- 1Department of Public Health, Directorate of Health Affairs in Taif, Ministry of Health, Riyadh, Saudi Arabia
- 2Department of Biomedical Informatics and Medical Statistics, Medical Research Institute, Alexandria University, Alexandria, Egypt
- 3Department of Nutrition, High Institute of Public Health, Alexandria University, Alexandria, Egypt
Background: Disordered eating behaviors (DEBs) are complex health issues that may lead to negative physical and mental health outcomes among college students. More studies should be directed toward the screening of DEBs. This study aimed to determine the prevalence of DEBs among Saudi female university students and their association with social networking site (SNSs) usage and composite lifestyle behaviors during the unprecedented period of COVID-19.
Methods: This cross-sectional study included 445 females recruited using stratified random sampling. The participants self-reported demographic, social, medical, and lifestyle data and completed the validated Arabic version of the Eating Attitudes Test-26, Social Networking Sites (SNSs) Usage Questionnaire, Bergen Social Media Addiction Scale, and Body Shape Questionnaire.
Results: The prevalence of DEBs was 27.2% among the female students at Taif University. From the pre-pandemic period until the current time, the DEBs-risk group had a significantly higher SNS navigation rate (36.4%) than the normal group (20.4%) (X2 = 30.015, p = 0.001). The regression analysis revealed that females with a significant body image concern, higher number of SNSs friends, and frequent visits to SNSs, and those seeking social-dependent information in relation to weight loss/dieting were more likely to develop DEBs (Overall Model: Chi-Square X2 = 158.071, p < 0.000**).
Conclusions: SNSs usage and DEBs were associated during the COVID-pandemic. However, the composite lifestyle score did not demonstrate a significant association with DEBs among the female students at Taif University. Investigating the magnitude of DEBs and understanding the role of SNS are essential for preventing disordered eating among young females.
Introduction
Disordered eating behaviors (DEBs) or high-risk disordered eating refers to problematic eating habits that are less severe in their behavioral manifestations than those required to meet the full criteria for the diagnosis of an eating disorder (ED) on the basis of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). It includes unhealthy eating habits such as fasting, restrictive dieting, skipping meals, compulsive overeating, unbalanced eating, vomiting, misuse of laxatives, diuretics, enemas, and the use of diet pills to lose weight (1).
DEBs are proven risk factors for EDs. Dieting and other obsessive weight control practices, fears of fatness, negative body image, and intensive food and weight preoccupation are types of eating impairments associated with an increased risk of developing anorexia and bulimia nervosa (2). In 2019, a systematic review of population-based studies revealed that EDs increases the vulnerability to psychiatric illnesses, diabetes, weight fluctuations, poor nutritional intake and quality, obesity, suicide, and other forms of premature mortality (3).
The prevalence of EDs ranged from 4.6% in the U.S. to 3.5% in Asia and 2.2% in Europe (4, 5). The prevalence of clinically diagnosed EDs is low; however, DEBs are prevalent among college-aged adolescents and young females (6). In a recent systematic review and meta-analysis conducted in the Middle East (16 countries including Saudi Arabia), the overall prevalence rate of DEBs was 22.07%, which was relatively higher than the global prevalence rate (7). Previous studies on female Saudi university students using the EAT-26 tool revealed that 35.4, 29.4, and 25.4% of them, demonstrated DEBs (8–10).
In a recent study conducted during the COVID-19 pandemic (2022), out of 1004 Saudi females, approximately 31.5% were at risk of developing EDs (11). Studies on DEBs-associated factors have focused mainly on socio-demographic factors (e.g., college-aged females), sociocultural factors (e.g., perceived pressure from family and peers), lifestyle factors, social media, concerns about body image, society's thin ideal, weight status, personality traits, as well as psychological, genetics, and biological factors (12–14). In addition, female university students who have DEBs are reported to have been under family pressure to lose weight, overweight or obese, married, physically active, studying in health science colleges, and with poor eating habits (8–11). In Saudi Arabia, youth aged 15–34 account for approximately one-third of the population, and approximately 50% are females (15). The prevalence of risky lifestyle behaviors is very high among young females. According to the National Saudi Health Information Survey including 2,382 youths, the prevalence of overweight or obesity, physical inactivity, and daily consumption of fewer than five servings of fruits and vegetables among Saudi young females was 43.9, 75.6, and 92%, respectively (16). In Taif university, 55% female students were overweight and obese, 9 % smoked cigarettes, 35% consumed vegetables and fruits lower than the recommended amounts, and 38 % used social media for 3 h or more per day (17).
Social networking sites (SNSs) are web-based services that enable users to create public or semi-public profiles and share connections with a detailed list of other users. SNSs have attracted the interest of many adolescents and young adults and have become a novel area of research. Females use SNSs more than men for various social purposes (18, 19), and females tend to be more likely to use SNSs to compare themselves with others and search for information (18). Recently, Aldakhil et al. (14) studied 763 university students in Jeddah, Saudi Arabia, and found that social media significantly affected females at risk of EDs more than men. As a response to current Western sociocultural influences, the increasing use of SNSs such as Facebook, Twitter, and Instagram offers numerous opportunities to promote beauty ideals, social comparisons, and the drive for thinness among female college students (13, 20). Consequently, it is negatively related to body satisfaction, leading to DEBs (21). A recently published meta-analysis involving 13,301 respondents revealed a positive correlation between the use of SNSs and DEBs (22). Nonetheless, a few studies reported no correlation between them (23, 24).
During the critical period of the COVID-19 pandemic and the resulting mandated social isolation measures, several studies revealed a significant impact of increased SNSs utilization for socialization and keeping up with local and global events on population mental health and lifestyle behaviors (25–27). According to the Internet world statistics released in 2021, 90.1% of the Saudi Arabian population uses the Internet. Research from the Global Web Index indicates that the amount of time Saudi Arabians spent on social media has increased by 25% from 2017 to 2021. In 2021, Saudis spent 196 min per day on social media on an average, 10 min more than that in 2019 (28).
Given that DEBs may develop into EDs with severe consequences, it is crucial to properly define DEBs, their risk factors, and their impact on general health so that preventive measures can be devised. Previous studies have found some discrepancies in the reported relationships between the duration spent on social media and DEBs (22, 29, 30), but they rarely considered the potential effects of SNS-affective experiences that may be reflected on the psychological well-being (31). Disordered eating may be associated with lifestyle factors such as physical activity, poor eating habits, smoking, sleep disturbance, and obesity (8–11). In addition, the clustering of unhealthy lifestyle behaviors has synergistic and more detrimental effects on health than the individual effects of health behaviors (32). Accordingly, we hypothesized that high-risk DEBs among Saudi female university students would be associated with SNSs usage, composite lifestyle behaviors, and self-perception of body image during the unprecedented COVID-19 pandemic period.
Subjects and methods
Design and study population
A cross-sectional study was carried out in female students at the University of Taif, Saudi Arabia, between January 17 and 30 during the academic year 2021–2022. Using the EPI-INFO 2002 software, the minimum sample requirement was determined to be 351, based on the prevalence rate of DEBs among female students (35.4%) determined using the EAT-26 tool that had a precision of 3% and a confidence level of 95%. Our total sample size was 445; we increased the sample size to more than 20% to minimize the sampling error. A multistage stratified random sampling technique was used to obtain a sample that best represents the entire population, ensuring that each subgroup of interest was represented (33). Stratification was based on the type of faculty (practical vs. theoretical) and grade level. Four out of 13 faculties of Taif University (nearly one-third of the 13 faculty members) were selected randomly through the lottery method (two practical and two theoretical faculties). The predetermined sample was proportionally allocated to the selected faculties: Faculty of Medicine (45/666 students), Faculty of Engineering (24/353 students), Faculty of Literature (152/2,264 students), and Faculty of Sharia and Regulation (224/3,353 students). In the subsequent stages, samples from each faculty were assigned equally to all the grades. In the third stage, a predetermined sample from each grade was collected from a randomly selected class. Females with a history of diagnosis or treatment of EDs and those affiliated with university branches outside Taif city were excluded. The self-administered paper-based questionnaires were delivered to the participants during the class activities to share in the study under the supervision of the main author for clarification and to ensure that there was no side talk and to avoid socially expected answers. Therefore, it is noteworthy to mention that the response rate was 96%; 10 questionnaires were excluded because of incompleteness. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all the procedures involving the research study participants were approved by the Research Ethics Committee of Taif Health Affairs, Ministry of Health, Saudi Arabia approved this study (IRB. HAP-02-T-067, 165). Written consent was obtained from all the participants before answering the questions, and confidentiality was assured.
Measures
Female students self-reported their demographic, medical, lifestyle, weight, and height information and completed validated questionnaires based on DEBs [Eating Attitudes Test-26 [EAT-26] (34), SNSs Usage (35), Bergen Social Media Addiction Scale (BSMAS) (36), and Body Shape Questionnaire (37)].
Eating attitudes test-26: EAT-26
The EAT-26 is a screening tool used worldwide to identify individuals who present attitudes associated with abnormal eating behaviors or those at risk of developing EDs (5, 38–40). It has been established as a reliable and valid instrument in Arabic (Cronbach's α = 0·89) (41). Additionally, the Arabic version of the EAT-26 has been validated among female students in Saudi Arabia, and the overall reliability of the Arabic version of the EAT-26 was assessed with Cronbach's α = 0.83. The EAT-26 comprises 26 questions, and each one has six possible answers ranging from “infrequently/almost never/never” [0/1/2] to “always” [3] (42). This scale includes three subscales: dieting, bulimia/food preoccupation, and oral control. It also includes four additional behavioral questions that assess self-reported binge eating, self-induced vomiting, use of laxatives or diuretics, and treatment of EDs. Females who scored ≥20 or answered affirmatively to any of the behavioral questions were classified as being at risk of EDs, and higher scores indicated a greater risk of EDs (34).
Social networking sites usage questionnaire
The questionnaire included questions on featured and affective SNSs usage. The featured subscale included 13 items assessing basic (questions on the frequency of use, the average extent of time of use, and the number of friends), interactive (frequency of sending messages, updating status, sharing or resending profiles, visiting a friend's homepage, and commenting on others' photos and comments), and self-display usage (writing notes/blogs, updating profile images, and posting photos) on a 7-point scale (1 = never, 7 = multiple times a day). For the affective SNSs usage items, participants rated the frequencies of experiencing eight negative and positive emotions using a scale ranging from 0 to 7, where higher scores indicated higher usage or frequency of emotions. The measure has been validated in young adults with good internal consistency (α = 0.82). Three questions were added to explore exposure the type and duration of social networks use including No 0) or Yes 1) responses to the following question “Please indicate which of the following accounts you have?” (Twitter, Snap Chat, Facebook, YouTube, WhatsApp, and Instagram); in the context of the most used SNSs in Saudi Arabia, “Which social networking site do you use the most?” and “When did you create your first account on social networking sites?” (35). We asked about the change in SNSs navigation rate from pre-pandemic stage to current time by a three-scale question Yes, I navigate it less than before 1), Yes, I navigate it more than before 2), and No change 0).
Some questions related to SNSs usage to fulfill specific gratifications related to weight loss/dieting, fitness/exercise, cooking, fashion, and bariatric surgery were added. These values were adapted from Park et al. (43) and Lee et al. (21). They included three types of SNSs use: information-seeking (e.g., “I visit SNSs to gather information about weight loss/dieting, cooking, fashion, bariatric surgery, and fitness/exercise,” with a dichotomous (i.e., yes or no) response for each; self-status seeking (e.g., “In the past 3 months, I posted messages on my own SNS with the intent to express my ideas and opinions about weight loss/dieting, fitness/exercise, cooking, fashion, bariatric surgeries,” with a dichotomous (i.e., yes or no) response for each); and socializing use (for example, “On an average, how many messages or comments do you post on others' posts with a desire to interact with another individual about weight loss/dieting, fitness/exercise, cooking, fashion, and bariatric surgeries?,” with six responses varying from never (0) to many times per day (7) (21). The frequencies for each type of SNSs use were summed to determine each participant's general tendency to use SNSs for information seeking, self-status seeking, and socializing use. In addition, the participants answered a question related to why they used SNSs in relation to weight loss/dieting, fitness/exercise, cooking, fashion, and bariatric surgery for checking the appropriate response. Responses ranged from very rarely (1) to very often (5), and the scores ranged from 11 to 55. Higher scores indicated higher social motives to use social media for weight loss/dieting, fitness/exercise, and body appearance (21, 43). The Networking SNSs Usage Questionnaire demonstrated good reliability with Cronbach's α = 0.813 for featured use, 0.76 for affective use, and 0.82 for the dependence scale.
Dependence on social networking sites
SNSs dependence was assessed using the Bergen Social Media Addiction Scale (BSMAS). It is a valid and reliable questionnaire which determines the use of social media activities generally rather than to one specific platform (36). It consists of six items that indicate addiction criteria such as withdrawal, salience, mood modification, conflict, tolerance, and relapse. It is rated on a five-point scale ranging from strongly disagree (1) to strongly agree (5), with scores ranging from 11 to 55. A score of 24 is set as the clinical cut-off point based on the gold standard for clinical diagnosis (44). The validated Arabic questionnaire demonstrated good reliability, with a Cronbach's α of 0.754.
Body shape questionnaire (BSQ-8)
The BSQ-8 is an 8-item scale with six response options on a Likert scale ranging from never = 1 to always = 6 (37). It showed adequate reliability among females, as evaluated by Cronbach's alpha (α = 0.91), to evaluate body image problems such as fears of weight gain, desires for weight loss, body shape concern, and low self-esteem due to one's physical appearance was used to assess body shape concerns. Item responses were summed up. A score of less than 19 indicates no concern with shape; a score of 19–25 indicates moderate concern with shape; and a score of more than 33 indicates severe concern with shape (45). The validated Arabic questionnaire demonstrated good reliability, with a Cronbach's α of 0.78.
Adoption and validation procedures
These procedures were conducted on 50 students for all questionnaires except the EAT-26. According to the Guidelines of Beaton et al. (46), forward translation was initially performed by two native Arab bilingual translators who were fluent in English. A backward translation was then performed by two native English-speaking translators who were fluent in Arabic and unfamiliar with the concepts of the scales. The back-translated English questionnaire was subsequently compared with the original English questionnaire, and inconsistencies between the two versions were resolved to ensure that the translation did not affect the content validity of the questionnaire.
Content validity was assessed to ensure the necessity of each item in the collected pilot using qualitative and quantitative methods by a five-expert panel consisting of a psychologist, two statisticians, a nutritionist, and a public health specialist. For the qualitative evaluation, we submitted only the Arabic translation without substitution. Each item was double-checked by two volunteer translators for the correct wording to ensure that the items were free of any ambiguous wording that could confuse the students. For the quantitative measurement of content validity, content validity index (CVI) and content validity ratio (CVR) were calculated holistically. CVI (0.90; range [0.86–1]) and CVR [0.85; range (0.80–1)] were both satisfactory.
Composite lifestyle index
Five lifestyle behaviors (physical activity, sleep, sitting, smoking, Body Mass Index (BMI) in kg/m2, and dietary habits) were assessed based on reported risk category calculation protocols (47). Dietary habits were measured based on index values reported by the Saudi Food-based Dietary Guidelines for 14 food items (48). The participants reported the number of fruit and vegetable servings per day; three is the optimal number of servings. The weekly frequencies of the remaining 12 food items were assessed, which included full-fat dairy products; non-refined cereals and bread; legumes and nuts; fish and seafood; red meat and other meat products; poultry; butter or margarine; fast foods; sweets; potato chips or French fries; sugar-sweetened drinks/soft drinks; and, energy drinks. Five options for eating frequency were established: “daily;” “5–6 times a week;” “3–4 times a week;” “1–2 times a week,” and “never or rarely.” The responses ranged from 0–4 (for food items recommended in the Saudi dietary guidelines) or the reverse (for food items that should be limited in the Saudi dietary guidelines). The total scores ranged from 0 to 56. The total score was subsequently classified into three tertiles using the following equation (first tertile = lower limit (11) + 0.33 × 32= 21.56, second tertile= lower limit (11) + 0.66 × 32 = 32.12). A score of one was generated for those below 21.56 (first level tertile or poor diet) and from 21.56 to less than 32.12 (second level tertile or average diet); a score of zero was generated for those above 32.12 (third level tertile or better diet). These tertiles were subsequently classified into low-risk (0 = third tertile) and high-risk (1 = first and second tertiles), based on a previous study (49). Sleeping, sitting, and smoking behaviors were dichotomized into healthy (low-risk) and unhealthy (high-risk) categories and scored as 1 and 0, respectively, whereas physical activity (PA) was scored as 0 (high PA), 1 (moderate PA), and 2 (low PA). Finally, BMI was calculated and categorized: 1 (underweight/overweight/obese) and zero (normal BMI). The scores for the five behaviors were added.
Statistical analysis
Statistical analyses were performed using IBM (SPSS) Statistics version 24.0* software. Descriptive statistics, including frequencies and percentages, were used for categorical variables, and median and range were used for continuous variables after determining normality using the Shapiro test. The rates of healthy and unhealthy dichotomies were calculated for each lifestyle behavior, and the rates of the participants engaging in one to seven unhealthy lifestyle behaviors were calculated. BMI (kg/m2) was computed based on the given weight and height and classified according to the World Health Organization guidelines.
Chi-squared test was used to compare the DEBs categories, and Monte Carlo exact test was used in case of violation of the chi-square assumption. Spearman's rho correlation coefficients were determined to test the association between the continuous variables, and Mann–Whitney U-test was used to test the difference in the motivation score between normal group and those at risk. A logistic regression model for the DEBs variable (dummy variable) was used to determine significant contributors. For all the statistical tests, the significance level was determined to be below 5% and quoted as a two-tailed hypothesis test.
Results
Totally, 445 university female students were included in the study and classified according to the EAT-26 cutoff values into the normal group (n = 324, 72.8%) and DEBs-risk group (n = 121, 27.2%). Approximately half of them were affiliated with the College of Sharia and Regulations (50.3%), and the rest were affiliated with Faculty of Literature (34.2%), Faculty of Medicine (10.1%), and Faculty of Engineering (5.4%). The majority were single, living with their families, and not working outside the study period; the median age was 21 years. The socioeconomic status did not differ significantly between the normal and DEBs-risk groups. Regarding the medical status, the DEBs-risk group showed a significantly higher rate of psychological illnesses, regular medication intake, and familial history of obesity than the normal group (proportional differences = 8.1, 7.2, and 14.5%, respectively, p < 0.05, Table 1). A simple frequency table of the items of the EAT-26 is summarized in Supplementary Table S1.
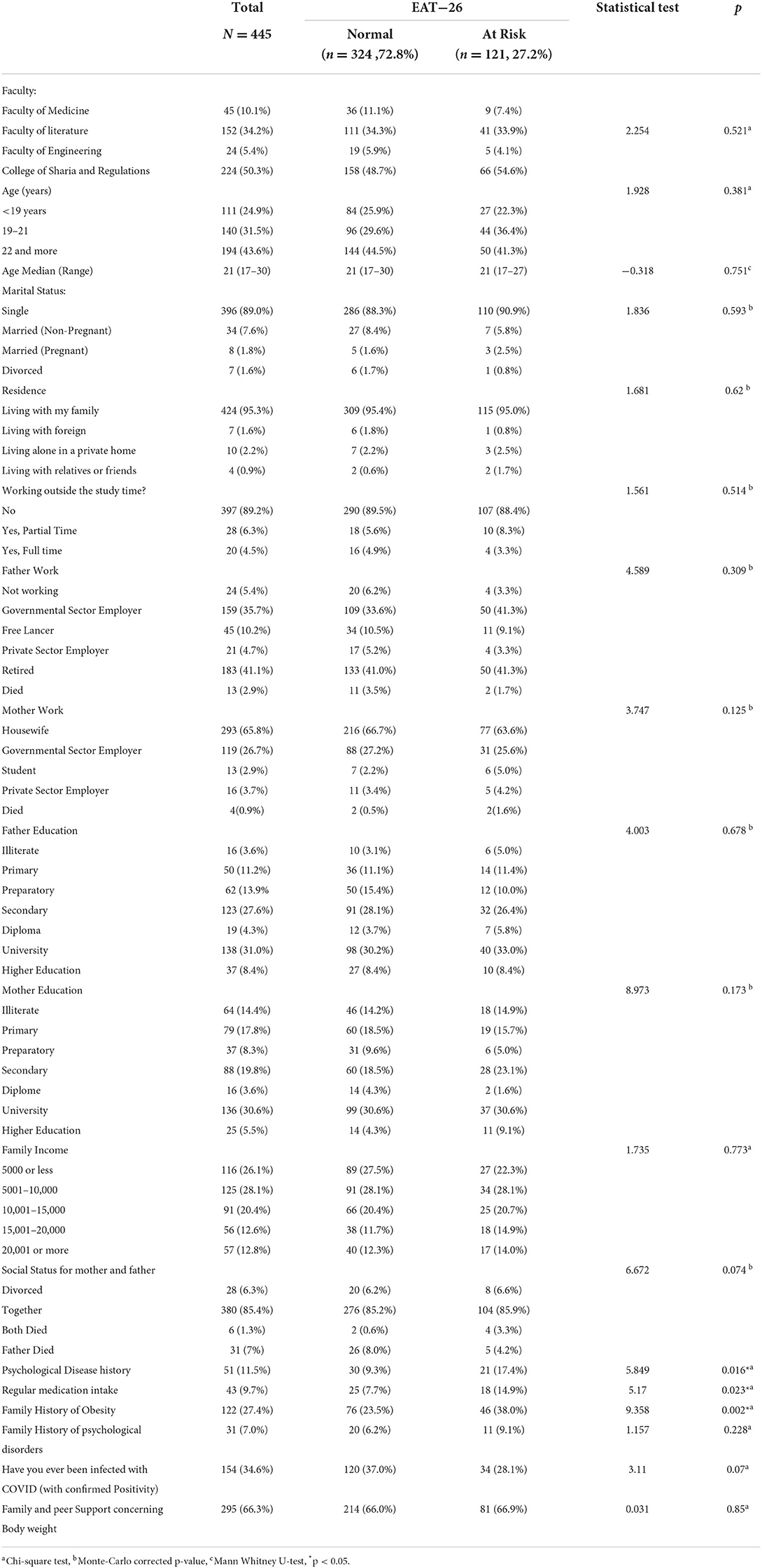
Table 1. Sociodemographic characteristics among female university students, classified according to EAT-26.
Table 2 illustrates the lifestyle characteristics and body image concerns of female students. The majority (74.8%) showed a low level of PA, although the DEBs-risk group showed a lower rate of low PA and a higher rate of high PA compared to the normal group (proportional differences = 7.5 and 7.3%, respectively, p = 0.018). Half of the students had normal body weights; however, the probability of being overweight and obese was significantly high in the DEBs-risk group (p = 0.008). There was a marked increase in the body image-related concern in the DEBs-risk group (37.2%). The normal group had higher proportions of students with no and mild body image concerns and a lower proportion of those with moderate body image concerns compared to the DEBs-risk group (proportional differences = 15.6, 2.9, and 3.2%, respectively, p = 0.001). There were no statistically significant differences between the DEBs categories with respect to smoking habits, dietary habits, sleeping habits, and overall composite lifestyle score (p > 0.05).
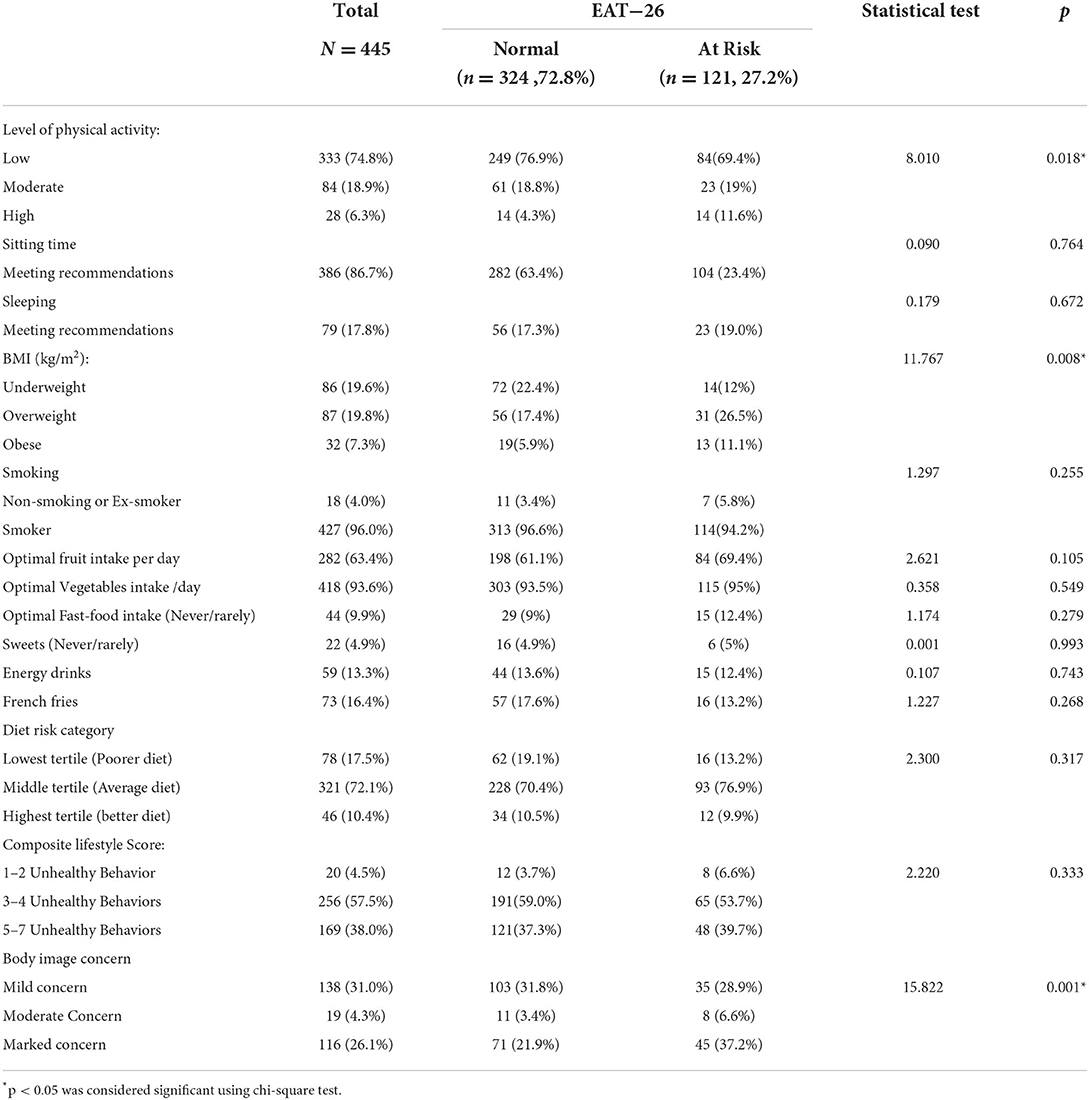
Table 2. Lifestyle characteristics and body image concern among female university students, classified according to EAT-26.
Table 3 illustrates the SNS use among female students. The SNSs accounts of the majority of the students (62%) were created more than 7 years. The Snapchat was used by 82% of the participants, followed by YouTube (70.8%) and TikTok (69.2%). When we asked them to rank how often they used social media, Snapchat came first (27.3%), followed by Tiktok (21.6%), then Instagram (17.8%). There was no association of the DEBs categories with the number of years and the preference for SNSs usage. Moreover, two-thirds (68%) of them visited SNSs (frequency of use is once or more than an hour), and approximately 40% of them spent from 30 min to 3 h in each access, and 30% of the students spent more than 3 h. For featured usage, the DEBs-risk group showed a higher frequency of account checking, duration of use, and number of friends on different SNSs compared to the normal group (p < 0.05). For affective usage, unhappiness was significantly linked with risky DEBs (p = 0.007). For addictive usage, there was no statistically significant difference between the DEBs categories. However, the median motivation score of using SNSs in relation to weight loss/dieting, fitness/exercise, cooking, fashion, and bariatric surgery was highly significant in the DEBs-risk group (p < 0.001). In addition, there was a significant difference in the SNSs usage between the pre-pandemic time and the current time among the DEB-risk group compared to the normal group (proportional differences in the high use, and less use = 16%, 13.1%, respectively, p = 0.001). The details of affective, featured use, and addiction of SNSs are displayed in Supplementary Table S2.
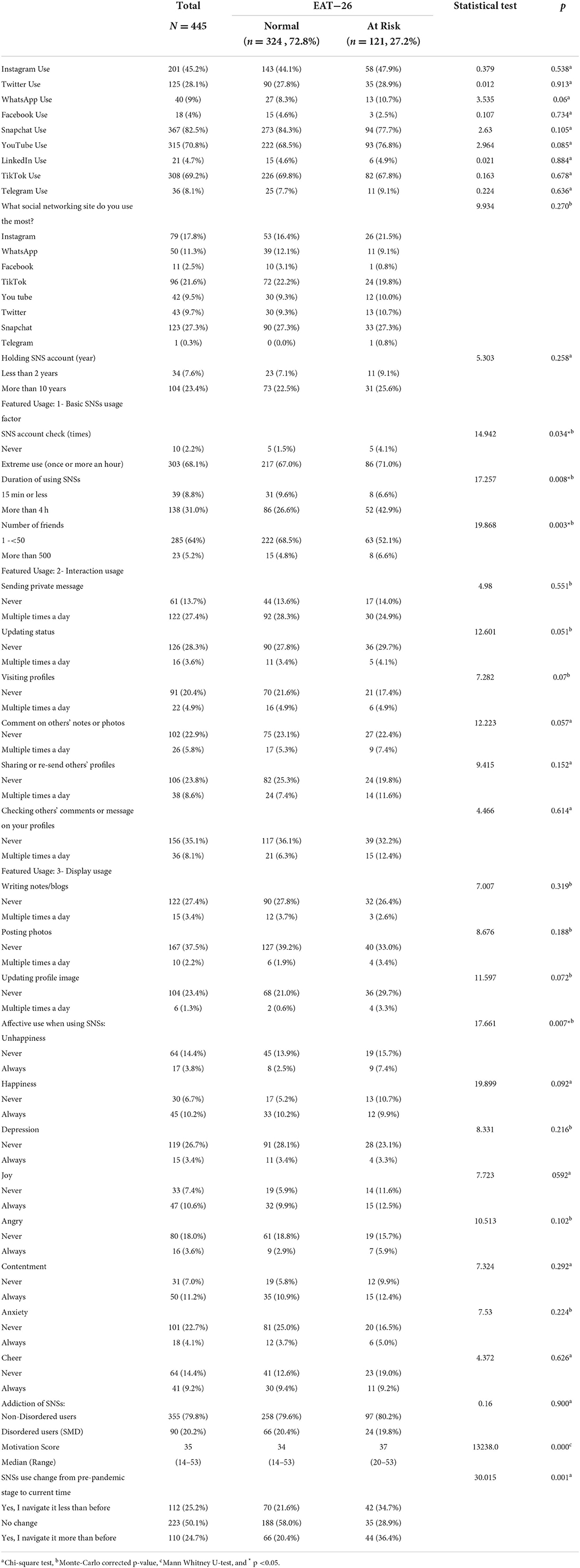
Table 3. Social network sites use (type, featured usage, affective use, SMD social media disorder and motive of SNSs use) among female university students, classified according to EAT-26.
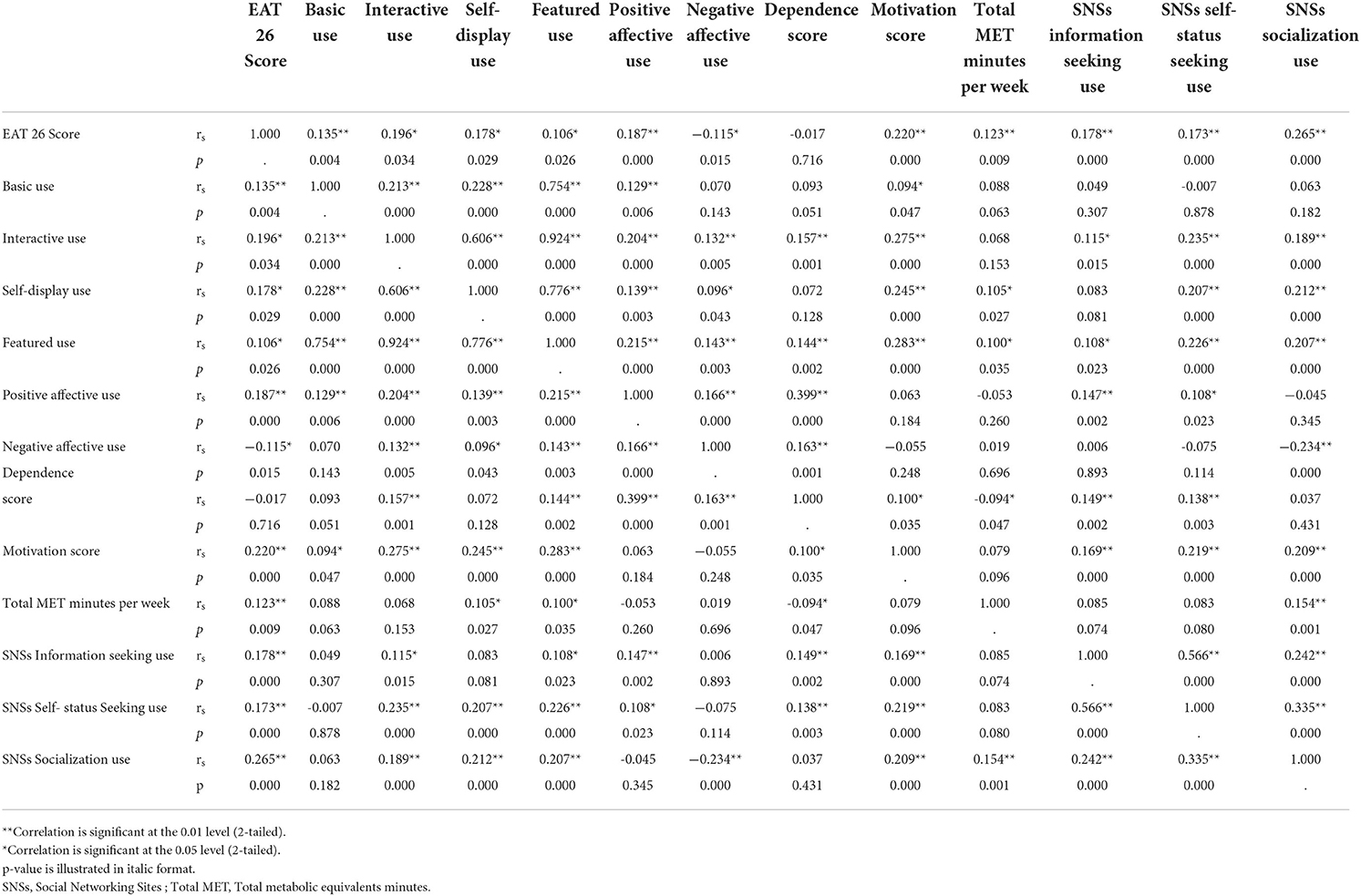
Basic, interactive, self-display, and featured SNSs usage as a whole showed a mild positive correlation with the EAT-26 score (rs = 0.135, 0.196, 0.178, and 0.106; p = 0.004, 0.034, 0.029, and 0.026, respectively). There was a mild positive association between basic, interactive, self-display, and featured SNSs use. Participants' general tendencies to use SNSs for information seeking, self-status seeking, and socializing to fulfill specific gratifications related to weight loss/dieting, fitness/exercise, cooking, fashion, and bariatric surgeries showed significant positive correlations with the EAT-26 score (rs = 0.178, 0.173, 0.265, all p < 0.001). Similarly, the motivation score showed a significant positive correlation with the EAT-26 score (r = 0.220, p < 0.001). Positive affective SNSs use showed a significant positive correlation with the DEBs score (rs = 0.187, p < 0.001). In contrast, negative affective SNSs use showed a significant negative correlation with the EAT-26 score (rs = −0.115, p = 0.015, Table 4).
Table 5 spots the factors, which significantly contribute to DEBs. Female students who navigated SNSs sites more in the current time compared to that in the pre-pandemic time were more prone to develop DEBs (adjusted OR = 4.225, 95% CI = 3.114–5.446, p < 0.001). Participants who had higher numbers of friends on SNSs and those who visited their SNSs once or for more than an hour were more likely to develop DEBs. The participants who were more likely to develop DEBs reported high motivation scores to use SNSs, marked body image concern, and a general tendency of information-seeking SNSs use [(adjusted OR = 5.032, 95% CI = (3.677–6.432), p < 0.001), (adjusted OR = 6.034, 95% CI = (4.791–16.097), p = 0.003) and (adjusted OR = 2.130, 95% CI = 2.048–3.219, p = 0.001), respectively]. On the other hand, regular drug use seemed to be a preventive factor against DEBs (adjusted OR = 0.277, 95% CI = 0.106–0.726, p = 0.009). Self-status seeking SNSs use was found to be a border line factor (adjusted OR = 0.933, 95% CI = 0.871–0.999, p = 0.045).
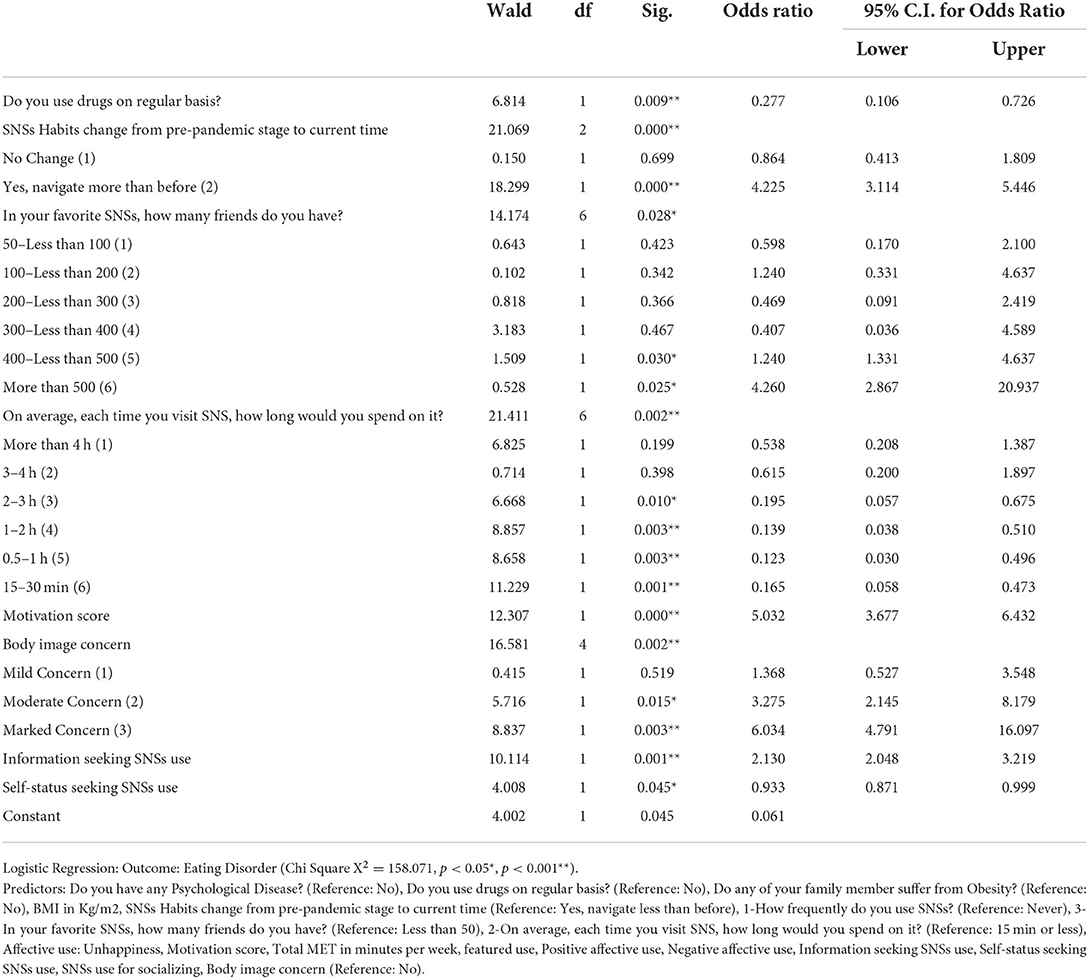
Table 5. Regression analysis of usage patterns of social networking sites and disordered eating behaviors among the female university students.
Discussion
This study investigated the prevalence of DEBs among Saudi female college students during the COVID-19 pandemic, as well as its association with students' lifestyle behaviors and SNSs use. More than a quarter of the participants (27.2%) had DEBs (Table 1). This finding contradicts those of a recently published study of Saudi college female students, which reported slightly higher rates of DEBs during the COVID-19 pandemic (11). This disparity may be explained by the timing of data collection, differences in population characteristics, and population resilience with the spread of the pandemic. The early stages of the COVID-19 pandemic were frequently associated with elevated levels of distress, depression, and anxiety, and a longitudinal follow-up revealed clear indications of resilience (50). Previous studies have reported more differences in distress, internet use, and eating behaviors among medical students as compared to those in other theoretical majors (51, 52). Nevertheless, a meta-analysis of different studies in Middle Eastern countries published in 2021 reported a slightly lower prevalence of DEBs (22.07%) compared to the current estimated prevalence, which is slightly higher than the global prevalence, owing to rapid social changes and acculturation occurring in the Arab world (7). Some studies conducted prior to the pandemic on Saudi female university students using the EAT-26 test found higher rates of DEBs than those reported in the current study (35.4%, 38.8%, and 29.4%) (8, 9, 14), whereas others showed slightly lower rates (25.4%) (10). Abd El-Azeem et al. (8) found that 35.4% of the 1,200 females at Taif, were at risk for EDs. These differences could be attributed to the timing of the study and various methodological factors such as study setting (university or school, or different cultures in different regions of Saudi Arabia), sample selection (gender and age), size, and assessment methods (self-reported or interviews).
The current study highlights the relationship between the patterns of SNSs use and DEBs. Students who navigate SNSs more frequently in the current time than in the pre-pandemic period were more likely to develop DEBs. Additionally, DEBs are significantly more prevalent among those with higher basic (higher frequency rate of account checking, duration of use, and number of friends on different SNSs), interactive, and self-display use rather than among those with higher addictive SNSs use (Tables 3–5). This finding aligns with the results of a recently published meta-analysis and several previous studies (22, 53, 54). Holland et al. (55), reported that specific actions on SNSs (such as viewing and uploading images, receiving negative comments via status updates, and making comments on other SNSs users' photos and statuses) were related to a higher drive for thinness, appearance comparison, and eating concerns. Body dissatisfaction may influence DEBs when SNSs are used. Based on the descriptive statistics of the main domains of EAT-26 tool, we concluded that the university students depicted a high level of oral control compared to the other two domains of DEBs as illustrated in Supplementary Table S1, this may be attributed to the desire to be slimmer. Exposure to media messages advocating a thin ideal body has been linked to disturbances in body image and DEBs. Murray et al. (56) illustrated that body esteem indicators mediate the relationship between SNSs use and EDs. In addition, greater SNSs use was associated with more weight gain and body dissatisfaction, which is associated with more severe EDs. Cohen et al. (57) demonstrated that engaging in photo-based activities (e.g., posting and sharing photos of oneself and friends) rather than general SNSs use was associated with EDs.
Almuhlafi et al. (58) found that 62% of 399 adolescent females in the city of Tabuk, northern Saudi Arabia, believed that social media exposure to fashion designs/modeling industry increased their desire to lose weight. More than half the individuals who felt pressure to be thin and those who thought social media influencers inspired them to work out reported signs of EDs, according to Al-Jumayan et al. (59). In contrast, other studies have reported that SNSs use was not directly related to DEBs (23). Ferguson et al. (60), who measured the impacts of SNSs use and peer competition on body satisfaction and EDs symptoms among teenage girls over a 6-month follow-up period. They found no concurrent or prospective correlations between SNSs use and body dissatisfaction or EDs symptoms. This absence of a relationship could be attributed to the variations in SNSs use measurement, which included activities like online gaming and blogging or the fact that the majority of the participants were Latino (94.1%) (60). Different cultures have different traditional aesthetics. White American adolescents strongly internalize the concept that “beauty is thin.” Therefore, studies on this subject from different regions may yield different findings (61).
In line with findings in the correlation analysis (Table 4), Easton et al. (62) found that viewing Fitspiration posts encouraged participants' obsession with calorie counting, and a some of them reported that some diet-related materials could even instigate EDs, particularly if the participants were unaware that they were developing unhealthy eating habits. In fact, the contents of some diets can induce DEBs (63). Likewise, Lee et al. (64) illustrated that social media use for body image information was negatively correlated with body satisfaction, and, thus, negatively affected DEBs (21). In accordance with the present study, Lee et al. (64) presented their participants with profile pictures of underweight or overweight users on Facebook. They discovered that Korean undergraduates who observed an underweight peer making online comments about wanting to lose weight were less satisfied with their bodies than those who observed an overweight peer expressing the same desire (64).
Previous studies have focused on the impact of SNS activity on well-being; nevertheless, they rarely consider the potential effects of SNS affective experiences that may predict psychological well-being (31). Regardless of individual's activities on SNSs, users are more likely to be satisfied and happier when they experience more positive and fewer negative affective experiences. Fear of not receiving comments/likes (i.e., online neglect) or the fear of receiving negative comments might trigger stressful experiences and negative feelings, resulting in decreased life satisfaction or poor psychological well-being. We found that unhappiness and negative affective experiences were significantly associated with DEBs (Tables 3–5), which is consistent with the results of Fabris et al. (65), who concluded that adolescents with higher levels of negative affective experiences might be at a greater risk for excessive social media use aimed at restoring gratification or compensation with respect to perceived needs, and, accordingly, may increase the probability of psychological consequences and disordered eating among the young population (22, 65). On the other hand, some females with EDs may develop internet addiction while they try to get dieting/weight control information or get social media support from people with similar problems (51, 63).
Previous studies among female university students found significant relationships between EAT-26 scores exceeding 20 and peer or family stress due to losing weight, marital status, studying in health science colleges, positive psychological illness history, overweight or obesity, poor eating habits, vegetarianism, and high levels of PA (8–12). A study conducted on 399 adolescent females in the city of Tabuk, northern Saudi Arabia, found high rates of overweight/obesity and DEBs, and participants with DEBs experienced more significant peer pressure to lose weight (58). Dooley-Hash et al. (66) found a correlation between EDs and depression in females, which is consistent with the reported association between poor psychiatric states and disordered eating. Psychiatric distress triggers emotional eating and unhealthy food choices as a coping mechanism (67). Nevertheless, the current study did not detect a statistically significant difference between DEBs groups regarding faculty type, family and peer support, diet, smoking, sleeping habits, and overall composite lifestyle score. Consistent with the results of Alwosaifer et al. (9), the current study found no significant risk among different academic majors. This could be because all the college students may have experienced similar consequences. Badrasawi et al. also showed that ED risk was not correlated with fast-food consumption, which is consistent with our results (68). The only significantly associated lifestyle behavior was PA, where DEBs is more prevalent among those practicing high PA, as reported in previous studies (59, 69). In 2021, Al-Jumayan et al. conducted a cross-sectional study of 560 sports center clients in Saudi Arabia. They found that exercise frequency was significantly associated with the risk of EDs; higher rates were reported in participants who exercised more frequently per week. DEBs frequency and the need for referral to mental health professionals were found more in participants who reported spending more time in the gym (59). This finding can be attributed to the fact that athletes are more likely to develop DEBs and exercise behaviors because of the pressure to perform well and acquire a specific appearance (70, 71). Our results also revealed that the probability of being overweight or obese, having body image concerns, or having a family history of obesity was relatively high in the DEBs-risk group, which is consistent with many published studies (6, 8, 10). These findings could be explained by psychological co-occurrences of high BMI, such as body concern or dissatisfaction, and weight stigma, thereby contributing to the increasing burden of DEBs (72). Concerns about body image are thought to be a risk factor for DEBs.
This is the first study to examine the relationship between SNSs and DEBs, considering unhealthy lifestyle behaviors during the COVID-19 pandemic. The strengths of this study include the calculation of the sample size, the recruitment of a random sample from various faculties, and the use of validated questionnaires. Additionally, college-aged individuals were targeted because DEBs tend to be more prevalent during this life stage. However, there are some limitations. Data are self-reported, which is susceptible to inevitable recall bias. Second, because of the cross-sectional, we could not infer causal relationships and could not investigate the effect of the COVID pandemic stage on SNSs navigation rate over time. Third, the results are not representative of female university students in Saudi Arabia as a whole but of only one university. Consequently, the findings cannot be generalized to other contexts. Using self-reported weight and height to calculate BMI may result in an underestimation bias, even though previous studies found few differences between self-reported and measured BMIs in females and men. Longitudinal studies are recommended to assess causality between SNSs use and DEBs.
Conclusion
DEBs are prevalent among female college students, particularly those who use SNSs excessively and have more friends on SNSs. The likelihood of developing DEBs is higher among females who report a high propensity for information-seeking SNSs use, high motivation for SNSs use in relation to weight loss/dieting, and significant body image concerns. Health practitioners need to screen young females for DEBs, necessitating early interventions to treat and prevent potentially harmful consequences. In addition, it is crucial to monitor adolescents' use of the internet, especially social media, which represents a significant risk factor for DEBs.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Research Ethics Committee of Taif Health Affairs, Ministry of Health, Saudi Arabia (IRB. HAP-02-T-067, 653). The patients/participants provided their written informed consent to participate in this study.
Author contributions
AR and NAb designed the study proposal and questionnaire and collected research data. NO and NAb analyzed data. NAb, AR, AMA, and NO shared in data interpretation, drafting the work, and article writing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.949051/full#supplementary-material
References
1. Fitzsimmons-Craft E, Ciao A, Accurso E. A naturalistic examination of social comparisons and disordered eating thoughts, urges, and behaviors in college women. Int J Eat Disord. (2015) 49:141–50. doi: 10.1002/eat.22486
2. Yannakoulia M, Matalas A, Yiannakouris N, Papoutsakis C, Passos M, Klimis-Zacas D. Disordered eating attitudes: an emerging health problem among Mediterranean adolescents. Eat Weight Disord. (2004) 9:126–33. doi: 10.1007/BF03325056
3. Wu XY, Yin WQ, Sun HW, Yang SX, Li XY, Liu HQ. The association between disordered eating and health-related quality of life among children and adolescents: a systematic review of population-based studies. PLoS ONE. (2019). 14:e0222777. doi: 10.1371/journal.pone.0222777
4. Marie G, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review, Am J Clin Nutr. (2019) 109:1402–13. doi: 10.1093/ajcn/nqy342
5. Ali AM, Hendawy AO, Abd Elhay ES, Ali EM, Alkhamees AA, Kunugi H, et al. The Bergen Facebook Addiction Scale: its psychometric properties and invariance among women with eating disorders. BMC Womens Health. (2022) 22:99. doi: 10.1186/s12905-022-01677-2
6. Abdullah Hasan Alhazmi Abdulaziz Al Johani. Prevalence Associated factors of eating disorders among students in taiba university, Saudi Arabia: a cross-sectional study. Malaysian J Public Health Med. (2019) 1:172–6. doi: 10.37268/mjphm/vol.19/no.1/art.80
7. Alfalahi M, Mahadevan S, al Balushi R, Chan MF, Saadon MA, Al-Adawi S, et al. Prevalence of eating disorders and disordered eating in Western Asia: a systematic review and meta-Analysis. Eat Disord. (2021) 4:1–30. doi: 10.1080/10640266.2021.1969495
8. Abd El-Azeem Taha AA, Abu-Zaid HA, El-Sayed Desouky D. Eating disorders among female students of Taif University, Saudi Arabia. Arch Iran Med. (2018) 21:111–7.
9. Alwosaifer AM, Alawadh SA, Abdel Wahab MM, Boubshait LA, Almutairi BA. Eating disorders and associated risk factors among Imam Abdulrahman bin Faisal university preparatory year female students in Kingdom of Saudi Arabia. Saudi Med J. (2018) 39:910–21. doi: 10.15537/smj.2018.9.23314
10. Fatima W, Ahmad LM. Prevalence of disordered eating attitudes among adolescent girls in Arar City, Kingdom of Saudi Arabia. Health Psychol Res. (2018) 6:7444. doi: 10.4081/hpr.2018.7444
11. Abukhaled JK, Alabdullah DW, Aleban SA, Almuqhim SA, El-Akabawy G, Assiri RA. Prevalence of eating disorders among Saudi female university students during the COVID-19 outbreak. J Taibah Univ Med Sci. (2022) 17:392–400. doi: 10.1016/j.jtumed.2022.02.001
12. Blanco C, Rubio JM, Wall M, Secades-Villa R, Beesdo-Baum K, Wang S. The latent structure and comorbidity patterns of generalized anxiety disorder and major depressive disorder: a national study. Depress Anxiety. (2014) 31:214–22. doi: 10.1002/da.22139
13. AlShebali M, AlHadi A, Waller G. The impact of ongoing westernization on eating disorders and body image dissatisfaction in a sample of undergraduate Saudi women. Eat Weight Disord. (2021) 26:1835–44. doi: 10.1007/s40519-020-01028-w
14. Aldakhil LO, Abaalkhail BA, Abu II. Influence of sociocultural factors on the risk of eating disorders among King Abdulaziz University students in Jeddah, Saudi Arabia. J Fam Community Med. (2022) 29:138–44. doi: 10.4103/jfcm.jfcm_85_22
15. General Authority for Statistics. Population Estimates 2020: Saudi Youth in Numbers. GASTAT (2020). Available online at: https://www.stats.gov.sa/sites/default/files/saudi_youth_in_numbers_report_2020en.pdf.
16. Moradi-Lakeh M, El Bcheraoui C, Tuffaha M, Daoud F, Al Saeedi M, Basulaiman M, et al. The health of Saudi youths: current challenges and future opportunities. BMC Fam Pract. (2016) 17:26. doi: 10.1186/s12875-016-0425-z
17. Sami R, Bushnaq T, Benajiba N, Helal M. Food consumption and lifestyle habits among university students in Saudi Arabia. Afr J Food Agric Nutr Dev. (2021) 21:17711–26. doi: 10.18697/ajfand.98.20245
18. Nina H, Eimler SC, Papadakis AM, Kruck JV. Men are from Mars, women are from Venus? Examining gender differences in self-presentation on social networking sites. Cyberpsychol Behav Soc Netw. (2012) 15:91–8. doi: 10.1089/cyber.2011.0151
19. Tifferet S, Vilnai-Yavetz I. Gender differences in Facebook self-presentation: An international randomized study. Comput Hum Behav. (2014) 35:388–99. doi: 10.1016/j.chb.2014.03.016
20. Brooks KR, Mond JM, Stevenson RJ, Stephen ID. Body image distortion and exposure to extreme body types: contingent adaptation and cross adaptation for self and other. Front Neurosci. (2016) 10:334. doi: 10.3389/fnins.2016.00334
21. Lee HR, Lee HE, Choi J, Kim JH, Han HL. Social media use, body image, and psychological well-being: a cross-cultural comparison of Korea and the United States. J Health Comm. (2014) 19:1343–58. doi: 10.1080/10810730.2014.904022
22. Zhang, J Wang, Y Li, Q and Wu, C. The relationship between SNS usage and disordered eating behaviors: a meta-analysis. Front. Psychol. (2021) 12:641919. doi: 10.3389/fpsyg.2021.641919
23. Howard LM, Heron KE, MacIntyre RI, Myers TA, Everhart RS. Is use of social networking sites associated with young women's body dissatisfaction and disordered eating? A look at Black-White racial differences. Body Image. (2017) 23:109–13. doi: 10.1016/j.bodyim.2017.08.008
24. Kim JW, Chock TM. Body image 2.0: associations between social grooming on Facebook and body image concerns. Comput. Hum. Behav. (2015) 48:331–9. doi: 10.1016/j.chb.2015.01.009
25. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
26. Romero-Blanco C, Rodríguez-Almagro J, Onieva-Zafra MD, Parra-Fernández ML, Prado-Laguna MDC, Hernández-Martínez A. Physical activity and sedentary lifestyle in university students: changes during confinement due to the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17:6567. doi: 10.3390/ijerph17186567
27. Luo T, Chen W, Liao Y. Social media use in China before and during COVID-19: Preliminary results from an online retrospective survey. J Psychiatr Res. (2021) 140:35–38. doi: 10.1016/j.jpsychires.2021.05.057
28. Global web index. The Biggest Social Media Trends for 2022: GWI's Flagship Report on the Latest Trends in Social Media. GWI (2022). Available online at: https://www.gwi.com/reports/social/ (accessed on May 16, 2022).
29. Holland G, Tiggemann M. “Strong beats skinny every time”: disordered eating compulsive exercise in women who post fitspiration on Instagram. Int J Eat Disord. (2017) 50:76–9. doi: 10.1002/eat.22559
30. Mabe AG, Forney KJ, Keel PK. Do you “like” my photo? Facebook use maintains eating disorder risk. Int J Eating Disord. (2014) 47:516–23. doi: 10.1002/eat.22254
31. Shi Y, Luo YLL, Liu Y, Yang Z. Affective experience on social networking sites predicts psychological well-being Off-line. Psychol Rep. (2019) 122:1666–77. doi: 10.1177/0033294118789039
32. Alzahrani SG, Watt RG, Sheiham A, Aresu M, Tsakos G. Patterns of clustering of six health-compromising Behaviors in Saudi adolescents. BMC Public Health. (2014) 14:1215. doi: 10.1186/1471-2458-14-1215
33. Tyrer S, Heyman B. Sampling in epidemiological research: issues, hazards and pitfalls. BJPsych Bulletin. (2016) 40:57–60. doi: 10.1192/pb.bp.114.050203
34. Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. (1982) 12:871–8. doi: 10.1017/S0033291700049163
35. Shi Y, Yu LLL, Yang Z, Liu Y, Cai H. The development and validation of the social network sites usage questionnaire. In: International Conference on Social Computing and Social Media, Vol. 8531. Cham: Springer (2014). pp. 113–24.
36. Andreassen CS, Pallesen S, Griffiths MD. The relationship between addictive use of social media, narcissism, and self-esteem: Findings from a large national survey. Addict Behav. (2017) 64:287–93. doi: 10.1016/j.addbeh.2016.03.006
37. Evans C, Dolan B. Body shape questionnaire: derivation of shortened “alternate forms”. Int J Eat Disord. (1993) 13:315–21. doi: 10.1002/1098-108X(199304)13:3<315::AID-EAT2260130310>3.0.CO;2-3
38. Harrison AN, James Bateman CCB, Younger-Coleman NOM, Williams MC, Rocke KD, Clato-Day Scarlett SC, et al. Disordered eating behaviours and attitudes among adolescents in a middle-income country. Eat Weight Disord. (2020) 25:1727–37. doi: 10.1007/s40519-019-00814-5
39. Al Sabbah H, Muhsineh S. Disordered eating attitudes and exercise behavior among female Emirati College Students in the United Arab Emirates: a cross- sectional study. Arab J Nutr Exerc. (2017) 1:62–76. doi: 10.18502/ajne.v1i2.1224
40. Sengör G, Gezer C. Food addiction and its relationship with disordered eating behaviours and obesity. Eat Weight Disord. (2019). 24:1031–9. doi: 10.1007/s40519-019-00662-3
41. Haddad C, Khoury C, Salameh P, Sacre H, Hallit R, Kheir N, et al. Validation of the Arabic version of the Eating Attitude Test in Lebanon: a population study. Public Health Nutr. (2021) 24:4132–43. doi: 10.1017/S1368980020002955
42. Al-Subaie A, Al-Shammari S, Bamgboye E, Al-Sabhan K, Al-Shehri S, Bannah AR. Validity of the Arabic version of the eating attitude test. Int J Eat Disord. (1996) 20:321–4. doi: 10.1002/(SICI)1098-108X(199611)20:3<321::AID-EAT12>3.0.CO;2-
43. Park N, Kee KF, Valenzuela S. Being immersed in social networking environment: Facebook groups, uses and gratifications, and social outcomes. Cyberpsychol Behav. (2009) 12:729–33. doi: 10.1089/cpb.2009.0003
44. Luo T, Qin L, Cheng L, Wang S, Zhu Z, Xu J, et al. Determination the cut-off point for the Bergen social media addiction (BSMAS): diagnostic contribution of the six criteria of the components model of addiction for social media disorder. J Behav Addic. (2021) 10:281–90. doi: 10.1556/2006.2021.00025
45. Makri V. Validation of the Body Shape Questionnaire in Saudi Arabia. Studenttheses.uu.nl. (2022). Available online at: https://studenttheses.uu.nl/handle/20.500.12932/41464?show=full.
46. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). (2000) 25:3186–91. doi: 10.1097/00007632-200012150-00014
47. Abd El-Fatah NK, Alshehri AA, Alsulami FH, Alasmari N, Osman NA. Association between mental health outcomes and changes in lifestyle behavior index among Saudi adults 16 weeks after COVID-19 pandemic lockdown release. Front Public Health. (2022) 9:728117. doi: 10.3389/fpubh.2021.728117
48. Alkhaldy AA, Aljahdli ES, Mosli MH, Jawa HA, Alsahafi MA, Qari YA. Adherence to the Saudi dietary guidelines and its relation to colorectal polyps: a university hospital-based study. J Taibah Univ Med Sci. (2019) 15:25–31. doi: 10.1016/j.jtumed.2019.11.001
49. Duncan MJ, Kline CE, Vandelanotte C, Sargent C, Rogers NL, Di Milia L. Cross-sectional associations between multiple lifestyle behaviors and health-related quality of life in the 10,000 Steps cohort. PLoS ONE. (2014) 9:e94184. doi: 10.1371/journal.pone.0094184
50. Manchia M, Gathier AW, Yapici-Eser H, Schmidt MV, de Quervain D, van Amelsvoort T, et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: a critical review across waves. Eur Neuropsychopharmacol. (2022) 55:22–83. doi: 10.1016/j.euroneuro.2021.10.864
51. Ali AM, Hendawy AO, Almarwani AM, Alzahrani N, Ibrahim N, Alkhamees AA, et al. The six-item version of the internet addiction test: its development, psychometric properties, and measurement invariance among women with eating disorders and healthy school and university students. Int J Environ Res Public Health. (2021) 18:12341. doi: 10.3390/ijerph182312341
52. Ali AM, Al-Amer R, Atout M, Ali TS, Mansour AMH, Khatatbeh H, et al. The nine-item internet gaming disorder scale (IGDS9-SF): its psychometric properties among Sri Lankan students and measurement invariance across Sri Lanka, Turkey, Australia, and the USA. Healthcare (Basel). (2022) 10:490. doi: 10.3390/healthcare10030490
53. Grabe S, Ward LM, Hyde JS. The role of the media in body image concerns among women: a meta-analysis of experimental and correlational studies. Psychol Bull. (2008). 134:460–76. doi: 10.1037/0033-2909.134.3.460
54. Smith AR, Hames JL, Joiner Jr TE. Status update: maladaptive Facebook usage predicts increases in body dissatisfaction and bulimic symptoms. J Affect Disord. (2013) 149:235–40. doi: 10.1016/j.jad.2013.01.032
55. Holland G, Tiggemann M. A systematic review of the impact of the use of social networking sites on body image and disordered eating outcomes. Body Image. (2016) 17:100–10. doi: 10.1016/j.bodyim.2016.02.008
56. Murray M, Maras D, Goldfield GS. Excessive time on social networking sites and disordered eating behaviors among undergraduate students: appearance and weight esteem as mediating pathways. Cyberpsychol Behav Soc Netw. (2016) 19:709–15. doi: 10.1089/cyber.2016.0384
57. Cohen R, Newton-John T, Slater A. ‘Selfie'-objectification: the role of selfies in self-objectification and disordered eating in young women. Comput. Hum. Behav. (2018) 79:68–74. doi: 10.1016/j.chb.2017.10.027
58. Almuhlafi M, Jamilah KA, Almutairi AF, Salam M. Relationship between early menarche, obesity, and disordered eating behaviors: a school-based cross-sectional survey in Northern Saudi Arabia. Diabetes Metab Syndr Obes. (2018) 11:743–51. doi: 10.2147/DMSO.S180697
59. Al-Jumayan AA, Al-Eid NA, AlShamlan NA, AlOmar RS. Prevalence and associated factors of eating disorders in patrons of sport centers in Saudi Arabia. J Family Community Med. (2021) 28:94–102. doi: 10.4103/jfcm.jfcm_113_21
60. Ferguson CJ, Muñoz ME, Garza A, Galindo M. Concurrent and prospective analyses of peer, television and social media influences on body dissatisfaction, eating disorder symptoms and life satisfaction in adolescent girls. J Youth Adolesc. (2014) 43:1–14. doi: 10.1007/s10964-012-9898-9
61. Klaczynski PA, Felmban WS. Thin idealization and causal attributions mediate the association between culture and obesity stereotypes: an examination of Chinese and American adolescents. Br. J. Dev. Psychol. (2019) 37:14–32. doi: 10.1111/bjdp.12250
62. Easton S, Morton K, Tappy Z, Francis D, Dennison L. Young people's experiences of viewing the fitspiration social media trend: qualitative study. J Med Int Res. (2018) 20:e219. doi: 10.2196/jmir.9156
63. Ali AM, Hori H, Kim Y, Kunugi H. Predictors of nutritional status, depression, internet addiction, Facebook addiction, and tobacco smoking among women with eating disorders in Spain. Front Psychiatry. (2021) 12:735109. doi: 10.3389/fpsyt.2021.735109
64. Lee HE, Taniguchi E, Modica A, Park H. Effects of witnessing fat talk on body satisfaction and psychological well-being: a cross-cultural comparison of Korea and the United States. Soc Behav. (2013) 41:1279–96. doi: 10.2224/sbp.2013.41.8.1279
65. Fabris MA, Marengo D, Longobardi C, Settanni M. Investigating the links between fear of missing out, social media addiction, and emotional symptoms in adolescence: the role of stress associated with neglect and negative reactions on social media. Addict Behav. (2020) 106:106364. doi: 10.1016/j.addbeh.2020.106364
66. Dooley-Hash S, Adam M, Walton M, Blow F, Cunningham R. The prevalence and correlates of eating disorders in adult emergency department patients. Int J Eat Disord. (2019) 52:1281e1290. doi: 10.1002/eat.23140
67. Konttinen H, Männistö S, Sarlio-Lähteenkorva S, Silventoinen K, Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite. (2010) 54:473–9. doi: 10.1016/j.appet.2010.01.014
68. Badrasawi M, Zidan S. Binge eating symptoms prevalence and relationship with psychosocial factors among female undergraduate students at Palestine Polytechnic University: a cross sectional study. J. Eat. Disord. (2019) 7:33. doi: 10.1186/s40337-019-0263-1
69. Sundgot-Borgen J, Torstveit M. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med. (2004) 14:25e32. doi: 10.1097/00042752-200401000-00005
70. Chapman J, Woodman T. Disordered eating in male athletes: a meta-analysis. J Sports Sci. (2016) 34:101–9. doi: 10.1080/02640414.2015.1040824
71. Krentz EM, Warschburger P. Sports-related correlates of disordered eating in aesthetic sports. Psychol. Sport Exerc. (2011) 12:375–82. doi: 10.1016/j.psychsport.2011.03.004
Keywords: Saudi Arabia, college, social network navigation, high-risk disordered eating, female, social media, COVID pandemic
Citation: Raja N AA, Osman NA, Alqethami AM and Abd El-Fatah NK (2022) The relationship between the high-risk disordered eating and social network navigation among Saudi college females during the COVID pandemic. Front. Public Health 10:949051. doi: 10.3389/fpubh.2022.949051
Received: 20 May 2022; Accepted: 11 August 2022;
Published: 06 September 2022.
Edited by:
Wulf Rössler, Charité Universitätsmedizin Berlin, GermanyReviewed by:
Tom Sander, Hochschule Ludwigshafen am Rhein, GermanyNashwa Ibrahim, Mansoura University, Egypt
Marta Kożybska, Pomeranian Medical University, Poland
Copyright © 2022 Raja N, Osman, Alqethami and Abd El-Fatah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nesrin Kamal Abd El-Fatah, bmVzcmluX2thbWFsQHlhaG9vLmNvbQ==
 Alotaibi Abdulaziz Raja N
Alotaibi Abdulaziz Raja N Nermin A. Osman
Nermin A. Osman Abdullah Muidh Alqethami1
Abdullah Muidh Alqethami1 Nesrin Kamal Abd El-Fatah
Nesrin Kamal Abd El-Fatah