- 1School of Nursing and Midwifery, Asrat Woldeyes Health Science Campus, Debre Berhan University, Debre Birhan, Ethiopia
- 2Department of Midwifery, Faculty of Public Health and Medical Science, Mettu University, Metu, Ethiopia
- 3Department of Midwifery, College of Medicine and Health Science, Debre Markos University, Debre Markos, Ethiopia
- 4Department of Midwifery, Bule Hora University, Bule Hora, Ethiopia
- 5Department of Midwifery, Jigjiga University, Jigjiga, Ethiopia
- 6Department of Clinical Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Global maternal deaths have either increased or stagnated tragically. Obstetric hemorrhage (OH) remains the major cause of maternal deaths. Non-Pneumatic Anti-Shock Garment (NASG) has several positive results in the management of obstetric hemorrhage in resource-limited settings where getting definitive treatments are difficult and limited. Therefore, this study aimed to assess the proportion and factors associated with the utilization of NASG for the management of obstetric hemorrhage among healthcare providers in the North Shewa zone, Ethiopia.
Methods: A cross-sectional study was conducted at health facilities of the north Shewa zone, Ethiopia from June 10th-30th/2021. A simple random sampling (SRS) technique was employed among 360 healthcare providers. Data were collected using a pretested self-administered questionnaire. EpiData version 4.6 and SPSS 25 were used for data entry and analysis, respectively. Binary logistic regression analyses were undertaken to identify associated factors with the outcome variable. The level of significance was decided at a value of p of <0.05.
Results: The utilization of NASG for the management of obstetric hemorrhage among healthcare providers was 39% (95%CI: 34–45). Healthcare providers who received training on NASG (AOR = 3.3; 95%CI: 1.46−7.48), availability of NASG in the health facility (AOR = 9.17; 95%CI: 5.10–16.46), diploma (AOR = 2.63; 95%CI: 1.39–3.68), bachelor degree (AOR = 7.89; 95%CI: 3.1–16.29) and those healthcare providers who have a positive attitude toward utilization of NASG (AOR = 1.63; 95%CI: 1.14–2.82) were variables positively associated with the utilization of NASG.
Conclusion: In this study, almost two-fifths of healthcare providers used NASG for the management of obstetrics hemorrhage. Arranging educational opportunities and continuous professional development training for healthcare providers, providing in-service and refresher training, and making it available at health facilities may help healthcare providers to effectively use the device, thereby reducing maternal morbidity and mortality.
Introduction
Global statistics show that more than 303,000 women die annually and 2.6 million babies were stillborn, half occurring during the third trimester (1) with the vast majority (94%) of these deaths occurring in low resource settings (2). From the global figure, approximately 14,000 maternal deaths occur each year in Ethiopia with a higher lifetime risk of maternal mortality (3). The current evidence shows that four women die from every 1,000 live births in Ethiopia, which is the highest maternal death in the world (4).
Obstetric hemorrhage (OH) remains one of the foremost contributing factors to maternal mortality (5), accounting for 25 percent of maternal deaths globally (5, 6). OH is an emergency in which a woman loses a very large amount of blood during pregnancy, during delivery, and after childbirth. An estimated, 150,000 women die from a preventable obstetric hemorrhage each year; most of these deaths occur in low-resource settings (7, 8). According to the World Health Organization (WHO) report almost all maternal deaths occurred in low-income and lower-middle-income countries, and two-thirds (65%) occurred in the African Region (3).
One of the effective and recently recommended first-aid devices for the management and prevention of OH is the use of a non-pneumatic anti-shock garment (NASG) (9). The NASG is a valuable innovation for reducing maternal mortality and morbidity in developing nations (10, 11). It is a lightweight, reusable garment made of neoprene and Velcro, containing five segments that are closed tightly around the legs, pelvis, and abdomen. It also applies pressure to decrease blood flow to and within the compressed area, and redirects blood to the vital organs (i.e., heart, lungs, and brain), thereby stabilizing vital signs and resolving hypovolemic shock (12). It has been demonstrated that NASG reduces mortality for women in shock at the time of referral (13, 14). A systematic review also reported that NASG reduces maternal death due to OH compared the non-users (15). Similarly, a global health study showed that NASG reduces blood loss by 42–55%, maternal morbidity by 44–66%, mortality by 34–66%, and the need for emergency hysterectomies by 45–56% (16). About 96% of women survive following the use of NASG for severe OH. NASG reduces financial losses, particularly the costs of transfusions and medical care (17). The WHO and International Federation of Obstetricians and Gynecologists (FIGO) recommended the use of NASG for the prevention and treatment of postpartum hemorrhage (PPH) (18, 19).
Investing in women’s health, including ensuring women have safe and healthy pregnancies, deliveries, and post-partum periods contributes not only to improving household health outcomes but also advances social and political developments for the country (20, 21). Early NASG application in primary health care for women in hypovolemic shock has the potential to be cost-effective across many clinical settings (22). Many women in low-resource settings deliver far from health institutions. Thus, once bleeding starts, these women die before reaching or receiving appropriate treatment. WHO recommends NASG as a temporary measure to regain hemodynamic stability and allow patient transfer for definitive PPH treatment (23). However, for women in mild shock, NASG has smaller and uncertain effects (17).
Despite the efficacy of NASG in reducing maternal morbidity and mortality, its utilization remains low. In Nigeria, 46% of midwives use NASG for the management of PPH (24). Similarly, in Jimma Ethiopia, only 36.2% of midwives use NASG for the management of PPH and only 54% of the midwives had good knowledge of NASG (13). Evidence addressing healthcare providers (HCPs) utilization of NASG for the management of OH in Ethiopia is not well-documented and challenges the healthcare system. Understanding the factors responsible for the non-utilization of NASG will give insight into probable interventions that might improve utilization. Therefore, this study aimed to assess the proportion of NASG utilization and its associated factors among HCPs in the North Shewa zone, Ethiopia.
Methods
Study design, setting, and period
This cross-sectional study was conducted at health facilities in the North Shewa zone, Amhara regional state, northeast Ethiopia from June 10th–30th/2021. Amhara regional state has 11 zones; of these, North Shewa is one of the zones in the Amhara regional state. Debre Birhan is the capital city of the North Shewa Zone and is located 130 km Northeast of Addis Ababa on the Ethiopian highway. The zone comprises 439 kebeles and 24 districts with an estimated total population of 2,335,205 with 1,138,737 females and 1,196,408 males. There are 95 health centers, 13 Hospitals (of which two are private primary hospitals) 10 primary, two general, and one comprehensive specialized hospital. There are 772 Nurses, 452 midwives, 120 Laboratory professionals, 130 Pharmacists, 219 General Practitioners, 15 Obstetric specialists, 54 integrated emergency surgical officers (IESO), 56 Anesthesia, 22 Radiology technicians, and 15 mental health professionals working in the zone. Therefore, the study was conducted at five public hospitals and seven health centers in the North Shewa zone. The named health institutions were Debre Berhan comprehensive specialized hospital, Enat hospital, Shewarobit hospital, Arerti hospital, Ataye hospital, Enewari health center, Shewarobit health center, Ataye health center, Alem ketema health center, Debresina health center, Arerti health center, and Ayer tenna health center.
Source and study population
All obstetric healthcare providers who were working in North Shewa Zone public Health facilities were the source of population. And all obstetric care providers who are working in the selected public healthcare facilities and fulfilled the selection were the study population.
Eligibility criteria
Inclusion criteria and exclusion criteria
All obstetric care providers who were staffed in the respective wards in each public health facility were included in this study, whereas obstetric care providers who had been on leave at the time of data collection were excluded.
Sample size determination
The sample size for this study was determined by using a single population proportion formula by considering the following assumptions: 95% level of confidence, 36.2% provider’s utilization of NASG for PPH from a previous study (13), and 5% margin of error.
Taking a non-response rate of 5%, a total of 373 study participants was obtained.
Sampling technique and procedure
Data were collected from 12 randomly selected health facilities (5 public hospitals, and 7 health centers). A sampling frame was prepared by obtaining the list of obstetric care providers from each health facility’s human resources office. The total number of health professionals in the study setting during the data collection period was 1,215 and 466 in the selected facilities. Then, the total sample size was allocated to each selected health facility proportionally. Finally, SRS technique was employed to choose the study participants using a table of random generation. Thus, Debre Berhan comprehensive specialized hospital (n = 116), Enat hospital (n = 73), Arerti hospital (n = 63), Shewarobit hospital (n = 61), Ataye hospital (n = 58), Enewari health center (n = 18), Shewarobit health center (n = 13), Ataye health center (n = 15), Alem ketema health center (n = 11), Debresina health center (n = 12), Arerti health center (n = 12); and Ayer Tenna health center (n = 14) were included in the study (Figure 1).
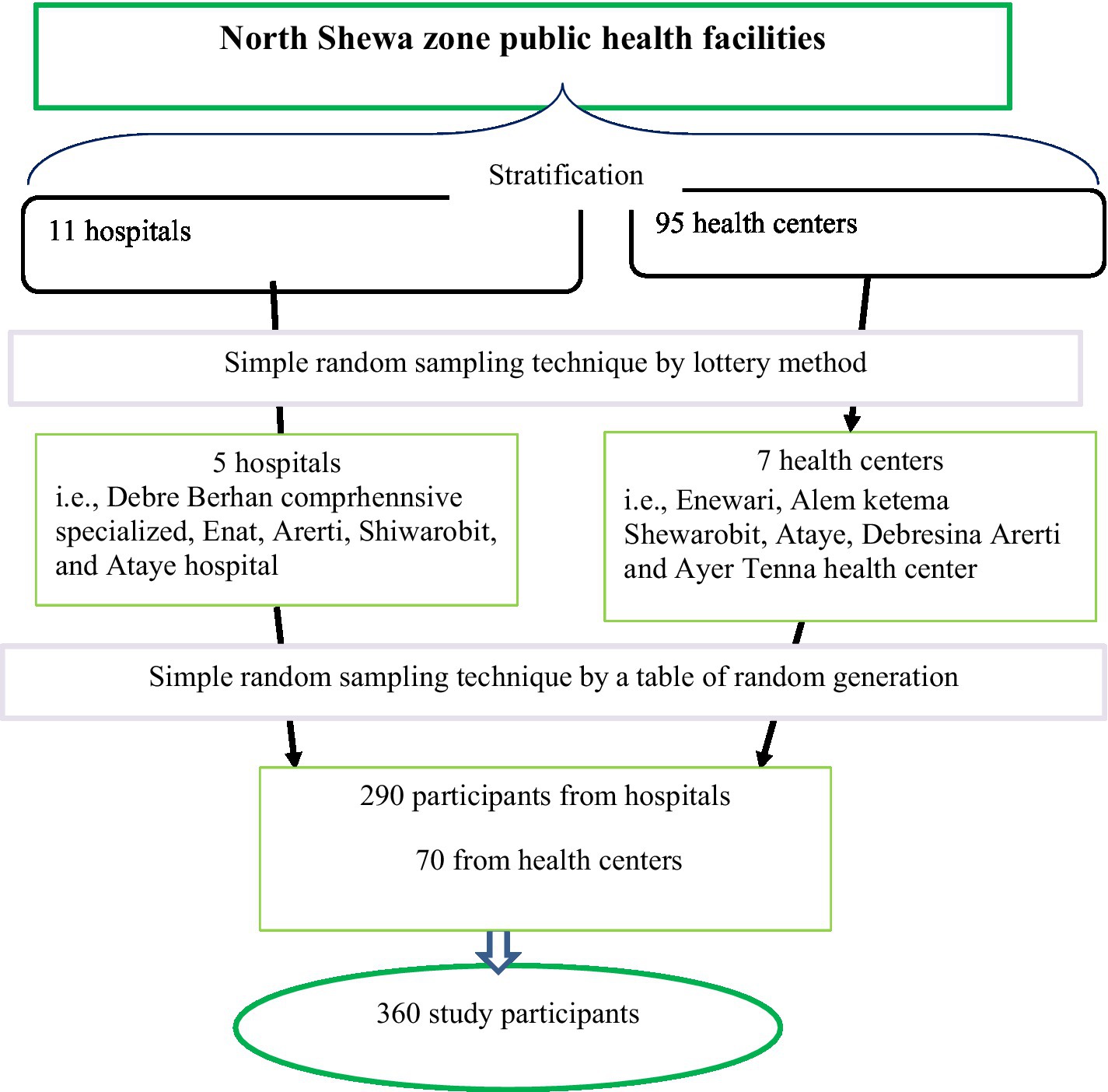
Figure 1. Utilization of non-pneumatic anti-shock garment for the management of obstetric hemorrhage among healthcare providers in north Shewa zone, Ethiopia.
Measurements and operational definitions
The dependent variable in this study was HCPs’ uptake of NASG. Accordingly, the participants were asked about their utilization of NASG in the management of obstetric hemorrhage at least once, the possible answers were Yes or No. A score of “1” was given for Yes and a score of “0” was given for No (13, 25).
Knowledge toward NASG
The study participants were asked 11 questions and those who scored 50% and above from all knowledge questions were considered as knowledgeable while those who below 50% were graded as having poor knowledge. Likewise, Attitude toward NASG refers to the extent to which an individual has a positive or negative estimation of the behavior of interest. HCPs’ attitude was measured using 10 questions: Each question has five points Likert scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree). The total score ranged from 10 to 50, attitude was considered “Positive” if the percentage score was 50% and above and “Negative” if less than 50% (13).
Educational level
In the Ethiopian context, a diploma means (grades 10 + 3 years of college or 12 + 3 years of college and a bachelor’s degree 12 + 3 or 4 years of university study).
Data collection tools, procedures, and quality control
The data collection tool was developed by reviewing literature (13, 26, 27) and data were collected using a structured self-readministered questionnaire. Initially, the questionnaire was prepared in English and translated into Amharic language and back to English to ensure its consistency and better understandability. Expert researchers judged the suitability of the questionnaire and the overall standardized alpha coefficient was used to measure the reliability or internal consistency of the tool, which became 0.86. The questionnaire comprises socio-demographic characteristics, professional and work-related characteristics, and questions assessing the healthcare provider’s knowledge of NASG and attitude toward its utilization.
Before the actual data collection, a pretest was done on 5% of the calculated sample size at Deneba hospital and appropriate corrections were made such as the logical order of some questions, and some words difficult to understand were revised. The two-day training was given on the overall data collection process and safety measures during the data collection. A total of 24 individuals have participated in the data collection and supervision process such as 13 Diploma, 6 BSc, and 4 MSc midwives. During data collection, the questionnaire was checked for completeness by the supervisors and the principal investigator.
Data processing and analysis
Data entry was carried out using EpiData version 4.6 and analyzed using SPSS version 25. Frequency tables and graphs were used to present descriptive and analytic statistics of participants. The multicollinearity assumption was checked and it was acceptable with a variance inflation factor of <10. The binary logistic regression (i.e., bivariable and multivariable) model was fitted to identify independent predictors, and variables having a value of p of less than 0.25 were included in the multivariable logistic regression analysis. In the multivariable logistic regression, a value of p of <0.05 with 95% CI for the AOR was used to determine the significant association of variables.
Ethical approval
The study was conducted under the Ethiopian Health Research Ethics Guideline and the declaration of Helsinki. Ethical clearance was obtained from the Institutional Ethical Review Board (IRB) of Debre Berhan University (protocol number: p014 and approval reference number: RCSCH 01/166/2013). A formal letter of administrative approval was gained from each selected hospital. Written informed consent was taken from each of the study participants after a clear explanation of the aim of the study and that participation was voluntary. Moreover, there are no individually detailed data, videos, or images.
Results
Socio-demographic characteristics
In this study, a total of 360 healthcare workers were involved, making a 96.5% response rate. The median age of the study participants was 28 years (ranging from 23 to 41). Of the study participants, 217 (60.3%) were within the age group of 25–29 years, 223 (61.9%) were male, and 326 (90.6%) were Amhara in ethnicity (Table 1).
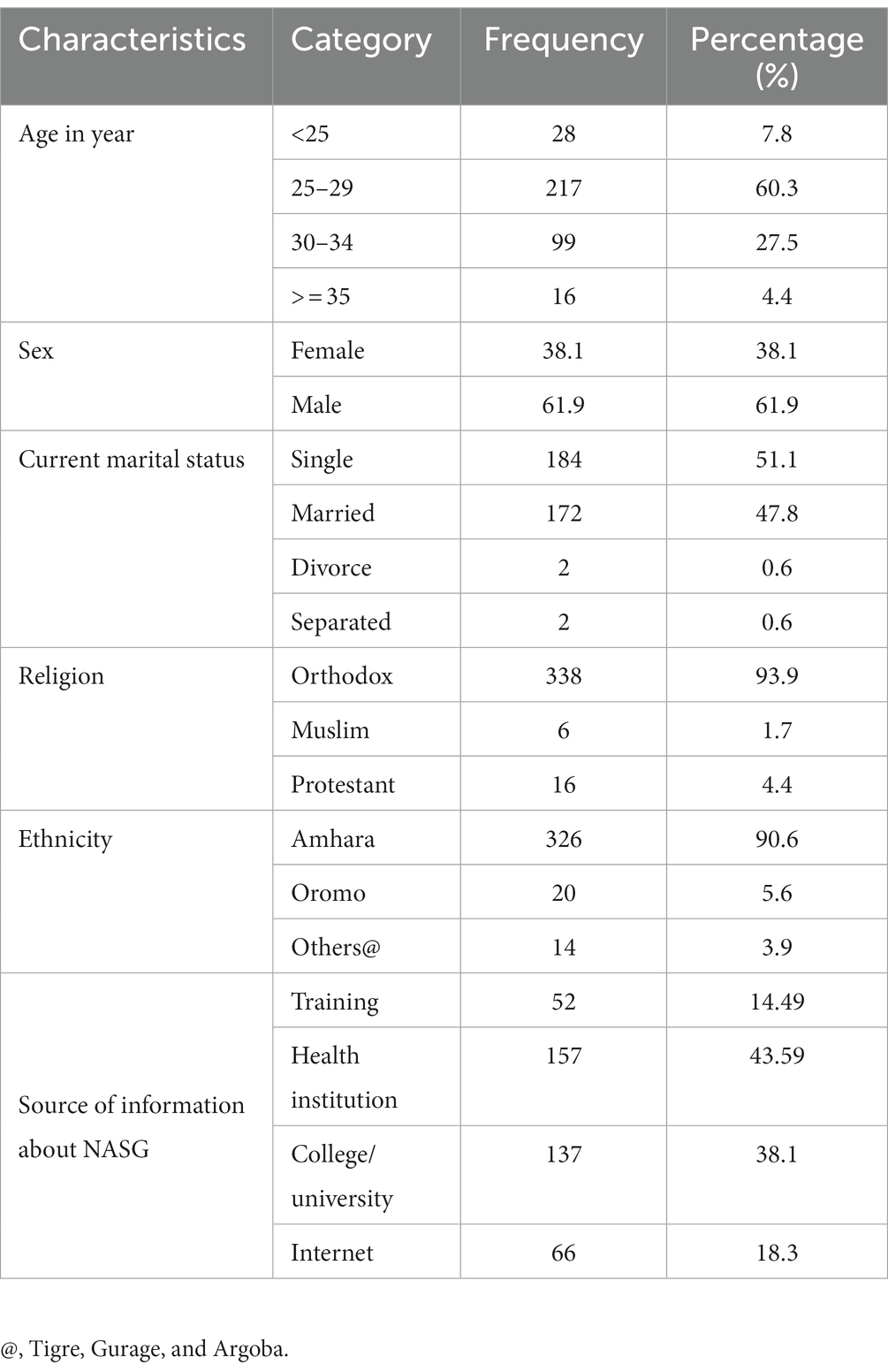
Table 1. Socio-demographic characteristics of study participants among healthcare providers in north Shew Shewa zone health facilities, 2021 (n = 360).
Workplace and profession-related characteristics
Among the participants, 290 (80.6%) were working from hospitals and 261 (72.5%) of them reported that they had working experience of 1–5 years. Three hundred and eight (85.6%) of HCPs did not receive training on NASG and 253 (70.3%) were Midwives by profession. Two third of the study participants (66.9%) had a bachelor’s degree (Table 2).
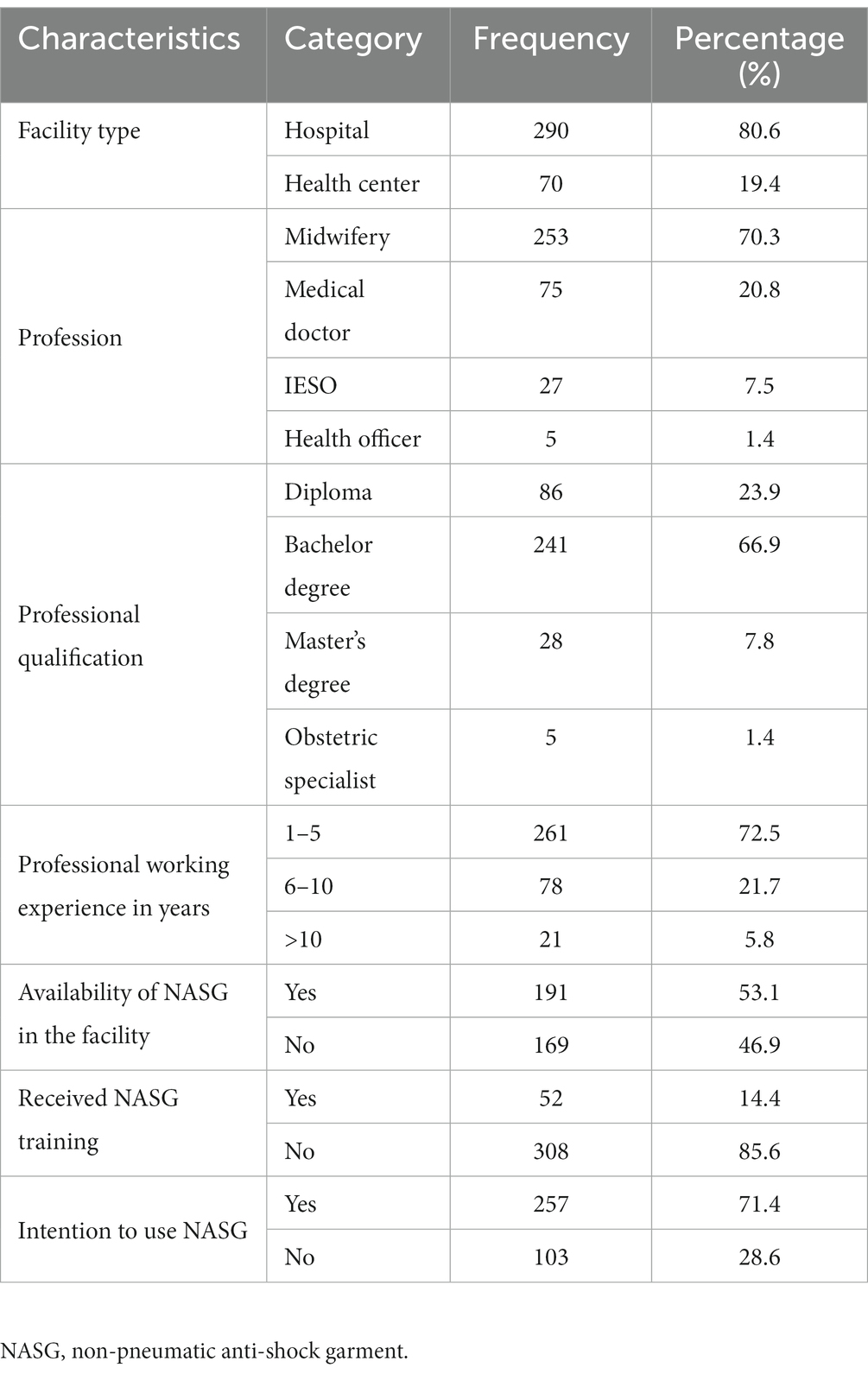
Table 2. Working place and profession-related characteristics among healthcare providers in north Shew Shewa zone health facilities, 2021 (n = 360).
HCPs’ knowledge of non-pneumatic anti-shock garment
In this study, 59.2% of respondents were knowledgeable about the NASG while 40.8% had poor knowledge of NASG.
Factors associated with the utilization of non-pneumatic anti-shock garment for obstetric hemorrhage management
Multivariable logistic regression analysis showed that HCPs who were; had the professional qualification of diploma and bachelor’s degree, received training on NASG, had availability of NASG in the health facility, and had a positive attitude toward utilization of NASG were found to be significantly associated with HCPs’ utilization of NASG.
HCPs with diploma and bachelor degree holders were 2.63 and 7.89 times more likely to be utilized NASG than senior obstetricians (AOR = 2.63; 95% CI: 1.39, 3.68) and (AOR = 7.89; 95% CI: 3.1, 16.29) respectively. Similarly, HCPs who received NASG training had 3.3 times more odds of the utilization of NASG than their counterparts (AOR = 3.3; 95% CI: 1.46, 7.48). Moreover, the odds of NASG utilization were 9.17 times higher among HCPs who were working in facilities where NASG is available as compared with their counterparts (AOR = 9.17; 95% CI: 5.10, 16.46). The likelihood of NASG utilization for OH was 1.63 times higher among HCPs who had a positive attitude compared with that of those who did not do so (AOR = 1.63; 95% CI: 1.14, 2.82) (Figure 2; Table 3).

Figure 2. Distribution of healthcare providers’ attitude toward non-pneumatic anti-shock garment utilization in north Shew zone health facilities, 2021.
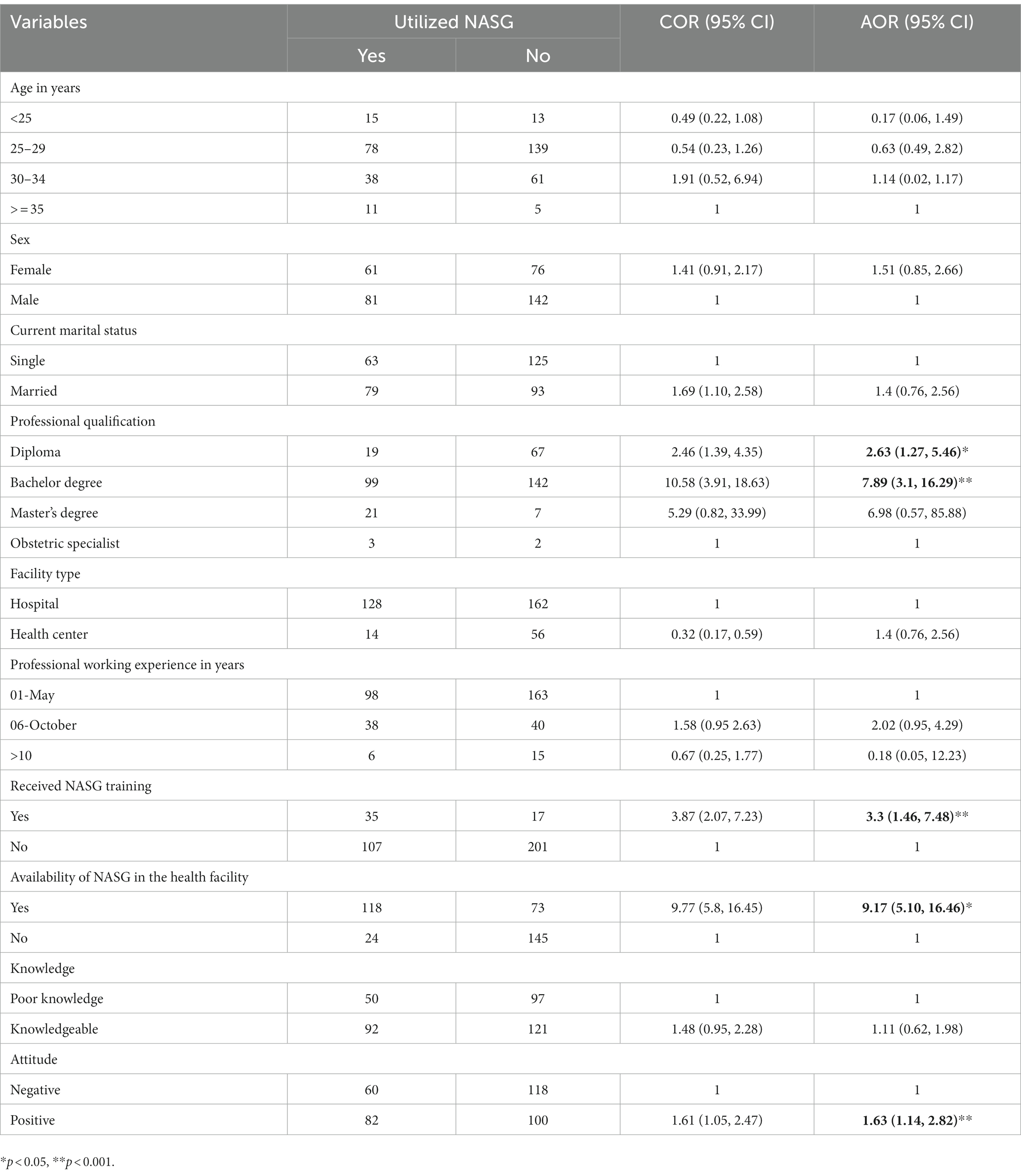
Table 3. Logistic regression analysis of factors associated with utilization of NASG for OH management among health care providers in North Shewa zone (n = 360).
Discussion
This study was conducted to assess the Utilization of Non-Pneumatic Anti-Shock Garment for the management of obstetric hemorrhage among healthcare providers in North Shewa, Ethiopia, 2021. Thus, this study revealed that the proportion of NASG utilization among healthcare providers was 39% with a 95% CI of (34–45). Besides, healthcare providers having professional qualifications of diploma and bachelor degree significantly associated factors with the utilization of NASG, who have received g training on NASG, availability of NASG in the facility, and having a positive attitude toward NASG were the variables significantly associated with the outcome variable.
The finding of this study is in line with the study conducted in Jimma zone, Ethiopia-36.2% (13) and Nigeria 35% (25). However, it is lower than the study from southern Ethiopia, 48.5% (26), Niger-46.4% (28), and Nigeria-73.7% (29). This could be due to variations in training and NASG availability and knowledge and attitude of healthcare providers. In this study, only 59.2% and nearly half (49.4%) of healthcare providers had adequate knowledge and unfavorable attitude, respectively. Besides, the unavailability of NASG in the health facility (46.9%) may contribute to the non-utilization and calls concerning bodies regarding the need for refresher training and availing the device in each health facility. In addition, the differences might be attributed to that the previous studies (26, 28, 29) were merely concerned with PPH management, but our study included the management of other obstetric hemorrhages.
This study indicated that HCPs who received training on NASG had 3.3 times more odds of the utilization of NASG than their counterparts. This may be because attending training can help healthcare providers to foster basic knowledge and skills on how to apply, and remove NASG and this can improve their utilization of non-pneumatic anti-shock garments. It was consistent with studies from the Jimma zone, Ethiopia (13), and southern Ethiopia (26) which showed that training could increase the likelihood of NASG utilization. Therefore, health professionals receiving NASG training are likely to have more knowledge and skills about the utilization of NASG for the management of OH, thereby adhering to the respective guidelines as compared to non-trained healthcare providers (13).
On the other hand, the likelihood of NASG utilization for OH was 1.63 times higher among HCPs who had a positive attitude compared with those who had a negative attitude. It was consistent with the study from Ethiopia (13). This might be explained by a positive attitude being one of the most important things that can lead to achieving the desired level of professional success. Similarly, this study revealed that the odds of NASG utilization were 9.17 times higher among HCPs who were working in facilities where NASG is available as compared with their counterparts. This might be due to the availability of NASG exposing the health care professionals to perform their acquired skills, as regular usage should make them familiar with it. This was also supplemented with the study from Jimma public hospitals (13). Besides, a study from Sokoto State Nigeria showed the non-availability of NASG plays on perceived hindrances to the utilization of this anti-shock garment (30).
Implication for practice
In this study findings, as gaps were found in the knowledge and attitude of HCPs on NASG, this calls for refresher training for HCPs on the usage of NASG. It is hoped that this will also improve the attitude of providers toward the equipment. In a bid to improve utilization of the low-cost technology equipment, a monitoring system is hereby recommended as this might help to improve utilization. Correspondingly, a large number of the respondents reported the non-availability of the NASG as a factor associated with non-usage, the hospital authority should ensure that all maternity units have access to the NASG. This result calls for stakeholders like the Ethiopian Midwife association (EMwA) and local health facilities to ensure the availability of NASG in health facilities and educational programs.
Strength and limitations
The authors would like to acknowledge some of the limitations of the current study. First, the cross-sectional nature of the study design might not be a guarantee to infer causality between utilization and the suggested explanatory variables. Finally, we did not get enough related articles to compare our results which makes our discussion shallow. Despite the above-mentioned limitations, this study sought to assess rarely addressed issues of OH and was able to provide important information to healthcare stakeholders.
Conclusion
In this study, almost two-fifths of healthcare providers used NASG for the management of obstetrics hemorrhage. Having professional qualifications of a diploma and bachelor’s degree, receiving training on NASG, its availability in the health facility, and a positive attitude toward utilization were positively associated factors with the utilization of NASG for OH management. The healthcare professionals who work in maternity units ought to get the training and handy equipment that may encourage the sustainable utilization of the garment.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Debre Berhan University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
BT had a major role in the conceptualization, data curation, develop the proposal, and data entry. All authors participate in the formal analysis and writing the original draft, equally participated in manuscript preparation and revision, and approved the manuscript to be considered for publication.
Acknowledgments
We appreciate and wish to thank Debre Berhan University for providing ethical clearance to carry out this study. We also would like to acknowledge the data collectors and study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1052885/full#supplementary-material
Abbreviations
NASG, Non-Pneumatic Anti-Shock Garment; HCP, Healthcare Provider; OH, Obstetric Hemorrhage; PPH, Postpartum Hemorrhage; WHO, World Health Organization.
References
1. Blencowe, H, Cousens, S, Jassir, FB, Say, L, Chou, D, Mathers, C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. (2016) 4:e98–e108. doi: 10.1016/S2214-109X(15)00275-2
2. Alkema, L, Chou, D, Hogan, D, Zhang, S, Moller, AB, Gemmill, A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. (2016) 387:462–74. doi: 10.1016/S0140-6736(15)00838-7
3. WHO, UNICEF UNFPA WBG and the U, dDivision NP. Maternal mortality: Levels and trends 2000 to 2017. UNFPA. (2019).
4. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Rockville: CSA and ICF (2016).
5. Miller, S, Turan, JM, Dau, K, Fathalla, M, Mourad, M, Sutherland, T, et al. Use of the non-pneumatic anti-shock garment (NASG) to reduce blood loss and time to recovery from shock for women with obstetric haemorrhage in Egypt. Glob Public Health. (2007) 2:110–24. doi: 10.1080/17441690601012536
6. Umar, AB, Ogwu, TN, and Chado, MA. Availability, and awareness of non-pneumatic antishock garment in tertiary hospitals of northern Nigeria. IOSR J Nurs Heal Sci. (2014) 3:46–58. doi: 10.9790/1959-03234658
7. Say, L, Chou, D, Gemmill, A, Tunçalp, Ö, Moller, AB, Daniels, J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. (2014) 2:e323–33. doi: 10.1016/S2214-109X(14)70227-X
8. Bonet, M, Oladapo, OT, Khan, DN, Matthews Mathai, A, and Gülmezoglu, M. New WHO guidance on prevention and treatment of maternal peripartum infections. Lancet Glob Health. (2015) 3:e667–8. doi: 10.1016/S2214-109X(15)00213-2
9. World Health Organization. Compendium of innovative health technologies for low-resource settings assistive devices EHealth solutions. Geneva: WHO (2014).
10. FIGO Safe Motherhood and Newborn Health (SMNH) Committee. Prevention and treatment of postpartum hemorrhage in low-resource settings. Int J Gynaecol Obstet. (2012) 117:108–18.
11. Seim, AR, Alassoum, Z, Lalonde, AB, and Souley, I. An integrating model for rapid reduction of maternal mortality due to primary postpartum haemorrhage - novel use of the catalyst approach to public health. Afr J Reprod Health. (2019) 23:18–26. doi: 10.29063/ajrh2019/v23i2.2
12. Turan, J, Ojengbede, O, Fathalla, M, Mourad-Youssif, M, Morhason-Bello, IO, Nsima, D, et al. Positive effects of the non-pneumatic anti-shock garment on delays in accessing care for postpartum. J Women’s Health. (2011) 20:91–8. doi: 10.1089/jwh.2010.2081
13. Bekele, G, Terefe, G, Sinaga, M, and Belina, S. Utilization of non-pneumatic anti-shock garment and associated factors for postpartum hemorrhage management among health care professionals’ in public hospitals of Jimma zone, south-west. Reprod Health. (2020) 17:1–10. doi: 10.1186/s12978-020-0891-6
14. Mbaruku, G, Therrien, MS, Tillya, R, Mbuyita, S, Mtema, Z, Kinyonge, I, et al. Implementation project of the non-pneumatic anti-shock garment and m-communication to enhance maternal health care in rural Tanzania. Reprod Health. (2018) 15:177. doi: 10.1186/s12978-018-0613-5
15. Pileggi-castro, C, Nogueira-pileggi, V, Tunçalp, Ö, Oladapo, OT, Vogel, JP, and Souza, JP. Non-pneumatic anti-shock garment for improving maternal survival following severe postpartum haemorrhage: a systematic review. Reprod Health. (2015) 12:28. doi: 10.1186/s12978-015-0012-0
16. Miller, S, and Belizán, JM. A promising device to save maternal lives associated with obstetric hemorrhage: the non-pneumatic anti-shock garment (NASG). Reprod Health. (2015) 12:19–21. doi: 10.1186/s12978-015-0019-6
17. Sutherland, T, Downing, J, Miller, S, Bishai, DM, Butrick, E, Fathalla, MMF, et al. Use of the non-pneumatic anti-shock garment (NASG) for life-threatening obstetric hemorrhage: a cost-effectiveness analysis in Egypt and Nigeria. PLoS One. (2013) 8:e62282. doi: 10.1371/journal.pone.0062282
18. FIGO Safe Motherhood and Newborn Health (SMNH) Committee. International journal of gynecology and obstetrics non-pneumatic anti-shock garment to stabilize women with hypovolemic shock secondary to obstetric hemorrhage ☆. Int J ofGynecology Obstet. (2015) 128:194–5. doi: 10.1016/j.ijgo.2014.10.014
19. Althabe, F, Therrien, MNS, Pingray, V, Hermida, J, Gülmezoglu, AM, Armbruster, D, et al. Postpartum hemorrhage care bundles to improve adherence to guidelines: a WHO technical consultation □. Int J Gynaecol Obstet. (2019) 148:290–9. doi: 10.1002/ijgo.13028
20. The World Health Organization, The Partnership for Maternal, Newborn & Child Health and the University of Washington. A global investment framework for women’s and children’s health: advocacy brochure. Geneva, Switzerland: WHO (2013).
21. Stenberg, K, Axelson, H, Sheehan, P, Anderson, I, Gülmezoglu, AM, Temmerman, M, et al. Study group for the global investment framework for women’s children’s health advancing social and economic development by investing in women’ s and children’ s health: a new global investment framework. Health Policy. (2013) 383:1333–54. doi: 10.1016/S0140-6736(13)62231-X
22. Downing, J, El Ayadi, A, Miller, S, Butrick, E, Mkumba, G, Magwali, T, et al. Cost-effectiveness of the non-pneumatic anti-shock garment (NASG): evidence from a cluster randomized controlled trial in Zambia and Zimbabwe. BMC Health Serv Res. (2015) 15:37. doi: 10.1186/s12913-015-0694-6
23. WHO recommendations on health promotion interventions for maternal and newborn health. Geneva: World Health Organization (World Health Organization, 2015).
24. Onasoga, OA, Duke, E, Danide, IU, and Jack-ide, IO. Midwives’ knowledge and utilization of non-pneumatic anti shock garment in reducing complication of postpartum haemorrhage in selected health care facilities in Bayelsa state Nigeria. Int J Reprod Contraception Obstet Gynecol. (2015) 4:977–81. doi: 10.18203/2320-1770.ijrcog20150410
25. Ajike, O, Adelani, TW, Oloyede, M, and Lawal, B. Midwives’ knowledge and utilization of anti-shock garment in prevention of postpartum haemorrhage shock at the university college hospital, Ibadan Nigeria. IOSR J Nurs Health Sci. (2014) 3:9–16. doi: 10.9790/1959-03140916
26. Gizachew, Y, Id, Y, Id, AB, and Aschalew, Z. Utilization of non-pneumatic anti-shock garment and associated factors for postpartum hemorrhage management among obstetric care providers in public health facilities of southern Ethiopia, 2020. PLoS One. (2021) 16:1–15. doi: 10.1371/journal.pone.0258784
27. Desta, AA, Berhane, M, and Woldearegay, TW. Utilization rate and factors associated with non-utilization of non-pneumatic anti-shock garment in the management of obstetric hemorrhage in public health care facilities of northern Ethiopia: a cross-sectional study. Int J Women’s Health. (2020) 12:943–51. doi: 10.2147/IJWH.S266534
28. Onasoga Olayinka, A, Duke, E, Danide, IU, and Jack-ide, IO. Midwives’ knowledge and utilization of non-pneumatic anti shock garment in reducing complication of postpartum haemorrhage in selected health care facilities in Bayelsa state Niger. Int J Reprod Contracept Obs Gynecol. (2015) 4:977–81. doi: 10.18203/2320-1770.ijrcog20150410
29. Oluwatosin, A, Lucia, YO, Teaching, AM, and History, M. Knowledge and utilisation of anti-shock garment among Midwives of Adeoyo maternity teaching hospital, Ibadan, Nigeria. African J Heal Nurs Midwifery. (2021) 4:26–37. doi: 10.52589/AJHNM-U47SAEMP
Keywords: healthcare provider, NASG, obstetrics hemorrhage, Ethiopia, women
Citation: Taye BT, Silesh Zerihun M, Moltot Kitaw T, Amogne FK, Kindie Behulu G, Lemma Demisse T, Chekole MS, Fitie GW, Worku SA, Kibiret DM, Ferede AA, Bejtual K, Desalegn T, Tiguh AE, Mihret MS and Kebede AA (2023) Utilization of non-pneumatic anti-shock garment for the management of obstetric hemorrhage among healthcare providers in north Shewa zone, Ethiopia. Front. Public Health. 11:1052885. doi: 10.3389/fpubh.2023.1052885
Edited by:
Shusen Sun, Western New England University, United StatesReviewed by:
Addisuu Bogale, Ethiopian Public Health Institute, EthiopiaSagni Girma Fage, Haramaya University, Ethiopia
Copyright © 2023 Taye, Silesh Zerihun, Moltot Kitaw, Amogne, Kindie Behulu, Lemma Demisse, Chekole, Fitie, Worku, Kibiret, Ferede, Bejtual, Desalegn, Tiguh, Mihret and Kebede. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Birhan Tsegaw Taye, dHNlZ2F3YmlyaGFuMkBnbWFpbC5jb20=
 Birhan Tsegaw Taye
Birhan Tsegaw Taye Mulualem Silesh Zerihun
Mulualem Silesh Zerihun Tebabere Moltot Kitaw
Tebabere Moltot Kitaw Fetene Kasahun Amogne
Fetene Kasahun Amogne Geremew Kindie Behulu1
Geremew Kindie Behulu1 Tesfanesh Lemma Demisse
Tesfanesh Lemma Demisse Moges Sisay Chekole
Moges Sisay Chekole Girma Wogie Fitie
Girma Wogie Fitie Solomon Adanew Worku
Solomon Adanew Worku Addisu Andualem Ferede
Addisu Andualem Ferede Agumas Eskezia Tiguh
Agumas Eskezia Tiguh Muhabaw Shumye Mihret
Muhabaw Shumye Mihret Azmeraw Ambachew Kebede
Azmeraw Ambachew Kebede