- School of Nursing, Hong Kong Polytechnic University, Hong Kong, Hong Kong SAR, China
Introduction: Alcohol use disorder is a medical condition characterized by an impaired ability to control or stop alcohol use despite adverse health outcomes. Despite several studies that have analyzed the prevalence and determinants, their results have been equivocal, and the reasons for the differences in prevalence rates and determinants of AUD across nationalities are unknown. Hence, this study estimated the pooled prevalence of alcohol use disorder and its determinant among adults in East Asian countries.
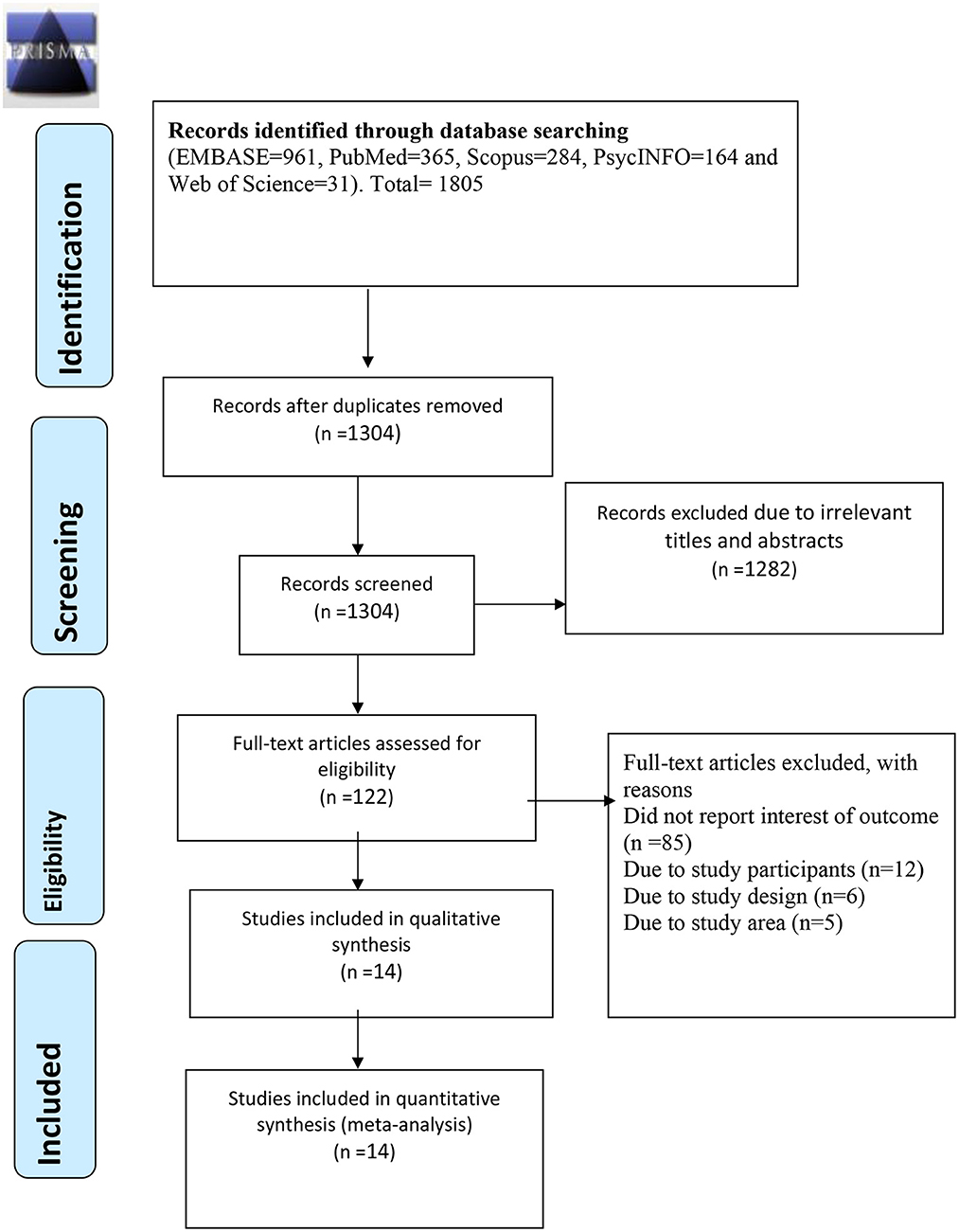
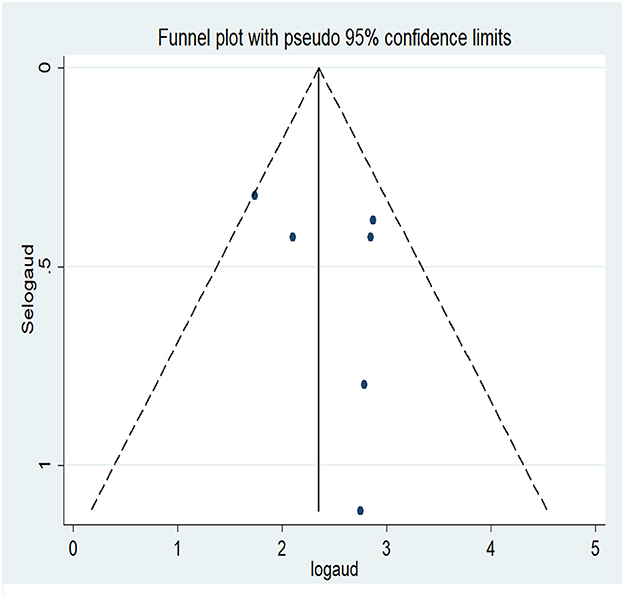
Methods: Articles were searched from PubMed, Web of Science, EMBASE, PsycINFO, and Scopus. All observational study designs that fulfilled the predefined criteria were included in the study. The findings were reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). The quality and heterogeneity of articles were assessed using the new castle-Ottawa scale (NOS) and I2, respectively. Additionally, publication bias was checked through funnel plot and Egger's regression test.
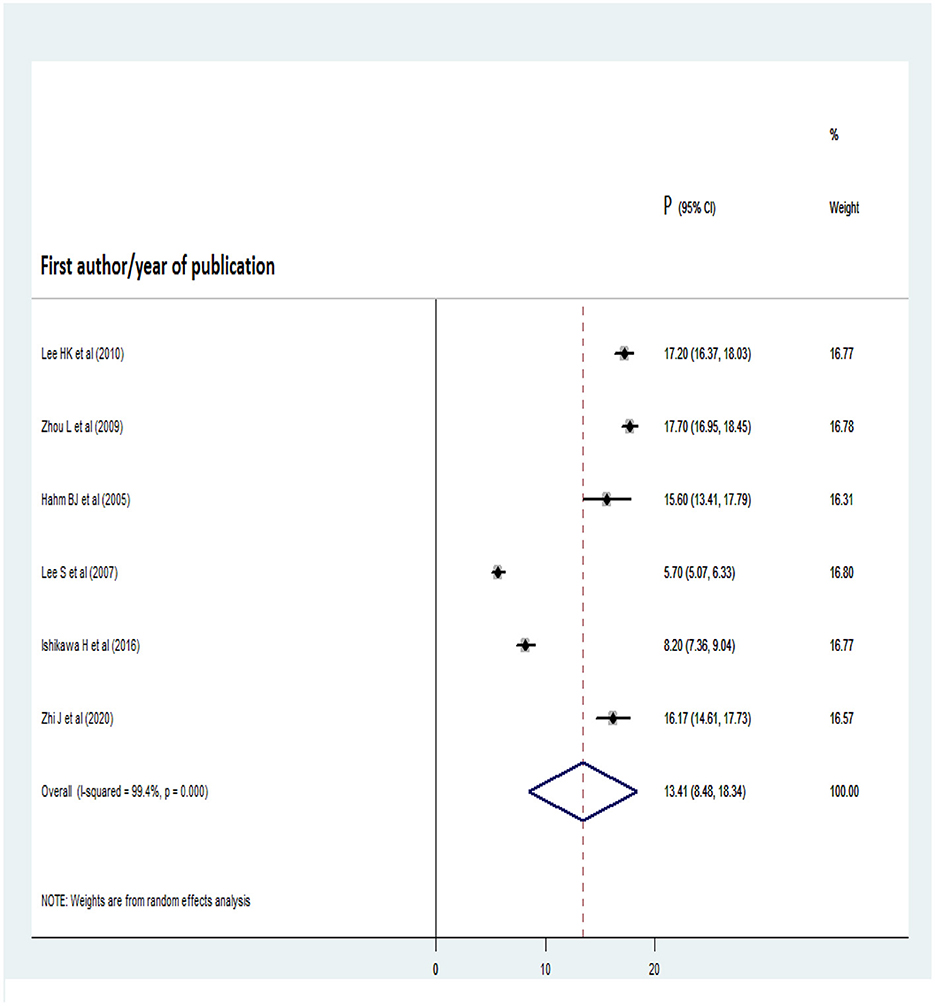
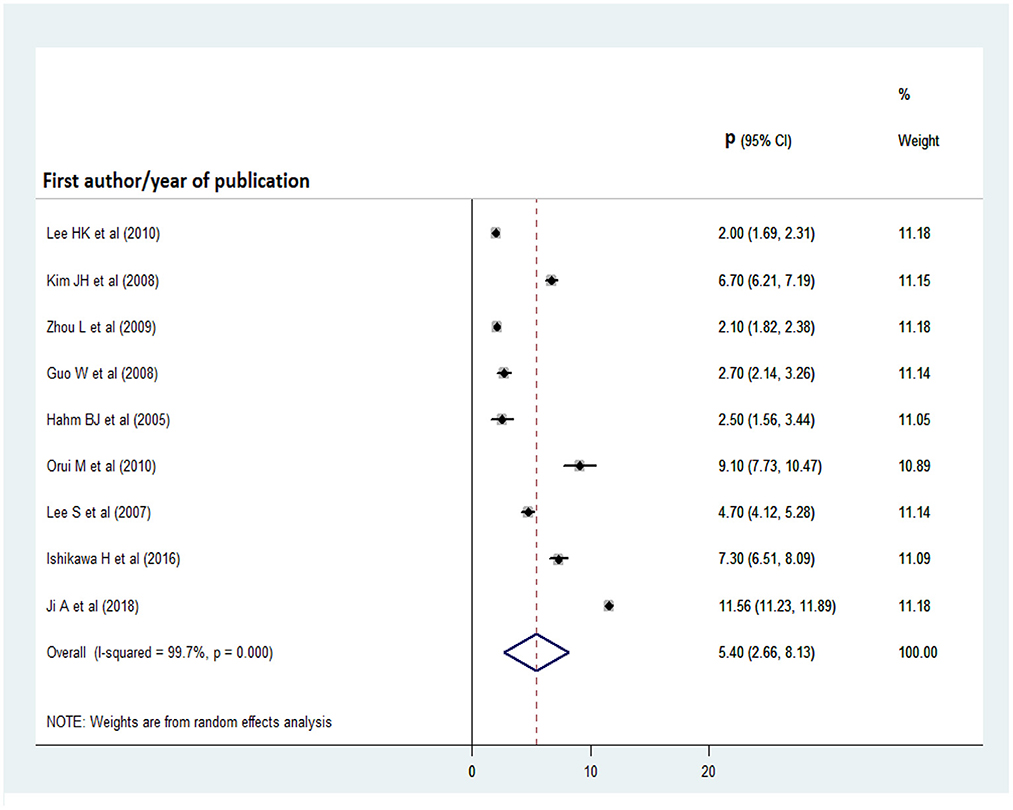
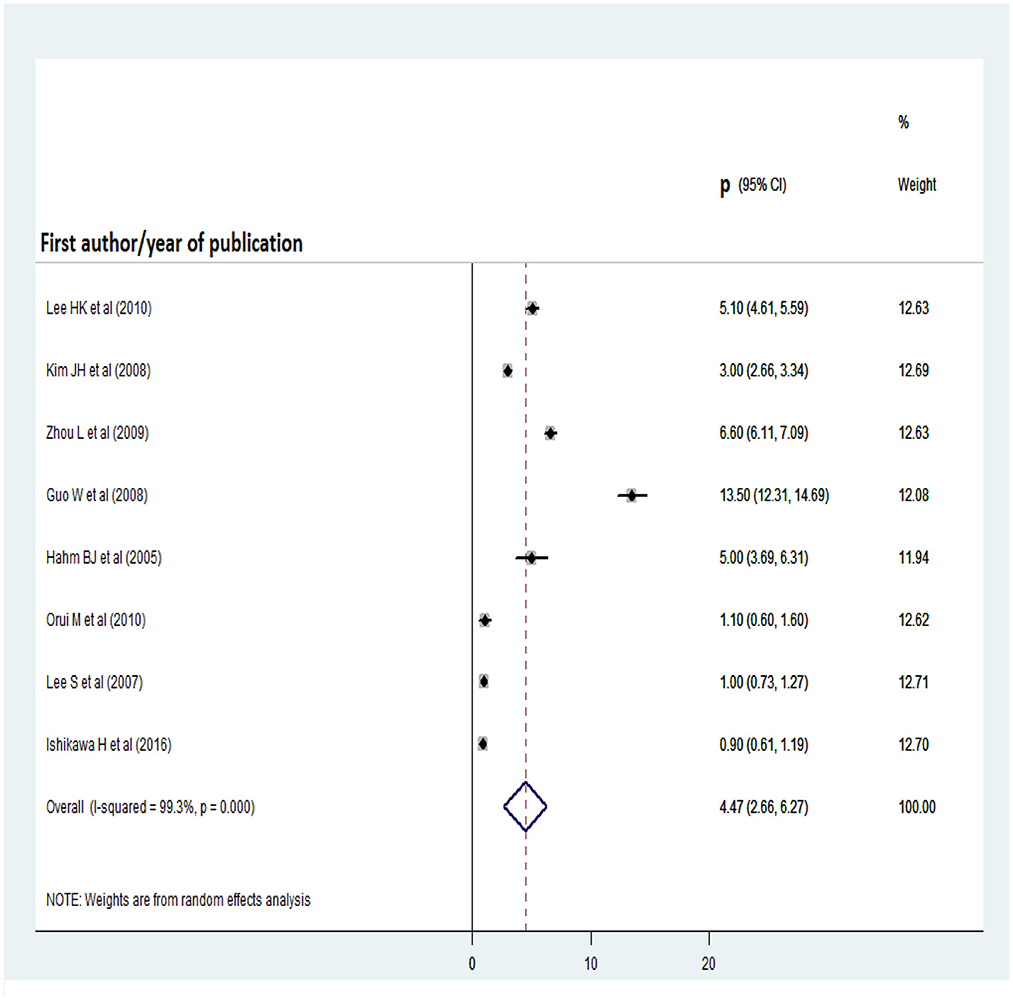
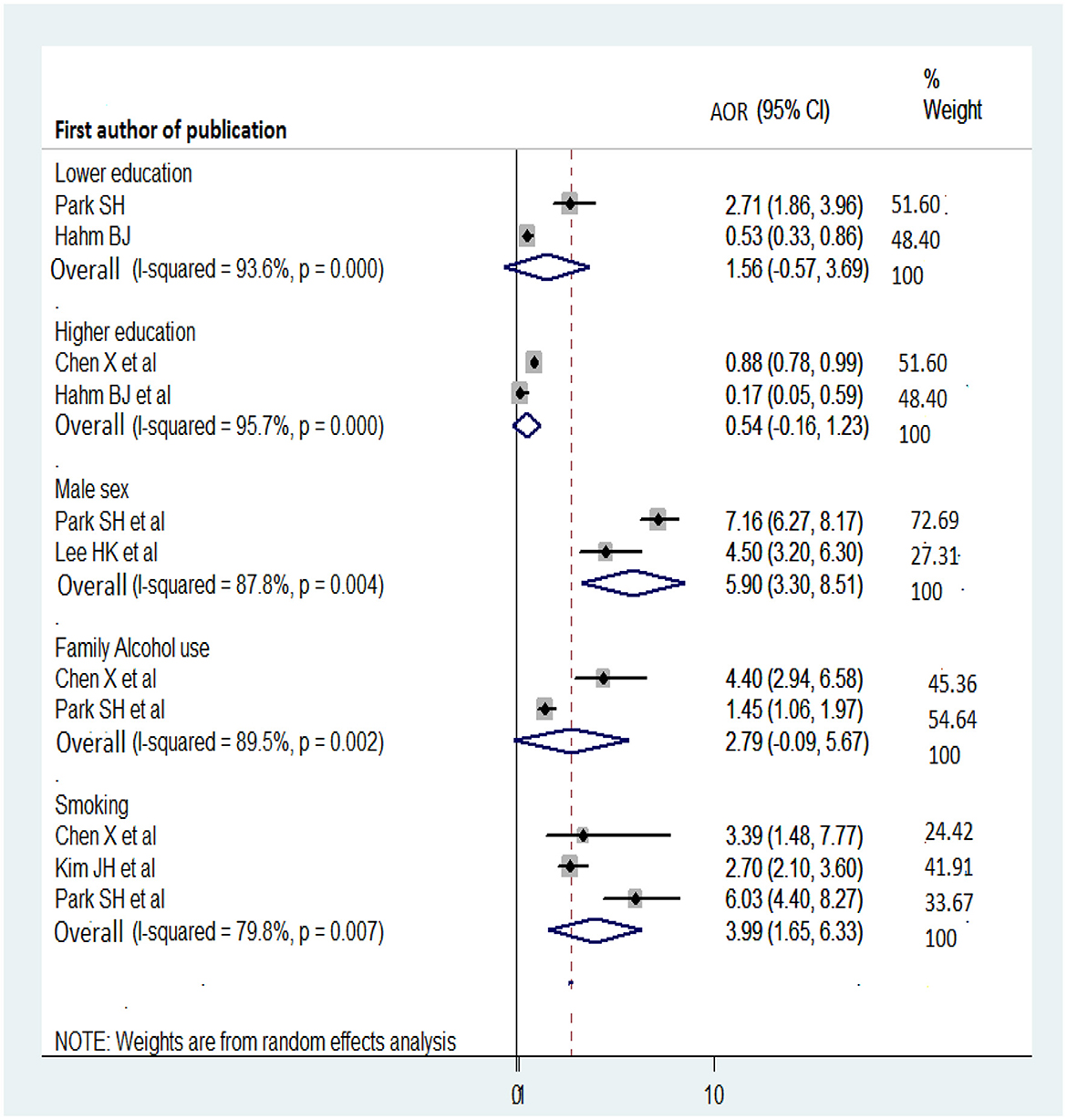
Results: A total of 14 articles with 93, 161 study participants were considered in the study. Of which 9 studies were included in the meta-analysis of the 1-year prevalence of alcohol use disorder, 6 in the lifetime, 9 in alcohol abuse, and 8 in alcohol dependency. Consequently, the overall pooled prevalence of one-year alcohol use disorder was 8.88% (95% CI: 6.32, 11.44), lifetime 13.41% (95%CI: 8.48, 18.34), alcohol abuse 5.4% (95% CI: 2.66, 8.13), and alcohol dependency 4.47% (95% CI: 2.66, 6.27). In the subgroup analysis by country, the highest 1-year and lifetime pooled prevalence of alcohol use disorder was observed in Korea at 9.78% (95% CI:4.40, 15.15) and 16.73% (95% CI: 15.31, 18.16), respectively. Besides, smoking (OR: 3.99; 95% CI: 1.65, 6.33) and male gender (OR: 5.9; 95% CI: 3.3, 8.51) were significant determinants of alcohol use disorder.
Conclusions: The magnitude of alcohol use disorder was high among adults in East Asian countries. Smoking and male gender were the key determinants of alcohol use disorders.
Introduction
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to control or stop alcohol use despite adverse health outcomes (1). According to the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Disease (ICD), AUD is defined as continued alcohol use despite negative biological, psychological, behavioral, and social consequences within the last 12 months. In the DSM-4, alcohol abuse and alcohol dependence were defined separately, while DSM-5 integrates these two disorders into a single disorder called AUD (1).
According to a national survey on drug use and health, about 71.4% American people aged >18 years were struggling with alcohol use, while 10.2% of American people aged ≥12 years had AUD (2). In Asia, about 4.9 million (37.2%) people aged ≥26 years were alcohol users in 2020, of whom 993,000 (7.5%) had AUD. Approximately 32.2% (656,000) of young adults (aged 18–25 years) were using alcohol, and 9% of them (184,000) had developed AUD (3). In recent years, the proportion of heavy and binge drinkers among the adult populations of many Asia-pacific countries and territories has increased and is now seen in approximately one in every two men and one in every five women (4). Hence, AUD is a major health problem in Asia (5).
According to a 2022 report from the World Health Organization (WHO), approximately 200 health conditions and injuries are associated with the harmful use of alcohol, including road injuries, violence, suicide attempts, and medical problems such as liver disease, cardiovascular disease, cancer, tuberculosis, and HIV/AIDS (6). The mortality attributable to alcohol consumption was much higher than that related to tuberculosis, HIV/AIDS, and diabetes (7). Globally, approximately 3 million deaths result from the harmful use of alcohol per year. For instance, in 2016, approximately 2.3 and 0.7 million men and women died due to AUD, respectively (7). In particular, an estimated 106.5 and 26.1 million Disability-adjusted life years (DALYs) in men and women were attributed to alcohol use, respectively (8). Generally, AUD results in diminished brain function, stomach complications, liver and kidney failure, and then finally leads to death (9). Besides, high-risk drinking causes societal-related health problems such as the breakdown of social relationships, domestic violence, compromised family care, mental health problems (e.g., depression, anxiety, and related forms of substance misuse), unsafe sex, financial problems, and homelessness (10).
The development of AUD is associated with multiple societal factors, including the availability of alcohol (11), level of economic development (12), and culture (12), as well as with individual factors like age (13, 14), gender (13–15), family history of alcohol use and smoking status (14, 15).
To tackle AUD, the WHO proposed a global strategy for reducing alcohol consumption that has been a public health priority since 2010. Pharmacological and psychosocial management approaches (e.g., brief interventions, cognitive behavioral therapy, acceptance and commitment therapy, and 12-step programs) have been used for treating AUD (16). However, AUD remains a major issue among the adult populations of East Asian countries.
Several studies have analyzed the prevalence and determinants of AUD in East Asian countries, but their results have been equivocal. In addition, the reasons for the differences in prevalence rates and determinants of AUD across nationalities are unknown. Therefore, a systematic review and meta-analysis is required.
The current study aimed to estimate the prevalence of AUD, and to identify its determinants, through the analysis of a large sample of participants. Large-pooled samples provide more precise estimates than individual studies. This study provides timely and comprehensive data for governments and policymakers and could inform the design of new prevention and treatment strategies for people with AUD in East Asian countries.
Methods
Searching strategies and data sources
The study protocol was registered in the International Prospective Register of Systematic Reviews and Meta-Analysis (PROSPERO; registration number: CRD42022361994). The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines were followed when reporting the results of this study (17) (Supplementary material 1). All potentially relevant articles were retrieved systematically from electronic databases including PubMed, EMBASE, Web of Science, PsycINFO, and Scopus. The search was limited to studies conducted in East Asian countries. The identified articles were exported into citation management software (EndNote version 20; Clarivate, London, UK) for further screening and assessment. The databases were searched using the following terms: “Alcohol abuse” OR “Alcohol depend*” OR “Alcohol use disord*” OR “Alcohol consumption” OR “Alcohol addiction” OR “alcohol intoxication” AND “prevalence” OR “incidence” OR “proportion” OR “magnitude” OR “burden” AND “determinants” OR “reasons” OR “factors” OR “associated factors” OR “risk factors” OR “facto*” OR “predictors” AND “Adults” OR “young adults” OR “adulthood” OR “adolescents” OR “young adult populations” AND “China” OR “Hong Kong” OR “Japan” OR “Taiwan” OR “South Korea” OR “North Korea” OR “Macau” OR “Mongolia.” Searches were conducted from September 10 to October 5, 2022.
Inclusion and exclusion criteria
Articles were selected and screened on the basis of predefined eligibility criteria. All observational studies, including but not limited to case-control, cross-sectional, and cohort studies, reporting the prevalence and/or magnitude of AUD and/or its determinants among adults in East Asian countries were included in this review. The search was limited to articles published in English since 2005. Systematic reviews, editorials, trials, qualitative studies, and conference papers were excluded, as were articles without full text (established through communication with the primary authors of the articles). We also excluded studies of adults with psychiatric or other health problems. This was because mental health issues increase the severity of AUD (18–20), and people with medical conditions are less likely to use alcohol because it exacerbates symptoms and is often contraindicated (21).
Outcome measures
The outcome measures of the current study included the prevalence of AUD and its determinants. In the DSM-IV and DSM-5, AUD is defined as the presence of at least 2 of the following 11 behaviors/symptoms: (I) had times when you ended up drinking more, or for longer, than you intended; (II) wanted to cut down or stop drinking more than once, but could not; (III) spent considerable time drinking, being sick or getting over other aftereffects of drinking; (IV) wanted to drink so badly that you could not think of anything else; (V) being sick from drinking often interfered with taking care of your family or home, or caused problems at school; (VI) continued to drink even though it caused trouble with your family or friends; (VII) gave up or cut back on activities that were important or interesting to you, or put pressure on you to drink; (VIII) entered into situations more than once, while or after drinking, which increased your chances of getting hurt; (IX) continued to drink even though it was making you feel depressed or anxious; (X) had to drink much more than you once did to achieve the effect that you wanted or found that your usual number of drinks had much less effect than before; or (XI) found that, when the effects of alcohol were wearing off, you had withdrawal systems like trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart or seizure (1).
In the DSM-5, AUD encompasses alcohol abuse and dependence. Alcohol abuse is defined as the continuation of drinking despite recurrent social, interpersonal, health and legal problems caused by alcohol use (22), or by the presence of at least one of the following symptoms: (I) sickness caused by drinking often interfered with taking care of your home or family; (II) entered into a situation more than once, during or after drinking, which increased your chances of getting hurt (e.g., swimming, driving, unsafe sex, or walking in a dangerous area); (III) arrested or held at the police station more than once, or experienced other legal problems, because of drinking; or (IV) continued drinking despite it causing trouble with your family or friends (1).
Alcohol dependence refers to the need for repeated consumption of alcohol or impaired control over drinking (23). According to the DSM-IV, the presence of three of the following symptoms indicates alcohol dependence: (I) spend a lot of time drinking; (II) wanted to cut down or stop drinking more than once but could not; (III) had to drink more than you once did to achieve the effect that you want; (IV) experience withdrawal symptoms; (V) had times when you ended up drinking more, or for longer, than you intended; or (IV) continued drinking despite it making you feel depressed or anxious (1).
Study screening and selection
All articles retrieved from the electronic databases were imported into EndNote, and duplicates were identified and removed. Then, five authors (GMB, KYH, KKWL, CSTW, and QL) screened and reviewed the titles and abstracts of each article. Disagreements were resolved through discussion and repeating the review process if necessary. Finally, the authors reviewed the full texts of the articles selected on the basis of their titles and abstracts.
Data extraction
Data extraction was done using Microsoft Excel (Microsoft Corp., Redmond, WAQ, USA) following the guidelines of Joanna Briggs Institute. The following information was systematically reviewed and extracted by two authors (GMB and KYH): first author, year of publication, country, study area, study population, study design, sample size, prevalence of alcohol abuse, alcohol dependence, and AUD (one year and lifetime), and adjusted odds ratios (AORs) of factors significantly associated with AUD (with 95% confidence intervals [CIs]). Discrepancies were resolved by repeating the data extraction procedure, as well as through discussion with a senior member of the research team (YWM). If additional information was needed, the primary author of the articles was contacted by email.
Quality appraisal
The Newcastle-Ottawa Scale (NOS) risk of bias tool was used for assessing cross-sectional, case-control, and cohort studies (24, 25). The NOS has three components (selection, comparability, and outcome/exposure) and has been validated for application to cross-sectional (rated from 0–10 stars), cohort and case-control studies (rated from 0–9 stars). For the selection component, star ratings of 0–5 are provided for cross-sectional studies, and 0–4 for case-control and cohort studies. For the comparability and outcome/exposure components, star ratings of 0–2 are provided, while study designs are rated as 0–3. Articles with 3 or 4 stars for the selection component, 1 or 2 stars for the comparability component, and 2 or 3 stars for the outcome/exposure component were categorized as “good quality.” Articles receiving 2 stars for the selection component, 1 or 2 stars for the comparability component, and 2 or 3 stars for the outcome/exposure component were classified as “fair quality.” Articles having 0 or 1 star for the selection component, 0 stars for the comparability component, or 0 or 1 star for the outcome/exposure component were classified as “poor quality” (26). The quality of the included studies was systematically and independently appraised by the authors (GMB and KYH) of this study. Disagreements among the two authors were resolved by repeating the quality appraisal procedure, and through discussion with a senior research team member (YWM).
Data synthesis
A narrative description approach was used to present the results of articles that did not report the outcomes of interest. All other articles were included in the meta-analysis, and STATA software (version 14; Stata Corp., College Station, TX, USA) was employed to calculate the overall prevalence rates of AUD, alcohol abuse and alcohol dependency. Pooled ORs were calculated for the determinants of the outcomes of interest. To minimize heterogeneity, a random effects model was employed (27). P-values < 0.05 were considered statistically significant.
Publication bias and heterogeneity
Heterogeneity among the included studies was assessed by visual inspection of the funnel plot and Egger's regression test. Heterogeneity was considered low, moderate, and high when the I2 values were <25%, 25–75%, and >75%, respectively (28).
Results
Search results
A total of 1,805 articles were retrieved (EMBASE, p = 961; PubMed, p = 365; Scopus, p = 284; PsycINFO, p = 164; Web of Science, p = 31; Figure 1). After removing 501 duplicate articles, the titles, and abstracts of 1,304 articles were screened. In total, 1,282 articles were excluded because their titles and abstracts indicate that they were not relevant to this study. The remaining 122 articles were downloaded, and full-text review was conducted by the two reviewers (GMB and KYH). A further 107 articles were then excluded for various reasons, including failure to report the outcomes of interest (p = 85), and unsuitable study populations (p = 12), study designs (p = 6), and study areas (p = 5). Of the excluded articles, one article (29) was not considered in the study as it was done through a meta-analysis which did not meet our inclusion criteria of observational studies. And, the other one (30) did not report the 1-year and lifetime prevalence of AUD, but rather reported the co-occurrence of mental disorders and AUD in past 30 days. As per our inclusion criteria, we excluded studies of adults with psychiatric or other mental health problems. Therefore, 14 peer-reviewed articles (31–44) were included in this systematic review and meta-analysis; 9 of them were suitable for analysis of the 1-year prevalence of AUD, 6 for analysis of the lifetime prevalence of AUD, 9 for analysis of the prevalence of alcohol abuse, and 8 for analysis of the prevalence of alcohol dependence.
Characteristics of the included studies
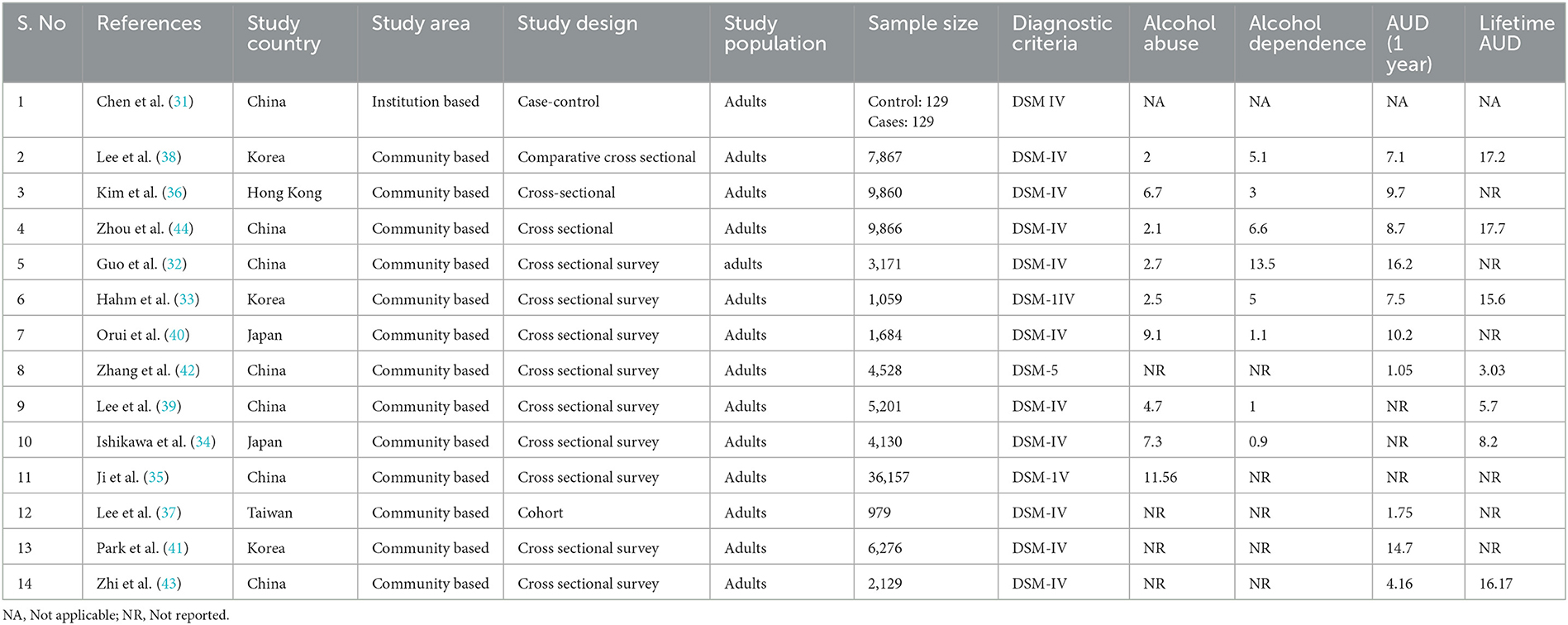
The 14 articles in this systematic review and meta-analysis included 93,161 participants (Table 1). The sample size of the included studies ranged from 258 to 36,157 participants, and they were published from 2005 to 2021. Most of the studies (32–36, 38–44) were cross-sectional, although there was one case-control (31), one cohort (37), and one comparative cross-sectional study (38). Most of the included studies were from China (31, 32, 35, 39, 42–44), followed by Korea (33, 38, 41), Japan (34, 40), Taiwan (37), and Hong Kong (36). The highest and lowest prevalence rates of AUD were reported in China, at 16.2% (32) and 1.05%, respectively (42). The highest and lowest lifetime prevalence rates of AUD were also reported in China, at 17.7 and 3.03%, respectively (42, 44).
Quality appraisal
The NOS was used to assess the quality of the included studies. The quality ratings ranged from 6 to 8 stars for cross-sectional studies (32–36, 38–44), seven for case-control studies (31) and six for cohort studies (37). The most common problems were an unsatisfactory response rate, failure to compare respondents and non-respondents (38, 41), and a lack of CIs for the determinants of AUD (32, 37).
Narrative description
Five studies (31, 34, 35, 39, 42) were not considered in the analysis of the 1-year prevalence of AUD: four of them (31, 34, 35, 39) did not report the prevalence rate, while the remaining study, which was conducted in China (42), reported it on the basis of the DSM-5 (which has different diagnostic criteria to the DSM-IV).
Eight articles (31, 32, 35–37, 40–42) were not included in the analysis of lifetime prevalence of AUD because they did not report that outcome. Four of those studies were conducted in China, including one case-control study (31) and three cross-sectional studies (32, 35, 42); the remaining four studies were from Korea (41), Hong Kong (36), Taiwan (37), and Japan (40).
Nine articles (32, 34, 35, 37, 39, 40, 42–44) were excluded from the analysis of determinants of AUD: six of them did not report these data (34, 35, 39, 40, 42, 43) and two did not provide 95% CIs allowing computation of the standard error of the log odds ratio (32, 37). A further study reported that unmarried marital status was a significant factor for AUD; however, because no other studies reported on marital status, this study was not included in the analysis (44). Therefore, five articles were included in the analysis of determinants of AUD, one of which was a case-control study conducted in China involving 129 controls and 129 cases; that study reported that history of family alcohol use (aOR: 4.4; 95% CI: 2.94, 658), smoking (aOR: 3.39; 95% CI: 1.48, 7.77), higher education level (aOR: 0.88; 95% CI: 0.78, 0.99), and induced drinking during childhood (aOR: 6.09; 95% CI:2.56, 14.51) were determinants of AUD (31).
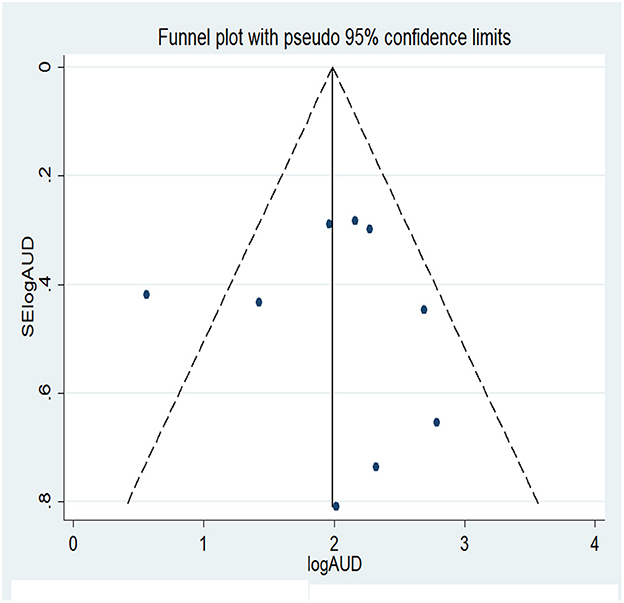
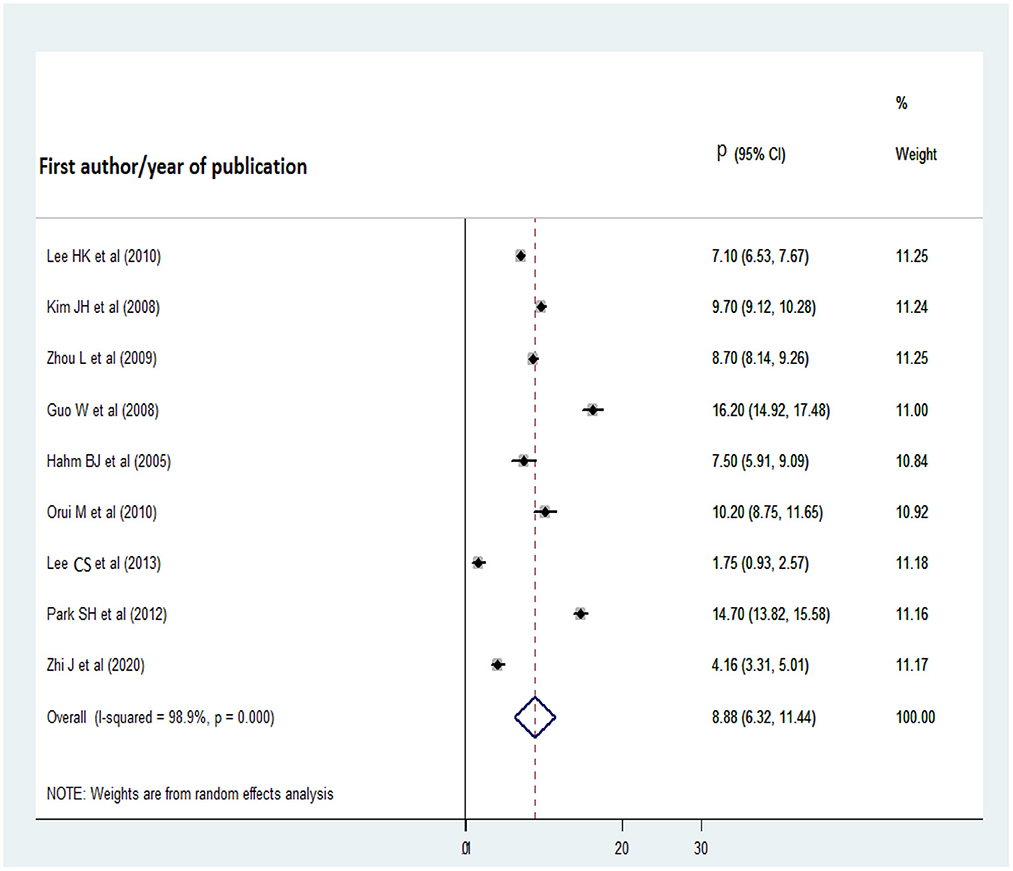
One-year pooled prevalence of AUD
Nine studies were included in the analysis of the 1-year pooled prevalence of AUD. Before computing the pooled prevalence, publication bias was assessed with a funnel plot and Egger's regression test. Visual inspection of the funnel plot revealed a symmetrical distribution of the studies and the Egger's regression test statistic was non-significant (t = 0.04, p = 0.970); therefore, there was no significant publication bias (Figure 2). On the basis of the aforementioned results, nine studies were included in the analysis of the 1-year pooled prevalence of AUD, published from 2008 to 2020. The highest and lowest prevalence rates of AUD were reported in studies from China (16.2%) and Taiwan (1.75%), respectively, and the 1-year pooled prevalence of AUD disorder was 8.88% (95% CI: 6.32, 11.44) (Figure 3).
A subgroup analysis was conducted for Korea and China because at least two studies conducted in these countries reported the 1-year pooled prevalence of AUD disorder (Korea, 9.78%; 95% CI: 4.40, 15.15; China, 9.66%; 95% CI: 4.31, 15.01).
Pooled lifetime prevalence of AUD
The lifetime pooled prevalence of AUD was estimated on the basis of six studies from Korea, China, Hong Kong, and Japan (total of 30,252 participants). Prior to the analysis, publication bias was assessed with a funnel plot and Egger's regression test. The symmetrical distribution of the articles in the funnel plot indicated that there was no publication bias (Figure 4), as did the non-significant Egger's regression test statistic (t = 0.88, p = 0.427). The overall pooled lifetime prevalence of AUD was 13.41% (95% CI: 8.48, 18.34) (Figure 5). In a subgroup analysis by country, the pooled lifetime prevalence was highest for Korea, at 16.73% (95% CI: 15.31, 18.16), followed by China (13.18%; 95% CI: 4.34, 22.02).
Pooled prevalence of alcohol abuse and dependence
As shown in Figures 6, 7, nine and eight articles were included in the analyses of alcohol abuse and dependence, respectively. Before the analyses, publication bias among studies was checked for by inspecting their distribution on the funnel plot and performing Egger's regression test. There was no significant publication bias among the studies of alcohol abuse or dependence, as evidenced by the Egger's regression test statistics (t = −2.17, p = 0.067 and t = 1.96, p = 0.098, respectively). The prevalence rate of alcohol abuse was highest in China (11.56%) and lowest in Korea (2%), while that of alcohol dependence was highest in China (13.5%) and lowest in Japan (0.9%). The overall pooled prevalence of alcohol abuse was 5.4% (95% CI: 2.66, 8.13), while that of alcohol dependence was 4.47% (95% CI: 2.66, 6.27).
Determinants of AUD
Among the studies included in the analysis of determinants of AUD, statistically significant factors included male gender (38, 41), history of family alcohol use (31, 41), smoking (31, 36, 41), binge drinking (36), education level (31, 33, 36, 38, 41, 44), income (38, 44), and unmarried status (41).
Studies conducted in China (31), Korea (41), and Hong Kong (36) revealed a positive relationship between smoking and AUD (overall OR: 3.99; 95% CI: 1.65, 6.33). History of family alcohol use was a determinant of AUD in a Chinese study (AOR: 4.4; 95% CI: 2.94, 658), as well as a Korean one (AOR: 1.45; 95% CI: 1.06, 1.97), although this factor was not significantly associated with AUD when all studies were considered (overall OR: 2.79; 95% CI: −0.09, 5.67). Sex was also identified as a determinant of AUD. Male gender was statistically significantly associated with AUD (overall OR: 5.9; 95% CI: 3.3, 8.51). Regarding education level, the results were inconsistent (31, 33, 38, 41); while some studies indicated that a higher education level was a protective factor for AUD (31, 33), others found that a lower education level was a protective factor (33). In the analysis of all studies, the overall odds ratios for lower and higher education levels were 1.68 (95% CI: 0.25, 3.12) and 0.54 (95% CI: −0.16, 1.23), respectively (Figure 8).
Discussion
Although various management strategies are emerging, AUD remains a major problem in East Asian countries. However, the reported prevalence and determinants of AUD vary among countries. Therefore, this systematic review and meta-analysis aimed to determine the pooled prevalence of AUD among the adult populations of East Asian countries and calculated pooled odds ratios for its determinants. The pooled 1-year prevalence of AUD was high, at 8.88% (95% CI: 6.32, 11.44), as was the lifetime prevalence, at 13.41% (95% CI: 8.48, 18.34) the rates of alcohol abuse and alcohol dependence were 5.4% (95% CI: 2.66, 8.13) and 4.47% (95% CI: 2.66, 6.27), respectively.
The pooled prevalence of AUD in this study was generally lower than that reported in American at 12% (45), Australia at 18% (46), Canada 19%, and in Brazil at 18.5% (14).
The difference in prevalence of AUD between East Asian and Western countries could be explained by cultural norms and beliefs. In Mediterranean countries, alcohol is integrated into daily life and activities (wet drinking culture) (47). This accords with the results of a comparative study showing that, in cultural terms, Western countries value wine more so than China (48). Second, most young adults in Western countries consider binge drinking normal (49), and some even rely on drinking to cope with stress in their daily lives (50). Such norms and beliefs may explain the high frequency and amount of alcohol consumption in Western countries (51), which would likely lead to a higher prevalence of AUD. In 2020, the alcohol use rate among Asian people aged ≥26 years was only 37.5% (52), which was much lower than the rate reported in the US (54.6%) (2).
The pooled prevalence rates of lifetime and 1-year AUD in the current study were higher than those reported for West Asian countries, including Israel (5.9%), Iraq (0.4%) (53), Lebanon (8.7%) (54), the United Arab Emirates (0.7%) (55), Jordan (0.4%) (56), and Bahrain (1.6%) (57). These differences could be explained by religious norms. In West Asian countries, Islam, which restricts alcohol use for its adherents, is the dominant religion (58–60). Moreover, while our results were derived from a meta-analysis of studies on the prevalence of AUD, studies from West Asian countries reported data for individual countries provided by the WHO. Furthermore, the prevalence variation could be attributed by difference in methodology and data collection tools used, as questionnaires adapted according to each country's culture, norms, language, and definitions may also vary (61, 62).
We performed a subgroup analysis to explore AUD by country. The highest pooled prevalence rates for 1-year and lifetime AUD were observed in Korea, at 9.78% (95% CI: 4.40, 15.15) and 16.73% (95% CI: 15.31, 18.16), respectively. This may be because of the relative affordability of alcohol in Korea, and its strong drinking culture, particularly in the context of dinners and team building activities (63). A qualitative study conducted in Hong Kong revealed that household and parental drinking were associated with increased alcohol consumption (64). According to a WHO report, alcohol use is high in Korea at 9.6 alcohol per capita (15+ liters of pure alcohol) (65). In our meta-analysis, China had the second-highest 1-year AUD prevalence, at 9.66% (95% CI: 4.31, 15.01), and the second-highest lifetime AUD prevalence, at 13.18% (95% CI: 4.34, 22.02). These rates are much higher than those reported in mainland China, possibly because alcohol has become more accessible to the Chinese population because of reduced prices (11, 66, 67), more advertisements, less strict regulation of sales (68), and an increase in the number of outlets providing alcohol (69). Second, incomes in China have been increasing, which would likely increase both alcohol consumption and AUD rates (70); alcohol use is lower among low-income groups (71). Third, exposure to alcoholic beverages is increasing in line with the number of factories producing alcoholic beverages. For instance, a modeling study on global alcohol exposure between 1990 and 2017 revealed that, globally, adult per capita alcohol consumption increased from 5.7 L in 1990 to 7.6 L in 2017 (72). Banning alcohol advertising, and making it less available and more expensive, are potential cost-effective strategies for reducing AUD (73).
In this study, smoking (overall OR: 3.99; 95% CI: 1.65, 6.33) was the main determinant of AUD; smokers were four times more likely than non-smokers to have AUD, in line with studies conducted in the United States (74–76), Brazil (14), and India (77). The association between smoking and AUD may be attributed to the synergetic effect of the chemicals present in tobacco and alcohol. For instance, a glucocorticoid receptor activated by nicotine can alter the sensitivity of the GABAergic system to ethanol (78). In addition, nicotine potentiates the rewarding effects of ethanol (79). In fact, nicotine and alcohol can both potentiate the rewarding effects of the other substance, and nicotine use increases the likelihood of relapse among those who have quit alcohol (80).
Our systematic review and meta-analysis showed that male gender is a risk factor for AUD (overall OR: 5.9; 95% CI: 3.3, 8.51). The AUD rate among males was approximately six times higher than that among females, consistent with a previous study reporting sex differences in the prevalence of AUD (81). This sex difference is mainly attributed to variations in dopamine receptor density and gonadal steroid hormones (82). In addition, the differences in societal roles between males and females may explain the gender difference in the AUD rate. For example, in East Asian countries, females are highly engaged in housework and take a role of caregiver for their family and thus have less opportunities for alcohol use. Besides, females who are pregnant or planning to get pregnant may abstain from alcohol drinking (83, 84).
Unlike Western studies that have identified several risk factors for AUD, such as the presence of mental health problems (85, 86), stigmatization and impulsiveness (87), a religious practice, education levels (88), and anxiety sensitivity (89), few studies of AUD conducted in East Asian countries explored its determinants. Eight of the studies included herein did not report determinants of AUD, such that our analysis of these factors was limited to two or three articles. Similarly, other studies conducted in China also revealed that mood and anxiety disorder (30), comorbid mental disorders, and marital status were significantly associated with AUD (29).
This systematic review and meta-analysis provided comprehensive, up-to-date data on the overall prevalence of AUD in East Asian countries, and also shed light on its determinants. Also, most of the included studies were nationwide epidemiological studies with large sample sizes, and thus high generalizability. The cohort, case-control, and cross-sectional studies in this meta-analysis were of high quality and used the NOS.
Limitations
As well as strengths, the current study also had some limitations. First, there was considerable publication bias among the included studies. Second, some of the studies failed to report all of the outcomes of interest. For example, one study reported on alcohol abuse but not alcohol dependence, while others reported the 1-year prevalence rate of AUD but not the lifetime prevalence (or vice versa). Five articles reported both the 1-year and lifetime AUD prevalence rates, while four reported only the former. Third, the findings may not be representative of Mongolia and Macau, because none of the included articles were conducted in those countries.
Conclusion
This systematic review and meta-analysis revealed that 1-year and lifetime AUD rates are high in East Asian countries, and that smoking and male gender are significant risk factors for AUD. The findings of this study provide baseline information for governments and policymakers that could inform new treatment approaches for AUD. Moreover, this study shows that greater awareness of the consequences of alcohol consumption, including mortality and associated morbidities, is urgently required. Finally, this review highlighted the need to focus on smokers because of their higher likelihood of developing AUD.
Author contributions
GB: conceptualization-equal, data curation-equal, formal analysis-equal, funding acquisition-equal, investigation-equal, methodology-equal, project administration-equal, resources-equal, software-equal, supervision-equal, validation-equal, visualization-equal, writing—original draft-equal, and writing—review and editing-equal. KL: conceptualization-equal, investigation-equal, methodology-equal, supervision-equal, validation-equal, writing—original draft-equal, and writing—review and editing-equal. QL: investigation-supporting, project administration-supporting, resources-supporting, and validation-supporting. CW: conceptualization-equal, methodology-equal, resources-equal, software-equal, and writing—review and editing-equal. YM: conceptualization-equal, methodology-equal, supervision-equal, validation-equal, writing—original draft-equal, and writing—review and editing-equal. KH: conceptualization-lead, data curation-equal, formal analysis-equal, investigation-equal, methodology-lead, project administration-equal, resources-lead, software-equal, supervision-lead, validation-equal, visualization-equal, writing—original draft-equal, and writing—review and editing-equal. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank Michael Irvine, PhD, from Edanz (www.edanz.com/ac) for editing a draft of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1144012/full#supplementary-material
References
1. National Institute. Alcohol Use Disorder: A Comparison Between DSM–IV and DSM−5 on on Alcohol abuse or Alcoholism. (2021). Available online at: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-use-disorder-comparison-between-dsm (accessed April, 2021).
2. Miriam E. The National Survey on Drug Use Health: 2020. (2020). Available online at: https://www.samhsa.gov/data/release/2020-national-survey-drug-use-and-health-nsduh-releases (accessed July, 2022).
3. SAMHSA. 2020 National Survey on Drug Use and Health:Asian/Native Hawaiians and Other Pacific Islanders (NHOPI). (2022).
4. WHO. Health at a glance: Asia/Pacific 2020 measuring progress towards universal health coverage: Measuring progress towards universal health coverage. OECD Publishing (2020).
5. Monzavi SM, Afshari R, Rehman N. Alcohol related disorders in Asia Pacific region: Prevalence, health consequences and impacts on the nations. Asia Pacific J Med Toxicol. (2015) 4:1–8.
8. WHO. Alcohol key fact sheet. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/alcohol (accessed May 09, 2022).
9. Polansky B. 13 Complications of Alcoholism: How Long-Term Heavy Drinking Affects Your Body, 1st step behavioral health. (2022). Available online at: https://firststepbhcom/blog/13-complications-of-alcoholism-how-long-term-heavy-drinking-affects-your-body/ (accessed September 21, 2020).
10. NICE National Institute. Alcohol use disorders: The NICE guideline on the diagnosis, assessment and management of harmful drinking and alcohol dependence. (2011). Report No.: 1904671268.
11. Kruse MI, Radnovich AJ, Kalapatapu RK, Mehdiyoun N, Chambers RA, Davidson D. Effects of alcohol availability, access to alcohol, and naltrexone on self-reported craving and patterns of drinking in response to an alcohol-cue availability procedure. J Stud Alcohol Drugs. (2012) 73:205–15. doi: 10.15288/jsad.2012.73.205
12. World Health Organization. Alcohol. World Health Organization (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/alcohol (accessed May 09, 2022).
13. Nepal R, Priyanka J, Chhetri P, Godar S, Timsina P, Doranga S. Factors Associated with Problematic Alcohol Consumption among Adults in Putalibazar Municipality of Syangja District, Nepal. Adv Public Health. (2022) 2022:7588153. doi: 10.1155/2022/7588153
14. Reisdorfer E, Büchele F, Pires ROM, Boing AF. Prevalence and associated factors with alcohol use disorders among adults: a population-based study in southern Brazil. Rev Brasileira de Epidemiol. (2012) 15:582–94. doi: 10.1590/S1415-790X2012000300012
15. Gebre BB. Factors associated with alcohol use disorder among people living with HIV/AIDS attending art Clinic, Mizan Tep University teaching hospital, south West Ethiopia. HIV/AIDS. (2019) 11:239. doi: 10.2147/HIV.S220211
16. Witkiewitz K, Litten R, Leggio L. Advances in the science and treatment of alcohol use disorder. Sci Adv. (2019) 5:eaax4043. doi: 10.1126/sciadv.aax4043
17. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006
18. Puddephatt J-A, Jones A, Gage SH, Fear NT, Field M, McManus S, et al. Associations of alcohol use, mental health and socioeconomic status in England: findings from a representative population survey. Drug Alcohol Depend. (2021) 219:108463. doi: 10.1016/j.drugalcdep.2020.108463
19. Kassew T, Kiflie M, Minichil W, Tilahun AD, Liyew B. Alcohol use disorder and its associate factors relating to patients with severe mental disorders attending psychiatric follow-ups in Northwest Ethiopia. Neuropsychiatr Dis Treat. (2021) 17:1801. doi: 10.2147/NDT.S309704
20. Puddephatt JA, Irizar P, Jones A, Gage SH, Goodwin L. Associations of common mental disorder with alcohol use in the adult general population: a systematic review and meta-analysis. Addiction. (2022) 117:1543–72. doi: 10.1111/add.15735
21. Sterling SA, Palzes VA, Lu Y, Kline-Simon AH, Parthasarathy S, Ross T, et al. Associations between medical conditions and alcohol consumption levels in an adult primary care population. JAMA Netw Open. (2020) 3:e204687. doi: 10.1001/jamanetworkopen.2020.4687
22. Buddy T. Alcohol Dependence vs. Alcohol Abuse: What's the Difference? Available online at: https://www.verywellmind.com/alcohol-abuse-vs-alcohol-dependence-63101#citation-1 (accessed April 02, 2022).
23. Peter Anderson and Ben Baumberg European Commission. Alcohol in Europe A public health perspective. Institute of Alcohol Studies UK (2006).
24. Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NO) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. (2011) 2:1–12.
25. Modesti P, Reboldi G, Cappuccio F. Newcastle-Ottawa quality assessment scale (adapted for cross sectional studies). PLoS ONE. (2016) 11:e0147601.
26. Penson D, Krishnaswami S, Jules A, Seroogy J, McPheeters M. Newcastle-Ottawa quality assessment form for cohort studies. Ottawa: Ottawa Hospital Research Institute. (2012).
27. Higgins JP, Thompson SG, Spiegelhalter DJ, A. re-evaluation of random-effects meta-analysis. J R Stat Soc. (2009) 172:137–59. doi: 10.1111/j.1467-985X.2008.00552.x
28. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
29. Phillips MR, Cheng HG Li X, Zhang J, Shi Q, Xu G, et al. Prevalence, correlates, comorbidity, and age of onset of alcohol use disorders in adult males from five provinces in China. Drug Alcohol Depend. (2017) 173:170–7. doi: 10.1016/j.drugalcdep.2016.12.026
30. Cheng H, Phillips M, Li X, Zhang J, Shi Q, Xu G, et al. Co-occurrence of DSM-IV mental disorders and alcohol use disorder among adult Chinese males. Psychol Med. (2017) 47:2811–22. doi: 10.1017/S0033291717001337
31. Chen X, Pan YM, Xu PR, Huang Y, Li N, Song Y. Family alcohol use, rather than childhood trauma, is more likely to cause male alcohol use disorder: findings from a case-control study in northern China. BMC Psychiatry. (2021) 21:1–8. doi: 10.1186/s12888-021-03566-8
32. Guo W, Lanzi G, Luobu O, Ma X, Zhen P, Ji Y, et al. An epidemiological survey of alcohol use disorders in a Tibetan population. Psychiatry Res. (2008) 159:56–66. doi: 10.1016/j.psychres.2007.09.012
33. Hahm BJ, Cho MJ. Prevalence of alcohol use disorder in a South Korean community. Changes in the pattern of prevalence over the past 15 years. Soc Psychiat Psychiatr Epidemiol. (2005) 40:114–9. doi: 10.1007/s00127-005-0854-9
34. Ishikawa H, Kawakami N, Kessler RC. Lifetime and 12-month prevalence, severity and unmet need for treatment of common mental disorders in Japan: Results from the final dataset of World Mental Health Japan Survey. Epidemiol Psychiatr Sci. (2016) 25:217–29. doi: 10.1017/S2045796015000566
35. Ji A, Lou P, Dong Z, Xu C, Zhang P, Chang G, et al. The prevalence of alcohol dependence and its association with hypertension: a population-based cross-sectional study4 in Xuzhou city, China. BMC Public Health. (2018) 18:364. doi: 10.1186/s12889-018-5276-1
36. Kim JH, Lee S, Chow J, Lau J, Tsang A, Choi J, et al. Prevalence and the factors associated with binge drinking, alcohol abuse, and alcohol dependence: A population-based study of chinese adults in Hong Kong. Alcohol Alcoholism. (2008) 43:360–70. doi: 10.1093/alcalc/agm181
37. Lee CS, Liao SF, Liu IC, Lee WC, Cheng AT. Incidence of first onset alcohol use disorder: a 16-year follow-up in the Taiwanese aborigines. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:955–63. doi: 10.1007/s00127-012-0600-z
38. Lee HK, Chou SP, Cho MJ, Park JI, Dawson DA, Grant BF. The prevalence and correlates of alcohol use disorders in the United States and Korea-a cross-national comparative study. Alcohol. (2010) 44:297–306. doi: 10.1016/j.alcohol.2010.02.005
39. Lee S, Tsang A, Zhang MY, Huang YQ, He YL, Liu ZR, et al. Lifetime prevalence and inter-cohort variation in DSM-IV disorders in metropolitan China. Psychol Med. (2007) 37:61–71. doi: 10.1017/S0033291706008993
40. Orui M, Kawakami N, Iwata N, Takeshima T, Fukao A. Lifetime prevalence of mental disorders and its relationship to suicidal ideation in a Japanese rural community with high suicide and alcohol consumption rates. Environ Health Prev Med. (2011) 16:384–9. doi: 10.1007/s12199-011-0209-y
41. Park SH, Kim CH, Kim DJ, Suk KT, Park HY, Lee JG, et al. Secular trends in prevalence of alcohol use disorder and its correlates in Korean adults: results from Korea National Health and Nutrition Examination Survey 2005 and 2009. Substance Abuse. (2012) 33:327–35. doi: 10.1080/08897077.2012.662209
42. Zhang T, Liu Z, Li G, Huang Y, Li Y, Geng H, et al. Correlates of transitions from alcohol use to disorder diagnosed by DSM-5 in China. BMC Psychiatry. (2021) 21:1–10. doi: 10.1186/s12888-021-03413-w
43. Zhi J, Zhang Y, You X, Long Q, Zhu Y, Liu J, et al. An epidemiological cross-sectional study of prevalence of mental disorders in Dulong nationality of Southwest China. Medicine. (2020) 99:e21884. doi: 10.1097/MD.0000000000021884
44. Zhou L, Conner KR, Phillips MR, Caine ED, Xiao S, Zhang R, et al. Epidemiology of alcohol abuse and dependence in rural chinese men. Alcoholism. (2009) 33:1770–6. doi: 10.1111/j.1530-0277.2009.01014.x
45. The Recovery Village. Facts and Statistics about Alcohol Abuse in the United States. (2022). Available online at: https://www.therecoveryvillage.com/alcohol-abuse/alcohol-facts-statistics/ (accessed January 03, 2023).
46. Teesson M, Hall W, Slade T, Mills K, Grove R, Mewton L, et al. Prevalence and correlates of DSM-IV alcohol abuse and dependence in Australia: findings of the 2007 National Survey of Mental Health and Wellbeing. Addiction. (2010) 105:2085–94. doi: 10.1111/j.1360-0443.2010.03096.x
47. National Institute. International Comparisons of Alcohol Consumption. (2003). Available online at: https://pubs.niaaa.nih.gov/publications/arh27-1/95-109.htm (accessed December, 2003).
48. Jiang L. Comparison of the difference between Chinese and Western drinking culture. Asian Soc Sci. (2011) 7:251. doi: 10.5539/ass.v7n5p251
49. Lyons AC, Willott SA. Alcohol consumption, gender identities and women's changing social positions. Sex Roles. (2008) 59:694–712. doi: 10.1007/s11199-008-9475-6
50. Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology. (2011) 218:1–17. doi: 10.1007/s00213-011-2236-1
51. Wuyts C, Barbier S, Loosveldt G. Comparison of alcohol consumption in European countries, and some methodological thoughts. In: ESS Conference. Lausanne (2016).
52. SAMHSA. 2020 National Survey on Drug Use and Health: Asian/Native Hawaiians and Other Pacific Islanders (NHOPI). (2020). Available online at: https://www.samhsa.gov/data/release/2020-national-survey-drug-use-and-health-nsduh-releases (accessed July, 2022).
53. World Health Organization. Alcohol Iraq 2019 Country Profile. World Health Organization (2019). Available online at: https://www.who.int/publications/m/item/alcohol-irq-2019 (accessed January 01, 2019).
54. World Health Organization. Alcohol Lebanon 2019 Country Profile. World Health Organization (2019). Available online at: https://www.who.int/publications/m/item/alcohol-lbn-2019 (accessed January 01, 2019).
55. World Health Organization. Alcohol United Arab Emirates 2019 Country Profile. World Health Organization (2019). Available online at: https://www.who.int/publications/m/item/alcohol-are-2019 (accessed January 01, 2019).
56. World Health Organization. Alcohol Jordan 2019 Country Profile. World Health Organization (2019). Available online at: https://www.who.int/publications/m/item/alcohol-jor-2019 (accessed January 01, 2019).
57. World Health Organization. Alcohol Bahrain 2019 Country Profile. World Health Organization (2019). Available online at: https://www.who.int/publications/m/item/alcohol-bhr-2019 (accessed January 01, 2019).
58. Alhashimi FH, Khabour OF, Alzoubi KH, Al-Shatnawi SF. Attitudes and beliefs related to reporting alcohol consumption in research studies: a case from Jordan. Pragm Observ Res. (2018) 9:55. doi: 10.2147/POR.S172613
59. Abu-Ras W, Ahmed S, Arfken CL. Alcohol use among US Muslim college students: Risk and protective factors. J Ethn Subst Abuse. (2010) 9:206–20. doi: 10.1080/15332640.2010.500921
60. Pan S, Wang L, Koenig H, Wang Z. Tobacco and alcohol use in Muslims compared with local Han population in Mainland China. J Psychiat Mental Diso. (2016) 1:1003.
61. Tevik K, Bergh S, Selbæk G, Johannessen A, Helvik A-S, A. systematic review of self-report measures used in epidemiological studies to assess alcohol consumption among older adults. PLoS ONE. (2021) 16:e0261292. doi: 10.1371/journal.pone.0261292
62. Greenfield TK, Kerr WC. Alcohol measurement methodology in epidemiology: recent advances and opportunities. Addiction. (2008) 103:1082–99. doi: 10.1111/j.1360-0443.2008.02197.x
63. Son H-G, Jeong K-H, Cho HJ, Lee M. Changes in types of drinking behavior in Korean adults: differences in demographics, depression, and suicidal thoughts. Int J Environ Res Public Health. (2021) 18:7514. doi: 10.3390/ijerph18147514
64. Mak YW, Leung D, Loke AY. The vulnerability to alcohol, tobacco, and drug use of adolescents in Hong Kong: a phenomenological study. BMC Pediatr. (2019) 19:1–12. doi: 10.1186/s12887-019-1678-1
65. WHO. Alcohol Democratic People's Republic of Korea 2019 country profile. (2019). Available online at: https://www.who.int/publications/m/item/alcohol-prk-2019 (accessed January 01, 2019).
66. Martín-Turrero I, Valiente R, Molina-de La Fuente I, Bilal U, Lazo M, Sureda X. Accessibility and availability of alcohol outlets around schools: An ecological study in the city of Madrid, Spain, according to socioeconomic area-level. Environ Res. (2022) 204:112323. doi: 10.1016/j.envres.2021.112323
67. Xu X, Chaloupka FJ. The effects of prices on alcohol use and its consequences. Alcohol Res Health. (2011) 34:236.
68. Dent CW, Grube JW, Biglan A. Community level alcohol availability and enforcement of possession laws as predictors of youth drinking. Prevent Med. (2005) 40:355–62. doi: 10.1016/j.ypmed.2004.06.014
69. Treno AJ, Grube JW, Martin SE. Alcohol availability as a predictor of youth drinking and driving: a hierarchical analysis of survey and archival data. Alcoholism. (2003) 27:835–40. doi: 10.1097/01.ALC.0000067979.85714.22
70. Crawford MJ, Parry AM, Weston AR, Seretis D, Zauter-Tutt M, Hussain A, et al. Relationship between price paid for off-trade alcohol, alcohol consumption and income in England: a cross-sectional survey. Alcohol Alcoholism. (2012) 47:738–42. doi: 10.1093/alcalc/ags091
71. Ejebu O, McKenzie L, Ludbrook A. Household purchasing of cheap alcohol: Who would be most affected by minimum unit pricing? Nordic J Health Econ. (2018) 6:11–29. doi: 10.5617/njhe.4878
72. Manthey J, Shield KD, Rylett M, Hasan OS, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet. (2019) 393:2493–502. doi: 10.1016/S0140-6736(18)32744-2
73. Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet. (2009) 373:2234–46. doi: 10.1016/S0140-6736(09)60744-3
74. Han BH, Moore AA, Sherman S, Keyes KM, Palamar JJ. Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005–2014. Drug Alcohol Depend. (2017) 170:198–207. doi: 10.1016/j.drugalcdep.2016.11.003
75. Grucza RA, Bierut LJ. Cigarette smoking and the risk for alcohol use disorders among adolescent drinkers. Alcoholism. (2006) 30:2046–54. doi: 10.1111/j.1530-0277.2006.00255.x
76. Jiang N, Lee YO, Ling PM. Association between tobacco and alcohol use among young adult bar patrons: a cross-sectional study in three cities. BMC Public Health. (2014) 14:1–9. doi: 10.1186/1471-2458-14-500
77. Thomas BE, Thiruvengadam K, Kadam D, Ovung S, Sivakumar S, Bala Yogendra Shivakumar SV, et al. Smoking, alcohol use disorder and tuberculosis treatment outcomes: A dual co-morbidity burden that cannot be ignored. PLoS ONE. (2019) 14:e0220507. doi: 10.1371/journal.pone.0220507
78. Britt JP, Bonci A. Alcohol and tobacco: how smoking may promote excessive drinking. Neuron. (2013) 79:406–7. doi: 10.1016/j.neuron.2013.07.018
79. Rose JE, Brauer LH, Behm FM, Cramblett M, Calkins K, Lawhon D. Psychopharmacological interactions between nicotine and ethanol. Nicotine Tobacco Res. (2004) 6:133–44. doi: 10.1080/14622200310001656957
80. Frie JA, Nolan CJ, Murray JE, Khokhar JY. Addiction-related outcomes of nicotine and alcohol co-use: new insights following the rise in vaping. Nicotine Tobacco Res. (2022) 24:1141–9. doi: 10.1093/ntr/ntab231
81. Agabio R, Pisanu C, Luigi Gessa G, Franconi F. Sex differences in alcohol use disorder. Curr Med Chem. (2017) 24:2661–70. doi: 10.2174/0929867323666161202092908
82. Ceylan-Isik AF, McBride SM, Ren J. Sex difference in alcoholism: who is at a greater risk for development of alcoholic complication? Life Sci. (2010) 87:133–8. doi: 10.1016/j.lfs.2010.06.002
83. Goh CMJ, Asharani P, Abdin E, Shahwan S, Zhang Y, Sambasivam R, et al. Gender differences in alcohol use: a nationwide study in a multiethnic population. In: International Journal of Mental Health and Addiction. (2022) 1–15. doi: 10.1007/s11469-022-00921-y
84. Wilsnack RW, Wilsnack SC, Obot IS. Why study gender, alcohol and culture. In: Alcohol, gender and drinking problems: Perspectives from low and middle income countries. (2005) 1–23.
85. Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. (2007) 64:830–42. doi: 10.1001/archpsyc.64.7.830
86. Roberts B, Murphy A, Chikovani I, Makhashvili N, Patel V, McKee M. Individual and community level risk-factors for alcohol use disorder among conflict-affected persons in Georgia. PLoS ONE. (2014) 9:e98299. doi: 10.1371/journal.pone.0098299
87. Fleury M-J, Grenier G, Bamvita J-M, Perreault M, Caron J. Predictors of alcohol and drug dependence. Canadian J Psychiatry. (2014) 59:203–12. doi: 10.1177/070674371405900405
88. Jaeger GP, Mola CLd, Silveira MF. Alcohol-related disorders and associated factors in a rural area in Brazil. Rev de Saúde Pública. (2018) 52:262. doi: 10.11606/S1518-8787.2018052000262
Keywords: alcohol use disorder, determinants, prevalence, East Asian countries, systematic review and meta-analysis
Citation: Belay GM, Lam KKW, Liu Q, Wu CST, Mak YW and Ho KY (2023) Magnitude and determinants of alcohol use disorder among adult population in East Asian countries: A systematic review and meta-analysis. Front. Public Health 11:1144012. doi: 10.3389/fpubh.2023.1144012
Received: 13 January 2023; Accepted: 08 February 2023;
Published: 28 February 2023.
Edited by:
Muthuraju Sangu, University of Houston, United StatesReviewed by:
Veena Vuttaradhi, University of Texas MD Anderson Cancer Center, United StatesGallus Bischof, University of Lübeck, Germany
Copyright © 2023 Belay, Lam, Liu, Wu, Mak and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ka Yan Ho,  a3lhbmhvQHBvbHl1LmVkdS5oaw==
a3lhbmhvQHBvbHl1LmVkdS5oaw==
 Getaneh Mulualem Belay
Getaneh Mulualem Belay Katherine Ka Wai Lam
Katherine Ka Wai Lam Qi Liu
Qi Liu Cynthia Sau Ting Wu
Cynthia Sau Ting Wu Yim Wah Mak
Yim Wah Mak Ka Yan Ho
Ka Yan Ho