- 1Department of Expanded Program on Immunization, Hangzhou Center for Disease Control and Prevention, Hangzhou, Zhejiang, China
- 2School of Public Health, Hangzhou Normal University, Hangzhou, Zhejiang, China
Background: Although influenza vaccination is recommended for people aged 70 and above in Hangzhou, and the vaccine is provided free of charge, the elderly influenza vaccination rate is still low. The purpose of this study was to understand the barriers and motivations of older people in deciding to receive free influenza vaccine through questionnaires.
Methods: The method of stratified random sampling was adopted to take samples. A questionnaire survey was conducted among the elderly aged 70 years and above by face-to-face interview or telephone interview.
Results: A total of 11,663 elderly people aged 70–100 years were successfully and effectively interviewed. 85.98% of the respondent were willing to get the influenza shot, 8.91% were unwilling to get the influenza shot, and 5.11% were on vaccine hesitancy. The people of age of 70–79 years old (hesitancy: OR70~79 = 0.668, 95%CI: 0.571 0.782, Unwilling: OR70 − 79 = 0.755, 95%CI: 0.622 0.916), primary school degree or below (hesitancy: ORSecondary school degree or above = 1.467, 95%CI: 1.249 1.724, Unwilling: ORSecondary school degree or above = 1.255, 95%CI: 1.028 1.535), remote areas (hesitancy: OR near central urban area = 2.111, 95%CI: 1.604 2.778, ORcentral urban area = 2.957, 95%CI: 2.255 3.877, Unwilling: OR near central urban area = 1.687, 95%CI: 1.230 2.313. ORcentralurbanarea = 2.218, 95%CI: 1.626 3.027), and convenient for movement (hesitancy: ORyes = 0.494, 95%CI: 0.420 0.580, Unwilling: ORyes = 0.585, 95%CI: 0.480 0.713), understanding of the free vaccine policy (hesitancy: ORunderstand = 0.204, 95%CI: 0.171 0.245, Unwilling: ORunderstand = 0.164, 95%CI: 0.128 0.210), influenza knowledge level≥ 13 points (hesitancy: OR≥13points = 0.628, 95%CI: 0.533 0.739, Unwilling: OR≥13points = 0.538, 95%CI: 0.437 0.662), influenza vaccine knowledge level≥ 12 points (hesitancy: OR≥12points = 0.422, 95%CI: 0.350 0.508, Unwilling: OR≥12points = 0.370, 95%CI: 0.290 0.472), and social trust level ≥ 12 points (hesitancy: OR≥12points = 0.134, 95%CI: 0.112 0.160, Unwilling: OR≥12points = 0.220, 95%CI: 0.180 0.269) are more willing to receive free influenza vaccine.
Conclusion: The proportion of elderly people aged 70 and above who are willing to receive free influenza vaccine is high in Hangzhou. But the level of knowledge about influenza, vaccine and trust in society is low. The government should continue to improve the elderly's awareness and trust in society through medical staff, family members, television and radio media, and guide the elderly to actively vaccinate against influenza. Effective publicity should be carried out through the above channels to guide the elderly to actively vaccinate against influenza.
1. Introduction
Influenza is an acute respiratory infectious disease caused by the influenza virus. Influenza has a high incidence in the population and has caused many outbreaks around the world. Influenza patients have mild upper respiratory tract catarrhal symptoms, but severe systemic symptoms such as high fever, headache, and fatigue (1). Elderly people are more susceptible to influenza because of their weakened immune function and prevalence of chronic diseases (2). Elderly influenza patients often suffer from severe pulmonary infection, which aggravates organ disease and is one of the main causes of death (3).
Studies have shown that population vaccination against influenza can reduce outbreaks of an influenza-like illness (4) and reduce hospital readmissions in older adults with cardiovascular or respiratory diseases (5). Antibodies produced after an influenza vaccination in frail older adults may disappear (6), but the vaccine can still reduce hospitalizations and deaths in these susceptible populations (7–9). Studies have also shown an inverse association between influenza vaccination coverage and SARS-CoV-2 seroprevalence, prevalence of hospitalized patients, prevalence of patients admitted to intensive care units, and deaths attributed to COVID-19 (10). Seasonal influenza vaccinations may have some influence on the incidence and severity of COVID-19 outbreaks (11). With or without additional protective benefits, an influenza vaccination is cost-effective compared with no vaccination (12). Influenza vaccinations for adults 60 years of age or older are highly cost-effective (13). At present, influenza vaccinations are still one of the most effective measures to prevent the occurrence and epidemic of influenza (14). Both the WHO (15) and National Immunization Advisory Committee Technical Working Group (16) recommend influenza vaccinations and that the annual influenza vaccine should be allocated to the elderly and other high-risk groups as priority before the rest of the population.
The average annual vaccination rate for influenza vaccine in China is only 2–3%. In most areas, influenza vaccinations require paying for themselves. Only a few provinces and cities, such as Beijing, Shanghai, Karamay in Xinjiang Province, Shenzhen in Guangdong province and Xinxiang in Henan province, have implemented free influenza vaccinations for the elderly or children (17).some scholars proposed that there should be financing strategies for influenza vaccinations for the elderly (18), including the individual-central-local mechanism (strategy 1), central-local mechanism (strategy 2) and local payment mechanism (strategy 3). Strategy 3 is the current elderly influenza vaccine payment strategy implemented in Hangzhou, Zhejiang Province, which is paid by the local government. Since 2020, Hangzhou has started to provide free influenza vaccines to individuals with a Zhejiang household registration who are 70 years old and above. About 250,000 people are vaccinated each year. In addition, about 50,000 elderly people aged 60 and above receive influenza vaccines at their own expense each year in Hangzhou, and the influenza vaccine coverage rate for this age group is about 15%. In Hangzhou and other parts of China (19), influenza vaccination rates among the elderly are still low. Studies involving the willingness of the elderly to be vaccinated, have shown that multi-component interventions, such as reminders and persuasion to vaccinate at a community-level, can help increase the vaccination rate and reduce the incidence of influenza in the elderly (20). This paper analyzes the reasons of influencing the free influenza vaccination for the elderly people aged 70 and above in Hangzhou. The aim is to prevent influenza through improve the influenza vaccination rate of the elderly population in Hangzhou.
2. Methods
2.1. Basic information and definitions
According to the distance from the central city of Hangzhou, it can be divided into central urban area, near central urban area and remote area. There are 14 districts or counties within Hangzhou, of which Xihufengjingmingsheng has a small population aged 70 and above and did not participate in the survey, 5 are classified as central urban areas (Shangcheng, Gongshu, Xihu, Binjiang and Qiantang), 5 are classified as near central urban area (Xiaoshan, Yuhang, Linping, Fuyang and Linan), and the rest are classified as remote areas (Tonglu, Jiande, Chunan).
Hesitation refers to vaccine hesitation, which refers to the delay or refusal of vaccination due to the lack of awareness of vaccine safety, effectiveness, and disease prevention.
Adverse event following immunization (AEFI) refers to the reaction during or after vaccination that may cause damage to tissues, organs, or functions of the recipients that are suspected to be related to vaccination.
2.2. Sampling method
The method of stratified random sampling was adopted to take samples from 13 districts and counties in equal proportion. The function n = (Z1−α/2/δ)2p(1-p) was used to calculate the overall sample size. the sample population aged 80 years and above was not <25% of the total sample population (at present, the elderly over 80 years old in Hangzhou account for 25% of the total number of elderly people aged 70 and above.). The number of people aged 70 and above was obtained from the 2021 population data from the “Chinese Information System for Disease Control and Prevention”. We estimated a sample size of 9,604 participants, based on α = 1.96, percentage willing to get influenza vaccine (p) = 50%, maximum permissible error (δ) = 0.01p. The total number of elderly people aged 70 and above was 1,172,655. According to the formula k = n/N (k is the sampling proportion, N is the number of individuals in the population, n is the sample size), the sampling proportion is 0.819%.
2.3. Survey methods
A self-designed questionnaire was used in the survey. The 13 district and county centers for Disease Control and prevention in Hangzhou conducted face-to-face surveys or telephone surveys through community workers or medical staff from the community healthcare center. After the survey, the written responses were entered into online web pages for data collection. The survey was conducted on a voluntary basis. After informed consent, the respondents answered the questions and the investigators filled out the questionnaire.
2.4. Survey questionnaire
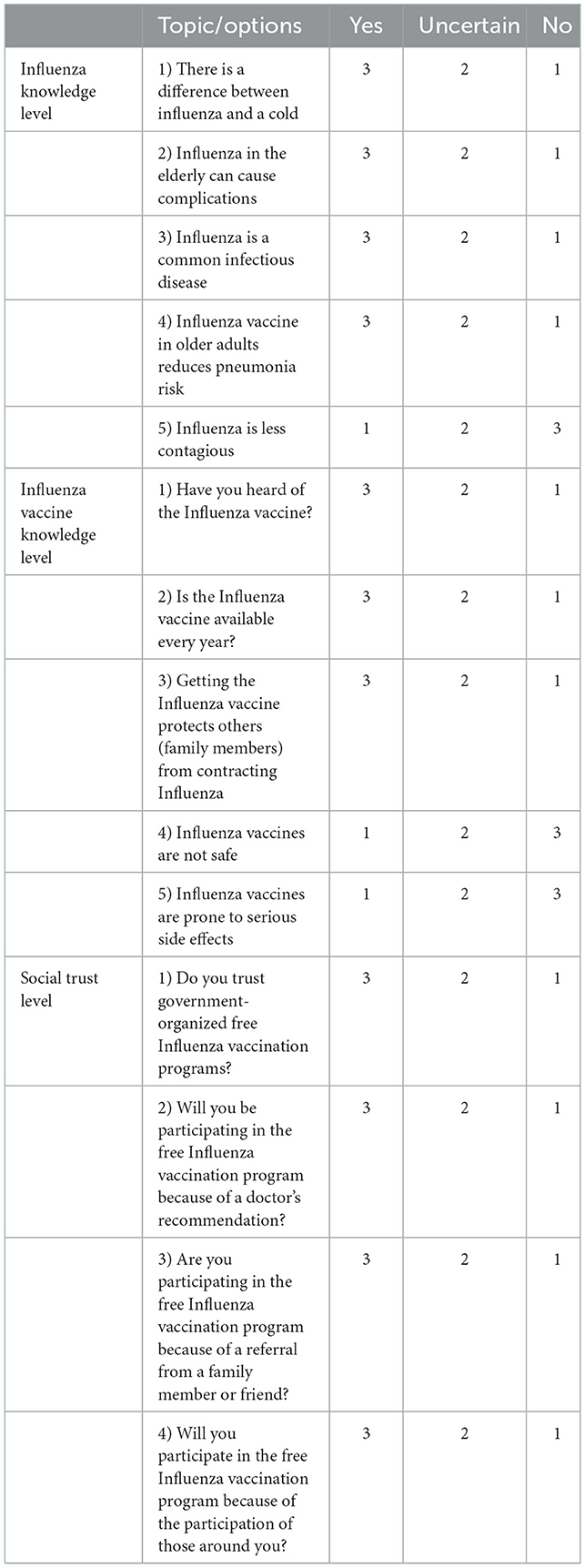
We surveyed selected older adults with a standardized, anonymous questionnaire. The questionnaire topics included sociodemographic characteristics, previous health status, knowledge of influenza and vaccines, intention of influenza vaccination in 2022, and social trust level. The responses to the questions regarding “Influenza knowledge level”, “Influenza vaccine knowledge level”, and “social trust level” were assigned with fixed scoring principles (Table 1).
2.5. Statistical analysis technique
SPSS 21.0 (IBM Corporation, New York, USA) software was used for data analysis. Counting data are described by frequency and composition ratio. Chi-square test, univariate and multivariate Logistic regression analysis were used for data analysis, with test level α = 0.05.
2.6. Ethical considerations
This study was approved by the Hangzhou CDC institutional review board. Both the processes involving data collection and the final storage of data are secure. The names of the interviewees have been anonymous in all the publicly available data.
3. Result
3.1. Demographics
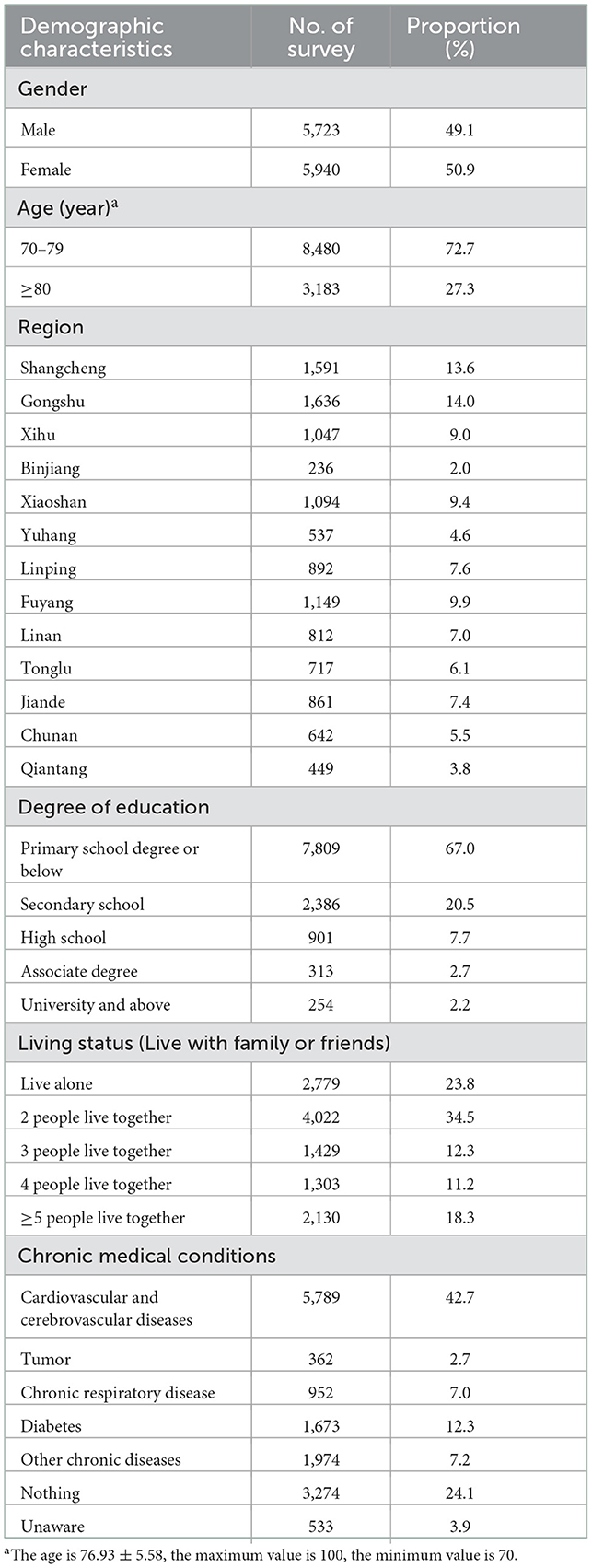
A total of 11,740 questionnaires were sent out and 11,663 were collected. The response rate and validity of the questionnaire were 99.34 and 100%, respectively. 11,663 people were surveyed, including 5,723 males and 5,940 females, with a sex ratio of 1:1.04. Due to the use of face-to-face surveys or telephone surveys by community workers or medical staff from a community healthcare center, and the strict control over the quality of each questionnaire, all 11,663 questionnaires were valid surveys. The average age of the respondents was 76.93±5.58 years old, of which 72.7% were 70–79 years old, and 27.3% were over 80 years old. The minimum age of the respondents was 70 years old, and the maximum age was 100 years old. The educational level of the respondents was mostly primary school or below, accounting for 67.0%. 71.9% of the respondents had a history of chronic diseases. The educational level of the elderly over 70 years old is relatively low, with only 33% having secondary school degree or above. 72% of the elderly over 70 years old suffer from cardiovascular and cerebrovascular diseases, tumor, chronic respiratory disease, diabetes and other chronic diseases (Table 2).
3.2. Univariate analysis of vaccination willingness
Among all the respondents, 10,028 (85.98%) were willing to receive a free influenza vaccine; 1,039 (8.91%) were reluctant to receive the free influenza vaccine, and 596 (5.11%) were hesitant. The willingness rate of influenza vaccination varied by age, region, degree of education, chronic medical conditions, convenience, understanding of the free vaccine policy, influenza knowledge level, influenza vaccine knowledge level, and social trust level. The differences were statistically significant (P < 0.05). Among them, people in urban areas, near central urban area and remote areas have different vaccination intentions, 80.76% (4005/4959), 87.78% (4484/3936) and 94.01% (2220/2087), respectively (Table 3).
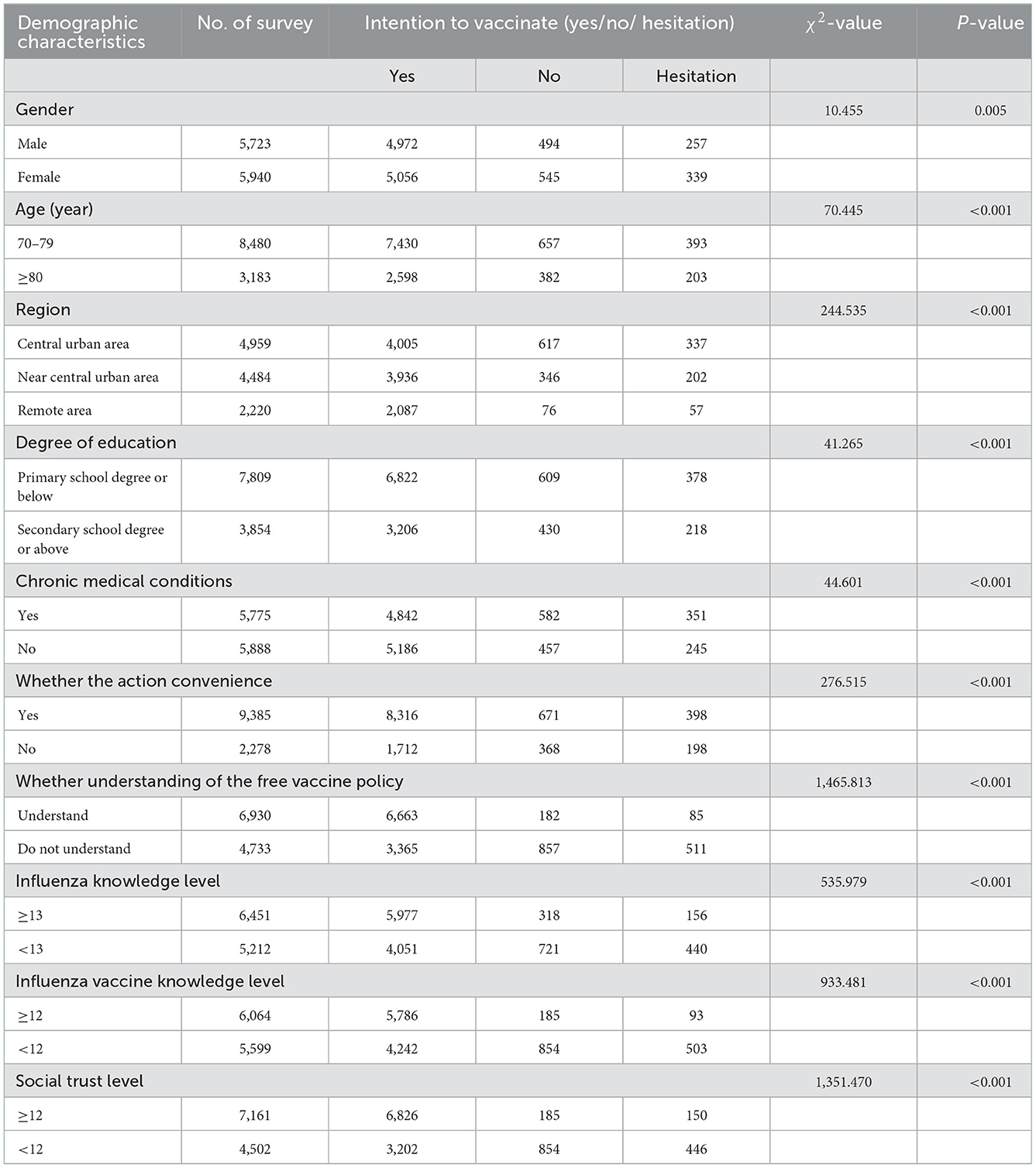
Table 3. Univariate analysis of the willingness of the elderly aged 70 years and above to receive free influenza vaccination in Hangzhou.
3.3. Multivariate analysis of vaccination willingness
Using the willingness to receive an influenza vaccination as the dependent variable, a multivariate Logistic regression analysis was performed on the variables where P <0.05. The results show that whether it is a comparative analysis of those who are willing to be vaccinated and those who are hesitant to be vaccinated, or a comparative analysis of those who are willing to be vaccinated and those who are unwilling to vaccinate, it is in line with the age of 70–79 years old, primary school degree or below, remote areas, and convenient for movement, understanding of the free vaccine policy, influenza knowledge level ≥13 points, influenza vaccine knowledge level ≥12 points, and social trust level ≥12 points are more willing to receive free influenza vaccine (Table 4).
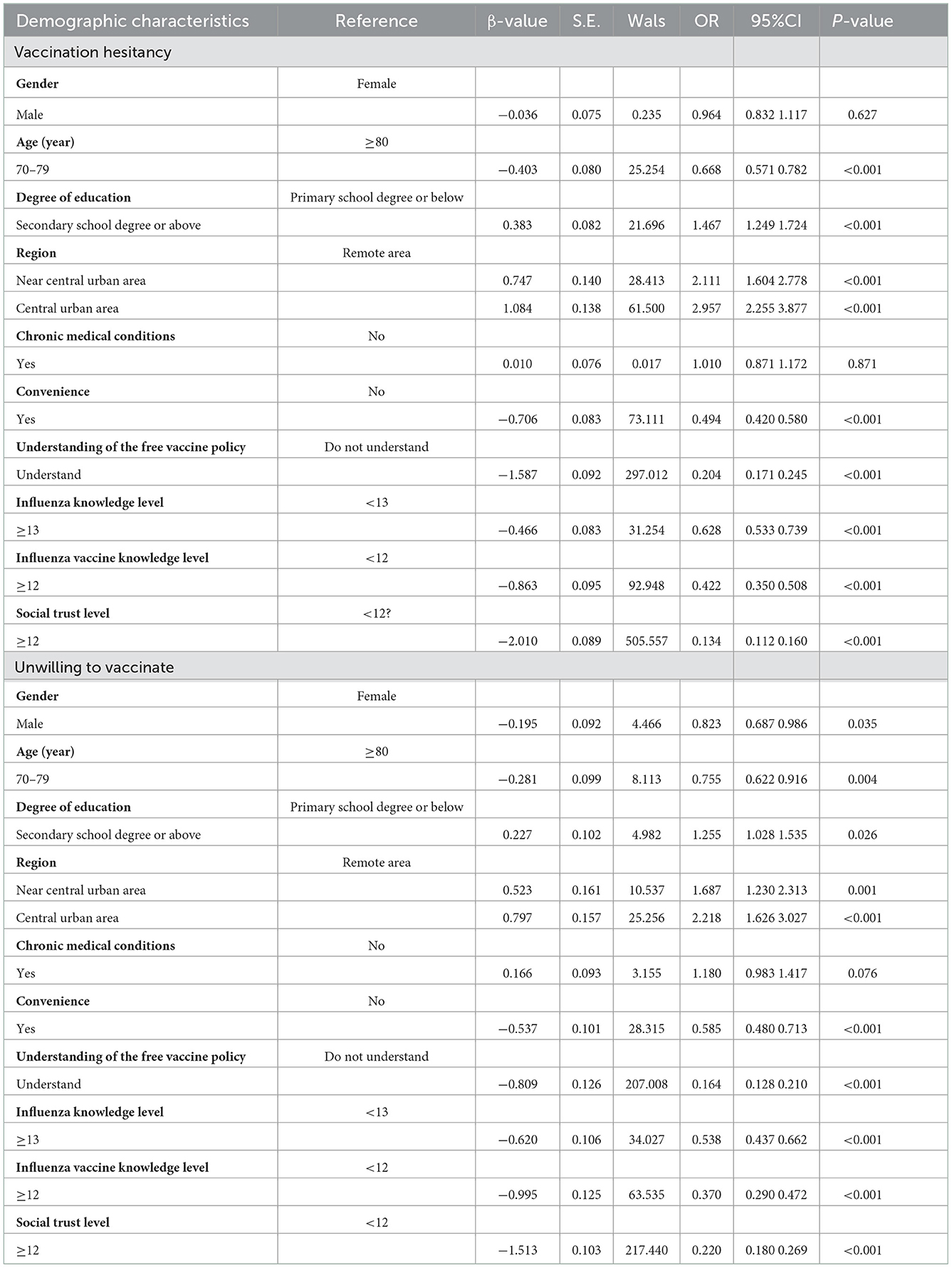
Table 4. Multivariate analysis of willingness to receive free influenza vaccine among the elderly aged 70 and above in Hangzhou.
3.4. Reasons for not getting the free influenza vaccine
A questionnaire survey was conducted among 1,039 respondents who were not willing to receive an influenza vaccine. It was found that the main reasons for not being willing to receive an influenza vaccine were fear of side effects after vaccination, inconvenience to go for a vaccination, uncommon influenza and low risk of influenza infection, accounting for 22, 15.1, 12.6, and 12.0%, respectively (Table 5).
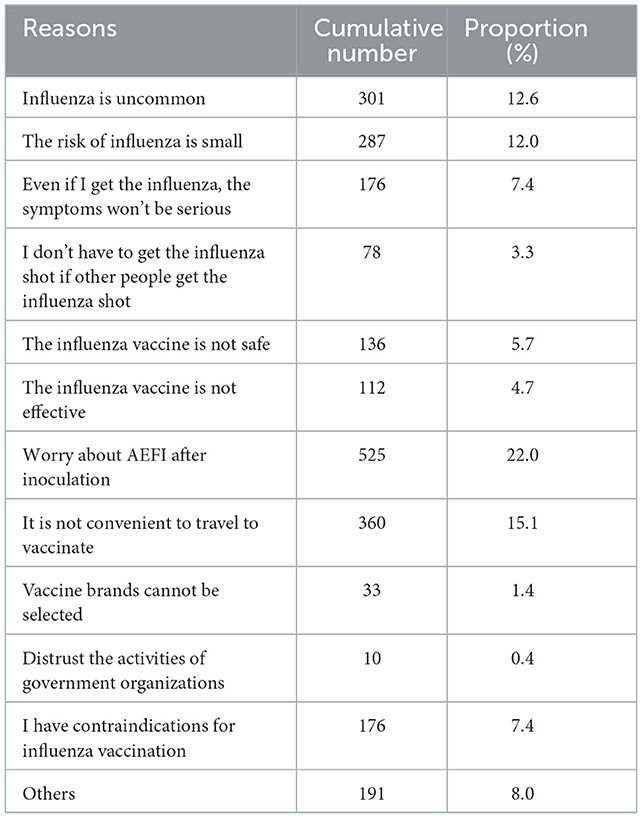
Table 5. Reasons why the elderly aged 70 years and above in Hangzhou are not willing to receive free influenza vaccines.
3.5. Access to health information
A questionnaire survey on the ways of obtaining health information among 11,663 elderly people aged 70 years and above showed that medical institutions and medical staff, family, friends, television and radio were the main ways of obtaining health information, accounting for 27.3, 26.7, and 22.1%, respectively (Table 6).
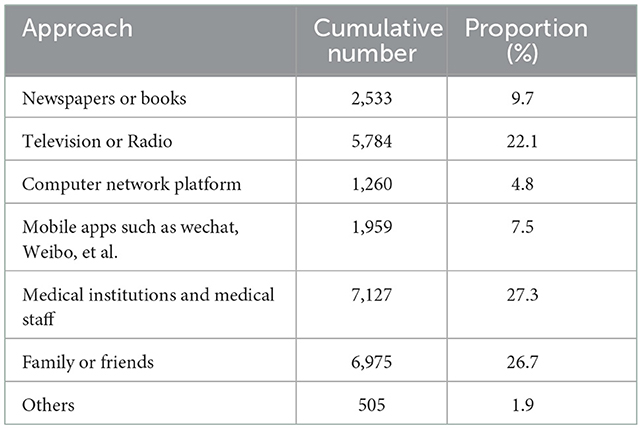
Table 6. Statistical table of ways for the elderly aged 70 years and above to obtain health information in Hangzhou.
4. Discussion
The study shows that a high proportion of people over 70 years old in Hangzhou are willing to get the free influenza vaccine. The proportion of elderly people willing to take an influenza vaccine in Hangzhou is relatively high, which is similar to the study results from the Jiaojiang District of Taizhou City (21) and Chongqing City (22), revealing that elderly people are subjectively willing to take an influenza vaccine. The elderly population with a secondary school degree or above had a lower willingness or more hesitation in taking an influenza vaccination, which was contrary to the results of Peng-Jun Lu (23), Qiushuang Li et al. (24) This may be related to the fact that people with higher education are more likely to form their own personal opinions and have vaccine hesitation after fully understanding the benefits of vaccination and possible AEFI. News media reports of a small number of severe AEFIs have heightened concerns about vaccination among the highly educated. Although the education level of the elderly over 70 years old in Hangzhou is generally not high, the phenomenon of refusing influenza vaccinations among the well-educated elderly population in the Hangzhou area deserves our reflection and further research. The central urban area and near central urban area elderly population in the Hangzhou area had a lower willingness to vaccinate against influenza, contrary to the situation in Poland reported in the literature (25). Although the per capita income of central urban area residents in Hangzhou is similar to that in Poland (74,700 yuan/16,700 U.S. dollars), the willingness of central urban area residents in the two places to be vaccinated is completely opposite, which deserves further study.
Foreign studies have found that there is a strong correlation between free vaccine and vaccination intention (26, 27). In China, where the burden of seasonal influenza is high and vaccination rates are extremely low, the study suggests that most participants expect the government and/or health insurance to partially cover the costs (28). The policy of free influenza vaccination for the elderly aged 70 and above in Hangzhou has successfully improved the vaccination rate. This policy provides policy reference for influenza vaccination of the elderly in other regions of China.
Among all the reasons for unwillingness to choose an influenza vaccination, “Worry about AEFI after inoculation” (22%) had the highest proportion among all reasons for unwillingness to vaccinate, which was consistent with the results of the study in Shanghai, China (29). This may be because most people aged 70 and above suffer from chronic diseases, and AEFI can lead to recurrence or exacerbation of chronic diseases. The results of the Shanxi Province study in China showed that older people preferred influenza vaccines with a longer protection duration, followed by lower serious adverse events and higher vaccine effectiveness (30), which were also similar to the results of this study. Abroad, the Tunisian study found that the two main reasons for refusing vaccinations among older adults were fear of side effects (71.5%) and belief that vaccines were ineffective in avoiding influenza (33.9%) (31). In South Korea, a report of a death allegedly related to an Influenza vaccination in 2020 got a lot of media attention (32), followed by a sharp drop in influenza vaccination rates, from 80.5 to 83.3% in 2015–2019 to 73.6% in 2020–2021. These studies indicates that we should pay attention to people's concerns about AEFI. This may be an important reason why people refuse to be vaccinated against influenza. The degree to which people are concerned about AEFI directly affects people's willingness to vaccinate. The responses “influenza is uncommon ”and “the risk of influenza is small”accounted for 12.6 and 12.0%, respectively. This indicates that the elderly in Hangzhou have an incorrect understanding of influenza and lack of awareness of influenza vaccines, which affects the elderly population's choice of an influenza vaccine (33). It is consistent with the results of Aldiane Gomes de Macedo Bacurau and L M Teo (34), indicating that most older people do not consider influenza as a potentially serious disease and do not believe in the efficacy of an influenza vaccine. The misunderstanding of influenza knowledge and vaccine knowledge in the elderly plays an important role in the decline of influenza vaccinations, suggesting the need to increase the knowledge about influenza and influenza vaccines in the elderly. Providing necessary influenza counseling to those who cannot read, those who do not have a spouse/partner, and explaining the merits of vaccination to at-risk groups may help older adults choose an influenza vaccination.
This study found that medical institutions and medical staff, family, friends, television and radio are the main ways for the elderly to obtain health information. Education about influenza and influenza vaccines by doctors may promote influenza vaccine selection among older adults, thereby increasing influenza vaccination rates. These findings are consistent with those of Agnieszka Wozniak-Kosek (35), Natsuki Kajikawa (36), BirteBödeker (37), Shanxi Province, China (30). It is suggested that health care providers should be encouraged to focus on informing older adults about different aspects of influenza vaccines and influenza illness, as individual perceptions of the benefits of vaccination are critical in decision-making. Informing high-risk groups of influenza vaccination by medical institutions and health care workers also contributes to raising awareness of influenza and helping to increase vaccination rates (38). Recommendations from family and friends are also important factors influencing the elderly to get the influenza vaccine. Studies have shown that elderly people living alone have lower vaccination rates than those living with spouses or children (39), suggesting that health education should be carried out not only for the elderly, but also for their family members.
Similar to findings from other countries (40), this study also shows that improving health literacy through different communication approaches and ultimately informing the public about preventive measures such as vaccination remains one of the most significant public health challenges. Lack of public awareness, lack of adequate knowledge, lack of motivation, and lack of awareness of positive health behaviors including seasonal influenza vaccination remain the status quo of the current level of disease and vaccine awareness among older adults.
This study has some limitations. It shows that the elderly people have a high willingness to receive an influenza vaccination, reaching 85.98%. However, even in the case of free influenza vaccination in 2020 and 2021, the proportion of people over 70 years old is still <40%, which is far lower than that in developed countries (41). Further research is needed to find out what causes people who are willing to get vaccinated to fail to get vaccinated. This study used face-to-face and telephone interviews with community doctors or disease control personnel. With this survey method, the interviewees may be unwilling to express their true wishes directly in person or over the phone because they are worried about continuing to receive medical and health services. This may lead to an increase in the respondents' willingness to vaccinate in the survey results, rather than the real willingness to vaccinate. Studies have shown that appropriate monetary incentives can increase influenza vaccination rates (42).Whether some incentives can be considered to improve vaccination coverage in the elderly population in the Hangzhou region requires further discussion. The main reason for refusing influenza vaccinations in this study was “worry about AEFI after inoculation”. At present, the evidence on the complications of influenza vaccinations in the elderly in China is of poor quality, insufficient or outdated, and there is a lack of specific guidance documents or expert opinions on influenza vaccinations for people aged 65 and above (43). There is also a lack of similar related research in the Hangzhou area, especially for people with chronic diseases, and this paper fails to conduct further research.
5. Conclusion
The proportion of elderly people aged 70 and above who are willing to receive free influenza vaccine is higher in Hangzhou. But the level of knowledge about influenza, vaccine and trust in society is not high. Lack of knowledge about influenza and influenza vaccine is the most important reason for people aged 70 and above to refuse vaccination. The government should continue to improve the elderly's awareness and trust in society through medical staff, family members, television and radio media, and guide the elderly to actively vaccinate against influenza. Effective publicity should be carried out through the above channels to guide the elderly to actively vaccinate against influenza.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Hangzhou CDC Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceived and designed the study: YL, XC, and WG. Obtained and organized the data: JuW, XC, and YX. Analyzed the data: FW and WJ. Contributed reagents, materials, and analysis tools: JD, XiZ, XuZ, and JiW. Wrote the manuscript: XC and YL. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by Basic Public Welfare Research Program of Zhejiang Province (LGF22H260012), Medical Science, Technology Project of Zhejiang Province (Grant No. 2020KY780), and Medical Science and Technology Project of Zhejiang Province (Grant No. A20210434).
Acknowledgments
We thank the staffs at county level Centers for Disease Control and Prevention and in Vaccination Clinics in Hangzhou, for their Questionnaire Collection Work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
3. Vu T, Farish S, Jenkins M, Heath K. A meta-analysis of effectiveness of influenza vaccine in persons aged 65 years and over living in the community. Vaccine. (2002) 20:1831–6. doi: 10.1016/S0264-410X(02)00041-5
4. Monto AS, Kenneth H, Ohmit SE. Influenza vaccine effectiveness among elderly nursing home residents: a cohort study. Am J Epidemiol. (2001) 154:155–60. doi: 10.1093/aje/154.2.155
5. Pang Y, Wang Q, Lv M, Yu M, Lu M, Huang Y, et al. Influenza vaccination and hospitalization outcomes among older patients with cardiovascular or respiratory diseases. J Infect Dis. (2021) 223:1196–204. doi: 10.1093/infdis/jiaa493
6. Sambhara S, Mcelhaney JE. Immunosenescence and influenza vaccine efficacy. Curr Top Microbiol Immunol. (2009) 333:413–29. doi: 10.1007/978-3-540-92165-3_20
7. Deguchi Y, Nishimura K. Efficacy of influenza vaccine in the elderly in welfare nursing homes: reduction in risks of mortality and morbidity during an influenza A (H3N2) epidemic. J Med Microbiol. (2000) 49:553–6. doi: 10.1099/0022-1317-49-6-553
8. Bellino S, Piovesan C, Bella A, Rizzo C, Pezzotti P, Ramigni M. Determinants of vaccination uptake, and influenza vaccine effectiveness in preventing deaths and hospital admissions in the elderly population; Treviso, Italy, 2014/2015-2016/2017 seasons. Hum Vaccin Immunother. (2020) 16:301–12. doi: 10.1080/21645515.2019.1661754
9. Fabiani M, Volpe E, Faraone M, Bella A, Pezzotti P, Chini F. Effectiveness of influenza vaccine in reducing influenza-associated hospitalizations and deaths among the elderly population; Lazio region, Italy, season 2016-2017. Expert Rev Vaccines. (2020) 19:479–89. doi: 10.1080/14760584.2020.1750380
10. Amato M, Werba JP, Frigerio B, Coggi D, Sansaro D, Ravani A, et al. Relationship between influenza vaccination coverage rate and COVID-19 outbreak: an Italian ecological study. Vaccines. (2020) 8:535. doi: 10.3390/vaccines8030535
11. Cocco P, Meloni F, Coratza A, Schirru D, Campagna M, De Matteis S. Vaccination against seasonal influenza and socio-economic and environmental factors as determinants of the geographic variation of COVID-19 incidence and mortality in the Italian elderly. Prev Med. (2021) 143:106351. doi: 10.1016/j.ypmed.2020.106351
12. Dilokthornsakul P, Lan LM, Thakkinstian A, Hutubessy R, Lambach P, Chaiyakunapruk N. Economic evaluation of seasonal influenza vaccination in elderly and health workers: a systematic review and meta-analysis. E Clin Med. (2022) 47:101410. doi: 10.1016/j.eclinm.2022.101410
13. Ortega-Sanchez IR, Mott JA, Kittikraisak W, Khanthamaly V, McCarron M, Keokhonenang S, et al. Cost-effectiveness of seasonal influenza vaccination in pregnant women, healthcare workers and adults >= 60 years of age in Lao People's Democratic Republic. Vaccine. (2021) 39:7633–45. doi: 10.1016/j.vaccine.2021.11.011
14. Rosano A, Bella A, Gesualdo F, Acampora A, Pezzotti P, Marchetti S, et al. Investigating the impact of influenza on excess mortality in all ages in Italy during recent seasons (2013/14-2016/17 seasons). Int J Infect Dis. (2019) 88:127–34. doi: 10.1016/j.ijid.2019.08.003
15. World Health Organization. Vaccines Against Influenza: WHO Position Paper. Weekly Epidemiological Record. Geneva: World Health Organization (2022). p. 19, 97.
16. National Immunization Advisory Committee Technical Working Group. Technical guidelines for seasonal influenza vaccination in China (2020-2021). Zhonghua Yu Fang Yi Xue Za Zhi. (2020) 54:1035–59. doi: 10.3760/cma.j.cn112150-20200911-01198
17. Peng ZB, Wang DY, Yang J, Yang P, Zhang YY, Chen J‘, et al. Current situation and related policies on the implementation and promotion of influenza vaccination, in China. Chin J Epidemiol. (2018) 39:1045–50. doi: 10.3760/cma.j.issn.0254-6450.2018.08.007
18. Lai XZ, Peng ZB, Qin Y, Feng LZ, Li ZJ, Feng ZJ, et al. Financing strategies and cost estimates of influenza vaccination for the elderly in China: explore a multi-party co-payment mechanism. Zhonghua Yi Xue Za Zhi. (2021) 101:2029–36. doi: 10.3760/cma.j.cn112137-20210205-00365
19. Wu S, Su J, Yang P, Zhang H, Li H, Chu Y, et al. Factors associated with the uptake of seasonal influenza vaccination in older and younger adults: a large, population-based survey in Beijing, China. BMJ Open. (2017) 7:e017459. doi: 10.1136/bmjopen-2017-017459
20. Rusli KBD, Bryar R. Maximising influenza vaccination awareness and uptake among older adults in Singapore. Br J Community Nurs. (2018) 23:244–9. doi: 10.12968/bjcn.2018.23.6.244
21. Huang L, Zheng X, Liu L, Qiu C, Li B, Chen Z. Analysis on the willingness and influencing factors of free influenza vaccination among the elderly population in Jiaojiang district. Prev Med. (2019) 31:806–12. doi: 10.19485/j.cnki.issn2096-5087.2019.08.013
22. Yang X, Ding X, Tang W, Tang C, He Y, Chen L. Willingness of influenza vaccination among elderly residents over 65 years old in Chongqing Municipality and its influence factors analysis. Chongqing Med. (2021) 50:1389–93. doi: 10.3969/j.issn.1671-8348.2021.08.028
23. Lu PJ, Srivastav A, Santibanez TA, Christopher Stringer M, Bostwick M, Dever JA, et al. Knowledge of influenza vaccination recommendation and early vaccination uptake during the 2015-16 season among adults aged ≥18years-United States. Vaccine. (2017) 35:4346–54. doi: 10.1016/j.vaccine.2017.06.074
24. Li Q, Zhang M, Chen H, Wu J, Xian J, Zheng L, et al. Influenza vaccination coverage among older adults with hypertension in Shenzhen, China: a cross-sectional survey during the COVID-19 pandemic. Vaccines. (2021) 9:1105. doi: 10.3390/vaccines9101105
25. Ganczak M, Gil K, Korzeń M, Bazydło M. Coverage and influencing determinants of influenza vaccination in elderly patients in a country with a poor vaccination implementation. Int J Environ Res Public Health. (2017) 14:665. doi: 10.3390/ijerph14060665
26. Thomas RE, Lorenzetti DL. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst Rev. (2018) 5:CD005188. doi: 10.1002/14651858.CD005188.pub4
27. Vaux S, Van Cauteren D, Guthmann JP, Le Strat Y, Vaillant V, de Valk H, et al. Influenza vaccination coverage against seasonal and pandemic influenza and their determinants in France: a cross-sectional survey. BMC Public Health. (2011) 11:30. doi: 10.1186/1471-2458-11-30
28. Lai X, Rong H, Ma X, Hou Z, Li S, Jing R, et al. Willingness to pay for seasonal influenza vaccination among children, chronic disease patients, and the elderly in china: a national cross-sectional survey. Vaccines. (2020) 8:405. doi: 10.3390/vaccines8030405
29. Yan S, Wang Y, Zhu W, Zhang L, Gu H, Liu D, et al. Barriers to influenza vaccination among different populations in Shanghai. Hum Vaccin Immunother. (2021) 17:1403–11. doi: 10.1080/21645515.2020.1826250
30. Jiang M, Li P, Yao X, Hayat K, Gong Y, Zhu S, et al. Preference of influenza vaccination among the elderly population in Shaanxi province, China. Hum Vaccin Immunother. (2021) 17:3119–25. doi: 10.1080/21645515.2021.1913029
31. Kharroubi G, Cherif I, Bouabid L, Gharbi A, Boukthir A, Ben Alaya N, et al. Influenza vaccination knowledge, attitudes, and practices among Tunisian elderly with chronic diseases. BMC Geriatr. (2021) 21:700. doi: 10.1186/s12877-021-02667-z
32. Kwon Y, Choe YJ, Yun JW, Kim HK, Kim S, Chun C, et al. Impact of media coverage on influenza vaccine coverage in elderly individuals from 2020 to 2021 in the Republic of Korea. Vaccines. (2021) 9:367. doi: 10.3390/vaccines9040367
33. Ye C, Zhu W, Yu J, Li Z, Hu W, Hao L, et al. Low coverage rate and awareness of influenza vaccine among older people in Shanghai, China: a cross-sectional study. Hum Vaccin Immunother. (2018) 14:2715–21. doi: 10.1080/21645515.2018.1491246
34. Gomes de Macedo Bacurau A, Sato APS, Francisco PMSB. Reasons for nonadherence to vaccination for influenza among older people in Brazil. PLoS One. (2021) 16:e0259640. doi: 10.1371/journal.pone.0259640
35. Wozniak-Kosek A, Kosek J, Rapiejko P. Compliance with vaccination against influenza among the elderly. Adv Exp Med Biol. (2015) 857:79–85. doi: 10.1007/5584_2015_122
36. Kajikawa N, Kataoka Y, Goto R, Maeno T, Yokoya S, Umeyama S, et al. Factors associated with influenza vaccination in Japanese elderly outpatients. Infect Dis Health. (2019) 24:212–21. doi: 10.1016/j.idh.2019.07.002
37. Bödeker B, Remschmidt C, Schmich P, Wichmann O. Why are older adults and individuals with underlying chronic diseases in Germany not vaccinated against flu? A population-based study. BMC Public Health. (2015) 15:618. doi: 10.1186/s12889-015-1970-4
38. Korkmaz P, Paşali Kilit T, Onbaşi K, Mistanoglu Ozatag D, Toka O. Influenza vaccination prevalence among the elderly and individuals with chronic disease, and factors affecting vaccination uptake. Cent Eur J Public Health. (2019) 27:44–9. doi: 10.21101/cejph.a5231
39. Fang R, Lyu M, Wu J, Pang X, Deng Y, Xie Z. Analysis of vaccination coverage of the elderly influenced by different family structures in Beijing. Zhonghua Yu Fang Yi Xue Za Zhi. (2015) 49:1028–31.
40. Cummings CL, Kong WY, Orminski J. A typology of beliefs and misperceptions about the influenza disease and vaccine among older adults in Singapore. PLoS ONE. (2020) 15:e0232472. doi: 10.1371/journal.pone.0232472
41. Jimenez-Trujillo I, López-de Andrés A, Hernández-Barrera V, Carrasco-Garrido P, Santos-Sancho JM, Jiménez-García R. Influenza vaccination coverage rates among diabetes sufferers, predictors of adherence and time trends from 2003 to 2010 in Spain. Hum Vaccin Immunother. (20130 9:1326–32. doi: 10.4161/hv.23926
42. Yue M, Wang Y, Low CK, Yoong JS, Cook AR. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health. (2020) 23:200–8. doi: 10.1016/j.jval.2019.08.006
Keywords: attitudes, influencing factors, influenza vaccines, elderly people, Hangzhou, China
Citation: Che X, Liu Y, Gu W, Wang F, Wang J, Jiang W, Du J, Zhang X, Xu Y, Zhang X and Wang J (2023) Analysis on the intention and influencing factors of free influenza vaccination among the elderly people aged 70 and above in Hangzhou in 2022. Front. Public Health 10:1052500. doi: 10.3389/fpubh.2022.1052500
Received: 24 September 2022; Accepted: 15 December 2022;
Published: 06 January 2023.
Edited by:
Quanman Li, Zhengzhou University, ChinaReviewed by:
Tianchi Yang, Ningbo Municipal Center for Disease Control and Prevention, ChinaHaimei Jia, Fuzhou Center for Disease Control and Prevention, China
Copyright © 2023 Che, Liu, Gu, Wang, Wang, Jiang, Du, Zhang, Xu, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Liu,  MjUwNTYwMzAxQHFxLmNvbQ==
MjUwNTYwMzAxQHFxLmNvbQ==
 Xinren Che1
Xinren Che1 Yan Liu
Yan Liu Xuechao Zhang
Xuechao Zhang