- 1School of Public Health, Peking University, Beijing, China
- 2Yunnan Center for Disease Control and Prevention, Kunming, China
- 3Chinese Center for Disease Control and Prevention, Beijing, China
- 4Center for Intelligent Public Health, Institute for Artificial Intelligence, Peking University, Beijing, China
- 5Center for Drug Abuse Control and Prevention, National Institute of Health Data Science, Peking University, Beijing, China
- 6Peking University Clinical Research Institute, Beijing, China
Background: Imported COVID-19 patients posed great challenges to border areas' COVID-19 control. However, research was scarce to reveal epidemiological characteristics of COVID-19 in border areas. This study aimed to explore the detailed transmission chains, and reveal epidemiological and clinical characteristics of the largest COVID-19 outbreak caused by Delta variant of concern (VOC) occurred in the China-Myanmar border area.
Methods: During the outbreak from July to September, 2021 in Ruili City, Yunnan Province, China, epidemiological investigation data and clinical-related data pertaining to confirmed COVID-19 patients were collected. Patients' contact history data and viral gene sequencing were used for inference of transmission chains. Sociodemographic and epidemiological characteristics, cycle threshold (Ct) value, and antibodies level were compared between patients who were vaccinated against COVID-19 or not.
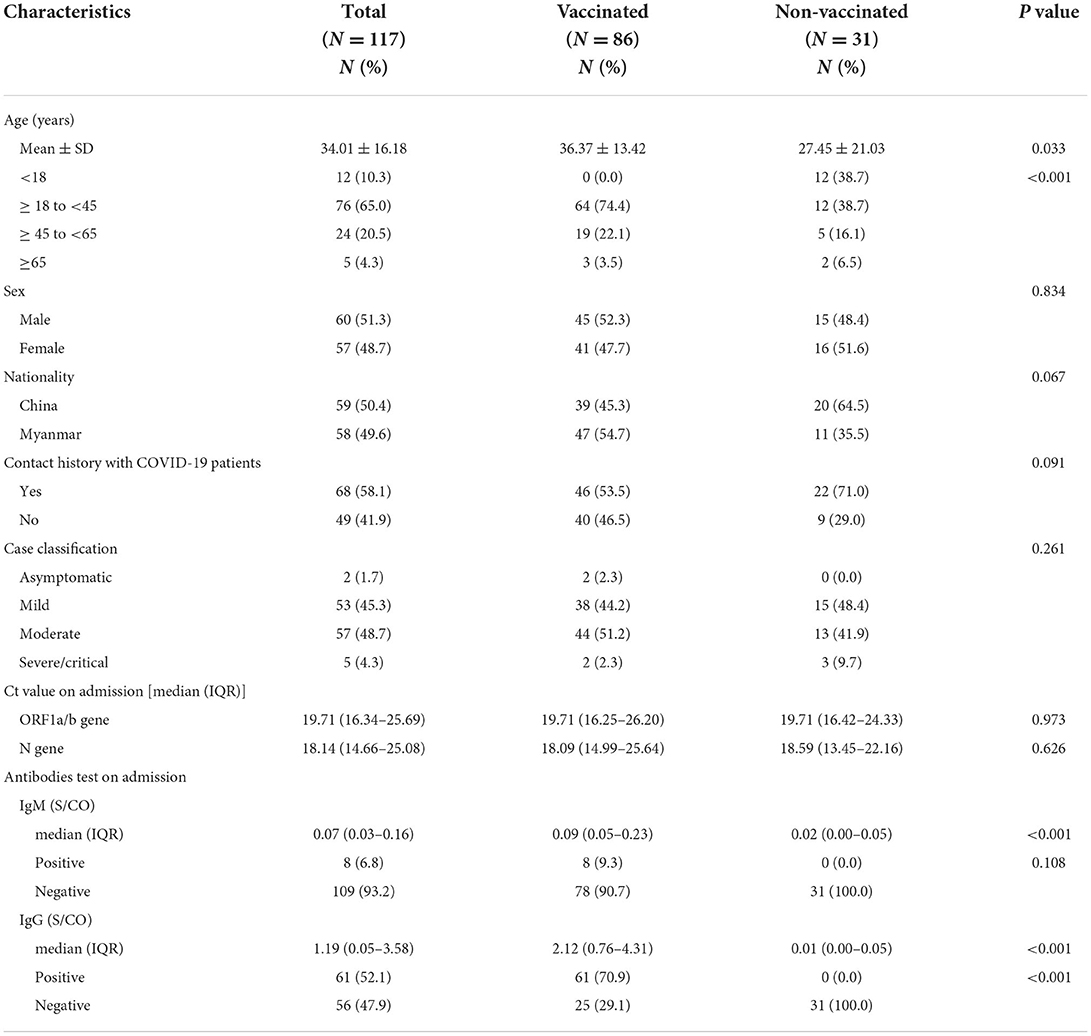
Results: A total of 117 COVID-19 patients were confirmed during the outbreak, among which 86 (73.5%) were breakthrough infections. These patients evenly split between Chinese and Myanmar people (50.4% vs. 49.6%). Most of these patients were mild (45.3%) or moderate (48.7%) infections with no death reported. Multi-source of infection led to 16 transmission chains with a maximum of 45 patients in one chain. Patients vaccinated against COVID-19 before infection had relatively higher antibodies (IgM and IgG) levels and more rapid response to infection than non-vaccinated patients (p < 0.05).
Conclusion: Land border areas have greater risks of imported COVID-19 and more complicated epidemics. It should be cautious in formulating entry and exit requirements for border areas. The immune effect of COVID-19 vaccines and related mechanism should be further explored.
Introduction
The ongoing coronavirus disease 2019 (COVID-19) epidemic has led to a high burden in public health and people's daily lives. After the highly infectious SARS-CoV-2 Delta variant strain (B.1.617.2) was first found in India, it spread rapidly around the world until now and was listed as one of the two currently circulating variants of concern (VOCs) by World Health Organization (WHO) (1). Although the Omicron VOC is now the dominant strain in many countries, a recent study has indicated that the Omicron has not eliminated Delta VOC and the Delta might have the risk to re-emerge (2). Considering the relatively higher infectivity and transmissibility of the Delta VOC (3), it still deserves enough attention.
Since the first local Chinese COVID-19 patient infected with SARS-CoV-2 Delta VOC was detected in Guangzhou, China on 21 May 2021, Delta VOC has spread to more than 50 cities around China and led to eleven outbreaks, all of which were caused by imported COVID-19 patients (4). The pressure of COVID-19 prevention and control brought by imported cases in border areas was even greater. China has 14 land neighbors, and the China-Myanmar border in the southwest is a typical representative of land borders. The border area is near the Kokang region in northern Shan State of Myanmar that are often at civil war, which results in poor accessibility to basic health services (5). In addition, represented by Jiegao Border Trade Zone, the commodity trade between China and Myanmar is prosperous in this area, which is also China's main jade raw material distribution center and a popular tourist destination. Because of the above geographical and cultural characteristics, the China-Myanmar border area in China is a traditional area with high risk of imported infectious diseases, such as malaria (6), which also faces the a huge pressure caused by imported COVID-19 cases and the risk of the epidemic spreading across the country during the COVID-19 pandemic. However, few studies have revealed the detailed epidemiological characteristics of COVID-19 in border areas.
On 4 July, 2021, three confirmed COVID-19 patients infected with Delta VOC was reported by the government of Ruili City, Yunnan Province, since then, the largest COVID-19 outbreak caused by Delta VOC in China's border areas occurred, which was named as the “July 4” COVID-19 outbreak. In this study, we aimed to explore the detailed transmission chains, and reveal epidemiological and clinical characteristics of this outbreak occurred in the China-Myanmar border areas.
Methods
Study design and epidemiological survey
All confirmed patients infected with SARS-CoV-2 Delta VOC during the “July 4” outbreak from July to September, 2021 in Ruili City, Yunnan Province, China, which is an important land border port city near the China-Myanmar border (Figure 1A), were included in this study. According to the National Health Commission's guidelines (7), the diagnosis of COVID-19 patients were confirmed by the local Center for Disease Control and Prevention (CDC), and were classified into mild, moderate, severe, and critical according to severity. Detailed epidemiological investigation and clinical data collection were conducted to confirmed patients and their close contacts by local CDC and the Yunnan Provincial CDC.
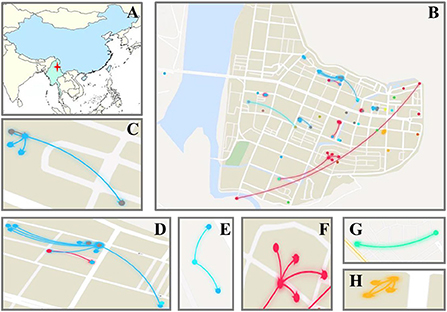
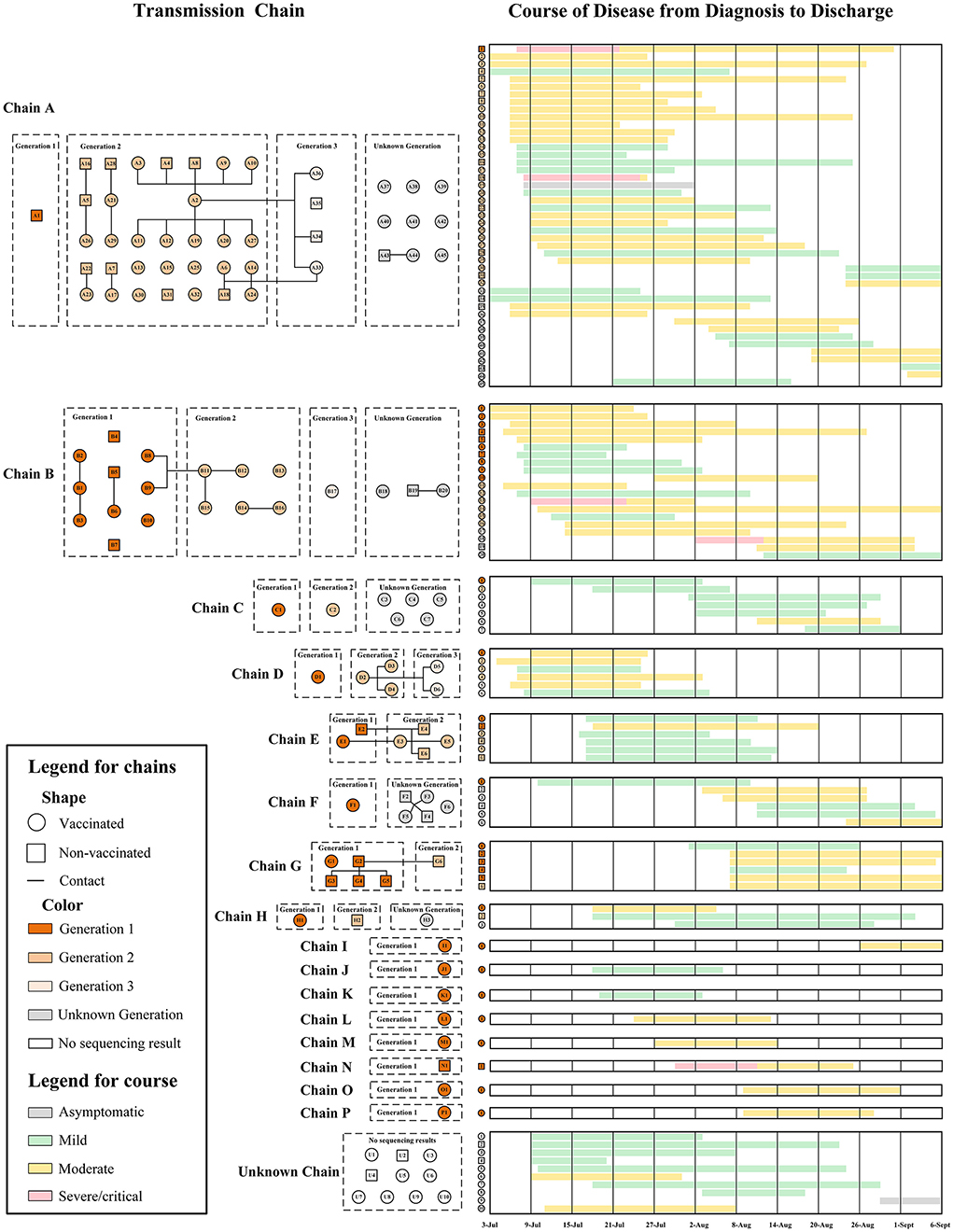
Figure 1. Geographical distribution of confirmed patients and transmission of the virus. (A): The location of Ruili City. (B–H): Geographical distribution of confirmed cases and transmission chains; the lines mean the virus transmission caused by close contacts; different colors of lines means different transmission chains.
Based on the epidemiological investigation, these patients' sociodemographic information, address where the patients might be infected (residential and/or workplace address), travel track, contact history, and other activities information were collected. These patients' close contacts were found based on epidemiological investigation data and travel history big data. The detailed epidemiological investigation was also conducted to the close contacts. Using the unique identifier making up of ID number and name, their COVID-19 vaccination records were extracted from the vaccination database by the local CDC's staff.
The ethical approval was provided by the Mang City Center for Disease Control and Prevention, Yunnan, China, and all participants gave oral informed consent because of their level of education and the urgency of emerging infectious disease's control.
Laboratory test
Regular nasopharyngeal swabs of confirmed COVID-19 patients were collected for SARS-CoV-2 nucleic acid testing using Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR) targeting of ORF1ab and N genes. The Novel Coronavirus 2019 Nucleic Acid Test Kit (manufactured by Bojie Medical Technology, Shanghai Municipality and Daan Gene Company, Guangzhou City, China). A cycle threshold (Ct) value of below 40 was considered as a positive result. Regular serum samples were collected from confirmed COVID-19 patients at least once a week for antibodies IgM and IgG testing. Anti-SARS-CoV-2 Rapid Test Kit (manufactured by Antubio Diagnostics Company, Zhengzhou, China) was used, and a value of over 1 S/CO was considered as positive result. The biological samples of these patients were also sent to the China CDC to obtain virus genotyping and inference of transmission chains. The information of transmission chains used in this study was obtained from China CDC's reports combining with the contacts history among patients. The complete genomic sequences were acquired from swab samples. Compared with the reference genome sequence of Wuhan (GenBank No.NC_045512), genome sequences from Ruili's patients existed 35–45 unique nucleotide mutation sites, which belonged to Delta variant strain (B.1.617.2). Based on the phylogenetic tree analysis, the genome sequences of Ruili's patients could be assigned to different lineages, and patients in the same lineages could be considered as the same transmission chains. The methods of genomic sequences analysis were described in previous studies in detail (8–10).
Outbreak control measures
In order to effectively control the outbreak, the following measures were implemented. First, patients were immediately transported to a designated hospital for treatment and quarantine, and their close contacts received medical observation at designated hotels or home for 14 days. Second, epidemiological investigations were conducted to confirmed COVID-19 patients and their close contacts to know details about the history of travel, work, contacts, and activities; and regular nucleic acid testing and serum SARS-CoV-2 antibody testing were provided to them. COVID-19 patients with two consecutive negative nucleic acid test results and without COVID-19-related symptoms, signs and imaging abnormalities could be discharged. For their close contacts, the medical observation could also be lifted for those who had no typical symptoms or positive nucleic acid test results during the 14 days. Third, regular SARS-CoV-2 nucleic acid testing for high-risk populations was conducted, and regular disinfection of public places, medical quarantine sites, and border areas were strengthened. Fourth, the administration of entry and exit in border areas was also strengthened, and all people entering China needed to be retested for SARS-CoV-2 nucleic acid regularly. Because of these proactive and positive measures, COVID-19 did not spread widely and the “July 4” outbreak was declared over on 15 September 2021.
Statistical analysis
The confirmed COVID-19 patients were divided into two groups according to whether they were vaccinated against COVID-19. Sociodemographic and epidemiological characteristics, Ct value, and antibodies level were described and compared between the two groups. Student's t test or Mann-Whitney U test was used to compare continuous variables when applicable, respectively. Categorical variables were compared by chi-square test or Fisher's exact test when data was limited. A p value of 0.05 or less was regarded as significant difference for the two-sided test. Statistical analyses were done with SPSS version 21.0 (IBM Corp).
Results
After the first three cases (index cases, including two Chinses men and one Myanmar man) were reported, two waves of cases were observed in the outbreak, of which the largest wave was in early July, and the other was in early August. After that, cases were sporadic until the outbreak ended in September (Supplementary Figure 1). A total of 117 COVID-19 patients were confirmed in the “July 4” outbreak with an average age of 34.01 ± 16.18 years, among which 86 (73.5%) were breakthrough infections with a median of 65 days (IQR: 34–159 days) from the date of the last dose of vaccine to the first positive nucleic acid test result. Most of these patients (65.0%) were 18–45 years and were evenly split between male (51.3%) and female (48.7%). About a half of them (49.6%) came from Myanmar, and 58.1% of them reported that they had clear contact history with other COVID-19 patients. Most of these patients were mild (45.3%) or moderate (48.7%) infections with no death in this outbreak (Table 1, Figure 2).
Based on gene sequence inference, 16 transmission chains were identified, of which the largest (Chain A) included 45 patients and the virus transmitted for three generations. There were also eight transmission chains (Chain I–P) that had only one patient (Figure 2). Nine of the 16 transmission chains included Myanmar patients, and the index cases (Generation 1 cases) in five of these transmission chains were confirmed to come from Myanmar. Majority of the transmission chains were in Jiegao Community, which was the largest land port and trade zone between China and Myanmar (Figure 1B). The address where the patients might be infected and the geographic connections of patients in different transmission chains were shown in Figures 1B–H. Some clustered transmissions in adjacent buildings or stories were observed in this outbreak (Figures 1E–H). Meanwhile, because of the transportation and the need of goods delivery, virus could also spread over longer distances across blocks (the red lines in Figure 1B, and the blue lines in Figures 1B–D).
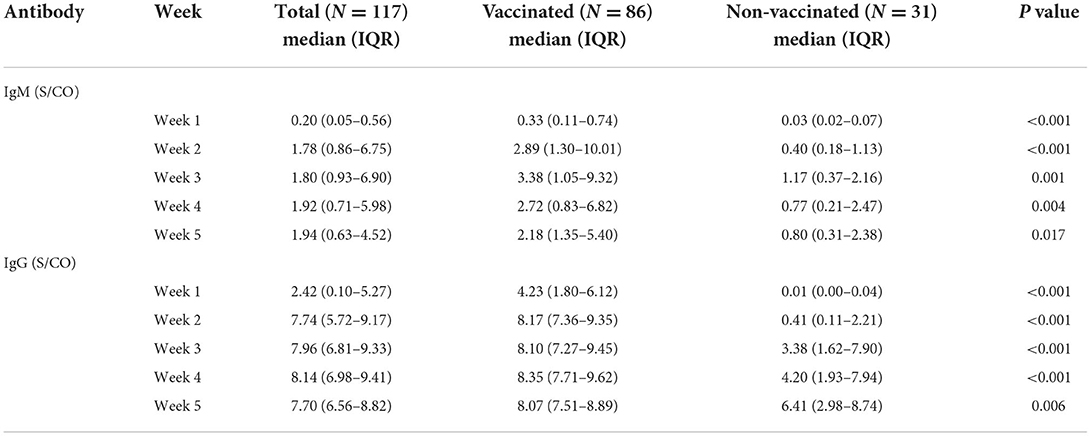
Patients who had been vaccinated against COVID-19 were older than non-vaccinated patients (p <0.05), and 38.7% of the non-vaccinated patients were children under 18 years, while no children infections were found among vaccinated patients (p < 0.05). On admission, the IgM and IgG values of vaccinated patients were higher than that of non-vaccinated patients (p < 0.05), 70.9% of vaccinated patients had positive IgG test results while no patient's IgG test result was positive among non-vaccinated patients (p < 0.05) (Table 1). During the five-week course of disease after diagnosis, the antibodies values of vaccinated patients were still higher than non-vaccinated (p < 0.05). In addition, the antibodies rose more quickly among vaccinated patients than non-vaccinated, which showed a sharper increase in the second week of both IgM and IgG among vaccinated patients, while the sharpest increase was observed in the third week of non-vaccinated patients (Table 2).
Discussion
This study was the first to clearly describe a COVID-19 outbreak event in land border area of China, which was the largest COVID-19 outbreak caused by Delta VOC in China's border areas. Because of timely control measures and proactive case detection and tracking, patients were detected and treated in a timely manner, with few cases of severe or critical illness and no deaths. The fact that nearly half of the COVID-19 patients came from Myanmar showed that this was a cross-border outbreak. Several imported outbreaks of Delta VOC have been reported in China, and most of them were related to imported cases on specific international flights, such as the outbreak in Nanjing and Guangzhou (3, 4, 11–13). The single source of infection led to the chains of transmission fewer and relatively clear in the outbreak caused by flights imported cases. The outbreak in Nanjing in July, 2021 was caused by a flight from Moscow, and the index case in China was a cabin cleaning staff member servicing the flight at Nanjing Lukou Airport (4, 11). After that, the virus spread to other cleaning staff, airport passengers, and then to local communities leading to community transmission, the transmission chain of which was relatively clear (4, 11). Similar to the outbreak in Nanjing, the outbreak in Guangzhou occurred from May 21 to Jun 18, 2021 was also due to the first confirmed local case's accidental exposure to an imported case (3). A clear seven-generation transmission chain including 157 patients was found based on epidemiological investigation (3). However, in stark contrast to those imported outbreaks related to international flights, the Ruili outbreak was due to imported Myanmar cases entering China through land border. Before the “July 4” COVID-19 outbreak, though the Ruili City's border management policy has not been relaxed, the newly reported COVID-19 cases in Myanmar increased sharply from late May, 2021, which could lead to an increase in the proportion of infected persons entering Ruili City from Myanmar and brought higher pressure of COVID-19 importations (Supplementary Figure 2). Therefore, because new sources of infection kept entering, the 16 transmission chains with Myanmar patients serving as index cases of several chains indicated the possibility of multi-source transmission of imported cases from Myanmar, which was also a good demonstration of the difficulties in COVID-19 control at land border ports. In addition, several transmission chains had only one case, there might be two reasons to explain this phenomenon. First, although the epidemiological investigation has been thorough, some potential contacts between the patients might not be found; and insidious transmission by probable cases who could not be detected by nucleic acid testing might exist (14), which could also make the initial transmission difficult to be observed. Second, it is possible that some imported cases were detected early under relatively strict outbreak control measures, which avoided further transmission.
Compared with the patients' characteristics in the Nanjing and Guangzhou's outbreak, more patients from Myanmar were found in the community transmission in Ruili City, while almost all of patients in Nanjing and Guangzhou's outbreak were Chinese (3, 11). Because many young adults were engaged in goods trading in Ruili City, the age of COVID-19 patients in Ruili's outbreak (34.01 ± 16.18 years) was much younger than that in the outbreak in Nanjing (43.25 ± 16.96 years) and Guangzhou (Median age 47.0 years) (3, 11). Similar with Nanjing and Guangzhou's outbreak, the majority of patients had mild and moderate symptoms, but the proportion of patients with severe or critical symptoms was much lower in Ruili's outbreak (4.3%) than Guangzhou's outbreak (12.5%), which might be due to the high proportion of elderly patients (33%) in Guangzhou's outbreak (3, 11). However, patients with mild symptoms may not be aware of their symptoms and may not seek medical services. The higher proportion of patients with mild symptoms in Ruili's outbreak than that in Guangzhou (45.3% vs. 25.8%) brought challenges to the effective implementation of symptom monitoring and was more likely to cause hidden spread in communities (3).
According to the comparison of breakthrough cases and those who did not vaccinated against COVID-19, one obvious difference was that no children infections were breakthrough cases. The reason was that China had not provided COVID-19 vaccination to minors prior to the current outbreak (15). Similar to previous study, the antibodies value rose sharply in the first 2 weeks on admission after onset of symptoms among both vaccinated and non-vaccinated patients (16). The more rapid response to infection of vaccinated patients' antibodies could be related to the presence of immune memory after vaccination; after infection of SARS-CoV-2, lymphocytes in the body would be activated and antibodies could be generated rapidly in a short time (17, 18).
This study had strong practical implications. First, it should be cautious in opening borders, especially for land borders which represented by the China-Myanmar border where the COVID-19 epidemic is under effective control on one side of the border, while the epidemic of the other side is out of control. Providing medical services and vaccinations to refugees around border areas is also beneficial to COVID-19 prevention and control in the importing countries, which could also provide references for some European countries where refugee crisis was worsening (19). Second, most of the patients in this outbreak were breakthrough cases, and previous report had indicated that the effectiveness of vaccines against infection was limited (20). Therefore, some necessary non-pharmacological interventions could not be abandoned, especially for personal protection measures, such as facemask wearing. However, a limitation of this study was that the follow-up period was relatively short, and the change of antibodies in a longer time after infection could not be reflected well. In further researches, it is necessary to strengthen the exploration of SARS-CoV-2 antibody response mechanism. In addition, it is essential to explore the similarities and differences of SARS-CoV-2 antibodies in determining the course of disease in vaccinated and non-vaccinated people, and to verify the feasibility of antibodies as biomarkers to determine the time of infection.
In conclusion, this study revealed the epidemiological and clinical characteristics of the largest COVID-19 outbreak caused by Delta VOC in the China-Myanmar border area. Different from the clear single transmission chain caused by international flights passengers in other cities' COVID-19 outbreaks, 16 transmission chains were found in the “July 4” outbreak. Patients vaccinated against COVID-19 before infection had relatively higher antibodies (IgM and IgG) levels and more rapid response to infection than non-vaccinated patients. This study indicated that attention should be paid to the control and research of imported COVID-19 cases in border areas, and research on the immune effect of COVID-19 vaccines and related mechanism should be strengthened.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Mang City Center for Disease Control and Prevention, Yunnan, China. All participants gave oral informed consent because of their level of education and the urgency of emerging infectious disease's control in accordance with the national legislation and the institutional requirements.
Author contributions
TS and BZ had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: XY and TS. Drafting of the manuscript: XY, ZW, and BZ. Statistical analysis: XY, XW, XZ, and ZW. Obtained funding: ZJ and BZ. Administrative, technical, or material support: LH and LC. Supervision: TS, TL, and BZ. Acquisition, analysis, or interpretation of data and critical revision of the manuscript for important intellectual content: All authors. All authors read and approved the final manuscript.
Funding
This work was supported by National Natural Science Foundation of China [Grant Numbers 72104008, 72174004, 91546203, and 91846302], National Key Research and Development Program of China [Grant Number 2021YFC0863400].
Acknowledgments
We thank the staff of CDC for their work of epidemiological investigations and laboratory testing. We also thank the confirmed COVID-19 cases and their close contacts for their cooperation in management and the research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.962214/full#supplementary-material
References
1. World Health Organization. Tracking SARS-CoV-2 variants. (2022). Available online at: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (accessed May 5, 2022).
2. Yaniv K, Ozer E, Shagan M, Paitan Y, Granek R, Kushmaro A. Managing an evolving pandemic: cryptic circulation of the Delta variant during the Omicron rise. Sci Total Environ. (2022) 836:155599. doi: 10.1016/j.scitotenv.2022.155599
3. Wang Y, Chen R, Hu F, Lan Y, Yang Z, Zhan C, et al. Transmission, viral kinetics and clinical characteristics of the emergent SARS-CoV-2 Delta VOC in Guangzhou, China. EClinicalMedicine. (2021) 40:101129. doi: 10.1016/j.eclinm.2021.101129
4. Zhou L, Nie K, Zhao H, Zhao X, Ye B, Wang J, et al. Eleven COVID-19 Outbreaks with Local Transmissions Caused by the Imported SARS-CoV-2 Delta VOC - China, July-August, 2021. China CDC Wkly. (2021) 3:863–8. doi: 10.46234/ccdcw2021.213
5. The Chindwin. Myanmar's Civil War: Nearly 2,000 Junta Soldiers Were Killed in a Month. Available online at: https://www.thechindwin.com/myanmars-civil-war-nearly-2000-junta-soldiers-were-killed-in-a-month/ (accessed May 1, 2022).
6. Wang X, Yang L, Jiang T, Zhang B, Wang S, Wu X, et al. Effects of a malaria elimination program: a retrospective study of 623 cases from 2008 to 2013 in a Chinese county hospital near the China–Myanmar border. Emerg Microbes Infect. (2016) 5:e6. doi: 10.1038/emi.2016.6
7. National Health Commission & State Administration of Traditional Chinese Medicine. Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 8 revised version). (2021). Available online at: http://www.gov.cn/zhengce/zhengceku/2021-04/15/5599795/files/e9ce837932e6434db998bdbbc5d36d32.pdf (accessed May 1, 2022).
8. Zhang M, Zhou J, Jia S, Zhao X, Chen Y, Sun Y, et al. Undocumented migrants reintroducing COVID-19, Yunnan Province, China. Emerg Infect Dis. (2021) 27:1543–5. doi: 10.3201/eid2705.204944
9. Tan W, Niu P, Zhao X, Pan Y, Zhang Y, Chen L, et al. Reemergent cases of COVID-19 - Xinfadi wholesales market, Beijing municipality, China, June 11, 2020. China CDC Wkly. (2020) 2:502–4. doi: 10.46234/ccdcw2020.132
10. Ma H, Wang Z, Zhao X, Han J, Zhang Y, Wang H, et al. Long distance transmission of SARS-CoV-2 from contaminated cold chain products to humans - Qingdao City, Shandong Province, China, September 2020. China CDC Wkly. (2021) 3:637–44. doi: 10.46234/ccdcw2021.164
11. Liu Y, Yang B, Liu L, Jilili M, Yang A. Occupational characteristics in the outbreak of the COVID-19 Delta variant in Nanjing, China: rethinking the occupational health and safety vulnerability of essential workers. Int J Environ Res Public Health. (2021) 18:10734. doi: 10.3390/ijerph182010734
12. Li Z, Nie K, Li K, Hu Y, Song Y, Kang M, et al. Genome characterization of the first outbreak of COVID-19 Delta variant B.1.617.2 - Guangzhou City, Guangdong Province, China, May 2021. China CDC Wkly. (2021) 3:587–9. doi: 10.46234/ccdcw2021.151
13. Zhang M, Xiao J, Deng A, Zhang Y, Zhuang Y, Hu T, et al. Transmission dynamics of an outbreak of the COVID-19 Delta variant B.1.617.2 - Guangdong Province, China, May-June 2021. China CDC Wkly. (2021) 3:584–6. doi: 10.46234/ccdcw2021.148
14. Yan X, Chang L, Wang Z, Hao L, Jia Z, Zhang B, et al. Exploring the bridge cases' role in the transmission of the SARS-CoV-2 Delta Variant — Ruili city, Yunnan Province, China, July–September 2021. China CDC Wkly. (2021) 3:1065–70. doi: 10.46234/ccdcw2021.239
15. Xinhua. China to Extend Mass Vaccination Program to Minors Aged 12–17. (2021). Available online at: http://www.china.org.cn/china/2021-07/18/content_77634978.htm (accessed February 20, 2022).
16. Peeling RW, Heymann DL, Teo YY, Garcia PJ. Diagnostics for COVID-19: moving from pandemic response to control. Lancet. (2022) 399:757–68. doi: 10.1016/S0140-6736(21)02346-1
17. Rodda LB, Netland J, Shehata L, Pruner KB, Morawski PA, Thouvenel CD, et al. Functional SARS-CoV-2-Specific Immune Memory Persists after Mild COVID-19. Cell. (2021) 184:169–83.e17. doi: 10.1016/j.cell.2020.11.029
18. Jarjour NN, Masopust D, Jameson SC. T Cell memory: understanding COVID-19. Immunity. (2021) 54:14–8. doi: 10.1016/j.immuni.2020.12.009
19. CNN. Crisis Worsens on Poland-Belarus Border as Migrants Congregate and Troops are Mobilized. (2021). Available online at: https://edition.cnn.com/2021/11/08/europe/poland-belarus-border-migrants-intl/index.html (accessed May 1, 2022).
20. Forbes. Pfizer Shot Just 39% Effective Against Delta Infection, But Largely Prevents Severe Illness, Israel Study Suggests. (2021). Available online at: https://www.forbes.com/sites/roberthart/2021/07/23/pfizer-shot-just-39-effective-against-delta-infection-but-largely-prevents-severe-illness-israel-study-suggests/?sh=4c029352584f (accessed May 1, 2022).
Keywords: China-Myanmar border, clinical characteristics, COVID-19 vaccination, outbreak, SARS-CoV-2 Delta VOC, transmission
Citation: Yan X, Hao L, Wang Z, Wang X, Zhang X, Li T, Jia Z, Chang L, Zhang B and Shui T (2022) Epidemiological and clinical characteristics of the largest COVID-19 outbreak along the China-Myanmar border in Ruili City, Yunnan Province, China. Front. Public Health 10:962214. doi: 10.3389/fpubh.2022.962214
Received: 06 June 2022; Accepted: 20 July 2022;
Published: 23 August 2022.
Edited by:
Xiaoming Wang, University of California, Irvine, United StatesReviewed by:
Naizhe Li, Beijing Normal University, ChinaYe Minn Htun, Health and Disease Control Unit, Myanmar
Copyright © 2022 Yan, Hao, Wang, Wang, Zhang, Li, Jia, Chang, Zhang and Shui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Zhang, emhhbmdibzAxMzZAcGt1LmVkdS5jbg==; Tiejun Shui, Njc2Mzc1MzlAcXEuY29t
†These authors have contributed equally to this work
 Xiangyu Yan
Xiangyu Yan Linhui Hao2†
Linhui Hao2† Zekun Wang
Zekun Wang Bo Zhang
Bo Zhang