- Food and Nutrition Department, Faculty of Human Sciences and Design, King Abdulaziz University, Jeddah, Saudi Arabia
Introduction: There is little research on the nutritional status of older people in Saudi Arabia. This study investigated the factors associated with the nutritional status of older people in the Makkah region, Saudi Arabia. We hypothesized that older people who are at risk of malnutrition are at higher risk of different diseases.
Materials and methods: This cross-sectional study surveyed 271 people aged ≥60 years from October 2021 to January 2022. We collected data on demographics, body mass index, the Geriatric Depression Scale-Short Form, Geriatric Oral Health Assessment Index, Mini Nutritional Assessment, Eating Attitudes Test, and Household Dietary Diversity score.
Results: Among the 271 participants, 13.3% were malnourished and 53.9% were at risk of malnutrition. The oral health (P < 0.001), depression (P < 0.001), and eating disorder (P < 0.002) scores were significantly associated with malnutrition. Congestive heart failure, asthma, peripheral vascular disease, Alzheimer's disease, and hypertension were more prevalent among malnourished participants—this supports our original hypothesis. The HDD score showed no significant differences between men and women.
Conclusion: Malnutrition was associated with overweight or obesity, poor oral health, and depression. Older people in the Makkah region, Saudi Arabia, had a high risk of malnutrition.
1. Introduction
Health problems related to malnutrition have increased worldwide in the older population. Malnutrition refers to insufficient (undernutrition) or excess (overnutrition) nutrient intake that contributes to health conditions such as obesity, diabetes, and coronary heart disease (1, 2). Studies have reported that malnutrition is significantly associated with hospitalization in older people, and ~90% of those in hospitals are malnourished or at risk of malnutrition (3). In Australia, 42.3% of older adults admitted to hospitals are malnourished (4). Many psychological and biological changes, such as loss of taste and smell sensitivity, chewing difficulties due to missing teeth, and impaired activities of daily living (5), which affect the intake of certain foods and nutrients are associated with old age and increase the risk of nutrition-related health problems.
Globally, the older population is rapidly expanding (6, 7), with individuals aged ≥65 years accounting for 10% of the global population (1). According to the World Health Organization (WHO), the older population will reach 1.2 billion by 2025, with most residing in low-income countries (7). Furthermore, it has been suggested that by 2025, the percentage of older people worldwide will increase by 300% above that in 2000 (8). With improved medical care and living conditions, Saudi Arabia's demographics are slowly but steadily changing, with life expectancy increasing in recent decades (8). Here, an estimated 4.3% of the population were aged 55–64 years in 2013, while it is predicted that 18.4% will be aged ≥65 years in 2050 (9). Saudi Arabia has witnessed remarkable development in socioeconomic status in the past 40 years, combined with significant lifestyle changes, such as the adoption of Western dietary patterns and reduction in physical activity levels, which has led to a high prevalence of chronic diseases and nutrition-related health problems among different age groups, including older people (10).
Malnutrition increases the risk of morbidity and mortality in the older population (11). Previous research has shown that malnutrition is associated with several factors, including socioeconomic factors (education, sex, and marital status) (12, 13), eating habits (14), and psychological (depression and dementia) (15) and medical factors (osteoporosis, dysphagia, and oral health problems) among older people (16–18). Hence, early detection and treatment of malnutrition in older people is critical for reducing morbidity and improving quality of life. Malnutrition has been reported to be prevalent in 25.6% of older adults in Bangladesh (19) and 17.9% in India (6). However, a previous study showed that only 5.8% of older adults in developed countries, including Switzerland, Sweden, and Japan, are malnourished (20). There is a paucity of research on the nutritional status and factors associated with malnutrition among older people in Saudi Arabia. Therefore, this study aimed to address this gap and investigate the factors associated with the nutritional status of the older population in the Makkah region of Saudi Arabia. We hypothesized that older people who are at risk of malnutrition are at higher risk of different diseases.
2. Materials and methods
2.1. Study design and participants
This cross-sectional study surveyed 271 men and women aged ≥60 years in the two largest cities in the Makkah region of Saudi Arabia, Makkah and Jeddah, from October 2021 to January 2022. As defined by the United Nations, individuals aged ≥60 years were considered as the older population (21). According to the General Authority for Statistics, a total of 321 769 people (both Saudis and non-Saudis) aged ≥60 years were living in the Makkah region during the time of data collection (22). Sample size calculation revealed that a sample of 271 was required to achieve sufficient statistical power based on a 90% confidence level, 5% margin of error, and 50% response distribution (23). The main inclusion criteria were an age ≥60 years and the ability to answer questions independently or with assistance from a caretaker. Participants were excluded if they had feeding tube, cognitive or physical disabilities, or were admitted to hospitals or institutions. This study was onducted in accordance with the guidelines of the Declaration of Helsinki, and all procedures were approved by the Biomedical Ethics Research Committee of King Abdulaziz University (Reference No. 503-21). Written informed consent was obtained from all participants. Data on all participants were collected via face-to-face interviews in public places, such as parks, malls, walking paths, Jeddah Corniche, and primary health care centers.
2.2. Data collection tools
2.2.1. Demographic and anthropometric characteristics
Data on the demographic characteristics of the participants, such as age, sex, nationality, and marital status, were obtained. The following additional questions were asked: “Do you use food delivery applications?” (Answers: yes/no) and “Who prepares your food?” (Answers: myself/family/nobody). After the participants were interviewed, height (centimeters) and weight (kilograms) measurements were taken in light clothing using a standard scale. Body mass index (BMI), calculated by dividing the weight by height squared (kg/m2), was grouped according to the WHO categories (<18.5 kg/m2, underweight; 18.5–24.9 kg/m2, normal weight; 25.0–29.9 kg/m2, overweight; 30.0–34.9 kg/m2, obese; and ≥35 kg/m2, severely obese) (24). Given that only four and six participants were classified as being underweight and severely obese, respectively, we combined the data of participants who were underweight with that of those with a normal weight for the analysis. Similarly, the data of participants who were severely obese were combined with that of those who were obese.
A validated semi-structured questionnaire for data collection through face-to-face interviews was developed based on previous studies that used the Geriatric Depression Scale-Short Form (GDS-SF) (25, 26), Geriatric Oral Health Assessment Index (GOHAI) (27, 28), Mini Nutritional Assessment (MNA) scale (29, 30), Household Dietary Diversity (HDD) score (31, 32), and Eating Attitudes Test (EAT-26) (33, 34). To ensure reliability and validity, the researchers translated the tools into Arabic. These were subsequently sent to 15 participants for pre-testing, following which necessary changes were made to ensure that the questionnaire was culturally consistent.
2.2.2. Geriatric depression scale-short form
This scale involved 15 questions that were highly associated with depressive symptoms based on the original GDS validation studies (25, 26). The GDS-15 examined the participants' mood. The given answers (yes/no) were based on how the participant felt in the past week. Depending on the question, 1 point was awarded to either a “yes” or “no” answer. Scores of 0 to 4 points were considered normal mental health, and 5 to 15 points were indicative of depression.
2.2.3. Geriatric oral health assessment index
The GOHAI comprised 12 questions. Responses on a Likert scale were used to assess oral health problems that might affect daily life, including physical functions, such as eating, swallowing, and speaking; and psychosocial functions, such as worrying or concerns regarding oral health and self-image, in addition to self-consciousness of oral health and limitation of contact with people due to oral health problems. The scale also assessed pain and inconvenience. Responses were scored as follows: never = 5, seldom = 4, sometimes = 3, often = 2, and always = 1. Scores ranging from 57 to 60 were considered adequate oral health, scores ranging from 56 to 51 were considered moderate oral health, and scores ≤50 were considered poor oral health (27, 28).
2.2.4. Mini nutritional assessment questionnaire
The MNA is a screening and assessment tool for older people that consists of 18 items. In this study, 16 items were used as the questions regarding mid-arm and calf circumferences were excluded. The tool is divided into two parts: the first part, which consists of questions regarding BMI, mobility, and weight loss, is used for screening, while the second part consists of questions regarding the living situation of participants, number of drugs used per day, self-perceptions of health and nutrition, and consumption of food and fluid. Each answer was scored and the sum of the points indicated the respondent's status. Participants with scores <17, 17–23.5, and ≥24 were considered malnourished, at risk of malnutrition, and well-nourished, respectively (29, 30).
2.2.5. Eating attitudes test
Eating attitudes and behaviors were evaluated using the EAT-26 self-report questionnaire. The scale had three subscales with 26 questions about dieting, bulimia, and oral control. The questionnaire was related to beliefs, behaviors, and attitudes about food, weight, and body shape (33). Each item, except the behavior subscale, had six response options with scores ranging from 0 to 3 (always = 3, usually = 2, often = 1, sometimes = 0, rarely = 0, and never = 0). The behavior subscale had reversed scores (“never,” “once a month or less,” and “2–3 times a month” = 0; “once a week” = 1; “2–6 times a week” = 2; and “once a day or more” = 3). The overall score was equal to the sum of the scores of the 26 items. A score of ≥20 was characteristic of a disordered eating attitude (34).
2.2.6. Household dietary diversity score
The HDD score was determined based on how many food groups were consumed in a week. The method was adapted from that of Clausen et al. (31). Twelve food groups were used to calculate the HDD score: (1) cereals; (2) roots and tubers; (3) vegetables; (4) fruits; (5) meat, poultry, and offal; (6) eggs; (7) fish and seafood; (8) legumes, nuts, and pulses; (9) milk and dairy products; (10) oil/fats; (11) sugar/honey; and (12) miscellaneous food types. For each food category, a score of 1 (if consumed) or 0 (if not consumed) was assigned. The HDD score, which ranged from 0 to 12, was determined by the total number of food categories consumed by the entire household. It was categorized based on the Food and Agricultural Organization of the United Nations' (32) recommendation: lowest dietary diversity (≤4 food groups), medium dietary diversity (>4 and <7 food groups), and high dietary diversity (≥7 food groups).
2.3. Statistical analyses
Descriptive statistics are presented as means and standard deviations. Linear regression models were used to assess the association of older age groups and nutritional status with oral health, depression, and eating disorder status, with age, sex, BMI, and marital status as covariates. Logistic regression models were constructed to determine the odds ratio (OR) between nutritional status and demographics (sex and age), BMI, oral health, depression, and eating disorders. In the logistic regression analysis, we combined the small number of participants with malnutrition (36 participants) with those at risk of malnutrition (146 participants) into a single group defined as the group at risk of malnutrition. Chi-square tests were used to analyze differences between nutritional status and comorbidities.
The life expectancy in Saudi Arabia in 2020 was estimated at 75 years (35); therefore, we opted for 70 years as the cutoff point to compare data between age groups, especially considering that most participants in this study were at the younger end of the age range of older people (<70 years). If we had opted for 75 years as the cutoff point, the comparison would not have been equivalent. Additionally, in Saudi Arabia, one in four adults have obesity or diabetes (36) (no data available for older people), and the prevalence of chronic diseases in Saudi men is high. One study reported that the percentage of participants aged ≥55 years with one and two or more chronic diseases is 31 and 34.5%, respectively. Furthermore, the prevalence of chronic diseases increases with age and obesity (37).
Statistical analyses were performed using SPSS version 28 (IBM Corp., Armonk, NY, USA). A P-value of 0.05 was set as the statistical significance level for all tests.
3. Results
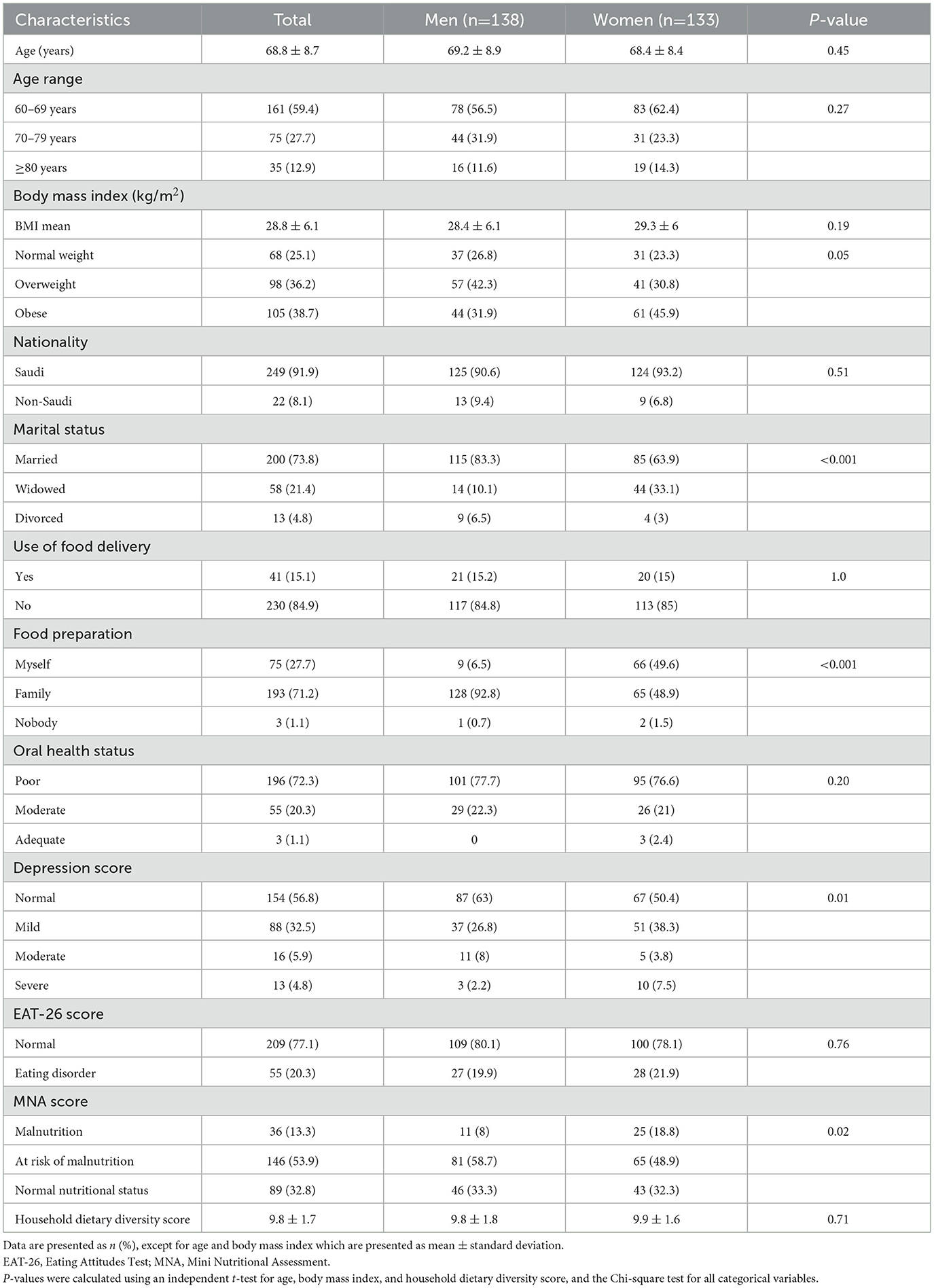
Women represented 49% (men, 51%) of the participants enrolled in the study (Table 1). The mean age of the men and women was 69.2 ± 8.9 years and 68.4 ± 8.4 years, respectively (minimum 60 years and maximum 115 years for the total sample size). The mean BMI of the men and women was 28.4 ± 6.1 kg/m2 and 29.3 ± 6 kg/m2, respectively. According to the BMI categories, in the total sample, 25.1% of the participants had a normal weight, 36.2% were overweight, and 38.7% were obese; in men, the percentages were 26.8, 42.3, and 31.9%, respectively, and in women, 23.3, 30.8, and 45.9%, respectively. Of the participants, 73.8, 21.4, and 4.8% were married, widowed, and divorced, respectively. There were more married men (83.3%) than there were married women (63.9%; P < 0.001). The majority of the participants did not use food delivery services and their families prepared meals for them. This was particularly true for men where 92.8%, compared with 48.9% of women, reported that their families prepared meals for them (P < 0.001). Regarding health questionnaire responses, 72.3% of the participants had poor oral health, 43.2% felt depressed (ranging from mild to severe), and 67.2% were malnourished or at risk of malnutrition. Men tended to feel less depressed (P = 0.01) and were more at risk of malnutrition (P = 0.02) than were women. Among the participants at risk of malnutrition, 14.3% reported weight loss of more than 3 kg in the previous 3 months, 25.3% reported weight loss of 1–3 kg, 26.4% reported no weight loss, and 32.4% did not know if they had lost weight. However, only 20.3% had eating disorders. The mean HDD score of the study participants was 9.8 ± 1.7 and there were no significant differences between men (9.8 ± 1.8) and women (9.9 ± 1.6).
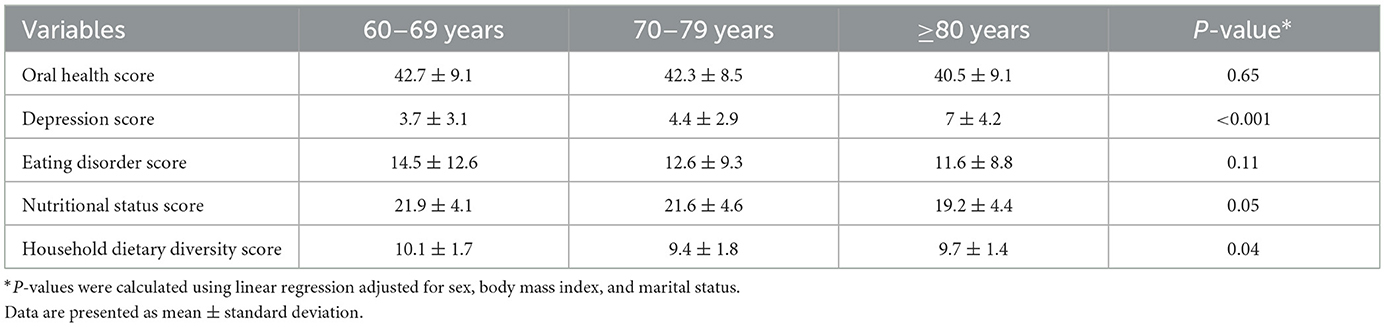
Table 2 compares the health status of older people aged 60–69 years, 70–79 years, and ≥80 years. Participants aged ≥80 years were at risk of depression (GDS score 7 ± 4.2) compared with those aged 70–79 years (GDS score 4.4 ± 2.9) and 60–69 years (GDS score 3.7 ± 3.1; P < 0.001) who had normal mean depression scores. Furthermore, the mean HDD score was significantly higher in participants aged 60–69 years (10.1 ± 1.7) than in those aged 70–79 years (9.4 ± 1.8) and ≥80 years (9.7 ± 1.4; P = 0.04).
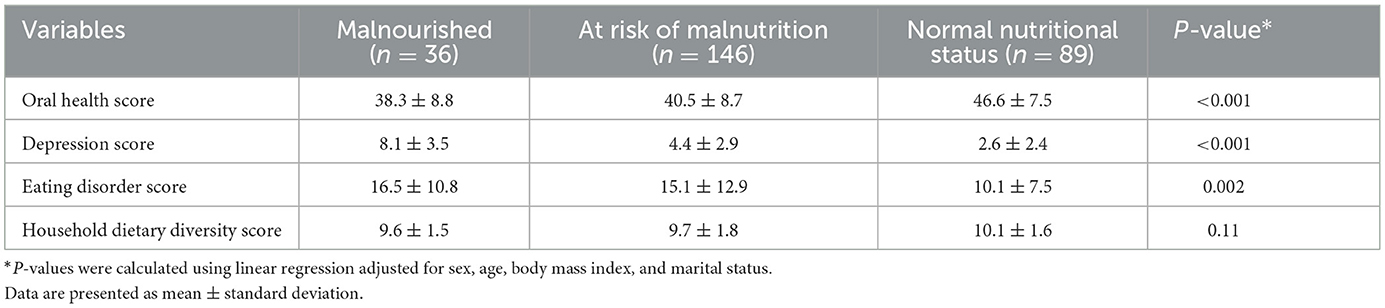
The association between nutritional status and other health conditions is shown in Table 3. Nutritional status was significantly associated with oral health (P < 0.001), depression (P < 0.001), and eating disorder scores (P = 0.002). Participants with malnutrition or at risk of malnutrition were depressed, had a poor oral health status, and had a higher risk of developing eating disorders compared with participants with a normal nutritional status.
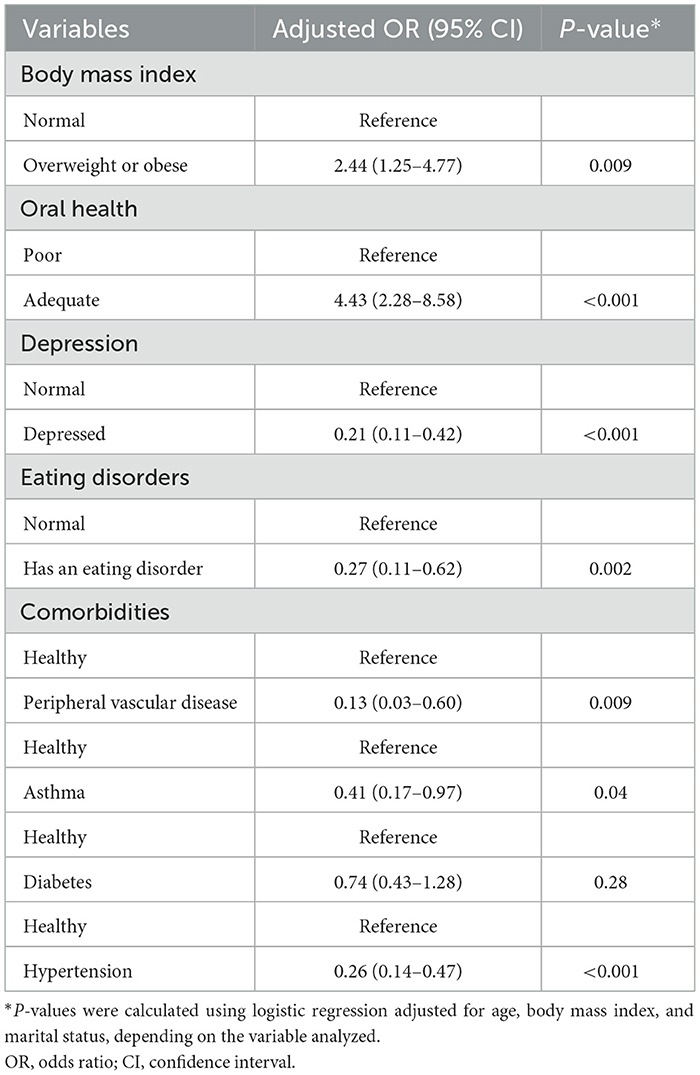
Table 4 shows the adjusted ORs of nutritional status derived from the logistic analysis. The factors associated with higher odds of malnutrition were overweight or obesity (OR, 2.44; 95% confidence interval [CI], 1.25–4.77; P = 0.009), oral health (OR, 4.43; 95% CI, 2.28–8.58; P < 0.001), depression (OR, 0.21; 95% CI, 0.11–0.42; P < 0.001), and eating disorders (OR, 0.27; 95% CI, 0.11–0.62; P < 0.002). Additionally, older individuals with peripheral vascular disease (P = 0.009), asthma (P = 0.04), and hypertension (P < 0.001) had a significant risk of malnutrition. Among older participants, overweight or obesity, oral health, and depression were factors associated with an increased risk of being malnourished or at risk of malnutrition when compared with participants with a normal nutritional status (all P ≤ 0.02; data not presented).
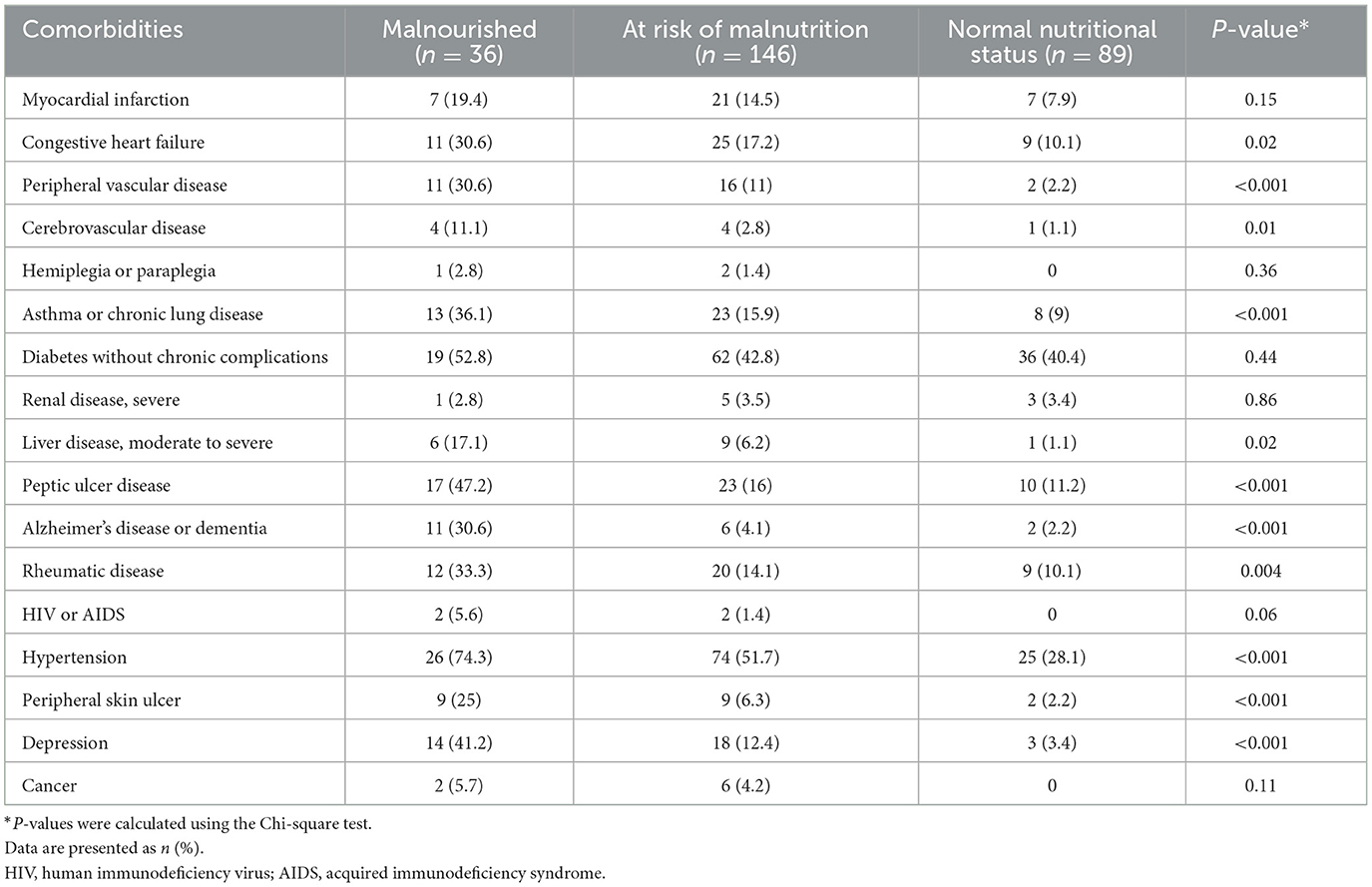
The frequency of comorbidities among older people based on nutritional status is shown in Table 5. The frequency of congestive heart failure (30.6%), peripheral vascular disease (30.6%), cerebrovascular disease (11.1%), asthma or chronic lung disease (36.1%), liver disease (17.1%), peptic ulcer disease (47.2%), Alzheimer's disease or dementia (30.6%), rheumatic disease (33.3%), hypertension (74.3%), peripheral skin ulcer (25%), and depression (41.2%) was significantly higher among participants with malnutrition than among those at risk of malnutrition or with an adequate nutritional status.
4. Discussion
This cross-sectional study aimed to investigate the factors associated with the nutritional status of older people in the Makkah region of Saudi Arabia. The study revealed that malnutrition among older people in Saudi Arabia was associated with oral health, HDD score, overweight or obesity, and depression. Furthermore, we found that compared with participants <80 years of age, participants ≥80 years were at higher risk of depression. In addition, a high percentage of the participants was obese, with a higher proportion of women being obese, and a higher proportion of men being overweight. Overall, this study revealed that older people at risk of malnutrition had significantly higher rates of peripheral vascular disease, asthma or chronic lung disease, peptic ulcers, Alzheimer's disease or dementia, hypertension, and depression than did participants with an adequate nutritional status. Thus, the study results support our hypothesis that older people with malnutrition are at higher risk of different diseases.
In this study, the proportion of participants with or at risk of malnutrition was 67%, which is consistent with the findings of studies from Australia (4) and India (38) that reported a proportion of 50–55%. In contrast, in Spain (6), Turkey (39), Sweden (40), and Hong Kong (12), the percentages were approximately one-third of those found in our study (27, 18.6, 17, and 1.1%, respectively), which may be explained by the high standard of health care for older people in these countries. The reported malnourished status could have resulted from unhealthy dietary choices and inadequate consumption of nutrient-rich foods. Another reason could be that systemic inflammation caused by obesity affects the absorption, distribution, and excretion of nutrients, thereby altering micronutrient metabolism (41). A study conducted among 782 French older adults (aged ≥65 years) found that 18% of overweight and 29% of obese individuals were at risk of undernutrition (42). Furthermore, in contrast with studies from India (6), Bangladesh (19), and France (42) that reported higher malnutrition rates among women than among men, we found that more men than women were at risk of malnutrition. A possible explanation for this might be that only 49% of women but the majority of men (92%) in our study were dependent on their families for food preparation. Previous studies have shown that poor health, a higher risk of diseases, and insufficient nutrient intake in older people may increase the risk of malnutrition. In addition, there are several factors associated with malnutrition or the risk of malnutrition, such as socioeconomic factors (low income, living alone [being single, widowed, or divorced], low education level), eating difficulties and disorders, and depression, especially in older people (40, 43–46). In the present study, the percentage of married men (83.3%) was higher than that of married women (63.9%); however, 21.4% and 4.8% of the participants were widowed and divorced, respectively. According to Bakker et al. (43), such participants may live alone without a helper, which may increase their risk of malnutrition compared with those who live with their families. Several studies have found that a significant percentage of older people at risk of malnutrition have a low socioeconomic status, such as low income and no education (13, 19), which influences dietary intake and eating patterns (13); however, we did not assess these factors in our study. These factors are related to age-related changes in taste, smell, dental health, and biological and physical activities, which can reduce the quality and quantity of nutrient intake and increase the risk of malnutrition in older people (6, 47, 48).
Eating difficulties are an important risk factor for malnutrition and can be caused by gradual muscle degradation, loss of teeth, and loss of motor coordination, leading to difficulties with the handling of food, putting food in the mouth, and chewing and swallowing (dysphagia) (39, 44). These difficulties can lead older people to opt for foods that are low in fiber and nutrients (44), which may increase their risk of malnutrition. In this study, 72.3% of the participants reported that they had poor oral health and 67% were at risk of malnutrition. In older people, There was a significant association between older people with poor oral health (chewing or swallowing difficulties) and being malnourished or at risk of malnutrition, which is consistent with the results of a Lebanese study (45) that used the GOHAI score and reported that 75% of older people had poor oral health and 41.5% were malnourished or at risk of malnutrition. Similarly, studies in Bangladesh (46) and India (38) have reported that 63% and 59.5% of older people who were malnourished, respectively, had poor oral health, whereas in Japan (49), the result (29.6%) was less than that reported in our study.
The mean HDD score was significantly higher in participants aged 60–69 years compared to in those aged ≥70 years; it was also high in comparison with that found in developing countries where there is limited HDD with food options mainly based on starchy staple foods (50). For example, the HDD score among the older population was found to be low in Sri Lanka (51), South Africa (52), and China (53). In contrast, the HDD score among older women was high in the United States (54). The high HDD score found in this study might be a result of high food availability and variability for older adults. In Saudi Arabia, family support and social relationships may play an important role in increasing HDD—family, friends, and neighbors can provide social and economic support (55). In addition, families in Saudi Arabia function as a unit socially and emotionally. Younger members of the family serve older members, and the concept of sending an older member to a nursing home is unacceptable in Saudi culture (56).
After 50 years of age, various changes occur in body composition, such as increases in fat mass and decreases in lean mass (sarcopenia) (57). Therefore, the basal metabolic rate decreases by ~15% between the ages of 30 and 80 years, which consequently reduces energy requirements. However, appetite and nutrient requirements remain the same or increase, which can further lead to weight gain during this age period (58). The frequency of obesity, which is associated with several chronic diseases, such as diabetes, hypertension, and cardiovascular disease, increases in older people aged between 60 and 70 years, particularly in women (59, 60). A high percentage of our study participants were obese (38.7%) and overweight (36.2%), and obesity was more prevalent in women (45.9%) than in men (31.9%), while more men were overweight (41.3%) than were women (30.8%). This is in contrast with the results of other studies showing that older women often have eating disorders because they are still concerned about their body shape (61, 62). In relation to other countries, similar trends in BMI status and the prevalence of overweight have been observed in older men (49 and 31.5%, respectively) and older women (39.8 and 40.8%, respectively) in Spain (63), while a comparatively lower prevalence of obesity has been observed in older people in India (32.5% in both men and women) (6). Our finding was also consistent with that of a study in Scotland (64), which found that obesity prevalence was particularly higher in older women. In the present study, participants at risk of malnutrition had low HDD scores compared with those with a normal nutritional status. Lv et al. found an inverse relationship between HDD score and mortality risk in older adults, with a 44% lower mortality risk among participants with the highest HDD score (65). A study in the United States found a correlation between HDD and BMI in women (54). Furthermore, in Zambia, most older adults were found to have a low HDD and a poor nutritional status (66).
The risk of malnutrition may increase in older individuals who have at least one chronic disease, such as respiratory disease, arthritis, stroke, depression, dementia, gastric diseases, or cancer (59, 67). Moreover, the use of medications for treating these conditions may affect the appetite and swallowing function of older people and reduce the quantity and quality of food consumption and nutrient bioavailability, thereby increasing the risk of malnutrition (59, 67). Our study reported that older adults with peripheral vascular disease, asthma, and hypertension had a significant risk of malnutrition. We also found that 55% of older Saudis were malnourished and diagnosed with hypertension, whereas studies in Algeria (60) and Bangladesh (19) reported that 39.8 and 88.9% of older people, respectively, were malnourished and diagnosed with hypertension. On the other hand, our study showed that 19.8% of the participants who were at risk of malnutrition had been diagnosed with asthma or chronic lung disease, significantly less than that reported in Bangladesh (79%) (19).
A total of 15% of the participants at risk of malnutrition had peripheral vascular disease, which is relatively high. However, studies have indicated that diabetes and heart failure are important risk factors for peripheral vascular disease (58), and almost a half and a quarter of the older people in our study were diagnosed with diabetes and heart failure, respectively. This may explain the percentage of peripheral vascular disease in our cohort (30.6%). In a study by Saquib et al. (37), conducted in the Al-Qassim region of Saudi Arabia, the prevalence of chronic diseases including hypertension, diabetes, heart disease, asthma, ulcers, and cancer in Saudi men was 71.3, 27.3, 16.4, 9.7, 8.9, and 2.0%, respectively. The participants in our study were relatively young (68.8 ± 8.7 years) based on the WHO definition of the young-old (60–74 years) (58); this group is usually healthy and independent. Furthermore, this study excluded participants with feeding tube and physical disabilities, as well as those who were admitted to hospitals or in-care institutions. Nevertheless, the prevalence of several diseases, such as asthma or chronic lung disease, Alzheimer's disease or dementia, hypertension, and depression, was relatively high in our study compared with studies conducted in other countries.
Regarding mental health status, the frequency of Alzheimer's disease or dementia and depression was relatively low in our study (9.3 and 17.6%, respectively). A Swedish systematic review reported that 1.5% and 35% of older people aged 64–69 and 90–94 years, respectively, have dementia and are at risk of malnutrition (68). Furthermore, our results showed an association between depression and the risk of malnutrition among older people; this association was more significant in those aged ≥80 years (mild depression) than in those aged <80 years (normal depression status). Similarly, Iranian (69) and Bangladeshi (19) studies have confirmed that malnutrition is significantly higher among older people with depression, with further studies in Bangladesh and Japan (19, 47) reporting the odds of malnutrition among older people who are depressed to be 15.6 and 6.3 times higher, respectively, than those who are not depressed (compared with 10 times higher in our study). Furthermore, among the participants at risk of malnutrition in our study, men tended to be less depressed than were women, which is in agreement with 69 among the 85 studies included in a review by Girgus et al. (70). Mantzorou et al. (71) also concluded that malnutrition is more common in older people who have cognitive decline and depressive symptoms. These results may be explained by the effect of depression on appetite and eating behaviors (69).
A health care system aimed at the older population has been developed in various countries. In European countries, the WHO has been working with governments to establish five priority intervention strategies: the prevention of falls and infectious diseases, promotion of physical activity, support for home care, and capacity building among health and social care workers (72). In Saudi Arabia, the Ministry of Health has established “The Home Care Program for Older Adults” to oversee all home medical services (73). Consequently, all stakeholders were required to contribute to developing policies, programs, and interventions for healthy older adults to maintain independence and remain as active as possible (74). In general, these health care systems can help to improve the health of older adults and reduce the occurrence of malnutrition in Saudi Arabia.
This study has several limitations. Despite the importance of socioeconomic level in terms of nutritional status, factors including economic status, educational level, and urban-rural were not assessed in this survey. Data on food intake, clinical signs, and laboratory investigations were also not collected to determine other factors of malnutrition. Furthermore, participants were from the Makkah region of Saudi Arabia, which limits the generalizability of the findings to the whole Kingdom. Further studies with larger sample sizes that recruit participants from all regions of Saudi Arabia are required to verify our findings. Moreover, the current study used convenience sampling which is a non-probability sampling method that might introduce selection bias, as those who were engaged in the research matter might have been more interested in participating. Nevertheless, this study is one of the few focused on the factors associated with nutritional status in Saudi Arabia, which is its the main strength. Another strength of this study is the use of several validated questionnaires, and the fact that anthropometric indices (weight and height) were measured and not self-reported. Additionally, there is a lack of research focusing on the nutritional and health statuses of older people globally, and particularly in Saudi Arabia, which highlights the importance of this study. Our findings can help to develop strategies to improve nutritional status and prevent malnutrition among older people, thereby reducing treatment costs.
5. Conclusion
Our study is one of the few studies assessing the factors associated with the nutritional status of older people, especially in Saudi Arabia. It can be concluded that there is a high proportion of malnutrition in the older population of the Makkah region of Saudi Arabia. The majority of older people of both sexes were overweight or obese, with a high risk of malnutrition. Oral health, depression, and eating disorders were factors related to the nutritional status of older people in Saudi Arabia. Among individuals with malnutrition, there was a significantly higher prevalence of peripheral vascular disease, asthma or chronic lung disease, peptic ulcers, Alzheimer's disease or dementia, hypertension, and depression than among individuals at risk of malnutrition and those with a healthy nutritional status. Generally, older people and their caretakers did not recognize symptoms of malnutrition in the early stages. Therefore, they did not seek treatments such as modified food or supplements until several conditions and complications had developed. The risk of malnutrition among older people in Saudi Arabia and globally can be reduced by regular nutritional screening and subsequent designing of nutritional interventions for timely treatment to prevent complications. The factors related to malnutrition among older people in Saudi Arabia should be studied in the future due to the increased proportion of this age group in this population group.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Biomedical Ethics Research Committee of King Abdulaziz University (Reference No. 503-21). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization: MA. Methodology: MA and IS. Formal analysis: IS. Data collection, writing—original draft preparation, reviewing, and editing of the manuscript: MA, IS, NAlm, and NAlj. All authors have read and agreed to the published version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Zhang X, Edwards BJ. Malnutrition in older adults with cancer. Curr Oncol Rep. (2019) 21:80. doi: 10.1007/s11912-019-0829-8
3. Persson MD, Brismar KE, Katzarski KS, Nordenström J, Cederholm TE. Nutritional status using mini nutritional assessment and subjective global assessment predict mortality in geriatric patients. J Am Geriatr Soc. (2002) 50:1996–2002. doi: 10.1046/j.1532-5415.2002.50611.x
4. Sharma Y, Miller M, Shahi R, Hakendorf P, Horwood C, Thompson C. Malnutrition screening in acutely unwell elderly inpatients. Br J Nurs. (2016) 25:1006–14. doi: 10.12968/bjon.2016.25.18.1006
5. Kwon SH, Park HR, Lee YM, Kwon SY, Kim OS, Kim HY, et al. Difference in food and nutrient intakes in Korean elderly people according to chewing difficulty: using data from the Korea National Health and Nutrition Examination survey 2013 (6th). Nutr Res Pract. (2017) 11:139–46. doi: 10.4162/nrp.2017.11.2.139
6. Krishnamoorthy Y, Vijayageetha M, Kumar SG, Rajaa S, Rehman T. Prevalence of malnutrition and its associated factors among elderly population in rural Puducherry using mini-nutritional assessment questionnaire. J Family Med Prim Care. (2018) 7:1429–33. doi: 10.4103/jfmpc.jfmpc_22_18
7. World Health Organization. Nutrition for Older Persons. Available online at: http://apps.who.int/iris/bitstream/10665/42515/2/9241562102_annexes.pdf (accessed July 11, 2021).
8. Karlin NJ, Weil J, Felmban W. Aging in Saudi Arabia: an exploratory study of contemporary older persons' views about daily life, health, and the experience of aging. Gerontol Geriatr Med. (2016) 2:2333721415623911. doi: 10.1177/2333721415623911
9. Abyad A. Alzheimer's and geriatrics in the middle east. MEJPA. (2015) 6:3–8. doi: 10.5742/MEPA.2015.92728
10. Aljefree N, Ahmed F. Prevalence of cardiovascular disease and associated risk factors among adult population in the Gulf region: a systematic review. Adv Public Health. (2015) 2015:1–23. doi: 10.1155/2015/235101
11. Brownie S. Why are elderly individuals at risk of nutritional deficiency? Int J Nurs Pract. (2006) 12:110–8. doi: 10.1111/j.1440-172X.2006.00557.x
12. Wong MM, So WK, Choi KC, Cheung R, Chan HY, Sit JW, et al. Malnutrition risks and their associated factors among home-living older Chinese adults in Hong Kong: hidden problems in an affluent Chinese community. BMC Geriatr. (2019) 19:138. doi: 10.1186/s12877-019-1148-5
13. Ghosh A, Dasgupta A, Paul B, Sembiah S, Biswas B, Mallik N. Screening for malnutrition among the elderly with MNA scale: a clinic-based study in a rural area of West Bengal. Int J Contemp Res. (2017) 4:1978–82.
14. Sutradhar I, Gayen P, Hasan M, Gupta RD, Roy T, Sarker M. Eye diseases: the neglected health condition among urban slum population of Dhaka, Bangladesh. BMC Ophthalmol. (2019) 19:38. doi: 10.1186/s12886-019-1043-z
15. Midlarsky E, Marotta AK, Pirutinsky S, Morin RT, McGowan JC. Psychological predictors of eating pathology in older adult women. J Women Aging. (2018) 30:145–57. doi: 10.1080/08952841.2017.1295665
16. Wong SK, Chin KY, Suhaimi FH, Ahmad F, Jamil NA, Ima-Nirwana S. Osteoporosis is associated with metabolic syndrome induced by high-carbohydrate high-fat diet in a rat model. Biomed Pharmacother. (2018) 98:191–200. doi: 10.1016/j.biopha.2017.12.042
17. Ebihara S, Sekiya H, Miyagi M, Ebihara T, Okazaki T. Dysphagia, dystussia, and aspiration pneumonia in elderly people. J Thorac Dis. (2016) 8:632–9. doi: 10.21037/jtd.2016.02.60
18. Cousson PY, Bessadet M, Nicolas E, Veyrune JL, Lesourd B, Lassauzay C. Nutritional status, dietary intake and oral quality of life in elderly complete denture wearers. Gerodontology. (2012) 29:e685–92. doi: 10.1111/j.1741-2358.2011.00545.x
19. Rahman KM, Khalequzzaman M, Khan FA, Rayna SE, Samin S, Hasan M, et al. Factors associated with the nutritional status of the older population in a selected area of Dhaka, Bangladesh. BMC Geriatr. (2021) 21:161. doi: 10.1186/s12877-021-02068-2
20. Kaiser MJ, Bauer JM, Rämsch C, Uter W, Guigoz Y, Cederholm T, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. (2010) 58:1734–8. doi: 10.1111/j.1532-5415.2010.03016.x
21. United Nations. World Population Ageing. (2017). Available online at: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf (Accessed September 3, 2021).
22. General Authority for Statistics. KSA. (2021). Available online at: https://www.stats.gov.sa/sites/default/files/ar-makkah.pdf (accessed September 3, 2021).
23. Raosoft Inc. Sample Size Calculator. Available online at: http://www.raosoft.com/samplesize.html (accessed September 3, 2021).
24. World Health Organization. The Challenge of Obesity in the WHO European Region and the Strategies for Response: Summary. (2007). Available online at: https://www.euro.who.int/__data/assets/pdf_file/0008/98243/E89858.pdf (accessed December 25, 2021).
25. Greenberg SA. How to try this: the geriatric depression scale: short form. Am J Nurs. (2007) 107:60–9. doi: 10.1097/01.NAJ.0000292204.52313.f3
26. Durmaz B, Soysal P, Ellidokuz H, Isik AT. Validity and reliability of Geriatric Depression Scale-15 (Short Form) in Turkish older adults. North Clin Istanb. (2018) 5:216–20. doi: 10.14744/nci.2017.85047
27. Tubert-Jeannin S, Riordan PJ, Morel-Papernot A, Porcheray S, Saby-Collet S. Validation of an oral health quality of life index (GOHAI) in France. Commu Dent Oral Epidemiol. (2003) 31:275–84. doi: 10.1034/j.1600-0528.2003.t01-1-00006.x
28. Aguirre-Bustamante J, Barón-López FJ, Carmona-González FJ, Pérez-Farinós N, Wärnberg J. Validation of a modified version of the Spanish Geriatric oral health assessment index (GOHAI-SP) for adults and elder people. BMC Oral Health. (2020) 20:61. doi: 10.1186/s12903-020-1047-3
29. Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: the mini nutritional assessment as part of the geriatric evaluation. Nutr Rev. (1996) 54:S59–65. doi: 10.1111/j.1753-4887.1996.tb03793.x
30. Pereira Machado RS, Santa Cruz Coelho MA. Risk of malnutrition among Brazilian institutionalized elderly: a study with the Mini Nutritional Assessment (MNA) questionnaire. J Nutr Health Aging. (2011) 15:532–5. doi: 10.1007/s12603-011-0059-8
31. Clausen T, Charlton KE, Gobotswang KS, Holmboe-Ottesen G. Predictors of food variety and dietary diversity among older persons in Botswana. Nutrition. (2005) 21:86–95. doi: 10.1016/j.nut.2004.09.012
32. Kennedy G, Ballard T, Dop MC. Guidelines for Measuring Household Individual Dietary Diversity. (2011). Available online at: https://www.fao.org/3/i1983e/i1983e00.pdf (accessed February 25, 2023).
33. Szabo CP, Allwood CW. Application of the Eating Attitudes Test (EAT-26) in a rural, Zulu speaking, adolescent population in South Africa. World Psychiatry. (2004) 3:169–71.
34. Saleh RN, Salameh RA, Yhya HH, Sweileh WM. Disordered eating attitudes in female students of An-Najah National University: a cross-sectional study. J Eat Disord. (2018) 6:16. doi: 10.1186/s40337-018-0204-4
35. The World Bank. Life Expectancy at Birth, Total (years)—Saudi Arabia. (2020). Available online at: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=SA (accessed August 8, 2020).
36. Alqurashi KA, Aljabri KS, Bokhari SA. Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med. (2011) 31:19–23. doi: 10.5144/0256-4947.2011.19
37. Saquib N, Saquib J, Alhadlag A, Albakour MA, Aljumah B, Sughayyir M, et al. Chronic disease prevalence among elderly Saudi men. Int J Health Sci. (2017) 11:11–6.
38. Agarwalla R, Saikia AM, Baruah R. Assessment of the nutritional status of the elderly and its correlates. J Family Commun Med. (2015) 22:39–43. doi: 10.4103/2230-8229.149588
39. Nazan S, Buket K. Evaluation of nutritional status of elderly patients presenting to the Family Health Center. Pak J Med Sci. (2018) 34:446–51. doi: 10.12669/pjms.342.14936
40. Johansson L, Sidenvall B, Malmberg B, Christensson L. Who will become malnourished? A prospective study of factors associated with malnutrition in older persons living at home. J Nutr Health Aging. (2009) 13:855–61. doi: 10.1007/s12603-009-0242-3
41. Kobylińska M, Antosik K, Decyk A, Kurowska K. Malnutrition in obesity: is it possible? Obes Facts. (2022) 15:19–25. doi: 10.1159/000519503
42. Sulmont-Rossé C, Van Wymelbeke-Delannoy VV, Maître I. Prevalence of undernutrition and risk of undernutrition in overweight and obese older people. Front Nutr. (2022) 9:892675. doi: 10.3389/fnut.2022.892675
43. Bakker MH, Vissink A, Spoorenberg SLW, Jager-Wittenaar H, Wynia K, Visser A. Are edentulousness, oral health problems and poor health-related quality of life associated with malnutrition in community-dwelling elderly (aged 75 years and over)? A cross-sectional study. Nutrients. (2018) 10:1965. doi: 10.3390/nu10121965
44. Natapov L, Kushnir D, Goldsmith R, Dichtiar R, Zusman SP. Dental status, visits, and functional ability and dietary intake of elderly in Israel. Isr J Health Policy Res. (2018) 7:58. doi: 10.1186/s13584-018-0252-x
45. El Osta N, Hennequin M, Tubert-Jeannin S, Abboud Naaman NB, El Osta L, Geahchan N. The pertinence of oral health indicators in nutritional studies in the elderly. Clin Nutr. (2014) 33:316–21. doi: 10.1016/j.clnu.2013.05.012
46. Ferdous T, Kabir ZN, Wahlin A, Streatfield K, Cederholm T. The multidimensional background of malnutrition among rural older individuals in Bangladesh–a challenge for the Millennium Development Goal. Public Health Nutr. (2009) 12:2270–8. doi: 10.1017/S1368980009005096
47. Carrard I, Rothen S. Factors associated with disordered eating behaviors and attitudes in older women. Eat Weight Disord. (2020) 25:567–75. doi: 10.1007/s40519-019-00645-4
48. Porter Starr KN, McDonald SR, Bales CW. Nutritional vulnerability in older adults: a continuum of concerns. Curr Nutr Rep. (2015) 4:176–84. doi: 10.1007/s13668-015-0118-6
49. Yoshimura K, Yamada M, Kajiwara Y, Nishiguchi S, Aoyama T. Relationship between depression and risk of malnutrition among community-dwelling young-old and old-old elderly people. Aging Ment Health. (2013) 17:456–60. doi: 10.1080/13607863.2012.743961
50. Ruel MT. Operationalizing dietary diversity: a review of micronutrient issues and research priorities. J Nutr. (2003) 133:3911–26. doi: 10.1093/jn/133.11.3911S
51. Rathnayake KM, Madushani PA, Silva KD. Use of dietary diversity score as a proxy indicator of nutrient adequacy of rural elderly people in Sri Lanka. BMC Res Notes. (2012) 5:1–6. doi: 10.1186/1756-0500-5-469
52. Oldewage-Theron WH, Kruger R. Food variety and dietary diversity as indicators of the dietary adequacy and health status of an elderly population in Sharpeville, South Africa. J Nutr Elder. (2008) 27:101–33. doi: 10.1080/01639360802060140
53. Yin Z, Fei Z, Qiu C, Brasher MS, Kraus VB, Zhao W, et al. Dietary diversity and cognitive function among elderly people: a population-based study. J Nutr Health Aging. (2017) 21:1089–94. doi: 10.1007/s12603-017-0912-5
54. Bernstein MA, Tucker KL, Ryan ND, O'Neill EF, Clements KM, Nelson ME, et al. Higher dietary variety is associated with better nutritional status in frail elderly people. J Am Diet Assoc. (2002) 102:1096–104. doi: 10.1016/S0002-8223(02)90246-4
55. Nguyen AW, Chatters LM, Taylor RJ, Mouzon DM. Social support from family and friends and subjective well-being of older African Americans. J Happiness Stud. (2016) 17:959–79. doi: 10.1007/s10902-015-9626-8
56. Saleh Al Mutair A, Plummer V, O'Brien PA, Clerehan R. Providing culturally congruent care for Saudi patients and their families. Contemp Nurse. (2014) 46:254–58. doi: 10.5172/conu.2014.46.2.254
57. Kyle UG, Genton L, Hans D, Karsegard L, Slosman DO, Pichard C. Age-related differences in fat-free mass, skeletal muscle, body cell mass and fat mass between 18 and 94 years. Eur J Clin Nutr. (2001) 55:663–72. doi: 10.1038/sj.ejcn.1601198
58. Bernstein M, McMahon K. “Older Adult Nutrition,” In: Nutrition Across Life Stages. Burlington, MA: Jones and Bartlett Publishers Learning (2018), p. 448–56.
59. Ortolani E. Nutritional status and drug therapy in older adults. J Gerontol Geriatr Res. (2013) 2:10–4172. doi: 10.4172/2167-7182.1000123
60. Merad-Boudia HN, Bereksi-Reguig K. Assessment of risk of malnutrition in elderly hypertensive patients with or without associated cardiovascular risk factors living at home (West Algeria) Sidi-Bel-Abbès. Int J Clin Med. (2016) 7:144–68. doi: 10.4236/ijcm.2016.72016
61. Brandsma L. Eating disorders across the life span. J Women Aging. (2007) 19:155–72. doi: 10.1300/J074v19n01_10
62. Peat CM, Peyerl NL, Muehlenkamp JJ. Body image and eating disorders in older adults: a review. J Gen Psychol. (2008) 135:343–58. doi: 10.3200/GENP.135.4.343-358
63. Gómez-Cabello A, Pedrero-Chamizo R, Olivares PR, Hernández-Perera R, Rodríguez-Marroyo JA, Mata E, et al. Sitting time increases the overweight and obesity risk independently of walking time in elderly people from Spain. Maturitas. (2012) 73:337–43. doi: 10.1016/j.maturitas.2012.09.001
64. Han TS, Tajar A, Lean ME. Obesity and weight management in the elderly. Br Med Bull. (2011) 97:169–96. doi: 10.1093/bmb/ldr002
65. Lv Y, Kraus VB, Gao X, Yin Z, Zhou J, Mao C, et al. Higher dietary diversity scores and protein-rich food consumption were associated with lower risk of all-cause mortality in the oldest old. Clin Nutr. (2020) 39:2246–54. doi: 10.1016/j.clnu.2019.10.012
66. Maila G, Audain K, Marinda PA. Association between dietary diversity, health and nutritional status of older persons in rural Zambia. South Afr J Clin Nutr. (2021) 34:34–9. doi: 10.1080/16070658.2019.1641271
67. Heuberger RA, Caudell K. Polypharmacy and nutritional status in older adults: a cross-sectional study. Drugs Aging. (2011) 28:315–23. doi: 10.2165/11587670-000000000-00000
68. The Swedish Council on Technology Assessment in Health Care. Dementia—Etiology and Epidemiology. A systematic review (2008). Available online at: https://www.sbu.se/contentassets/2c12ea9230ef419a84a0078c5fa48ae7/dementia_vol12.pdf (accessed June 10, 2022).
69. Vedantam A, Subramanian V, Rao NV, John KR. Malnutrition in free-living elderly in rural south India: prevalence and risk factors. Public Health Nutr. (2010) 13:1328–32. doi: 10.1017/S1368980009991674
70. Girgus JS, Yang K, Ferri CV. The gender difference in depression: are elderly women at greater risk for depression than elderly men? Geriatrics. (2017) 2:35. doi: 10.3390/geriatrics2040035
71. Mantzorou M, Vadikolias K, Pavlidou E, Serdari A, Vasios G, Tryfonos C, et al. Nutritional status is associated with the degree of cognitive impairment and depressive symptoms in a Greek elderly population. Nutr Neurosci. (2020) 23:201–9. doi: 10.1080/1028415X.2018.1486940
72. World Health Organization. Policies and Priority Interventions for Health Ageing. (2012). Available online at: https://www.euro.who.int/__data/assets/pdf_file/0006/161637/WHD-Policies-and-Priority-Interventions-for-Healthy-Ageing.pdf (accessed February 19, 2023).
73. Nelson KM, Helfrich C, Sun H, Hebert PL, Liu CF, Dolan E, et al. Implementation of the patient-centered medical home in the Veterans Health Administration: associations with patient satisfaction, quality of care, staff burnout, and hospital and emergency department use. JAMA Intern Med. (2014) 174:1350–8. doi: 10.1001/jamainternmed.2014.2488
Keywords: malnutrition, aging, older people, overweight, nutritional status, depression, eating disorders, Saudi Arabia
Citation: Althaiban MA, Aljefree NM, Almoraie NM and Shatwan IM (2023) Malnutrition is associated with increased disease risk in older people in the Makkah region of Saudi Arabia: A cross-sectional study. Front. Public Health 11:1149739. doi: 10.3389/fpubh.2023.1149739
Received: 22 January 2023; Accepted: 20 March 2023;
Published: 03 April 2023.
Edited by:
Nai Peng Tey, University of Malaya, MalaysiaReviewed by:
Jagmeet Madan, SNDT Women's University, IndiaSakinah Harith, Sultan Zainal Abidin University, Malaysia
Copyright © 2023 Althaiban, Aljefree, Almoraie and Shatwan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maha A. Althaiban, bXRoYWliYW5Aa2F1LmVkdS5zYQ==
 Maha A. Althaiban
Maha A. Althaiban Najlaa M. Aljefree
Najlaa M. Aljefree Noha M. Almoraie
Noha M. Almoraie Israa M. Shatwan
Israa M. Shatwan