- 1Department of Health Service Management, School of Health Service Management, Anhui Medical University, Hefei, China
- 2Department of Geriatrics, The First Affiliated Hospital of University of Science and Technology of China, Gerontology Institute of Anhui, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, China
- 3Anhui Key Laboratory of Tumor Immunotherapy and Nutrition Therapy, Hefei, China
Background: Depressive symptoms and mild cognitive impairment (MCI) are highly prevalent in rural China. The study aimed to investigate the longitudinal associations between changes in depressive symptoms and cognitive decline and MCI incidence among Chinese rural elderly individuals.
Methods: A 2-year follow-up study was conducted among 1,477 participants from the Anhui Healthy Longevity Survey (AHLS). Depressive symptoms were assessed by the 9-item Patient Health Questionnaire (PHQ-9), and cognitive status was evaluated by the Mini Mental State Examination (MMSE). Multivariable linear regression and logistic regression were employed.
Results: Every 1-unit PHQ-9 score increase was significantly associated with more cognitive decline (β = 0.157, 95% CI: 0.092, 0.221, p < 0.001) and a higher risk of MCI incidence (OR = 1.063, 95% CI: 1.025, 1.103, p = 0.001). The participants who experienced worsening of depression symptoms had a larger decline in the 2-year MMSE score (β = 0.650, 95% CI: 0.039, 1.261, p = 0.037) and elevated risks of incident MCI (OR = 1.573, 95% CI: 1.113, 2.223, p = 0.010).
Limitations: Screening tools rather than standard diagnostic procedures were used in the study. Moreover, the long-term associations still need further exploration since the follow-up time was short.
Conclusions: Increased depressive symptoms were associated with more cognitive decline and higher risks of incident MCI among Chinese rural residents.
Introduction
Alzheimer's disease (AD) is a significant and common public health threat worldwide, not only creating enormous physical, emotional and economical stress for individuals and their families but also imposing a very large disease burden on societies. In China, the number of people living with AD has been projected to be 300 million, with a disease burden as high as 2000 billion RMB in 2050 (1). Due to the slow progress toward curing AD, preventive strategies through elucidating and modifying its risk factors might be the key response initiatives to combat AD (2). Mild cognitive impairment (MCI) has been regarded as a predementia stage of great public health importance (3, 4), because individuals with MCI have the potential to regain normal cognitive function if early and effective interventions can be taken (5).
Depression and cognitive decline often present together (6–8), indicating the possible close relationship between them, although the exact mechanism seems to be complicated and needs further exploration. Many studies have suggested that depressive symptoms increase the risk of cognitive impairment through pathways of immune dysregulation, which may simultaneously drive other comorbid medical conditions (9, 10). However, some researchers hold the view that depression is one of the prodromes of cognitive decline because people with depression show a negative bias in information processing that affects their attention, memory, and response to feedback (11). Additional evidence has revealed that depressive symptoms play a major role in the progression of MCI to AD (12, 13); thus, depression has been regarded as a predictor of progressive cognitive decline (14, 15).
Despite relatively numerous studies on the relationship between depression and cognitive decline, a few gaps exist in the literature. First, although depression is very common among elderly individuals (16), available studies are often limited to middle-aged people (17), clinical patients (18), and urban areas (19, 20). In addition, longitudinal studies, which are essential to investigate the causal effect of depression on the onset of cognitive decline, are still insufficient (21, 22). Although several longitudinal studies have implied a relationship between depression and cognitive decline (23, 24), evidence from less developed areas, e.g., rural China, is still very rare.
Therefore, in the current study, we aimed to explore the relationship between depression and cognitive decline and the incidence of MCI among a rural Chinese elderly sample through a longitudinal study with 2-year follow-up, particularly to determine whether baseline depression and depression status change were associated with cognitive decline and MCI incidence. The findings of the current study might contribute to preventing MCI and slowing the development of AD among older adults in rural areas.
Methods
Study Population
The present study was based on data collected from the Anhui Healthy Longevity Survey (AHLS), the details of which have been reported elsewhere (25). Briefly, 6,211 participants who were aged 60 or higher were initially enrolled from four cities (Chuzhou, Lu'an, Xuancheng, and Fuyang) in July 2019. After approximately two years, the follow-up visit (wave 1) was conducted the participants from rural areas of the three cities (Chuzhou, Lu'an and Xuancheng). Among the 2,308 rural participants who were investigated at baseline, 1,566 participants completed the follow-up in 2021, for a response rate of 67.9% (742 participants were lost to follow-up, including 88 cases of death, 23 cases of loss of communication ability, 201 cases of migration and 430 cases of refusal to participate).
In the current study, we further excluded the participants if they (1) were not able to finish the cognitive function assessment or depressive symptoms assessment (n = 16) or (2) had any missing covariate data (n = 73). Finally, 1,477 participants were included in the analysis, and none of them reported a previous history of depression or cognitive impairment. For the analysis of the relationship between depression and 2-year MCI incidence, the participants with pre-existing MCI at baseline (n = 983) were excluded. All the procedures complied with the ethical standards of the Anhui Medical University committee (No. 2020H011).
Assessment of Depressive Symptoms
The Patient Health Questionnaire (PHQ-9) (26) was used to measure the depression symptoms of the participants at baseline and at follow-up. The instrument assessed the severity of depression by asking about the frequency of occurrence of the major symptoms of depression within the last two weeks. The total score of the PHQ-9 is 30, with higher scores indicating more severe depression symptoms. The Cronbach's α was 0.89 in the pilot study, showing the appropriate internal consistency of the PHQ-9 scale. For the current analysis, total PHQ-9 scores were categorized as “not depressed” (0–4) and “depressed” (5–30).
The depression score change was calculated by the formula
i = P − Q where, P = PHQ-9 score at follow up; Q = PHQ-9 score at baseline.
A greater value of i indicates an increase in PHQ-9 scores at follow-up, i.e., more elevated depressive symptoms. Worsening depressive symptoms were classified into “None” (i was ≤ 0) and “Yes” (i was higher than 0).
Assessment of Cognitive Function
The cognitive status of the participants was evaluated by the Mini Mental State Examination (MMSE) (27) at baseline and at follow-up. The MMSE was the most widely used tool for cognition assessment, with good accuracy in the detection of dementia (sensitivity and specificity were 87 and 89%, respectively) (28) as well as in MCI (sensitivity and specificity were 79.8 and 81.3% respectively) (29). A previous study concluded good applicability of MMSE as a cognitive function screen instrument in community settings of China (30). The total score of the MMSE scale is 30 points, with higher scores indicating better cognitive function. The Cronbach's α was 0.69 in the pilot study, showing the acceptable internal consistency of the MMSE. In the current study, the education-based criterion for MCI was adopted due to the potential impact of educational level (31). Specifically, MCI was determined if the participants were illiterate and had MMSE scores <18, if they had 1–6 years of education and had MMSE scores lower than 21, or if they had 6 or more years of education with MMSE scores lower than 25 (32).
Two-year cognitive change and MCI incidence were also identified according to the measurement of MMSE scores at baseline and at follow-up. The changes in MMSE scores were calculated by the formula
j = M E where, M = MMSE score at baseline; E = MMSE score at follow-up.
A greater value of j indicates a larger decrease in the MMSE score after 2 years of follow-up, i.e., a severe decline in cognitive performance.
The participants who were free of MCI at baseline and classified as having MCI at follow-up were judged as having incident MCI. The participants were divided into two groups (yes, no) according to whether they developed MCI within the 2-year follow-up.
Assessment of Covariates
Baseline data of sociodemographic characteristics (city, sex, age, education, marital status, annual income, and living alone), behavioral factors [body mass index (BMI), drinking, smoking, sedentary hours, self-rated sleep quality], and chronic conditions (diabetes and hypertension) were treated as covariates. Age was self-reported by the participants. Education was divided into three groups according to the participant's years of formal education (low: 0, medium: 1–6 years and high: more than 6 years). Marital status was classified into married and others (including divorce, widowed and never married). Annual income was classified into two groups (lower than 6,500 RMB and 6,500 RMB or higher). Living alone was assessed by asking the participants “Do you live alone?” The options were “yes” and “no.” BMI was calculated by measuring height and weight by the formula weight (kg)/height (m)2 and introduced as a continuous variable. Drinking status was dichotomized as never, former, and current. Smoking was classified into two groups (yes and no) according to whether they smoked. Self-rated sleep quality was assessed by asking the participants “How do you evaluate your sleep quality in the last month?” The options were “very good,” “good,” and “not good.” Continuous daily sitting time was self-reported and used as an indicator reflecting the physical activity status of the participants. Two chronic conditions (hypertension and diabetes) were divided into two groups (yes and no) according to whether the participants had been diagnosed with hypertension/diabetes at a hospital at the county level or above.
Statistical Analyses
Multivariable linear regression and logistic regression were employed to assess the associations between depressive symptoms and cognition by including 2-year cognitive decline and MCI incidence as dependent variables, respectively. The baseline PHQ-9 score and changes in PHQ-9 scores (i) were treated as independent variables and introduced into the regression models together with all the covariates. The regression models used simultaneous entry of variables (enter method). Since many studies have indicated that sex and age might be related to cognitive decline and depression (33–35), sex- and age-stratified analyses were also performed. In addition, accumulating evidence suggested that having more years of education is a protective factor for cognitive impairment (36, 37); thus, additional analyses stratified by education levels were also conducted to examine the associations in different subgroups.
Stata version 15.1 software (Stata Corp, College Station, TX) was used for all analyses. All the tests were two-sided, and the significance level was set at p < 0.05.
Results
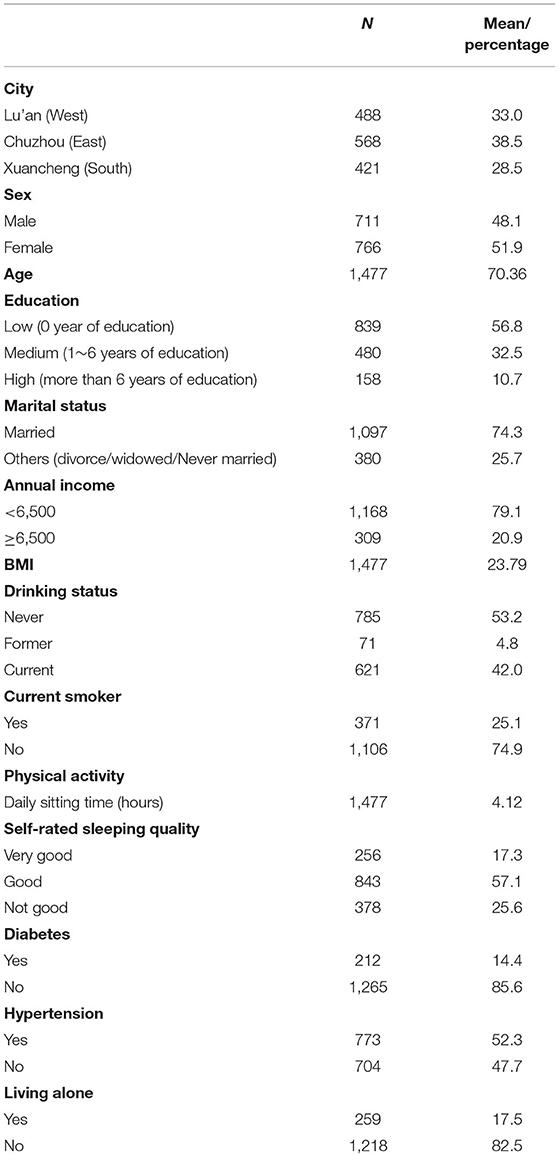
Table 1 presents the basic characteristics of the study sample (n = 1,477). The mean age of the participants was 70.36 years, and 51.9% of the participants were women. More than half of the participants (56.8%) enrolled in the current study were illiterate. The mean BMI of the participants was 23.79 kg/m2. A total of 14.4% of the participants reported having diabetes, and more than half of the participants (52.3%) reported having high blood pressure.
The associations between depression status at baseline and at follow-up and cognitive function are shown in Table 2. Depression status at baseline was not associated with two-year cognitive decline or MCI incidence. For depression status at follow-up, every 1-unit PHQ-9 score increase was significantly associated with a larger 2-year cognitive decline (β = 0.157, 95% CI: 0.092, 0.221, p < 0.001) and a higher risk of MCI incidence (OR = 1.063, 95% CI: 1.025, 1.103, p = 0.001). The participants who experienced worsening depressive symptoms had a larger decline in the 2-year MMSE score (β = 0.650, 95% CI: 0.039, 1.261, p = 0.037) and elevated risks of incident MCI (OR = 1.573, 95% CI: 1.113, 2.223, p = 0.010).
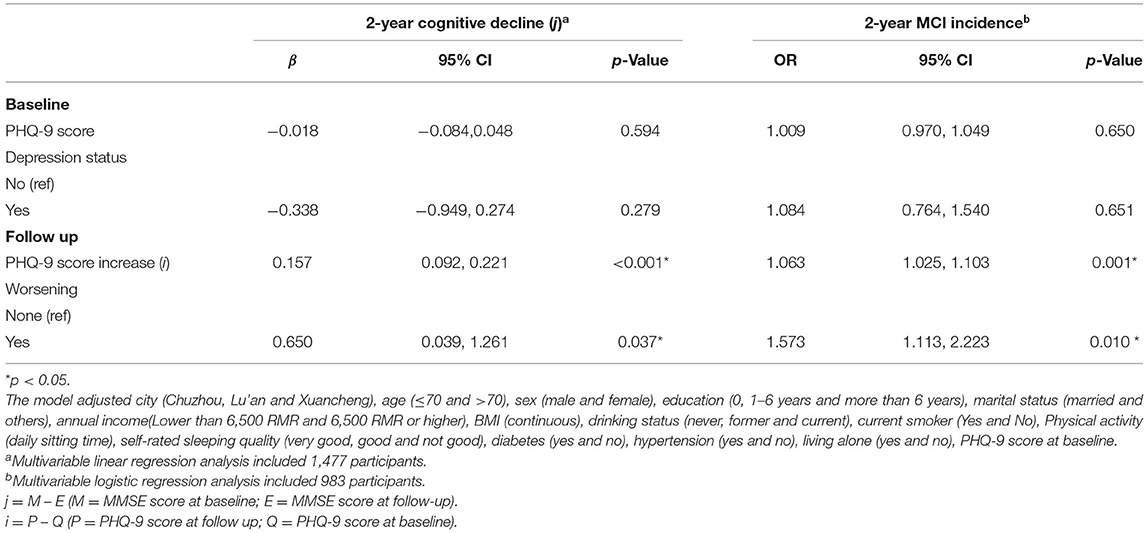
Table 2. The associations between depression and cognitive function: Coefficients and 95% CIs for 2-year cognitive decline and Odds Ratios and 95% CIs for 2-year MCI incidence.
Table 3 shows the results of the sex-stratified analysis. No significant association was detected between baseline depression and cognitive decline and 2-year MCI incidence for either males or females. For males, PHQ-9 score increases were associated with cognitive decline (β = 0.277, 95% CI: 0.128, 0.326, p < 0.001) and 2-year MCI incidence (OR = 1.103, 95% CI: 1.041, 1.168, p = 0.001), whereas PHQ-9 score increases were associated with only 2-year cognitive decline among females (β = 0.103, 95% CI: 0.015, 0.190, p = 0.022). Experienced worsening depression symptoms was associated with a significant larger decline in the 2-year MMSE score in males (β = 1.016, 95% CI: 0.135, 1.897, p = 0.024) but not in females.
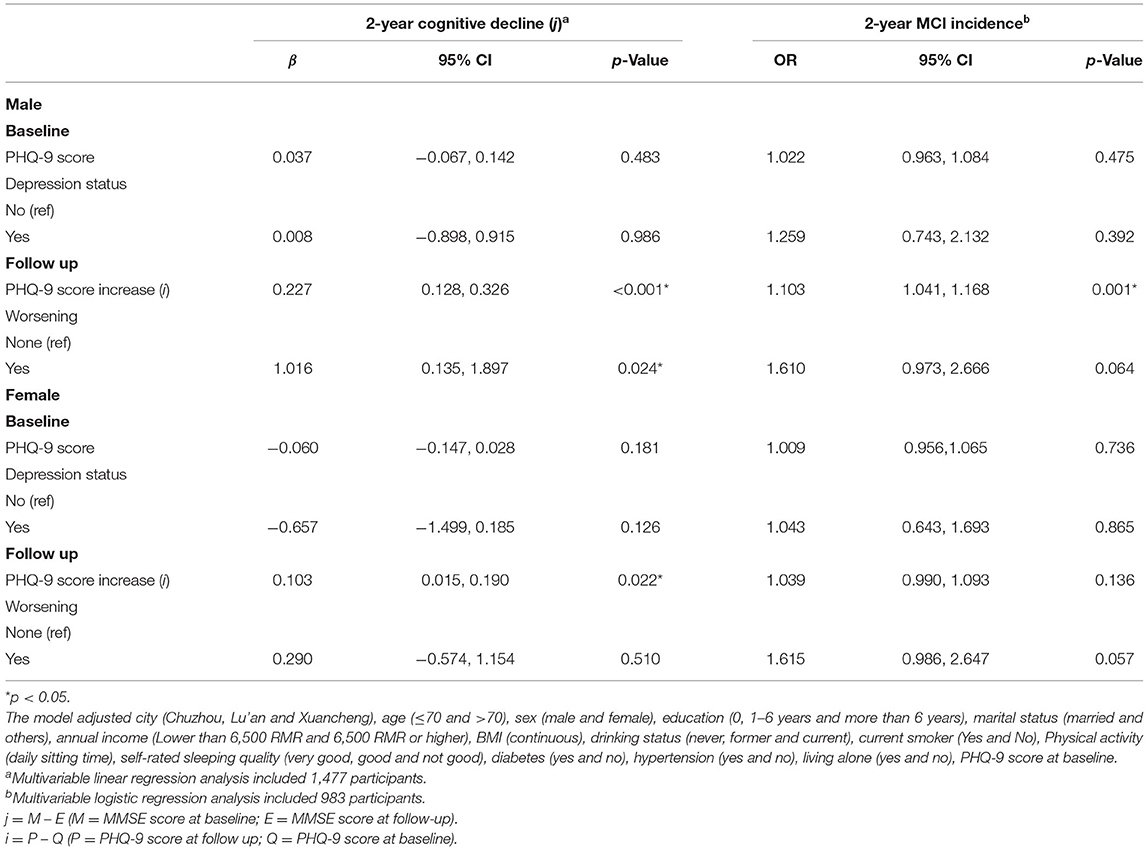
Table 3. The associations between depression and cognitive function by sexes: Coefficients and 95% CIs for 2-year cognitive decline and Odds Ratios and 95% CIs for 2-year MCI incidence.
The results of the age-stratified analysis are shown in Table 4. For both the older group (aged 70 and older) and younger group (aged under 70), baseline depression status was associated with neither 2-year cognitive decline nor MCI incidence. For both of the age-stratified groups, PHQ-9 score increases were associated with 2-year cognitive decline: for the participants who were under 70, a 1-unit PHQ-9 score increase was significantly associated with a 2-year MMSE score decline of 0.135 (β = 0.135, 95% CI: 0.051,0.220, p = 0.002), and for those who were aged 70 and older, a 1-unit PHQ-9 score increase was significantly associated with a 0.168-unit MMSE score decline (β = 0.168, 95% CI: 0.066, 0.270, p = 0.001). Whereas PHQ-9 score increases were only associated with 2-year MCI incidence in older group (OR = 1.062, 95% CI: 1.005, 1.222, p = 0.033) but not in younger group. Worsening depressive symptoms was not statistically associated with 2-year cognitive decline or MCI incidence for either the older or younger group.
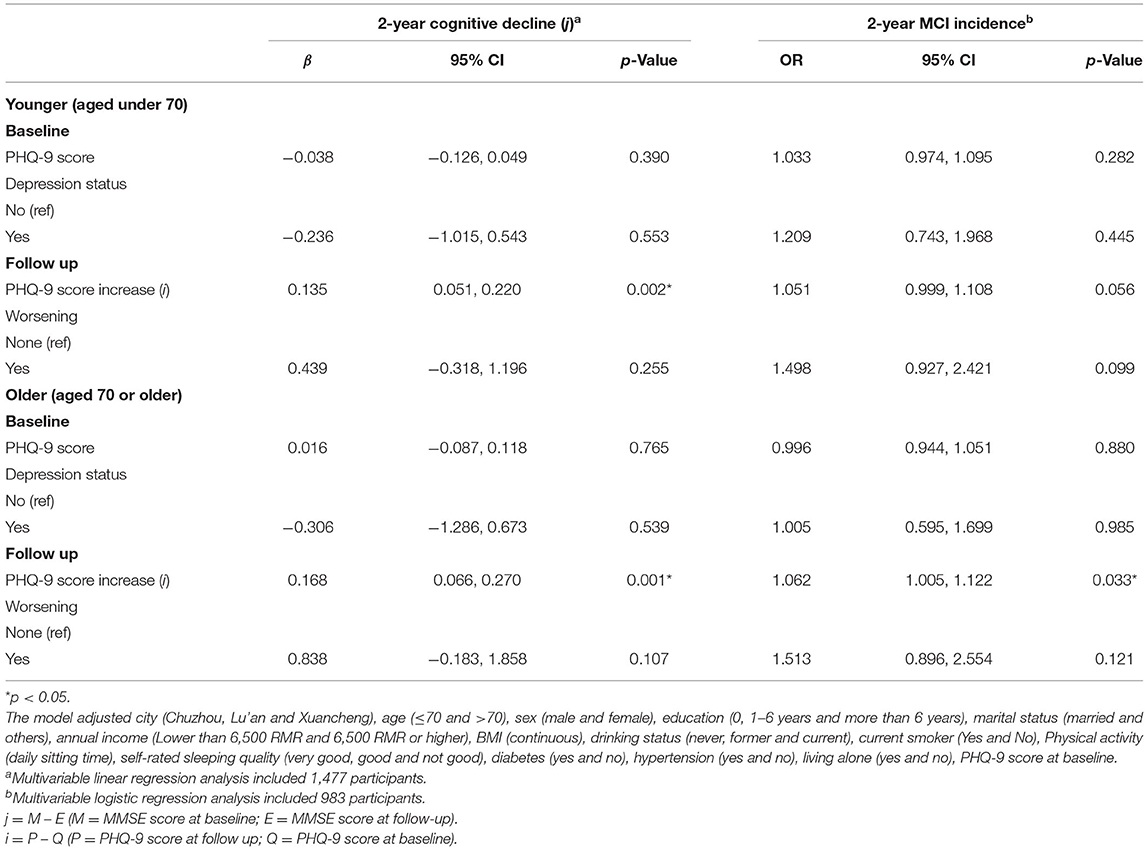
Table 4. The associations between depression and cognitive function by age: Coefficients and 95% CIs for 2-year cognitive decline and Odds Ratios and 95% CIs for 2-year MCI incidence.
The results of the analysis stratified by different education levels are shown in Supplementary Table S1. Baseline depression was not associated with cognitive decline and 2-year MCI incidence in the three subgroups. For those who were categorized into the low education group, PHQ-9 score increases were significantly associated with cognitive decline (β = 0.124, 95% CI: 0.036, 0.212, p = 0.006) and 2-year MCI incidence (OR = 1.066, 95% CI: 1.018, 1.118, p = 0.007), whereas this factor was only associated with 2-year cognitive decline (β = 0.207, 95% CI: 0.097, 0.317, p < 0.001) among the participants who had a medium education level. For those who had a high education level, PHQ-9 score increases were only associated with 2-year MCI incidence (OR = 1.272, 95% CI: 1.028, 1.573, p = 0.027). Experiencing worsening depressive symptoms was associated with elevated risks of 2-year MCI incident only among those who were categorized in the low education group (OR = 2.184, 95% CI: 1.362, 3.503, p = 0.001).
Discussion
In this longitudinal study with 2-year follow-up, aggravated depressive symptoms were associated with greater cognitive decline and an increased MCI incidence among rural elderly people. Many previous studies have suggested a higher prevalence of depression and cognitive impairment in rural areas than in urban areas in China (38–42). Considering the relatively lower educational level of rural dwellers as well as the barriers due to the constraints of the economy and medical resources in rural regions (43, 44), urban-rural disparities will further expand if effective intervention are not adopted. The current study was the first to investigate the longitudinal associations between depressive symptoms and cognition among Chinese rural elderly individuals.
Consistent with our findings, longitudinal associations between increased depressive symptoms and cognitive decline as well as higher MCI risks have been revealed in many studies (20, 45, 46). However, baseline depression status was not associated with cognitive decline or MCI incidence in this study, which contradicts some studies (21, 47). This might be attributed to the relatively short follow-up duration (2 years) and may also be related to different screening tools for depression assessment, differences in study design and sample size, and heterogeneity of the population.
Similar to many studies (34, 48), in the current study, sex disparities were also found in the associations between depression and cognition, which might be explained through biological or psychosocial pathways. A previous study reported that a type of vascular depression among males might be linked to cerebral vascular pathology, which in turn accelerated the process of cognitive decline, although this phenomenon was not investigated among females (49). Underreported depression symptoms due to the gender bias in reporting depressive symptoms might also contribute to sex disparities since males tend to be unwilling to express their discomfort due to the influences of societal expectations (50). Although some studies reported age-modified associations between depression and cognition (35, 51), in the current study, increased depression symptoms were similarly associated with more cognitive decline among different age groups. Some previous studies reported education-modified associations between depression and cognition (36, 52). Similarly, education level moderated associations between depression symptoms and cognition decline were also detected in the current study.
The strengths of the present study include the prospective study design with a 2-year follow-up period and the relatively high follow-up rate. Moreover, depression symptoms were measured at baseline and at follow-up so that the 2-year change in depressive symptoms could be investigated. However, this study also has several limitations. First, the widely used MMSE was used for assessing the cognitive performance of the participants. However, the MMSE is not a diagnostic tool, although the validity of MMSE has been verified by many studies worldwide. This limitation makes it difficult to grasp the true associations between depression symptoms and cognitive decline. A standard diagnostic procedure should be considered in future studies to achieve a more reliable conclusion. Second, reverse causation cannot be totally avoided due to the short period of follow-up. Future studies addressing the long-term relationship between depression and cognition are still needed. Finally, many studies indicated that some neurological and endocrine conditions might affect the associations, for example, stroke (53, 54) and hypothyroidism (55, 56) might lead to both depression and cognitive impairment; however, such conditions were not considered in the present study. Additionally, some genetic factors were not included in the current study. Future studies conducted under a more comprehensive framework with additional measurements such as blood tests and neuroimaging are needed to verify the associations.
Conclusion
Worsening depressive symptoms were related to more cognitive decline and a higher risk of incident MCI among rural-dwelling Chinese elderly individuals. Our study highlighted the great importance of depression intervention for preventing cognitive impairment in Chinese elderly individuals living in rural areas. Considering the significant vulnerability of Chinese rural-dwelling elderly individuals, special attention should be given to providing health services regarding effective interventions to reduce depression to combat AD challenges in the future.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
SZ drafted the manuscript. SH, GS, and YZ framed the concept and designed the study. The data collection and material preparation were conducted by SZ, QioW, QinW, and JZ and the data analysis was performed by FH and YZ. All authors meet the criteria for authorship according to their contributions to the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the National Natural Science Foundation of China, Grant Number 72004003 to YZ, the Key Projects of Science and the Key Project of Science and Technology of Anhui Province, Grant Number 2019b11030012 to SH, Gant Number 202004b11020019 to GS, and the Hefei Municipal Natural Science Foundation, Grant Number 2021005 to GS, and the APC was funded by GS.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank all participants in the AHLS for their cooperation and data sharing. We also thank all the colleagues for their time and efforts on data collection and project management.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.939150/full#supplementary-material
References
1. Jia J, Wei C, Chen S, Li F, Tang Y, Qin W, et al. The cost of Alzheimer's disease in China and re-estimation of costs worldwide. Alzheimers Dement. (2018) 14:483–91. doi: 10.1016/j.jalz.2017.12.006
2. Diniz BS, Butters MA, Albert SM, Dew MA, Reynolds CF 3rd. Late-life depression and risk of vascular dementia and Alzheimer's disease: systematic review and meta-analysis of community-based cohort studies. Br J Psychiatry. (2013) 202:329–35. doi: 10.1192/bjp.bp.112.118307
3. Sanford AM. Mild cognitive impairment. Clin Geriatr Med. (2017) 33:325–37. doi: 10.1016/j.cger.2017.02.005
4. Demurtas J, Schoene D, Torbahn G, Marengoni A, Grande G, Zou L, et al. Physical activity and exercise in mild cognitive impairment and dementia: an umbrella review of intervention and observational studies. J Am Med Dir Assoc. (2020) 21:1415–22.e6. doi: 10.1016/j.jamda.2020.08.031
5. Anderson ND. State of the science on mild cognitive impairment (MCI). CNS Spectrums. (2019) 24:78–87. doi: 10.1017/S1092852918001347
6. Ismail Z, Elbayoumi H, Fischer CE, Hogan DB, Millikin CP, Schweizer T, et al. Prevalence of depression in patients with mild cognitive impairment: a systematic review and meta-analysis. JAMA Psychiatry. (2017) 74:58–67. doi: 10.1001/jamapsychiatry.2016.3162
7. Panza F, Frisardi V, Capurso C, D'Introno A, Colacicco AM, Imbimbo BP, et al. Late-life depression, mild cognitive impairment, and dementia: possible continuum? Am J Geriatr Psychiatry. (2010) 18:98–116. doi: 10.1097/JGP.0b013e3181b0fa13
8. Steffens DC. Depressive symptoms and mild cognitive impairment in the elderly: an ominous combination. Biol Psychiatry. (2012) 71:762–4. doi: 10.1016/j.biopsych.2012.02.002
9. Smith RS. The macrophage theory of depression. Med Hypotheses. (1991) 35:298–306. doi: 10.1016/0306-9877(91)90272-Z
10. Hayley S, Hakim AM, Albert PR. Depression, dementia and immune dysregulation. Brain. (2021) 144:746–60. doi: 10.1093/brain/awaa405
11. Dehn LB, Beblo T. Depressed, biased, forgetful: The interaction of emotional and cognitive dysfunctions in depression. Neuropsychiatrie. (2019) 33:123–30. doi: 10.1007/s40211-019-0307-4
12. Ismail Z, Malick A, Smith EE, Schweizer T, Fischer C. Depression versus dementia: is this construct still relevant? Neurodegener Dis Manag. (2014) 4:119–26. doi: 10.2217/nmt.14.5
13. Mourao RJ, Mansur G, Malloy-Diniz LF, Castro Costa E, Diniz BS. Depressive symptoms increase the risk of progression to dementia in subjects with mild cognitive impairment: systematic review and meta-analysis. Int J Geriatr Psychiatry. (2016) 31:905–11. doi: 10.1002/gps.4406
14. Hu M, Shu X, Wu X, Chen F, Hu H, Zhang J, et al. Neuropsychiatric symptoms as prognostic makers for the elderly with mild cognitive impairment: a meta-analysis. J Affect Disord. (2020) 271:185–92. doi: 10.1016/j.jad.2020.03.061
15. Ismail Z, Gatchel J, Bateman DR, Barcelos-Ferreira R, Cantillon M, Jaeger J, et al. Affective and emotional dysregulation as pre-dementia risk markers: exploring the mild behavioral impairment symptoms of depression, anxiety, irritability, and euphoria. Int Psychogeriatr. (2018) 30:185–96. doi: 10.1017/S1041610217001880
16. Udeh-Momoh C, Price G, Ropacki MT, Ketter N, Andrews T, Arrighi HM, et al. Prospective evaluation of cognitive health and related factors in elderly at risk for developing Alzheimer's dementia: a longitudinal cohort study. J Prev Alzheimers Dis. (2019) 6:256–66. doi: 10.14283/jpad.2019.31
17. Aguilera M, Paz C, Compañ V, Medina JC, Feixas G. Cognitive rigidity in patients with depression and fibromyalgia. Int J Clin Health Psychol. (2019) 19:160–4. doi: 10.1016/j.ijchp.2019.02.002
18. Egan SJ, Laidlaw K, Starkstein S. Cognitive behaviour therapy for depression and anxiety in parkinson's disease. J Parkinsons Dis. (2015) 5:443–51. 10.3233/JPD-150542. doi: 10.3233/JPD-150542
19. Sundermann EE, Katz MJ, Lipton RB. Sex differences in the relationship between depressive symptoms and risk of amnestic mild cognitive impairment. Am J Geriatr Psychiatry. (2017) 25:13–22. doi: 10.1016/j.jagp.2016.08.022
20. Makizako H, Shimada H, Doi T, Tsutsumimoto K, Hotta R, Nakakubo S, et al. Comorbid mild cognitive impairment and depressive symptoms predict future dementia in community older adults: a 24-Month follow-up longitudinal study. J Alzheimers Dis. (2016) 54:1473–82. doi: 10.3233/JAD-160244
21. Vloeberghs R, Opmeer EM, De Deyn PP, Engelborghs S, De Roeck EE. Apathy, depression and cognitive functioning in patients with MCI and dementia. Tijdschr Gerontol Geriatr. (2018) 49:95–102. doi: 10.1007/s12439-018-0248-6
22. Aajami Z, Kazazi L, Toroski M, Bahrami M, Borhaninejad V. Relationship between depression and cognitive impairment among elderly: a cross-sectional study. J Caring Sci. (2020) 9:148–53. doi: 10.34172/jcs.2020.022
23. Yaffe K, Blackwell T, Gore R, Sands L, Reus V, Browner WS. Depressive symptoms and cognitive decline in nondemented elderly women: a prospective study. Arch Gen Psychiatry. (1999) 56:425–30. doi: 10.1001/archpsyc.56.5.425
24. Wilson RS, Barnes LL, Mendes de., Leon CF, Aggarwal NT, Schneider JS, Bach J, et al. Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology. (2002) 59:364–70. doi: 10.1212/WNL.59.3.364
25. Fangfang H, Xiao H, Shuai Z, Qiong W, Jingya Z, Guodong S, et al. Living Environment, Built environment and cognitive function among older Chinese adults: results from a cross-sectional study. J Prev Alzheimers Dis. (2022) 9:126–35. doi: 10.14283/jpad.2021.59
26. Levis B, Benedetti A, Thombs BD. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
27. Arevalo-Rodriguez I, Smailagic N, Roqué IFM, Ciapponi A, Sanchez-Perez E, Giannakou A, et al. Mini-mental state examination (MMSE) for the detection of Alzheimer's disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. (2015) 2015:Cd010783. doi: 10.1002/14651858.CD010783.pub2
28. Huo Z, Lin J, Bat BKK, Chan JYC, Tsoi KKF, Yip BHK. Diagnostic accuracy of dementia screening tools in the Chinese population: a systematic review and meta-analysis of 167 diagnostic studies. Age Ageing. (2021) 50:1093–101. doi: 10.1093/ageing/afab005
29. Mitchell AJ. A meta-analysis of the accuracy of the mini-mental state examination in the detection of dementia and mild cognitive impairment. J Psychiatr Res. (2009) 43:411–31. doi: 10.1016/j.jpsychires.2008.04.014
30. Lu L, Chen L, Wu W, Wang Y, Liu Z, Xu J, et al. Consistency and applicability of different brief screen instrument of cognitive function in elderly population. BMC Neurol. (2021) 21:95. doi: 10.1186/s12883-021-02048-4
31. Bravo G, Hébert R. Age- and education-specific reference values for the Mini-Mental and modified mini-mental state examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry. (1997) 12:1008–18. doi: 10.1002/(sici)1099-1166(199710)12:10<1008::aid-gps676>3.0.co;2-a
32. Zhang MY, Katzman R, Salmon D, Jin H, Cai GJ, Wang ZY, et al. The prevalence of dementia and Alzheimer's disease in Shanghai, China: impact of age, gender, and education. Ann Neurol. (1990) 27:428–37. doi: 10.1002/ana.410270412
33. Fuhrer R, Antonucci TC, Gagnon M, Dartigues JF, Barberger-Gateau P, Alperovitch A. Depressive symptomatology and cognitive functioning: an epidemiological survey in an elderly community sample in France. Psychol Med. (1992) 22:159–72. doi: 10.1017/S0033291700032815
34. Geda YE, Knopman DS, Mrazek DA, Jicha GA, Smith GE, Negash S, et al. Depression, apolipoprotein E genotype, and the incidence of mild cognitive impairment: a prospective cohort study. Arch Neurol. (2006) 63:435–40. doi: 10.1001/archneur.63.3.435
35. Eraydin IE, Mueller C, Corbett A, Ballard C, Brooker H, Wesnes K, et al. Investigating the relationship between age of onset of depressive disorder and cognitive function. Int J Geriatr Psychiatry. (2019) 34:38–46. doi: 10.1002/gps.4979
36. Jansen MG, Geerligs L, Claassen J, Overdorp EJ, Brazil IA, Kessels RPC, et al. Positive effects of education on cognitive functioning depend on clinical status and neuropathological severity. Front Hum Neurosci. (2021) 15:723728. doi: 10.3389/fnhum.2021.723728
37. Staekenborg SS, Kelly N, Schuur J, Koster P, Scherder E, Tielkes CEM, et al. Education as proxy for cognitive reserve in a large elderly memory clinic: 'window of benefit'. J Alzheimers Dis. (2020) 76:671–9. doi: 10.3233/JAD-191332
38. Dong X, Simon MA. Health and aging in a Chinese population: urban and rural disparities. Geriatr Gerontol Int. (2010) 10:85–93. doi: 10.1111/j.1447-0594.2009.00563.x
39. Li N, Pang L, Chen G, Song X, Zhang J, Zheng X. Risk factors for depression in older adults in Beijing. Canad J Psychiatry. (2011) 56:466–73. doi: 10.1177/070674371105600804
40. Chen R, Wei L, Hu Z, Qin X, Copeland JR, Hemingway H. Depression in older people in rural China. Arch Intern Med. (2005) 165:2019–25. doi: 10.1001/archinte.165.17.2019
41. Zhang L, Xu Y, Nie H, Zhang Y, Wu Y. The prevalence of depressive symptoms among the older in China: a meta-analysis. Int J Geriatr Psychiatry. (2012) 27:900–6. doi: 10.1002/gps.2821
42. Saenz JL, Downer B, Garcia MA, Wong R. Cognition and context: rural-Urban differences in cognitive aging among older Mexican adults. J Aging Health. (2018) 30:965–86. doi: 10.1177/0898264317703560
43. Galvin JE, Fu Q, Nguyen JT, Glasheen C, Scharff DP. Psychosocial determinants of intention to screen for Alzheimer's disease. Alzheimers Dement. (2008) 4:353–60. doi: 10.1016/j.jalz.2007.09.005
44. Kirk Wiese L, Williams CL, Tappen RM. Analysis of barriers to cognitive screening in rural populations in the United States. ANS Adv Nurs Sci. (2014) 37:327–39. doi: 10.1097/ANS.0000000000000049
45. Han FF, Wang HX, Wu JJ, Yao W, Hao CF, Pei JJ. Depressive symptoms and cognitive impairment: a 10-year follow-up study from the survey of health, ageing and retirement in Europe. Eur Psychiatry. (2021) 64:e55. doi: 10.1192/j.eurpsy.2021.2230
46. Lara E, Koyanagi A, Domènech-Abella J, Miret M, Ayuso-Mateos JL, Haro JM. The Impact of depression on the development of mild cognitive impairment over 3 years of follow-up: a population-based study. Dement Geriatr Cogn Disord. (2017) 43:155–69. doi: 10.1159/000455227
47. Lee CH, Kim DH, Moon YS. Differential associations between depression and cognitive function in MCI and AD: a cross-sectional study. Int Psychogeriatr. (2019) 31:1151–8. doi: 10.1017/S1041610218001527
48. Dal Forno G, Palermo MT, Donohue JE, Karagiozis H, Zonderman AB, Kawas CH. Depressive symptoms, sex, and risk for Alzheimer's disease. Ann Neurol. (2005) 57:381–7. doi: 10.1002/ana.20405
49. Fuhrer R, Dufouil C, Dartigues JF. Exploring sex differences in the relationship between depressive symptoms and dementia incidence: prospective results from the PAQUID Study. J Am Geriatr Soc. (2003) 51:1055–63. doi: 10.1046/j.1532-5415.2003.51352.x
50. Joiner TE Jr., Alfano MS, Metalsky GI. When depression breeds contempt: reassurance seeking, self-esteem, and rejection of depressed college students by their roommates. J Abnorm Psychol. (1992) 101:165–73. doi: 10.1037/0021-843X.101.1.165
51. Lugtenburg A, Zuidersma M, Wardenaar KJ, Aprahamian I, Rhebergen D, Schoevers RA, et al. Subtypes of late-life depression: a data-driven approach on cognitive domains and physical frailty. J Gerontol A Biol Sci Med Sci. (2021) 76:141–50. doi: 10.1093/gerona/glaa110
52. da Costa Dias FL, Teixeira AL, Guimarães HC, Santos APB, Resende EPF, Machado JCB, et al. The influence of age, sex and education on the phenomenology of depressive symptoms in a population-based sample aged 75+ years with major depression: the Pietà Study. Aging Ment Health. (2021) 25:462–7. doi: 10.1080/13607863.2019.1698517
53. Makin SD, Turpin S, Dennis MS, Wardlaw JM. Cognitive impairment after lacunar stroke: systematic review and meta-analysis of incidence, prevalence and comparison with other stroke subtypes. J Neurol Neurosurg Psychiatry. (2013) 84:893–900. doi: 10.1136/jnnp-2012-303645
54. Das J, Rajanikant GK. Post stroke depression: the sequelae of cerebral stroke. Neurosci Biobehav Rev. (2018) 90:104–14. doi: 10.1016/j.neubiorev.2018.04.005
55. Gorkhali B, Sharma S, Amatya M, Acharya D, Sharma M. Anxiety and depression among patients with thyroid function disorders. J Nepal Health Res Counc. (2020) 18:373–8. doi: 10.33314/jnhrc.v18i3.2499
Keywords: depression, mild cognitive impairment, elderly, rural area, Alzheimer's disease
Citation: Zhou S, Wang Q, Zhang J, Wang Q, Hou F, Han X, Hu S, Shen G and Zhang Y (2022) Depressive Symptoms and Cognitive Decline Among Chinese Rural Elderly Individuals: A Longitudinal Study With 2-Year Follow-Up. Front. Public Health 10:939150. doi: 10.3389/fpubh.2022.939150
Received: 08 May 2022; Accepted: 22 June 2022;
Published: 13 July 2022.
Edited by:
Rosa Magallon, University of Zaragoza, SpainReviewed by:
Carlos Márquez, University of Chile, ChileMasaraf Hussain, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, India
Copyright © 2022 Zhou, Wang, Zhang, Wang, Hou, Han, Hu, Shen and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shilian Hu, aHVzaGlsaWFuQDEyNi5jb20=; Guodong Shen, Z2RzaGVuQHVzdGMuZWR1LmNu; Yan Zhang, emhhbmd5bWFpbEBhaG11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Shuai Zhou1†
Shuai Zhou1† Guodong Shen
Guodong Shen Yan Zhang
Yan Zhang