpakaran N, Ruktrakul R. Reliability and validity of the multidimensional scale of perceived social support (MSPSS): Thai version. Clin Pract Epidemiol Ment Heal. (2011) 7:161–6. doi: 10.2174/1745017901107010161
37. Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma For HIV + youth. Adolesc Heal. (2008) 23:1–7. doi: 10.1038/jid.2014.371
38. Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Heal. (2001) 24:518–29. doi: 10.1002/nur.10011
39. Petersen W. Society and the Adolescent Self-Image. vol. 148. Princeton, NJ: Princeton University Press (1965).
40. Visintini R. An assessment of self-esteem in HIV-positive patients. AIDS Care. (2010) 7:99–104. doi: 10.1080/09540129550126902
41. Davis EE, Breathnach A, Moran R. A study of the factor structure of attitudinal measures of major social psychological constructs in an irish sample. Econ Soc Rev. (1977) 9:27–50.
42. Castrighini CD, Reis RK, Neves LA, Brunini S, Canini SR, Gir E. Evaluation of self-esteem in people living with HIV/AIDS in the city of Ribeirão Preto, State of São Paulo, Brazil Autoestima Em Pessoas Vivendo Com HIV/AIDS No Município De Ribeirão Preto, Estado De São Paulo, Brasil. Texto Contexto Enfermagem. (2013) 22:1049.
43. Cash TF, Jakatdar TA, Williams EF. The body image quality of life inventory: further validation with college men and women. Body Image. (2004) 1:279–87. doi: 10.1016/S1740-1445(03)00023-8
44. Blashill AJ, Vander Wal JS. The role of body image dissatisfaction and depression on HAART adherence in HIV positive men: tests of mediation models. AIDS Behav. (2010) 14:280–8. doi: 10.1007/s10461-009-9630-2
45. Helena L, Leite M, Papa A, Castanheiras Valentini R, Objetivo MO. Body image dissatisfaction and adherence to antiretroviral therapy in people with HIV/AIDS. Rev Nutr. (2011) 24:873–81.
46. Tao J, Wang L, Kipp AM, Qian H-L, Yin L, Ruan Y, et al. Diagnosed Chinese men who have sex with men. AIDS Behav J. (2018) 21:292–9. doi: 10.1007/s10461-016-1477-8
47. Ahaneku H, Ross MW, Nyoni JE, Selwyn B, Troisi C, Mbwambo J, et al. Depression and HIV risk among men who have sex with men in Tanzania. AIDS Care Psychol Socio-Medical Asp AIDS/HIV. (2016) 28:140–7. doi: 10.1080/09540121.2016.1146207
48. Hansson M, Chotai J, Nordstöm A, Bodlund O. Comparison of two self-rating scales to detect depression: HADS and PHQ-9. Br J Gen Pract. (2009) 59:650–4. doi: 10.3399/bjgp09X454070
49. Ngum PA, Fon PN, Ngu RC, Verla VS, Luma HN. Depression among HIV/AIDS patients on highly active antiretroviral therapy in the southwest regional hospitals of cameroon: a cross-sectional study. Neurol Ther. (2017) 6:103–14. doi: 10.1007/s40120-017-0065-9
50. Legesse TA, Reta MA. Adherence to antiretroviral therapy and associated factors among people living with HIV/AIDS in Hara Town and its surroundings, North-Eastern Ethiopia: a cross-sectional study. Ethiop J Health Sci. (2019) 29:299–308. doi: 10.4314/ejhs.v29i3.2
51. Wasti SP, Simkhada P, Randall J, Freeman JV, van Teijlingen E. Factors influencing adherence to antiretroviral treatment in Nepal: a mixed-methods study. PLoS ONE. (2012) 7:e35547. doi: 10.1371/journal.pone.0035547
52. Saqib A, Atif M, Ikram R, Riaz F, Abubakar M, Scahill S. Factors affecting patients' knowledge about dispensed medicines: a qualitative study of healthcare professionals and patients in Pakistan. PLoS ONE. (2018) 13:e0197482. doi: 10.1371/journal.pone.0197482
53. Amberbir A, Woldemichael K, Getachew S, Girma B, Deribe K. Predictors of adherence to antiretroviral therapy among HIV-infected persons: a prospective study in Southwest Ethiopia. BMC Public Health. (2008) 8:265. doi: 10.1186/1471-2458-8-265
54. Buathong N, Hiransuthikula N, Tangwongchaib S, Komoltric C. Association between depression and adherence to highly active antiretroviral therapy among adult HIV infected patients in Thailand. Asian Biomed. (2009) 3:127–33.
55. Shah B, Walshe L, Saple DG, Mehta SH, Ramnani JP, Kharkar RD, et al. Adherence to antiretroviral therapy and virologic suppression among HIV-infected persons receiving care in private clinics in Mumbai, India. Clin Infect Dis. (2007) 44:1235–44. doi: 10.1086/513429
56. Poudel KC, Buchanan DR, Amiya RM, Poudel-Tandukar K. Perceived family support and antiretroviral adherence in HIV-positive individuals: results from a community-based positive living with HIV study. Int Q Community Health Educ. (2015) 36:71–91. doi: 10.1177/0272684X15614220
57. Russell CJ, Keel PK. Homosexuality as a specific risk factor for eating disorders in men. Eat Disord. (2002) 31:300–06. doi: 10.1002/eat.10036
58. Blashill AJ, Gordon JR, Safren SA. Depression longitudinally mediates the association of appearance concerns to ART non-adherence in HIV-infected individuals with a history of injection drug use. J Behav Med. (2014) 37:166–72. doi: 10.1007/s10865-012-9476-3
59. Brennan DJ, Craig SL, Thompson DE. Factors associated with a drive for muscularity among gay and bisexual men. Cult Heal Sex. (2012) 14:1–15. doi: 10.1080/13691058.2011.619578
60. Brennan DJ, Crath R, Hart TA, Gadalla T, Gillis L. Body satisfaction and disordered eating among men who have sex with men in Canada. Int J Mens Heal. (2011) 10:253–68. doi: 10.3149/jmh.1003.253
61. Theodore PS, Achiro RP, Duran RE, Antoni MH. Body dissatisfaction and methamphetamine use among HIV-positive gay and bisexual men: a pilot study. Subst Use Misuse. (2011) 46:1745–9. doi: 10.3109/10826084.2011.618998
62. Hunt CJ, Gonsalkorale K, Nosek BA. Links between psychosocial variables and body dissatisfaction in homosexual men: differential relations with the drive for muscularity and the drive for thinness. Int J Mens Health. (2012) 11:127–36.
63. Ammassari A, Antinori A, Cozzi-Lepri A, Trotta MP, Nasti G, Ridolfo AL. Relationship between HAART adherence and adipose tissue alterations. J Acquir Immune Defic Syndr. (2002) 15:S140–4. doi: 10.1097/00126334-200212153-00011
64. Plankey M, Bacchetti P, Jin C, Grimes B, Hyman C, Cohen M, et al. Self-perception of body fat changes and HAART adherence in the women's interagency HIV study. AIDS Behav. (2009) 13:53–9. doi: 10.1007/s10461-008-9444-7
65. Ten Have M, de Graaf R, Monshouwer K. Physical exercise in adults and mental health status findings from the Netherlands mental health survey and incidence study (NEMESIS). J Psychosom Res. (2011) 71:342–8. doi: 10.1016/j.jpsychores.2011.04.001
66. Ouansafi I, Chibanda D, Munetsi E, Simms V. Impact of friendship bench problem-solving therapy on adherence to ART in young people living with HIV in Zimbabwe: a qualitative study. PLoS ONE. (2021) 16:1–13. doi: 10.1371/journal.pone.0250074
Keywords: depression, adherence, anxiety, antiretroviral therapy (ART), men who have sex with men (MSM), Philippines
Citation: Elsayed H, O'Connor C, Leyritana K, Salvana E and Cox SE (2021) Depression, Nutrition, and Adherence to Antiretroviral Therapy in Men Who Have Sex With Men in Manila, Philippines. Front. Public Health 9:644438. doi: 10.3389/fpubh.2021.644438
Received: 21 December 2020; Accepted: 19 August 2021;
Published: 21 September 2021.
Edited by:
Roger C. Ho, National University of Singapore, SingaporeReviewed by:
Alvona Zi Hui Loh, MOH Holdings, SingaporeFengyi Hao, First People's Hospital of Chongqing Liangjiang New District, China
Copyright © 2021 Elsayed, O'Connor, Leyritana, Salvana and Cox. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hend Elsayed, aGVuZC5lbGFiYmFzeUBob3RtYWlsLmNvbQ==
 Hend Elsayed
Hend Elsayed Cara O'Connor2,3
Cara O'Connor2,3 Sharon E. Cox
Sharon E. Cox