- 1Curtin School of Allied Health, Curtin University, Perth, WA, Australia
- 2Department of Aged Care and Rehabilitation, Armadale Kelmscott Memorial Hospital, East Metropolitan Health Service, Armadale, WA, Australia
- 3Amana Living Inc., Perth, WA, Australia
Introduction: Continued evaluation of Transition Care Programs (TCP) is essential to improving older adults' outcomes and can guide which older adults may benefit from undertaking TCP. The aim of this study was to audit a transition care service to identify the association between the characteristics of older adults undertaking a facility-based TCP and (i) discharge destination and (ii) functional improvement.
Materials and methods: An audit (n = 169) of older adults aged 60 years and above who completed a facility-based TCP in Australia was conducted. Outcomes audited were performance of activities of daily living (ADL) measured using the Modified Barthel Index (MBI) and discharge destination. Data were analyzed using logistic regression and linear mixed modeling.
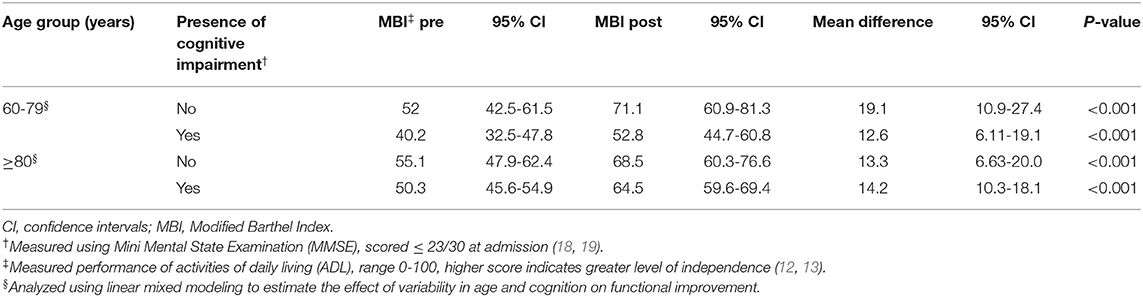
Results: Older adults [mean age 84.2 (±8.3) years] had a median TCP stay of 38 days. Fifty-four older adults (32.0%) were discharged home, 20 (11.8%) were readmitted to hospital and 93 (55%) were admitted to permanent residential aged care. Having no cognitive impairment [OR = 0.41 (95% CI 0.18-0.93)], being independent with ADL at admission [OR = 0.41 (95% CI 0.16-1.00)] and a pre-planned team goal of home discharge [OR = 24.98 (95% CI 5.47-114.15)] was significantly associated with discharge home. Cases discharged home showed greater improvement in functional ability [MBI 21.3 points (95% CI 17.0-25.6)] compared to cases discharged to other destinations [MBI 9.6 points (95% CI 6.5-12.7)].
Conclusion: Auditing a facility-based TCP identified that older adults who were independent in ADL and had good cognitive levels were more likely to be discharged home. Older adults with cognitive impairment also made clinically significant functional improvements.
Introduction
Older adults requiring an episode of hospitalization are more susceptible to developing new functional deficits during their stay, in part due to prior decline in functional ability (1, 2). Thirty-five to 60% of older adults demonstrate functional decline at hospital discharge, making it challenging for them to successfully return home (1, 2). In order to bridge the gap between hospital and home and prevent premature admission into residential aged care (RAC), Australia established a step-down rehabilitation service known as “Transition Care” (3). Other countries also provide transitional programs for at risk patients, usually older adults, after hospital discharge known as “Intermediate Care” in United Kingdom (4) and “Skilled Nursing” in United States (5). The goal of providing Transition Care Programs (TCP) in either facility-based or community settings is to deliver ongoing multidisciplinary rehabilitation for older adults immediately after an acute hospital admission (3). TCP aim to rehabilitate older adults to regain their functional independence while enabling them and family members to plan for discharge home or transfer to RAC if required (3).
However, there is mixed evidence about whether older adults who complete TCP demonstrate improved physical or cognitive function (3, 6). A recent large national study in Australia found that only 38% of older adults who completed a TCP demonstrated improvement in functional independence (3). Proportions and predictors of discharge home from TCPs varies within and between countries, with ~50% of older adults in Australia being discharged home compared 80% in Norway (3, 6). Characteristics associated with discharge home have been found to include absence of cognitive impairment, being younger, and having better performance of ADL (3, 6). This variation is thought to be due in part to the differences in the setting, type and intensity of TCP provided and type of population admitted to each TCP, including older adults' functional ability at admission (3, 4, 6, 7). A key difference in program settings is that some TCP are delivered in the home using a re-ablement model while others are delivered in facilities (3, 4). Older adults requiring a higher level of care and those with less social support are often admitted to a facility-based TCP as there is 24 h care support available. A national audit in Australia found that Western Australia provided TCP mainly in facility-based settings compared to other states (3). There is also wide variation between countries in health outcomes achieved from TCP (3, 4), in particular the success of the program in reducing admission to RAC. Therefore, continued evaluation of TCP is essential to assist understanding what type of TCP improve older adults' outcomes, including functional ability and eventual discharge destination and allocating scarce health resources (4). Program evaluation is also important to measure effectiveness and quality.
Audit and feedback (A&F) enables clinical care staff and organizations to evaluate their program performance against evidence-based guidelines and to compare programs within and across services (8). In Western Australia one such organization delivers TCP in both facility and home settings. This organization decided to conduct an audit to use as a comparison with current TCP and with similar programs across the broader health setting. This aimed to form a foundation from which to improve TCP and inform future allocation of scarce health resources. The aim of the study was to conduct a retrospective audit to identify the association between older adult characteristics and (i) discharge destination, and (ii) functional improvement in a Transition Care (TC) facility-based setting.
Materials and Methods
Design
We conducted a secondary data analysis of de-identified data from a cohort of older adults who had undertaken facility-based TC rehabilitation. Cases were identified from electronic medical records, and additional data collected by hand searching archived paper medical files.
Ethical Considerations
This study was approved by Curtin University Human Research Ethics Committee and the participating organization's clinical governance committee (Amana Living Inc.). A de-identified data base was supplied by the organization.
Setting and Sample
All cases admitted to a 47 bed TC facility in metropolitan Perth Western Australia from January 1st to October 31st 2018 were reviewed. Cases consisted of older adults aged 60 years and above, who were admitted to the facility to undertake a TCP during the study period. Cases were excluded if the older adult was admitted for palliative care, or for <2 weeks duration.
The facility health professional staffing included a manager, registered nurse, physiotherapist, social worker, and an occupational therapist. A general practitioner, speech pathologist, nutritionist, and podiatrist visited as required. Care assistant staff also assisted clients with daily personal care. The TCP included physiotherapy for functional and mobility training, occupational therapy for cognitive activities and home visits, and social work for discharge planning and care support at home.
Variables
Data recorded for each case at time of TC admission were collected. These variables were age, gender, socioeconomic status measured using Index of Relative Socio-Economic Advantage and Disadvantage (IRSAD) 2016 (9), length of stay (LOS) in hospital prior to admission to the TC facility, whether assistance for ADL or IADL was required prior to hospital admission, living situation prior to hospital admission (alone or with others), use of walking aid, primary diagnosis, number of medications on admission, falls history (prior to TC facility admission), presence of cognitive impairment, presence of depression, and malnourishment (see Supplementary Table 1). The primary diagnosis for cases was categorized as neurological, cardiorespiratory, orthopedic, general medicine/surgical, or geriatric conditions. Where case notes recorded a diagnosis of a mental health condition by the psychiatric team in addition to the primary diagnosis, this was categorized as a separate independent variable. Receiving assistance prior to admission was categorized as receiving assistance with activities of daily living (ADL) using the Katz Index (10) or instrumental activities of daily living (IADL) using the Lawton scale (11).
Each case also had recorded a “pre-planned discharge destination,” which was defined as the participant's expected discharge destination on completion of TCP and was pre-determined by the multidisciplinary team in the hospital prior to Transition Care admission. This pre-planned discharge destination plan was provided to the TCP team at point of admission. The plans nominated the older adult to be discharged after completing their TCP to (i) home or (ii) RAC facility. Previous research suggests that older adults with limited social support, multiple hospital readmissions over the 12 months, high levels of care needs, and multiple medical comorbidities were the most likely candidates to have a pre-planned discharge to residential aged care (7).
Outcomes
The primary outcomes were:
(i) discharge destination categorized as home, RAC facility, or hospital readmission. For group comparisons, discharge was defined as home vs. not home.
(ii) functional ability measured using:
• the Modified Barthel Index (MBI) which measures the older adult's ability to complete personal care tasks including showering and toileting (score 0 to 100—higher scores indicating better ADL performance) (12, 13). This was measured at admission and discharge from TCP to determine changes in functional ability that occurred during TCP;
• whether or not the older adult received carer assistance either for personal care tasks, such as showering or toileting (Katz ADL scale) (10, 14) or for instrumental care tasks such as shopping or cleaning (Lawton's scale) (11) prior to hospitalization and when discharged home after TCP.
Statistical Analysis
Data were summarized using descriptive statistics (frequency distributions for categorical data and means and standard deviations or medians and interquartile ranges (IQR) for continuous data). Group comparisons between cases who were discharged home and those who were discharged elsewhere (RAC, hospital) were made using Chi squared or Fisher Exact tests, as appropriate, for categorical data and t-tests or Mann-Whitney U-tests for continuous data, depending on normality of the distribution. Logistic regression was used to determine case characteristics that were predictors of being discharged home. Univariable logistic regression was undertaken and univariately significant variables (with a p-value of < 0.05) were entered into a multivariable model. Linear mixed modeling was used to determine predictors of improvement in functional ability during their stay in TCP (measured by MBI) from admission to discharge. Analyses were completed using IBM SPSS version 24.0 (Armonk, NY) and STATA version 16.1 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
The sample size was determined based on the minimal clinically important difference (MCID) that has been established for the MBI (15). It was determined that a sample of n = 166 cases has 80% power (alpha = 0.05) to detect a standardized mean difference (effect size dz) of 0.22 (based on mean ± SD = 1.85 ± 8.5) in a matched pairs t-test to compare pre-post measures in a single group (using statistical power analysis program G*Power 3.1.9.2) (16). The sample was drawn from all cases admitted to a 47 bed TC facility in metropolitan Perth Western Australia from January 1st to October 31st 2018.
Results
Case Characteristics
There were n = 169 cases extracted from the database. All cases had a discharge destination and an admission MBI recorded and n = 133 cases had a discharge MBI score. Baseline characteristics of cases are presented in Supplementary Table 1. Approximately one third (n = 56) of the cases had a primary orthopedic diagnosis (this included cases having total hip replacement surgery after hip fracture).
Discharge Destination
There were 32.0% (n = 54) cases discharged home, 55.0% (n = 93) admitted to RAC, and 11.8% (n = 20) readmitted to hospital. Cases who were discharged to their pre-planned discharge destination compared to their actual discharge destination are presented in Figure 1A. Of those who had a pre-planned destination of home, 52.1% (n = 49) went home and 34.0% (n = 32) went to residential care while 81.3% (n = 61) of those whose plan was for discharge to RAC were admitted to RAC. Percentages of cases categorized by level of cognitive impairment who were discharged home compared to other settings are presented in Figure 1B. Of those who discharged home (n = 54), there was a statistically significant increase in the number of older adults requiring assistance with ADL at discharge (n = 32) compared to admission (n = 14) (p = 0.027). There was no statistical difference for the number of older adults requiring assistance with IADL at discharge (n = 47) compared to admission (n = 53) (p = 0.130).
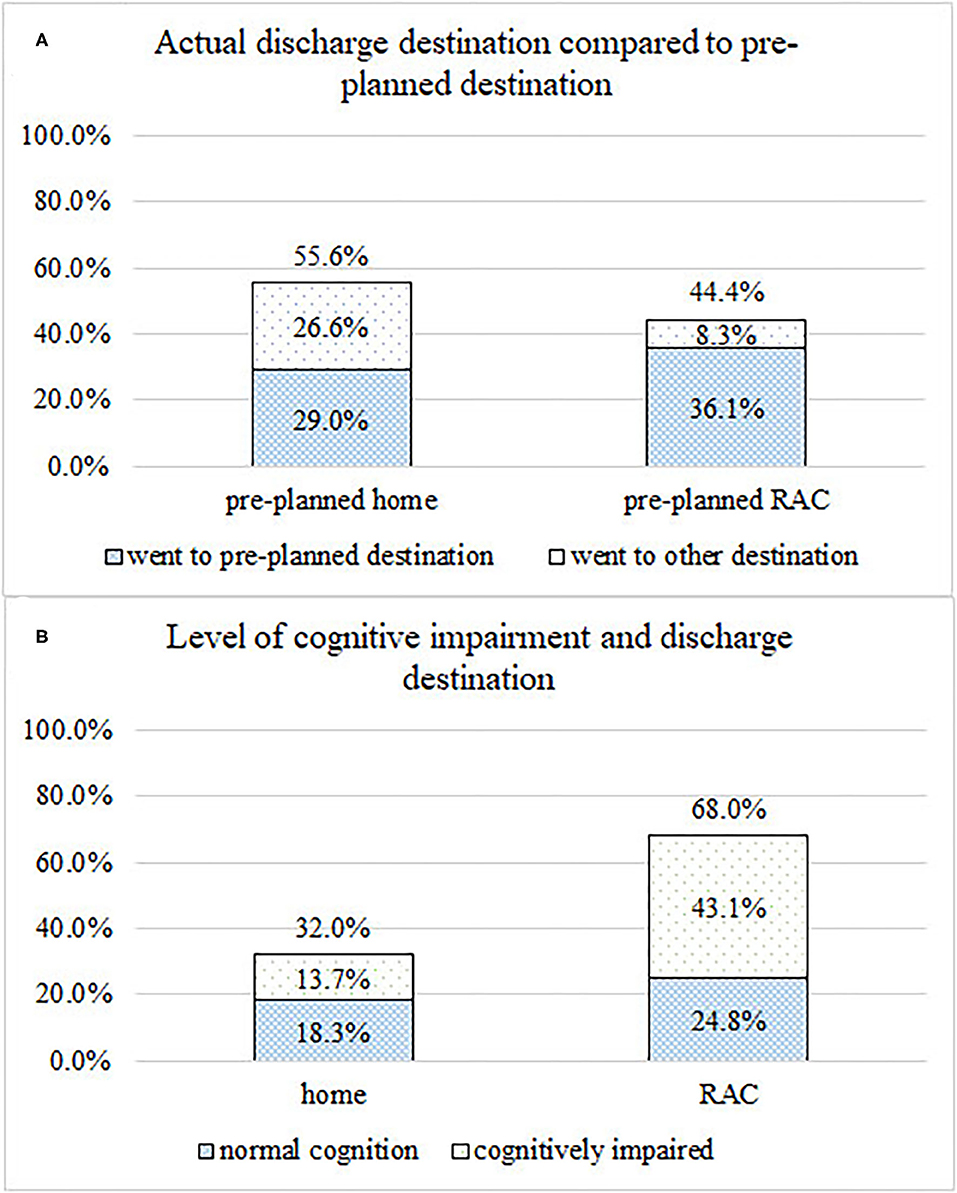
Figure 1. (A) Proportion of cases actual discharge destination compared to pre-planned discharge destination. (B) Number of cases discharged home compared to other discharge destinations, categorized by presence or absence of cognitive impairment.
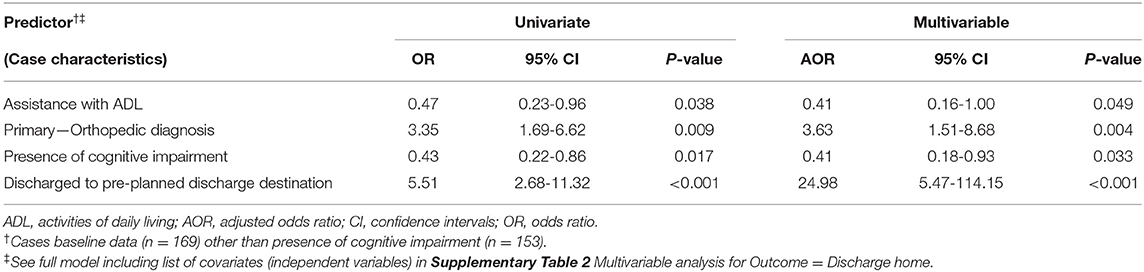
Characteristics of cases discharged home compared to other settings are presented in Table 1. Univariable analyses for the outcome of discharge home are presented in supporting information online Supplementary Table 2. Cases who were receiving assistance with ADL prior to hospitalization, had cognitive impairment or had a diagnosis of a cardiorespiratory condition were significantly less likely to be discharged home. Cases who had a history of falls prior to hospital admission or had a pre-planned discharge destination home were more likely to be discharged home. Adjusted multivariable modeling for the outcome of discharge home is presented in Table 2. Older adults were significantly more likely to be discharged home if they did not require ADL support at home prior to hospitalization, had an orthopedic diagnosis, had no cognitive impairment and had an initial team plan that aimed for discharge home.
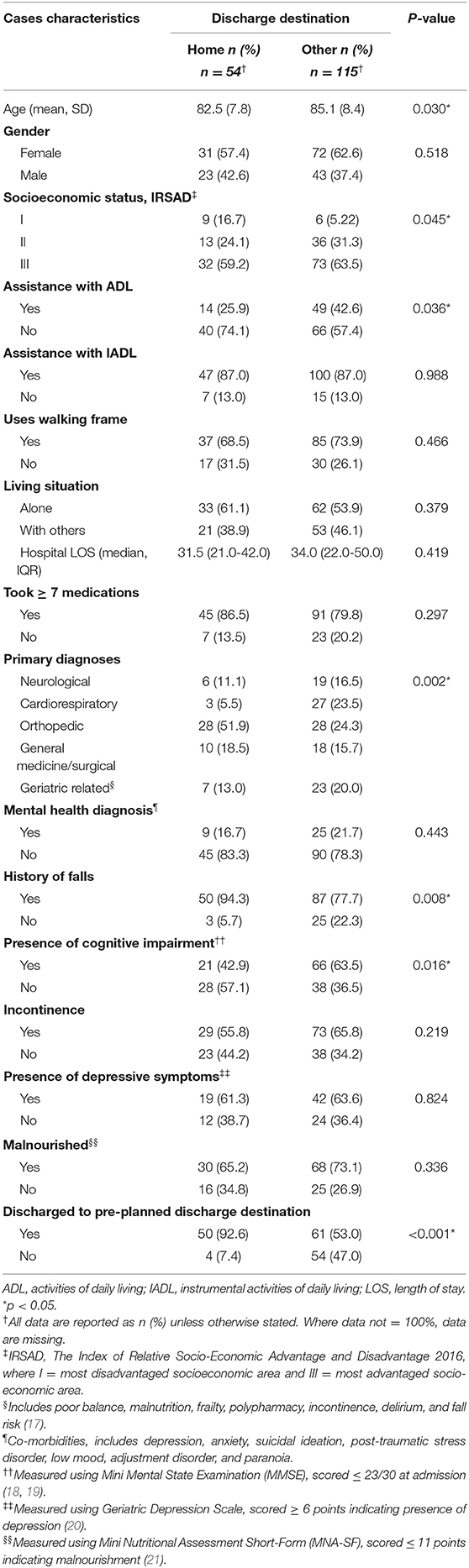
Table 1. Older adults' characteristics—group comparisons for cases discharged home compared to other discharge destination.
Functional Ability
There was a significant mean difference of 13.7 points (95% CI 11.0-16.4, p < 0.001) between cases' functional ability at admission [MBI 48.8 points (95% CI 45.4-52.2)] and discharge [MBI 62.5 points (95% CI 58.9-66.1)]. Cases who were discharged home had a mean improvement in functional ability (MBI) 21.3 points (95% CI 17.0-25.6, p < 0.001) as compared to cases who were discharged to other destination who made a mean improvement of (MBI) 9.6 points (95% CI 6.5-12.7, p < 0.001).
Comparisons of improvements in functional ability by age and presence or absence of cognitive impairment are presented in Table 3, (see also Supplementary Figure 1). There was no significant difference between the improvement made by the four groups [coefficient 7.4 (95% CI −5.603-20.496) (p = 0.263)]. However, there were significant within groups improvements made between admission and discharge.
Discussion
In this Australian cohort of older adults who completed a facility-based TCP, 32% were discharged home. Being independent with ADL at home prior to hospitalization, having an orthopedic diagnosis, having no cognitive impairment and a pre-planned goal of discharge home were significantly associated with returning home. Higher levels of independence with ADL at admission to TC facilities have previously been found to predict discharge home in participants with various diagnoses including stroke (6, 22). A randomized controlled trial conducted in Norway found no difference between the proportions of older adults discharged home from an IC facility compared to those who stayed in hospital, but found that more older adults who were discharged from an IC facility lived independently without home health care services (23). In contrast, a national study in Australia found that older adults who were undertaking TCP in a facility-based setting were more likely to be discharged to RAC and less likely to improve their functional abilities compared to those who undertake TCP in community-based settings (3). Since the goal of TCP is to promote discharge home and avoid RAC admissions, these differences between countries suggest that further evaluation of TCP is required to understand what programs are most effective. Approximately 60% of the older adults who were discharged to RAC had cognitive impairment which accords with other studies that found cognitive impairment significantly reduced the likelihood of older adults returning home (3, 6, 24).
In this TC setting, a health professional team from the discharging hospitals provided a discharge plan, based on assessment of the older adult prior to their transfer to the TC facility discharge. However, only 64% of these discharge plans were accurate predictors of the actual discharge destination achieved by older adults following TCP. This finding concurs with another Australian retrospective study that reported 60% of these types of predictive discharge plans were accurate (25). Other studies have suggested that that having a pre-determined plan influences TCP staff and older adults' motivation and behaviors in engaging with rehabilitation (25, 26). This may negatively impact outcomes for older adults if their discharge plan was pre-determined as admission to RAC.
The cohort's levels of independence in ADL improved significantly and above a MCID through undertaking facility-based TCP. Improvement in ADL has been shown to vary across TCP settings with a range of between −9.26 points to 28 points (6, 27, 28). This could be due to differences in therapy duration, type of rehabilitation provided or the number of rehabilitation staff available, as suggested by a previous study that reported higher staff ratios were a significant predictor of functional improvement (29). There was no significant difference in the amount of improvement in functional ability based on age and cognitive impairment. However, adults in an older age range (80 years and over) with cognitive impairment had a lower functional level on admission. Some older adults discharged home were provided with extra personal and social support compared to admission, indicating that recovery to pre-admission levels might not have occurred. Additionally, older adults with cognitive impairment are at increased risk of experiencing adverse effects of hospitalization, such as functional decline, and are less likely to recover to their previous functional ability (30).
Findings from this audit suggest that TCP rehabilitation may need to be more tailored for older adults with cognitive impairment (31, 32) or more comprehensive home support services are required after discharge from TCP (33). Investigation into whether programs are effectively targeted to older adults with cognitive impairment is important as many older adults, including those with dementia, want to remain in their own home and currently only 5% lived in shared accommodation (34). Since motivation may affect engagement in rehabilitation, facility-based TCP should also consider a policy of engaging all older adults in their family to aim for discharge home as a first option rather than pre-plan for discharge to RAC.
Strengths and Limitations of the Research
Our audit was strengthened by being conducted by the researchers in collaboration with the organization, as it is known that audits conducted by people who want change are more likely to result in change (35). A further audit of home-based TCP in the organization would be of value to compare patients' health outcomes and use of resources. The audit provided a detailed summary of a cohort of older adults that attended a facility-based TCP, evaluating what proportions were successfully discharged home, together with comparison of levels of functional improvement. Case notes were able to be examined in detail as well as electronic records. Although this audit was conducted at one facility it provides useful information on the characteristics of older adults undertaking facility-based TCP in Australia. While admission criteria for all Australian TCP are similar, heterogeneity between settings is likely to be present. There are limited studies that have specifically examined facility-based TCP. These findings may be useful as a comparison for other facility-based transition care services. However, this was a retrospective study using medical case files and there were limited outcome measures available for retrieval. The audit also identified that there was a gap in measuring other health outcomes that would be helpful to evaluate during rehabilitation such as mental and emotional well-being. Other research has also suggested that more comprehensive assessments should be completed in TCP to understand changes in older adults' health and wellbeing (3). Further prospective studies that evaluate a broad range of functional outcomes such as in a comprehensive geriatric assessment are required to assist in evaluating the effectiveness of TCP. A recent study suggested that older adults who completed home based TCP demonstrated better health outcomes compared to those who completed facility-based TCP (3). As only one setting was examined, further studies are required to investigate differences between settings and countries to determine how to make best use of scarce resources for older adults who require transition care after hospital discharge.
Conclusions
An audit identified that older adults admitted to a facility-based TCP were significantly more likely to be discharged home if they were independent with ADL at admission, had an orthopedic diagnosis, had good levels of cognition, and had a pre-planned team goal to be discharged home. Those cases discharged home, made significantly more improvement in performance of ADL than those discharged elsewhere. Older adults with cognitive impairment had lower levels of functional ability on TC admission, however there were no significant differences in the magnitude of improvement in functional ability between these older adults and those without cognitive impairment. Older adults with cognitive impairment were significantly more likely to be discharged to RAC.
Future research that compares facility-based TCP with other forms of TCP would assist in determining the most effective means of providing older adults with transition care after hospitalization.
Data Availability Statement
The datasets presented in this article are not readily available because due to the organization's privacy policy, a deidentified dataset could only be provided if suitable ethics approvals are obtained. Requests to access the datasets should be directed to Professor Anne-Marie Hill; QW5uZS1NYXJpZS5IaWxsQGN1cnRpbi5lZHUuYXU=.
Ethics Statement
The studies involving human participants were reviewed and approved by Curtin University Human Research Ethics Committee and Amana Living Inc's clinical governance committee. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
J-AH led the drafting of the manuscript with support from JF-C, CN, and A-MH. J-AH, JF-C, and A-MH led the research design with support from NW and KP, and assisted with monitoring the research. J-AH and A-MH led the research with support from JF-C and NW. J-AH collected data at the designated site and KP led management of the research at the facility. CN and AJ contributed to statistical analysis. J-AH undertook this research project as part of her doctoral studies under the guidance of JF-C, NW, and A-MH. All authors provided critical evaluation and approval of the final submitted manuscript.
Funding
J-AH is undertaking this research as part of her doctoral studies with the support of an Australian Government Research Training Program Scholarship. A-MH is supported by a National Health and Medical Research Council of Australia Career Development award.
Conflict of Interest
KP is employed by Amana Living Inc. organization.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to acknowledge the assistance of Amana Living Inc. staff throughout the research.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.688640/full#supplementary-material
Abbreviations
ADL, activities of daily living; AOR, adjusted odds ratio; A&F, audit and feedback; CI, confidence intervals; IRSAD, Index of Relative Socio-Economic Advantage and Disadvantage; IADL, Instrumental Activities of Daily Living; IQR, interquartile ranges; LOS, length of stay; MCID, Minimal Clinically Important Difference; MBI, Modified Barthel Index; OR, odds ratio; RAC, residential aged care; TCP, transition care programs; TC, transition care.
References
1. Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. (2003) 51:451-8. doi: 10.1046/j.1532-5415.2003.51152.x
2. Hoogerduijn JG, Buurman BM, Korevaar JC, Grobbee DE, de Rooij SE, Schuurmans MJ. The prediction of functional decline in older hospitalised patients. Age Ageing. (2012) 41:381-7. doi: 10.1093/ageing/afs015
3. Cations M, Lang C, Crotty M, Wesselingh S, Whitehead C, Inacio MC. Factors associated with success in transition care services among older people in Australia. BMC Geriatr. (2020) 20:496. doi: 10.1186/s12877-020-01914-z
4. Social Care Institute for Excellence. Intermediate Care: SCIE Highlights. (2017). Available online at: https://www.scie.org.uk/prevention/independence/intermediatecare/highlights (accessed March 25, 2021).
5. Medicare.gov. Skilled Nursing Facility (SNF) Care (n.d.). Available online at: https://www.medicare.gov/coverage/skilled-nursing-facility-snf-care (accessed March 25, 2021).
6. Abrahamsen JF, Haugland C, Nilsen RM, Ranhoff AH. Predictors for return to own home and being alive at 6 months after nursing home intermediate care following acute hospitalization. Eur Geriatr Med. (2014) 5:108-12. doi: 10.1016/j.eurger.2013.10.012
7. Morita K, Ono S, Ishimaru M, Matsui H, Naruse T, Yasunaga H. Factors affecting discharge to home of geriatric intermediate care facility residents in Japan. J Am Geriatr Soc. (2018) 66:728-34. doi: 10.1111/jgs.15295
8. Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. CD000259 (2012). doi: 10.1002/14651858.CD000259.pub3
9. Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA) 2016. (2018). Available online at: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/2033.0.55.001Main+Features12016?OpenDocument (accessed March 20, 2021).
10. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. (1963) 185:914-9. doi: 10.1001/jama.1963.03060120024016
11. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. (1969) 9:179-86. doi: 10.1093/geront/9.3_Part_1.179
12. Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. (1965) 14:61-5. doi: 10.1037/t02366-000
13. Shah S, Cooper B, Maas F. The barthel index and ADL evaluation in stroke rehabilitation in Australia, Japan, the UK and the USA. Aust Occup Ther J. (1992) 39:5-13. doi: 10.1111/j.1440-1630.1992.tb01729.x
14. Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. (1970) 10:20-30. doi: 10.1093/geront/10.1_Part_1.20
15. Hsieh YW, Wang CH, Wu SC, Chen PC, Sheu CF, Hsieh CL. Establishing the minimal clinically important difference of the barthel index in stroke patients. Neurorehabil Neural Repair. (2007) 21:233-8. doi: 10.1177/1545968306294729
16. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. (2009) 41:1149-60. doi: 10.3758/BRM.41.4.1149
17. Buurman BM, Hoogerduijn JG, de Haan RJ, Abu-Hanna A, Lagaay AM, Verhaar HJ, et al. Geriatric conditions in acutely hospitalized older patients: prevalence and one-year survival and functional decline. PLoS ONE. (2011) 6:e26951. doi: 10.1371/journal.pone.0026951
18. Creavin ST, Wisniewski S, Noel-Storr AH, Trevelyan CM, Hampton T, Rayment D, et al. Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev. CD011145.pub2 (2016). doi: 10.1002/14651858.CD011145.pub2
19. Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189-98. doi: 10.1016/0022-3956(75)90026-6
20. Yesavage JA, Sheikh JI. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. (1986) 5:165-73. doi: 10.1300/J018v05n01_09
21. Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Validation of the Mini Nutritional Assessment short-form (MNA®-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. (2009) 13:782. doi: 10.1007/s12603-009-0214-7
22. Vluggen TPMM, van Haastregt JCM, Tan FES, Kempen GIJM, Schols JMGA, Verbunt JA. Factors associated with successful home discharge after inpatient rehabilitation in frail older stroke patients. BMC Geriatr. (2020) 20:25. doi: 10.1186/s12877-020-1422-6
23. Herfjord JK, Heggestad T, Ersland H. Intermediate care in nursing home after hospital admission: a randomized controlled trial with one year follow-up. BMC Res Notes. (2014) 7:889-99. doi: 10.1186/1756-0500-7-889
24. Clancy U, Brown M, Alio Z, Wardle K, Pendleton N. Older people with hip fracture transferred to intermediate care: outcomes in an integrated health and social care model. Future Healthc J. (2018) 5:58-63. doi: 10.7861/futurehosp.5-1-58
25. Iddagoda MT, Inderjeeth CA, Chan K, Raymond WD. Prognostication accuracy of final destination in poststroke patients requiring transitional care. Australas J Ageing. (2019) 39:e194-200. doi: 10.1111/ajag.12742
26. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42-53. doi: 10.1186/1748-5908-6-42
27. Lawler K, Shields N, Taylor NF. Training family to assist with physiotherapy for older people transitioning from hospital to the community: a pilot randomized controlled trial. Clin Rehabil. (2019) 33:1625-35. doi: 10.1177/0269215519853874
28. Lenze EJ, Lenard E, Bland M, Barco P, Miller JP, Yingling M, et al. Effect of enhanced medical rehabilitation on functional recovery in older adults receiving skilled nursing care after acute rehabilitation: a randomized clinical trial. JAMA Netw Open. (2019) 2:e198199. doi: 10.1001/jamanetworkopen.2019.8199
29. Brusco NK, Taylor NF, Hornung I, Schaffers S, Smith A, de Morton NA. Factors that predict discharge destination for patients in transitional care: a prospective observational cohort study. Aust Health Rev. (2012) 36:430-6. doi: 10.1071/AH11052
30. Fogg C, Griffiths P, Meredith P, Bridges J. Hospital outcomes of older people with cognitive impairment: an integrative review. Int J Geriatr Psychiatry. (2018) 33:1177-97. doi: 10.1002/gps.4919
31. McFarlane RA, Isbel ST, Jamieson MI. Factors determining eligibility and access to subacute rehabilitation for elderly people with dementia and hip fracture. Dementia. (2017) 16:413-23. doi: 10.1177/1471301215599704
32. Toba K, Nakamura Y, Endo H, Okochi J, Tanaka Y, Inaniwa C, et al. Intensive rehabilitation for dementia improved cognitive function and reduced behavioral disturbance in geriatric health service facilities in Japan. Geriatr Gerontol Int. (2014) 14:206-11. doi: 10.1111/ggi.12080
33. Seitz DP, Gill SS, Austin PC, Bell CM, Anderson GM, Gruneir A, et al. Rehabilitation of older adults with dementia after hip fracture. J Am Geriatr Soc. (2016) 64:47-54. doi: 10.1111/jgs.13881
34. Australian Institute of Health and Welfare. Australia's Welfare 2017: in Brief. (2017). Available online at: https://www.aihw.gov.au/getmedia/5c7b48ba-f5a2-46a6-96bd-2bbae02a5139/AIHW-AUS215-AW17_inbrief.pdf (accessed May 19, 2021).
35. Gould NJ, Lorencatto F, Stanworth SJ, Michie S, Prior ME, Glidewell L, et al. Application of theory to enhance audit and feedback interventions to increase the uptake of evidence-based transfusion practice: an intervention development protocol. Implement Sci. (2014) 9:92. doi: 10.1186/s13012-014-0092-1
Keywords: aged, continuity of patient care, independent living, intermediate care, outcome assessment (health care)
Citation: Hang JA, Francis-Coad J, Naseri C, Jacques A, Waldron N, Purslowe K and Hill AM (2021) Identifying the Association Between Older Adults' Characteristics and Their Health-Related Outcomes in a Transition Care Setting: A Retrospective Audit. Front. Public Health 9:688640. doi: 10.3389/fpubh.2021.688640
Received: 31 March 2021; Accepted: 04 June 2021;
Published: 28 June 2021.
Edited by:
Shubing Cai, University of Rochester, United StatesReviewed by:
Li-Fan Liu, National Cheng Kung University, TaiwanLi-Nien Chien, Taipei Medical University, Taiwan
Copyright © 2021 Hang, Francis-Coad, Naseri, Jacques, Waldron, Purslowe and Hill. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jo-Aine Hang, am8tYWluZS5oYW5nQHBvc3RncmFkLmN1cnRpbi5lZHUuYXU=
 Jo-Aine Hang
Jo-Aine Hang Jacqueline Francis-Coad
Jacqueline Francis-Coad Chiara Naseri
Chiara Naseri Angela Jacques1
Angela Jacques1 Kate Purslowe
Kate Purslowe Anne-Marie Hill
Anne-Marie Hill