Abstract
Typhoid fever, a common enteric disease in Pakistan, caused by Salmonella typhi, is becoming an extended drug-resistant organism and is preventable through the typhoid conjugate vaccine (TCV). Public adherence to preventive measures is influenced by knowledge and attitude toward the vaccine. This study investigates the knowledge, attitudes, and practices of the general population of Pakistan toward TCV. The differences in mean scores and factors associated with typhoid conjugate vaccine knowledge, attitudes, and practices were investigated. A total of 918 responses were received with a mean age of 25.9 ± 9.6, 51% were women, and 59.6% had graduation-level education. The majority of them responded that vaccines prevent illness (85.3%) and decrease mortality and disability (92.6%), and typhoid could be prevented by vaccination (86.7%). In total, 77.7 and 80.8% considered TCV safe and effective, respectively. Of 389 participants with children, 53.47% had vaccinated children, according to the extended program on immunization (EPI). Higher family income has a higher odds ratio (OR) for willingness toward booster dose of TCV [crude odds ratio (COR) = 4.920, p–value <0.01; adjusted odds ratio (aOR) = 2.853, value of p <0.001], and negative attitude regarding the protective effect of TCV has less willingness toward the booster dose with statistical significance (COR = 0.388, value of p = 0.017; aOR = 0.198, value of p = 0.011). The general population of Pakistan had a good level of knowledge about the benefits of TCV, and attitude and practices are in favor of the usage of TCV. However, a few religious misconceptions are prevalent in public requiring the efforts to overcome them to promote the usage of vaccines to prevent the disease and antibiotic resistance.
Introduction
Typhoid fever is a systemic infection characterized by fever, vomiting, and diarrhea caused by Salmonella typhi (S. typhi) (1, 2). The disease is transmitted by consuming fecal-contaminated water and food (3). Annually, typhoid affects 11 to 20 million people with 128,000 to 161,000 deaths worldwide.4 Underprivileged communities and children are at higher risk for typhoid fever (4). Children younger than 5 years of age had the highest rates of morbidity and mortality (12.6% of cases and 17% of deaths), followed by children aged 5 to 9 years (56% of cases and 59% of deaths). Typhoid fever is also a common disease in Pakistan, affecting 451.7 people per 100,000 each year (5). The improvements in sanitary infrastructure significantly control enteric fever in developed countries. The misusage of antibiotics in lower-middle-income countries (LMICs) for the treatment of S. typhi is growing antibiotic resistance, raising danger to global public health (1, 6). The mortality rate due to S. typhi had also increased, attributing to antibiotic resistance. S. typhi strains resistant to antibiotics such as chloramphenicol, ampicillin, trimethoprim–sulfamethoxazole, fluoroquinolones, and third-generation cephalosporin are labeled as extended drug-resistant (XDR) (7).
Pakistan had one of the highest rates of typhoid cases in South Asia. The rising level of antibiotic resistance in the country is raising global fear. The dire state of the sewage and water system along with low vaccination rates, non-compliance to treatment, and overcrowding are the major elements contributing to the spread of XDR typhoid within Pakistan (8). Furthermore, in 2016, XDR typhoid outbreak occurred in Sindh, Pakistan (9). The prevalence of positive cultures of S. paratyphi A raised from 0.2% in 2017 to 0.3% in 2018, then up to 0.9% in 2019 and increasing the prevalence of XDR typhoid fever across the country, indicating spread outside Sindh (9). Without active and effective measures, the preexisting and increased burden of XDR typhoid is expected to worsen, given the strain coronavirus disease 2019 (COVID-19) is putting on the healthcare system (10, 11). The prevalence of diseases, disabilities, and deaths has been significantly reduced because of vaccination (12).
Vaccines prevent 4–5 million people from dying from fatal diseases each year (13). Numerous success stories against polio, tetanus, influenza, hepatitis B, diphtheria, pertussis, measles, mumps, and rubella (MMR) had been made possible by effective vaccination. Typhoid vaccination had been proven effective for the prevention and control of typhoid. Pakistan is the first country to introduce typhoid conjugate vaccine (TCV) in the extended program on immunization (EPI) and had vaccinated over 30 million children in the country with an effectiveness of 95% against protection from typhoid (14). The first single dose of TCV provides prolonged immunity and is effective and safe for children between 6 months and 2 years of age (15).
The vaccine coverage gap does, however, exist between nations and even within a nation (16). The World Health Organization (WHO) identified vaccine reluctance as one of the threats to global health (17). Vaccine hesitation had been caused by several factors, including erroneous safety worries about immunization as a result of measles, diphtheria, and pertussis outbreaks (12). Influential religious and political figures and false religious beliefs greatly influenced vaccine refusal (18, 19). Personal or philosophical convictions, such as the idea that a healthy lifestyle will prevent sickness or that active immunity obtained after natural infection is superior to that acquired by vaccination, are other factors contributing to vaccination refusal (20) (Figures 1–3).
Figure 1
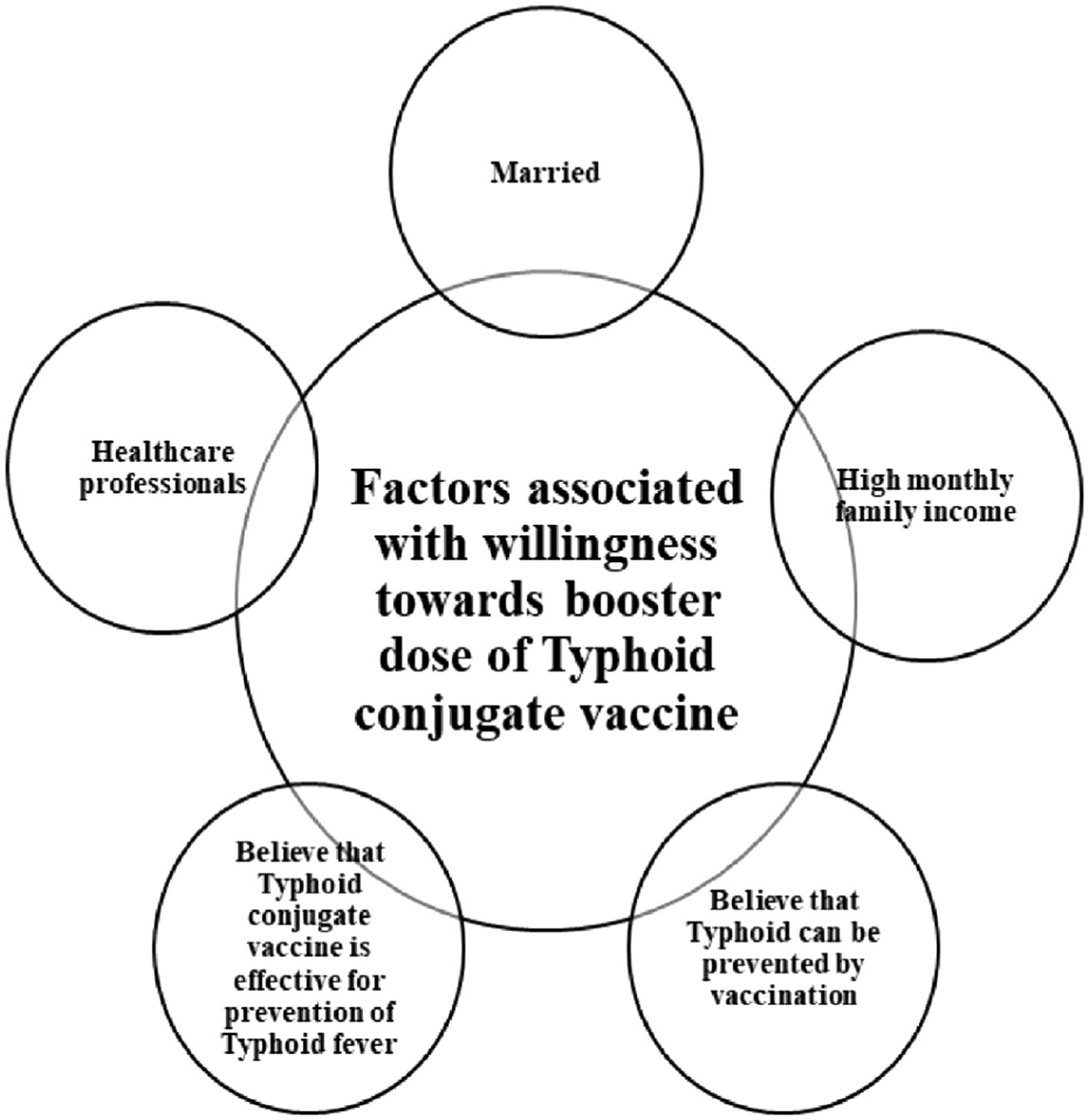
Factors associated with willingness toward booster dose of typhoid conjugate vaccine.
Figure 2
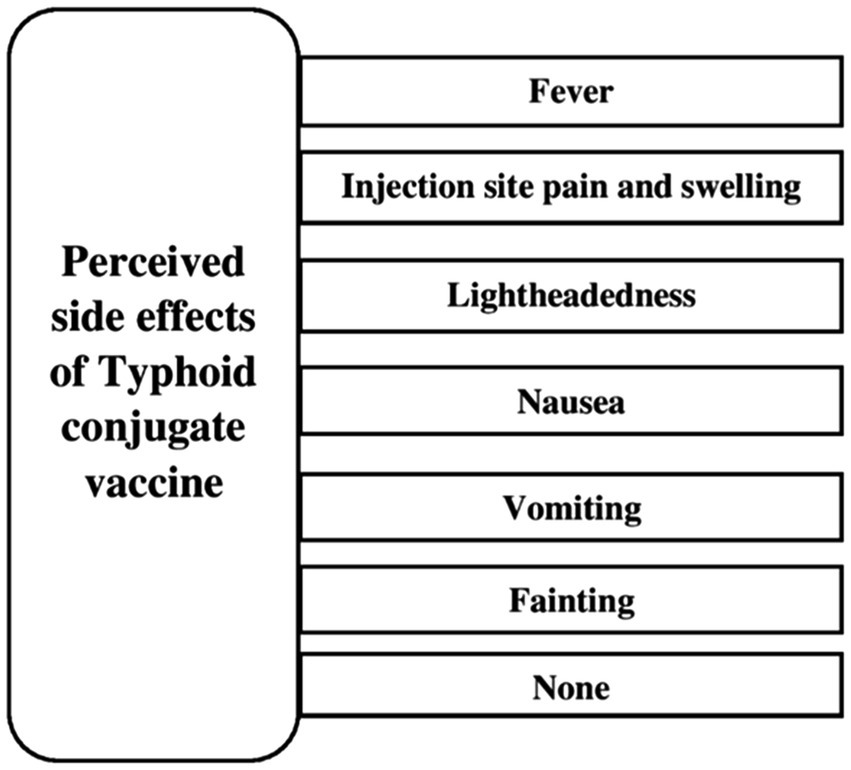
Perceived side effects of typhoid conjugate vaccine.
Figure 3
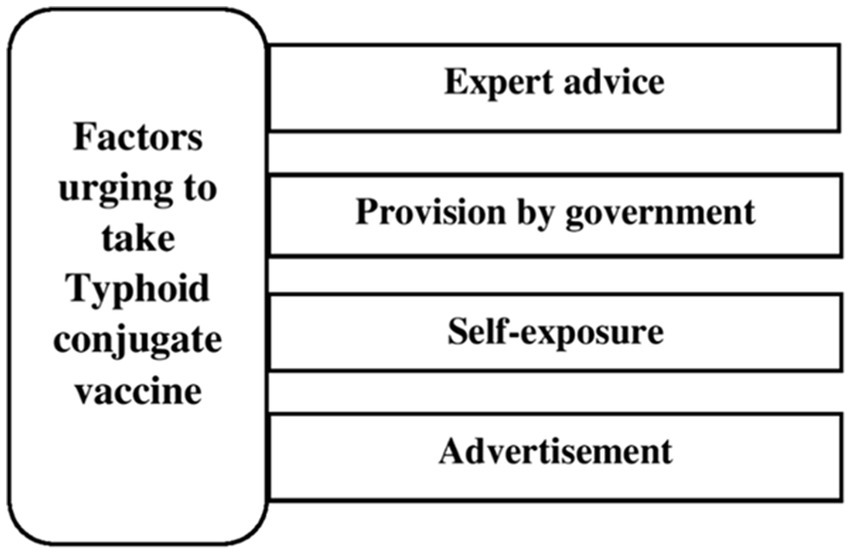
Factors urging to take typhoid conjugate vaccine.
The vaccination rates of Pakistan’s population are below the required levels worldwide (21). The vaccination rates for Bacillus Calmette–Guérin (BCG), polio combined with DPT (Diptheria, Pertussis, and Tetanus), and measles are each stated to be at 80, 65, and 67%, respectively (21). This is a result of logistical challenges, inadequately qualified medical staff, inadequate parental education and awareness, and political, religious, and commercial influences on the promotion of vaccine products (21–23). Education and vaccines are the most powerful tools, proven to be valuable, against preventable diseases (24, 25). Previously, in Pakistan, the literature had been published regarding awareness and attitudes toward TCV involving a specific and localized population (26). We are conducting this study among the general population of Pakistan to assess the knowledge, attitude, and practices regarding TCV and willingness toward the booster dose of TCV.
Materials and methods
Study design and study setting
A cross-sectional, web-based study was conducted among the general population of Pakistan, involving participants from all provinces, from 15 October 2021 to 30 November 2021.
Ethical considerations
Participation in this study was completely voluntary. Before beginning the survey, each participant provided informed consent and was given the option to withdraw from the study at any time before submitting their response. The anonymity of the participants was assured by not collecting any personal information such as name, email, or any other contact information. The review committee of Pir Abdul Qadir Shah Jeelani Institute of Medical Sciences, Gambat, Pakistan, with reference number: IRB/22/13, approved ethical approval for the study. Furthermore, the STROBE checklist is followed to report this study.
Sample size
The population of Pakistan is 227.3 million with a median age of 23.2 years and 51.5 and 48.5% being men and women, respectively, with the literacy rate of 62.3% (27, 28). The online Rao soft calculator [n = NxI ((N–1)E2 + x)] was used to calculate the sample size of the study (29). A minimum sample size of 846 was calculated with a 98% confidence interval, 50% proportion of the population, and 4% margin of error. A total of 918 responses were included with a 96% response rate.
Data collection
A Google® form was used to collect the responses through a convenient sampling method. The questionnaire link was circulated among friends and contacts in multiple social media groups such as WhatsApp and Facebook. Individuals were unable to understand the language of the survey, and non-Pakistani nationals were excluded from the study.
Questionnaire designing
The questionnaire was designed after a substantial literature review (12, 16, 24, 30, 31). It was validated by medical education and public health experts. To assess the relevancy and simplicity of the questionnaire, a pilot study was conducted with 40 individuals from the target population. The questionnaire was comprised of demographic information and questions about knowledge, attitude, and practices regarding TCV. The sociodemographic characteristics include age, gender, education, occupation, residence, marital and employment status, monthly family income, and the number of household individuals. The knowledge section was comprised of action, benefits, availability, cost, source of information, side effects of TCV, and awareness about the TCV vaccination program conducted by the Government of Pakistan. The attitude assessed participants’ beliefs about safety, efficacy, recommendation, and need for TCV for children. Furthermore, attitudes regarding religious beliefs toward vaccines were also inquired. Regarding practices of TCV, vaccination of own child, to comply with the booster dose, and family restrictions regarding vaccine were inquired.
Statistical analysis
The statistical package for social sciences (SPSS) version 21 (IBM) was used for data analysis. Mean and standard deviation were used to present the numerical variables, and for categorical data, frequencies and percentages were used. Depending upon the nature of the variables, inferential analysis was applied. Univariate and multivariate logistic regression analyses of sociodemographic, knowledge, and attitude with willingness for a booster dose of TCV were conducted, and a value of p of <0.05 was considered significant.
Results
Sample characteristics
A total of 918 responses were received with a response rate of 96%. The mean age and number of family members were 25.9 ± 9.6 and 5.9 ± 3.7, respectively. Regarding sociodemographic information, 51% (468) were women, 25.7% (236) were married, and 39.5% (363) were employed. Among the majority of the people, 82.7% (759) belonged to urban areas, 59.6% (547) had graduation-level education, and 60.2% (533) had a monthly family income of more than 50,000 PKR (Table 1).
Table 1
| Variables | Characteristics | Frequency/percentage |
|---|---|---|
| Age (in years) | Mean (SD) | 25.9 (9.6) |
| Gender | Female | 468 (51.0%) |
| Male | 450 (49.0%) | |
| Marital status | Unmarried | 682 (74.3%) |
| Married | 236 (25.7%) | |
| Residence | Rural | 159 (17.3%) |
| Urban | 759 (82.7%) | |
| Monthly family income (PKR) | < 25,000 | 162 (17.6%) |
| 25,000–50,000 | 203 (22.1%) | |
| > 50,000 | 553 (60.2%) | |
| Level of education | No formal education | 25 (2.7%) |
| Primary up to Matric | 68 (7.4%) | |
| Secondary/Intermediate | 191 (20.8%) | |
| Graduate | 547 (59.6%) | |
| Post-graduation | 87 (9.5%) | |
| Number of household members | Mean (SD) | 5.9 (3.7) |
| Employment status | Unemployed | 555 (60.5%) |
| Employed | 363 (39.5%) | |
| Occupation | Healthcare workers | 253 (27.6%) |
| Others/No occupation | 665 (72.4%) |
General characteristics and demographics of the study participants (n = 918).
PKR, Pakistani Rupee; SD, standard deviation.
Assessment of knowledge in the participants
The majority of the people (783) responded that vaccine is used to prevent illness (85.3%), 834 (90.8%) reported that healthy child needs vaccination, 850 (92.6%) reported that vaccine lowers disability and mortality, and 796 (86.7%) reported that typhoid could be prevented by vaccination. In total, 54.2% (498) were aware of TCV, and 52.1% (478) of TCV vaccination programs conducted by the Government of Pakistan. Mass media [35.1% (322)] and healthcare workers [16.2% (149)] were major sources of information. Regarding side effects, fever [462 (50.3%)] and injection site pain and swelling [453 (49.3%)] were considered the most common reactions to TCV (Table 2).
Table 2
| Variables | Characteristics | Frequency (%) |
|---|---|---|
| What do you think vaccination do? | I do not know | 45 (4.9%) |
| It’s just an injection | 22 (2.4%) | |
| It’s used to cure disease | 68 (7.4%) | |
| Prevent illness | 783 (85.3%) | |
| Do you know that even healthy child needs | No | 84 (9.2%) |
| vaccination? | Yes | 834 (90.8%) |
| Do you know vaccination decreases the rates of mortality and disabilities? | No | 68 (7.4%) |
| Yes | 850 (92.6%) | |
| Do you know typhoid could be prevented by | No | 122 (13.3%) |
| vaccination? | Yes | 796 (86.7%) |
| Do you know about Typhoid Conjugate | No | 420 (45.8%) |
| Vaccine? | Yes | 498 (54.2%) |
| Do you know that the government of Pakistan had started typhoid vaccination in different districts of Pakistan? | No | 440 (47.9%) |
| Yes | 478 (52.1%) | |
| How did you come to know about typhoid vaccination? | Doctors and Nurses | 149 (16.2%) |
| Friends And Relatives | 139 (15.1%) | |
| Mass Media (TV/Newspaper) | 322 (35.1%) | |
| Personal knowledge | 126 (13.7%) | |
| I do not know | 182 (19.8%) | |
| Do you know which age group children should get typhoid vaccination? | 0–5 years | 335 (36.5%) |
| 5–13 years | 246 (26.8%) | |
| More than 13 years | 98 (10.7%) | |
| I do not know | 239 (26.0%) | |
| What do you know about booster dose? | Given to cover missed dose | 71 (7.7%) |
| Gives more protection | 667 (72.7%) | |
| I do not know | 180 (19.6%) | |
| Is typhoid vaccine available free in Pakistan or patient bear its price? | Patient bear its price | 208 (22.7%) |
| Typhoid vaccine available free in Pakistan | 498 (54.2%) | |
| I do not know | 212 (23.1%) | |
| What side effects does TCV have? | Fever | 462 (50.3%) |
| Lightheadedness | 187 (20.4%) | |
| Nausea | 173 (18.8%) | |
| Vomiting | 102 (11.1%) | |
| Fainting | 41 (4.5%) | |
| Pain and swelling at injection site | 453 (49.3%) | |
| None | 35 (3.8%) | |
| I do not know | 478 (52.1%) |
Knowledge about typhoid as a disease and vaccination of the study participants (n = 918).
TV, Television; TCV, Typhoid Conjugate Vaccine.
Assessment of the attitude of participants
In total, 77.7% (713) and 80.8% (742) considered TCV safe and effective, respectively, and 91.8% (843) were in favor of vaccination programs designed by healthcare authorities. In total, 92.3% (847) would advise TCV to family and friends, 617 (67.2%) would strongly recommend others to vaccinate their children, and 53.3% (489) followed expert advice for TCV vaccination. Only 21.6% (198) had fear about TCV, and 13.1% (120) considered it a conspiracy theory against Pakistan; however, 623 (67.9%) believed that it may contain contents forbidden by Islamic law (Table 3).
Table 3
| Variables | Characteristics | Frequency (%) |
|---|---|---|
| Are you in favor of obligatory vaccination | No | 75 (8.2%) |
| programs designed by the health authorities? | Yes | 843 (91.8%) |
| Will you advice your relatives and family | No | 71 (7.7%) |
| members to immunize their children? | Yes | 847 (92.3%) |
| Do you believe that typhoid conjugate vaccine is safe? | No | 36 (3.9%) |
| Yes | 713 (77.7%) | |
| I do not know | 169 (18.4%) | |
| Do you believe that typhoid conjugate vaccine is effective for prevention of typhoid fever? | No | 34 (3.7%) |
| Yes | 742 (80.8%) | |
| I do not know | 142 (15.5%) | |
| Will you recommend vaccine to other children? | Discourage taking vaccine | 31 (3.4%) |
| Only if they ask | 142 (15.5%) | |
| Strongly recommend | 617 (67.2%) | |
| No comments | 128 (13.9%) | |
| Will you vaccinate the child if he/she is already sick? | No | 536 (58.4%) |
| Yes | 382 (41.6%) | |
| Do you have any fears about this vaccination? | No | 720 (78.4%) |
| Yes | 198 (21.6%) | |
| What encourages you to get the child vaccinated with Typhoid Conjugate Vaccine? | Advertisements | 28 (3.1%) |
| Expert Advice | 489 (53.3%) | |
| Government Provides Vaccination | 274 (29.8%) | |
| Self-experience | 98 (10.7%) | |
| Will not vaccinate my child | 29 (3.2%) | |
| Would you support it if it is added in Govt. vaccination program? | No | 62 (6.8%) |
| Yes | 856 (93.2%) | |
| Do you think it is an international conspiracy against Pakistani children? | No | 798 (86.9%) |
| Yes | 120 (13.1%) | |
| Do you think it may contain contents forbidden by Islamic law? | No | 199 (21.7%) |
| Yes | 623 (67.9%) | |
| I do not know | 96 (10.5%) |
Attitude of the study participants toward typhoid vaccination (n = 918).
Assessment of practices of participants
Only 389 (42%) participants had children, and 208 (22.7%) had vaccinated their children according to EPI including TCV. In total, 763 (83.1%) would comply with the booster dose, and 829 (90.3%) had family restrictions regarding vaccination. The majority would consult with the doctor for side effects of vaccination [533 (58.1%)], the missed dose of TCV [842 (91.7%)], and the next vaccination [845 (92.0%)] (Table 4).
Table 4
| Variables | Characteristics | Frequency |
|---|---|---|
| Have you given your children the obligatory vaccines including typhoid vaccine? | No | 69 (7.5%) |
| Yes | 208 (22.7%) | |
| Given vaccines other than typhoid | 112 (12.2%) | |
| I have no children | 529 (57.6%) | |
| Was the vaccine from Government Campaign or taken privately? | Government Campaign | 262 (28.5%) |
| Privately | 87 (9.5%) | |
| Not vaccinated | 34 (3.7%) | |
| Not applicable | 535 (58.3%) | |
| Would you comply with a booster dose? | No | 155 (16.9%) |
| Yes | 763 (83.1%) | |
| Do you have family restrictions regarding this vaccine? | No | 89 (9.7%) |
| Yes | 829 (90.3%) | |
| What side effects you think it has?* | Fever | 462 (50.3%) |
| Lightheadedness | 187 (20.4%) | |
| Nausea | 173 (18.8%) | |
| Vomiting | 102 (11.1%) | |
| Fainting | 41 (4.5%) | |
| Pain and swelling at injection site | 453 (49.3%) | |
| None | 35 (3.8%) | |
| I do not know | 478 (52.1%) | |
| What would you do if the child experience any of the side effect following vaccination? | Believe that vaccination is working | 115 (12.5%) |
| Consult a doctor | 533 (58.1%) | |
| Give fever medication at home | 197 (21.5%) | |
| Stop giving the vaccination | 26 (2.8%) | |
| I do not know | 187 (20.4%) | |
| Who would you contact if the child missed the dose? | Doctor | 842 (91.7%) |
| Nurse | 16 (1.7%) | |
| Pharmacist | 21 (2.3%) | |
| Family or friends | 14 (1.5%) | |
| Handle myself | 25 (2.7%) | |
| Who will you contact for next vaccination? | Doctor | 845 (92.0%) |
| Nurse | 23 (2.5%) | |
| Pharmacist | 28 (3.1%) | |
| Family or friends | 22 (2.4%) |
Practice of study participants toward typhoid vaccination (n = 918).
*This question had multiple options to choose with.
Regression analysis of factors associated with willingness for a booster dose of typhoid vaccine
Being married has a significant association with willingness for a booster dose of TCV [crude odds ratio (COR) = 0.285, value of p < 0.001; adjusted odds ratio (aOR) = 0.562, value of p =0.038]. Participants with a monthly family income of more than 50,000 PKR have higher OR than those with lower income (COR = 4.920, value of p <0.01; aOR = 2.853, value of p < 0.001). Based on univariate and multivariate analyses, a negative attitude regarding the protective effect of TCV has less willingness toward the booster dose with statistical significance (COR = 0.388, value of p = 0.017; aOR = 0.198, value of p = 0.011) (Table 5).
Table 5
| Variables | Univariate | p-value | Multivariate | p-value |
|---|---|---|---|---|
| Gender | ||||
| Male | 1.000 | - | 1.000 | – |
| Female | 1.652 (1.163–2.346) | 0.005* | 1.132 (0.735–1.744) | 0.573 |
| Age groups | ||||
| ≤20 years (n = 199) | 3.658 (1.738–7.702) | 0.001* | 0.875 (0.307–2.497) | 0.803 |
| 21–30 years (n = 574) | 5.236 (2.624–10.448) | <0.001* | 1.520 (0.606–3.815) | 0.372 |
| 31–50 years (n = 107) | 1.434 (0.672–3.063) | 0.351 | 0.968 (0.402–2.331) | 0.942 |
| >50 years (n = 38) | 1.000 | - | 1.000 | - |
| Marital status | ||||
| Unmarried | 1.000 | - | 1.000 | - |
| Married | 0.285 (0.199–0.409) | <0.001* | 0.562 (0.326–0.969) | 0.038* |
| Residence | ||||
| Urban | 1.000 | - | 1.000 | - |
| Rural | 0.255 (0.173–0.376) | <0.001* | 0.673 (0.403–1.124) | 0.130 |
| Monthly family income (PKR) | ||||
| < 25,000 | 1.000 | - | 1.000 | - |
| 25,000–50,000 | 1.090 (0.694–1.710) | 0.709 | 0.826 (0.496–1.374) | 0.461 |
| > 50,000 | 4.920 (3.138–7.714) | <0.001* | 2.853 (1.655–4.916) | <0.001* |
| Number of household members | ||||
| 1–2 (n = 56) | 2.036 (0.874–4.740) | 0.099 | 2.133 (0.850–5.354) | 0.107 |
| 3–4 (n = 195) | 1.890 (1.138–3.140) | 0.014* | 1.414 (0.795–2.516) | 0.239 |
| 5–6 (n = 414) | 1.561 (1.050–2.321) | 0.028* | 1.066 (0.675–1.684) | 0.784 |
| >6 (n = 253) | 1.000 | - | 1.000 | - |
| Level of Education | ||||
| No formal education | 0.250 (0.099–0.634) | 0.003* | 0.692 (0.221–2.165) | 0.526 |
| Primary up to Matric | 0.514 (0.257–1.028) | 0.060 | 1.382 (0.618–3.093) | 0.431 |
| Secondary/Intermediate | 2.214 (1.154–4.247) | 0.017* | 2.013 (0.942–4.305) | 0.071 |
| Graduate | 2.168 (1.249–3.763) | 0.006* | 1.370 (0.729–2.576) | 0.328 |
| Post-graduation | 1.000 | - | 1.000 | - |
| Employment status | ||||
| Employed | 0.589 (0.416–0.833) | 0.003* | 1.024 (0.634–1.653) | 0.923 |
| Unemployed | 1.000 | - | 1.000 | - |
| Occupation | ||||
| Healthcare workers | 3.635 (2.147–6.155) | <0.001* | 2.339 (1.314–4.163) | 0.004* |
| Others/No occupation | 1.000 | - | 1.000 | - |
| Do you know typhoid could be prevented by vaccination? | ||||
| No | 0.146 (0.097–0.222) | <0.001* | 0.337 (0.196–0.580) | <0.001* |
| Yes | 1.000 | - | 1.000 | - |
| Do you know that Government of Pakistan have started typhoid vaccine drive? | ||||
| No | 0.505 (0.354–0.719) | <0.001* | 0.667 (0.421–1.056) | 0.084 |
| Yes | 1.000 | - | 1.000 | - |
| Do you believe that typhoid conjugate vaccine is safe? | ||||
| No | 0.790 (0.384–1.627) | 0.523 | 1.595 (0.756–3.366) | 0.267 |
| Yes | 6.707 (4.518–9.957) | <0.001* | 2.078 (0.571–7.566) | 0.220 |
| I do not know | 1.000 | - | 1.000 | - |
| Do you believe that typhoid conjugate vaccine is effective for prevention of typhoid fever? | ||||
| No | 0.388 (0.178–0.845) | 0.017* | 0.198 (0.057–0.688) | 0.011* |
| Yes | 6.417 (4.254–9.680) | <0.001* | 1.379 (0.686–2.771) | 0.367 |
| I do not know | 1.000 | - | 1.000 | - |
| Do you have any fears about this vaccination? | ||||
| No | 2.965 (2.045–4.299) | <0.001* | 1.117 (0.672–1.856) | 0.670 |
| Yes | 1.000 | - | 1.000 | - |
| Do you think it is an international conspiracy against Pakistani children? | ||||
| No | 1.000 | - | 1.000 | - |
| Yes | 0.389 (0.252–0.601) | <0.001* | 0.979 (0.496–1.933) | 0.952 |
| Do you think it may contain contents forbidden by Islamic law? | ||||
| No | 6.642 (4.437–9.943) | <0.001* | 1.988 (1.060–3.728) | 0.032* |
| Yes | 1.469 (0.869–2.484) | 0.151 | 0.968 (0.427–2.196) | 0.939 |
| I do not know | 1.000 | - | 1.000 | - |
Regression analysis of factors associated with willingness for booster dose of typhoid vaccine.
PKR, Pakistani Rupee. Significant p-values are denoted by *. The dependent variable compliance with a booster dose of typhoid vaccine has been responded to as ‘Yes’.
Discussion
Typhoid conjugate vaccine (TCV) had been proven effective in reducing the burden of S. typhi-induced morbidity and mortality, especially in regions with XDR S. typhi. The routine TCV vaccination prevents antimicrobial resistance and misusage of antibiotics. This study assessed the knowledge, attitude, and practices of the general population of Pakistan regarding TCV. In total, 85.3% of our study population responded that vaccines prevent illnesses consistent with the study by Sankar et al. that 91.86% responded as vaccines provide prevention against illnesses (30). Only 54.2% of participants were aware of TCV being lower than the study by Hanif et al. as 75% of the sample population knew about TCV in Sindh, Pakistan (21). It can be attributed to the possibility that Hanif et al. had conducted the study in the vicinity of the vaccination center having the probability of raising consciousness and awareness about the vaccines.
Mass media (35.1%) and doctors and nurses (16.1%) followed by friends and relatives are the major sources of information for TCV while Debnath et al. had reported that healthcare workers (39.2%), mass media (25.6%), and relatives (12.8%) are the sources of knowledge for vaccines and vaccine-preventable diseases (31). Humans are now living in the era of mass and social media, and people depend on technological services even for basic daily needs making it the major source of information (23, 32). Social media campaigns had been proven effective in promoting awareness about health information such as their appeal, broad coverage, rapid provision, and cost-effectiveness (33).
The majority of the participants have a positive attitude toward TCV, as it was considered safe and effective by 77.7 and 80.8%, respectively. Memon et al. depicted that 75.7 and 87% believed that TCV is safe and effective, respectively (26). However, participants responded that TCV may contain contents forbidden by Islamic law (67.9%), have fear about the vaccine (21.6%), and is an international conspiracy against Pakistan (13.1%). Memon et al. reported that TCV is an international conspiracy against Pakistani children (73.5%), harmful (24.3%), and may have harmful contents (11.4%), and 92% would accept the vaccine if their issues and concerns were answered (26). Previously, religious leaders had spread the idea that polio vaccination will cause vaccine-induced infertility. Similarly, for the COVID-19 vaccine, people believed that it will make the population sterile, or the person getting vaccinated will die in 2 years (18). Similarly, the assumptions had been made against the other vaccines as TCV being comprised of harmful contents and would have hazardous effects on human health in the long run.
The advice from an expert (53.3%) and the provision of vaccination by the government (29.8%) would encourage the participants to vaccinate the children with TCV. Tahir et al. reported that the compulsion of vaccination by the government (48.06%) and the recommendation by the doctor (39.37%) are the reasons leading to vaccination against COVID-19 (12).
Healthcare workers are the most significant and trustworthy source of knowledge to the public for disease prevention and treatment, especially immunization, educating about the benefits of vaccination, and myths prevalent about the vaccine in society. Therefore, good communication between HCWs and the general population would promote vaccination and encourage them to vaccinate themselves and others in society (26). Majority, would consult a doctor for the missed dose of vaccine (58.1 %) and for side effects of vaccine (91.7%), and for the next vaccination (92.0%) corresponding with Sankar et al. as 70.2 and 29% would contact a doctor and nurse, respectively, for a missed dose of vaccine (30).
The higher income, education level, and less number of household members had more willingness for a booster dose of TCV. The higher income level contributes more to the affordability of medical treatments and utilizes available health facilities for healthy living and protection against diseases (34). Similarly, a higher education level raises awareness and knowledge regarding healthcare and reduces false beliefs resulting in a positive attitude toward the prevention and treatment of diseases and a willingness for vaccination. Older age, higher level of the perceived threat from the diseases, and positive attitude toward the vaccine are other factors contributing to the willingness for vaccination (35). The sociodemographic groups with low levels of education and income had lower willingness toward vaccination suggesting the modification in strategies to overcome the social inequalities to provide equal opportunities to vaccinate (36).
Limitations of the study
This study, however, would have some limitations. First, convenient sampling was utilized for which there would be chances of selection bias. It was an online survey, and people with the facility to the Internet had only participated in the study. Second, this study would have recall bias. Third, compared to Pakistan’s overall population, our sample size was more educated, wealthier, and more urban. Finally, despite the fact that the replies were anonymous because the study was self-reported, participants may have felt under pressure to adopt the favorable attitudes and perceptions that were socially acceptable. This study calls for additional research focused on the population residing in rural areas and with low education levels.
Conclusion
The general population of Pakistan had knowledge about the benefits of vaccination and the role of booster doses but was found to be lacking regarding the provision of TCV by the government in the country and its effectiveness against typhoid fever. The attitude and practices were reported to be in favor of promoting vaccination, but some false religious and national beliefs are also prevalent demanding the need to be addressed. People will also comply with the booster dose of TCV, indicating the awareness of the general population about the importance of completing a treatment course of vaccine for disease prevention. Furthermore, healthcare authorities, media, and government professionals should collaborate to conduct seminars and campaigns on domestic and national levels and should utilize electronic and print media to make an effort to address negative views about immunization and raise awareness about the disease, its adversities, mode of transmission, and the role of vaccines in the prevention of diseases and saving human lives.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Pir Abdul Qadir Shah Jeelani Institute of Medical Sciences, Gambat. The patients/participants provided their written informed consent to participate in this study.
Author contributions
IU, MT, and MS conceived the idea. MZ, JS, and UF collected the data. MA analyzed and interpreted the data. MZ, MT, JS, WT, FA, RI, UF, and AA performed write-up of the manuscript. AA, MA, MT, WT, KU, and MS reviewed the manuscript for intellectual content critically. All authors approved the final version of the manuscript.
Acknowledgments
The authors are thankful to all the participants who voluntarily contributed to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Qamar FN Yousafzai MT Khaliq A Karim S Memon H Junejo A et al . Adverse events following immunization with typhoid conjugate vaccine in an outbreak setting in Hyderabad, Pakistan. Vaccine. (2020) 38:3518–23. doi: 10.1016/j.vaccine.2020.03.028
2.
Kim J-H Im J Parajulee P Holm M Cruz Espinoza LM Poudyal N et al . A systematic review of typhoid fever occurrence in Africa. Clin Infect Dis. (2019) 69:S492–8. doi: 10.1093/cid/ciz525
3.
Garrett DO Longley AT Aiemjoy K Yousafzai MT Hemlock C Yu AT et al . Incidence of typhoid and paratyphoid fever in Bangladesh, Nepal, and Pakistan: results of the surveillance for enteric fever in Asia project. Lancet Glob Health. (2022) 10:e978–88. doi: 10.1016/S2214-109X(22)00119-X
4.
Organization WH . Health topics-typhoid. Available at: https://www.who.int/health-topics/typhoid#tab=tab_1
5.
Stanaway JD Reiner RC Blacker BF Goldberg EM Khalil IA Troeger CE et al . The global burden of typhoid and paratyphoid fevers: a systematic analysis for the global burden of disease study 2017. Lancet Infect Dis. (2019) 19:369–81. doi: 10.1016/S1473-3099(18)30685-6
6.
Browne AJ Kashef Hamadani BH Kumaran EA Rao P Longbottom J Harriss E et al . Drug-resistant enteric fever worldwide, 1990 to 2018: a systematic review and meta-analysis. BMC Med. (2020) 18:1–22. doi: 10.1186/s12916-019-1443-1
7.
Klemm EJ Shakoor S Page AJ Qamar FN Judge K Saeed DK et al . Emergence of an extensively drug-resistant Salmonella enterica serovar Typhi clone harboring a promiscuous plasmid encoding resistance to fluoroquinolones and third-generation cephalosporins. MBio. (2018) 9:e00105–18. doi: 10.1128/mBio.00105-18
8.
Jabeen K Saleem S Nizamuddin S Arshad F Jahan S Hasnain F et al . Reporting of azithromycin activity against clinical isolates of extensively drug-resistant Salmonella enterica Serovar Typhi. Am J Trop Med Hyg. (2023) 108:942–7. doi: 10.4269/ajtmh.22-0557
9.
Nizamuddin S Ching C Kamal R Zaman MH Sultan F . Continued outbreak of ceftriaxone-resistant Salmonella enterica serotype Typhi across Pakistan and assessment of knowledge and practices among healthcare workers. Am J Trop Med Hyg. (2021) 104:1265–70. doi: 10.4269/ajtmh.20-0783
10.
Khan EA . XDR typhoid: the problem and its solution. J Ayub Med Coll Abbottabad. (2019) 31:139–40.
11.
Ahmad S Tsagkaris C Aborode AT Haque MTU Khan SI Khawaja UA et al . A skeleton in the closet: the implications of COVID-19 on XDR strain of typhoid in Pakistan. Public Health in Prac. (2021) 2:100084. doi: 10.1016/j.puhip.2021.100084
12.
Tahir MJ Saqlain M Tariq W Waheed S Tan SH Nasir SI et al . Population preferences and attitudes towards COVID-19 vaccination: a cross-sectional study from Pakistan. BMC Public Health. (2021) 21:1–12. doi: 10.1186/s12889-021-11814-5
13.
Ahmed A Dujaili J Sandhu AK Hashmi FK . Concerns of HIV-positive migrant workers in COVID-19 pandemic: a call for action. Journal of. Glob Health. (2020) 10:342. doi: 10.7189/jogh.10.020342
14.
Oberman E. (2022). Reaching every child in Pakistan: TCV rolls out to remaining provinces completing nationwide introduction 2175 K street, NW, suite 400 Washington, DC 20037: Coalition Against Typhoid. Available at: https://www.coalitionagainsttyphoid.org/reaching-every-child-in-pakistan-tcv-rolls-out-to-remaining-provinces-completing-nationwide-introduction/ (Accessed May 18, 2022).
15.
Aslam F Yue Y Aziz M . Introduction of typhoid vaccine in the expanded immunization program of Pakistan. Hum Vaccin Immunother. (2021) 17:2132. doi: 10.1080/21645515.2020.1869496
16.
Pinna C Kaewkungwal J Hattasingh W Swaddiwudhipong W Methakulchart R Moungsookjareoun A et al . Evaluation of immunization Services for Children of migrant workers along Thailand–Myanmar border: compliance with global vaccine action plan (2011–2020). Vaccine. (2020) 8:68. doi: 10.3390/vaccines8010068
17.
Thangaraju P Venkatesan S . WHO ten threats to global health in 2019: antimicrobial resistance. Cukurova Med J. (2019) 44:1150–1. doi: 10.17826/cumj.514157
18.
Rutten LJF Zhu X Leppin AL Ridgeway JL Swift MD Griffin JM et al . Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clin Proc. (2021) 96:699–707. doi: 10.1016/j.mayocp.2020.12.024
19.
Sallam M . COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccine. (2021) 9:160. doi: 10.3390/vaccines9020160
20.
McKee C Bohannon K . Exploring the reasons behind parental refusal of vaccines. J Pediatric Pharmacol Therap. (2016) 21:104–9. doi: 10.5863/1551-6776-21.2.104
21.
Butt M Mohammed R Butt E Butt S Xiang J . Why have immunization efforts in Pakistan failed to achieve global standards of vaccination uptake and infectious disease control?Risk Manag Healthcare Policy. (2020) 13:111–24. doi: 10.2147/RMHP.S211170
22.
Jamal D Zaidi S Husain S Orr DW Riaz A Farrukhi AA et al . Low vaccination in rural Sindh, Pakistan: a case of refusal, ignorance or access?Vaccine. (2020) 38:4747–54. doi: 10.1016/j.vaccine.2020.05.018
23.
Junaid Tahir M Tariq W Anas Tahseen Asar M Irfan Malik M Kamal Akhtar F Malik M et al . Psychological impact of COVID-19 on doctors and medical students of Punjab, Pakistan: a logistic regression analysis. J Multidiscip Healthc. (2022) 15:1297–308. doi: 10.2147/JMDH.S369452
24.
Mogasale VV Ramani E Mogasale V Park JY Wierzba TF . Estimating typhoid fever risk associated with lack of access to safe water: a systematic literature review. J Environ Public Health. (2018) 2018:1–14. doi: 10.1155/2018/9589208
25.
Tavolacci MP Dechelotte P Ladner J . COVID-19 vaccine acceptance, hesitancy, and resistancy among university students in France. Vaccine. (2021) 9:654. doi: 10.3390/vaccines9060654
26.
Memon MH Saeed F Iqbal M Khan MA . Opinion of parents regarding conjugate typhoid vaccine. Annals Abbasi Shaheed Hospital Karachi Med Dent Coll. (2020) 25:144–50. doi: 10.58397/ashkmdc.v25i3.244
27.
Kemp S. (2022). Digital 2022: Pakistan: Datareportal. Available at: https://datareportal.com/reports/digital-2022-pakistan#:~:text=Pakistan%27s%20population%20in%202022&text=48.5%20percent%20of%20Pakistan%27s%20population,percent%20lived%20in%20rural%20areas (Accessed January 20, 2023).
28.
Training MoFEaP . Adult Literacy: Goverment of Pakistan. Available at: http://mofept.gov.pk/ProjectDetail/NjQ4ZTg2NjItOWM2NC00Y2IxLTkzMDgtMjU2OTFhMjA4NzNh (Accessed January 20, 2023).
29.
Raosoft . Sample size calculator. Available at: http://www.raosoft.com/samplesize.html (Accessed January 20, 2023).
30.
Sankar BK Rameh S Sunny A . A study to assess and correlate the knowledge, attitude and practices of vaccination among mothers with educational status in a teaching hospital in South India. Primary Health Care Open Access. (2018) 8:1–6. doi: 10.4172/2167-1079.1000290
31.
Debnath M Golui P Roychoudhury N Sarkar S . A cross-sectional study on mothers’ knowledge, attitude and practice regarding the vaccines given at the routine immunisation clinic of a tertiary care hospital in West Bengal. J Undergraduate Med Res. (2022) 4:31–40.
32.
Kumar G Shardha HK Tariq W Qazi MA Kumar K Maheshwari C et al . Assessment of knowledge and attitude of healthcare professionals regarding the use of telemedicine: a cross-sectional study from rural areas of Sindh, Pakistan. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.967440
33.
Gomez Bravo R Gomez Bravo M Lygidakis C Vögele C . Social media as an opportunity for public health interventions: the# Metoo movement as an exemplar. J Int Soc Telemed eHealth. (2019) 7:1–7. doi: 10.29086/JISfTeH.7.e5
34.
Baumgaertner B Ridenhour BJ Justwan F Carlisle JE Miller CR . Risk of disease and willingness to vaccinate in the United States: a population-based survey. PLoS Med. (2020) 17:e1003354. doi: 10.1371/journal.pmed.1003354
35.
Galanis P Vraka I Siskou O Konstantakopoulou O Katsiroumpa A Kaitelidou D . Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. (2022) 157:106994. doi: 10.1016/j.ypmed.2022.106994
36.
Abedin M Islam MA Rahman FN Reza HM Hossain MZ Hossain MA et al . Willingness to vaccinate against COVID-19 among Bangladeshi adults: understanding the strategies to optimize vaccination coverage. PLoS One. (2021) 16:e0250495. doi: 10.1371/journal.pone.0250495
Summary
Keywords
typhoid fever, enteric fever, extended drug resistance, willingness, booster dose
Citation
Tahir MJ, Zaman M, Saffi J, Asghar MS, Tariq W, Ahmed F, Islam R, Farooqui US, Ullah I, Saqlain M, Ullah K and Ahmed A (2023) Knowledge, attitudes, and practices of the general population of Pakistan regarding typhoid conjugate vaccine: findings of a cross-sectional study. Front. Public Health 11:1151936. doi: 10.3389/fpubh.2023.1151936
Received
27 January 2023
Accepted
28 April 2023
Published
02 June 2023
Volume
11 - 2023
Edited by
Saba Tufail, Aligarh Muslim University, India
Reviewed by
Hemant Khuntia, Siksha O Anusandhan University, India; Carlos Mier-Aguilar, University of Alabama at Birmingham, United States
Updates
Copyright
© 2023 Tahir, Zaman, Saffi, Asghar, Tariq, Ahmed, Islam, Farooqui, Ullah, Saqlain, Ullah and Ahmed.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muhammad Sohaib Asghar, sohaib_asghar123@yahoo.com
†ORCID: Muhammad Junaid Tahirhttps://orcid.org/0000-0002-0335-6681Muhammad Sohaib Asghar https://orcid.org/0000-0001-6705-2030Waleed Tariq https://orcid.org/0000-0001-8480-2710Faizan Ahmed https://orcid.org/0000-0002-3816-6175Rabia Islam https://orcid.org/0000-0001-6664-3613Usman Shakeel Farooqui https://orcid.org/0000-0002-3443-1912Irfan Ullah https://orcid.org/0000-0003-1100-101XMuhammad Saqlain https://orcid.org/0000-0002-5966-4165Ali Ahmed https://orcid.org/0000-0002-8964-1853
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.