- 1Institute of Hematology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2Department of Hematology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 3Department of Hematology, Jingzhou Central Hospital, The Second Clinical Medical College, Yangtze University, Jingzhou, China
- 4Department of Hematology, Yichang Central People's Hospital, The First College of Clinical Medical Science, China Three Gorges University, Yichang, China
- 5Department of Hematology, Jingzhou First People's Hospital and First Affiliated Hospital of Yangtze University, Jingzhou, China
Background: To curb the spread of the coronavirus disease 2019 (COVID-19) epidemic, the Chinese government shut down Wuhan city from January 23rd to April 8th, 2020. The COVID-19 epidemic not only leads to widespread illness but also affects the diagnosis and treatment of hematopoietic stem-cell transplant (HSCT) recipients.
Objective: To investigate the medical-seeking pattern and daily behavior changes in Hubei Province during the COVID-19 epidemic in Hubei Province during the lockdown.
Methods: We conducted a multicenter, cross-sectional, web-based investigation among 325 HSCT recipients by online questionnaires in Hubei Province during the COVID-19 epidemic.
Results: A total of 145 complete responses were collected both before and during the epidemic questionnaires. The participants from pre-epidemic group preferred to go to hospital (68.29%) when they experienced influenza-like symptoms. The majority of the patients elected to take oral drugs by themselves (40%) or consulted their attending physicians online or by telephone during the lockdown (23.33%). 64.83% had difficulties in purchasing drugs during the lockdown, which was significantly higher than the proportion of the pre-epidemic group (24.83%) (P < 0.05). The participants preferred to purchase drugs online (23.40%) and decrease or withdraw drugs (18.09%) during the epidemic. The number of participants received regular re-examinations during the epidemic decreased sharply. The proportion of wearing masks and isolating themselves at home increased significantly during the epidemic. No statistic difference was observed in the incidence of graft-versus-host disease (GVHD)complications in participants between the during the epidemic group and the pre-epidemic group. In our study, six patients were confirmed to have COVID-19, and half of them died due to COVID-19-related complications.
Conclusion: The medical-seeking pattern and daily behavior of HSCT recipients changed during the lockdown; the methods of self-protection, online consultation and drug delivery can help patients receive necessary follow-up and reduce the occurrence of COVID-19.
Introduction
To curb the spread of the coronavirus disease 2019 (COVID-19) epidemic, the Chinese government shut down Wuhan city from January 23rd to April 8th, 2020 (1, 2). Transportation within Wuhan city and transportation between Wuhan city and other cities in Hubei Province was highly restricted. To date, the COVID-19 vaccine has not been administered to the entire population, and thus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may be lead to another pandemic (3, 4). Areas of unmet need and future research questions are also highlighted. The waves of the COVID-19 pandemic are predicted to be followed by an “endemic” phase and therefore an ongoing risk within a “new normality” (5).
COVID-19 not only leads to widespread illness but also affects the diagnosis and treatment of patients with other diseases due to strict prevention and control strategies. Among these patients, hematopoietic stem-cell transplant (HSCT) recipients are likely to be seriously affected (6–8). Due to the severity of the primary disease and the development of immunosuppression after transplantation, recipients of HSCT are constantly at risk for serious complications such as graft-versus-host disease (GVHD), pulmonary infection, and relapse of primary disease (8, 9). Regular follow-up and re-examination can directly determine the prognosis of HSCT recipients. Thus, how doctors treat HSCT recipients and subsequent complications during the lockdown have become two crucial problems.
Leading global institutions, such as the European Society for Blood and Marrow Transplantation (EBMT) and American Society for Transplantation and Cellular Therapy (ASTCT), have published guidelines for COVID-19 management among HSCT recipients (9, 10). The EBMT recommends that potential transplant recipients should home isolate for 14 days pretransplant (9). The EBMT and the ASTCT recommend that transplant-related procedures be delayed 14–21 days from the last contact and potential recipients be monitored for SARS-CoV-2 infection in patients if they had come in close contact to persons infected with SARS-CoV-2 (9, 10). A major transplant center in China suggested that social distancing, mask wearing, and education for patients and donors are essential preventative measures in these patients (11). They also recommend potential transplant recipients and donors to finish SARS-CoV-2 with qRT-PCR, serum antibody detection, and a lung CT scan pretransplant (11).
Data about medical-seeking pattern and daily behavior changes during lockdown are still rare. Therefore, we performed a retrospective multicenter investigation to explore the changes in the medical-seeking pattern and daily behavior of HSCT recipients, and the incidence and mortality of HSCT recipients with COVID-19 in Hubei Province during lockdown.
Methods
Study participants and survey design
We conducted a multicenter, cross-sectional, web-based investigation among HSCT recipients using online questionnaires. This survey was conducted from 25 April to 30 May 2020. Patients were recruited from Hubei Province. The physicians used WeChat (the most popular social app in China) and DoctorWith (an online medical app used by HSCT recipients) to publicize and distribute the survey link to the patients or their direct relatives.
Respondents were informed that their participation was voluntary, and consent was implied on the completion of the questionnaire. The inclusion criteria were that the respondents were at least 18 years old, could read and comprehend Chinese, and were under travel restrictions. This study was approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China (Approval: 2022-S078).
Data collection
The research team develop two questionnaires to investigate HSCT recipients' medical-seeking pattern and daily behavior changes during the COVID-19 epidemic. Participants were recruited through multiple cities online panel providers for each city to avoid coverage bias: ZDZ and YCZ provided 157 responsers across Wuhan city; YSZ, JMG, and ZPH provided 109 responders from 3 cities in Hubei province except Wuhan. Respondents' identities were verified using IP addresses and mobile phone numbers to ensure that each participant was real and unique upon initial registration.
This survey included questions that assessed: (1) demographic background, the diagnosis of primary disease, HSCT complications; (2) self-perceived health status, daily behavior, medical-seeking pattern; (3) COVID-19 experience, the difficulties in suffering uncomfortable symptoms, the most fear during the COVID-19 epidemic.
Two online questionnaires (Supplement 1) were distributed and collected by physicians from each center. The first questionnaire investigated the medical-seeking pattern and daily behavior during COVID-19 epidemic, and the second questionnaire assessed the patient's routine before the COVID-19 epidemic. The questionnaire included 28 questions that assessed: (1) demographic characteristics, primary disease information, HSCT complications; (2) self-perceived health status, diagnosis and treatment modes, daily behavior, (3) COVID-19 experience, the difficulties in suffering uncomfortable symptoms, the most fear during the COVID-19 epidemic diagnosis, treatment regimen and mental stress during and before the COVID-19 epidemic.
The diagnosis of COVID-19 was made according to the diagnostic and treatment guidelines for COVID-19 issued by the Chinese National Health Committee (version 3–5). Two physicians independently reviewed the forms to verify the data. If data were not available from the questionnaire, the researchers directly communicated with the patients, health-care providers and/or patients' families to ascertain epidemiology and symptoms.
Statistical analysis
For the HSCT recipients, data on HSCT related complications, and behavior patterns were expressed as descriptive statistics; continuous variables were expressed as medians and interquartile ranges (IQRs); and categorical variables were expressed as proportions and frequencies. Medians were compared using independent samples t-tests when the data were normally distributed; otherwise, the Mann-Whitney test or Kruskal-Wallis test was used. Proportions for categorical variables were compared using the χ2 test, although the Fisher's exact test was used when the data were limited. A P value of <0.05 was considered statistically significant. The analysis was completed in GraphPad Prism software, version 8.0.
Results
Characteristics of HSCT recipients during the COVID-19 epidemic
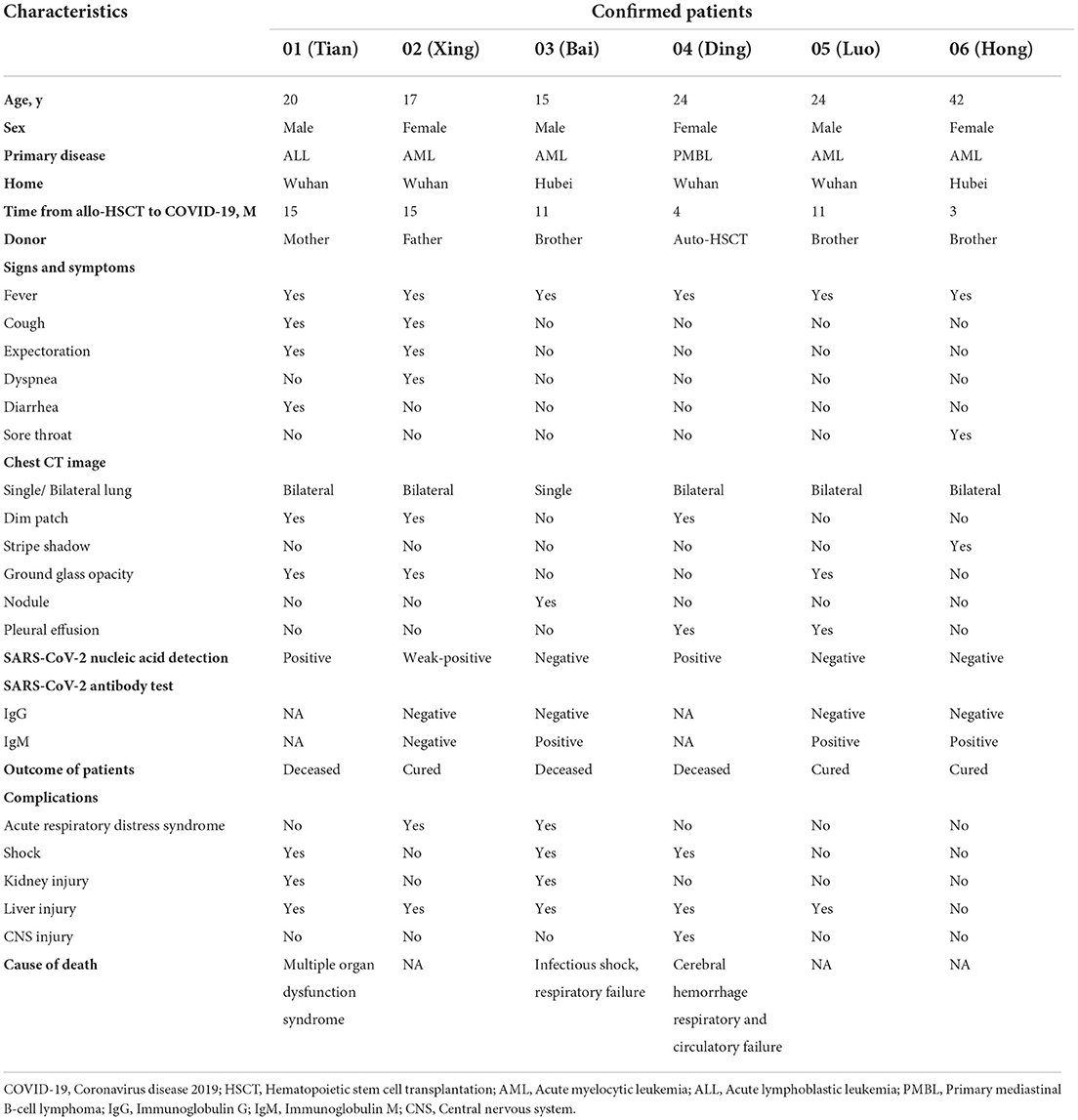
A total of 501 complete responses from 325 HSCT recipients were received, including 228 responses before the COVID-19 outbreak (from October 2019 to December 2019) and 273 during the epidemic (from February 2020 to April 2020). The overall response to the survey was poor. Only 145 participants returned both questionnaires at the same time. The demographics and baseline characteristics of the HSCT recipients are shown in Table 1 and Figure 1. Of note, all of the cohorts comprised HSCT recipients from Hubei Province, because of the largest number of confirmed cases in Hubei Province. The median age of the participants was 33 (23–41, IQR) years. A higher proportion of participants from other cities in in Hubei Province except Wuhan (66.21%) than Wuhan city (22.07%) and other provinces (11.72%) responded to our questionnaires. Figure 1 shows the diagnosis of primary diseases of responses. The great majority had matched sibling donors (97.93%) compared to matched unrelated donors (2.07%).
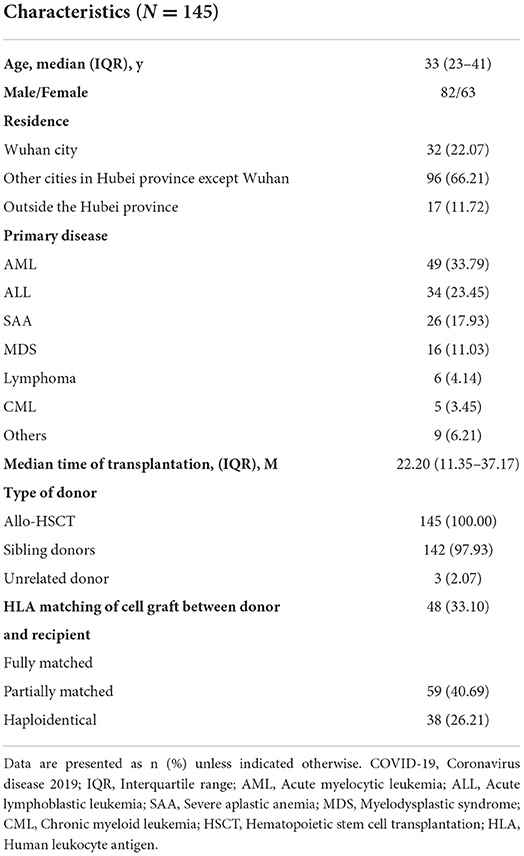
Table 1. Characteristics of hematopoietic stem cell transplantation recipients during the COVID-19 epidemic.
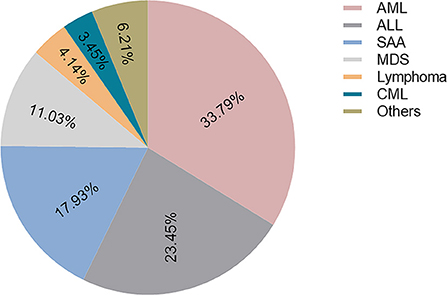
Figure 1. The diagnosis of primary disease. AML, Acute myelocytic leukemia; ALL, Acute lymphoblastic leukemia; SAA, Severe aplastic anemia; MDS, Myelodysplastic syndrome; CML, Chronic myeloid leukemia.
HSCT complications during the COVID-19 epidemic
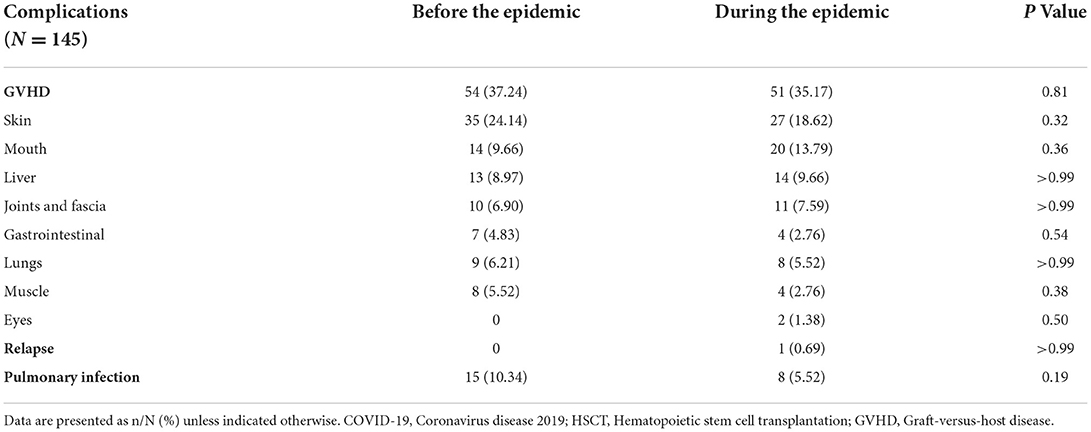
Interestingly, no statistic difference was observed in the incidence of GVHD in HSCT recipients between the during the epidemic group (35.17%) and the before group (37.24%) (P = 0.81). The involved organs include skin, mouth, liver, joints and fascia, gastrointestinal, lungs, muscle, and eyes. Each of involved organ had similar incidence of GVHD between these two groups. In addition, only one patient experienced relapse of the primary disease during epidemic. The number of patients developed a pulmonary infection during the epidemic (5.52%) had no statistic difference in the pre-epidemic group (10.34%) (P = 0.19). Data on complications among HSCT recipients are shown in Table 2.
Medical treatments and daily behavior patterns of HSCT recipients
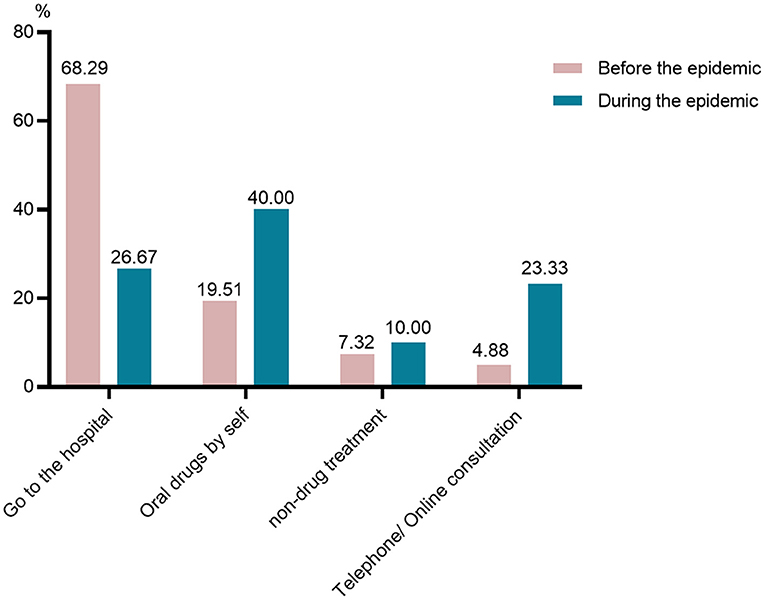
Our study found that the number of participants with cough or fever did not increase during the epidemic. The proportion of participants with influenza-like symptoms was 20.69% during the epidemic and 28.28% before the epidemic (P = 0.17). Although the number of participants experienced influenza-like symptoms did not increase during the epidemic, they differ in solutions for these uncomfortable symptoms (Figure 2). The participants from pre-epidemic group preferred to go to hospital (68.29%) when they experienced cough or fever. However, 40% of the patients elected to take oral drugs by themselves during the lockdown. What can be clearly seen in Figure 2 is the growth of the number of patients consulted their attending physicians online or by telephone during the epidemic (23.33%).
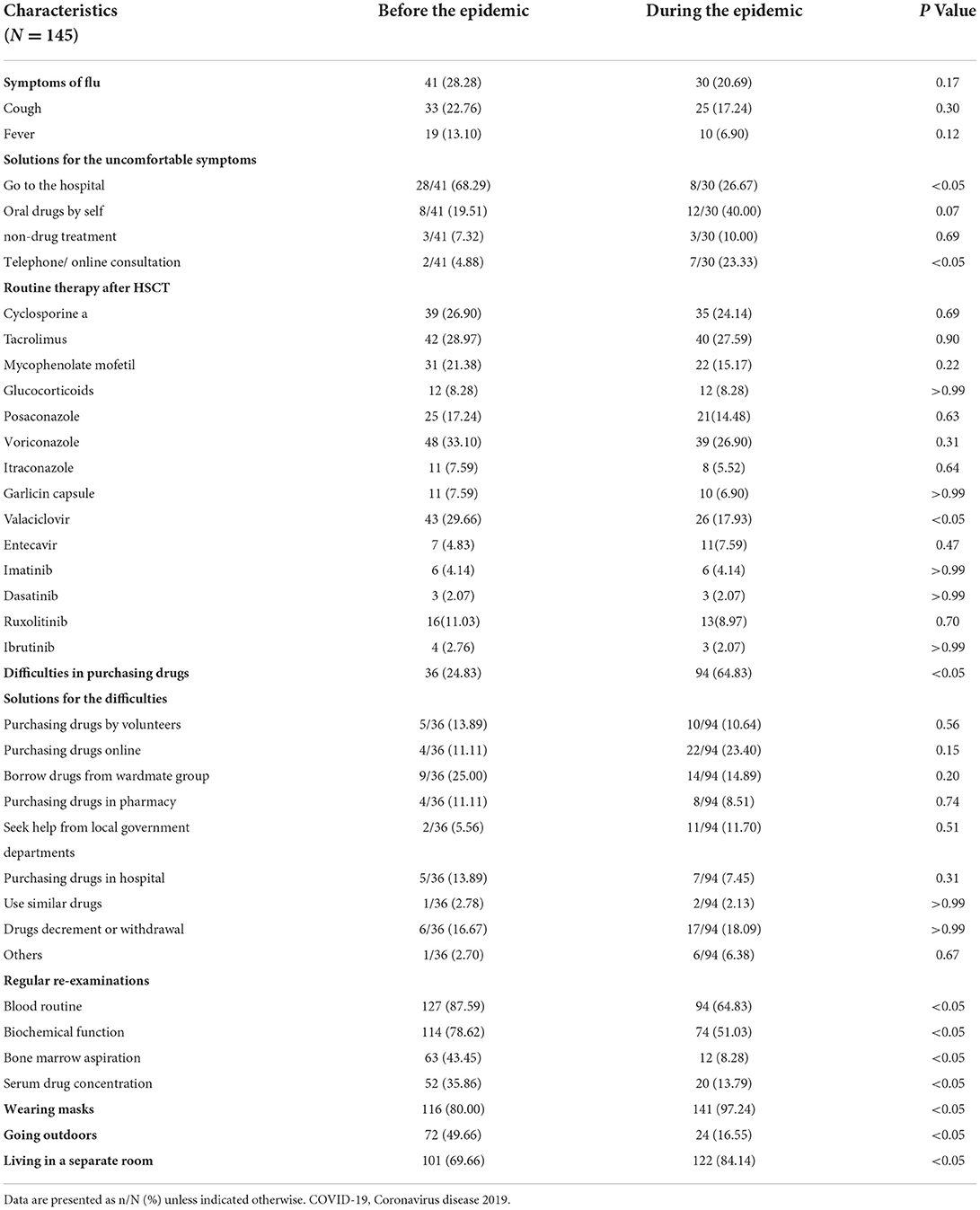
The participants received routine therapy after hematopoietic stem-cell transplantation, including immunosuppressive therapy (cyclosporine a, or tacrolimus, and/or mycophenolate mofetil, or glucocorticoids), antifungal therapy (posaconazole, or voriconazole, or itraconazole, and/or garlicin capsules), antiviral therapy (valaciclovir, and/or entecavir), micromolecule targeted medicines (imatinib, or dasatinib, or ruxolitinib, or ibrutinib). The number of patients on medicines were shown in the Table 3. We found that of 145 participants, 64.83% had difficulties in purchasing drugs during the lockdown, which was significantly higher than the proportion of the pre-epidemic group (24.83%) (P < 0.05). The evidence shows that the participants preferred to purchase drugs online (23.40%) and decrease or withdraw drugs (18.09%) during the epidemic. And patients in the pre-epidemic group preferred borrow drugs from wardmate group (25.00%) and decrease or withdraw drugs (16.67%) when they were hard to purchasing medicines. What stands out in Figure 3 is the dramatic decline in the number of patients on valaciclovir after the lockdown.
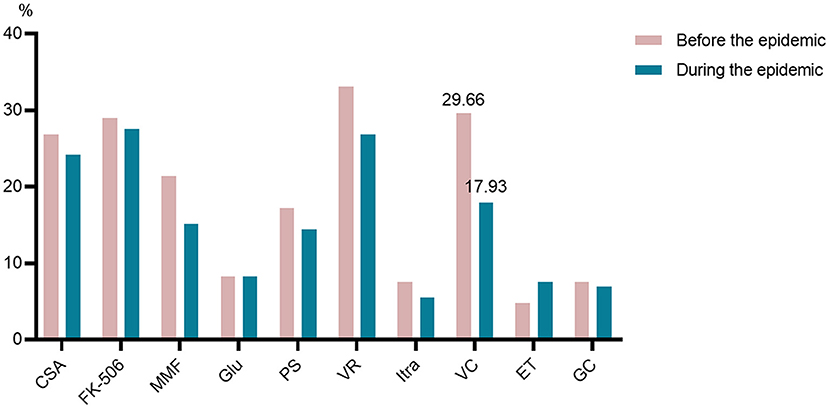
Figure 3. Routine medicines after hematopoietic stem-cell transplantation. CSA, cyclosporine a; FK-506, tacrolimus; MMF, mycophenolate mofetil; GLU, glucocorticoids; PS, posaconazole; VR, voriconazole; Itra, itraconazole; GC, garlicin capsules; VC, valaciclovir; ET, entecavir.
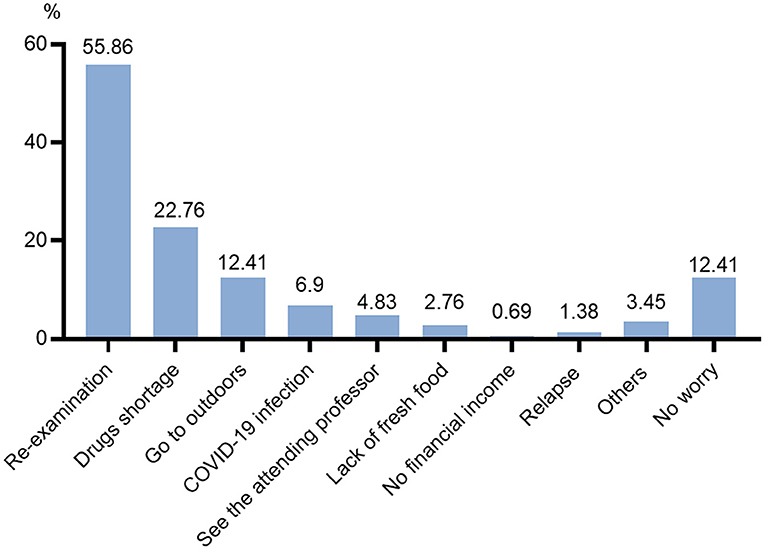
Figure 4 and Table 3 reveals that there has been a sharp drop in the number of participants received regular re-examinations during the epidemic, whether blood routine, biochemical function, bone marrow aspiration, or serum drug concentration of cyclosporine or tacrolimus. Furthermore, this is the biggest fear of the participants during the epidemic (Figure 5). With the lockdown, the probability of wearing masks increased by 17.24% (P < 0.05). Meanwhile, the proportion of going outdoors reached 16.55% during the epidemic far fewer the pre-epidemic group (49.66%) (P < 0.05). Also, more participants lived in a separate room (84.14%) during the lockdown than before (69.66%) (P < 0.05).
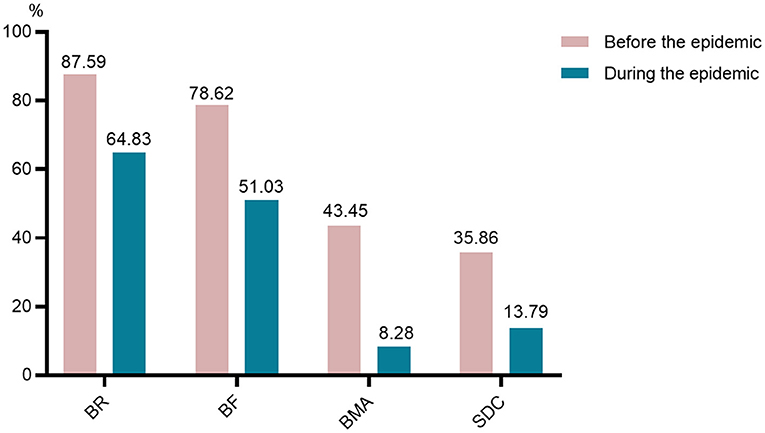
Figure 4. Changes of regular re-examinations. BR, blood routine; BF, biochemical function; BMA, bone marrow aspiration; SDC, serum drug concentration of cyclosporine or tacrolimus.
Characteristics of patients with COVID-19 after HSCT
In our study, six patients were confirmed to have COVID-19, which was not higher than that in the general population (12, 13). Their clinical features and auxiliary examinations are shown in Table 4. Four patients lived in Wuhan, and two had sojourn in Wuhan city. All confirmed patients had a fever. Their chest CT scan showed that almost all of them had bilateral lung infections (5/6). SARS-CoV-2 nucleic acid was detected in 3 patients. The antibody test was performed in 4 patients: three of them were IgM positive, and all were IgG negative. In total, three patients died during the pandemic, the leading cause of death were multiple organ dysfunction syndrome (1/3), infectious shock (1/3), cerebral hemorrhage (1/3), and respiratory and circulatory failure (2/3).
Discussion
To our knowledge, this is the first published survey of HSCT recipients whose changes in medical-seeking pattern and daily behavior patterns before and during the COVID-19 epidemic. We observed the majority of participants had medical-seeking pattern and daily behavior patterns changes during the lockdown. The survey shows that there has been a marked increase in the number of patients wearing masks and living a separate room during epidemic. Meanwhile, participants have to travel less and better insulate their homes due to the lockdown. Compared with participants in pre-epidemic period, participants in epidemic changed their medical-seeking pattern and purchasing medicine mode. The participants stay alert to influenza-like symptoms all the time, but in contrast to go to hospital immediately when they had a fever or cough, seek medical advices from a distance was an alternative choice.
To enhance the awareness of COVID-19 prevention among HSCT recipients, we strengthened patient education and psychological counseling through online platforms during the lockdown. We also provided consultations and advices to patients online. Therefore, HSCT recipients paid more attention to personal protection, they preferred to wear masks; and they refrained from going outdoors. As a result, only 6 of 375 HSCT recipients experienced SARS-CoV-2 infections. In addition, our study showed that the recommendation to wear masks and limit going outdoors may reduce the risk of SARS-CoV-2 infection. This conclusion was consistent with Bundgaard.H's research (14).
Prior to this survey, there has only been a small amounts of published articles describing how to manage hematopoietic cell transplant during the SARS-CoV-2 pandemic (11, 15–19). They reported that patients received HSCT are at increased risk of infection with SARS-CoV-2 and COVID-19 (18). A major transplant center in China recommended that self-isolation and minimal contact with family members, and nonessential clinic visits should be deferred or substituted with telemedicine consultations if possible (11).
Based on a patient's specific adverse effects to HSCT and his/her uncomfortable symptoms, an individualized stratified diagnosis and treatment plan is programmed online through WeChat or DoctorWith software. The incidence of HSCT complications such as GVHD, infection, and relapse did not increase during the pandemic, which may suggest that seeking medical advice online is a useful strategy for the management of HSCT recipients and other chronic diseases. The difficulty of purchasing drugs during the lockdown maybe the important factor for drugs decrement or withdrawal. In this study, approximately a quarter of those who are short of medicines appealed to wardmate group or volunteers to borrow or purchase drugs and send them directly. We hypothesized that these wardmates and volunteers may have helped the patients with purchasing drugs before the epidemic.
This study has several limitations. First, the number of patients responded to the survey is small; however, it parallels the size of other studies that have had a significant influence in the field of HSCT recipients (18, 20). Despite the small size of this survey, it was representatively in medical-seeking pattern and daily behavior patterns changes of HSCT recipients during the lockdown. Therefore, a larger cohort is required to ascertain whether these initial findings are transferable to specialized at-risk cohorts. In contrast to other patients, HSCT recipients are more likely to develop opportunistic infections due to impaired immunity (12, 21). In addition, GVHD, infection, and relapse usually occur sequentially in patients after transplantation, and are the leading causes of premature death (21–24). There were insufficient severe HSCT complications to provide a conclusive evaluation of the changes of incidence and severity of complications during the epidemic.
The other limitation is that the participants who obtained and completed the link of questionnaires aged 18–60 years were overrepresented, which may lead to selection bias. All of participants are HSCT recipients who were younger than the general population (25–27), one of the main reasons is the age limitation of HSCT, also due to the primary user community of WeChat or DoctorWith are younger and middle-aged. In addition, the diagnosis of COVID-19 was made according to the diagnostic and treatment guidelines for COVID-19 issued by the Chinese National Health Committee (version 3–5) in the early epidemic. Therefore, many COVID-19 patients were empirically diagnosed and lacked a molecular diagnosis. Also, the RT-PCR kits in use (likely the first kits developed for SARS-CoV-2 detection), the lack of standard methods for COVID-19 testing may lead to false negative nucleic acid results (28–30). Finally, we relied on several patient families completed questionnaires in special patients, and thus, blinding to the intervention was not possible.
In conclusion, in light of their changes in medical-seeking pattern and daily behavior patterns during the lockdown, online consultation and drug delivery can help patients receive necessary follow-up and reduce the occurrence of adverse events. Further studies would need to evaluate the availability of telemedicine in the management of HSCT recipients under the normalization of the epidemic.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology. Respondents were informed that their participation was voluntary and written informed consent was obtained to participate in this study.
Author contributions
ZZ, FC, and YiZ designed the research. ZH, SC, JG, YoZ, ML, WC, and HY collected the data. RX and XZ analyzed results and wrote the paper. ZZ, YY, PZ, and FC interpreted data and reviewed the paper. All authors reviewed the results and approved the final version of the manuscript.
Acknowledgments
We appreciate all of the patients and doctors who have contributed to this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.918081/full#supplementary-material
References
1. Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, et al. Effect of non-pharmaceutical i nterventions to contain COVID-19 in China. Nature. (2020) 585:410–3. doi: 10.1101/2020.03.03.20029843
2. Zhang Y, Xu J, Li H, Cao B. A novel coronavirus (COVID-19) outbreak: a call for action. Chest. (2020) 157:E99–E101. doi: 10.1016/j.chest.2020.02.014
3. Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. (2021) 27:225–8. doi: 10.1038/s41591-020-1124-9
4. Verelst F, Willem L, Beutels P. Behavioural change models for infectious disease transmission: a systematic review (2010-2015). J R Soc Interface. (2016) 13:20160820. doi: 10.1098/rsif.2016.0820
5. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–90. doi: 10.1038/s41586-020-2012-7
6. Alhuraiji A, Eldadah S, Alfraih F, Pandita R, Absi A, Hanbali A, et al. Optimal management of acute lymphoblastic leukemia (ALL) in adult patients during the novel coronavirus disease 2019 (COVID-19) pandemic. Gulf J Oncolog. (2020) 1:7–18.
7. Li W, Wang D, Guo J, Yuan G, Yang Z, Gale RP, et al. COVID-19 in persons with chronic myeloid leukaemia. Leukemia. (2020) 34:1799–804. doi: 10.1038/s41375-020-0853-6
8. Broxmeyer HE, Parker GC. Impact of COVID-19 and future emerging viruses on hematopoietic cell transplantation and other cellular therapies. Stem Cells Dev. (2020) 29:625–6. doi: 10.1089/scd.2020.0064
9. Ljungman P, Mikulska M, de la Camara R, Basak GW, Chabannon C, Corbacioglu S, et al. The challenge of COVID-19 and hematopoietic cell transplantation; EBMT recommendations for management of hematopoietic cell transplant recipients, their donors, and patients undergoing CAR T-cell therapy. Bone Marrow Transplant. (2020) 55:2071–6. doi: 10.1038/s41409-020-0919-0
10. Mahmoudjafari Z, Alexander M, Roddy J, Shaw R, Shigle TL, Timlin C, et al. American society for transplantation and cellular therapy pharmacy special interest group position statement on pharmacy practice management and clinical management for COVID-19 in hematopoietic cell transplantation and cellular therapy patients in the United States. Biol Blood Marrow Transplant. (2020) 26:1043–9. doi: 10.1016/j.bbmt.2020.04.005
11. Xiao H, Luo Y, Shi J, Jin A, Mohty M, Nagler A, et al. How do we manage hematopoietic cell transplant during the SARS-CoV-2 pandemic? Acta Haematol. (2021) 144:500–7. doi: 10.1159/000513036
12. Sharma A, Bhatt NS, St Martin A, Abid MB, Bloomquist J, Chemaly RF, et al. Clinical characteristics and outcomes of COVID-19 in haematopoietic stem-cell transplantation recipients: an observational cohort study. Lancet Haematol. (2021) 8:e185–e93. doi: 10.1016/S2352-3026(20)30429-4
13. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. (2020) 55:105924. doi: 10.1016/j.ijantimicag.2020.105924
14. Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, Norsk JB, et al. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in danish mask wearers : a randomized controlled trial. Ann Intern Med. (2021) 174:335–43. doi: 10.7326/M20-6817
15. Bailey AJM, Kirkham AM, Monaghan M, Shorr R, Buchan CA, Bredeson C, et al. A portrait of SARS-CoV-2 infection in patients undergoing hematopoietic cell transplantation: a systematic review of the literature. Curr Oncol. (2022) 29:337–49. doi: 10.3390/curroncol29010030
16. Lafarge A, Mabrouki A, Yvin E, Bredin S, Binois Y, Clere-Jehl R, et al. Coronavirus disease 2019 in immunocompromised patients: a comprehensive review of coronavirus disease 2019 in hematopoietic stem cell recipients. Curr Opin Crit Care. (2022) 28:83–9. doi: 10.1097/MCC.0000000000000907
17. Sahu KK, Siddiqui AD. A review on recipients of hematopoietic stem cell transplantation patients with COVID-19 infection. Ther Adv Infect Dis. (2021) 8:20499361211013252. doi: 10.1177/20499361211013252
18. Belsky JA, Tullius BP, Lamb MG, Sayegh R, Stanek JR, Auletta JJ. COVID-19 in immunocompromised patients: a systematic review of cancer, hematopoietic cell and solid organ transplant patients. J Infect. (2021) 82:329–38. doi: 10.1016/j.jinf.2021.01.022
19. Shahzad M, Chaudhary SG, Zafar MU, Hassan MA, Hussain A, Ali F, et al. Impact of COVID-19 in hematopoietic stem cell transplant recipients: a systematic review and meta-analysis. Transpl Infect Dis. (2022) 24:e13792. doi: 10.1111/tid.13792
20. Liu H, Yang D, Chen X, Sun Z, Zou Y, Chen C, et al. The effect of anticancer treatment on cancer patients with COVID-19: a systematic review and meta-analysis. Cancer Med. (2021) 10:1043–56. doi: 10.1002/cam4.3692
21. Mohty B, Mohty M. Long-term complications and side effects after allogeneic hematopoietic stem cell transplantation: an update. Blood Cancer J. (2011) 1:e16. doi: 10.1038/bcj.2011.14
22. Boyiadzis M, Arora M, Klein JP, Hassebroek A, Hemmer M, Urbano-Ispizua A, et al. Impact of chronic graft-versus-host disease on late relapse and survival on 7,489 patients after myeloablative allogeneic hematopoietic cell transplantation for leukemia. Clin Cancer Res. (2015) 21:2020–8. doi: 10.1158/1078-0432.CCR-14-0586
23. Chang YJ, Weng CL, Sun LX, Zhao YT. Allogeneic bone marrow transplantation compared to peripheral blood stem cell transplantation for the treatment of hematologic malignancies: a meta-analysis based on time-to-event data from randomized controlled trials. Ann Hematol. (2012) 91:427–37. doi: 10.1007/s00277-011-1299-8
24. Singh AK, McGuirk JP. Allogeneic stem cell transplantation: a historical and scientific overview. Cancer Res. (2016) 76:6445–51. doi: 10.1158/0008-5472.CAN-16-1311
25. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. (2020) 75:1730–41. doi: 10.1111/all.14238
26. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with Novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2019) 2020:E1–9. doi: 10.1001/jama.2020.1585
27. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. doi: 10.1016/S0140-6736(20)30211-7
28. Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, Zambrano-Achig P, Del Campo R, Ciapponi A, et al. False-negative results of initial RT-PCR assays for COVID-19: a systematic review. PLoS ONE. (2020) 15:e0242958. doi: 10.1371/journal.pone.0242958
29. Ji T, Liu Z, Wang G, Guo X, Akbar Khan S, Lai C, et al. Detection of COVID-19: A review of the current literature and future perspectives. Biosens Bioelectron. (2020) 166:112455. doi: 10.1016/j.bios.2020.112455
Keywords: hematopoietic stem-cell transplantation, medical-seeking pattern, daily behavior, COVID-19, lockdown
Citation: Xie R, Zhang Y, Huang Z, Cheng S, Guo J, Zhang Y, Liu M, Zhu X, You Y, Zou P, Chen W, Yan H, Cheng F and Zhong Z (2022) Changes in the medical-seeking pattern and daily behavior of hematopoietic stem-cell transplant recipients during the COVID-19 epidemic: An online survey in Hubei Province, China. Front. Public Health 10:918081. doi: 10.3389/fpubh.2022.918081
Received: 12 April 2022; Accepted: 12 September 2022;
Published: 04 October 2022.
Edited by:
Diego Raul Hijano, St. Jude Children's Research Hospital, United StatesReviewed by:
Salim Moussa, Beirut Arab University, LebanonSilvia Nozza, San Raffaele Hospital (IRCCS), Italy
Copyright © 2022 Xie, Zhang, Huang, Cheng, Guo, Zhang, Liu, Zhu, You, Zou, Chen, Yan, Cheng and Zhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fanjun Cheng, Y2hlbmdmYW5qdW4wMDFAc2luYS5jb20=; Zhaodong Zhong, d2h4aHp6ZDAwOEAxMjYuY29t
†These authors have contributed equally to this work
 Rong Xie
Rong Xie Yicheng Zhang
Yicheng Zhang Zhiping Huang3†
Zhiping Huang3† Si Cheng
Si Cheng Xiaojian Zhu
Xiaojian Zhu Han Yan
Han Yan Fanjun Cheng
Fanjun Cheng Zhaodong Zhong
Zhaodong Zhong