- 1Department of Health Management, College of Public Health, Zhengzhou University, Zhengzhou, China
- 2Department of Science and Laboratory Technology, Dar es Salaam Institute of Technology, Dar es Salaam, Tanzania
- 3Henan Provincial People's Hospital, People's Hospital of Zhengzhou University, Zhengzhou, China
- 4School of Medicine, Southern University of Science and Technology, Shenzhen, China
Objective: To examine the COVID-19 vaccination rate among a representative sample of adults from 31 provinces on the Chinese mainland and identify its influencing factors.
Methods: We gathered sociodemographic information, data on people's awareness and behavior regarding COVID-19 and the COVID-19 vaccine, the accessibility of COVID-19 vaccination services, community environmental factors influencing people's awareness and behavior regarding the vaccination, information about people's skepticism on COVID-19 vaccine, and information about people's trust in doctors as well as vaccine developers through an online nationwide cross-sectional survey among Chinese adults (18 years and older). The odds ratios (OR) and 95% confidence intervals (CI) for the statistical associations were estimated using logistic regression models.
Results: A total of 29,925 participants (51.4% females and 48.6% males) responded. 89.4% of the participants had already received a COVID-19 vaccination. After adjusting for demographic characteristics, awareness of COVID-19 pandemic/ COVID-19 vaccine, community environmental factors, awareness and behavior of general vaccinations, we discovered that having no religious affiliation, having the same occupational status as a result of coronavirus epidemic, being a non-smoker, always engaging in physical activity, having a lower social status, perceiving COVID-19 to be easily curable, and having easier access to vaccination are all associated with high vaccination rate (all P <0.05).
Conclusions: 31 provinces in mainland China currently have a relatively high rate of COVID-19 vaccination. To further increase the rate of COVID-19 vaccination, we must remove barriers associated with the community context and improve access to COVID-19 vaccine services. In addition, taking proactive and effective measures to address the reasons for non-vaccination with COVID-19 will aid in epidemic prevention and control.
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2, emerged as a serious threat to human life at the end of 2019 and quickly spread to become a global pandemic, resulting in over 100 million illnesses and approximately one million deaths (1). Globally, weekly cases had been increasing for more than a month, with over 4 million cases reported in the past weeks and an average of over 570,000 cases were reported each day (2). As of August 4, 2021, there had been 93,374 confirmed cases and 4,636 deaths in mainland China (3). This epidemic has had a significant impact on social development and economic activity throughout the world, straining medical systems in numerous countries (1, 4). Personal preventive methods, including wearing masks and maintaining social distance, have been shown to be successful in slowing the spread of COVID-19, but may not completely eradicate the worldwide large-scale effects of COVID-19 (5–8).
Vaccination has evolved into a routine and highly effective method of illness prevention over the last century, significantly reducing or even eliminating certain viral diseases (9–11), and it is also one of the most effective public health interventions to date (12). Experts and researchers claim COVID-19 vaccination to be the most efficient way to contain this global pandemic (13, 14). Multiple pharmaceutical companies, scientific research and experimental institutes worldwide are rapidly designing, producing, and testing vaccines in response to the global consequences of COVID-19.
The population is vaccinated against COVID-19 using a variety of vaccines including mRNA vaccines (Pfizer, America), adenovirus vector vaccines (AstraZeneca, England), inactivated vaccines (CNBG, China), recombinant subunit vaccines (ZFSW, China), etc. (15, 16). Various companies have provided COVID-19 vaccines to countries around the world. As of August 4, 2021, more than 4 billion vaccination doses had been administered worldwide (17), with China accounting for 1.7 billion doses (18). Although the current data shows that the COVID-19 vaccine biotechnology is safe (1, 4, 19, 20), countries around the world are constantly boosting vaccine supply in order to improve vaccination accessibility. However, the global vaccination rate is still not high enough to build a population immunity barrier (2, 19). This situation exists as a result of major differences in vaccine supply around the globe (17), which contribute greatly to the disparity in vaccination rates between countries. In comparison to the vaccines for other infectious diseases, the COVID-19 vaccine was developed and approved for use in humans for a shorter period of time, as a result of which some people express hesitancy about vaccination (4, 21, 22). Concerns regarding vaccination safety are another factors that may affect people's decision to take a COVID-19 vaccine (23, 24).
However, studies indicate that depending exclusively on biotechnological advancements (effectiveness and safety) may be insufficient to further increase the COVID-19 vaccination rate in the population (4, 22). Thus, an unquantifiable gap may exist between the manufacturing and supply of the next round of global COVID-19 vaccination and its actual use. As a result, the risk of vaccine waste is increasing due to overproduction and investments in developing new vaccine manufacturing technology. It is hence critical to explore the actual factors that affect the coverage rate of the COVID-19 vaccine. In 2021, the COVID-19 epidemic occurred in some regions of China, including Guangzhou, Shenzhen, Nanjing, Chengdu, and Zhengzhou. Studies suggest that the severity of the COVID-19 outbreaks in various places, as well as the level of public awareness of the pandemic and the accessibility of the vaccination services may greatly influence the vaccination rates. However, it is still unclear how and to what extent these factors influenced COVID-19 vaccination rates in China mainland.
In the current study, we also assessed the community context, medical environment, and the acquisition of COVID-19 vaccinations as factors that may influence the vaccination rate. However, it is unclear if these factors influenced COVID-19 vaccination rates and the extent to which they did.
We recruited a saturated sample of participants from 31 provinces throughout mainland China and investigated the current COVID-19 vaccination rate while exploring its influencing factors. And further to provide effective analysis and suggestions for increasing the COVID-19 vaccination rate in China.
Methods
Participants and Procedures
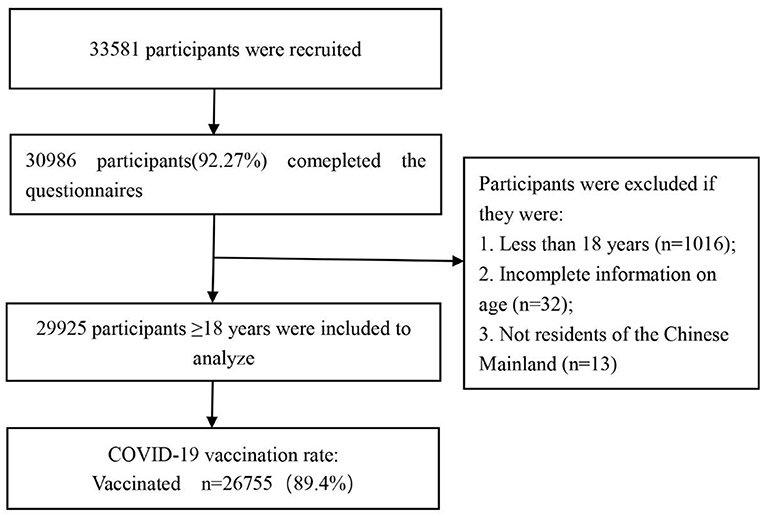
On July 10, 2021, we performed a preliminary online survey in Zhongmou County, Henan Province. Based on the COVID-19 vaccination rate and the reliability (α = 0.927) and validity (KMO = 0.966) of the questionnaire, we estimated the minimum sample size required for the formal survey to be 6,639 participants. This was likewise predicated on an 83.43% COVID-19 vaccination rate in the preliminary online survey, with a 1 percent acceptable error and taking into account the missing 20% sample size (detailed calculations are shown in Annex 1). A subsequent national cross-sectional online survey employing a snowball sampling approach among Chinese adults (≥18 years old) was conducted from 6th to 9th August 2021 by a market research company. During the study period, participants were unaware of the topic prior to their tentative consent to complete the survey. In order to ensure that the sample size for the current study was sufficient for estimating the vaccine coverage rate, sample saturation was monitored during the investigation (Annex 2). We ended the online survey when the sample reached 29,925 on 9th August 2021. Figure 1 depicts the flowchart for participant selection. The study protocol was approved by the Life Science Ethics Review Committee of the Zhengzhou University (Approval number: 2021-01-12-05).
Assessments
The questionnaire used in the current study was designed based on the Oxford COVID-19 vaccine Hesitancy Scale, Vaccination knowledge Scale, Oxford Trust in Doctors and Developers Questionnaire, Vaccine Conspiracy Beliefs Scale (4), and the EuroQol Five Dimensions Questionnaire (5).
The questionnaire begins with a question on whether the respondent had ever received the primary COVID-19 vaccine. This question was designed to elicit information about vaccination rates whereby, item-specific response options coded ranging from 1 to 5 were used, including (1) Vaccinated, (2) Being vaccinated, (3) No, but prepared to receive the COVID-19 vaccine, (4) No, and I am not certain if I will receive the COVID-19 vaccine, and (5) No, I am hesitant to receive the COVID-19 vaccine. During the analysis, options (1) and (2) were merged into “Vaccinated” whereas options (3), (4), and (5) were merged into “Unvaccinated.”
Following that, our questionnaire elicited exploratory and confirmatory factors from five dimensions including; (1) Individual characteristics (i.e. sociodemographic data, subjective social status, and health status); (2) perceptions of COVID-19 pandemic progress (i.e. awareness of the global COVID-19 pandemic, local epidemic situation, and risk of COVID-19 infection); (3) perceptions of COVID-19 vaccine (i.e., trust in doctors and vaccine developers, skepticism in coronavirus and COVID-19 vaccine).
Statistical Analysis
The Chi-square goodness-of-fit test was used to monitor sample saturation throughout the online survey (Annex 2). The Chi-square test was carried out to detect differences in COVID-19 vaccination rates across groups. Binary logistic regression was used to examine factors associated with COVID-19 vaccination coverage rate while adjusting for demographic and socio-economic confounders. All statistical analyses were carried out using SPSS version 21.0 and STATA version 16.0. P-value < 0.05 was considered statistically significant.
Results
A total of 33,581 samples were gathered from 31 provinces on the Chinese mainland, with 30,986 respondents completing the survey. All participants filled out the form online. Following the deletion of ineligible samples in accordance with the inclusion and exclusion criteria, 29,925 samples remained. The flowchart of participant selection is presented in Figure 1.
The COVID-19 Vaccination Rate in Mainland China
The sociodemographic characteristics, awareness level of the COVID-19 pandemic, awareness of the COVID-19 vaccine as well as COVID-19 vaccination coverage rate of the study participants are summarized in Table 1. All the results presented here are based on 29,925 valid questionnaires completed online in real time. Overall, 89.4% of participants (n = 26,755) had been vaccinated against COVID-19 whereas 10.6% (n = 3,170) had not. 51.4% of participants were female and the majority were non-religious (85%). The marital status of the individuals varied, with the majority being single (35.2%) or married (61.4%). 87.2% of the participants had completed at least a high school education whereas more than half of the participants did not change employment as a result of the coronavirus epidemic (56.1%). The COVID-19 vaccine hesitancy rate was 8.4%, with the majority of participants believing that their risk of novel coronavirus infection was either very low (65.6%) or moderate (15.5%), and 15.7% believing that they were at high risk of infection.
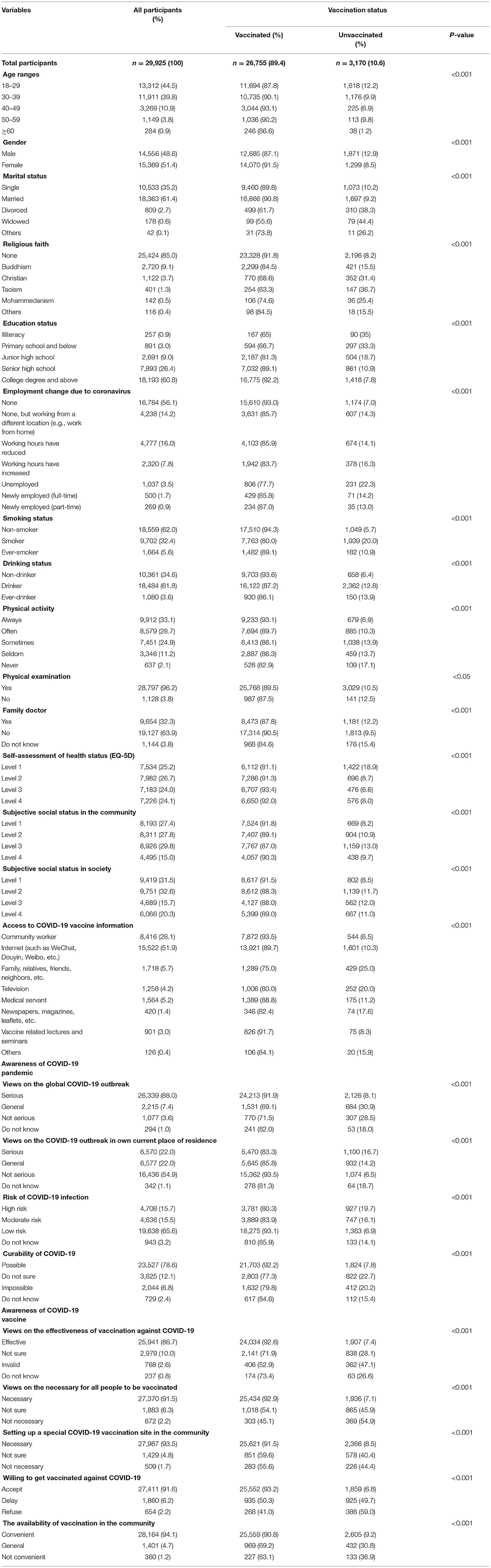
Table 1. Socio-demographic, awareness of COVID-19 pandemic, awareness of COVID-19 vaccine and COVID-19 vaccination rate information (n = 29,925).
The study also indicates that women vaccinated against COVID-19 at a higher rate (52.6%) compared to men (47.4%).Vaccination acceptance was found to be associated with participants age (18–39), female gender, married status, having no religious affiliation, being a graduate of high school and above, maintaining occupational status following the epidemic, being non-smoker, being physically active, physical examination, and having lower social status in the community, to mention a few. Additional participant characteristics are shown in Table 1.
As illustrated in Figure 2, the COVID-19 vaccination rate in all provinces in mainland China exceeded 81.3%, with Shandong province having the highest rate of vaccination at 96%. Additional detailed data is presented in Figure 2.
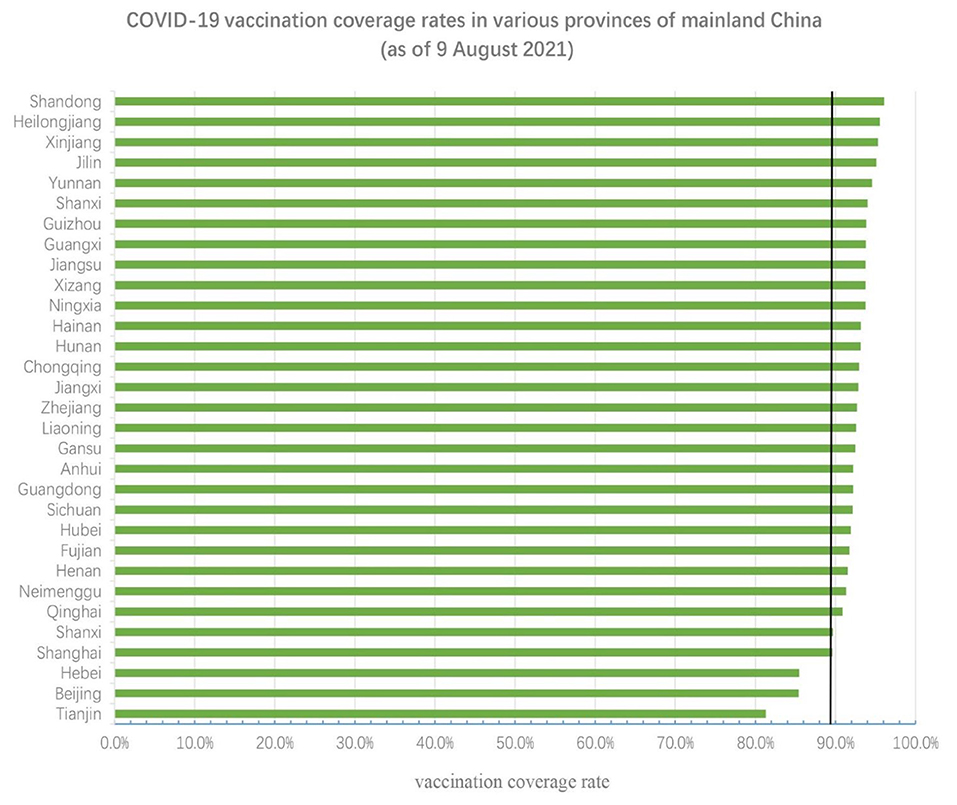
Figure 2. COVID-19 vaccination rates in different provinces. The black vertical line represents the national average level (89.4%).
Factors Affecting the Rate of COVID-19 Vaccination
The logistic regression model showed that age, marital status, religion, employment change due to coronavirus, smoking status, physical activity, self-assessment of health status (EQ-5D), subjective social status in the community, information source for COVID-19 vaccine, the awareness of COVID-19 pandemic and the awareness of COVID-19 vaccine were found to be independently associated with COVID-19 vaccination coverage rate. Being married, non-smoker and willing to get vaccinated, were all positively associated with vaccination rate. Detailed results are shown in Table 2.
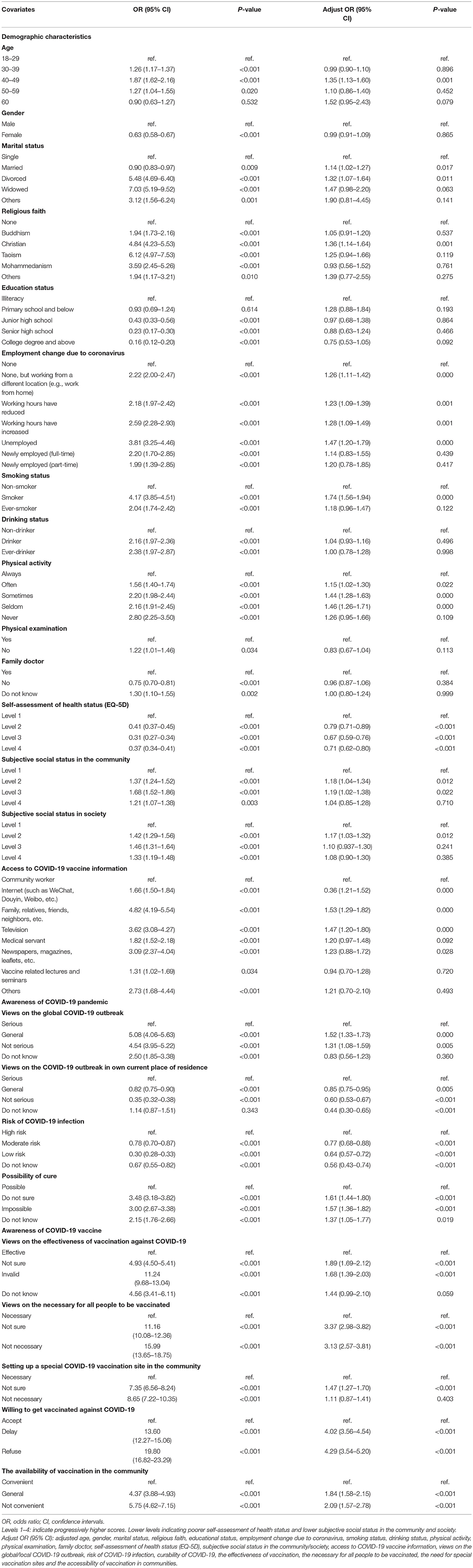
Table 2. Associations of demographic factors, awareness of COVID-19 pandemic, awareness of COVID-19 vaccine with COVID-19 vaccination rate (individual regressions) (n = 29,925).
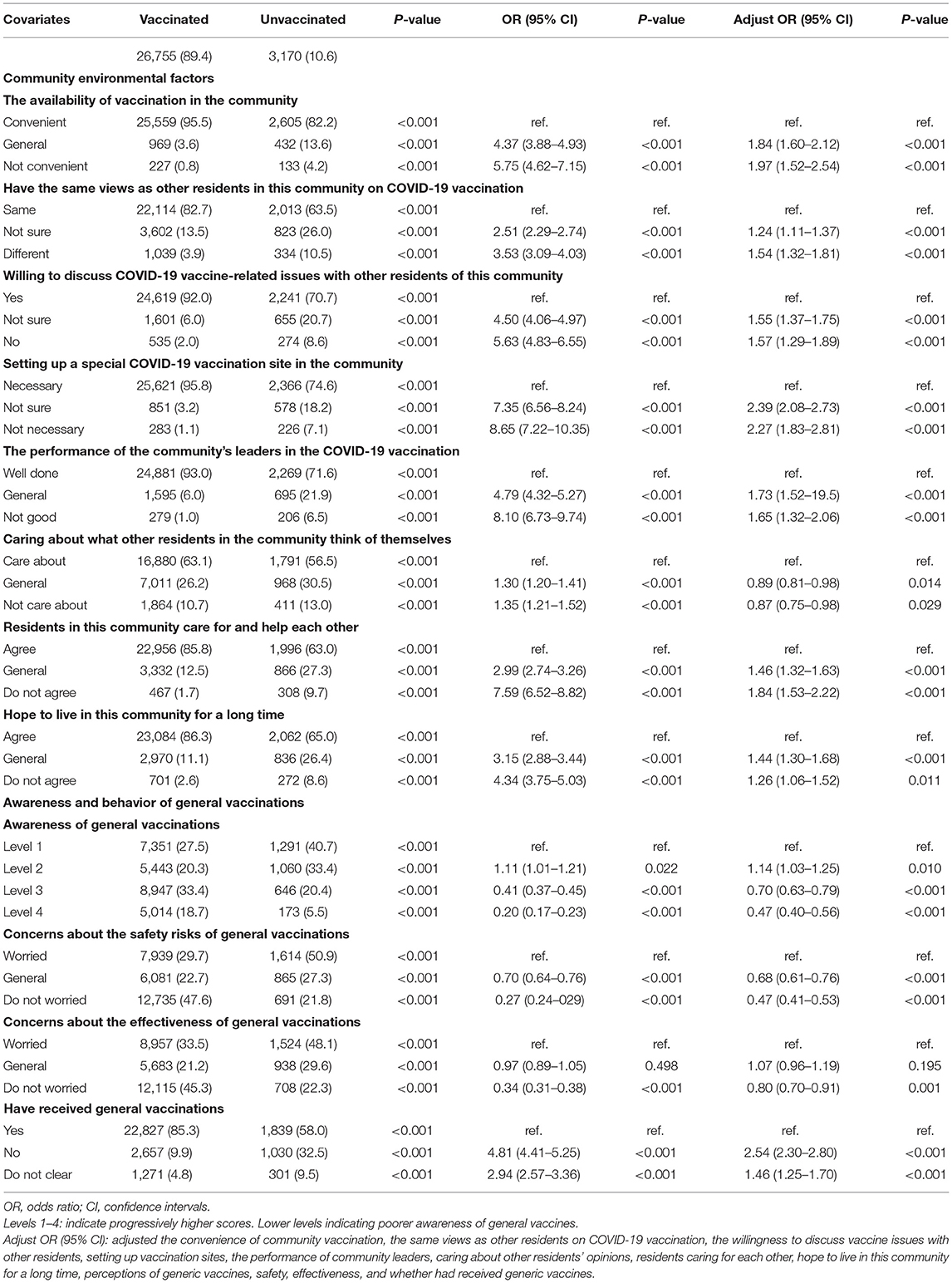
Additionally, as shown in Table 3, we discovered that contextual factors such as community environmental factors, vaccine perception and behavior influence COVID-19 vaccination uptake. The binary logistic regression model indicates that having easier access to vaccination, sharing similar views on COVID-19 vaccination with other residents, being willing to discuss vaccine issues with other residents, setting up vaccination sites, the good performance of community leaders, residents' concern for one another, hope to live in their community for a long time, and perceptions of generic vaccines, safety, and effectiveness are also independently associated with COVID-19 vaccination.
In addition, low level of coronavirus skepticism, COVID-19 vaccine skepticism and trust in healthcare system are also positively associated with COVID-19 vaccination. Detailed results are presented in Table 4.
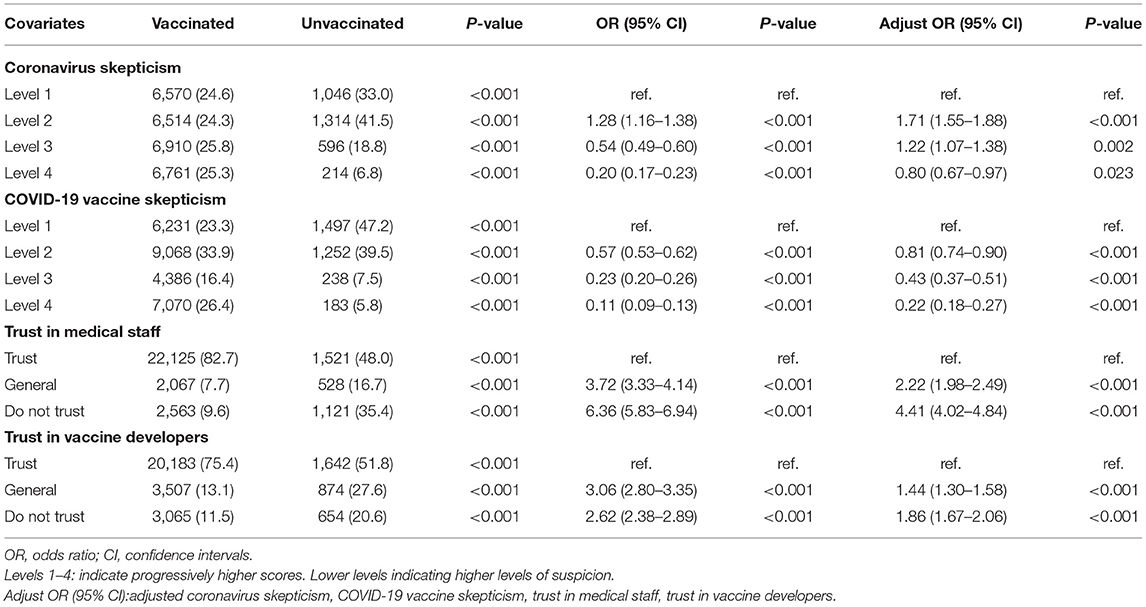
Table 4. Associations of coronavirus skepticism, COVID-19 vaccine skepticism, trust in healthcare system with COVID-19 vaccination coverage rate.
Analysis of the Reasons for Non-vaccination Against COVID-19
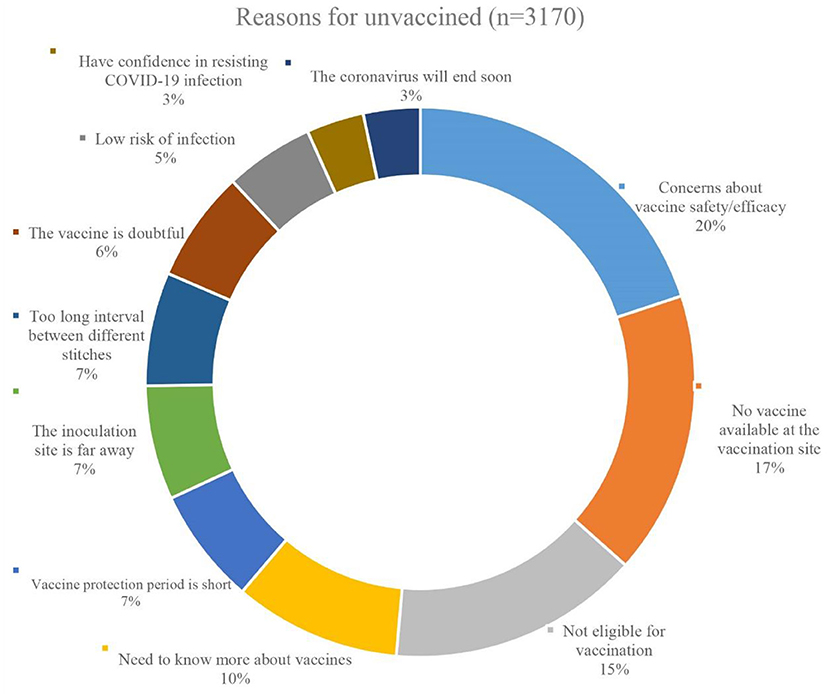
Three thousand one hundred and seventy participants were unvaccinated against COVID-19 out of a total of 29,925. As a result, we conducted research and analysis on the factors that contributed to this portion of the individuals being unvaccinated. As demonstrated in Figure 3, the most frequently cited reasons for non-vaccination were specific concerns about the COVID-19 vaccine's safety or effectiveness (20%), or a request for additional vaccine information (10%). 17% of those who were not vaccinated cited a lack of vaccine at the vaccination location, while 15% were not vaccinated owing to a medical condition that precluded them from obtaining COVID-19 vaccine. Figure 3 illustrates the remaining causes for non-vaccination.
Discussion
COVID-19 vaccination has emerged as a critical component of the global public health response to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic (11, 13, 25). As a result, the World Health Organization (WHO) is dedicated to urging countries worldwide to boost COVID-19 vaccine coverage and to collaborating on the development of an effective epidemic prevention and control mechanism (12, 17). China may be a world leader in COVID-19 vaccination coverage. This study examined COVID-19 vaccination in a large representative sample of 31 provinces in mainland China. As of August 4, 2021, the majority of participants (89.4%) had received COVID-19 vaccinations, while just a minority (10.6%) had not. This ratio is likely to stay high throughout the impending COVID-19 vaccination booster, although further investigation and confirmation are necessary. The high COVID-19 vaccination rate in China mainland may be attributable to the following factors: First, China has formulated a vaccine management law and successfully passed the WHO evaluation of its National Vaccine Management System (NRS) which guarantees the quality and supply of vaccines (26, 27). Second, the Chinese government has continued to increase post-marketing surveillance of vaccinations, placing a priority on vaccine safety and effectiveness, and has a continuous track record of vaccine-preventable diseases and public acceptance of vaccines. Additionally, vaccination usage experience and big data on vaccines are being developed and tracked (28). Third, China has strengthened the risk communication, increased publicity to inform recipients as well as the public about the benefits and risks of vaccination, and actively promoted the scientific premise that the overall benefits of vaccines outweigh the risks. Finally, China is committed to expanding the availability of vaccines by setting up temporary vaccination sites according to the characteristics of the jurisdiction and population, which greatly facilitates the vaccination of residents.
The global outbreak of the epidemic will lead to an increase in the demand of people for COVID-19 vaccine, which will in turn increase its vaccination rate (1, 29, 30). Table 2 indicates that people's awareness of COVID-19 had an obvious effect on vaccination rate. The global epidemic outbreak, the evolution of the epidemic situation in one's area of residency, and the risk of infection with COVID-19 all contribute to the vaccination rate. At present, some parts of mainland China including Nanjing, Zhengzhou, and other places, are experiencing point-like outbreaks and the recurrence of the epidemic, a situation that encourage people to take COVID-19 vaccine. Similarly, we discovered that individuals' perceptions of the COVID-19 vaccine have an effect on vaccination uptake. The belief in the efficacy of vaccines and the necessity for universal vaccination promotes COVID-19 vaccination, which is consistent with earlier research (4, 13, 16). These findings underscore the critical importance of public education regarding the COVID-19 vaccine, which has demonstrated the potential to be exceedingly effective.
Certain background information had a minor but significant effect on the COVID-19 vaccination rate, which was also unaccounted for in previous studies. The results demonstrate that convenience to vaccination, having similar views as other residents on COVID-19 vaccination, being willing to discuss about COVID-19 vaccine-related issues with other residents, set up a special COVID-19 vaccination site, the outstanding administrative performance of community leaders, residents care for each other, and having plans to live in their respective community for an extended period of time contributed to COVID-19 vaccination uptake. This indicates that effective management at the grassroots level may make a significant contribution to the development of an epidemic prevention and control system. At the same time, attitudes and behaviors toward vaccines in general affect COVID-19 vaccination uptake. General vaccines have long been considered important preventive measures against certain diseases (1, 31, 32), and COVID-19 vaccine has been used for <2 years since it was developed. People's perception of vaccines in general may greatly impact their vaccination uptake. The findings in Table 3 indicate that the more accurate one's understanding of vaccinations is, the less concerned one is about their safety and effectiveness, and the higher the vaccination uptake. This is consistent with previous studies in the UK and Turkey and other countries (16, 23).
People's decisions on whether or not to get the COVID-19 vaccine will be influenced by their level of skepticism. Previous research in the United Kingdom and Italy found that skepticism about the epidemic and the COVID-19 vaccine can cause people to delay or refuse to receive the vaccine (4, 21, 33). Additionally, we discovered that there is a high level of skepticism regarding the epidemic or the vaccine, resulting in a very low vaccination rate. Detailed results are presented in Table 4. In our research, mainland Chinese residents were generally less skeptical about the epidemic and COVID-19 vaccine. Detailed results are shown in Annexes 3, 4.
We also found that there is a considerable link between distrust among doctors and vaccine developers when it comes to COVID-19 vaccination. Ultimately, the willingness to be vaccinated is a matter of trust that the vaccine is necessary, it will work, and it is safe (16, 28). Public trust in healthcare professionals and vaccine developers has declined significantly as a result of occasional vaccine-related adverse events and growing instances of counterfeit vaccines (34). Therefore, this is a reminder that we need to build confidence in vaccines. On the one hand, vaccination service institutions should increase the number of vaccination medical staff and enhance the quality of vaccination service evaluation; on the other hand, we should accelerate the development of the vaccine industry's credit system, encourage enterprises to take the lead in vaccine production and distribution, and ensure the quality and safety of vaccine products.
The current study also investigated the reasons why participants were not vaccinated against COVID-19 (n = 3,170). In addition to personal ineligibility for vaccination (15%) and temporary lack of vaccine supply at the vaccination site (17%), 20% of unvaccinated participants were concerned about the safety or efficacy of the vaccine while 10% of them wanted more information about the vaccine before making their decision. This shows that the main reason for individuals not receiving COVID-19 vaccination is still uncertainty regarding the vaccine's safety and efficacy, which is consistent with findings from previous studies in Russia and other countries (35–37). Therefore, in the subsequent explanatory work, we must emphasize the importance of the prosocial benefits of the COVID-19 vaccine, as well as the necessity of being transparent about the data on the safety and efficacy in order to further dispel people's doubts about the COVID-19 vaccine and improve the vaccination rate. This may aid in raising the willingness to uptake the vaccine.
This is the first survey to examine the current state of COVID-19 vaccination among Chinese residents throughout 31 provinces on the Chinese mainland. From a broader viewpoint, this article examines the factors that contribute to the current COVID-19 vaccine coverage rate. Prior research concentrated primarily on special groups, biosafety technologies, and vaccination willingness, whereas our research delved deeper into community environmental factors, epidemic/vaccine perception, epidemic/vaccine skepticism, and trust on vaccine developers, among other factors. However, there are limitations to the survey that need to be addressed. Our study's shortcomings include its cross-sectional design, which precluded the establishment of a cause-and-effect relationship. Some potential confounding factors may have impacted the robustness of our results, such as vaccine's adverse reactions. Moreover, despite the fact that we used data from a large sample of the population drawn from 31 provinces, due to the epidemic, we were compelled to collect data via online questionnaires using the snowball sampling technique. Therefore, these research findings may differ from those estimated using probability sampling. Additionally, the factors influencing COVID-19 vaccine uptake found in the current study may be different for individuals without Internet access. In future, we intend to conduct a larger survey with a more representative sample, using detailed in-home interviews to continuously track and assess the changes and causes of COVID-19 vaccination rate, as well as conducting intervention studies in a small area to infer causal associations between specific factors and COVID-19 vaccination rate.
Conclusions
Thirty-one provinces in mainland China currently have a relatively high rate of COVID-19 vaccination. To further increase the rate of COVID-19 vaccination, we need to remove barriers associated with the community context and enhance the accessibility of COVID-19 vaccine services. Additionally, by taking proactive and effective actions to address the reasons for non-vaccination against COVID-19, the construction of an epidemic prevention and control system will be considerably facilitated.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethics study protocol and online survey were approved by the Life Science Ethics Review Committee of the Zhengzhou University.
Author Contributions
YM, JW, MM, MW, and JG: conceptualization. YM, BY, MM, QL, and WW: data curation. XF, JW, QL, and YM: formal analysis. MW and JG: funding acquisition. JW, YM, BY, MM, QL, LZ, and ZM: investigation. JW, YM, MM, and CT: methodology. JW and XF: project administration. JW, YM, and XF: resources. MM, LZ, and ZM: software. MM and JW: writing—original draft. YM, QL, CT, MW, and JG: writing—review editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Social Science Fund of China (No. 21BGL222), the Collaborative Innovation Key Project of Zhengzhou (No. 20XTZX05015), 2021 Postgraduate Education Reform and Quality Improvement Project of Henan Province (No. YJS2021KC07), Zhengzhou University 2020 Key Project of Discipline Construction (No. XKZDQY202007), the Performance Evaluation of New Basic Public Health Service Projects in Henan Province (No. 2020130B) and Teaching Reform Project of Zhengzhou University (No. 2021-153).
Author Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the government agencies and NGOs.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank all participants for their involvement.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.796467/full#supplementary-material
References
1. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. (2020) 173:964–73. doi: 10.7326/M20-3569
2. World Health Organization. Weekly Epidemiological Update on COVID-19 - 3 August 2021. (2021). Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-−3-august-2021 (accessed September 10, 2021).
3. National Health Commission PRC. The Latest Situation of the COVID-19 Coronavirus Pneumonia Epidemic as of August 4. (2021). Available online at: http://www.nhc.gov.cn/xcs/yqtb/202108/7df2b123c2b74683a43afa906b9e3839.shtml (accessed September 10, 2021).
4. Freeman D, Loe BS, Chadwick A, Vaccari C, Waite F, Rosebrock L, et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. (2020) 12:1–15. doi: 10.1017/S0033291720005188
5. Jian W, Quan L, Clifford ST, Mei W, Jian G, Wei w, et al. COVID-19 vaccine hesitancy among Chinese Population: a Large-Scale National Study. Front Immunol. (2021) 12:781161. doi: 10.3389/fimmu.2021.781161
6. Bundgaard H, Bundgaard JS, Raaschou-Pedersen D, von Buchwald C, Todsen T, Norsk JB, et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in danish mask wearers: a randomized controlled trial. Ann Intern Med. (2021) 174:335–43. doi: 10.7326/M20-6817
7. Martinelli L, Kopilaš V, Vidmar M, Heavin C, Machado H, Todorović Z, et al. Face masks during the COVID-19 pandemic: a simple protection tool with many meanings. Front Public Health. (2021) 8:606635. doi: 10.3389/fpubh.2020.606635
8. Kucharski AJ, Klepac P, Conlan AJK, Kissler SM, Tang ML, Fry H, et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis. (2020) 20:1151–60. doi: 10.1016/S1473-3099(20)30457-6
9. Abbas K, Procter SR, van Zandvoort K, Clark A, Funk S, Mengistu T, et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health. (2020) 8:e1264–72. doi: 10.1016/S2214-109X(20)30308-9
10. Benn CS, Fisker AB, Rieckmann A, Sørup S, Aaby P. Vaccinology: time to change the paradigm?. Lancet Infect Dis. (2020) 20:e274–83. doi: 10.1016/S1473-3099(19)30742-X
11. Jentsch PC, Anand M, Bauch CT. Prioritising COVID-19 vaccination in changing social and epidemiological landscapes: a mathematical modelling study. Lancet Infect Dis. (2021) 21:1097–106. doi: 10.1016/S1473-3099(21)00057-8
12. Schaffer DeRoo S, Pudalov NJ, Fu LY. Planning for a COVID-19 vaccination program. JAMA. (2020) 323:2458–9. doi: 10.1001/jama.2020.8711
13. Begum J, Mir NA, Dev K, Buyamayum B, Wani MY, Raza M. Challenges and prospects of COVID-19 vaccine development based on the progress made in SARS and MERS vaccine development. Transbound Emerg Dis. (2021) 68:1111–24. doi: 10.1111/tbed.13804
14. Cyranoski D. What China's speedy COVID vaccine deployment means for the pandemic. Nature. (2020) 586:343–4. doi: 10.1038/d41586-020-02807-2
15. Oliver SE, Gargano JW, Marin M, Wallace M, Curran KG, Chamberland M, et al. The advisory committee on immunization practices' interim recommendation for use of Pfizer-BioNTech COVID-19 Vaccine-United States, December 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1922–4. doi: 10.15585/mmwr.mm6950e2
16. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. (2021) 384:403–16. doi: 10.1056/NEJMoa2035389
17. World Health Organization. Remarks by the Director-General of WHO at the Media Briefing on the COVID-19 Outbreak on August 4, 2021. (2021). Available online at: https://www.who.int/zh/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-4-august-2021 (accessed September 10, 2021).
18. National Health Commission PRC. COVID-19 Vaccination Status. (2021). Available online at: http://www.nhc.gov.cn/jkj/s7915/202108/39679e47dbb849e386f64247fd241082.shtml (accessed September 16, 2021).
19. Anand U, Jakhmola S, Indari O, Jha HC, Chen ZS, Tripathi V, et al. Potential therapeutic targets and vaccine development for SARS-CoV-2/COVID-19 pandemic management: a review on the recent update. Front Immunol. (2021) 12:658519. doi: 10.3389/fimmu.2021.658519
20. Yan Y, Pang Y, Lyu Z, Wang R, Wu X, You C, et al. The COVID-19 vaccines: recent development, challenges and prospects. Vaccines. (2021) 9:349. doi: 10.3390/vaccines9040349
21. Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. (2021) 12:29. doi: 10.1038/s41467-020-20226-9
22. Salali GD, Uysal MS. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol Med. (2020) 10:1–3. doi: 10.1017/S0033291720004067
23. Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med. (2020) 383:2603–15. doi: 10.1056/NEJMoa2034577
24. Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. (2021) 397:99–111. doi: 10.1016/S0140-6736(20)32661-1
25. Wang W, Wu Q, Yang J, Dong K, Chen X, Bai X, et al. Global, regional, and national estimates of target population sizes for COVID-19 vaccination: descriptive study. BMJ. (2020) 371:m4704. doi: 10.1136/bmj.m4704
26. The National People's Congress of the People's Republic of China (2019). Available online at: http://www.npc.gov.cn/npc/c30834/201907/11447c85e05840b9b12c62b5b645fe9d.shtml (accessed September 10, 2021).
27. WHO (2021). Available online at: https://extranet.who.int/pqweb/sites/default/files/documents/Status_COVID_VAX_20Jan2021_v2.pdf. (accessed September 16, 2021).
28. Su S, Du L, Jiang S. Learning from the past: development of safe and effective COVID-19 vaccines. Nat Rev Microbiol. (2021) 19:211–9. doi: 10.1038/s41579-020-00462-y
29. Hurley LP, Bridges CB, Harpaz R, Allison MA, O'Leary ST, Crane LA, et al. U.S. physicians' perspective of adult vaccine delivery. Ann Intern Med. (2014) 160:161. doi: 10.7326/M13-2332
30. Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. (2020) 38:7789–98. doi: 10.1016/j.vaccine.2020.10.027
31. Freeman D, Lambe S, Yu LM, Freeman J, Chadwick A, Vaccari C, et al. Injection fears and COVID-19 vaccine hesitancy. Psychol Med. (2021) 7:1–11. doi: 10.1017/S0033291721002609
32. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated?. Vaccine. (2020) 38:6500–7. doi: 10.1016/j.vaccine.2020.08.043
33. Palamenghi L, Barello S, Boccia S, Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. (2020) 35:785–8. doi: 10.1007/s10654-020-00675-8
34. Du F, Chantler T, Francis MR, Sun FY, Zhang X, Han K, et al. The determinants of vaccine hesitancy in China: a cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. (2020) 38:7464–71. doi: 10.1016/j.vaccine.2020.09.075
35. Logunov DY, Dolzhikova IV, Tukhvatullin AI, Shcheblyakov DV. Safety and efficacy of the Russian COVID-19 vaccine: more information needed - authors' reply. Lancet. (2020) 396:e54–5. doi: 10.1016/S0140-6736(20)31970-X
36. Hodgson SH, Mansatta K, Mallett G, Harris V, Emary KRW, Pollard AJ. What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical efficacy of vaccines against SARS-CoV-2. Lancet Infect Dis. (2021) 21:e26–35. doi: 10.1016/S1473-3099(20)30773-8
Keywords: COVID-19, COVID-19 vaccine, vaccination, COVID-19 vaccination rate, China
Citation: Wu J, Ma M, Miao Y, Ye B, Li Q, Tarimo CS, Wang M, Gu J, Wei W, Zhao L, Mu Z and Fu X (2022) COVID-19 Vaccination Acceptance Among Chinese Population and Its Implications for the Pandemic: A National Cross-Sectional Study. Front. Public Health 10:796467. doi: 10.3389/fpubh.2022.796467
Received: 16 October 2021; Accepted: 14 January 2022;
Published: 08 February 2022.
Edited by:
Bronwyne Coetzee, Stellenbosch University, South AfricaReviewed by:
Angela Stufano, University of Bari Aldo Moro, ItalyLi Li, Southern Medical University, China
Copyright © 2022 Wu, Ma, Miao, Ye, Li, Tarimo, Wang, Gu, Wei, Zhao, Mu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoli Fu, eGxmdTY2QDEyNi5jb20=
 Jian Wu
Jian Wu Mingze Ma
Mingze Ma Yudong Miao
Yudong Miao Beizhu Ye1
Beizhu Ye1 Clifford Silver Tarimo
Clifford Silver Tarimo Meiyun Wang
Meiyun Wang Jianqin Gu
Jianqin Gu Wei Wei
Wei Wei Lipei Zhao
Lipei Zhao Zihan Mu
Zihan Mu