Abstract
Background and purpose:
The findings of clinical studies exploring essential oils (EOs) for anxiety remain disputed, and no studies have yet clarified the differences in the efficacy of EOs. The purpose of the study was to directly or indirectly compare the efficacy of different types of EOs on anxiety by pooling the results of randomized controlled trials (RCTs).
Methods:
PubMed, Cochrane Library, Embase, Scopus, Web of Science and the Cochrane Central Register of Controlled Trials (CENTRAL) databases were searched from inception to November 2022. Only full texts of RCTs that investigated the effects of EOs on anxiety were included. The trial data were extracted and the risk of bias was assessed by two reviewers independently. Pairwise meta-analysis and network meta-analysis were performed by Stata 15.1 or R 4.1.2 software.
Results:
Forty-four RCTs (fifty study arms) involving 10 kinds of EOs and 3419 anxiety patients (1815 patients in EOs group and 1604 patients in control group) were included. Pairwise meta-analyses showed that EOs were effective in reducing State Anxiety Inventory scores (SAIS) [WMD = −6.63, 95% CI−8.17, −5.08] and Trait Anxiety Inventory scores (TAIS) [WMD = −4.97, 95% CI−6.73, −3.20]. Additionally, EOs could decrease systolic blood pressure (SBP) [WMD = −6.83, (95% CI −10.53, −3.12), P < 0.001] and heart rate (HR) [WMD = −3.43, (95% CI −5.51, −1.36), P < 0.001]. Network meta-analyses demonstrated that regarding the outcome of SAIS, Jasminum sambac (L.)Ait. (jasmine) was the most effective with a weighted mean difference (WMD) of−13.61 (95% CrI−24.79, −2.48). Followed by Citrus (citrus aurantium L.), which had a WMD of−9.62 (95% CrI−13.32, −5.93). Moderate effect sizes were observed for Rosa rugosa Thunb. (damask rose) (WMD = −6.78, 95% CrI−10.14, −3.49) and Lavandula angustifolia Mill. (lavender) (WMD = −5.41, 95% CrI−7.86, −2.98). Regarding the results of TAIS, citrus aurantium L. was the best ranked intervention with a WMD of−9.62 (95% CrI−15.62, −3.7). Moderate-to-large effect sizes were observed for Citrus limon (L.) Burm. F. (lemon) (WMD:−8.48; 95% CrI−16.67, −0.33) and lavender (WMD:−5.5; 95% CrI−8.7, −2.46).
Conclusion:
According to the comprehensive analysis, EOs are effective in reducing both state anxiety and trait anxiety, and citrus aurantium L. essential oil seems to be the most recommended type of EO for treating anxiety because of its significant effects in reducing SAIS and TAIS.
Systematic review registration:
https://www.crd.york.ac.uk/PROSPERO/, identifier: CRD42022331319.
1. Introduction
Anxiety disorders are one of the most disabling mental disorders and a major contributor to the global burden of disease (1). The prevalence of anxiety disorders is susceptible to political, social, economic and environmental changes, especially in the context of the era of the COVID-19 epidemic in the last 3 years, which has increased the prevalence of anxiety disorders by more than 25% (2, 3).
Currently, benzodiazepines (BDZs) and selective serotonin reuptake inhibitors (SSRIs) remain the cornerstones of treating anxiety disorders. These drugs provide a large short-term benefit, but their long-term efficacy is still limited and may cause certain side effects (4). In this context, complementary and alternative medicine (CAM) therapies are becoming increasingly accepted for their naturalness, affordability and fewer adverse effects. Aromatherapy, as its most important component, uses essential oils (EOs) to effectively balance the mind, body and spirit of the individual (5, 6). EOs are natural products from plants with small molecular weight and certain volatility (7). Essential oil (EO) molecules can affect the hypothalamus, autonomic nervous system and endocrine system (8), improve peripheral blood circulation, regulate blood pressure, pulse and respiration, and ultimately reduce anxiety (9–11).
Recently, a growing number of clinical trials have begun to explore the effects of EOs on anxiety due to various causes. However, the findings of EOs reduce anxiety remained somewhat controversial. Some studies have shown that EOs are effective in relieving anxiety, but others have concluded the opposite. Since the chemical constituents of EOs may vary greatly due to the species, origin place, extraction method, and concentrations in different clinical trials. Furthermore, different intervention procedures can also lead to differences in the effective constituents of which EOs exert their efficacy in the body (12). Therefore, the efficacy of EO may vary in different clinical trials even with the same type of EO. Herein, the efficacy of EOs in alleviating anxiety states still needs to be evaluated by meta-analysis. Of all the types of EOs, lavender is the most extensively studied. There is a meta-analysis has shown that Lavandula angustifolia Mill. (lavender) EO could ameliorate anxiety and its associated physiological parameters such as systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and respiratory rate (RR) (13). Interestingly, another meta-analysis concluded that inhalation of lavender EO does not significantly reduce SBP (14). Furthermore, conventional pairwise meta-analyses are unable to integrate all the evidence from different types of EOs for anxiety at the same time, making it difficult to comprehensively and systematically evaluate the differences in the efficacy of various EOs and to select the best EO treatment regimen.
Given the limitations of the above studies, we used network meta-analysis combining both direct and indirect evidence to rank essential oils according to State Anxiety Inventory scores (SAIS) and Trait Anxiety Inventory scores (TAIS), and provide evidence-based medical evidence for the adoption of EOs for the treatment of anxiety disorders.
2. Methods
This study was conducted in accordance with the System Preferred Reporting Item Review and Meta-Analysis (PRISMA 2020) guidelines (15). The study was designed to explore the efficacies of common EOs on different causes of anxiety.
2.1. Protocol and registration
The protocol of the review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) with registration number: CRD42022331319.
2.2. Data sources and search strategy
Two investigators (LT and F-FL) independently performed the database search. PubMed, Cochrane Library, Embase, Scopus, Web of Science and the Cochrane Central Register of Controlled Trials (CENTRAL) databases were searched with the terms combined medical subject headings (MeSH) and entry terms: [“oils, volatile”(MeSH) or “essential oils” or “volatile oils” or “aromatherapy” or “odorant”] AND [“anxiety” (MeSH) or “anxious” or “nervousness” or “hypervigilance” or “affect” or “mood” or “PHQ” or “GAD”] AND (“randomized controlled trial” or “clinical trial” or “RCT”) from inception to Nov 25, 2022. The detailed search strategies are listed in Supplementary Table S1. Moreover, the reference lists of the included studies and relevant review articles were manually checked to identify potential records that met the established criteria. Searches were not restricted by language.
2.3. Inclusion and exclusion criteria
The inclusion criteria were based on the Participant, Intervention, Comparison, Outcome, and Study design framework: (1) participant: adults (aged ≥ 18) with anxiety meet the diagnostic criteria of Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-V), or the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10), or with scores of at least 20 in the Spielberger State-Trait Anxiety Inventory (STAI) questionnaire (mild anxiety), or have a specific trigger for anxiety and no olfactory problems and no allergies to aromatic substances; (2) intervention: inhalation of EOs (of any duration and frequency) in the trial group; (3) comparison: inhalation of unscented oil or only routine therapy in the control group; (4) outcomes: baseline and post-treatment SAIS, with or without TAIS and vital sign parameters, such as SBP, DBP, HR and RR; and (5) study design: randomized controlled trials (RCTs).
The following exclusion criteria were implemented: (1) the intervention was a mixture of EOs rather than a single type of EO; (2) studies with skewed baseline data for SAIS; (3) articles for which the full text was not available, and studies with incomplete primary outcome data; (4) duplicate publications; (5) studies were published as comments, conference abstracts, or letters to the editor.
2.4. Data extraction and quality assessment
After excluding trials that did not meet the eligibility criteria, two reviewers (LT and F-FL) independently read the full text of the remaining articles, and conducted data collection according to a validated extraction sheet based on the guidance of the Cochrane Handbook for Systematic Reviews of Interventions. The extracted data included: (1) general information (first author, publication year, and country); (2) participants (sample size, mean age, percentage of male participants, and causes of anxiety); (3) content of EOs (type of EO, cumulative duration of intervention, intervention doses); (4) details of the control group; and (5) outcomes (primary: SAIS and TAIS; secondary: SBP, DBP, HR, and RR). Disagreements were resolved through discussing with a third investigator (HQ).
Two reviewers independently assessed the risk of bias of the included studies with the Cochrane Risk of Bias assessment tool (RoB 2.0) (16). The overall risk of bias was classified as high risk (–), unclear risk (?), or low risk (+), based on the following domains: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of the outcome, bias in selection of the reported result and overall risk of bias. An adapted version of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool was used to evaluate the quality or confidence of evidence for each outcome by means of a web-based application Confidence in Network Meta-Analysis (CINeMA) (17).
2.5. Data synthesis and statistical analysis
A pair-wise meta-analysis was performed firstly by Der Simonian and Laird method. Then, a quantitative network meta-analysis of with random effects and uninformative priors based on Bayesian theorem was conducted to establish a comprehensive evaluation of the efficacy of EOs in treating anxiety.
The consistency model and the inconsistency model were applied to evaluate the hypothesis of overall consistency between networks in the meta-analysis. Then the deviance information criteria (DIC) of the two models were compared, and the model with the lower DIC value was selected. Subsequently, an ensemble node-split models were used to explore whether there was any statistical local inconsistency between direct and indirect comparisons (P-values > 0.1 indicated local consistency). A consistent model was accepted when there were no inconsistencies. Due to there were closed-loop structures between interventions, we conducted a loop inconsistency test to determine the existence of inconsistency according to the inconsistency factor (IF) value. If the IF value 95% CI contains 0, it indicates that there is no loop inconsistency.
Weighted mean difference (WMD) and 95% confidence interval (CI) were chosen as the effect sizes to report the results of the meta-analysis, while WMD and 95% credibility interval (CrI) as the effect sizes to report the results of the network meta-analysis. A WMD of 0.20 is considered a small difference between the trial and the control group; 0.50, a moderate difference; and 0.80, a large difference. The Higgins I-squared (I2) index was used to estimate the potential heterogeneity. Random effects models were chosen to compare treatment efficacy considering the clinical and methodological heterogeneity between studies. Each model was calculated by generating 10, 000 sample iterations, with an initial burn-in period of 2, 000 iterations (thin = 1). To rank the interventions, the probability of each intervention being ranked first, second, etc was calculated. The efficacy of each intervention was also ranked by calculating the surface under the cumulative ranking curve (SUCRA).
In view of the significant heterogeneity, exploratory subgroup analyses were conducted based on type of EO, country, cause of anxiety, and accumulative duration of intervention for SAIS, TAIS, SBP, DBP, HR, and RR. Meta-regression analyses were performed based on the accumulative duration of intervention, baseline SAIS and baseline TAIS. Additionally, sensitivity analyses were performed to assess the robustness of the results based on excluding the studies with < 30 patients per intervention arm to ensure that large or overestimated treatment benefits were excluded, since small studies tend to have larger effects compared with larger studies. Potential publication bias was evaluated by visual assessment of funnel plots.
Conventional pairwise meta-analyses were performed by STATA version 15.1 (Stata Corp, College Station, TX, USA). Network meta-analyses were conducted using R version 4.1.2 software (“netmeta” and “gemtc” 1.0.1 packages). Network pictures were created to visualize network geometry and node connectivity.
3. Results
3.1. Study selection
The screening process of a PRISMA study flow diagram was shown in Figure 1. We retrieved 5, 553 articles through a systematic search, of which 5, 265 were excluded after a preliminary screening of titles and abstracts since they were completely unrelated to the topic of “essential oil for anxiety”. Two hundred and eighty-eight articles were potentially eligible records whose full text was reviewed. Finally, 44 articles were included in present review (14, 18–60).
Figure 1
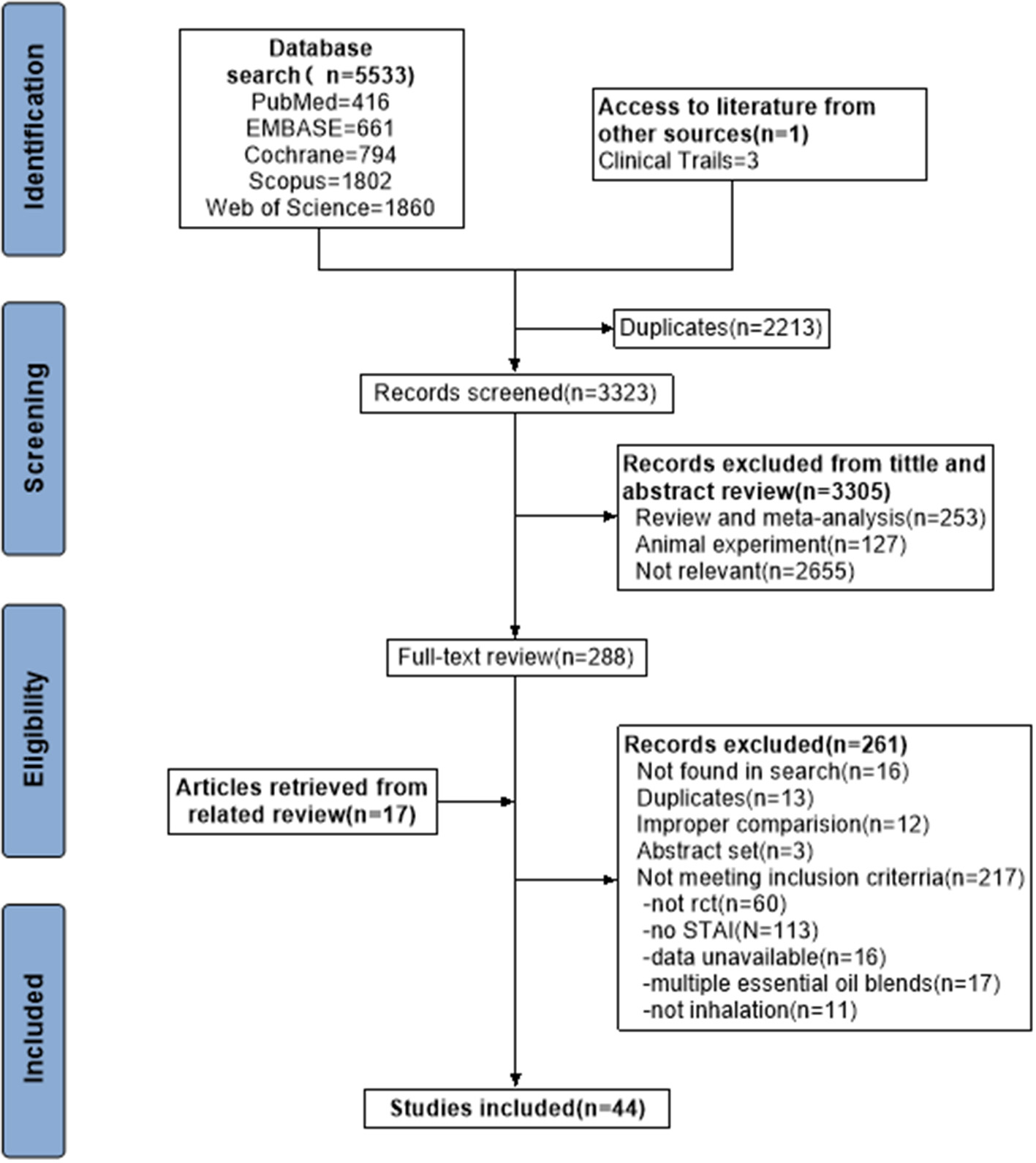
Flow diagram of study identification, screening, eligibility assessment, and inclusion.
3.2. Characteristics of included trials
Publication dates ranged from 2010 to 2022 (median, 2016), with 86% of trials published after 2016. Most trials were conducted by Iranian scholars (33/44, 75% trials). The second highest number of trials was conducted in Turkey, with eight. The EOs involved lavender, Rosa rugosa Thunb. (damask rose), Citrus (citrus aurantium L.), Phyla nodiflora (Linn.) E. L. Greene (lippia alba), Mentha haplocalyx Briq. (mint), Citrus limon (L.) Burm. F. (lemon), Eucalyptus citriodora Hook. f. (lippia citriodora), Pelargonium hortorum Bailey (geranium), Jasminum sambac (L.)Ait. (jasmine), and Balsam capivi, jesuits'resin (copaiba). Fourteen trials explored the effects of EOs on operation-related anxiety, while 12 trials about the invasive examinations induced anxiety. Overall, 44 studies involving 3,419 anxiety patients (1,815 patients in EOs group and 1604 patients in control group) were included (14, 18–60). The detailed characteristics of the studies included in this review were listed in Table 1.
Table 1
| Author, year | Country | Participants (EG, CG) | Causes of anxiety | Content of intervention (EG, CG) | Scale | Physiological parameters | |||
|---|---|---|---|---|---|---|---|---|---|
| Sample size (male/female) | Mean age (M ±SD or range) | Essential oil type | Duration of intervention | Volume of essential oil | |||||
| Abbasijahromi et al. (14) | Iran | EG1:30 EG2:30 CG:30 | EG1:29.73 ± 5.29 EG2:26.79 ± 5.53 CG:27.6 ± 5.31 | C-section | EG1: Lavender EG2: Damask rose | 30 min | 3 drops | STAI | NR |
| Alvarado-García et al. (18) | Perú | EG1:27 (12/15) EG2:27 (12/15) CG:26 (12/14) | EG1:39.50 ± 5.97 EG2:39.84 ± 5.90 CG:39.87 ± 5.85 | Spontaneous anxiety | EG1: Lippia alba EG2: Lippia citriodora | 30 min | 2 drops | STAI | NR |
| Amzajerdi et al. (19) | Iran | EG:33 (0/33) CG:33 (0/33) | EG:26.97 ± 4.57 CG:28.4 ± 3.91 | Pregnant | Mint | 280 min | 4 drops | SAI | NR |
| Babatabar Darzi et al. (20) | Iran | EG1:40(25/15) EG2:40(28/12) CG:40 (19/21) | EG1:60.50 ± 5.26 EG2:58.05 ± 5.26 CG:62.27 ± 6.49 | Open Heart Surgery | EG1: Damask rose EG2: Lavender | 15 min | 3 drops | SAI | NA |
| Bahadori et al. (21) | Iran | EG:30 (12/18) CG:30 (10/20) | EG:31.23 ± 4.41 CG:33.2 ± 7.49 | Operating room nurses | Damask Rose | 10 min | 2 drops | SAI | NR |
| Bakhsha et al. (22) | Iran | EG:50 CG:50 | NR | Preoperative Anxiety | Lavender | 1 min | NR | SAI | NR |
| Beyliklioglu and Arslan (23) | Turkey | EG:40 CG:40 | EG:51.48 ± 17.31 CG:48.00 ± 10.63 | Before Breast Surgery | Lavender | 20 min | 3.5 drops | SAI | NR |
| Eslami et al. (24) | Iran | EG:30 (15/15) CG:30 (15/15) | EG:51.93 ± 7.26 CG:51.47 ± 5.87 | Candidates for surgery | Citrus aurantium L. | 20 min | 2 drops | STAI | NR |
| Eslami et al. (25) | Iran | EG1:30 (15/15) EG2:30 (15/15) CG:30 (15/15) | EG1:51.87 ± 7.81 EG2:51.93 ± 7.26 CG:51.47 ± 5.87 | Laparoscopic cholecystectomy | EG1: Lavender EG2: Citrus aurantium L. | 20 min | 2 drops | STAI | NR |
| Farzaneh et al. (26) | Iran | EG:19 CG:19 | EG:49.21 ± 10.63 CG:47.74 ± 15.47 | Preoperative Anxiety | Damas Rose | 10 min | 3 drops | STAI | NR |
| Fayazi et al. (27) | Iran | EG:36 CG:36 | NR | Preoperative Anxiety | Lavender | 20 min | 2 drops | SAI | NA |
| Ganji et al. (28) | Iran | EG:44 (32/12) CG:44 (27/17) | EG:46.0 ± 11.5 CG:44.0 ± 13.5 | Kidney stones | Damask Rose | 15 min | 3 drops | SAI | NR |
| Haddadi et al. (29) | Iran | EG:40 (15/25) CG:40 (17/23) | NR | Myaocardial infarction | Damask Rose | 225 min | 3 drops | SAI | NR |
| Hamdamian et al. (30) | Iran | EG:55 CG:55 | EG:25.87 ± 5.17 CG:26.24 ± 5.15 | During first stage of labor | Damask Rose | 30 min | 2 drops | SAI | NR |
| Hekmatpou et al. (31) | Iran | EG:30 CG:30 | NR | Fractured limbs admitted | Citrus aurantium L. | 360 min | 4 drops | SAI | NR |
| Hu et al. (32) | China | EG:14 (9/5) CG:13 (6/7) | NR | Colonoscopy-related surgery | Citrus aurantium L. | 5 min | 1 drop | SAI | SBP, DBP, RR, HR |
| Jirdehi et al. (33) | Iran | EG1:35 (15/20) EG2:35 (11/24) CG:35 (19/16) | NR | Candidate for endoscopy | EG1: Lavender EG2: Damask Rose | 30 min | 2 drops | SAI | NR |
| Jodaki et al. (34) | Iran | EG:30 (16/14) CG:30 (15/15) | EG:62.8 ± 11.8 CG:61.5 ± 12.75 | Cardiac disease | Damask Rose | 1440 min | 5 drops | SAI | NR |
| Jokar. et al. (35) | Iran | EG:31 (0/31) CG:31 (0/31) | EG:55.95 ± 5.70 CG:53.56 ± 2.67 | Perimenopause | Lavender | 560 min | 2 drops | STAI | NR |
| Kasar et al. (36) | Turkey | EG:22 (6/16) CG:22 (3/19) | EG:48.6 ± 12.0 CG:48.1 ± 11.9 | Trigger Point Injection | Lavender | 12.5 min | 5 drops | SAI | NR |
| Mokhtari et al. (37) | Iran | EG:30 (16/14) CG:30 (15/15) | NR | Burn | Damask Rose | 480 min | 5 drops | SAI | NR |
| Moradi et al. (38) | Iran | EG:40 (21/19) CG:40 (24/16) | EG:55.71 ± 1.65 CG:55.95 ± 1.76 | Coronary arteriography | Citrus aurantium L. | 17.5 min | 4 mL | SAI | SBP, DBP, RR, HR |
| Moslemi et al. (39) | Iran | EG:70 (29/41) CG:70 (37/33) | EG:56.76 ± 11.39 CG:56.69 ± 11.37 | Acute coronary syndrome | Citrus aurantium L. | 20 min | 1.5 drops | SAI | NR |
| Ozkaraman et al. (40) | Turkey | EG:30 (6/24) CG:20 (3/17) | EG:57.73 ± 12.81 CG:57.55 ± 12.87 | Chemotherapy | Lavender | 150 min | 3 drops | STAI | NR |
| Pasyar et al. (41) | Iran | EG:30 (9/21) CG:30 (10/20) | EG:38.10 ± 12.37 CG:38.4 ± 9.58 | Laparoscopic cholecystectomy | Citrus aurantium L. | 20 min | 2 drops | SAI | NR |
| Pimenta et al. (42) | Brazil | EG:14 CG:14 | NR | Chronic Myeloid Leukemia | Citrus aurantium L. | 30 min | 10 mL | SAI | SBP, DBP, RR, HR |
| Rambod et al. (43) | Iran | EG:50 (27/23) CG:50 (28/22) | EG:61.42 ± 14.98 CG:61.84 ± 11.3 | Acute myocardial infarction | Lemon | 2160 min | 5 drops | STAI | SBP, DBP, HR |
| Reyes et al. (44) | Philippines | EG:25 (14/11) CG:25 (13/12) | EG:52.04 ± 10.38 CG:57.52 ± 13.51 | Puncture for hemodialysis patients | Citrus aurantium L. | 5 min | 3 drops | SAI | NR |
| Sahin et al. (45) | Turkey | EG:36 (19/17) CG:38 (23/15) | EG:50.75 ± 18.02 CG:53.62 ± 11.03 | Puncture for hemodialysis patients | Lavender | 15 min | 5 drops | STAI | NR |
| Saritas et al. (46) | Turkey | EG:45 (30/15) CG:45 (26/19) | EG:49.26 ± 14.57 CG:50.62 ± 14.58 | ERCP | Lavender | 30 min | 4 drops | SAI | SBP, DBP, HR |
| Shirzad et al. (47) | Iran | EG:34 (12/22) CG:34 (14/20) | EG:28.2 ± 7 CG:27.1 ± 5.9 | Septorhinoplasy and Rhinoplasty | Lavender | 20 min | 3 drops | STAI | NA |
| Soleimani et al. (48) | Iran | EG:32 (16/16) CG:32 (16/16) | NR | acute coronary syndrome | Mint | 60 min | 3 drops | SAI | NA |
| Soto-Vásquez et al. (49) | Peru | EG:28 (12/16) CG:27 (13/14) | NR | Spontaneous anxiety | Lippia alba | 360 min | 4 drops | STAI | NR |
| Stanley et al. (50) | Singapore | EG:39 (17/22) CG:36 (16/20) | EG:61.6 ± 7.0 CG:63.25 ± 7.7 | Cataract Surgery | Lavender | 20 min | 20 drops | SAI | SBP, DBP, RR, HR, SpO2 |
| Tahmasbi et al. (51) | Iran | EG:45 (18/27) CG:46 (23/23) | NR | Coronary angiography | Lavender | 3 min | 2 drops | STAI | NA |
| Tahmasebi et al. (52) | Iran | EG1:33 (12/21) EG2:35 (18/17) CG:33 (14/19) | EG1:60.12 ± 6.79 EG2:57.80 ± 6.21 CG:58.64 ± 6.11 | Coronary angiography | EG1: Lavender EG2: Citrus aurantium L. | 20 min | 2 drops | SAI | SBP, DBP, RR, HR, SpO2 |
| Wen et al. (53) | China | EG:50 (17/33) CG:50 (14/36) | EG:47.2 ± 14.5 CG:47.1 ± 14.2 | MRI examinations | Lavender | 20 min | 8 drops | SAI | NR |
| Fakarian and Tabatabaeichehr (54) | Iran | EG:49 (24/25) CG:48 (21/27) | EG:23 ± 7 CG:21 ± 5 | The first stage of labor | Geranium | 20 min | NR | SAI | SBP, DBP, RR, HR |
| Babaii et al. (55) | Iran | EG:30 CG:30 | EG:53.63 ± 9.99 CG:56.96 ± 7.89 | Cardiac Catheterization | Damask Rose | 18 min | NR | STAI | NR |
| Inci and Çetinkaya (56) | Turkey | EG:48 (30/18) CG:48 (28/20) | EG:60.89 ± 8.74 CG:56.54 ± 11.62 | Coronary angiography | Lavender | 15 min | 5 drops | SAI | SBP, DBP, RR, HR |
| Karan (57) | Turkey | EG:63 (13/50) CG:63 (17/46) | NR | Oral surgery | Lavender | 3 min | NR | SAI | SBP, DBP, RR, HR |
| Yadegari et al. (58) | Iran | EG:42 (33/9) CG:42 (33/9) | EG:35.55 ± 12.75 CG:36.26 ± 13.39 | Laparotomy | Jasmine | 60 min | 2 drops | SAI | NR |
| Zhang et al. (59) | China | EG:11 CG:11 | NR | Mental Workload | Copaiba | 20 min | NR | STAI | NA |
| Tugut et al. (60) | Turkey | EG:78 CG:78 | EG:35.0 ± 9.7 CG:33.5 ± 12.4 | Gynecological examination | Lavender | 12.5 min | NR | SAI | NR |
Characteristics of included studies.
EG, Experimental group (When there are two controlled trials in the same literature, EG1 and EG2 are used to represent the two experimental groups respectively); CG, Control group; NR, Not Reported; NA, No Analyzed (The study reported, but did not present original data that could be analyzed); STAI, Spielberger State-Trait Anxiety Inventory; SAI, State Anxiety Inventory.
3.3. Assessment of risk of bias
As shown in Figures 2, 3, all included trials were assessed for risk of bias (RoB 2.0) tool. Seventeen studies had a high risk of bias (18, 20, 22, 23, 30, 33, 35, 37, 38, 42–44, 46, 54, 55, 58, 59), and one-quarter of the studies (25%) were at “unclear risk of bias” (24, 25, 27, 29, 31, 32, 36, 45, 48, 50, 51), mostly due to deviations from the intended interventions and selection of the reported results. The remaining 16 studies were at low risk of bias (14, 19, 21, 26, 28, 34, 39–41, 47, 49, 52, 53, 56, 57, 60), with all assessed domains in these studies being at low risk.
Figure 2
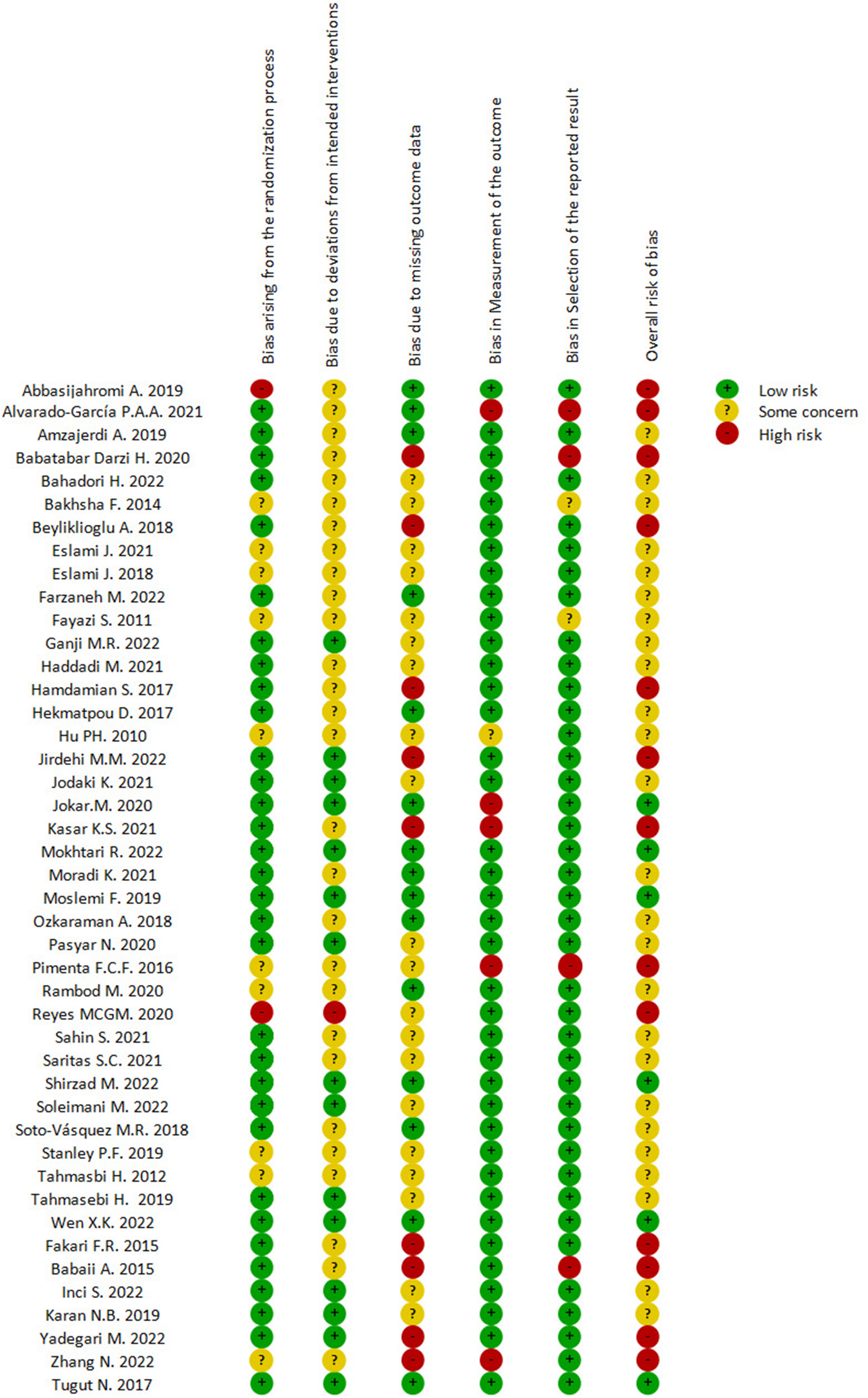
Summary of the risk of bias assessment.
Figure 3
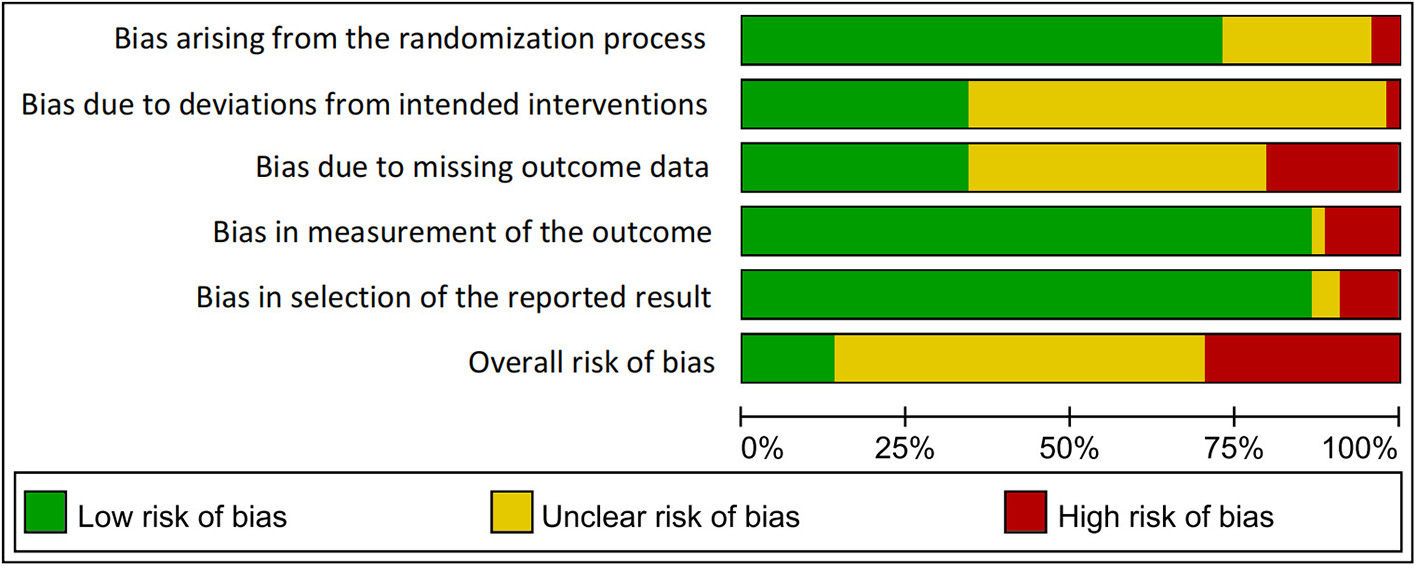
Risk of bias graph.
3.4. Direct pairwise meta-analysis
3.4.1. State anxiety inventory
Forty-four trials (50 study arms), including 3,419 anxiety patients (1,815 patients in EOs group vs. 1,604 patients in control group), evaluated the effects of EOs on their anxiety by State Anxiety Inventory (SAI). The pooled WMD showed that EOs therapy led to a significant lower level of state anxiety compared to control group [WMD = −6.63 (95% CI −8.17, −5.08), P < 0.001], with moderate heterogeneity (I2 = 93.2%, P < 0.001) (Figure 4).
Figure 4
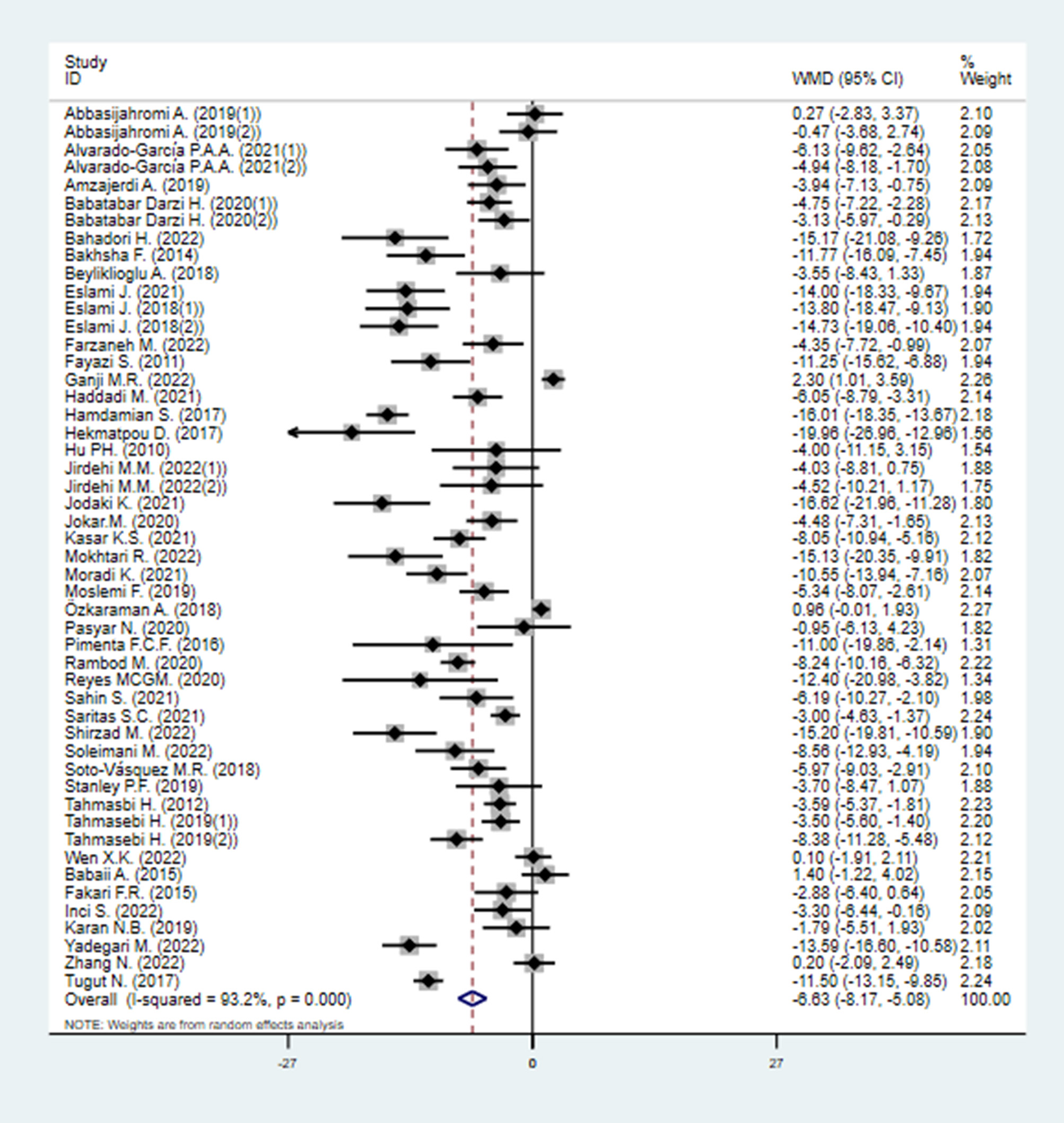
Direct pairwise random-effects meta-analyses of SAIS. SAIS, State Anxiety Inventory scores.
3.4.2. Trait anxiety inventory
A total of 14 studies (17 study arms), including 940 anxiety patients (518 patients in EOs group vs. 422 patients in control group), investigated the effects of EOs therapy on anxiety by Trait Anxiety Inventory (TAI). Pooled effect sizes from the eligible studies indicated that EOs therapy significant lowered the level of trait anxiety compared to control group [WMD = −4.97 (95% CI −6.73, −3.20), I2 = 93.9%, P < 0.001] (Figure 5).
Figure 5
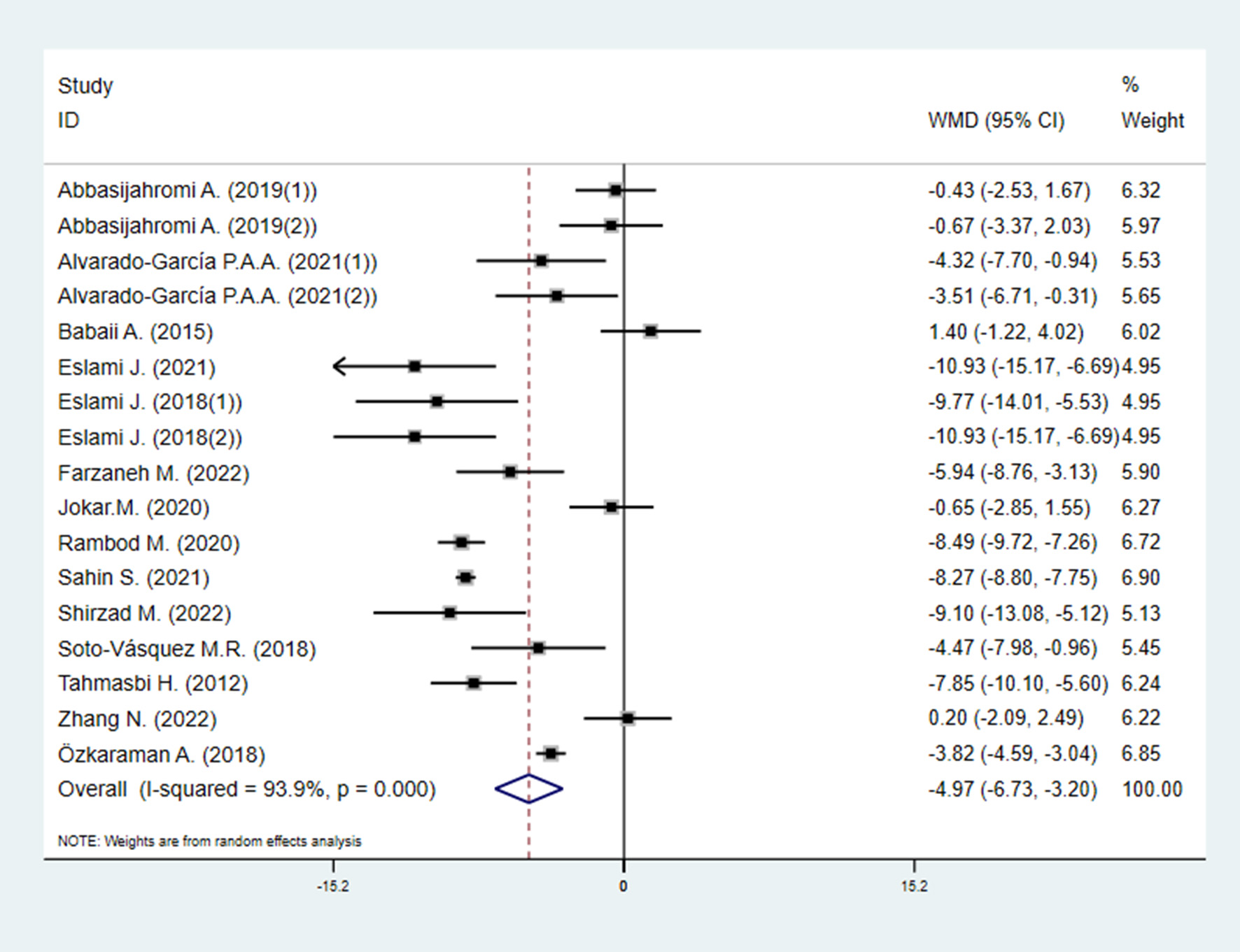
Direct pairwise random-effects meta-analyses of TAIS. TAIS, Trait Anxiety Inventory scores.
3.4.3. Vital signs
As presented in Figure 6, compared with the control, EOs could decrease SBP [WMD = −6.83 (95% CI−10.53, −3.12), P < 0.001] (Figure 6A) and HR [WMD = −3.43 (95% CI−5.51, −1.36), P < 0.001] (Figure 6C). The effects of EOs on DBP and RR were also evaluated. EOs had a tendency of decreasing DBP [WMD = −2.11 (95% CI−4.35, 0.13), P < 0.001] (Figure 6B) and RR [WMD = −0.53 (95% CI−1.52, 0.46), P < 0.001] (Figure 6D), but they were not statistically significant.
Figure 6
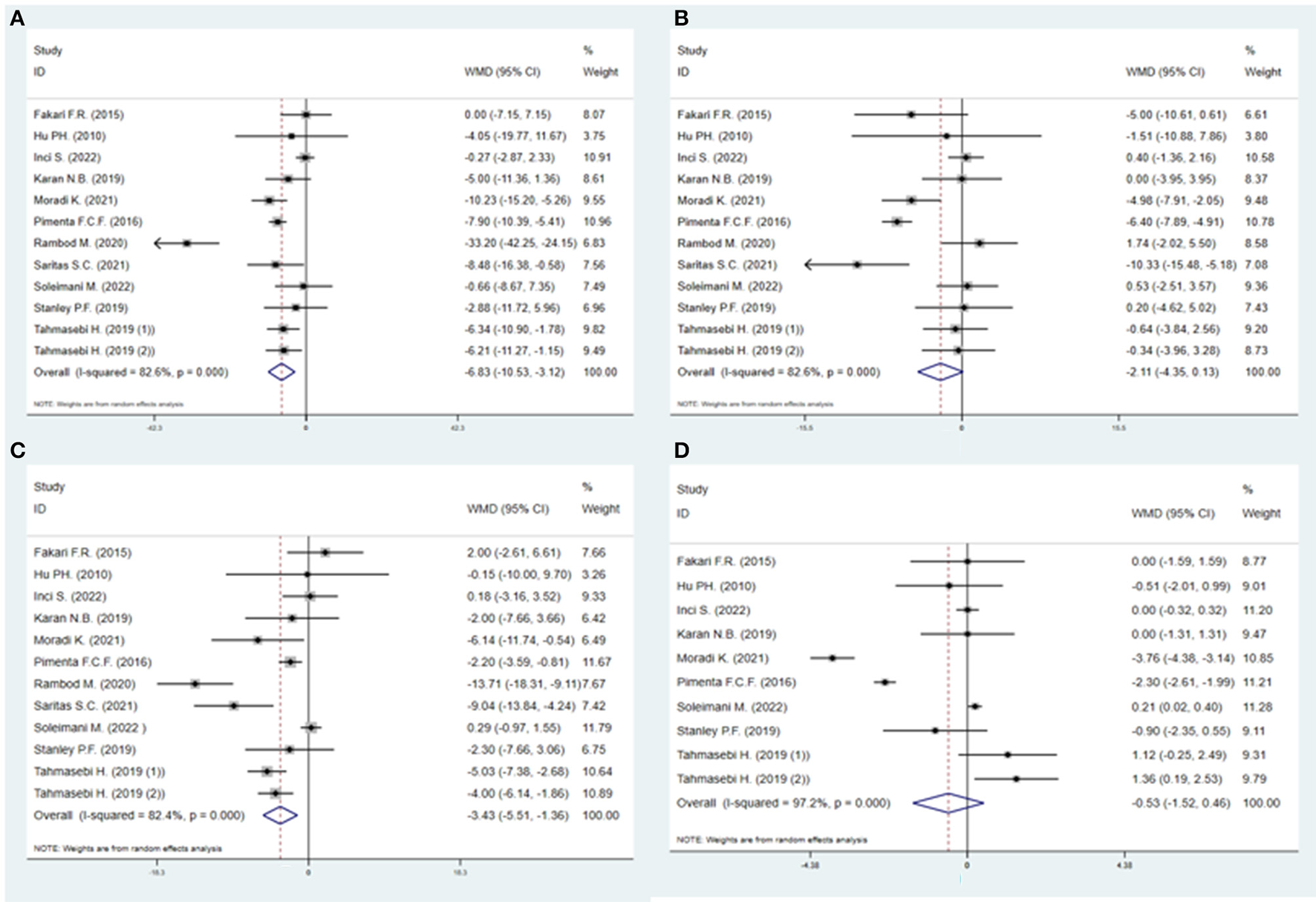
Direct pairwise random-effects meta-analyses of vital signs. (A) Systolic blood pressure (SBP); (B) Diastolic blood pressure (DBP); (C) Heart rate (HR); (D) Respiratory rate (RR).
3.5. Network meta-analysis
3.5.1. Indirect-comparisons meta-analysis for EOs on state anxiety scores
The network consisted of 38 studies with two arms and 6 studies with three arms reporting on 10 different EOs (20 arms on lavender, 11 damask rose, 9 citrus aurantium L., two arms each on lippia alba, mint, and lemon, one arm each on lippia citriodora, geranium, jasmine, and copaiba, and 50 arms were control groups). The network formed by the direct comparisons between different interventions was shown in Figure 7A.
Figure 7
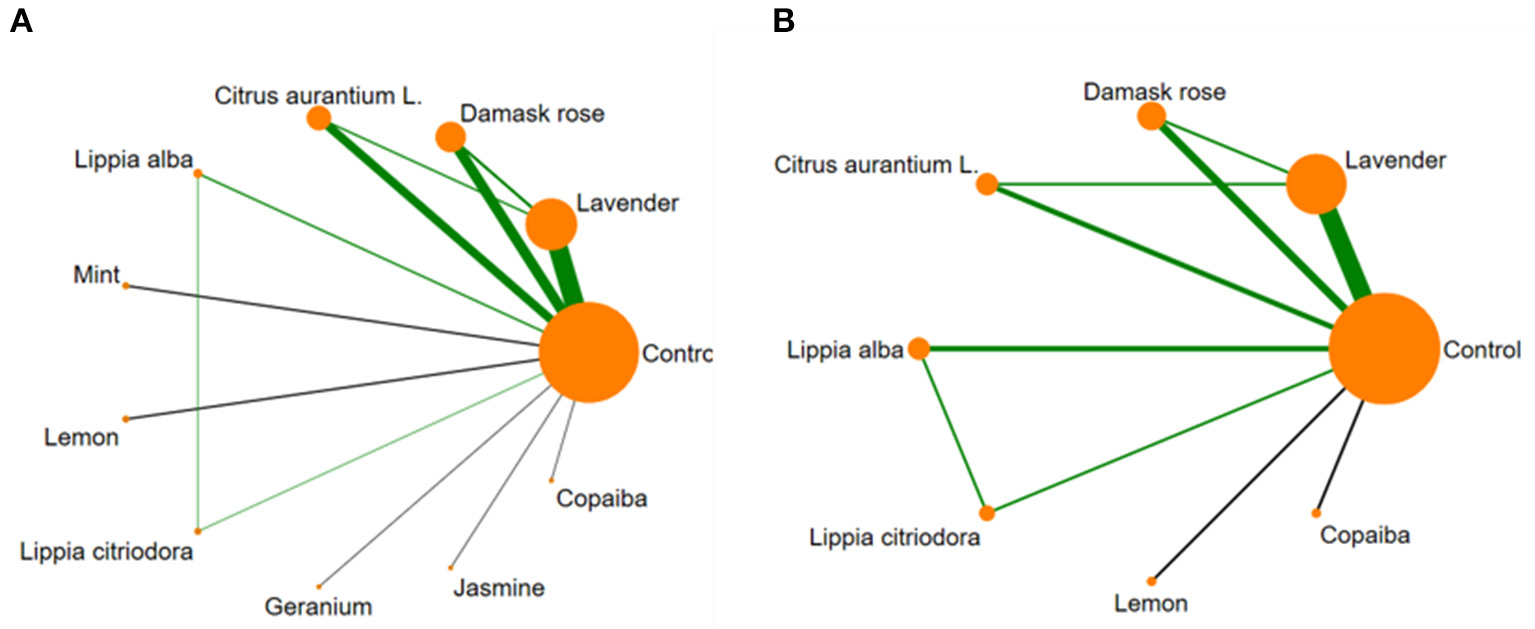
Network meta-analysis of available comparisons between 10 essential oils and the control. (A) State Anxiety Inventory scores (SAIS); (B) Trait Anxiety Inventory scores (TAIS). Line width is proportional to the number of trials that included each pair of treatments (direct comparisons). Circle size is proportional to the total number of participants for each treatment in the network.
Comparing the DIC of the consistency and inconsistency models revealed that the consistency model should be used for the analysis (DICconsistency = 183.12, DICinconsistency = 183.20).
The effect sizes for the differences between all EOs were presented in league table (Table 2). Figure 8A presented the findings of the indirect-comparisons meta-analysis as effect sizes and their 95% CrI for the different types of EOs interventions on SAIS compared with control group. Four (40%) among 10 interventions significantly decreased SAIS compared with the control group. Jasmine was the best ranked intervention with a WMD of−13.61 (95% CrI−24.79, −2.48) for state anxiety. Second only to jasmine is citrus aurantium L., which had an effect size of−9.62 (95% CrI−13.32, −5.93). Moderate effect sizes were observed for damask rose (WMD = −6.78, 95% CrI−10.14, −3.49) and lavender (WMD = −5.41, 95% CrI−7.86, −2.98), compared with the control group. The following interventions had credible intervals including a zero effect, including mint (WMD = −6.16, 95% CrI−14.23, 1.83), lippia alba (WMD = −6.06, 95% CrI−13.98, 1.81), lemon (WMD = −8.22, 95% CrI−19.12, 2.61), lippia citriodora (WMD = −4.9, 95% CrI−15.34, 5.48), and geranium (WMD = −2.86, 95% CrI−14.19, 8.4).
Table 2
| Treatment | Trait anxiety inventory scores | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jasmine | – | – | – | – | – | – | – | – | – | – | ||
| −3.98 (−15.71, 7.71) | Citrus aurantium L. | 6.98 (−0.48, 14.54) | – | 5.24 (−3.36, 13.89) | 4.11 (−2.19, 10.41) | 5.24 (−3.36, 13.89) | 1.13 (−8.93, 11.35) | – | 9.82 (−0.38, 20.18) | 9.62 (3.7, 15.62) | ||
| −6.82 (−18.45, 4.79) | −2.84 (−7.75, 2.13) | Damask rose | – | −1.76 (−9.5, 6.07) | −2.87 (−8.19, 2.36) | −1.76 (−9.5, 6.07) | −5.84 (−15.26, 3.6) | – | 2.84 (−6.72, 12.46) | 2.64 (−2.06, 7.35) | ||
| State anxiety inventory scores | ||||||||||||
| −7.45 (−21.19, 6.22) | −3.46 (−12.28, 5.39) | −0.63 (−9.33, 8.07) | Mint | – | – | – | – | – | – | – | ||
| −7.51 (−21.16, 6.13) | −3.57 (−12.22, 5.14) | −0.71 (−9.28, 7.84) | −0.09 (−11.31, 11.15) | Lippia alba | −1.11 (−8.12, 5.73) | 0.85 (−7.32, 9) | −4.08 (−14.37, 6.2) | – | 4.61 (−5.84, 15.05) | 4.4 (−1.77, 10.54) | ||
| −8.18 (−19.61, 3.18) | −4.22 (−8.43, 0.05) | −1.38 (−5.27, 2.48) | −0.76 (−9.12, 7.64) | −0.64 (−8.94, 7.59) | Lavender | 1.11 (−5.73, 8.12) | −2.97 (−11.68, 5.83) | – | 5.71 (−3.16, 14.7) | 5.5 (2.46, 8.7) | ||
| −8.69 (−24.01, 6.56) | −5.61 (−16.54, 5.23) | −1.88 (−12.82, 9.02) | −1.25 (−14.41, 11.83) | −1.15 (−11.55, 9.2) | −0.51 (−11.18, 10.23) | Lippia citriodora | −4.95 (−16.52, 6.55) | – | 3.73 (−7.89, 15.41) | 3.53 (−4.56, 11.64) | ||
| −5.37 (−20.88, 10.29) | −1.38 (−12.85, 10.07) | 1.45 (−9.94, 12.81) | 2.07 (−11.45, 15.62) | 2.17 (−11.23, 15.56) | 2.83 (−8.34, 13.95) | 3.31 (−11.72, 18.46) | Lemon | – | 8.69 (−2.99, 20.43) | 8.48 (0.33, 16.67) | ||
| −10.76 (−26.63, 5.22) | −6.75 (−18.62, 5.13) | −3.91 (−15.68, 7.85) | −3.31 (−17.14, 10.55) | −3.2 (−17.01, 10.55) | −2.55 (−14.09, 9.05) | −2.06 (−17.39, 13.3) | −5.37 (−21.06, 10.31) | Geranium | – | – | ||
| −13.82 (−29.47, 1.75) | −9.84 (−21.4, 1.7) | −7.01 (−18.42, 4.37) | −6.38 (−19.93, 7.24) | −6.28 (−19.8, 7.24) | −5.63 (−16.84, 5.58) | −5.13 (−20.27, 9.97) | −8.46 (−23.9, 6.97) | −3.08 (−18.85, 12.56) | Copaiba | −0.2 (−8.56, 8.17) | ||
| −13.61 (−24.79, −2.48) | −9.62 (−13.32, −5.93) | −6.78 (−10.14, −3.49) | −6.16 (−14.23, 1.83) | −6.06 (−13.98, 1.81) | −5.41 (−7.86, −2.98) | −4.9 (−15.34, 5.48) | −8.22 (−19.12, 2.61) | −2.86 (−14.19, 8.4) | 0.22 (−10.72, 11.16) | Control | ||
Network meta-analysis diagram of SAIS and TAIS.
SAIS, State Anxiety Inventory scores; TAIS, Trait Anxiety Inventory scores. The orange represents the different types of essential oils. The green represents the effect size of essential oils that significantly decrease SAIS or TAIS.
Figure 8
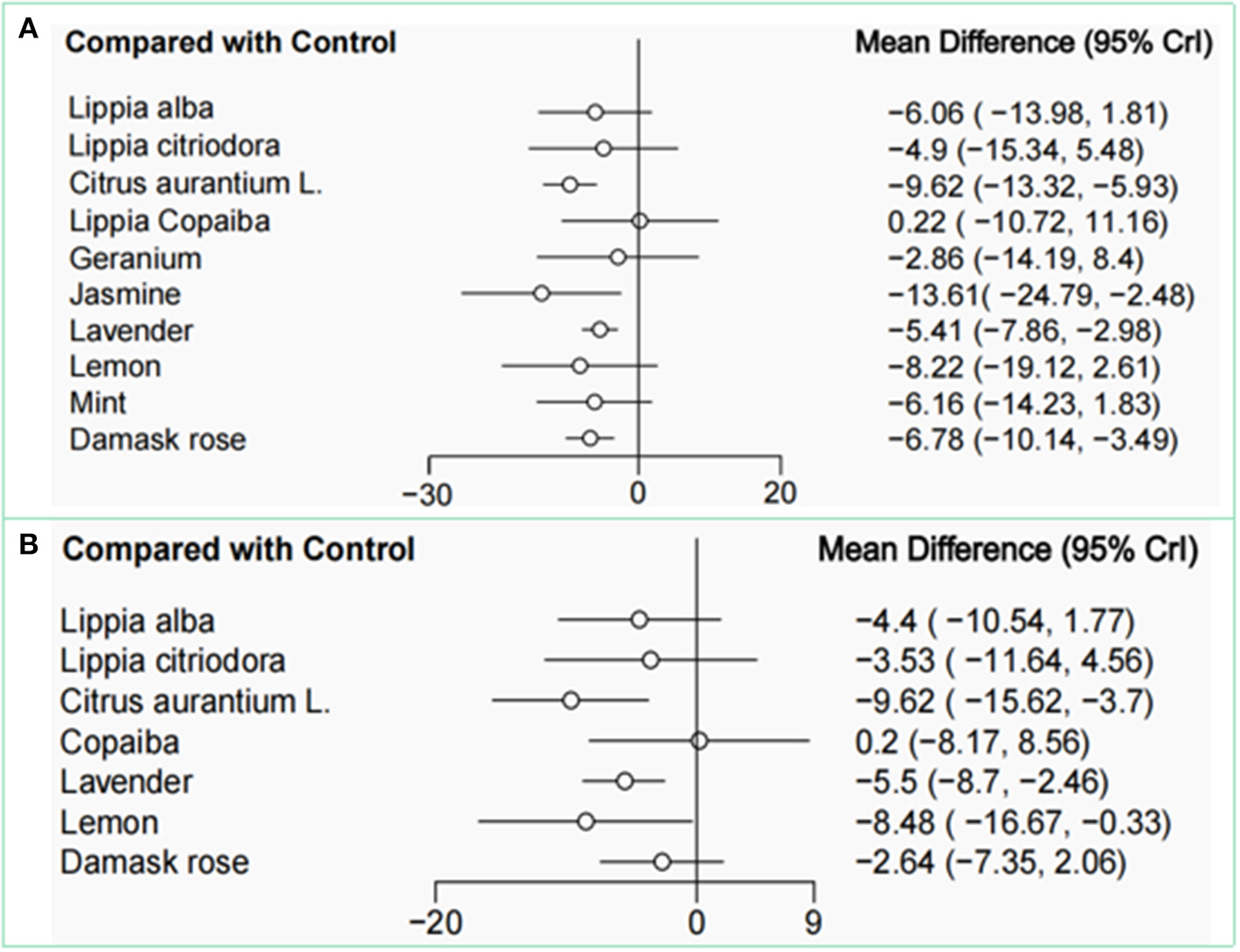
Network meta-analysis for comparisons with the control group of SAIS (A) and TAIS (B). SAIS, State Anxiety Inventory scores; TAIS, Trait Anxiety Inventory scores.
As shown in Table 3, the SUCRA indicated that jasmine was the best ranked intervention with a SUCRA of 88.1. The control intervention had the lowest SUCRA of 11.6 (Figures 9, 10).
Table 3
| Treatment | SUCRA | PrBest | MeanRank |
|---|---|---|---|
| SAIS | |||
| Control | 11.6 | 0 | 9.8 |
| Lavender | 45.4 | 0 | 6.5 |
| Damaskrose | 57.9 | 0.5 | 5.2 |
| CitrusaurantiumL | 79.3 | 8.7 | 3.1 |
| Lippiaalba | 52 | 3.1 | 5.8 |
| Mint | 53.2 | 4.1 | 5.7 |
| Lemon | 64.5 | 15.6 | 4.6 |
| Lippiacitriodora | 45.3 | 4.8 | 6.5 |
| Geranium | 33.9 | 3.2 | 7.6 |
| Jasmine | 88.1 | 59.1 | 2.2 |
| Copaiba | 19 | 0.7 | 9.1 |
| TAIS | |||
| Control | 11.5 | 0 | 7.2 |
| Lavender | 63.8 | 1.5 | 3.5 |
| Damaskrose | 36.3 | 0.1 | 5.5 |
| CitrusaurantiumL | 90.6 | 55.2 | 1.7 |
| Lippia alba | 53.1 | 2.8 | 4.3 |
| Lippia citriodora | 45.3 | 3.8 | 4.8 |
| Lemon | 81.9 | 36.2 | 2.3 |
| Copaiba | 17.4 | 0.4 | 6.8 |
Ranking of values of SUCRA for SAIS and TAIS.
SAIS, State Anxiety Inventory scores; TAIS, Trait Anxiety Inventory scores.
Figure 9
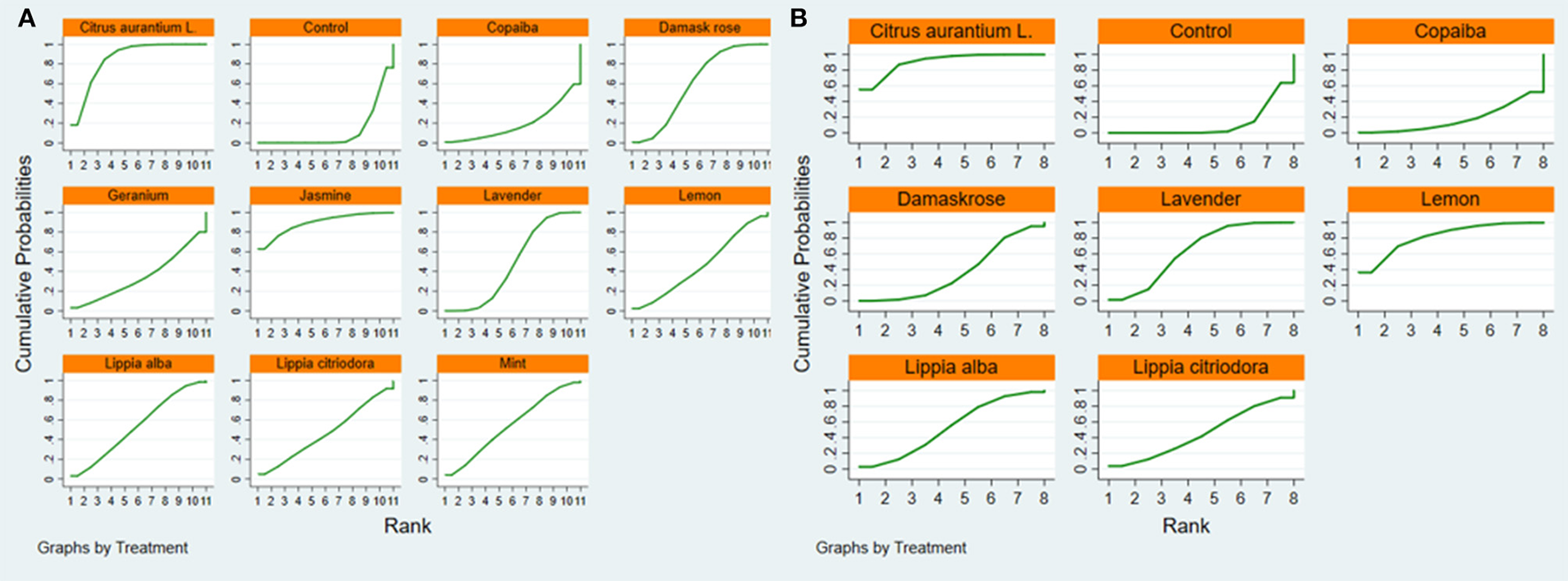
SUCRA figure of SAIS (A) and TAIS (B). Note: SUCRA = surface under the cumulative ranking. SAIS, State Anxiety Inventory scores; TAIS, Trait Anxiety Inventory scores.
Figure 10
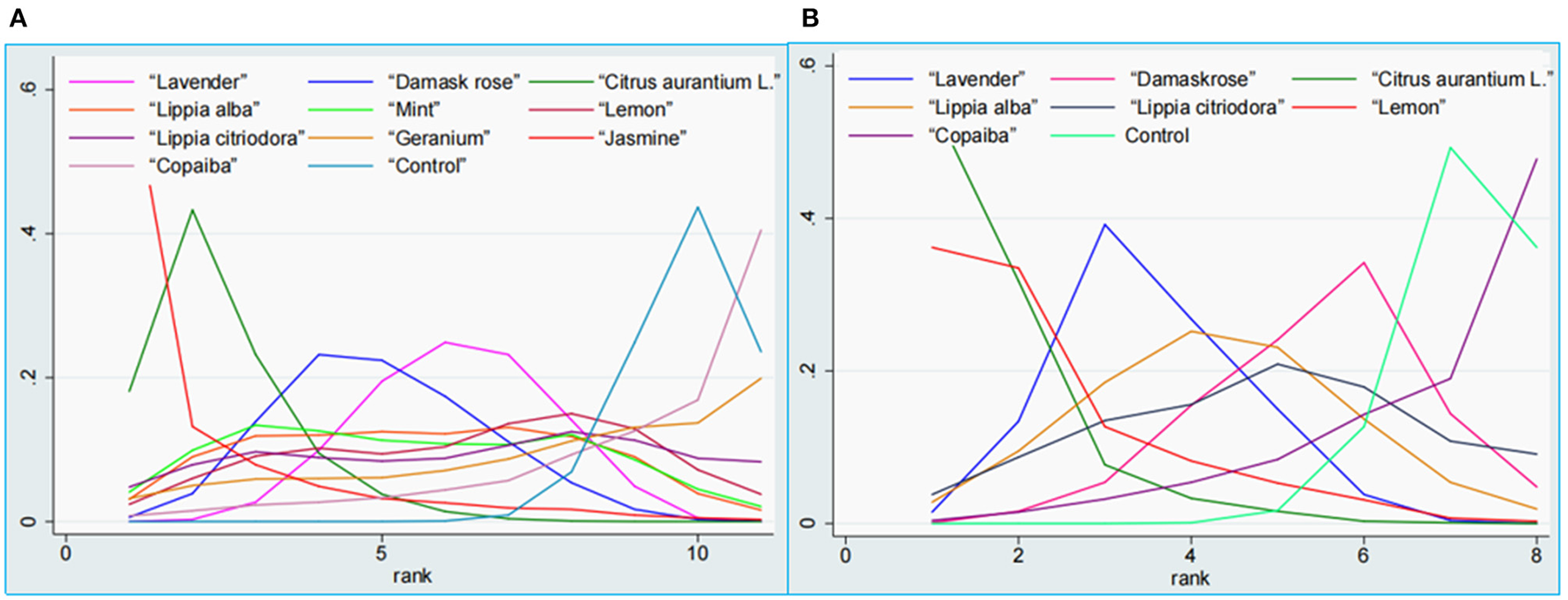
Ranking probability plot of SAIS (A) and TAIS (B). SAIS, State Anxiety Inventory scores; TAIS, Trait Anxiety Inventory scores.
There are 3 loops were formed between the pairwise comparisons, and the loop inconsistency test indicated that there was no significant loop inconsistency (Table 4). The node-splitting model test showed no statistical local inconsistency between direct and indirect comparisons (P > 0.1). However, the overall heterogeneity remained high (93.2%), indicating that inconsistency did not explain the heterogeneity.
Table 4
| Outcomes | Loop | IF | seIF | z-value | p-value | CI_95 | Loop_Heterog_tau2 |
|---|---|---|---|---|---|---|---|
| SAIS | Con-Lav-Dam | 2.14 | 4.02 | 0.79 | 0.43 | (0.00, 10.06) | 20.88 |
| Con-Lav-Cit | 1.33 | 4.15 | 0.32 | 0.75 | (0.00, 9.46) | 31.66 | |
| Con-Alb-Citrio | 0.16 | 2.81 | 0.06 | 0.96 | (0.00, 5.67) | 0.00 | |
| TAIS | Con-Lav-Dam | 4.87 | 4.43 | 1.10 | 0.27 | (0.00, 13.55) | 10.06 |
| Con-Lav-Cit | 4.85 | 5.03 | 0.96 | 0.34 | (0.00, 14.70) | 11.32 | |
| Con-Alb-Citrio | 0.15 | 2.97 | 0.05 | 0.96 | (0.00, 5.96) | 0.00 |
Loop-specific approach.
SAIS, State Anxiety Inventory scores; TAIS, Trait Anxiety Inventory scores; Con, Control; Lav, Lavender; Dam, Damask rose; Cit, Citrus aurantium L.; Alb, Lippia alba; Citrio, Lippia citriodora.
3.5.2. Indirect-comparisons meta-analysis for EOs on trait anxiety scores
This network consisted of 14 RCTs, including 11 studies with two arms and 3 studies with three arms, involving 7 different EOs (7 lavender, 3 damask rose, two arms each on citrus aurantium L. and lippia alba, one arm each on lippia citriodora, lemon, and copaiba, and 17 arms were control groups). The most applied EO was lavender. The network formed by the direct comparisons between different interventions was shown in Figure 7B.
Comparing the DIC for the consistency and inconsistency models revealed that the consistency model was to be preferred (DICconsistency = 60.77, DICinconsistency = 60.84).
The effect sizes for the differences between all EOs on TAIS were presented in league table (Table 2). Figure 8B presented the findings of the indirect-comparisons meta-analysis as effect sizes and their 95% CrI for the different types of EOs interventions on trait anxiety scores (TAS) compared with control group. Three (43%) among 7 interventions significantly decreased TAS compared with the control group. Citrus aurantium L. was the highest ranked intervention with a WMD of −9.62 (95% CrI−15.62, −3.7) for trait anxiety. Moderate-to-large effect sizes were observed for lemon (WMD: −8.48; 95% CrI−16.67, −0.33) and lavender (WMD: −5.5; 95% CrI−8.7, −2.46). The following 4 interventions had credible intervals including a zero effect, including lippia alba (WMD = −4.4, 95% CrI−10.54, 1.77), lippia citriodora (WMD = −3.53, 95% CrI−11.64, 4.56), damask rose (WMD = −2.64, 95% CrI−7.35, 2.06), and copaiba (WMD = 0.2, 95% CrI−8.17, 8.56).
As shown in Table 3, the SUCRA indicated that citrus aurantium L. was the highest ranked intervention with a SUCRA of 90.6. The control intervention had the lowest SUCRA of 11.5 (Figures 9, 10).
There are 3 loops were formed between the pairwise comparisons, and the loop inconsistency test indicated that there was no significant loop inconsistency (Table 4). The node-splitting model test confirmed statistical inconsistency between local direct and indirect comparisons (P < 0.1), suggesting that inconsistency may explain the overall high heterogeneity (I2 = 93.9%).
3.6. Subgroup and meta-regression analysis
Subgroup analyses stratified by type of EOs, country, causes of anxiety, and cumulative duration of intervention were performed (Supplementary Table S5 and Figure S5).
According to the results of subgroups by types of EOs, most EOs could significantly reduce SAIS, TAIS, SBP, DBP, HR or RR. However, citrus aurantium L. had no significant effect on RR [WMD = −1.402 (95% CI−3.066, 0.263), P = 0.099]. Lemon could not significantly reduce SAIS [WMD = −8.24 (95% CI−10.16, −6.32), P = 0.167] and DBP [WMD = 1.740 (95% CI−2.018, 5.498), P = 0.364]. Mint failed to reduce SBP [WMD = −0.660 (95% CI−8.673, 7.353), P = 0.872], DBP [WMD = 0.530 (95% CI−2.513, 3.573), P = 0.733] and HR [WMD = 0.290 (95% CI−0.969, 1.549), P = 0.652]. Lavender failed to reduce DBP [WMD = −1.627 (95% CI−4.655, 1.401), P = 0.292] and RR [WMD = 0.039 (95% CI−0.493, 0.570), P = 0.887], and geranium had no significant improvement on SAIS [WMD = −2.88 (95% CI−6.40, 0.64), P = 0.108], SBP [WMD = 0 (95% CI−7.151, 7.151), P = 1], DBP [WMD = −5 (95% CI−10.614, 0.6144), P = 0.081] and HR [WMD = 2.000 (95% CI−2.605, 6.605), P = 0.395]. Copaiba had the weakest efficacy and could not reduce SAIS [WMD = 0.20 (95% CI−2.09, 2.49), P = 0.864] and TAIS [WMD = 0.20 (95% CI−2.09, 2.49), P = 0.395].
With respect to the country, studies from Iran, Peru, and Turkey found that EOs could significantly reduce SAIS and TAIS. Studies in Brazil and Philippines have only reported that EOs reduced SAIS. However, Turkish studies concluded that EOs had no significant effect on SBP [WMD = −3.527 (95% CI−8.479, 1.425), P = 0.163] and HR [WMD = −3.498 (95% CI−9.246, 2.251), P = 0.233]. According to the studies of Singapore, EOs could not reduce SAIS [WMD = −3.7 (95% CI−8.465, 1.065), P = 0.128], SBP [WMD = −2.880 (95% CI−11.724, 5.964), P = 0.523] and HR [WMD = −2.3 (95% CI−7.664, 3.064), P = 0.401], and the Chinese study believed that EOs could not reduce SAIS [WMD = −0.033 (95% CI−1.512, 1.445), P = 0.965], TAIS [WMD = 0.2 (95% CI−2.090, 2.490), P = 0.864], SBP [WMD = −4.050 (95% CI−19.770, 11.670), P = 0.614] and HR [WMD = −0.150 (95% CI−9.996, 9.696), P = 0.976]. Interestingly, only the Brazilian study concluded that EOs significantly reduced DBP [WMD = −6.4 (95% CI−7.886, −4.914), P < 0.001] and RR [WMD = −2.3 (95% CI−2.605, −1.995), P < 0.001], while other countries found that EOs had no obvious improvement in them.
In causes of anxiety respect, our results showed that EOs could not reduce SAIS in patients with burn-related anxiety [WMD = −15.13 (95% CI−20.354, −9.906), P = 0.481] and TAIS in menopause-related anxiety [WMD = −0.650 (95% CI−2.849, 1.549), P = 0.562]. EOs were poorly efficacious in delivery-related anxiety, failing to reduce TAIS, SBP, DBP, HR, and RR. Similarly, EOs had no significant effect on TAIS [WMD = −3.250 (95% CI−12.315, 5.815), P = 0.482], DBP [WMD = −2.745 (95% CI−5.952, 0.462), P = 0.093], and RR [WMD = −0.362 (95% CI−2.698, 1.974), P = 0.761] in patients with invasive examination-related anxiety. EOs could not improve the physiological parameters of operation-related anxiety, including SBP [WMD = −4.256 (95% CI−9.159, 0.648), P = 0.089], DBP [WMD = −0.072 (95% CI−2.977, 2.832), P = 0.961], HR [WMD = −1.887 (95% CI−5.508, 1.735), P = 0.307], and RR [WMD = −0.434 (95% CI−1.249, 0.381), P = 0.296]. Additionally, EOs did not have apparent effects on SBP [WMD = −16.859 (95% CI−48.747, 15.029), P = 0.3], DBP [WMD = 1.009 (95% CI−1.356, 3.374), P = 0.403], and HR [WMD = −6.528 (95% CI−20.243, 7.187), P = 0.351] in cardiovascular disease-induced anxiety.
Regarding the cumulative duration of intervention, we found that the general efficacy of EOs for anxiety was optimal when the cumulative duration of intervention was 10~30 min, which could not only effectively reduce SAIS [WMD = −5.815 (95% CI−7.779, −3.851), P < 0.001] and TAIS [WMD = −4.935 (95% CI−7.882, −1.989), P < 0.001], but also stabilize vital signs, including lowering SBP [WMD = −5.372 (95% CI−8.484, −2.259), P = 0.001], DBP [WMD = −3.235 (95% CI−6.002, −0.467), P = 0.022], and HR [WMD = −3.184 (95% CI−5.050, −1.318), P = 0.001]. In fact, EOs reduced SAIS regardless of the duration of the intervention, as evidenced by further meta-regression analysis (P > 0.05). However, EOs had no significant effect on SBP, DBP, and HR when the cumulative duration of intervention was < 10 min or maintained at 30~100 min, and had no improvement on TAIS when it was >500 min [WMD = −4.625 (95% CI−12.307, 3.057), P = 0.238]. Meta-regression analysis confirmed that the effect size of EOs in lowering DBP was significantly negatively correlated with the intervention time when it was within 30 min (regression = −2.70, P = 0.027). Additionally, the effect size of EOs in lowering SBP and HR also showed a negative trend with the intervention time when it was controlled within 30 min, but it was not statistically significant (P > 0.05) (Table 5).
Table 5
| Effect size | Coef. | Std. Err. | t | P>|t| | 95% CI | tau2 | Adj R-squared (%) |
|---|---|---|---|---|---|---|---|
| SAIS | −0.003 | 0.002 | −1.42 | 0.163 | −0.007~0.001 | 25.34 | 1.68 |
| TAIS | −0.001 | 0.002 | −0.58 | 0.571 | −0.005~0.003 | 15.01 | −4.82 |
| SBP | −0.178 | 0.162 | −1.10 | 0.304 | −0.550~0.195 | 7.131 | 13.88 |
| DBP | −0.296 | 0.110 | −2.70 | 0.027 | −0.549~-0.043 | 3.789 | 58.81 |
| HR | −0.137 | 0.131 | −1.05 | 0.326 | −0.439~0.165 | 5.275 | −15.56 |
Meta-regression of weighted mean difference according to cumulative duration of intervention.
SAIS, State Anxiety Inventory scores; TAIS, Trait Anxiety Inventory scores; SBP, systolic blood pressure; DBP, diastolic blood pressure; HR, heart rate.
3.7. Sensitivity analysis
In the sensitivity analyses to test the effect of smaller sample sizes on the overall weighted mean in the “State Anxiety Inventory” studies, the effect sizes of most comparisons were decreased. The overall effect size for EO interventions on SAIS was reduced from −6.63 to −0.84 when excluding smaller studies, although none of the confidence intervals included the zero effect. Additionally, the exclusion of small studies did not generate a reduction in heterogeneity (Supplementary Figure S6A).
Interestingly, in the sensitivity analyses to test the effect of smaller sample sizes on the overall weighted mean, studies using the Trait Anxiety Inventory as an evaluator showed the same effect size trends as the State Anxiety Inventory. The overall effect size for EO interventions on TAIS was reduced from −4.97 to −1.51 when excluding smaller studies, and none of their credible intervals included the zero effect. The exclusion of small studies did not decrease the heterogeneity (Supplementary Figure S6B).
3.8. Publication bias
Supplementary Figure S7 presented the funnel plot of the publication bias. The distribution of most dots in the figure was relatively symmetrical and uniform, indicating little evidence of publication bias. However, there are some dots distributed outside of the 95% CI, suggesting the effect of small sample size may exist.
3.9. Certainty of evidence
CINeMA application was used to conduct GRADE judgments. The therapeutic effect of EO on anxiety was measured by SAI inventory, twenty-six of comparisons were judged to be low rating, with twenty-nine very low comparisons while measured by TAI inventory, eighteen of comparisons were judged as low rating, with ten very low comparisons (Supplementary Tables S3.1, S3.2).
4. Discussion
4.1. Main study findings
To the best of our knowledge, this was the first study about different EOs for treating anxiety using Bayesian network meta-analysis. Anxiety was assessed with the Spielberger State-Trait Anxiety Inventory (STAI), which is currently the most extensively used inventory for evaluating anxiety levels and consists of two parts, SAI and TAI. The changes of SAIS and TAIS were used as the primary outcomes to evaluate the therapeutic effects of EOs on anxiety in this study. Pairwise meta-analyses indicated that EOs could effectively reduce SAIS and TAIS. Further network meta-analyses showed that jasmine was the most effective EO in reducing SAIS, followed by citrus aurantium L., which ranked first in reducing TAIS.
Vital signs are considered to be important physiological indicators of anxiety indirectly (13). Emotional signals of anxiety are sent from the amygdala and hippocampus of the limbic system to the hypothalamus, activating the hypothalamic-pituitary-adrenocortical (HPA) axis (61). Moreover, anxiety could cause increased sympathetic excitability, which leads to increased blood pressure, HR and RR. Herein, vital signs may be helpful in objective assessment of anxiety. Our results found that EOs dramatically reduced SBP and HR, and had a tendency to lower DBP and RR, but were not statistical significance.
4.2. Possible explanation for study findings
Our findings were consistent with previous conventional meta-analyses focusing on EOs for anxiety. Indicating that EOs significantly alleviate anxiety (62, 63). Additionally, our results further confirmed the results of a previous meta-analysis pooling animal experiments from a clinical perspective (64).
Pairwise meta-analyses suggested that EOs had a stronger total therapeutic effect on state anxiety than trait anxiety. This was consistent with the results of an earlier meta-analysis (65). Moreover, we further found that EOs were effective in reducing state anxiety regardless of the cumulative duration of the intervention. However, EOs could not alleviate trait anxiety when the cumulative intervention time exceeded 500 min, with the largest effect size within 10 min of the intervention time. Thus, the efficacy of EOs on trait anxiety was more inclined to immediate intervention. The reason for these results may be related to the mechanisms of state anxiety and trait anxiety. Previous study has shown that state anxiety and trait anxiety are mapped differently in the brain (66). State anxiety is a transient intense emotional state associated with a temporary increase in sympathetic nervous system activity without a specific pathological condition, and it can disappear with the removal of stress or danger (66). Trait anxiety is a personality tendency that remains stable over time (67). It may be associated with different psychopathological conditions and continuous high arousal. It does not disappear easily when the stress is relieved, and people with high trait anxiety are easy to develop anxiety disorders (68). Therefore, EOs have a more obvious therapeutic effect on state anxiety. Trait anxiety symptoms could restore to their stable personality characteristics soon, although a short period of EOs stimulation can effectively alleviate them.
Network meta-analyses suggested that that jasmine was the strongest type of EO for reducing SAIS. Contrary to previous studies that suggested that jasmine could only improve nervousness and not reduce symptoms of anxiety and stress (58), our study found that jasmine significantly improved state anxiety symptoms and thus reduced SAIS. Pharmacological studies suggested that the mechanisms by which jasmine reduced SAIS may be related to the increase of β wave in the frontal cortex center and left occipital cortex caused by olfactory stimulation (69). However, only one study explored the efficacy of jasmine on anxiety, so the credibility of this result is low and more researches are indispensable to confirm this result.
Considering that there was only one RCT reporting jasmine for anxiety, the results may be highly biased and less credible. Citrus aurantium L. (85.6%) and jasmine (89.3%) had similar efficacy in reducing SAIS according to SUCRA values, and citrus aurantium L. ranked first in reducing TAIS. Furthermore, citrus aurantium L. could dramatically reduce the objective indicators reflecting anxiety, including SBP, DBP, and HR. The anxiolytic activity of citrus aurantium L. was mediated by the serotonergic system (5-HT1A receptor) (7, 70). Interestingly, citrus aurantium L. significantly ameliorated anxiety and did not interfere with physiological levels of melatonin and corticosterone (71). Thus, it could be reasonably inferred that citrus aurantium L. EO has the greatest benefits in treating anxiety.
Previous studies on the treatment of anxiety with lemon EO are still somewhat controversial. An RCT investigating the effect of lemon EO on anxiety during the active phase in primiparas showed that lemon EO had no effect on anxiety (72). However, another multicenter, assessor-blinded trial demonstrated the efficacy of aromatherapy with lemon EO inhalation in relieving anxiety (43). To the best of our knowledge, this study was the first meta-analysis of lemon EO for anxiety. Our paired meta-analysis confirmed that lemon EO significantly ameliorated trait anxiety, but did not alleviate state anxiety. Further, our network meta-analysis found that lemon ranked second among all EOs in the aspect of reducing TAIS. The main component of lemon is s-limonene. The anti-trait anxiety effect of lemon is closely related to the 5-serotonergic pathway, particularly through the 5-HT (1A) receptor. In addition, lemon significantly accelerated the metabolic turnover of dopamine (DA) in the hippocampus and 5-HT in the prefrontal cortex and striatum (69).
Current network meta-analyses also found that damask rose was the third most anti-anxiety EO after jasmine and citrus aurantium L. in reducing SAIS. However, damask rose could not reduce TAIS. This finding was in line with a previous meta-analysis that pooled the studies about damask rose mill on anxiety, indicating that damask rose dramatically decreased state anxiety but had no obvious effect on trait anxiety (73). Damask rose mainly contains isoflavones. On one hand, isoflavones can directly bind to GABA receptors to reduce anxiety (74). On the other hand, isoflavones inhibit inducible nitric oxide synthase (iNOS) and then reduce the production of nitric oxide, which regulates the concentration of neurotransmitters such as serotonin, dopamine, norepinephrine and glutamate, and inhibits the activation of soluble guanylate cyclase, which in turn reduces the production of cyclic guanosine monophosphate (cGMP), thereby reducing anxiety (75).
The number of studies using lavender as an intervention were the largest for both state anxiety and trait anxiety. Our results indicated that the efficacy of lavender in reducing SAIS and TAIS was comparable. This was consecutive with the results of previous meta-analyses (12, 13). Researches in pharmacology have found that the anxiolytic effects of lavender are related to the interaction of its monoterpene components such as linalool and linalyl acetate with NMDA receptors. Additionally, the anxiolytic effect could be partially attributed to its inhibition of serotonin transporter (SERT) and protection of SH-SY5Y cells from hydrogen peroxide-induced neurotoxicity (76).
Results of an RCT using mint intervention in emergency cardiac patients found that mint reduced anxiety and its induced increase in respiratory rate. In keeping with this, our study indicated that mint could significantly reduce SAIS. Mint affects the hypothalamus by stimulating the olfactory pathway, which reduces the secretion of adrenocorticotropin-releasing hormone, adrenocorticotropin and cortisol, ultimately reducing anxiety (77, 78).
Finally, the results of our study showed that neither geranium nor copaiba could reduce anxiety, and copaiba ranked the worst. However, the RCTs on geranium and copaiba for anxiety each only one was included, which tends to cause significant heterogeneity, so these results should be interpreted with caution and more studies are needed to confirm these conclusions in the future.
No adverse events were reported in any of the trials, and their safety remains uncertain. EOs gas molecules can be inhaled and then transported to the central nervous system after entering the bloodstream through the lung, or they can cross the neuronal network of the olfactory system and directly reach and act on the corresponding brain areas, causing activation in different brain regions to induce anxiolytic effects (8). Several studies concluded that EOs appeared to be well tolerated, as inhalation of different doses of EOs did not cause changes or show signs of toxicity (48).
In summary, the most effective was jasmine intervention with a cumulative duration of 30 to 100 min for state anxiety, while citrus aurantium L. intervention with a cumulative duration of 10 min or less were most efficacious for trait anxiety. Nevertheless, combining self-reported SAIS and TAIS with objective indicators, a cumulative intervention of 10 to 30 min with citrus aurantium L. was optimal, because it reduced not only SAIS and TAIS, but also SBP, DBP, and HR. However, it is worth noting that due to the lack of reports on adverse effects, the studies with EOs included in this study could not be fully used to rank the safety of EOs. This limitation requires special attention in future studies.
4.3. Strength and limitations
The current study has several strengths. We developed rigorous eligibility criteria, conducted a comprehensive search, assessed the risk of bias, addressed key outcomes, performed valuable sensitivity and subgroup analyses, and rated the certainty of the evidence using CINeMA by GRADE criteria. For the first time, a network meta-analysis was used to compare the differences in efficacy of various types of commonly used EOs, providing clinicians with a rational choice of essential oils for the treatment of anxiety.
However, the study also had a number of limitations. To comprehensively summarize the efficacy of EOs, we included a wide range of interventions that varied in terms of number of interventions, duration, dose, co-morbidities, or causes of anxiety, so that there may be large heterogeneity across trials. Moreover, most of the trials had a high risk of bias and low or very low quality of evidence. Therefore, the credibility of the results was low and we need to be cautious in interpreting the results. In addition, the intrinsic characteristics of EOs, such as the species, place of origin, and the intervention procedures of EOs, including extraction method, exposure concentration, method of exposure, duration of exposure, and route of administration, could affect the amount of active ingredients of EOs in the body and thus the efficacy of EOs. Thus, only by controlling for these variables can the efficacy of EOs for anxiety in different clinical trials be more accurately determined. What's more, more high-quality RCTs that rigorously document the characteristics and intervention procedures of EO, may be needed in the future to improve the reliability of meta-analysis conclusions.
5. Conclusion
This study confirmed that EOs may be effective in treating anxiety, and citrus aurantium L. appeared to be the most recommended type, as it showed a large effect size in reducing both SAIS and TAIS. However, due to the obvious heterogeneity among the included studies, our results should be interpreted with caution and more high-quality RCTs are expected to confirm this result in the future.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LT and F-fL: conceptualization, visualization, investigation, and writing-original draft. L-zL and C-gF: conceptualization, visualization, and writing – review and editing. X-cM: investigation and writing – review and editing. Y-xP: formal analysis and writing – review and editing. J-mL and HQ: funding acquisition and writing – review and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Youth Talent Promotion Project of China Association for Science and Technology (no. 2020-QNRCI-02) and the Science and Technology Innovation Project of China Academy of Chinese Medical Sciences (no. CI2021A05013).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1144404/full#supplementary-material
References
1.
KrauseKRChungSAdewuyaAOAlbanoAMBabins-WagnerRBirkinshawLet al. International consensus on a standard set of outcome measures for child and youth anxiety, depression, obsessive-compulsive disorder, and post-traumatic stress disorder. Lancet Psychiatry. (2021) 8:76–86. 10.1016/S2215-0366(20)30356-4
2.
TwengeJMJoinerTEUS. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. (2020) 37:954–6. 10.1002/da.23077
3.
SantomauroDFHerreraAMShadidJZhengPAshbaughCPigottDM. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. 10.1016/S0140-6736(21)02143-7
4.
AltmannHStahlSTGebaraMALenzeEJMulsantBHBlumbergerDMet al. Coprescribed Benzodiazepines in Older Adults Receiving Antidepressants for Anxiety and Depressive Disorders: Association With Treatment Outcomes. J Clin Psychiatry. (2020) 81:823. 10.4088/JCP.20m13283
5.
MalcolmBJTallianK. Essential oil of lavender in anxiety disorders: Ready for prime time?Ment Health Clin. (2017) 7:147–55. 10.9740/mhc.2017.07.147
6.
CuiJLiMWeiYLiHHeXYangQet al. Inhalation aromatherapy via brain-targeted nasal delivery: natural volatiles or essential oils on mood disorders. Front. Pharmacol. (2022) 13:860043. 10.3389/fphar.2022.860043
7.
WangZJHeinbockelT. Essential oils and their constituents targeting the gabaergic system and sodium channels as treatment of neurological diseases. Molecules. (2018) 23:1061. 10.3390/molecules23051061
8.
ZhangNYaoL. Anxiolytic effect of essential oils and their constituents: a review. J Agric Food Chem. (2019) 67:13790–808. 10.1021/acs.jafc.9b00433
9.
Lizarraga-ValderramaLR. Effects of essential oils on central nervous system: focus on mental health. Phytother Res. (2021) 35:657–79. 10.1002/ptr.6854
10.
ChungYHChenSJLeeCLWuCWChangYS. Relaxing Effects of Breathing Pseudotsuga menziesii and Lavandula angustifolia Essential Oils on psychophysiological status in older adults. Int. J. Environ. Res. Public Health. (2022) 19:251. 10.3390/ijerph192215251
11.
YvonYRaoelisonEGRazafindrazakaRRandriantsoaARomdhaneMChabirNet al. Relation between chemical composition or antioxidant activity and antihypertensive activity for six essential oils. J Food Sci. (2012) 77:H184–91. 10.1111/j.1750-3841.2012.02812.x
12.
DonelliDAntonelliMBellinazziCGensiniGFFirenzuoliF. Effects of lavender on anxiety: a systematic review and meta-analysis. Phytomedicine. (2019) 65:153099. 10.1016/j.phymed.2019.153099
13.
KimMNamESLeeYKangHJ. Effects of lavender on anxiety, depression, and physiological parameters: systematic review and meta-analysis. Asian Nurs Res. (2021) 15:279–90. 10.1016/j.anr.2021.11.001
14.
AbbasijahromiAHojatiHNikooeiSJahromiHKDowlatkhahHRZareanVet al. Compare the effect of aromatherapy using lavender and Damask rose essential oils on the level of anxiety and severity of pain following C-section: A double-blinded randomized clinical trial. J Complement Integr Med. (2020) 17. 10.1515/jcim-2019-0141
15.
PageMJMcKenzieJEBossuytPMBoutronIHoffmannTCMulrowCDet al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. 10.1136/bmj.n71
16.
SterneJACSavovićJPageMJElbersRGBlencoweNSBoutronIet al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. 10.1136/bmj.l4898
17.
NikolakopoulouAHigginsJPTPapakonstantinouTChaimaniADel GiovaneCEggerMet al. CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. (2020) 17:e1003082. 10.1371/journal.pmed.1003082
18.
Alvarado-GarcíaPAASoto-VásquezMRRosales-CerquinLEJara-AguilarDRBenitesSM. Anxiolytic-like effect of luma chequen essential oil: a pilot study. Phcog J. (2021) 13:1607–13. 10.5530/pj.2021.13.207
19.
AmzajerdiAKeshavarzMMontazeriABekhradiR. Effect of mint aroma on nausea, vomiting and anxiety in pregnant women. J Family Med Prim Care. (2019) 8:2597–601. 10.4103/jfmpc.jfmpc_480_19
20.
Babatabar DarziHVahedian-AzimiAGhasemiSEbadiASathyapalanTSahebkarA. The effect of aromatherapy with rose and lavender on anxiety, surgical site pain, and extubation time after open-heart surgery: A double-center randomized controlled trial. Phytother Res. (2020) 34:2675–84. 10.1002/ptr.6698
21.
BahadoriHAmiriMHSharafiHEntezariA. The effect of aromatherapy with damask rose on anxiety, accuracy and job stress in operating room nurses. J. evid. based med. healthc. (2022) 12:56–62. 10.22038/EBCJ.2022.64364.2670
22.
BakhshaFMazandaraniMAryaeiMJafariSYBayateH. Phytochemical and anti-oxidant activity of Lavandula Angustifolia mill. Essential oil on preoperative anxiety in patients undergoing diagnostic curettage. Int J Womens Health Reprod Sci. (2014) 2:268–71. 10.15296/ijwhr.2014.42
23.
BeylikliogluAArslanS. Effect of lavender oil on the anxiety of patients before breast surgery. J PeriAnesthesia Nurs. (2019) 34:587–93. 10.1016/j.jopan.2018.10.002
24.
EslamiJEbrahimiADarvishiIMomeniKAkbarzadehM. Relaxation effects of aromatherapy intervention on female and male anxiety: a randomized control trial. Shiraz E Medical J. (2021) 22:822. 10.5812/semj.110822
25.
EslamiJEbrahimiAHosseinkhaniAKhazaeiZDarvishiI. The effect of aromatherapy using Lavender (Lavandula angustifolia Miller) and Citrus aurantium L. extracts to treat anxiety of patients undergoing laparoscopic cholecystectomy: a randomized clinical trial in Iran. Biomed Res Ther. (2018) 5:2096–110. 10.15419/bmrat.v5i3.423
26.
FarzanehMZareanVAbbasijahromiAMohitMAmirkhaniMBadiyepeymaiejahromiZet al. A randomized controlled trial examining the effect of aromatherapy using the damask rose essential oil on pre-operative anxiety levels. Nephrourol Mon. (2022) 14:116696. 10.5812/numonthly.116696
27.
FayaziSBabashahiMRezaeiM. The effect of inhalation aromatherapy on anxiety level of the patients in preoperative period. Iran J Nurs Midwifery Res. (2011) 16:278–83.
28.
Rohi GanjiMJafariFRezaeianSAbdiHFarzaeiMHKhatonyA. The effect of inhalation aromatherapy and music therapy on anxiety in patients undergoing shockwave lithotripsy: a randomized controlled clinical trial. Evid.-based Complement Altern. Med. (2022) 2022:1–18. 10.1155/2022/8015798
29.
HaddadiMRobat SarpooshiHJaghouriEDehnabiA. The effect of aromatherapy with rose essential oil on apparent anxiety in patients with myocardial infarction. J Complement Integr Med. (2022) 19:1007–12. 10.1515/jcim-2021-0126
30.
HamdamianSNazarpourSSimbarMHajianSMojabFTalebiA. Effects of aromatherapy with Rosa damascena on nulliparous women's pain and anxiety of labor during first stage of labor. J Integr Med. (2018) 16:120–5. 10.1016/j.joim.2018.02.005
31.
HekmatpouDPourandishYFarahaniPVParvizradR. The effect of aromatherapy with orange essential oil on anxiety and pain in patients with fractured limbs admitted to an emergency ward: a randomized clinical trial. Cent. Eur. J. Nurs. Midwifery. (2017) 8:717–22. 10.15452/CEJNM.2017.08.0024
32.
HuPHPengYCLinYTChangCSOuMC. Aromatherapy for reducing colonoscopy related procedural anxiety and physiological parameters: a randomized controlled study. Hepatogastroenterology. (2010) 57:1082–6.
33.
JirdehiMMMonfaredAGhanaeiFMLeyliEK. Effect of aromatherapy with lavender and damask rose extracts on anxiety in endoscopy patients: a randomised trial. Gastrointest Nurs. (2022) 20:S24–31. 10.12968/gasn.2022.20.Sup8.S24
34.
JodakiKAbdiKMousaviMSMokhtariRAsayeshHVandaliVet al. Effect of rosa damascene aromatherapy on anxiety and sleep quality in cardiac patients: a randomized controlled trial. Complement Ther Clin Pract. (2021) 42:101299. 10.1016/j.ctcp.2020.101299
35.
JokarMDelamHBakhtiariSPakiSAskariABazrafshanMRet al. The Effects of inhalation lavender aromatherapy on postmenopausal women's depression and anxiety: a randomized clinical trial. JNP-J Nurse Pract. (2020) 16:617–22. 10.1016/j.nurpra.2020.04.027
36.
KasarKSYildirimYSenuzun AykarFUyarMSaginFGAtayS. Effect of inhalation aromatherapy on pain, anxiety, comfort, and cortisol levels during trigger point injection. Holist Nurs Pract. (2020) 34:57–64. 10.1097/HNP.0000000000000350
37.
MokhtariRAjorpazNMabdiKGolitalebM. The effects of Rosa damascene aromatherapy on anxiety and sleep quality in burn patients: a randomized clinical trial. Burns. (2022) 4:17. 10.1016/j.burns.2022.07.017
38.
MoradiKAshtarianHDanzimaNYSaeediHBijanBAkbariFet al. Essential oil from citrus aurantium alleviates anxiety of patients undergoing coronary angiography: a single-blind, randomized controlled trial. Chin J Integr Med. (2021) 27:177–82. 10.1007/s11655-020-3266-5
39.
MoslemiFAlijanihaFNaseriMKazemnejadACharkhkarMHeidariMR. Citrus aurantium aroma for anxiety in patients with acute coronary syndrome: a double-blind placebo-controlled trial. J Altern Complement Med. (2019) 25:833–9. 10.1089/acm.2019.0061
40.
ÖzkaramanADügümÖYilmazHÖYeşilbalkanÖU. Aromatherapy: The effect of lavender on anxiety and sleep quality in patients treated with chemotherapy. Clin J Oncol Nurs. (2018) 22:203–10. 10.1188/18.CJON.203-210
41.
PasyarNRambodMAraghiF. The effect of bergamot orange essence on anxiety, salivary cortisol, and alpha amylase in patients prior to laparoscopic cholecystectomy: A controlled trial study. Complement Ther Clin Pract. (2020) 39:101153. 10.1016/j.ctcp.2020.101153
42.
PimentaFCFAlvesMFPimentaMBFMeloSALde AlmeidaAAFLeiteJRet al. Anxiolytic Effect of Citrus aurantium L. on Patients with Chronic Myeloid Leukemia Phytother Res. (2016) 30:613–7. 10.1002/ptr.5566
43.
RambodMRakhshanMTohidinikSNikooMH. The effect of lemon inhalation aromatherapy on blood pressure, electrocardiogram changes, and anxiety in acute myocardial infarction patients: a clinical, multi-centered, assessor-blinded trial design. Complement Ther Clin Pract. (2020) 39:101155. 10.1016/j.ctcp.2020.101155
44.
ReyesMCGMReyesMCGMRibayKGLParagasED. Effects of sweet orange aromatherapy on pain and anxiety during needle insertion among patients undergoing hemodialysis: A quasi-experimental study. Nurs Forum. (2020) 55:425–32. 10.1111/nuf.12447
45.
SahinSTokgözBDemirG. Effect of lavender aromatherapy on arteriovenous fistula puncture pain and the level of state and trait anxiety in hemodialysis patients: a randomized controlled trial. Pain Manag Nurs. (2021) 22:509–15. 10.1016/j.pmn.2021.01.009
46.
SaritasSCBuyukbayramZSerinEKBilgicY. Effects of lavender oil intervention before endoscopic retrograde cholangiopancreatography on patients' vital signs, pain and anxiety: A randomized controlled study. Explore-J Sci Heal. (2021) 17:446–50. 10.1016/j.explore.2020.07.011
47.
ShirzadMNasiriEHesamirostamiMAkbariH. The effect of lavender on anxiety and hemodynamic status before septorhinoplasy and rhinoplasty. J PeriAnesthesia Nurs. (2022). 10.1016/j.jopan.2022.05.067
48.
SoleimaniMKashfiLSMirmohamadkhaniMGhodsAA. The effect of aromatherapy with peppermint essential oil on anxiety of cardiac patients in emergency department: a placebo-controlled study. Complement Ther Clin Pract. (2022) 46:101533. 10.1016/j.ctcp.2022.101533
49.
Soto-VasquezMRAlvarado-GarciaPAA. Anxiolytic-like effect of Lippia alba essential oil: a randomized, placebo-controlled trial. Complement med res. (2018) 7:101–7. 10.5455/jice.20171019022824
50.
StanleyPFWanLFKarimRAA. Randomized prospective placebo-controlled study of the effects of lavender aromatherapy on preoperative anxiety in cataract surgery patients. J Perianesth Nurs. (2020) 35:403–6. 10.1016/j.jopan.2019.12.004
51.
TahmasbiHAbasiEZafariMHasanPAbdiH. The association of state anxiety and factors that are related to increased anxiety before coronary angiography. Healthmed. (2012) 6:3571–6.
52.
TahmasebiHPoorkhizAJoubariHA. Comparing the aromatherapeutic effects of orange and lavender essential oils on anxiety and physiological indicators in patients undergoing coronary angiography: a clinical trial study. Med Surg Nurs J. (2019) 8:1–7. 10.5812/msnj.98459
53.
WenXShiJTanWJiangHWangDSuJet al. Effects of aromatherapy and music therapy on patients' anxiety during MRI examinations: a randomized controlled trial. Eur Radiol. (2022) 33:2518–27. 10.1007/s00330-022-09230-3
54.
FakariFRTabatabaeichehrM. Comparing the effect of geranium and orange essential oils on level of anxiety during delivery. J Mazandaran Univ Med Sci. (2015) 25:212–5.
55.
BabaiiAAbbasiniaMHejaziSFSeyyed TabaeiSRDehghaniF. Effect of rosa aromatherapy on anxiety before cardiac catheterization: a randomized controlled trial. Health Spiritual Med Ethics J. (2015) 2:2–8.
56.
InciSÇetinkayaF. Effect of aromatherapy on the anxiety of patients before coronary angiograph. Explore. (2022) 19:203. 10.1016/j.explore.2022.04.006
57.
KaranNB. Influence of lavender oil inhalation on vital signs and anxiety: a randomized clinical trial. Physiol Behav. (2019) 211:112676. 10.1016/j.physbeh.2019.112676
58.
YadegariMMahmoodi-ShanGRKamkarMZVakiliMA. Effects of inhaling jasmine essential oil on anxiety and blood cortisol levels in candidates for laparotomy: a randomized clinical trial. J Nurs Midwifery Sci. (2021) 8:128–33. 10.4103/JNMS.JNMS_125_20
59.
ZhangNChenJDongWYYaoL. The effect of copaiba oil odor on anxiety relief in adults under mental workload: a randomized controlled trial. Evid.-based Complement Altern. Med. (2022) 2022. 10.1155/2022/3874745
60.
TugutNDemirelGBaserMAtaEEKarakusS. Effects of lavender scent on patients' anxiety and pain levels during gynecological examination. Complement Ther Clin Pract. (2017) 28:65–9. 10.1016/j.ctcp.2017.05.006
61.
GuoPLiPZhangXLiuNWangJYangSet al. The effectiveness of aromatherapy on preoperative anxiety in adults: a systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. (2020) 111:103747. 10.1016/j.ijnurstu.2020.103747
62.
CandyBArmstrongMFlemmingKKupeliNStonePVickerstaffVet al. The effectiveness of aromatherapy, massage and reflexology in people with palliative care needs: A systematic review. Palliat Med. (2020) 34:179–94. 10.1177/0269216319884198
63.
de SousaDPde Almeida Soares HocayenPAndradeLNAndreatiniR. A systematic review of the anxiolytic-like effects of essential oils in animal models. Molecules. (2015) 20:18620–60. 10.3390/molecules201018620
64.
GongMDongHTangYHuangWLuF. Effects of aromatherapy on anxiety: A meta-analysis of randomized controlled trials. J Affect Disord. (2020) 274:1028–40. 10.1016/j.jad.2020.05.118
65.
SaviolaFPappaianniEMontiAGrecucciAJovicichJDe PisapiaN. Trait and state anxiety are mapped differently in the human brain. Sci Rep. (2020) 10:11112. 10.1038/s41598-020-68008-z
66.
GaudryEVaggPSpielbergerCD. Validation of the state-trait distinction in anxiety research. Multivariate Behav Res. (1975) 10:331–41. 10.1207/s15327906mbr1003_6
67.
WegerMSandiC. High anxiety trait: a vulnerable phenotype for stress-induced depression. Neurosci Biobehav Rev. (2018) 87:27–37. 10.1016/j.neubiorev.2018.01.012
68.
KomiyaMTakeuchiTHaradaE. Lemon oil vapor causes an anti-stress effect via modulating the 5-HT and DA activities in mice. Behav Brain Res. (2006) 172:240–9. 10.1016/j.bbr.2006.05.006
69.
CostaCACuryTCCassettariBOTakahiraRKFlórioJCCostaM. Citrus aurantium L. essential oil exhibits anxiolytic-like activity mediated by 5-HT(1A)-receptors and reduces cholesterol after repeated oral treatment. BMC Complement Altern Med. (2013) 13:42. 10.1186/1472-6882-13-42
70.
WolffenbüttelANZamboniABeckerGDos SantosMKBorilleBTde Cássia MariottiKet al. Citrus essential oils inhalation by mice: Behavioral testing, GCMS plasma analysis, corticosterone, and melatonin levels evaluation. Phytother Res. (2018) 32:160–9. 10.1002/ptr.5964
71.
GhazizadehJSadigh-EteghadSMarxWFakhariAHamedeyazdanSTorbatiM. et al. The effects of lemon balm (Melissa officinalis L) on depression and anxiety in clinical trials: a systematic review and meta-analysis. Phytother Res. (2021) 35:6690–705. 10.1002/ptr.7252
72.
SirkeciICaganOKocS. The effect of ylang oil and lemon oil inhalation on labor pain and anxiety pregnant women: a randomized controlled trial. Complement Ther Clin Pract. (2023) 52:101748. 10.1016/j.ctcp.2023.101748
73.
Matias Nascimento MaiaWAndradeFAlves FilgueirasLNogueira MendesAFonseca Costa AssunçãoADavidson Sérvulo RodriguesNet al. Antidepressant activity of rose oxide essential oil: possible involvement of serotonergic transmission. Heliyon. (2021) 7:e06620. 10.1016/j.heliyon.2021.e06620
74.
MohamadiNPourkorraniMHSLangarizadehMARanjbartavakoliMSharififarFAsgaryS. Evidence for Rosa damascena efficacy in mental disorders in preclinical animal studies and clinical trials: a systematic review. Phytother Res. (2022) 36:3016–31. 10.1002/ptr.7496
75.
LópezVNielsenBSolasMRamírezMJJägerAK. Exploring pharmacological mechanisms of lavender (Lavandula angustifolia) essential oil on central nervous system targets. Front Pharmacol. (2017) 8:280. 10.3389/fphar.2017.00280
76.
Alinia-NajjarRBagheri-NesamiMShorofiSAMousavinasabSNSaatchiK. The effect of foot reflexology massage on burn-specific pain anxiety and sleep quality and quantity of patients hospitalized in the burn intensive care unit (ICU). Burns. (2020) 46:1942–51. 10.1016/j.burns.2020.04.035
77.
FungTKHLauBWMNgaiSPCTsangHWH. Therapeutic effect and mechanisms of essential oils in mood disorders: interaction between the nervous and respiratory systems. Int J Mol Sci. (2021) 22, 844. 10.3390/ijms22094844
78.
MicaleVDragoF. Endocannabinoid system, stress and HPA axis. Eur J Pharmacol. (2018) 834:230–9. 10.1016/j.ejphar.2018.07.039
Summary
Keywords
anxiety, aromatherapy, essential oils, State-Trait Anxiety Inventory, network meta-analysis
Citation
Tan L, Liao F-f, Long L-z, Ma X-c, Peng Y-x, Lu J-m, Qu H and Fu C-g (2023) Essential oils for treating anxiety: a systematic review of randomized controlled trials and network meta-analysis. Front. Public Health 11:1144404. doi: 10.3389/fpubh.2023.1144404
Received
14 January 2023
Accepted
15 May 2023
Published
01 June 2023
Volume
11 - 2023
Edited by
Mohamed Elsadek, Tongji University, China
Reviewed by
Olívia Rodrigues Pereira, Polytechnic Institute of Bragança (IPB), Portugal; Thiago da Silva Domingos, Federal University of São Paulo, Brazil; Minkai Sun, Suzhou University of Science and Technology, China
Updates
Copyright
© 2023 Tan, Liao, Long, Ma, Peng, Lu, Qu and Fu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Qu hua_qu@yeah.netChang-geng Fu fucgbs@163.com
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.