- 1Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA, United States
- 2DotHouse Health, Dorchester, MA, United States
- 3Caring Health Center, Springfield, MA, United States
- 4Lynn Community Health Center, Lynn, MA, United States
Introduction: Access to COVID-19 testing has been inequitable and misaligned with community need. However, community health centers have played a critical role in addressing the COVID-19 testing needs of historically disadvantaged communities. The aim of this paper is to explore the perceptions of COVID-19 testing barriers in six Massachusetts communities that are predominantly low income and describe how these findings were used to build tailored clinical-community strategies to addressing testing inequities.
Methods: Between November 2020 and February 2021, we conducted 84 semi-structured qualitative interviews with 107 community health center staff, community partners, and residents. Resident interviews were conducted in English, Spanish, Vietnamese, and Arabic. We used a 2-phase framework analysis to analyze the data, including deductive coding to facilitate rapid analysis for action and an in-depth thematic analysis applying the Social Ecological Model.
Results: Through the rapid needs assessment, we developed cross-site suggestions to improve testing implementation and communications, as well as community-specific recommendations (e.g., locations for mobile testing sites and local communication channels). Upstream barriers identified in the thematic analysis included accessibility of state-run testing sites, weak social safety nets, and lack of testing supplies and staffing that contributed to long wait times. These factors hindered residents' abilities to get tested, which was further exacerbated by individual fears surrounding the testing process and limited knowledge on testing availability.
Discussion: Our rapid, qualitative approach created the foundation for implementing strategies that reached underserved populations at the peak of the COVID-19 pandemic in winter 2021. We explored perceptions of testing barriers and created actionable summaries within 1–2 months of data collection. Partnering community health centers in Massachusetts were able to use these data to respond to the local needs of each community. This study underscores the substantial impact of upstream, structural disparities on the individual experience of COVID-19 and demonstrates the utility of shifting from a typical years' long research translation process to a rapid approach of using data for action.
Introduction
Since the detection of the first COVID-19 case in the U.S. in January 2020, the country has surpassed over 50 million COVID-19 infections and more than 800,000 deaths (1). Higher social vulnerability has been associated with higher COVID-19 case fatality rates (2). National and state level data indicate that the COVID-19 pandemic has disproportionately affected Black and Latinx populations in the U.S., with these groups experiencing higher rates of infection, hospitalization, and mortality (3, 4)1. Black populations have had up to 3.5 times the risk for infection compared to White populations, and Black and Latinx populations have had three times the risk of mortality from COVID-19 compared to white populations (5). Inequities in COVID-19 infections and deaths have also been identified in Native American, Asian American, and Pacific Islander populations. Additionally, U.S. counties with more immigrants have also been found to have more COVID-19 cases (6).
These patterns highlight how structural racism, defined as “the totality of ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care, and criminal justice” (7), perpetuates health inequities in many communities of color (7–9). In particular, these disparities are reflective of the social determinants of health and comorbidity rates that further affect the level of burden of COVID-19 in these populations (10). Communities with poorer housing conditions (e.g., overcrowded, high housing cost burden) are at higher risk for COVID-19, in part due to their inability to isolate (11). Additionally, racial/ethnic minorities are over-represented in essential jobs that increase exposure to the virus (12, 13). Furthermore, poor treatment by healthcare institutions and the government, both in the past and currently, has negatively impacted trust with communities of color and subsequently affected adherence to COVID-19 public health recommendations (14). Unsurprisingly, the highest COVID-19 death rates in Massachusetts have been observed among those living in the most disadvantaged areas based on zip code tabulation area data (i.e., poverty level, household crowding, percentage population of color, and racialized economic segregation) (15). For these populations, recommended prevention and mitigation strategies such as social distancing are often not feasible.
The inequitable patterns of COVID-19 disease burden have highlighted the urgent need for improved testing, surveillance and monitoring, data transparency, and targeting of public health interventions to the circumstances in which people live, work, play, and pray. In particular, access to testing in underserved communities is imperative for combatting the COVID-19 virus. Yet, throughout the pandemic, testing access has often been inequitable and not aligned with community need. Communities of color and low-income communities have had less access to testing, and as a result have had lower testing rates. Studies in both New York City and Massachusetts indicate that COVID-19 testing has been much more accessible in neighborhoods that are more affluent and with larger White populations, even though COVID-19 exposure as well as the proportion of positive tests has often been higher in more racially diverse neighborhoods and areas with lower socioeconomic status (16, 17).
Prior studies have explored residents' perceived barriers to both coping with COVID-19 and COVID-19 testing. Barriers to testing identified include lack of access to testing, confusion about testing guidelines and eligibility, social stigma and concerns about the consequences of testing positive, cost of testing, logistics including transportation to testing sites, and fear and mistrust (18, 19). In order to address these barriers, public health and healthcare institutions have partnered with community-based organizations (e.g., churches, schools) and community health centers to increase COVID-19 testing and COVID-19 communications in under-resourced communities (20–23).
Community health centers (CHCs), “community-based and patient-directed organizations that deliver comprehensive, culturally competent, high-quality primary care services…regardless of patient's ability to pay” (24)2, have been on the front lines of the pandemic. CHCs disproportionately serve low-income populations (91% of patients) and people of color (over 60% of patients) (25). Early in the pandemic, CHCs were facing significant financial loss due to the drop-off in primary care visits, while at the same time they took on the challenge of scaling up public testing. For a variety of reasons, most private primary care providers did not engage in testing, and testing was largely provided by CHCs and governmental agencies. Nationally, ninety percent of CHCs have been providing COVID-19 testing and over half (57%) of people tested at these sites are people of color (25)3. The Commonwealth of Massachusetts also rolled out a free “Stop the Spread” testing program in July 2020 with mass testing sites across the state (26). At the peak of the pandemic, the statewide initiative included over 35 sites (26); however, as of the end of 2021, the program continues at 10 sites across the state (27)4. There is limited research linking barriers to COVID-19 testing with solutions, particularly the role of CHC partnerships to address these challenges. Additionally, there is limited research on the unique barriers to testing faced by people with limited English proficiency and immigrant populations in the U.S.
Given the widespread need for COVID-19 testing support, following Congress-approved funding in April 2020, the National Institutes of Health (NIH) created the Rapid Acceleration of Diagnostics (RADx) program. The aim of the RADx program is to develop innovative diagnostic technologies and strategies to increase testing access. One of the four RADx programs is Rapid Acceleration of COVID-19 Testing in Underrepresented Populations (RADx-UP), which aims to understand factors that have led to the disproportionate burden of the pandemic on underserved populations and to support improved access and uptake of COVID-19 testing through community-engaged efforts (28).
The RADx-UP program funded our project in Massachusetts (RADx-MA), one of over 70 RADx-UP projects throughout the U.S. This project is led by a collaboration between the Harvard T.H. Chan School of Public Health, Massachusetts General Hospital, and the Massachusetts League of Community Health Centers and is supported through the infrastructure of the Implementation Science Center for Cancer Control Equity (ISCCCE). It builds on existing and new partnerships between CHCs and community organizations in six Massachusetts COVID-19 hotspot communities with both high rates of illness and racial/ethnic gaps. The aim of this project is to work with the CHC-community partnerships to develop expanded testing implementation strategies and to conduct a series of community-engaged pilot studies to assess the impact of different approaches to addressing barriers to testing. To prepare for the planned work supporting implementation of testing strategies to reach underserved populations, we conducted a rapid, comprehensive needs assessment with stakeholders at multiple levels. In this paper, we explore the perceptions of COVID-19 testing barriers among community health center staff, community partners, and residents gathered through this rapid needs assessment. We also describe how these community-identified needs and assets can be translated to build tailored clinical-community strategies for addressing testing inequities.
Materials and Methods
Qualitative Interview Design, Recruitment, and Consent
This needs assessment utilized 30-min qualitative semi-structured interviews to gather a broad range of perspectives across six Massachusetts communities. First, in November 2020, the lead author conducted interviews with staff members at nine participating community health centers. Next, from November 2020 to February 2021, the lead author and two research assistants used a snowball sampling approach to conduct interviews with staff and volunteers from organizations the health center staff identified as current or future partners in COVID-19 testing. Types of organizations interviewed included community coalitions, local boards of health, housing authorities and shelters, food banks, and immigrant advocacy groups. Finally, from December 2020 to February 2021, four additional research assistants conducted resident interviews in English, Spanish, Vietnamese, and Arabic, reflecting primary languages in the participating communities. Separate interview guides (see Appendix A) for staff, partners, and residents were developed with parallel questions to capture actionable feedback to inform changes to testing practices and communications. Study staff worked with health center and partner organization staff to recruit a convenience sample of community residents for interviews, distributing recruitment flyers in four languages through newsletters, social media, and via online community meetings. Residents contacted study staff by phone or email to learn about the study activities, risks and benefits, and to schedule the interview. Verbal consent detailing the study purpose, logistics, and confidentiality was obtained prior to the start of each interview and a written consent script was also distributed to participants via email or text. The study was approved by the Harvard Longwood Campus Institutional Review Board.
Qualitative Interview Procedures
All interviews were conducted using semi-structured interview guides with parallel questions for each audience about the experience of COVID-19 testing in their community, perceived barriers to testing, communication and education needs, perspectives on mobile and rapid testing strategies, and local successes. Community health center staff and partners were also asked about strategies for partnership to improve access to, utilization of, and communication about testing. Individuals were compensated $25 for participation in interviews. Interviews were conducted over Zoom, recorded, and transcribed verbatim. Prior to analysis, transcripts of interviews conducted in Spanish, Vietnamese, and Arabic were translated into English by the bilingual research assistants who conducted the interviews.
Qualitative Analysis
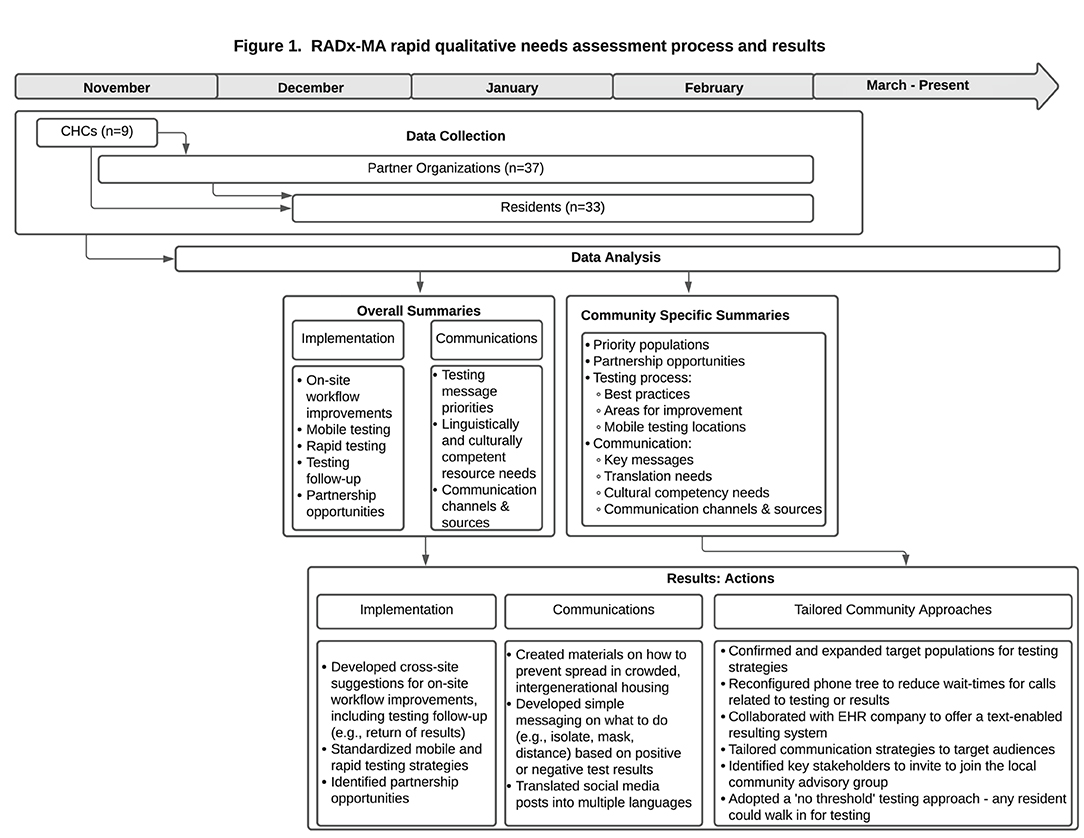
We conducted a 2-phase framework analysis (29) to facilitate rapid return of results (30, 31) and utilization of data for action (Figure 1). First, two coders (SA and VH) categorized and summarized content from health center and partner interviews to share with the RADx project testing implementation team and communication team in January 2021. In March 2021, community-specific summaries from health center, partner, and resident interviews were developed for local action.
In the second phase, the research team conducted an in-depth thematic analysis, deductively coding interviews into the five levels of the Social-Ecological Model (policy and environmental; community; organizational; interpersonal; individual) (32) according to the framing described by the interviewees and into three pre-figured codes drawn from the interview guide (testing process, communications, and partnerships). This was followed by inductive coding to develop constructs and sub-constructs within these five levels. This framework was selected to emphasize the multilevel influences on COVID-19 testing experience. A codebook was developed and shared with other members of the research team to gather feedback and define agreed upon constructs. The same coders proceeded to double-code 16 interviews, reconciling codes, and revising the codebook in consultation with the senior author as appropriate. The remaining transcripts were single coded, divided between the two coders. Analyses were conducted using NVivo qualitative data analysis software Version 11 and then summarized and condensed into salient themes.
Results
Findings from the qualitative analysis are organized by phase. The Phase 1 action-oriented qualitative process and results are presented in Figure 1. The Phase 2 thematic analysis is organized by theme within the five levels of the Social Ecological Model (32), starting with the societal level to emphasize the structural determinants described by participants (see Figure 2; Tables 1–5). Similar themes were often identified among health center staff, partners, and residents. However, when discordant views emerged between groups, a detailed description of these differing perspectives is provided. Exemplar quotes within each theme are also displayed in tables by role. A total of 107 individuals - community health center staff (n = 12), partners (n = 57) and residents (n = 38) - across 84 interviews, participated in the interviews and are included in both phases of the results.
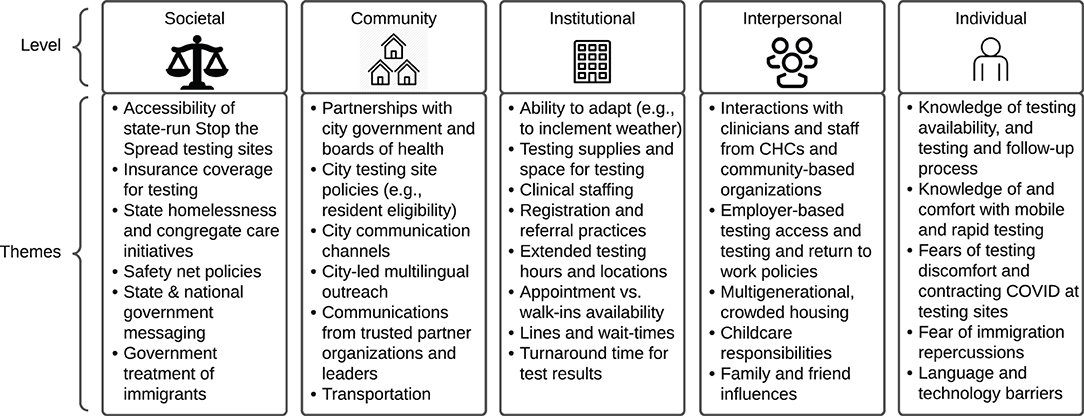
Figure 2. COVID-19 testing barriers & facilitators themes organized by the social ecological framework.
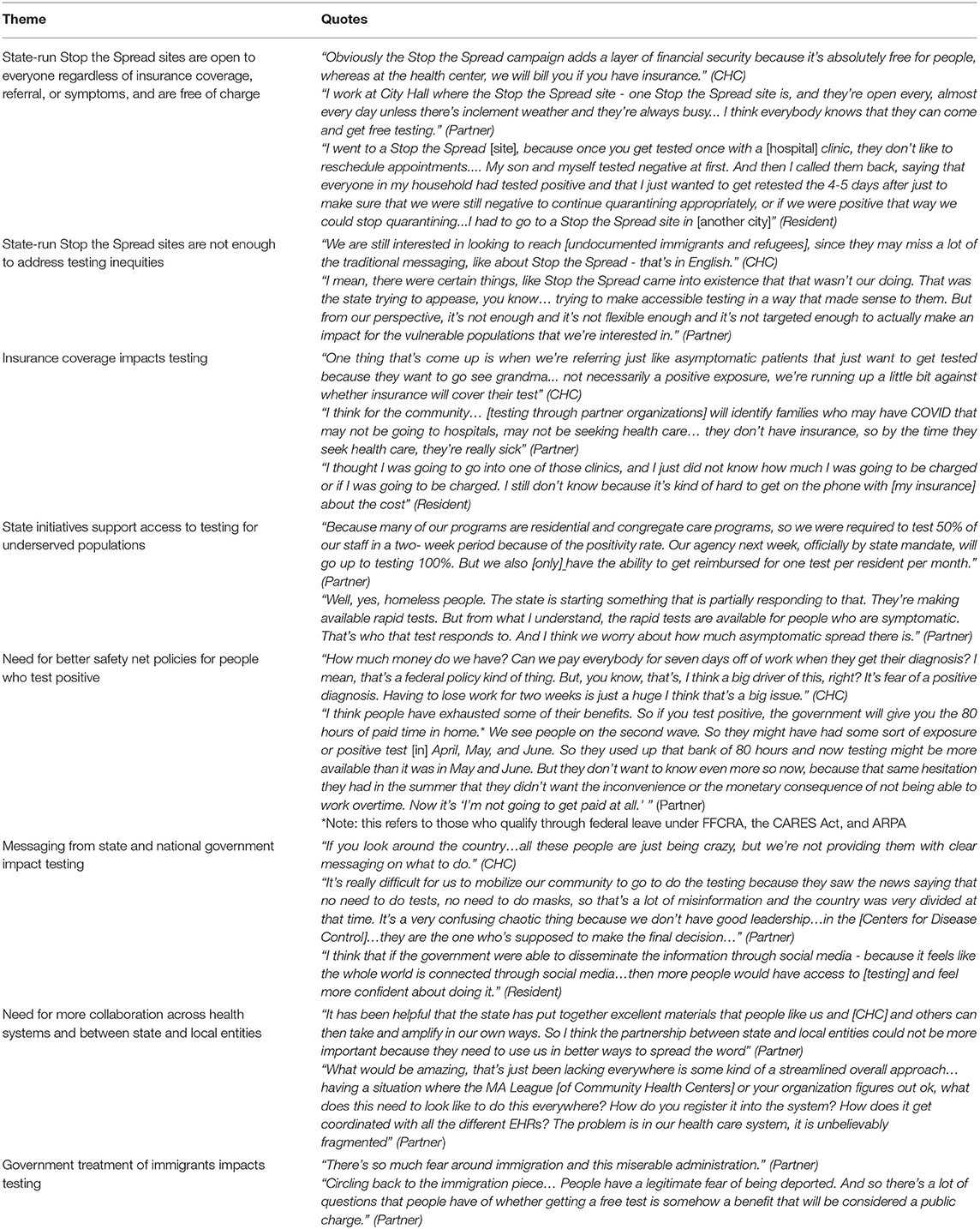
Table 1. Societal factors influencing COVID-19 testing reported by community health center staff, partners, and residents.
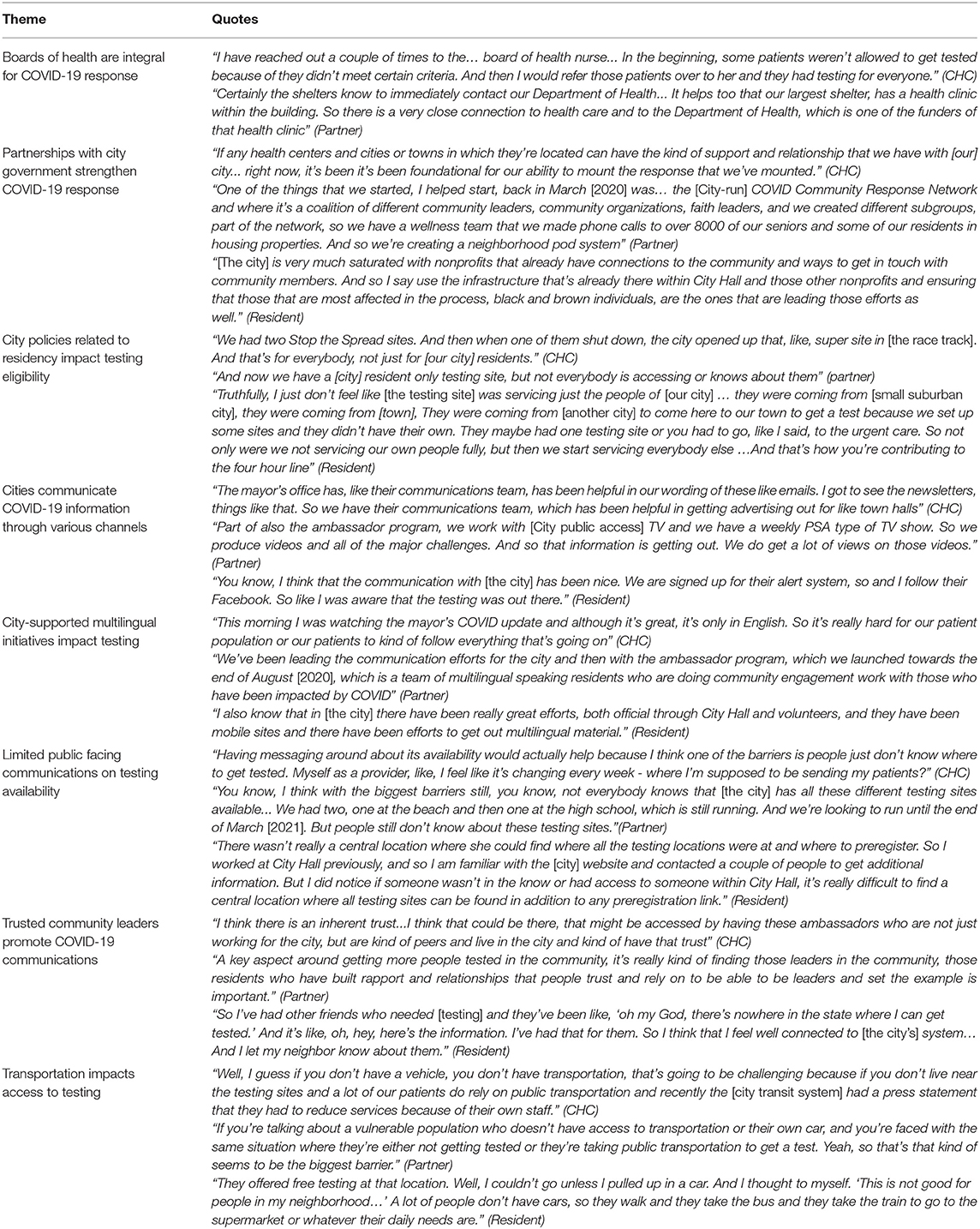
Table 2. Community factors influencing COVID-19 testing reported by community health center staff, partners, and residents.
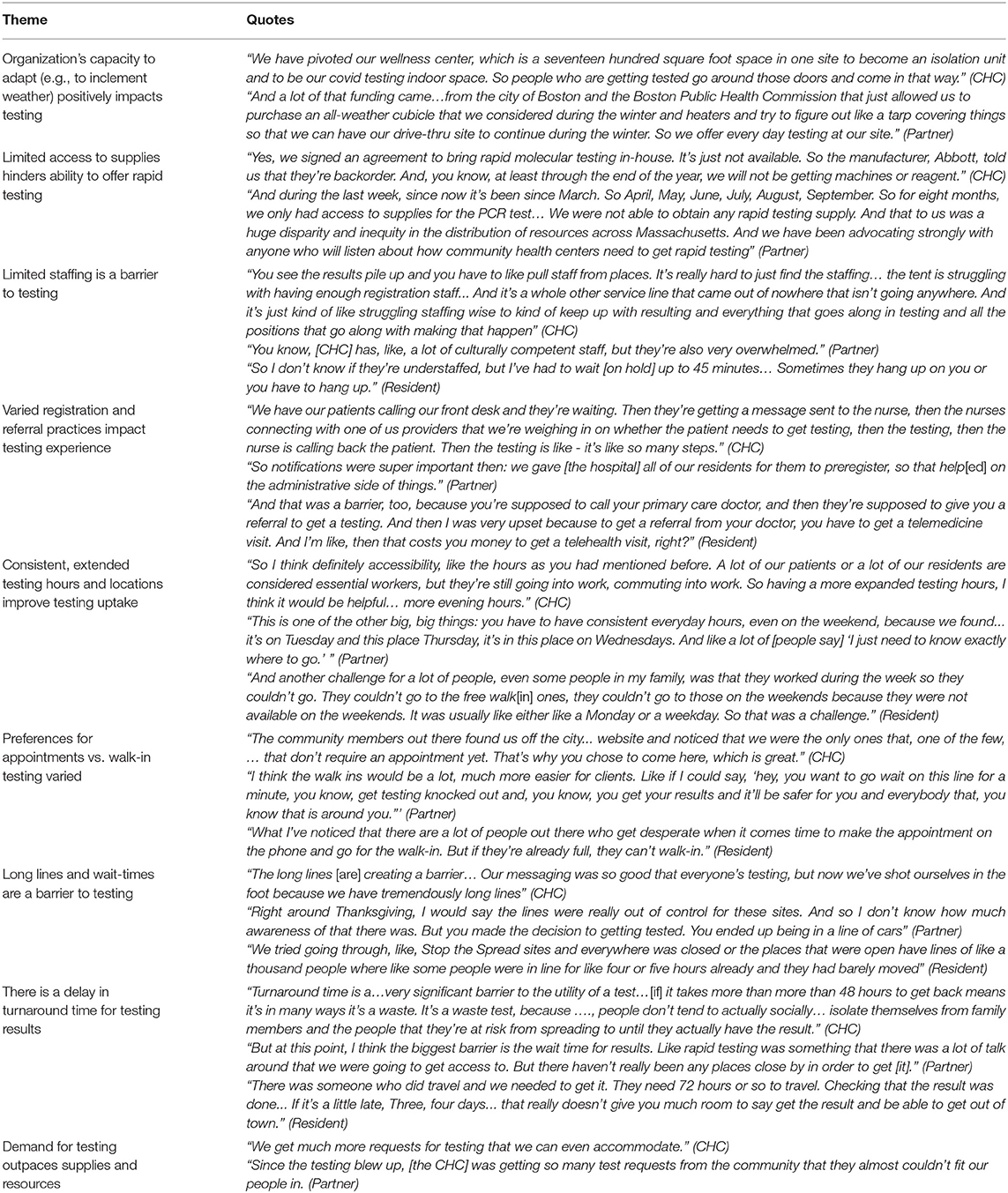
Table 3. Institutional and Organizational factors influencing COVID-19 testing reported by community health center staff, partners, and residents.
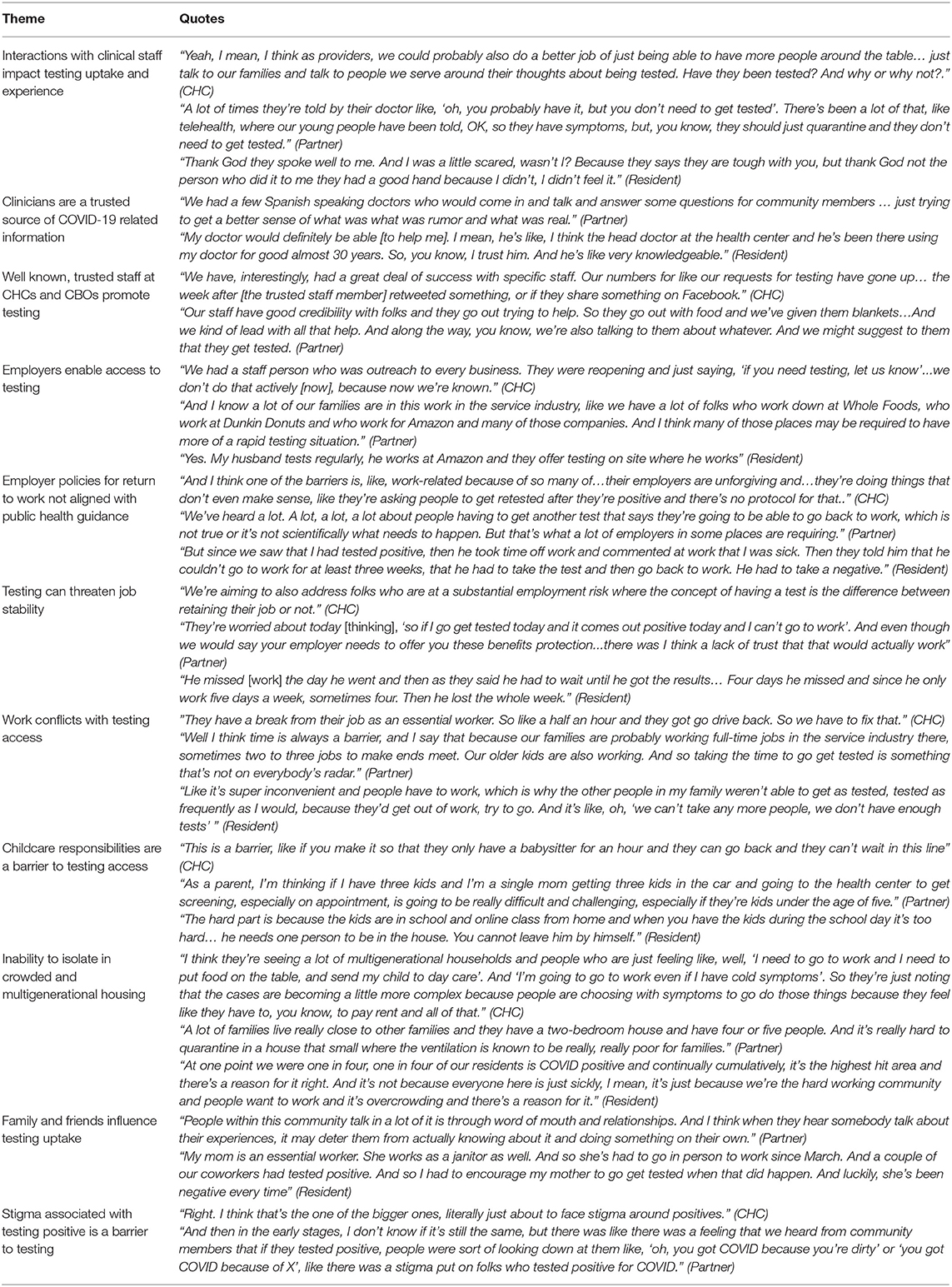
Table 4. Interpersonal factors influencing COVID-19 testing reported by community health center staff, partners, and residents.
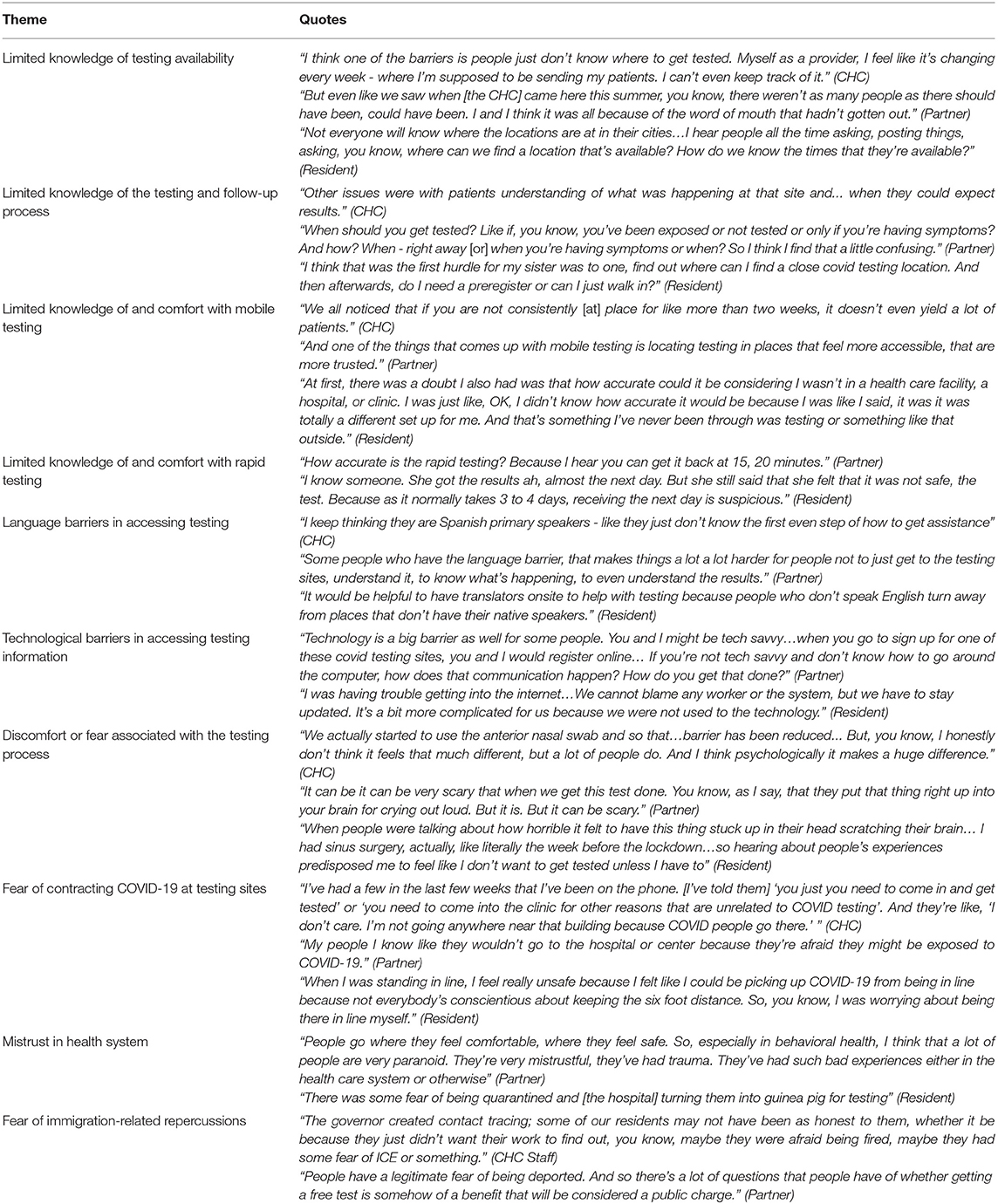
Table 5. Individual factors influencing COVID-19 testing reported by community health center staff, partners, and residents.
Phase 1—Data for Action
Figure 1 provides an overview of the data collection process and results from Phase 1. Codes related to implementation of testing by the CHCs were used to develop cross-site suggestions for on-site workflow improvements, mobile testing strategies, rapid testing strategies, testing follow-up (e.g., return of results) strategies, and partnership opportunities. Summaries of the suggested strategies were provided to study staff to work directly with the CHCs to rapidly implement changes to the testing process. Codes related to COVID-19 communications captured priorities for messaging (e.g., topics of confusion), linguistically and culturally competent resource needs, and suggestions for communication channels (e.g., fliers, social media) and sources (e.g., faith-based leaders). These communications summaries were provided to study staff specializing in communications to develop simple messages in multiple languages for CHCs to disseminate to patients and partners. Community-specific analyses captured updated priority populations and partnership opportunities, testing areas for improvement, specific mobile testing site recommendations, key messages for tailored communications, translation needs, and suggested local communication channels and sources. Examples of how data were used for local action include:
• Interview data was used to confirm and expand target populations for testing strategies. Segments of the population prioritized included culturally and linguistically diverse populations, individuals with disabilities, individuals experiencing housing insecurity and homelessness, as well as those living in multigenerational housing where isolating may not be feasible when exposed to the virus.
• Interview data from patients helped reveal an operational challenge in a CHC contact center. Residents reported long wait times when calling one CHC to inquire about testing or results. Using this information, the CHC reconfigured their phone tree to put COVID-19 testing and resulting as the first two prompts, which shortened the wait time for patients. Separating COVID-19 from non-COVID-19 calls early in the call process allowed the CHC to connect patients with the correct staff and reduce the time it takes to receive COVID-19 results or to make an appointment for COVID-19 testing.
• Patients' descriptions of challenges receiving timely results prompted the CHCs to address these challenges internally and externally. Another CHC worked with their electronic medical record systems to offer a text enabled resulting system. Another CHC successfully advocated directly with the test vendor to prioritize specimens given the high prevalence rate in its community.
• Interview data helped the CHCs tailor communication strategies to their target populations. Partner organizations suggested that one CHC employ different channels of communication to connect with members of the community. In response, the CHC hosted COVID-19 discussion sessions at local businesses, popular gathering spots, and places of worship. They also employed methods such as paper and virtual fliers, video postings on social media, as well as regular updates on the CHC website.
• Partner interview data was used to identify key external stakeholders to be invited to join the local community advisory group. One CHC included leadership from a local shelter in its community advisory group. The CHC also partnered with this shelter to host mobile COVID-19 testing and vaccination events to reach individuals experiencing homelessness.
• Interview data was used to better understand the need for mobile and static testing strategies and possible locations or frequency. These topics became the agenda content of the local community advisory group for one CHC early in the project.
• Interviews revealed that individual CHCs' testing eligibility criteria was confusing and difficult to navigate for patients. This moved a CHC to adopt a “no threshold” approach: any resident could walk in for testing, without an appointment, whether they were a CHC patient or not and whether they were symptomatic or not.
• Interviews revealed that the fear of being billed for a COVID-19 test, even for insured individuals, was an obstacle. One health center looked for other avenues to get paid for testing when a patient was uninsured or when their insurance denied payment. This included using grant funding or billing the state's uninsured portal.
Phase 2—Thematic Analysis
The major themes identified in this qualitative analysis are displayed in Figure 2. Tables 1–5 and narrative summaries below further explore these themes in greater depth with exemplar quotes from each stakeholder group (e.g., CHC staff, partners, residents) corresponding to the theme in each table.
Societal
CHC staff, partners, and residents across multiple communities described the state-run Stop the Spread mass vaccination sites as influential for accessing testing (33)5. These sites were open to everyone regardless of insurance coverage, referral, or symptom during the peak months of the pandemic and were free of charge. However, health center staff and partners expressed that these sites were not enough to address testing inequities and were particularly limited in terms of language accessibility. In addition to these public testing sites, partners described how separate state initiatives for congregate care settings and homeless shelters supported access to testing for underserved populations and the staff working in these settings. Another societal factor mentioned by all interviewee types was the impact of insurance coverage on testing—both lack of insurance and uncertainty in reimbursement were frequently mentioned as deterrents to seeking care. CHC staff and partners also discussed the need for better safety net policies for people who test positive to be able to take paid time off from work to stop the spread of the virus. Finally, many participants described how unclear messaging from state and national government hindered testing uptake, and partners emphasized that government mistreatment of immigrants (e.g., fears of Immigrant and Customs Enforcement) further exacerbated these challenges.
Community
CHC staff, partners, and residents described partnerships with city government as important to strengthening the COVID-19 response. City communications channels such as email newsletters, public access TV, and social media pages were described as important for disseminating COVID-19 education in multiple languages. However, public facing information about testing availability—locations and hours—was reportedly difficult to find. Stakeholders in cities where state mass vaccination sites were located also described how city policies related to residency impacted testing eligibility. Because state Stop the Spread sites were flooded with people from nearby cities and towns, those who lived in the city often struggled with access. Creating rules to limit city-run sites to local residents helped improve testing access. Transportation was another community level barrier to testing mentioned by CHC staff, partners, and residents—those without access to a vehicle could not access drive-thru testing sites and riding public transit to distant sites could increase risk of exposure. Finally, trusted community leaders—both individuals and community-based organizations—were described as important for promoting COVID-19 communication.
Organizational
Institutional and organizational factors influencing COVID-19 testing primarily focused on infrastructure of the CHCs. CHC staff and partners described the ability of the facilities to adapt their testing space as a facilitator for testing, particularly for inclement weather as the pandemic surged in the winter months. Barriers frequently mentioned were limited staffing, long lines and wait times, and delayed turnaround times for testing results. At the peak of the pandemic, the demand for testing also outpaced supplies such as machines and reagent to perform rapid testing. Interview participants reported varied experiences with registration and referral practices that impacted the likelihood of seeking testing—expressing a clear preference for an approach that is simple. Patients viewed the referral process that was sometimes required outside of CHC settings as adding extra time and cost burdens to seeking testing. Participants also expressed mixed experiences and preferences for COVID-19 testing with appointments vs. walk-in—with the suggestion to provide both options. CHC staff, partners and residents all agreed that consistent, extended testing hours and locations improved testing uptake.
Interpersonal
CHC staff, partners, and residents described interpersonal interactions with clinicians and community-based organization staff as positive influences on testing uptake and as trusted sources of information. Employers both enabled access to testing with on-site accessibility and hindered testing with return-to-work policies that did not align with public health guidance and threatened job stability. Family and friends were reported as influencing testing uptake and crowded, multigenerational housing often hindered the ability for residents to isolate in an attempt to mitigate spread.
Individual
Interviews uncovered limited knowledge of the testing and follow-up process, testing availability, mobile testing, and rapid testing. This translated to some discomfort with the ideas of mobile and rapid testing. Fears of the testing process and contracting COVID-19 at testing sites were also expressed. Individuals expressed how mistrust in the healthcare system and fears of immigration-related repercussions decreased the likelihood of residents seeking testing. Language barriers and challenges with technology needed to make appointments and receive timely results also limited access to testing.
Discussion
This rapid, qualitative needs assessment of COVID-19 testing laid the groundwork for implementation of strategies to reach underserved populations at the peak of the pandemic in winter 2021. Using a 2-phase analysis process, we explored the perceptions of COVID-19 testing barriers among over 100 CHC staff, community partners, and residents. We created actionable summaries for the research team and CHC leaders to apply changes to testing strategies and address communication challenges immediately, prior to the completion of the theme identification process and full analysis. Additionally, this approach allowed for later more in-depth exploration of the multilevel factors influencing COVID-19 testing.
Massachusetts CHCs, along with the Massachusetts League of Community Health Center as a key advocate for needed policies and resources, were uniquely well-positioned to achieve the goal of the project to address COVID-19 testing inequities among underserved populations in “hotspot” communities. Their geographically identified service areas and majority patient-led and patient-engaged structure gave these CHCs the ability to use data to respond to the “hyper-local” needs of each community. This stands in contrast to the state mass vaccination sites that were very efficient, but unable to respond to the specific needs of underserved populations, particularly communities of color.
It is important to recognize that not all healthcare providers consider themselves to be a part of the essential public health infrastructure. As a result, when it comes to assuming risk to address a public health emergency like the COVID-19 pandemic, there are a number of critical questions that need to be addressed, such as who is accountable to the needs of the public's health—particularly the members of the public who are underserved? COVID-19 testing was about more than who had the resources to build and sustain this new service for residents. Setting up a testing program meant that staff members were at risk due to being exposed to potentially infectious individuals, and that staffing needs were increased, at a time when there was significant pressure on workforce availability. Developing a COVID-19 testing response was also incredibly disruptive to usual clinical care operations. As a result, the task fell primarily to healthcare institutions whose mission is to serve individuals and communities directly impacted by structural inequities, regardless of the cost or available resources. As we strive to learn how to do this better for the next pandemic or the next wave of this pandemic, do we make responsiveness to the community a criteria for public funding or non-profit status? Invest in government-run and tax-funded public health infrastructure? Or strengthen existing mission-driven community health partners like CHCs to be able to expand services/surge existing services to meet a public health need? Critical questions that must be answered are how do we build systems that are responsive to the needs of communities, and how do we mitigate structural barriers to care.
This qualitative study moves beyond individual perceptions of COVID-19 testing and underscores the substantial impact of upstream, structural disparities on the individual level experience of COVID-19, from infection to morbidity to mortality as well as on access to information and resources and uptake of preventive behaviors such as mask wearing and social distancing (19, 34). While we found that stakeholders expressed barriers and facilitators to testing at each level of the Social Ecological Model—individual, interpersonal, organization, community, and societal—the solutions for addressing these influences depend on institutional and governmental changes (32). Furthermore, while we discuss interpersonal factors such as the inability to isolate in crowded housing as circumstances of collective cultural household living, it is necessary to underscore that societal-level inequities (i.e., housing policies) create and perpetuate such factors in marginalized communities (35). The structural barriers identified, such as inadequate safety net policies for workers, immigration policies, and transportation, have lasting and multiplicative impacts at the individual level and may serve as launch points for next steps and future translational research. While prior studies have explored barriers and facilitators to COVID-19 testing among the general population or among one specific sub-population (18, 19, 36, 37), our study drew on a diverse array of perspectives to understand barriers and facilitators specific to several underserved populations (e.g., individuals experiencing homelessness, immigrant populations, individuals living in multigenerational households). This data better informed how CHCs and community partners could apply targeted approaches most relevant to specific populations disproportionally impacted by COVID-19.
Strengths of this study include its rapid approach to qualitative data collection and analysis that enabled the project to translate data for action in real time—this was essential for responding to a rapidly evolving pandemic. We were also able to interview 107 individuals across nine communities and in four languages—an approach that allowed for generating cross-cutting recommendations and identifying tailored community-specific needs. Building RADx-MA into our existing implementation science infrastructure in CHCs ensured that the project was uniquely health center-centric and responsive. Actionable response to findings was not prescribed to the CHCs, but rather the findings were provided to the health centers and each used the data to develop responses unique to their setting and to best meet the needs of their communities and resource structure. We shared results with CHC leaders and CABs to receive feedback on accuracy of data interpretation. Our CHC co-authors on this paper bolstered these perspectives, but we were unable to carry out member checking with residents. A trade-off with the breadth and action-oriented nature of the rapid needs assessment was our ability to capture demographics beyond the role and primary language of the participants. We were also only able to double-code a small sample of our interviews and did not have the staffing with the language skills to conduct interviews in Haitian Creole and Cape Verdean Creole—two language needs expressed by our CHC partners.
The lessons learned from this study were put to the test as the Omicron variant hit communities in December 2021. For instance, during the 2-week peak of the surge one CHC was able to accommodate an acute 10-fold increase in testing demand by pivoting back to the strategies identified through the rapid needs assessment and put in place earlier in the year. The CHC was able to quickly shift clinician resources to provide culturally and linguistically accessible positive result notification and medical evaluation of newly identified community residents with COVID-19 infection. Looking forward, these qualitative findings point to the importance of looking upstream to structural solutions at the organizational, community, and societal levels to prepare CHCs and the historically disadvantaged populations they serve for potential future surges and the endemic stage of the virus.
The COVID-19 pandemic has solidified the notion that health and social wellbeing are inextricably intertwined. In response to the pandemic, CHCs reached into the community to develop cross-sector partnerships that support health and wellness. Medical and non-medical drivers of health, and the relationship between them, should continue to gain recognition in the future of health care and offer insights into the social value of CHC's efforts to shape the health of communities. The present study lifts up examples of multilevel influences on health and demonstrates a shift from the typical years' long research translation process to a rapid approach of using data for action.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Harvard Longwood Campus Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
KE and RL contributed to the conception and design of the study. RL participated in the data collection. VH and SA conducted the qualitative analysis. All authors participated in the data interpretation, drafted the manuscript for intellectual content, contributed to manuscript revisions, and approved the submitted version.
Funding
This work was conducted with support from the National Institutes of Health (3P50CA244433-02S1), Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR002541), and financial contributions from Harvard University and its affiliated Academic Healthcare Centers.
Author Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated Academic Healthcare Centers, or the National Institutes of Health.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The study team thank the Massachusetts League of Community Health Centers as well as all of the Community Health Centers and partnering organizations for their collaboration on this study. The team also thank the brilliant research assistants who supported the recruitment, conduct, translation, and transcription of the qualitative interviews. Finally, this study would not have been possible without the diverse insights provided by the community residents from across the state of Massachusetts.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.838544/full#supplementary-material
Footnotes
1. ^https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-deaths.html
2. ^https://bphc.hrsa.gov/about/what-is-a-health-center/index.html
3. ^https://www.kff.org/coronavirus-covid-19/issue-brief/impact-of-coronavirus-on-community-health-centers/
References
1. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. (2020) 20:533–4. doi: 10.1016/S1473-3099(20)30120-1
2. Nayak A, Islam SJ, Mehta A, Ko Y-A, Patel SA, Goyal A, et al. Impact of social vulnerability on COVID-19 incidence and outcomes in the United States. medRxiv. (2020). doi: 10.1101/2020.04.10.20060962
3. Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, Felix SEB, . Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020 | MMWR. Coronavirus Dis 2019 Case Surveill — U S January 22–May 30 2020. Available online at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6924e2.htm (accessed September 20, 2021).
4. Disparities in COVID-19 Deaths Racial and Ethnic Health Disparities. Centers for Disease Control (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/disparities-deaths.html (accessed September 20, 2021).
5. Mackey K, Ayers CK, Kondo KK, Saha S, Advani SM, Young S, et al. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: a systematic review. Ann Intern Med. (2021) 174:362–73. doi: 10.7326/M20-6306
6. Strully K, Yang T-C, Liu H. Regional variation in COVID-19 disparities: connections with immigrant and Latinx communities in U.S. counties. Ann Epidemiol. (2021) 53:56–62.e2. doi: 10.1016/j.annepidem.2020.08.016
7. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. (2017) 389:1453–63. doi: 10.1016/S0140-6736(17)30569-X
8. Gee GC, Ford CL. Structural racism and health inequities. Bois Rev Soc Sci Res Race. (2011) 8:115–32. doi: 10.1017/S1742058X11000130
9. Ford CL. Commentary: addressing inequities in the era of COVID-19: the pandemic and the urgent need for critical race theory. Fam Community Health. (2020) 43:184–6. doi: 10.1097/FCH.0000000000000266
10. Williams DR, Cooper LA. COVID-19 and health equity—a new kind of “herd immunity.” JAMA. (2020) 323:2478. doi: 10.1001/jama.2020.8051
11. Ahmad K, Erqou S, Shah N, Nazir U, Morrison AR, Choudhary G, et al. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS ONE. (2020) 15:e0241327. doi: 10.1371/journal.pone.0241327
12. Rogers TN, Rogers CR, VanSant-Webb E, Gu LY, Yan B, Qeadan F. Racial disparities in COVID-19 mortality among essential workers in the United States. World Med Health Policy. (2020) 12:311–27. doi: 10.1002/wmh3.358
13. Do DP, Frank R. Unequal burdens: assessing the determinants of elevated COVID-19 case and death rates in New York City's racial/ethnic minority neighbourhoods. J Epidemiol Community Health. (2021) 75:321–6. doi: 10.1136/jech-2020-215280
14. Best AL, Fletcher FE, Kadono M, Warren RC. Institutional distrust among African Americans and building trustworthiness in the COVID-19 response: implications for ethical public health practice. J Health Care Poor Underserved. (2021) 32:90–8. doi: 10.1353/hpu.2021.0010
15. Krieger N, Waterman PD, Chen JT. COVID-19 and overall mortality inequities in the surge in death rates by zip code characteristics: Massachusetts, January 1 to May 19, 2020. Am J Public Health. (2020) 110:1850–2. doi: 10.2105/AJPH.2020.305913
16. Lieberman-Cribbin W, Tuminello S, Flores RM, Taioli E. Disparities in COVID-19 testing and positivity in New York City. Am J Prev Med. (2020) 59:326–32. doi: 10.1016/j.amepre.2020.06.005
17. Dryden-Peterson S, Velásquez GE, Stopka TJ, Davey S, Lockman S, Ojikutu B. Disparities in SARS-CoV-2 testing in massachusetts during the COVID-19 pandemic. JAMA Netw Open. (2020) 4:e2037067. doi: 10.1001/jamanetworkopen.2020.37067
18. Sim M, Embrett M. Barriers to COVID-19 Testing Testing Hesitancy: A Rapid Scoping Review.pdf. Strategy for Patient-Oriented Research Evidence Alliance. (2021). Available online at: https://sporevidencealliance.ca/key-activities/covid-19-evidence-synthesis/ (accessed December 12, 2021).
19. Bevan I, Stage Baxter M, Stagg HR, Street A. Knowledge, attitudes, and behavior related to COVID-19 testing: a rapid scoping review. Diagnostics. (2021) 11:1685. doi: 10.3390/diagnostics11091685
20. Towns R, Corbie-Smith G, Richmond A, Gwynne M, Fiscus L. Rapid deployment of a community-centered mobile Covid 19 testing unit to improve health equity. NEJM Catal Innov Care Deliv. (2020). doi: 10.1056/CAT.20.0522
21. Brewer LC, Woods C, Patel A, Weis J, Jones C, Abbenyi A, et al. Establishing a SARS-CoV-2 (COVID-19) drive-through collection site: a community-based participatory research partnership with a federally qualified health center. Am J Public Health. (2021) 111:658–62. doi: 10.2105/AJPH.2020.306097
22. Bigelow BF, Saxton R, Flores-Miller A, Mostafa HH, Loss MJ, Phillips KH, et al. Community testing and SARS-CoV-2 rates for Latinxs in Baltimore. Am J Prev Med. (2021) 60:e281–e6. doi: 10.1016/j.amepre.2021.01.005
23. Galiatsatos P, Monson K, Oluyinka M, Negro D, Hughes N, Maydan D, et al. Community calls: lessons and insights gained from a medical–religious community engagement during the COVID-19 pandemic. J Relig Health. (2020) 59:2256–62. doi: 10.1007/s10943-020-01057-w
24. What is a Health Center? Health Resources and Service Administration (2021). Available online at: https://bphc.hrsa.gov/about/what-is-a-health-center/index.html (accessed November 26, 2021).
25. Impact of Coronavirus on Community Health Centers | KFF. Available online at: https://www.kff.org/coronavirus-covid-19/issue-brief/impact-of-coronavirus-on-community-health-centers/ (accessed September 20, 2021).
26. Stening T. Massachusetts Extending Free COVID Testing Through ‘Stop the Spread' Program Until June 30. masslive (2021). Available online at: https://www.masslive.com/coronavirus/2021/03/massachusetts-extending-free-covid-testing-through-stop-the-spread-program-until-june-30-see-where-you-can-get-tested.html (accessed December 12, 2021).
27. Stop the Spread MA. Transform Healthcare. Available online at: https://transformativehc.com/stop-the-spread/ (accessed December 12, 2021).
28. Tromberg BJ, Schwetz TA, Pérez-Stable EJ, Hodes RJ, Woychik RP, Bright RA, et al. Rapid scaling up of Covid-19 diagnostic testing in the United States — The NIH RADx Initiative. N Engl J Med. (2020) 383:1071–7. doi: 10.1056/NEJMsr2022263
29. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13:117. doi: 10.1186/1471-2288-13-117
30. Palinkas LA, Zatzick D. Rapid Assessment Procedure Informed Clinical Ethnography (RAPICE) in pragmatic clinical trials of mental health services implementation: methods and applied case study. Adm Policy Ment Health Ment Health Serv Res. (2019) 46:255–70. doi: 10.1007/s10488-018-0909-3
31. Gale RC, Wu J, Erhardt T, Bounthavong M, Reardon CM, Damschroder LJ, et al. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement Sci. (2019) 14:11. doi: 10.1186/s13012-019-0853-y
32. Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. (1996) 10:282–98. doi: 10.4278/0890-1171-10.4.282
33. Find, a COVID-19 Test | Mass,.gov. Mass.gov. Available online at: https://www.mass.gov/info-details/find-a-covid-19-test (accessed November 27, 2021).
34. McElfish PA, Purvis R, James LP, Willis DE, Andersen JA. Perceived barriers to COVID-19 testing. Int J Environ Res Public Health. (2021) 18:2278. doi: 10.3390/ijerph18052278
35. Airhihenbuwa CO, Iwelunmor J, Munodawafa D, Ford CL, Oni T, Agyemang C, et al. Culture matters in communicating the global response to COVID-19. Prev Chronic Dis. (2020) 17:E60. doi: 10.5888/pcd17.200245
36. Garcini LM, Pham TT, Ambriz AM, Lill S, Tsevat J. COVID-19 diagnostic testing among underserved Latino communities: barriers and facilitators. Health Soc Care Commun. (2021) 1–10. doi: 10.1111/hsc.13621
37. Bateman LB, Schoenberger Y-MM, Hansen B, Osborne TN, Okoro GC, Speights KM, et al. Confronting COVID-19 in under-resourced, African American neighborhoods: a qualitative study examining community member and stakeholders' perceptions. Ethn Health. (2021) 26:49–67. doi: 10.1080/13557858.2021.1873250
Keywords: COVID-19 testing, community health centers, structural inequities, qualitative, needs assessment, rapid analysis, immigrant populations
Citation: Lee RM, Handunge VL, Augenbraun SL, Nguyen H, Torres CH, Ruiz A, and Emmons KM for the RADx-MA Research Partnership (2022) Addressing COVID-19 Testing Inequities Among Underserved Populations in Massachusetts: A Rapid Qualitative Exploration of Health Center Staff, Partner, and Resident Perceptions. Front. Public Health 10:838544. doi: 10.3389/fpubh.2022.838544
Received: 17 December 2021; Accepted: 28 February 2022;
Published: 24 March 2022.
Edited by:
Tushar Trivedi, Regional Medical Center, United StatesReviewed by:
Tony Kuo, University of California, Los Angeles, United StatesJanet Hayes Southerland, University of Texas Medical Branch at Galveston, United States
Copyright © 2022 Lee, Handunge, Augenbraun, Nguyen, Torres, Ruiz, Emmons and for the RADx-MA Research Partnership. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rebekka M. Lee, cmxlZUBoc3BoLmhhcnZhcmQuZWR1
 Rebekka M. Lee
Rebekka M. Lee Veronica L. Handunge
Veronica L. Handunge Samantha L. Augenbraun
Samantha L. Augenbraun Huy Nguyen
Huy Nguyen Cristina Huebner Torres
Cristina Huebner Torres Alyssa Ruiz
Alyssa Ruiz Karen M. Emmons
Karen M. Emmons